

What Are We Told About the Health of Biden and Trump? They Decide.
President Biden and former President Donald J. Trump are the oldest people ever to seek the presidency, challenging norms about what the public should know about candidates’ health.
President Biden is 81 and his rival, Donald J. Trump, is 77, and many voters believe both men are too old for another term. Credit... Photographs by Doug Mills/The New York Times
Supported by
- Share full article

By Michael D. Shear
Michael Shear has written about the health of presidents and presidential candidates often over the past 17 years.
- April 4, 2024
In 2008, when Senator John McCain was the oldest person to seek a first term in the White House, his campaign set out to reassure the public about his health. It let reporters examine 1,173 pages of handwritten notes, lab results and insurance documents, including details of the senator’s biopsies, his prostate exams and even the “very light tan freckling” on his buttocks.
He was 71 years old.
Listen to this article with reporter commentary
Open this article in the New York Times Audio app on iOS.
Today, President Biden is 81 and his rival, Donald J. Trump, is 77, and many voters believe both men are too old for another term . Their doctors proclaim them fit to serve, but neither has agreed to throw open his medical charts to prove it.
Mr. Biden released a six-page summary of medical test results in February, but his doctor has refused to be interviewed by reporters, breaking from past practice. Mr. Trump has revealed less than Mr. Biden; his last public note from his doctor, in November, was three paragraphs long . Neither man has sat for a comprehensive assessment of his mental fitness, a battery of tests often administered to people their age.
The longstanding truth about the American political system is that presidents and presidential candidates choose what to test, what to ignore, how much medical information to release to the public and, in the end, what voters will know about their health and well-being.
But the election between the two oldest people to ever seek the presidency is challenging that notion. Not only are Mr. Biden and Mr. Trump failing to do anything extra to reassure Americans that they can lead well into their ninth decade of life, they are doing less than their predecessors in some important ways.
The New York Times sent five-page letters to the Trump campaign and the White House with detailed questions about the health of the candidates. The Trump campaign did not respond to the letter, which included questions on mental fitness, cardiac health and whether he has taken Ozempic to lose weight.
The White House directed questions about Mr. Biden’s health to his doctor’s summary of the president’s physical in February, which concluded that Mr. Biden was fit for duty. “Joe Biden is proud to have been transparent with his health records as vice president, as a presidential candidate and as president,” said Andrew Bates, a White House spokesman. “He believes all leaders owe that level of honesty to the American people.”
The Times’s questions about mental fitness, however, were not addressed in the summary.
“I don’t want to be ageist, and I would never make an armchair diagnosis, but I do think we need full-blown neuropsychological exams” for both candidates, said Dr. Rudolph E. Tanzi, a professor of neurology at Harvard Medical School and the director of the McCance Center for Brain Health at Massachusetts General Hospital.
He was referring to a series of 33 tests known as the Neuropsychological Assessment Battery, which can detect dementia and other brain dysfunction.
“You’ve got to take an exam to drive,” Dr. Tanzi said. “These guys are taking the exam to be in the White House, where you have buttons you can push that might end the world.”
In interviews with a dozen of the country’s leading experts on aging, all described inexorable patterns that almost always accelerate after age 80. The body becomes more frail, more prone to damage and less likely to recover quickly. The risk of cognitive disease grows . Three percent of people between 65 and 69 have been diagnosed with dementia; by age 90, it is 35 percent.
Questions about the age and health of the two candidates are coursing through the political debate. So far, the answers have not been forthcoming.
That means Americans are left to judge their fitness for office in what experts on aging say is the worst possible way: from afar, largely based on snippets of their public appearances — the good and the bad.
The unknowns about Mr. Biden

