A healthy, balanced diet
What is a healthy balanced diet.
The key to a healthy eating is having a balance of different foods and nutrients in your diet.
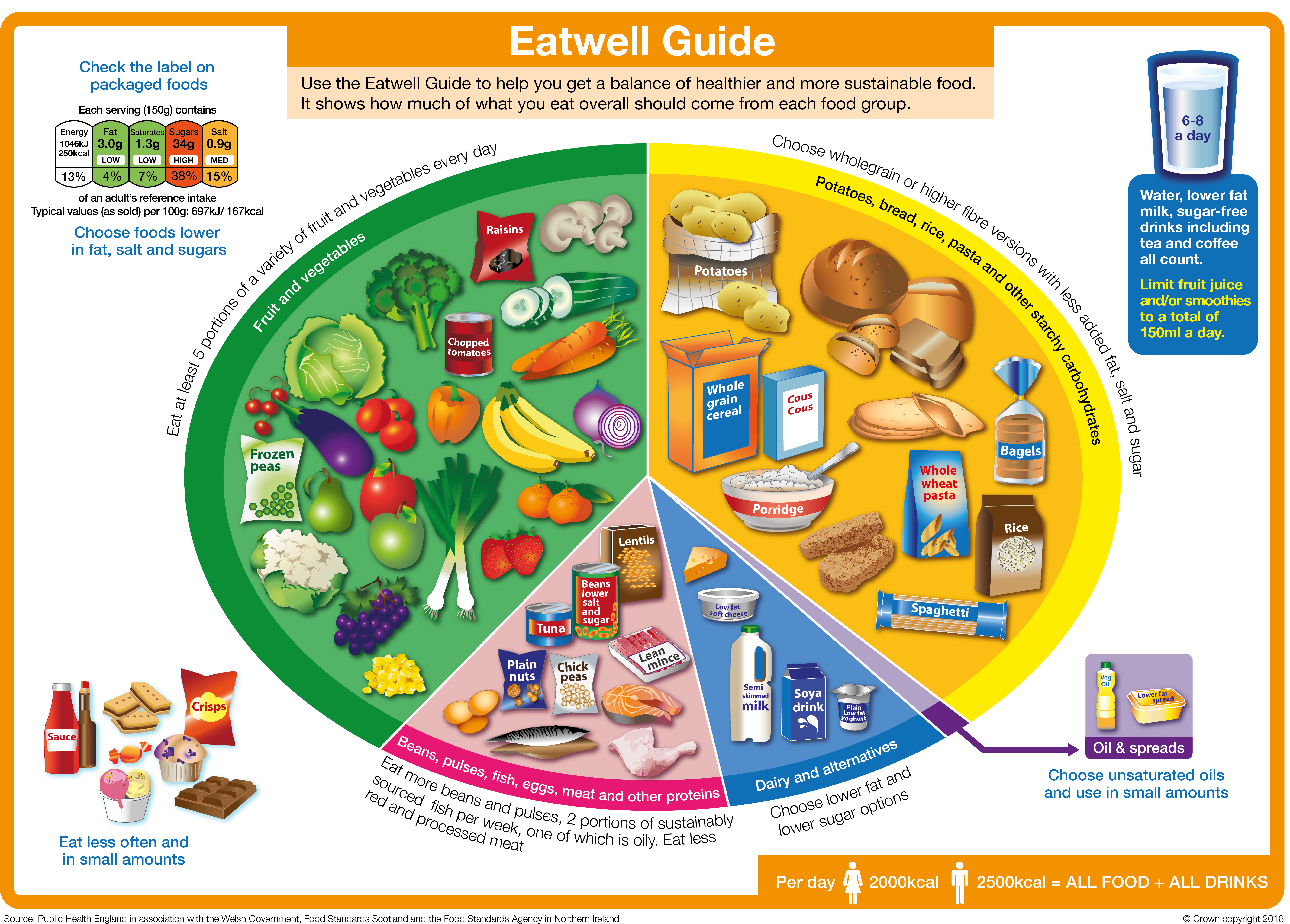
In the UK, the healthy eating model is called the Eatwell Guide .
There are a range of different types of eating (e.g. vegan and vegetarian) but the key principles of a healthy dietary pattern should run through all of these.

The six principles of healthy eating
Although there is no ‘one size fits all’ healthy diet, there are six principles we recommend.

At least 5 A DAY
Remember to include at least five portions of fruit and vegetables a day.

Include plenty of fibre-rich foods, especially wholegrains.

Include a range of protein foods, especially beans, peas & lentils.

Dairy and alternatives
Include some dairy foods or fortified alternatives.

Choose the right fats
Mainly unsaturated fats and oils.

Eat fewer foods and drinks that are high in fat, salt and sugars.
Key facts about healthy, balanced diets
- Fruit and vegetables are a key part of a healthy diet , and we should aim to get our 5 A DAY.
- Starchy foods like bread, potatoes, pasta, rice and other grains are part of a healthy diet , but the quality of what we choose is important.
- Plant-based protein foods , like beans and lentils, are naturally low in saturated fat and are sources of protein and fibre . We should aim to include these regularly in the diet.
- Animal protein foods like fish, eggs, meat and dairy provide a range of vitamins and minerals .
- Dairy foods provide protein, calcium, B vitamins and iodine .If choosing plant-based dairy alternatives, then look for those that are fortified with calcium and ideally other vitamins and minerals.

Why do I need a balanced diet?
Following a healthy, balanced diet helps make sure that our bodies get all the nutrients needed to work well and feel good. There’s plenty of evidence that shows eating healthily can also reduce the risk of diseases like heart disease, stroke, type 2 diabetes and some types of cancer.
Around the world, governments provide guidance on the balance of foods and drinks that make up a healthy diet. The guidelines vary in how they are presented but the message is similar; a healthy diet is about getting a balance and variety of foods from the main food groups.
What are the current healthy eating guidelines in the UK?
In the UK, our healthy eating model is called the Eatwell Guide. The guide has been developed scientifically, using modelling to look at the balance of different foods and drinks that provides the nutrients the body needs in the recommended amounts .
The Eatwell Guide shows the proportions that each of the food groups should make up in our diet and is designed to apply to most of us (although not to children under 2 years old as their dietary needs are different).
You can learn more about the Eatwell Guide on this page from the NHS .
The main food groups that feature in the Eatwell Guide, are outlined below. Each section has a useful guide to that food group.
- Fruit and vegetables
- Starchy foods
- Protein foods
- Dairy foods and alternatives
- Fats and oils
- Foods high in fat, salt and sugar
Fruit and vegetables - eat more!
The fruit and vegetables group is the biggest in the Eatwell Guide and we are recommended to eat at least 5 A DAY. Diets high in fruit and vegetables are linked to a lower risk of diseases like heart disease, stroke and some types of cancer.
Fruit and vegetables provide a range of essential nutrients and fibre, as well as chemical compounds that occur naturally in plants that may have health benefits. Fruit and vegetables can also help you maintain a healthy weight as they are generally low in calories, so you can have plenty for relatively few calories.
Only 1 in 3 adults and 1 in 10 11-18 year olds are getting their 5 A DAY
Helena Gibson-Moore, Nutrition Scientist, British Nutrition Foundation
To get the most nutritional benefit out of your 5 A DAY it’s important to have a variety of fruits and vegetables. This is because different types and colours of fruits and vegetables contain different combinations of important nutrients such as:
- Vitamin C - important for keeping body tissues, such as skin and cartilage healthy.
- Vitamin A - important for normal vision, skin and the immune system.
- Folate - important for making red blood cells and supporting the immune system
- Potassium – important for healthy blood pressure and to support the nervous system
- Fibre – helps to maintain a healthy gut and can reduce the risk of diseases like type 2 diabetes and heart disease.
Did you know? Fresh, frozen, dried and canned fruits and vegetables all count towards our 5 A DAY.
Table 1: 5 A DAY. What counts as a portion?
You can find out more about 5 A DAY portion sizes by reading this NHS page .
5 Top Tips For Eating More Fruit & Vegetables
- Add fresh or dried fruit to breakfast cereal or porridge
- Snack on fresh fruit or vegetable sticks
- Experiment with salads – you could try using red cabbage, adding brightly coloured vegetables such as grated carrot or sliced pepper and including leftover cooked vegetables like broccoli or peas in your salads.
- Add plenty of vegetables to dishes like pasta sauces, stews or curries – frozen or canned vegetables can be a quick and easy way to do this.
- Try fruit-based puddings like fruit salad or canned/dried fruits with plain yogurt
Starchy foods - go for wholegrain and higher fibre!
Also known as ‘carbs,’ starchy foods like bread, pasta, potatoes, rice and other grains are one of the main food groups included in healthy dietary guidelines all over the world.
These foods are sometimes (incorrectly) thought of as ‘fattening’ but what’s important is the types and portion sizes we eat
Sara Stanner, Science Director, British Nutrition Foundation
Starchy foods are a key source of fibre as well as vitamins and minerals such as iron, calcium, folate and B vitamins. For a healthier diet, we should choose more wholegrains and higher fibre starchy foods, such as wholemeal breads, wholemeal pasta, wholegrain breakfast cereals or oats and potatoes with skins.
Top tip! Try swapping white versions of bread, pasta or rice for wholegrain versions, go for wholegrains cereals or oats and try other types of wholegrains such as bulgur wheat, quinoa, freekeh, barley and spelt.
Looking for more information? Download: A guide to the food group 'Potatoes, bread, rice, pasta and other starchy carbohydrates'.
Protein foods - variety is key.
In the Eatwell Guide, this food group is called ‘Beans, pulses, fish, eggs, meat and other proteins'. This group of foods are a source of protein as well as other vitamins and minerals. It is a good idea to eat a variety of different types, and to include more plant-based sources of protein, such as beans, lentils or chickpeas, as these are higher in fibre and naturally low in fat.
Nuts and seeds (plain, unsalted) are included in this food group and contain vitamins, minerals and fibre. They are also high in fat but the majority of this is ‘healthier’ fat (unsaturated) and are a nutritious option in moderation (keeping portion sizes to just a small handful).
It’s recommended that we eat at least two portions (2 x 140g cooked weight) per week of sustainably sourced fish (fresh, frozen or canned), including a portion of oily fish. Oily fish includes salmon, sardines, mackerel and trout. Fish are sources of lots of vitamins and minerals. In particular, oily fish are natural sources of vitamin D and are the richest source of a special type of fat called long chain omega-3’s, which may help to prevent heart disease.
Meat can be part of a healthy diet and can be a source of several vitamins and minerals including iron, zinc and selenium. We are advised not to eat too much red or processed meat as high consumption has been linked with a higher risk of bowel cancer. You can cut down the fat content of meat by choosing leaner cuts such as lower fat mince, cutting off visible fat and taking the skin off poultry and using less fat when cooking, such as grilling instead of frying.
Looking for more information? Download: Beans, pulses, fish, eggs, meat and other proteins
Dairy foods and alternatives – go for lower sugar.
This food group includes milk, yogurt and cheese as well as plant-based alternatives to these. Dairy foods are an important source of calcium as well as protein, iodine and B vitamins. The nutritional content of dairy alternatives varies depending on what they are made from (such as soya, rice or oats) and whether they are fortified. If having dairy alternatives such as soya or oat milk, it’s best to choose those that are fortified with calcium and ideally other vitamins and minerals.
Dairy foods contain saturated fat, which we’re advised to eat less of (see below). Some studies suggest that despite their saturated fat content, dairy foods like milk, cheese and yogurt have a neutral effect on heart health. However, lower-fat versions of milk, cheese and plain yogurt are also lower in energy (calories) and so can be helpful if you are trying to manage your weight.
Fats and oils - choose unsaturated types!
There are different types of fats and oils in the diet – those that are mostly saturated such as butter, coconut oil, ghee, lard and palm oil, and those that are mostly unsaturated such as vegetable (usually rapeseed), sunflower and olive oils and spreads made from these. High intakes of saturated fat are linked to higher blood cholesterol and swapping saturated for unsaturated fats has been shown to reduce blood cholesterol and risk of heart disease. So it is a good idea to choose unsaturated fats and oils most of the time for cooking and spreading.
All fats are high in calories, even unsaturated fats, so it is important to use them in small amounts to avoid adding more calories than you need.
Looking for more information? Download: A guide to oils and spreads in the diet
Foods high in fat, salt and sugar – keep portions small.
Foods high in saturated fat, salt and sugar such as crisps, sweets, biscuits, cakes, chocolate and sugary drinks are not within the main food groups of the Eatwell Guide as they are not needed as part of a healthy diet. Sometimes called ‘treat foods’ we probably all know that these are foods to eat less of. If you do include them, then it is best to have small portions – for example, those that provide about 100-150kcal such as a small chocolate biscuit bar, 4 small squares of chocolate, 2 small biscuits, a small multipack bag of crisps, a mini muffin or a small chocolate mousse.
When it comes to sugary drinks it is best to swap these for water or sugar free versions.
What is the healthy eating guidance for different dietary patterns ?
The main food groups above are the building blocks of a healthy, balanced diet but they can be put together in different ways, based on our culture, preferences and dietary requirements. There are a whole range of different types of eating but the key principles of a healthy dietary pattern run through all of these
Applying these principles to your diet will help make sure it is balanced and healthy. There are a whole range of diets out there in books, in the press and on social media, some of which claim to have specific effects on health or to help with weight loss. It is not always easy to work out whether these diets are healthy – they may be promoted by doctors or mention scientific studies.
Diets that do not follow the healthy eating principles, for example those that cut out whole food groups, are probably going to be difficult to stick with and not likely to be good for your health in the longer term.
Zoe Hill, Nutrition Scientist, British Nutrition Foundation
The Mediterranean diet
The Mediterranean diet is often thought of as one of the healthiest eating patterns and features plenty of fruit, vegetables, pulses, wholegrains, olive oil, fish and smaller amounts of meat, dairy, eggs and sugary foods. A Mediterranean diet contains a higher proportion of fat than other healthy eating patterns, but most of this is unsaturated fats from olive oil, nuts and seeds and oily fish. This style of eating may reduce the risk of heart disease and have other potential health benefits. If this way of eating works for you then that’s great! However, it is not the only way to eat healthily, and may not work for everyone.
Vegetarian and vegan diets
Vegetarian and vegan diets have had a lot of interest and some research suggests that these diets may reduce the risk of heart disease. A healthy, balanced vegetarian or vegan diet will typically provide plenty of vegetables, pulses and wholegrains and so be rich in fibre and low in saturated fat.
Looking for more information? Read our page on vegetarian and vegan diets to find out more.
Plant-based diets.
The term ‘plant-based diet’ is increasingly popular but there is some confusion about what it means. Some people think this refers to a vegetarian or vegan diet, but many authoritative bodies agree that plant-based eating means proportionately choosing more of your foods from plant sources and so is a diet mainly made up of plant foods, but may still include some meat, fish, eggs and dairy foods. Most healthy eating guidelines, including the Eatwell Guide recommend a mainly plant-based diet. The two biggest food groups; fruit and vegetables and starchy foods, are both plant-based and we are also encouraged to eat more beans and pulses and to use plant-based oils and spreads. So you can make your diet more ‘plant-based’ by including a wider variety of fruits and vegetables, including wholegrains as well as choosing more plant-based sources of protein.
Looking for more information? Read our information on how to put a healthy diet into practice including planners, tips and information on portion sizes.
At a glance:.
- Research looking at the relationship between diet and health outcomes has shown a positive relationship between healthier dietary patterns and better health outcomes.
- To help people achieve a healthy balanced diet, governments around the world have developed food-based dietary guidance to illustrate what a healthy diet means in practice.
- Food-based dietary guidelines around the world vary in their presentation and format but the messages about the characteristics of healthy and balanced diets are relatively consistent.
- The UK Eatwell Guide was developed using optimisation modelling to find the proportions of the main food groups needed to fulfil current dietary recommendations.
- It has been estimated that following a dietary pattern consistent with the Eatwell Guide would benefit population health as well as being more environmentally sustainable.

What are dietary guidelines?
While nutrition recommendations often focus on individual nutrients or food components, food-based advice is important to help people put nutrition recommendations into practice.
Governments around the world have developed food-based dietary guidelines to communicate healthy eating recommendations in a nationally and culturally appropriate and practical way. The guidelines typically divide foods into food groups and provide advice on the proportion each of these groups should make up in the diet. Most guidelines also include a range of advice for people on how to put this into practice, including guidance on making healthier choices within the food groups (such as choosing wholegrain foods), how often to eat specific types of food (such as 5 A DAY), information on appropriate portion sizes as well tools such as planners or recipes.
While presentation of national food-based dietary guidance varies from country to country, the dietary pattern they present is broadly similar, with fruit and vegetables and starchy foods making up the largest groups, often with a particular focus on wholegrains. Dairy foods and protein food groups make up a smaller proportion, along with advice to limit foods high in fat, salt and sugar.
Redevelopment of UK food-based dietary guidance
UK food-based guidance has been through several iterations over the decades. Most recently, following changes to recommendations on fibre and free sugars in 2015, the government redeveloped the UK model the Eatwell Guide (then the Eatwell Plate) to take these changes into account.
Modelling was carried out by scientists at the University of Oxford using data on dietary intakes from the National Diet and Nutrition Survey (NDNS). Different scientific methods to recalculate the proportions of the food groups in the guide were considered and optimisation modelling using linear programming was selected. This used statistical techniques to model how current diets would need to change to meet current nutrition recommendations – both nutrient recommendations, such as those for fibre, and food-based recommendations, including 5 A DAY, were incorporated.
The results are summarised in Figure 1 below, showing that the proportion of foods from the fruit and vegetables and starchy foods groups would have to increase significantly and that the proportion of foods from all other groups would have to decrease. The food categories within the food groups did not always follow this pattern – in the ‘proteins’ food group, the modelling found that beans and pulses would have to increase by 90% and red meat would have to decrease by 78%.
Studies that have looked at the effect of following the Eatwell Guide compared to the average diet in the UK have found that it could significantly improve population health. One analysis carried out in 2016 when the Eatwell Guide was revised found that following the guidance (without increasing energy intake) could potentially avoid 17.8 million years of ill-health or early death (disability adjusted life years or DALYs) over the lifetime of the population.
Much of the benefit seen was due to prevention of type 2 diabetes as well as prevention of cancer and cardiovascular disease. Another analysis carried out in 2020, found that following at least five of the nine Eatwell Guide recommendations reduced mortality risk by approximately 7% as well as reducing carbon emissions by 30% compared to following 2 or fewer of the recommendations.
While there is increasing evidence for the benefits following healthier dietary patterns as set out in the Eatwell Guide and other models, we are a long way from making this a reality. As shown in the studies mentioned above, significant changes in eating habits are needed for current average UK diets to meet Eatwell Guide recommendations. It has been estimated that less than 1% of the population meet all current dietary guidelines and that only about 30% are meeting five or more of the nine specific recommendations in the Eatwell Guide.
Current UK diets are a long way from following the Eatwell Guide. Significant changes to diets are needed including increases in fruit and vegetable, fish and wholegrain consumption and reductions in foods high in saturated fat, salt and sugar
Anne de la Hunty, Senior Nutrition Scientist, British Nutrition Foundation
While trend data from the NDNS from 2008-2017 shows that there has been some progress in reducing intakes of free sugars and sugary drinks in recent years, intakes of free sugars, saturated fat and salt remain higher than recommended. There has been no appreciable increase in fruit and vegetable, fish, or fibre intakes. The broad principles of what makes up a healthy diet are well established but the challenge of how to encourage people in the population to take up this advice remains.
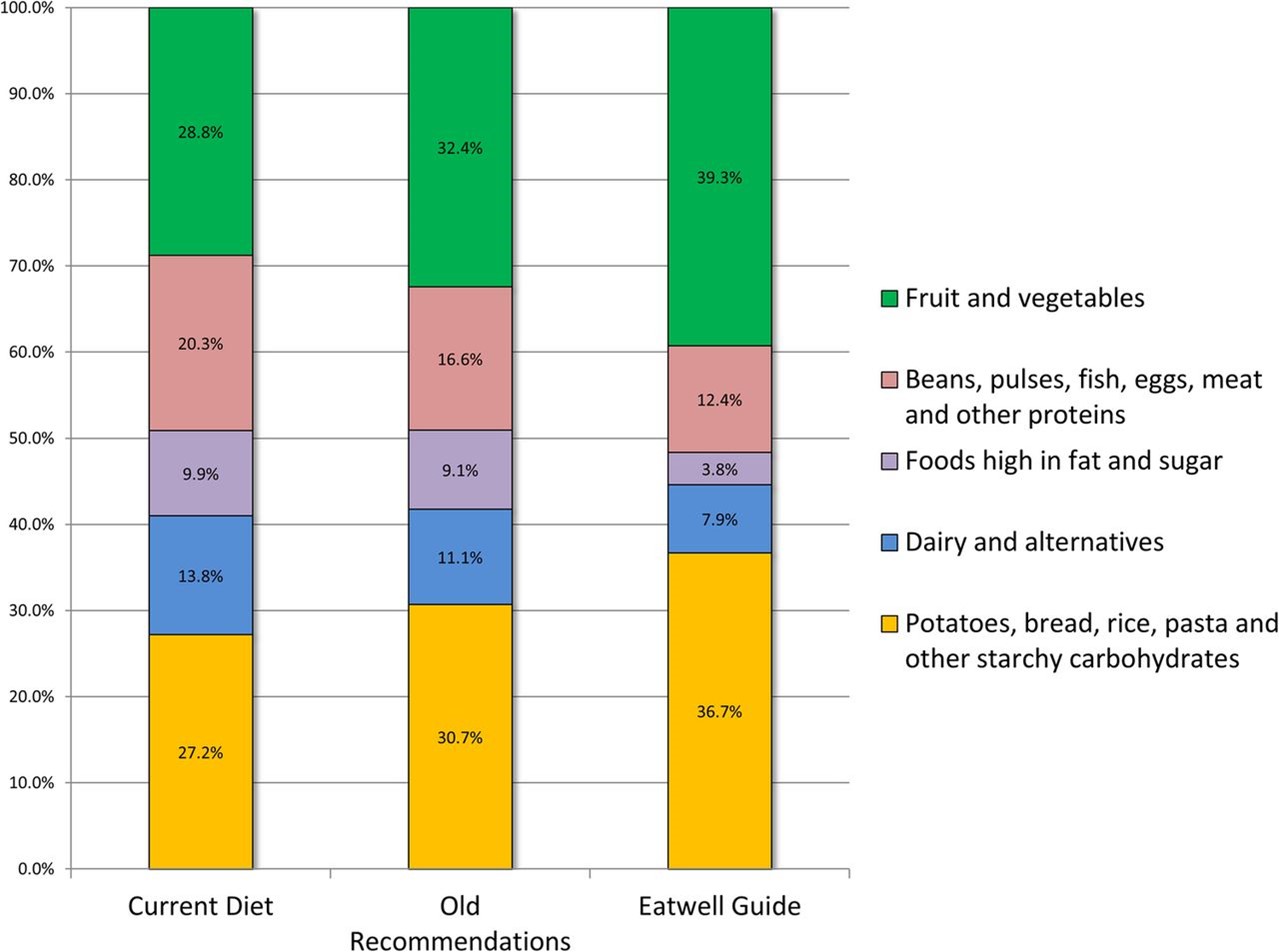
Breakdown of the diet by Eatwell Guide food group categories for current consumption, the ‘Eatwell Guide’ scenario and the ‘old recommendations’ (using previous recommendations for sugars and fibre) scenario
Scarborough et al. 2016
Research on dietary patterns
In recognition of the importance of dietary patterns rather than single foods or nutrients, researchers have developed methods for measuring healthy diets as part of cohort or intervention studies. This section will look at some examples of these measures and studies that have used them.
The Healthy Eating Index (HEI) is a measure of diet quality used to assess how well a set of foods aligns with key recommendations of the Dietary Guidelines for Americans.
The HEI-2015 includes 13 components that reflect the key recommendations in the 2015-2020 guidelines. There are two groups, ‘adequacy components’ and ‘moderation components’.
‘Adequacy components’ represent the elements of the diet that are encouraged in the guidelines. For these components, higher scores reflect higher intakes, because higher intakes are desirable.
The adequacy components are:
- Total fruit
- Whole fruit
- Total vegetables
- Greens and beans
- Wholegrains
- Total protein foods
- Seafood and plant proteins
‘Moderation components’ represent the foods or nutrients where there are recommended limits to consumption. In this case higher scores reflect lower intakes because lower intakes are more desirable.
The moderation components are:
- Refined grains
- Added sugars
- Saturated fats
Overall, a higher total HEI score suggests a diet that aligns better with the US dietary recommendations. Studies have found that greater adherence to the HEI is associated with lower risk of all-cause, cardiovascular and cancer mortality.
Alternative Healthy Eating Index (AHEI)
The AHEI was developed as an alternative to the HEI and focussed on foods and nutrients associated with reducing the risk of chronic disease. It is based on 11 components: six where the highest intakes are considered ideal (vegetables, fruit, whole grains, nuts and legumes, long chain omega-3 fats [docosahexaenoic acid and eicosapentaenoic acid], and polyunsaturated fatty acids), alcohol, for which moderate intake was considered ideal, and four components for which avoidance was recommended (sugar sweetened drinks and fruit juice, red and processed meat, trans fat and sodium). Each component is given a score between zero and ten, all the components adding up to a potential maximum score of 110, with higher scores suggesting better dietary quality.
The DASH diet
The DASH diet was developed to help lower blood pressure and it emphasises higher consumption of fruit, vegetables, legumes and nuts, wholegrains and low-fat dairy and limits sugary drinks, meat and sodium. The DASH score quantifies the level of adherence to the diet.
A systematic review and meta-analysis looking at dietary quality as assessed by the HEI, AHEI and the Dietary Approaches to Stop Hypertension (DASH) scores and health outcomes found that higher diet quality according to these methods was associated with reduced risk of all-cause mortality, reduced risk of cardiovascular and cancer incidence and mortality as well as reduced risk of type 2 diabetes and neurodegenerative disease.
The Nordic diet
The Nordic diet focuses on healthier foods that are locally produced in the Nordic region, and which are considered of importance to cultural and gastronomic identity in these countries. A Nordic style diet generally includes fruits such as apples, pears and berries, vegetables including roots, cruciferous vegetables and cabbages, as well as wholegrain and rye breads, a high intake of fish, low-fat dairy products, potatoes and vegetable fats.
Different scores have been developed to define a healthy Nordic diet, including the Baltic Sea Diet score (from Finland), Healthy Nordic Food Index (from Denmark) and the New Nordic Diet score (from Norway). Evidence from observational studies suggest that a Healthy Nordic is associated with lower risk of type 2 diabetes, stroke and a reduced risk of mortality (particularly from cardiovascular disease). Results from a small number of trials also suggest that a Nordic diet may help improve body weight, blood pressure and blood lipids. However, there is a general lack of evidence in non-Nordic populations to support these potentially beneficial effects if such a dietary pattern is adopted more widely.
Mediterranean diet
The Mediterranean diet, which is usually used to refer to the types of diets traditionally consumed in countries such as Italy and Greece, has been the subject of a lot of research over recent decades. Researchers have developed several different ways of measuring adherence to a Mediterranean dietary pattern. While these differ in exactly what is measured and how the score is calculated, higher consumption of fruit, vegetables, legumes, cereals, olive oil and fish and lower intakes of meat, dairy foods eggs and sugar are generally included. Research suggests that greater adherence to a Mediterranean diet may be associated with lower risk of coronary heart disease, lower levels of inflammation and a reduced risk of cognitive decline.
Plant-based diets have been the subject of much popular and scientific discussion in recent years. A set of plant-based diet indices have been developed as a research tool to investigate the health effects of such diets. The plant-based diet index (PDI) looks at the consumption of plant-based vs animal-based foods in the diet overall. The ‘healthful plant-based diet index’ (hPDI) emphasises plant-based foods that were considered to be healthy, including wholegrains, fruits, vegetables, nuts, legumes and tea and coffee. The ‘unhealthful plant-based diet index’ (uPDI) includes plant foods they considered as less healthy including fruit juices, refined grains, potatoes, sugary drinks and sweets. In each case, diets were scored according to their content of plant- vs animal-based foods and drinks, with an emphasis on healthy/less healthy plant-based elements for the hPDI and uPDI scores, respectively.
In a study looking at body weight in three large cohort studies, researchers found that a higher PDI score was associated with greater weight loss, but that this effect was greater with the hPDI score than the uPDI score. Another study looked at the association between these plant-based indices and risk of type 2 diabetes. The overall PDI score was associated with reduced risk although this was attenuated when it was controlled for body mass index (BMI). The hPDI score was associated with reduced risk of type 2 diabetes and the relationship remained after controlling for BMI. Conversely the uPDI score was associated with a higher risk of type 2 diabetes. A similar pattern was seen in a study looking at risk of coronary heart disease (CHD). The overall PDI score was associated with reduced risk of CHD, with a greater reduction seen with the hPDI score. Whereas the uPDI score was associated with increased risk of CHD.
Key references:
- EFSA (2010) Scientific Opinion on establishing Food-Based Dietary Guidelines https://www.efsa.europa.eu/en/efsajournal/pub/1460
- Morze et al. (2020) Diet Quality as Assessed by the Healthy Eating Index, Alternate Healthy Eating Index, Dietary Approaches to Stop Hypertension Score, and Health Outcomes: A Second Update of a Systematic Review and Meta-Analysis of Cohort Studies. Journal of the Academy of Nutrition and Dietetics https://doi.org/10.1016/j.jand.2020.08.076
- PHE (2016) From Plate to Guide: What, why and how for the Eatwell model https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/579388/eatwell_model_guide_report.pdf
- Scarborough et al. (2016) Eatwell Guide: modelling the dietary and cost implications of incorporating new sugar and fibre guidelines. BMJ Open 6:e013182. http://dx.doi.org/10.1136/bmjopen-2016-013182
More on vitamins and minerals
Calcium counts
This resource looks at the calcium content in dairy and non-dairy foods that may contribute calcium to your diet.
Calcium Counts

