Borderline Personality Disorder Overview Essay
Personality disorders are a group of mental health illnesses defined by specific behavior patterns and distinctive cognitive and affective characteristics. Such disorders are characterized by significant deviations in the way of thinking about oneself and others, emotional responses, regulating behavior, and the ability to relate to other people (Robitz, 2018). This essay will consider borderline personality disorder (BPD), its manifestations, personal characteristics and cognitive features associated with the disease, and potential genetic causes and neurochemical features.
BPD is a severe disorder that can significantly affect one’s health, well-being, and ability to develop meaningful relationships. Patients with BPD often experience sudden mood swings and regularly change their interests and personal values due to the present uncertainty of their place in the world (National Institute of Mental Health, 2017). People diagnosed with the disorder are not capable of building stable relationships as their views and opinions, including those of other people, change suddenly and radically.
BPD is traditionally assessed by completing an in-depth interview with the patient and a medical examination employed to rule out other causes for behavioral manifestations (National Institute of Mental Health, 2017). In addition, the McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD) can be employed for the initial assessment of BPD (Dabaghi et al., 2020). Family history and the patient’s medical history can also be included in the evaluation.
Several risk factors are distinguished when discussing BPD and its development. According to the National Institute of Mental Health (2017), environmental, cultural, social, and family factors are substantial risk factors for developing the disorder. Some studies show a possibility of a genetic predisposition to BPD and state that specific genes can modulate the effect of stressful events on one’s impulsivity and aggression (Bassir Nia et al., 2018).
In particular, catechol o-methyltransferase (COMT) val158met polymorphism and 5-HTTPLR ss/sl polymorphism were found to have a determining effect on one’s aggression and impulsivity. Furthermore, persons diagnosed with BPD often present with structural and functional changes in the brain, specifically, in the prefrontal cortex, responsible for regulating impulses (Bassir Nia et al., 2018; National Institute of Mental Health, 2017). Thus, it can be argued that BPD is the result of the intercorrelation of multiple factors, including genetics, brain structure, and social and environmental aspects.
BPD is generally associated with several typical personality characteristics and cognitive features. The National Institute of Mental Health (2017) distinguishes several BPD personality traits, including feelings of emptiness, distorted self-image, inability to trust other people and build relationships with them, and self-harming behaviors. The disorder is also associated with such cognitive impairments as “deficits in executive functions, response inhibition, attention, and cognitive control and abnormal social cognition” (Bassir Nia et al., 2018, p. 63). Thus, persons with BPD often display intense anger, severe mood swings, impulsive behavior, and suicidal ideation (National Institute of Mental Health, 2017).
Considering the complex nature of the disorder and the genetic, social, family, and environmental factors that determine it, the development of BPD cannot be prevented. However, it can be diagnosed early and managed with effective therapies.
In summary, BPD is a severe, complex mental health disorder characterized by a pattern of unstable moods, impulsive behavior, and destructive self-image. Individuals diagnosed with BPD experience difficulties in building relationships and tend to change their opinions and values regularly. Furthermore, BPD is presented with issues with controlling aggression, focus, and communication. Research into the disorder shows that the risk factors for BPD include genetic predisposition, structural and functional changes in the brain, and environmental, social, and familial factors.
Bassir Nia, A., Eveleth, M. C., Gabbay, J. M., Hassan, Y. J., Zhang, B., & Perez-Rodriguez, M. M. (2018). Past, present, and future of genetic research in borderline personality disorder. Current Opinion in Psychology , 21 , 60–68. Web.
Dabaghi, P., Asl, E., & Taghva, A. (2020). Screening borderline personality disorder: The psychometric properties of the Persian version of the McLean screening instrument for borderline personality disorder . Journal of Research in Medical Sciences , 25 (1), 97–104. Web.
National Institute of Mental Health. (2017). Borderline personality disorder . Web.
Robitz, R. (2018). What are personality disorders? American Psychiatric Association. Web.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, August 14). Borderline Personality Disorder Overview. https://ivypanda.com/essays/borderline-personality-disorder-overview/
"Borderline Personality Disorder Overview." IvyPanda , 14 Aug. 2022, ivypanda.com/essays/borderline-personality-disorder-overview/.
IvyPanda . (2022) 'Borderline Personality Disorder Overview'. 14 August.
IvyPanda . 2022. "Borderline Personality Disorder Overview." August 14, 2022. https://ivypanda.com/essays/borderline-personality-disorder-overview/.
1. IvyPanda . "Borderline Personality Disorder Overview." August 14, 2022. https://ivypanda.com/essays/borderline-personality-disorder-overview/.
Bibliography
IvyPanda . "Borderline Personality Disorder Overview." August 14, 2022. https://ivypanda.com/essays/borderline-personality-disorder-overview/.
- Borderline Personality Disorder: History, Causes, Treatment
- Pain Tolerance in Borderline Personality Disorder
- Borderline Personality Disorder Pathogenesis and Treatment
- Case History of a Borderline Personality Disorder
- Borderline Personality Disorder
- Psychological Therapy: Borderline Personality Disorder
- Causes of Borderline Personality Disorder
- How Childhood Trauma Leads to BPD
- Borderline Personality Disorder Case Report
- Borderline Personality Disorder and Dialectical Behavior Therapy
- Delirium, Dementia and Immobility Disorders
- Psychological Disorders: Causes, Symptoms, Treatment
- The Use of the Cognitive Behavioral Therapy
- Mental Health Project: Binge-Eating Disorder
- Intake Report and Treatment Plan: Obsessive-Compulsive Disorder (OCD)
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

What Triggers a Person With Borderline Personality Disorder?
- BPD Triggers
- BPD Episode
- Helping Someone With BPD
Borderline personality disorder (BPD) is a mental health disorder that is characterized by ongoing patterns of changing moods, behaviors, and self-image. When a person has BPD, they often experience periods of intense feelings of anger, anxiety , or depression that can last for a few hours or a few days. The mood swings experienced by people with BPD can lead to issues with impulsive behavior and can contribute to relationship problems.
People with BPD have various triggers that can set their symptoms in motion. Common triggers include rejection or abandonment in relationships or the resurfacing of a memory of a traumatic childhood event.
This article covers the triggers of borderline personality disorder, how to cope with them, and ways to help someone during a BPD episode.
Verywell / Theresa Chiechi
BPD Episode Triggers
A trigger is an event or situation that brings on symptoms. They can be internal, like a thought or a memory, or external, like an argument in a relationship or losing a job. Triggers that can lead to intense symptoms in a person with BPD include the following:
Relationships
Relationships are one of the most common triggers for people with BPD. People with the disorder tend to experience a higher-than-usual sensitivity to being abandoned by their loved ones. This leads to feelings of intense fear and anger.
In some cases, a person with BPD may self-harm , act impulsively, or attempt suicide if the relationship they are in makes them feel rejected, criticized, or as though they may be abandoned.
For example, people with BPD may jump to negative conclusions if they reach out to a friend and don’t hear back in a short time. When that happens, their thoughts spin out of control, they conclude that they have no friends, and because of that, begin to experience intense emotions that may lead to self-harm.
Relationship Triggers and BPD
Romantic relationships are not the only ones that can trigger a person with BPD to experience an episode. Their relationships with friends, family, and colleagues can also spark symptoms if they experience any sort of rejection, criticism, or threat of abandonment.
Childhood trauma can play a role in both the development of BPD as well as future triggers. Research has found that people with BPD have high rates of childhood abuse, such as emotional and physical neglect and sexual abuse.
When a person with BPD is reminded of a traumatic event, either in their mind or through physical reminders such as seeing a certain person or place, their symptoms can become exacerbated (worsened) and their emotions intensify.
Having BPD may cause a person to be extremely sensitive to any type of criticism. When someone with BPD is criticized, they don’t see it as an isolated incident but rather an attack on their character that paints an entire picture of rejection. When a person with BPD feels rejected, their symptoms can intensify and so can impulsive or self-harming behaviors.
Losing a job is a common trigger for people with BPD because it tends to bring up feelings of rejection and criticism. Since rejection and criticism are so largely triggering, any type of situation that makes them feel that way can worsen or bring on intense symptoms.
How Does Family History Contribute to a BPD Episode?
Many people with BPD have a family history of childhood abuse or neglect. When memories of the events resurface, it can be quite triggering. Research has found that a family history of childhood abuse may also contribute to the development of BPD.
During a BPD Episode
Each person with the disorder is unique and experiences their symptoms in different ways. Some common signs symptoms are worsening in a person with BPD include:
- Intense outbursts of unwarranted anger
- Bouts of high depression or anxiety
- Suicidal or self-harming behaviors
- Impulsive acts they wouldn’t engage in when not in a dysregulated state, such as excessive spending or binge eating
- Unstable self-image
- Dissociation , which is disconnecting from one’s thoughts and feelings or memories and identity
BPD and Substance Abuse
When a person with BPD is having a flare-up of symptoms, they may engage in reckless or impulsive behaviors like substance use. Some research has shown that close to 53% of people with BPD develop a substance use disorder at some point in their lifetimes. People with both BPD and substance use disorder are more impulsive and engage in suicidal behavior more often than those who only have BPD.
Coping Through BPD Triggers
Coping with BPD triggers can be difficult. The first step in being able to do so is by identifying what triggers you.
Because you may be triggered by something that another person with BPD is not triggered by, it can be hard to determine your personal triggers until you investigate which feelings, thoughts, events, and situations set off your symptoms.
Once you have done that, you can avoid your triggers and practice other coping skills.
There are several specialized evidence-based therapies found to be effective in helping people with BPD manage their disorder:
- Dialectical behavior therapy: Dialectical behavior therapy is a type of cognitive behavioral therapy that uses mindfulness, acceptance, and emotion-regulation strategies to change negative thinking patterns and make positive behavioral changes.
- Mentalization-based treatment: Mentalization-based therapy works by helping a person with BPD develop an increased capacity to imagine the thoughts and feelings in their mind and the minds of others to improve interpersonal interactions.
- Schema-focused therapy: This form of therapy helps to identify unhelpful patterns that a person may have developed as a child and replace them with healthier ones.
- Transference-focused psychotherapy: For people with BPD, this type of therapy is centered around building and exploring aspects of a relationship with a therapist to change how relationships are experienced.
- Systems training for emotional predictability and problem-solving (STEPPS): STEPPS is a psycho-educational, group-based treatment that teaches people with BPD more about their disorder and the skills needed to manage their feelings and change unhealthy behaviors.
Can People With BPD Cope Without Medication?
Although people with BPD are often prescribed antidepressants, antipsychotics, and mood-stabilizing anticonvulsant medications, there is no medication formally approved for the treatment of BPD. Research has found that the most effective treatment is different therapies designed to help people with BPD recognize their emotions and react differently to negative thoughts and feelings.
There are several self-care techniques that you can adopt to help you cope and manage your disorder:
- Learning mindfulness techniques through meditation apps
- Grounding yourself in difficult moments so that you can bring your focus to the present time
- Seeking out emotional and practical support such as therapy groups and friends and family
- Acknowledging unhealthy behaviors and avoiding them by pressing pause on your feelings before you act or react
- Staying active to keep your mind distracted when you have high levels of anger or irritability
Pressing Pause on Negative Emotions
While it can be difficult to just force yourself to stop feeling a certain way, you can practice patience and pause to collect yourself when you do feel an overwhelming rush of negative emotions. By taking a step back from the situation and taking a few deep breaths, you may be able to calm your mind and, thus, lessen the negative emotions that are trying to take over.
How to Help Someone Else During a BPD Episode
When someone you care about has BPD, it can be hard to know how to help them. However, there are things that you can do to support them with the ups and downs of their condition:
- Educate yourself about the disorder and all that it entails: People with BPD often engage in mean-spirited behaviors, but that is their illness taking over. It’s important to learn about the disorder so that you can better understand what is motivating their behavior.
- Support them when they reach out for help: While you can’t force someone to seek professional help, you can be patient with them and support them when they finally do. To support their decision, you can voice how proud you are of them or offer to accompany them to their appointments. People with BPD who have strong support systems see a greater improvement in their symptoms than those without any support.
- Listen and validate: You don’t have to agree with how a person with BPD sees a situation to listen attentively and validate that they are not wrong to feel what they’re feeling. Just knowing that they have validation can provide relief to someone with BPD during an episode.
- Never ignore self-harming behaviors or threats: Many people with BPD may threaten to harm themselves several times without acting on it. This can lead to their loved ones taking their suicidal ideations less seriously. However, as many as 75% of people with BPD attempt suicide at some point in their life so even threats need to be taken seriously.
What to Do if Your Loved One With BPD Threatens Suicide
If your loved one threatens suicide, call 911 immediately. It can also be helpful to recognize signs that your loved one is thinking about self-harming behaviors because they may not always voice them aloud. Suicidal actions or threats always warrant professional evaluation.
People who cope with BPD often go through times of normalcy that are broken up by episodes. Everyone has unique triggers because each person is different, but one common theme among many people with BPD is the fear of rejection or abandonment.
To cope with the illness, it’s important to recognize triggers so that you can avoid them when possible. When symptoms do arise, seeking help or practicing self-care techniques may allow you to manage the symptoms and avoid overindulging in unhealthy behaviors.
Bungert M, Liebke L, Thome J, Haeussler K, Bohus M, Lis S. Rejection sensitivity and symptom severity in patients with borderline personality disorder: effects of childhood maltreatment and self-esteem. Borderline Personal Disord Emot Dysregul. 2015 Mar 20;2:4. doi:10.1186/s40479-015-0025-x
Miskewicz K, Fleeson W, Arnold EM, Law MK, Mneimne M, Furr RM. A Contingency-Oriented Approach to Understanding Borderline Personality Disorder: Situational Triggers and Symptoms. J Pers Disord. 2015 Aug;29(4):486-502. doi:10.1521/pedi.2015.29.4.486
Kulacaoglu F, Kose S. Borderline Personality Disorder (BPD): In the Midst of Vulnerability, Chaos, and Awe. Brain Sci. 2018 Nov 18;8(11):201. doi:10.3390/brainsci8110201
National Institute of Mental Health. Borderline Personality Disorder .
Trull TJ, Freeman LK, Vebares TJ, Choate AM, Helle AC, Wycoff AM. Borderline personality disorder and substance use disorders: an updated review. Borderline Personal Disord Emot Dysregul . 2018;5:15. doi:10.1186/s40479-018-0093-9
Choi-Kain LW, Finch EF, Masland SR, Jenkins JA, Unruh BT. What Works in the Treatment of Borderline Personality Disorder. Curr Behav Neurosci Rep. 2017;4(1):21-30. doi:10.1007/s40473-017-0103-z
Biskin RS. The Lifetime Course of Borderline Personality Disorder. Can J Psychiatry. 2015 Jul;60(7):303-308. doi:10.1177/070674371506000702
Ng FY, Bourke ME, Grenyer BF. Recovery from Borderline Personality Disorder: A Systematic Review of the Perspectives of Consumers, Clinicians, Family and Carers . PLoS One. 2016 Aug 9;11(8):e0160515. doi:10.1371/journal.pone.0160515
Goodman M, Tomas IA, Temes CM, Fitzmaurice GM, Aguirre BA, Zanarini MC. Suicide attempts and self-injurious behaviours in adolescent and adult patients with borderline personality disorder . Personal Ment Health. 2017 Aug;11(3):157-163. doi:10.1002/pmh.1375
By Angelica Bottaro Angelica Bottaro is a professional freelance writer with over 5 years of experience. She has been educated in both psychology and journalism, and her dual education has given her the research and writing skills needed to deliver sound and engaging content in the health space.
- Patient Care & Health Information
- Diseases & Conditions
- Borderline personality disorder
Borderline personality disorder is a mental health condition that affects the way people feel about themselves and others, making it hard to function in everyday life. It includes a pattern of unstable, intense relationships, as well as impulsiveness and an unhealthy way of seeing themselves. Impulsiveness involves having extreme emotions and acting or doing things without thinking about them first.
People with borderline personality disorder have a strong fear of abandonment or being left alone. Even though they want to have loving and lasting relationships, the fear of being abandoned often leads to mood swings and anger. It also leads to impulsiveness and self-injury that may push others away.
Borderline personality disorder usually begins by early adulthood. The condition is most serious in young adulthood. Mood swings, anger and impulsiveness often get better with age. But the main issues of self-image and fear of being abandoned, as well as relationship issues, go on.
If you have borderline personality disorder, know that many people with this condition get better with treatment. They can learn to live stabler, more-fulfilling lives.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Borderline personality disorder affects how you feel about yourself, relate to others and behave.
Symptoms may include:
- A strong fear of abandonment. This includes going to extreme measures so you're not separated or rejected, even if these fears are made up.
- A pattern of unstable, intense relationships, such as believing someone is perfect one moment and then suddenly believing the person doesn't care enough or is cruel.
- Quick changes in how you see yourself. This includes shifting goals and values, as well as seeing yourself as bad or as if you don't exist.
- Periods of stress-related paranoia and loss of contact with reality. These periods can last from a few minutes to a few hours.
- Impulsive and risky behavior, such as gambling, dangerous driving, unsafe sex, spending sprees, binge eating, drug misuse, or sabotaging success by suddenly quitting a good job or ending a positive relationship.
- Threats of suicide or self-injury, often in response to fears of separation or rejection.
- Wide mood swings that last from a few hours to a few days. These mood swings can include periods of being very happy, irritable or anxious, or feeling shame.
- Ongoing feelings of emptiness.
- Inappropriate, strong anger, such as losing your temper often, being sarcastic or bitter, or physically fighting.
When to see a doctor
If you're aware that you have any of the symptoms above, talk to your doctor or other regular healthcare professional or see a mental health professional.
If you have thoughts about suicide
If you have fantasies or mental images about hurting yourself, or you have thoughts about suicide, get help right away by taking one of these actions:
- Call 911 or your local emergency number right away.
- Contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline, available 24 hours a day, seven days a week. Or use the Lifeline Chat . Services are free and confidential.
- U.S. veterans or service members who are in crisis can call 988 and then press "1" for the Veterans Crisis Line . Or text 838255. Or chat online.
- The Suicide & Crisis Lifeline in the U.S. has a Spanish language phone line at 1-888-628-9454 (toll-free).
- Call your mental health professional, doctor or another member of your healthcare team.
- Reach out to a loved one, close friend, trusted peer or co-worker.
- Contact someone from your faith community.
If you notice symptoms in a family member or friend, talk to that person about seeing a doctor or mental health professional. But you can't force someone to change. If the relationship causes you a lot of stress, you may find it helpful to see a therapist.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
As with other mental health conditions, the causes of borderline personality disorder aren't fully known. In addition to environmental factors — such as a history of child abuse or neglect — borderline personality disorder may be linked to:
- Genetics. Some studies of twins and families suggest that personality disorders may be inherited or strongly related to other mental health conditions among family members.
- Changes in the brain. Some research has shown that changes in certain areas of the brain affect emotions, impulsiveness and aggression.
Risk factors
Factors related to personality development that can raise the risk of getting borderline personality disorder include:
- Hereditary predisposition. You may be at a higher risk if a blood relative — your mother, father, brother or sister — has the same or a like condition.
- Stressful childhood. Many people with the condition report being sexually or physically abused or neglected during childhood. Some people have lost or were separated from a parent or close caregiver when they were young or had parents or caregivers with substance misuse or other mental health issues. Others have been exposed to hostile conflict and unstable family relationships.
Complications
Borderline personality disorder can damage many areas of your life. It can negatively affect close relationships, jobs, school, social activities and how you see yourself.
This can result in:
- Repeated job changes or losses.
- Not finishing an education.
- Multiple legal issues, such as jail time.
- Conflict-filled relationships, marital stress or divorce.
- Injuring yourself, such as by cutting or burning, and frequent stays in the hospital.
- Abusive relationships.
- Unplanned pregnancies, sexually transmitted infections, motor vehicle accidents, and physical fights due to impulsive and risky behavior.
- Attempted suicide or death due to suicide.
Also, you may have other mental health conditions, such as:
- Depression.
- Alcohol or other substance misuse.
- Anxiety disorders.
- Eating disorders.
- Bipolar disorder.
- Post-traumatic stress disorder (PTSD).
- Attention-deficit/hyperactivity disorder (ADHD).
- Other personality disorders.
- Personality disorders. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5-TR. 5th ed. American Psychiatric Association; 2022. https://dsm.psychiatryonline.org. Accessed April 28, 2023.
- Borderline personality disorder. National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/borderline-personality-disorder/. Accessed April 28, 2023.
- Skodol A. Borderline personality disorder: Epidemiology, pathogenesis, clinical features, course, assessment and diagnosis. https://www.uptodate.com/contents/search. Accessed April 28, 2023.
- Skodol A. Approach to treating patients with borderline personality disorder. https://www.uptodate.com/contents/search. Accessed April 28, 2023.
- The lifeline and 988. 988 Suicide & Crisis Lifeline. https://988lifeline.org/current-events/the-lifeline-and-988/. Accessed April 28, 2023.
- Borderline personality disorder. National Alliance on Mental Illness. https://www.nami.org/About-Mental-Illness/Mental-Health-Conditions/Borderline-Personality-Disorder. Accessed April 28, 2023.