The president has a common retort for anyone who expresses concern about his age and mental fitness: “Watch me.”
His aides have said he works out regularly, lifting weights some mornings and exercising on a Peloton. Last month, he delivered a forceful, energetic State of the Union address. And for the past few weeks, he has crisscrossed the country to give speeches and collect campaign cash at a pace that might exhaust any candidate, of any age.
But other appearances are enormously damaging . At an exclusive New York fund-raiser last summer, he recounted the racial violence in Charlottesville, Va., that inspired him to run for president in 2020. Minutes later, he told the same story again, practically word for word, drawing concerned glances from the crowd.
“I know I look like I’m 30,” Mr. Biden later joked to tepid laughter in the room. “I’ve been around doing this a long time.”
In February, the special counsel investigating Mr. Biden’s handling of classified documents described him as an elderly man with “diminished faculties.” The report, by the prosecutor Robert K. Hur, enraged Mr. Biden and his allies, who said it painted a wildly inaccurate picture.
A New York Times review of the transcript of the interview, which stretched over two days in October as Mr. Biden was responding to the Hamas attack on Israel, found that he was clear and cogent through most of the questioning, fumbling only on occasion with dates and the sequence of events.
All of the doctors interviewed for this story said it is difficult, if not impossible, to diagnose someone based on isolated moments or observations. They said stress, a lack of sleep or multitasking — rather than any mental decline — could lead to flubs.
“Those things are real, OK? But they’re not telling you if he can make a decision or not,” said Dr. Nir Barzilai, the director of the Institute for Aging Research at the Albert Einstein College of Medicine.
During Mr. Biden’s physical, his physician and a team of specialists chose not to conduct the Neuropsychological Assessment Battery, or a similar comprehensive assessment of his mental fitness.
The doctor decided there was no need for such a test because Mr. Biden regularly demonstrated what the medical team considered high-level executive functioning, according to people familiar with the decision.
One person on Mr. Biden’s team put it this way: After the president navigates hours of complicated foreign policy meetings during grueling trips overseas, it would be pointless to have him sit for a test asking which picture is a lion and which is a rhinoceros.
Dr. Sayed Azizi, the clinical chief of behavioral neurology and memory disorders at Yale University, said exams that go well beyond those kinds of simple questions are common in some fields after a certain age.
“Oftentimes, even in medicine, physicians who are over age 70 or so, they have to yearly go to the doctor and either take those tests or not, or somebody has to certify them that they’re OK to practice medicine,” he said. “Most hospitals have that.”
The White House contends that the details released by Dr. Kevin O’Connor , Mr. Biden’s physician, are sufficient and several past presidential doctors have chosen not to address reporters in the White House briefing room. Dr. O’Connor said an “extremely detailed” exam yielded no findings that would be consistent with neurological disorders such as a stroke, multiple sclerosis or Parkinson’s disease.
He said Mr. Biden’s noticeably stiffer walk was the result of arthritis of the spine, pain in his hip and peripheral neuropathy, a condition defined by a loss of sensation in his feet.
Dr. O’Connor’s summary also included the results of common blood tests, medications being taken and a discussion of the president’s struggle with sleep apnea. But Dr. O’Connor has not provided any supporting documents.
The biggest omission, according to medical experts, was the lack of cognitive testing. Dr. Tanzi said such tests should be administered to any presidential candidate 50 years or older, by doctors who do not have any political or personal allegiance to them.
“It has to be an independent assessment,” he said. “That’s absolutely essential.”
The unknowns about Mr. Trump
Even by the standards of previous candidates — and in contrast to Mr. Biden — the information Mr. Trump has provided about his own health has been exceptionally opaque.
In his letter in November, Dr. Bruce A. Aronwald said Mr. Trump’s “cognitive exams were exceptional.”
But he offered no backup for any of his claims. He did not say what kinds of tests the former president had been given. He did not provide the results of any bloodwork. He did not say what medicine Mr. Trump is taking. He did not explain what cognitive exams the former president took, when he took them or what the specific results were.
Without more information or testing, medical experts say it is impossible to judge Mr. Trump’s health with any precision, beyond the fact that he is subject to the same kinds of rapid declines that often afflict people his age.
“It can go down very quickly,” said Dr. Azizi, who studies the way the brain ages, losing about a gram of weight every year from the age of 16. He said that as the brain gets older, a person’s longstanding tendencies and habits are often amplified.
Mr. Trump, who is running for president while defending himself against dozens of felony counts, regularly talks about his stamina and vitality. He holds lengthy and bombastic rallies, often staying onstage for more than an hour.
But he has also had a series of gaffes .
During a campaign speech in New Hampshire in January, he confused Nikki Haley, his Republican opponent, for former Speaker Nancy Pelosi. He has claimed he defeated former President Barack Obama in 2016, when he actually ran against Hillary Clinton.
Recently, during a news conference, he seemed to confuse Gov. Kathy Hochul of New York with the state’s former governor Andrew Cuomo, who has not held that office since 2021.
Fred Trump, the former president’s father, developed Alzheimer’s in his mid-80s. Those who study the disease say Mr. Trump’s risk of developing Alzheimer’s, already higher because of his age, increases by about 30 percent because of his father’s diagnosis.
In 2018, the former president’s doctor revealed that Mr. Trump insisted on taking a dementia screening test known as the Montreal Cognitive Assessment and answered all 30 questions correctly. Dr. Ronny Jackson, then the White House physician, concluded that “the president is mentally very, very sharp; very intact.”
Mr. Trump went on TV to boast about his results , listing the words that he had been asked to remember in the right order: “Person. Woman. Man. Camera. TV.”
Medical experts quickly noted that the test does not measure intellect and that just about everyone without Alzheimer’s or another kind of dementia should get a perfect score.
Because of the absence of information Mr. Trump’s campaign has released, it is also difficult to know whether the former president’s risk of other health issues has increased in recent years.
When Mr. Trump was president, his weight, history of high cholesterol and lack of exercise put him at higher risk of developing cardiac disease that could lead to a heart attack or stroke, according to a letter released by his doctor in 2018.
In 2018, Mr. Trump’s doctor said he was 239 pounds, just one pound shy of the medical definition of obesity for his height and age. Last year, when he was booked at the Fulton County jail in Georgia, he listed his weight at 215 pounds — a figure that many critics called into question.
Much of the public information about his health has been riddled with exaggerations. After Mr. Trump announced his candidacy in 2015, his doctor, Harold Bornstein, a gastroenterologist from New York, wrote that “if elected, Mr. Trump, I can state unequivocally, will be the healthiest individual ever elected to the presidency.”
The doctor later admitted that Mr. Trump dictated the line, adding “I just made it up as I went along.”
‘You want to be reassured’
In a New York Times/Siena College poll of six battleground states last fall, 70 percent of voters said Mr. Biden was too old to be president. Less than half of voters expressed similar misgivings about Mr. Trump, though his critics say his disregard for facts and word-salad speeches prove that he is unfit to hold office again.
Doctors have expressed deep skepticism about relying only on information provided by candidates’ personal physicians for information about their health.
“There is a public need to know about the physical and mental fitness of anybody who’s going to go into the highest office in the country,” said Dr. Joe Verghese, a professor of neurology and medicine and the director of the Resnick Gerontology Center at the Albert Einstein College of Medicine.
“You want to be reassured that steps have been taken to ensure that the person you’re electing into office will have the physical and mental capability,” he said.
There are no legal requirements to release health information, and candidates often invoke the same desire for personal privacy at the heart of protections against the release of medical records for all Americans.
Mr. McCain’s political advisers in 2008 considered his disclosures vital to dealing with voter concerns about his age and the potential for illness in office.
Barack Obama, who was 47 when he defeated Mr. McCain, released a one-page letter from his doctor during the 2008 campaign, but later offered supporting lab tests and electrocardiograms .
In 1988, both Michael S. Dukakis, the Democratic candidate, and George Bush, the Republican, gave interviews about their health and allowed reporters to talk directly to their doctors. After Mr. Bush took office, his physician continued to give interviews, and a panel of doctors held a news conference to talk about his health challenges and treatments.
Bill Clinton resisted releasing his records in 1992 and again during his re-election in 1996, even after his opponent, Bob Dole, released detailed health information and allowed his personal physician to be questioned by reporters. George W. Bush and his doctor gave interviews about his health during the 2000 campaign, and the younger Mr. Bush’s doctor answered reporters’ questions in 2002 after the president choked on a pretzel .
Neither Mr. Biden nor Mr. Trump has acknowledged making any accommodations because of his age.
For both men, doctors say, caution is medically warranted: Old people are more frail than younger ones. Last week, former Senator Joseph I. Lieberman of Connecticut died from complications of a fall at 82.
“Falls are one of the biggest killers of older Americans,” said Dr. Zaldy Tan, a professor of neurology and director of the memory and aging program at Cedars-Sinai Health System.
Mr. Biden and Mr. Trump now face seven months of a grueling campaign. Early in her political career, Vice President Kamala Harris compared being on the trail to the rigors of being a lawyer during an extended trial.
“It requires adrenaline and stamina; it requires being in shape mentally and emotionally,” she said. “It’s a marathon.”
Read by Michael D. Shear
Audio produced by Adrienne Hurst .
An earlier version of this article misstated when Kamala Harris described the rigors of campaigning. She made the comments early in her political career in California, not during the 2020 campaign.
How we handle corrections
Michael D. Shear is a White House correspondent for The New York Times, covering President Biden and his administration. He has reported on politics for more than 30 years. More about Michael D. Shear
Our Coverage of the 2024 Presidential Election
News and Analysis
Former President Donald Trump said that abortion rights should be left up to the states , remarks that came after months of mixed signals on the issue.
With his clearest statement yet on the future of abortion rights since the fall of Roe v. Wade, Trump laid bare how faulty a messenger he had always been for the anti-abortion cause .
President Biden released details of his new student loan debt forgiveness plan for nearly 30 million borrowers. Here is what to know about the proposal , which will have to withstand expected legal challenges.
Protests over the Biden administration’s handling of the war in Gaza are disrupting the activities of Democratic officials, complicating their ability to campaign during a pivotal election year .
For all Trump’s populist rhetoric in 2016, his presidency proved to be business-friendly. But Trump and those around him are signaling that a second term would be different .
It’s usually a given that Republicans will win voters 65 and over, but that’s not the case in this election. Nate Cohn, our chief political analyst, explains Biden’s strength among seniors .
In Chicago, restaurants and venues are booking fast for the Democratic National Convention in August. But Milwaukee, host of the Republican National Convention in July, is wondering if customers will come .
Advertisement
- Newsletters
- Account Activating this button will toggle the display of additional content Account Sign out
There Are Two Sides to the Debate on Health Care for Trans Kids. Here’s What You’re Missing About One of Them.
Here are some things we know about gender-affirming health care: We know that the number of young patients being seen by gender clinics has increased , and that the gender balance of these young patients has changed, with more female-assigned youth seeking care. (We don’t see the same gender imbalance outside of clinics, where young people identify as trans in roughly equal numbers regardless of birth-assigned sex.) We also know that autism is more common in trans youth than in the broader population.
We don’t know why these things are true. Nonetheless, these facts have helped spur a wave of coverage and concern around gender-affirming health care for young people experiencing gender dysphoria. This concern presents itself on the front page of the New York Times , in New York magazine , in the account of a woman who used to work at a gender clinic. At the heart of this concern—among good-faith debaters, those who are not merely trying to ban access for all trans people—is the idea that young people today who are identifying as trans may grow out of it, and come to deeply regret treatments like cross-sex hormones or surgeries. (It’s worth saying upfront that only a minority of young people who experience gender dysphoria are even receiving these treatments.)
We know that research on gender-affirming care for tweens and teens has shown generally positive results, and that side effects are usually mild (and that medical treatments always pose trade-offs). We know that accessing gender-affirming care can be extremely difficult. But it’s true that we don’t know how teens who are treated today with, say, puberty blockers will feel about that treatment 50 years from now.
There are—speaking extremely broadly—two things to do about the unknowns in gender-affirming care, and the expanding, and underserved, patient population. We could work to increase access and reduce barriers, to help patients have access to a promising treatment. We could do this with the understanding that medical choices always involve a highly personal calculus of benefit versus downsides and risks. Or, we could react to the increase in patients seeking treatment with broad-brush skepticism, positing that the new patients won’t necessarily benefit the way previous, but much smaller, cohorts have. We can make minimizing any chance of regret in pursuing gender-affirming medicine and procedures the centerpiece of our policies. The first side wants to reduce standardized gatekeeping around procedures, leaving the matter of the right age at which to, say, undergo top surgery up to the doctor, parents, and teen. Guidance in this case looks like providing doctors with some general things to consider, such as how long the teen has identified as another gender, how much distress they’re experiencing, and whether there are other mental health concerns. The second side worries that allowing access to top surgery for young people at all is reckless, and could lead to regret.
Advocates for the first approach believe increased visibility and acceptance of trans people is leading more young people to feel comfortable coming out as trans. They point to the rapid increase in left-handedness as social stigma waned as a precedent for this, and the increase in the number of people willing to openly identify as lesbian, gay, or bi in recent years. They note that tightly controlling care with an eye toward minimizing any possible regret would entail accepting serious harm to trans youth who need that care .
Advocates for the second approach believe many of the new patients may be falsely and temporarily believing themselves to have gender dysphoria due to the influence of transgender peers, either in person or on social media. This idea, which holds that the new patients are suffering from a “social contagion,” is related to the phenomenon of cultural concepts of distress , where mental illness may be mediated through culture and result in symptoms specific to the environment a person finds themself in. They point to the higher incidence of eating disorders in the West, or the fact that suicide is more common in some cultures than others, as precedents.
As a trans man and a journalist who has spent years covering these issues, it makes more sense to me to remain in the first camp until evidence has been provided to back up the second. If you find yourself at all in the second—perhaps unwittingly!—I hope you’ll consider my thinking on this. I think it is all too easy to dismiss people advocating for more care as warm, fuzzy activists, and not careful people who have evaluated the evidence, the risks, and the unknowns, and decided that more care is the best-informed course of action at this time.
Much of the recent coverage of gender-affirming care has focused on laying out the criticisms of the status quo (doctors seeking to provide gender-affirming care) that are being made by proponents of the social contagion idea (commentators, and even some providers, who worry that gender-affirming care is being provided to people who do not need it, and may in fact be harmed by it). Gender-affirming care is portrayed as something incredibly easy to access, with doctors giving it out quickly and with little discretion. An extreme version of this can be found in the caricature provided by former gender clinic worker Jamie Reed. “The center’s working assumption was that the earlier you treat kids with gender dysphoria, the more anguish you can prevent later on,” Reed writes. She claims that doctors were pushing parents and children into treatments after only two or three visits, without giving patients and families adequate information, and regardless of any other mental health concerns. Something similar can be found in an article for the New York Times about teens who are accessing top surgery (by all accounts still an exceedingly rare practice), which described a doctor who has performed some surgeries on minors as “proudly flouting professional mores in favor of connecting with hundreds of thousands of followers.” In an interview with Reuters , a Dutch psychiatrist who is in favor of more stringent assessments frames the dilemma as being whether to abide by the “the do-not-harm principle of medical intervention” or whether to privilege “the transgender right or child’s right.”
Many people who specialize in gender-affirming care do feel great love for the trans community, and for transgender kids. Given the stigma and hardship that come with being trans, adults in a trans child’s life often try to mitigate the cruelty of the outside world by showing them kindness and approval rather than skepticism. But showing empathy and care for vulnerable children doesn’t mean that professionals who work with trans youth are in a hurry to suggest medical treatments, ignore co-occurring mental health concerns, or fail to stay abreast of the most recent research. Rather than cheerleaders, these are professionals who have looked at the evidence and come to a different conclusion than proponents of the social contagion idea—the conclusion that kids are accurate reporters of their trans and nonbinary identities. This is an empirical idea that has so far been borne out by data, and may, like all scientific ideas, be disproven with yet more data.
In medicine, you have to take the best available evidence and make decisions with it. Doctors are doing that by administering treatment after careful evaluations and discussions of side effects, on timelines that are tailored to the patient’s particular case. Reed’s allegations have been directly contradicted in multiple local news outlets by parents, patients, and former co-workers at the clinic where she worked, who describe a slow, methodical process. A child who walked in at age 12 asking for hormones and surgery was told to “give it time”; he went to nearly 100 appointments with a therapist, and his dad dove into the medical literature and generally came around the idea of gender-affirming care.
But consider that it also could have made medical sense for a child to be offered medical interventions much sooner than that. For some parents whose children have already been socially transitioned for many years, the months of waiting and dozens of appointments feel excessive for their particular child’s needs, especially if they’ve only sought treatment because puberty has commenced. Reducing some of these requirements, particularly for patients whose identity has been stable for years before they first see a doctor, is an example of what the reduced-gatekeeping side hopes to see.
Caution and circumspection are warranted with any kind of ongoing medical intervention, particularly when it involves kids. But the research on gender-affirming care provides ample reason to believe that most kids who present with gender dysphoria in a clinical setting will become trans adults , and that puberty blockers and hormones are helpful for these youth. Many of the studies are small, and the positive effects tend to be weak, but the overall evidence isn’t dissimilar to that for other much less controversial medical interventions, including every known treatment for obesity in youth . This is due to well-known practical barriers to studying kids. More research is still needed, but as studies have come in in drips and drops, the picture has pointed toward the stability of kids’ identities and the benefits from early intervention, and away from there being reason to deny care. This has led many in the field to shift their focus away from exploring whether the treatments work and toward reducing barriers to ensure that kids who need them can access these meds.
“We have to be really thoughtful about the structural barriers that we are creating ourselves as providers,” Dr. Gina Sequeira, a co-director of the Seattle Children’s Gender Clinic, told Sabrina Imbler for a 2021 New York Times story on barriers faced by trans youth. (Unlike a recent wave of stories that have garnered criticism, this one didn’t make the front page.) “The majority of the kids I see have already overcome many, many barriers.”
In addition to those studies, there’s some circumstantial support for the idea that more—not fewer—young people would benefit from gender-affirming care. The New York Times has reported that about 1.4 percent of 13- to 17-year-olds in America say they’re transgender. The number of patients who are currently being treated medically for gender dysphoria remains quite small. Reporting by Reuters produced the best estimate yet , using a comprehensive look at insurance claims. They found 121,882 youth had been diagnosed with gender dysphoria between 2017 and 2021, and 17,683 (or about 14.5 percent of those diagnosed) had been given prescriptions for puberty blockers or hormones during that time. (This is likely to be a slight undercount because some families may pay for treatment out of pocket.)
Adults identify as transgender at a rate of 0.5 percent. Taking the more conservative figure—assuming that the entire increase in trans youth is due to a social contagion and there are no adults suppressing their identities due to widespread stigma and shame—we’d expect 130,000 American youth, 0.5 percent of those between 12 and 17, to grow up to be transgender adults.
While every adult who identifies as trans does not pursue medical transition, most do, and very, very few regret it . According to the United States Transgender Survey, a large, wide-ranging survey of trans adults conducted in 2015 , 84 percent of respondents said they were either currently living as a different gender than the one on their birth certificate, or wanted to do so. Seventy-eight percent said they wanted hormone therapy (though only 49 percent said they’d received it). It’s therefore downright conservative to believe that somewhere between 65,000 and 100,000 young people between the ages of 12 and 17 would benefit from transitioning young. It’s also entirely plausible to imagine a number significantly higher than that, if you think trans identities are more common among youth because of reduced stigma, not social contagion effects.
Either way, the youth who are receiving hormones and blockers now represent only a fraction of the adult trans population seeking medical care for gender dysphoria. In the absence of more data on long-term regret rates for this particular cohort of trans youth, it’s entirely reasonable to make the empirical argument that the numbers support helping more kids get treatment by cutting down wait times and barriers whenever possible.
The debate around trans youth—when it happens in good faith—isn’t, at its core, about whether to believe trans youth because it’s the kind thing to do. It’s about whether believing trans youth will lead to better outcomes for more patients, or not. The side wanting to reduce gatekeeping is supported by at least as much evidence, if not more, than the side that has predicted that a coming wave of detransitions due to insufficient gatekeeping has been just over the horizon for many years now , and has yet to materialize in any actual results.
The independent source for health policy research, polling, and news.
Dying Broke: A New Jointly Reported Series on America’s Long-Term Care Crisis from KFF Health News and The New York Times
Series examines the ways in which the financial and emotional toll of providing and paying for long-term care are wreaking havoc on the lives of millions of americans..
Nov 14, 2023
- Tammie Smith
Today, KFF Health News and The New York Times published the first phase of an investigation into America’s long-term care crisis, which has left many in the boomer generation facing the prospect of exhausting their financial resources as the price tag for care explodes. Dying Broke , the investigative series, uses KFF polling, original analysis and interviews with experts and impacted individuals and their families to examine the challenges facing families and caregivers in navigating long-term care.
The financial and emotional toll of providing and paying for long-term care is wreaking havoc on the lives of millions of Americans. Paid care, either at home or in a facility, is often so expensive that only the wealthy can afford it, and many of the for-profit companies providing care raised their prices sharply during the pandemic. The ongoing shortage of health care workers is also worsening the situation.
The project found that nearly three million older Americans who need long-term help are not receiving it, in large part because of the high costs of assisted living facilities, nursing homes and aides at home. The United States spends less on long-term care than do most wealthy countries. As part of this project, KFF conducted polling to help shed light on the U.S. public’s awareness of, attitudes about and experiences with long-term care services and supports.
The series tells the stories of some of the many people who must drain their lifetime savings to pay for care as well as the stories of the spouses and children, particularly daughters, who must make tremendous sacrifices to provide care. The first articles appear today on kffhealthnews.org and nytimes.com .
“There’s a reason this topic is a staple of so many family Thanksgiving dinner conversations,” said Jordan Rau, a senior correspondent at KFF Health News. “The kinds of no-win choices facing the people and their families we profile in these articles are ones that can happen to anyone—and too often do.”
“In interviewing many families with aging relatives, I was struck by how woefully unaware people are of how much long-term care can cost,” said Reed Abelson, health care reporter at The New York Times. “Many are amazingly resilient in finding ways to get care for their loved ones, but the lack of available help means people are often making tremendous sacrifices, both financially and emotionally, to provide support.”
The series includes reporting from Jordan Rau, senior correspondent at KFF Health News; Reed Abelson, health care reporter at The New York Times and JoNel Aleccia, formerly at KFF Health News. Holly K. Hacker, KFF Health News’ data editor, and Albert Sun, a graphics editor at The New York Times, conducted data analysis.
About The New York Times The New York Times Company is a trusted source of quality, independent journalism whose mission is to seek the truth and help people understand the world. With more than 10 million subscribers across a diverse array of print and digital products — from news to cooking to games to sports — The Times has evolved from a local and regional news leader into a diversified media company with curious readers, listeners and viewers around the globe. Follow news about the company at NYTCo.com .
About KFF and KFF Health News KFF Health News is an award-winning news service with a national newsroom in Washington, D.C., and a rapidly growing network of regional bureaus in California, the Midwest, the Mountain States, and the South. It is the independent source for health policy research, polling, and journalism, with a mission to serve as a nonpartisan source of information for policymakers, the media, the health policy community, and the public. KFF Health News is one of four core programs at KFF and an important contributor to the field of journalism.
KFF Health News works with many editorial partners, and media outlets can publish its stories at no charge. KFF Health News also publishes stories on kffhealthnews.org and promotes them through its social media platforms. KFF Health News journalists are available for interviews about their stories. News organizations interested in working with KFF Health News should contact the news service at [email protected] , and those interested in helping to expand and improve health journalism around the country should contact KFF at [email protected] .
About KFF’s Polling The survey, The Affordability of Long-term Care and Support Services , was designed and analyzed by public opinion researchers at KFF. Conducted May 5 -14, 2022 online and by telephone, the survey includes a nationally representative sample of 1,573 U.S. adults (1,502 in English and 71 in Spanish). The margin of sampling error – including the design effect for the full sample – is plus or minus 3 percentage points. For results based on other subgroups, the margin of sampling error may be higher.
- Health Costs
- KFF Health News
- Nursing Facilities
- Long-Term Care
The Coming Collapse of the U.S. Health Care System
I t’s four in the morning and you awaken with crushing chest pain. Your family calls 911 and paramedics arrive and diagnose a cardiac event. They inform you that they need to transport you forty-five minutes away because your two local hospitals have closed over the last several months. Even when you arrive at the hospital, there is massive overcrowding and they inform you that there are no ICU beds open for you in that fifty percent of the beds in the cardiac unit are “browned out” due to lack of staff. This nightmare is an all too familiar post pandemic reality about the delivery of health care in our country. This is not the expectation that the public expects in the delivery of health care in one of the richest nations in the world that has been at the cutting edge of health care innovation of the last century.
What has led to this post-pandemic nightmare is multifactorial. The pandemic changed how health care professionals are both valued and how they see themselves. During the height of the pandemic they were heroes that were endangering their lives to help the community. But now things look different.
Around 7,000 nurses on strike in New York City nursing strike is emblematic of the dire situation. Nurses, who are essential to the critical functioning of all hospitals, are entitled not only to more equitable compensation and benefits, but ultimately safer staffing ratios in all patient care settings. What’s ironic is that the strike will force these very health care systems to replace employed nurses with temporary nurses from staffing agencies, further compounding their financial woes, and ultimately, their bottom lines. Until we invest in people and their value in healthcare, we won’t be able to see light at the end of the tunnel.
Everyday we read about hospitals throughout the country losing millions if not billions of dollars per year. Hospitals are closing urgent care centers, obstetric, pediatric and other services to try to survive. One of the major factors that has triggered this crisis is the lack of staff. Post-pandemic hospital staffing has massively decreased with a rise in temporary locum staffing dependency. Hospitals and clinicians no longer have regular staff that can build professional and patient relationships; instead, they are dependent on locum staff with short term contracts to provide such services. Those locum providers are at all levels of the professional ladder from physicians, mid-level providers, nurse, respiratory therapists, and radiology technologists. This staffing model has led to many issues both professionally and financially.
On the professional level this massive shortfall of staff and dependency on temporary staff has created a critical issue in the realm of patient care. Hospitals and clinics have shut down services in all vital patient services. It is not uncommon to hear that health care systems have shut down Pediatrics, Psychiatry, Obstetrics, and ICU. Other healthcare systems have gone to the point of closing down entire hospitals because of staffing issues. Another important factor is the crisis is that outpatient services have reduced hours and days. It is obvious that this reduction of services has greatly affected access to health care. Individuals have lost the ability to get timely appointments, x-rays, and tests. In many communities, it is the underserved that have payed the greatest price in terms of getting timely care.
Hospitals have had to also close down operating rooms due to staffing thus delaying both elective and emergent services. Critically ill patients boarded in the emergency department have also spent long hours or days waiting for inpatient beds due to lack of trained staff even when beds become available. Even when they may be ready for hospital discharge patients have long waits to find rehab and skilled nursing facilities because they have also been affected by short staffing. This inability to transfer patients to appropriate facilities only adds to the short fall of inpatient beds.
During the pandemic, it was not uncommon for older providers with health issues to retire than to go into work. Individuals that did go to work worked long hours and had increased levels of stress. Post pandemic, many of these individuals were not financially rewarded: they saw COVID-19 relief money go to upgrade facilities, build new buildings, and other non-employee rewards. This obviously changed the relationship between the bedside providers and hospital leadership.
Adding to this breakdown for many were the city and state vaccine mandates. Many believed that they had worked hard with limited resources and experience against COVID-19 and now the appreciation is losing your job over your own ability to make health care decisions. Another major issue is the shortfall of individuals who wish to be health care providers. Many individuals and families observed how hard healthcare workers were required to work and to work while other professions and jobs could work from home.
One of the most important aspects in the shift was the introduction of massive numbers of temporary workers during the pandemic which continues today. Temporary workers (typically known as Locums) are a major contribution to staffing issues. As regular hospital staff learn about the financial rewards that locum providers receive, it only leads to more individuals questioning, “why do I still work here?”
Locum providers may be receiving two to three times the hourly rate of pay, and in some cases, free housing, rental cars and meal allowances. This is not a good model for worker satisfaction where an individual works through the pandemic with all its stress and is now training an individual who will make many folds their salary with additional perks who has no loyalty to the facilities. In some areas of the country locum health workers may be from the hospital down the street. Employees from hospital A go to hospital B then hospital C without having to travel.
Also integral to this discussion is the high pre-pandemic levels of burnout and attrition among providers that further devastated the supply of available healthcare providers leading into the pandemic. Addressing this issue is integral for the ongoing supply of providers throughout the U.S.
The widespread use of locums also affects the way and quality of the care provided. In the complex environment of health care delivery over the last few decades, we have learned that the best care is provided by individuals who work as teams caring for specific issues or problems. Prime examples of this are operating rooms and ICUs. Here, providers know the individual expertise and skills of each provider and protocols and guidelines needed to care for specific conditions. You can easily see how this would generate the best care. With short term locum providers, use of this system collapses into a world where individuals do not know the guidelines, location of supplies, the needs of individual providers and what each individual brings to the table. What also suffers is the ability to run through simulations and learning scenarios because staff is temporary. Many of us will see a rise in complications and poor outcomes in the next few years because of the breakdown in the healthcare team.
The massive financial drain imposed by staff shortages and use of locums has led to many health care facilities reaching the point of financial instability. Daily reports of massive quarterly losses by both internationally known and local hospitals where billions of dollars are being lost in an industry which was already working on a slim margin will lead to many additional facility closures. This has affected not only rural hospitals with slim operating margins, but larger urban healthcare facilities as well. The loss of such important services in hospitals and associated outpatient facilities will impact care for our communities for future generations.
So, if all of the hospital and healthcare facility close, where will we get our care? The answer is bleak. If we are hit with another pandemic where will the care be delivered, where will the beds be? This critical financial issue is also going to affect other industries. Medical technology companies cannot sell cutting edge ventilators, monitors and imaging devices to facilities that have no cash flow. Aging medical infrastructure cannot be repaired, upgraded or replaced in this financial environment.
As a backdrop to this evolving crisis, we wonder why is this not a major news story. Why are our local and national leaders not addressing these issues?
More Must-Reads From TIME
- Exclusive: Google Workers Revolt Over $1.2 Billion Contract With Israel
- Stop Looking for Your Forever Home
- Jane Fonda Champions Climate Action for Every Generation
- Hormonal Birth Control Doesn’t Deserve Its Bad Reputation
- The Sympathizer Counters 50 Years of Hollywood Vietnam War Narratives
- Essay: The Relentless Cost of Chronic Diseases
- The Best TV Shows to Watch on Peacock
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]
You May Also Like
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
News: For a Healthier 2021, Keep the Best... (The New York Times) - Behind the headlines
In the news.
Media coverage of health and science topics
Jan. 1, 2021
For a Healthier 2021, Keep the Best Habits of a Very Bad Year (Published 2021)
Our 7-Day Well Challenge will show you how to build on the healthy habits you learned during pandemic life.