A healthy balanced diet
We can probably all agree that eating a healthy, balanced diet is a good thing, but what does this mean in practice?

Vital Vitamin D
There are a limited number of foods naturally containing or fortified with vitamin D.
Healthy Diet FAQs
Is a healthy diet more sustainable?
As well as thinking about how what we eat affects our health, it’s also good to consider how it affects the planet. The good news is that healthier diets also tend to be more environmentally sustainable.
Should I try a different diet if I am overweight?
There are a whole range of other popular diets such as keto, paleo or raw food diets, some of which claim to have specific effects on health or to help with weight loss. However, those diets which do not follow the healthy eating principles are typically harder to stick to and may be detrimental to your overall health in the longer term.
To lose weight, you need to create a calorie deficit in your diet. That means you need to burn more calories than you consume. To learn more about how to lose weight healthily read our page on healthy weight loss here.
Last reviewed October 2023. Next review due October 2026.
Did you find this page useful?
We'd love to hear your feedback. If you would like a response, please contact us. Please note that advice provided on our website about nutrition and health is general in nature. We do not provide any individualised advice on prevention, treatment and management for patients or their family members.
- Find your local Age UK

- Site search Enter search keywords
- Back Information and advice
- Back Money & legal
- Back Benefits and Entitlements
- Attendance Allowance
- Benefit rates 2024-25
- Benefits Calculator – what are you entitled to?
- Bereavement Support Payment
- Carer's Allowance
- Benefits for mixed age couples
- Changes to the benefit system
- Cold Weather Payment
- Council Tax Reduction
- Disability Living Allowance
- Employment and Support Allowance
- Free bus pass and transport concessions
- Free prescriptions for over 60s
- Housing Benefit
- How to apply for a Blue Badge
- How to challenge a benefit decision through mandatory reconsideration
- How to get help with urgent or one-off expenses
- How your benefits are means tested
- Income Support
- Jobseeker's Allowance
- Pension Credit
- Personal Independence Payment
- Returning to the UK after living abroad
- Support for Mortgage Interest
- TV licence concessions
- Universal Credit
- Warm Home Discount
- Council Tax rebate
- Winter Fuel Payment
- More money in your pocket information guide
- Back Debt and savings
- 8 ways to make the most of your savings
- Debt help & advice
- Energy advice for the home
- Financial jargon checker
- How to reduce your water bills
- How to trace lost money
- Using credit wisely
- Back Income and tax
- What is equity release?
- Ways to reduce Council Tax
- Inheritance tax
- How to make money in retirement
- Equity release information guide
- Back End of life planning
- Back Legal issues
- Finding legal advice
- How to be an executor information guide
- Making a will
- Power of attorney
- Power of attorney information guide
- Thinking about end of life information guide
- What is a living will (advance decision)?
- What to do when someone dies
- Wills and estate planning information guide
- Back Pensions advice
- Annuities explained
- Finding old pensions
- Pension calculator
- Pensions scams and fraud
- State Pension
- What are workplace pensions?
- What pension options do I have?
- Back Scams and fraud
- How to spot a catfish
- Spotting TV Licence scams
- Doorstep scams
- Postal scams
- Phone scams
- What to do if you're the victim of a scam
- Investment scams and fraud
- Avoiding scams information guide
- Help with the cost of living
- Back Consumer advice
- Changes to landline telephones
- Back Health & wellbeing
- Back Conditions and illnesses
- Bladder and bowel problems information guide
- Bowel problems
- Coronavirus
- Depression and anxiety
- Hearing loss
- High blood pressure
- Influenza (flu) prevention
- Malnutrition
- Osteoporosis
- Seasonal affective disorder (SAD)
- Urinary incontinence
- Urinary tract infections (UTIs)
- Back Health services
- Dental services for older people
- 9 health tests that could save your life
- Getting the most from your medicines
- Getting help when feeling unwell
- NHS continuing healthcare
- Your hospital stay
- GP services for older people
- Leaving hospital
- Complaining about NHS services and hospitals
- What standards you should expect from NHS services
- Your hospital stay information guide
- Back Being active
- Getting active when you find exercise difficult
- Getting active but not sure where to start
- Helping someone to get active
- Preventing falls
- How to look after your feet
- Walking tips
- Physical activity videos to use at home
- Staying steady information guide
- Back Mind and body
- 10 tips for ageing better
- 5 tips to boost your mood
- Getting a good night's sleep
- Your mind matters
- Mindfulness
- Staying cool in a heatwave
- Staying sharp
- Preventing and treating burns
- Back Loneliness
- A Life Less Lonely
- Caring for someone who's lonely
- Feeling lonely
- Back Keep well this winter
- Keeping warm and well in winter
- Keep your spirits up
- Look after each other
- Cold weather advice and tips
- Managing money in winter
- Winter wrapped up information guide
- Winter illnesses
- Back Relationships and family
- Financial and legal tips before remarrying
- Planning for end of life
- Protection from abuse and neglect
- Dating in later life
- Sex in later life
- How to deal with grief after a bereavement
- How to adjust to living alone
- Top tips for grandparents
- Worried about someone?
- Back Care & support
- Back Finding and arranging social care
- Care needs assessment
- Home care: how to find the care you need at home
- Back Paying for care
- Financial assessment explained
- Paying for residential care
- Paying for homecare
- How much does care cost?
- Back Help for carers looking after a loved one
- Carer's assessment
- Financial support for carers
- Balancing working and caring responsibilities
- Caring for someone with dementia
- Looking after yourself as a carer
- Respite care: having a break from caring
- What to do when your caring role changes or ends
- Carer's checklist
- Back Housing options in later life
- Assisted living and extra-care housing
- Safety in the home
- Home adaptations to simplify home tasks
- Specialist housing options
- Renting and social housing
- Homelessness
- Moving in with family
- Residential park homes
- Sheltered housing
- Back Problems with care
- How to complain about care to your local council
- Problems with homecare
- Back Work & learning
- Back Making the most of the internet
- Computer training courses
- Glossary of online terms
- Getting started on the internet
- Staying safe online
- Keeping in touch using a video call
- Making your device easier to use
- How to download apps
- Email essentials
- What's WhatsApp?
- Using social media
- Is online banking safe?
- How to transfer money and make payments
- Shopping safely online
- Online password security
- Age UK's digital instruction guides
- Back Discrimination and rights
- EU citizens and settled status after Brexit
- Help for Ukrainian nationals in the UK
- Human rights
- The Equality Act
- Windrush Scheme
- Your rights at work
- Back Education and training
- Build up your skills
- Classes and courses
- Higher education and university
- u3a – Later life learning
- Back Looking for work
- Be your own boss
- CVs and job applications
- Job interview tips
- Back Retirement
- Preparing emotionally for retirement
- Paul Lewis: Retirement planning advice
- Living abroad after retirement
- Retirement age
- Back For professionals
- Benefits hub for professionals
- Mental health hub for professionals
- Winter hub for professionals
- Information guides and factsheets
Age UK Advice Line 0800 678 1602
Free to call 8am – 7pm 365 days a year Find out more
Telephone friendship
Get a free weekly friendship call. We'll match you with one of our volunteers. Our service is flexible to suit the different needs of everyone who takes part.
- Sign up for telephone befriending
- Find services near you
- Find charity shops near you
Popular services
- Age UK Advice Line
- Befriending services
- The Silver Line Helpline
- Day Centres
- Exercise and physical activity
- Handyperson services
- IT Training
- Social activities
- Back Services
- Back Get involved
- Back Donate
- Make a donation
- Back Leave a gift in your will
- How to leave a gift in your will
- Making and amending your will to include a gift to Age UK
- Information for executors
- The difference a gift in your will could make
- Ways to write your will
- Free Wills Month 2024
- Will Aid 2024
- Back Donate to our shops
- Age UK and The Wombles join forces
- Age UK's eBay store
- Sustainability
- Back Donate in memory
- Make a donation in memory
- Fundraise for Age UK in memory of your loved one
- Make a one-off donation
- Funeral donations and collections
- Set up a Tribute Fund
- Meaningful ways to remember your loved one
- Make a major gift
- The difference your money makes
- Our professional fundraisers
- Back Fundraise
- Back The innocent Big Knit – get knitting for charity
- innocent Big Knit updates
- Back Sporting events
- Run for charity
- Skydive for charity
- Cycle for charity
- Charity walks and treks
- Charity triathlon events and obstacle courses
- Do your challenge for Age UK
- Back Fundraising ideas
- Most popular ideas
- Sporty ideas
- Fundraise at work
- Fundraise at school
- Fundraise while you celebrate
- Fundraise as a community
- Let's get fundraising
- Pay in your fundraising
- Fundraising resources
- Leeds Abbey Dash
- TCS London Marathon
- Back Stream for Ages
- Your free downloads
- Back Lottery and raffle
- Play the Age UK lottery
- Tuesday Treat Draw
- Play the Age UK raffle
- Gift the Lottery
- Player Zone
- How every entry helps
- Are you a winner?
- Lottery and Raffle rules
- Back Volunteering
- Telephone Friendship Service volunteering
- The Silver Line Helpline volunteering
- Connect and Support Service volunteering
- Age UK shops volunteering
- Local Age UK volunteering
- Support our campaigns
- Back Corporate partnerships
- Why partner with Age UK
- Back Ways we could work together
- Can your company support the Age UK Telephone Friendship Service?
- Latest jobs with Age UK
Age UK. Know what to do.
Last year, over 10 million people trusted us to help them with some of the biggest issues in their lives. Learn more about how we help.
How your support helps
Here's how, with your support, Age UK is supporting older people through the cost of living crisis.
- See the difference your donations make
Making older people's voices heard
- Age UK know what to do
- Campaigning with older people
- Discover - news, stories and features
- Media Centre
- Policy and research
- Wellbeing programmes
- Politics and government
- Back Our impact
- Back Buy products
- Back Over-50s Insurance
- Car insurance
- Home insurance
- Motor breakdown cover
- Travel insurance
- Travel insurance with medical conditions
- Back Independent living
- Bathing Solutions
- Stairlifts and Homelifts
- Personal Alarms
- Back Financial services
- Funeral Plans
- Legal services
- Back Healthcare
- Incontinence products
Healthy eating
- Alcohol advice
Healthy eating guide
- Healthy eating: fact vs fiction
- Vitamins for older people
Eating well means you’re more likely to feel healthier, stay active for longer and protect yourself against illness.
How to eat well
What are the best foods to stay healthy , what foods are high in fat and sugar, how to read food labels, how much fluid should i be drinking every day, how can i save money on food and eat healthily, how do i keep a healthy weight, what should i do next.
Eating well means enjoying your food and having plenty of variety in your diet so you get all the nutrients you need and maintain a healthy weight.
The Eatwell guide shows how much of what you eat overall should come from each food group
It’s never too late to start eating healthily, and a healthy diet doesn’t have to be boring or expensive.
Eating well doesn’t have to mean giving up the less healthy things you enjoy – it just means eating them in moderation and as part of a balanced diet.
Fruit and vegetables
Fruit and vegetables contain a range of vitamins, minerals and fibre. Research shows that people who eat plenty of fruit and vegetables are less likely to develop heart disease and certain cancers.
Aim for at least five portions of different-coloured fruit and vegetables each day. These can be fresh, frozen or canned.
A portion is roughly the amount you can fit in the palm of your hand, for example:
- two satsumas
- three apricots
Beans, pulses, fish, eggs, meat and other proteins
These foods all contain protein, minerals and vitamins which help maintain and repair your body after an injury or surgery.
You don’t need to eat meat every day – try eggs, beans, lentils or meat substitutes such as Quorn or tofu instead.
Oily fish are rich in vitamin D and a type of fat that helps to reduce your risk of heart disease. Try to eat fish twice a week, with one portion being oily fish such as salmon or sardines.
Potatoes, bread, rice, pasta and other starchy carbohydrates
These foods give you energy and a range of nutrients. Try to eat wholegrain versions such as brown rice, wholegrain bread or pasta. These are good sources of B vitamins, minerals and fibre which helps prevent constipation.
Dairy and alternatives
These foods contain protein and vitamins and are a good source of calcium, which helps to keep bones strong. Try to choose lower-fat versions, such as semi-skimmed milk, half-fat cheese and low-fat paneer.
Oils and spreads
We do need some fat in our diets, but only a small portion.
Try to keep an eye out for the type of fat that’s in the oil or spread you use. Eating too much food high is saturated fat can increase the risk of heart disease, whilst food containing unsaturated fat can help reduce your risk. Other fats, such as omega-3 can protect against heart disease.
Read more about looking after your heart on HEART UK
Browse our selection of healthy recipes
Diets that are high in fat, sugar and salt have been linked to common health conditions such as heart disease, some types of cancer, high blood pressure, stroke, obesity and tooth decay.
Many processed foods, ready meals and savoury snacks can be quite high in fat, sugar and salt. These foods should be eaten in moderation as part of a balanced diet and in many cases it may be best to consider them as treats.
Eating too much salt can increase your risk of high blood pressure and stroke. Look for lower-salt versions of foods where you can.
Foods that are high in saturated fat such as cakes, sausages and cheese increase cholesterol levels in the blood and raise your risk of heart disease and stroke. Try to see these as a treat rather than an everyday snack.
All major supermarkets have agreed to help make choosing healthy food easier with a standard label that lets you see how much fat, saturated fat (saturates), sugar and salt is inside.
What is a food label?
All food manufacturers must use a standard label on the front of food packaging.
Looking at the food labels found on most pre-packaged foods can help you make healthy choices. Try to get in the habit of reading pack labels and comparing brands before you buy.
What information should be on a food label?
Food labels can help you see which foods are high in fat, salt and added sugars. They can also show you how many calories are in a product.
The traffic-light colours (red, amber and green) quickly show you levels of sugar, fat and salt in food.
Red: high levels - You should try to eat these less often and in small amounts.
Amber: medium (neither high nor low amounts) - You can eat these foods most of the time.
Green: low - This is the healthier choice.
Several red lights on the food label indicate you should eat the food less often or in small amounts.
Often forgotten about, fluids are just as important as the other food groups. Water is vital for our bodies to work properly so it’s important to drink plenty. Not drinking enough can cause constipation, dehydration, and increase your risk of a fall.
Aim for 6-8 glasses of fluid every day. This doesn’t have to be water – milk, soups, tea and coffee all count. Alcohol is best avoided.
Certain medical problems can affect the amount of water you drink. If you have heart failure, you may need to restrict the amount of fluid each day. If you have urinary incontinence , you may be drinking less to avoid going to the toilet often but it’s important to drink enough. If you have a long-term condition, talk to your doctor about how much fluid you should drink every day.
It's easier than most people think to eat healthily on a budget.
Try these tips to eat well and spend less:
- Plan your meals and stick to a shopping list so you buy only the items you need.
- Try not to rely on ready meals as they are more expensive than making meals yourself, and can be higher in fat, sugar and salt.
- Try making extra portions of meals and freezing them so you can have them later in the week.
- Choose cheaper own brands in supermarkets.
- Look for money-off coupons in magazines or online.
- Check for offers on storable foods such as pasta, cereal, and tinned food.
- The reduced items shelf for goods that are reaching their use-by date often has some good bargains.
- Frozen or tinned fruit or vegetables still count towards your ‘5 a day’.
Keeping to a healthy weight is important. There are health risks with being overweight or underweight. It’s easy for weight to creep up or drop off without us noticing. Next time you’re at your doctors surgery ask them to check that your weight is within a healthy range.
Poor appetite and weight loss
If you’re finding it difficult to eat enough, you might find yourself feeling tired, depressed and low on energy. This is because you’re lacking essential vitamins and minerals. It can also lead to unwanted weight loss.
Signs to watch out for include your clothes feeling looser and jewellery, such as a ring seeming too big.
If you only feel like eating a little, it’s important that the food you do eat is nourishing. Keeping a food diary listing what you eat over a few days may be helpful. Here are some tips you might try:
- Eat six small meals and snacks every day, rather than 3 main meals. Snack on yoghurt, cheese and crackers, toast with a savoury topping, a milky drink, a fruit smoothie, or breakfast cereal with milk, rather than biscuits and sweets.
- If you have problems chewing and wear dentures or have a bridge, ask your dentist to check that they fit properly. While any dental problems are being corrected, try easy-to-eat foods such as minced meat, casseroles, mashed potato, canned fruit and cooked vegetables.
- Keep a store of food for when you want a quick meal or snack, such as cans of soup or frozen meals.
- If you’re finding it difficult to shop or cook for yourself, consider getting help. Talk to your local adult social services department and explain any problems you’re having with day-to-day tasks. There may also be a local meal delivery service in your area like Meals on Wheels.
- Keeping active will help improve your appetite. Try going for a short walk every day or find another activity you enjoy that keeps you on the move. If you find this difficult, ask your doctor for advice about activities suitable for your level of mobility and fitness.
Find out more on the Malnutrition Task Force website
Trying to lose weight
Being very overweight puts us at risk of heart disease, stroke, diabetes and some cancers, including bowel cancer and breast cancer.
Losing weight isn’t easy. If you’ve gradually gained weight over the years, try to lose it slowly but steadily rather than crash dieting.
Try keeping a food diary for a week. Write down everything you eat each day then check through to see where you might cut down or change your habits, for example by switching to healthier snacks.
Staying active
Being physically active can help you maintain a healthy weight or lose excess weight.
Visit our section on physical activity for ideas about staying active
Download our Healthy living guide
Read the Eatwell guide
More information you might find useful
- Age UK Information Guide: Healthy living (PDF, 4 MB)
- Age UK's healthy recipes page
- The Eatwell Guide
- British Nutrition Foundation
- Malnutrition Task Force
For more information call the Age UK Advice Line on 0800 678 1602 . We’re open 8am to 7pm, every day of the year.
Please help us be there for older people in need
By donating today, you could help us answer more calls to our advice line, campaign harder for older people’s rights and fair treatment and provide regular friendship calls to people who are desperately lonely.
Share this page
- Share on Facebook
Last updated: Oct 24 2022
Become part of our story
- Please enter a valid email address
Back to top
- Child Health
- Heart Health
- Men's Health
- Mental Health
- Sexual Health
- Skin Conditions
- Travel Vaccinations
- Treatment and Medication
- Women's Health
- View all categories
- Bones and Joints
- Digestive Health
- Healthy Living
- Signs and Symptoms
Try our Symptom Checker Got any other symptoms?
- Nervous System
- Heart Disease
- Inflammation
- Painkillers
- Muscle Pain
- View all Medicines and Drugs
- Type 2 Diabetes
- Bacterial Vaginosis
- View all Treatments
- BMI Calculator
- Pregnancy Due Date Calculator
- Screening Tests
- Blood Tests
- Liver Function Tests
- Am I Pregnant?
- Am I Depressed?
- View all Tools
- Latest Features
- Health Videos
- Bronchiolitis
- Molluscum Contagiosum
- Actinic Keratosis
- Abdominal Pain in Children
- Subdural Haematoma
- Obesity in Adults
- View all Pro Articles
- View all Medical Calculators
- Login / Register
- Patient Access
- Health Info
Healthy Eating
Remove from Saved
Healthy eating may help to prevent certain long-term (chronic) diseases such as heart disease, stroke and diabetes. It may also help to reduce your risk of developing some cancers and help you to maintain a healthy weight. This leaflet explains the principles of a healthy diet. It is general advice for most people. The advice may be different for certain groups of people, including pregnant women, people with certain health problems or those with special dietary requirements.
In this article
What are the benefits of healthy eating, food groups, what makes up a healthy diet, tips for healthy eating.
Healthy eating may help to prevent certain serious diseases such as heart disease , stroke and type 2 diabetes . It may also help to reduce your risk of developing some cancers. If you become sick, eating a healthy diet may help you to recover more quickly. Also, a main way of preventing obesity and overweight is to eat a healthy diet . If you are overweight or obese, eating a healthy diet can help you lose weight .
As well as healthy eating, regular physical exercise is also very important for health and to avoid or reduce obesity. See also the separate leaflet called Exercise and Physical Activity .
The truth about the fat in your diet
Dietary fat has received its share of bad press, but not all fat is bad for us. We delve into ...