- Starcevic V, et al. Pharmacotherapy of borderline personality disorder: Replacing confusion with prudent pragmatism. Current Opinion in Psychiatry. 2018; doi:10.1097/YCO.0000000000000373.
- Veterans Crisis Line. U.S. Department of Veteran Affairs. https://www.veteranscrisisline.net/. Accessed April 28, 2023.
- Allen ND (expert opinion). Mayo Clinic. June 21, 2023.
- Ekiz E, et al. Systems Training for Emotional Predictability and Problem-Ssolving for borderline personality disorder: A systematic review. Personal Mental Health. 2023; doi:10.1002/pmh.1558.
- Mendez-Miller M, et al. Borderline personality disorder. American Family Physician. 2022. https://www.clinicalkey.com. Accessed April 28, 2023.
- Lebow J. Overview of psychotherapies. https://www.uptodate.com/contents/search. Accessed April 28, 2023.
- Elsevier Point of Care. Borderline personality disorder. https://www.clinicalkey.com. Accessed April 28, 2023.
Associated Procedures
- Psychotherapy
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
REVIEW article
Twenty years of research on borderline personality disorder: a scientometric analysis of hotspots, bursts, and research trends.

- 1 Department of Psychology, School of Humanities and Social Sciences, Anhui Agricultural University, Hefei, China
- 2 College of Computing & Informatics, Drexel University, Philadelphia, PA, United States
- 3 Department of Psychology, School of Education, China University of Geosciences, Wuhan, China
- 4 Department of Information Management, Anhui Vocational College of Police Officers, Hefei, China
Borderline personality disorder (BPD), a complex and severe psychiatric disorder, has become a topic of considerable interest to current researchers due to its high incidence and severity of consequences. There is a lack of a bibliometric analysis to visualize the history and developmental trends of researches in BPD. We retrieved 7919 relevant publications on the Web of Science platform and analyzed them using software CiteSpace (6.2.R4). The results showed that there has been an overall upward trend in research interest in BPD over the past two decades. Current research trends in BPD include neuroimaging, biological mechanisms, and cognitive, behavioral, and pathological studies. Recent trends have been identified as “prevention and early intervention”, “non-pharmacological treatment” and “pathogenesis”. The results are like a reference program that will help determine future research directions and priorities.
1 Introduction
Borderline personality disorder (BPD) is a complex and severe psychiatric disorder characterized by mood dysregulation, interpersonal instability, self-image disturbance, and markedly impulsive behavior (e.g., aggression, self-injury, suicide) ( 1 ). In addition, people with BPD may have chronic, frequent, random feelings of emptiness, fear, and so on. These symptoms often lead them to use unhealthy coping mechanisms in response to negative emotions, such as alcohol abuse ( 2 ). BPD has a long course, which makes treatment difficult and may have a negative impact on patients’ quality of life ( 3 ). Due to its clinical challenge, BPD is by far the most studied category of personality disorder ( 4 ). This disorder is present in 1−3% of the general population as well as in 10% of outpatients, 15−20% of inpatients, and 30−60% of patients with a diagnosed personality disorder, and has a suicide rate of up to 10% ( 5 , 6 ). Families of individuals with serious mental illness often experience distress, and those with relatives diagnosed with BPD tend to carry a heavier burden compared to other mental illnesses ( 7 , 8 ). As early as the 20th century, scholars began describing BPD and summarizing its symptoms. However, there was some debate regarding the precise definition of BPD.
In the past few decades, the research community has made remarkable progress in the study of BPD, equipping us with a wider range of perspectives and tools for understanding this intricate condition. However, numerous challenges still remain to be tackled by researchers. Diagnosing BPD is inherently challenging and often more difficult than anticipated. The symptoms of BPD are complex, diverse, and often overlap with those of other mental health conditions. For example, individuals with BPD may experience extreme mood swings similar to those observed in individuals with bipolar disorder ( 9 ); At the same time, they may also be entrenched in long-term depression, making it easy for doctors to initially misdiagnose them with depression ( 10 ). Because these symptoms overlap and interfere with each other, doctors often face the risk of misdiagnosing or overlooking the condition during initial diagnosis. Therefore, researchers are working to develop more accurate and comprehensive diagnostic tools and methods.
According to the “Neuro-behavioral Model” proposed by Lieb ( 1 ), the process of BPD formation is very complex and is determined by the interaction of several factors. The interaction between different factors can be complex and dynamic. Genetic factors and adverse childhood experiences may contribute to emotional disorders and impulsivity, leading to dysfunctional behaviors and inner conflicts. These, in turn, can reinforce emotional dysregulation and impulsivity, exacerbating the preexisting conditions. Genetic factors are an important factor in the development of BPD ( 11 ). Psychosocial factors, including adverse childhood experiences, have also been strongly associated with the development of BPD ( 12 ). Emotional instability and impulsive behavior are even more common in patients with BPD ( 13 ). The current study is based on the “Neuro-behavioral Model” and conducts a literature review of previous scientific research on BPD through bibliometric analysis to reorganize the influencing factors. Through large-sample data analysis, the association between BPD and other diseases is explored, which contributes to further refining this theory’s explanation of the common neurobiological mechanisms among various mental illnesses.
It is worth noting that with the development of BPD, some scholars have conducted bibliometrics studies on BPD to provide insights into this academic field. To date, the current study has identified two published bibliometric studies on the field: One is Ilaria M. A. Benzi and her colleagues’ 2020 metrological analysis of the literature in the field of BPD pathology for the period 1985−2020 ( 14 ). The other is a bibliometric analysis by Taylor Reis and his colleagues of the growth and development of research on personality disorders between 1980 and 2019 ( 15 ). Ilaria M. A. Benzi and her colleagues integrated and sorted out the research results of borderline personality pathology, and revealed the research results and development stages in this field through the method of network and cluster analysis. The results of the study clearly demonstrate that the United States and European countries are the main contributors, that institutional citations are more consistent, and that BPD research is well developed in psychiatry and psychology. At the same time, the development of research in borderline personality pathology is demonstrated from the initial development of the construct, through studies of treatment effects, to the results of longitudinal studies. Taylor Reis and his colleagues used a time series autoregressive moving average model to analyze publishing trends for different personality disorders to reveal their historical development patterns, and projected the number of publications for the period 2024 to 2029. The study finds a trend towards diversity in the research and development of personality disorders, with differences in publication rates for different types of personality disorders, and summarizes the reasons that influence these differences. This may ultimately determine which personality disorders will remain in future psychiatric classifications. These studies have provided valuable insights into the evolution of BPD, focusing primarily on its pathology or a broader personality disorder perspective. While basic bibliometric analyses of these studies have been conducted, there is a need for more in-depth investigations of specific trends in the evolution of BPD and a clearer delineation of emerging research foci. Therefore, in order to enhance the current study, this study extends the analysis to 2022 and utilizes a comprehensive structural variation analysis of the literature using scientometric methods. Building on previous bibliometric studies, we expect to provide new insights and additions to research in this area. At the same time, the research trends and hot topics in the field of BPD are further explored. In addition, several cocitation-based analyses are also carried out in order to better understand citation performance.
2.1 Objectives
One of our goals was to understand the current status and progress of researches on BPD, and to summarize the latest developments and research findings in BPD, such as new treatment methods and disease mechanisms. Through the intuitive presentation of knowledge graphs and other images or data, we aimed to provide clinical practice and research guidance for clinicians, researchers, and policymakers.
Our second goal was to help identify future research directions and priorities, and provide more scientific and systematic research guidance for researchers. For example, by identifying hotspots and associations in certain research areas, we can determine the fields and issues that require further investigations, thus providing clearer directions and focus for researches. Additionally, through bibliometric analysis, we can provide researchers with more targeted and practical research strategies and methods, improving research efficiency and the quality of research outcomes.
2.2 Search strategy and data collection
The selection of appropriate methods and tools in the process of analyzing research information is crucial. Web of Science (WOS) is a popular database for bibliometric analysis that includes numerous respectable and high-impact academic journals. In addition, data information, such as references and citations, is more extensive than other academic databases ( 16 ). Data collection took place on the date of May 10, 2023. The search strategy included the following: topic=“Neuro-behavioral Model” or “borderline characteristics” or “borderline etiology” or “borderline personality disorder”, database selected=WOS Core Collection, time span=2003−2022, index=Science Citation Index Expanded (SCI-EXPENDED) and Social Sciences Citation Index (SSCI). The “Neuro-behavioral Model” serves as a theoretical framework that is useful for explaining the development and pathophysiology of BPD; “borderline characteristics” can describe the related symptoms and features of BPD; “borderline etiology” helps to understand the factors that contribute to the development of BPD; “borderline personality disorder” is the most commonly used terms in relevant research. Using these as keywords in title searches can help researchers find researches related to BPD more accurately, facilitating deeper understanding of the characteristics, pathophysiology, etiology, and other aspects of BPD. In the current study, we focused only on two types of literature: articles and review articles, and limited the language to English. After removing all literature unrelated to BPD, a total of 7919 records met the criteria. They were exported in record and reference formats, and saved in plain text file format.
2.3 Data analysis and tools
Bibliometrics was first proposed by Alan Pritchard in 1969, as a method that combines data visualization to analyze publications statistically and quantitatively in specific fields and journals ( 17 ). Bibliometric analysis is a good way to analyze the trend of knowledge structure and research activities in scientific fields over time, and has been widely used in various fields since it was first used ( 18 ). Scientometrics is the application of bibliometrics in scientific fields, and it focuses on the quantitative characteristics and features of science and scientific researches ( 19 ). Compared to traditional literature review studies, visualized knowledge graphs can accurately identify key articles from many publications, comprehensively and systematically combing existing research in a field ( 20 ).
Currently, two important academic indicators are included in research. The impact factor (IF) is used as an indicator of a publication’s impact to assess the quality and importance of the publication ( 21 ). However, some researchers believe that IF has defects such as inaccuracy and misuse ( 22 ). Although many researchers have proposed to replace the impact factor with other indicators, IF is still one of the most effective ways to measure the impact of a journal ( 23 ). The IF published in the 2021 Journal Citation Reports were used. Another indicator is the H-index, which is an important measure of a scholar’s academic achievements. Some researchers consider it as a correction or supplement to the traditional IF ( 24 ).
All data were imported into CiteSpace (6.2.R4) and Scimago Graphica (1.0.30) for analysis. CiteSpace was used to obtain collaboration networks and impact networks. Scimago Graphica was used to construct a network graph of country collaboration. CiteSpace is a Java-based software developed in the context of scientometrics and data visualization ( 25 ). It combines scientific knowledge mapping with bibliometric analysis to determine the progress and current research frontiers in a particular field, as well as predict the development trends in that field ( 26 ). Scimago Graphica is a no-code tool. It can not only perform visualization analysis on communication data but also explore exploratory data ( 27 ). Currently, it is used for visual analysis of national cooperation relationships, displaying the geographic distribution of countries and publication trends.
3.1 Analysis of publication outputs, and growth trend prediction
Annual publications can provide an overview of the evolution of a research area and its progress ( 28 ). We retrieved 7919 articles from the WOS database on BPD between 2003 and 2022, including 6834 research articles and 1085 reviews ( Figure 1 ). As of the search date, these articles had received a total of 289,958 citations, equating to an average of 14,498 citations per year. Over the past two decades, the number of research articles published on BPD has shown a fluctuating upward trend. In addition, citations to these publications have increased significantly. A polynomial curve fit of the literature on BPD clearly indicates a strong correlation between the year of publication and the number of publications ( R 2 = 0.973). The number of research articles on BPD has indeed fluctuated and increased over the past two decades. This observation does, to some extent, indicate an upward trend, probably due to increasing interest in BPD. However, there are other factors to consider as well. For example, the accumulation of data or technological advances, government policies and corporate investment may also affect the direction of BPD research development.
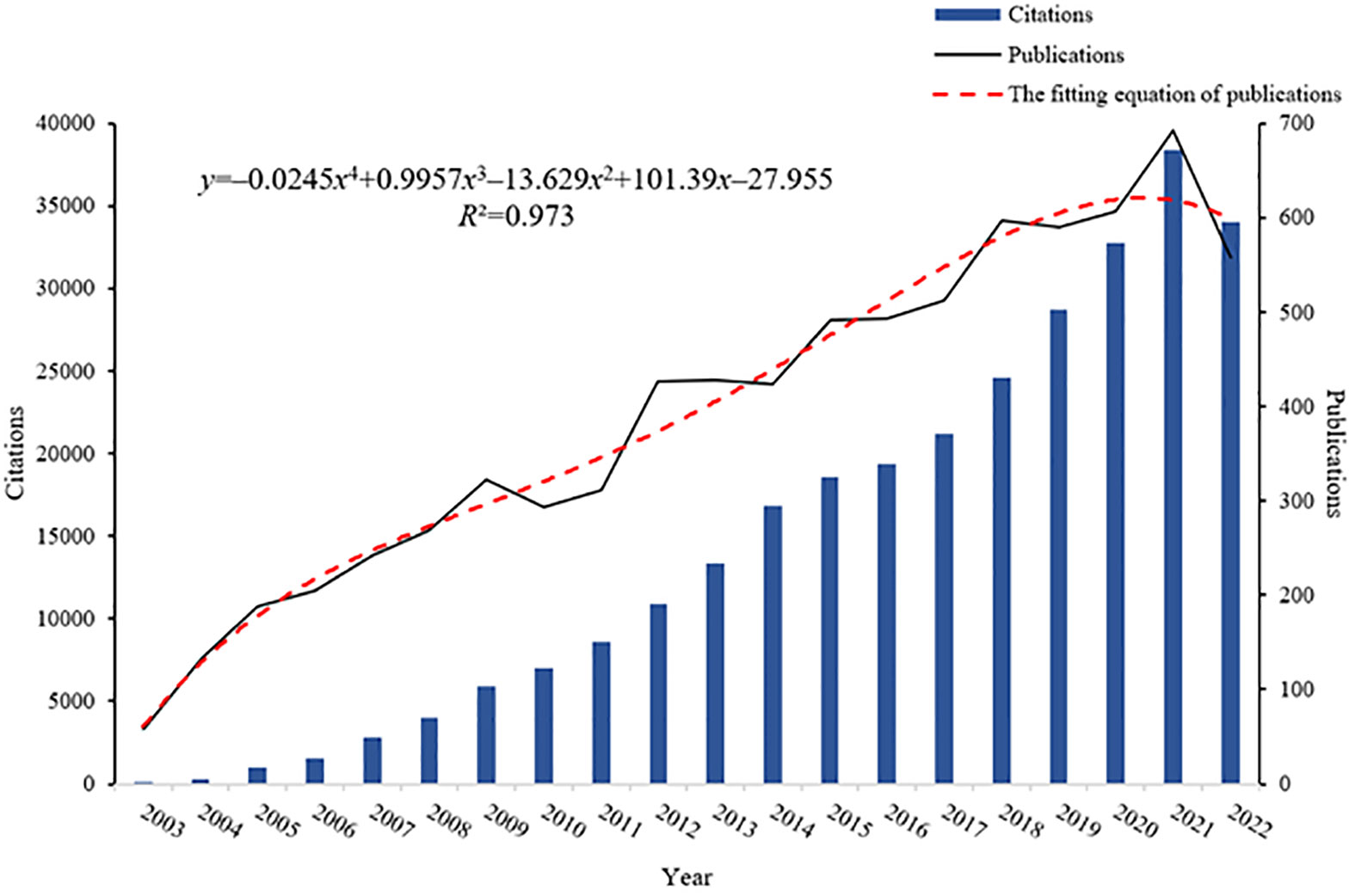
Figure 1 Annual publications, citation counts, and the fitting equation for annual publications in BPD.
3.2 Analysis of co-citation references: clusters and timeline of research
Co-cited references, which are cited by multiple papers concurrently, are considered a crucial knowledge base in any given field ( 28 ). In the current study, CiteSpace clustering was utilized to identify common themes within BPD-related literature. Figure 2 presented a co-citation network of highly cited references between 2003 and 2022, comprising 1163 references. A time slice of 1 was used, with the g -index was set at k =25, which resulted in the identification of 14 clusters representing distinct research themes in BPD. The significant cluster structure is denoted by a modularity value ( Q value) of 0.7974, and the high confidence level in the clusters by an average profile value ( S value) of 0.9176.
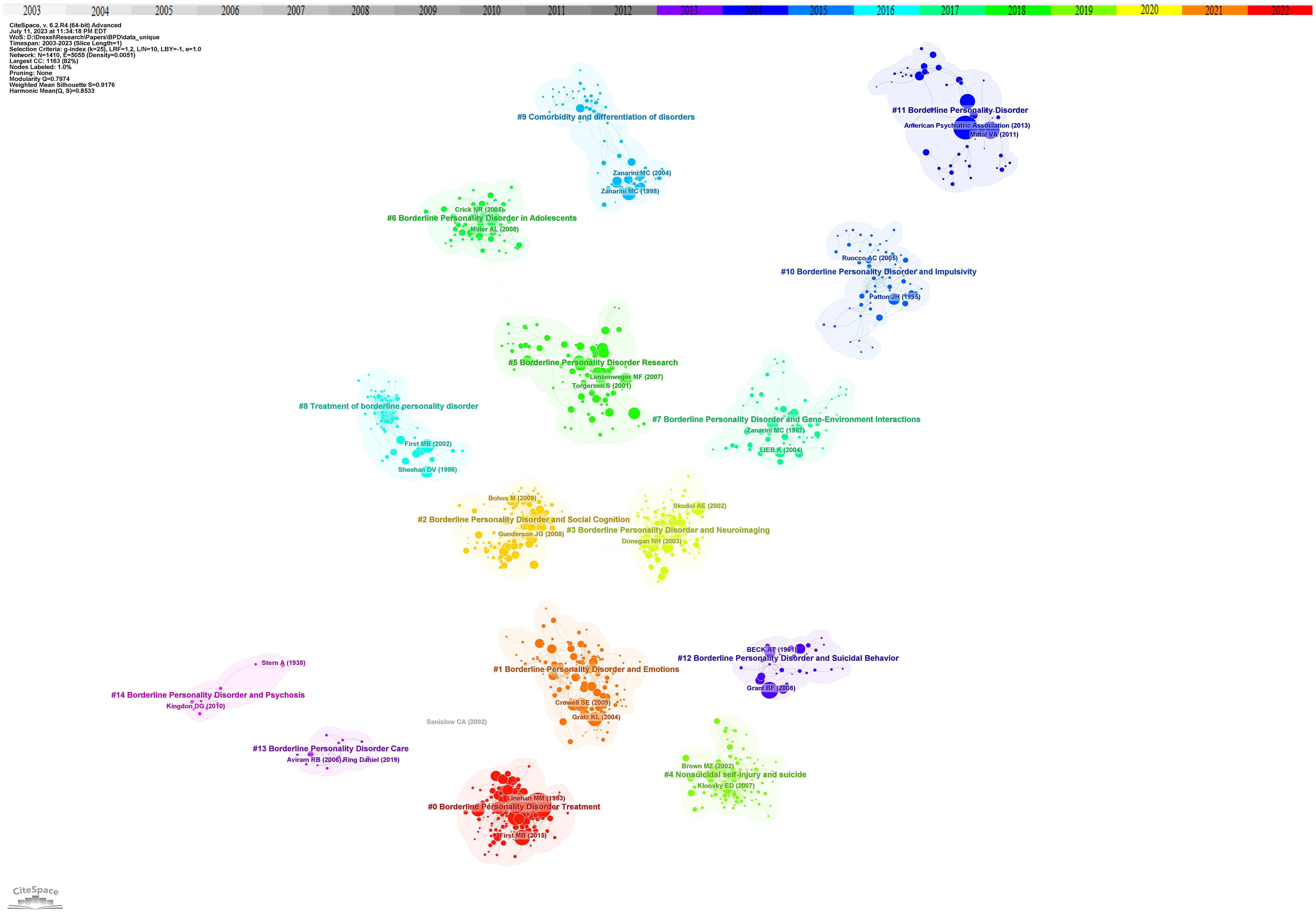
Figure 2 Reference co-citation network with cluster visualization in BPD. Trend 1 clinical researches, sub-trend clinical characteristics includes clusters #1, #2, #4, #10, #12; biological mechanisms include clusters #3, #7; nursing treatments includes clusters #0, #8, #13. Trend 2 associations and complications includes clusters #5, #6, #9, #11, #14.