Behind the headlines
Research findings and data from the National Library of Medicine
PubMed articles
Does gratitude writing improve the mental health of psychotherapy clients evidence from a randomized controlled trial.
Although the past decade has witnessed growing research interest in positive psychological interventions (PPIs), their potential as adjunctive interventions for psychothe …
Related content
Similar articles, people also viewed, also of interest.
Additional recent and related news
How to Write a Gratitude Letter (Published 2021)
Concerned about a friend or a loved one who may be feeling the winter doldrums? Try writing them a gratitude letter.
You Should Actually Send That Thank You Note You’ve Been Meaning to Write (Published 2018)
New research showed the recipients of an emailed expression of gratitude felt much more “ecstatic” than writers expected.
How to Build Healthy Habits (Published 2020)
It’s not about willpower. Good habits happen when we set ourselves up for success. Our new challenge will show you how.
Reduce stress and boost happiness with 4 daily gratitude practices
Practicing gratitude regularly offers many health benefits that can help you de-stress and boost your happiness year-round. Here are four easy-to-follow daily gratitude practices, all backed by science.
These Recharge Rooms Are Helping Health Care Workers Cope
Using voice-activation tech and nature-inspired soundscapes, these space are designed to give medical workers some respite from the Covid-19 front lines.
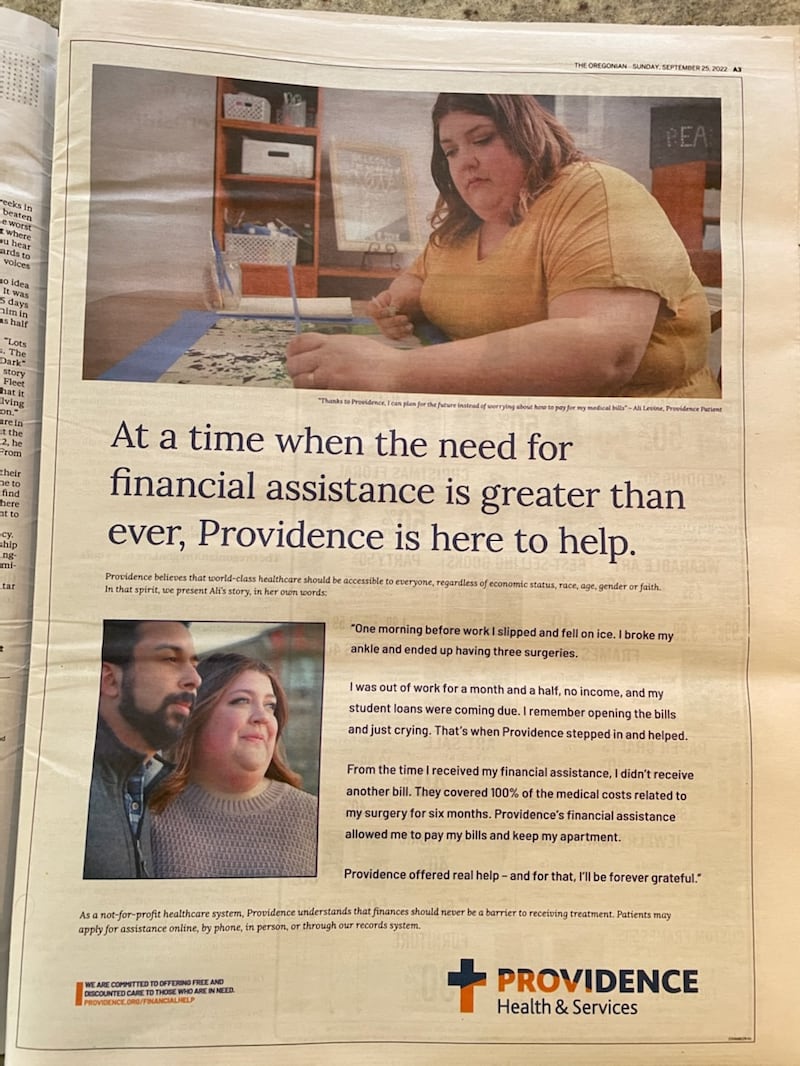
A New York Times Investigation Examines Providence’s Aggressive Financial Practices
Oregon’s largest health care provider provides less charity care than average and targeted low-income patients, the times found. providence disagrees..