5 warming soup recipes

How much water should you drink a day?

What vitamins do I need?
Your body needs energy to work normally and keep you alive. You obtain this energy from nutrients in the food that you eat - mostly, carbohydrates, fats and proteins. Minerals and vitamins are other nutrients that are also important in your diet to help your body stay healthy.
It is important to find the right balance between these different nutrients to achieve maximum health benefits (see below). A balanced diet generally contains food from each of the following food groups:
- Fruit and vegetables.
- Milk and dairy foods.
- Protein foods. These include meat, fish, eggs and other non-dairy sources of protein (including nuts, tofu, beans, pulses, etc).
- Starchy foods such as bread, rice, potatoes, pasta, etc.
Fatty and sugary foods are the fifth food group that you eat. However, only a small amount of what you eat should be made up from fatty and sugary foods.
In addition to the above, having plenty of fibre and water in your diet is also important for your health.
In the past, the advice was to base your meals on starchy carbohydrates such as potatoes/pasta/rice/bread, and some agencies still suggest this, but this advice is changing as more is discovered about the effects of some carbohydrates, particularly processed ones, on our blood sugar, insulin levels, and weight. The focus now is more towards eating fresh whole foods, including some wholegrain/wholefood carbohydrates, plenty of vegetables, fruit (especially if in season), protein from oily fish, some meat, some dairy and nuts and seeds. This is often referred to as a Mediterranean diet.
It used to be advised that a low fat diet was best, but for most people there is a role for some healthy fats in the diet, eg, from olive oil, oily fish, avocado and some dairy. Healthy fats in small quantities can help you to feel full after a meal and reduce snacking. However other types of fats should be avoided where possible eg, trans fats (trans-unsaturated fatty acids), as these are bad for heart health. Too much animal fat may also be unhealthy. You should limit the amount of foods and drinks that are high in sugar.
It is best to avoid ultra processed foods (UPF) where possible. These are foods that have been heavily processed and had chemicals added eg, as preservatives or emulsifiers. A general rule is to check the packet and if there are a lot of ingredients and you wouldn't find them in the average kitchen cupboard, it is likely to be ultra processed.
The dietary guidance to reduce your risk of heart disease is as follows:
- Cut down on foods and drinks high in saturated fats and trans fats. Replace saturated and trans fats with unsaturated fats found in oils from plants and fish. Current government recommendations are to eat no more than 20g (women) or 30g (men) of saturated fat daily.
- Eat two portions of fruit and at least three portions of vegetables per day. Another more recent suggestion is to aim to eat 30 different plants over the week. This includes nuts, seeds, herbs and spices.
- Eat at least two portions of fish (preferably oily fish) per week.
- Consider regularly eating whole grains and nuts.
- Keep the amount of salt in your diet to less than 6 g per day.
- Limit alcohol intake to less than 14 units per week for men and less than 14 units per week for women. See also the separate leaflet called Alcohol and Sensible Drinking .
- Avoid or reduce the following in your diet:
- Processed meats or commercially produced foods (including 'ready meals') which tend to be high in salt and trans fatty acids.
- Refined carbohydrates, such as white bread and processed cereals.
- Sugar-sweetened drinks.
- High-calorie but nutritionally poor snacks, such as sweets, cakes and crisps.
Below, the principles of a healthy diet are explained. It is general advice for most people. If you have a specific health problem, or specific dietary requirements, this advice may not apply to you. If in doubt, you should check with your doctor. There are also some changes that pregnant women need to make to their diet.
See the separate leaflet called Planning to Become Pregnant for more details .
Carbohydrates
Much of the energy (calories) in what we eat comes from carbohydrate. These are divided into two carbohydrate types:
- Complex carbohydrates - generally starchy foods such as bread, pasta, rice and potatoes.
- Simple carbohydrates - the sweet sugary foods.
There is a lot being written about how much of our food should be made up of carbohydrates but most of the guidelines recommend about one third. This should be mostly starchy carbohydrates, preferably higher-fibre options such as wholemeal bread, wholegrain cereals and brown rice. Sugar/simple carbohydrates should not be eaten regularly. Bread, pasta and white rice also should not be eaten in large quantities. Whole grains such as oats, whole wheat, bulgur wheat, buckwheat, whole rye, bulgur wheat, barley, quinoa and brown rice contain much more fibre and usually cause less rise in blood sugar and are more filling than pasta and bread. Starchy vegetables such as potatoes can be eaten in small - medium quantities.
Glycaemic index The glycaemic index of a food is the rate at which the food raises blood sugar levels after it has been eaten. If a food has a low glycaemic index, it is processed by the body in a way which means it is less likely to lead to problems such as diabetes and obesity. You can find out more about the role of food on your blood sugar from our leaflet on Type 2 Diabetes Diet .
Higher-fibre carbohydrates, such as whole grains, tend to have a lower glycaemic index than more refined starches such as white bread, snack foods and sugary drinks. This means they are a healthier option for this reason as well as for the fibre they contain.
Eat plenty of fruit and vegetables
New research suggests that eating two portions of fruit and at least five portions of vegetables daily reduces the risks of many illnesses, such as stroke, heart disease and some cancers. Ideally there should be more vegetables than fruit in your diet. In addition to these benefits, fruit and vegetables:
- Contain lots of fibre which helps to keep your bowels healthy. Problems such as constipation and diverticular disease are less likely to develop.
- Contain plenty of vitamins and minerals, which are needed to keep you healthy.
- Are naturally low in fat.
- Help to make you feel full after a meal but are low in calories.
An average portion of vegetables may be about a handful, or about 80g. Alternatively, one portion of fruit or vegetables is roughly equivalent to one of the following:
- One large fruit such as an apple, pear, banana, orange, or a large slice of melon or pineapple.
- Two smaller fruits such as plums, kiwis, satsumas, clementines, etc.
- One cup (or a handful) of small fruits such as grapes, strawberries, raspberries, cherries, etc.
- Two large tablespoons of fruit salad, stewed or canned fruit in natural juices.
- One tablespoon of dried fruit.
- About three heaped tablespoons of any vegetable.
- One dessert bowl of salad.
Some tips on how to increase fruit and vegetables in your diet include:
- Try some different types that you have not tried before. The variety of tastes and textures may be surprising. Frozen, canned and dried varieties all count.
- Try adding chopped bananas, apples, or other fruits to breakfast cereals.
- Aim to include at least two different vegetables with most main meals. Do not over-boil vegetables. Steaming, stir-frying, or lightly boiling are best to retain the nutrients.
- Try to have fruit with a meal..
- Try new recipes which include fruit. For example, some curries or stews include fruit such as dried apricots. Have fruit-based puddings. Fruit with yoghurt is a common favourite.
- Consider cherry tomatoes, carrot sticks, dried apricots, or other fruits as part of packed lunches.
- Fruit is great for snacks. Encourage children to snack with fruit rather than with sweets.
Eat plenty of fibre
High fibre foods include:
- Wholegrain breakfast cereals, wholewheat pasta, brown rice, wholegrain bread and oats, barley and rye.
- Fruits such as berries, pears, melon and oranges.
- Vegetables such as broccoli, carrots, sweetcorn and potatoes (with skin).
- Peas, beans, chickpeas and lentils.
- Nuts and seeds.
There are two types of dietary fibre:
- Soluble fibre, which is found in oats, peas, beans and many fruits and vegetables, dissolves in water to form a gel-like material. It increases feelings of fullness and can lower blood cholesterol and glucose levels.
- Insoluble fibre is mostly found in whole grains, and also in fruit and vegetable skins. It is not digested by the body but forms bulk in the gut, which helps to keep the bowels moving normally.
Starchy foods and fruit and vegetables contain the most fibre. So the tips above on starchy foods and fruit and vegetables will also increase fibre. Choosing wholemeal rice and pasta, and wholemeal bread can significantly increase your fibre intake. Pulses like lentils and beans are also full of fibre.
Eating higher-fibre foods can make you feel full for longer, which can help if you are trying to watch your weight.
Have plenty to drink when you eat a high-fibre diet (at least 6-8 cups of fluid a day).
See the separate leaflet called Fibre and Fibre Supplements for more details .
Milk and dairy foods
Milk and other dairy foods such as cheese and yoghurt are important in your diet, as they provide calcium which is needed for healthy teeth and bones. They are also a source of protein and can provide other vitamins and minerals important for your health
To make sure that you have enough calcium in your diet, you need three servings a day from this food group. One serving is:
- 200 ml of milk.
- A small (150 g) pot of yogurt.
- A 30 g serving of cheese (about the size of a small matchbox).
Natural or unflavoured yoghurt/milk is preferable to flavoured, as it will contain less sugar and not be ultra-processed.
Non-dairy sources of calcium include leafy green vegetables, tinned fish (particularly if the bones are included), dried figs, almonds, oranges, sesame seeds, seaweed and some types of beans.
Non-dairy calcium needs to be eaten with a source of vitamin D, as the body needs this to help it absorb the calcium. Vitamin D can be found in eggs, fish and mushrooms but is mostly made in the skin by contact with sunshine.
Some foods are fortified with calcium, such as breakfast cereals, some soya drinks and tofu. These may already have added vitamin D.
Other protein-containing foods include meat, fish, eggs and plant sources of protein. Plant sources of protein include nuts, seeds, tofu, beans such as red kidney beans and canned beans, and pulses such as lentils and chickpeas.
You need a certain amount of protein to keep healthy. Protein is important for energy and for growth and repair in your body. Some of these high-protein foods can also be a source of iron and vitamins, including B vitamins and vitamin D. However, most people eat more protein than is necessary. Beware, some meats are also high in saturated fat.
Some protein helps you stay full after a meal.
Choose poultry such as chicken, or lean meat. One portion of beans or pulses such as chickpeas or lentils is three heaped tablespoons. Eggs can be boiled or poached rather than fried.
There is some evidence that eating oily fish helps to protect against heart disease. Oily fish include herring, sardines, mackerel, salmon, fresh tuna (not tinned), kippers, pilchards, trout, whitebait, anchovies and swordfish. It is thought that omega-3 fatty acids in the fish oil help to reduce 'furring of the arteries' (the build-up of atheroma) which causes angina and heart attacks. Aim to eat at least two portions of fish per week, one of which should be oily.
Protein combining Vegetarian sources of protein do not provide the correct balance of amino acids (the building blocks of proteins) for the body to use unless combined with each other. So people who are not eating a lot of fish, meat or eggs need to make sure that their meals contain two of the following:
- Dairy products.
- Legumes (for example, beans, lentils).
Examples of protein-balanced meals are:
- Baked beans on toast.
- Dhal and rice or chapatti.
- Baked potato with baked beans and cheese
Red meat and processed meat
Red meat refers mainly to beef, veal, pork and lamb. Processed meat refers to meat that has been processed to improve the flavour or to help preserve the meat. Examples of processed meat include ham and sausages, as well as canned meat and meat-based ready meals and sauces.
There is evidence that eating red and processed meat increases the risk of bowel cancer .
Eating red and processed meat has also been shown to increase the risk of stroke, heart disease and type 2 diabetes. The health risks from eating processed meat increase with increasing amounts of processed meat that you eat.
On the other hand, restricting the intake of meat can increase the risk of iron-deficiency anaemia . For this reason, the UK Government's Scientific Advisory Committee on Nutrition (SACN) recommend that your intake of red and processed meat should be no more than 70 g/day.
For a long time, obesity and many other health problems have been blamed on the amount of fat that we eat. This makes sense because fat contains about twice as many calories as carbohydrate or protein per gram. However, more recent research suggests the picture is more complex than that. It suggests that carbohydrate plays a larger role in weight gain than we previously thought.
Also, the advice about which types of fats are better to eat has been under discussion.
It probably is still a good idea to eat less fat if you are trying to lose weight.
Tips to reduce fat in your diet include the following:
- Whenever possible, do not fry food. It is better to grill, bake, poach, barbecue or boil food. If you do fry, use unsaturated oil. Drain the oil off the food before eating.
- Choose lean cuts of meat and cut off any excess fat.
- Avoid adding unnecessary fat to food. For example, measure out small portions of oil for cooking, etc.
- Watch out for hidden fats that are in pastries, chocolate, cakes and biscuits.
See the leaflet called Low-fat diet sheet for more details .
Trans fats Trans fats (or trans fatty acids) are unsaturated fatty acids. Trans fats increase the risk of heart disease. They increase LDL cholesterol and decrease HDL cholesterol.
See also the separate leaflet called High Cholesterol for further information .
Trans fatty acids occur naturally in small amounts in a wide range of foods, such as milk, beef and lamb. However, most of the trans fatty acids in the diet are produced during the processing of vegetable oils. Trans fats are therefore found in hard margarines and in some baking products (for example, biscuits, pastries and cakes), fried foods and other processed foods.
Foods that are labelled as containing partially hydrogenated oils or fats contain trans fatty acids. When buying fat-containing foods, it is much healthier to buy ones labelled with a high content of mono-unsaturates or polyunsaturates.
Research has shown that trans fatty acids produced during the processing (hardening) of vegetable oils are much more harmful to health than natural trans fatty acids (for example, in milk, beef and lamb). You can reduce your intake of trans fats by avoiding or reducing the amount of fried foods, high-fat snacks and high-fat baked foods you eat.
In the UK the intake of trans fats is much lower than it was 20-30 years ago. However, as part of a healthy diet, you should aim to keep both the amount of saturated fats and trans fats to a minimum.
A 2019 review by the SACN (The Scientific Advisory Committee on Nutrition) determined that reducing your intake of saturated fats lowers your risk of developing coronary heart disease, although there was no evidence that it reduces the rate of dying from these conditions. Trans fats were associated with an increased risk of heart disease and stroke. The review recommended that the intake of both saturated fats and trans fats should be kept to a minimum.
Eat lots of vegetables
Vegetables provide energy, fibre, vitamins and minerals and are filling. Frozen are as good as fresh.
Avoid sugary foods and drinks
Sugary foods and drinks are high in calories and too much may cause weight gain. It isn't just the amount of sugar that may be bad. Even eating small amounts of sugary foods (sweets, etc) too often is bad for teeth. Tips include:
- Try not to add sugar to tea, coffee and breakfast cereals. Your taste for sweetness often changes with time. Use artificial sweeteners only if necessary.
- Reduce sugar in any kind of recipe. Use fruit as an alternative to add sweetness to recipes.
- Give children water or milk as their main drink.
- If you eat chocolate or sweets, try to keep the quantity down.
We do not yet know the long term effects of artificial sweeteners so they are best avoided, but they may help people to lose weight if they find avoiding sweet foods and drinks difficult.
Don't eat too much salt
Too much salt increases your risk of developing high blood pressure. Guidelines recommend that we should have no more than 6 g of salt per day. Most people in the UK currently have more than this. If you are used to a lot of salt, try gradually to reduce the amount that you have. Your taste for salt will eventually change. Tips on how to reduce salt include:
- Use herbs and spices rather than salt to flavour food.
- Limit the amount of salt used in cooking and do not add salt to food at the table.
- Choose foods labelled 'no added salt'.
- As much as possible, avoid processed foods, salt-rich sauces, takeaways and packet soups which are often high in salt.
Don't forget portion sizes
You may be eating very healthy foods but you still need to keep an eye on your portion sizes because if they are too large, you will still gain weight. Deliberately try to take smaller portions when you have a meal.
Do not feel that you have to empty your plate. Perhaps change the plates that you have in your cupboard (which may be large) to more medium-sized plates. In this way you will naturally serve up smaller portions. Fill up on fruit and vegetables. Ask for a smaller portion when eating out or ordering a takeaway.
Think about what you are drinking
Many drinks, including alcoholic and many non-alcoholic drinks, contain calories. Think about what you are drinking.
- Choose healthier non-alcoholic drinks . Some tips: water contains no calories and can be both refreshing and healthy. Add a slice of lemon or lime to your water. Keep a jug in the fridge so that it stays cool. Try sparkling water.
- Half a pint of ordinary-strength beer, lager, or cider (3-4% alcohol by volume); or
- A small pub measure (25 ml) of spirits (40% alcohol by volume); or
- A standard pub measure (50 ml) of fortified wine such as sherry or port (20% alcohol by volume).
- A small glass (125 ml) of ordinary-strength wine (12% alcohol by volume); or
- A standard pub measure (35 ml) of spirits (40% alcohol by volume).
- Men should drink no more than 14 units of per week, spread evenly over several days and with at least two alcohol-free days a week.
- Women should drink no more than 14 units of alcohol per week, spread evenly over several days and with at least two alcohol-free days a week.
- Pregnant women . Advice from the Department of Health states that: ... "pregnant women or women trying to conceive should not drink alcohol at all".
The gut microbiome
This is a new area of research and discovery. Scientists are starting to discover that the microscopic organisms that live in our guts may be of much more importance to our health than previously known about. What we eat may affect the health of those organisms (known collectively as the microbiome) and this may affect many areas of our health, including our weight and possibly even conditions such as depression.
Tips for keeping your microbiome healthy include:
- Avoiding ultra-processed foods as much as possible.
- Eating fermented foods such as kefir, kimchi and blue cheese.
- Eating lots of different plants eg, aiming for 30 per week.
- Having a fasting period of 12 hours every 24hrs eg, from 7pm-7am.
Loss of Appetite
Are you protected against flu?
See if you are eligible for a free NHS flu jab today.
Join our weekly wellness digest
from the best health experts in the business
Further reading and references
Glycaemic Index ; diabetes.org.uk
The Eatwell Guide ; Public Health England, 2018
Saturated fats and health ; Scientific Advisory Committee on Nutrition, 2019
Scientific Advisory Committee on Nutrition Iron and Health Report ; GOV.UK, February 2011
Mehta SS, Arroyave WD, Lunn RM, et al ; A Prospective Analysis of Red and Processed Meat Consumption and Risk of Colorectal Cancer in Women. Cancer Epidemiol Biomarkers Prev. 2020 Jan29(1):141-150. doi: 10.1158/1055-9965.EPI-19-0459. Epub 2019 Oct 1.
Key T et al ; Diet, nutrition, and cancer risk: what do we know and what is the way forward? BMJ 2020 368 doi: https://doi.org/10.1136/bmj.m511 (Published 05 March 2020)
Freire R ; Scientific evidence of diets for weight loss: Different macronutrient composition, intermittent fasting, and popular diets. Nutrition. 2020 Jan69:110549. doi: 10.1016/j.nut.2019.07.001. Epub 2019 Jul 4.
De Stefani E, Boffetta P, Ronco AL, et al ; Processed meat consumption and risk of cancer: a multisite case-control study in Uruguay. Br J Cancer. 2012 Oct 23107(9):1584-8. doi: 10.1038/bjc.2012.433. Epub 2012 Sep 25.
Davis CD ; The Gut Microbiome and Its Role in Obesity. Nutr Today. 2016 Jul-Aug51(4):167-174. doi: 10.1097/NT.0000000000000167.
DeMartino P, Cockburn DW ; Resistant starch: impact on the gut microbiome and health. Curr Opin Biotechnol. 2020 Feb61:66-71. doi: 10.1016/j.copbio.2019.10.008. Epub 2019 Nov 22.
Cardiovascular disease: risk assessment and reduction, including lipid modification ; NICE Clinical Guideline (July 2014 -last updated May 2023) Replaced by NG238
Healthy eating - fats explained ; British Heart Foundation
Related Information
- Exercise and Physical Activity
- High Cholesterol
- Epidemiology of Coronary Heart Disease Pro
- Coronary Revascularisation Pro
- Acute Myocardial Infarction Pro

7 easy and delicious noodle recipes for students

Why does my stomach bloat in hot weather?
Every now and then I get this weird feeling in the left side of my chest which can last anywhere from 1min to 45mins+. During the duration of the episode, whenever I exhale or inhale beyond a certain... jake55266
Disclaimer: This article is for information only and should not be used for the diagnosis or treatment of medical conditions. Egton Medical Information Systems Limited has used all reasonable care in compiling the information but make no warranty as to its accuracy. Consult a doctor or other health care professional for diagnosis and treatment of medical conditions. For details see our conditions .