Cluster analysis is performed through CiteSpace. Related clusters are classified into the same trend based on the knowledge of related fields and whether the clusters show similar trends. At the same time, based on the analysis of time series, to identify the movement of one cluster to another. Based on the cluster map of co-cited references on BPD, several different research trends were identified. The first major research trend is clinical research on BPD, which in turn consists of three sub-trends: clinical characterization of BPD, biological mechanisms, and nursing treatment. Of the data obtained, the earliest research on the clinical characterization of BPD began in 1992 with cluster #12, “borderline personality disorder and suicidal behavior” ( S =0.979; 1992). Paul H. Soloff and his colleagues conducted a comparative study of suicide attempts between major depressives and patients with BPD. The aim of this study was to develop more effective intervention strategies for suicide prevention ( 29 ). This cluster was further developed in cluster #4, “nonsuicidal self-injury and suicide” ( S =0.96; 2004). Thomas A. Widiger and Timothy J. Trull proposed a more flexible dimension-based categorization model to overcome the previous drawbacks of personality disorder categorization ( 30 ). Next in cluster #10 “borderline personality disorder and impulsivity” ( S =0.93; 2000), Jim H. Patton and his colleagues revised the Barratt Impulsivity Scale to measure impulsivity to facilitate practical clinical research ( 31 ). Related research continues to evolve into cluster #1 “borderline personality disorder and emotions” ( S =0.87; 2007) and cluster #2 “borderline personality disorder and social cognition” ( S =0.911; 2009), researchers have focused on understanding the causal relationship between BPD traits and factors such as social environment, emotion regulation, and interpersonal evaluative bias, as well as their potential impact ( 32 , 33 ). In the sub-trend of biological mechanisms, two main clusters are involved: cluster #7 “borderline personality disorder and gene-environment interactions” ( S =0.871; 2002) and cluster #3 “borderline personality disorder and neuroimaging” ( S =0.938; 2007). In the related cluster, researchers have found a relationship between BPD and genetic and environmental factors ( 34 ). Researchers have also utilized various external techniques to explore the degree of correlation between the risk of developing BPD and its biological mechanisms, aiming to reveal the complex mechanisms that influence the emergence and development of BPD ( 35 ). In nursing treatment, cluster #8 “treatment of borderline personality disorder “ ( S =0.968; 2001), Silvio Bellino and his colleagues systematically analyzed the current publications on BPD pharmacotherapy research and summarized relevant clinical trials and findings ( 36 ). However, due to the complexity of BPD, there is still a lack of information on the exact efficacy of pharmacotherapy in BPD, and therefore pharmacotherapy remains an area of ongoing development and research. This trend continues to be developed in cluster #0 “borderline personality disorder treatment” ( S =0.887; 2006), which emphasizes the development of novel pharmacotherapies for BPD. Cluster #13 “borderline personality disorder care” ( S =0.997; 2013) mainly focuses on the comprehensive care of people with borderline personality disorder and the education of patients and families. The goal is to improve patients’ quality of life, reduce self-injury and suicidal behavior, and promote full recovery.
The second major research trend is association and comorbidity. This trend first began in cluster #9 “comorbidity and differentiation of disorders” ( S =0.946; 1999). Mary C Zanarini and his colleagues explored the comorbidity of BPD with other psychiatric disorders on Axis I ( 37 ). Cluster #14 “borderline personality disorder and psychosis” ( S =0.966; 2003) also explored symptoms associated with BPD ( 38 ). This trend continues, with researchers studying BPD research in cluster #11 “borderline personality disorder” ( S =0.935; 2004) and cluster #5 “borderline personality disorder research” ( S =0.881; 2007) ( 39 , 40 ). In addition, cluster #6 “borderline personality disorder in adolescents” ( S =0.894; 2011) points out that the focus of BPD research is increasingly shifting towards adolescents ( 41 ).
Figure 3 showed the time span and research process of the developmental evolution of these different research themes. The temporal view reveals the newest and most active clusters, namely #0 “dialectical behavior therapy”, #1 “daily life”, and #2 “social cognition”, which have been consistently researched for almost a decade. Cluster #0 “dialectical behavior therapy” has the largest number and the longest duration, lasting almost 10 years. Similarly, this article by Rebekah Bradley and Drew Westen on understanding the psychodynamic mechanisms of BPD from the perspective of developmental psychopathology has the largest node ( 34 ).
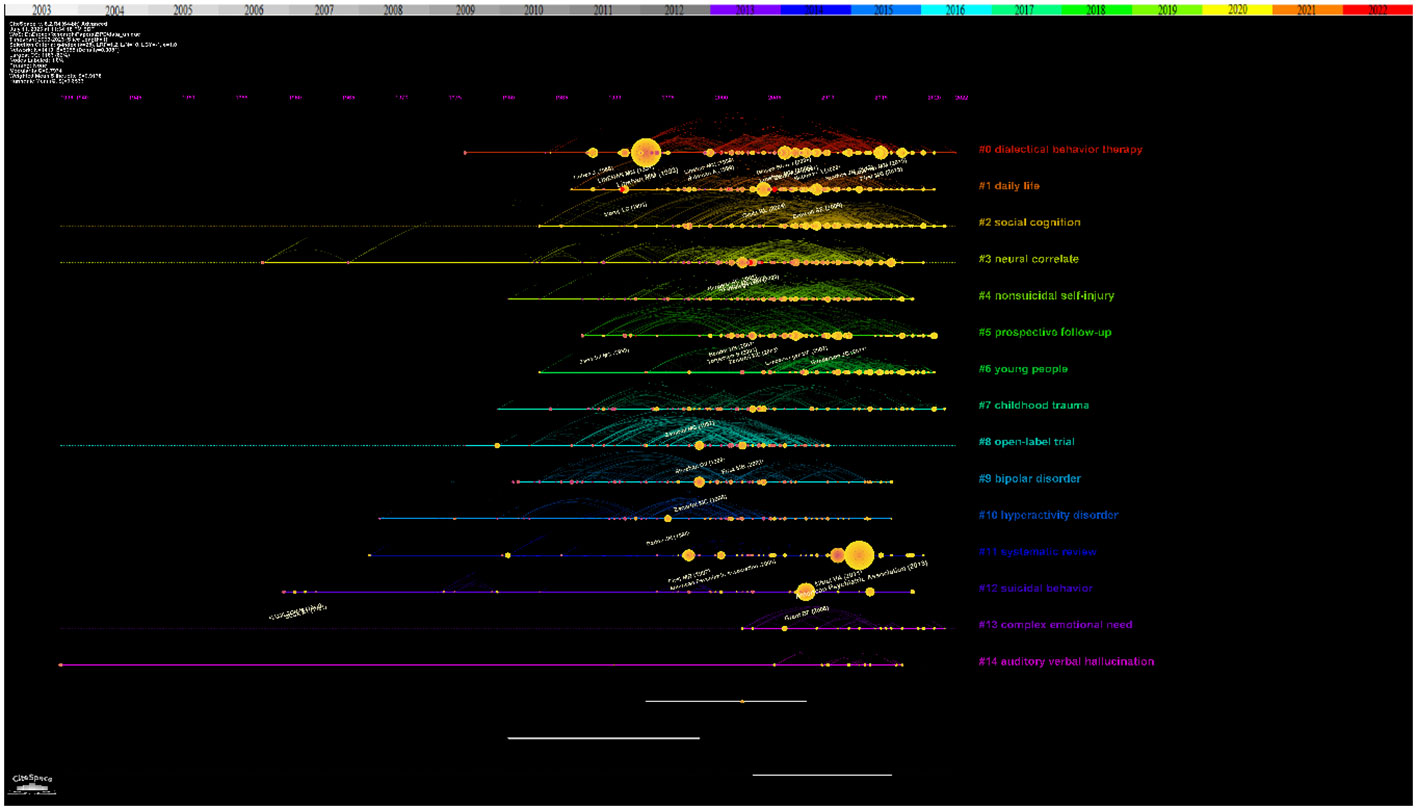
Figure 3 Reference co-citation network with timeline visualization in BPD.
3.3 Most cited papers
The top 10 highly cited papers on BPD research were presented in Table 1 . The most cited paper, by Marsha M. Linehan and colleagues, focus on the treatment of suicidal behavior in BPD ( 42 ). The transition between suicidal and non-suicidal self-injurious behavior in individuals with BPD has attracted researchers’s attention, mainly in cluster #4 “nonsuicidal self-injury and suicide” ( 52 ). The second is the experimental study by Josephine Giesen-Bloo and his colleagues on the psychotherapy of BPD ( 43 ). In cluster #0 “borderline personality disorder treatment” and Cluster #8 “treatment of borderline personality disorder”, researchers strive to find non-pharmacological approaches with comparable or enhanced therapeutic effects. This was followed by Sheila E. Crowell and her colleagues’ study of the biological developmental patterns of BPD ( 44 ). Research on the biological mechanisms and other contributing factors of BPD, including #7 “borderline personality disorder and gene-environment interactions” have been closely associated with the development of BPD ( 53 ).
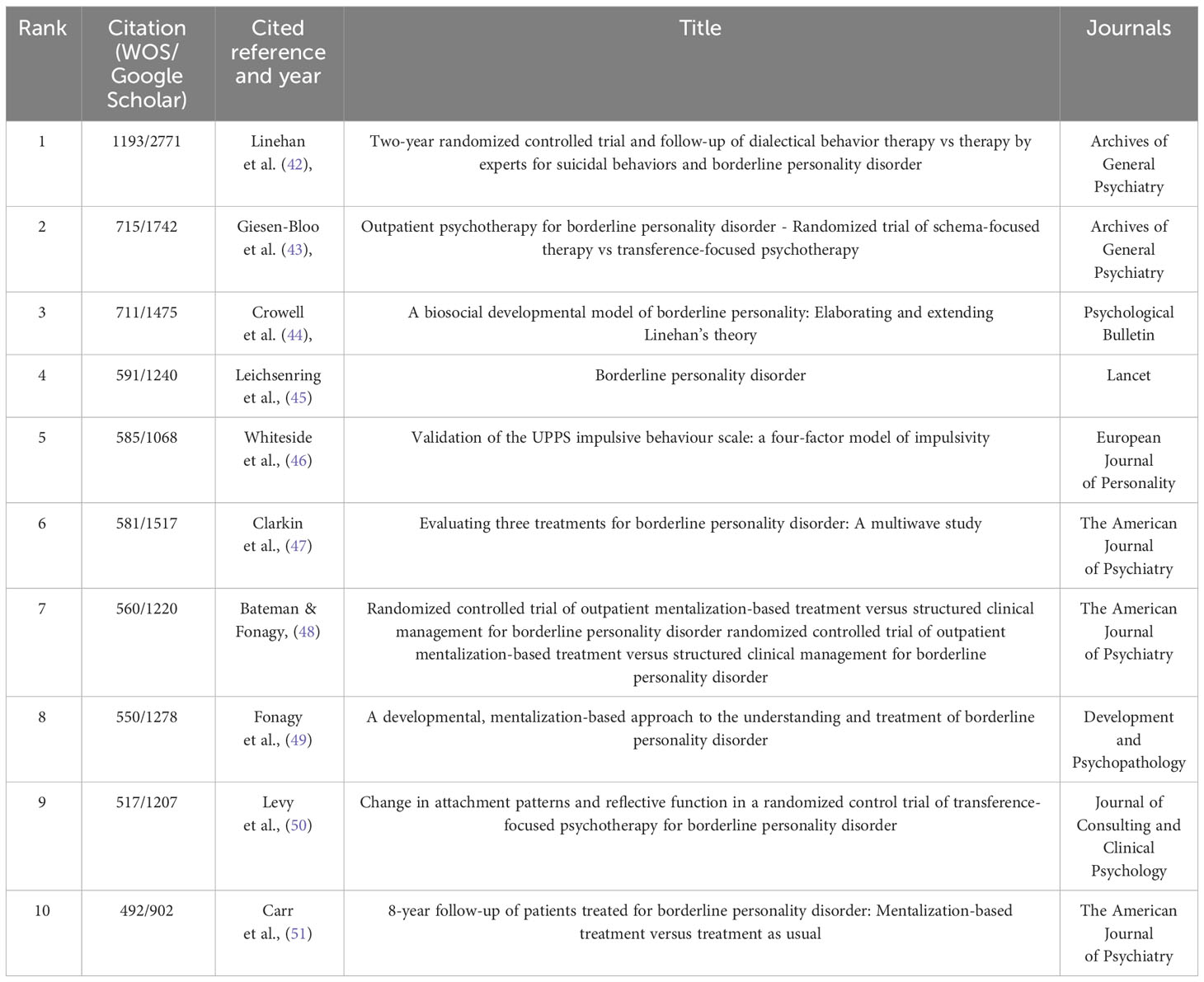
Table 1 Top 10 cited references that published BPD researches.
3.4 Burst analysis and transformative papers
The “citation explosion” reflects the changing research focus of a field over time and indicates that certain literature has been frequently cited over time. Figure 4 showed the top 9 references with the highest citation intensity. The three papers with the greatest intensity of outbursts during the period 2003−2022 are: The first is the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders ( 54 ). In the second article, Vijay A. Mittal and Elaine F. Walker discuss key issues surrounding dyspraxia, tics, and psychosis that are likely to appear in an upcoming edition of the Diagnostic and Statistical Manual of Mental Disorders ( 39 ). In addition, Ioana A. Cristea and colleagues conducted a systematic review and meta-analysis to evaluate the effectiveness of psychotherapy for borderline personality disorder ( 55 ).
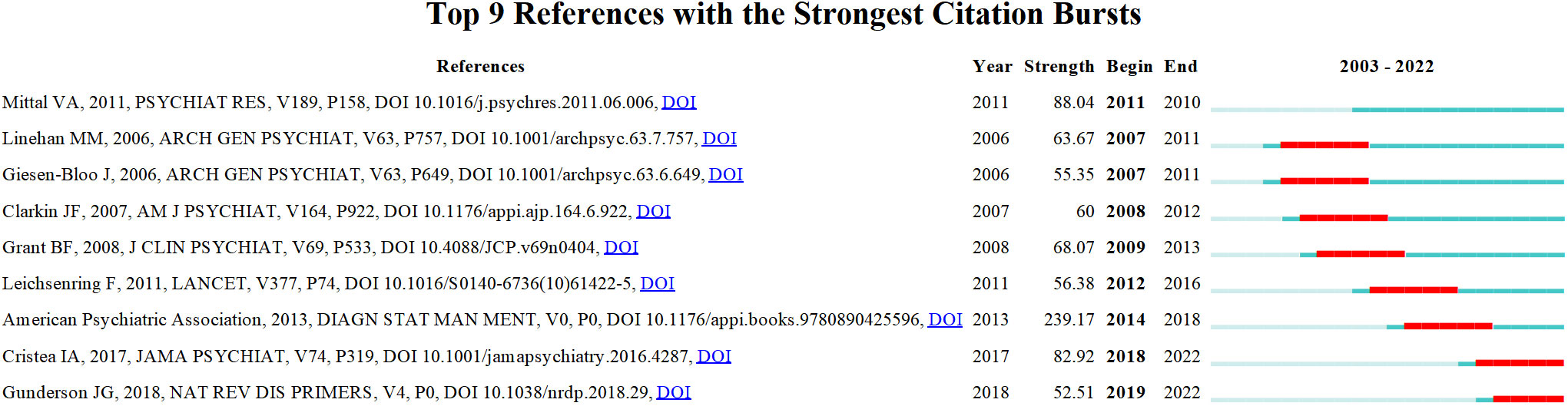
Figure 4 References with the strongest occurrence burst on BPD researches. Article titles correspond from top to bottom: Mittal VA et al. Diagnostic and Statistical Manuel of Mental Disorders; Linehan MM et al. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder; Giesen-Bloo J et al. Outpatient psychotherapy for borderline personality disorder: Randomized trial of schema-focused therapy vs transference-focused psychotherapy; Clarkin Jf et al. Evaluating three treatments for borderline personality disorder: A multiwave study; Grant BF et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: Results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions; Leichsenring F et al. Borderline personality disorder; American Psychiatric Association, DSM-5 Task Force. Diagnostic and statistical manual of mental disorders: DSM-5™ (5th ed.); Cristea IA et al. Efficacy of psychotherapies for borderline personality disorder: A systematic review and meta-analysis; Gunderson JG et al. Borderline personality disorder.
Structural variation analysis can be understood as a method of measuring and studying structural changes in the field, mainly reflecting the betweenness centrality and sigma of the references. The high centrality of the reference plays an important role in the connection between the preceding and following references and may help to identify critical points of transformation, or intellectual turning points. Sigma values, on the other hand, are used to measure the novelty of a study, combining a combination of citation burst and structural centrality ( 56 ). Table 2 listed the top 10 structural change references that can be considered as landmark studies connecting different clusters. The top three articles with high centrality are the studies conducted by Milton Z. Brown and his colleagues on the reasons for suicide attempts and non-suicidal self-injury in BPD women ( 57 ); the research by Nelson H. Donegan and his colleagues on the impact of amygdala on emotional dysregulation in BPD patients ( 59 ); and the fMRI study by Sabine C. Herpertz and her colleagues on abnormal amygdala function in BPD patients ( 61 ). In addition, publications with high sigma values are listed. They are Larry J. Siever and Kenneth L. Davis on psychobiological perspectives on personality disorders ( 58 ); Ludger Tebartz van Elst and his colleagues on abnormalities in frontolimbic brain functioning ( 60 ); and Marsha M. Linehan on therapeutic approaches in BPD research ( 62 ). These works are recognized as having transformative potential and may generate some new ideas.
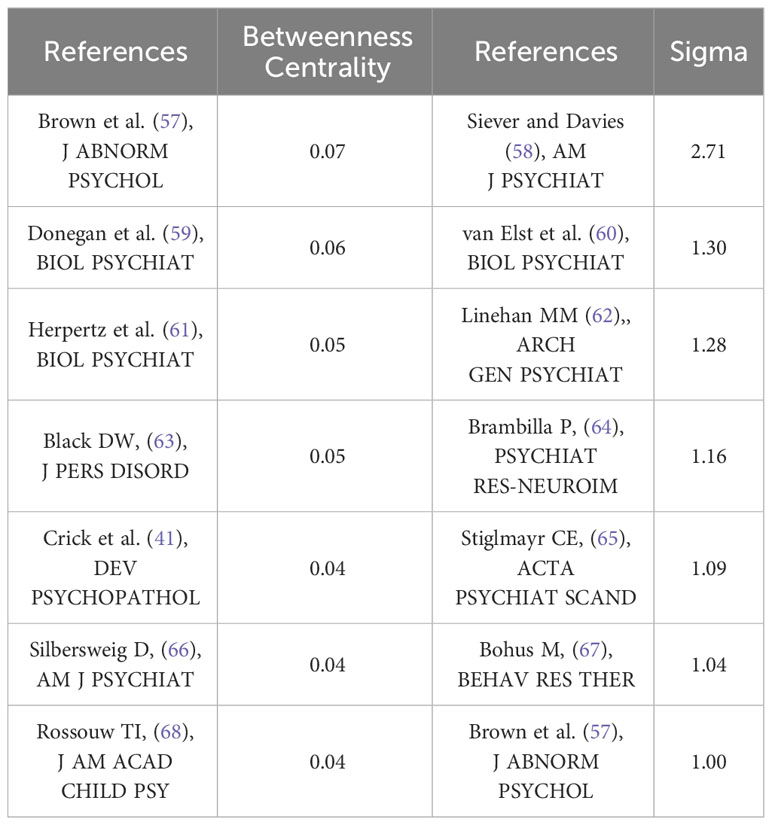
Table 2 Top 7 betweenness centrality and stigma references.
3.5 Analysis of authors and co-authors
Figure 5 showed a map of the co-authorship network over the last two decades. In total, 10 different clusters are shown, each of which gathers co-authors around the same research topic. For example, the main co-authors of cluster #0 “remission” are Christian Schmahl, Martin Bohus, Sabine C. Herpertz, Timothy J. Trull and Stefan Roepke. More recently, the three authors with the greatest bursts of research have been Mary C. Zanarini, Erik Simonsen, and Carla Sharp. As shown in Table 3 , the three most published authors are Martin Bohus (145 publications; 1.83%; H-index=61), Mary C. Zanarini (144 publications; 1.82%; H-index=80) and Christian Schmahl (142 publications; 1.79%; H-index=54).
