

What does the scholarly research say about the effect of gender transition on transgender well-being?
We conducted a systematic literature review of all peer-reviewed articles published in English between 1991 and June 2017 that assess the effect of gender transition on transgender well-being. We identified 55 studies that consist of primary research on this topic, of which 51 (93%) found that gender transition improves the overall well-being of transgender people, while 4 (7%) report mixed or null findings. We found no studies concluding that gender transition causes overall harm. As an added resource, we separately include 17 additional studies that consist of literature reviews and practitioner guidelines.
Bottom Line
This search found a robust international consensus in the peer-reviewed literature that gender transition, including medical treatments such as hormone therapy and surgeries, improves the overall well-being of transgender individuals. The literature also indicates that greater availability of medical and social support for gender transition contributes to better quality of life for those who identify as transgender.
Below are the 8 findings of our review, and links to the 72 studies on which they are based. Click here to view our methodology . Click here for a printer-friendly one-pager of this research analysis .
Suggested Citation : What We Know Project, Cornell University, “What Does the Scholarly Research Say about the Effect of Gender Transition on Transgender Well-Being?” (online literature review), 2018.
Research Findings
1. The scholarly literature makes clear that gender transition is effective in treating gender dysphoria and can significantly improve the well-being of transgender individuals.
2. Among the positive outcomes of gender transition and related medical treatments for transgender individuals are improved quality of life, greater relationship satisfaction, higher self-esteem and confidence, and reductions in anxiety, depression, suicidality, and substance use.
3. The positive impact of gender transition on transgender well-being has grown considerably in recent years, as both surgical techniques and social support have improved.
4. Regrets following gender transition are extremely rare and have become even rarer as both surgical techniques and social support have improved. Pooling data from numerous studies demonstrates a regret rate ranging from .3 percent to 3.8 percent. Regrets are most likely to result from a lack of social support after transition or poor surgical outcomes using older techniques.
5. Factors that are predictive of success in the treatment of gender dysphoria include adequate preparation and mental health support prior to treatment, proper follow-up care from knowledgeable providers, consistent family and social support, and high-quality surgical outcomes (when surgery is involved).
6. Transgender individuals, particularly those who cannot access treatment for gender dysphoria or who encounter unsupportive social environments, are more likely than the general population to experience health challenges such as depression, anxiety, suicidality and minority stress. While gender transition can mitigate these challenges, the health and well-being of transgender people can be harmed by stigmatizing and discriminatory treatment.
7. An inherent limitation in the field of transgender health research is that it is difficult to conduct prospective studies or randomized control trials of treatments for gender dysphoria because of the individualized nature of treatment, the varying and unequal circumstances of population members, the small size of the known transgender population, and the ethical issues involved in withholding an effective treatment from those who need it.
8. Transgender outcomes research is still evolving and has been limited by the historical stigma against conducting research in this field. More research is needed to adequately characterize and address the needs of the transgender population.
Below are 51 studies that found that gender transition improves the well-being of transgender people. Click here to jump to 4 studies that contain mixed or null findings on the effect of gender transition on transgender well-being. Click here to jump to 17 studies that consist of literature reviews or guidelines that help advance knowledge about the effect of gender transition on transgender well-being.
Ainsworth and spiegel, 2010.

Ainsworth, T., & Spiegel, J. (2010). Quality of life of individuals with and without facial feminization surgery or gender reassignment surgery. Quality of Life Research , 19 (7), 1019-1024.
Objectives: To determine the self-reported quality of life of male-to-female (MTF) transgendered individuals and how this quality of life is influenced by facial feminization and gender reassignment surgery. Methods: Facial Feminization Surgery outcomes evaluation survey and the SF-36v2 quality of life survey were administered to male-to-female transgender individuals via the Internet and on paper. A total of 247 MTF participants were enrolled in the study. Results: Mental health-related quality of life was statistically diminished (P < 0.05) in transgendered women without surgical intervention compared to the general female population and transwomen who had gender reassignment surgery (GRS), facial feminization surgery (FFS), or both. There was no statistically significant difference in the mental health-related quality of life among transgendered women who had GRS, FFS, or both. Participants who had FFS scored statistically higher (P < 0.01) than those who did not in the FFS outcomes evaluation. Conclusions: Transwomen have diminished mental health-related quality of life compared with the general female population. However, surgical treatments (e.g. FFS, GRS, or both) are associated with improved mental health-related quality of life.
Bailey, Ellis, & McNeil, 2014

Bailey, L., Ellis, S. J., & McNeil, J. (2014). Suicide risk in the UK trans population and the role of gender transition in decreasing suicidal ideation and suicide attempt. The Mental Health Review , 19 (4), 209-220.
Purpose: The purpose of this paper is to present findings from the Trans Mental Health Study (McNeil et al., 2012) – the largest survey of the UK trans population to date and the first to explore trans mental health and well-being within a UK context. Findings around suicidal ideation and suicide attempt are presented and the impact of gender dysphoria, minority stress and medical delay, in particular, are highlighted. Design/methodology/approach: This represents a narrative analysis of qualitative sections of a survey that utilised both open and closed questions. The study drew on a non-random sample (n 1⁄4 889), obtained via a range of UK-based support organisations and services. Findings: The study revealed high rates of suicidal ideation (84 per cent lifetime prevalence) and attempted suicide (48 per cent lifetime prevalence) within this sample. A supportive environment for social transition and timely access to gender reassignment, for those who required it, emerged as key protective factors. Subsequently, gender dysphoria, confusion/denial about gender, fears around transitioning, gender reassignment treatment delays and refusals, and social stigma increased suicide risk within this sample. Research limitations/implications: Due to the limitations of undertaking research with this population, the research is not demographically representative. Practical implications: The study found that trans people are most at risk prior to social and/or medical transition and that, in many cases, trans people who require access to hormones and surgery can be left unsupported for dangerously long periods of time. The paper highlights the devastating impact that delaying or denying gender reassignment treatment can have and urges commissioners and practitioners to prioritise timely intervention and support. Originality/value: The first exploration of suicidal ideation and suicide attempt within the UK trans population revealing key findings pertaining to social and medical transition, crucial for policy makers, commissioners and practitioners working across gender identity services, mental health services and suicide prevention.
Bar et al., 2016

Bar, M. A., Jarus, T., Wada, M., Rechtman, L., & Noy, E. (2016). Male-to-female transitions: Implications for occupational performance, health, and life satisfaction. The Canadian Journal of Occupational Therapy , 83 (2), 72-82.
Background. People who undergo a gender transition process experience changes in different everyday occupations. These changes may impact their health and life satisfaction. Purpose. This study examined the difference in the occupational performance history scales (occupational identity, competence, and settings) between male-to-female transgender women and cisgender women and the relation of these scales to health and life satisfaction. Method. Twenty-two transgender women and 22 matched cisgender women completed a demographic questionnaire and three reliable measures in this cross-sectional study. Data were analyzed using a two-way analysis of variance and multiple linear regressions. Findings. The results indicate lower performance scores for the transgender women. In addition, occupational settings and group membership (transgender and cisgender groups) were found to be predictors of life satisfaction. Implications. The present study supports the role of occupational therapy in promoting occupational identity and competence of transgender women and giving special attention to their social and physical environment.
Bodlund and Kullgren, 1996

Bodlund, O., & Kullgren, G. (1996). Transsexualism–general outcome and prognostic factors: A five-year follow-up study of nineteen transsexuals in the process of changing sex. Archives of Sexual Behavior , 25 (3), 303-316.
Nineteen transsexuals, approved for sex reassignement, were followed-up after 5 years. Outcome was evaluated as changes in seven areas of social, psychological, and psychiatric functioning. At baseline the patients were evaluated according to axis I, II, V (DSM-III-R), SCID screen, SASB (Structural Analysis of Social Behavior), and DMT (Defense Mechanism Test). At follow-up all but 1 were treated with contrary sex hormones, 12 had completed sex reassignment surgery, and 3 females were waiting for phalloplasty. One male transsexual regretted the decision to change sex and had quit the process. Two transsexuals had still not had any surgery due to older age or ambivalence. Overall, 68% (n = 13) had improved in at least two areas of functioning. In 3 cases (16%) outcome were judged as unsatisfactory and one of those regarded sex change as a failure. Another 3 patients were mainly unchanged after 5 years. Female transsexuals had a slightly better outcome, especially concerning establishing and maintaining partnerships and improvement in socio-economic status compared to male transsexuals. Baseline factors associated with negative outcome (unchanged or worsened) were presence of a personality disorder and high number of fulfilled axis II criteria. SCID screen assessments had high prognostic power. Negative self-image, according to SASB, predicted a negative outcome, whereas DMT variables were not correlated to outcome.
Bouman et al., 2016

Bouman, W. P., Claes, L., Marshall, E., Pinner, G. T., Longworth, J., et al. (2016). Sociodemographic variables, clinical features, and the role of preassessment cross-sex hormones in older trans people. The Journal of Sexual Medicine , 13 (4), 711-719.
Introduction: As referrals to gender identity clinics have increased dramatically over the last few years, no studies focusing on older trans people seeking treatment are available. Aims: The aim of this study was to investigate the sociodemographic and clinical characteristics of older trans people attending a national service and to investigate the influence of cross-sex hormones (CHT) on psychopathology. Methods: Individuals over the age of 50 years old referred to a national gender identity clinic during a 30-month period were invited to complete a battery of questionnaires to measure psychopathology and clinical characteristics. Individuals on cross-sex hormones prior to the assessment were compared with those not on treatment for different variables measuring psychopathology. Main Outcome Measures: Sociodemographic and clinical variables and measures of depression and anxiety (Hospital Anxiety and Depression Scale), self-esteem (Rosenberg Self-Esteem Scale), victimization (Experiences of Transphobia Scale), social support (Multidimensional Scale of Perceived Social Support), interpersonal functioning (Inventory of Interpersonal Problems), and nonsuicidal self-injury (Self-Injury Questionnaire). Results: The sex ratio of trans females aged 50 years and older compared to trans males was 23.7:1. Trans males were removed for the analysis due to their small number (n = 3). Participants included 71 trans females over the age of 50, of whom the vast majority were white, employed or retired, and divorced and had children. Trans females on CHT who came out as trans and transitioned at an earlier age were significantly less anxious, reported higher levels of self-esteem, and presented with fewer socialization problems. When controlling for socialization problems, differences in levels of anxiety but not self-esteem remained. Conclusion: The use of cross-sex hormones prior to seeking treatment is widespread among older trans females and appears to be associated with psychological benefits. Existing barriers to access CHT for older trans people may need to be re-examined.
Boza and Nicholson, 2014

Boza, C., & Nicholson Perry, K. (2014). Gender-related victimization, perceived social support, and predictors of depression among transgender Australians. International Journal Of Transgenderism , 15 (1), 35-52.
This study examined mental health outcomes, gender-related victimization, perceived social support, and predictors of depression among 243 transgender Australians (n= 83 assigned female at birth, n= 160 assigned male at birth). Overall, 69% reported at least 1 instance of victimization, 59% endorsed depressive symptoms, and 44% reported a previous suicide attempt. Social support emerged as the most significant predictor of depressive symptoms (p>.05), whereby persons endorsing higher levels of overall perceived social support tended to endorse lower levels of depressive symptoms. Second to social support, persons who endorsed having had some form of gender affirmative surgery were significantly more likely to present with lower symptoms of depression. Contrary to expectations, victimization did not reach significance as an independent risk factor of depression (p=.053). The pervasiveness of victimization, depression, and attempted suicide represents a major health concern and highlights the need to facilitate culturally sensitive health care provision.
Budge et al., 2013

Budge, S. L., Katz-Wise, S. L., Tebbe, E. N., Howard, K. A. S., Schneider, C. L., et al. (2013). Transgender emotional and coping processes: Facilitative and avoidant coping throughout gender transitioning. The Counseling Psychologist , 41 (4), 601-647.
Eighteen transgender-identified individuals participated in semi-structured interviews regarding emotional and coping processes throughout their gender transition. The authors used grounded theory to conceptualize and analyze the data. There were three distinct phases through which the participants described emotional and coping experiences: (a) pretransition, (b) during the transition, and (c) posttransition. Five separate themes emerged, including descriptions of coping mechanisms, emotional hardship, lack of support, positive social support, and affirmative emotional experiences. The authors developed a model to describe the role of coping mechanisms and support experienced throughout the transition process. As participants continued through their transitions, emotional hardships lessened and they used facilitative coping mechanisms that in turn led to affirmative emotional experiences. The results of this study are indicative of the importance of guiding transgender individuals through facilitative coping experiences and providing social support throughout the transition process. Implications for counselors and for future research are discussed.
Cardoso da Silva et al., 2016

Cardoso da Silva, D., Schwarz, K., Fontanari, A.M.V., Costa, A.B., Massuda, R., et al. (2016). WHOQOL-100 Before and after sex reassignment surgery in Brazilian male-to-female transsexual individuals. Journal of Sexual Medicine , 13 (6), 988-993.
Introduction: The 100-item World Health Organization Quality of Life Assessment (WHOQOL-100) evaluates quality of life as a subjective and multidimensional construct. Currently, particularly in Brazil, there are controversies concerning quality of life after sex reassignment surgery (SRS). Aim: To assess the impact of surgical interventions on quality of life of 47 Brazilian male-to-female transsexual individuals using the WHOQOL-100. Methods: This was a prospective cohort study using the WHOQOL-100 and sociodemographic questions for individuals diagnosed with gender identity disorder according to criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. The protocol was used when a transsexual person entered the ambulatory clinic and at least 12 months after SRS. Main Outcome Measures: Initially, improvement or worsening of quality of life was assessed using 6 domains and 24 facets. Subsequently, quality of life was assessed for individuals who underwent new surgical interventions and those who did not undergo these procedures 1 year after SRS. Results: The participants showed significant improvement after SRS in domains II (psychological) and IV (social relationships) of the WHOQOL-100. In contrast, domains I (physical health) and III (level of independence) were significantly worse after SRS. Individuals who underwent additional surgery had a decrease in quality of life reflected in domains II and IV. During statistical analysis, all results were controlled for variations in demographic characteristics, without significant results. Conclusion: The WHOQOL-100 is an important instrument to evaluate the quality of life of male-to-female transsexuals during different stages of treatment. SRS promotes the improvement of psychological aspects and social relationships. However, even 1 year after SRS, male-to-female transsexuals continue to report problems in physical health and difficulty in recovering their independence.
(Due to a citation error, this study was initially listed twice.)
Castellano et al., 2015

Castellano, E., Crespi, C., Dell’Aquila, R., Rosato, C., Catalano, V., et al. (2015). Quality of life and hormones after sex reassignment surgery. Journal of Endocrinological Investigation , 38 (12), 1373-1381.
Background: Transpeople often look for sex reassignment surgery (SRS) to improve their quality of life (QoL). The hormonal therapy has many positive effects before and after SRS. There are no studies about correlation between hormonal status and QoL after SRS. Aim: To gather information on QoL, quality of sexual life and body image in transpeople at least 2 years after SRS, to compare these results with a control group and to evaluate the relations between the chosen items and hormonal status. Subjects and methods: Data from 60 transsexuals and from 60 healthy matched controls were collected. Testosterone, estradiol, LH and World Health Organization Quality of Life (WHOQOL-100) self-reported questionnaire were evaluated. Student’s t test was applied to compare transsexuals and controls. Multiple regression model was applied to evaluate WHOQOL’s chosen items and LH. Results: The QoL and the quality of body image scores in transpeople were not statistically different from the matched control groups’ ones. In the sexual life subscale, transwomen’s scores were similar to biological women’s ones, whereas transmen’s scores were statistically lower than biological men’s ones (P = 0.003). The quality of sexual life scored statistically lower in transmen than in transwomen (P = 0.048). A significant inverse relationship between LH and body image and between LH and quality of sexual life was found. Conclusions: This study highlights general satisfaction after SRS. In particular, transpeople’s QoL turns out to be similar to Italian matched controls. LH resulted inversely correlated to body image and sexual life scores.
Colizzi, Costa, & Todarello, 2014

Colizzi, M., Costa, R. & Todarello, O. (2014). Transsexual patients’ psychiatric comorbidity and positive effect of cross-sex hormonal treatment on mental health: Results from a longitudinal study. Psychoneuroendocrinology , 39 , 65-73.
The aim of the present study was to evaluate the presence of psychiatric diseases/symptoms in transsexual patients and to compare psychiatric distress related to the hormonal intervention in a one year follow-up assessment. We investigated 118 patients before starting the hormonal therapy and after about 12 months. We used the SCID-I to determine major mental disorders and functional impairment. We used the Zung Self-Rating Anxiety Scale (SAS) and the Zung Self-Rating Depression Scale (SDS) for evaluating self-reported anxiety and depression. We used the Symptom Checklist 90-R (SCL-90-R) for assessing self-reported global psychological symptoms. Seventeen patients (14%) had a DSM-IV-TR axis I psychiatric comorbidity. At enrollment the mean SAS score was above the normal range. The mean SDS and SCL-90-R scores were on the normal range except for SCL-90-R anxiety subscale. When treated, patients reported lower SAS, SDS and SCL-90-R scores, with statistically significant differences. Psychiatric distress and functional impairment were present in a significantly higher percentage of patients before starting the hormonal treatment than after 12 months (50% vs. 17% for anxiety; 42% vs. 23% for depression; 24% vs. 11% for psychological symptoms; 23% vs. 10% for functional impairment). The results revealed that the majority of transsexual patients have no psychiatric comorbidity, suggesting that transsexualism is not necessarily associated with severe comorbid psychiatric findings. The condition, however, seemed to be associated with subthreshold anxiety/depression, psychological symptoms and functional impairment. Moreover, treated patients reported less psychiatric distress. Therefore, hormonal treatment seemed to have a positive effect on transsexual patients’ mental health.
Colizzi et al., 2013

Colizzi. M., Costa, R., Pace, V., & Todarello, O. (2013). Hormonal treatment reduces psychobiological distress in gender identity disorder, independently of the attachment style. The Journal of Sexual Medicine , 10 (12), 3049–3058.
Introduction: Gender identity disorder may be a stressful situation. Hormonal treatment seemed to improve the general health as it reduces psychological and social distress. The attachment style seemed to regulate distress in insecure individuals as they are more exposed to hypothalamic–pituitary–adrenal system dysregulation and subjective stress. Aim: The objectives of the study were to evaluate the presence of psychobiological distress and insecure attachment in transsexuals and to study their stress levels with reference to the hormonal treatment and the attachment pattern. Methods: We investigated 70 transsexual patients. We measured the cortisol levels and the perceived stress before starting the hormonal therapy and after about 12 months. We studied the representation of attachment in transsexuals by a backward investigation in the relations between them and their caregivers. Main Outcome Measures: We used blood samples for assessing cortisol awakening response (CAR); we used the Perceived Stress Scale for evaluating self‐reported perceived stress and the Adult Attachment Interview to determine attachment styles. Results: At enrollment, transsexuals reported elevated CAR; their values were out of normal. They expressed higher perceived stress and more attachment insecurity, with respect to normative sample data. When treated with hormone therapy, transsexuals reported significantly lower CAR (P < 0.001), falling within the normal range for cortisol levels. Treated transsexuals showed also lower perceived stress (P < 0.001), with levels similar to normative samples. The insecure attachment styles were associated with higher CAR and perceived stress in untreated transsexuals (P < 0.01). Treated transsexuals did not expressed significant differences in CAR and perceived stress by attachment. Conclusion: Our results suggested that untreated patients suffer from a higher degree of stress and that attachment insecurity negatively impacts the stress management. Initiating the hormonal treatment seemed to have a positive effect in reducing stress levels, whatever the attachment style may be.
Colton-Meier et al., 2011

Colton-Meier, S. L., Fitzgerald, K. M., Pardo, S. T., & Babcock, J. (2011). The effects of hormonal gender affirmation treatment on mental health in female-to-male transsexuals. Journal of Gay & Lesbian Mental Health , 15 (3), 281-299.
Hormonal interventions are an often-sought option for transgender individuals seeking to medically transition to an authentic gender. Current literature stresses that the effects and associated risks of hormone regimens should be monitored and well understood by health care providers (Feldman & Bockting, 2003). However, the positive psychological effects following hormone replacement therapy as a gender affirming treatment have not been adequately researched. This study examined the relationship of hormone replacement therapy, specifically testosterone, with various mental health outcomes in an Internet sample of more than 400 self-identified female-to-male transsexuals. Results of the study indicate that female-to-male transsexuals who receive testosterone have lower levels of depression, anxiety, and stress, and higher levels of social support and health related quality of life. Testosterone use was not related to problems with drugs, alcohol, or suicidality. Overall findings provide clear evidence that HRT is associated with improved mental health outcomes in female-to-male transsexuals.
Costantino et al., 2013

Costantino, A., Cerpolini, S., Alvisi, S., Morselli, P. G., Venturoli, S., & Meriggiola, M. C. (2013). A prospective study on sexual function and mood in female-to-male transsexuals during testosterone administration and after sex reassignment surgery. Journal of Sex & Marital Therapy , 39 (4), 321-335.
Testosterone administration in female-to-male transsexual subjects aims to develop and maintain the characteristics of the desired sex. Very little data exists on its effects on sexuality of female-to-male transsexuals. The aim of this study was to evaluate sexual function and mood of female-to-male transsexuals from their first visit, throughout testosterone administration and after sex reassignment surgery. Participants were 50 female-to-male transsexual subjects who completed questionnaires assessing sexual parameters and mood. The authors measured reproductive hormones and hematological parameters. The results suggest a positive effect of testosterone treatment on sexual function and mood in female-to-male transsexual subjects.
Davis and Meier, 2014

Davis, S. A. & Meier, S. C. (2014). Effects of testosterone treatment and chest reconstruction surgery on mental health and sexuality in female-to-male transgender people. International Journal of Sexual Health , 26 (2), 113-128.
Objectives: This study examined the effects of testosterone treatment with or without chest reconstruction surgery (CRS) on mental health in female-to-male transgender people (FTMs). Methods: More than 200 FTMs completed a written survey including quantitative scales to measure symptoms of anxiety and depression, feelings of anger, and body dissatisfaction, as well as qualitative questions assessing shifts in sexuality after the initiation of testosterone. Fifty-seven percent of participants were taking testosterone and 40% had undergone CRS. Results: Cross-sectional analysis using a between-subjects multivariate analysis of variance showed that participants who were receiving testosterone endorsed fewer symptoms of anxiety and depression as well as less anger than the untreated group. Participants who had CRS in addition to testosterone reported less body dissatisfaction than both the testosterone-only or the untreated groups. Furthermore, participants who were injecting testosterone on a weekly basis showed significantly less anger compared with those injecting every other week. In qualitative reports, more than 50% of participants described increased sexual attraction to nontransgender men after taking testosterone. Conclusions: Results indicate that testosterone treatment in FTMs is associated with a positive effect on mental health on measures of depression, anxiety, and anger, while CRS appears to be more important for the alleviation of body dissatisfaction. The findings have particular relevance for counselors and health care providers serving FTM and gender-variant people considering medical gender transition.
De Cuypere et al., 2006

De Cuypere, G., Elaut, E., Heylens, G., Maele, G. V., Selvaggi, G., et al. (2006). Long-term follow-up: Psychosocial outcome of Belgian transsexuals after sex reassignment surgery. Sexologies , 15 (2), 126-133.
Background: To establish the benefit of sex reassignment surgery (SRS) for persons with a gender identity disorder, follow-up studies comprising large numbers of operated transsexuals are still needed. Aims: The authors wanted to assess how the transsexuals who had been treated by the Ghent multidisciplinary gender team since 1985, were functioning psychologically, socially and professionally after a longer period. They also explored some prognostic factors with a view to refining the procedure. Method: From 107 Dutch-speaking transsexuals who had undergone SRS between 1986 and 2001, 62 (35 male-to-females and 27 female-to-males) completed various questionnaires and were personally interviewed by researchers, who had not been involved in the subjects’ initial assessment or treatment. Results: On the GAF (DSM-IV) scale the female-to-male transsexuals scored significantly higher than the male-to-females (85.2 versus 76.2). While no difference in psychological functioning (SCL-90) was observed between the study group and a normal population, subjects with a pre-existing psychopathology were found to have retained more psychological symptoms. The subjects proclaimed an overall positive change in their family and social life. None of them showed any regrets about the SRS. A homosexual orientation, a younger age when applying for SRS, and an attractive physical appearance were positive prognostic factors. Conclusion: While sex reassignment treatment is an effective therapy for transsexuals, also in the long term, the postoperative transsexual remains a fragile person in some respects.
Dhejne et al., 2014

Dhejne, C., Öberg, K., Arver, S., & Landén, M. (2014). An analysis of all applications for sex reassignment surgery in sweden, 1960-2010: Prevalence, incidence, and regrets. Archives of Sexual Behavior , 43 (8), 1535-1545.
Incidence and prevalence of applications in Sweden for legal and surgical sex reassignment were examined over a 50-year period (1960-2010), including the legal and surgical reversal applications. A total of 767 people (289 natal females and 478 natal males) applied for legal and surgical sex reassignment. Out of these, 89 % (252 female-to-males [FM] and 429 male-to-females [MF]) received a new legal gender and underwent sex reassignment surgery (SRS). A total of 25 individuals (7 natal females and 18 natal males), equaling 3.3 %, were denied a new legal gender and SRS. The remaining withdrew their application, were on a waiting list for surgery, or were granted partial treatment. The incidence of applications was calculated and stratified over four periods between 1972 and 2010. The incidence increased significantly from 0.16 to 0.42/100,000/year (FM) and from 0.23 to 0.73/100,000/year (MF). The most pronounced increase occurred after 2000. The proportion of FM individuals 30 years or older at the time of application remained stable around 30 %. In contrast, the proportion of MF individuals 30 years or older increased from 37 % in the first decade to 60 % in the latter three decades. The point prevalence at December 2010 for individuals who applied for a new legal gender was for FM 1:13,120 and for MF 1:7,750. The FM:MF sex ratio fluctuated but was 1:1.66 for the whole study period. There were 15 (5 MF and 10 MF) regret applications corresponding to a 2.2 % regret rate for both sexes. There was a significant decline of regrets over the time period.
Eldh, Berg, & Gustafsson, 1997

Eldh, J., Berg, A., Gustafsson, M. (1997). Long-term follow up after sex reassignment surgery. Scandinavian Journal of Plastic and Reconstructive Surgery and Hand Surgery , 27 (1), 39-45.
A long-term follow up of 136 patients operated on for sex reassignment was done to evaluate the surgical outcome. Social and psychological adjustments were also investigated by a questionnaire in 90 of these 136 patients. Optimal results of the operation are essential for a successful outcome. Personal and social instability before operation, unsuitable body build, and age over 30 years at operation correlated with unsatisfactory results. Adequate family and social support is important for postoperative functioning. Sex reassignment had no influence on the person’s ability to work.
Fisher et al., 2014

Fisher, A. D., Castellini, G., Bandini, E., Casale, H., Fanni, E., et al. (2014). Cross‐sex hormonal treatment and body uneasiness in individuals with gender dysphoria. The Journal of Sexual Medicine , 11 (3), 709–719.
Introduction: Cross‐sex hormonal treatment (CHT) used for gender dysphoria (GD) could by itself affect well‐being without the use of genital surgery; however, to date, there is a paucity of studies investigating the effects of CHT alone. Aims: This study aimed to assess differences in body uneasiness and psychiatric symptoms between GD clients taking CHT and those not taking hormones (no CHT). A second aim was to assess whether length of CHT treatment and daily dose provided an explanation for levels of body uneasiness and psychiatric symptoms. Methods: A consecutive series of 125 subjects meeting the criteria for GD who not had genital reassignment surgery were considered. Main Outcome Measures: Subjects were asked to complete the Body Uneasiness Test (BUT) to explore different areas of body‐related psychopathology and the Symptom Checklist‐90 Revised (SCL‐90‐R) to measure psychological state. In addition, data on daily hormone dose and length of hormonal treatment (androgens, estrogens, and/or antiandrogens) were collected through an analysis of medical records. Results: Among the male‐to‐female (MtF) individuals, those using CHT reported less body uneasiness compared with individuals in the no‐CHT group. No significant differences were observed between CHT and no‐CHT groups in the female‐to‐male (FtM) sample. Also, no significant differences in SCL score were observed with regard to gender (MtF vs. FtM), hormone treatment (CHT vs. no‐CHT), or the interaction of these two variables. Moreover, a two‐step hierarchical regression showed that cumulative dose of estradiol (daily dose of estradiol times days of treatment) and cumulative dose of androgen blockers (daily dose of androgen blockers times days of treatment) predicted BUT score even after controlling for age, gender role, cosmetic surgery, and BMI. Conclusions: The differences observed between MtF and FtM individuals suggest that body‐related uneasiness associated with GD may be effectively diminished with the administration of CHT even without the use of genital surgery for MtF clients. A discussion is provided on the importance of controlling both length and daily dose of treatment for the most effective impact on body uneasiness.
Glynn et al., 2016

Glynn, T. R., Gamarel, K. E., Kahler, C. W., Iwamoto, M., Operario, D., & Nemoto, T. (2016). The role of gender affirmation in psychological well-being among transgender women. Psychology Of Sexual Orientation And Gender Diversity , 3 (3), 336-344.
High prevalence of psychological distress, including greater depression, lower self-esteem, and suicidal ideation, has been documented across numerous samples of transgender women and has been attributed to high rates of discrimination and violence. According to the gender affirmation framework (Sevelius, 2013), access to sources of gender-affirmative support can offset such negative psychological effects of social oppression. However, critical questions remain unanswered in regards to how and which aspects of gender affirmation are related to psychological well-being. The aims of this study were to investigate the associations among 3 discrete areas of gender affirmation (psychological, medical, and social) and participants’ reports of psychological well-being. A community sample of 573 transgender women with a history of sex work completed a 1-time self-report survey that assessed demographic characteristics, gender affirmation, and mental health outcomes. In multivariate models, we found that social, psychological, and medical gender affirmation were significant predictors of lower depression and higher self-esteem whereas no domains of affirmation were significantly associated with suicidal ideation. Findings support the need for accessible and affordable transitioning resources for transgender women to promote better quality of life among an already vulnerable population. However, transgender individuals should not be portrayed simplistically as objects of vulnerability, and research identifying mechanisms to promote wellness and thriving is necessary for future intervention development. As the gender affirmation framework posits, the personal experience of feeling affirmed as a transgender person results from individuals’ subjective perceptions of need along multiple dimensions of gender affirmation. Thus, personalized assessment of gender affirmation may be a useful component of counseling and service provision for transgender women.
Gomez-Gil et al., 2012

Gomez-Gil, E., Zubiaurre-Elorz, L., Esteva, I., Guillamon, A., Godas, T., Cruz Almaraz, M., Halperin, I., Salamero, M. (2012). Hormone-treated transsexuals report less social distress, anxiety and depression. Psychoneuroendocrinology , 37 (5), 662-670.
Introduction: The aim of the present study was to evaluate the presence of symptoms of current social distress, anxiety and depression in transsexuals. Methods: We investigated a group of 187 transsexual patients attending a gender identity unit; 120 had undergone hormonal sex-reassignment (SR) treatment and 67 had not. We used the Social Anxiety and Distress Scale (SADS) for assessing social anxiety and the Hospital Anxiety and Depression Scale (HADS) for evaluating current depression and anxiety. Results: The mean SADS and HADS scores were in the normal range except for the HAD-Anxiety subscale (HAD-A) on the non-treated transsexual group. SADS, HAD-A, and HAD-Depression (HAD-D) mean scores were significantly higher among patients who had not begun cross-sex hormonal treatment compared with patients in hormonal treatment (F = 4.362, p = .038; F = 14.589, p = .001; F = 9.523, p = .002 respectively). Similarly, current symptoms of anxiety and depression were present in a significantly higher percentage of untreated patients than in treated patients (61% vs. 33% and 31% vs. 8% respectively). Conclusions: The results suggest that most transsexual patients attending a gender identity unit reported subclinical levels of social distress, anxiety, and depression. Moreover, patients under cross-sex hormonal treatment displayed a lower prevalence of these symptoms than patients who had not initiated hormonal therapy. Although the findings do not conclusively demonstrate a direct positive effect of hormone treatment in transsexuals, initiating this treatment may be associated with better mental health of these patients.
Gomez-Gil et al., 2014

Gómez-Gil, E., Zubiaurre-Elorza, L., de Antonio, E. D., Guillamon, A., & Salamero, M. (2014). Determinants of quality of life in Spanish transsexuals attending a gender unit before genital sex reassignment surgery. Quality of Life Research , 23 (2), 669-676.
Purpose: To evaluate the self-reported perceived quality of life (QoL) in transsexuals attending a Spanish gender identity unit before genital sex reassignment surgery, and to identify possible determinants that likely contribute to their QoL. Methods: A sample of 119 male-to-female (MF) and 74 female-to-male (FM) transsexuals were included in the study. The WHOQOL-BREF scale was used to evaluate self-reported QoL. Possible determinants included age, sex, education, employment, partnership status, undergoing cross-sex hormonal therapy, receiving at least one non-genital sex reassignment surgery, and family support (assessed with the family APGAR questionnaire). Results: Mean scores of all QoL domains ranged from 55.44 to 63.51. Linear regression analyses revealed that undergoing cross-sex hormonal treatment, having family support, and having an occupation were associated with a better QoL for all transsexuals. FM transsexuals have higher social domain QoL scores than MF transsexuals. The model accounts for 20.6 % of the variance in the physical, 32.5 % in the psychological, 21.9 % in the social, and 20.1 % in the environment domains, and 22.9 % in the global QoL factor. Conclusions: Cross-sex hormonal treatment, family support, and working or studying are linked to a better self-reported QoL in transsexuals. Healthcare providers should consider these factors when planning interventions to promote the health-related QoL of transsexuals.
Gorin-Lazard et al., 2012

Gorin‐Lazard, A., Baumstarck, K., Boyer, L., Maquigneau, A., Gebleux, S., Penochet, J., Pringuey, D., Albarel, F., Morange, I., Loundou, A., Berbis, J., Auquier, P., Lançon, C. and Bonierbale, M. (2012). Is hormonal therapy associated with better quality of life in transsexuals? A cross‐sectional study. The Journal of Sexual Medicine , 9 (2), 531–541.
Introduction: Although the impact of sex reassignment surgery on the self‐reported outcomes of transsexuals has been largely described, the data available regarding the impact of hormone therapy on the daily lives of these individuals are scarce. Aims: The objectives of this study were to assess the relationship between hormonal therapy and the self‐reported quality of life (QoL) in transsexuals while taking into account the key confounding factors and to compare the QoL levels between transsexuals who have, vs. those who have not, undergone cross‐sex hormone therapy as well as between transsexuals and the general population (French age‐ and sex‐matched controls). Methods: This study incorporated a cross‐sectional design that was conducted in three psychiatric departments of public university teaching hospitals in France. The inclusion criteria were as follows: 18 years or older, diagnosis of gender identity disorder (302.85) according to the Diagnostic and Statistical Manual, fourth edition text revision (DSM‐IV TR), inclusion in a standardized sex reassignment procedure following the agreement of a multidisciplinary team, and pre‐sex reassignment surgery. Main Outcome Measure. QoL was assessed using the Short Form 36 (SF‐36). Results: The mean age of the total sample was 34.7 years, and the sex ratio was 1:1. Forty‐four (72.1%) of the participants received hormonal therapy. Hormonal therapy and depression were independent predictive factors of the SF‐36 mental composite score. Hormonal therapy was significantly associated with a higher QoL, while depression was significantly associated with a lower QoL. Transsexuals’ QoL, independently of hormonal status, did not differ from the French age‐ and sex‐matched controls except for two subscales of the SF‐36 questionnaire: role physical (lower scores in transsexuals) and general health (lower scores in controls). Conclusion: The present study suggests a positive effect of hormone therapy on transsexuals’ QoL after accounting for confounding factors. These results will be useful for healthcare providers of transgender persons but should be confirmed with larger samples using a prospective study design.
Gorin-Lazard et al., 2013