- Health professionals
- International projects
- Local neighbourhoods
- Our services
- Why prevention?
- How to get involved
- Our partners and funders
- Our vision and history
- Annual review
Blog » Food consumption trends in the UK
Food consumption trends in the UK

Obesity is a global pandemic influenced by the food environment and individual choices. [1] Obesity prevalence in the UK is amongst the worst in Europe with more than 60% of adults living with overweight or obesity. [2] In England, 20 % of year 6 children were classified as living with obesity in 2020 with a prevalence twice as high in the most deprived areas than the least deprived area. [3] Trends in food consumption are worth looking at as some are important factors contributing to rising levels of obesity (e.g., increasing consumption of meals out home).
Although consumers are not meeting the dietary guidelines recommendations, there has been reduction in salt, sugar, and red meat consumption. However, consumption of fruits, vegetables and fibre has shown little or no change, and consumption of salt, sugar and red meat are still too high. [4]
The latest data on salt intake for adults shows that average salt intake in 2020 was still higher (8.4g) than the recommended intake of 6g per day. While salt intake has been decreasing slowly over time, this decrease has slowed since 2014. [5]
There has been a fall in red and processed meat consumption over the past decade (-17.4 per capita per day over the last decade), most likely for environmental and health reasons. Significantly, all adults now consume less red meat and processed meat but more white meat. The proportion of meat consumers has decreased over time, whereas the proportion of individuals identifying as vegetarian, and vegan has increased. [6]
The consumption of free sugars by mean average for the general population were significantly lower in 2016 to 2019 than in 2014 to 2016, but were still more than double the recommended maximum of no more than 5% of total energy. The fall in free sugars intake in children is at least partly attributable to a reduction in consumption of sugar-sweetened soft drinks in all age groups following the implementation of the sugar tax in 2018. However, further data shows that while consumption of sugary drinks has fallen, there has been no decline in sweet confectionery and chocolate consumption, with intake even going up in some groups.
Healthy diets typically include greater consumption of fruit, vegetables and whole grains, and reduced consumption of sugar, salt, processed foods, and red meat. [7] The UK population continues to consume too much saturated fat and not enough fruit, vegetables, and fibre.
Mean intakes of fibre were below recommendations in all age groups. In adults mean intakes were around 18g per day over age groups, below the recommendation of 30g. Only 4% of children aged 11-18 years are currently meeting fibre recommendations. Low fibre intake in the UK is thought to be the result of the low intake of fruits and vegetables, as well as a lack of knowledge about where to find fibre and how important it is for our health. In 2018, only 28% of adults were eating the recommended portion of fruits and vegetables and young people aged 16-24 years were less likely than other adults to get their five-a-day. [8]
Most notable changes in eating habits
Purchases of white bread have dropped 75% since 1974, according to the survey, while those of brown and wholemeal bread have risen by 85%.
Skimmed milk (referring both to skimmed and semi-skimmed) overtook whole-fat milk in the 1990s and British households now drink four times as much.
Italian-style cooking is widespread today. Pizza (frozen and not frozen) rose even more dramatically, with average purchase from 2g per week in 1975 to 53g in 2014. The number of takeaway pizzas bought per household shot up 1,000% over the same period.
Reported purchases in the category “chips (frozen and not frozen)” were three times higher in 2014 than in 1974. [9]
Cheaper food and rise of Ultra-Processed food
According to the data from the National Diet and Nutrition Survey, some 24% of a typical pay packet went on food in 1974 compared with 11% today. However, falling prices have sometimes meant a drop in quality of some products at the bottom end of the market too. More than half (57%) of all calories consumed on average across the UK population come from ultra-processed foods. As the ultra-processed food consumption increased, the dietary content of carbohydrates, free sugars, total fats, saturated fats, and sodium increased significantly while the content of protein, fibre, and potassium decreased. Decreasing the dietary share of ultra-processed foods may substantially improve the nutritional quality of diets and contribute to the prevention of diet related NCDs. [10]
How is it consumed?
Channels through which consumers are purchasing food are diversifying. Data from IGD research shows that online grocery market shopping will increase its market share from 18.6 to 23.4 % by 2024. However, large grocery stores will still account for half of the market (50.1%) in 2024. [11] Forms of home delivery other than supermarket delivery include HelloFresh, Amazon Fresh or vegetables.
Out of home environment on the rise
Overall, the consumption of food and beverages from outside the home have considerably increased during the last decades. [12] More than a quarter of adults and one fifth of children eat food from outlets such as cafes, takeaways, or restaurants at least once a week. These meals can be high in calories, fat, sugar, and salt. Eating out of home in places like restaurants’ take-away and fast food is increasingly growing in younger adults’ and adolescents’ diet compared to older adults who prefer to eat at home. Takeaway and fast food environments are a significant contributor to this age-group’s diet. [13] Some evidence shows that children from lower income households are more likely to eat takeaway meals at home or purchase food from outside schools. [14] This emphasises the importance of creating healthy food environment around schools.
The widening of inequalities and increase in levels of food poverty
Poor diet puts people at risk for poor health. There are socio-demographic differences in the consumption of a healthy diet as costs shape what people can afford to eat. Low-income groups consume less healthy food and less fruits and vegetables. Low socio-economic status (in terms of education level, work status and income) is the single most consistent risk factor for an unhealthy diet. [3] Lower incomes, economic deprivation and lower levels of education are associated with a poorer diet and living with overweight/obesity. [15] The local environment has also a huge impact as our behaviours influence our food choices. Figures from Public Health England (PHE) reveal England’s poorest areas are fast food hotspots, with 5 times more outlets found in these communities than in the most affluent. Children in deprived areas are the most exposed to those outlets and on their way back to school may find it difficult to find healthier options. [16]
C3 and ASPIRE
C3 is currently working with seven communities in the North of France and the South of England via an EU-funded project ASPIRE (Adding to Social capital and individual Potential In disadvantaged Regions). The four French sites are in “Les Hauts de France”, the region with the highest obesity rate in France. This multi-partner project is aiming to provide people living with obesity/overweight and/or unemployed the tools they need to make healthier lifestyle choices and improve their employability. Through multi-sector collaboration, C3 works with communities to make it easier for everyone to make healthier choices, which we know is especially difficult for those living in disadvantaged communities. [17]
Read more about C3’s ASPIRE projects:
- Insight session in Abbeville for ASPIRE
- ASPIRE in the town of Ham
- Project ASPIRE: Wimereux
- The ASPIRE project: Obesity and unemployment – what’s the link?
[1] The state of food security and nutrition in the world (2018). Food and Agriculture Organization of the United Nations (FAO)
[2] Cancer research UK. Overweight and obesity statistics (2019) As of 10 January 2022 https://www.cancerresearchuk.org/health-professional/cancer-statistics/risk/overweight-and-obesity
[3] Digital NHS UK. Statistics on obesity, physical activity, and diet, England. (2020). https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-obesity-physical-activity-and-diet/england-2020
[4] D’Angello, C., Gloison, E.R., Draper, A., Guthrie, S., (2020). Food consumption in the UK: Trends, attitudes and drivers. RAND Europe.
[5] UK Health Security Agency blog: new data reveals how your diet are changing overtime. Retrieved from internet 20/01/2022 https://ukhsa.blog.gov.uk/2020/12/21/new-data-reveals-how-our-diets-are-changing-over-time/
[6] Steward,S., Piernas,C.,Cook,B.,Jebb,S.A., (2021). Trends in the UK meat consumption: analysis data from year 1-11(2008-2009 2018-2019) of National Diet and Nutrition Survey rolling program. Lancet Planet Health.
[7] Public Health England. 2018. The Eatwell Guide.
[8] NHS digital: Fruits and vegetables. 2018. As of 10 January 2022, http://healthsurvey.hscic.gov.uk/data-visualisation/data-visualisation/explore-the-trends/fruit-vegetables.aspx
[9] 10 ways the UK eating habits have changed. (2016) 10 ways the UK eating habits have changed. BBC news magazine.
[10] Rauber et al., 2018.Ultra-processed food consumption and chronic non-communicable diseases related dietary nutrient profile in the UK (2008-2014). Nutrients.10.587.
[11] IGD.2019.UK food sale to grow by £24bn by 2024 as of 19 January 2022 https://www.igd.com
[12] FSA. 2019.The food and you survey-wave five. As of 15 January 2022 https://www.food.gov.uk/print/pdf/node/2101
[13] Tyrrell, R.L et al., (2017). Food environments of young people: linking individual behaviour to environmental context. Journal of Public Health. Vol. 39, No. 1, pp. 95–104. doi:10.1093/pubmed/fdw019
[14] Wills, W., Danesi, G., Kapetanaki, A.B., Hamilton,L., (2019). Socio-Economic Factors, the Food Environment and Lunchtime Food Purchasing by Young People at Secondary School Int. J. Environ. Res. Public Health 2019, 16 , 1605; doi:10.3390/ijerph16091605
[15] Penne, T., Goedeme, T., (2021). Can low-income households afford a healthy diet? Insufficient income as a driver of food insecurity in Europe. Food Policy. vol 99,101978. https://doi.org/10.1016/j.foodpol.2020.101978
[16] England’s poorest areas are fast food outlets in Englands most deprived communities. 2018. Public Health England https://www.gov.uk/government/news/englands-poorest-areas-are-fast-food-hotspots
[17] C3 Collaborating for Health website https://www.c3health.org/international-projects/
About the Author


Nathalie Vauterin
- The wealth health gap: my health my right
- Nurses and smoking
- Nursing workforce and NCDs – a double crisis
- NCDs and diet
- Inspirited Minds
Get involved with C3!
Donate, sponsor our International Seminars, become our partner, & attend our events! Learn more here .
Cookies on GOV.UK
We use some essential cookies to make this website work.
We’d like to set additional cookies to understand how you use GOV.UK, remember your settings and improve government services.
We also use cookies set by other sites to help us deliver content from their services.
You have accepted additional cookies. You can change your cookie settings at any time.
You have rejected additional cookies. You can change your cookie settings at any time.
- Health and social care
- Public health
National Diet and Nutrition Survey
The National Diet and Nutrition Survey assesses the diet, nutrient intake and nutritional status of the general population of the UK.
Responsibility for the National Diet and Nutrition Survey moved from Public Health England to the Office for Health Improvement and Disparities (OHID) on 1 October 2021.
The National Diet and Nutrition Survey ( NDNS ) rolling programme is a continuous, cross-sectional survey. It is designed to collect detailed, quantitative information on the food consumption, nutrient intake and nutritional status of the general population living in private households in the UK. Fieldwork began in 2008 and has now completed its 15th year.
OHID and the UK Food Standards Agency ( FSA ) jointly fund the UK NDNS . Under the contract for years 11 to 15, Northern Ireland government bodies have funded additional recruitment to allow separate reporting of results for Northern Ireland.
The contract for years 11 to 15 (2018 to 2023) is delivered by NatCen Social Research, working with the MRC Epidemiology Unit at the University of Cambridge.
A contract to deliver years 16 to 20 of the rolling programme (2024 to 2029) has been awarded to NatCen Social Research working with the MRC Epidemiology Unit at the University of Cambridge. This will include a urinary sodium survey of adults in England in 2025.
NDNS provides essential evidence on the diet and nutrition of the UK population to enable OHID to identify and address nutritional issues in the population, and monitor progress towards public health nutrition objectives.
Current NDNS results
The most recent results are available below.
- 22 September 2021
- Official Statistics
- 11 December 2020
- 25 March 2020
Methods reports
- 6 November 2023
- Research and analysis
Previous NDNS results
- 23 January 2019
- 11 April 2018
- 28 November 2017
- 28 February 2017
- 9 September 2016
- 22 March 2016
Archive of NDNS reports
Earlier and archived NDNS reports are also still available.
See below for the previous, years 1, 2 and 3 rolling programme reports published by the then Department of Health.
See the UK Government Archives for the year 1 rolling programme report and pre-rolling programme reports published by the FSA .
- 25 July 2012
- 27 October 2011
- 21 July 2011
- Policy paper
Updated to reflect the latest information on the NDNS rolling programme and added the 'Evaluation of change in dietary methodology in NDNS rolling programme: stage 2' report to collection.
Added 'Evaluation of change in dietary methodology in NDNS rolling programme: Stage 1'.
Added National Diet and Nutrition Survey: assessment of salt intake from urinary sodium in adults in England, 2018 to 2019.
Added 'NDNS: time trend and income analyses for Years 1 to 9'.
Added 'NDNS: results from years 7 and 8 (combined)'.
First published.
Related content
Is this page useful.
- Yes this page is useful
- No this page is not useful
Help us improve GOV.UK
Don’t include personal or financial information like your National Insurance number or credit card details.
To help us improve GOV.UK, we’d like to know more about your visit today. We’ll send you a link to a feedback form. It will take only 2 minutes to fill in. Don’t worry we won’t send you spam or share your email address with anyone.
- Open supplemental data
- Reference Manager
- Simple TEXT file
People also looked at
Original research article, impact of the covid-19 pandemic on diet behaviour among uk adults: a longitudinal analysis of the hebeco study.