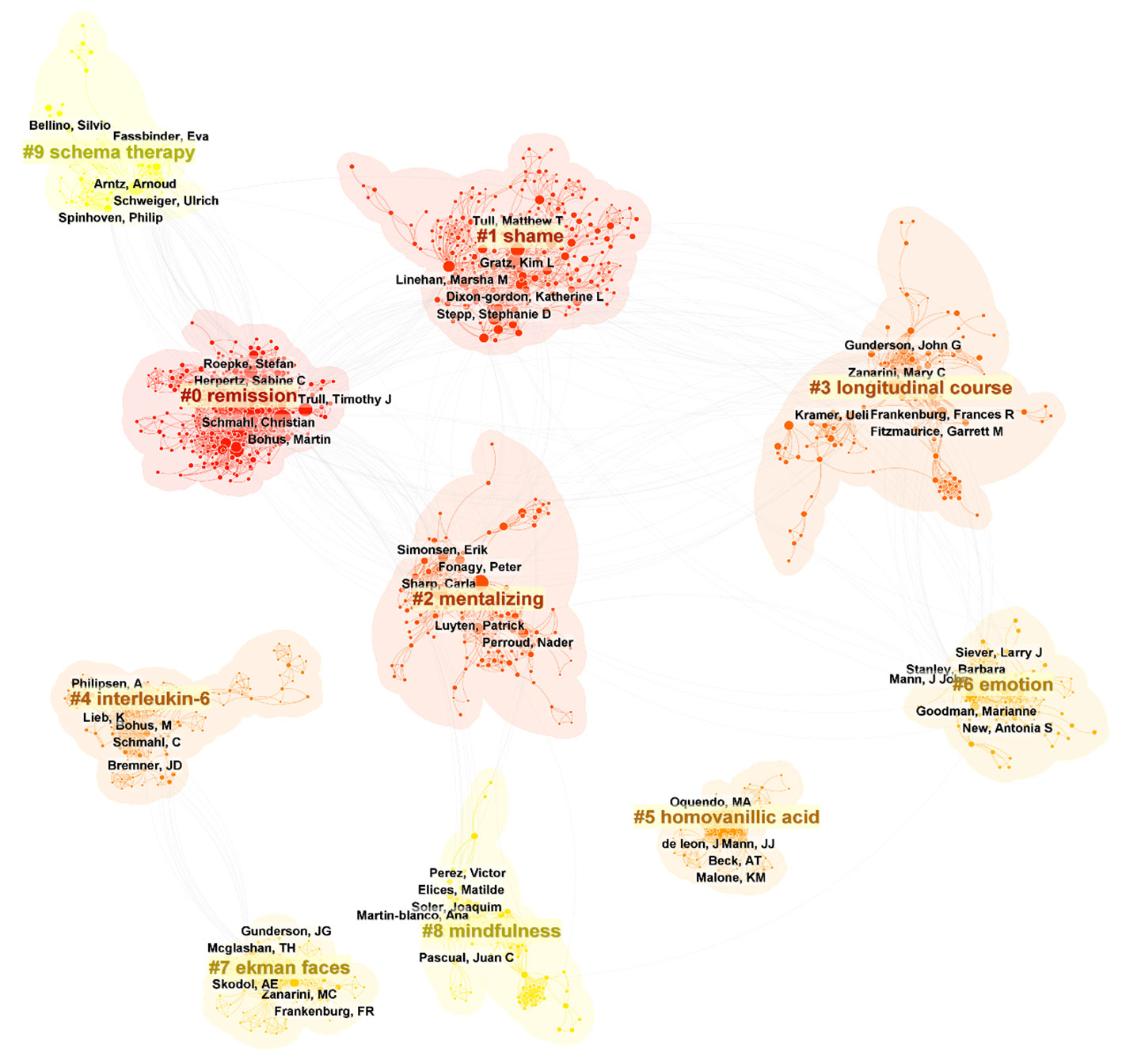
Figure 5 Top 10 clusters of coauthors in BPD (2003–2023). Selection Criteria: Top 10 per slice. Clusters labeled by keywords. The five authors with the highest number of publications in each cluster were labeled.
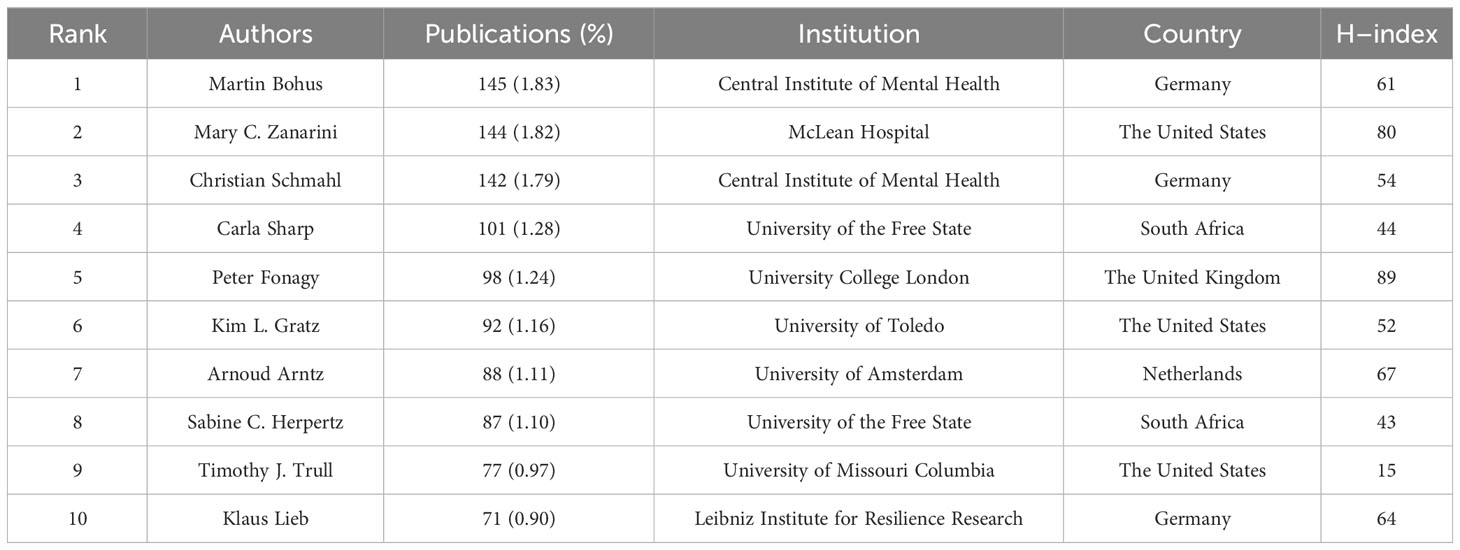
Table 3 Top 10 authors that published BPD researches.
3.6 Analysis of cooperation networks across countries
The top 10 countries in terms of number of publications in the BPD are added in Table 4 . With 3,440 published papers, or nearly 43% of all BPD research papers, the United States is the leading contributor to BPD research. This is followed by Germany (1196 publications; 15.10%) and the United Kingdom (1020 publications; 9.32%). Centrality refers to the degree of importance or centrality of a node in a network and is a measure of the importance of a node in a network ( 69 ). In Table 4 the United States is also has the highest centrality (0.43). Figure 6 shows the geographic collaboration network of countries in this field, with 83 countries contributing to BPD research, primarily from the United States and Europe.
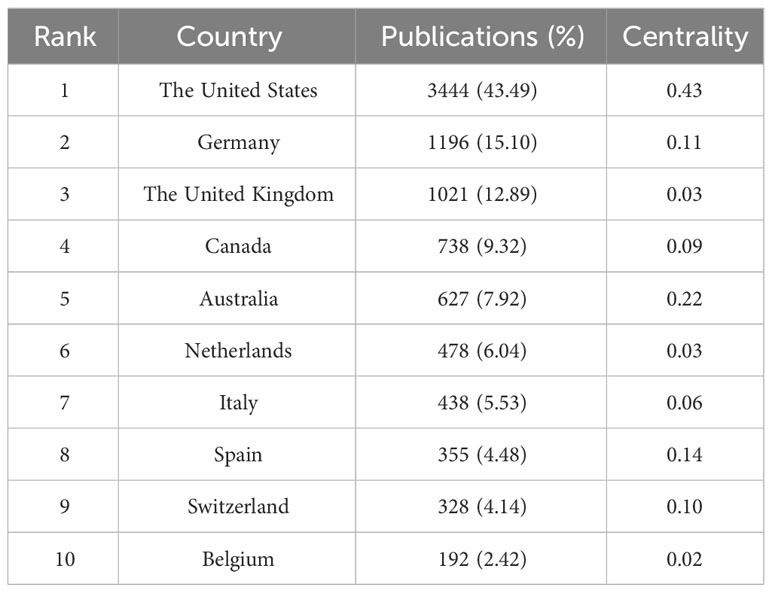
Table 4 Top 10 countries that published BPD researches.
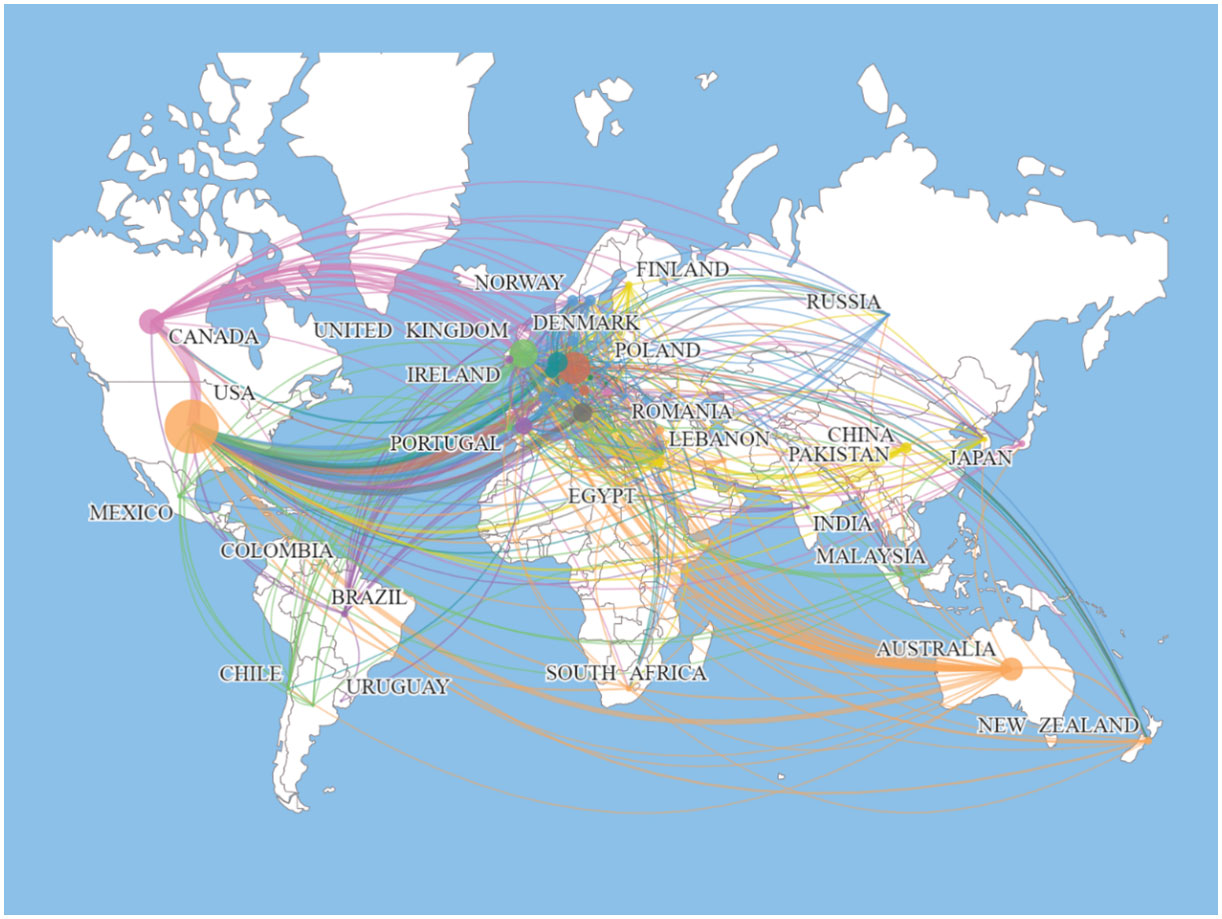
Figure 6 Map of the distribution of countries/regions engaged in BPD researches.
3.7 Analysis of the co-author’s institutions network
Table 5 listed the top 10 institutions ranked by the number of publications. The current study shows that Research Libraries Uk is the institution with the highest number of publications, with 766 publications (9.67%). The subsequent institutions are Harvard University and Ruprecht Karls University Heidelberg with 425 (5.37%) and 389 (4.91%) publications respectively. As can be seen from Table 4 , six of the top 10 institutions in terms of number of publications are from the United States. In part, this reflects the fact that the United States institutions are at the forefront of the BPD field and play a key role in it.
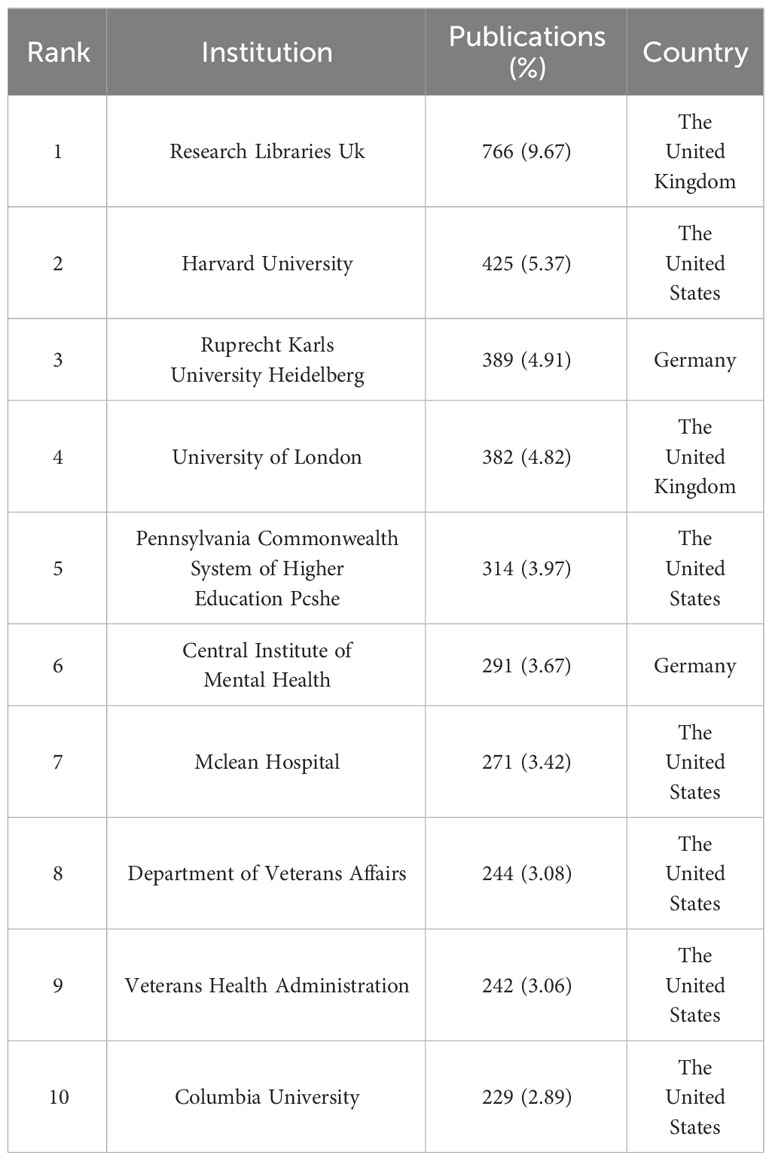
Table 5 Top 10 institutions that published BPD researches.
3.8 Analysis of journals and cited journals
If the more papers are published in a particular journal and at the same time it has a high number of citations, then it can be considered that the journal is influential ( 70 ). The top 10 journals in the field of BPD in terms of number of publications are listed in Table 6 . Journal of Personality Disorders from the Netherlands published the most literature on BPD with 438 (5.53%; IF=3.367) publications. This was followed by two journals from the United States: Psychiatry Research and Personality Disorders Theory Research and Treatment , with 269 (3.40%, IF=11.225) and 232 (2.93%; IF=4.627) publications, respectively. Among the top 10 journals in terms of number of publications published, Psychiatry Research has the highest impact factor.
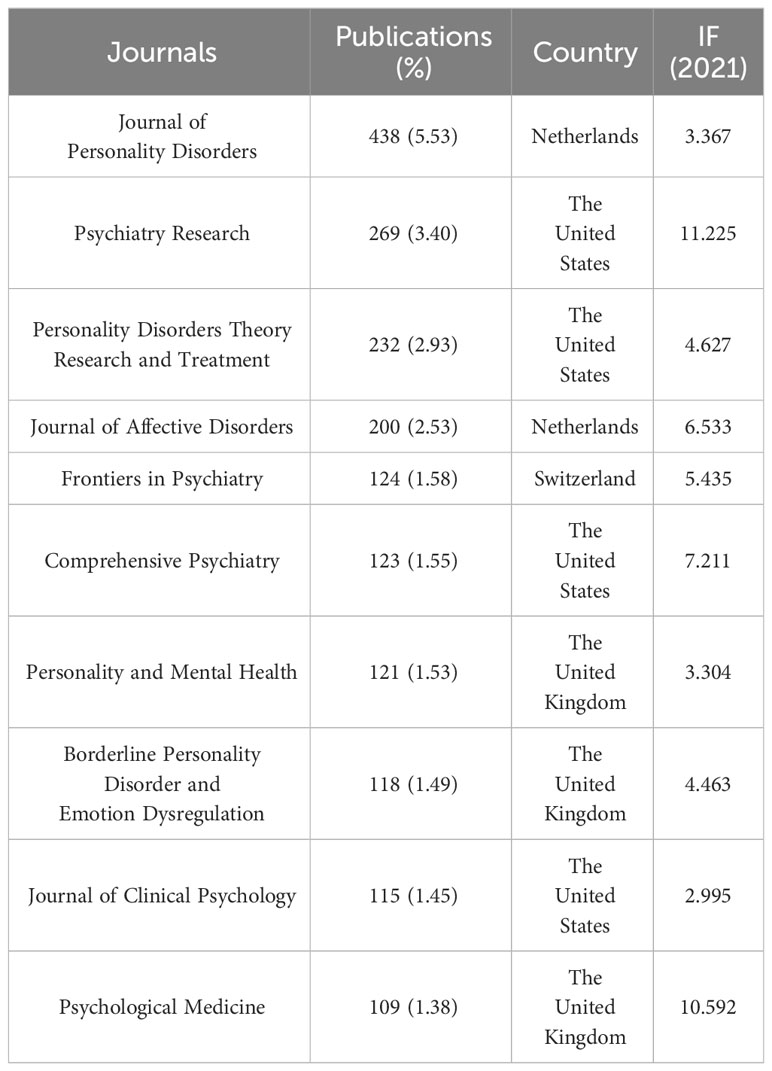
Table 6 Top 10 journals that published BPD researches.
3.9 Analysis of keywords and keywords co-occurrence
Keyword co-occurrence analysis can help researchers to understand the research hotspots in a certain field and the connection between different research topics. As shown in Figure 7 , all keywords can be categorized into 9 clusters: cluster #0 “diagnostic interview”, cluster #1 “diagnostic behavior therapy”, cluster #3 “social cognition”, cluster #4 “emotional regulation”, cluster #5 “substance use disorders “, cluster #6 “posttraumatic stress disorder”, cluster #7 “suicide” and cluster #8 “double blind”. These keywords have all been important themes in BPD research during the last 20 years.
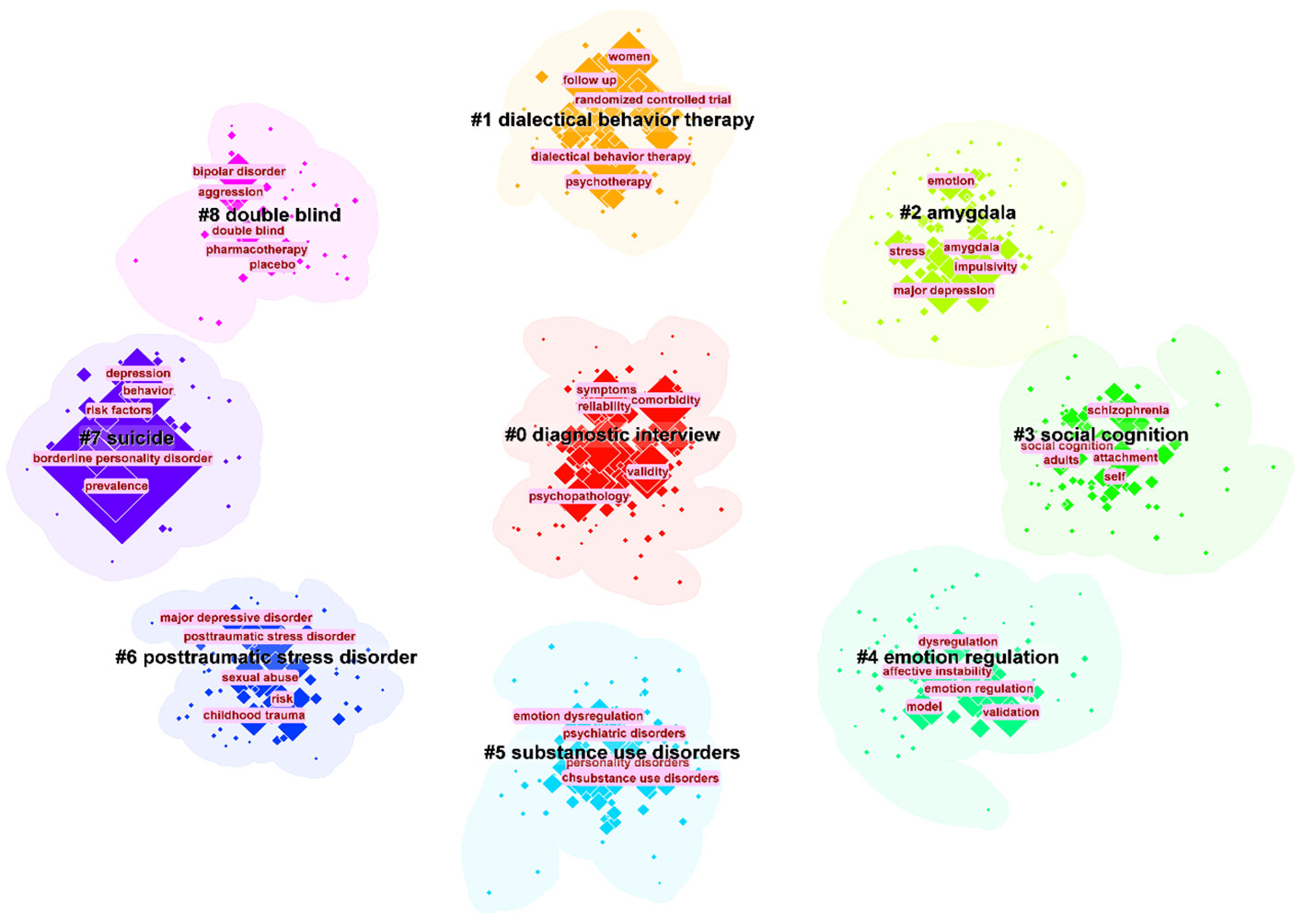
Figure 7 The largest 9 clusters of co-occurring keywords. The top 5 most frequent keywords in each cluster are highlighted.