Gorin-Lazard, A., Baumstarck, K., Boyer, L., Maquigneau, A., Penochet, J. C., et al. (2013). Hormonal therapy is associated with better self-esteem, mood, and quality of life in transsexuals. Journal of Nervous and Mental Disease , 201 (11), 996–1000.
Few studies have assessed the role of cross-sex hormones on psychological outcomes during the period of hormonal therapy preceding sex reassignment surgery in transsexuals. The objective of this study was to assess the relationship between hormonal therapy, self-esteem, depression, quality of life (QoL), and global functioning. This study incorporated a cross-sectional design. The inclusion criteria were diagnosis of gender identity disorder (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision) and inclusion in a standardized sex reassignment procedure. The outcome measures were self-esteem (Social Self-Esteem Inventory), mood (Beck Depression Inventory), QoL (Subjective Quality of Life Analysis), and global functioning (Global Assessment of Functioning). Sixty-seven consecutive individuals agreed to participate. Seventy-three percent received hormonal therapy. Hormonal therapy was an independent factor in greater self-esteem, less severe depression symptoms, and greater “psychological-like” dimensions of QoL. These findings should provide pertinent information for health care providers who consider this period as a crucial part of the global sex reassignment procedure.
Hess et al., 2014

Hess, J., Neto, R. R., Panic, L., Rübben, H., & Senf, W. (2014). Satisfaction with male-to-female gender reassignment surgery: Results of a retrospective analysis. Deutsches Ärzteblatt International , 111 (47), 795–801.
Background: The frequency of gender identity disorder is hard to determine; the number of gender reassignment operations and of court proceedings in accordance with the German Law on Transsexuality almost certainly do not fully reflect the underlying reality. There have been only a few studies on patient satisfaction with male-to-female gender reassignment surgery. Methods: 254 consecutive patients who had undergone male-to-female gender reassignment surgery at Essen University Hospital’s Department of Urology retrospectively filled out a questionnaire about their subjective postoperative satisfaction. Results: 119 (46.9%) of the patients filled out and returned the questionnaires, at a mean of 5.05 years after surgery (standard deviation 1.61 years, range 1–7 years). 90.2% said their expectations for life as a woman were fulfilled postoperatively. 85.4% saw themselves as women. 61.2% were satisfied, and 26.2% very satisfied, with their outward appearance as a woman; 37.6% were satisfied, and 34.4% very satisfied, with the functional outcome. 65.7% said they were satisfied with their life as it is now. Conclusion: The very high rates of subjective satisfaction and the surgical outcomes indicate that gender reassignment surgery is beneficial. These findings must be interpreted with caution, however, because fewer than half of the questionnaires were returned.
Heylens et al., 2014

Heylens, G., Verroken, C., De Cock, S., T’Sjoen, G., & De Cuypere, G. (2014). Effects of different steps in gender reassignment therapy on psychopathology: a prospective study of persons with a gender identity disorder. The Journal of Sexual Medicine , 11 (1), 119–126.
Introduction: At the start of gender reassignment therapy, persons with a gender identity disorder (GID) may deal with various forms of psychopathology. Until now, a limited number of publications focus on the effect of the different phases of treatment on this comorbidity and other psychosocial factors. Aims: The aim of this study was to investigate how gender reassignment therapy affects psychopathology and other psychosocial factors. Methods: This is a prospective study that assessed 57 individuals with GID by using the Symptom Checklist‐90 (SCL‐90) at three different points of time: at presentation, after the start of hormonal treatment, and after sex reassignment surgery (SRS). Questionnaires on psychosocial variables were used to evaluate the evolution between the presentation and the postoperative period. The data were statistically analyzed by using SPSS 19.0, with significance levels set at P < 0.05. Main Outcome Measures: The psychopathological parameters include overall psychoneurotic distress, anxiety, agoraphobia, depression, somatization, paranoid ideation/psychoticism, interpersonal sensitivity, hostility, and sleeping problems. The psychosocial parameters consist of relationship, living situation, employment, sexual contacts, social contacts, substance abuse, and suicide attempt. Results: A difference in SCL‐90 overall psychoneurotic distress was observed at the different points of assessments (P = 0.003), with the most prominent decrease occurring after the initiation of hormone therapy (P < 0.001). Significant decreases were found in the subscales such as anxiety, depression, interpersonal sensitivity, and hostility. Furthermore, the SCL‐90 scores resembled those of a general population after hormone therapy was initiated. Analysis of the psychosocial variables showed no significant differences between pre‐ and postoperative assessments. Conclusions: A marked reduction in psychopathology occurs during the process of sex reassignment therapy, especially after the initiation of hormone therapy.
Imbimbo et al., 2009

Imbimbo, C., Verze, P., Palmieri, A., Longo, N., Fusco, F., Arcaniolo, D., & Mirone, V. (2009). A report from a single institute’s 14-year experience in treatment of male-to-female transsexuals. The Journal of Sexual Medicine , 6 (10), 2736–2745.
Introduction: Gender identity disorder or transsexualism is a complex clinical condition, and prevailing social context strongly impacts the form of its manifestations. Sex reassignment surgery (SRS) is the crucial step of a long and complex therapeutic process starting with preliminary psychiatric evaluation and culminating in definitive gender identity conversion. Aim: The aim of our study is to arrive at a clinical and psychosocial profile of male-to-female transsexuals in Italy through analysis of their personal and clinical experience and evaluation of their postsurgical satisfaction levels SRS. Methods: From January 1992 to September 2006, 163 male patients who had undergone gender-transforming surgery at our institution were requested to complete a patient satisfaction questionnaire. Main Outcome Measures: The questionnaire consisted of 38 questions covering nine main topics: general data, employment status, family status, personal relationships, social and cultural aspects, presurgical preparation, surgical procedure, and postsurgical sex life and overall satisfaction. Results: Average age was 31 years old. Seventy-two percent had a high educational level, and 63% were steadily employed. Half of the patients had contemplated suicide at some time in their lives before surgery and 4% had actually attempted suicide. Family and colleague emotional support levels were satisfactory. All patients had been adequately informed of surgical procedure beforehand. Eighty-nine percent engaged in postsurgical sexual activities. Seventy-five percent had a more satisfactory sex life after SRS, with main complications being pain during intercourse and lack of lubrication. Seventy-eight percent were satisfied with their neovagina’s esthetic appearance, whereas only 56% were satisfied with depth. Almost all of the patients were satisfied with their new sexual status and expressed no regrets. Conclusions: Our patients’ high level of satisfaction was due to a combination of a well-conducted preoperative preparation program, competent surgical skills, and consistent postoperative follow-up.
Johansson et al., 2010

Johansson, A., Sundbom, E., Höjerback, T., & Bodlund, O. (2010). A five-year follow-up study of Swedish adults with gender identity disorder. Archives of Sexual Behavior , 39 (6), 1429-1437.
This follow-up study evaluated the outcome of sex reassignment as viewed by both clinicians and patients, with an additional focus on the outcome based on sex and subgroups. Of a total of 60 patients approved for sex reassignment, 42 (25 male-to-female [MF] and 17 female-to-male [FM]) transsexuals completed a follow-up assessment after 5 or more years in the process or 2 or more years after completed sex reassignment surgery. Twenty-six (62%) patients had an early onset and 16 (38%) patients had a late onset; 29 (69%) patients had a homosexual sexual orientation and 13 (31%) patients had a non-homosexual sexual orientation (relative to biological sex). At index and follow-up, a semi-structured interview was conducted. At follow-up, 32 patients had completed sex reassignment surgery, five were still in process, and five—following their own decision—had abstained from genital surgery. No one regretted their reassignment. The clinicians rated the global outcome as favorable in 62% of the cases, compared to 95% according to the patients themselves, with no differences between the subgroups. Based on the follow-up interview, more than 90% were stable or improved as regards work situation, partner relations, and sex life, but 5–15% were dissatisfied with the hormonal treatment, results of surgery, total sex reassignment procedure, or their present general health. Most outcome measures were rated positive and substantially equal for MF and FM. Late-onset transsexuals differed from those with early onset in some respects: these were mainly MF (88 vs. 42%), older when applying for sex reassignment (42 vs. 28 years), and non-homosexually oriented (56 vs. 15%). In conclusion, almost all patients were satisfied with the sex reassignment; 86% were assessed by clinicians at follow-up as stable or improved in global functioning.
Keo-Meier et al., 2015

Keo-Meier, C. L., Herman, L. I., Reisner, S. L., Pardo, S. T., Sharp, C., & Babcock, J. C. (2015). Testosterone treatment and MMPI-2 improvement in transgender men: A prospective controlled study. Journal of Consulting and Clinical Psychology, 83 , 143-156.
Objective: Most transgender men desire to receive testosterone treatment in order to masculinize their bodies. In this study, we aimed to investigate the short-term effects of testosterone treatment on psychological functioning in transgender men. This is the 1st controlled prospective follow-up study to examine such effects. Method: We examined a sample of transgender men (n = 48) and nontransgender male (n = 53) and female (n = 62) matched controls (mean age = 26.6 years; 74% White). We asked participants to complete the Minnesota Multiphasic Personality Inventory (2nd ed., or MMPI–2; Butcher, Graham, Tellegen, Dahlstrom, & Kaemmer, 2001) to assess psychological functioning at baseline and at the acute posttreatment follow-up (3 months after testosterone initiation). Regression models tested (a) Gender × Time interaction effects comparing divergent mean response profiles across measurements by gender identity; (b) changes in psychological functioning scores for acute postintervention measurements, adjusting for baseline measures, comparing transgender men with their matched nontransgender male and female controls and adjusting for baseline scores; and (c) changes in meeting clinical psychopathological thresholds. Results: Statistically significant changes in MMPI–2 scale scores were found at 3-month follow-up after initiating testosterone treatment relative to baseline for transgender men compared with female controls (female template): reductions in Hypochondria (p < .05), Depression (p < .05), Hysteria (p < .05), and Paranoia (p < .01); and increases in Masculinity–Femininity scores (p < .01). Gender × Time interaction effects were found for Hysteria (p < .05) and Paranoia (p < .01) relative to female controls (female template) and for Hypochondria (p < .05), Depression (p < .01), Hysteria (p < .01), Psychopathic Deviate (p < .05), Paranoia (p < .01), Psychasthenia (p < .01), and Schizophrenia (p < .01) compared with male controls (male template). In addition, the proportion of transgender men presenting with co-occurring psychopathology significantly decreased from baseline compared with 3-month follow-up relative to controls (p < .05). Conclusions: Findings suggest that testosterone treatment resulted in increased levels of psychological functioning on multiple domains in transgender men relative to nontransgender controls. These findings differed in comparisons of transgender men with female controls using the female template and with male controls using the male template. No iatrogenic effects of testosterone were found. These findings suggest a direct positive effect of 3 months of testosterone treatment on psychological functioning in transgender men.
Kraemer et al., 2008

Kraemer, B., Delsignore, A., Schnyder, U., & Hepp, U. (2008). Body image and transsexualism. Psychopathology , 41 (2), 96-100.
Background: To achieve a detailed view of the body image of transsexual patients, an assessment of perception, attitudes and experiences about one’s own body is necessary. To date, research on the body image of transsexual patients has mostly covered body dissatisfaction with respect to body perception. Sampling and Methods: We investigated 23 preoperative (16 male-to-female and 7 female-to-male transsexual patients) and 22 postoperative (14 male-to-female and 8 female-to-male) transsexual patients using a validated psychological measure for body image variables. Results: We found that preoperative transsexual patients were insecure and felt unattractive because of concerns about their body image. However, postoperative transsexual patients scored high on attractiveness and self-confidence. Furthermore, postoperative transsexual patients showed low scores for insecurity and concerns about their body. Conclusions: Our results indicate an improvement of body image concerns for transsexual patients following standards of care for gender identity disorder. Follow-up studies are recommended to confirm the assumed positive outcome of standards of care on body image.
Landen et al., 1998

Landén, M., Wålinder, J., Hambert, G., & Lundström, B. (1998). Factors predictive of regret in sex reassignment. Acta Psychiatrica Scandinavica , 97 (4), 284-289.
The objective of this study was to evaluate the features and calculate the frequency of sex-reassigned subjects who had applied for reversal to their biological sex, and to compare these with non-regretful subjects. An inception cohort was retrospectively identified consisting of all subjects with gender identity disorder who were approved for sex reassignment in Sweden during the period 1972-1992. The period of time that elapsed between the application and this evaluation ranged from 4 to 24 years. The total cohort consisted of 218 subjects. The results showed that 3.8% of the patients who were sex reassigned during 1972-1992 regretted the measures taken. The cohort was subdivided according to the presence or absence of regret of sex reassignment, and the two groups were compared. The results of logistic regression analysis indicated that two factors predicted regret of sex reassignment, namely lack of support from the patient’s family, and the patient belonging to the non-core group of transsexuals. In conclusion, the results show that the outcome of sex reassignment has improved over the years. However, the identified risk factors indicate the need for substantial efforts to support the families and close friends of candidates for sex reassignment.
Lawrence, 2003

Lawrence, A. A. (2003). Factors associated with satisfaction or regret following male-to-female sex reassignment surgery. Archives of Sexual Behavior , 32 (4), 299-315.
This study examined factors associated with satisfaction or regret following sex reassignment surgery (SRS) in 232 male-to-female transsexuals operated on between 1994 and 2000 by one surgeon using a consistent technique. Participants, all of whom were at least 1-year postoperative, completed a written questionnaire concerning their experiences and attitudes. Participants reported overwhelmingly that they were happy with their SRS results and that SRS had greatly improved the quality of their lives. None reported outright regret and only a few expressed even occasional regret. Dissatisfaction was most strongly associated with unsatisfactory physical and functional results of surgery. Most indicators of transsexual typology, such as age at surgery, previous marriage or parenthood, and sexual orientation, were not significantly associated with subjective outcomes. Compliance with minimum eligibility requirements for SRS specified by the Harry Benjamin International Gender Dysphoria Association was not associated with more favorable subjective outcomes. The physical results of SRS may be more important than preoperative factors such as transsexual typology or compliance with established treatment regimens in predicting postoperative satisfaction or regret.
Lawrence, 2006

Lawrence, A. A. (2006). Patient-reported complications and functional outcomes of male-to-female sex reassignment surgery. Archives of Sexual Behavior , 35 (6), 717-727.
This study examined preoperative preparations, complications, and physical and functional outcomes of male-to-female sex reassignment surgery (SRS), based on reports by 232 patients, all of whom underwent penile-inversion vaginoplasty and sensate clitoroplasty, performed by one surgeon using a consistent technique. Nearly all patients discontinued hormone therapy before SRS and most reported that doing so created no difficulties. Preoperative electrolysis to remove genital hair, undergone by most patients, was not associated with less serious vaginal hair problems. No patients reported rectal-vaginal fistula or deep-vein thrombosis and reports of other significant surgical complications were uncommon. One third of patients, however, reported urinary stream problems. No single complication was significantly associated with regretting SRS. Satisfaction with most physical and functional outcomes of SRS was high; participants were least satisfied with vaginal lubrication, vaginal touch sensation, and vaginal erotic sensation. Frequency of achieving orgasm after SRS was not significantly associated with most general measures of satisfaction. Later years of surgery, reflecting greater surgeon experience, were not associated with lower prevalence rates for most complications or with better ratings for most physical and functional outcomes of SRS.
Lobato et al., 2006

Lobato M. I., Koff, W. J., Manenti, C., da Fonseca Seger, D., Salvador, J., et al. (2006). Follow-up of sex reassignment surgery in transsexuals: a Brazilian cohort. Archives of Sexual Behavior, 35(6) , 711–715.
This study examined the impact of sex reassignment surgery on the satisfaction with sexual experience, partnerships, and relationship with family members in a cohort of Brazilian transsexual patients. A group of 19 patients who received sex reassignment between 2000 and 2004 (18 male- to-female, 1 female-to-male) after a two-year evaluation by a multidisciplinary team, and who agreed to participate in the study, completed a written questionnaire. Mean age at entry into the program was 31.21 ± 8.57 years and mean schooling was 9.2 ± 1.4 years. None of the patients reported regret for having undergone the surgery. Sexual experience was considered to have improved by 83.3% of the patients, and became more frequent for 64.7% of the patients. For 83.3% of the patients, sex was considered to be pleasurable with the neovagina/neopenis. In addition, 64.7% reported that initiating and maintaining a relationship had become easier. The number of patients with a partner increased from 52.6% to 73.7%. Family relationships improved in 26.3% of the cases, whereas 73.7% of the patients did not report a difference. None of the patients reported worse relationships
Manieri et al., 2014

Manieri, C., Castellano, E., Crespi, C., Di Bisceglie, C., Dell’Aquila, C., et al. (2014). Medical treatment of subjects with gender identity disorder: The experience in an Italian public health center. International Journal Of Transgenderism , 15 (2), 53-65.
Hormonal treatment is the main element during the transition program for transpeople. The aim of this paper is to describe the care and treatment of subjects, highlighting both the endocrine-metabolic effects of the hormonal therapy and the quality of life during the first year of cross-sex therapy in an Italian gender team. We studied 83 subjects (56 male-to-female [MtF], 27 female-to-male [FtM]) with hematological and hormonal evaluations every 3 months during the first year of hormonal therapy. MtF persons were treated with 17βestradiol and antiandrogens (cyproterone acetate, spironolactone, dutasteride); FtM persons were treated with transdermal or intramuscular testosterone. The WHO Quality of Life questionnaire was administered at the beginning and 1 year later. Hormonal changes paralleled phenotype modifications with wide variability. Most of both MtF and FtM subjects reported a statistically significant improvement in body image (p < 0.05). In particular, MtF subjects reported a statistically significant improvement in the quality of their sexual life and in the general quality of life (p < 0.05) 1 year after treatment initiation. Cross-sex therapy seems to be free of major risks in healthy subjects under clinical supervision during the first year. Selected subjects show an optimal adaptation to hormone-induced neuropsychological modifications and satisfaction regarding general and sexual life.
Megeri and Khoosal, 2007

Megeri, D., & Khoosal, D. (2007). Anxiety and depression in males experiencing gender dysphoria. Sexual & Relationship Therapy , 22 (1), 77-81.
Objective: The aim of the study was to compare anxiety and depression scores for the first 40 male to female people experiencing gender dysphoria attending the Leicester Gender Identity Clinic using the same sample as control pre and post gender realignment surgery. Hypothesis: There is an improvement in the scores of anxiety and depression following gender realignment surgery among people with gender dysphoria (male to female – transwomen). Results: There was no significant change in anxiety and depression scores in people with gender dysphoria (male to female) pre- and post-operatively.
Nelson, Whallett, & Mcgregor, 2009

Nelson, L., Whallett, E., & McGregor, J. (2009). Transgender patient satisfaction following reduction mammaplasty. Journal of Plastic, Reconstructive & Aesthetic Surgery , 62 (3), 331-334.
Aim: To evaluate the outcome of reduction mammaplasty in female-to-male transgender patients. Method: A 5-year retrospective review was conducted on all female-to-male transgender patients who underwent reduction mammaplasty. A postal questionnaire was devised to assess patient satisfaction, surgical outcome and psychological morbidity. Results: Seventeen patients were identified. The senior author performed bilateral reduction mammaplasties and free nipple grafts in 16 patients and one patient had a Benelli technique reduction. Complications included two haematomas, one wound infection, one wound dehiscence and three patients had hypertrophic scars. Secondary surgery was performed in seven patients and included scar revision, nipple reduction/realignment, dog-ear correction and nipple tattooing. The mean follow-up period after surgery was 10 months (range 2–23 months). Twelve postal questionnaires were completed (response rate 70%). All respondents expressed satisfaction with their result and no regret. Seven patients had nipple sensation and nine patients were satisfied with nipple position. All patients thought their scars were reasonable and felt that surgery had improved their self-confidence and social interactions. Conclusion: Reduction mammaplasty for female-to-male gender reassignment is associated with high patient satisfaction and a positive impact on the lives of these patients.
Newfield et al., 2006

Newfield, E., Hart, S., Dibble, S., & Kohler, L. (2006). Female-to-male transgender quality of life. Quality of Life Research , 15 (9), 1447-1457.
Objectives: We evaluated health-related quality of life in female-to-male (FTM) transgender individuals, using the Short-Form 36-Question Health Survey version 2 (SF-36v2). Methods: Using email, Internet bulletin boards, and postcards, we recruited individuals to an Internet site ( http://www.transurvey.org ), which contained a demographic survey and the SF36v2. We enrolled 446 FTM transgender and FTM transsexual participants, of which 384 were from the US. Results: Analysis of quality of life health concepts demonstrated statistically significant (p<0.0\) diminished quality of life among the FTM transgender participants as compared to the US male and female population, particularly in regard to mental health. FTM transgender participants who received testosterone (67%) reported statistically significant higher quality of life scores (/?<0.01) than those who had not received hormone therapy. Conclusions: FTM transgender participants reported significantly reduced mental health-related quality of life and
Padula, Heru, & Campbell, 2016

Padula, W. V., Heru, S. & Campbell, J. D. (2016). Societal implications of health insurance coverage for medically necessary services in the U.S. transgender population: A cost-effectiveness analysis. Journal of General Internal Medicine , 31 ( 4), 394-401.
Background: Recently, the Massachusetts Group Insurance Commission (GIC) prioritized research on the implications of a clause expressly prohibiting the denial of health insurance coverage for transgender-related services. These medically necessary services include primary and preventive care as well as transitional therapy. Objective: To analyze the cost-effectiveness of insurance coverage for medically necessary transgender-related services. Design: Markov model with 5- and 10-year time horizons from a U.S. societal perspective, discounted at 3 % (USD 2013). Data on outcomes were abstracted from the 2011 National Transgender Discrimination Survey (NTDS). Patients: U.S. transgender population starting before transitional therapy. Interventions: No health benefits compared to health insurance coverage for medically necessary services. This coverage can lead to hormone replacement therapy, sex reassignment surgery, or both. Main Measures: Cost per quality-adjusted life year (QALY) for successful transition or negative outcomes (e.g. HIV, depression, suicidality, drug abuse, mortality) dependent on insurance coverage or no health benefit at a willingness-to-pay threshold of $100,000/QALY. Budget impact interpreted as the U.S. per-member-per-month cost. Key Results: Compared to no health benefits for transgender patients ($23,619; 6.49 QALYs), insurance coverage for medically necessary services came at a greater cost and effectiveness ($31,816; 7.37 QALYs), with an incremental cost-effectiveness ratio (ICER) of $9314/QALY. The budget impact of this coverage is approximately $0.016 per member per month. Although the cost for transitions is $10,000–22,000 and the cost of provider coverage is $2175/year, these additional expenses hold good value for reducing the risk of negative endpoints —HIV, depression, suicidality, and drug abuse. Results were robust to uncertainty. The probabilistic sensitivity analysis showed that provider coverage was cost-effective in 85 % of simulations. Conclusions: Health insurance coverage for the U.S. transgender population is affordable and cost-effective, and has a low budget impact on U.S. society. Organizations such as the GIC should consider these results when examining policies regarding coverage exclusions.
Parola et al., 2010

Parola, N., Bonierbale, M., Lemaire, A., Aghababian, V., Michel, A., & Lançon, C. (2010). Study of quality of life for transsexuals after hormonal and surgical reassignment. Sexologies , 19 (1), 24-28.
Aim: The main objective of this work is to provide a more detailed assessment of the impact of surgical reassignment on the most important aspects of daily life for these patients. Our secondary objective was to establish the influence of various factors likely to have an impact on the quality of life (QoL), such as biological gender and the subject’s personality. Methods: A personality study was conducted using Eysenck Personality Inventory (EPI) so as to analyze two aspects of the personality (extraversion and neuroticism). Thirty-eight subjects who had undergone hormonal surgical reassignment were included in the study. Results: The results show that gender reassignment surgery improves the QoL for transsexuals in several different important areas: most are satisfied of their sexual reassignment (28/30), their social (21/30) and sexual QoL (25/30) are improved. However, there are differences between male-to-female (MtF) and female-to-male (FtM) transsexuals in terms of QoL: FtM have a better social, professional, friendly lifestyles than MtF. Finally, the results of this study did not evidence any influence by certain aspects of the personality, such as extraversion and neuroticism, on the QoL for reassigned subjects.
Pfäfflin, 1993

Pfäfflin, F. (1993). Regrets after sex reassignment surgery. Journal of Psychology & Human Sexuality , 5 (4), 69-85.
Using data draw from the follow-up literature covering the last 30 years, and the author’s clinical data on 295 men and women after SRS, an estimation of the number of patients who regretted the operations is made. Among female-to-male transsexuals after SRS, i.e., in men, no regrets were reported in the author’s sample, and in the literature they amount to less than 1%. Among male-to- female transsexuals after SRS, i.e., in women, regrets are reported in 1-1.5%. Poor differential diagnosis, failure to carry out the real-life- test, and poor surgical results seem to be the main reasons behind the regrets reported in the literature. According to three cases observed by the author in addition to personality traits the lack of proper care in treating the patients played a major role.
Pimenoff and Pfäfflin, 2011

Pimenoff, V., & Pfäfflin, F. (2011). Transsexualism: Treatment outcome of compliant and noncompliant patients. International Journal Of Transgenderism , 13 (1), 37-44.
The objective of the study was a follow-up of the treatment outcome of Finnish transsexuals who sought sex reassignment during the period 1970–2002 and a comparison of the results and duration of treatment of compliant and noncompliant patients. Fifteen male-to-female transsexuals and 17 female-to-male transsexuals who had undergone hormone and surgical treatment and legal sex reassignment in Finland completed a questionnaire on psychosocial data and on their experience with the different phases of clinical assessment and treatment. The changes in their vocational functioning and social and psychic adjustment were used as outcome indicators. The results and duration of the treatment of compliant and noncompliant patients were compared. The patients benefited significantly from treatment. The noncompliant patients achieved equally good results as the compliant ones, and did so in a shorter time. A good treatment outcome could be achieved even when the patient had told the assessing psychiatrist a falsified story of his life and sought hormone therapy, genital surgery, or legal sex reassignment on his own initiative without a recommendation from the psychiatrist. Based on these findings, it is recommended that the doctor-patient relationship be reconsidered and founded on frank cooperation.
Rakic et al., 1996

Rakic, Z., Starcevic, V., Maric, J., & Kelin, K. (1996). The outcome of sex reassignment surgery in Belgrade: 32 patients of both sexes. Archives of Sexual Behavior , 25 (5), 515-525.
Several aspects of the quality of life after sex reassignment surgery in 32 transsexuals of both sexes (22 men, 10 women) were examined. The Belgrade Team for Gender Identity Disorders designed a standardized questionnaire for this purpose. The follow-up period after operation was from 6 months to 4 years, and four aspects of the quality of life were examined: attitude towards the patients’ own body, relationships with other people, sexual activity, and occupational functioning. In most transsexuals, the quality of life was improved after surgery inasmuch as these four aspects are concerned. Only a few transsexuals were not satisfied with their life after surgery.
Rehman et al., 1999

Rehman, J., Lazer, S., Benet, A. E., Schaefer, L. C., & Melman, A. (1999). The reported sex and surgery satisfactions of 28 postoperative male-to-female transsexual patients. Archives of Sexual Behavior , 28 (1), 71-89.
From 1980 to July 1997 sixty-one male-to-female gender transformation surgeries were performed at our university center by one author (A.M.). Data were collected from patients who had surgery up to 1994 (n = 47) to obtain a minimum follow-up of 3 years; 28 patients were contacted. A mail questionnaire was supplemented by personal interviews with 11 patients and telephone interviews with remaining patients to obtain and clarify additional information. Physical and functional results of surgery were judged to be good, with few patients requiring additional corrective surgery. General satisfaction was expressed over the quality of cosmetic (normal appearing genitalia) and functional (ability to perceive orgasm) results. Follow-up showed satisfied who believed they had normal appearing genitalia and the ability to experience orgasm. Most patients were able to return to their jobs and live a more satisfactory social and personal life. One significant outcome was the importance of proper preparation of patients for surgery and especially the need for additional postoperative psychotherapy. None of the patients regretted having had surgery. However, some were, to a degree, disappointed because of difficulties experienced post operatively in adjusting satisfactorily as women both in their relationships with men and in living their lives generally as women. Findings of this study make a strong case for making a change in the Harry Benjamin Standards of Care to include a period of postoperative psychotherapy.
Rotondi et al., 2011

Rotondi, N. K., Bauer, G. R., Scanlon, K., Kaay, M., Travers, R., & Travers, A. (2011). Prevalence of and risk and protective factors for depression in female-to-male transgender Ontarians: Trans PULSE Project. Canadian Journal Of Community Mental Health , 30 (2), 135-155.
Although depression is understudied in transgender and transsexual communities, high prevalences have been reported. This paper presents original research from the Trans PULSE Project, an Ontario-wide, community-based initiative that surveyed 433 participants using respondent-driven sampling. The purpose of this analysis was to determine the prevalence of, and risk and protective factors for, depression among female-to-male (FTM) Ontarians (n = 207). We estimate that 66.4% of FTMs have symptomatology consistent with depression. In multivariable analyses, sexual satisfaction was a strong protective factor. Conversely, experiencing transphobia and being at the stage of planning but not having begun a medical transition (hormones and/or surgery) adversely affected mental health in FTMs.
Ruppin and Pfäfflin, 2015

Ruppin, U., & Pfäfflin, F. (2015). Long-term follow-up of adults with gender identity disorder. Archives of Sexual Behavior , 44 (5), 1321-1329.
The aim of this study was to re-examine individuals with gender identity disorder after as long a period of time as possible. To meet the inclusion criterion, the legal recognition of participants’ gender change via a legal name change had to date back at least 10 years. The sample comprised 71 participants (35 MtF and 36 FtM). The follow-up period was 10–24 years with a mean of 13.8 years (SD = 2.78). Instruments included a combination of qualitative and quantitative methods: Clinical interviews were conducted with the participants, and they completed a follow-up questionnaire as well as several standardized questionnaires they had already filled in when they first made contact with the clinic. Positive and desired changes were determined by all of the instruments: Participants reported high degrees of well-being and a good social integration. Very few participants were unemployed, most of them had a steady relationship, and they were also satisfied with their relationships with family and friends. Their overall evaluation of the treatment process for sex reassignment and its effectiveness in reducing gender dysphoria was positive. Regarding the results of the standardized questionnaires, participants showed significantly fewer psychological problems and interpersonal difficulties as well as a strongly increased life satisfaction at follow-up than at the time of the initial consultation. Despite these positive results, the treatment of transsexualism is far from being perfect.
Smith et al., 2005

Smith, Y. L. S., Van Goozen, S. H. M., Kuiper, A. J., & Cohen-Kettenis, P. (2005). Sex reassignment: Outcomes and predictors of treatment for adolescent and adult transsexuals. Psychological Medicine, 35 (1), 89-99.
Background: We prospectively studied outcomes of sex reassignment, potential differences between subgroups of transsexuals, and predictors of treatment course and outcome. Method: Altogether 325 consecutive adolescent and adult applicants for sex reassignment participated: 222 started hormone treatment, 103 did not; 188 completed and 34 dropped out of treatment. Only data of the 162 adults were used to evaluate treatment. Results between subgroups were compared to determine post-operative differences. Adults and adolescents were included to study predictors of treatment course and outcome. Results were statistically analysed with logistic regression and multiple linear regression analyses. Results: After treatment the group was no longer gender dysphoric. The vast majority functioned quite well psychologically, socially and sexually. Two non-homosexual male-to-female transsexuals expressed regrets. Post-operatively, female-to-male and homosexual transsexuals functioned better in many respects than male-to-female and non-homosexual transsexuals. Eligibility for treatment was largely based upon gender dysphoria, psychological stability, and physical appearance. Male-to-female transsexuals with more psychopathology and cross-gender symptoms in childhood, yet less gender dysphoria at application, were more likely to drop out prematurely. Non-homosexual applicants with much psychopathology and body dissatisfaction reported the worst post-operative outcomes. Conclusions: The results substantiate previous conclusions that sex reassignment is effective. Still, clinicians need to be alert for non-homosexual male-to-females with unfavourable psychological functioning and physical appearance and inconsistent gender dysphoria reports, as these are risk factors for dropping out and poor post-operative results. If they are considered eligible, they may require additional therapeutic guidance during or even after treatment.
van de Grift et al., 2017

van de Grift, T. C., Elaut, E., Cerwenka, S. C., Cohen-Kettenis, P. T., Cuypere, G. D., Richter-Appelt, H., & Kreukels, B. P. (2017). Effects of medical interventions on gender dysphoria and body image. Psychosomatic Medicine , 79 (7), 815-823.
Objective: The aim of this study from the European Network for the Investigation of Gender Incongruence is to investigate the status of all individuals who had applied for gender confirming interventions from 2007 to 2009, irrespective of whether they received treatment. The current article describes the study protocol, the effect of medical treatment on gender dysphoria and body image, and the predictive value of (pre)treatment factors on posttreatment outcomes. Methods: Data were collected on medical interventions, transition status, gender dysphoria (Utrecht Gender Dysphoria Scale), and body image (Body Image Scale for transsexuals). In total, 201 people participated in the study (37% of the original cohort). Results: At follow-up, 29 participants (14%) did not receive medical interventions, 36 hormones only (18%), and 136 hormones and surgery (68%). Most transwomen had undergone genital surgery, and most transmen chest surgery. Overall, the levels of gender dysphoria and body dissatisfaction were significantly lower at follow-up compared with clinical entry. Satisfaction with therapy responsive and unresponsive body characteristics both improved. High dissatisfaction at admission and lower psychological functioning at follow-up were associated with persistent body dissatisfaction. Conclusions: Hormone-based interventions and surgery were followed by improvements in body satisfaction. The level of psychological symptoms and the degree of body satisfaction at baseline were significantly associated with body satisfaction at follow-up.

van de Grift, T. C., Elaut, E., Cerwenka, S. C., Cohen-Kettenis, P. T., & Kreukels, B. P. (2017). Surgical satisfaction, quality of life, and their association after gender-affirming surgery: A follow-up study. Journal of Sex & Marital Therapy , 44 (2), 138-148.
We assessed the outcomes of gender-affirming surgery (GAS, or sex-reassignment surgery) 4 to 6 years after first clinical contact, and the associations between postoperative (dis)satisfaction and quality of life (QoL). Our multicenter, cross-sectional follow-up study involved persons diagnosed with gender dysphoria (DSM-IV-TR) who applied for medical interventions from 2007 until 2009. Of 546 eligible persons, 201 (37%) responded, of whom 136 had undergone GAS (genital, chest, facial, vocal cord and/or thyroid cartilage surgery). Main outcome measures were procedure performed, self-reported complications, and satisfaction with surgical outcomes (standardized questionnaires), QoL (Satisfaction With Life Scale, Subjective Happiness Scale, Cantril Ladder), gender dysphoria (Utrecht Gender Dysphoria Scale), and psychological symptoms (Symptom Checklist-90). Postoperative satisfaction was 94% to 100%, depending on the type of surgery performed. Eight (6%) of the participants reported dissatisfaction and/or regret, which was associated with preoperative psychological symptoms or self-reported surgical complications (OR= 6.07). Satisfied respondents’ QoL scores were similar to reference values; dissatisfied or regretful respondents’ scores were lower. Therefore, dissatisfaction after GAS may be viewed as indicator of unfavorable psychological and QoL outcomes.
Vujovic et al., 2009

Vujovic, S., Popovic, S., Sbutega-Milosevic, G., Djordjevic, M., & Gooren, L. (2009). Transsexualism in Serbia: A twenty-year follow-up study. The Journal of Sexual Medicine , 6 (4), 1018-1023.
Introduction: Gender dysphoria occurs in all societies and cultures. The prevailing social context has a strong impact on its manifestations as well as on applications by individuals with the condition for sex reassignment treatment. Aim: To describe a transsexual population seeking sex reassignment treatment in Serbia, part of former Yugoslavia. Methods: Data, collated over a period of 20 years, from subjects applying for sex reassignment to the only center in Serbia, were analyzed retrospectively. Main Outcome Measures: Age at the time of application, demographic data, family background, sex ratio, the prevalence of polycystic ovarian syndrome (PCOS) among female-to-male (FTM) transsexuals, and readiness to undergo surgical sex reassignment were tabulated. Results: Applicants for sex reassignment in Serbia are relatively young. The sex ratio is close to 1:1. They often come from single-child families. More than 10% do not wish to undergo surgical sex reassignment. The prevalence of PCOS among FTM transsexuals was higher than in the general population but considerably lower than that reported in the literature from other populations. Of those who had undergone sex reassignment, none expressed regret for their decision. Conclusions: Although transsexualism is a universal phenomenon, the relatively young age of those applying for sex reassignment and the sex ratio of 1:1 distinguish the population in Serbia from others reported in the literature.

