An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Can Med Educ J
- v.12(3); 2021 Jun


Writing, reading, and critiquing reviews
Écrire, lire et revue critique, douglas archibald.
1 University of Ottawa, Ontario, Canada;
Maria Athina Martimianakis
2 University of Toronto, Ontario, Canada
Why reviews matter
What do all authors of the CMEJ have in common? For that matter what do all health professions education scholars have in common? We all engage with literature. When you have an idea or question the first thing you do is find out what has been published on the topic of interest. Literature reviews are foundational to any study. They describe what is known about given topic and lead us to identify a knowledge gap to study. All reviews require authors to be able accurately summarize, synthesize, interpret and even critique the research literature. 1 , 2 In fact, for this editorial we have had to review the literature on reviews . Knowledge and evidence are expanding in our field of health professions education at an ever increasing rate and so to help keep pace, well written reviews are essential. Though reviews may be difficult to write, they will always be read. In this editorial we survey the various forms review articles can take. As well we want to provide authors and reviewers at CMEJ with some guidance and resources to be able write and/or review a review article.
What are the types of reviews conducted in Health Professions Education?
Health professions education attracts scholars from across disciplines and professions. For this reason, there are numerous ways to conduct reviews and it is important to familiarize oneself with these different forms to be able to effectively situate your work and write a compelling rationale for choosing your review methodology. 1 , 2 To do this, authors must contend with an ever-increasing lexicon of review type articles. In 2009 Grant and colleagues conducted a typology of reviews to aid readers makes sense of the different review types, listing fourteen different ways of conducting reviews, not all of which are mutually exclusive. 3 Interestingly, in their typology they did not include narrative reviews which are often used by authors in health professions education. In Table 1 , we offer a short description of three common types of review articles submitted to CMEJ.
Three common types of review articles submitted to CMEJ
More recently, authors such as Greenhalgh 4 have drawn attention to the perceived hierarchy of systematic reviews over scoping and narrative reviews. Like Greenhalgh, 4 we argue that systematic reviews are not to be seen as the gold standard of all reviews. Instead, it is important to align the method of review to what the authors hope to achieve, and pursue the review rigorously, according to the tenets of the chosen review type. Sometimes it is helpful to read part of the literature on your topic before deciding on a methodology for organizing and assessing its usefulness. Importantly, whether you are conducting a review or reading reviews, appreciating the differences between different types of reviews can also help you weigh the author’s interpretation of their findings.
In the next section we summarize some general tips for conducting successful reviews.
How to write and review a review article
In 2016 David Cook wrote an editorial for Medical Education on tips for a great review article. 13 These tips are excellent suggestions for all types of articles you are considering to submit to the CMEJ. First, start with a clear question: focused or more general depending on the type of review you are conducting. Systematic reviews tend to address very focused questions often summarizing the evidence of your topic. Other types of reviews tend to have broader questions and are more exploratory in nature.
Following your question, choose an approach and plan your methods to match your question…just like you would for a research study. Fortunately, there are guidelines for many types of reviews. As Cook points out the most important consideration is to be sure that the methods you follow lead to a defensible answer to your review question. To help you prepare for a defensible answer there are many guides available. For systematic reviews consult PRISMA guidelines ; 13 for scoping reviews PRISMA-ScR ; 14 and SANRA 15 for narrative reviews. It is also important to explain to readers why you have chosen to conduct a review. You may be introducing a new way for addressing an old problem, drawing links across literatures, filling in gaps in our knowledge about a phenomenon or educational practice. Cook refers to this as setting the stage. Linking back to the literature is important. In systematic reviews for example, you must be clear in explaining how your review builds on existing literature and previous reviews. This is your opportunity to be critical. What are the gaps and limitations of previous reviews? So, how will your systematic review resolve the shortcomings of previous work? In other types of reviews, such as narrative reviews, its less about filling a specific knowledge gap, and more about generating new research topic areas, exposing blind spots in our thinking, or making creative new links across issues. Whatever, type of review paper you are working on, the next steps are ones that can be applied to any scholarly writing. Be clear and offer insight. What is your main message? A review is more than just listing studies or referencing literature on your topic. Lead your readers to a convincing message. Provide commentary and interpretation for the studies in your review that will help you to inform your conclusions. For systematic reviews, Cook’s final tip is most likely the most important– report completely. You need to explain all your methods and report enough detail that readers can verify the main findings of each study you review. The most common reasons CMEJ reviewers recommend to decline a review article is because authors do not follow these last tips. In these instances authors do not provide the readers with enough detail to substantiate their interpretations or the message is not clear. Our recommendation for writing a great review is to ensure you have followed the previous tips and to have colleagues read over your paper to ensure you have provided a clear, detailed description and interpretation.
Finally, we leave you with some resources to guide your review writing. 3 , 7 , 8 , 10 , 11 , 16 , 17 We look forward to seeing your future work. One thing is certain, a better appreciation of what different reviews provide to the field will contribute to more purposeful exploration of the literature and better manuscript writing in general.
In this issue we present many interesting and worthwhile papers, two of which are, in fact, reviews.
Major Contributions
A chance for reform: the environmental impact of travel for general surgery residency interviews by Fung et al. 18 estimated the CO 2 emissions associated with traveling for residency position interviews. Due to the high emissions levels (mean 1.82 tonnes per applicant), they called for the consideration of alternative options such as videoconference interviews.