The New York Times put the financial practices of Oregon’s largest hospital system, Providence Health, under the microscope on page A1 today. What the paper found isn’t pretty.
The Times drew on a lawsuit in Washington state and interviews throughout the Providence system, which includes 51 hospitals and 900 clinics across the West and Texas. (Providence operates six hospitals in Oregon.)
Among the findings, Providence, a nonprofit exempt from tax on profits, paid the consulting firm McKinsey & Co. $45 million for advice on how to increase revenues, through a program called “Rev-Up.”
Providence aggressively pursued payment from Medicaid patients in Oregon, Washington and California, the Times found, seemingly in violation of laws that say hospitals must accept government reimbursement for the patients whose low incomes qualify them for Medicaid and not pursue additional charges.
In return for tax-exempt status, hospitals are supposed to provide a certain amount of free care for patients who cannot afford treatment. The Times found Providence’s efforts wanting:
“Providence is sitting on $10 billion that it invests, Wall Street-style, alongside top private equity firms. It even runs its own venture capital fund,” the paper found.
“In 2018, before the Rev-Up program kicked in, Providence spent 1.24 percent of its expenses on charity care, a standard way of measuring how much free care hospitals provide . That was below the average of 2 percent for nonprofit hospitals nationwide.”
Oregon hospitals are nearly all nonprofits, and critics have long questioned whether they provide enough charity care. That issue was the subject of a WW cover story in 2016. Lawmakers passed a bill in 2019 establishing minimum levels of charity care at Oregon hospitals.
Related: The Five Things Hospitals Don’t Want You to Know About Obamacare
Providence pushed back hard against the Times story, calling it “absurd” in an internal email sent to staff and issuing a lengthy statement in response.
“The notion that Providence intentionally takes advantage of those who are vulnerable could not be further from the truth of who we are,” the statement said, noting that the Providence system “provided $1.9 billion in community benefit in 2021. This includes $271 million in charity care and $1.2 billion in Medicaid losses.”
Providence acknowledged its charity care percentage has declined but said there’s a reason for that.
“With regard to a decline in charity care levels, it’s important to note that our Medicaid losses have simultaneously gone up,” Providence said. “This is because many people who would have previously qualified for charity care are now covered by Medicaid thanks to the Affordable Care Act.”
Providence also purchased a full page ad today in the front section of The Oregonian extolling its generosity.
Willamette Week’s reporting has concrete impacts that change laws, force action from civic leaders, and drive compromised politicians from public office. Support WW's journalism today.
- Sports Betting
- Sports Entertainment
- Sportsbooks
- Betting Apps
- North Carolina Betting
- Action Network
- Online Casinos
Masters 2024 predictions, picks: Best PGA long-shot bets at Augusta
- View Author Archive
- Get author RSS feed
Thanks for contacting us. We've received your submission.