Weigert et al., 2013

Weigert, R., Frison, E., Sessiecq, Q., Al Mutairi, K., & Casoli, V. (2013). Patient satisfaction with breasts and psychosocial, sexual, and physical well-being after breast augmentation in male-to-female transsexuals. Plastic and Reconstructive Surgery, 132 (6), 1421-1429.
Background: Satisfaction with breasts, sexual well-being, psychosocial well-being, and physical well-being are essential outcome factors following breast augmentation surgery in male-to-female transsexual patients. The aim of this study was to measure change in patient satisfaction with breasts and sexual, physical, and psychosocial well-being after breast augmentation in male-to-female transsexual patients. Methods: All consecutive male-to-female transsexual patients who underwent breast augmentation between 2008 and 2012 were asked to complete the BREAST-Q Augmentation module questionnaire before surgery, at 4 months, and later after surgery. A prospective cohort study was designed and postoperative scores were compared with baseline scores. Satisfaction with breasts and sexual, physical, and psychosocial outcomes assessment was based on the BREAST-Q. Results: Thirty-five male-to-female transsexual patients completed the questionnaires. BREAST-Q subscale median scores (satisfaction with breasts, +59 points; sexual well-being, +34 points; and psychosocial well-being, +48 points) improved significantly (p < 0.05) at 4 months postoperatively and later. No significant change was observed in physical well-being. Conclusions: In this prospective, noncomparative, cohort study, the current results suggest that the gains in breast satisfaction, psychosocial well-being, and sexual well-being after male-to-female transsexual patients undergo breast augmentation are statistically significant and clinically meaningful to the patient at 4 months after surgery and in the long term.
Weyers et al., 2009

Weyers, S., Elaut, E., De Sutter, P., Gerris, J., T’Sjoen, G., et al. (2009). Long-term assessment of the physical, mental, and sexual health among transsexual women. The Journal of Sexual Medicine , 6 (3), 752-760.
Introduction: Transsexualism is the most extreme form of gender identity disorder and most transsexuals eventually pursue sex reassignment surgery (SRS). In transsexual women, this comprises removal of the male reproductive organs, creation of a neovagina and clitoris, and often implantation of breast prostheses. Studies have shown good sexual satisfaction after transition. However, long-term follow-up data on physical, mental and sexual functioning are lacking. Aim: To gather information on physical, mental, and sexual well-being, health-promoting behavior and satisfaction with gender-related body features of transsexual women who had undergone SRS. Methods: Fifty transsexual women who had undergone SRS >or=6 months earlier were recruited. Main Outcome Measures: Self-reported physical and mental health using the Dutch version of the Short-Form-36 (SF-36) Health Survey; sexual functioning using the Dutch version of the Female Sexual Function Index (FSFI). Satisfaction with gender-related bodily features as well as with perceived female appearance; importance of sex, relationship quality, necessity and advisability of gynecological exams, as well as health concerns and feelings of regret concerning transition were scored. Results: Compared with reference populations, transsexual women scored good on physical and mental level (SF-36). Gender-related bodily features were shown to be of high value. Appreciation of their appearance as perceived by others, as well as their own satisfaction with their self-image as women obtained a good score (8 and 9, respectively). However, sexual functioning as assessed through FSFI was suboptimal when compared with biological women, especially the sublevels concerning arousal, lubrication, and pain. Superior scores concerning sexual function were obtained in those transsexual women who were in a relationship and in heterosexuals. Conclusions: Transsexual women function well on a physical, emotional, psychological and social level. With respect to sexuality, they suffer from specific difficulties, especially concerning arousal, lubrication, and pain.
Back to Top
Below are 4 studies that contain mixed or null findings on the effect of gender transition on transgender well-being. Click here to jump to the 17 studies that consist of literature reviews or guidelines that help advance knowledge about the effect of gender transition on transgender well-being . Click here to jump to the 51 studies that found that gender transition improves the well-being of transgender people .
Barrett, 1998.

Barrett J. (1998). Psychological and social function before and after phalloplasty. The International Journal of Transgenderism , 2 (1), 1-8.
There are no quantitative assessments of the benefits of phalloplasty in a female transsexual population. The study addresses this question, comparing transsexuals accepted for such surgery with transsexuals after such surgery has been performed. A population of 23 transsexuals accepted for phalloplasty was compared to a population of 40 who had undergone such surgery between six and one hundred and sixty months previously. The General Health Questionnaire (GHQ), Symptom Checklist 90 (SCL-90), Bem Sex Role Inventory and Social Role Performance Schedule (SRPS) were employed. Additionally, a questionnaire assessing satisfaction with cosmetic appearance, sexual function, relationship and urinary function was used, along with a semi-structured interview quantifying alcohol, cigarette and drug usage, and current sexual practice. There were significant differences between the populations. The post operative group showed higher depression ratings on the depression subscale of the GHQ. The masculine pre-operative Bem scores were neutral post-operatively as feminine sub-scores increased. There was improved satisfaction with genital appearance post-operatively, but satisfaction with relationships fell, although to a non-significant extent. Most other changes were in the expected direction but did not achieve significance. Transsexuals accepted for phalloplasty have very good psychological health. Tendency to further improvement is the case after phalloplasty. Depression is commoner, however, and quality of relationships declines somewhat, perhaps in consequence. Surgeons might advise partners as well as patients of realistic expectations from such surgery.
Lindqvist et al., 2017

Lindqvist, E. K., Sigurjonsson, H., Möllermark, C., Rinder, J., Farnebo, F., et al. (2017). Quality of life improves early after gender reassignment surgery in transgender women. European Journal of Plastic Surgery , 40 (3), 223-226.
Background: Few studies have examined the long-term quality of life (QoL) of individuals with gender dysphoria, or how it is affected by treatment. Our aim was to examine the QoL of transgender women undergoing gender reassignment surgery (GRS). Methods: We performed a prospective cohort study on 190 patients undergoing male-to-female GRS at Karolinska University Hospital between 2003 and 2015. We used the Swedish version of the Short Form-36 Health Survey (SF-36), which measures QoL across eight domains. The questionnaire was distributed to patients pre-operatively, as well as 1, 3, and 5 years post-operatively. The results were compared between the different measure points, as well as between the study group and the general population. Results: On most dimensions of the SF-36 questionnaire, transgender women reported a lower QoL than the general population. The scores of SF-36 showed a non-significant trend to be lower 5 years post-GRS compared to pre-operatively, a decline consistent with that of the general population. Self-perceived health compared to 1 year previously rose in the first post-operative year, after which it declined. Conclusions: To our knowledge, this is the largest prospective study to follow a group of transgender patients with regards to QoL over continuous temporal measure points. Our results show that transgender women generally have a lower QoL compared to the general population. GRS leads to an improvement in general well-being as a trend but over the long-term, QoL decreases slightly in line with that of the comparison group. Level of evidence: Level III, therapeutic study.
Simonsen et al., 2016

Simonsen, R. K., Giraldi, A., Kristensen, E., & Hald, G. M. (2016). Long-term follow-up of individuals undergoing sex reassignment surgery: Psychiatric morbidity and mortality. Nordic Journal Of Psychiatry , 70 (4), 241-247.
Background: There is a lack of long-term register-based follow-up studies of sex-reassigned individuals concerning mortality and psychiatric morbidity. Accordingly, the present study investigated both mortality and psychiatric morbidity using a sample of individuals with transsexualism which comprised 98% (n = 104) of all individuals in Denmark. Aims: (1) To investigate psychiatric morbidity before and after sex reassignment surgery (SRS) among Danish individuals who underwent SRS during the period of 1978–2010. (2) To investigate mortality among Danish individuals who underwent SRS during the period of 1978–2010.Method: Psychiatric morbidity and mortality were identified by data from the Danish Psychiatric Central Research Register and the Cause of Death Register through a retrospective register study of 104 sex-reassigned individuals. Results: Overall, 27.9% of the sample were registered with psychiatric morbidity before SRS and 22.1% after SRS (p = not significant). A total of 6.7% of the sample were registered with psychiatric morbidity both before and after SRS. Significantly more psychiatric diagnoses were found before SRS for those assigned as female at birth. Ten individuals were registered as deceased post-SRS with an average age of death of 53.5 years. Conclusions: No significant difference in psychiatric morbidity or mortality was found between male to female and female to male (FtM) save for the total number of psychiatric diagnoses where FtM held a significantly higher number of psychiatric diagnoses overall. Despite the over-representation of psychiatric diagnoses both pre- and post-SRS the study found that only a relatively limited number of individuals had received diagnoses both prior to and after SRS. This suggests that generally SRS may reduce psychological morbidity for some individuals while increasing it for others.
Udeze, 2008

Udeze, B., Abdelmawla, N., Khoosal, D., & Terry, T. (2008). Psychological functions in male-to-female transsexual people before and after surgery. Sexual & Relationship Therapy , 23 (2), 141-145.
Patients with gender dysphoria (GD) suffer from a constant feeling of psychological discomfort related to their anatomical sex. Gender reassignment surgery (GRS) attempts to release this discomfort. The aim of this study was to compare the functioning of a cohort or patients with GD before and after GRS. We hypothesized that there would be an improvement in the scores of the self-administered SCL-90R following gender reassignment surgery among male-to-female people with gender dysphoria. We studied 40 patients with a DSM-IV diagnosis of Gender Identity Disorder (GID) who attended Leicester Gender Identity Clinic. We compared their functioning as measured by Symptom Check List-90R (SCL-90R) which was administered to 40 randomly selected male-to-female patients before and within six months after GRS using the same sample as control pre-and post-surgery. There was no significant change in the different sub-scales of the SCL-90R scores in patients with male-to-female GID pre- and within six months post-surgery. The results of the study showed that GRS had no significant effect on functioning as measured by SCL-90R within six months of surgery. Our study has the advantage of reducing inter-subject variability by using the same patients as their own control. This study may be limited by the duration of reassessment post-surgery. Further studies with larger sample size and using other psychosocial scales are needed to elucidate on the effectiveness of surgical intervention on psychosocial parameters in patients with GD.
Below are 17 studies that consist of literature reviews or guidelines that help advance knowledge about the effect of gender transition on transgender well-being. Click here to jump to the 4 studies that contain mixed or null findings on the effect of gender transition on transgender well-being. Click here Click here to jump to the 51 studies that found that gender transition improves the well-being of transgender people .
American psychological, 2015.

Guidelines for psychological practice with transgender and gender nonconforming people. (2015). American Psychologist, 70 (9), 832-864.
In 2015, the American Psychological Association adopted Guidelines for Psychological Practice with Transgender and Gender Nonconforming Clients in order to describe affirmative psychological practice with transgender and gender nonconforming (TGNC) clients. There are 16 guidelines in this document that guide TGNC-affirmative psychological practice across the lifespan, from TGNC children to older adults. The Guidelines are organized into five clusters: (a) foundational knowledge and awareness; (b) stigma, discrimination, and barriers to care; (c) lifespan development; (d) assessment, therapy, and intervention; and (e) research, education, and training. In addition, the guidelines provide attention to TGNC people across a range of gender and racial/ethnic identities. The psychological practice guidelines also attend to issues of research and how psychologists may address the many social inequities TGNC people experience.
Bockting et al., 2016

Bockting, W., Coleman, E., Deutsch, M. B., Guillamon, A., Meyer, W., et al. (2016). Adult development and quality of life of transgender and gender nonconforming people. Current Opinion in Endocrinology & Diabetes and Obesity , 23 (2), 188–197.
Purpose of review: Research on the health of transgender and gender nonconforming people has been limited with most of the work focusing on transition-related care and HIV. The present review summarizes research to date on the overall development and quality of life of transgender and gender nonconforming adults, and makes recommendations for future research. Recent findings: Pervasive stigma and discrimination attached to gender nonconformity affect the health of transgender people across the lifespan, particularly when it comes to mental health and well-being. Despite the related challenges, transgender and gender nonconforming people may develop resilience over time. Social support and affirmation of gender identity play herein a critical role. Although there is a growing awareness of diversity in gender identity and expression among this population, a comprehensive understanding of biopsychosocial development beyond the gender binary and beyond transition is lacking. Summary: Greater visibility of transgender people in society has revealed the need to understand and promote their health and quality of life broadly, including but not limited to gender dysphoria and HIV. This means addressing their needs in context of their families and communities, sexual and reproductive health, and successful aging. Research is needed to better understand what factors are associated with resilience and how it can be effectively promoted.
Byne et al., 2012

Byne, W., Bradley, S.J., Coleman, E., et al. (2012). Report of the American Psychiatric Association task force on treatment of gender identity disorder. Archives of Sexual Behavior, 41 (4): 759–796.
Both the diagnosis and treatment of Gender Identity Disorder (GID) are controversial. Although linked, they are separate issues and the DSM does not evaluate treatments. The Board of Trustees (BOT) of the American Psychiatric Association (APA), therefore, formed a Task Force charged to perform a critical review of the literature on the treatment of GID at different ages, to assess the quality of evidence pertaining to treatment, and to prepare a report that included an opinion as to whether or not sufficient credible literature exists for development of treatment recommendations by the APA. The literature on treatment of gender dysphoria in individuals with disorders of sex development was also assessed. The completed report was accepted by the BOT on September 11, 2011. The quality of evidence pertaining to most aspects of treatment in all subgroups was determined to be low; however, areas of broad clinical consensus were identified and were deemed sufficient to support recommendations for treatment in all subgroups. With subjective improvement as the primary outcome measure, current evidence was judged sufficient to support recommendations for adults in the form of an evidence-based APA Practice Guideline with gaps in the empirical data supplemented by clinical consensus. The report recommends that the APA take steps beyond drafting treatment recommendations. These include issuing position statements to clarify the APA’s position regarding the medical necessity of treatments for GID, the ethical bounds of treatments of gender variant minors, and the rights of persons of any age who are gender variant, transgender or transsexual.
Carroll, 1999

Carroll, R. A. (1999). Outcomes of treatment for gender dysphoria. Journal of Sex Education and Therapy , 24 (3), 128–136.
This paper reviews the empirical research on the psychosocial outcomes of treatment for gender dysphoria. Recent research has highlighted the heterogeneity of transgendered experiences. There are four possible outcomes for patients who present with the dilemma of gender dysphoria: an unresolved outcome, acceptance of one’s given gender, engaging in a cross-gender role on a part-time basis, and making a full-time transition to the other gender role. Clinical work, but not empirical research, suggests that some individuals with gender dysphoria may come to accept their given gender role through psychological treatment. Many individuals find that it is psychologically sufficient to express the transgendered part of themselves through such activities as cross-dressing or gender blending. The large body of research on the outcome of gender reassignment surgery indicates that, for the majority of those who undergo this process, the outcome is positive. Predictors of a good outcome include good pre-reassignment psychological adjustment, family support, at least 1 year of living in the desired role, consistent use of hormones, psychological treatment, and good surgical outcomes. The outcome literature provides strong support for adherence to the Standards of Care of the Harry Benjamin International Gender Dysphoria Association. Implications to be drawn from this research include an appreciation of the diversity of transgendered experience, the need for more research on non-reassignment resolutions to gender dysphoria, and the importance of assisting the transgendered individual to identify the resolution that best suits him or her.
Cohen-Kettenis and Gooren, 1999

Cohen-Kettenis, P. T., & Gooren, L. J. G. (1999). Transsexualism: A review of etiology, diagnosis and treatment. Journal of Psychosomatic Research , 46 (4), 315-333.
Transsexualism is considered to be the extreme end of the spectrum of gender identity disorders characterized by, among other things, a pursuit of sex reassignment surgery (SRS). The origins of transsexualism are still largely unclear. A first indication of anatomic brain differences between transsexuals and nontranssexuals has been found. Also, certain parental (rearing) factors seem to be associated with transsexualism. Some contradictory findings regarding etiology, psychopathology and success of SRS seem to be related to the fact that certain subtypes of transsexuals follow different developmental routes. The observations that psychotherapy is not helpful in altering a crystallized cross-gender identity and that certain transsexuals do not show severe psychopathology has led clinicians to adopt sex reassignment as a treatment option. In many countries, transsexuals are now treated according to the Standards of Care of the Harry Benjamin International Gender Dysphoria Association, a professional organization in the field of transsexualism. Research on postoperative functioning of transsexuals does not allow for unequivocal conclusions, but there is little doubt that sex reassignment substantially alleviates the suffering of transsexuals. However, SRS is no panacea. Psychotherapy may be needed to help transsexuals in adapting to the new situation or in dealing with issues that could not be addressed before treatment.
Coleman et al., 2012

Coleman, E., Bockting, W., Botzer, M., Cohen-Kettenis, P., DeCuypere, G., et al. (2012). Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. International Journal of Transgenderism , 13 (4), 165-232.
The Standards of Care (SOC) for the Health of Transsexual, Transgender, and Gender Nonconforming People is a publication of the World Professional Association for Transgender Health (WPATH). The overall goal of the SOC is to provide clinical guidance for health professionals to assist transsexual, transgender, and gender nonconforming people with safe and effective pathways to achieving lasting personal comfort with their gendered selves, in order to maximize their overall health, psychological well-being, and self-fulfillment. This assistance may include primary care, gynecologic and urologic care, reproductive options, voice and communication therapy, mental health services (e.g., assessment, counseling, psychotherapy), and hormonal and surgical treatments. The SOC are based on the best available science and expert professional consensus. Because most of the research and experience in this field comes from a North American and Western European perspective, adaptations of the SOC to other parts of the world are necessary. The SOC articulate standards of care while acknowledging the role of making informed choices and the value of harm reduction approaches. In addition, this version of the SOC recognizes that treatment for gender dysphoria i.e., discomfort or distress that is caused by a discrepancy between persons gender identity and that persons sex assigned at birth (and the associated gender role and/or primary and secondary sex characteristics) has become more individualized. Some individuals who present for care will have made significant self-directed progress towards gender role changes or other resolutions regarding their gender identity or gender dysphoria. Other individuals will require more intensive services. Health professionals can use the SOC to help patients consider the full range of health services open to them, in accordance with their clinical needs and goals for gender expression.
Committee on Health Care for Underserved, 2011

Committee Opinion No. 512: Health Care for Transgender Individuals. (2011). Obstetrics & Gynecology , 118 (6), 1454–1458.
Transgender individuals face harassment, discrimination, and rejection within our society. Lack of awareness, knowledge, and sensitivity in health care communities eventually leads to inadequate access to, underutilization of, and disparities within the health care system for this population. Although the care for these patients is often managed by a specialty team, obstetrician–gynecologists should be prepared to assist or refer transgender individuals with routine treatment and screening as well as hormonal and surgical therapies. The American College of Obstetricians and Gynecologists opposes discrimination on the basis of gender identity and urges public and private health insurance plans to cover the treatment of gender identity disorder.
Costa and Colizzi, 2016

Costa, R., & Colizzi, M. (2016). The effect of cross-sex hormonal treatment on gender dysphoria individuals’ mental health: A systematic review. Neuropsychiatric Disease and Treatment , 12 , 1953-1966.
Cross-sex hormonal treatment represents a main aspect of gender dysphoria health care pathway. However, it is still debated whether this intervention translates into a better mental well-being for the individual and which mechanisms may underlie this association. Although sex reassignment surgery has been the subject of extensive investigation, few studies have specifically focused on hormonal treatment in recent years. Here, we systematically review all studies examining the effect of cross-sex hormonal treatment on mental health and well-being in gender dysphoria. Research tends to support the evidence that hormone therapy reduces symptoms of anxiety and dissociation, lowering perceived and social distress and improving quality of life and self-esteem in both male-to-female and female-to-male individuals. Instead, compared to female-to-male individuals, hormone-treated male-to-female individuals seem to benefit more in terms of a reduction in their body uneasiness and personality-related psychopathology and an amelioration of their emotional functioning. Less consistent findings support an association between hormonal treatment and other mental health-related dimensions. In particular, depression, global psychopathology, and psychosocial functioning difficulties appear to reduce only in some studies, while others do not suggest any improvement in these domains. Results from longitudinal studies support more consistently the association between hormonal treatment and improved mental health. On the contrary, a number of cross-sectional studies do not support this evidence. This review provides possible biological explanation vs psychological explanation (direct effect vs indirect effect) for the hormonal treatment-induced better mental well-being. In conclusion, this review indicates that gender dysphoria-related mental distress may benefit from hormonal treatment intervention, suggesting a transient reaction to the nonsatisfaction connected to the incongruent body image rather than a stable psychiatric comorbidity. In this perspective, timely hormonal treatment intervention represents a crucial issue in gender dysphoria individuals’ mental health-related outcome.
Dhejne et al., 2016

Dhejne, C., Van Vlerken, R., Heylens, G., & Arcelus, J. (2016). Mental health and gender dysphoria: A review of the literature. International Review Of Psychiatry , 28 (1), 44-57.
Studies investigating the prevalence of psychiatric disorders among trans individuals have identified elevated rates of psychopathology. Research has also provided conflicting psychiatric outcomes following gender-confirming medical interventions. This review identifies 38 cross-sectional and longitudinal studies describing prevalence rates of psychiatric disorders and psychiatric outcomes, pre- and post-gender-confirming medical interventions, for people with gender dysphoria. It indicates that, although the levels of psychopathology and psychiatric disorders in trans people attending services at the time of assessment are higher than in the cis population, they do improve following gender-confirming medical intervention, in many cases reaching normative values. The main Axis I psychiatric disorders were found to be depression and anxiety disorder. Other major psychiatric disorders, such as schizophrenia and bipolar disorder, were rare and were no more prevalent than in the general population. There was conflicting evidence regarding gender differences: some studies found higher psychopathology in trans women, while others found no differences between gender groups. Although many studies were methodologically weak, and included people at different stages of transition within the same cohort of patients, overall this review indicates that trans people attending transgender health-care services appear to have a higher risk of psychiatric morbidity (that improves following treatment), and thus confirms the vulnerability of this population.
Gijs and Brewaeys, 2007

Gijs, L., & Brewaeys, A. (2007). Surgical treatment of gender dysphoria in adults and adolescents: Recent developments, effectiveness, and challenges. Annual Review of Sex Research , 18 (1), 178-224.
In 1990 Green and Fleming concluded that sex reassignment surgery (SRS) is an effective treatment for transsexuality because it reduced gender dysphoria drastically. Since 1990, many new outcome studies have been published, raising the question as to whether the conclusion of Green and Fleming still holds. After describing terminological and conceptual developments related to the treatment of gender identity disorder (GID), follow-up studies, including both adults and adolescents, of the outcomes of SRS are reviewed. Special attention is paid to the effects of SRS on gender dysphoria, sexuality, and regret. Despite methodological shortcomings of many of the studies, we conclude that SRS is an effective treatment for transsexualism and the only treatment that has been evaluated empirically with large clinical case series.
Gooren, 2011

Gooren, L. J. (2011). Care of transsexual persons. New England Journal of Medicine , 364 (13), 1251–1257.
This Journal feature begins with a case vignette highlighting a common clinical problem. Evidence supporting various strategies is then presented, followed by a review of formal guidelines, when they exist. The article ends with the author’s clinical recommendations. A healthy and successful 40-year-old man finds it increasingly difficult to live as a male. In childhood he preferred playing with girls and recalls feeling that he should have been one. Over time he has come to regard himself more and more as a female personality inhabiting a male body. After much agonizing, he has concluded that only sex reassignment can offer the peace of mind he craves. What would you advise? A healthy and successful 40-year-old man finds it increasingly difficult to live as a male. In childhood he preferred playing with girls and recalls feeling that he should have been one. Over time he has come to regard himself more and more as a female personality inhabiting a male body. After much agonizing, he has concluded that only sex reassignment can offer the peace of mind he craves. What would you advise?
Hembree et al., 2009

Hembree, W. C., Cohen-Kettenis, P., Delemarre-van de Waal, H. A., Gooren, L. J., Meyer, W., et al. (2009). Endocrine treatment of transsexual persons: An endocrine society clinical practice guideline. The Journal of Clinical Endocrinology & Metabolism, 94 (9), 3132–3154.
Objective: The aim was to formulate practice guidelines for endocrine treatment of transsexual persons. Evidence: This evidence-based guideline was developed using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) system to describe the strength of recommendations and the quality of evidence, which was low or very low. Consensus Process: Committees and members of The Endocrine Society, European Society of Endocrinology, European Society for Paediatric Endocrinology, Lawson Wilkins Pediatric Endocrine Society, and World Professional Association for Transgender Health commented on preliminary drafts of these guidelines. Conclusions: Transsexual persons seeking to develop the physical characteristics of the desired gender require a safe, effective hormone regimen that will 1) suppress endogenous hormone secretion determined by the person’s genetic/biologic sex and 2) maintain sex hormone levels within the normal range for the person’s desired gender. A mental health professional (MHP) must recommend endocrine treatment and participate in ongoing care throughout the endocrine transition and decision for surgical sex reassignment. The endocrinologist must confirm the diagnostic criteria the MHP used to make these recommendations. Because a diagnosis of transsexualism in a prepubertal child cannot be made with certainty, we do not recommend endocrine treatment of prepubertal children. We recommend treating transsexual adolescents (Tanner stage 2) by suppressing puberty with GnRH analogues until age 16 years old, after which cross-sex hormones may be given. We suggest suppressing endogenous sex hormones, maintaining physiologic levels of gender-appropriate sex hormones and monitoring for known risks in adult transsexual persons. Endocrine treatment of transsexual persons should include suppression of endogenous sex hormones, physiologic levels of gender-appropriate sex hormones, and suppression of puberty in adolescents (Tanner stage 2).
Michel et al., 2002

Michel, A., Ansseau, M., Legros, J., Pitchot, W., & Mormont, C. (2002). The transsexual: What about the future? European Psychiatry , 17 (6), 353-362.
Since the 1950s, sexual surgical reassignments have been frequently carried out. As this surgical therapeutic procedure is controversial, it seems important to explore the actual consequences of such an intervention and objectively evaluate its relevance. In this context, we have carried out a review of the literature. After looking at the methodological limitations of follow-up studies, the psychological, sexual, social, and professional futures of the individuals subject to a transsexual operation are presented. Finally, prognostic aspects are considered. In the literature, follow-up studies tend to show that surgical transformations have positive consequences for the subjects. In the majority of cases, transsexuals are very satisfied with their intervention and any difficulties experienced are often temporary and disappear within a year after the surgical transformation. Studies show that there is less than 1% of regrets, and a little more than 1% of suicides among operated subjects. The empirical research does not confirm the opinion that suicide is strongly associated with surgical transformation.
Murad et al., 2010

Murad, M. H., Elamin, M. B., Garcia, M. Z., Mullan, R. J., Murad, A., Erwin, P. J., & Montori, V. M. (2010). Hormonal therapy and sex reassignment: A systematic review and meta-analysis of quality of life and psychosocial outcomes. Clinical Endocrinology , 72 (2), 214-231.
Objective: To assess the prognosis of individuals with gender identity disorder (GID) receiving hormonal therapy as a part of sex reassignment in terms of quality of life and other self‐reported psychosocial outcomes. Methods: We searched electronic databases, bibliography of included studies and expert files. All study designs were included with no language restrictions. Reviewers working independently and in pairs selected studies using predetermined inclusion and exclusion criteria, extracted outcome and quality data. We used a random‐effects meta‐analysis to pool proportions and estimate the 95% confidence intervals (CIs). We estimated the proportion of between‐study heterogeneity not attributable to chance using the I2 statistic. Results: We identified 28 eligible studies. These studies enrolled 1833 participants with GID (1093 male‐to‐female, 801 female‐to‐male) who underwent sex reassignment that included hormonal therapies. All the studies were observational and most lacked controls. Pooling across studies shows that after sex reassignment, 80% of individuals with GID reported significant improvement in gender dysphoria (95% CI = 68–89%; 8 studies; I2 = 82%); 78% reported significant improvement in psychological symptoms (95% CI = 56–94%; 7 studies; I2 = 86%); 80% reported significant improvement in quality of life (95% CI = 72–88%; 16 studies; I2 = 78%); and 72% reported significant improvement in sexual function (95% CI = 60–81%; 15 studies; I2 = 78%). Conclusions: Very low quality evidence suggests that sex reassignment that includes hormonal interventions in individuals with GID likely improves gender dysphoria, psychological functioning and comorbidities, sexual function and overall quality of life.
Reisner et al., 2016

Reisner, S. L., Poteat, T., Keatley, J., Cabral, M., Mothopeng, T., et al. (2016). Global health burden and needs of transgender populations: A review. The Lancet , 388 (10042), 412-436.
Transgender people are a diverse population affected by a range of negative health indicators across high-income, middle-income, and low-income settings. Studies consistently document a high prevalence of adverse health outcomes in this population, including HIV and other sexually transmitted infections, mental health distress, and substance use and abuse. However, many other health areas remain understudied, population-based representative samples and longitudinal studies are few, and routine surveillance efforts for transgender population health are scarce. The absence of survey items with which to identify transgender respondents in general surveys often restricts the availability of data with which to estimate the magnitude of health inequities and characterise the population-level health of transgender people globally. Despite the limitations, there are sufficient data highlighting the unique biological, behavioural, social, and structural contextual factors surrounding health risks and resiliencies for transgender people. To mitigate these risks and foster resilience, a comprehensive approach is needed that includes gender affirmation as a public health framework, improved health systems and access to health care informed by high quality data, and effective partnerships with local transgender communities to ensure responsiveness of and cultural specificity in programming. Consideration of transgender health underscores the need to explicitly consider sex and gender pathways in epidemiological research and public health surveillance more broadly.
Schmidt and Levine, 2015

Schmidt, L., & Levine, R. (2015). Psychological Outcomes and Reproductive Issues Among Gender Dysphoric Individuals. Endocrinology and Metabolism Clinics of North America , 44 (4), 773-785.
Gender dysphoria is a condition in which a person experiences discrepancy between the natal anatomic sex and the gender he or she identifies with, resulting in internal distress and a desire to live as the preferred gender. There is increasing demand for treatment, which includes suppression of puberty, cross-sex hormone therapy, and sex reassignment surgery. This article reviews longitudinal outcome data evaluating psychological well-being and quality of life among transgender individuals who have undergone cross-sex hormone treatment or sex reassignment surgery. Proposed methodologies for diagnosis and initiation of treatment are discussed, and the effects of cross-sex hormones and sex reassignment surgery on future reproductive potential.
White Hughto and Reisner, 2016

White Hughto, J. M., & Reisner, S. L. (2016). A systematic review of the effects of hormone therapy on psychological functioning and quality of life in transgender individuals. Transgender Health , 1 (1), 21–31.
Objectives: To review evidence from prospective cohort studies of the relationship between hormone therapy and changes in psychological functioning and quality of life in transgender individuals accessing hormone therapy over time. Data Sources: MEDLINE, PsycINFO, and PubMed were searched for relevant studies from inception to November 2014. Reference lists of included studies were hand searched. Results: Three uncontrolled prospective cohort studies, enrolling 247 transgender adults (180 male-to-female [MTF], 67 female-to-male [FTM]) initiating hormone therapy for the treatment of gender identity disorder (prior diagnostic term for gender dysphoria), were identified. The studies measured exposure to hormone therapy and subsequent changes in mental health (e.g., depression, anxiety) and quality of life outcomes at follow-up. Two studies showed a significant improvement in psychological functioning at 3–6 months and 12 months compared with baseline after initiating hormone therapy. The third study showed improvements in quality of life outcomes 12 months after initiating hormone therapy for FTM and MTF participants; however, only MTF participants showed a statistically significant increase in general quality of life after initiating hormone therapy. Conclusions: Hormone therapy interventions to improve the mental health and quality of life in transgender people with gender dysphoria have not been evaluated in controlled trials. Low quality evidence suggests that hormone therapy may lead to improvements in psychological functioning. Prospective controlled trials are needed to investigate the effects of hormone therapy on the mental health of transgender people.
Share this:
Read our research on: Abortion | Podcasts | Election 2024
Regions & Countries

The Experiences, Challenges and Hopes of Transgender and Nonbinary U.S. Adults
Findings from pew research center focus groups, table of contents, introduction.
Transgender and nonbinary people have gained visibility in the U.S. in recent years as celebrities from Laverne Cox to Caitlyn Jenner to Elliot Page have spoken openly about their gender transitions. On March 30, 2022, the White House issued a proclamation recognizing Transgender Day of Visibility , the first time a U.S. president has done so.
More recently, singer and actor Janelle Monáe came out as nonbinary , while the U.S. State Department and Social Security Administration announced that Americans will be allowed to select “X” rather than “male” or “female” for their sex marker on their passport and Social Security applications.
At the same time, several states have enacted or are considering legislation that would limit the rights of transgender and nonbinary people . These include bills requiring people to use public bathrooms that correspond with the sex they were assigned at birth, prohibiting trans athletes from competing on teams that match their gender identity, and restricting the availability of health care to trans youth seeking to medically transition.
A new Pew Research Center survey finds that 1.6% of U.S. adults are transgender or nonbinary – that is, their gender is different from the sex they were assigned at birth. This includes people who describe themselves as a man, a woman or nonbinary, or who use terms such as gender fluid or agender to describe their gender. While relatively few U.S. adults are transgender, a growing share say they know someone who is (44% today vs. 37% in 2017 ). One-in-five say they know someone who doesn’t identify as a man or woman.
In order to better understand the experiences of transgender and nonbinary adults at a time when gender identity is at the center of many national debates, Pew Research Center conducted a series of focus groups with trans men, trans women and nonbinary adults on issues ranging from their gender journey, to how they navigate issues of gender in their day-to-day life, to what they see as the most pressing policy issues facing people who are trans or nonbinary. This is part of a larger study that includes a survey of the general public on their attitudes about gender identity and issues related to people who are transgender or nonbinary.
The terms transgender and trans are used interchangeably throughout this essay to refer to people whose gender is different from the sex they were assigned at birth. This includes, but is not limited to, transgender men (that is, men who were assigned female at birth) and transgender women (women who were assigned male at birth).
Nonbinary adults are defined here as those who are neither a man nor a woman or who aren’t strictly one or the other. While some nonbinary focus group participants sometimes use different terms to describe themselves, such as “gender queer,” “gender fluid” or “genderless,” all said the term “nonbinary” describes their gender in the screening questionnaire. Some, but not all, nonbinary participants also consider themselves to be transgender.
References to gender transitions relate to the process through which trans and nonbinary people express their gender as different from social expectations associated with the sex they were assigned at birth. This may include social, legal and medical transitions. The social aspect of a gender transition may include going by a new name or using different pronouns, or expressing their gender through their dress, mannerisms, gender roles or other ways. The legal aspect may include legally changing their name or changing their sex or gender designation on legal documents or identification. Medical care may include treatments such as hormone therapy, laser hair removal and/or surgery.
References to femme indicate feminine gender expression. This is often in contrast to “masc,” meaning masculine gender expression.
Cisgender is used to describe people whose gender matches the sex they were assigned at birth and who do not identify as transgender or nonbinary.
Misgendering is defined as referring to or addressing a person in ways that do not align with their gender identity, including using incorrect pronouns, titles (such as “sir” or “ma’am”), and other terms (such as “son” or “daughter”) that do not match their gender.
References to dysphoria may include feelings of distress due to the mismatch of one’s gender and sex assigned at birth, as well as a diagnosis of gender dysphoria , which is sometimes a prerequisite for access to health care and medical transitions.
The acronym LGBTQ+ refers to lesbian, gay, bisexual, transgender, queer (or, in some cases, questioning), and other sexual orientations or gender identities that are not straight or cisgender, such as intersex, asexual or pansexual.
Pew Research Center conducted this research to better understand the experiences and views of transgender and nonbinary U.S. adults. Because transgender and nonbinary people make up only about 1.6% of the adult U.S. population, this is a difficult population to reach with a probability-based, nationally representative survey. As an alternative, we conducted a series of focus groups with trans and nonbinary adults covering a variety of topics related to the trans and nonbinary experience. This allows us to go more in-depth on some of these topics than a survey would typically allow, and to share these experiences in the participants’ own words.
For this project, we conducted six online focus groups, with a total of 27 participants (four to five participants in each group), from March 8-10, 2022. Participants were recruited by targeted email outreach among a panel of adults who had previously said on a survey that they were transgender or nonbinary, as well as via connections through professional networks and LGBTQ+ organizations, followed by a screening call. Candidates were eligible if they met the technology requirements to participate in an online focus group and if they either said they consider themselves to be transgender or if they said their gender was nonbinary or another identity other than man or woman (regardless of whether or not they also said they were transgender). For more details, see the Methodology .
Participants who qualified were placed in groups as follows: one group of nonbinary adults only (with a nonbinary moderator); one group of trans women only (with a trans woman moderator); one group of trans men only (with a trans man moderator); and three groups with a mix of trans and nonbinary adults (with either a nonbinary moderator or a trans man moderator). All of the moderators had extensive experience facilitating groups, including with transgender and nonbinary participants.
The participants were a mix of ages, races/ethnicities, and were from all corners of the country. For a detailed breakdown of the participants’ demographic characteristics, see the Methodology .
The findings are not statistically representative and cannot be extrapolated to wider populations.
Some quotes have been lightly edited for clarity or to remove identifying details. In this essay, participants are identified as trans men, trans women, or nonbinary adults based on their answers to the screening questionnaire. These words don’t necessarily encompass all of the ways in which participants described their gender. Participants’ ages are grouped into the following categories: late teens; early/mid/late 20s, 30s and 40s; and 50s and 60s (those ages 50 to 69 were grouped into bigger “buckets” to better preserve their anonymity).
These focus groups were not designed to be representative of the entire population of trans and nonbinary U.S. adults, but the participants’ stories provide a glimpse into some of the experiences of people who are transgender and/or nonbinary. The groups included a total of 27 transgender and nonbinary adults from around the U.S. and ranging in age from late teens to mid-60s. Most currently live in an urban area, but about half said they grew up in a suburb. The groups included a mix of White, Black, Hispanic, Asian and multiracial American participants. See Methodology for more details.
Identity and the gender journey