Understanding community family medicine preceptors’ involvement in educational scholarship: perceptions, influencing factors and promising areas for action by Ward and team 19 identified barriers, enablers, and opportunities to grow educational scholarship at community-based teaching sites. They discovered a growing interest in educational scholarship among community-based family medicine preceptors and hope the identification of successful processes will be beneficial for other community-based Family Medicine preceptors.
Exploring the global impact of the COVID-19 pandemic on medical education: an international cross-sectional study of medical learners by Allison Brown and team 20 studied the impact of COVID-19 on medical learners around the world. There were different concerns depending on the levels of training, such as residents’ concerns with career timeline compared to trainees’ concerns with the quality of learning. Overall, the learners negatively perceived the disruption at all levels and geographic regions.
The impact of local health professions education grants: is it worth the investment? by Susan Humphrey-Murto and co-authors 21 considered factors that lead to the publication of studies supported by local medical education grants. They identified several factors associated with publication success, including previous oral or poster presentations. They hope their results will be valuable for Canadian centres with local grant programs.
Exploring the impact of the COVID-19 pandemic on medical learner wellness: a needs assessment for the development of learner wellness interventions by Stephana Cherak and team 22 studied learner-wellness in various training environments disrupted by the pandemic. They reported a negative impact on learner wellness at all stages of training. Their results can benefit the development of future wellness interventions.
Program directors’ reflections on national policy change in medical education: insights on decision-making, accreditation, and the CanMEDS framework by Dore, Bogie, et al. 23 invited program directors to reflect on the introduction of the CanMEDS framework into Canadian postgraduate medical education programs. Their survey revealed that while program directors (PDs) recognized the necessity of the accreditation process, they did not feel they had a voice when the change occurred. The authors concluded that collaborations with PDs would lead to more successful outcomes.
Experiential learning, collaboration and reflection: key ingredients in longitudinal faculty development by Laura Farrell and team 24 stressed several elements for effective longitudinal faculty development (LFD) initiatives. They found that participants benefited from a supportive and collaborative environment while trying to learn a new skill or concept.
Brief Reports
The effect of COVID-19 on medical students’ education and wellbeing: a cross-sectional survey by Stephanie Thibaudeau and team 25 assessed the impact of COVID-19 on medical students. They reported an overall perceived negative impact, including increased depressive symptoms, increased anxiety, and reduced quality of education.
In Do PGY-1 residents in Emergency Medicine have enough experiences in resuscitations and other clinical procedures to meet the requirements of a Competence by Design curriculum? Meshkat and co-authors 26 recorded the number of adult medical resuscitations and clinical procedures completed by PGY1 Fellow of the Royal College of Physicians in Emergency Medicine residents to compare them to the Competence by Design requirements. Their study underscored the importance of monitoring collection against pre-set targets. They concluded that residency program curricula should be regularly reviewed to allow for adequate clinical experiences.
Rehearsal simulation for antenatal consults by Anita Cheng and team 27 studied whether rehearsal simulation for antenatal consults helped residents prepare for difficult conversations with parents expecting complications with their baby before birth. They found that while rehearsal simulation improved residents’ confidence and communication techniques, it did not prepare them for unexpected parent responses.
Review Papers and Meta-Analyses
Peer support programs in the fields of medicine and nursing: a systematic search and narrative review by Haykal and co-authors 28 described and evaluated peer support programs in the medical field published in the literature. They found numerous diverse programs and concluded that including a variety of delivery methods to meet the needs of all participants is a key aspect for future peer-support initiatives.
Towards competency-based medical education in addictions psychiatry: a systematic review by Bahji et al. 6 identified addiction interventions to build competency for psychiatry residents and fellows. They found that current psychiatry entrustable professional activities need to be better identified and evaluated to ensure sustained competence in addictions.
Six ways to get a grip on leveraging the expertise of Instructional Design and Technology professionals by Chen and Kleinheksel 29 provided ways to improve technology implementation by clarifying the role that Instructional Design and Technology professionals can play in technology initiatives and technology-enhanced learning. They concluded that a strong collaboration is to the benefit of both the learners and their future patients.
In his article, Seven ways to get a grip on running a successful promotions process, 30 Simon Field provided guidelines for maximizing opportunities for successful promotion experiences. His seven tips included creating a rubric for both self-assessment of likeliness of success and adjudication by the committee.
Six ways to get a grip on your first health education leadership role by Stasiuk and Scott 31 provided tips for considering a health education leadership position. They advised readers to be intentional and methodical in accepting or rejecting positions.
Re-examining the value proposition for Competency-Based Medical Education by Dagnone and team 32 described the excitement and controversy surrounding the implementation of competency-based medical education (CBME) by Canadian postgraduate training programs. They proposed observing which elements of CBME had a positive impact on various outcomes.
You Should Try This
In their work, Interprofessional culinary education workshops at the University of Saskatchewan, Lieffers et al. 33 described the implementation of interprofessional culinary education workshops that were designed to provide health professions students with an experiential and cooperative learning experience while learning about important topics in nutrition. They reported an enthusiastic response and cooperation among students from different health professional programs.
In their article, Physiotherapist-led musculoskeletal education: an innovative approach to teach medical students musculoskeletal assessment techniques, Boulila and team 34 described the implementation of physiotherapist-led workshops, whether the workshops increased medical students’ musculoskeletal knowledge, and if they increased confidence in assessment techniques.