Keyword burst is used to identify keywords with a significant increase in the frequency of occurrence in a topic or domain, helping to identify emerging concepts, research hotspots or keyword evolutions in a specific domain ( 71 ). Figure 8 presented the top 32 keywords with the strongest citation bursts in BPD from 2003−2023. Significantly, the keywords “positron emission tomography” (29.63), “major depression” (27.93), and “partial hospitalization” (27.1) had the highest intensity of outbreaks.
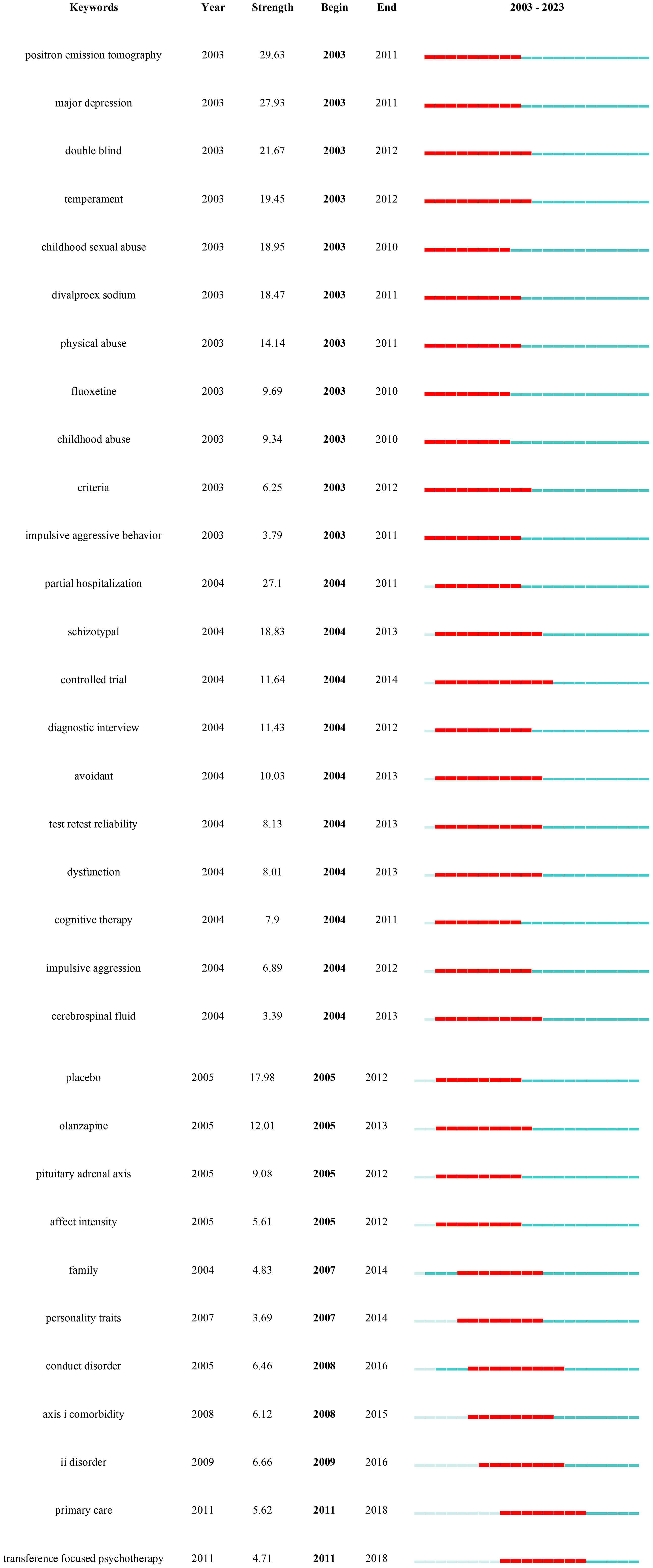
Figure 8 Keywords with the strongest occurrence burst on BPD researches.
4 Discussion
4.1 application of the “neuro-behavioral model” to bpd research.
In this study, we chose specific search terms, particularly “Neuro-behavioral Model”, to efficiently collect and analyze BPD research literature related to this emerging framework. This choice of keyword helped narrow the research scope and ensure its relevance to our objectives. However, it may have excluded some studies using different terminology, thus limiting comprehensiveness. In addition, the ‘Neuro-behavioral Model’, as an interdisciplinary field, encompasses a wide range of connotations and extensions, which also poses challenges to our research. This undoubtedly adds to the complexity of the study, yet it enhances our understanding of the field’s diversity.
4.2 Summary of the main findings
This current study utilized CiteSpace and Scimago Graphic software to conduct a comprehensive bibliometric analysis of the research literature on BPD. The study presented the current status of research, research hotspots, and research frontiers in BPD over the past 20 years (2003–2022) through knowledge mapping. The scientific predictions of future trends in BPD provided by this study can guide researchers interested in this field. This study also uses bibliometrics analysis method to show the knowledge structure and research results in the field of BPD, as well as the scientific prediction of the future trend of BPD research.

4.3 Identification of research hotspots
Previous studies have indicated an increasing trend in the number of papers focused on BPD, with the field gradually expanding into various areas. The first major research trend involves clinical studies on BPD. This includes focusing on emotional recognition difficulties in BPD patients, as well as studying features related to suicide attempts and non-suicidal self-injury. Clinical recognition and confirmation of BPD remains low, mainly related to the lack of clarity of its biological mechanisms ( 72 ). The nursing environment for BPD patients plays an important role in the development of the condition, which has become a focus of research. Researchers are also exploring the expansion of treatment options from conventional medication to non-pharmacological approaches, particularly cognitive-behavioral therapy. Another major research trend involves the associations and complications of BPD, including a greater focus on the adolescent population to reduce the occurrence of BPD starting from adolescence. Additionally, many researchers are interested in the comorbidity of BPD with various clinical mental disorders.
4.4 Potential trends of future research on BPD
Based on the results of the above studies and the results of the research trends in the table of details of the co-citation network clusters in 2022 ( Table 7 ), several predictions are made for the future trends in the field of BPD. In Table 7 , there were some trends related to previous studies, including #1”dialectical behavior therapy”, #7 “dialectical behavior therapy” ( 73 ), #5 “mentalization” ( 74 ), and #9 “non-suicidal self-injury” ( 75 ). The persistence of these research trends is evidence that they have been a complex issue in this field and a focus of researchers. The recently emerged turning point paper provides a comprehensive assessment about BPD, offering practical information and treatment recommendations ( 76 ). New research is needed to improve standards and suggest more targeted and cost-effective treatments.
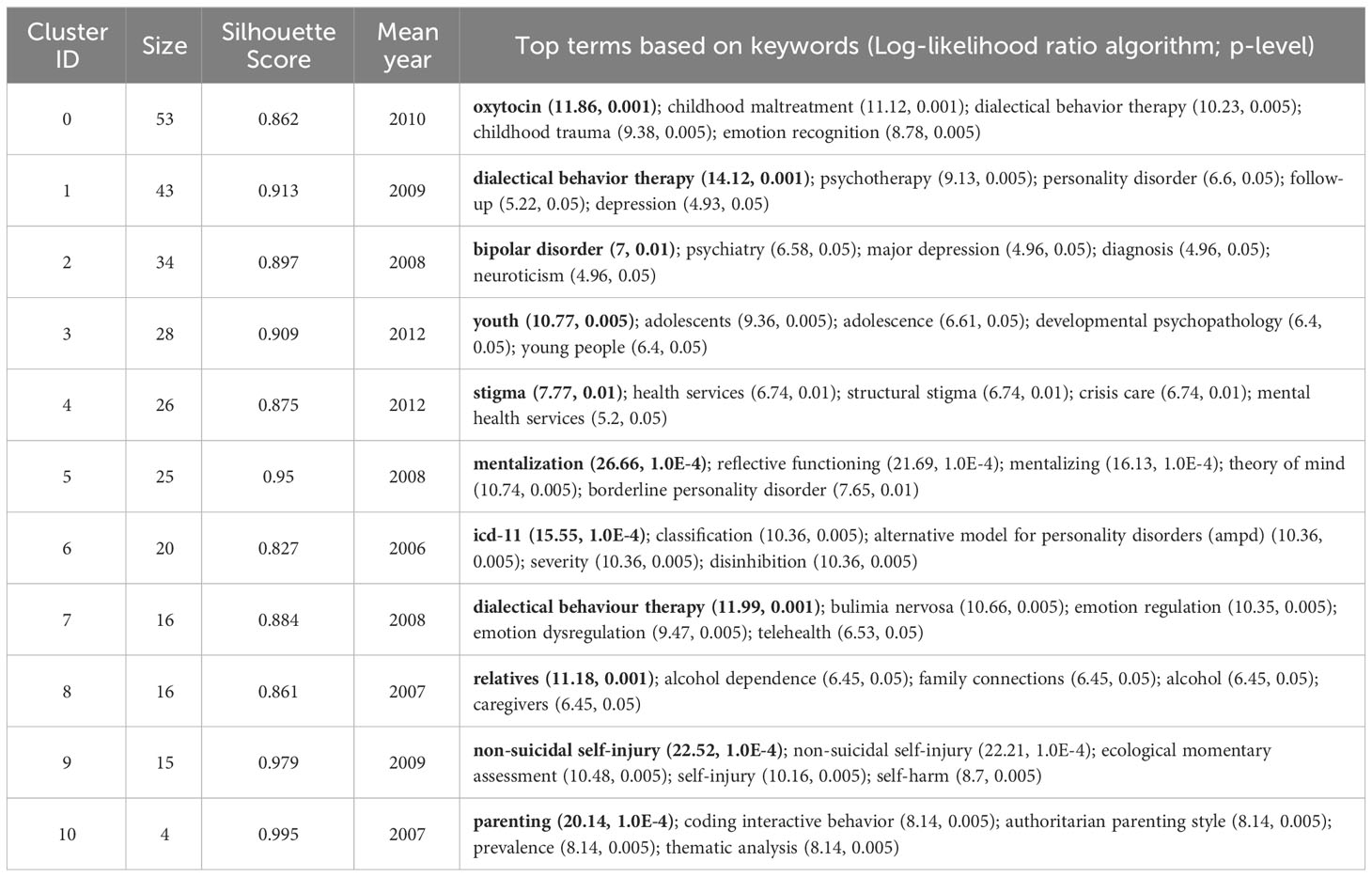
Table 7 The references co-citation network cluster detail (2022).
BPD symptoms in adolescents have been shown to respond to interventions with good results, so prevention and intervention for BPD is warranted ( 77 ). This trend can be observed in #3 “youth” ( 78 ). Mark F. Lenzenweger and Dante Cicchetti summarized the developmental psychopathology approach to BPD, one of the aims of which is to provide information for the prevention of BPD ( 79 ). Prevention and early intervention of BPD has been shown to provide many benefits, including reduced occurrence of secondary disorders, improved psychosocial functioning, and reduced risk of interpersonal conflict ( 80 ). However, there are differences between individuals, and different prevention goals are recommended for adolescents at risk for BPD. Therefore, prevention and early intervention for BPD has good prospects for the future.
The etiology of BPD is closely related to many factors, and its pathogenesis is often ignored by clinicians. The exploration of risk factors has been an important research direction in the study. Some studies have found that BPD is largely the product of traumatic childhood experiences, which may lead to negative psychological effects on children growing up ( 81 ). It has also been found that the severity of borderline symptoms in parents is positively associated with poor parenting practices ( 82 ). Future researches need to know more about the biological-behavioral processes of parents in order to provide targeted parenting support and create a good childhood environment.
Because pharmacotherapy is only indicated for comorbid conditions that require medication, psychotherapy has become one of the main approaches to treating BPD. The increasingly advanced performance and availability of contemporary mobile devices can help to take advantage of them more effectively in the context of optimizing the treatment of psychiatric disorders. The explosion of COVID-19 is forcing people to adapt to online rather than face-to-face offline treatment ( 83 ). The development of this new technology will effectively advance the treatment of patients with BPD. Although telemedicine has gained some level of acceptance by the general public, there are some challenges that have been reported, so further research on the broader utility of telemedicine is needed in the future.
4.5 The current study compares with a previous bibliometric review of BPD
As mentioned earlier, there have been previous bibliometric studies conducted by scholars in the field of BPD. This paper focuses more on BPD in personality disorders than the extensive study of personality disorders as a category by Taylor Reis et al. ( 15 ). The results of both studies show an increasing trend in the number of publications in the field of BPD, suggesting positive developments in the field. Taylor Reis et al. focused primarily on quantifying publications on personality disorders and did not delve into other specific aspects of BPD. Ilaria M.A. Benzi et al. focused on a bibliometric analysis of the pathology of BPD ( 14 ). They give three trends for the future development of BPD pathology: first, the growing importance of self-injurious behavior research; second, the association of attention deficit hyperactivity disorder with BPD and the influence of genetics and heritability on BPD; and third, the new focus on the overlap between fragile narcissism and BPD. The study in this paper also concludes that there are three future development directions for BPD: first, the prevention and early intervention of BPD; second, the non-pharmacological treatment of BPD; and third, research into the pathogenesis of BPD. Owing to variations in research backgrounds and data sources, the outcomes presented in the two studies diverge significantly. Nevertheless, both contributions hold merit in advancing the understanding of BPD. In addition to this, this paper also identifies trends in BPD over the past 20 years: the first trend is the clinical research of BPD, which is specifically subdivided into three sub-trends; the second trend is association and comorbidity. The identification of these trends is important for understanding the disorder, improving diagnosis and treatment, etc. Structural variant analysis also features prominently in the study. The impact of literature in terms of innovativeness is detected through in-depth mining and analysis of large amounts of literature data. This analysis is based on research in the area of scientific creativity, especially the role and impact of novel reorganizations in creative thinking. Structural variation analysis is precisely designed to find and reveal embodiments of such innovative thinking in scientific literature, enabling researchers to more intuitively grasp the dynamics and cutting-edge advances in the field of science.
5 Limitations
However, it must be admitted that our study has some limitations. The first is the limited nature of data resources. The data source for our study came from only one database, WOS. Second, the limitation of article type. Search criteria are limited to papers and reviews in SCI and SSCI databases. Third, the effect of language type. In the current study, only English-language literature could be included in the analysis, which may lead us to miss some important studies published in other languages. Fourth, limitations of research software. Although this study used well-established and specialized software, the results obtained by choosing different calculation methods may vary. Finally, the diversity of results interpretation. The results analyzed by the software are objective, but there is also some subjectivity in the interpretation and analysis of the research results. While we endeavor to be comprehensive and accurate in our research, the choice of search terms inevitably introduces certain limitations. Using “Neuro-behavioral Model” as the search term enhances the study’s relevance, but it may also cause us to miss significant studies in related areas. This limits the generalizability and replicability of our results. Furthermore, the inherent complexity and diversity of neurobehavioral models might introduce subjectivity and bias in our interpretation and application of the literature. Although we endeavored to reduce bias via multi-channel validation and cross-referencing, we cannot entirely eliminate its potential impact on our findings.
6 Conclusion
Overall, a comprehensive scientometrics analysis of BPD provides a comprehensive picture of the development of this field over the past 20 years. This in-depth examination not only reveals research trends, but also allows us to understand which areas are currently hot and points the way for future research efforts. In addition, this method provides us with a framework to evaluate the value of our own research results, which helps us to more precisely adjust the direction and strategy of research. More importantly, this in-depth analysis reveals the depth and breadth of BPD research, which undoubtedly provides valuable references for researchers to have a deeper understanding of BPD, and also provides a reference for us to set future research goals. In short, this scientometrics approach gives us a window into the full scope of BPD research and provides valuable guidance for future research.
Author contributions
YL: Data curation, Formal analysis, Investigation, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing. CC: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. YZ: Validation, Visualization, Writing – review & editing. NZ: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. SL: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. SL is supported by the Outstanding Youth Program of Philosophy and Social Sciences in Anhui Province (2022AH030089) and the Starting Fund for Scientific Research of High-Level Talents at Anhui Agricultural University (rc432206).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Lieb K, Zanarini MC, Schmahl C, Linehan MM, Bohus M. Borderline personality disorder. Lancet (2004) 364:453–61. doi: 10.1016/S0140-6736(04)16770-6
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Chugani CD, Byrd AL, Pedersen SL, Chung T, Hipwell AE, Stepp SD. Affective and sensation-seeking pathways linking borderline personality disorder symptoms and alcohol-related problems in young women. J Pers Disord . (2020) 34:420–31. doi: 10.1521/pedi_2018_32_389
3. Bagge CL, Stepp SD, Trull TJ. Borderline personality disorder features and utilization of treatment over two years. J Pers Disord . (2005) 19:420–39. doi: 10.1521/pedi.2005.19.4.420
4. Paris J. Suicidality in borderline personality disorder. Medicina . (2019) 55:223. doi: 10.3390/medicina55060223
5. Lenzenweger MF, Lane MC, Loranger AW, Kessler RC. DSM-IV personality disorders in the National Comorbidity Survey Replication. Biol Psychiatry . (2007) 62:553–64. doi: 10.1016/j.biopsych.2006.09.019
6. Skodol AE, Gunderson JG, Pfohl B, Widiger TA, Livesley WJ, Siever LJ. The borderline diagnosis I: Psychopathology, comorbidity, and personality structure. Biol Psychiatry . (2002) 51:936–50. doi: 10.1016/s0006-3223(02)01324-0
7. Bailey RC, Grenyer BF. Burden and support needs of carers of persons with borderline personality disorder: A systematic review. Harvard Rev Psychiatry . (2013) 21:248–58. doi: 10.1097/HRP.0b013e3182a75c2c
CrossRef Full Text | Google Scholar
8. Weimand BM, Hedelin B, Sällström C, Hall-Lord M-L. Burden and health in relatives of persons with severe mental illness: A Norwegian cross-sectional study. Issues Ment Health Nursing . (2010) 31:804–15. doi: 10.3109/01612840.2010.520819
9. Saccaro LF, Schilliger Z, Dayer A, Perroud N, Piguet C. Inflammation, anxiety, and stress in bipolar disorder and borderline personality disorder: A narrative review. Neurosci Biobehav Rev . (2021) 127:184−192. doi: 10.1016/j.neubiorev.2021.04.017
10. Dixon-Gordon KL, Laws H. Emotional variability and inertia in daily life: Links to borderline personality and depressive symptoms. J Pers Disord . (2021) 35:162−171. doi: 10.1521/pedi_2021_35_504
11. Torgersen S. Genetics of patients with borderline personality disorder. Psychiatr Clinics North A . (2000) 23:1–9. doi: 10.1016/S0193-953X(05)70139-8
12. Quenneville AF, Kalogeropoulou E, Küng AL, Hasler R, Nicastro R, Prada P, et al. Childhood maltreatment, anxiety disorders and outcome in borderline personality disorder. Psychiatry Res . (2020) 284:112688. doi: 10.1016/j.psychres.2019.112688
13. Antoine SM, Fredborg BK, Streiner D, Guimond T, Dixon-Gordon KL, Chapman AL, et al. Subgroups of borderline personality disorder: A latent class analysis. Psychiatry Res . (2023) 323:115131. doi: 10.1016/j.psychres.2023.115131
14. Benzi IMA, Di Pierro R, De Carli P, Cristea IA, Cipresso P. All the faces of research on borderline personality pathology: Drawing future trajectories through a network and cluster analysis of the literature. J Evidence-Based Psychotherapies . (2020) 20:3–30. doi: 10.24193/jebp.2020.2.9
15. Reis T, Gekker M, Land MGP, Mendlowicz MV, Berger W, Luz MP, et al. The growth and development of research on personality disorders: A bibliometric study. Pers Ment Health . (2022) 16:290–9. doi: 10.1002/pmh.1540
16. Singh VK, Singh P, Karmakar M, Leta J, Mayr P. The journal coverage of Web of Science, Scopus and Dimensions: A comparative analysis. Scientometrics . (2021) 126:5113–42. doi: 10.1007/s11192-021-03948-5