Most focus group participants said they knew from an early age – many as young as preschool or elementary school – that there was something different about them, even if they didn’t have the words to describe what it was. Some described feeling like they didn’t fit in with other children of their sex but didn’t know exactly why. Others said they felt like they were in the wrong body.
“I remember preschool, [where] the boys were playing on one side and the girls were playing on the other, and I just had a moment where I realized what side I was supposed to be on and what side people thought I was supposed to be on. … Yeah, I always knew that I was male, since my earliest memories.” – Trans man, late 30s
“As a small child, like around kindergarten [or] first grade … I just was [fascinated] by how some people were small girls, and some people were small boys, and it was on my mind constantly. And I started to feel very uncomfortable, just existing as a young girl.” – Trans man, early 30s
“I was 9 and I was at day camp and I was changing with all the other 9-year-old girls … and I remember looking at everybody’s body around me and at my own body, and even though I was visually seeing the exact shapeless nine-year-old form, I literally thought to myself, ‘oh, maybe I was supposed to be a boy,’ even though I know I wasn’t seeing anything different. … And I remember being so unbothered by the thought, like not a panic, not like, ‘oh man, I’m so different, like everybody here I’m so different and this is terrible,’ I was like, ‘oh, maybe I was supposed to be a boy,’ and for some reason that exact quote really stuck in my memory.” – Nonbinary person, late 30s
“Since I was little, I felt as though I was a man who, when they were passing out bodies, someone made a goof and I got a female body instead of the male body that I should have had. But I was forced by society, especially at that time growing up, to just make my peace with having a female body.” – Nonbinary person, 50s
“I’ve known ever since I was little. I’m not really sure the age, but I just always knew when I put on boy clothes, I just felt so uncomfortable.” – Trans woman, late 30s
“It was probably as early as I can remember that I wasn’t like my brother or my father [and] not exactly like my girl cousins but I was something else, but I didn’t know what it was.” – Nonbinary person, 60s
Many participants were well into adulthood before they found the words to describe their gender. For those focus group participants, the path to self-discovery varied. Some described meeting someone who was transgender and relating to their experience; others described learning about people who are trans or nonbinary in college classes or by doing their own research.
“I read a Time magazine article … called ‘Homosexuality in America’ … in 1969. … Of course, we didn’t have language like we do now or people were not willing to use it … [but] it was kind of the first word that I had ever heard that resonated with me at all. So, I went to school and I took the magazine, we were doing show-and-tell, and I stood up in front of the class and said, ‘I am a homosexual.’ So that began my journey to figure this stuff out.” – Nonbinary person, 60s
“It wasn’t until maybe I was 20 or so when my friend started his transition where I was like, ‘Wow, that sounds very similar to the emotions and challenges I am going through with my own identity.’ … My whole life from a very young age I was confused, but I didn’t really put a name on it until I was about 20.” – Nonbinary person, late 20s
“I knew about drag queens, but I didn’t know what trans was until I got to college and was exposed to new things, and that was when I had a word for myself for the first time.” – Trans man, early 40s
“I thought that by figuring out that I was interested in women, identifying as lesbian, I thought [my anxiety and sadness] would dissipate in time, and that was me cracking the code. But then, when I got older, I left home for the first time. I started to meet other trans people in the world. That’s when I started to become equipped with the vocabulary. The understanding that this is a concept, and this makes sense. And that’s when I started to understand that I wasn’t cisgender.” – Trans man, early 30s
“When I took a human sexuality class in undergrad and I started learning about gender and different sexualities and things like that, I was like, ‘oh my god. I feel seen.’ So, that’s where I learned about it for the first time and started understanding how I identify.” – Nonbinary person, mid-20s
Focus group participants used a wide range of words to describe how they see their gender. For many nonbinary participants, the term “nonbinary” is more of an umbrella term, but when it comes to how they describe themselves, they tend to use words like “gender queer” or “gender fluid.” The word “queer” came up many times across different groups, often to describe anyone who is not straight or cisgender. Some trans men and women preferred just the terms “man” or “woman,” while some identified strongly with the term “transgender.” The graphic below shows just some of the words the participants used to describe their gender.
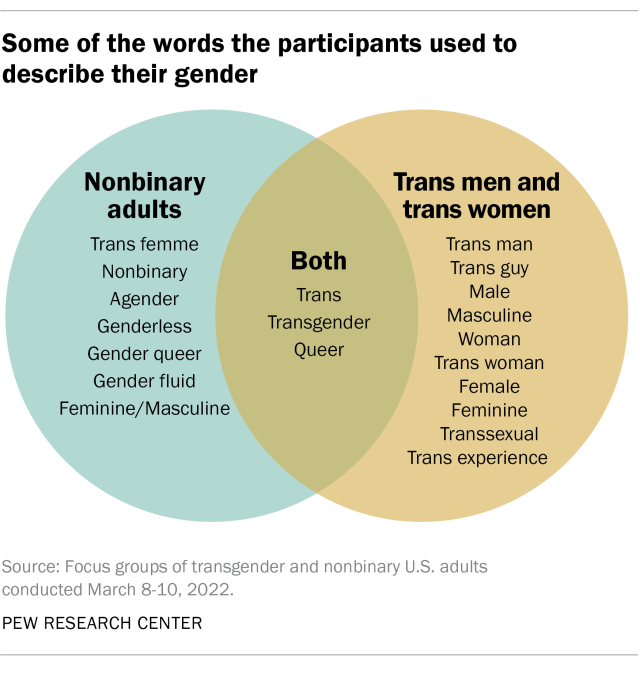
The way nonbinary people conceptualize their gender varies. Some said they feel like they’re both a man and a woman – and how much they feel like they are one or the other may change depending on the day or the circumstance. Others said they don’t feel like they are either a man or a woman, or that they don’t have a gender at all. Some, but not all, also identified with the term transgender.
“I had days where I would go out and just play with the boys and be one of the boys, and then there would be times that I would play with the girls and be one of the girls. And then I just never really knew what I was. I just knew that I would go back and forth.” – Nonbinary person, mid-20s
“Growing up with more of a masculine side or a feminine side, I just never was a fan of the labelling in terms of, ‘oh, this is a bit too masculine, you don’t wear jewelry, you don’t wear makeup, oh you’re not feminine enough.’ … I used to alternate just based on who I felt I was. So, on a certain day if I felt like wearing a dress, or a skirt versus on a different day, I felt like wearing what was considered men’s pants. … So, for me it’s always been both.” – Nonbinary person, mid-30s
“I feel like my gender is so amorphous and hard to hold and describe even. It’s been important to find words for it, to find the outlines of it, to see the shape of it, but it’s not something that I think about as who I am, because I’m more than just that.” – Nonbinary person, early 30s
“What words would I use to describe me? Genderless, if gender wasn’t a thing. … I guess if pronouns didn’t exist and you just called me [by my name]. That’s what my gender is. … And I do use nonbinary also, just because it feels easier, I guess.” – Nonbinary person, late 20s
Some participants said their gender is one of the most important parts of their identity, while others described it as one of many important parts or a small piece of how they see themselves. For some, the focus on gender can get tiring. Those who said gender isn’t a central – or at least not the most central – part of their identity mentioned race, ethnicity, religion and socioeconomic class as important aspects that shape their identity and experiences.
“It is tough because [gender] does affect every factor of your life. If you are doing medical transitioning then you have appointments, you have to pay for the appointments, you have to be working in a job that supports you to pay for those appointments. So, it is definitely integral, and it has a lot of branches. And it deals with how you act, how you relate to friends, you know, I am sure some of us can relate to having to come out multiple times in our lives. That is why sexuality and gender are very integral and I would definitely say I am proud of it. And I think being able to say that I am proud of it, and my gender, I guess is a very important part of my identity.” – Nonbinary person, late 20s
“Sometimes I get tired of thinking about my gender because I am actively [undergoing my medical transition]. So, it is a lot of things on my mind right now, constantly, and it sometimes gets very tiring. I just want to not have to think about it some days. So, I would say it’s, it’s probably in my top three [most important parts of my identity] – parent, Black, queer nonbinary.” – Nonbinary person, mid-40s
“I live in a town with a large queer and trans population and I don’t have to think about my gender most of the time other than having to come out as trans. But I’m poor and that colors everything. It’s not a chosen part of my identity but that part of my identity is a lot more influential than my gender.” – Trans man, early 40s
“My gender is very important to my identity because I feel that they go hand in hand. Now my identity is also broken down into other factors [like] character, personality and other stuff that make up the recipe for my identity. But my gender plays a big part of it. … It is important because it’s how I live my life every day. When I wake up in the morning, I do things as a woman.” – Trans woman, mid-40s
“I feel more strongly connected to my other identities outside of my gender, and I feel like parts of it’s just a more universal thing, like there’s a lot more people in my socioeconomic class and we have much more shared experiences.” – Trans man, late 30s
Some participants spoke about how their gender interacted with other aspects of their identity, such as their race, culture and religion. For some, being transgender or nonbinary can be at odds with other parts of their identity or background.
“Culturally I’m Dominican and Puerto Rican, a little bit of the macho machismo culture, in my family, and even now, if I’m going to be a man, I’ve got to be a certain type of man. So, I cannot just be who I’m meant to be or who I want myself to be, the human being that I am.” – Trans man, mid-30s
“[Judaism] is a very binary religion. There is a lot of things like for men to do and a lot of things for women to do. … So, it is hard for me now as a gender queer person, right, to connect on some levels with [my] religion … I have just now been exposed to a bunch of trans Jewish spaces online which is amazing.” – Nonbinary person, mid-40s
“Just being Indian American, I identify and love aspects of my culture and ethnicity, and I find them amazing and I identify with that, but it’s kind of separated. So, I identify with the culture, then I identify here in terms of gender and being who I am, but I kind of feel the necessity to separate the two, unfortunately.” – Nonbinary person, mid-30s
“I think it’s really me being a Black woman or a Black man that can sometimes be difficult. And also, my ethnic background too. It’s really rough for me with my family back home and things of that nature.” – Nonbinary person, mid-20s
Navigating gender day-to-day

For some, deciding how open to be about their gender identity can be a constant calculation. Some participants reported that they choose whether or not to disclose that they are trans or nonbinary in a given situation based on how safe or comfortable they feel and whether it’s necessary for other people to know. This also varies depending on whether the participant can easily pass as a cisgender man or woman (that is, they can blend in so that others assume them to be cisgender and don’t recognize that they are trans or nonbinary).
“It just depends on whether I feel like I have the energy to bring it up, or if it feels worth it to me like with doctors and stuff like that. I always bring it up with my therapists, my primary [care doctor], I feel like she would get it. I guess it does vary on the situation and my capacity level.” – Nonbinary person, late 20s
“I decide based on the person and based on the context, like if I feel comfortable enough to share that piece of myself with them, because I do have the privilege of being able to move through the world and be identified as cis[gender] if I want to. But then it is important to me – if you’re important to me, then you will know who I am and how I identify. Otherwise, if I don’t feel comfortable or safe then I might not.” – Nonbinary person, early 30s
“The expression of my gender doesn’t vary. Who I let in to know that I was formerly female – or formerly perceived as female – is kind of on a need to know basis.” – Trans man, 60s
“It’s important to me that people not see me as cis[gender], so I have to come out a lot when I’m around new people, and sometimes that’s challenging. … It’s not information that comes out in a normal conversation. You have to force it and that’s difficult sometimes.” – Trans man, early 40s
Work is one realm where many participants said they choose not to share that they are trans or nonbinary. In some cases, this is because they want to be recognized for their work rather than the fact that they are trans or nonbinary; in others, especially for nonbinary participants, they fear it will be perceived as unprofessional.
“It’s gotten a lot better recently, but I feel like when you’re nonbinary and you use they/them pronouns, it’s just seen as really unprofessional and has been for a lot of my life.” – Nonbinary person, early 30s
“Whether it’s LinkedIn or profiles [that] have been updated, I’ve noticed people’s resumes have their pronouns now. I don’t go that far because I just feel like it’s a professional environment, it’s nobody’s business.” – Nonbinary person, mid-30s
“I don’t necessarily volunteer the information just to make it public; I want to be recognized for my character, my skill set, in my work in other ways.” – Trans man, early 30s
Some focus group participants said they don’t mind answering questions about what it’s like to be trans or nonbinary but were wary of being seen as the token trans or nonbinary person in their workplace or among acquaintances. Whether or not they are comfortable answering these types of questions sometimes depends on who’s asking, why they want to know, and how personal the questions get.
“I’ve talked to [my cousin about being trans] a lot because she has a daughter, and her daughter wants to transition. So, she always will come to me asking questions.” – Trans woman, early 40s
“It is tough being considered the only resource for these topics, right? In my job, I would hate to call myself the token nonbinary, but I was the first nonbinary person that they hired and they were like, ‘Oh, my gosh, let me ask you all the questions as you are obviously the authority on the subject.’ And it is like, ‘No, that is a part of me, but there are so many other great resources.’” – Nonbinary person, late 20s
“I don’t want to be the token. I’m not going to be no spokesperson. If you have questions, I’m the first person you can ask. Absolutely. I don’t mind discussing. Ask me some of the hardest questions, because if you ask somebody else you might get you know your clock cleaned. So, ask me now … so you can be educated properly. Otherwise, I don’t believe it’s anybody’s business.” – Trans woman, early 40s
Most nonbinary participants said they use “they/them” as their pronouns, but some prefer alternatives. These alternatives include a combination of gendered and gender-neutral pronouns (like she/they) or simply preferring that others use one’s names rather than pronouns.
“If I could, I would just say my name is my pronoun, which I do in some spaces, but it just is not like a larger view. It feels like I’d rather have less labor on me in that regard, so I just say they/them.” – Nonbinary person, late 20s
“For me personally, I don’t get mad if someone calls me ‘he’ because I see what they’re looking at. They look and they see a guy. So, I don’t get upset. I know a few people who do … and they correct you. Me, I’m a little more fluid. So, that’s how it works for me.” – Nonbinary person, mid-30s
“I use they/she pronouns and I put ‘they’ first because that is what I think is most comfortable and it’s what I want to draw people’s attention to, because I’m 5 feet tall and 100 pounds so it’s not like I scream masculine at first sight, so I like putting ‘they’ first because otherwise people always default to ‘she.’ But I have ‘she’ in there, and I don’t know if I’d have ‘she’ in there if I had not had kids.” – Nonbinary person, late 30s
“Why is it so hard for people to think of me as nonbinary? I choose not to use only they/them pronouns because I do sometimes identify with ‘she.’ But I’m like, ‘Do I need to use they/them pronouns to be respected as nonbinary?’ Sometimes I feel like I should do that. But I don’t want to feel like I should do anything. I just want to be myself and have that be accepted and respected.” – Nonbinary person, early 30s
“I have a lot of patience for people, but [once someone in public used] they/them pronouns and I thanked them and they were like, ‘Yeah, I just figure I’d do it when I don’t know [someone’s] pronouns.’ And I’m like, ‘I love it, thank you.’” – Nonbinary person, early 30s
Transgender and nonbinary participants find affirmation of their gender identity and support in various places. Many cited their friends, chosen families (and, less commonly, their relatives), therapists or other health care providers, religion, or LGBTQ+ spaces as sources of support.
“I’m just not close with my family [of origin], but I have a huge chosen family that I love and that fully respects my identity.” – Nonbinary person, early 30s
“Before the pandemic I used to go out to bars a lot; there’s a queer bar in my town and it was a really nice place just being friends with everybody who went and everybody who worked there, it felt really nice you know, and just hearing everybody use the right pronouns for me it just felt really good.” – Nonbinary person, early 30s
“I don’t necessarily go to a lot of dedicated support groups, but I found that there’s kind of a good amount of support in areas or groups or fandoms for things that have a large LGBT population within them. Like certain shows or video games, where it’s just kind of a joke that all the gay people flock to this.” – Trans woman, late teens
“Being able to practice my religion in a location with a congregation that is just completely chill about it, or so far has been completely chill about it, has been really amazing.” – Nonbinary person, late 30s
Many participants shared specific moments they said were small in the grand scheme of things but made them feel accepted and affirmed. Examples included going on dates, gestures of acceptance by a friend or social group, or simply participating in everyday activities.
“I went on a date with a really good-looking, handsome guy. And he didn’t know that I was trans. But I told him, and we kept talking and hanging out. … That’s not the first time that I felt affirmed or felt like somebody is treating me as I present myself. But … he made me feel wanted and beautiful.” – Trans woman, late 30s
“I play [on a men’s rec league] hockey [team]. … I joined the league like right when I first transitioned and I showed up and I was … nervous with locker rooms and stuff, and they just accepted me as male right away.” – Trans man, late 30s
“I ended up going into a barbershop. … The barber was very welcoming, and talked to me as if I was just a casual customer and there was something that clicked within that moment where, figuring out my gender identity, I just wanted to exist in the world to do these natural things like other boys and men would do. So, there was just something exciting about that. It wasn’t a super macho masculine moment, … he just made me feel like I blended in.” – Trans man, early 30s
Participants also talked about negative experiences, such as being misgendered, either intentionally or unintentionally. For example, some shared instances where they were treated or addressed as a gender other than the gender that they identify as, such as people referring to them as “he” when they go by “she,” or where they were deadnamed, meaning they were called by the name they had before they transitioned.
“I get misgendered on the phone a lot and that’s really annoying. And then, even after I correct them, they keep doing it, sometimes on purpose and sometimes I think they’re just reading a script or something.” – Trans man, late 30s
“The times that I have been out, presenting femme, there is this very subconscious misgendering that people do and it can be very frustrating. [Once, at a restaurant,] I was dressed in makeup and nails and shoes and everything and still everyone was like, ‘Sir, what would you like?’ … Those little things – those microaggressions – they can really eat away at people.” – Nonbinary person, mid-40s
“People not calling me by the right name. My family is a big problem, they just won’t call me by my name, you know? Except for my nephew, who is of the Millennial generation, so at least he gets it.” – Nonbinary person, 60s
“I’m constantly misgendered when I go out places. I accept this – because of the way I look, people are going to perceive me as a woman and it doesn’t cause me huge dysphoria or anything, it’s just nice that the company that I keep does use the right pronouns.” – Nonbinary person, early 30s
Some participants also shared stories of discrimination, bias, humiliation, and even violence. These experiences ranged from employment discrimination to being outed (that is, someone else disclosing the fact that they are transgender or nonbinary without their permission) without their permission to physical attacks.
“I was on a date with this girl and I had to use the bathroom … and the janitor … wouldn’t let me use the men’s room, and he kept refusing to let me use the men’s room, so essentially, I ended up having to use the same bathroom as my date.” – Trans man, late 30s
“I’ve been denied employment due to my gender identity. I walked into a supermarket looking for jobs. … And they flat out didn’t let me apply. They didn’t even let me apply.” – Trans man, mid-30s
“[In high school,] this group of guys said, ‘[name] is gay.’ I ignored them but they literally threw me and tore my shirt from my back and pushed me to the ground and tried to strip me naked. And I had to fight for myself and use my bag to hit him in the face.” – Trans woman, late 20s
“I took a college course [after] I had my name changed legally and the instructor called me out in front of the class and called me a liar and outed me.” – Trans man, late 30s
Seeking medical care for gender transitions

Many, but not all, participants said they have received medical care , such as surgery or hormone therapy, as part of their gender transition. For those who haven’t undergone a medical transition, the reasons ranged from financial barriers to being nervous about medical procedures in general to simply not feeling that it was the right thing for them.
“For me to really to live my truth and live my identity, I had to have the surgery, which is why I went through it. It doesn’t mean [that others] have to, or that it will make you more or less of a woman because you have it. But for me to be comfortable, … that was a big part of it. And so, that’s why I felt I had to get it.” – Trans woman, early 40s
“I’m older and it’s an operation. … I’m just kind of scared, I guess. I’ve never had an operation. I mean, like any kind of operation. I’ve never been to the hospital or anything like that. So, it [is] just kind of scary. But I mean, I want to. I think about all the time. I guess have got to get the courage up to do it.” – Trans woman, early 40s
“I’ve decided that the dysphoria of a second puberty … would just be too much for me and I’m gender fluid enough where I’m happy, I guess.” – Nonbinary person, early 30s
“I’m too old to change anything, I mean I am what I am. [laughs]” – Nonbinary person, 60s
Many focus group participants who have sought medical treatment for their gender transition faced barriers, although some had positive experiences. For those who said there were barriers, the cost and the struggle to find sympathetic doctors were often cited as challenges.
“I was flat out turned down by the primary care physician who had to give the go-ahead to give me a referral to an endocrinologist; I was just shut down. That was it, end of story.” – Nonbinary person, 50s
“I have not had surgery, because I can’t access surgery. So unless I get breast cancer and have a double mastectomy, surgery is just not going to happen … because my health insurance wouldn’t cover something like that. … It would be an out-of-pocket plastic surgery expense and I can’t afford that at this time.” – Nonbinary person, 50s
“Why do I need the permission of a therapist to say, ‘This person’s identity is valid,’ before I can get the health care that I need to be me, that is vital for myself and for my way of life?” – Nonbinary person, mid-40s
“[My doctor] is basically the first person that actually embraced me and made me accept [who I am].” – Trans woman, late 20s
Many people who transitioned in previous decades described how access has gotten much easier in recent years. Some described relying on underground networks to learn which doctors would help them obtain medical care or where to obtain hormones illegally.
“It was hard financially because I started so long ago, just didn’t have access like that. Sometimes you have to try to go to Mexico or learn about someone in Mexico that was a pharmacist, I can remember that. That was a big thing, going through the border to Mexico, that was wild. So, it was just hard financially because they would charge so much for testosterone. And there was the whole bodybuilding community. If you were transitioning, you went to bodybuilders, and they would charge you five times what they got it [for], so it was kind of tough.” – Trans man, early 40s
“It was a lot harder to get a surgeon when I started transitioning; insurance was out of the question, there wasn’t really a national discussion around trans people and their particular medical needs. So, it was challenging having to pay everything out of pocket at a young age.” – Trans man, early 30s
“I guess it was hard for me to access hormones initially just because you had to jump through so many hoops, get letters, and then you had to find a provider that was willing to write it. And now it’s like people are getting it from their primary care doctor, which is great, but a very different experience than I had.” – Trans man, early 40s
Connections with the broader LGBTQ+ community

The discussions also touched on whether the participants feel a connection with a broader lesbian, gay, bisexual, transgender, and queer (LGBTQ+) community or with other people who are LGBTQ+. Views varied, with some saying they feel an immediate connection with other people who are LGBTQ+, even with those who aren’t trans or nonbinary, and others saying they don’t necessarily feel this way.
“It’s kind of a recurring joke where you can meet another LGBT person and it is like there is an immediate understanding, and you are basically talking and giving each other emotional support, like you have been friends for 10-plus years.” – Trans woman, late teens
“I don’t think it’s automatic friendship between queer people, there’s like a kinship, but I don’t think there’s automatic friendship or anything. I think it’s just normal, like, how normal people make friends, just based on common interests.” – Nonbinary person, early 30s
“I do think of myself as part of the LGBT [community] … I use the resources that are put in place for these communities, whether that’s different health care programs, support groups, they have the community centers. … So, I do consider myself to be part of this community, and I’m able to hopefully take when needed, as well as give back.” – Trans man, mid-30s
“I feel like that’s such an important part of being a part of the [LGBTQ+] alphabet soup community, that process of constantly learning and listening to each other and … growing and developing language together … I love that aspect of creating who we are together, learning and unlearning together, and I feel like that’s a part of at least the queer community spaces that I want to be in. That’s something that’s core to me.” – Nonbinary person, early 30s
“I identify as queer. I feel like I’m a part of the LGBT community. That’s more of a part of my identity than being trans. … Before I came out as trans, I identified as a lesbian. That was also a big part of my identity. So, that may be too why I feel like I’m more part of the LGB community.” – Trans man, early 40s
While many trans and nonbinary participants said they felt accepted by others in the LGBTQ+ community, some participants described their gender identity as a barrier to full acceptance. There was a sense among some participants that cisgender people who are lesbian, gay or bisexual don’t always accept people who are transgender or nonbinary.
“I would really like to be included in the [LGBTQ+] community. But I have seen some people try to separate the T from LGB … I’ve run into a few situations throughout my time navigating the [LGBTQ+] community where I’ve been perceived – and I just want to say that there’s nothing wrong with this – I’ve been perceived as like a more feminine or gay man in a social setting, even though I’m heterosexual. … But the minute that that person found out that I wasn’t a gay man … and that I was actually a transgender person, they became cold and just distancing themselves. And I’ve been in a lot of those types of circumstances where there’s that divide between the rest of the community.” – Trans man, early 30s
“There are some lesbians who see trans men as being traitors to womanhood. Those are not people that I really identify with or want to be close to.” – Trans man, early 40s
“It’s only in the past maybe dozen or so years, that an identity like gender fluid or gender queer was acceptable even within the LGBTQ+ community. … I tried to go to certain LGBTQ+ events as a trans man and, you know, I was not allowed in because I looked too female. The gay men would not allow me to participate.” – Nonbinary person, 50s
“Technically based on the letters [in the acronym LGBTQ+] I am part of that community, but I’ve felt discrimination, it’s very heavily exclusive to people who are either gay or lesbian and I think that’s true … for queer or bisexual or asexual, intersex … anybody who’s not like exclusively hardcore gay or lesbian. It’s very exclusive, like excluding to those people. … I feel like the BTQ is a separate group of people…. So, I identify with the second half of the letters as a separate subset.” – Trans man, late 30s
Policy and social change

When asked to name the most important policy or political issues facing transgender and nonbinary people in the United States today, many participants named basic needs such as housing, employment, and health care. Others cited recent legislation or policies related to people who are transgender that have made national news.
“Housing is a huge issue. Health care might be good in New York, it might be good in California, but … it’s not a national equality for trans folks. Health care is not equal across the states. Housing is not equal across the states. So, I think that the issues right now that we’re all facing is health care and housing. That’s the top, the most important things.” – Trans woman, early 40s
“Definitely education. I think that’s very important … Whether you identify as trans or not as a young child, it’s good to understand and know the different things under the umbrella, the queer umbrella. And it is also just a respect thing. And also, the violence that happens against trans and nonbinary people. I feel like educating them very young, that kind of helps – well, it is going to help because once you understand what’s going on and you see somebody that doesn’t identify the same as you, you’ll have that respect, or you’ll have that understanding and you’re less likely to be very violent towards them.” – Nonbinary person, mid-20s
“Employment is a big one. And I know that some areas, more metropolitan progressive-leaning areas, are really on top of this, but they’re trans people everywhere that are still being discriminated against. I think it’s a personal thing for me that goes back to my military service, but still, it’s just unfortunate. It’s an unfortunate reality.” – Trans man, early 30s
“I think just the strong intersectionality of trans people with mental health issues, or even physical health issues. … So in that way, accessing good health care or having good mental health.” – Trans man, late 30s
“I honestly think that the situation in Texas is the most pressing political and policy situation because it is a direct attack on the trans community. … And it is so insidious because it doesn’t just target bathrooms. This is saying that if you provide medical care to trans youth it is tantamount to child abuse. And it is so enraging because it is a known proven fact that access to gender affirming medical care saves lives. It saves the lives of trans youth. And trans youth have the highest suicide rate in the country.” – Nonbinary person, mid-40s
Participants had different takes on what gets in the way of progress on issues facing transgender and nonbinary people. Some pointed to the lack of knowledge surrounding the history of these issues or not knowing someone who is transgender or nonbinary. Others mentioned misconceptions people might have about transgender and nonbinary people that influence their political and policy perspectives.
“People who don’t know trans people, honestly … that’s the only barrier I can understand because people fear what they don’t know and then react to it a lot of the time.” – Nonbinary person, early 30s
“Sometimes even if they know someone, they still don’t consider them to be a human being, they are an ‘other,’ they are an ‘it,’ they are a ‘not like me,’ ‘not like my family,’ person and so they are put into a place socially where they can be treated badly.” – Nonbinary person, 50s
“Just the ignorance and misinformation and this quick fake social media fodder, where it encourages people who should not be part of the conversation to spread things that are not true.” – Trans man, late 30s
“Also, the political issues that face nonbinary people, it’s that people think nonbinary is some made-up thing to feel cool. It’s not to feel cool. And if someone does do it to feel cool, maybe they’re just doing that because they don’t feel comfortable within themselves.” – Nonbinary person, mid-30s
“There’s so much fear around it, and misunderstanding, and people thinking that if you’re talking to kids about gender and sexuality, that it’s sexual. And it’s like, we really need to break down that our bodies are not inherently sexual. We need to be able to talk with students and children about their bodies so that they can then feel empowered to understand themselves, advocate for themselves.” – Nonbinary person, early 30s
When asked what makes them hopeful for the future for trans and nonbinary people, some participants pointed to the way things in society have already changed and progress that has been made. For example, some mentioned greater representation and visibility of transgender and nonbinary people in entertainment and other industries, while others focused on changing societal views as things that give them hope for the future.
“I am hopeful about the future because I see so many of us coming out and being visible and representing and showing folks that we are not to stereotype.” – Trans woman, early 40s
“Also, even though celebrity is annoying, it’s still cool when people like Willow [Smith] or Billie Eilish or all these popstars that the kids really love are like, ‘I’m nonbinary, I’m queer,’ like a lot more progressive. … Even just more visibility in TV shows and movies, the more and more that happens the more it’s like, ‘Oh yeah, we are really here, you can’t not see us.’” – Nonbinary person, late 20s
“We shouldn’t have to look to the entertainment industry for role models, we shouldn’t have to, we should be able to look to our leaders, our political leaders, but I think, that’s what gives me hope. Soon, it’s going to become a nonissue, maybe in my lifetime.” – Trans man, 60s
“I have gotten a little bit into stand-up comedy in the last few weeks, and it is like the jokes that people made ten years ago are resurfacing online and people are enraged about it. They are saying like, ‘Oh, this is totally inappropriate.’ But that comes with the recognition that things have changed, and language has changed, and people are becoming more intolerant of allowing these things to occur. So that is why I am hopeful, is being able to see that progression and hopeful continued improvement on that front.” – Nonbinary person, late 20s
“I think because of the shift of what’s happening, how everything has become so normal, and people are being more open, and within the umbrella of queerness so many different things are happening, I think as we get more comfortable and we progress as a society, it’s just going to be better. So, people don’t have to hide who they are. So, that gives me hope.” – Nonbinary person, mid-20s
For many, young people are a source of hope. Several participants talked about younger generations being more accepting of those who are transgender or nonbinary and also being more accepted by their families if they themselves are trans or nonbinary.
“And then the other portion that gives me hope are the kids, because I work now with so many kids who are coming out as trans earlier and their families are embracing them and everything. … So I really am trusting in the young generation.” – Nonbinary person, 60s
“I mean kids don’t judge you the same way as adults do about gender, and they’re so expansive and have so much creativity. … So it’s just the kids, Gen Z, and it just makes me feel really, really hopeful.” – Nonbinary person, early 30s
“The youth, the youth. They understand almost intrinsically so much more about these things than I feel like my generation did. They give me so much hope for the future.” – Nonbinary person, early 30s
“I think future generations, just seeing this growing amount of support that they have, that it’s just going to keep improving … there’s an increase in visibility but there’s also an increase in support … like resources for parents where they can see that they don’t have to punish their kids. Their kids can grow up feeling like, ‘This is okay to be this way.’ And I feel like that’s not something that can be stopped.” – Trans man, late 30s
Additional materials
- Acknowledgments
- Methodology
Lead photo: (Angela Weiss/AFP via Getty Images)
Social Trends Monthly Newsletter
Sign up to to receive a monthly digest of the Center's latest research on the attitudes and behaviors of Americans in key realms of daily life
About Pew Research Center Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Transgender Identity and the Path to Self-Acceptance
Walter Bockting , a clinical psychologist and the founding director of the Gender and Sexuality Program at Columbia University Irving Medical Center (CUIMC), explains why more young people are identifying as transgender and discusses issues surrounding care.
Tell us about the Gender and Sexuality Program. What is its mission? Who does it serve?
We launched our program in 2018 to serve people identifying as transgender or nonbinary. It now offers comprehensive mental-health services to those who are questioning their gender or sexuality or struggling to navigate life with an identity that does not conform to traditional expectations. The majority of our patients are adolescents and teenagers, some of whom are considering medical treatments to align their bodies with their gender identity. We also see adults who are considering making such changes. And sometimes parents will come in with young children who appear to identify with another gender. They want to understand what their children are going through and how best to support them.
What exactly do the terms “transgender” and “nonbinary” mean?
Transgender is an umbrella term used to describe anyone with a gender identity that differs significantly from the sex they were assigned on their birth certificate, based on their outward anatomy. This can include people whose gender is the opposite of the sex they were assigned at birth — that is, a person assigned male at birth who identifies as a girl or woman or a person assigned female at birth who identifies as a boy or man. Transgender people may undergo medical interventions to align their appearance with their gender identity, or they may choose not to do so. Nonbinary individuals, who identify as neither boy nor girl, man nor woman, are generally considered part of the transgender community too. Their identities may combine aspects of masculinity or femininity or transcend these binary categories. Research conducted by my group and others has shown that gender identity and expression exist on a spectrum. For many people they are composed of different characteristics not easily reducible to being either male or female, masculine or feminine.
Is the transgender population growing?
There’s been a significant increase in people who openly identify as transgender or nonbinary over the past decade, especially among young people. Surveys indicate that 2 to 3 percent of adolescents and teenagers and about 5 percent of young adults in the United States now identify as transgender, with half or more of these individuals considering themselves nonbinary. Among older adults, that number is less than 1 percent, which is in line with historical trends dating back to the mid-twentieth century, when the concept of gender identity as distinct from biological sex first emerged.
What explains the rise?
Of course, there are cultural forces at work. As more and more people have embraced diverse gender identities, less stigma is associated with being trans. Which isn’t to say that it’s particularly easy to come out as transgender, because gender-nonconforming people are still among the most stigmatized in society. But transgender people feel freer to be themselves now, compared to previous decades. This is especially true for young people who’ve grown up seeing transgender individuals depicted positively in the media and meeting other transgender folks in school, on the job, or through friends and family. I think that older adults who grew up when it was less socially acceptable to be transgender are more likely to have suppressed or concealed any gender-identity issues they had, which is why you see a generational divide in these statistics.
How many Americans now undergo gender-affirming surgeries?
It’s difficult to say for sure, because the US has no centralized system for collecting data on such procedures, but it’s probably on the order of ten thousand people a year, the vast majority of whom are adults. Only a few hundred adolescents undergo gender-affirming surgeries annually, although thousands of young people do receive puberty suppressants or hormones to feminize or masculinize their bodies.
Before they perform gender-affirming surgery, physicians typically require a referral from a mental-health professional who can attest that a patient has thought the decision through, and in the past obtaining such a referral was more challenging than it is today. For example, until the mid-1990s, people who sought genital surgery were often turned down if they exhibited symptoms of severe anxiety or depression, which were seen as signs of mental instability. Now we know that feeling an incongruence between one’s gender identity and sex assigned at birth can contribute to mood disorders and that it is often appropriate to provide a person gender-affirming care at the same time that you’re treating them for other mental-health conditions.
People who opt for gender-affirming surgeries typically carry a diagnosis of gender dysphoria, a condition characterized by a discomfort with one’s sex assigned at birth that is so intense that it becomes debilitating, making daily life difficult if not impossible. Many, but not all, teenagers and young adults who now identify as transgender experience gender dysphoria. And having gender dysphoria does not necessarily lead a person to seek puberty suppression, hormone therapy, surgery, or any other gender-affirming medical interventions. Gender dysphoria plays out differently for each person.
Do your patients at the Gender and Sexuality Program tend to have dysphoria?
Most of them do, yes. We see people who are in a lot of emotional pain. In addition to experiencing incongruence between their gender identity and physical sex characteristics, which is incredibly frustrating, many are also socially isolated. Before coming to us, some have never spoken to anybody at length about what they’re going through. They might also have experienced bullying, harassment, violence, and discrimination. And it’s not uncommon for them to have internalized other people’s negative attitudes about transgender people and to feel ashamed of who they are. The cumulative stress can contribute to a wide range of mental-health issues, including substance abuse, suicidal thoughts, self-harm, anxiety, and mood disorders. When we help them come up with a plan to alleviate their gender dysphoria, we often need to address these issues, too.