Instagram as a virtual art display for medical students by Karly Pippitt and team 35 used social media as a platform for showcasing artwork done by first-year medical students. They described this shift to online learning due to COVID-19. Using Instagram was cost-saving and widely accessible. They intend to continue with both online and in-person displays in the future.
Adapting clinical skills volunteer patient recruitment and retention during COVID-19 by Nazerali-Maitland et al. 36 proposed a SLIM-COVID framework as a solution to the problem of dwindling volunteer patients due to COVID-19. Their framework is intended to provide actionable solutions to recruit and engage volunteers in a challenging environment.
In Quick Response codes for virtual learner evaluation of teaching and attendance monitoring, Roxana Mo and co-authors 37 used Quick Response (QR) codes to monitor attendance and obtain evaluations for virtual teaching sessions. They found QR codes valuable for quick and simple feedback that could be used for many educational applications.
In Creation and implementation of the Ottawa Handbook of Emergency Medicine Kaitlin Endres and team 38 described the creation of a handbook they made as an academic resource for medical students as they shift to clerkship. It includes relevant content encountered in Emergency Medicine. While they intended it for medical students, they also see its value for nurses, paramedics, and other medical professionals.
Commentary and Opinions
The alarming situation of medical student mental health by D’Eon and team 39 appealed to medical education leaders to respond to the high numbers of mental health concerns among medical students. They urged leaders to address the underlying problems, such as the excessive demands of the curriculum.
In the shadows: medical student clinical observerships and career exploration in the face of COVID-19 by Law and co-authors 40 offered potential solutions to replace in-person shadowing that has been disrupted due to the COVID-19 pandemic. They hope the alternatives such as virtual shadowing will close the gap in learning caused by the pandemic.
Letters to the Editor
Canadian Federation of Medical Students' response to “ The alarming situation of medical student mental health” King et al. 41 on behalf of the Canadian Federation of Medical Students (CFMS) responded to the commentary by D’Eon and team 39 on medical students' mental health. King called upon the medical education community to join the CFMS in its commitment to improving medical student wellbeing.
Re: “Development of a medical education podcast in obstetrics and gynecology” 42 was written by Kirubarajan in response to the article by Development of a medical education podcast in obstetrics and gynecology by Black and team. 43 Kirubarajan applauded the development of the podcast to meet a need in medical education, and suggested potential future topics such as interventions to prevent learner burnout.
Response to “First year medical student experiences with a clinical skills seminar emphasizing sexual and gender minority population complexity” by Kumar and Hassan 44 acknowledged the previously published article by Biro et al. 45 that explored limitations in medical training for the LGBTQ2S community. However, Kumar and Hassen advocated for further progress and reform for medical training to address the health requirements for sexual and gender minorities.
In her letter, Journey to the unknown: road closed!, 46 Rosemary Pawliuk responded to the article, Journey into the unknown: considering the international medical graduate perspective on the road to Canadian residency during the COVID-19 pandemic, by Gutman et al. 47 Pawliuk agreed that international medical students (IMGs) do not have adequate formal representation when it comes to residency training decisions. Therefore, Pawliuk challenged health organizations to make changes to give a voice in decision-making to the organizations representing IMGs.
In Connections, 48 Sara Guzman created a digital painting to portray her approach to learning. Her image of a hand touching a neuron showed her desire to physically see and touch an active neuron in order to further understand the brain and its connections.

JAY SIWEK, M.D., MARGARET L. GOURLAY, M.D., DAVID C. SLAWSON, M.D., AND ALLEN F. SHAUGHNESSY, PHARM.D.
Am Fam Physician. 2002;65(2):251-258
Traditional clinical review articles, also known as updates, differ from systematic reviews and meta-analyses. Updates selectively review the medical literature while discussing a topic broadly. Nonquantitative systematic reviews comprehensively examine the medical literature, seeking to identify and synthesize all relevant information to formulate the best approach to diagnosis or treatment. Meta-analyses (quantitative systematic reviews) seek to answer a focused clinical question, using rigorous statistical analysis of pooled research studies. This article presents guidelines for writing an evidence-based clinical review article for American Family Physician . First, the topic should be of common interest and relevance to family practice. Include a table of the continuing medical education objectives of the review. State how the literature search was done and include several sources of evidence-based reviews, such as the Cochrane Collaboration, BMJ's Clinical Evidence , or the InfoRetriever Web site. Where possible, use evidence based on clinical outcomes relating to morbidity, mortality, or quality of life, and studies of primary care populations. In articles submitted to American Family Physician , rate the level of evidence for key recommendations according to the following scale: level A (randomized controlled trial [RCT], meta-analysis); level B (other evidence); level C (consensus/expert opinion). Finally, provide a table of key summary points.
American Family Physician is particularly interested in receiving clinical review articles that follow an evidence-based format. Clinical review articles, also known as updates, differ from systematic reviews and meta-analyses in important ways. 1 Updates selectively review the medical literature while discussing a topic broadly. An example of such a topic is, “The diagnosis and treatment of myocardial ischemia.” Systematic reviews comprehensively examine the medical literature, seeking to identify and synthesize all relevant information to formulate the best approach to diagnosis or treatment. Examples are many of the systematic reviews of the Cochrane Collaboration or BMJ's Clinical Evidence compendium. Meta-analyses are a special type of systematic review. They use quantitative methods to analyze the literature and seek to answer a focused clinical question, using rigorous statistical analysis of pooled research studies. An example is, “Do beta blockers reduce mortality following myocardial infarction?”