17. Pritchard A. Statistical bibliography or bibliometrics. J Documentation . (1969) 25:348.
Google Scholar
18. Price DJ. Networks of scientific papers. Science . (1965) 149:510–5. doi: 10.1126/science.149.3683.510
19. Sabe M, Chen C, Perez N, Solmi M, Mucci A, Galderisi S, et al. Thirty years of research on negative symptoms of schizophrenia: A scientometric analysis of hotspots, bursts, and research trends. Neurosci Biobehav Rev . (2023) 144:104979. doi: 10.1016/j.neubiorev.2022.104979
20. Shen Z, Ji W, Yu S, Cheng G, Yuan Q, Han Z, et al. Mapping the knowledge of traffic collision reconstruction: A scientometric analysis in CiteSpace, VOSviewer, and SciMAT. Sci Justice . (2023) 63:19–37. doi: 10.1016/j.scijus.2022.10.005
21. Wu H, Wang Y, Tong L, Yan H, Sun Z. Global research trends of ferroptosis: A rapidly evolving field with enormous potential. Front Cell Dev Biol . (2021) 9:646311. doi: 10.3389/fcell.2021.646311
22. Brody S. Impact factor: Imperfect but not yet replaceable. Scientometrics . (2013) 96:255–7. doi: 10.1007/s11192-012-0863-x
23. Kaldas M, Michael S, Hanna J, Yousef GM. Journal impact factor: A bumpy ride in an open space. J Invest Med . (2020) 68:83–7. doi: 10.1136/jim-2019-001009
24. Schubert A, Glänzel W. A systematic analysis of Hirsch-type indices for journals. J Informetrics . (2007) 1:179–84. doi: 10.1016/j.joi.2006.12.002
25. Chen C. CiteSpace II: Detecting and visualizing emerging trends and transient patterns in scientific literature. J Am Soc Inf Sci Technol . (2006) 57:359–77. doi: 10.1002/asi.20317
26. Cheng K, Guo Q, Shen Z. Bibliometric analysis of global research on cancer photodynamic therapy: Focus on nano-related research. Front Pharmacol . (2022) 13:927219. doi: 10.3389/fphar.2022.927219
27. Hassan-Montero Y, De-Moya-Anegón F, Guerrero-Bote VP. SCImago Graphica: A new tool for exploring and visually communicating data. Profesional la Información . (2022) 31:e310502. doi: 10.3145/EPI
28. Wang Y, Li D, Jia Z, Hui J, Xin Q, Zhou Q, et al. A bibliometric analysis of research on the links between gut microbiota and atherosclerosis. Front Cardiovasc Med . (2022) 9:941607. doi: 10.3389/fcvm.2022.941607
29. Soloff PH, Lynch KG, Kelly TM, Malone KM, Mann JJ. Characteristics of suicide attempts of patients with major depressive episode and borderline personality disorder: a comparative study. Am J Psychiatry . (2000) 157:601–8. doi: 10.1176/appi.ajp.157.4.601
30. Widiger TA, Trull TJ. Plate tectonics in the classification of personality disorder: shifting to a dimensional model. Am Psychol . (2007) 62:71–83. doi: 10.1037/0003-066X.62.2.71
31. Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol . (1995) 51:768–74. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1
32. Bartow S, Stopsack M, Grabe HJ, Meinke C, Spitzer C, Kronmüller K, et al. Interpersonal evaluation bias in borderline personality disorder. Behav Res Ther . (20092009) 47:359–65. doi: 10.1016/j.brat.2009.02.003
33. Cheavens JS, Rosenthal MZ, Daughters SB, Nowak J, Kosson D, Lynch TR, et al. An analogue investigation of the relationships among perceived parental criticism, negative affect, and borderline personality disorder features: The role of thought suppression. Behav Res Ther . (2005) 43:257–68. doi: 10.1016/j.brat.2004.01.006
34. Bradley R, Westen D. The psychodynamics of borderline personality disorder: a view from developmental psychopathology. Dev Psychopathol . (2005) 17:927–57. doi: 10.1017/s0954579405050443
35. Tzourio-Mazoyer N, Landeau B, Papathanassiou D, Crivello F, Etard O, Delcroix N, et al. Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. NeuroImage . (2002) 15:273–89. doi: 10.1006/nimg.2001.0978
36. Bellino S, Rinaldi C, Bozzatello P, Bogetto F. Pharmacotherapy of borderline personality disorder: a systematic review for publication purpose. Curr Medicinal Chem . (2011) 18:3322–9. doi: 10.2174/092986711796504682
37. Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A. Axis I comorbidity of borderline personality disorder. Am J Psychiatry . (1998) 155:1733–9. doi: 10.1176/ajp.155.12.1733
38. Yee L, Korner AJ, McSwiggan S, Meares RA, Stevenson J. Persistent hallucinosis in borderline personality disorder. Compr Psychiatry . (2005) 46:147–54. doi: 10.1016/j.comppsych.2004.07.032
39. Mittal VA, Walker EF. Diagnostic and statistical manual of mental disorders. Psychiatry Res . (2011) 189:158–9. doi: 10.1016/j.psychres.2011.06.006
40. Torgersen S, Kringlen E, Cramer V. The prevalence of personality disorders in a community sample. Arch Gen Psychiatry . (2001) 58:590–6. doi: 10.1001/archpsyc.58.6.590
41. Crick NR, Murray-Close D, Woods K. Borderline personality features in childhood: A short-term longitudinal study. Dev Psychopathol . (2005) 17:1051–70. doi: 10.1017/S0954579405050492
42. Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, et al. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Arch Gen Psychiatry . (2006) 63:757–66. doi: 10.1001/archpsyc.63.7.757
43. Giesen-Bloo J, van Dyck R, Spinhoven P, van Tilburg W, Dirksen C, van Asselt T, et al. Outpatient psychotherapy for borderline personality disorder: Randomized trial of schema-focused therapy vs transference-focused psychotherapy. Arch Gen Psychiatry . (2006) 63:649–58. doi: 10.1001/archpsyc.63.6.649
44. Crowell SE, Beauchaine TP, Linehan MM. A biosocial developmental model of borderline personality: Elaborating and extending Linehan's theory. psychol Bulletin . (2009) 135:495–510. doi: 10.1037/a0015616
45. Leichsenring F, Leibing E, Kruse J, New AS, Leweke F. Borderline personality disorder. Lancet (2011) 377(9759):74–84. doi: 10.1016/S0140-6736(10)61422-5
46. Whiteside SP, Lynam DR, Miller JD, Reynolds SK. Validation of the UPPS impulsive behaviour scale: A four-factor model of impulsivity. Eur J Pers (2005) 19(7):559–74. doi: 10.1002/per.556
47. Clarkin JF, Levy KN, Lenzenweger MF, Kernberg OF. Evaluating three treatments for borderline personality disorder: A multiwave study. Am J Psychiatry (2007) 164(6):922–8. doi: 10.1176/ajp.2007.164.6.922
48. Bateman A, Fonagy P. Randomized controlled trial of outpatient mentalization-based treatment versus structured clinical management for borderline personality disorder. Am J Psychiatry (2009) 166(12):1355–64. doi: 10.1176/appi.ajp.2009.09040539
49. Fonagy P, Luyten P. A developmental, mentalization-based approach to the understanding and treatment of borderline personality disorder. Dev Psychopathol (2009) 21(4):1355–81. doi: 10.1017/S0954579409990198
50. Levy KN, Meehan KB, Kelly KM, Reynoso JS, Weber M, Clarkin JF, et al. Change in attachment patterns and reflective function in a randomized control trial of transference-focused psychotherapy for borderline personality disorder. J Consulting Clin Psychol (2006) 74(6):1027–40. doi: 10.1037/0022-006X.74.6.1027
51. Carr DS, Francis A. Childhood familial environment, maltreatment and borderline personality disorder symptoms in a non-clinical sample: A cognitive behavioural perspective. Clin Psychol (2009) 13(1):28–37. doi: 10.1080/13284200802680476
52. Selby EA, Kranzler A, Fehling KB, Panza E. Nonsuicidal self-injury disorder: The path to diagnostic validity and final obstacles. Clin Psychol Review . (2015) 38:79–91. doi: 10.1016/j.cpr.2015.03.003
53. Skoglund C, Tiger A, Rück C, Petrovic P, Asherson P, Hellner C, et al. Familial risk and heritability of diagnosed borderline personality disorder: A register study of the Swedish population. Mol Psychiatry . (2021) 26:999–1008. doi: 10.1038/s41380-019-0442-0
54. American Psychiatric Association, DSM-5 Task Force. Diagnostic and statistical manual of mental disorders: DSM-5™ . 5th ed. Washington: American Psychiatric Publishing, Inc., (2013). doi: 10.1176/appi.books.9780890425596
55. Cristea IA, Gentili C, Cotet CD, Palomba D, Barbui C, Cuijpers P. Efficacy of psychotherapies for borderline personality disorder: A systematic review and meta-analysis. JAMA Psychiatry . (2017) 74:319–28. doi: 10.1001/jamapsychiatry.2016.4287
56. Chen C. Predictive effects of structural variation on citation counts. J Am Soc Inf Sci Technol . (2012) 63:431–49. doi: 10.1002/asi.21694
57. Brown MZ, Comtois KA, Linehan MM. Reasons for suicide attempts and non-suicidal self-injury in women with borderline personality disorder. J Abnormal Psychol . (2002) 111:198–202. doi: 10.1037//0021-843x.111.1.198
58. Siever LJ, Davis KL. A psychobiological perspective on the personality disorders. Am J Psychiatry . (1991) 148:1647–58. doi: 10.1176/ajp.148.12.1647
59. Donegan NH, Sanislow CA, Blumberg HP. Amygdala hyperreactivity in borderline personality disorder: Implications for emotional dysregulation. Biol Psychiatry . (2003) 54:1284–93. doi: 10.1016/S0006-3223(03)00636-X
60. Tebartz van Elst L, Hesslinger B, Thiel T, Geiger E, Haegele K, Lemieux L, et al. Frontolimbic brain abnormalities in patients with borderline personality disorder: A volumetric magnetic resonance imaging study. Biol Psychiatry . (2003) 54:163–71. doi: 10.1016/s0006-3223(02)01743-2
61. Herpertz SC, Dietrich TM, Wenning B, Krings T, Erberich SG, Willmes K, et al. Evidence of abnormal amygdala functioning in borderline personality disorder: A functional MRI study. Biol Psychiatry . (2001) 50:292–8. doi: 10.1016/S0006-3223(01)01075-7
62. Linehan MM. Cognitive-behavioral treatment of borderline personality disorder . New York: Guilford Press (1993).
63. Black DW, Blum N, Pfohl B, Hale N. Suicidal behavior in borderline personality disorder: Prevalence, risk factors, prediction, and prevention. J Pers Disord (2004) 18(3):226–39. doi: 10.1521/pedi.18.3.226.35445
64. Brambilla P, Soloff PH, Sala M, Nicoletti MA, Keshavan MS, Soares JC. Anatomical MRI study of borderline personality disorder patients. Psychiatry Res (2004) 131(2):125–33. doi: 10.1016/j.pscychresns.2004.04.003
65. Stiglmayr CE, Grathwol T, Linehan MM, Ihorst G, Fahrenberg J, Bohus M. Aversive tension in patients with borderline personality disorder: A computer-based controlled field study. Acta Psychiatrica Scandinavica (2005) 111(5):372–9. doi: 10.1111/j.1600-0447.2004.00466.x
66. Silbersweig D, Clarkin JF, Goldstein M, Kernberg OF, Tuescher O, Levy KN, et al. Failure of frontolimbic inhibitory function in the context of negative emotion in borderline personality disorder. Am J Psychiatry (2007) 164(12):18321841. doi: 10.1176/appi.ajp.2007.06010126
67. Bohus M, Haaf B, Stiglmayr C, Pohl U, Böhme R, Linehan M. Evaluation of inpatient dialectical-behavioral therapy for borderline personality disorder–a prospective study. Behav Res Ther (2000) 38(9):875887. doi: 10.1016/s0005-7967(99)00103-5
68. Rossouw TI, Fonagy P. Mentalization-based treatment for self-harm in adolescents: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry (2012) 51(12):13041313. doi: 10.1016/j.jaac.2012.09.018
69. Zhang S, Wang S, Liu R. A bibliometric analysis of research trends of artificial intelligence in the treatment of autistic spectrum disorders. Front Psychiatry . (2022) 13:967074. doi: 10.3389/fpsyt.2022.967074
70. Dzikowski P. A bibliometric analysis of born global firms. J Business Res . (2018) 85:281–94. doi: 10.1016/j.jbusres.2017.12.054
71. Chen C, Ibekwe-SanJuan F, Hou J. The structure and dynamics of cocitation clusters: A multiple-perspective cocitation analysis. J Am Soc Inf Sci Technol . (2010) 61:1386–409. doi: 10.1002/asi.21309
72. Gunderson JG, Herpertz SC, Skodol AE, Torgersen S, Zanarini MC. Borderline personality disorder. Nat Rev Dis Primers . (2018) 4:18029. doi: 10.1038/nrdp.2018.29
73. Tan MYL, McConnell B, Barlas J. Application of Dialectical Behaviour Therapy in treating common psychiatric disorders: Study protocol for a scoping review. BMJ Open . (2002) 12:e058565. doi: 10.1136/bmjopen–2021–058565
74. Quevedo Y, Booij L, Herrera L, Hernández C, Jiménez JP. Potential epigenetic mechanisms in psychotherapy: A pilot study on DNA methylation and mentalization change in borderline personality disorder. Front Hum Neurosci . (2022) 16:955005. doi: 10.3389/fnhum.2022.955005
75. Uhlmann C, Tschöke S, Steinert T, Schmid P. Can you see and hear how bad I feel right now? Self–injury and suicidal communication in borderline personality disorder-A secondary analysis. Psychiatrische Praxis . (2022) 49:329–33. doi: 10.1055/a–1820–0438
76. Bohus M, Stoffers-Winterling J, Sharp C, Krause-Utz A, Schmahl C, Lieb K. Borderline personality disorder. Lancet (2022) 398:1528–40. doi: 10.1016/S0140–6736(21)00476–1
77. Schuppert HM, Giesen-Bloo J, van Gemert TG, Wiersema HM, Minderaa RB, Emmelkamp PMG, et al. Effectiveness of an emotion regulation group training for adolescents—A randomized controlled pilot study. Clin Psychol Psychother . (2009) 16:467–78. doi: 10.1002/cpp.637
78. American Psychiatric Association. Diagnostic and statistical manual of mental disorders, text revision . 4th ed. Washington: American Psychiatric Association (2000).
79. Lenzenweger MF, Cicchetti D. Toward a developmental psychopathology approach to borderline personality disorder. Dev Psychopathol . (2005) 17:893–8. doi: 10.1017/S095457940505042X
80. Chanen AM, Jovev M, McCutcheon LK, Jackson HJ, McGorry PD. Borderline personality disorder in young people and the prospects for prevention and early intervention. Curr Psychiatry Rev . (2008) 4:48–57. doi: 10.2174/157340008783743820
81. Pohl S, Steuwe C, Mainz V, Driessen M, Beblo T. Borderline personality disorder and childhood trauma: Exploring the buffering role of self-compassion and self-esteem. J Clin Psychol . (2021) 77:837–45. doi: 10.1002/jclp.23070
82. Bartsch DR, Roberts R, Proeve M. Relationships between parental borderline symptom severity, empathy, parenting styles and child psychopathology. Clin Psychol . (2022) 26:211–21. doi: 10.1080/13284207.2022.2031947
83. Lakeman R, Hurley J, Campbell K, Hererra C, Leggett A, Tranter R, et al. High fidelity dialectical behaviour therapy online: Learning from experienced practitioners. Int J Ment Health Nursing . (20222022) 31:1405–16. doi: 10.1111/inm.13039
Keywords: neuro-behavioral model, borderline personality disorder, BPD, bibliometric, Scimago Graphica
Citation: Liu Y, Chen C, Zhou Y, Zhang N and Liu S (2024) Twenty years of research on borderline personality disorder: a scientometric analysis of hotspots, bursts, and research trends. Front. Psychiatry 15:1361535. doi: 10.3389/fpsyt.2024.1361535
Received: 12 January 2024; Accepted: 19 February 2024; Published: 01 March 2024.
Reviewed by:
Copyright © 2024 Liu, Chen, Zhou, Zhang and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shen Liu, [email protected] ; Chaomei Chen, [email protected] ; Na Zhang, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Borderline Personality Disorder: A Clinical Guide
- ROBERT STERN , M.D., Ph.D. ,
Search for more papers by this author
If this book were a new opera composed by John Gunderson and conducted by him at a worldwide premiere performance at one of the famed houses in Milan, Paris, London, or New York, everyone in the audience, including this critic, would stand up impulsively and cheer. Indeed, stand up and cheer we must.
John Gunderson became interested in borderline patients during his psychiatric residency at the Massachusetts Mental Health Center in Boston. In 1971 he went to the National Institute of Mental Health and, together with William Carpenter and John Strauss within the framework of the International Pilot Study of Schizophrenia, compared a sample of 29 patients with schizophrenia and a group of 24 borderline patients who had all recently been admitted for hospitalization on the severity of 27 psychopathological dimensions ranging from anxiety to withdrawal (1) . They demonstrated that in regard to symptoms, these severely ill borderline people, until then often diagnosed and lumped together with patients with schizophrenia, were clearly distinct from the group with schizophrenia.
In the course of this work, Gunderson also reviewed the then existing descriptive accounts, theories, psychodynamic formulations, psychological testing results, and treatment recommendations of borderline patients, some 25–50 papers in all, including important and seminal contributions by Adolph Stern (2) , Roy Grinker (3) , Otto Kernberg (4) , James Masterson (5) , and Gerald Adler (6) . Some of the publications were semantically confusing, discrepant, or simply a jumble of words describing behavior, dynamic formulations, or symptoms. In an audacious, vigorous, youthful, and memorable article, Gunderson and Singer (7) distilled this material and identified six coherent factors they judged characteristic of most borderline patients according to most of the publications. I well remember reading that article with astonishment and saying to myself that this essay would change the world of borderline patients. It did.
Gunderson’s work, together with the brilliant contributions of Grinker (3) , Kernberg (4) , Masterson (5) , and Michael Stone (8) on the one hand and Kety, Rosenthal, and Wender (9) on the other, enabled Spitzer, Endicott, and Gibbon to develop a 22-item set that they mailed to 4,000 members of the American Psychiatric Association in January 1977. There were 808 usable responses, and these ultimately resulted in the first formulation of criteria for borderline personality disorder and schizotypal personality disorder (10) . Thus, to a very large extent, not only Gunderson’s conception but also his delivery led to the birth of borderline personality disorder in DSM-III for the first time in 1980. This in turn brought this large group of very ill and difficult patients, once the subject mostly of theorizing and treatment in the psychoanalytic community, into mainstream general psychiatric thought and investigation.
And a large group of patients it is. As Michael Stone (11) has pointed out, estimates of the prevalence of borderline personality disorder in the United States are in the range of 2.5%–3.0%—about the size of the population of Denmark or Sweden. To be sure, the specific diagnosis of borderline personality disorder defines a significantly more selective universe of patients than Kernberg’s very creative and valuable category of borderline personality organization, a structural diagnostic qualifier encompassing several specific diagnoses that includes approximately “10% or more of the entire population, or, in the case of the United States, a separate ‘nation’ of patients with borderline disorder as populous as Canada” (11) or Argentina.
Since Gunderson and Singer’s 1975 article, thousands of books, clinical reports, and research studies have been published on borderline personality disorder in the United States alone, not counting the entirely independent French work on les états limites or les psychoses blanches and the influence of U.S. work on German publications on das Borderline-Syndrom and die Borderline-Persönlichkeitsstörung . Gunderson’s innovative persistence and his findings, together with Zanarini and Frankenburg (12) , first hinted at in 1975 (1) , that brief, transient, and reversible psychotic (“quasi-psychotic”) experiences are a characteristic of the lives of many patients with borderline disorder led to the inclusion of transient paranoid ideation and severe dissociative symptoms among the nine criteria for borderline personality disorder in DSM-IV.
Borderline Personality Disorder: A Clinical Guide is an utterly distinguished and unerringly honest book, a meticulously crafted state-of-the-art summary of our knowledge about the diagnosis, the levels of treatment, and modalities of psychotherapy for this illness. This volume gives the reader Gunderson’s expert views as refracted through the prism of his 30-year-long experience in research on borderline disorders as well as teaching, consulting, and treating borderline patients.
Unfortunately, at present, a disquieting and unbridgeable moat separates the estimated 7–8 million people in our nation with borderline personality disorder from the resources necessary for its successful treatment, so graphically illustrated—with evidence from about 700 publications—in this work. While reflecting on Gunderson’s timetable for changes in these patients in the course of at least 5 years of psychotherapy (Figure 3-2, p. 73), I recalled my last conversation with a utilization manager of a company “managing” psychiatric benefits for health insurance firms and their authorization of seven psychotherapy appointments for one of my patients! Our society has made the anachronistic decisions to provide vigorous financial support for research on neuroscience and mental illnesses but to withhold the funds necessary for the implementation of the practical conclusions of these projects for the benefit and treatment of mentally ill people—thus abandoning them.
Two early chapters of the book provide background on diagnosis and differential diagnosis. Gunderson goes over in great detail the provenance of the diagnostic criteria for borderline personality disorder from the research of the major contributors to the field and the subjective suffering patients experience living life with borderline disorder. He makes the point that borderline personality disorder, by far the most important type of personality disorder, is such a major disorder of the self that it requires priority in planning meaningful rehabilitative treatments and therefore deserves categorical status of equal weight with axis I disorders. This then leads to dilemmas in differential diagnosis thoughtful psychiatrists can encounter in having to decide on a primary diagnosis of borderline personality disorder versus one of bipolar disorder, major depression, posttraumatic stress disorder, narcissistic personality disorder, or antisocial personality disorder.