Typically, it’s the big names that win the Masters .
Jon Rahm, Scottie Scheffler, Hideki Matsuyama, Dustin Johnson and Tiger Woods won the last five Green Jackets , so it’s been a while since we’ve seen a true shock-winner at Augusta.
Danny Willett in 2016 was surely a surprise, but he was bet down to 66/1 by Round 1, and Patrick Reed qualified when he took home the Green Jacket in 2011.
And while that was a long time ago, it was part of a stretch where we saw dark horses regularly win at Augusta.
Zach Johnson, Trevor Immelman and Angel Cabrera won in 2007, 2008 and 2009, respectively, and they had odds of longer than 100/1.
It would be a true stunner if a triple-digit long shot was able to upset this field , but Augusta National is a place where magical things can happen and it has been the year of the long shot in golf , so why not throw a couple of darts this week?

Best Masters long-shot bets
Sungjae im (125/1, caesars ).
It’s been a trying year for Sungjae Im and his 10-over showing at the Valspar Championship at the end of March seemed to be a rock-bottom moment for the 26-year-old.
And while it’s never fun to back a player in this kind of form, the formula changes a bit when you’re getting a player with Im’s ceiling at this price.
And it definitely becomes more palatable when you consider Im’s history at Augusta National.
The South Korean has played the Masters four times and has a runner-up, a T8 and a T16 finish in his account already.
Maybe this is the place where Sungjae gets back on track.
Sergio Garcia (150/1, FanDuel )
There’s always a surprising name or two at the top of the leaderboard at the business end of every Masters and I wouldn’t be shocked if Sergio Garcia ticks that box this year.
The Spaniard is coming off a runner-up finish at LIV Miami last week and is a former winner at Augusta, so you don’t need to do too much work to find the logic of a punt on Garcia at this price.