The best clinical review articles base the discussion on existing systematic reviews and meta-analyses, and incorporate all relevant research findings about the management of a given disorder. Such evidence-based updates provide readers with powerful summaries and sound clinical guidance.
In this article, we present guidelines for writing an evidence-based clinical review article, especially one designed for continuing medical education (CME) and incorporating CME objectives into its format. This article may be read as a companion piece to a previous article and accompanying editorial about reading and evaluating clinical review articles. 1 , 2 Some articles may not be appropriate for an evidence-based format because of the nature of the topic, the slant of the article, a lack of sufficient supporting evidence, or other factors. We encourage authors to review the literature and, wherever possible, rate key points of evidence. This process will help emphasize the summary points of the article and strengthen its teaching value.
Topic Selection
Choose a common clinical problem and avoid topics that are rarities or unusual manifestations of disease or that have curiosity value only. Whenever possible, choose common problems for which there is new information about diagnosis or treatment. Emphasize new information that, if valid, should prompt a change in clinical practice, such as the recent evidence that spironolactone therapy improves survival in patients who have severe congestive heart failure. 3 Similarly, new evidence showing that a standard treatment is no longer helpful, but may be harmful, would also be important to report. For example, patching most traumatic corneal abrasions may actually cause more symptoms and delay healing compared with no patching. 4
Searching the Literature
When searching the literature on your topic, please consult several sources of evidence-based reviews ( Table 1 ) . Look for pertinent guidelines on the diagnosis, treatment, or prevention of the disorder being discussed. Incorporate all high-quality recommendations that are relevant to the topic. When reviewing the first draft, look for all key recommendations about diagnosis and, especially, treatment. Try to ensure that all recommendations are based on the highest level of evidence available. If you are not sure about the source or strength of the recommendation, return to the literature, seeking out the basis for the recommendation.
In particular, try to find the answer in an authoritative compendium of evidence-based reviews, or at least try to find a meta-analysis or well-designed randomized controlled trial (RCT) to support it. If none appears to be available, try to cite an authoritative consensus statement or clinical guideline, such as a National Institutes of Health Consensus Development Conference statement or a clinical guideline published by a major medical organization. If no strong evidence exists to support the conventional approach to managing a given clinical situation, point this out in the text, especially for key recommendations. Keep in mind that much of traditional medical practice has not yet undergone rigorous scientific study, and high-quality evidence may not exist to support conventional knowledge or practice.
Patient-Oriented vs. Disease-Oriented Evidence
With regard to types of evidence, Shaughnessy and Slawson 5 – 7 developed the concept of Patient-Oriented Evidence that Matters (POEM), in distinction to Disease-Oriented Evidence (DOE). POEM deals with outcomes of importance to patients, such as changes in morbidity, mortality, or quality of life. DOE deals with surrogate end points, such as changes in laboratory values or other measures of response. Although the results of DOE sometimes parallel the results of POEM, they do not always correspond ( Table 2 ) . 2 When possible, use POEM-type evidence rather than DOE. When DOE is the only guidance available, indicate that key clinical recommendations lack the support of outcomes evidence. Here is an example of how the latter situation might appear in the text: “Although prostate-specific antigen (PSA) testing identifies prostate cancer at an early stage, it has not yet been proved that PSA screening improves patient survival.” (Note: PSA testing is an example of DOE, a surrogate marker for the true outcomes of importance—improved survival, decreased morbidity, and improved quality of life.)
Evaluating the Literature
Evaluate the strength and validity of the literature that supports the discussion (see the following section, Levels of Evidence). Look for meta-analyses, high-quality, randomized clinical trials with important outcomes (POEM), or well-designed, nonrandomized clinical trials, clinical cohort studies, or case-controlled studies with consistent findings. In some cases, high-quality, historical, uncontrolled studies are appropriate (e.g., the evidence supporting the efficacy of Papanicolaou smear screening). Avoid anecdotal reports or repeating the hearsay of conventional wisdom, which may not stand up to the scrutiny of scientific study (e.g., prescribing prolonged bed rest for low back pain).
Look for studies that describe patient populations that are likely to be seen in primary care rather than subspecialty referral populations. Shaughnessy and Slawson's guide for writers of clinical review articles includes a section on information and validity traps to avoid. 2
Levels of Evidence
Readers need to know the strength of the evidence supporting the key clinical recommendations on diagnosis and treatment. Many different rating systems of varying complexity and clinical relevance are described in the medical literature. Recently, the third U.S. Preventive Services Task Force (USPSTF) emphasized the importance of rating not only the study type (RCT, cohort study, case-control study, etc.), but also the study quality as measured by internal validity and the quality of the entire body of evidence on a topic. 8
While it is important to appreciate these evolving concepts, we find that a simplified grading system is more useful in AFP . We have adopted the following convention, using an ABC rating scale. Criteria for high-quality studies are discussed in several sources. 8 , 9 See the AFP Web site ( www.aafp.org/afp/authors ) for additional information about levels of evidence and see the accompanying editorial in this issue discussing the potential pitfalls and limitations of any rating system.
Level A (randomized controlled trial/meta-analysis): High-quality randomized controlled trial (RCT) that considers all important outcomes. High-quality meta-analysis (quantitative systematic review) using comprehensive search strategies.