The ensuing three chapters provide an overview for the treatment of borderline patients. These include therapeutic processes and the functions they serve; a potential sequence and timetable of expectable changes in behavior, affect, social functioning, and object relations; three sequential levels of alliance; case management and the responsibilities of the primary clinician; assessing and responding to recurrent suicidality; boundary violations; and various modalities of care, i.e., hospitalization, residential treatment, partial hospitalization, and outpatient psychotherapy. Here Gunderson distinguishes between treatment that is prescribed to patients, e.g., hospitalization or medications, who receive them with acceptance or resistance, and psychotherapy that to be successful requires assertive collaboration, inquisitiveness, and sharing of goals on the part of the patient.
There are valuable nuggets to be harvested in these chapters: initial “no-therapy” therapy (p. 90); “contracting for safety” (p. 93); responding to chronic suicidality with “false submission” (p. 97); sequential responses to boundary transgressions (p. 102); and the concept that the splits of patients with borderline disorder are not solely the product of their projections (p. 103). However, the language of Sidebar 3-2 (p. 80) is confusing. Patients with borderline disorder are certainly able to contract for therapy and to sometimes experience their therapists as caring and likable (Table 3-4, p. 79), but their internalized representations of others and of themselves are partial and polarized, typically leading to split-off, alternating idealized or persecutory perceptions of their therapists. As a result, they cannot establish a reliable collaborative working alliance until well into treatment, hence, the “myth of the alliance” described by Gerald Adler (13) .
Along the way, Gunderson introduces pharmacotherapy; cognitive behavior therapies, including dialectical-behavior therapy and psychoeducation; family therapies, including suggestions for psychoeducational materials; and interpersonal group therapy. The detailed discussion of working with families of patients with borderline disorder as potential supports for their treatment, beginning with initial meetings and then establishing an alliance and on through psychoeducation to possible selectively used psychodynamic family therapy, is immensely helpful.
Gunderson is straightforward in regard to dynamic psychotherapy: appropriate patients need to be able to control their impulses and be introspective, psychologically minded, and motivated to change. Even so, the dropout rate is very high. Many psychiatrists, psychologists, social workers, and advance practice nurses are not interested in the issues borderline patients struggle with and are not competent to do psychotherapy with them. Those who are competent have their own lives together, are capable of “holding” patients, believe the patient is suffering and can change, are convinced they can help with issues of dependency and anger, and are themselves nothing less than attentive, authoritative, challenging, clear, confident, conscientious, durable, engaged, and responsive. Competence, not gender of the therapist, is the issue. Table 11-5 (p. 254) helps patients choose such a paragon of virtue as a therapist, and Table 12-5 (p. 272) lists the expectable ultimate results of intensive, long-term psychodynamic therapy.
According to Gunderson, patients move in therapy from engagement to a relational alliance, then through acceptance of a positive dependency on their therapists to secure attachment and a true working alliance, and, finally, to consolidation and integration of their selves. In the course of these phases of therapy, they need, at different junctures, both Gerald Adler’s deficit-oriented Kohutian validating corrective relationship and Otto Kernberg’s conflict-model interpretive transference analysis. These theoretical perambulations are judiciously sprinkled with examples of inquisitive, gentle, and nonauthoritarian interventions, Gunderson’s style in conducting psychotherapy.
Throughout, Gunderson champions split treatment, i.e., treatment that involves “two treaters, two modalities, or any two components…e.g., hospital and psychotherapist, psychopharmacologist and family therapist, a primary clinician and self-assessment group” (p. 104) to safeguard the psychotherapist from becoming a “bad object” from which the patient must flee. I applaud the principle and goal of these suggestions. Unfortunately, such multiple modalities, other than two treaters, are not readily available in a noninstitutional, office-based practice where the vast majority of patients with borderline disorder are seen as outpatients. If it is difficult to find one competent psychiatrist for dynamic psychotherapy, as the author avers, what are the chances of finding two competent, independent professionals, in agreement on goals and methodology, to take care of a single borderline patient? Split treatment by two independent treaters, in a noninstitutional setting, is fraught with great dangers and difficulties for a person with borderline personality disorder. No one knows that better than Gunderson, who, together with Sara Bolton (14) , has eloquently described the tragic result such split treatment had for a female physician with borderline personality disorder.
That said, this volume is a first-rate work of scholarship that I highly recommend to all those interested and involved in the treatment of persons with borderline personality disorder, including and especially psychiatric residents. Gunderson writes affectingly and gives an attuned, resonant account of the conflicted lives and deficits of these uncommitted people and the dilemmas their physicians face. The writing tempers rigor with compassion, is minutely detailed, and puts these dislocated people and our growing understanding of them into context. Gunderson’s work and this book are admirable and immensely valuable achievements.
Reprints are not available; however, Book Forum reviews can be downloaded at http://ajp.psychiatryonline.org.
By John G. Gunderson, M.D. Washington, D.C., American Psychiatric Publishing, 2001, 329 pp., $57.00.
1. Gunderson JG, Carpenter WT Jr, Strauss JS: Borderline and schizophrenic patients: a comparative study. Am J Psychiatry 1975 ; 132:1257-1264 Link , Google Scholar
2. Stern A: Psychoanalytic therapy in the borderline neuroses. Psychoanal Q 1945 ; 14:190-198 Crossref , Google Scholar
3. Grinker R: The Borderline Syndrome: A Behavioral Study of Ego-Functions. New York, Basic Books, 1968 Google Scholar
4. Kernberg O: Borderline personality organization. J Am Psychoanal Assoc 1967 ; 15:641-685 Crossref , Medline , Google Scholar
5. Masterson J: Treatment of the Borderline Adolescent: A Developmental Approach. New York, John Wiley & Sons, 1972 Google Scholar
6. Adler G: Hospital treatment of borderline patients. Am J Psychiatry 1973 ; 130:32-35 Link , Google Scholar
7. Gunderson JG, Singer MT: Defining borderline patients: an overview. Am J Psychiatry 1975 ; 132:1-10 Link , Google Scholar
8. Stone MH: The Borderline Syndromes: Constitution, Coping, and Character. New York, McGraw-Hill, 1980 Google Scholar
9. Kety SS, Rosenthal D, Wender PH, Schulsinger F: Mental illness in the biological and adoptive families of adopted schizophrenics. Am J Psychiatry 1971 ; 128:302-306 Link , Google Scholar
10. Spitzer RL, Endicott J, Gibbon M: Crossing the border into borderline personality and borderline schizophrenia. Arch Gen Psychiatry 1979 ; 36:17-24 Crossref , Medline , Google Scholar
11. Stone MH: The role of pharmacotherapy in the treatment of patients with borderline personality disorder. Psychopharmacol Bull 1989 ; 25:564-571 Medline , Google Scholar
12. Zanarini MC, Gunderson JG, Frankenburg FR: Cognitive features of borderline personality disorder. Am J Psychiatry 1990 ; 147:57-63 Link , Google Scholar
13. Adler G: The myth of the alliance with borderline patients. Am J Psychiatry 1979 ; 136:642-645 Link , Google Scholar
14. Bolton S, Gunderson JG: Distinguishing borderline personality disorder from bipolar disorder: differential diagnosis and implications (case conf). Am J Psychiatry 1996 ; 153:1202-1207 Link , Google Scholar
- Cited by None


- Personality
Are BPD Sufferers Manipulative, Sadistic, and Worse?
The hurt and anger caused by—and also suffered by—folks with bpd can be potent..
Updated March 31, 2024 | Reviewed by Jessica Schrader
- What Is Personality?
- Find a therapist near me

Women and men with borderline personality disorder seem not to know how to stop arguing . Often described as "drama queens" or "abusive," they too frequently create chaos in situations where others would smoothly deal with the normal differences and disappointments that arise from time to time for all of us.
Marsha Linehan, creator of DBT (Dialectical Behavior Therapy ) which is the treatment method that is most often recommended for people with borderline issues, bases her understandings of this disorder on the belief that people with BPD "feel the mental squalls of rage, emptiness, and anxiety far more intensely than most people do ." This intensity of emotional pain was the theme of the first post in a series of articles I have begun posting on the inner experience of people with borderline disorders.
This article is the second in that series. Like the first post, this article records my dialogue with H.O., a very insightful physician who herself has been diagnosed with borderline personality disorder. Like many BPD sufferers, she has been determined to find routes to recovery.
I have written earlier PT articles on borderline personality disorder from the point of view of people who suffer from having to deal with an individual with difficult-to-deal-with BPD behaviors such as adult children of mothers with BPD . This current series of posts, by contrast, clarifies the painful inner experience of someone who struggles with a borderline personality disorder him/herself.
Warmest thanks to H.O. for sharing her insights with us.
To Dr. Heitler, I wrote to you after reading three of your posts published in the Psychology Today website: " Evil Genes? An Unconventional Perspective On BPD ," " From Cute Little Girl To Boderline Personality " and " You Can End Your Borderline Personality Style ." I have to say I disagree with a fundamental tenet especially of the first article which refers to "manipulative" or even " sadistic " behaviours of BPD sufferers. The choice of the term "manipulative" suggests some kind of Machiavellian scheming and cunning to reach objectives which are not immediately obvious. I think Dr. Linehan was the closest to the truth in interpreting the so-called "manipulative" behaviours of BPD patients when she declared they were blunt, clumsy and ineffective efforts to have the BPD's needs met. To all concerned the objective of these behaviours is also blatantly obvious thus removing any element of manipulation. I would strongly recommend avoiding the use of term "manipulative" in reference to any clumsy efforts of BPD patients to achieve anything, because these efforts are anything but. At best these behaviours (eg threatening suicide in the case of abandonment by a loved one) are somewhat pathetic efforts, when a BPD patient actually begs and humiliates herself in inevitably unsuccessful attempt to avoid abandonment. The use of the term "sadistic" in my humble opinion is a misinterpretation of motives behind BPD's "bad" behaviours, achieving nothing but greater stigmatization. In my work with very poorly functioning patients with BPD what I commonly saw was that these girls were victims of sadistic, inhuman abuse as kids. They themselves however never intentionally upset or harmed anyone for the pure evil joy of it. The arguments and even physical acts of violence never involved any gratification from inflicting pain, ever. They were solely vents for frustration and anger at having BPD's needs and demands not met yet again. The source of these common misconceptions about the intentions and motives of BPD patients lies in fundamental misunderstanding. Please believe me, BPD makes it impossible to function in the world as it is, where most people are indifferent and don't care at all and others are trying hard, but rarely succeeding in getting the needs of BPDs met. This is because these needs are so immense! A person with BPD could function, when symptomatic, only in the world where everybody loves her like her own mother, unconditionally and patiently. Of course such world will never exist and thus BPDs with their enormous, unfulfilled needs of love and affection will forever remain frustrated and angry, and resort to behaviours which are misunderstood as "manipulation." A normal person derives strength in daily functioning in the indifferent or occasionally hostile world from their own healthy ego. A BPD has no healthy ego to base their survival on. A BPD can only survive on constant stream of love and affection, and if it dries out the BPD's world collapses. This is where the frantic efforts to avoid abandonment come from--because BPDs know painfully well that they are unable to function without it. The fact that terms such as "bad", "sadistic," and "manipulative" are used to describe how the "normal" world perceives and judges BPD's desperate attempts to have their needs met is a sad testimony to the fact that the world is, in fact, more often than not hostile to these patients. The only way to understand these patients is to assume their needs in terms of affection, support, understanding and human warmth are infinitely larger than the needs that can reasonably be met in the world as it is. This is why these needs will inevitably remain unmet and result in a BPD person feeling frustration, anger and hostility. As "bad" as these patients are it is much worse to be in their shoes. I would argue that in terms of quality of life BPD is in the same league as terminal cancer. The irony is, of course, that while everybody is compassionate to patients with cancer, few, if any have genuine compassion for patients with BPD because these patients through their utter lack of social skills and use of behaviours which are considered inappropriate at best, and "sadistic" at worst are absolute masters in antagonizing everyone around them. This is the vicious circle of BPD — while these patients' need for human compassion is infinitely greater than that of functioning individuals, their clumsiness in getting this need met results in even less, if any compassion at all. I really appreciate your lending an ear to the perspective of a BPD sufferer. With regards, H.O. -----------
As a result of what I have been learning from our correspondence, and consonant with Marsha Linehan's observations, I find myself increasingly limiting my use of the term BPD to referring only to pervasive patterns of emotional hyper-reactivity.
There may well be some individuals with BPD who are genuinely manipulative or sadistic.
These habits now would suggest to me co-morbid diagnoses, that is, a combination of borderline personality emotional hyper-reactivity with narcissistic (ignoring others' feelings and concerns) and/or psychopathic (conning) patterns.
In the Journal of Personality Disorders a 2006 an excellent article by Nancy Nyquist Potter, PhD entitled "What is Manipulative Behavior Anyway?" looked to define the term manipulative . "In the Hare Psychopathy Checklist (cited in Bowers, 2002) ... manipulation is defined as deception used for personal gain, without concern for victims."
Interestingly, the point of Dr. Potter's article, like the point of your writing, H.O., in this post, is that many clinicians, and laypeople also, too readily utilize the term manipulative with clients who have a BPD diagnosis. BPD sufferers get further stigmatized this way. These terms show no sympathy for the suffering that their hyper-intense emotions cause them to endure.
At the same time, it is unclear what might be a more sympathetic terminology for labeling the aggressive attempts by individuals with BPD patterns to get others to give them what they feel that they desperately need.
For now, therefore, the pejorative term manipulative (especially referring to females), and the term controlling (more often used in reference to men) may be the only terms we have.
Perhaps the best we can do is to be sure that we are using the terms only to describe specific behaviors, not the whole person. Yet saying that false accusations, for instance, are manipulative behaviors still is going to lead others to say, "Yes, the person who has been falsely accusing me of x and y is manipulative."

Maybe readers of this post can offer better options?
Again, thanks so much to you H.O. for sharing your insights.
With warmest appreciation,
Dr. Heitler
--------------------------
Learn more about positive communication skills on Susan Heitler’s website .

Susan Heitler, Ph.D ., is the author of many books, including From Conflict to Resolution and The Power of Two . She is a graduate of Harvard University and New York University.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
- Entertainment
- Environment
- Information Science and Technology
- Social Issues
Home Essay Samples Health
Essay Samples on Borderline Personality Disorder
Dialectical behavioral therapy for borderline personality disorder.
We are proposing a group designed to work with teens with a history of sexual abuse and whom have been diagnosed with borderline personality disorder (BPD). The teen years are important development stages for individuals, where they develop separation, identity, cognitive/emotive regulation, and self-image (Aronson...
- Borderline Personality Disorder
- Cognitive Behavioral Therapy
Impairment and Distress Caused by Borderline Personality Disorder
Borderline Personality disorder is a disorder that makes things such as social norms and dynamics of relationships difficult to understand. Borderline Personality Disorder gets its name from history because they considered this disorder to be on the “borderline” between neurosis and psychosis. This disorder approximately...
- Psychological Disorders
Development Stages and Delays with Borderline Personality Disorder
Growing up, I spent a lot of time with my family. I have a family member who has been diagnosed with borderline personality disorder. He has always been one to shut people out, has trouble connecting with others and fearing being abandoned. I have known...
Borderline Personality Disorder: Reasons and Environment
Ever been a victim of sexual or physical abuse when you were younger? Or suffered from emotional abuse and the lack of parental acceptance during your childhood? If so and you are experiencing a difficult adulthood, then borderline personality disorder could be the solution to...
Case Study On Borderline Personality Disorder
Over 3 million residents in the United States of America deal with a mental disorder called borderline personality disorder. Manuel Herrera is a United States Soldier for army. All his life he has been very strange, and has showed too many emotions that show he...
- Mental Disorder
Stressed out with your paper?
Consider using writing assistance:
- 100% unique papers
- 3 hrs deadline option
Best topics on Borderline Personality Disorder
1. Dialectical Behavioral Therapy For Borderline Personality Disorder
2. Impairment and Distress Caused by Borderline Personality Disorder
3. Development Stages and Delays with Borderline Personality Disorder
4. Borderline Personality Disorder: Reasons and Environment
5. Case Study On Borderline Personality Disorder
- Eating Disorders
- Antibiotics
- Childhood Obesity
- Tuberculosis
Need writing help?
You can always rely on us no matter what type of paper you need
*No hidden charges
100% Unique Essays
Absolutely Confidential
Money Back Guarantee
By clicking “Send Essay”, you agree to our Terms of service and Privacy statement. We will occasionally send you account related emails
You can also get a UNIQUE essay on this or any other topic
Thank you! We’ll contact you as soon as possible.

Essay on Borderline Personality Disorder
Students are often asked to write an essay on Borderline Personality Disorder in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Borderline Personality Disorder
What is borderline personality disorder.
Borderline Personality Disorder, or BPD, is a mental health condition. It affects how a person thinks, feels, and behaves. People with BPD often have trouble managing their emotions and thoughts, which can lead to impulsive actions and problems in relationships.
Signs of BPD
People with BPD may have intense mood swings, feel unsure about their identity, and have a fear of being abandoned. They may also have trouble controlling their anger and can act impulsively. These symptoms can cause problems in their daily life.
Causes of BPD
The exact cause of BPD is unknown. It is likely a combination of genetic factors, brain structure, and environmental influences. Traumatic events during childhood, such as abuse or neglect, may also play a role.
Treatment for BPD
Treatment for BPD often includes therapy. This can help people learn to manage their emotions, reduce impulsive behaviors, and improve their relationships. Sometimes, medication may also be used to help with symptoms.
Living with BPD
Living with BPD can be challenging, but with the right treatment and support, people with this condition can lead fulfilling lives. It’s important for them to have a strong support system, including friends, family, and mental health professionals.
250 Words Essay on Borderline Personality Disorder
Borderline Personality Disorder, or BPD, is a mental health problem. People with BPD have a hard time controlling their emotions. They may feel very sad or angry for no clear reason. This can lead to problems in their daily life, like fights with friends or family.
Signs of Borderline Personality Disorder
People with BPD often feel empty inside. They may also be scared of being alone. They might do risky things, like drive too fast or spend too much money. They might also hurt themselves or think about suicide. These signs are serious and need help from a doctor or therapist.
Causes of Borderline Personality Disorder
We don’t know for sure what causes BPD. It might be a mix of things, like genes and things that happen in life. For example, if someone has a family member with BPD, they might be more likely to have it too. And if someone has been through tough things, like abuse or neglect, they might also be more likely to have BPD.
Treatment of Borderline Personality Disorder
BPD can be treated with therapy. This is a type of talk with a trained person. The goal is to learn new ways to handle emotions and relationships. Sometimes, medicine can also help. But it’s important to remember that getting better takes time.
In short, BPD is a serious but treatable mental health problem. If you or someone you know shows signs of BPD, it’s important to get help from a doctor or therapist. They can provide the right treatment and support.
500 Words Essay on Borderline Personality Disorder
Borderline Personality Disorder (BPD) is a mental health condition. It affects the way a person thinks and feels about themselves and others. This can cause problems in everyday life. People with BPD often have a hard time managing their emotions and thoughts. They may feel very worried about people leaving them, and may go to great lengths to stop this from happening.
Signs and Symptoms
There are many signs that someone might have BPD. They might have extreme changes in mood that last just a few hours or a few days. They might have a hard time having stable relationships. They might also have a poor self-image, meaning they do not feel good about themselves. They may feel empty inside, get very angry, or even feel out of touch with reality. Some people with BPD might also hurt themselves or have thoughts of ending their life.
The exact cause of BPD is not known. But it is believed to be a mix of things. These include genetics, meaning it can run in families. It can also be due to brain abnormalities. This means that some parts of the brain that control emotions might not work as well in people with BPD. Lastly, it could be due to environmental factors. For example, people who have experienced abuse or neglect in their childhood may be more likely to develop BPD.
BPD is a serious condition, but it can be treated. The main treatment is a type of talking therapy called psychotherapy. This can help people with BPD understand and manage their feelings better. Sometimes, medication may also be used to help with certain symptoms, like mood swings or feelings of emptiness. Overall, the goal of treatment is to help people with BPD live a more normal and fulfilling life.
Living with BPD can be challenging. But with the right help and support, people with BPD can lead meaningful lives. It’s important for them to get proper treatment and to stick with it. It’s also important for them to have a strong support system. This can include family, friends, and mental health professionals.
In conclusion, BPD is a complex mental health disorder that affects a person’s emotions and relationships. It can be difficult to live with, but with the right treatment and support, people with BPD can lead fulfilling lives. Understanding and awareness about BPD are crucial for reducing stigma and providing support to those affected by this disorder.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Discrimination On Gender
- Essay on Discrimination Of Skin Color
- Essay on Discrimination And Equality
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Invited essay: Identity and borderline personality disorder
Affiliation.