Nick Taylor (250/1, FanDuel )
Most folks want to back players with loads of experience at Augusta National, but Nick Taylor can be the exception at this price.
The Winnipeg native is a four-time winner on the PGA Tour and has shown an innate ability to keep himself calm in big moments.
Get the lowdown on the Best USA Sports Betting Sites and Apps
- Check out the best sports betting sites
- Download the best sports betting app
Taylor won as a triple-digit long shot at the Waste Management — another tournament with a monster field — in February and that was his second time he lifted a trophy after a playoff.
That bodes well in a tournament that usually comes down to holding your nerve in big situations.
Share this article:

The Business of Fashion
Agenda-setting intelligence, analysis and advice for the global fashion community.
News & Analysis
- Professional Exclusives
- The News in Brief
- Sustainability
- Direct-to-Consumer
- Global Markets
- Fashion Week
- Workplace & Talent
- Entrepreneurship
- Financial Markets
- Newsletters
- Case Studies
- Masterclasses
- Special Editions
- The State of Fashion
- Read Careers Advice
- BoF Professional
- BoF Careers
- BoF Insights
- Our Journalism
- Work With Us
- Read daily fashion news
- Download special reports
- Sign up for essential email briefings
- Follow topics of interest
- Receive event invitations
- Create job alerts
A New York Members Club for the Health Obsessed Expands to Geneva

Health-focused members club The Well has set sights on Geneva for its first location in Europe.
It’s part of an expansion drive for a company in a fast-growing sector. The wellness industry was worth $5.6 trillion in 2022, according to a report from the Global Wellness Institute, up from $4.93 trillion in 2019.
The location in Geneva is set to open in 2026 in a newly renovated hotel and will offer stand-alone memberships for those living and working in the Swiss city. It will span roughly 20,000 square feet overlooking Lake Geneva, with both indoor and outdoor swimming pools and a landscaped terrace. Prices have not been finalised.
“Geneva is our first stop in Europe, but we’re very quickly going to be in London and some other major European markets,” says co-founder Kane Sarhan, speaking exclusively with Bloomberg about the announcement.
ADVERTISEMENT
The brand started in New York in 2019 with a 13,000-square-foot, light-filled space that offers members and non-members such services as $85 vitamin B12 drips and $560 lifting facials. Monthly fees start at $355 and entail unlimited movement classes including yoga and strength training; complimentary cold plunges and infrared saunas; and dedicated spaces in which to socialise and work.
Each member is paired with a health coach who can work one-on-one to address such issues as nutrition, sleep and ways to handle stress and anxiety. The Well approach combines Western and Eastern medicine, with experts in sports medicine, ayurveda and acupuncture.
In 2020, the company pivoted from being a purely membership driven-model, adding real estate and hospitality partnerships as pandemic restrictions shut its flagship Manhattan space for more than a year.
“The pandemic really woke a lot of people up to how foundational health is. So while the whole world contracted, we were able to expand,” Sarhan says. Formerly the head of brand for Starwood Capital Group’s 1 Hotels, he says developer contacts from the real estate world started inquiring about partnerships in the branded residences sector.
“We just started getting calls from former colleagues, saying that people want wellness but don’t know how to execute it,” he says. Those discussions resulted in partnerships for branded residences such as one with Miami-based real estate developer Terra.
Beth McGroarty, director of research at the Global Wellness Institute, agrees that the pandemic turned a lot of people into homebodies, so more attention is being given to creating communities and homes with health spaces.
“The fastest-growing market in wellness is homes and communities designed around wellness, so the Well is slotting into this huge trend,” she says. “Wellness used to be all about travel, where you’d go somewhere for a week and then fall off the wagon the second you’d get home,” says McGroarty. “Now, with these clubs, you can have resort-style programming in your home city.”
Rebecca Parekh, the Well’s chief executive officer, and who previously headed cross-product sales at Deutsche Bank, says Geneva makes sense as an initial European destination: It’s an international business city in a nation with many health and wellness practitioners to staff the facility.
Fflur Roberts, global head of luxury goods at Euromonitor, says a lot of wealth is concentrated in Geneva, where the world’s richest fly in and out for work and pleasure. “By default, the Swiss generally also care deeply about health and well-being and, as a destination, it’s steeped in wellness,” Roberts says.
Sarhan says the Geneva location will include strong physical therapy programmes. “One of the things we learned when doing our research about Geneva is that February onward is called boot season, because everyone skis and gets injured,” he says. “So everyone’s walking around with broken leg boots. We’re doing research on new modalities like hyperbaric chambers and oxygen chambers so we can help people recover from injury.”
That focus is different from the one in New York, where most clients’ primary concern is coping with stress, says Parekh. “Our community in New York is pretty well versed in wellness,” she says. “But it’s the challenge of getting there. People societally are navigating immense amounts of pressure and they don’t know where to start — and that’s where our health coaches play a vital role.”
While the Well was a pioneer in socially driven wellness space when it opened in 2019, competition is growing.
“There are a lot of clubs opening, and many are positioned at higher-end consumers,” says McGroarty. “If you look at New York, there are so many wellness companies and clubs now, it’s astounding.”
Six blocks from The Well in New York stands Remedy Place , which offers its members hyperbaric oxygen chambers, vitamin drips and functional medicine consultations. Continuum is set to open soon in Greenwich Village; it says it will use artificial intelligence to better its members’ health, along with float tanks, acupuncture, Himalayan salt saunas and massage. Aman New York has a $200,000 membership component alongside its 25,000-square-foot spa, with a fully functional medical practice that has Ivy League-trained doctors on staff.
The Well, says McGroarty, is primarily a wellness social club with space for people to socialise, work on health goals and meet others amid what she calls a “loneliness epidemic” that followed the surge in working from home.
We are likely to see more such clubs opening in major financial capitals driven by an ageing population and health anxieties, says Roberts from Euromonitor.
“The age of most of the high-net-worth individuals in the world are the late 40s, 50s and upwards,” Roberts explains. “As they age, they’re realising they need to take their health more seriously.” She says the wellness trend — with its plush spas and membership clubs — is very attractive to this class of consumer. “On the back of the pandemic, health has become our biggest asset.”
Co-founder Sarhan says The Well is focused on expansion both in the US and Europe. The company has 12 locations in the pipeline, adding up to a million square feet under development. Well Bay Harbor Islands in Miami is set to open next year as its first wellness club with branded residences and office space. Home prices start at $1.3 million, and more than half have been sold.
Two additional locations are planned for Miami. A second wellness club in Brickell has a 2026 planned opening date, and branded residences in Coconut Grove are set for 2027. The Well sees South Florida, with so many new residents, as a hot market.
The Well has also partnered with hotels and is currently working with boutique hotel favourites Auberge Resorts Collection to add wellness spaces to resorts in Costa Rica, Los Cabos in Mexico and the Mayflower Inn in Connecticut.
CEO Parekh says the company’s five years — and a global pandemic months after its doors opened — have shown people the importance of preventative health and wellness, sustaining the Well’s growth.
“I think a lot of people are rolling their eyes at wellness at times,” she says. “But it’s a very real need.”
By Sarah Rappaport
How ‘Anti-Spas’ Sell Wellness to Men
Remedy Place, a luxury social wellness club, has completely rebranded the spa experience with an eye on the male demographic. This year, the company has an ambitious plan to expand starting with its third and largest 7,400-square-foot club in New York’s SoHo neighbourhood this spring and an upcoming product line that brings self-care into the home.
The BoF Podcast: Inside the Business of Wellness
In the latest episode of Inside Fashion, co-founders of mindbodygreen Jason and Colleen Wachob discuss cutting-edge trends in health and wellbeing, how they intersect with fashion and bringing wellness into the workplace.
Why Beauty Brands Want a Bigger Piece of the $1.5 Trillion Wellness Pie
The State of Fashion: Beauty finds that brands have a growing opportunity to tap into emerging wellness subcategories — from sleep to sexual intimacy to ingestible beauty — by upgrading existing products or expanding portfolios, provided they do so with credibility and authenticity.
- Beauty : Wellness
© 2024 The Business of Fashion. All rights reserved. For more information read our Terms & Conditions

The Death of the Detox
Gen-Z aren’t into all-or-nothing health practices, or the hallmarks of wellness that have become cornerstones. What’s left is something far more subversive.

Op-Ed | Puig Is Betting We Haven’t Reached Peak Beauty
A cooling in the red-hot beauty market may be the company’s biggest threat to its initial public offering. It must put its best face — or fragrance — forward.