- 1 Department of Behavioural Science and Health, University College London, London, United Kingdom
- 2 Policy and Implementation Research, Cancer Research UK, London, United Kingdom
- 3 Department of Clinical, Educational, and Health Psychology, University College London, London, United Kingdom
COVID-19 pandemic restrictions impacted dietary habits during the initial months of the pandemic, but long-term effects are unclear. In this longitudinal study, self-selected UK adults ( n = 1,733, 71.1% female, 95.7% white ethnicity) completed three online surveys (May–June, August–September, and November–December 2020, with a retrospective pre-pandemic component in the baseline survey), self-reporting sociodemographics, lifestyle, and behaviours, including high fat, salt, and sugar (HFSS) snacks, HFSS meals, and fruit and vegetable (FV) intake. Data were analysed using generalised estimating equations. Monthly HFSS snacks portion intake increased from pre-pandemic levels (48.3) in May–June (57.6, p < 0.001), decreased in August–September (43.7, p < 0.001), before increasing back to pre-pandemic levels in November–December (49.2, p < 0.001). A total of 48.5% self-reported increased [25.9 (95% confidence interval: 24.1, 27.8)] and 47.7% self-reported decreased [24.1 (22.4, 26.0)] monthly HFSS snacks portion intakes in November–December compared with pre-pandemic levels. Monthly HFSS meals portion intake decreased from pre-pandemic levels (7.1) in May–June (5.9, p < 0.001), was maintained in August–September (5.9, p = 0.897), and then increased again in November–December (6.6, p < 0.001) to intakes that remained lower than pre-pandemic levels ( p = 0.007). A total of 35.2% self-reported increased [4.8 (4.3, 5.3)] and 44.5% self-reported decreased [5.1 (4.6, 5.6)] monthly HFSS meals portion intakes in November–December compared with pre-pandemic levels. The proportion meeting FV intake recommendations was stable from pre-pandemic through to August–September (70%), but decreased in November–December 2020 (67%, p = 0.034). Increased monthly HFSS snacks intake was associated with female gender, lower quality of life, and – in a time - varying manner – older age and higher HFSS meals intake. Increased monthly HFSS meals intake was associated with female gender, living with adults only, and higher HFSS snacks intake. Reduced FV intake was associated with higher body mass index (BMI) and lower physical activity. These results suggest large interindividual variability in dietary change during the first year of the pandemic, with important public health implications in individuals experiencing persistent increases in unhealthy diet choices, associated with BMI, gender, quality of life, living conditions, physical activity, and other dietary behaviours.
Introduction
2020 has seen widespread disruption to the lives of individuals across the globe due to the COVID-19 pandemic. In the UK, pandemic restrictions were imposed from late March 2020 onwards. Since then, varying levels of restrictions have impacted how individuals and societies live their lives ( 1 ). Restrictions were slowly eased from June until September, before progressively becoming stricter, with full lockdown conditions in December 2020. Diet is a major factor influencing bodyweight, blood pressure, metabolic health, and the risk of non-communicable disease. As such, diet is one of the largest contributors to the burden of disease [as measured using disability-adjusted life years (DALYs)] globally and in the UK ( 2 , 3 ). The widespread disruption to people's lifestyles from the COVID-19 pandemic may result in significant shifts in health behaviours, including diet.
Factors that can impact energy intake and dietary behaviour including food accessibility, changes in work life, home life, stress, and other health behaviours including sleep, physical activity, smoking, and alcohol consumption have been affected by COVID-19 restrictions ( 4 – 7 ). Closures of restaurants and fast food outlets, increased usage of food delivery services, changes in the affordability and availability of foods alongside disruptions to the home and working environment, as well as changes in employment status may all impact diet behaviour during the pandemic ( 8 – 13 ). Indeed, initial reports find that a significant proportion of adults altered their food choices and dietary habits at the start of the pandemic compared to pre-pandemic food choices and habits ( 9 , 14 – 17 ). Despite no overall change in diet quality, there has been large interindividual variability ( 1 , 5 , 14 , 17 – 19 ). A scoping review of 23 studies (17 cross-sectional) from the initial months of the pandemic demonstrate that individuals are making favourable and unfavourable changes to their diet, including changes in snacking, high fat, salt, or sugar (HFSS) food intake, and fruit and vegetable (FV) intake ( 14 ). Significant proportions of people have increased their overall food intake and are snacking more ( 5 , 7 , 14 , 19 , 20 ), but equally people have also decreased their overall food intake and are snacking less ( 1 , 9 , 17 , 19 ).
These changes in diet behaviours during the pandemic are associated with several factors including age, gender, body mass index (BMI), physical activity, and experiencing a larger psychological impact and larger shifts in lifestyle as a result of lockdown restrictions ( 4 , 14 , 21 – 27 ). Given the relationship between a sub-optimal diet and relative risk of cardiovascular disease, cancer, and all-cause mortality, there could be serious long-term public health consequences if the initial unfavourable changes in dietary behaviours during the pandemic are maintained ( 28 , 29 ). Understanding the dietary changes that have occurred, and the key predictors associated with these changes is important to identify at-risk groups of unhealthful dietary change, to inform future interventions, develop targeted approaches, and guide efficient resource allocation. Given the impact of culture on diet and the specific impacts of lockdown restrictions across the globe, it is important to assess the longitudinal impact, including in the UK. However, studies to date assessing the influence of COVID-19 lockdown restrictions on dietary behaviours in UK adults have largely been cross-sectional and undertaken during the initial months of lockdown ( 7 , 14 , 19 ). Some cross-sectional analyses show dietary changes during August–October 2020 compared to the pre-pandemic period ( 1 , 30 , 31 ), and changes in consumer habits during November–December 2020 ( 10 ). Herle et al. identified multiple eating trajectories of UK adults during the initial months of the pandemic, including individuals with an initial increase in eating at the start of the pandemic, followed by a gradual return to pre-pandemic food intake by May 2020 ( 21 ). One longitudinal UK study analysing food purchases found increased calorie intake across 2020 ( 16 ), but longitudinal analyses are scarce ( 16 , 21 , 32 ). Dietary changes compared to pre-pandemic levels and key predictors of any change during the first year of the pandemic to December 2020 in UK adults are largely unknown.
The HEalth BEhaviours during the COVID-19 pandemic (HEBECO) study is a longitudinal UK cohort assessing the impact of the COVID-19 pandemic on health behaviours, and their influences. The objective of this study was to address the following research questions (RQs):
RQ1. What was the average (i) HFSS snacks, (ii) HFSS meals, and (iii) FV intake in UK adults before, at the beginning of, and at 3- and 6-month follow-ups during the COVID-19 pandemic?
RQ2. To what extent are sociodemographic, COVID-19-related, and behavioural factors associated with a change in (i) HFSS snacks, (ii) HFSS meals, or (iii) a reduction in FV intake across 6 months of follow-up during the COVID-19 pandemic compared with pre-pandemic intakes in UK adults?
Materials and Methods
Study design.
The study design has been previously reported ( 33 ). Briefly, this study is a longitudinal analysis of data from an online study of adults, the HEBECO study. 1 The study was approved by the Ethics Committee at the UCL Division of Psychology and Language Sciences (CEHP/2020/759). Participants were self-selected and gave consent prior to data collection. The full recruitment strategy is available online (see footnote 1). Participants were recruited through multiple online channels including paid and unpaid advertisements across social media (Facebook, Google, and Reddit) and mailing lists of UK universities, charities, local government, and networks within Cancer Research UK and Public Health England. Data were captured and managed by the REDCap electronic data system at UCL ( 34 , 35 ). The surveys used in this analysis cover a period of 8 months since the beginning of the pandemic (May–December 2020), as well as a retrospective survey at baseline of the pre-pandemic period. Baseline data were collected between 5 May and 14 June 2020 (inclusive). The 3-months follow-up survey corresponds to the periods of eased pandemic restrictions in the UK during August–September 2020, and the 6-months follow-up survey corresponds to the tighter restrictions in the UK during November–December 2020. The re-introduction of tighter restrictions at the end of 2020 varied across the UK. Tiered restrictions were introduced after a UK-wide lockdown during November and December, with some regions remaining under strict lockdown, and others with more relaxed restrictions. The study protocol and statistical analysis plan were pre-registered on the Open Science Framework prior to analysis. 2 Deviations from the pre-registered protocol are described in the Supplementary Materials . The main study protocol 3 provides further detail on the survey.
Study Sample
The analysis uses data from UK adults (18+) who completed baseline data collection and provided data of interest at the 6-months follow-up survey as a minimum, for the outcome variables defined below.
Full details of outcome and predictor measures can be found in the Supplementary Materials , and have been previously defined ( 33 ).
Participants were asked at baseline, “ Before COVID-19, how often did you usually eat or drink... ” for nine food items: eight HFSS food items [(i) ready meals, (ii) fast food, (iii) takeaways, (iv) sugary or sweetened drinks, (v) sweets or chocolate, (vi) cakes and biscuits, (vii) desserts, and (viii) savoury snacks], and one item for fruit and vegetable intake. For each food item, respondents could answer on a 7-point scale: “A few times per day,” “Once a day,” “A few times per week,” “Once a week,” “A few times per month,” “Once a month,” “Less often/never,” and “Not sure.” Participants were also asked at baseline “ Since COVID-19, how often did you usually eat or drink... ,” and then at 3- and 6-month follow-ups, “ In the past month, how often did you usually eat or drink... ” for the same nine food items. The HEBECO study food item questions are based on previous research study survey questions, and are derived from Public Health England's sugar reduction programme definitions as policy-relevant measures ( 36 – 38 ).
To estimate monthly portion intake frequency, responses for all food item questions were converted into monthly portion frequencies, based on previous research ( 33 ). Assuming a minimum of 4 weeks per calendar month, an answer of “A few times per day” was scaled up to 56 portions per month (i.e., 2 daily portions × 7 days × 4 weeks), “Once a day” was scaled up to 28 portions per month, “Few times per week” as 12 portions per month, “Once a week” as 4 portions per month, “Few times per month” as 2 portions per month, “Once a month” as 1 portion per month, and “Less often/never” as 0.5 portions per month.
Using the above monthly portion intake frequencies, (iv) sugary or sweetened drinks, (v) sweets or chocolate, (vi) cakes and biscuits, (vii) desserts, and (viii) savoury snacks monthly frequencies were summed to produce a “HFSS snacks intake” monthly portion frequency. (i) Ready meals, (ii) fast food, and (iii) takeaways monthly frequencies were summed to produce a “HFSS meals intake” monthly portion frequency. The change scores “Change in self-reported HFSS snacks intake” and “Change in self-reported HFSS meals intake” used as outcomes in RQ2 were computed from pre-pandemic HFSS snacks and HFSS meals intakes retrospectively reported at baseline, which were deducted from HFSS snacks and HFSS meals intakes reported at the time of the baseline survey, and at 3- and 6-month follow-up surveys.
FV intake was converted into a binary outcome variable, grouped into “Consuming a few portions per day of fruit and vegetables” (responses of “A few times per day”) vs. “Less than a few portions per day” (all other responses besides “A few times per day”). This cut-off was used to reflect health recommendations for several daily portions of fruit and vegetables ( 39 ). The binary change score used as the outcome in RQ2 was computed as a categorical reduction (“Reduced intake” vs. “All other”) in FV intake at the time of the baseline survey, and at 3- and 6-month follow-up surveys, compared to pre-pandemic levels retrospectively reported at baseline.
HFSS snacks intake was the primary outcome of interest, given that a systematic review identified large changes in snacking during the initial months of the pandemic ( 19 ), which in turn have been associated with self-reported weight change during the pandemic ( 5 , 40 , 41 ).
Explanatory Variables
Time-invariant.
Explanatory variables recorded at baseline included gender (female vs. all other), age (continuous), ethnicity (white vs. all other), occupation and work from home (categorical: unemployed (which includes retired persons and full-time parents/carers), employed and working from home, employed and not working from home), living arrangements (living alone, living with children (with or without adults), living with adults only), and a socioeconomic score . The socioeconomic score (categorical score from 0–3) was based on household income, housing status, and level of education; participants scored 0 if they had an income <£50,000, lived in unowned housing and had no higher education, or scored 1, 2, or 3 if participants met 1, 2, or all 3 criteria of having an income of ≥£50,000, owning their housing/having a mortgage, or having higher education. The current cohort had a higher income on average than the average UK income. As such, £50,000 was used as the cut-off point.
Sensitivity analyses also included an unhealthy eating through boredom, stress, or comfort variable. This measure was not included in the main RQ2 analysis as not all participants were shown the question to reduce participant burden. At baseline, participants were asked to what extent they agreed with the following statements: “ I eat unhealthy food out of boredom ,” “ I eat unhealthy food because I'm stressed ,” “ I eat unhealthy food because it's comforting” on a 0–100 scale, where 0 = completely disagree; 50 = neutral; and 100 = completely agree. A continuous mean score (0–100) was computed for eating for comfort, stress, and from boredom. A higher score indicated eating unhealthy food out of boredom, stress, or comfort.
Time-Variant
Explanatory variables reported at baseline, 3-, and 6-month follow-up surveys included BMI (continuous: self-reported weight in kilograms divided by self-reported height in metres squared), isolation status (total/some isolation vs. general/no isolation), quality of life , an average continuous rating from 1-5 of quality of living, wellbeing, social and family relationships (1 = poor, 5 = excellent), and health behaviours as detailed below.
Physical activity was a continuous measure of metabolic equivalent (MET)-hours per week. At each time point, participants self-reported the number of days they performed strengthening physical activity (SPA) per week, and the number of days and average duration of a session of moderate or vigorous physical activity (MVPA) per week. The number of days performing SPA per week was multiplied by an average session duration of 45 minutes and multiplied by 4 to convert to MET-minutes per week, to reflect the nature of SPA as moderate- to high-intensity bouts, interspersed with rest periods ( 42 ). The 45-min length reflects the American College of Sports Medicine recommendations for the typical number of exercises, reps, sets, and duration of rest periods for a resistance training session ( 43 , 44 ). MVPA number of days per week was multiplied by the self-reported average session length, and then multiplied by 6 to convert to MET-minutes per week, as an average of moderate and vigorous physical activity ( 45 ). Scores were then summed for SPA and MVPA and divided by 60 to produce a MET-h per week score. An upper limit of 4 standard deviations above the mean MET-h per week was applied, as some individuals self-reported activity levels not physically possible. This upper limit corresponded to ~8 h of moderate physical activity per day, which is several standard deviations above the physical activity levels reported from large observational studies ( 46 ).
Alcohol consumption was based on government low-risk drinking recommendations (≤14 weekly alcohol units vs. >14 weekly alcohol units) ( 47 ), and smoking status was based on the self-reported use of tobacco or cigarettes (yes vs. no).
HFSS snacks intake, HFSS meals intake , and FV intake were also used as continuous explanatory variables (but excluded in analyses of the same kind, e.g., HFSS snacks intake was excluded from “Change in self-reported HFSS snacks intake” analyses).
Statistical Analysis
Statistical analysis was conducted in SPSS Statistics version 27 (IBM). Significance was defined as p < 0.05.
We described baseline participant characteristics in RQ1 [weighted participant characteristics, based on census data from the Office for National Statistics for age, gender, country of living, ethnicity, education, and income are presented in the Supplementary Materials ( 48 )].
We reported the unweighted means with 95% confidence intervals (95% CI) for HFSS snacks and HFSS meals monthly portion intake and the proportion consuming a few portions of FV per day at each timepoint. We also reported the percentage of the sample increasing or decreasing HFSS snacks or HFSS meals intake, or categorically increasing or decreasing FV intake from the reference timepoint (pre-pandemic levels reported at baseline, levels during May–June 2020 reported at baseline, or at 3-months follow-up). Lastly, we reported the mean change in portion frequency (with 95% CI) in those increasing or decreasing HFSS snacks or HFSS meals intake between timepoints.
Given that more distantly spaced participant measures over time are expected to be less closely correlated ( 49 ), an unadjusted, unweighted generalised estimating equation (GEE) using the AR(1) covariance structure was used to assess changes in self-reported HFSS snacks and HFSS meals monthly portion intake over time, using pairwise time comparisons between timepoints, adjusted for with sequential Šidák correction.
GEE models were used to determine the association between the explanatory variables and (i) changes in HFSS snacks intake and (ii) changes in HFSS meals intake across the follow-up period. The GEE models for a change in HFSS snacks and HFSS meals monthly portion intake used the identity link function for a linear scale response, as the change scores were normally distributed continuous outcome variables. The GEE models for FV used a binary logistic model and logit link function for the binary outcome variable (reduced FV intake vs. all other).
Univariate GEE models were computed to determine the association between each explanatory variable and changes in HFSS snacks intake, changes in HFSS meals intake, and a reduction in FV intake. Each explanatory variable model was adjusted for a main effect of time and for an “explanatory variable * time” interaction. Fully adjusted GEE models containing all explanatory variables were then computed.
All significant explanatory variable * time interactions were then added to the fully adjusted GEE model containing all explanatory variables, to assess temporal differences in the association of explanatory variables with continuous changes in HFSS snacks and HFSS meals monthly portion intake, or a reduction in FV intake over time. The time variable was categorical, as the trajectory of change in dietary intakes was not expected to be linear ( 50 ). Explanatory variable * time interactions were retained in the full GEE model if they improved goodness of fit [Quasi-likelihood under Independence Model Criterion (QIC) QIC > 2] over the full GEE model without interactions, and the interaction itself remained significant ( p < 0.05).
Independent variables were retained after checking for collinearity using Pearson correlations, with all correlations r < 0.4.
For binary outcomes using the logit link function, linearity of logit assumptions were checked, as detailed in the Supplementary Materials .
Sensitivity Analyses
The supplementary analyses used complete cases only (those participants completing all dietary measures at all three surveys: baseline, 3-, and 6-month follow-ups). Further analyses were then conducted for the primary outcome of HFSS snacks intake using two binary logistic GEE models with logit link function for an “increase” in HFSS snacks intake vs. “all other,” and a “decrease” in HFSS snacks intake vs. “all other.” A change was defined as an increase or decrease in intake by 10% or more from pre-pandemic intakes retrospectively self-reported at baseline, based on a cut-off used in a previous large study of dietary intakes during the pandemic ( 4 ).
Analyses were repeated for the sub-sample of participants self-reporting eating behaviour measures. Univariate GEE models were computed for changes in HFSS snacks intake, changes in HFSS meals intake, and a reduction in FV intake outcomes using the unhealthy eating through boredom, stress, or comfort variable. Unhealthy eating through boredom, stress, or comfort was also added to the fully adjusted GEE models (with and without significant time interactions from the univariate models).
Multiple observations in the literature have indicated that gender, smoking, and physical activity are likely related to changes in snacking behaviour during the pandemic ( 4 , 7 ). Bayes Factor analyses were pre-registered online in the event of non-significant findings for gender, smoking, and physical activity with change in HFSS snacks intake in the main analysis. 4 Snacking Bayes factors prior mean differences were obtained from differences in change in daily energy intake from before COVID-19 to since COVID-19 between predictors and converted into snacking portions per month (further details can be found in the Supplementary Materials ). Alternative hypotheses were modelled using a half-normal distribution with a peak at zero, given that smaller effect sizes nearer to null are more likely than larger effect sizes ( 51 , 52 ). The standard deviation (SD) was set to 5.32 for gender, 7.35 for physical activity, and 11.17 for smoking for a change in HFSS snack portions per month ( 4 ). Bayes factors were calculated using an online calculator: http://bayesfactor.info/ .
Out of a total of 2,992 UK adult participants recruited into the HEBECO baseline survey, 1,733 (weighted = 1,532) participants met the inclusion criteria for analyses. The unweighted baseline characteristics are shown in Table 1 (for weighted characteristics, see Supplementary Table 1 ). Included participants were more likely to be female, older, of white ethnicity, have a higher BMI, be unemployed (which includes retired persons and full-time parents/carers), have a higher socioeconomic score, live with adults only, be in total or some isolation, have a higher quality of life score, consume fewer HFSS meals, consume more FV, and be less likely to smoke.
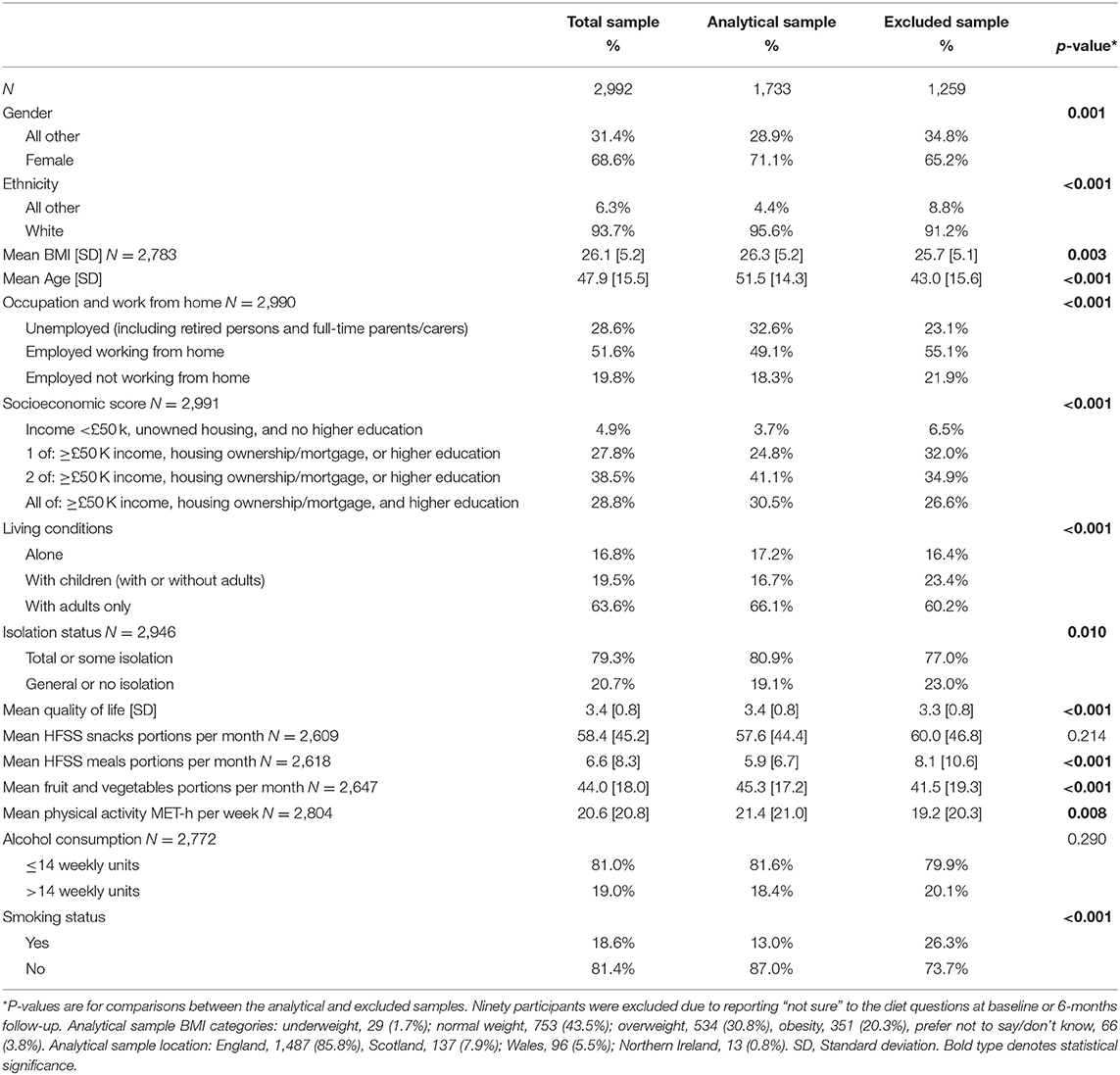
Table 1 . Unweighted baseline participant characteristics for included, excluded, and total samples.
What Were the Intakes of HFSS Snacks, Meals, and FV in UK Adults Before, at the Beginning of, and at 3- and 6-Month Follow-Ups During the COVID-19 Pandemic?
HFSS snacks monthly portion intake increased from before the pandemic to the start of the pandemic (by May–June 2020) (48.3 to 57.6 per month, p < 0.001; Figure 1 ). At 3-months follow-up (by August–September 2020), HFSS snacks monthly portion intake significantly decreased (to 43.7 per month, p < 0.001). At 6-months follow-up (by November–December 2020), HFSS snacks monthly portion intake significantly increased (to 49.2 per month, p < 0.001) to intakes that were not significantly different to retrospectively reported intakes before the pandemic ( p = 0.297).
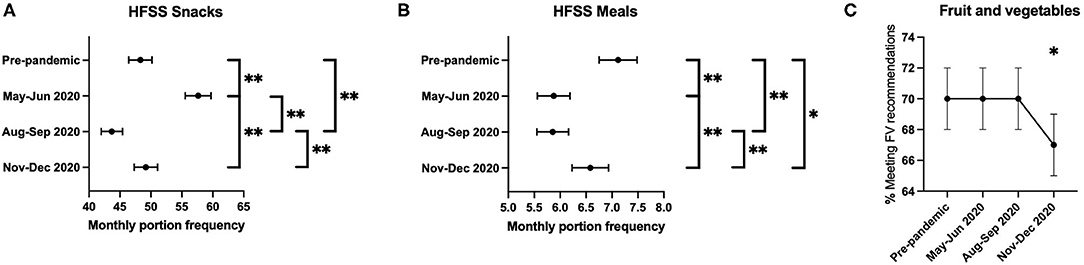
Figure 1. (A–C) Means, 95% confidence intervals, and pairwise comparisons between pre-pandemic, baseline (May–June 2020), 3-month (August–September 2020), and 6-month (November–December 2020) follow-up surveys. *Denotes pairwise comparisons between categories were significant at the 0.05 level. **Denotes pairwise comparisons comparisons between categories were significant at the 0.005 level.
HFSS meals monthly portion intake decreased from before the pandemic to the start of the pandemic (by May–June 2020) (7.1 to 5.9 per month, p < 0.001; Figure 1 ). At 3-months follow-up (by August–September 2020), HFSS meals monthly portion intake was maintained (5.9 per month, p = 0.897). At 6-months follow-up (by November–December 2020), HFSS meals monthly portion intake significantly increased (5.9–6.6 per month, p < 0.001) to intakes that were significantly lower than retrospectively reported intakes before the pandemic (7.1 to 6.6 per month, p = 0.007).
For FV intake, 70% [95% CI: 68, 72] were consuming a few portions per day before the pandemic, at the start of the pandemic [95% CI: 68, 72] (May–June 2020), and at 3-months follow-up [95% CI: 68, 72] (August–September 2020), but this significantly decreased to 67% [95% CI: 65, 69] ( p = 0.034) at 6-months follow-up (November–December 2020) ( Figure 1 ).
From the pre-pandemic period to 6-months follow-up (November–December 2020), 48.5% of individuals self-reported an increase in HFSS snacks intake, by an average of 25.9 [95% CI: 24.1, 27.8] portions per month. A similar proportion (47.7%) reported a decrease in HFSS snacks intake, by an average of 24.1 [95% CI: 22.4, 25.9] portions per month ( Table 2 ). From pre-pandemic to 6-months follow-up, 35.2% of individuals self-reported an increase in HFSS meals intake, by an average of 4.8 [95% CI: 4.3, 5.3] portions per month. A total of 44.5% self-reported a decrease in HFSS meals intake, by an average of 5.1 [95% CI: 4.6, 5.6] portions per month. For FV intake, 11.4% were no longer meeting daily FV intake recommendations, and 8.4% were now meeting daily FV intake recommendations at 6-months follow-up compared with pre-pandemic levels.
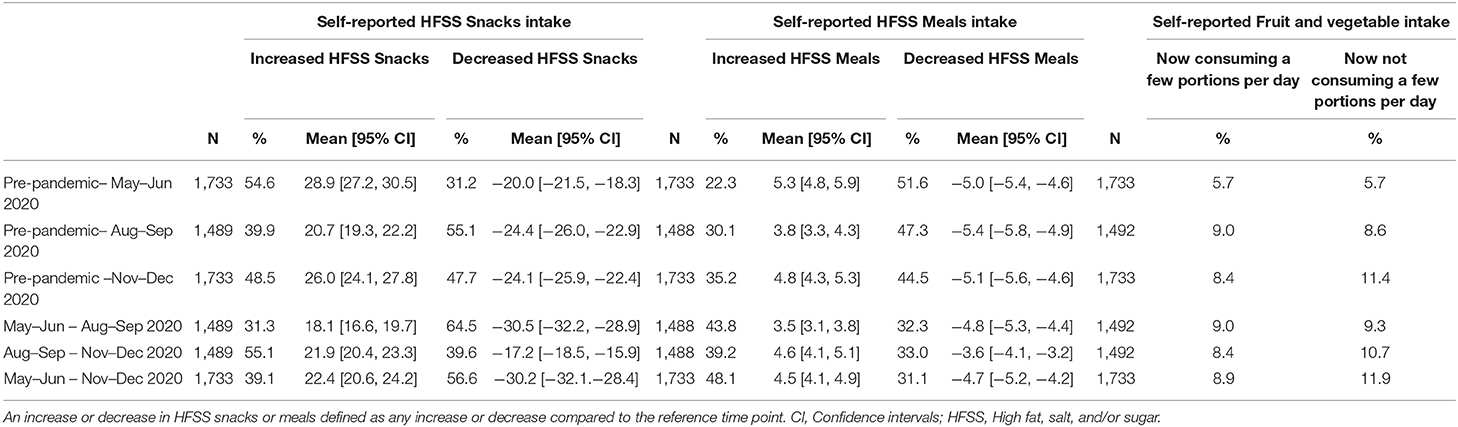
Table 2 . Unweighted proportions increasing or decreasing HFSS snacks, HFSS meals, and fruit and vegetables intake, and mean changes with 95% confidence intervals in HFSS snacks and HFSS meals intake.
The changes in portion frequency consumption across the pandemic for each food item is shown in Supplementary Figure 1 .
Which Explanatory Variables Were Associated With Changes in Monthly HFSS Snacks and Meals Intakes, or a Reduction in FV Intake in UK Adults Across 6 Months of Follow-Up During the COVID-19 Pandemic?
In the unadjusted GEE models ( Supplementary Table 2 ), female gender, higher baseline BMI, total or some isolation, a lower quality of life score, a higher HFSS meals intake, and lower physical activity levels were significantly associated with an increase in self-reported HFSS snacks intake across 6 months of follow-up during the pandemic. In the fully adjusted GEE model ( Table 3 ), female gender [ B = 6.568 (95% CI: 3.653, 9.483)] and a lower quality of life score [ B = −2.882 (95% CI: −4.387, −1.377)] were associated with an increase in monthly HFSS snacks intake across the pandemic. HFSS meals intake was also significantly associated with a change in monthly HFSS snacks intake across the pandemic, but this was time-varying. Similarly, age showed significant time interactions and improved model fit.
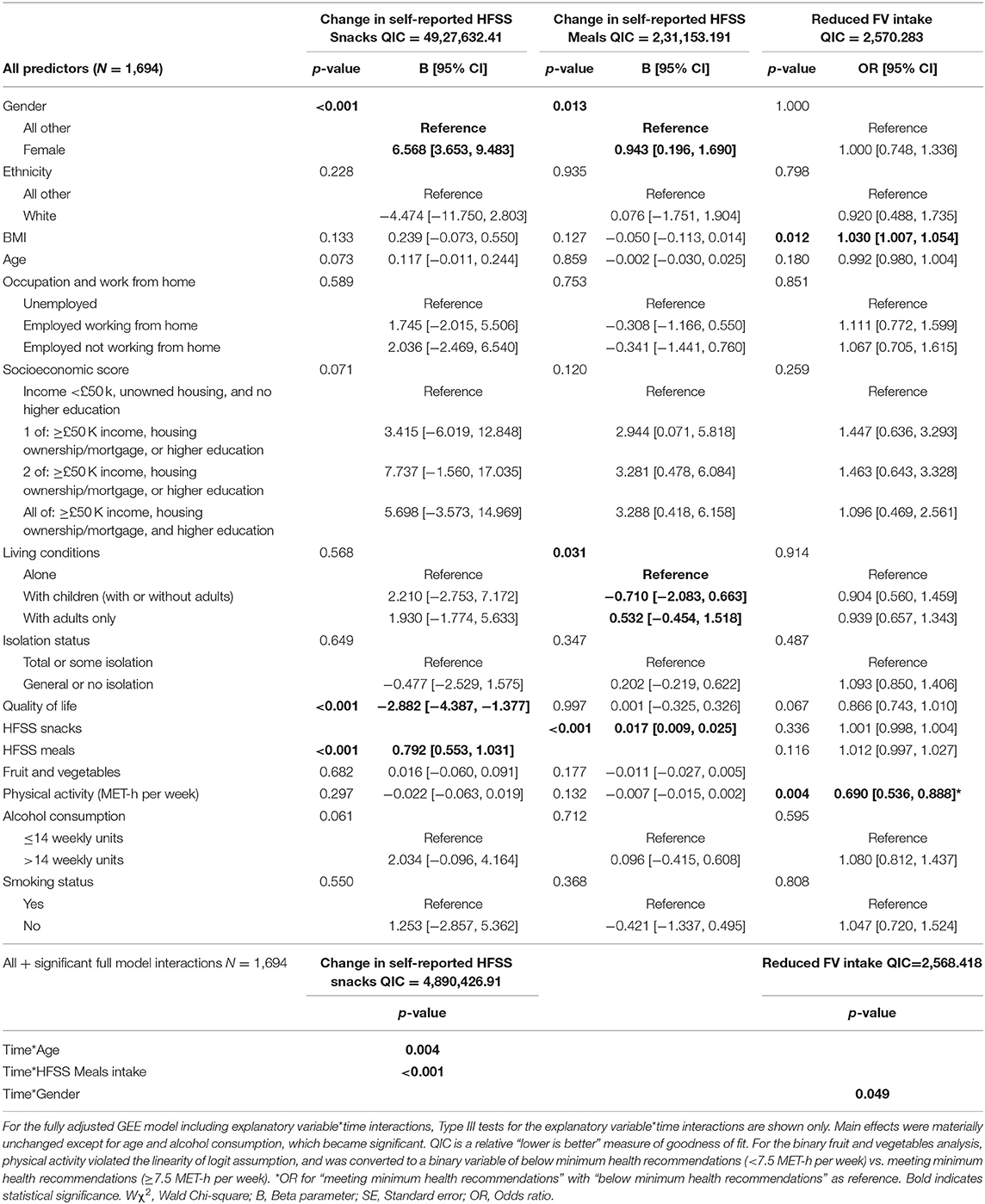
Table 3 . Fully adjusted GEE model containing all predictor variables and the fully adjusted GEE model including significant explanatory variable * time interactions.
Figure 2 exhibits the time-varying associations of age and HFSS meals intake with a change in HFSS snacks intake across the pandemic. All ages increased HFSS snacks intake at the start of the pandemic, but younger ages tended to decrease HFSS snacks intake during the latter months of 2020 (November–December 2020), whereas older ages tended to maintain or increase intakes from pre-pandemic levels. Higher HFSS meals intakes were associated with larger increases in HFSS snacks intake at the start of the pandemic (May–June), with higher and lower HFSS meals intakes decreasing HFSS snacks intake at 3-months follow-up (August–September). Individuals with a higher HFSS meals intake then returned to, or increased HFSS snacks intake above pre-pandemic levels at 6-months follow-up, whereas those with lower HFSS meals intakes maintained the reduced HFSS snacks intake.
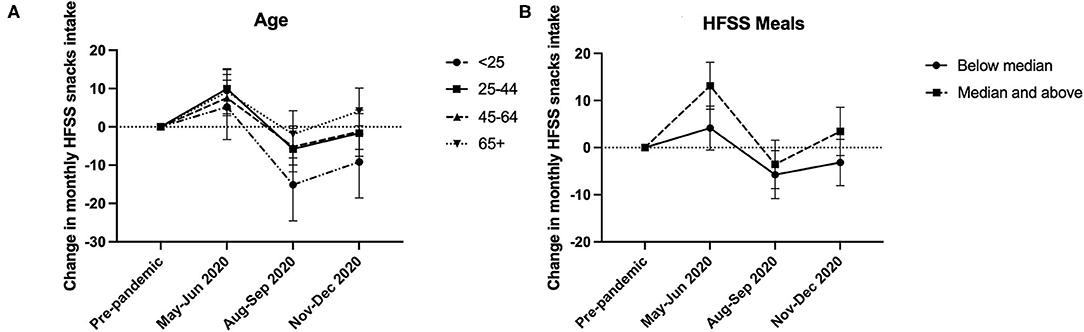
Figure 2 . Graphical illustrations of the time-varying associations of (A) age and (B) HFSS meals intake with change in monthly HFSS snacks intake at baseline (May–June 2020), 3-month (August–September 2020), and 6-month follow-ups (November–December 2020) compared with pre-pandemic intakes.
In the unadjusted GEE models of HFSS meals intake ( Supplementary Table 2 ), female gender and a higher HFSS snacks intake were associated with an increase in HFSS meals across the pandemic. In the fully adjusted GEE model ( Table 3 ), female gender [ B = 0.943 (95% CI: 0.196, 1.690)], living with adults only [ B = 0.532 (95% CI: −0.454, 1.518)], and higher intakes of HFSS snacks [ B = 0.017 (95% CI: 0.009, 0.025)] were associated with an increase in HFSS meals intake across the pandemic. There were no significant explanatory variable * time interactions.
In the unadjusted GEE models of FV intake ( Supplementary Table 2 ), higher BMI, lower socioeconomic score, general or no isolation (compared with total or some isolation), lower quality of life, higher HFSS meals intake, and lower physical activity levels were associated with a reduction in FV intake. In the fully adjusted GEE model ( Table 3 ), reduced FV intake across the pandemic was associated with a higher BMI [odds ratio (OR) = 1.030 (95% CI: 1.007, 1.054)] and lower physical activity levels [OR = 0.690 (95% CI: 0.536, 0.888)]. A gender interaction with time while significant, did not improve model fit and was not retained.
Complete case analyses of RQ1 and RQ2 demonstrated materially unchanged differences in HFSS snacks and HFSS meals intakes across timepoints and in adjusted analyses compared with the main analysis ( Supplementary Tables 3 – 5 ). For a change in FV intake, however, the gender interaction with time improved model fit and remained significant when added to the fully adjusted model, as shown in Supplementary Figure 2 .
Unadjusted analyses of binary outcomes for HFSS snacks used in the sensitivity analysis are presented in Supplementary Table 6 . In the full binary logistic GEE models for an increase or decrease in HFSS snacks intakes vs. all other, female gender, a higher BMI, a lower quality of life score, and a higher HFSS meals intake were more likely to increase HFSS snacks intake across the pandemic ( Supplementary Table 7 ). Non-female gender, younger age, higher quality of life, lower HFSS meals intake, and low-risk alcohol consumption were associated with decreased HFSS snacks intake across the pandemic. Age and alcohol consumption interactions had a time-varying impact on increased HFSS snacks intake vs. all other ( Supplementary Figure 3 ). There were no significant explanatory variable * time interactions for a decrease in HFSS snacks vs. all other ( Supplementary Table 6 ).
Unadjusted analyses of unhealthy eating through boredom, stress, or comfort are also presented in Supplementary Table 8 . In fully adjusted GEE models including unhealthy eating through boredom, stress, or comfort, a higher score was significantly associated with an increase in HFSS snacks intake ( Supplementary Table 9 ). Unhealthy eating through boredom, stress, or comfort had a time-varying impact ( Supplementary Figure 4 ).
Because of the null findings reported here for smoking status on a change in HFSS snacks intake, Bayes factors were calculated. The Bayes factor suggests the data provided evidence for no effect of smoking status (BF = 0.32) on change in HFSS snacks intake.
In this study of a sample of UK adults, initial average trends in HFSS snacking and meal consumption are not maintained across the pandemic. There is substantial interindividual variability, with some individuals experiencing long-term, unhealthy dietary behaviour changes. Combined, our results suggest that gender, BMI, living conditions, quality of life, other dietary behaviours, and physical activity are associated with adverse self-reported dietary behaviour changes.