Level B (other evidence): A well-designed, nonrandomized clinical trial. A nonquantitative systematic review with appropriate search strategies and well-substantiated conclusions. Includes lower quality RCTs, clinical cohort studies, and case-controlled studies with non-biased selection of study participants and consistent findings. Other evidence, such as high-quality, historical, uncontrolled studies, or well-designed epidemiologic studies with compelling findings, is also included.
Level C (consensus/expert opinion): Consensus viewpoint or expert opinion.
Each rating is applied to a single reference in the article, not to the entire body of evidence that exists on a topic. Each label should include the letter rating (A, B, C), followed by the specific type of study for that reference. For example, following a level B rating, include one of these descriptors: (1) nonrandomized clinical trial; (2) nonquantitative systematic review; (3) lower quality RCT; (4) clinical cohort study; (5) case-controlled study; (6) historical uncontrolled study; (7) epidemiologic study.
Here are some examples of the way evidence ratings should appear in the text:
“To improve morbidity and mortality, most patients in congestive heart failure should be treated with an angiotensin-converting enzyme inhibitor. [Evidence level A, RCT]”
“The USPSTF recommends that clinicians routinely screen asymptomatic pregnant women 25 years and younger for chlamydial infection. [Evidence level B, non-randomized clinical trial]”
“The American Diabetes Association recommends screening for diabetes every three years in all patients at high risk of the disease, including all adults 45 years and older. [Evidence level C, expert opinion]”
When scientifically strong evidence does not exist to support a given clinical recommendation, you can point this out in the following way:
“Physical therapy is traditionally prescribed for the treatment of adhesive capsulitis (frozen shoulder), although there are no randomized outcomes studies of this approach.”
Format of the Review
Introduction.
The introduction should define the topic and purpose of the review and describe its relevance to family practice. The traditional way of doing this is to discuss the epidemiology of the condition, stating how many people have it at one point in time (prevalence) or what percentage of the population is expected to develop it over a given period of time (incidence). A more engaging way of doing this is to indicate how often a typical family physician is likely to encounter this problem during a week, month, year, or career. Emphasize the key CME objectives of the review and summarize them in a separate table entitled “CME Objectives.”
The methods section should briefly indicate how the literature search was conducted and what major sources of evidence were used. Ideally, indicate what predetermined criteria were used to include or exclude studies (e.g., studies had to be independently rated as being high quality by an established evaluation process, such as the Cochrane Collaboration). Be comprehensive in trying to identify all major relevant research. Critically evaluate the quality of research reviewed. Avoid selective referencing of only information that supports your conclusions. If there is controversy on a topic, address the full scope of the controversy.
The discussion can then follow the typical format of a clinical review article. It should touch on one or more of the following subtopics: etiology, pathophysiology, clinical presentation (signs and symptoms), diagnostic evaluation (history, physical examination, laboratory evaluation, and diagnostic imaging), differential diagnosis, treatment (goals, medical/surgical therapy, laboratory testing, patient education, and follow-up), prognosis, prevention, and future directions.
The review will be comprehensive and balanced if it acknowledges controversies, unresolved questions, recent developments, other viewpoints, and any apparent conflicts of interest or instances of bias that might affect the strength of the evidence presented. Emphasize an evidence-supported approach or, where little evidence exists, a consensus viewpoint. In the absence of a consensus viewpoint, you may describe generally accepted practices or discuss one or more reasoned approaches, but acknowledge that solid support for these recommendations is lacking.
In some cases, cost-effectiveness analyses may be important in deciding how to implement health care services, especially preventive services. 10 When relevant, mention high-quality cost-effectiveness analyses to help clarify the costs and health benefits associated with alternative interventions to achieve a given health outcome. Highlight key points about diagnosis and treatment in the discussion and include a summary table of the key take-home points. These points are not necessarily the same as the key recommendations, whose level of evidence is rated, although some of them will be.
Use tables, figures, and illustrations to highlight key points, and present a step-wise, algorithmic approach to diagnosis or treatment when possible.
Rate the evidence for key statements, especially treatment recommendations. We expect that most articles will have at most two to four key statements; some will have none. Rate only those statements that have corresponding references and base the rating on the quality and level of evidence presented in the supporting citations. Use primary sources (original research, RCTs, meta-analyses, and systematic reviews) as the basis for determining the level of evidence. In other words, the supporting citation should be a primary research source of the information, not a secondary source (such as a nonsystematic review article or a textbook) that simply cites the original source. Systematic reviews that analyze multiple RCTs are good sources for determining ratings of evidence.
The references should include the most current and important sources of support for key statements (i.e., studies referred to, new information, controversial material, specific quantitative data, and information that would not usually be found in most general reference textbooks). Generally, these references will be key evidence-based recommendations, meta-analyses, or landmark articles. Although some journals publish exhaustive lists of reference citations, AFP prefers to include a succinct list of key references. (We will make more extensive reference lists available on our Web site or provide links to your personal reference list.)
You may use the following checklist to ensure the completeness of your evidence-based review article; use the source list of reviews to identify important sources of evidence-based medicine materials.
Checklist for an Evidence-Based Clinical Review Article
The topic is common in family practice, especially topics in which there is new, important information about diagnosis or treatment.
The introduction defines the topic and the purpose of the review, and describes its relevance to family practice.
A table of CME objectives for the review is included.
The review states how you did your literature search and indicates what sources you checked to ensure a comprehensive assessment of relevant studies (e.g., MEDLINE, the Cochrane Collaboration Database, the Center for Research Support, TRIP Database).