What does treatment typically look like?
It starts with talk therapy to facilitate self-acceptance and identity exploration. We ask patients to describe how they’d ideally like to express their gender and what, if anything, is holding them back. If they haven’t lived openly as a transgender person yet, we might suggest that they first learn about the possibilities online and then try expressing their gender identity in a safe, private setting, like in the company of supportive friends or family members. After exploring their identity and expression in this way, some people may decide that they don’t need to change their gender identity in a formal sense. They might conclude that they’re simply uncomfortable with traditional gender norms and can be happy continuing to identify as a man or woman if they bend the rules to their liking a bit. But more often than not, among the patients we see, such experiences are affirming, encouraging people to move forward and continue transitioning. Then we might help them develop a plan for coming out at school or work, which can include preparing to address changes in pronoun use, how they dress, and bathroom access. We’ll work with their families to ensure that individuals get the emotional and social support they need. And if a patient is determined to change their body, we’ll help them think through the available options. We’ll also support them after they’ve made any physical changes, because the challenges of being transgender don’t end at that point.
You’ve been counseling transgender people and studying their lives for more than three decades. In particular, you’ve researched how their identities evolve over time. What have you learned?
One insight is that most transgender people, as they get older, become less interested in trying to pass as cisgender men and women and more comfortable identifying primarily as trans men, trans women, or nonbinary individuals. It can take them years to get to this point, because many transgender people, especially when they’re young, have internalized our society’s binary conception of gender and feel compelled to adopt the stereotypical gender expressions of men or women. They may initially think, “Well, I know I’m not a girl, so I must be a boy. Now I need to look and behave exactly like one!” This isn’t surprising. It’s human nature to seek a sense of belonging by carving out rather neatly defined identities for ourselves. And realizing that your gender identity is different or ambiguous can be nerve-racking. When my colleagues and I counsel transgender people, we encourage them to unearth and face some of this anxiety. We’ve found that by accepting the complexity and uniqueness of their gender identities, and by embracing the fact that, as transgender people, their experiences will always be unique and a bit different from cisgender people’s, they’re able to feel better about themselves and ultimately find more meaning in their lives.
Shortly before coming to Columbia in 2012, you served as president of the World Professional Association for Transgender Health (WPATH). In that role, you oversaw the creation of treatment guidelines that have made it easier for nonbinary people in many countries to access appropriate gender-affirming medical care.
Yes, these guidelines, which are now followed by most medical professionals and endorsed by their associations, stipulate that people who identify as nonbinary should have access to the same high-quality care as other transgender people. This is important because, as recently as the early 2000s, people who needed to change their bodies but didn’t necessarily want to look like cisgender men or women were often turned away. Maybe they just wanted to alter their chest, tone of voice, or hair-growth patterns while forgoing other procedures. If a physician asked if they identified as a man or woman and they responded, “Neither,” they might have been told, “Well, come back when you figure it out.” Now they’re treated equally and can access gender-affirming medical interventions appropriate to their identities and needs.
You’re also credited with improving access to care for transgender people who identify as gay, lesbian, or bisexual.
Yes, when I entered this field, another common requirement for getting gender-affirming surgery was to identify as heterosexual after transitioning. Can you believe that? In other words, you couldn’t be sexually attracted to members of your own gender identity but rather only to members of the sex you were originally assigned at birth. This was rooted in a twentieth-century theory called the “inversion hypothesis,” which held that the desire to transition one’s gender was the manifestation of intense same-sex attraction — basically, an extreme form of homosexuality. So, for example, a person who was assigned male at birth and sexually attracted to other men — and who had an unusually “de-masculinized and feminized” mind — might eventually want to become a woman. Transgender people who were brave enough to disclose their same-gender attractions faced significant barriers to accessing gender-affirming medical care. And transgender men who were attracted to men weren’t even thought to exist. But in the late 1980s and early 1990s, I published a series of papers documenting that transgender men who are attracted to men do exist and are quite happy and well-adjusted. This research, together with other scholars’ observations that transgender women often identify as lesbian, helped usher in a paradigm shift, where gender identity and sexual orientation were finally understood as separate components of one’s overall identity.
Today there is fierce debate about whether it has become too easy for adolescents to access gender-affirming medical care. In the past couple of years, more than twenty states have passed laws banning anyone under the age of eighteen from receiving puberty suppressants, hormone therapies, and surgeries. What do you make of this?
I’m shocked at how thoroughly the public discussion on this issue has become politicized and inundated by misinformation. Opponents of transgender rights, who’ve now organized themselves into a powerful movement, would have Americans believe that their kids are being brainwashed into thinking they’re transgender and greenlighted for medical procedures that they don’t need and will later regret. Of course, this isn’t true. Even among youth with gender dysphoria, only those with the most pronounced symptoms access medical interventions, usually after extensive counseling and therapy. What’s really happening is that young people in nearly half the United States are being denied access to health care that they desperately need, care that nearly every major medical organization in the country has deemed safe and essential. It’s a disgrace. Honestly, it makes me so upset that it’s difficult for me to talk about it.
“I’m shocked at how thoroughly the public discussion on this issue has become politicized and inundated by misinformation.”
When you meet a young person with gender dysphoria and hear them describe what they’re going through, you don’t forget it. It’s heartbreaking. I’m talking about kids who are overwhelmed by despair related to their sex characteristics. Who take showers in the dark to avoid seeing their bodies. Who can’t focus in school because they’re so upset about going through puberty. To these kids and their families, having access to gender-affirming care can feel like a matter of life or death.
Puberty blockers are now given to transgender kids as young as ten or eleven, which critics point out is a pretty tender age to be making medical decisions whose effects could last a lifetime.
Helping kids to change their bodies raises serious questions and concerns, there’s no doubt about it. I think that everyone working in the field of transgender health right now is asking themselves: Will any of these kids come to regret this decision? Will the puberty blockers cause any unintended effects later in life? Exactly how much therapy should these kids be getting before they transition? We don’t have conclusive answers to these questions yet. The best data available comes from a clinic in Amsterdam where gender-affirming medical care was first provided to adolescents in the 1990s. I grew up and trained in the Netherlands, and I’ve conducted research with some of the people who developed that program, which has shaped my thinking. In any case, the results from patients of that clinic are so far positive, which is why health-care providers throughout Europe and the US have since started offering puberty suppression and hormone therapies to adolescents. Hundreds of Dutch people who received gender-affirming care as youngsters decades ago are still being followed by researchers. Very few say they regret transitioning or show signs of serious unintended effects. And as a group, they have lower rates of anxiety and depression than other transgender people who attain access to gender-affirming care later in life or not at all.
What are you studying now?
For the past eight years, I’ve been leading a longitudinal study following the lives of more than three hundred transgender people, who now range in age from about twenty to ninety, in New York City, San Francisco, and Atlanta. My colleagues and I are hoping to follow these participants for years to come. We want to learn what aspects of their lives are most challenging, what brings them happiness and contentment, and how they develop resilience in the face of stigma, discrimination, and the associated stress. Among our discoveries so far is that transgender people who maintain close friendships with other transgender people are happier and healthier overall, as are those who are in regular contact with their parents, siblings, or other close family members and friends.
The importance of family, I think, is particularly interesting. Other studies have shown that transgender people are often rejected by their families or subjected to such awful abuse at home that they have to cut ties. Some of our participants have experienced this too. But many others told us things like, “You know, my folks weren’t very nice to me at first and actually said some terrible things. But I was patient and left the door open, and eventually they came around and accepted me. And I’m glad I gave them a chance, for my own sake and theirs.”
That’s inspiring. Do you share those types of stories with your patients?
I do. I’m always telling my patients about the dignity, strength, and courage of other transgender people. I’ll recommend movies, TV shows, and books, and I’ll tell them anecdotes about some of the amazing patients and research participants I’ve known over the years. When they’re ready, I’ll help them connect meaningfully with other transgender people in group therapy and support meetings. And I’ll tell them, “I know that being transgender isn’t easy — but it’s also exciting, beautiful, and, yes, fabulous. And you are now among these fabulous people who, just by being themselves and holding their heads up high, are changing the world.”
This article appears in the Winter 2023-23 print edition of Columbia Magazine with the title "Beyond the Binary."
More From Health & Medicine

Sign up for our newsletter.
General Data Protection Regulation
Columbia University Privacy Notice
Find anything you save across the site in your account
We Need to Change the Terms of the Debate on Trans Kids
By Masha Gessen

Every night, when I walk my dog, several strangers, similarly tethered, will ask me the same two questions: “Boy or girl?” and “How old?” The pragmatic meaning of these questions escapes me. The answers do not inform the interactions between our dogs, nor do they tell a story. Wouldn’t it be more interesting to learn whether the dog was a longtime family member or a pandemic puppy, whether it lived with other pets, how much exercise it got or desired, how it tolerated last summer’s orgy of fireworks, or to learn at least the dog’s name? These are the questions I usually ask other dog owners as our pets sniff each other, but in response I am still asked—hundreds of times a year—about my dog’s age and gender. These categories, it seems, are so central to the way we organize the world around us that we apply them to everything, including random dogs in the night.
No wonder, then, that attempts to subvert these two categories make people uncomfortable and, often, scared and angry. This happens when children act with particular independence; when people challenge the norms of gender; and, especially, when both of these things happen at once, as in the case of trans children. In December, the British High Court of Justice ruled on the question of whether young people under the age of eighteen are capable of giving informed consent to treatments that forestall puberty. Such treatments can be prescribed to children given a diagnosis of gender dysphoria, both to alleviate discomfort that can stem from the physical changes brought on by puberty and to pave the way for later medical gender transition. The court ruled that children under sixteen cannot consent to such treatment because they are unable to grasp its long-term consequences, and cast doubt on the ability of young people between the ages of sixteen and eighteen to give informed consent. The decision effectively bars British children and adolescents from transitioning medically.
British media coverage of the High Court’s decision was generally positive. “Other countries should learn from a transgender verdict in England” the Economist wrote . “The court was correct to curb a disturbing trend,” the Observer wrote . Later in the month, the BBC’s media editor, Amol Rajan, published his list of the five best essays of the year, among them J. K. Rowling’s piece explaining her position “on sex and gender issues.” Rowling, who presents herself as a defender of bathrooms, dressing rooms, and other “single-sex spaces” against trans women, wrote that she was “concerned about the huge explosion in young women wishing to transition and also about the increasing numbers who seem to be detransitioning.” She cited the controversial hypothesis that some adolescent transitions may stem from a kind of social contagion. Had transition been an option during her own adolescence, Rowling wrote, she might have chosen it as a way to deal with her own mental-health challenges: “The allure of escaping womanhood would have been huge.”
In the United States, this line of argument has been advanced by Abigail Shrier, a writer for the Wall Street Journal who published a book last year titled “ Irreversible Damage: The Transgender Craze Seducing Our Daughters .” The cover art is a drawing of a prepubescent girl with a giant round cutout where her abdomen should be. The book is currently ranked “#1 Bestseller in Transgender Studies” on Amazon. Bills that would ban trans care for young people have already been prefiled for this year’s legislative sessions in Alabama, Texas, and Missouri; last year, a similar bill was defeated in South Dakota, thanks to opposition from the pharmaceutical industry. When such bills contain language explaining their rationale, they make similar arguments to those of Rowling, Shrier, and the British High Court: that the effects of trans care are irreversible and that many people who want to transition when they are adolescents will ultimately choose to identify with the gender they were assigned at birth.
The state bills tend to lump all kinds of trans care—puberty blockers, cross-sex hormones, and surgeries—together. As a narrative, this is not unreasonable: the vast majority of people who receive puberty blockers do go on to take cross-sex hormones, and many choose surgery. But the short- and long-term effects of the medical interventions are markedly different. Agonists of gonadotropin-releasing hormone, originally developed to treat prostate cancer and endometriosis in adults, can have the effect of preventing puberty-related changes: genital growth, breasts, body and facial hair, and voice changes. Estrogen promotes breast growth, and testosterone will likely lead to a lower voice and more body and facial hair; both kinds of hormones affect fat and muscle distribution. The effects of hormones are not as predictable—and the line between reversible and irreversible effects of hormone treatments isn’t as clear—as their opponents seem to think, but a person whose puberty is effectively prevented and who later receives cross-sex hormones is unlikely to preserve their fertility. Some European researchers are experimenting with reserving gonad tissue that may be used to create biological progeny later (similar efforts are made with children undergoing cancer treatment that is likely to render them infertile). Natal males and females who transition during adolescence forfeit their fertility equally, but Rowling, Shirer, and other opponents of pediatric trans care seem particularly concerned with people they see as girls clamoring to escape womanhood. (The lead plaintiff in the British case, Keira Bell, who was assigned female at birth, began taking puberty blockers at sixteen and testosterone at seventeen and had a double mastectomy at twenty. Bell later transitioned back to being female.)
“Women and children are always mentioned in the same breath,” the visionary feminist activist Shulamith Firestone observed in the book “ The Dialectic of Sex: The Case for Feminist Revolution ,” from 1970. “I submit . . . that the nature of this bond is no more than shared oppression. And that moreover this oppression is intertwined and mutually reinforcing in such complex ways that we will be unable to speak of the liberation of women without also discussing the liberation of children, and vice versa.” Firestone noted that women and children were inextricably linked not only by the women’s duty of childbearing and child rearing but by the obligation, for both groups, to maintain innocence, fragility, immaturity, and dependence on others. She saw the path to liberation in divorcing the reproductive function from women’s biology, and in abolishing childhood. One might argue that young people who seek trans care are pursuing both of these projects, and that is why they inspire such panicked opposition.
Yet the arguments in favor of trans care for young people are usually not so much liberationist as they are determinist. Advocates generally claim that trans children are innately, immutably different from cis children and that access to medical transition is essential for staving off depression and even suicide. “The fear that puberty per se can be a threat to life for transgender children permeates pediatric trans care,” Sahar Sadjadi wrote in an essay in Transgender Studies Quarterly last year. (Sadjadi is a medical anthropologist who has studied clinical practices for transitioning and other non-gender-conforming children for a decade.) This type of advocacy, she argues, builds on two long-standing tendencies: the habit of thinking of gender transition as primarily a medical process, and the habit of grounding L.G.B.T. civil-rights claims in “born this way” rhetoric. These habits make for a compelling, easily digestible argument: transness is an immutable characteristic, and denying young people access to medical transition can be tantamount to killing them. This argument is grounded in the lived experience of some advocates, whose own medical transition relieved extreme anguish. But an argument rooted in despair cannot and should not represent all young trans people.
When we are not talking about children and adolescents, trans people talk about a much broader range of options than medical transition—a spectrum of gender expression more varied than the linear path of puberty blockers followed by cross-sex hormones. Some adult trans people consider themselves binary, and some don’t; some use hormones and have surgeries, some choose one or the other, some try different approaches, and some eschew medical interventions altogether. Medical intervention requires a diagnosis of gender dysphoria, even if the person is paying for surgery and hormones out of pocket. In general, though, adults are not required to prove that they have always felt like they were in the wrong body (although some have).
If we hold to the premise that transness is an immutable, inborn trait, it follows that every young person who chooses to detransition will undermine the case any other young person may have for seeking trans care. “The main debate has become whether these young people will ‘persevere,’ ” Sadjadi told me by Zoom from Montreal, where she is on the faculty at McGill University’s Department of Social Studies of Medicine. “I think this is the wrong question. Gender changes with age. The gender of a fifty-year-old woman is not the same as of a five-year-old girl. Nothing terrible happens if a person transitions again, which is how I think we should think about it.”
The British High Court’s decision makes a point that appears compelling and compassionate. A child, the panel decided, cannot fully comprehend the meaning of infertility and possible loss of sexual function that come with transitioning at a young age. (One concern is that puberty blockers prevent genital growth, making gender-affirming bottom surgery more complicated.) But this argument rests not only on a narrow definition of sexual pleasure but on an impossible ideal of comprehension: we can never fully imagine loss, especially the loss of something we’ve never had. Keira Bell testified, “It is only until recently that I have started to think about having children and if that is ever a possibility, I have to live with the fact that I will not be able to breastfeed my children. I still do not believe that I have fully processed the surgical procedure that I had to remove my breasts and how major it really was.” As heartbreaking as that admission is, all available data indicate that such regrets are exceedingly rare. That one person’s testimony convinced the court to make a decision that will affect untold thousands tells us more about the pull that human reproduction has on the imagination than it does about gender transition.
“People change their minds about all kinds of decisions,” Sadjadi added. Hers is not an argument against thinking of transition as a serious, consequential decision, but rather an argument for viewing gender transition as one of the many important choices some people face. People—including young people, acting legally, with their parents’ support—choose to have babies, move continents, subject themselves to extreme physical risk by engaging in certain sports, make what often amounts to commitments to lifelong medical intervention with S.S.R.I.s for depression or stimulants for attention deficit hyperactivity disorder, join the R.O.T.C. or the National Guard. None of these decisions is just like the decision to transition. But are they really so much lighter, so much less consequential, that the possibility of one person reversing course shouldn’t prevent others from making the same choices?
In her 1970 book, Firestone discussed the arbitrary historical boundaries of childhood. In other eras, boys would be expected to abandon toys and take up adult vocations at the age of seven; girls were historically married off as soon as they went through puberty. Firestone’s point was that childhood was a relatively new category, and an unstable one. Our own ideas of maturity are no less arbitrary than our ancestors’. We know that a fifteen-year-old is probably better equipped to make life decisions than is a nine-year-old, who is still vastly more experienced and informed than a four-year-old. But for the purposes of the law, we lump them in the same category. An eighteen-year-old, on the other hand, is deemed capable of making the full range of life choices—except for whether to ingest alcohol. There is little doubt, however, that the experience, wisdom, and skill for assessing risk and making decisions continue to accumulate well past middle age. If you think about it, a fifty-year-old who has experienced life in a particular gender is in a much better position to make a decision about transition than is a twenty-year-old. But at that point, it’s too late to decide to be a young person in the other gender, and this, too, is irreversible. I began my own transition at fifty, long after experiencing the misery of pregnancy and the incomparable joy of breastfeeding. I have no regrets. Had I had the option of transitioning as a teen-ager, I would have chosen to do so—and I am almost certain that I would have had no regrets then, either, because I would have had a different life.
Sadjadi, who was a physician before she became an anthropologist, has written that puberty blockers are not as medically inconsequential as they are often portrayed. Although they appear to have no long-term physical effects if they are used for a short time (a year or less), some studies suggest that they can have long-term detrimental effects for the musculoskeletal system if they are used for three or four years. (Long-term data comes from the use of puberty blockers to forestall what is deemed “precocious” puberty, occurring in children under the age of nine.) The manufacturer of Lupron, the drug most commonly used as a puberty blocker, warns of depression as a possible side effect. Sadjadi suggested freeing gender transition in young people from the assumption that they will necessarily take puberty blockers. For some kids, she said, it may be worth considering social transition as the first or even only step. Social transition is often conspicuously absent from the menu offered to adolescents. For others, cross-sex hormones may be preferable to puberty blockers, which are supposed to “buy time” before a child is deemed old enough to make the commitment to transitioning. There is not enough data to say whether and when these may be the better care options.
To be able to talk about a range of transition options, at different times in life, we would need to change the terms of the debate. We would need to view both age and gender on a continuum, not as binary states. None of us has ever been as innocent and ignorant as the children of our imagination, and none of us will ever be as wise and competent as the adults we make ourselves out to be. What if we saw ourselves as always changing, always uncertain, but always capable of making choices? What if we accepted that some losses are desirable and some are regrettable, and that we can’t always know the difference? What if we knew that we are always changing not only as individuals but as societies, and the categories we use to sort ourselves mutate faster than we realize? Then maybe we could have a real conversation about trans care for young people.
By signing up, you agree to our User Agreement and Privacy Policy & Cookie Statement . This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.

By Rebecca Mead

By Jessica Winter
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- NEWS FEATURE
- 24 April 2019
The largest study involving transgender people is providing long-sought insights about their health
- Sara Reardon
You can also search for this author in PubMed Google Scholar
Benita Arren wishes that the human body came with instructions. “We have a manual with every little thing we buy, in eight languages, but not for myself,” she says. About a decade ago, Arren was struggling with inner conflict. Designated male at birth, she had secretly dressed up in her mother’s clothes as a child, but she suppressed her feelings for decades. Then in her forties, married with two children and busy with a job in Antwerp, Belgium, she found them resurfacing. The masculine persona in her head — how she had long known herself to be — was falling away, leaving her feeling as though she had no personality at all. “Your consciousness is not fast enough to understand all those emotions,” she says.
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
185,98 € per year
only 3,65 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
Nature 568 , 446-449 (2019)
doi: https://doi.org/10.1038/d41586-019-01237-z
Heylens, G. et al. J. Sex. Med. 11 , 119–126 (2014).
Article PubMed Google Scholar
Burke, S. M. et al. J. Psychiatry Neurosci . 41 , 395–404 (2016).
Getahun, D. Ann. Intern. Med. 169 , 205–213 (2018).
Download references
Reprints and permissions
Related Articles

- Human behaviour
- Health care

Innate immunity in neurons makes memories persist
News & Views 27 MAR 24

Memories are made by breaking DNA — and fixing it
News 27 MAR 24

Ketamine is in the spotlight thanks to Elon Musk — but is it the right treatment for depression?
News Explainer 20 MAR 24

Artificial intelligence and illusions of understanding in scientific research
Perspective 06 MAR 24

Online images amplify gender bias
Article 14 FEB 24

Economists count the cost of ‘risky’ science
Career News 06 FEB 24

Anti-ageing antibodies revive the immune system

Abortion-pill challenge provokes doubt from US Supreme Court
News 26 MAR 24

The future of at-home molecular testing
Outlook 21 MAR 24
Senior Scientist, Research
Be part of something altogether life-changing! Working at Cytiva means being at the forefront of providing new solutions to transform human heal...
Vancouver, British Columbia (CA)
Postdoctoral positions in the integrative structural biology of cancer and immunity
Postdoctoral positions in the integrative structural biology study of signaling complexes important in cancer and the immune system
Farmington, Connecticut (US)
University of Connecticut Health Center (UCHC)
Faculty Positions & Postdocs at Institute of Physics (IOP), Chinese Academy of Sciences
IOP is the leading research institute in China in condensed matter physics and related fields. Through the steadfast efforts of generations of scie...
Beijing, China
Institute of Physics (IOP), Chinese Academy of Sciences (CAS)
Postdoctoral Scholar - PHAST Alzheimer
Memphis, Tennessee
The University of Tennessee Health Science Center (UTHSC)
Postdoctoral Associate- Neurodevelopmental Disease
Houston, Texas (US)
Baylor College of Medicine (BCM)
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Share full article
Advertisement
Supported by
The Debate Over Transgender Care and Detransitioning
Readers discuss a column by Pamela Paul about children with gender dysphoria who regret their transitions.

To the Editor:
Re “ Gender Dysphoric Kids Deserve Better Care ,” by Pamela Paul (column, Feb. 4):
I’m an L.G.B.T.Q.+ teenager. Ms. Paul cites stories of detransitioners as if they are damning to the practice of gender-affirming care as a whole. Not all detransitioners regret their transition, and not all transgender people will medically transition. An overwhelming 98 percent of people who started their transition care as youths continue into adulthood, per a 2022 study from the Netherlands published in The Lancet.
Speaking from experience, my peers and friends who have undergone medical transitions have never “regretted” it, and after beginning care, their quality of life greatly improved. If Ms. Paul wants to demonize a procedure with a high rate of regret, she should look toward knee replacement, where one in five people end up dissatisfied .
By writing this article, Ms. Paul further stigmatizes health care for transgender people. Transition care may be good for some people. It may not be for others. This is a basic premise of medicine — people must have the right to make decisions with their doctors on what is right for them.
What we do know is that transgender youth are under attack across the nation. Texas’s attorney general, Ken Paxton, last month demanded records from providers outside his state to single out hospitals or clinics that have treated transgender youth from Texas.
I fear for my future. I fear for my friends and their futures.
By continuing to harbor this dangerous rhetoric in her pieces, Ms. Paul makes it harder and harder for trans people to get the care that they desperately need as lawmakers across the country clamp down on our rights. I understand her concern, but it is misplaced.
Charles Yale Omaha
I was a trans child. From 12 to 17, I identified as male and was entrenched in the online world of radical trans activism. And, like many other female detransitioners, I am a lesbian, a survivor of childhood sexual abuse and on the autism spectrum.
My doctors knew all these things, and prescribed me testosterone at 15 anyway with minimal questioning. When I was approved for “top surgery,” I had just been released from a two-month stay in a teen rehabilitation facility after suffering severe suicidal ideation.
Now, I’m 17, and I feel as if my adolescence was taken from me. When I decided to detransition, it felt like leaving a cult. I was quickly forced into the role of “outsider.”
Detransitioners are viewed as just a rare minority who made a mistake. It’s all our fault for not thinking our transition through, despite doctors and trans activists assuring us every step of the way that this was the only way we could ever be happy.
I was officially diagnosed with gender dysphoria and was in many ways the textbook presentation of transgender identity, and I still ended up growing out of it. If it can happen to me, it can certainly happen to the thousands of teenagers who get on hormones after identifying as trans for significantly shorter periods of time.
Our stories have to be listened to and taken seriously, and I am grateful for people like Pamela Paul who are willing to give us a chance.
Maxine Doak Doylestown, Pa.
As the father of a healthy, thriving late 20s trans and nonbinary child who transitioned in their teens, I’m appalled at the lack of credible, large-scale research in Pamela Paul’s column.
We parents notice the media’s drumbeat of detransition stories, with no similar focus on the overwhelming majority of trans people who lead healthy, fulfilling and successful lives — thanks in large part to their ability to access proven and affirming health care.
The research done to date on whether the majority of people who received gender-affirming medical care have any regrets is crystal clear — overwhelmingly good, positive news.
In a meta study across 7,928 people in 13 countries who had received gender-affirming medical care, only 1 percent expressed regret.
We are begging you to cover positive and affirming stories of trans people who are leading “normal” happy and comfortable lives thanks to the care they’ve received.
Tom Murphy Long Beach, Calif.
Thank you so much for having the courage to print Pamela Paul’s piece on detransitioning. I am the mother of a socially transitioning college-aged person (assigned female at birth). My child is gay and has autism, A.D.H.D., major depressive disorder and anxiety. They exhibited no gender dysphoria or nonconforming behaviors until their junior year of high school.
Their mental health struggles are extremely complex, but we have been told by multiple therapists to be affirming and not question their identity. I am concerned that the challenges they are facing will not be resolved through gender-affirming care alone. My kid is desperate for a fix for why they don’t fit in, why they don’t feel well. They are searching for community and exploring their identity.
I fear that the therapy they receive will focus too much on gender affirmation and miss the unique and complex person that they are while leading them down a path that will result in more harm than good.
Angie W. Atascadero, Calif. The writer’s last name has been withheld to protect the privacy of her child.
Pamela Paul’s column misses an opportunity to shed light on the very complex and nuanced topic of adolescent mental health and gender identity. Just like the gender binary itself, the black-and-white thinking laid out in the piece is overplayed, outdated and simply unhelpful.
In my work as a parent of a trans kid — and the leader of a support group for parents/caregivers of trans kids — I have observed the very real phenomenon of teens questioning their gender at the onset of puberty. It makes sense because this is the time when kids’ bodies are changing, and they are being slotted into binary gender lanes.
What I see is a generation of kids who simply do not buy into gender binary norms. All of us old folks can sit around wringing our hands about transitions and detransitions. But the social construct of gender is changing.
Instead of fear mongering and drawing lines in the sand, the Gray Lady might dust herself off and put her Opinion section to better use illuminating the societal changes in the way we think about gender.
Kate Rubick Portland, Ore. The writer is chair of the Portland chapter of TransParent .
As someone who is seen as a “detransitioner,” I reject this label. I was on hormone replacement therapy and presented as a woman for five years, starting when I was 27. That period turned out to be one of the most emotionally and intellectually fruitful of my life thus far, and it’s for this reason that I don’t regret any of it.
I stopped my hormone regimen because I had doubts about the idea of marrying a straight man, since they’re generally less funny than gay men. However, I continued to have access to prescription estrogen, and would dabble for months at a time when I felt I wanted to mix things up.
If this lifestyle sounds irresponsible or unsustainable, then this is because we operate within a conception of identity that forces us to conform to the same systems that privilege heterosexuality as the norm.
Unfortunately, when it comes to gender-affirming care, it is indeed political, as long as we continue to treat people like they’re “born this way” and therefore only valid insofar as they satisfy a standard of biological determinism. It’s political because politics should be able to account for lives that inevitably twist and turn and proceed, unbidden by convention or expectation.
I never detransitioned, I just kept transitioning, but my driver’s license certainly looks outdated.
Audry Basch Brooklyn
As a health care provider, I have found it exceedingly frustrating in recent years to realize that any questioning on my part of the need for gender-affirming care puts me at risk of being ostracized in my profession as anti-L.G.B.T.Q. The care of gender-questioning patients can be more comprehensive and depoliticized.
I have been in health care for over 30 years and have seen the tides turn on many treatment beliefs. It is heartbreaking to have to acknowledge a parent’s fears and be unable to give them a comprehensive response about their adolescent’s care with science backing up our decision-making.
I can cite a particular case of a young adult who opted to transition because of hate for their body. They suffered many years of childhood sexual abuse. This history was never asked about, the trauma never addressed. That young adult was labeled as “borderline personality” when requesting detransition and is now being treated for complex trauma, as well as suffering from health and psychological effects of irreversible hormone and surgical therapies.
There is much more that can be done so providers like me won’t have to mince words and be indirect in our approaches to a holistic assessment of a patient who is suffering from distress related to identity and their lived experience.
Thank you for publishing this piece.
Ann Dryden Vermont The writer is a psychiatric and mental health nurse practitioner.
As a trans woman and civil rights advocate, I am deeply alarmed by Pamela Paul’s piece. She has chosen to ignore the lived experiences of most detransitioners — those who have medically or socially transitioned and then returned to living as the gender they were assigned at birth.
I, myself, am a detransitioner. I initially pursued transition when I was 17. Then, at 19, I detransitioned.
Like most young people who detransition, I did so not because I was coerced, “medicalized” or misled. I did so because of the harassment, familial rejection and violence I experienced as a visibly trans person in a world that has grown increasingly hostile to the existence of people like me.
Then, I once again pursued transition. I’ve now been living successfully, happily and openly as a trans woman for six years.
My experience aligns with the majority of detransitioners, who cite external pressures as their primary motivation for detransitioning and, ultimately, end up pursuing transition again.
Like many far-right lawmakers I met with in 2023 to discuss their attempts to ban gender-affirming care for minors in Kentucky, Ms. Paul chose to elevate the small group of outspoken detransitioners seeking to further restrict this care without regard for the majority of us who do not regret the care we received.
Instead of painting a nuanced portrait of how we treat youth experiencing gender dysphoria, Ms. Paul chose to peddle the very same anti-trans propaganda that she claims to denounce.
Emma Curtis Lexington, Ky.
Thank you for publishing Pamela Paul’s extremely balanced column. As someone who spent several years thinking I was trans, I understand that the topic is complex.
Ms. Paul does an excellent job of debunking the idea that all opposition to transition is right-wing. When it comes to pediatric medical intervention, the public is in notable disagreement with Democratic Party orthodoxy.
A 2023 survey of 1,262 registered voters across the country on behalf of Women’s Declaration International USA reported that “when asked what adults should do when female children say they are boys, ‘nonbinary’ or something else other than girls, just 12 percent of respondents, including 17 percent of Democrats, thought they should seek immediate medical intervention for a 15-year-old, and only 7 percent (including 11 percent of Democrats) supported immediate medical intervention for an 8-year-old.”
I am a leftist radical feminist. Americans across the political spectrum have legitimate questions about what it means to “identify as a gender.” It’s refreshing to see that The New York Times acknowledges that.
Elizabeth Chesak Chesterton, Ind. The writer is coordinator of the Women’s Declaration International USA Desisted and Detransitioned Women’s Caucus.
Things you buy through our links may earn Vox Media a commission
My surgeries were a bridge across realities, a spirit customizing its vessel to reflect its nature.