In Context of COVID-19 Research
Reviews from the initial months of the pandemic indicate an overall trend for increased food consumption ( 7 , 53 ), with increased FV consumption in some individuals, but also increased HFSS foods consumption in others ( 6 , 54 ). In particular, increased snacking has been identified during the start of the pandemic ( 19 , 54 – 56 ), with a greater proportion of individuals increasing than decreasing HFSS snacks intake ( 19 , 54 ), as with our results.
Dietary changes can have both protective and harmful impacts on health and well-being. Understanding the contexts associated with dietary changes is central to developing targeted interventions. Female gender, higher BMI, lower quality of life, reduced physical activity, and experiencing a greater negative impact from the pandemic have been previously recognised as predictors of unhealthy dietary changes during the pandemic ( 55 , 57 , 58 ). Our study builds upon the current literature, showing these factors are important long-term predictors of adverse dietary change during the pandemic.
Pandemic-related dietary changes may have occurred from shop closures, or changes in food availability, accessibility, or shopping habits ( 31 , 55 ). Increased HFSS snacking at the start of the pandemic may have resulted from convenience, or greater inconvenience of accessing fresh foods ( 55 , 59 ). Given their high availability, affordability, and long shelf-life, individuals may have prioritised HFSS snacks over fresh foods from the uncertainty over food supply during the pandemic ( 55 , 59 – 61 ).
In our study, a lower quality of life or unhealthy eating through stress, boredom, or comfort was associated with unhealthy changes in HFSS foods intake during the first year of the pandemic. Individuals tend to consume more palatable and less healthy foods during stressful life periods ( 62 ). A greater decline in mental health or increased stress, boredom, or anxiety from COVID-19 has been associated with increased ultra-processed, HFSS foods intake, decreased FV intake, and using snacking as a coping mechanism ( 9 , 14 , 32 , 55 , 56 , 63 – 65 ). The increased HFSS snacking at the start of the pandemic may reflect such maladaptive coping mechanisms ( 63 , 66 ). For some individuals, the increase may have been maintained through strengthening of a cue-trigger-reward feedback cycle and habit formation ( 67 ).
At the start of the UK lockdown in 2020, being female (vs. not) was associated with greater dietary changes, namely to consistently eat less, and to eat more ( 21 ). There may be psycho-social, cultural, and environmental reasons for this possible difference. For example, it is more likely for females to use any form of coping strategy than males ( 68 ). UK females also experienced greater disruption to sleep at the start of the pandemic ( 69 ), which can alter dietary behaviour ( 70 ). The association between female gender and self-reported adverse dietary behaviour changes in this study may therefore reflect maladaptive coping strategies of female participants, with a reduction in healthy foods consumption, and increases in unhealthy foods consumption. The initially high levels of COVID-19-related stress experienced by women at the start of the pandemic declined, which may suggest women then formed unhealthy dietary habits ( 71 , 72 ).
We found that living with adults was associated with increased HFSS meals intake. Higher numbers of adults were shown to consume more meals per day during the second COVID-19 wave in the UK (October 2020) compared with pre-pandemic, with increases in both ready meals and homemade meals ( 30 ). More shared mealtimes during lockdown may have altered eating behaviours ( 73 ), with existing or changing HFSS meal habits of some adults in the household potentially influencing the dietary habits of others ( 73 ).
Policy Implications
The World Health Organisation recommends limiting HFSS foods to reduce the risk of weight gain, cardiovascular disease, and high blood pressure ( 55 , 74 ). In the UK, average free sugar and saturated fat consumption exceeds recommendations, and average FV intakes are below recommendations ( 31 , 75 ). This study suggests the pandemic is associated with long-term adverse changes in dietary behaviours, which could amplify the existing sub-optimal dietary patterns of UK adults. A poor diet is the largest behavioural risk factor for DALYs lost ( 3 ) and second only to smoking for years of life lost ( 76 ), indicating a strong need for policy action to help individuals make healthy dietary choices. The pandemic has impacted people differently, therefore strategies need to consider and prioritise those who might be vulnerable to sustained unhealthy dietary changes (e.g., women, older individuals, or the physically inactive), and those who face greater barriers to healthy change.
The new UK government obesity campaign needs to not only ensure that HFSS foods are less accessible (e.g., placing lower limits on cost or limiting advertising), but also ensure that healthier options such as fruit and vegetables are more accessible (i.e., cheaper or more readily available) ( 77 , 78 ). COVID-19 restrictions have altered the work-life balance for many individuals. Strategies need to consider the social impact from changes in household dynamics in the COVID-19 era on dietary behaviours and how to incorporate healthy eating into social norms and identities ( 79 ). Given the impact of COVID-19 on face-to-face communication and increased telecommunication, remotely accessible resources should be made available for successful behavioural change and habit formation, promoting autonomy and satisfaction from healthful dietary changes ( 67 ).
Strengths and Limitations
There are several strengths of this study. This is one of the first studies in UK adults examining changes in dietary behaviours and predictors of dietary change across the first year of the COVID-19 pandemic, from May to December 2020 compared with pre-pandemic. The longitudinal nature builds upon the largely cross-sectional current literature, providing a greater understanding of the long-term impacts of the pandemic on dietary behaviour. The analysis included a range of variables that reflect the wide-ranging impact of the pandemic, with time-varying measures to reflect the changing conditions of the pandemic over time. A range of health behaviours were also considered that are important for dietary behaviour. The use of GEE models for the longitudinal analysis provided several advantages over common analytical methods, including the ability to handle repeated measures, model different data distributions, and use time-varying predictors. Complete case analyses and sensitivity analyses with binary cut-offs demonstrating largely similar associations indicate the robustness of the associations identified in this study.
However, there are several limitations which may have introduced bias. First, the study sample was self-selected and largely female, older, and well-educated. Second, there were differences in various characteristics between included and excluded participants. Included participants were more likely to be female, of white ethnicity, and have a higher socioeconomic score, which may limit the generalisability of results. It cannot be ruled out that the associations between female gender and adverse self-reported dietary changes are an artefact of sample selection. Third, causality cannot be concluded from the observational study design. Fourth, measures of interest were self-reported; however epidemiological studies during COVID-19 have been largely self-reported, and dietary assessments in general are routinely self-reported ( 80 ). The survey did not include a complete dietary analysis of all food groups or energy intake. Individuals generally tend to underestimate energy intake, and more so in individuals living with being overweight or obesity ( 80 , 81 ). However, this study focused on key food groups and their frequency of consumption, including HFSS foods and fruit and vegetables. Furthermore, self-reported dietary data still hold important value to inform health policy ( 82 ). Assessing fruit and vegetable intake using separate questions may have provided further insights into self-reported dietary changes. Using dietary change scores as the outcome variables enabled participants to act as their own controls which helped to minimise within-subject measurement error. Participants were also not explicitly asked if their diet had changed, nor told that dietary change was an outcome of interest, reducing the risk of expectation bias. The use of several diet recalls at each survey would help to strengthen the study findings. Fifth, participants were asked about their behaviours in the past week or month, which may have introduced a recall bias. Sixth, the survey focused on HFSS snacking specifically, rather than any snacking. However, most studies to date have considered HFSS snacks ( 19 ). Seventh, the unhealthy eating through boredom, stress, or comfort variable was based on a visual analogue scale using relevant questions to assess influences on eating. However, use of a validated eating behaviour measure may have aided generalisability of results. Eighth, our results are presented for the UK as a whole. There were varying restrictions across the UK during the November–December follow-up study, which may have differently impacted individuals. However, isolation status was not significantly associated with dietary changes. The window for completing the 6-months follow-up survey combined with the variation in imposing stricter restrictions during December within the same region means that participants may have completed the survey under different levels of restrictions.
While HFSS snacks intake fluctuated across the first year of the pandemic, it returned to pre-pandemic levels by the end of 2020. In contrast, HFSS meals also fluctuated but remained below pre-pandemic levels by November–December 2020. FV intake, while initially stable, decreased by the end of the year compared with pre-pandemic levels. These changes at population level do however, mask large interindividual changes in dietary behaviours, driven by differences in anthropometric (BMI), sociodemographic (gender), lifestyle (quality of life and living conditions), and behavioural (other dietary choices and physical activity levels) factors.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by UCL Division of Psychology and Language 1220 Sciences (CEHP/2020/759). Participants provided their informed consent to participate in this study.
Author Contributions
SD, JM, JN, EB, DK, AH, and LS: conceptualisation and methodology. EB: statistical support. SD and JM: formal analysis. SD: first manuscript draft. EB, LS, DK, and AH: writing—review and editing. AH and LS: supervision. All authors approved the final manuscript.
This project was partially funded by an ongoing Cancer Research UK Programme Grant to UCL Tobacco and Alcohol Research Group (C1417/A22962) and by SPECTRUM, a UK Prevention Research Partnership Consortium (MR/S037519/1). SD and JM are funded by an MRC grant (MR/N013867/1).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer LS declared a shared affiliation with the authors to the handling Editor at time of review.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2021.788043/full#supplementary-material
Abbreviations
BF, Bayes factor; BMI, body mass index; CI, confidence interval; DALYs, disability-adjusted life years; FV, fruit and vegetables; GEE, generalized estimating equation; HEBECO, HEalth BEhaviours during the COVID-19 pandemic; HFSS, high fat, salt, and/or sugar; MET, metabolic equivalent; MVPA, moderate to vigorous physical activity; OR, odds ratio; SD, standard deviation; SPA, strengthening physical activity; QIC, Quasi-likelihood under Independence Model Criterion; WHO, World Health Organisation.
1. ^ https://osf.io/sbgru/
2. ^ https://osf.io/279zd/
3. ^ https://osf.io/mav3y/
4. ^ https://osf.io/279zd/
1. Mazidii M, Leeming E, Merino J, Nguyen L, Selvachandran S, Maher T, et al. Impact of COVID-19 on health behaviours and body weight: a prospective observational study in a cohort of 1.1 million UK and US individuals. Res Squ [Preprint]. (2021). doi: 10.21203/rs.3.rs-179013/v1
CrossRef Full Text | Google Scholar
2. Stanaway JD, Afshin A, Gakidou E, Lim SS, Abate D, Abate KH, et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1923–94. doi: 10.1016/S0140-6736(18)32225-6
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Newton JN, Briggs ADM, Murray CJL, Dicker D, Foreman KJ, Wang H, et al. Changes in health in England, with analysis by English regions and areas of deprivation, 1990-2013: a systematic analysis for the Global Burden of Disease Study (2013). Lancet Lond Engl. (2015) 386:2257–74. doi: 10.1016/S0140-6736(15)00195-6
4. Deschasaux-Tanguy M, Druesne-Pecollo N, Esseddik Y, de Edelenyi FS, Allès B, Andreeva VA, et al. Diet and physical activity during the coronavirus disease 2019 (COVID-19) lockdown (March–May 2020): results from the French NutriNet-Santé cohort study. Am J Clin Nutr . (2021). 113:924–38. doi: 10.1093/ajcn/nqaa336
5. Khan MA, Menon P, Govender R, Samra A, Nauman J, Ostlundh L, et al. Systematic review of the effects of pandemic confinements on body weight and their determinants. Br J Nutr . (2021) 2021:1–74. doi: 10.1017/S0007114521000921
6. Doraiswamy S, Cheema S, Al Mulla A, Mamtani R. COVID-19 lockdown and lifestyles: a narrative review. F1000Research. (2021) 10:363. doi: 10.12688/f1000research.52535.1
7. Chew HSJ, Lopez V. Global impact of COVID-19 on weight and weight-related behaviors in the adult population: a scoping review. Int J Environ Res Public Health. (2021) 18:1876:1–1876:27. doi: 10.3390/ijerph18041876
8. Wielgoszewska B, Maddock J, Green MJ, Gessa GD, Parsons S, Griffith GJ, et al. The UK coronavirus job retention scheme and changes in diet, physical activity and sleep during the COVID-19 pandemic: evidence from eight longitudinal studies. MedRxiv [Preprint] . (2021) 2021:2021.06.08.21258531. doi: 10.1101/2021.06.08.21258531
9. Robinson E, Boyland E, Chisholm A, Harrold J, Maloney NG, Marty L, et al. Obesity, eating behavior and physical activity during COVID-19 lockdown: a study of UK adults. Appetite. (2021) 156:104853. doi: 10.1016/j.appet.2020.104853
10. Ogundijo DA, Tas AA, Onarinde BA. Exploring the impact of COVID-19 pandemic on eating and purchasing behaviours of people living in England. Nutrients. (2021) 13:1499. doi: 10.3390/nu13051499
11. Albalawi A, Hambly C, Speakman JR. The impact of the novel coronavirus movement restrictions in the United Kingdom on food outlet usage and body mass index. Obes Sci Pract. (2021) 7:302–6. doi: 10.1002/osp4.477
12. Kubo Y, Ishimaru T, Hino A, Nagata M, Ikegami K, Tateishi S, et al. A cross-sectional study of the association between frequency of telecommuting and unhealthy dietary habits among Japanese workers during the COVID-19 pandemic. MedRxiv [Preprint] . (2021) 2021:2021.06.28.21259558. doi: 10.1101/2021.06.28.21259558
13. Salon D, Conway MW, Silva DC da, Chauhan RS, Derrible S, Mohammadian A (Kouros), et al. The potential stickiness of pandemic-induced behavior changes in the United States. Proc Natl Acad Sci USA. (2021) 118:e2106499118. doi: 10.1073/pnas.2106499118
14. Bennett G, Young E, Butler I, Coe S. The impact of lockdown during the COVID-19 outbreak on dietary habits in various population groups: a scoping review. Front Nutr. (2021) 8:626432. doi: 10.3389/fnut.2021.626432
PubMed Abstract | CrossRef Full Text
15. Wilson JJ, McMullan I, Blackburn NE, Klempel N, Yakkundi A, Armstrong NC, et al. Changes in dietary fat intake and associations with mental health in a UK public sample during the COVID-19 pandemic. J Public Health Oxf Engl. (2021) 2021:fdab009. doi: 10.1093/pubmed/fdab009
16. Stroud R, Smith K, O'Connell M. The dietary impact of the COVID-19 pandemic. IFS. (2021). doi: 10.1920/wp.ifs.2021.1821 Available online at: https://ifs.org.uk/publications/15503
17. Buckland NJ, Swinnerton LF, Ng K, Price M, Wilkinson LL, Myers A, et al. Susceptibility to increased high energy dense sweet and savoury food intake in response to the COVID-19 lockdown: the role of craving control and acceptance coping strategies. Appetite. (2021) 158:105017. doi: 10.1016/j.appet.2020.105017
18. Food Standards Agency. The COVID-19 Consumer Research . Food Standards Agency (2021). Available online at: https://www.food.gov.uk/research/research-projects/the-covid-19-consumer-research (accessed on March 24, 2021).
19. Bakaloudi DR, Jeyakumar DT, Jayawardena R, Chourdakis M. The impact of COVID-19 lockdown on snacking habits, fast-food and alcohol consumption: a systematic review of the evidence. Clin Nutr Edinb Scotl. (2021). doi: 10.1016/j.clnu.2021.04.020. [Epub ahead of print].
20. Yang G, Lin X, Fang A, Zhu H. Eating habits and lifestyles during the initial stage of the COVID-19 lockdown in china: a cross-sectional study. Nutrients. (2021) 13:970. doi: 10.3390/nu13030970
21. Herle M, Smith AD, Bu F, Steptoe A, Fancourt D. Trajectories of eating behavior during COVID-19 lockdown: longitudinal analyses of 22,374 adults. Clin Nutr Espen. (2021) 42:158–65. doi: 10.1016/j.clnesp.2021.01.046
22. Al-Musharaf S. Prevalence and predictors of emotional eating among healthy young saudi women during the COVID-19 pandemic. Nutrients. (2020) 12:2923. doi: 10.3390/nu12102923
23. Bonaccio M, Costanzo S, Ruggiero E, Persichillo M, Esposito S, Olivieri M, et al. Changes in ultra-processed food consumption during the first Italian lockdown following the COVID-19 pandemic and major correlates: results from two population-based cohorts. Public Health Nutr. (2021) 24:3905–15. doi: 10.1017/S1368980021000999
24. Cecchetto C, Aiello M, Gentili C, Ionta S, Osimo SA. Increased emotional eating during COVID-19 associated with lockdown, psychological and social distress. Appetite. (2021) 160:105122. doi: 10.1016/j.appet.2021.105122
25. Di Renzo L, Gualtieri P, Cinelli G, Bigioni G, Soldati L, Attinà A, et al. Psychological aspects and eating habits during COVID-19 home confinement: results of EHLC-COVID-19 Italian online survey. Nutrients. (2020) 12:2152. doi: 10.3390/nu12072152
26. Kaufman-Shriqui V, Navarro DA, Raz O, Boaz M. Multinational dietary changes and anxiety during the coronavirus pandemic-findings from Israel. Isr J Health Policy Res. (2021) 10:28. doi: 10.1186/s13584-021-00461-1
27. Ruggiero E, Mignogna C, Costanzo S, Persichillo M, Castelnuovo AD, Esposito S, et al. Changes in the consumption of foods characterising the Mediterranean dietary pattern and major correlates during the COVID-19 confinement in Italy: results from two cohort studies. Int J Food Sci Nutr. (2021) 72:1105–17. doi: 10.1080/09637486.2021.1895726
28. Schwingshackl L, Schwedhelm C, Hoffmann G, Lampousi A-M, Knüppel S, Iqbal K, et al. Food groups and risk of all-cause mortality: a systematic review and meta-analysis of prospective studies. Am J Clin Nutr. (2017) 105:1462–73. doi: 10.3945/ajcn.117.153148
29. Aune D, Giovannucci E, Boffetta P, Fadnes LT, Keum N, Norat T, et al. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality—a systematic review and dose-response meta-analysis of prospective studies. Int J Epidemiol. (2017) 46:1029–56. doi: 10.1093/ije/dyw319
30. Skotnicka M, Karwowska K, Kłobukowski F, Wasilewska E, Małgorzewicz S. Dietary habits before and during the COVID-19 epidemic in selected european countries. Nutrients. (2021) 13:1690. doi: 10.3390/nu13051690
31. Public Health England. National Diet and Nutrition Survey: Diet and Physical Activity—A Follow-up Study During COVID-19 . (2021). Available online at: https://www.gov.uk/government/statistics/ndns-diet-and-physical-activity-a-follow-up-study-during-covid-19 (accessed September 23, 2021).
32. Villadsen A, Patalay P, Bann D. Mental health in relation to changes in sleep, exercise, alcohol and diet during the COVID-19 pandemic: examination of four UK cohort studies. MedRxiv [Preprint]. (2021) 2021:2021.03.26.21254424. doi: 10.1101/2021.03.26.21254424
33. Dicken SJ, Mitchell JJ, Newberry Le Vay J, Beard E, Kale D, Herbec A, et al. Impact of COVID-19 pandemic on weight and BMI among UK adults: a longitudinal analysis of data from the HEBECO study. Nutrients. (2021) 13:2911. doi: 10.3390/nu13092911
34. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. (2009) 42:377–81. doi: 10.1016/j.jbi.2008.08.010
35. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O'Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. (2019) 95:103208. doi: 10.1016/j.jbi.2019.103208
36. Critchlow N, Bauld L, Thomas C, Hooper L, Vohra J. Awareness of marketing for high fat, salt or sugar foods, and the association with higher weekly consumption among adolescents: a rejoinder to the UK government's consultations on marketing regulation. Public Health Nutr. (2020) 23:2637–46. doi: 10.1017/S1368980020000075
37. Thomas C, Hooper L, Petty R, Thomas F, Rosenberg G, Vohra J. 10 Years On: New Evidence on TV Marketing and Junk Food Eating Amongst 11–19 Year Olds 10 Years After Broadcast Regulations . (2018). Available online at: https://www.basw.co.uk/resources/10-years-new-evidence-tv-marketing-and-junk-food-eating-amongst-11-19-year-olds-10-years (accessed April 8, 2021).
38. Newman A, Newberry Le Vay J, Critchlow N, Froguel A, Clark M, Vohra J. The HFSS beat goes on: awareness of marketing for high fat, salt and sugar foods and the association with consumption in the 2017 and 2019. Youth Obesity Policy Surveys. (2020). Available online at: hfss_beat_goes_on_december_2020_-_full_report/the_hfss_beat_goes_on_december_2020_-_full_report.pdf (accessed March 18, 2021).
39. NHS. Eat Well . (2019). Available online at: https://www.nhs.uk/live-well/eat-well/ (accessed April 15, 2019).
40. Bhutani S, vanDellen MR, Cooper JA. Longitudinal weight gain and related risk behaviors during the COVID-19 pandemic in adults in the US. Nutrients. (2021) 13:671. doi: 10.3390/nu13020671
41. Kriaucioniene V, Bagdonaviciene L, Rodríguez-Pérez C, Petkeviciene J. Associations between changes in health behaviours and body weight during the COVID-19 quarantine in Lithuania: the Lithuanian COVIDiet study. Nutrients. (2020) 12:3119. doi: 10.3390/nu12103119
42. Sigal RJ, Kenny GP, Wasserman DH, Castaneda-Sceppa C. Physical activity/exercise and type 2 diabetes. Diabetes Care. (2004) 27:2518–39. doi: 10.2337/diacare.27.10.2518
43. American College of Sports Medicine. American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med Sci Sports Exerc . (2009). 41:687–708. doi: 10.1249/MSS.0b013e3181915670
44. Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee I-M, et al. American college of sports medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. (2011) 43:1334–59. doi: 10.1249/MSS.0b013e318213fefb
45. IPAQ. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ)—Short Form . (2004). Available online at: https://www.physio-pedia.com/images/c/c7/Quidelines_for_interpreting_the_IPAQ.pdf (accessed June 12, 2021).
Google Scholar
46. Kaminsky LA, Montoye AHK. Physical activity and health: what is the best dose? J Am Heart Assoc. (2014) 3:e001430. doi: 10.1161/JAHA.114.001430
47. GOV.UK. Alcohol Consumption: Advice on Low Risk Drinking . (2016). Available online at: https://www.gov.uk/government/publications/alcohol-consumption-advice-on-low-risk-drinking (accessed May 27, 2021).
48. Office for National Statistics. Population Estimates for the UK, England and Wales, Scotland and Northern Ireland . (2019). Available online at: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/bulletins/annualmidyearpopulationestimates/mid2018 (accessed April 7, 2021).
49. Ballinger GA. using generalized estimating equations for longitudinal data analysis. Organ Res Methods. (2004) 7:127–50. doi: 10.1177/1094428104263672
50. Azuero A, Pisu M, McNees P, Burkhardt J, Benz R, Meneses K. An application of longitudinal analysis with skewed outcomes. Nurs Res. (2010) 59:301–7. doi: 10.1097/NNR.0b013e3181e507f1
51. Lakens D, McLatchie N, Isager PM, Scheel AM, Dienes Z. Improving Inferences about Null Effects with Bayes Factors and Equivalence Tests. J Gerontol B Psychol Sci Soc Sci . (2020) 75:45–57. doi: 10.1093/geronb/gby065
52. Dienes Z. Using Bayes to get the most out of non-significant results. Front Psychol. (2014) 5:781. doi: 10.3389/fpsyg.2014.00781
53. Neira C, Godinho R, Rincón F, Mardones R, Pedroso J. Consequences of the COVID-19 syndemic for nutritional health: a systematic review. Nutrients. (2021) 13:1168. doi: 10.3390/nu13041168
54. Zupo R, Castellana F, Sardone R, Sila A, Giagulli VA, Triggiani V, et al. Preliminary trajectories in dietary behaviors during the COVID-19 pandemic: a public health call to action to face obesity. Int J Environ Res Public Health. (2020) 17:7073. doi: 10.3390/ijerph17197073
55. Zhang X, Chen B, Jia P, Han J. Locked on salt? Excessive consumption of high-sodium foods during COVID-19 presents an underappreciated public health risk: a review. Environ Chem Lett . (2021) 1:1–13. doi: 10.2139/ssrn.3804495
56. Zeigler Z. COVID-19 self-quarantine and weight gain risk factors in adults. Curr Obes Rep. (2021) 10:423–433. doi: 10.1007/s13679-021-00449-7
57. Salazar-Fernández C, Palet D, Haeger PA, Román Mella F. The perceived impact of COVID-19 on comfort food consumption over time: the mediational role of emotional distress. Nutrients. (2021) 13:1910. doi: 10.3390/nu13061910
58. Rolland B, Haesebaert F, Zante E, Benyamina A, Haesebaert J, Franck N. Global changes and factors of increase in caloric/salty food intake, screen use, and substance use during the early COVID-19 containment phase in the general population in france: survey study. JMIR Public Health Surveill. (2020) 6:e19630. doi: 10.2196/19630
59. Jafri A, Mathe N, Aglago EK, Konyole SO, Ouedraogo M, Audain K, et al. Food availability, accessibility and dietary practices during the COVID-19 pandemic: a multi-country survey. Public Health Nutr. (2021) 24:1798–805. doi: 10.1017/S1368980021000987
60. Monteiro C, Cannon G, Lawrence M, Louzada ML, Machado P. Ultra- processed foods, Diet Quality, and Health Using the NOVA Classification System . (2019). Available online at: http://www.fao.org/3/ca5644en/ca5644en.pdf (accessed March 3, 2020).
61. Janssen M, Chang BPI, Hristov H, Pravst I, Profeta A, Millard J. Changes in Food consumption during the COVID-19 pandemic: analysis of consumer survey data from the first lockdown period in Denmark, Germany, and Slovenia. Front Nutr. (2021) 8:635859. doi: 10.3389/fnut.2021.635859
62. Devonport TJ, Nicholls W, Fullerton C. A systematic review of the association between emotions and eating behaviour in normal and overweight adult populations. J Health Psychol. (2019) 24:3–24. doi: 10.1177/1359105317697813
63. Coulthard H, Sharps M, Cunliffe L, van den Tol A. Eating in the lockdown during the Covid 19 pandemic; self-reported changes in eating behaviour, and associations with BMI, eating style, coping and health anxiety. Appetite. (2021) 161:105082. doi: 10.1016/j.appet.2020.105082
64. Sadler JR, Thapaliya G, Jansen E, Aghababian AH, Smith KR, Carnell S. COVID-19 stress and food intake: protective and risk factors for stress-related palatable food intake in U.S. Adults. Nutrients. (2021) 13:901. doi: 10.3390/nu13030901
65. McAtamney K, Mantzios M, Egan H, Wallis DJ. Emotional eating during COVID-19 in the United Kingdom: exploring the roles of alexithymia and emotion dysregulation. Appetite. (2021) 161:105120. doi: 10.1016/j.appet.2021.105120
66. Theobald C, White A. British nutrition foundation healthy eating week 2020–insights into the effect of COVID-19 on eating activity habits of adults children in the UK. Nutr Bull. (2021). 46:238–45. doi: 10.1111/nbu.12500
67. Brewer JA, Ruf A, Beccia AL, Essien GI, Finn LM, Lutterveld R van, et al. Can mindfulness address maladaptive eating behaviors? Why traditional diet plans fail and how new mechanistic insights may lead to novel interventions. Front Psychol. (2018) 9:1418. doi: 10.3389/fpsyg.2018.01418
68. Fluharty M, Fancourt D. How Have People Been Coping during the COVID-19 Pandemic? Patterns and Predictors of Coping Strategies amongst 26,016 UK Adults. BMC Psychol . (2021) 9:107–9. doi: 10.31234/osf.io/nx7y5
69. Bann D, Villadsen A, Maddock J, Hughes A, Ploubidis GB, Silverwood R, et al. Changes in the behavioural determinants of health during the COVID-19 pandemic: gender, socioeconomic and ethnic inequalities in five British cohort studies. J Epidemiol Community Health. (2021) 75:1136–42. doi: 10.1101/2020.07.29.20164244
70. Greer SM, Goldstein AN, Walker MP. The impact of sleep deprivation on food desire in the human brain. Nat Commun. (2013) 4:2259. doi: 10.1038/ncomms3259
71. Aknin L, Neve J-ED, Dunn E, Fancourt D, Goldberg E, Helliwell J, et al. Mental health during the first year of the COVID-19 pandemic: a review and recommendations for moving forward. Perspect Psychol Sci. (in press). doi: 10.31234/osf.io/zw93g
72. Saunders R, Buckman JEJ, Fonagy P, Fancourt D. Understanding different trajectories of mental health across the general population during the COVID-19 pandemic. Psychol Med. (2021) 2021:1–9. doi: 10.1017/S0033291721000957
73. Robinson E, Blissett J, Higgs S. Social influences on eating: implications for nutritional interventions. Nutr Res Rev. (2013) 26:166–76. doi: 10.1017/S0954422413000127
74. World Health Organisation. Healthy Diet . (2018). Available online at: https://www.who.int/publications/m/item/healthy-diet-factsheet394 (accessed February 25, 2021).
75. GOV.UK. National Diet and Nutrition Survey Rolling programme Years 9 to 11 (2016/2017 to 2018/2019) . (2020). Available online at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/943114/NDNS_UK_Y9-11_report.pdf (accessed February 26, 2021).
76. Steel N, Ford JA, Newton JN, Davis ACJ, Vos T, Naghavi M, et al. Changes in health in the countries of the UK and 150 English Local authority areas 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Lond Engl. (2018) 392:1647–61. doi: 10.1016/S0140-6736(18)32207-4
77. GOV.UK. Tackling Obesity: Empowering Adults and Children to Live Healthier Lives . (2020). Available online at: https://www.gov.uk/government/publications/tackling-obesity-government-strategy/tackling-obesity-empowering-adults-and-children-to-live-healthier-lives (accessed June 28, 2021).
78. GOV.UK. New Obesity Strategy Unveiled as Country Urged to Lose Weight to Beat Coronavirus (COVID-19) and Protect the NHS . (2020). Available online at: https://www.gov.uk/government/news/new-obesity-strategy-unveiled-as-country-urged-to-lose-weight-to-beat-coronavirus-covid-19-and-protect-the-nhs (accessed June 28, 2021).
79. Conklin AI, Forouhi NG, Surtees P, Khaw K-T, Wareham NJ, Monsivais P. Social relationships and healthful dietary behaviour: evidence from over-50s in the EPIC cohort, UK. Soc Sci Med. (2014) 100:167–75. doi: 10.1016/j.socscimed.2013.08.018
80. McClung HL, Ptomey LT, Shook RP, Aggarwal A, Gorczyca AM, Sazonov ES, et al. Dietary intake and physical activity assessment: current tools, techniques, and technologies for use in adult populations. Am J Prev Med. (2018) 55:e93–104. doi: 10.1016/j.amepre.2018.06.011
81. Hill RJ, Davies PS. The validity of self-reported energy intake as determined using the doubly labelled water technique. Br J Nutr. (2001) 85:415–30. doi: 10.1079/BJN2000281
82. Subar AF, Freedman LS, Tooze JA, Kirkpatrick SI, Boushey C, Neuhouser ML, et al. Addressing current criticism regarding the value of self-report dietary data. J Nutr. (2015) 145:2639–45. doi: 10.3945/jn.115.219634
Keywords: COVID-19, dietary behaviours, HFSS, snacking, BMI, health behaviours, weight management, diet
Citation: Dicken SJ, Mitchell JJ, Newberry Le Vay J, Beard E, Kale D, Herbec A and Shahab L (2022) Impact of the COVID-19 Pandemic on Diet Behaviour Among UK Adults: A Longitudinal Analysis of the HEBECO Study. Front. Nutr. 8:788043. doi: 10.3389/fnut.2021.788043
Received: 01 October 2021; Accepted: 22 November 2021; Published: 13 January 2022.
Reviewed by:
Copyright © 2022 Dicken, Mitchell, Newberry Le Vay, Beard, Kale, Herbec and Shahab. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Samuel J. Dicken, samuel.dicken.20@ucl.ac.uk
† These authors share senior authorship
Talk to us about diabetes
0345 123 2399
customer support
Kick-start healthy eating habits
Happy new year.
How many of us will make a New Year’s resolution to lose some weight, try to eat more fruit and veg, or do more exercise? While we set out with good intentions, nearly 80 per cent of us fail to maintain our resolution – some of us quitting after as little as nine days.
The trouble is we often set ourselves unrealistic goals – “I’m going to lose a stone by February,” or “I’m going to go to the gym five times a week” – or we simply believe we can do it by willpower alone. But it’s more realistic to make small lifestyle changes that are easier to stick to. Try these simple, easy-to-maintain changes and reap the rewards.
'I resolve to eat more fruit and veg'
Sounds simple, doesn’t it? But recent figures show about 60–70% of us aren’t eating our five a day. Fruits and vegetables are packed with important vitamins, minerals and fibre, so failing to eat your recommended daily intake could lead to serious gaps in your diet.