Several sources of evidence-based reviews on the topic are evaluated ( Table 1 ) .
Where possible, POEM (dealing with changes in morbidity, mortality, or quality of life) rather than DOE (dealing with mechanistic explanations or surrogate end points, such as changes in laboratory tests) is used to support key clinical recommendations ( Table 2 ) .
Studies of patients likely to be representative of those in primary care practices, rather than subspecialty referral centers, are emphasized.
Studies that are not only statistically significant but also clinically significant are emphasized; e.g., interventions with meaningful changes in absolute risk reduction and low numbers needed to treat. (See http://www.cebm.net/index.aspx?o=1116 .) 11
The level of evidence for key clinical recommendations is labeled using the following rating scale: level A (RCT/meta-analysis), level B (other evidence), and level C (consensus/expert opinion).
Acknowledge controversies, recent developments, other viewpoints, and any apparent conflicts of interest or instances of bias that might affect the strength of the evidence presented.
Highlight key points about diagnosis and treatment in the discussion and include a summary table of key take-home points.
Use tables, figures, and illustrations to highlight key points and present a step-wise, algorithmic approach to diagnosis or treatment when possible.
Emphasize evidence-based guidelines and primary research studies, rather than other review articles, unless they are systematic reviews.
The essential elements of this checklist are summarized in Table 3 .
Siwek J. Reading and evaluating clinical review articles. Am Fam Physician. 1997;55:2064-2069.
Shaughnessy AF, Slawson DC. Getting the most from review articles: a guide for readers and writers. Am Fam Physician. 1997;55:2155-60.
Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med. 1999;341:709-17.
Flynn CA, D'Amico F, Smith G. Should we patch corneal abrasions? A meta-analysis. J Fam Pract. 1998;47:264-70.
Slawson DC, Shaughnessy AF, Bennett JH. Becoming a medical information master: feeling good about not knowing everything. J Fam Pract. 1994;38:505-13.
Shaughnessy AF, Slawson DC, Bennett JH. Becoming an information master: a guidebook to the medical information jungle. J Fam Pract. 1994;39:489-99.
Slawson DC, Shaughnessy AF. Becoming an information master: using POEMs to change practice with confidence. Patient-oriented evidence that matters. J Fam Pract. 2000;49:63-7.
Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, et al. Methods Work Group, Third U.S. Preventive Services Task Force. Current methods of the U.S. Preventive Services Task Force. A review of the process. Am J Prev Med. 2001;20(3 suppl):21-35.
CATbank topics: levels of evidence and grades of recommendations. Retrieved November 2001, from: http://www.cebm.net/ .
Saha S, Hoerger TJ, Pignone MP, Teutsch SM, Helfand M, Mandelblatt JS. for the Cost Work Group of the Third U.S. Preventive Services Task Force. The art and science of incorporating cost effectiveness into evidence-based recommendations for clinical preventive services. Am J Prev Med. 2001;20(3 suppl):36-43.
Evidence-based medicine glossary. Retrieved November 2001, from: http://www.cebm.net/index.aspx?o=1116 .
Continue Reading
More in afp, more in pubmed.
Copyright © 2002 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
- Search Menu
- Advance Articles
- Editor's Choice
- CME Reviews
- Best of 2021 collection
- Abbreviated Breast MRI Virtual Collection
- Contrast-enhanced Mammography Collection
- Author Guidelines
- Submission Site
- Open Access
- Self-Archiving Policy
- Accepted Papers Resource Guide
- About Journal of Breast Imaging
- About the Society of Breast Imaging
- Guidelines for Reviewers
- Resources for Reviewers and Authors
- Editorial Board
- Advertising Disclaimer
- Advertising and Corporate Services
- Journals on Oxford Academic
- Books on Oxford Academic

- < Previous
A Step-by-Step Guide to Writing a Scientific Review Article
- Article contents
- Figures & tables
- Supplementary Data
Manisha Bahl, A Step-by-Step Guide to Writing a Scientific Review Article, Journal of Breast Imaging , Volume 5, Issue 4, July/August 2023, Pages 480–485, https://doi.org/10.1093/jbi/wbad028
- Permissions Icon Permissions
Scientific review articles are comprehensive, focused reviews of the scientific literature written by subject matter experts. The task of writing a scientific review article can seem overwhelming; however, it can be managed by using an organized approach and devoting sufficient time to the process. The process involves selecting a topic about which the authors are knowledgeable and enthusiastic, conducting a literature search and critical analysis of the literature, and writing the article, which is composed of an abstract, introduction, body, and conclusion, with accompanying tables and figures. This article, which focuses on the narrative or traditional literature review, is intended to serve as a guide with practical steps for new writers. Tips for success are also discussed, including selecting a focused topic, maintaining objectivity and balance while writing, avoiding tedious data presentation in a laundry list format, moving from descriptions of the literature to critical analysis, avoiding simplistic conclusions, and budgeting time for the overall process.
- narrative discourse
Email alerts
Citing articles via.
- Recommend to your Librarian
- Journals Career Network
Affiliations
- Online ISSN 2631-6129
- Print ISSN 2631-6110
- Copyright © 2024 Society of Breast Imaging
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
How to Write a Review Article
Cite this chapter.
3291 Accesses
- Eating Disorder
- Journal Editor
- Preventive Service Task
- Borderline Personality Disorder
- Medical Writing
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Unable to display preview. Download preview PDF.