“However, to be ogbanje is to be categorized other and to bring alterity home in a way that transcends the more ordinary bifurcated ‘otherness’ of gender. We could even speculate that ogbanje children fall under a third category of gender, of human-looking spirit. This gender is marked from birth—as male and female statuses are marked—by special behaviors towards and physical adornment of the child. The sexual appearance of the ogbanje may, indeed, be seen as a sham—yet another promise that the ogbanje is likely to break in its refusal to act according to human norms.” — Misty Bastian, “Irregular Visitors: Narratives about Ogbanje (Spirit Children) in Southern Nigerian Popular Writing.”
The robot was called a da Vinci.
It was delicate, precise, inserted through my navel to slice my uterus and fallopian tubes into small unimportant pieces, which were then suctioned out of my body. The procedure had a technical name that filled my mouth — a robotic-assisted subtotal hysterectomy with a bilateral salpingectomy. I had to repeat this about seven times on the day of my surgery, as nurses came in with forms clarifying that I knew what I was getting, but I didn’t mind. I’d waited years for this surgery. In another life, I’d trained to be a surgeon myself, dissecting cadavers and cutting through layers of dermis and fascia and muscle with a ten-blade. But in this one, I was 28 and cold, my numb skin wrapped in a hospital gown as nurses draped warmed blankets over me. Still, anticipation rang clear chimes. I couldn’t wait for when they’d wheel me out of that operating room, finally sterile.
It had been five years since I figured out I was transgender, after falling into a vibrant queer scene in Brooklyn that showed me so many more ways to be than I’d ever known. I moved there from Massachusetts, leaving behind scalpels and skinned horses dangling from a warehouse ceiling at a veterinary school, coming to reddened cabaret nights and play parties and a brief stint as a drag king. With a new world wrapping around me, the discomfort that had been spreading sour and wrong through my body for ages finally had a name — gender dysphoria. It came with a sort of relief: If I knew what it was, I knew what I could do about it.
My best friend Rachel flew into upstate New York for the hysterectomy. After the excision, she unfolded a cot in my hospital room while I ordered waffles from room service. When the nurses came in, they tried to get me to stand up, but the pain was a riptide dragging me under. I swayed, nearly collapsing, so they eased me back into bed and upped my pain meds. I caught my breath as Rachel and I exchanged alarmed looks, her hand warm around mine.
“I didn’t think it would be this bad,” I managed to say.
“Me either,” she replied.
The nurse gave us a brief but incredulous look. “You got an entire organ removed from your body,” she pointed out. “It’s kind of a major surgery.”
I made it out of bed a few hours later, walking in slow motion around the hospital floor with my IV stand rolling beside me, my palm scraping against the walls and the nurse at my elbow. The next day, Rachel drove me home to my attic apartment. Most of my early recovery was spent there, in a wingback recliner the color of wet moss. It had a wooden handle on the side that opened the back hinge and made the foothold pop up with a creaky jerk, stretching the chair out. I slept in it for a week because I had difficulty standing up or bending into narrow angles, and my bed was too close to the floor. I was full of stitches and hydrocodone, and my guts had been rearranged. It wasn’t my first mutilation, but it was one of my best.
An ogbanje is an Igbo spirit that’s born into a human body, a kind of malevolent trickster, whose goal is to torment the human mother by dying unexpectedly only to return in the next child and do it all over again. They come and go. They are never really here — if you are a thing that was born to die, you are a dead thing even while you live. Igbo ontology explains that everyone is in a cycle of reincarnation anyway — you are your ancestor, you will become an ancestor, the loop will keep looping within the lineage. Ogbanje , however, are intruders in this cycle, unwelcome deviations. They do not come from the lineage; they come from nowhere. As such, it’s important for an ogbanje never to reproduce: if it did, it would contribute to the lineage, and when it died, its spirit would join those of the humans, participating in their reincarnation loop.
Removing a uterus is an efficient way to make sure this never happens.
While my gender had asserted itself in different ways since my childhood, one of its strongest features was always a violent aversion toward reproduction, toward having a body that was marked by its reproductive potential — a uterus to carry children, full breasts to feed them with. My first surgery was an outpatient procedure two years after I moved to Brooklyn, a breast reduction: some fat removed from my chest, some glands, some skin, nothing much. It required a letter from my therapist to prove that I was sane.
“I’ve never heard of anyone like this,” the surgeon told me. He was an old white man who had performed many surgeries on trans patients, from breast augmentations to double mastectomies. “Male to female, female to male, fine. But this in-between thing?”
I ground my teeth into a smile and handed him my letter, along with printed images of the chest I wanted. It was one that felt right for me, one that wouldn’t move much, wouldn’t sway with pendulous wrongness or leave me gasping shallow breaths because my ribs were encased in the flattening black of a chest binder every day. I paid his office $10,000 skimmed from my student loans and tried not to be angry at the hoops I had to jump through. If I’d asked for an augmentation, it would’ve been fine, but wanting smaller breasts in the absence of back pain was considered ridiculous enough to require a therapist’s approval. During my post-op visit, the surgeon complained that he’d never had to spend as much time in consultation with a patient as he had with me. We’d spent maybe 30 minutes together over a few appointments.
My scars hypertrophied, leaving shiny brown keloids and flat glossy rivers on my chest. Sometimes, when I felt like I wasn’t trans enough, I’d look at them to remind myself that I’d chosen to modify my body and even though dysphoria and surgery aren’t prerequisites for being trans, the scars still served as a grounding reflection of my own certainty. I wasn’t sure then what I was transitioning my body to, but I was clear that the gender I’d been raised as was inaccurate — I’d never been a woman.
After that first surgery, my depression lifted significantly. It was a connection I hadn’t made before, how my dysphoria was affecting my mental health — the suicide attempt I’d survived just four months before the surgery. The choice to finally modify my body felt like a big deal in large part because other people treated it that way. Their alarm was almost infectious, but I was the one who had to live in this body; I was the one who suffered in it. The reduction was simply a necessary procedure, something that helped pull me away from wanting to die, something that made living a little easier.
Still, there was a deep sense of transgression about what I was doing that I couldn’t shake, especially as a Nigerian. It was too easy to tune into our communities and hear the voices heavy with disgust, saying that what I had done was disfiguring, that God had made me one way for a reason and I had no right to say or do otherwise, that I was mutilating myself. There was an ideal my body was supposed to conform to, and I was deviating from it by having surgery. I was rejecting it as a center and choosing something else: a world where the deviation itself was the ideal. I chose it readily. I’ve never minded being a mutilated thing.
If ogbanje represent an overlapping of realities — a spirit who looks incredibly convincing as a human, then what does it look like for one to experience gender dysphoria and take surgical steps to resolve that? Our language around gender identity is often so Western, how can we intersect that with non-Western realities? For example, is there a term for the dysphoria experienced by spirits who find themselves embodied in human form? It was inevitable that I’d be drawn to these overlaps, since I live there, inhabiting simultaneous realities that are usually considered mutually exclusive.
The possibility that I was an ogbanje occurred to me around the same time I realized I was trans, but it took me a while to collide the two worlds. I suppressed the former for a few years because most of my education had been in the sciences and all of it was Westernized — it was difficult for me to consider an Igbo spiritual world equally, if not more valid. The legacy of colonialism had always taught us that such a world wasn’t real, that it was nothing but juju and superstition. When I finally accepted its validity, I revisited what that could mean for my gender. Did ogbanje even have a gender to begin with? Gender is, after all, such a human thing.
However, being trans means being any gender different from the one assigned to you at birth. Whether ogbanje are a gender themselves or without gender didn’t really matter, it still counts as a distinct category, so maybe my transition wasn’t located within human categories at all. Instead, the surgeries were a bridge across realities, a movement from being assigned female to assigning myself as ogbanje ; a spirit customizing its vessel to reflect its nature.
It is considerably difficult to convince a doctor to remove an uninjured organ, even if your wholeness depends on its absence, especially if that organ is a reproductive one and they think you’re a woman.
I didn’t have a letter for my uterus — it was too difficult to find a therapist who had experience with nonbinary trans patients and I didn’t have any money. But I thought perhaps I could save up for it one day, so I made appointments with a few gynecologists to discuss my options. I chose not to disclose my gender (or lack thereof), but instead expressed my desire for the surgery as an elective choice, only because I didn’t want children. The doctors received me with resistance and thin contempt.
“What if you change your mind?” they asked me, in exam room after exam room, metal and glass and white coats all blurring into a single closed door. I had a thousand comebacks but I bit them all back because these people had what I needed — gloved hands to cut me open and toss my uterus into the bright plastic of biological waste, or wherever unwanted organs end up. My dysphoria had built a tight knot of a home in my body, since I had no idea how I was going to afford another surgery or, at this rate, even find a doctor willing to perform it. It wasn’t as severe as before my first surgery, but it was still there — a reminder so red it was almost black, showing up every month. I couldn’t rest easy knowing there was even a chance I could get pregnant, so I tried an IUD. When they inserted it, I screamed from the pain, the excruciating wrongness of something passing through my cervix. In the months afterward, I bled too heavily, through ultra tampons and overnight pads, flooding menstrual cups. Eventually, an ultrasound showed that the IUD was out of position, so they had to remove it. It felt like my body had spat it out, a reminder that nothing short of an excision would suffice.
I’d left Brooklyn and moved upstate by then, to the attic apartment with the moss green recliner. Occasionally, I would have bouts of searing pelvic pain that trapped me in bed for hours. A few weeks into my second winter there, I went to see a urogynecologist, thinking there was something wrong with my bladder. It took the entire afternoon to run tests; then he called me into his office to tell me there was an 84 percent chance I had endometriosis. “We could put you on birth control,” he suggested. I refused.
“Why not?” he asked, and just like that, the air in his office stopped moving. I could feel my nerves jangling, the familiar taste of the moment right before each and every disclosure like a sharp film over my tongue.
It’s easier when I’m alone. My friends and family know I’m not a woman — I’ve told them — but some continue to think of me as one anyway. I ignore it because sometimes it’s easier to not fight, to accept the isolation of being unseen as a safe place. I exist separate from the inaccurate concept of gender as a binary; without the stricture of those categories, I don’t even have to think about my gender. Alone, there’s just me, and I see myself clearly.
Speaking to other people, though, requires channeling who or what I am into language they can understand. “I’m trans,” I explained. “And I’ve had a breast reduction, so hormones would reverse that.”
The doctor nodded while my stomach churned. “I’ve had a few trans patients,” he said. “We could do a hysterectomy, if that’s something you’d want. Your insurance would cover it.”
I stared at him, hope and disbelief numbing my hands. I’d been terrified that he was going to say something transphobic, that I’d have to deal with the violence of that tearing through my skin, a bullet I hadn’t scheduled when I showed up there that afternoon. Instead, when I left his office, I had a surgery date only two weeks away.
He renovated my navel during the hysterectomy, unfolding it and then tucking it back into my abdomen in its new configuration. At my post-op appointment, he called the nurse over to brag about how well it had healed. There were only two small scars, each barely a centimeter long, at the top and bottom of my new navel. I called my mother a week or two after the surgery and told her what I’d done, even though I knew she wouldn’t understand. She sighed with the resignation of a mother who has tried to stop her child before and failed. “Could you try not to cut off any more parts of your body?” she said, and I laughed so hard my stitches hurt.
I flew to her house for Christmas a few days later, attendants pushing me around both airports in a wheelchair, weak but giddy. The rest of my recovery was uneventful. After 17 years and approximately 200 periods, I slipped easily into my new and bloodless life.
There is a vivid history of mutilation with ogbanje : a dead one can be cut, scarred to prevent it from returning undetected. Ogbanje are also a cohort, they separate from each other when they get born, but they return to the cohort when they die. I like to think that there is a form of shared or generational memory within that; being dead or mutilated are not unfamiliar things to any of us, we’re not afraid of either.
It has been grueling to remake myself each time I learn more about who or what I am — to take the steps that such remaking requires, to bear the costs. Sometimes, those costs are worn on your heart, like when the people you love no longer have space in their worldview for you. Other times, it’s the body that bears them, in markings and modifications. By now, I’ve come to think of mutilation as a shift from wrongness to alignment, and of scars as a form of adornment that celebrates this shift. The keloids on my chest and the small lines spilling out of my navel function as reminders — that even when it meant stepping out of one reality to be swallowed by another, I kept choosing to move toward myself.
- first person
- transgender issues
The Cut Shop
Most viewed stories.
- This Mercury Retrograde in Aries Will Be Peak Chaos
- The Case for Marrying an Older Man
- Madame Clairevoyant: Horoscopes for the Week of March 31–April 6
- What We Know About the Mommy Vlogger Accused of Child Abuse
- Random Punching Attacks Rattle New York City Women
- When Your Kid Is the Classroom Problem Child
Editor’s Picks

Most Popular
What is your email.
This email will be used to sign into all New York sites. By submitting your email, you agree to our Terms and Privacy Policy and to receive email correspondence from us.
Sign In To Continue Reading
Create your free account.
Password must be at least 8 characters and contain:
- Lower case letters (a-z)
- Upper case letters (A-Z)
- Numbers (0-9)
- Special Characters (!@#$%^&*)
As part of your account, you’ll receive occasional updates and offers from New York , which you can opt out of anytime.
10 trans people share how their life satisfaction has changed after transition
Transgender people overwhelmingly describe their lives after transitioning as “happier,” “authentic” and “comforting” despite a deluge of state legislation in recent years that seeks to restrict their access to health care and other aspects of life.
Over the last three years, nearly half of states have passed restrictions on transition-related medical care — such as puberty blockers, hormone therapy and surgery — for minors. Supporters of the legislation have argued that many transgender people later regret their transitions, though studies have found that only about 1%-2% of people who transition experience regret.
Earlier this year, the 2022 U.S. Transgender Survey — the largest nationwide survey of the community, with more than 90,000 trans respondents — found that 94% of respondents reported that they were “a lot more satisfied” or “a little more satisfied” with their lives.
Transgender Day of Visibility, observed on March 31, is an annual awareness day dedicated to celebrating the accomplishments of trans people and acknowledging the violence and discrimination the community faces. NBC News asked transgender people from across the country to share how their life satisfaction has changed after transition. Out of two dozen respondents, all but one said they feel more joy in their lives. Here are some of their stories.
Ash Orr, 33
Morgantown, west virginia.
Orr, who is the press relations manager for the National Center for Transgender Equality, the trans rights advocacy group that conducted the nationwide survey, began socially transitioning in his mid-20s, and at 33, he received gender-affirming top surgery.

“The impact of this surgery … has been life-changing,” Orr said. “My body now feels like a comforting and familiar home, a place I had yearned for and have finally returned to.”
When Orr isn’t working, he loves immersing himself in nature, whether that’s through gardening or playing pickleball with friends. He also chases tornadoes in the Midwest — “Yes, like the movie ‘Twister’!” he said.
“My transition journey has been a profound lesson in self-discovery,” Orr said. “It has shown me that there are countless versions of myself waiting to be unearthed.”
Criss Smith, 63
After transitioning, Smith said he felt a sense of congruence between his internal sense of self and his external presentation.

“I was so broken and uncertain, and now I have a profound sense of relief, empowerment and alignment with how I feel and being the best human possible,” he said. Smith said he worked on Wall Street in financial services for more than 30 years for major companies including Merrill Lynch and JPMorgan Chase. He now works as a substitute teacher for the New York City Department of Education.
“My mind is more at rest and I am at ease with every moment,” Smith said of life after his transition. “A joy fills my soul that I never thought possible before. I am truly living a full human experience presenting all of my authenticity. I live in a liberation garden.”
Gavin Grimm, 24
Hampton roads, virginia.
Grimm was the plaintiff in a landmark 2020 court case in which the 4th Circuit U.S. Court of Appeals upheld the rights of transgender students to use the school bathrooms that aligned with their gender identities. In 2021, the Supreme Court declined to hear the case and allowed the circuit court’s decision in Grimm’s favor to stand.

Now, nearly three years later, Grimm plans to go back to college to become a middle or high school teacher. He came out and began his transition in 2013, and “to date, I have absolutely zero regrets,” he said.
“While I do still struggle with unrelated strife in my personal life, the ability to be myself fully and completely for the last decade has given me the strength and joy that I have needed to carry on,” Grimm said. “Despite these challenges, I remain very, fundamentally happy. Exquisitely happy, even, in just finding small joy each day in a world where I had the ability to access myself.”
Dani Stewart, 57
Springfield, missouri.
Stewart said transitioning was “a life saver” for her and that she feels more confident than she ever has before.

“I feel like I belong in society,” said Stewart, who said she was formerly a news desk producer at CNN and worked for various TV stations. “However, dark clouds remain for all trans people. We need better and more representation in media. We need to see more of ourselves integrated with the world around us.”
Andrea Montañez, 58
Orlando, florida.
Montañez said her son and her co-workers both observed the same change in her after she transitioned in 2018: They said they noticed her smile.

“You always were a nice person, but we didn’t know you could smile,” Montañez recalled her co-workers telling her. “I lost a lot, but I won freedom and happiness.”
Montañez is the director of advocacy and immigration at the Hope CommUnity Center in Orlando and is involved in advocating against legislation targeting LGBTQ people in Florida — work that she said has helped her build community, find happiness and “bring the magic” to her and others’ lives.
“We are a gift,” she said. “Trans people are a gift.”
Elizabeth ‘Lizzy’ Graham, 34
Silver spring, maryland.
In 2015, Graham said she kept a bag of women’s clothes in her car so that when she finished her shift at work as a tech support professional, she could drive to a Starbucks and change in the bathroom. She was also driving for Uber at the time, and one day she decided to dress as herself so she could practice coming out to her passengers before she came out to her family.

She came out fully in the summer of 2015, and said her gender dysphoria, or the distress caused by a misalignment between one’s sex assigned at birth and gender identity, went away with time.
“Once I began my transition journey and began living full time, my focus and productivity improved,” she said. “Many friends and people I know who knew me prior to transitioning said that they could tell I was happier now that I came out and was living my authentic life.”
Now, Graham is a service coordinator who helps autistic children who receive Medicaid-funded services, and she leads a support group for transgender people in her area.
Jordan Reid, 27
Harper woods, michigan.
Reid said her coming out as a transgender woman in 2022 happened alongside a number of other life changes. She had just gotten divorced, and then she dropped out of medical school, or, as she says, “exploded” all of her career aspirations.

But the last two years have been much happier, she said. Reid is back in school studying computer science and data science, and has rekindled her love for music. She has played guitar since she was 10, but said she stopped because she didn’t like her singing voice. Now, she sings in the shower every day.
“On paper, it may look like I have taken quite a few steps back in life,” Reid said. “In reality, what’s on paper doesn’t matter one bit if, instead of sacrificing my joy, I get to spend the majority of my time not only smiling, but truly feeling a reason to smile.”
Tiffany Jones, 35
Newark, new jersey.
Jones, who works in an Amazon warehouse, said transitioning has helped reduce her suicidal ideation.

“I am happy that I am living as my unapologetically authentic self,” Jones said, adding that her transition “helped me improve my self-confidence” and allowed her to be more creative. She now writes poetry, cosplays as anime characters and has a stronger support network, she said.
She said she worries about her personal safety as a Black trans woman, but “I just think about the positive things in life, and that there’s so much out there in the world, so much inspiration.”
Kylie Blackmon, 26
Azle, texas.
Blackmon said her life changed dramatically when she came out in 2021.

“It seemed like everything clicked mentally with me. No longer was I burdened with living a lie and having that weigh on me constantly,” she said. However, she said things are harder socially in her small Texas town of about 15,000 people, northwest of Fort Worth. She said she faces transphobia from her co-workers, and that some of her family members don’t understand her identity.
She’s currently training to be a phlebotomy technician, which is someone who collects and tests blood samples, and in her free time she enjoys doing makeup, shopping and spending time with her friends.
Cristina Angelica Piña, 23
Central valley, california.
Piña, a consultant, said that being trans can be difficult, but that “underneath this pain, there is an unfettered joy, power and beauty.”

“My existence reminds people of choice,” said Piña, who enjoys fashion, poetry, rap, cooking and spending time with her friends and her dog, Bella. “We have the autonomy to decide how we exist in the world. We have the freedom to present ourselves in a way we see fit — not what others have placed upon us.”
For more from NBC Out, sign up for our weekly newsletter .
Jo Yurcaba is a reporter for NBC Out.

- Leadership Crisis
- Editor's Pick

In Private, Garber Acknowledges Harvard Has a Fundraising Problem

‘Like a Horror Movie’: Freshmen Complain About Mice in Dorms
Ivy League Federal Lobbying Expenditure Rose 12% in 2023, Harvard Spent $530,000

Harvard Undergraduate Association Co-President Shikoh Hirabayashi Is Also Facing Recall Effort

As Many Mourn the ‘Death of the Humanities,’ Harvard Profs. Say It’s Not That Simple
I’m Trans, and My Gender Is a Choice. So Is Yours.
Transcriptions.

What if I told you that being transgender is a choice?
If you already feel apprehensive, I don’t blame you. Conservative actors have long leveraged similar rhetoric to delegitimize and attack the trans community. They are wrong to suggest that being trans is made-up.
But the fact remains: I chose to be trans. And every day I wake up and I choose it again.
By this I mean that, though my gender is innate and deeply-felt, I decide how to translate it into outward expression. And I’m not alone. As much as gender is a choice for trans people like myself, so too is it a choice for cisgender people, whether they are conscious of it or not.
We are all constantly making choices that impact the way others perceive and engage with our gender, from the clothes that we wear to the cut of our hair. Just because someone chooses to perform gender in alignment with their sex assigned at birth, doesn’t mean it is any less of a choice.
Framing gender this way — as a choice, rather than a fact — clarifies why the recent explosion of bans on gender-affirming care for trans youth are not just harmful but downright undemocratic: When politicians regulate gender, what they’re actually regulating is an individual’s freedom to exercise choice over their gender.
The most vocal force behind these bans — conservatives who fundamentally object to trans identity — market the legislation as a means of protecting impressionable kids from being “seduced” by “transgender ideology.” For this camp, youth are ground zero for an all-out assault on the transgender community, who they feel threaten the social order.
However, there is another, less obvious group opposing gender-affirming healthcare: Liberals and moderates whose support of trans identity is complicated by concern that youth are not developmentally mature enough to make permanent decisions about their bodies.
This second camp, though often well-meaning, lends credence to fringe or methodologically-flawed evidence that contradicts the well-established value of gender-affirming care.
I don’t question that youth are generally more impressionable and less mature than the average adult. But this doesn’t mean they must be denied access to care. And before you come at me with pitchforks, please hear my case.
First, let’s be specific about what gender-affirming care means. I’m not advocating for small children to undergo gender-affirming surgeries. Really, no one is.
In reality, medical professionals have crafted a wide menu of consensus best practices for administering gender-affirming care to youth in age-appropriate, carefully-considered ways. There is no exact, one-size-fits-all approach, but options typically range from reversible puberty blockers for younger adolescents to hormone replacement therapy to, yes, in some cases, surgery for older adolescents. Almost never are these treatments undertaken hastily or without ample informed consent.
Second, opponents of gender-affirming care fixate heavily on the possibility of regret, despite regret rates being incredibly low. Most recently, the largest survey of trans adults in the US found that more than 97 percent of respondents were more satisfied with life after receiving gender-affirming hormone treatment or gender-affirming surgery.
Of course, it is inevitable that some people will eventually regret the choice to receive gender-affirming healthcare. But absolutely universal satisfaction is a ridiculous standard. We don’t expect the many to sacrifice their personal freedom in the name of minimizing regret for the few when it comes to almost any other decision.
Choosing to receive gender-affirming care is not a far cry from choices that youth make all the time, like getting a piercing or undergoing elective cosmetic surgery . In these cases we seem to have no problem allowing youth — pending parental permission and informed consent — to make permanent changes to their bodies, even though they run the risk of regret.
Why do we treat a 16-year-old girl who wants a breast reduction so differently from a 16-year-old trans boy who wants a mastectomy? Why don’t we allow trans kids to exercise autonomy over their bodies, even under the supervision of their parents and informed medical professionals?
It is time we embrace the idea that every person has the right to exercise autonomy over their own body and self-expression, no matter who they are. By allowing trans kids to access gender-affirming care, we empower them to make the very same choices their cis peers make each and every day.
I chose to come out as trans when I was 16 years old. I didn’t choose it just because I felt uncomfortable and inauthentic living as a woman. I chose it because I have never felt more euphoric and myself than when I present as a man. I chose it because I wanted to. And every day I wake up and I want to choose it again.
It’s hard to imagine I’ll ever feel differently. But even if I did, I still wouldn’t regret choosing to be trans. The euphoria it gained me will have been enough.
E. Matteo Diaz ’27, a Crimson Editorial editor, lives in Grays Hall. His column, “ Transcriptions ,” runs bi-weekly on Thursdays.

Want to keep up with breaking news? Subscribe to our email newsletter.

Gender Transitioning in Minors
How young is too young.
Posted May 2, 2023 | Reviewed by Michelle Quirk
- Find a counsellor who understands gender identity
- While increased awareness of an issue is beneficial, too much emphasis on it when it has become part of the zeitgeist may be harmful.
- Creating blanket laws permitting youth transitioning gives rise to opposing laws meant to prevent gender transitioning.
- Before an attempt is made to come to a legal solution, we need to understand the underlying facts.

When discussing transgender issues in minors, “harm” is understood in precisely opposite ways by those on either side of the debate. Where there are calls for children under the age of 18—the age of legal majority in most U.S. states—to be able to transition, one side argues that “harm” would be preventing minors from doing so, and the other side argues that “harm” would be allowing minors to do so.
Arguments For and Against
One argument for preventing minors from gender transitioning is that they are too young to make that kind of permanent, life-changing decision, and they therefore must wait until they have reached the age of legal majority to make such a decision, with the assumption being that by age 18 they will be prepared and mature enough to make permanent, life-changing decisions.
One counterargument deals with the concept of maturity in an alternative fashion, such that if children don’t transition before puberty , they will in fact develop into biologically mature males or females, which later transitioning will not be able to reverse even with the use of hormones . Another argument is that 18 is an arbitrary age and that decision-making capacity is not significantly less developed in 17-year-olds or 16-year-olds.
A Psychology, Rather Than Legal, Perspective
Instead of immediately brandishing picket signs and legislative pens, we must think about how to approach the issue as it applies to minors. If we consider the question from a psychology perspective rather than a legal perspective, we will be able to evaluate how many individuals actually suffer from gender dysphoria , the age at which decision-making capacity ripens, at what age allowing children to transition might be abusive (the analysis may be different for a 17-year-old and a 7-year-old, for instance), the long-term harms of youth transitioning, and whether something like this emerges in waves in society.
That is, for example, does zeitgeist play a part in the emergence and disappearance of certain disorders simply by virtue of it being widely in the public consciousness? If this is true, how many children are we harming by—to a degree—normalizing gender dysphoria when it’s actually a minority of people who suffer from it?
While increased awareness of an issue is beneficial, too much emphasis on it when it has become part of the zeitgeist may be harmful, such that it may become more difficult for those suffering from gender dysphoria to be taken seriously and get the treatment they need—which may indeed include medical intervention, such as gender reassignment surgery (also referred to as “gender affirmation surgery”).
The Least Harm for the Greatest Number
Assume that the goal is to find a solution that results in the least harm for the greatest number of individuals. If the status quo is that only those who have reached the age of legal majority can make the decisions necessary to facilitate gender transitioning (for reasons that would need to be delineated, such as brain development with regard to decision-making capacity and the percentage of the minor population actually affected by gender dysphoria), the correct immediate step to take in finding the solution that will result in the least harm for the greatest number of individuals may not be reevaluating what laws should exist about preventing or permitting transgender “treatments” for minors—whether that is gender reassignment surgery or otherwise—but what exceptions to the laws should be available to minors.
Perhaps individuals under the age of 18 (the youngest age to which this could apply would need to be discussed) who actually suffer from gender dysphoria rather than experience standard, minor confusion or dissatisfaction with their body would be able to transition sooner—assuming that transitioning is the recommended clinical “treatment” for such a psychological disorder (gender dysphoria is in the Diagnostic and Statistical Manual of Mental Disorders )—if the laws allowed for exceptions in particular cases. Exceptions would be granted, for example, based on the recommendation of trusted psychologists after evaluating the minor, and of doctors after evaluating the child’s medical fitness for a particular course of treatment.
Questions about whether exceptions should be granted for the minor without the consent of the parents would need to be answered. The parents’ involvement would need to be a part of the psychological evaluation of the minor as well: Are the parents unreasonably unsupportive? Supportive but hesitant? Irrational? How does their behavior affect the child’s self-image and perspective on the issue? In addition, there would need to be an evaluation of the long-term effects of transitioning: Aside from long-term physical effects, would the child be mentally capable of thriving in society as a transgender individual? Do the risks outweigh the benefits in this particular case?

Creating blanket laws permitting youth transitioning that do not necessarily apply to the greater population gives rise to opposing laws meant to prevent gender transitioning for all minors, including the small percentage that might actually benefit from such an early transition as determined by medical professionals. This is because lawmakers of the latter persuasion see the harm that is potentially done by large-scale encouragement of youth transitioning where no gender dysphoria exists on a large scale.
Before an attempt is made to come to a legal solution about what path allows for the least harm for the greatest number of individuals, if that is indeed the agreed-upon goal, we need to understand the underlying facts about child psychology, the prevalence of gender dysphoria in minors, and the long-term risks and benefits of transitioning at an early age—and how early is too early from a developmental rather than legal perspective is a key question.
This article draws from ideas discussed in Episodes 6 and 7: “Transitioning Minors” of my Grey Matter video podcast series on Spotify.
Copyright © 2023 Kaitlin Puccio

Kaitlin Puccio, Esq., M.S. , is a lawyer, bioethicist, producer, and host of the "Grey Matter" video podcast. Her work explores and magnifies cultural topics buried at the intersection of philosophy, psychology, politics, bioethics, and law.
- Find a Therapist
- Find a Treatment Center
- Find a Support Group
- International
- New Zealand
- South Africa
- Switzerland
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- PMC10322945