- Set yourself a specific goal and put steps in place to make it happen – for example, aim to have a piece of fruit at work/home mid-morning or two servings of vegetables with your evening meal.
- Don’t forget, frozen and tinned veggies all count, so add a small tin of sweet corn to a salad, or add some frozen berries to your porridge at breakfast. Dried fruit also counts, but can be quite high in natural sugar, so only sprinkle a small portion over your breakfast cereal.
- Maybe bring in some mini tins of fruit in natural juice with a convenient ring pull to have as an easy go-to snack mid-morning so you are less tempted to reach for the biscuits. Keeping a couple of cans at work so that if you forget to bring any fresh fruit in, you can still reach your goal.
- Try these fruit kebabs .
Weight-loss planner
"I keep a daily diary and log my weight and activity. It keeps me accountable and focused." Edward Morrison, who lost over four stone – read his story .
You can download My weight-loss planner (PDF, 534KB) to set goals and track your progress. By putting a plan in place and noting down your progress, you'll be able to see the positive changes you're making.
Three ways to add veg to your main meals:
- Add carrots to a chilli
- Add lentils to a curry
- Pop a can of beans in your casserole.
Remember fruit and veg have a different mix of nutrients so you get more goodness by eating a range of them – try a new fruit or veg whenever you get the opportunity.
‘I resolve to reduce my oil’
Even if you already use healthier unsaturated fats, such as olive oil, rapeseed and sunflower oil, be aware that all fats contain similar amounts of calories, so keep an eye on how much oil you’re using if you’re trying to manage your weight. Try these quick tricks:
- Make measuring spoons your new best friend. Too often we pour from the bottle and don’t realise how much we’re using. Read the recipe and make sure you measure how much you use.
- Try dry-frying foods with a little water and no oil. You’ll cut calories without noticing.
- If you prefer, some of the shop-bought, low-calorie sprays can be a convenient way of cutting the amount of oil you use.
- Don’t drizzle olive oil straight from the bottle onto a salad. You can make a dressing with lemon juice, balsamic vinegar and olive oil, then use a teaspoon to dress the leaves. It’s a lot tastier, too.
‘I resolve to make smart food swaps’
Healthy eating doesn’t mean you have to stop eating all your favourite foods, but you need to think carefully about how often and how much you eat and how these foods affect your diabetes management.
Four tips if you love cheese…
- If you love strong cheese grate it to make it go further.
- Add grated carrot to cheese sandwiches bulk it out.
- Choose a mature cheese which has more flavour so you get away with using less.
- If you haven’t tried reduced-fat cheeses recently give them a try – you may be surprised. Many people find they can’t tell the difference between reduced-fat cheese and the ordinary version.
For an occasional treat, you can even have cream on your desserts if you make another smart food swap. Using thick single cream rather than double will cut the calorie and fat content – just don’t do it every day.
Using 0% fat, low-fat crème-fraiche, natural yogurt or fat-free fromage frais rather than cream in cooking will cut your calorie intake even further.
‘I resolve to eat real food’
It can be tempting to look for a quick fix, such as special diet foods or foods labelled ‘diabetic’. It’s important to focus on the food you eat, and base your food choices on the overall goal of a healthy, balanced diet, rather than just one particular nutrient.
We all know that cooking from scratch is best because it means you have greater control over the ingredients you use, which is why our recipe finder is really handy – it’s packed full of nutritious and healthier, easy-to-cook recipes.
Get label savvy. For a product to be labelled reduced fat, light or lite it has to contain at least 30 per cent less fat than a similar product.
But if the food is already high in fat, the reduced-fat version may still be high in fat (17.5g or more of fat per 100g). For example, a lower-fat mayonnaise although labelled 30 per cent lower in fat than the standard version, is still high-fat.
Products labelled low-fat aren't necessarily low in calories. Sometimes the manufacturers replace the fat with sugar. For example, so-called ‘light’ biscuits are very often higher in sugar compared to the standard version.
There’s no special diet for people with diabetes, so enjoy eating the same healthy, balanced diet as your friends and family. Just watch your portions and don’t overdo it, and your healthy eating resolutions should last long after the Christmas decorations have come down.
'I resolve to up my activity levels'
Most of us have probably let our activity routine slip after Christmas and now feel the need to get moving again. If you're someone who hasn’t been active for a while, you can make small changes to fit around your life and budget.
Try these tips:

- If time’s precious, instead of meeting friends or family for a coffee why not suggest doing something active? You could go for a walk-and-talk, a swim, or take the kids to the park with a ball.
- Although your body – and mind – benefit as soon as you become more active, you may not see visible changes immediately and this can be disheartening. It can also take time for your body to adapt to the activity, so keep going and set goals that are right for you.
- By setting yourself goals, you’re more likely to stick to an active lifestyle but be realistic with both short- and long-term goals. Set your goals to be more challenging and review them on a regular basis.
- Keep an exercise diary and tick off your achievements – you’ll be amazed at the improvement and progress you’ll see and feel. When you reach a goal, plan a reward for all your hard work – buy a new top or book a beauty treatment.
- If you’re starting a new activity, check with your healthcare team to see how this could affect your diabetes.
Share this Page
© The British Diabetic Association operating as Diabetes UK, a charity registered in England and Wales (no. 215199) and in Scotland (no. SC039136). A company limited by guarantee registered in England and Wales with (no.00339181) and registered office at Wells Lawrence House, 126 Back Church Lane London E1 1FH

Information and guidance about eating a healthy, balanced diet.
- How to eat a balanced diet
- Food guidelines and food labels
- Digestive health

Home - About us - Press releases and news - How Brits’ eating habits have changed in three de…
How Brits’ eating habits have changed in three decades
Out with tea, white bread and red meat; in with fruit and pizza.
3 September 2020
To mark 30 years of delivering life-changing research and health information advice, World Cancer Research Fund (WCRF) is highlighting how the nation’s eating and food shopping habits have changed – alongside people’s awareness of cancer prevention – as part of its ‘ 30 days has September ’ campaign.
A lot has changed in 30 years; fashion, culture, sport, music, but also what we know about the links between diet and the risks of developing cancer. As part of WCRF’s 30th birthday the charity looked back on data collected annually by the Department for Environment, Food & Rural Affairs on weekly food purchasing 1 to see how diets have changed over 30 years.
The data revealed that we are buying 50 per cent less tea, 56 per cent less white bread and 32 per cent less red meat (pork, lamb and beef) in 2018 than we were in 1992. We are also buying 23 per cent more fresh fruit. However, while the nation has become healthier in some aspects – lowering consumption of red meat and eating more plant-based foods (fruit, vegetable, pulses, etc) both help to lower cancer risk 2 – we have also started buying more unhealthy food such as confectionary. Consumption of chocolate bars increased by 13 per cent over the same period.
One major influence on the nation’s dietary habits has been the advance in technology, leading to freezers and microwaves being commonplace in the British kitchen. As a result, we have become much more reliant on ready meals instead of home cooked meals – with purchases up 100 per cent since 1992. Sales of pizza (frozen, not-frozen and takeaway) have increased by 143 per cent.
What is the impact on obesity and cancer?
Eating fast foods and having a ‘Western-type’ diet, characterised by high intakes of meat, fat and sugar, are linked to excess weight gain, overweight and obesity 2 – overweight and obesity rates have increased in England from 53 percent of adults in 1993 to 63 per cent in 2018 3 . Alcohol purchasing has also increased by 38 per cent; drinking alcohol is strongly linked to six different types of cancer, including breast cancer 2 .
Rachael Gormley, CEO of WCRF UK, said:
When WCRF was founded in the UK 30 years ago, the link between diet and cancer wasn’t widely known. Since 1990, WCRF has invested more than £100m in cancer prevention and survival research. Today, thanks in part to our key role in funding research and public health messaging, more people than ever before are now aware that they can lower their risk of cancer through making moderate, but impactful, changes to their diet and lifestyle.
This Summer, the government announced a new campaign to make the country healthier; the Better Health campaign aims to get people to eat healthier and move more to lose weight. Previous public health campaigns over the decades have had moderate success – 2004’s Sid the Slug campaign led to approximately a 10 per cent reduction in salt in diets 4 , and the 5 A DAY campaign launched in 2003 led to an initial increase in people eating their 5 A DAY, but in 2018 this has stalled at around 28 per cent 5 .
Dr Giota Mitrou, Director of Research at WCRF, said:
Our world-leading research shows that being overweight or obese increases the risk of at least 12 different types of cancer. The rise in overweight and obesity is not due to one food alone being eaten more, but rather our overall behaviour patterns changing. Known as the nutrition transition, it has resulted in people being more reliant on processed foods that are high in fat, salt or sugar. That is why we recognise the need to focus more on dietary patterns instead of individual foods or food components, and why our Cancer Prevention Recommendations should be followed as a package of healthy behaviours for maximum benefit.
WCRF’s Cancer Health Check tool and Cancer Prevention Recommendations help people understand what changes they could make to reduce the risk of getting cancer. Based on the latest scientific research, the advice is practical and simple to understand.
Notes to editors
For more information and media enquiries contact Maxine Lenza, Senior Press and Communications Officer at WCRF, on 07717 131 883 or [email protected] .
1 UK – household purchases, Family food datasets, UK government, accessed 26 August 2020: https://www.gov.uk/government/statistical-data-sets/family-food-datasets 2 World Cancer Research Fund/American Institute for Cancer Research, Diet, nutrition, physical activity and cancer: a global perspective, accessed 26 August 2020: dietandcancerreport.org 3 Obesity Indicator, Nuffield Trust, accessed 26 August 2020: https://www.nuffieldtrust.org.uk/resource/obesity?gclid=Cj0KCQjwg8n5BRCdARIsALxKb96xVa5ZF_8mPSoXPMXYzjTGBbh9zIpOLPni5azN_7s48acvg99b43waAk2xEALw_wcB 4 An evaluation of the UK Food Standards Agency’s salt campaign, Health Economics, 22: 243–250 (2013), accessed 26 August 2020: https://www.tse-fr.eu/sites/default/files/medias/stories/sem_12_13/afio/shankar.pdf 5 Health Survey, NHS Digital, accessed 26 August 2020: http://healthsurvey.hscic.gov.uk/data-visualisation/data-visualisation/explore-the-trends/fruit-vegetables.aspx
About World Cancer Research Fund Network
World Cancer Research Fund UK is part of a network of cancer charities with a global reach, dedicated to the prevention and survival of cancer through a healthy diet, maintaining a healthy weight, and being more physically active. By funding and supporting research, developing policy guidance and providing health information, we ensure that people can make informed lifestyle choices to reduce their risk of developing a preventable cancer.
Find out more: www.wcrf-uk.org Follow us on social media: Twitter , Facebook , Instagram
RELATED CONTENT
- Directors and Trustees
- Our values and core beliefs
- Annual reviews
- Our partnerships
- Our network
- Feedback and complaints
- Clubbercise founder Claire on life after bowel cancer
- Honouring Mum in beautiful Kew: why I ran a 10k for cancer prevention
- In sickness and in health: Ken, Shirley and cancer
- Why World Cancer Research Fund means so much to Joan
- Sign up to our email newsletter
- Media centre
- Equality, Diversity and Inclusion Policy
- Privacy Notice
- Cookies policy
- Linking policy

The home of GREAT British food
British Food Traditions: 20 Great Eating Habits Of The UK

We people of Britain have some peculiar habits when it comes to food. At least, that’s how it probably seems to the rest of the world. But to us, they’re just tradition, and we’re ridiculously proud of them. Even if it has people wondering whether British food is the worst in the world 🤔
If you want to learn about British food traditions, then clearly, the British Grub Hub is the place to be.
Traditional British dishes are one thing, but right here we’re talking food traditions from Great Britain, like turkey at Christmas, chocolate eggs at Easter, and rolling down hills after cheese (seriously!)
So, without further ado, get ready for a bunch of British food traditions to marvel at, or more likely, reaffirm your beliefs that the best cuisine in the world is anything other than British.
Food Traditions In Britain
Here’s those British food traditions you were wondering about:
Three Meals A Day
For most Brits, breakfast, lunch, followed by dinner (a.k.a ‘tea’ or ‘supper’) are the three meals each day which is ‘tradition’, unless of course you’re a Brit who’s prone to get peckish in between. Which is where brunch, afternoon tea and British snacks come in, naturally.
The Sunday Roast
As well as a typical British breakfast , lunch and dinner, one of the ultimate food traditions in Britain is eating a classic Roast on a Sunday, and that’s just a fact.
Classic British Dishes
The Sunday Roast is just one of the many classic British dishes . Other mouth-watering traditional meals from the UK include the Full English Breakfast, Fish & Chips, Pie & Mash and Shepherd’s Pie; not to mention traditional British delicacies like the Scotch egg and Pork Pie.
Great Britain is famous for its many traditional desserts , with it being tradition to enjoy dishes such as a classic apple crumble or sticky toffee pudding as the end to a meal.
Valentine’s Day Dining
It’s again just tradition in Britain, this time for the 14th day in February to creep up on 50% of a relationship. There’s nothing quite like the traditional last-minute panic over where to eat in the UK on Valentine’s Day. 😉
Pancake Day
Officially known by Christian observers as Shrove Tuesday, ‘Pancake Day’ is a key food tradition on the British food calendar , the day before Ash Wednesday each year.
Easter Food
Spring lamb, hot-cross buns and chocolate eggs are practically all that’s eaten at Easter time in Britain, if you follow tradition. Oh, and the odd tip of asparagus.
Summer BBQs
Another food tradition in Britain says that you must cook food on a BBQ as soon as you spot a glimmer of sun through the clouds.
Scary Snacks at Halloween
Nothing says scary like cakes with spider legs, jelly and ice cream with eyeballs, or chocolate eggs filled with snot.
Weird Food Names
A further food related tradition in Blighty is the historic naming of our dishes in the weirdest ways possible. Spotted Dick and Toad in the hole are two examples of weird British food names that make it hard to believe that British cuisine is actually the best in the world .
Defending British Food
It’s no secret that most of the planet considers that British food is the worst in the world , so it’s pretty much a tradition for us Brits to stubbornly defend our cuisine by over-emphasising that modern British food is different . 😃
Eating Any Other Cuisine But British Food
As much as we Brits love our own cuisine, we also enjoy food from plenty of other countries around the world. So it’s practically now a tradition (and a tad ironic) that Britain actually eats more international food than its own. 😆
Supermarket Snobbery
The British food tradition that may well run longest into the future is the UK’s (perceived) supermarket hierarchy. Showing our reluctance at getting involved, here it is in alphabetical order for you to rearrange as you see fit:
- Marks & Spencer
- Sainsbury’s
It’s fair to say that shows like Saturday Kitchen, Sunday Brunch, Great British Menu, Masterchef and obviously The Great British Bake Off mean that TV shows are a firmly fixed food tradition in the UK.
Britain loves a takeaway, or nowadays, a home delivery, especially at the weekend. Whether it’s Chinese, Indian, Italian, American, Fish & Chips or anything else, as long as we don’t have to cook on a Friday or Saturday night, we’re traditionally happy.
The traditions continue thick and, well, fast, when it comes to food in Blighty. We’re all about convenience in the UK, which you might say is proved by 100 million fast-food meals being served annually (as of 2017).
Eating Food In Pubs
As much as the restaurant scene in Britain is second to none, there’s nothing quite like the tradition of eating in a traditional British pub . As well as the traditional British ‘boozer’ that serves the UK’s classic dishes , modern British food is also a thing, meaning that nowadays there’s even pubs in Britain with Michelin stars.
Hangover Food
It’s well known that traditional British breakfast items are among the best in the world for helping a hangover, and the people of Britain made this a tradition long-ago. Whether it’s a bacon butty, sausage and egg sarnie, or the holy-grail of the Full English Breakfast , British food tradition means there’s a solution to getting sloshed at those British pubs we rave about.
Christmas Food Traditions in Britain
Everyone knows by now that the ultimate British food tradition is eating turkey at Christmas with ‘all the trimmings’ of a classic Roast Dinner, not to mention scoffing mince pies from 1st December and wolfing down Christmas pudding an hour before an evening spread.
New Year Food Traditions in the UK
While Britain in general doesn’t necessarily have many specific food traditions related to New Year, Hogmanay is a Scottish event which is essentially the last day of the year, when it’s traditional to eat the classic dishes of Scotland, such as Haggis .
So that’s your menu of British food traditions. Which ones will you experience on your visit to Blighty…?
British Grub Hub The home of great British food
- Consumer Goods & FMCG ›
- Food & Nutrition
Generational food trends in the UK - statistics & facts
Diets and intolerances, meat and dairy consumption across the ages, key insights.
Detailed statistics
Population of the UK 1990-2022, by generation
Millennial diets and nutrition in the UK 2022/23
Gen Z diets and nutrition in the UK 2022/23
Editor’s Picks Current statistics on this topic
Current statistics on this topic.
Food & Beverage
Grocery market value in the United Kingdom (UK) 2004-2027
Eating Behavior
Share of adults that plan to not eat meat by generation in Great Britain in 2023
Related topics
Food trends in the uk.
- Organic food market in the UK
- Food shopping behavior in the UK
- Health and wellness food trends in the UK
Generational comparisons
- Generational grocery shopping behavior in the UK
- U.S. generations: grocery shopping behavior
- Generation Z food consumption in the U.S.
- Gen Z alcohol consumption in the U.S.
Recommended statistics
- Premium Statistic Grocery shopping by type in the United Kingdom 2023, by generation
- Premium Statistic Generation Z weekly food spend in the UK 2022, by channel
- Premium Statistic Social media food behavior of young consumers in Europe in 2022
- Premium Statistic Leading factors considered by Gen Z when making a purchase in the UK 2022
Grocery shopping by type in the United Kingdom 2023, by generation
Grocery shopping by type in the United Kingdom as of December 2023, by generation
Generation Z weekly food spend in the UK 2022, by channel
Average spending per week on groceries by Generation Z in the UK in 2022, by channel
Social media food behavior of young consumers in Europe in 2022
Popular social media food activities of Millennials and Generation Z in Europe in 2022
Leading factors considered by Gen Z when making a purchase in the UK 2022
Leading considerations influencing Gen Z consumers purchasing decisions in the United Kingdom (UK) in 2022
Diets and nutrition
- Premium Statistic Consumers with food intolerances in the UK 2022/23, by generation
- Premium Statistic Gen Z diets and nutrition in the UK 2022/23
- Premium Statistic Millennial diets and nutrition in the UK 2022/23
- Premium Statistic Generation X diets and nutrition in the UK 2022/23
Consumers with food intolerances in the UK 2022/23, by generation
Share of consumers with one or more food intolerances in the UK in 2022/23, by generation
Do you follow one or more of the following nutrition rules?
Generation X diets and nutrition in the UK 2022/23
Eating and cooking habits
- Premium Statistic Share of consumers who actively try to eat heathy in the UK 2022/23, by generation
- Premium Statistic Share of consumers who prefer food to be convenient in the UK 2022/23, by generation
- Premium Statistic How often Gen Z and Millennial use DIY meal boxes in the UK 2022
- Premium Statistic University students' change in eating habits in the UK 2022
Share of consumers who actively try to eat heathy in the UK 2022/23, by generation
Consumers who actively try to eat healthy in the UK in 2022/23, by generation
Share of consumers who prefer food to be convenient in the UK 2022/23, by generation
Consumers who think that food must be convenient and fast in the UK in 2022/23, by generation
How often Gen Z and Millennial use DIY meal boxes in the UK 2022
Frequency of meal kit usage among Generation Z and young Millennials in the UK in 2022
University students' change in eating habits in the UK 2022
Changes in eating habits in the past year amongst undergraduate students in the United Kingdom (UK) as of February 2022
Meat and dairy consumption
- Premium Statistic Share of adults that plan to not eat meat by generation in Great Britain in 2023
- Premium Statistic Meat substitute consumers in the UK 2023, by generation
- Premium Statistic Willingness to try cultured meat in the UK 2022/23, by generation
- Premium Statistic Dairy substitute consumers in the UK 2022/23, by generation
- Premium Statistic Plant-based milk consumers in the United Kingdom 2022, by milk type & age group
Share of adults that plan to not eat meat in Great Britain in 2023, by generation
Meat substitute consumers in the UK 2023, by generation
Share of consumers who eat meat substitutes in the UK in 2023, by generation
Willingness to try cultured meat in the UK 2022/23, by generation
Consumers who are open to trying cultured meat in the UK in 2022/23, by generation
Dairy substitute consumers in the UK 2022/23, by generation
Share of consumers who eat dairy substitutes in the UK in 2022/23, by generation
Plant-based milk consumers in the United Kingdom 2022, by milk type & age group
Which, if any, of the following do you include in your diet nowadays?
Favorite dishes
- Premium Statistic Most popular British dishes among millennials in Great Britain Q1 2023
- Premium Statistic Most popular British dishes among the Generation X in Great Britain Q1 2023
- Premium Statistic Most popular British dishes among baby boomers in Great Britain Q1 2023
- Premium Statistic Leading types of takeaway food in Great Britain 2021, by age group
Most popular British dishes among millennials in Great Britain Q1 2023
Millennials' favorite British dishes in Great Britain (GB) as of Q1 2023
Most popular British dishes among the Generation X in Great Britain Q1 2023
Generation X's favorite British dishes in Great Britain (GB) as of Q1 2023
Most popular British dishes among baby boomers in Great Britain Q1 2023
Baby boomers' favorite British dishes in Great Britain (GB) as of Q1 2023
Leading types of takeaway food in Great Britain 2021, by age group
Most popular types of takeaway cuisine in Great Britain as of January 2021, by age group
Further reports Get the best reports to understand your industry
Get the best reports to understand your industry.
Mon - Fri, 9am - 6pm (EST)
Mon - Fri, 9am - 5pm (SGT)
Mon - Fri, 10:00am - 6:00pm (JST)
Mon - Fri, 9:30am - 5pm (GMT)
- International edition
- Australia edition
- Europe edition

UK Covid takeaway habits endure as fast food calorie intake remains high
Study shows delivery apps such as Deliveroo and Just Eat still popular after pandemic boom in orders
Delivery app riders pedalling through cities and tailbacks at drive-throughs were familiar signs of Britain’s hunger for takeaway food at the peak of the Covid pandemic . Now a study suggests it became an enduring habit.
After a boom in orders on Deliveroo, Just Eat and other platforms by locked-down consumers, research by the Institute for Fiscal Studies (IFS) suggests the popularity of takeaways, meal deliveries and food-on-the-go bought from retailer such as sandwiches and crisps has remained above pre-pandemic levels after the removal of Covid restrictions.
Analysing data on shopping habits from thousands of consumers, the thinktank said calorie consumption from takeaway food grew by more than 50% during the height of the pandemic – and had stayed high thereafter, as households continued to opt for a night in front of the TV instead of a meal at restaurant or pub.
Highlighting a big shift in the country’s diet and sources of nutrition, the IFS said a legacy of the Covid lockdowns could include long-term effects on health and weight.
The study, which was funded by the Obesity Policy Research Unit at University College London, estimated that before the pandemic, the average UK adult consumed about 270 calories a week from takeaways. This increased to 395 calories a week during the first lockdown in 2020, when restaurants, pubs and cafes were forced to close as the pandemic spread.
While the reopening of hospitality later in the year fuelled a decline in takeaway consumption, levels still remained higher than before the pandemic – even while the government’s “eat out to help out” scheme was in place.
During the third national lockdown in England in 2021, calorie consumption from takeaways ballooned further to an average of 470 calories a week as the country adapted to living with the pandemic and more restaurants and pubs switched to accommodate takeaway orders .
However, despite the easing of restrictions, these higher levels endured after the widespread reopening of hospitality venues, at about 400 calories a week by early 2022 – 50% above pre-pandemic levels.
The researchers said they had only been able to examine data up to the first quarter of 2022 , before the cost of living crisis . This meaning it is not entirely clear whether the UK’s takeaway habit survived the sharpest jump in food prices since the 1970s . However, the initial findings suggest a marked shift.
after newsletter promotion
The study also found the size of households’ food shopping baskets increased at the height of the pandemic in 2020, but then largely returned to normal. Overall calorie purchases had returned to 2019 levels by 2022, suggesting that the increase in takeaways has come at the expense of coffee shops, pubs and restaurants.
Andrew McKendrick, a research economist at IFS, said: “Lockdowns and closures of hospitality left a bigger role for consumption of food at home and for takeaways. But, by the start of 2022, most of these changes had been reversed: households had largely gone back to purchasing as much as they did in 2019.
“The pandemic did leave one legacy, though, in the much-increased use of takeaways.”
- Food & drink industry
- Couriers/delivery industry
- Hospitality industry
Most viewed

IMAGES
VIDEO
COMMENTS
3. Eat more fish, including a portion of oily fish. Fish is a good source of protein and contains many vitamins and minerals. Aim to eat at least 2 portions of fish a week, including at least 1 portion of oily fish. Oily fish are high in omega-3 fats, which may help prevent heart disease.
eat at least 5 portions of a variety of fruit and vegetables every day. base meals on potatoes, bread, rice, pasta or other starchy carbohydrates, choosing wholegrain versions where possible. have ...
What are the current healthy eating guidelines in the UK? In the UK, our healthy eating model is called the Eatwell Guide. ... As shown in the studies mentioned above, significant changes in eating habits are needed for current average UK diets to meet Eatwell Guide recommendations. It has been estimated that less than 1% of the population meet ...
Changing eating habits. Many consumers reported that they are adopting a 'flexitarian' diet - that is, eating mostly plant-based foods while eating meat and other animal products only occasionally. In the UK, 25% of the public described themselves as "still eating but cutting down on meat, dairy and animal products".
an apple. a banana. Beans, pulses, fish, eggs, meat and other proteins. These foods all contain protein, minerals and vitamins which help maintain and repair your body after an injury or surgery. You don't need to eat meat every day - try eggs, beans, lentils or meat substitutes such as Quorn or tofu instead.
Another more recent suggestion is to aim to eat 30 different plants over the week. This includes nuts, seeds, herbs and spices. Eat at least two portions of fish (preferably oily fish) per week. Consider regularly eating whole grains and nuts. Keep the amount of salt in your diet to less than 6 g per day.
A healthy diet rich in fruits, vegetables, whole grains and low-fat dairy can help to reduce your risk of heart disease by maintaining blood pressure and cholesterol levels. High blood pressure and cholesterol can be a symptom of too much salt and saturated fats in your diet. Eating a portion of oily fish - such as salmon and trout - each ...
Being able to eat healthily is on the mind of a little over 45 percent of UK consumers. This ranks somewhat low among their food-related worries . However, more concerns relate to healthy eating.
10 ways the UK eating habits have changed. (2016) 10 ways the UK eating habits have changed. BBC news magazine. Rauber et al., 2018.Ultra-processed food consumption and chronic non-communicable diseases related dietary nutrient profile in the UK (2008-2014). Nutrients.10.587. IGD.2019.UK food sale to grow by £24bn by 2024 as of 19 January 2022 ...
The latest wave of the Food Standards Agency's (FSA) Food and You 2 survey, conducted between April and July 2022, shows that most people surveyed in England, Wales and Northern Ireland had made changes to their eating habits in the last year, with financial reasons being the biggest driver. Latest findings from our flagship survey, published ...
The National Diet and Nutrition Survey ( NDNS) rolling programme is a continuous, cross-sectional survey. It is designed to collect detailed, quantitative information on the food consumption ...
COVID-19 pandemic restrictions impacted dietary habits during the initial months of the pandemic, but long-term effects are unclear. In this longitudinal study, self-selected UK adults (n = 1,733, 71.1% female, 95.7% white ethnicity) completed three online surveys (May-June, August-September, and November-December 2020, with a retrospective pre-pandemic component in the baseline survey ...
Three ways to add veg to your main meals: Add carrots to a chilli. Add lentils to a curry. Pop a can of beans in your casserole. Remember fruit and veg have a different mix of nutrients so you get more goodness by eating a range of them - try a new fruit or veg whenever you get the opportunity.
Eat well. Information and guidance about eating a healthy, balanced diet.
Jun 14, 2022. As of 2019, Kitchen Stories conducted a survey on the eating habits among people in the United Kingdom (UK). It was found that 40.42 percent of the respondents followed a healthy and ...
Ministers must accelerate changes in people's eating habits and food culture if the UK is to meet its targets on health, climate and nature, it says. The UK's consumption of meat and ultra ...
3 September 2020. To mark 30 years of delivering life-changing research and health information advice, World Cancer Research Fund (WCRF) is highlighting how the nation's eating and food shopping habits have changed - alongside people's awareness of cancer prevention - as part of its '30 days has September' campaign. A lot has changed in 30 years; fashion, culture, sport, music, but ...
Share of respondents who are eating more healthy snacks United Kingdom (UK) 2017 Ways U.S. parents encourage healthy eating habits in kids 2016 Mexico: gluten-free products influence on diet ...
Hangover Food. It's well known that traditional British breakfast items are among the best in the world for helping a hangover, and the people of Britain made this a tradition long-ago. Whether it's a bacon butty, sausage and egg sarnie, or the holy-grail of the Full English Breakfast, British food tradition means there's a solution to ...
Consumers who actively try to eat healthy in the UK in 2022/23, by generation. ... University students' change in eating habits in the UK 2022.
Analysing data on shopping habits from thousands of consumers, the thinktank said calorie consumption from takeaway food grew by more than 50% during the height of the pandemic - and had stayed ...