- 1 Department of Psychology, University of Aarhus, Nobelparken, Jens Chr.Skous Vej 4, DK-8000 Aarhus C, Denmark. [email protected]
- PMID: 20545499
- DOI: 10.1521/pedi.2010.24.3.344
The general consensus is that disturbed identity is one of the defining characteristics of borderline personality disorder. So far it has not been possible to reach a generally accepted definition of identity, and the clinical phenomenon of identity disturbance involves inner subjective states that are not directly accessible to observation and reliable assessment. In this article a preliminary definition of identity is suggested and different levels, dimensions, and categories of identity are delineated. Essential elements of identity disturbance or identity diffusion in BPD patients are described and related to other aspects of borderline personality disorder: mentalization failures, disrupted relationships, impulsive or nonvolitional behavior, deficits in memory, dissociation, and dysfunctional self-narratives.
Publication types
- Borderline Personality Disorder / psychology*
- Self Concept*
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Borderline personality disorder.
Jennifer Chapman ; Radia T. Jamil ; Carl Fleisher .
Affiliations
Last Update: June 2, 2023 .
- Continuing Education Activity
The Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) lists ten personality disorders that are divided into three clusters, clusters A, B, and C. Borderline personality disorder (BPD) is a cluster B disorder that is characterized by hypersensitivity to rejection and resulting instability of interpersonal relationships, self-image, affect and behavior. Borderline personality disorder causes significant impairment and distress and is associated with multiple medical and psychiatric co-morbidities. Surveys have estimated the prevalence of borderline personality disorder to be 1.6% in the general population and 20% in the inpatient psychiatric population. This activity examines the presentation and evaluation of borderline personality disorder and highlights the role of the interprofessional team in its management.
- Identify the epidemiology of borderline personality disorder.
- Describe the presentation of a patient with borderline personality disorder.
- Outline the treatment options available for borderline personality disorder.
- Explain interprofessional team strategies for improving care coordination and communication to advance the management of borderline personality disorder and optimize patient outcomes.
- Introduction
A personality disorder is a disorder involving a rigid and unhealthy pattern of thinking. Personality disorders are prevalent in the general population and more so in clinical populations. In the pediatric population, all personality disorders can be diagnosed, except antisocial personality disorder, as long as the pathologic behavior has been present for a year or more. The Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) lists ten personality disorders divided into the 3 clusters (A, B, and C). [1] Borderline personality disorder (BPD) is 1 of 4 cluster-B disorders that include borderline, antisocial, narcissistic, and histrionic. Borderline personality disorder (BPD) is characterized by hypersensitivity to rejection and resulting instability of interpersonal relationships, self-image, affect, and behavior. [2] Borderline personality disorder causes significant impairment and distress and is associated with multiple medical and psychiatric co-morbidities. Surveys have estimated the prevalence of borderline personality disorder to be 1.6% in the general population and 20% of the psychiatric inpatient population. [3]
In contrast, obsessive-compulsive personality disorder (OCPD) appears to be the most prevalent personality disorder, with rates around 5% of the general population in some studies. [4] Patients with borderline personality disorder have been shown to utilize extensive treatment resources and are at increased morbidity and mortality compared with the general population. This is perhaps the reason why borderline personality disorder has been studied more extensively than other personality disorders.
Borderline personality disorder is multifactorial in etiology. There is a genetic predisposition. Twin studies show over 50% heritability (greater than that for major depression). [5] Twin studies performed in 2000 and 2008 both demonstrated higher concordance of the rate of borderline personality disorder for monozygotic versus dizygotic twins. Environmental factors that have been identified as contributing to the development of borderline personality disorder include primarily childhood maltreatment (physical, sexual, or neglect), found in up to 70% of people with BPD, as well as maternal separation, poor maternal attachment, inappropriate family boundaries, parental substance abuse, and serious parental psychopathology.
There are many theories about the development of borderline personality disorder. In the mentalizing model of Peter Fonagy and Anthony Bateman, borderline personality disorder is the result of a lack of resilience against psychological stressors. In this framework, Fonagy and Bateman define resilience as the ability to generate adaptive re-appraisal of negative events or stressors; patients with impaired re-appraisal accumulate negative experiences and fail to learn from good experiences. [6] In the biosocial model popularized by Dr. Marsha Linehan, genetic vulnerability interacts with a "chronically invalidating environment" to produce the constellation of borderline personality disorder symptoms. In another theory, borderline personality disorder arises from the inability to regulate effect and the lack of formation of appropriate coping mechanisms in response to stress. [7] Otto Kernberg theorized that lack of integration in the early maternal relationship led to borderline personality disorder. [8] Kernberg hypothesized that the infant experiences the maternal figure in a dichotomous framework, the loving and nurturing mother who provides for the child and the punishing, hateful mother who deprives the child. This contradiction causes intense anxiety and, if not integrated into a more moderate unitary concept, ultimately leads to the development of splitting. The term "splitting" refers to the defense mechanism in which the patient cannot form a realistic view of another person. At any given time, the other person is viewed as entirely good or entirely bad. This inability to view others as having both positive and negative attributes impairs personal relationships.
Neuroimaging studies have identified differences in the amygdala, hippocampus, and medial temporal lobes in patients with borderline personality disorder. Such studies also suggest that patients with borderline personality disorder misattribute negative emotions (fear, anger, disgust) to neutral faces more so than controls or other patients, despite having the perception of happy and upset faces equivalent to those groups. Neurobiological studies have suggested that impaired neuropeptide function, particularly serotonin, may be present in patients with borderline personality disorder. On neuropsychological testing, a meta-analysis published in 2005 showed that patients with borderline personality disorder had lower performance on neurocognitive testing in the following domains: attention, cognitive flexibility, learning and memory, planning, speed processing, and visuospatial abilities. [9]
- Epidemiology
Large, nationwide epidemiologic studies published in 2007 and 2008 estimated the point prevalence of borderline personality disorder in the general population at 1.6%, with a lifetime prevalence of 5.9%. No significant difference in rates of borderline personality disorder was found between females and males in the general population. In the clinical setting, however, the ratio of females to males has been reported as 3:1. These studies challenged previous reports that borderline personality disorder was more prevalent in women. The prevalence of borderline personality disorder in the psychiatric outpatient population has been estimated at 11%, and in the psychiatric inpatient population, as high as 20%. Multiple studies examining the relationship between ethnicity and borderline personality disorder have not produced similar results. [10] [11]
- Pathophysiology
The pathophysiology of borderline personality disorder is likely a combination of genetic predisposition combined with early childhood environmental factors and neurobiological dysfunction. A greater understanding of neurobiology and, specifically, neurotransmitter dysfunction may lead to improved therapeutic options for treating borderline personality disorder. A recent study published in 2015 examined the role of oxytocin in the regulation of social reward and empathy networks as a contributing cause of borderline personality disorder and other personality disorders. Specifically, serotonin dysregulation reducing the sensitivity of the 5HT-1A receptor may contribute to borderline personality disorder. Increased rates of learning disorders, attention-deficit/hyperactivity disorder, and neurocognitive deficits, as well as abnormal electroencephalographic findings, have also been reported in patients with borderline personality disorder.
- History and Physical
A careful history and physical examination should be performed before performing a comprehensive psychiatric assessment. There are structured diagnostic screening tools that are used to assess personality disorders and specifically borderline personality disorder, for example, the Zanarini Rating Scale for borderline personality disorder.
The DSM-5 Diagnostic Criteria for Borderline Personality Disorder
A pervasive pattern of instability of interpersonal relationships, of self-image, and affects as well as marked impulsivity beginning by early adulthood and present in a variety of contexts as indicated by five or more of the following:
- Frantic efforts to avoid real or imagined abandonment. Note: Do not include suicidal or self-mutilating behavior covered in criterion 5.
- A pattern of unstable and intense interpersonal relationships characterized by alternating between extremes of idealization and devaluation.
- Identity disturbance: Markedly and persistently unstable self-image or sense of self.
- Impulsivity in at least two areas that are potentially self-damaging, for example, spending, substance abuse, reckless driving, sex, binge eating, etc. Note: Do not include suicidal or self-mutilating behavior covered in criterion 5.
- Affective instability is caused by a marked reactivity of mood, for example, intense episodic dysphoria, anxiety, or irritability, usually lasting a few hours and rarely more than a few days.
- Chronic feelings of emptiness.
- Inappropriate, intense anger, or difficulty controlling anger, for example, frequent displays of temper, constant anger, recurrent physical fights.
- Transient paranoid ideation or severe dissociative symptoms.
Several diagnostic instruments are available to aid in the diagnosis, such as:
- The McClean screening instrument for borderline personality disorder
- Personality diagnostic questionnaire
- Structured clinical interview for DSM-5 personality disorders
- The Minnesota borderline personality disorder scale
- The personality assessment inventory-borderline features scale
Diagnostic tools may be separated into the general categories of the self-report and structured interview.
Patients with borderline personality disorder have been shown to have high rates of comorbid disorders:
- Mood disorders 80% to 96%
- Anxiety disorders 88%
- Substance abuse disorders 64%
- Eating disorders 53%
- Attention deficit hyperactivity disorder (ADHD) 10% to 30%
- Bipolar disorder 15%
- Somatoform disorders 10%
- Treatment / Management
Treatment of borderline personality disorder relies on psychotherapy. Three evidence-based therapies are effective for patients with borderline personality disorder. First, mentalizing-based therapy (MBT) helps patients manage emotion dysregulation by feeling understood, allowing them to be more curious and make fewer assumptions about the intentions of the people around them. A second therapy, dialectical behavior therapy (DBT), combines mindfulness practices with concrete interpersonal and emotion regulation skills. Third, transference-focused psychotherapy (TFP) focuses on using the patient-therapist relationship to develop the patient's awareness of problematic interpersonal dynamics. MBT and DBT each incorporate individual and group treatment over 12 to 18 months. For adolescents, family therapy may be an appropriate substitute for group therapy, though not always.
No medications are FDA-approved for the treatment of borderline personality disorder. Medications such as SSRIs, mood stabilizers, and antipsychotics have shown limited effectiveness in trials aiming at the control of symptoms such as anxiety, sleep disturbance, depression, or psychotic symptoms. Anxiety can be challenging to treat because patients may label their internal experiences with the word anxiety, even when they are not truly based on fear. Thus, "anxiety" may need to be accurately re-labeled, with treatment recommendations stemming from the patient's specific internal experience. The exception to the misleading use of the word anxiety is that patients with borderline personality disorder often have a fear of being alone; in other words, they have attachment-related anxiety. However, attachment-related anxiety is not necessarily similar in etiology or treatment to recognized anxiety disorders.
Self-injurious behavior, boundary issues, and frequent suicidal threats present therapeutic challenges specific to the treatment of patients with borderline personality disorder. High rates of comorbid substance abuse may also confound the treatment of borderline personality disorder patients. Patients with borderline personality disorder do not typically require hospitalization; however, inpatient care may be required in certain situations, such as:
- Imminent risk of high lethality behaviors due to overt suicidal ideation or impulsivity
- Severe social stressors causing intense negative thoughts or transient psychosis
- The rapid escalation in the severity of self-injurious behavior
- Decompensation of comorbid psychiatric diagnoses or severe substance abuse
The traditional belief that prolonged (longer than one week) inpatient hospitalization is counterproductive or even deleterious for patients with borderline personality disorder was not supported in a recent study. The data showed equal improvement among inpatients with and without borderline personality disorder over several weeks of hospitalization.
Given high comorbidity with ADHD, all patients with borderline personality disorder should be screened for this condition. When dealing with adolescents, parents, and teachers should be asked to fill out a standardized questionnaire (Conners, SNAP, Vanderbilt). For adults, no standard of care is established for self-report or observer-report of inattentive or hyperactive symptoms. A combination of 2 self-reports to guide clinical decision-making, the ADHD Symptom Rating Scale (World Health Organization) and the Wender-Utah ADHD Rating Scale (WURS-25), provide more than 80% sensitivity and specificity.
- Differential Diagnosis
When considering a diagnosis of borderline personality disorder, the differential diagnosis should always include other personality disorders since overlap is common, especially within cluster B. Other diagnostic considerations include:
- Substance use disorder
- Non-suicidal self-injury disorder (a time-limited phenomenon in many patients)
- Bipolar disorder (5-times less prevalent, but co-morbidity approaches 15%)
- Autism spectrum disorder (patients with congenital deficits in theory of mind may also show severe mood dysregulation)
There is a good prognosis for patients with borderline personality disorder. A longitudinal study of 290 inpatients diagnosed with borderline personality disorder and reassessed at 2-year intervals over 16 years yielded the following rates of remission: [12]
- 35% remission after 2 years
- 91% remission after 10 years
- 99% remission after 16 years
Unfortunately, the authors of this study noted that remission was associated with impoverished social relationships, leading them to suggest that patients may appear to remit because they avoid interpersonal relationships rather than gradually developing better interpersonal skills. Once achieved, remission was nonetheless sustained for over eight years in 75% of patients. Several factors were associated with the faster onset of remission, including lack of co-morbid, axis-1 disorders, no history of childhood sexual abuse, no history of family substance abuse, high baseline functioning (demonstrated at school or in the workplace), and less than 25 years. Sustained remission from borderline personality disorder has been demonstrated in several other studies as well. [13] [14]
- Complications
The complications of borderline personality disorder include:
- Engaging in risky behavior (e.g., rash driving)
- Not completing education
- Getting in trouble with the law
- Problems with relationships
- Suicide attempts
- Deterrence and Patient Education
Patients and their families should be educated about borderline personality disorder and be provided with the necessary literature to learn about the condition. The families should be advised that the patients may get angry and suicidal and told to seek help immediately. In addition, patients should be encouraged to seek and continue psychotherapy until they experience sustained benefits.
- Enhancing Healthcare Team Outcomes
Borderline personality disorder is one of the most difficult mental health disorders to manage; it is best managed with an interprofessional team, including psychiatrists, psychologists, pharmacists, mental health nurses, and social workers. Pharmacists review prescribed medications, check for drug-drug interactions and provide patient education. Mental health nurses and social workers provide care, monitor patients, participate in the education of patients and their families, and provide follow-up to the team. Unfortunately, there are no medications that seem to help; psychotherapy may help some patients, but compliance with treatment is low. The outcomes for most patients are poor, with many running into legal, social, and personal problems. [Level 5]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Jennifer Chapman declares no relevant financial relationships with ineligible companies.
Disclosure: Radia Jamil declares no relevant financial relationships with ineligible companies.
Disclosure: Carl Fleisher declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Chapman J, Jamil RT, Fleisher C. Borderline Personality Disorder. [Updated 2023 Jun 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- [Personality disorders in a nonclinical sample of adolescents]. [Encephale. 2002] [Personality disorders in a nonclinical sample of adolescents]. Chabrol H, Chouicha K, Montovany A, Callahan S, Duconge E, Sztulman H. Encephale. 2002 Nov-Dec; 28(6 Pt 1):520-4.
- Obsessive-Compulsive Personality Disorder. [StatPearls. 2024] Obsessive-Compulsive Personality Disorder. Rizvi A, Torrico TJ. StatPearls. 2024 Jan
- Histrionic Personality Disorder. [StatPearls. 2024] Histrionic Personality Disorder. French JH, Torrico TJ, Shrestha S. StatPearls. 2024 Jan
- Review The comorbidity of multiple personality disorder and DSM-III-R axis II disorders. [Psychiatr Clin North Am. 1991] Review The comorbidity of multiple personality disorder and DSM-III-R axis II disorders. Fink D. Psychiatr Clin North Am. 1991 Sep; 14(3):547-66.
- Review Borderline personality disorder: Prevalence and psychiatric comorbidity among male offenders on probation in Sweden. [Compr Psychiatry. 2015] Review Borderline personality disorder: Prevalence and psychiatric comorbidity among male offenders on probation in Sweden. Wetterborg D, Långström N, Andersson G, Enebrink P. Compr Psychiatry. 2015 Oct; 62:63-70. Epub 2015 Jun 26.
Recent Activity
- Borderline Personality Disorder - StatPearls Borderline Personality Disorder - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
This essay will consider borderline personality disorder (BPD), its manifestations, personal characteristics and cognitive features associated with the disease, and potential genetic causes and neurochemical features. BPD is a severe disorder that can significantly affect one's health, well-being, and ability to develop meaningful relationships.
Borderline personality disorder (BPD) is a mental illness characterized by sharp variations in emotions, behavior, and self-image. These changes often result in impulsive behavior and unstable relationships of the affected individuals. People with BPD can experience depression, prolonged anxiety, and intense feelings of anger.
Borderline personality disorder is a severe mental disorder that impacts an individual's behavior, relationships, and mood. The disorder usually begins during adolescence or young adulthood. People with BPD have a tendency of rapid change in attitude or feelings toward others because they cannot regulate them. 1361 Words.
Borderline personality disorder (BPD) is a mental health disorder that is characterized by ongoing patterns of changing moods, behaviors, and self-image. When a person has BPD, they often experience periods of intense feelings of anger, anxiety, or depression that can last for a few hours or a few days. The mood swings experienced by people ...
1. Introduction. Borderline personality disorder (BPD) is a chronic psychiatric disorder characterized by pervasive patterns of affective instability, self-image disturbances, instability of interpersonal relationships, marked impulsivity, and suicidal behavior (suicidal ideation and attempt) causing significant impairment and distress in individual's life [].
Borderline personality disorder (BPD) is a severe mental health condition characterized by emotional instability, impulsive and self-damaging behaviors, and stormy interpersonal relationships (American Psychiatric Association, 2013).This disorder heavily taxes the mental health care system (Bagge, Stepp, & Trull, 2005; Comtois et al., 2003) and results in high personal, economic, and societal ...
Borderline personality disorder is a mental health condition that affects the way people feel about themselves and others, making it hard to function in everyday life. It includes a pattern of unstable, intense relationships, as well as impulsiveness and an unhealthy way of seeing themselves. Impulsiveness involves having extreme emotions and ...
Borderline personality disorder (BPD) is a contested diagnosis for a number of reasons: the phenotype is heterogeneous, there is extensive symptom overlap with other psychiatric diagnoses and debate about the validity of the BPD diagnosis in the literature. ... Jorgensen, CR (2010) Invited essay: identity and borderline personality disorder ...
1 Introduction. Borderline personality disorder (BPD) is a complex and severe psychiatric disorder characterized by mood dysregulation, interpersonal instability, self-image disturbance, and markedly impulsive behavior (e.g., aggression, self-injury, suicide) ().In addition, people with BPD may have chronic, frequent, random feelings of emptiness, fear, and so on.
I well remember reading that article with astonishment and saying to myself that this essay would change the world of borderline patients. It did. ... There were 808 usable responses, and these ultimately resulted in the first formulation of criteria for borderline personality disorder and schizotypal personality disorder . Thus, to a very ...
Introduction. Borderline Personality Disorder (BPD) impacts upon a wide range of cognitive and behavioral domains, resulting in symptoms such as intense dysphoric affect, chronic instability of mood, problematic interpersonal relationships, disturbed cognition and recurrent self-harm [].Rates of attempted suicide range between 38% to 73% in people with BPD, and 10% die by suicide, giving the ...
Objective: Borderline personality disorder (BPD) is the most common personality disorder, affecting 1.8% of the general population, 10% of psychiatric outpatients, and 15%-25% of psychiatric inpatients. Practice guidelines recommend psychotherapies as first-line treatments. However, psychotherapies commonly used for the treatment of BPD are numerous, and little is known about the comparative ...
This article is the second in that series. Like the first post, this article records my dialogue with H.O., a very insightful physician who herself has been diagnosed with borderline personality ...
View Full Essay. Borderline Personality Disorder Individuals with Borderline Personality Disorder are afflicted with a continual state of emotional conflict and chaos, often swinging from one extreme of emotion to another. Patients with BPD are traditionally known to exhibit symptoms of depression, anger and anxiety at varying times, and ...
A randomized controlled trial comparing the clinical efficacy and cost-effectiveness of eye movement desensitization and reprocessing (EMDR) and integrated EMDR-dialectical behavioural therapy (DBT) in the treatment of patients with post-traumatic stress disorder and comorbid (Sub)clinical borderline personality disorder: study design.
Impairment and Distress Caused by Borderline Personality Disorder. Borderline Personality disorder is a disorder that makes things such as social norms and dynamics of relationships difficult to understand. Borderline Personality Disorder gets its name from history because they considered this disorder to be on the "borderline" between ...
100 Words Essay on Borderline Personality Disorder What is Borderline Personality Disorder? Borderline Personality Disorder, or BPD, is a mental health condition. It affects how a person thinks, feels, and behaves. People with BPD often have trouble managing their emotions and thoughts, which can lead to impulsive actions and problems in ...
The general consensus is that disturbed identity is one of the defining characteristics of borderline personality disorder. So far it has not been possible to reach a generally accepted definition of identity, and the clinical phenomenon of identity disturbance involves inner subjective states that are not directly accessible to observation and reliable assessment.
Borderline personality disorder causes significant impairment and distress and is associated with multiple medical and psychiatric co-morbidities. Surveys have estimated the prevalence of borderline personality disorder to be 1.6% in the general population and 20% of the psychiatric inpatient population.[3] A personality disorder is a disorder ...
Search 217,699,779 papers from all fields of science. Search. Sign In Create Free Account. DOI: 10.1016/j.amp.2023.09.015; ... the structure and timing of rest‐activity patterns and symptoms of impulsivity and mood instability in bipolar disorder (BD), borderline personality disorder …