Day RA. How to publish a scientific paper. 5th ed. Westport, CT: Oryx; 1998:163.
Google Scholar
Siwek J, Gourlay ML, Slawson DC, Shaughnessy AF. How to write an evidence-based clinical review article. Am Fam Phys 2002;65:251–258.
Journal of the American Medical Association. Instructions for authors. JAMA 2004;291:125–131. Available at: http://jama. ama-assn.org/ifora_current/dtl.
Harris RP, Helfand M, Wolff SH, et al. Methods Work Group, Third U.S. Preventive Services Task Force. Current methods of the U.S. Preventive Services Task Force. A review of the process. Am J Prev Med 2001;20(3 suppl):21–35.
CAS PubMed Google Scholar
Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. Am Fam Phys 2004;69:548–556.
Download references
Rights and permissions
Reprints and permissions
Copyright information
© 2005 Springer Science+Business Media, Inc.
About this chapter
(2005). How to Write a Review Article. In: The Clinician’s Guide to Medical Writing. Springer, New York, NY. https://doi.org/10.1007/0-387-27024-8_6
Download citation
DOI : https://doi.org/10.1007/0-387-27024-8_6
Publisher Name : Springer, New York, NY
Print ISBN : 978-0-387-22249-3
Online ISBN : 978-0-387-27024-1
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

Structure for writing an effective clinical review articles
Pre-or post-publication Peer review of Scientific Manuscripts: Thoughts on Pros and Cons
Guidelines to authors in Writing an effective Medical Case Report (MCR)
Clinicians need clinical review articles that have well-organized structure for easy reading and understanding. Only then it will help them to apply it practically on patients and for further research. Traditional clinical review articles, also known as updates, discuss a topic broadly and selectively review the medical literature. An excellent structured clinical research article will resolve controversy generated by studies that contradict one another.
Before knowing how to structure a clinical review article, you have to know some background facts on why good structure is crucial for it.
For clinicians to upgrade their knowledge, they rely only on peer-reviewed medical journals. But most studies at best only provide preliminary evidence due to
- Limited scope
- Poor design
- Inefficient execution
- Inadequate sample size to have significant clinical benefits or detection of adverse effects
- Play of chances
Clinicians reading these studies, have to integrate and compare it with existing evidence to conclude, whether the clinical policy had to be changed on the accumulated evidence. Even in the case of original studies, only a portion of the clinical problem is addressed. Hence, most clinicians take a short cut to read the clinical reviews done by others. These clinic review articles include evidence from available studies on the specific clinical problem.
But the clinical review if not structured properly, will not do justice to the original evidence. And the clinician will end up with false conclusions which will finally be borne by the patients. In research by Mulrow conducted on 50 published reviews, only one adhered to the specific methods of identifying, selecting, and validating included information.
Notes: – The word count in the Article structure excludes the Abstract, References, Acknowledgement and figure captions. The word count should be indicated at the foot of the title page. – Keywords (3-6) should be provided at the foot of the abstract.
Now let us see how a clinical research article can be structured:
PRISMA or Preferred Reporting Items for Systematic Reviews and Meta-analyses has issued a statement listing 27 item checklists to make the writing of clinic review feasible.
Though IMRAD (Introduction, Methods, Results, Discussion and Conclusions) structure is the basis of many reviews, there could be variations in guidelines as per the nature of research. But the general structure for most of the clinic review structure is as follows
Elements of a review article
1. title page :.
- Length: The title should be in a range of 8 -12 words describing the topic and its aspect.
E.g. The title “Pancreatic Disease” will be too generic. Instead, “Challenges in Diagnosing Subclinical Pancreatic Disease” will describe the concise nature and aspect of the research.
- The title must be short
- The title should have all the critical elements of the subject matter (or informative)
- Order of authors: The first author has done most of the research
- Second and in between authors would have contributed one way or another
- The last author coordinated the project
- Tense: Results: the present tense stresses the general validity and demonstrates that the author is trying to achieve with the article. The paste tense indicates that results are not established yet.
- Citations: None
2. Abstract:
- Citation: No citations needed in the abstract
- Elements: Descriptive Abstract for narrative reviews
- Objectives: Present
- Materials and Methods, results: Past
- Conclusion: Present
- Should include acronyms and abbreviations only if they are used more than once
- Length: It should be written within a range of 200 – 500 words outlining the main points or synthesis in subheadings as per the nature of the review
E.g., Abstract requirements for content and format differ according to the type of review or journal. Some prefer unstructured abstracts, and the others require structured abstracts containing the elements in subheadings.
- Another style needs the subheadings content, evidence, acquisition, results, and conclusions
3. Introduction:
- Tense: Should be written in present tense addressing the research question and the objective purpose of the review
- Citations: Many
- Length: 10% and 20% of the core text
- Note: It should explain why the review of the field or topic essential at this time and what is that you are going to cover in the review
E.g., Review on DMS or deep brain stimulation for Dystonia
However, one must acknowledge that published results obtained with DBS in Dystonia are few and that conclusions from these preliminary reports should be drawn very cautiously. Nonetheless, promising findings are emerging from single case reports or small case series, and the notion that DBS may be of great help in selected cases is progressively growing… . In this review, we discuss the results reported in the literature. Some critical issues regarding the evaluation of the results are also mentioned
4. Materials and Methods
Tense: Should be written in the past tense to provide the reason to repeat the review
Elements: It should include:
- Search strategies
- Criteria of inclusion and exclusion of methods
- Data sources
- Geographical information
- Characteristics of study subjects
- Details of used statistical analyses
Length: Approx. 5% of the core text
Citations: Few (e.g. software and statistical analyses used)
5. Main Body Part of the Review Article
Section Structure: A coherent structure of the topic mentioning their relevance to the objective. Subheadings reflecting the topic organisation and indicate the content in various sections including methodological approaches adopted, theories or models used, critical appraisal of studies, in chronological order
Links: Links the research findings to the research questions
Tense: Three tenses are frequently used: Present tense, when reporting what another author thinks, and writes. Example: It is believed….