UK Ads Promoting Holiday ‘Butt Lifts’ in Potential Breach of Rules
Social media and reality TV shows such as Love Island have promoted an aesthetic that is fuelling medical tourism for hair transplants, Brazilian butt lifts and tummy tucks abroad.

Puig Aims to Raise €2.5 Billion in IPO
The family-owned premium beauty conglomerate has confirmed it will float shares on the Spanish stock exchange while retaining majority control, following months of speculation.
Subscribe to the BoF Daily Digest
The essential daily round-up of fashion news, analysis, and breaking news alerts.
Our newsletters may include 3rd-party advertising, by subscribing you agree to the Terms and Conditions & Privacy Policy .
Our Products
- BoF Insights Opens in new window

Watch CBS News
Why is looking at a solar eclipse dangerous without special glasses? Eye doctors explain.
By Sara Moniuszko
Edited By Allison Elyse Gualtieri
Updated on: April 8, 2024 / 8:54 AM EDT / CBS News
The solar eclipse will be visible for millions of Americans on April 8, 2024, making many excited to see it — but how you watch it matters, since it can be dangerous for your eyes.
A solar eclipse occurs when the moon passes between the sun and Earth, blocking the sun's light . When the moon blocks some of the sun, it's a partial solar eclipse, but when moon lines up with the sun, blocking all of its light, a total solar eclipse occurs, NASA explains . Either way, you need eye protection when viewing.
"The solar eclipse will be beautiful, so I hope that everyone experiences it — but they need to experience it in the right way," said Dr. Jason P. Brinton, an ophthalmologist and medical director at Brinton Vision in St. Louis.
Here's what to know to stay safe.
Why is looking at a solar eclipse dangerous?
Looking at the sun — even when it's partially covered like during an eclipse — can cause eye damage.
There is no safe dose of solar ultraviolet rays or infrared radiation, said Dr. Yehia Hashad , an ophthalmologist, retinal specialist and the chief medical officer at eye health company Bausch + Lomb.
"A very small dose could cause harm to some people," he said. "That's why we say the partial eclipse could also be damaging. And that's why we protect our eyes with the partial as well as with the full sun."
Some say that during a total eclipse, it's safe to view the brief period time when the moon completely blocks the sun without eye protection. But experts warn against it.
"Totality of the eclipse lasts only about 1 to 3 minutes based on geographic location, and bright sunlight suddenly can appear as the moon continues to move," notes an eclipse viewing guide published in JAMA , adding, "even a few seconds of viewing the sun during an eclipse" can temporarily or permanently damage your vision.
Do I need special glasses for eclipse viewing?
Yes. Eclipse glasses are needed to protect your eyes if you want to look at the eclipse.
Regular sunglasses aren't protective enough for eclipse viewing — even if you stack more than one.
"There's no amount of sunglasses that people can put on that will make up for the filtering that the ISO standard filters and the eclipse glasses provide," Brinton said.
You also shouldn't look at the eclipse through a camera lens, phone, binoculars or telescope, according to NASA, even while wearing eclipse glasses. The solar rays can burn through the lens and cause serious eye injury.
Eclipse glasses must comply with the ISO 12312-2 international safety standard , according to NASA, and should have an "ISO" label printed on them to show they comply. The American Astronomical Society has a list of approved solar viewers.
Can't find these, or they're sold out near you? You can also make homemade viewers , which allow you to observe the eclipse indirectly — just don't accidentally look at the sun while using one.
How to keep kids safe during the solar eclipse
Since this eclipse is expected to occur around the time of dismissal for many schools across the country, it may be tempting for students to view it without the proper safety precautions while getting to and from their buses. That's why some school districts are canceling classes early so kids can enjoy the event safely with their families.
Dr. Avnish Deobhakta, vitreoretinal surgeon at New York Eye and Ear Infirmary at Mount Sinai, said parents should also be careful because it can be difficult for children to listen or keep solar eclipse glasses on.
"You want to actually, in my opinion, kind of avoid them even looking at the eclipse, if possible," he said. "Never look directly at the sun, always wear the right eclipse sunglasses if you are going to look at the sun and make sure that those are coming from a reliable source."
Brinton recommends everyone starts their eclipse "viewing" early, by looking at professional photos and videos of an eclipse online or visiting a local planetarium.
That way, you "have an idea of what to expect," he said.
He also recommends the foundation Prevent Blindness , which has resources for families about eclipse safety.
What happens if you look at a solar eclipse without eclipse glasses?
While your eyes likely won't hurt in the moment if you look at the eclipse without protection, due to lowered brightness and where damage occurs in the eye, beware: The rays can still cause damage .
The harm may not be apparent immediately. Sometimes trouble starts to appear one to a few days following the event. It could affect just one or both eyes.
And while some will regain normal visual function, sometimes the damage is permanent.
"Often there will be some recovery of the vision in the first few months after it, but sometimes there is no recovery and sometimes there's a degree to which it is permanent," Brinton said.
How long do you have to look at the eclipse to damage your eyes?
Any amount of time looking at the eclipse without protection is too long, experts say.
"If someone briefly looks at the eclipse, if it's extremely brief, in some cases there won't be damage. But damage can happen even within a fraction of a second in some cases," Brinton said. He said he's had patients who have suffered from solar retinopathy, the official name for the condition.
Deobhakta treated a patient who watched the 2017 solar eclipse for 20 seconds without proper eye protection. She now has permanent damage in the shape of a crescent that interferes with her vision.
"The crescent that is burned into the retina, the patient sees as black in her visual field," he said. "The visual deficit that she has will never go away."
How to know if you've damaged your eyes from looking at the eclipse
Signs and symptoms of eye damage following an eclipse viewing include headaches, blurred vision, dark spots, changes to how you see color, lines and shapes.
Unfortunately, there isn't a treatment for solar retinopathy.
"Seeing an eye care professional to solidify the diagnosis and for education I think is reasonable," Brinton said, but added, "right now there is nothing that we do for this. Just wait and give it time and the body does tend to heal up a measure of it."
Sara Moniuszko is a health and lifestyle reporter at CBSNews.com. Previously, she wrote for USA Today, where she was selected to help launch the newspaper's wellness vertical. She now covers breaking and trending news for CBS News' HealthWatch.
More from CBS News

Photos from total solar eclipse show awe as moon covers sun

Astrophotographer chases best images of Monday's total solar eclipse

Storms keep eclipse travelers on their toes as North Texas exodus begins

Group camps out early in North Texas for Monday's total solar eclipse
Taiwan's strongest earthquake in 25 years kills 9 people, 50 missing
- Medium Text
- Earthquake kills nine, more than 900 injured
- Fifty on minibuses heading to national park missing
- Epicentre just off Taiwan's sparsely populated east coast
- Workers return to semiconductor giant TSMC facilities

FIGHTER JETS

CHIP SUPPLIES

The Reuters Daily Briefing newsletter provides all the news you need to start your day. Sign up here.
Reporting by Yimou Lee and Fabian Hamacher, Shanghai and Hong Kong newsrooms; Writing by Ben Blanchard; Editing by Clarence Fernandez, Chizu Nomiyama, Alison Williams and Josie Kao
Our Standards: The Thomson Reuters Trust Principles. New Tab , opens new tab
Thomson Reuters
Yimou Lee is a Senior Correspondent for Reuters covering everything from Taiwan, including sensitive Taiwan-China relations, China's military aggression and Taiwan's key role as a global semiconductor powerhouse. A three-time SOPA award winner, his reporting from Hong Kong, China, Myanmar and Taiwan over the past decade includes Myanmar's crackdown on Rohingya Muslims, Hong Kong protests and Taiwan's battle against China's multifront campaigns to absorb the island.

World Chevron
Us coast guard says boardings of chinese fishing vessels in south pacific legal.
The U.S. Coast Guard has rejected comments by a Chinese diplomat that its recent boardings of Chinese fishing boats in the Pacific Islands alongside local police are illegal, saying the joint patrols are at the behest of Pacific nations to protect coastal fisheries.