Transition Regret and Detransition: Meanings and Uncertainties
Sarah c. j. jorgensen.
Institute of Medical Science, Temerty Faculty of Medicine, University of Toronto, 1 King’s College Circle, Toronto, ON M5S 1A8 Canada
Associated Data
Not applicable.
Gender transition is undertaken to improve the well-being of people suffering from gender dysphoria. However, some have argued that the evidence supporting medical interventions for gender transition (e.g., hormonal therapies and surgery) is weak and inconclusive, and an increasing number of people have come forward recently to share their experiences of transition regret and detransition. In this essay, I discuss emerging clinical and research issues related to transition regret and detransition with the aim of arming clinicians with the latest information so they can support patients navigating the challenges of regret and detransition. I begin by describing recent changes in the epidemiology of gender dysphoria, conceptualization of transgender identification, and models of care. I then discuss the potential impact of these changes on regret and detransition; the prevalence of desistance, regret, and detransition; reasons for detransition; and medical and mental healthcare needs of detransitioners. Although recent data have shed light on a complex range of experiences that lead people to detransition, research remains very much in its infancy. Little is known about the medical and mental healthcare needs of these patients, and there is currently no guidance on best practices for clinicians involved in their care. Moreover, the term detransition can hold a wide array of possible meanings for transgender-identifying people, detransitioners, and researchers, leading to inconsistences in its usage. Moving forward, minimizing harm will require conducting robust research, challenging fundamental assumptions, scrutinizing of practice patterns, and embracing debate.
Introduction
Gender transition is undertaken with the goal of improving the well-being of people suffering from gender dysphoria (Coleman et al., 2022 ). However, some have argued that the evidence supporting medical interventions for gender transition (e.g., hormonal therapies and surgery) is weak and inconclusive (Block, 2023 ; COHERE, 2020 ; Hembree et al., 2017 ; Ludvigsson et al., 2023 ; NICE, 2020a , b ), and an increasing number of people have come forward over the past few years to share their experiences of transition regret and detransition (Levine, 2018b ; Marchiano, 2020 ; r/detrans, 2023 ; Respaut et al., 2022 ; Valdes & MacKinnon, 2023 ). Regret is broadly defined as a negative, cognitive-based emotion involving counterfactual inference and feelings of personal agency or self-blame (Zeelenberg & Pieters, 2007 ). Studies evaluating regret following medical transition have used non-standardized definitions, and methods to ascertain regret have been heterogeneous (Blanchard et al., 1989 ; Dhejne et al., 2014 ; Lawrence, 2003 ; Narayan et al., 2021 ; Pfäfflin, 1993 ; Rehman et al., 1999 ; van de Grift et al., 2018 ; Weyers et al., 2009 ; Wiepjes et al., 2018 ). Likewise, definitions of detransition vary across studies, but most include discontinuing medications, having surgery to reverse the effects of transition, or both (Exposito-Campos, 2021 ; Littman, 2021 ; Vandenbussche, 2022 ). Desistance is a closely related phenomenon that is often applied to children whose gender dysphoria resolves before undergoing medical interventions (Drummond et al., 2008 ; Ristori & Steensma, 2016 ; Singh et al., 2021 ).
Although regret and detransition overlap in many people, they are distinct concepts and not all people who regret their transition take steps to detransition (Exposito-Campos, 2021 ; MacKinnon et al., 2022b ). Many surgeries are irreversible, and changing or discontinuing hormonal therapies confers new risks. Likewise, not all of those who detransition feel regret about their decision to transition (Exposito-Campos, 2021 ; Littman, 2021 ; MacKinnon et al., 2022b ; Pullen Sansfaçon et al., 2023 ; Vandenbussche, 2022 ). External factors, such as medical complications or discrimination, may drive some peoples’ decision to detransition (Littman, 2021 ; MacKinnon et al., 2022b ; Turban et al., 2021b ; Vandenbussche, 2022 ).
Detransition poses multiple medical (Biggs, 2021 ; Hembree et al., 2017 ; Irwig, 2018 ; Stolk et al., 2023 ) and bioethical (D'Angelo, 2018 ; Kimberly et al., 2018 ; Levine, 2018a ) challenges. Although recent data have shed light on a complex range of experiences that lead people to detransition, research remains very much in its infancy. Little is known about the medical and mental healthcare needs of these patients, and there is currently no guidance on best practices for clinicians involved in their care. In this essay, I discuss emerging clinical and research issues related to transition regret and detransition. I begin by describing recent changes in the epidemiology of gender dysphoria, conceptualization of transgender identification, and models of care. I then discuss the potential impact of these changes on regret and detransition; the prevalence of desistance, regret, and detransition; reasons for detransition; and lastly, medical and mental healthcare needs of detransitioners. My objective is to arm clinicians with the latest information in this rapidly evolving field so they can support patients navigating the challenges of transition regret and detransition.
The Changing Landscape of Gender Dysphoria
Gender clinics throughout the Western world are grappling with a sharp and poorly understood rise in the number of young people presenting with gender dysphoria or claiming a transgender identity (Bauer et al., 2021 ; Cass, 2022 ; Handler et al., 2019 ; Kaltiala et al., 2020a ; Segev-Becker et al., 2020 ; van der Loos et al., 2023 ; Wood et al., 2013 ; Zucker, 2019 ). The newly presenting cases are markedly different from historical presentations (Aitken et al., 2015 ; Kaltiala-Heino et al., 2015 ; Steensma et al., 2018 ; van der Loos et al., 2023 ; Wood et al., 2013 ; Zucker, 2019 ). Before the early 2000s, most of those seeking medical interventions for gender transition presented in mid-adulthood and were almost exclusively male (Blanchard, 1989 ). A small number of cases seen in gender clinics were prepubescent children, often with a history of gender dysphoria beginning in early childhood and a sex ratio of two to six males to each female (Cohen-Kettenis et al., 2003 ; Steensma et al., 2018 ; Wood et al., 2013 ; Zucker, 2019 ). In youth presenting today, gender dysphoria typically begins or is first expressed in adolescence or young adulthood, and there has been a notable shift in the sex ratio to one favoring females (Aitken et al., 2015 ; Arnoldussen et al., 2022 ; Kaltiala-Heino et al., 2015 ; Steensma et al., 2018 ; van der Loos et al., 2023 ; Wood et al., 2013 ; Zucker, 2019 ). Moreover, significant mental health problems and neurodevelopmental comorbidities, such as autism and attention deficit disorder, frequently complicate the clinical presentation (Kaltiala-Heino et al., 2015 ; Thrower et al., 2020 ; Wood et al., 2013 ; Zucker, 2019 ).
Causes of this epidemiological shift are vigorously debated. At least three hypotheses have been proposed. First, some believe changes simply reflect society’s increased acceptance of gender diversity (Rosenthal, 2021 ). The magnitude of the increase in cases, coupled with the predominance of adolescent females, suggests that societal acceptance may only be part of the explanation, however. Second, others have observed the terms “transgender” and “gender-diverse” are far broader than previously used terms such as “transsexual” and encompass mere nonconformity to traditional sex stereotypes (Wright, 2022 ). Moreover, they point to evidence showing that, at least during childhood and adolescence, females are more likely to engage in traditionally “masculine” behaviors than males are to engage in traditionally “feminine” behaviors (Wright, 2022 ; Zucker et al., 1997 ). Last, there is evidence to support the hypothesis that epidemiological changes could be driven by prevalent maladaptive coping mechanisms together with sociocultural factors and peer influences (Haltigan et al., 2023 ; Littman, 2018 , 2021 ; Withers, 2020 ). Many young people adopted a transgender identity in the context of family dysfunction or psychosocial issues (Bonfatto & Crasnow, 2018 ; D'Angelo, 2018 ; Kaltiala-Heino et al., 2015 ; Zucker, 2019 ). Precursors have included sexual assault and trauma (Evans, 2023 ; Gribble et al., 2023 ; Littman, 2018 , 2021 ; Marchiano, 2021 ; Pullen Sansfaçon et al., 2023 ; Respaut et al., 2022 ). Parents have reported the onset of gender dysphoria in the context of heavy engagement with social media and cases have clustered within peer groups where one or multiple members identified as transgender or non-binary (Haltigan et al., 2023 ; Kornienko et al., 2016 ; Littman, 2018 ; Sanders et al., 2023 ).
Changes in the Conceptualization of Transgender Identity and Models of Care
The marked epidemiological shift in those presenting with gender dysphoria or claiming a transgender identity has been accompanied by efforts to de-pathologize cross-sex identification, with the aim of decreasing stigma and enhancing civil rights protections for transgender people (Coleman et al., 2012 ; D'Angelo, 2020 ; Rafferty et al., 2018 ). In the past, it was recommended that those seeking medical interventions for gender transition undergo comprehensive psychological assessments with attempts to determine whether distress related to gender was secondary to, or better accounted for, by other mental health problems or sociocultural influences (Coleman et al., 2012 ; de Vries & Cohen-Kettenis, 2012 ). However, many transgender-identified people perceived these assessments as burdensome, intrusive, and impinging on patient autonomy (Ashley, 2019 ; Coleman et al., 2022 ). As a result of transgender advocacy, there has been a move away from what was believed to be unnecessary medical “gatekeeping” (Amengual et al., 2022 ; Coleman et al., 2022 ). Proponents of a less restrictive framework believe that transgender-identified people are best situated to determine what interventions they need to improve their well-being, regardless of age, mental health status, or duration of gender dysphoria (Ashley, 2019 , 2022 ; Schulz, 2017 ). Transition-related medical interventions are now conceptualized as a means of realizing fundamental aspects of personal identity or “embodiment goals” (Ashley, 2022 ; Coleman et al., 2022 ; Schulz, 2017 ), in contrast to conventional medical care, which is pursued with the objective of treating an underlying illness or injury to restore health and functioning. Accordingly, in-depth mental health evaluations as a prerequisite for accessing hormonal therapy and surgery are eschewed as antithetical to “affirmation” of gender identity and are either not required or are highly abbreviated at many clinics across the USA (Ashley, 2019 ; Levine et al., 2022 ; Rafferty et al., 2018 ; Schulz, 2017 ; Terhune et al., 2022 ). Moreover, proponents of the gender-affirmation model argue that comorbid mental health problems should not be a barrier to accessing hormonal therapies and surgery. They attribute elevated rates of mental illness in people with gender dysphoria to prolonged exposure to hostile external responses to gender nonconformity, i.e., minority stress, which could, they believe, be alleviated by gender transition (Coleman et al., 2022 ; Kingsbury et al., 2022 ; Valentine & Shipherd, 2018 ). However, the minority stress model has been challenged recently by a growing number of studies that reveal high rates of mental illness and childhood adversity pre-dating the onset of gender-incongruent feelings (Becerra-Culqui et al., 2018 ; Kaltiala et al., 2020b ; Kaltiala-Heino et al., 2015 ; Kozlowska et al., 2020 ; Littman, 2021 ). This may explain why people with preexisting mental health problems continue to struggle when social transition, hormones, or surgery fail to alleviate other problems that are frequently tied up with feelings of gender dysphoria (Kaltiala et al., 2020b ; Morandini et al., 2023 ).
Potential Implications of Epidemiological Changes and the Gender-Affirmation Model on Transition Regret and Detransition
The upsurge in adolescents and young adults seeking transition-related medical interventions coupled with less restrictive eligibility criteria has important implications for transition regret and detransition. First, even if only a small percentage of people who transitioned as minors or young adults later take steps to detransition, a small percentage of a population that has grown exponentially in the last decade means many more detransitioners will emerge in the coming years. Second, decisions to transition are now being made by young people who might lack the cognitive and emotional maturity to fully appreciate the long-term repercussions of their decisions. A qualitative interview study of adolescents attending two Dutch gender clinics found that most adolescents who were interviewed believed certain aspects of medical transition (e.g., loss of fertility and impact on future romantic relationships) simply cannot be understood and appreciated by young people below a certain age and most interviewees admitted they were not aware of the importance and impact of their decision to halt pubertal development at the time of their consent/assent (Vrouenraets et al., 2022 ). As one adolescent in the study remarked: “Of course, I was very young at the time [when I decided about starting the treatment with puberty suppression], but I had been whining about it for a long time already. It was more like: ‘I have to do it, I have to do it.’ Did I think it through [what the treatment with puberty suppression and its (possible) consequences entailed]? No.” (Vrouenraets et al., 2022 ).
The findings of this study are not surprising, given that the human brain does not reach maturity until the mid-twenties and the executive functions are the last abilities to fully develop (Casey et al., 2008 ; UNICEF, 2017 ). Executive functions include the ability to plan, prioritize, and strategize to achieve long-term goals as well as the ability to thoughtfully weigh information to make decisions (Casey et al., 2008 ; UNICEF, 2017 ). In the adolescent brain, connections between the prefrontal cortex or decision-making center and the amygdala or emotional center are still evolving (Casey et al., 2008 ; UNICEF, 2017 ). Consequently, adolescents often prioritize feelings over facts when making decisions (Casey et al., 2008 ; UNICEF, 2017 ). Moreover, because corticostriatal connectivity is not fully developed until adulthood, adolescents do not assess risk like adults. An adolescent’s ability to judge the value of an outcome in the future, resulting from a decision made today, is often impaired, especially when the outcome is far in the future and outside their present experience (Casey et al., 2008 ; UNICEF, 2017 ). Peer influence is another uniquely powerful factor that impacts judgement and decision-making in adolescence. Neuroimaging studies have shown that peer pressure promotes high levels of activation in the amygdala (emotional center) (Knoll et al., 2015 ; Somerville, 2013 ). This is not seen to the same extent during interactions with adults and may explain why adolescents value the opinions of their peers more than those of adults when assessing risk (Knoll et al., 2015 ; Somerville, 2013 ).
Feeling disconnected or uncomfortable with one’s body is a normal experience for adolescents and common in those with autism, anxiety disorders, eating disorders, or trauma (Bornioli et al., 2021 ; Krumm et al., 2017 ; Lantz et al., 2018 ). However, when distress is seen through the lens of gender identity, the priority becomes affirmation of gender identity and other important mental and/or medical healthcare needs might be overlooked or assumed to be related to gender dysphoria, i.e., diagnostic overshadowing (Cass, 2022 ). Moreover, a young person’s identity can be fluid and evolve over time in response to biological, psychological, and social factors (Crocetti, 2017 ; Kroger et al., 2009 ); solely relying on a subjective sense of gender identity might not be a reliable basis for medical decision-making about often irreversible interventions.
Prevalence of Desistance, Regret, and Detransition
In the past, 61% to 98% of cases diagnosed with gender identity disorder/gender dysphoria in early childhood reconciled their gender identity with their birth sex through the natural course of puberty, if not earlier (Drummond et al., 2008 ; Ristori & Steensma, 2016 ; Singh et al., 2021 ). Many of these children simply grew up to be gay or lesbian adults. Traditionally “feminine” boys were far more likely to grow up to be gay men rather than transgender women, and the same was true for gender-nonconforming girls (Drummond et al., 2008 ; Ristori & Steensma, 2016 ; Singh et al., 2021 ). Less is known about desistance in the novel cohort of young people presenting today. Unlike in the past when clinicians actively worked with children and their parents to lessen gender dysphoria or adopted a neutral strategy of “watchful waiting” (Cohen-Kettenis & Pfäfflin, 2003 ; Zucker, 2008a , 2008b ), many of today’s youth undergo some form of gender social transition (e.g., change in clothes, haircut, name, and pronouns; breast binding; use of opposite sex facilities, etc.) before contemplating medical interventions (Morandini et al., 2023 ; Olson et al., 2022 ; Zucker, 2020 ). Although social transition is often described as a neutral intervention with little, if any, long-term consequences, several studies support the hypothesis that it can concretize gender dysphoria (Olson et al., 2022 ; Turban et al., 2021a ; Zucker, 2020 ). Moreover, recent evidence suggests that social transition might not be associated with improved mental health status in the short term (Morandini et al., 2023 ).
Nearly all minors (> 95%) who start the process of medical transition with puberty blockade at the onset of puberty, or shortly after, go on to receive cross-sex hormones (Brik et al., 2020 ; Carmichael et al., 2021 ; de Vries et al., 2011 ). Proponents of gender-affirming care attribute this persistence after starting puberty blockers to a robust and effective selection process, resulting in few false positives. However, this explanation is at odds with the push for abbreviated psychological assessments and a diagnostic approach, endorsed by affirming clinicians, which is based upon the premise that children “know who they are,” and adults should follow the child’s lead on decisions about medical interventions (Ehrensaft, 2016 ). A more troubling interpretation of the high rate of persistence following pubertal suppression is that preventing physical and sexual maturation with hormonal interventions crystalizes transgender identification (Griffin et al., 2021 ; Levine et al., 2022 ). Rather than being a “reversible pause,” puberty blockade might instead constitute the first step in a cascade of escalating medical interventions (Griffin et al., 2021 ).
Historical data suggest that regret following gender transition in adulthood is rare (Blanchard et al., 1989 ; Dhejne et al., 2014 ; Lawrence, 2003 ; Pfäfflin, 1993 ; Rehman et al., 1999 ; van de Grift et al., 2018 ; Weyers et al., 2009 ; Wiepjes et al., 2018 ). However, studies reporting low rates of regret are generally from an era when hormonal therapy and surgery were only undertaken under strict protocol. Regret was ascertained by a variety of methods, including retrospective review of medical charts for documentation of regret, or unvalidated questionnaires and semi-structured interviews, which are susceptible to non-response bias (Blanchard et al., 1989 ; Lawrence, 2003 ; Rehman et al., 1999 ; van de Grift et al., 2018 ; Weyers et al., 2009 ; Wiepjes et al., 2018 ). Other researchers have used a very narrow definition of regret, such as application to have birth sex reinstated as legal sex (Dhejne et al., 2014 ). More recently, patients with post-operative regret were identified using requests for surgical reversal, although it is unknown what proportion of those who experience regret pursue further surgery (Narayan et al., 2021 ). Patients who started hormonal therapies but did not proceed further with surgical removal of the ovaries or testes were often excluded from assessments of regret (Dhejne et al., 2014 ; Wiepjes et al., 2018 ); it is possible that those who were disqualified from or choose not to undergo gonadectomy had higher levels of regret than those who went on to complete their surgical transition (D'Angelo, 2018 ). Many studies also suffered from high rates of loss to follow-up, and patients who died by suicide or from medical complications were frequently not included in the analyses (Dhejne et al., 2014 ; Wiepjes et al., 2018 ), which may mask regret.
A Dutch study, which is often cited as demonstrating a low rate of regret in transgender adults following medical transition, illustrates how selection bias and high rates of loss to follow-up might lead to underestimates of regret (Wiepjes et al., 2018 ). The study included nearly 7000 patients who sought hormonal therapy and surgery from 1972 to 2015. Extensive mental health evaluations were performed on all patients to determine eligibility. In total, 70% were started on hormonal therapy and 78% of this group went on to have their ovaries or testes removed. Among those who underwent gonadectomy, rates of regret, as ascertain from retrospective review of documentation in medical charts, were only 0.3% for transgender men and 0.6% for transgender women, with an average time to regret of approximately 11 years. Regret in those who did not undergo gonadectomy was not reported and a lower proportion of patients proceeded to gonadectomy over the course of the study (79% from 1972 to 1979 versus 69% from 2005 to 2009). Moreover, 36% of patients were lost to follow-up; the prevalence of regret is unknown for those lost to follow-up.
Recent data, capturing the upsurge in the predominant adolescent-onset variant of gender dysphoria, suggest that detransition and/or regret could be more frequent than previously reported (Boyd et al., 2022 ; Butler et al., 2022 ; Cohen et al., 2023 ; Hall et al., 2021 ; Roberts et al., 2022 ). For example, a retrospective case-note review of 175 patients who medically transitioned at an adult gender clinic in the UK reported that 6.9% of patients detransitioned within only 16 months of starting medical transition; an additional 3.4% did not strictly meet the criteria of detransitioning but had a pattern of care suggestive of detransition (Hall et al., 2021 ). A further 22% disengaged from care and were discharged from the clinic without completing their planned treatment. A second study from a UK primary care practice that included 41 transgender-identifying patients (median age 22 years, range 19 to 89 years) found that 12% of those who had started hormonal treatments either detransitioned or documented regret after an average of five years (Boyd et al., 2022 ). In addition, 7.3% stopped hormonal therapy for medical or unknown reasons. An analysis of 1089 young people referred to pediatric endocrine clinics in England between 2008 and 2021 reported that 5.3% stopped treatment with puberty blockers or cross-sex hormones and reidentified with their birth sex before their eighteenth birthday (Butler et al., 2022 ). Outcomes following transfer to an adult service at age 18 were not reported.
A similar pattern has been documented in the USA. A recent study of 68 adolescents receiving care within the Children’s National gender services program found that 29% had what the authors termed a “shift” in their request for hormonal therapy over two years of follow-up (Cohen et al., 2023 ). Eighteen had a shift before starting hormonal therapy and two after. The most common pattern in the former group was withdrawing the request, followed by resubmitting the original request (9/18). Five youth withdrew the request with no new request at two years and one was still considering hormonal therapy as a possibility in the future. Two had a pattern of oscillating requests with one ultimately starting hormonal therapy. Among the two patients that stopped hormonal therapy, one viewed their experience as negative and the other reported meeting their gender-related goals. Another study that included 952 transgender adolescents and adults in the US military healthcare system found 29% discontinued hormonal therapies within four years (Roberts et al., 2022 ). While stopping hormonal therapy is not synonymous with regret, this high rate of discontinuation for a therapy that is usually intended to be life-long is notable. Moreover, regret can take up to 10 years to materialize (Dhejne et al., 2014 ; Wiepjes et al., 2018 ), so these numbers likely underestimate the full scope of regret and detransition.
Reasons for Detransition
Recent data have shed light on a complex range of experiences that lead people to detransition (Exposito-Campos, 2021 ; Littman, 2021 ; MacKinnon et al., 2022b ; Pullen Sansfaçon et al., 2023 ; Turban et al., 2021b ; Vandenbussche, 2022 ). It should be noted, however, that the term detransition can hold a wide array of possible meanings for transgender people, detransitioners, and researchers, leading to inconsistences in its usage. Nonetheless, two typologies that fit under a broad definition of detransition, but that appear to have distinct causes and trajectories have emerged from the available literature (Exposito-Campos, 2021 ). First, external forces, such as discrimination, pressure from family, difficulties finding employment, or loss of health insurance, seem to drive the decision to detransition in studies that largely focused on participants who detransitioned at some point but later reidentified as transgender or gender-diverse (Exposito-Campos, 2021 ; MacKinnon et al., 2022b ; Turban et al., 2021b ). Moreover, rates of regret were generally low in these studies, and many participants believed their transition, detransition, and retransition were opportunities to explore and clarify their gender identity (MacKinnon et al., 2022b ; Turban et al., 2021b ). A second pattern is apparent in studies where most participants who detransitioned returned to identifying with their birth sex (Exposito-Campos, 2021 ; Littman, 2021 ; Vandenbussche, 2022 ). Participants in these studies frequently cited internal factors as the main drivers of their decision to detransition; worsening mental health or the realization that gender dysphoria was a maladaptive response to trauma, misogyny, internalized homophobia, or pressure from social media and online communities were examples of internal factors shared by participants (Exposito-Campos, 2021 ; Littman, 2021 ; Vandenbussche, 2022 ). Additionally, most participants in these studies deeply regretted their decision to transition and felt they were harmed by the clinicians and healthcare systems that facilitated it (Littman, 2021 ; Vandenbussche, 2022 ).
A study using data from the 2015 U.S. Trans Survey (USTS) illustrates the first narrative, whereby sociocultural forces appeared to drive the decision to detransition (Turban et al., 2021b ). The USTS contains data from 27,715 transgender and gender-diverse adults recruited through LGBTQ-specific organizations, support groups, health centers, and online communities. Reasons for detransition were evaluated in the subset of 2,242 people who previously detransitioned but reidentified as transgender or gender-diverse at the time of the survey. In total, 83% cited at least one external factor as a reason for detransitioning (e.g., pressure from family members, pressure from the community, societal stigma, pressure from an employer, or difficulty finding employment, etc.); only 16% cited at least one internal factor.
Similar themes emerged from a qualitative study of 28 Canadian adults who identified as “detransitioning, retransitioning, detrans, retrans, reidentifying, experiencing a shift in gender identity after initiating transition, or having stopped transition” (MacKinnon et al., 2022b ). Reasons for discontinuing or reversing gender transition included physical or mental health concerns, surgical complications, postoperative pain, unsupportive parents or romantic partners, employment discrimination, and difficulties accessing healthcare. A minority of participants experienced regret (22%) or ambivalence (11%), while most (67%) reported that they had positive feelings about the transition-related medical interventions they received. Many in the latter group identified as non-binary or gender-fluid at the time of the study and had come to accept the permanent changes to their body as part of their gender identity “journey.”
A very different narrative emerged from a study that recruited 237 participants from online communities of detransitioners who answered affirmatively to the question, “Did you transition medically and/or socially and then stopped?”(Vandenbussche, 2022 ). The most cited reasons for detransitioning included: realization that gender dysphoria was related to other issues (71%), health concerns (62%), transition failed to help with dysphoria (50%), found other ways to manage dysphoria (45%), unhappiness with social changes (44%), and change in political views (43%). Only 13% and 10% cited a lack of social support and discrimination as reasons for detransition, respectively. In total, 60% reported needing psychological support to cope with feelings of regret.
High rates of regret (80% any level of regret and 50% strong or very strong regret) were also reported in a study describing the experiences of 100 detransitioners recruited with outreach to sources with different perspectives about transition and detransition, including the World Professional Association for Transgender Health (WPATH) listserv and online detransition forums (Littman, 2021 ). All participants in this study received hormonal therapies and/or had undergone surgery and then stopped medications or had surgery to reverse changes from transition. At the time of the study, 61% of participants had returned to identifying solely as their birth sex and another 10% identified as their birth sex plus a second identification. The most frequently reported reason for detransitioning by both sexes was that their personal definition of male and female had changed so that they became more comfortable identifying with their birth sex (60%). Other reasons for detransition differed between male and female participants. Males reported ongoing mental health problems, dissatisfaction with physical results of transition, deteriorating physical health, and discrimination (36% each). By contrast, females cited concern about potential medical complications (58%), dissatisfaction with physical results (51%), ongoing mental health problems (45%), and the realization that gender dysphoria was caused by other factors such as trauma, abuse, or mental health conditions (41%). Only 17% of females cited discrimination as contributing to their decision to detransition.
Gaps in Medical and Mental Healthcare
Gaps in the quality and accessibility of medical and mental healthcare have consistently been highlighted in studies and personal testimonies of detransitioners (Littman, 2021 ; MacKinnon et al., 2022b ; Vandenbussche, 2022 ). Many detransitioners reported not feeling properly informed about health implications of treatments before undergoing them (Gribble et al., 2023 ; Littman, 2021 ; Pullen Sansfaçon et al., 2023 ; Vandenbussche, 2022 ). Likewise, many felt that they did not receive sufficient exploration of preexisting psychological and emotional problems and continued to struggle post-transition when they realized gender transition was not a panacea (Littman, 2021 ; Pullen Sansfaçon et al., 2023 ; Respaut et al., 2022 ; Sanders et al., 2023 ; Vandenbussche, 2022 ). Despite ongoing medical needs, most patients did not maintain contact with their gender clinic during their detransition (Littman, 2021 ; MacKinnon et al., 2022b ; Vandenbussche, 2022 ). In one study, only 24% informed the physicians and clinics that facilitated their transition that they had detransitioned (Littman, 2021 ). For some, feelings of shame and fear of stigma were barriers to accessing medical care. Others believed the medical establishment failed them by allowing, and even encouraging, them to transition without adequate assessment or discussion of other ways to address, treat, or live with gender dysphoria (Exposito-Campos, 2021 ; Sanders et al., 2023 ). For many, needed supports and clinical expertise were simply not available (MacKinnon et al., 2022b ; Vandenbussche, 2022 ).
Detransitioners consistently reported wanting more information about stopping or changing hormones as well as information on surgical reversal and restoration options, long-term effects of hormones, and tests to determine reproductive capacity (MacKinnon et al., 2022b ; Sanders et al., 2023 ; Vandenbussche, 2022 ). Many stopped hormonal therapies “cold turkey” without medical supervision, instead turning to online detransition networks and social media (MacKinnon et al., 2022b ). Patients who underwent gonadectomies as part of their transition, and therefore needed to change rather than discontinue hormonal therapy, reported that medical supervision was often suboptimal, and clinicians were not sufficiently knowledgeable to manage their care (MacKinnon et al., 2022b ).
With regard to mental health needs, patients reported requiring psychological support to manage mental health problems that were unaddressed or exacerbated by transition (Marchiano, 2021 ; Vandenbussche, 2022 ). Moreover, some needed support to cope with feelings of grief and regret and to accept physical changes that could not be reversed, such as deepened voice, facial hair, and alopecia from testosterone or breast growth from estrogen (Marchiano, 2021 ; Pullen Sansfaçon et al., 2023 ; Vandenbussche, 2022 ). However, many therapists were reluctant to be involved in the care of detransitioners due to fears that they would be accused of performing conversion therapy if they deviated from the affirmative approach (Griffin et al., 2021 ). Detransitioners also described being vilified by the transgender community once they started to express doubts or questions regarding transition, compounding feelings of isolation (MacKinnon et al., 2022a ; Respaut et al., 2022 ; Vandenbussche, 2022 ).
As outlined in this essay, there is still a great deal to learn about how to best support detransitioners. Unfortunately, gender services remain fragmented in most countries, and no one is systematically tracking how many young people regret transition or, for that matter, how many are helped by it. Moreover, many detransitioners appear to feel betrayed by the clinicians and medical system that facilitated their transition and do not return for follow-up (Littman, 2021 ), making assessing outcomes challenging. Given the novelty of the gender affirmation model and a “honeymoon” period of up to 10 years (Dhejne et al., 2014 ; Wiepjes et al., 2018 ), the full extent of regret and detransition in young people transitioning today, under vastly different circumstances than in the past, will not be known for many years. Moreover, regret is an emotion that is unique in its relation to personal agency (Zeelenberg & Pieters, 2007 ), but the exercise of personal agency in the transition process might have been limited for people who began transition as minors, whose decision-making capacity was compromised by mental illness, or who were not fully informed of known and potential adverse health implications. Feelings of profound grief about lost opportunities and negative repercussions of transition might not be fully captured by framing the emotional experience in terms of regret.
While there is growing recognition of the need to support detransitioners, clinicians lack guidance on best practices. There is no single narrative to describe their experiences and clinicians will need to be prepared to respond to the diversity of their experiences and trajectories. Some detransitioners might continue to have gender dysphoria or will have iatrogenic dysphoria related to irreversible effects of hormones and surgery and will need non-medical ways to cope with it, as well as ongoing psychological support to manage possible anxiety, regret, and shame related to detransitioning. Moreover, research is urgently needed to determine the safest way to discontinue or change hormonal therapies, as well as reversal or reconstructive surgical options.
Natural questions that arise are whether detransition can be prevented and, importantly, whether inappropriate transitions can be avoided. Multiple external forces that contribute to some peoples’ decision to detransition can be intervened upon. These include connecting patients with legal support in the face of employment discrimination and ensuring those with medical or surgical complications receive appropriate medical care (Turban et al., 2022 ). Comprehensive psychosocial support during the transition process could fortify people against societal or workplace discrimination, as well as pressure from friends and family (Exposito-Campos, 2021 ). However, clinicians should avoid creating unrealistic expectations about the challenges people will face following medical transition. As society learns to become more accepting, transgender people will still need to contend with the reality that gender identity cannot take precedence over sex in all circumstances. Moreover, when obtaining informed consent, clinicians should ensure patients understand that medical transition is not an antidote for the enduring consequences of childhood adversity, co-existing physical or phycological disadvantages, or unfortunate family circumstances (Levine et al., 2022 ). Additionally, failing to discuss alternatives to medicalization and promoting unsubstantiated claims that suicide is the inevitable alternative to medical transition (Biggs, 2022 ; Kirkup, 2020 ) robs patients of the opportunity to explore other management strategies.
The finding that many people were motivated to detransition due to a change in their personal definition of male or female, which in turn led to them to feel more comfortable identifying with their birth sex (Littman, 2021 ), raises questions about whether some individuals interpret gender nonconformity as transgender identification. Engaging in traditionally “feminine” tasks does not make one less of a man. Likewise, “masculine” pursuits are not incompatible with womanhood. Clothes, haircuts, colors, mannerisms, etc., do not have a sex. The original Dutch protocol for transition of minors emphasized the role of psychotherapy in fostering self-acceptance of gender-nonconformity prior to contemplating medical interventions (de Vries et al., 2006 ) and a growing body of literature describes an exploratory psychotherapeutic approach that can help people expand their definition of what it means to be a man or a woman, thereby potentially eliminating the need for transition-related medical interventions (Bonfatto & Crasnow, 2018 ; Churcher Clarke & Spiliadis, 2019 ; Evans, 2022 ; Hakeem, 2018 ).
Since our ability to predict with who will benefit from medical transition and who will be harmed is limited, it is imperative that we learn from the experiences of detransitioners to improve the process of evaluation, counseling, and informed consent. Communication and language have been important in the debate about appropriate medical care for people with gender dysphoria. The finding that many detransitioners felt the information they received about medical interventions was overly positive about potential benefits while risks were downplayed (Littman, 2021 ), suggests communication needs to be more balanced, evidence-informed, and precise. Patients, parents, and the general public in North America are often told that the use of hormonal therapies and surgery is uncontroversial and backed by rigorous science, yet there is a great deal of disagreement within the international medical community about the benefits and harms of these interventions (Block, 2023 ). Multiple European countries that were once strong proponents of the youth gender transition are now reversing course and prioritizing psychological support and treatment for comorbid psychiatric conditions after their own systematic reviews found the evidence underpinning gender-affirming medical interventions to be weak and uncertain (Block, 2023 ; Cass, 2022 ; COHERE, 2020 ; Socialstyrelsen, 2022 ).
Regarding language, efforts to normalize or destigmatize treatments for those who might benefit from them have obscured the severity of some interventions. One’s reaction to “top surgery” versus “double mastectomy,” “bottom surgery” versus “phalloplasty” or “vaginoplasty,” for example, are likely to be very different. Even the term “detransition” has become verboten among some transgender advocates due to fears that it could be weaponized to deny medical care to those seeking gender transition (Turban et al., 2022 ). Phrases such as “gender-identity journey” and “dynamic desires for gender-affirming medical interventions” have been proposed as alternatives (Turban et al., 2022 ). However, we should be cautious about adopting euphemisms that might mask iatrogenic harm.
Primum non nocere has been the guiding tenet of medicine for millennia. Adhering to this principle is relatively straightforward when a diagnosis is based on clearly defined objective criteria and practice is guided by high-quality evidence establishing a treatment as both safe and effective. However, complex clinical cases are often fraught with diagnostic uncertainty and many treatments are not backed by compelling scientific evidence. In these situations, minimizing iatrogenic harm requires application of cautious, thoughtful clinical judgement, meticulous examination of the data that are available, as well as a willingness to change practice in the face of new evidence. Moving forward, the field of gender medicine will need to commit to conducting robust research, challenging fundamental assumptions, scrutinizing their practice patterns, and embracing debate.
Open access funding provided by the Society for Evidence-Based Gender Medicine.
Data Availability
Code availability, declarations.
None to declare.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- Aitken M, Steensma TD, Blanchard R, VanderLaan DP, Wood H, Fuentes A, Spegg C, Wasserman L, Ames M, Fitzsimmons CL, Leef JH, Lishak V, Reim E, Takagi A, Vinik J, Wreford J, Cohen-Kettenis PT, de Vries ALC, Kreukels BPC, Zucker KJ. Evidence for an altered sex ratio in clinic-referred adolescents with gender dysphoria. Journal of Sexual Medicine. 2015; 12 (3):756–763. doi: 10.1111/jsm.12817. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Amengual T, Kunstman K, Lloyd RB, Janssen A, Wescott AB. Readiness assessments for gender-affirming surgical treatments: A systematic scoping review of historical practices and changing ethical considerations. Frontiers in Psychiatry. 2022; 13 :1006024. doi: 10.3389/fpsyt.2022.1006024. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Arnoldussen M, de Rooy FBB, de Vries ALC, van der Miesen AIR, Popma A, Steensma TD. Demographics and gender-related measures in younger and older adolescents presenting to a gender service. European Child & Adolescent Psychiatry. 2022 doi: 10.1007/s00787-022-02082-8. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ashley F. Gatekeeping hormone replacement therapy for transgender patients is dehumanising. Journal of Medical Ethics. 2019; 45 (7):480–482. doi: 10.1136/medethics-2018-105293. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ashley F. Adolescent medical transition is ethical: An analogy with reproductive health. The Kennedy Institute of Ethics Journal. 2022; 32 (2):127–171. doi: 10.1353/ken.2022.0010. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bauer GR, Pacaud D, Couch R, Metzger DL, Gale L, Gotovac S, Mokashi A, Feder S, Raiche J, Speechley KN, Temple Newhook J, Ghosh S, Pullen Sansfacon A, Susset F, Lawson ML. Transgender youth referred to clinics for gender-affirming medical care in Canada. Pediatrics. 2021; 148 (5):e2020047266. doi: 10.1542/peds.2020-047266. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Becerra-Culqui TA, Liu Y, Nash R, Cromwell L, Flanders WD, Getahun D, Giammattei SV, Hunkeler EM, Lash TL, Millman A, Quinn VP, Robinson B, Roblin D, Sandberg DE, Silverberg MJ, Tangpricha V, Goodman M. Mental health of transgender and gender nonconforming youth compared with their peers. Pediatrics. 2018; 141 (5):e20173845. doi: 10.1542/peds.2017-3845. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Biggs M. Revisiting the effect of GnRH analogue treatment on bone mineral density in young adolescents with gender dysphoria [Letter to the Editor] Journal of Pediatric Endocrinology and Metabolism. 2021; 34 (7):937–939. doi: 10.1515/jpem-2021-0180. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Biggs M. Suicide by clinic-referred transgender adolescents in the United Kingdom [Letter to the Editor] Archives of Sexual Behavior. 2022; 51 (2):685–690. doi: 10.1007/s10508-022-02287-7. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Blanchard R. The concept of autogynephilia and the typology of male gender dysphoria. Journal of Nervous and Mental Disease. 1989; 177 (10):616–623. doi: 10.1097/00005053-198910000-00004. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Blanchard R, Steiner BW, Clemmensen LH, Dickey R. Prediction of regrets in postoperative transsexuals. Canadian Journal of Psychiatry. 1989; 34 (1):43–45. doi: 10.1177/070674378903400111. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Block J. Gender dysphoria in young people is rising-and so is professional disagreement. BMJ. 2023; 380 :382. doi: 10.1136/bmj.p382. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bonfatto M, Crasnow E. Gender/ed identities: An overview of our current work as child psychotherapists in the Gender Identity Development Service. Journal of Child Psychotherapy. 2018; 44 (1):29–46. doi: 10.1080/0075417x.2018.1443150. [ CrossRef ] [ Google Scholar ]
- Bornioli A, Lewis-Smith H, Slater A, Bray I. Body dissatisfaction predicts the onset of depression among adolescent females and males: A prospective study. Journal of Epidemiology & Community Health. 2021; 75 (4):343–348. doi: 10.1136/jech-2019-213033. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Boyd, I., Hackett, T., & Bewley, S. (2022). Care of transgender patients: A general practice quality improvement approach. Healthcare, 10 (1). 10.3390/healthcare10010121 [ PMC free article ] [ PubMed ]
- Brik T, Vrouenraets L, de Vries MC, Hannema SE. Trajectories of adolescents treated with gonadotropin-releasing hormone analogues for gender dysphoria. Archives of Sexual Behavior. 2020; 49 (7):2611–2618. doi: 10.1007/s10508-020-01660-8. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Butler G, Adu-Gyamfi K, Clarkson K, El Khairi R, Kleczewski S, Roberts A, Segal TY, Yogamanoharan K, Alvi S, Amin N, Carruthers P, Dover S, Eastman J, Mushtaq T, Masic U, Carmichael P. Discharge outcome analysis of 1089 transgender young people referred to paediatric endocrine clinics in England 2008–2021. Archives of Disease in Childhood. 2022; 107 (11):1018–1022. doi: 10.1136/archdischild-2022-324302. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carmichael P, Butler G, Masic U, Cole TJ, De Stavola BL, Davidson S, Skageberg EM, Khadr S, Viner RM. Short-term outcomes of pubertal suppression in a selected cohort of 12 to 15 year old young people with persistent gender dysphoria in the UK. PLoS ONE. 2021; 16 (2):e0243894. doi: 10.1371/journal.pone.0243894. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Casey BJ, Jones RM, Hare TA. The adolescent brain. Annals of the New York Academy of Sciences. 2008; 1124 (1):111–126. doi: 10.1196/annals.1440.010. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cass, H. (2022). The Cass review. Independent review of gender identity services for children and young people. Interim report. https://cass.independent-review.uk/publications/interim-report/
- Churcher Clarke A, Spiliadis A. 'Taking the lid off the box': The value of extended clinical assessment for adolescents presenting with gender identity difficulties. Clinical Child Psychology and Psychiatry. 2019; 24 (2):338–352. doi: 10.1177/1359104518825288. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cohen A, Gomez-Lobo V, Willing L, Call D, Damle LF, D'Angelo LJ, Song A, Strang JF. Shifts in gender-related medical requests by transgender and gender-diverse adolescents. Journal of Adolescent Health. 2023; 72 (3):428–436. doi: 10.1016/j.jadohealth.2022.10.020. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cohen-Kettenis PT, Owen A, Kaijser VG, Bradley SJ, Zucker KJ. Demographic characteristics, social competence, and behavior problems in children with gender identity disorder: A cross-national, cross-clinic comparative analysis. Journal of Abnormal Child Psychology. 2003; 31 (1):41–53. doi: 10.1023/a:1021769215342. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cohen-Kettenis PT, Pfäfflin F. Transgenderism and intersexuality in childhood and adolescence: Making choices. Sage Publications; 2003. [ Google Scholar ]
- COHERE (Council for the Choices in Health Care). (2020). Palveluvalikoimaneuvoston Suositus: Alaikäisten Sukupuoli-identiteetin Variaatioihin Liittyvän Dysforian Lääketieteelliset Hoitomenetelmät [Recommendation of the Council for Choices in Health Care in Finland: Medical treatment methods for dysphoria related to gender variance in minors].
- Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J, Fraser L, Green J, Knudson G, Meyer WJ, Monstrey S, Adler RK, Brown GR, Devor AH, Ehrbar R, Ettner R, Eyler E, Garofalo R, Karasic DH, Zucker K. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. International Journal of Transgenderism. 2012; 13 (4):165–232. doi: 10.1080/15532739.2011.700873. [ CrossRef ] [ Google Scholar ]
- Coleman E, Radix AE, Bouman WP, Brown GR, de Vries ALC, Deutsch MB, Ettner R, Fraser L, Goodman M, Green J, Hancock AB, Johnson TW, Karasic DH, Knudson GA, Leibowitz SF, Meyer-Bahlburg HFL, Monstrey SJ, Motmans J, Nahata L, Arcelus J. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; 23 (Suppl 1):S1–S259. doi: 10.1080/26895269.2022.2100644. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Crocetti E. Identity formation in adolescence: The dynamic of forming and consolidating identity commitments. Child Development Perspectives. 2017; 11 (2):145–150. doi: 10.1111/cdep.12226. [ CrossRef ] [ Google Scholar ]
- D'Angelo R. Psychiatry's ethical involvement in gender-affirming care. Australasian Psychiatry. 2018; 26 (5):460–463. doi: 10.1177/1039856218775216. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- D'Angelo R. The complexity of childhood gender dysphoria. Australasian Psychiatry. 2020; 28 (5):530–532. doi: 10.1177/1039856220917076. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- de Vries ALC, Cohen-Kettenis PT. Clinical management of gender dysphoria in children and adolescents: The Dutch approach. Journal of Homosexuality. 2012; 59 (3):301–320. doi: 10.1080/00918369.2012.653300. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- de Vries ALC, Cohen-Kettenis PT, Delemarre-van de Waal H. Clinical management of gender dysphoria in adolescents. International Journal of Transgenderism. 2006; 9 (3–4):83–94. doi: 10.1300/J485v09n03_04. [ CrossRef ] [ Google Scholar ]
- de Vries ALC, Steensma TD, Doreleijers TA, Cohen-Kettenis PT. Puberty suppression in adolescents with gender identity disorder: A prospective follow-up study. Journal of Sexual Medicine. 2011; 8 (8):2276–2283. doi: 10.1111/j.1743-6109.2010.01943.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dhejne C, Oberg K, Arver S, Landen M. An analysis of all applications for sex reassignment surgery in Sweden, 1960–2010: Prevalence, incidence, and regrets. Archives of Sexual Behavior. 2014; 43 (8):1535–1545. doi: 10.1007/s10508-014-0300-8. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Drummond KD, Bradley SJ, Peterson-Badali M, Zucker KJ. A follow-up study of girls with gender identity disorder. Developmental Psychology. 2008; 44 (1):34–45. doi: 10.1037/0012-1649.44.1.34. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ehrensaft, D. (2016). The gender spread. In The gender creative child: Pathways for nurturing and supporting children who live outside gender boxes . The Experiment, LLC.
- Evans M. ‘If only I were a boy …’: Psychotherapeutic explorations of transgender in children and adolescents. British Journal of Psychotherapy. 2022; 38 (2):269–285. doi: 10.1111/bjp.12733. [ CrossRef ] [ Google Scholar ]
- Evans M. Assessment and treatment of a gender-dysphoric person with a traumatic history. Journal of Child Psychotherapy. 2023; 49 (1):60–75. doi: 10.1080/0075417x.2023.2172741. [ CrossRef ] [ Google Scholar ]
- Exposito-Campos P. A typology of gender detransition and its implications for healthcare providers. Journal of Sex and Marital Therapy. 2021; 47 (3):270–280. doi: 10.1080/0092623X.2020.1869126. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gribble KD, Bewley S, Dahlen HG. Breastfeeding grief after chest masculinisation mastectomy and detransition: A case report with lessons about unanticipated harm. Frontiers in Global Womens Health. 2023; 4 :1073053. doi: 10.3389/fgwh.2023.1073053. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Griffin L, Clyde K, Byng R, Bewley S. Sex, gender and gender identity: A re-evaluation of the evidence. Bjpsych Bulletin. 2021; 45 (5):291–299. doi: 10.1192/bjb.2020.73. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hakeem A. Psychotherapy for gender identity disorders. Advances in Psychiatric Treatment. 2018; 18 (1):17–24. doi: 10.1192/apt.bp.111.009431. [ CrossRef ] [ Google Scholar ]
- Hall R, Mitchell L, Sachdeva J. Access to care and frequency of detransition among a cohort discharged by a UK national adult gender identity clinic: Retrospective case-note review. BJPsych Open. 2021; 7 (6):e184. doi: 10.1192/bjo.2021.1022. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Haltigan JD, Pringsheim TM, Rajkumar G. Social media as an incubator of personality and behavioral psychopathology: Symptom and disorder authenticity or psychosomatic social contagion? Comprehensive Psychiatry. 2023; 121 :152362. doi: 10.1016/j.comppsych.2022.152362. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Handler T, Hojilla JC, Varghese R, Wellenstein W, Satre DD, Zaritsky E. Trends in referrals to a pediatric transgender clinic. Pediatrics. 2019; 144 (5):e20191368. doi: 10.1542/peds.2019-1368. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hembree WC, Cohen-Kettenis PT, Gooren L, Hannema SE, Meyer WJ, Murad MH, Rosenthal SM, Safer JD, Tangpricha V, T'Sjoen GG. Endocrine treatment of gender-dysphoric/gender-incongruent persons: An Endocrine Society Clinical Practice Guideline. Journal of Clinical Endocrinology Metabolism. 2017; 102 (11):3869–3903. doi: 10.1210/jc.2017-01658. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Irwig MS. Cardiovascular health in transgender people. Reviews in Endocrine and Metabolic Disorders. 2018; 19 (3):243–251. doi: 10.1007/s11154-018-9454-3. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kaltiala R, Bergman H, Carmichael P, de Graaf NM, Egebjerg Rischel K, Frisen L, Schorkopf M, Suomalainen L, Waehre A. Time trends in referrals to child and adolescent gender identity services: A study in four Nordic countries and in the UK. Nordic Journal of Psychiatry. 2020; 74 (1):40–44. doi: 10.1080/08039488.2019.1667429. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kaltiala R, Heino E, Tyolajarvi M, Suomalainen L. Adolescent development and psychosocial functioning after starting cross-sex hormones for gender dysphoria. Nordic Journal of Psychiatry. 2020; 74 (3):213–219. doi: 10.1080/08039488.2019.1691260. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kaltiala-Heino R, Sumia M, Tyolajarvi M, Lindberg N. Two years of gender identity service for minors: Over representation of natal girls with severe problems in adolescent development. Child and Adolescent Psychiatry and Mental Health. 2015; 9 (1):9. doi: 10.1186/s13034-015-0042-y. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kimberly LL, Folkers KM, Friesen P, Sultan D, Quinn GP, Bateman-House A, Parent B, Konnoth C, Janssen A, Shah LD, Bluebond-Langner R, Salas-Humara C. Ethical issues in gender-affirming care for youth. Pediatrics. 2018; 142 (6):e20181537. doi: 10.1542/peds.2018-1537. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kingsbury M, Hammond NG, Johnstone F, Colman I. Suicidality among sexual minority and transgender adolescents: A nationally representative population-based study of youth in Canada. Canadian Medical Association Journal. 2022; 194 (22):E767–E774. doi: 10.1503/cmaj.212054. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kirkup, J. 2020. The BBC should be ashamed of its reporting on trans teenagers. The Spectator . https://www.spectator.co.uk/article/the-bbc-should-be-ashamed-of-its-reporting-on-trans-teenagers/?zephr_sso_ott=8ysQD7 .
- Knoll LJ, Magis-Weinberg L, Speekenbrink M, Blakemore SJ. Social influence on risk perception during adolescence. Psychological Science. 2015; 26 (5):583–592. doi: 10.1177/0956797615569578. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kornienko O, Santos CE, Martin CL, Granger KL. Peer influence on gender identity development in adolescence. Developmental Psychology. 2016; 52 (10):1578–1592. doi: 10.1037/dev0000200. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kozlowska K, Chudleigh C, McClure G, Maguire AM, Ambler GR. Attachment patterns in children and adolescents with gender dysphoria. Frontiers in Psychology. 2020; 11 :582688. doi: 10.3389/fpsyg.2020.582688. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kroger J, Martinussen M, Marcia JE. Identity status change during adolescence and young adulthood: A meta-analysis. Journal of Adolescence. 2009; 33 (5):683–698. doi: 10.1016/j.adolescence.2009.11.002. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Krumm A, Ferraro FR, Ingvalson B. Exploring the relationship between autistic traits and body image, body satisfaction, and body competence. Journal of Psychology. 2017; 151 (6):566–579. doi: 10.1080/00223980.2017.1372343. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lantz EL, Gaspar ME, DiTore R, Piers AD, Schaumberg K. Conceptualizing body dissatisfaction in eating disorders within a self-discrepancy framework: A review of evidence. Eating and Weight Disorders—Studies on Anorexia, Bulimia and Obesity. 2018; 23 (3):275–291. doi: 10.1007/s40519-018-0483-4. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lawrence AA. Factors associated with satisfaction or regret following male-to-female sex reassignment surgery. Archives of Sexual Behavior. 2003; 32 (4):299–315. doi: 10.1023/a:1024086814364. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Levine SB. Ethical concerns about emerging treatment paradigms for gender dysphoria. Journal of Sex & Marital Therapy. 2018; 44 (1):29–44. doi: 10.1080/0092623X.2017.1309482. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Levine SB. Transitioning back to maleness. Archives of Sexual Behavior. 2018; 47 (4):1295–1300. doi: 10.1007/s10508-017-1136-9. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Levine SB, Abbruzzese E, Mason JW. Reconsidering informed consent for trans-identified children, adolescents, and young adults. Journal of Sex & Marital Therapy. 2022; 48 (7):706–727. doi: 10.1080/0092623X.2022.2046221. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Littman L. Parent reports of adolescents and young adults perceived to show signs of a rapid onset of gender dysphoria. PLoS ONE. 2018; 13 (8):e0202330. doi: 10.1371/journal.pone.0202330. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Littman L. Individuals treated for gender dysphoria with medical and/or surgical transition who subsequently detransitioned: A survey of 100 detransitioners. Archives of Sexual Behavior. 2021; 50 (8):3353–3369. doi: 10.1007/s10508-021-02163-w. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ludvigsson JF, Adolfsson J, Hoistad M, Rydelius PA, Kristrom B, Landen M. A systematic review of hormone treatment for children with gender dysphoria and recommendations for research. Acta Paediatrica. 2023 doi: 10.1111/apa.16791. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- MacKinnon KR, Gould AW, Ashley F, Enxuga G, Kia H, Ross LE. (De)transphobia: Examining the socio-politically driven gender minority stressors experienced by people who detransitioned. Bulletin of Applied Transgender Studies. 2022; 1 (3):235–259. doi: 10.57814/8nd4-6a89. [ CrossRef ] [ Google Scholar ]
- MacKinnon KR, Kia H, Salway T, Ashley F, Lacombe-Duncan A, Abramovich A, Enxuga G, Ross LE. Health care experiences of patients discontinuing or reversing prior gender-affirming treatments. JAMA Network Open. 2022; 5 (7):e2224717. doi: 10.1001/jamanetworkopen.2022.24717. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Marchiano, L. (2020). The ranks of gender detransitioners are growing. We need to understand why. Quilette . https://quillette.com/2020/01/02/the-ranks-of-gender-detransitioners-are-growing-we-need-to-understand-why/ .
- Marchiano L. Gender detransition: A case study. Journal of Analytical Psychology. 2021; 66 (4):813–832. doi: 10.1111/1468-5922.12711. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Morandini JS, Kelly A, de Graaf NM, Malouf P, Guerin E, Dar-Nimrod I, Carmichael P. Is social gender transition associated with mental health status in children and adolescents with gender dysphoria? Archives of Sexual Behavior. 2023; 52 (3):1045–1060. doi: 10.1007/s10508-023-02588-5. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Narayan, S. K., Hontscharuk, R., Danker, S., Guerriero, J., Carter, A., Blasdel, G., Bluebond, L. R., Ettner, R., Radix, A., Schechter, L., & Berli, J. U. (2021). Guiding the conversation-types of regret after gender-affirming surgery and their associated etiologies. Annals of Translational Medicine, 9 (7). 10.21037/atm-20-6204 [ PMC free article ] [ PubMed ]
- National Institute of Health and Care Excellence (NICE). (2020a). Evidence review: Gender-affirming hormones for children and adolescents with gender dysphoria . https://cass.independent-review.uk/nice-evidence-reviews/ .
- National Institute of Health and Care Excellence (NICE). (2020b). Evidence review: Gonadotrophin releasing hormone analogues for children and adolescents with gender dysphoria . https://cass.independent-review.uk/nice-evidence-reviews/ .
- Olson KR, Durwood L, Horton R, Gallagher NM, Devor A. Gender identity 5 years after social transition. Pediatrics. 2022; 150 (2):e2021056082. doi: 10.1542/peds.2021-056082. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pfäfflin F. Regrets after sex reassignment surgery. Journal of Psychology & Human Sexuality. 1993; 5 (4):69–85. doi: 10.1300/J056v05n04_05. [ CrossRef ] [ Google Scholar ]
- Pullen Sansfaçon A, Gelly MA, Gravel R, Medico D, Baril A, Susset F, Paradis A. A nuanced look into youth journeys of gender transition and detransition. Infant and Child Development. 2023; 32 (2):e2402. doi: 10.1002/icd.2402. [ CrossRef ] [ Google Scholar ]
- r/detrans. 2023. [Reddit]. https://www.reddit.com/r/detrans/ .
- Rafferty, J., Committee on Psychosocial Aspects of Child and Family Health, Committee on Adolescence, Section on Lesbian, Gay, Bisexual, and Transgender Health & Wellness. (2018). Ensuring comprehensive care and support for transgender and gender-diverse children and adolescents. Pediatrics , 142 (4), e20182162. 10.1542/peds.2018-2162 [ PubMed ]
- Rehman J, Lazer S, Benet AE, Schaefer LC, Melman A. The reported sex and surgery satisfactions of 28 postoperative male-to-female transsexual patients. Archives of Sexual Behavior. 1999; 28 (1):71–89. doi: 10.1023/a:1018745706354. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Respaut, R., Terhune, C., & Conlin, M. 2022. Why detransitioners are crucial to the science of gender care. Reuters . https://www.reuters.com/investigates/special-report/usa-transyouth-outcomes/ .
- Ristori J, Steensma TD. Gender dysphoria in childhood. International Review of Psychiatry. 2016; 28 (1):13–20. doi: 10.3109/09540261.2015.1115754. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Roberts CM, Klein DA, Adirim TA, Schvey NA, Hisle-Gorman E. Continuation of gender-affirming hormones among transgender adolescents and adults. Journal of Clinical Endocrinology & Metabolism. 2022; 107 (9):e3937–e3943. doi: 10.1210/clinem/dgac251. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rosenthal SM. Challenges in the care of transgender and gender-diverse youth: An endocrinologist's view. Nature Reviews Endocrinology. 2021; 17 (10):581–591. doi: 10.1038/s41574-021-00535-9. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sanders T, du Plessis C, Mullens AB, Bromdal A. Navigating detransition borders: An exploration of social media narratives. Archives of Sexual Behavior. 2023; 52 (3):1061–1072. doi: 10.1007/s10508-023-02556-z. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schulz SL. The informed consent model of transgender care: An alternative to the diagnosis of gender dysphoria. Journal of Humanistic Psychology. 2017; 58 (1):72–92. doi: 10.1177/0022167817745217. [ CrossRef ] [ Google Scholar ]
- Segev-Becker A, Israeli G, Elkon-Tamir E, Perl L, Sekler O, Amir H, Interator H, Dayan SC, Chorna E, Weintrob N, Oren A. Children and adolescents with gender dysphoria in Israel: Increasing referral and fertility preservation rates. Endocrine Practice. 2020; 26 (4):423–428. doi: 10.4158/EP-2019-0418. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Singh D, Bradley SJ, Zucker KJ. A follow-up study of boys with gender identity disorder. Frontiers in Psychiatry. 2021; 12 :632784. doi: 10.3389/fpsyt.2021.632784. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Socialstyrelsen, The National Board of Health and Welfare. (2022). Care of children and adolescents with gender dysphoria . https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/kunskapsstod/2022-3-7799.pdf .
- Somerville LH. Special issue on the teenage brain: Sensitivity to social evaluation. Current Directions in Psychological Science. 2013; 22 (2):121–127. doi: 10.1177/0963721413476512. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Steensma TD, Cohen-Kettenis PT, Zucker KJ. Evidence for a change in the sex ratio of children referred for gender dysphoria: Data from the Center of Expertise on Gender Dysphoria in Amsterdam (1988–2016) [Letter to the Editor] Journal of Sex & Marital Therapy. 2018; 44 (7):713–715. doi: 10.1080/0092623X.2018.1437580. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stolk THR, Asseler JD, Huirne JAF, van den Boogaard E, van Mello NM. Desire for children and fertility preservation in transgender and gender-diverse people: A systematic review. Best Practice & Research Clinical Obstetrics & Gynaecology. 2023; 87 :102312. doi: 10.1016/j.bpobgyn.2023.102312. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Terhune, C., Respaut, R., & Conlin, M. 2022. As more transgender children seek medical care, families confront many unknowns. Reuters . https://www.reuters.com/investigates/special-report/usa-transyouth-care/ .
- Thrower E, Bretherton I, Pang KC, Zajac JD, Cheung AS. Prevalence of autism spectrum disorder and attention-deficit hyperactivity disorder amongst individuals with gender dysphoria: A systematic review. Journal of Autism and Developmental Disorders. 2020; 50 (3):695–706. doi: 10.1007/s10803-019-04298-1. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Turban JL, Brady C, Olson-Kennedy J. Understanding and supporting patients with dynamic desires for gender-affirming medical interventions [Invited Commentary] JAMA Network Open. 2022; 5 (7):e2224722. doi: 10.1001/jamanetworkopen.2022.24722. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Turban JL, King D, Li JJ, Keuroghlian AS. Timing of social transition for transgender and gender diverse youth, K-12 harassment, and adult mental health outcomes. Journal of Adolescent Health. 2021; 69 (6):991–998. doi: 10.1016/j.jadohealth.2021.06.001. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Turban JL, Loo SS, Almazan AN, Keuroghlian AS. Factors leading to "detransition" among transgender and gender diverse people in the United States: A mixed-methods analysis. LGBT Health. 2021; 8 (4):273–280. doi: 10.1089/lgbt.2020.0437. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- UNICEF. (2017). The adolescent brain: A second window of opportunity. https://www.unicef-irc.org/publications/pdf/adolescent_brain_a_second_window_of_opportunity_a_compendium.pdf .
- Valdes, L., & MacKinnon, K. R. 2023. Take detransitioners seriously. The Atlantic . https://www.theatlantic.com/ideas/archive/2023/01/detransition-transgender-nonbinary-gender-affirming-care/672745/ .
- Valentine SE, Shipherd JC. A systematic review of social stress and mental health among transgender and gender non-conforming people in the United States. Clinical Psychology Review. 2018; 66 :24–38. doi: 10.1016/j.cpr.2018.03.003. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- van de Grift TC, Elaut E, Cerwenka SC, Cohen-Kettenis PT, Kreukels BPC. Surgical satisfaction, quality of life, and their association after gender-affirming surgery: A follow-up study. Journal of Sex & Marital Therapy. 2018; 44 (2):138–148. doi: 10.1080/0092623X.2017.1326190. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- van der Loos M, Klink DT, Hannema SE, Bruinsma S, Steensma TD, Kreukels BPC, Cohen-Kettenis PT, de Vries ALC, den Heijer M, Wiepjes CM. Children and adolescents in the Amsterdam cohort of gender dysphoria: Trends in diagnostic and treatment trajectories during the first 20 years of the Dutch protocol. Journal of Sexual Medicine. 2023; 20 (3):398–409. doi: 10.1093/jsxmed/qdac029. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vandenbussche E. Detransition-related needs and support: A cross-sectional online survey. Journal of Homosexuality. 2022; 69 (9):1602–1620. doi: 10.1080/00918369.2021.1919479. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vrouenraets L, de Vries ALC, Arnoldussen M, Hannema SE, Lindauer RJL, de Vries MC, Hein IM. Medical decision-making competence regarding puberty suppression: Perceptions of transgender adolescents, their parents and clinicians. European Child & Adolescent Psychiatry. 2022 doi: 10.1007/s00787-022-02076-6. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Weyers S, Elaut E, De Sutter P, Gerris J, T'Sjoen G, Heylens G, De Cuypere G, Verstraelen H. Long-term assessment of the physical, mental, and sexual health among transsexual women. Journal of Sexual Medicine. 2009; 6 (3):752–760. doi: 10.1111/j.1743-6109.2008.01082.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wiepjes CM, Nota NM, de Blok CJM, Klaver M, de Vries ALC, Wensing-Kruger SA, de Jongh RT, Bouman MB, Steensma TD, Cohen-Kettenis PT, Gooren LJG, Kreukels BPC, den Heijer M. The Amsterdam Cohort of Gender Dysphoria Study (1972–2015): Trends in prevalence, treatment, and regrets. Journal of Sexual Medicine. 2018; 15 (4):582–590. doi: 10.1016/j.jsxm.2018.01.016. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Withers R. Transgender medicalization and the attempt to evade psychological distress. Journal of Analalytical Psychology. 2020; 65 (5):865–889. doi: 10.1111/1468-5922.12641. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wood H, Sasaki S, Bradley SJ, Singh D, Fantus S, Owen-Anderson A, Di Giacomo A, Bain J, Zucker KJ. Patterns of referral to a gender identity service for children and adolescents (1976–2011): Age, sex ratio, and sexual orientation [Letter to the Editor] Journal of Sex & Marital Therapy. 2013; 39 (1):1–6. doi: 10.1080/0092623X.2012.675022. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wright, C. 2022. Every tomboy is tagged 'transgender'. Wall Street Journal . https://www.wsj.com/articles/every-tomboy-is-tagged-transgender-transsexual-gender-dysphoria-children-hormones-clinic-terminology-expectations-11663872092?mod=opinion_lead_pos5 .
- Zeelenberg M, Pieters R. A theory of regret regulation 1.0. Journal of Consumer Psychology. 2007; 17 (1):3–18. doi: 10.1207/s15327663jcp1701_3. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zucker KJ. Children with gender identity disorder: Is there a best practice? Neuropsychiatrie de L'enfance et de L'adolescence. 2008; 56 (6):358–364. doi: 10.1016/j.neurenf.2008.06.003. [ CrossRef ] [ Google Scholar ]
- Zucker KJ. On the "natural history" of gender identity disorder in children [Editorial] Journal of the American Academy of Child & Adolescent Psychiatry. 2008; 47 (12):1361–1363. doi: 10.1097/CHI.0b013e31818960cf. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zucker KJ. Adolescents with gender dysphoria: Reflections on some contemporary clinical and research issues. Archives of Sexual Behavior. 2019; 48 (7):1983–1992. doi: 10.1007/s10508-019-01518-8. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zucker KJ. Debate: Different strokes for different folks. Child and Adolescent Mental Health. 2020; 25 (1):36–37. doi: 10.1111/camh.12330. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zucker KJ, Bradley SJ, Sanikhani M. Sex differences in referral rates of children with gender identity disorder: Some hypotheses. Journal of Abnormal Child Psychology. 1997; 25 (3):217–227. doi: 10.1023/a:1025748032640. [ PubMed ] [ CrossRef ] [ Google Scholar ]
Gender: The Process Of Transition Essay
Gender is the most important function in our society today. There are some many people out in the world that struggle finding their true identify. Transgender is a term for those who feel different because of their gender. Some people may define the word Transgender differently; some would like to be called Trans, or Transsexual. As a society we need to educate ourselves more on transgender people because it a process of change that impact them mentally, physical and socially.
The Process of Transition “The term transgender is often used as an all-purpose descriptor for a wide range of nonconventional gender identities that include individual’s identified as transsexual, female-to male trans men, male-to-female trans women, gender queer, nongendered, two-spirited, cross dressers, drag queens and drag kings (Robert)”. “A relatively simple definition provided by Brill and Pepper (2008), defines a Trans person as an ‘individual whose gender identity does not match their assigned birth gender.
For example, a transgender child self-identifies as a girl but is biologically male . The term can also be applied to individuals with a history of ‘transitioning sex’, even though they may not have openly identified themselves with any of the previously mentioned gender identities (Robert)”. The beginning process of being transgender is mentally, at a young age a child who is biologically born male of female identifies themselves as something else; even when they don’t understand what that maybe.
The word two- spirted, is how many Trans feel trapped in another person body, and then they beginning to emotional change the way they feel and think. “For example in many traditional American-Indian cultures, transgender individuals were once known as ‘two-spirit’ people who undertook distinctive forms of work and achieved unique status. In contrast, cross-dressing and transgender expression are disapproved of elsewhere by nearly all religious traditions (Robert)”. The life of a transgender mentally can be very dangerous.
Many Trans still develop emotions of not feeling normal or helplessness and feeling out of place. “For instance, acceptance and support, or rejection and marginalization, affect a person’s role in society and their personal relationships in particular. While trans people struggle internally with feelings of not belonging or not fitting into accepted cultural norms, these feelings are often exacerbated by external factors ranging from mild harassment and discrimination to the denial of basic rights and violence that in some cases can result in serious injury or even death (Robert)”. However, existing studies reveal links between minority stress, emotional distress and mental health problems in the general LGBT population (Health Service Executive, 2009; King et al. , 2008; Kuyper & Fokkema, 2009; Meyer, 1995). King et al. (2008) completed a met analysis of 25 studies that investigated mental disorder, suicide and self-harm in LGB people. Results indicated a twofold increase in suicide attempts and significantly higher rates of depression, anxiety disorders and alcohol dependence among LGB participants (Higgin Agnes)”.
When a transgender fully accept who there are they are mentally prepare for the physically part to transitioning. Coming out for Gays, Lesbians and Bisexuals as well as Trans genders is hard. “Hence, outwardly genderconforming transgender individual usually proceed through the development stages of coming out later in life, often following a long period of pre-coming when years of hiding their crossgender feelings take a different kind of toll (Etther)”. Gender reassignment is term that used for sex change for transgender. Gender reassignment (which includes psychotherapy, hormonal therapy and surgery) has been demonstrated as the most effective treatment for patients affected by gender dysphoria (or gender identity disorder), in which patients do not recognize their gender (sexual identity) as matching their genetic and sexual characteristics (Gennario Selvaggi)”.
Gender reassignment is a produce where the genitals or breast, or face gets removed or changed to fit the proper gender. Genital procedures performed for gender dysphoria, such as vaginoplasty, clitorolabioplasty, penectomy and orchidectomy in male-to-female transsexuals, and penile and scrotal reconstruction in female-to-male transsexuals, are the core procedures in gender reassignment surgery. Nongenital procedures, such as breast enlargement, mastectomy, facial feminization surgery, voice surgery, and other masculinization and feminization procedures complete the surgical treatment available (Gennario Selvaggi)”. Recently, the term Transgender has rebirth into society with the shocking revelation of Bruce Jenner coming out as being Transgender.
Bruce Jenner is an Olympic hero that won the gold medal for the decathlon 1976, the world saw him as male leader. In 2015 Bruce Jenner came out to world on national television and announced that he was living a life internal as a Trans women, Jenner shared that he would cross dress in hotel rooms, and in his home. Bruce Jenner who now is called Caitlyn Jenner changed the world and now we’ve become more aware of Transgender people. For Transgender changing their physically appearance is not the only struggle they face; socially they are not treated equally the same as other. The National Transgender Discrimination Survey found that 90% of respondents were harassed or mistreated at work for being transgender or hid who they were to avoid such treatment, and 26% had lost a job because they were transgender (Tuttle)”. Transgender people all around the world are being mistreated and harassed.
“However, transphobia– institutional, societal, and individual-level discrimination against transgender persons–is still pervasive in the United States and elsewhere. It often takes the form of laws, regulations, violence (physical, sexual, and verbal), harassment, prejudices, and egative attitudes directed against transgender persons (PHD and Brte)”. Unfortunately numerous people suffer from transphobia and or hostile towards Trans and make it hard for them at work, school anywhere social or in the media. “Studies have reported that transgender persons lack access to gendersensitive health care and often experience transphobia in health care and treatment. Transgender persons are frequently exposed to violence, sexual assault, and harassment in everyday life, mainly because of transphobia (PHD and Brte)”. The down fall from being socially harassed leads to depression.
Depression is one of the leading causes to several health risk of the LGBT community. “Psychological indicators such as depression and suicidal ideation and attempts have been reported among transgender persons (PHD and Brte)”. “A major mental health problem among both the transgender population and the non-transgender population is depression. It is important to stress, however, that depression is rarely caused simply by having a transgender identity (Bockting, Coleman, and Benner (2007), but more likely arises from external pressures such as isolation (Robert)”.
Over millions of young Trans teens are being killed and committing suicide. “Specific causes of depression among the transgender population include worries about disclosing their gender identity, family rejection, balancing transition costs, social isolation and an inability to settle down with an understanding partner (Robert)”. The everyday lives for Transgender is a struggle mentally, physically, and emotionally. Transiting to another gender has is scuffle, but I’m sure for the Trans it’s a process that there are willing to take.
More Essays
- The Argument About Gender-Neutral Dishroom Research Paper
- Gender Stereotypes Affecting People’s Identity Essay
- Gender Roles In Media Portrayal Of Gender Stereotypes Research Paper
- Sex: The Invisible Boundaries Of Gender Identity Essay
- Ezekiel: Mixed Gender Schools Essay
- Essay On Media And Gender Inequality
- Gender Roles In Moby Dick And The Yellow Wall-Paper
- Gender Construction Essay
- Media Influence On Society’s Perception Of Gender Essay
- Non-Acceptance In Schools Essay