When and where the solar eclipse will be crossing the U.S.
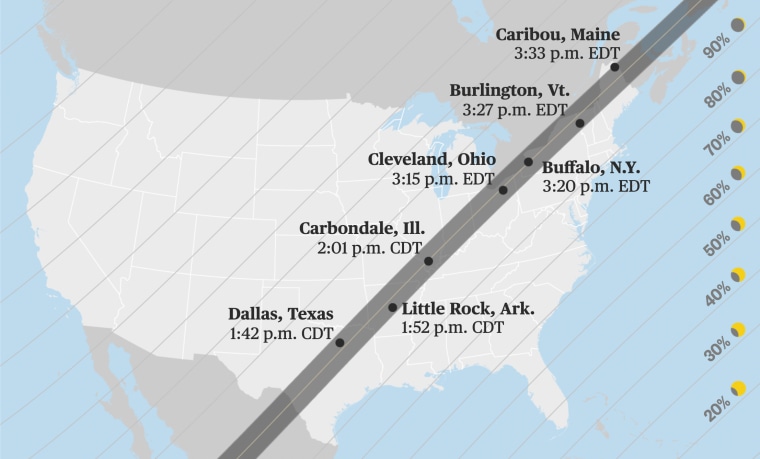
A total solar eclipse will grace the skies over North America on Monday, one of the most hotly anticipated sky-watching events in recent years.
Weather permitting , millions of people in Mexico, 15 U.S. states and eastern Canada will have the chance to see the moon slip between Earth and sun, temporarily blocking the sun’s light .
The total solar eclipse will be visible along a “path of totality” that measures more than 100 miles wide and extends across the continent. Along that path, the moon will fully obscure the sun, causing afternoon skies to darken for a few minutes.
Follow live updates on the solar eclipse
In all other parts of the continental U.S., a partial solar eclipse will be visible, with the moon appearing to take a bite out of the sun. Exactly how big a bite depends on the location.
The first spot in North America that will experience totality on Monday is on Mexico’s Pacific coast at around 11:07 a.m. PT, according to NASA .
After moving northeast across Mexico, the eclipse’s path travels through Texas, Oklahoma, Arkansas, Missouri, Illinois, Kentucky, Indiana, Ohio, Pennsylvania, New York, Vermont, New Hampshire and Maine. Slivers of Michigan and Tennessee will also be able to witness totality if conditions are clear.
In Canada, the eclipse will be visible in parts of southern Ontario, Quebec, New Brunswick, Prince Edward Island and Cape Breton, at the eastern end of Nova Scotia.
The timing of the eclipse and the duration of totality varies by location. Most places will experience around 2 minutes of darkness, but the longest periods of totality are typically in the center of the eclipse’s path.
This year, the longest stretch of totality will last 4 minutes and 28 seconds in an area northwest of Torreón, Mexico.

Below is a list of timings for some U.S. cities along the path of totality, according to NASA .
- Dallas: Partial eclipse begins at 12:23 p.m. CT and totality at 1:40 p.m. CT.
- Idabel, Oklahoma: Partial eclipse begins at 12:28 p.m. CT and totality at 1:45 p.m. CT.
- Little Rock, Arkansas: Partial eclipse begins at 12:33 p.m. CT and totality at 1:51 p.m. CT.
- Poplar Bluff, Missouri: Partial eclipse begins at 12:39 p.m. CT and totality at 1:56 p.m. CT.
- Paducah, Kentucky: Partial eclipse begins at 12:42 p.m. CT and totality at 2:00 p.m. CT.
- Carbondale, Illinois: Partial eclipse begins at 12:42 p.m. CT and totality at 1:59 p.m. CT.
- Evansville, Indiana: Partial eclipse begins at 12:45 p.m. CT and totality at 2:02 p.m. CT.
- Cleveland: Partial eclipse begins at 1:59 p.m. ET and totality at 3:13 p.m.
- Erie, Pennsylvania: Partial eclipse begins at 2:02 p.m. ET and totality at 3:16 p.m. ET.
- Buffalo, New York: Partial eclipse begins at 2:04 p.m. ET and totality at 3:18 p.m.
- Burlington, Vermont: Partial eclipse begins at 2:14 p.m. ET and totality at 3:26 p.m. ET.
- Lancaster, New Hampshire: Partial eclipse begins at 2:16 p.m. ET and totality at 3:27 p.m.
- Caribou, Maine: Partial eclipse begins at 2:22 p.m. ET and totality at 3:32 p.m. ET.
Other resources can also help you figure out when the various phases of the eclipse will be visible where you live, including NationalEclipse.com and TimeandDate.com .
If you plan to watch the celestial event, remember that it’s never safe to look directly at the sun, including through binoculars, telescopes or camera lenses. Special eclipse glasses are required to safely view solar eclipses and prevent permanent eye damage.
Denise Chow is a reporter for NBC News Science focused on general science and climate change.

IMAGES
COMMENTS
The latest news on health and medicine, covid, vaccines, global health, mental health, Obamacare, health insurance, Medicare, Medicaid, opioids, cancer, heart disease ...
A New York Times review of hundreds of health departments in all 50 states indicates that local public health across the country is less equipped to confront a pandemic now than it was at the ...
The New York Times also petitioned two federal courts for materials under seal. April 7, 2024 Weeks after undergoing heart surgery, Gail Lawson found herself back in an operating room.
Rachel Bujalski for The New York Times. Bird flu outbreaks among dairy cows in multiple states, and at least one infection in farmworker in Texas, have incited fears that the virus may be the next ...
The particular virus in these new cases, called H5N1, was first identified in 1996 in geese in China, and in people in Hong Kong in 1997. In 2020, a new, highly pathogenic form of H5N1 emerged in ...
April 7, 2024, 3:02 a.m. ET. Large health insurers are working with a little-known data company to boost their profits, often at the expense of patients and doctors, a New York Times investigation ...
By Aishvarya Kavi. Reporting from Washington. April 9, 2024, 3:35 p.m. ET. President Biden condemned a decision by Arizona's Supreme Court on Tuesday to uphold an 1864 ban on nearly all ...
A New York Times investigation of insurers' relationship with MultiPlan found that countering predatory billing is just one aspect of the collaboration. Low payments have burdened patients with ...
Open this article in the New York Times Audio app on iOS. Today, President Biden is 81 and his rival, Donald J. Trump, is 77, and many voters believe both men are too old for another term .
The New York Times Aug. 17, 2021 Racial Inequities Persist in Health Care Despite Expanded Insurance (Published 2021) by Roni Caryn Rabin. A series of studies in an influential medical journal takes a close look at longstanding gaps in medical care. Read more at The New York Times
The New York Times has reported that about 1.4 percent of 13- to 17-year-olds in America say they're transgender. The number of patients who are currently being treated medically for gender ...
Today, KFF Health News and The New York Times published the first phase of an investigation into America's long-term care crisis, which has left many in the boomer generation facing the prospect ...
The New York Times Feb. 17, 2021 'Nobody Has Openings': Mental Health Providers Struggle to Meet Demand (Published 2021) by Christina Caron. With anxiety and depression on the rise during the pandemic, it has been challenging for people to get the help they need. Read more at The New York Times
Health disparities in the COVID-19 pandemic. Research shows that minority groups are disproportionally impacted by this pandemic. According to the 2019 American Community Survey (ACS) (U.S. Census Bureau, 2020a), about 5.7 million residents live in NYC are minorities.For example, Black and Hispanic populations are about 1.5 times more likely to contract the virus, about 4 times more likely to ...
The nursing strike in New York is emblematic of the huge stresses the U.S. health care faces coming out of the pandemic ... Locum providers may be receiving two to three times the hourly rate of ...
The New York Times Jan. 1, 2021 For a Healthier 2021, Keep the Best Habits of a Very Bad Year (Published 2021) by Tara Parker-Pope. Our 7-Day Well Challenge will show you how to build on the healthy habits you learned during pandemic life. Read more at The New York Times
Ascension, a nonprofit health system that includes 139 hospitals in 19 states, yesterday published a detailed response to a New York Times article that examined staffing at the health system. "Ascension is deeply committed to providing a positive workplace culture for our nurses, as well as other clinicians and associates," the Ascension blog states.
September 25, 2022 at 12:33 pm PDT. The New York Times put the financial practices of Oregon's largest hospital system, Providence Health, under the microscope on page A1 today. What the paper ...
Jon Rahm, Scottie Scheffler, Hideki Matsuyama, Dustin Johnson and Tiger Woods won the last five Green Jackets, so it's been a while since we've seen a true shock-winner at Augusta. Danny ...
Health-focused members club The Well has set sights on Geneva for its first location in Europe. It's part of an expansion drive for a company in a fast-growing sector. The wellness industry was worth $5.6 trillion in 2022, according to a report from the Global Wellness Institute, up from $4.93 trillion in 2019.
Why looking directly at a solar eclipse is so dangerous for your eyes 01:41. The solar eclipse will be visible for millions of Americans on April 8, 2024, making many excited to see it — but how ...
Taiwan's biggest earthquake in at least 25 years killed nine people on Wednesday and injured more than 900, while 50 workers travelling in minibuses to a hotel in a national park were missing.
Lancaster, New Hampshire: Partial eclipse begins at 2:16 p.m. ET and totality at 3:27 p.m. Caribou, Maine: Partial eclipse begins at 2:22 p.m. ET and totality at 3:32 p.m. ET. Other resources can ...