IMAGES
VIDEO
COMMENTS
Overview We conducted a systematic literature review of all peer-reviewed articles published in English between 1991 and June 2017 that assess the effect of gender transition on transgender well-being. We identified 55 studies that consist of primary research on this topic, of which 51 (93%) found that gender transition improves the overall well-being of transgender […]
References to gender transitions relate to the process through which trans and nonbinary people express their gender as different from social expectations associated with the sex they were assigned at birth. This may include social, legal and medical transitions. ... In this essay, participants are identified as trans men, trans women, or ...
This essay approaches this by proposing that we counter unhelpful and harmful questions about gender transition by instead reframing these inquires as a question of how transitions become possible. Doing so allows us to set aside both if and why questions of transition. Focusing on how transitions unfold is a concern distinct from what Julia ...
That gender-affirming health care saves lives is clear: A 2018 literature review by Cornell University concluded that 93 percent of studies found that transition improved transgender people's ...
This was rooted in a twentieth-century theory called the "inversion hypothesis," which held that the desire to transition one's gender was the manifestation of intense same-sex attraction — basically, an extreme form of homosexuality. ... I published a series of papers documenting that transgender men who are attracted to men do exist ...
This type of advocacy, she argues, builds on two long-standing tendencies: the habit of thinking of gender transition as primarily a medical process, and the habit of grounding L.G.B.T. civil ...
People who transition early in life, for instance, might have different brain characteristics from those who transition later, owing to the way their brains are shaped by societal gender roles or ...
Jamie Lindemann Nelson, PhD is a professor of philosophy at Michigan State University in East Lansing, Michigan. She is also a fellow of the Hastings Center and co-editor of IJFAB: International Journal of Feminist Approaches to Bioethics.Her work on philosophical and bioethical issues sparked by gender and transgender has appeared in the Hastings Center Report, Journal of Bioethical Inquiry ...
1 INTRODUCTION. Transgender and nonbinary youths (TNBY) are youths who feel an incongruence between their gender identity and sex assigned at birth, sometimes experiencing distress known as gender dysphoria (American Psychiatric Association, 2022).Transitions, which can alleviate dysphoria, can be social (changes in presentation, such as in hair, name, or pronouns), legal (changes of name or ...
Also, it discusses in gender transition the relation between "the right to self-determination", "the right to delete", and "the right to identity and individuality". Conclusions on the ethical admissibility of the 'right to be forgotten' to control gender-affirming information are presented. Keywords: Ethics, 'Right to be ...
Statistics on gender transition medical care for children in the United States are not easy to find, but last year Reuters performed an analysis of insurance data to try to quantify the number of ...
Gender transition is the process of changing one's gender presentation or sex characteristics to accord with one's internal sense of gender identity - the idea of what it means to be a man or a woman, or to be non-binary, genderqueer, bigender, or pangender, or to be agender (genderless). For transgender and transsexual people, this process commonly involves reassignment therapy (which may ...
In their essay, 'Transition' (2018a), Emezi challenges Western notions of gender through an African lens and reclaims their indigenous beliefs from a decolonial perspective. In defining what it means to be transgender, Emezi posits the notion that they might be an ogbanje, a spirit child found in some African pre-colonial cultures that does ...
Interest in early-childhood gender nonconformity and later transgender identity has recently become especially pronounced (Dreger, 2009; Green, 2017), as some families are supporting their prepubescent children through social transitions (Edwards-Leeper, Leibowitz, & Sangganjanavanich, 2016; Sherer, 2016; Turban, 2017).Social transitions, as they apply to prepubescent gender-nonconforming ...
The research done to date on whether the majority of people who received gender-affirming medical care have any regrets is crystal clear — overwhelmingly good, positive news. In a meta study ...
Gender Identity Transition Essay. 449 Words 2 Pages. Topics concerning transgender can be very overwhelming for some. When one thinks of the term transgender, one may think of the process of an individual identifying as the opposite sex. The opposite sex of what he or she was born as. For some, this may involve undergoing surgical procedures or ...
By Akwaeke Emezi. "However, to be ogbanje is to be categorized other and to bring alterity home in a way that transcends the more ordinary bifurcated 'otherness' of gender. We could even speculate that ogbanje children fall under a third category of gender, of human-looking spirit. This gender is marked from birth—as male and female ...
These guidelines support Berkeley Lab's Nondiscrimination Policy, which includes gender identity and expression. This document is intended for use by supervisors and employees. If any assistance understanding something in this document is needed, contact the IDEA Office at [email protected]. As with all change, gender transition affects many ...
March 31, 2024, 4:00 AM PDT. By Jo Yurcaba. Transgender people overwhelmingly describe their lives after transitioning as "happier," "authentic" and "comforting" despite a deluge of ...
Second, opponents of gender-affirming care fixate heavily on the possibility of regret, despite regret rates being incredibly low. Most recently, the largest survey of trans adults in the US found that more than 97 percent of respondents were more satisfied with life after receiving gender-affirming hormone treatment or gender-affirming surgery.
One argument for preventing minors from gender transitioning is that they are too young to make that kind of permanent, life-changing decision, and they therefore must wait until they have reached ...
Gender transition is undertaken with the goal of improving the well-being of people suffering from gender dysphoria (Coleman et al., 2022). ... In this essay, I discuss emerging clinical and research issues related to transition regret and detransition. I begin by describing recent changes in the epidemiology of gender dysphoria ...
The Process of Transition "The term transgender is often used as an all-purpose descriptor for a wide range of nonconventional gender identities that include individual's identified as transsexual, female-to male trans men, male-to-female trans women, gender queer, nongendered, two-spirited, cross dressers, drag queens and drag kings (Robert)".
New York Magazine drops essay defending child gender transition days after leaked WPATH documents reveal doctors have concerns about risks of giving hormones to kids.