Present Perfect, when referring to an area of research with a number of researchers Example: They have found….
while simple past referring to what a specific researcher found, referring to a single study. Example: They found….
Citations: Usually indirect but can also be cited directly
Length: 70 to 90% of the core text
6. Discussion:
Elements: Discuss the results and their significance clearly and concisely. Identify any unresolved questions.
Function: Reiterate the objective and background information
Citations: Few or more
Tense: Present tense
Despite 30 years of continued investigation, the precise mechanism of CD4 T-cell loss induced by HIV infection remains controversial. HIV-mediated destruction of its preferred target, the activated CD4 T cell, is certainly central to HIV pathogenesis, but does not explain why many uninfected cells die or why the host cannot merely replace lost cells.21,22 As first proposed in the 1990s,23 researchers now know that the pro-inflammatory nature of HIV infection is a key part of disease pathogenesis.2,25
7. Conclusions:
- Conclude the review to give the reader a sense of what the review means by discussing the objective mentioned in introduction, including findings and interpretations.
- I should also discuss what the future is by identifying the unresolved questions
Future studies evaluating novel stroke biomarkers should answer questions that address their unique clinical contribution in the diagnosis, management, and risk prediction of stroke: has the patient had a stroke? Is the stroke of ischemic or hemorrhagic etiology? Are symptoms suggestive of additional intensive investigation or thrombolytic therapy? Is the patient at risk for stroke or reoccurrence of cardiovascular events? Modern stroke diagnosis remains heavily reliant on clinical interpretation, and further translational research efforts toward discovery of stroke biomarkers have the possibility to greatly improve patient outcomes and quality of care
8. References:
Length: References should be written in 50 to 100 words and could cite only those in text, and online sources are not allowed.
Plagiarism: Strictly Avoid
The above details will help you to structure your clinical review article and if you need any further assistance seek professional help.
clinical review articles | medical literature | clinical case | Schemantic reviews | Meta analysis | writing of clinical review | clinical review structure
pubrica-academy
Related posts.

Making Sense of Effect Size in Meta-Analysis based for Medical Research

Copy of PUB-Evidence-based analyses to look at cost-effectiveness, cost-benefit information & clinical data from RT-Device Manufacturers
The Role of Packaging Design In Drug Development

PUB - Selecting material for drug development
Selecting materials for medical device industry
Comments are closed.

- Previous Article
- Next Article
Are All Review Articles Useful and Have Clear Goals?
How do we define a review article and what are some of its key attributes, conflict of interest statement, funding sources, author contributions, what is a review article and what are its purpose, attributes, and goal(s).
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Richard Balon; What Is a Review Article and What Are Its Purpose, Attributes, and Goal(s). Psychother Psychosom 2 May 2022; 91 (3): 152–155. https://doi.org/10.1159/000522385
Download citation file:
- Ris (Zotero)
- Reference Manager
Review articles are an important staple of medical and other scientific literature that are liked and sought after by both readers and journals. The common perception is that they provide credible and reliable information about a specific area to readers and bring readership to journals. During the last decade or two we have seen a departure from the traditional narrative and integrated review articles to more specialized review articles such as systematic reviews with or without meta-analyses, umbrella reviews, viewpoints, and scoping reviews. It is not always clear what a review article and its different variations and permutations are, and also their goals, attributes, and utility.
Three recent articles [1-3] on the seemingly very similar topic of coexistence of anxiety and depression are a case in point of the lack of clarity of what a review article is and what its attributes and goals are The first one by Saha et al. [1] is a systematic review and meta-analysis which “found robust and consistent evidence of comorbidity between broadly defined mood and anxiety disorders. Clinicians should be vigilant for the prompt identification and treatment of this common type of comorbidity.” The second article by Cosci and Fava [2] (Editor and Associate Editor of this journal, where I am member of the Editorial Board) also states that depressive and anxiety disorders are frequently associated, and that depression may be a complication of anxiety and vice versa. They argue that the selection of treatment of coexisting anxiety and depression “should take into account the modalities of presentation and be filtered by clinical judgment.” The third review by Goodwin [3] states that: “Many antidepressant agents are also effective for symptoms of GAD [generalized anxiety disorder], including selective serotonin reuptake inhibitors (SSRIs)” and “Likewise, drug classes used to treat GAD are also effective in the treatment of depression with anxious symptoms (e.g., SSRIs, serotonin-noradrenaline reuptake inhibitors, tricyclic antidepressants, and agomelatine).”
I do not want to discount what is presented in these articles, but the question that comes to my mind (and I hope to the mind of other readers) is: what did we learn from these three articles and who benefits from them? Most clinicians know that anxiety and depression frequently coexist in spite of the fact that our nomenclature system has ignored this until the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders [4]. Thus, stating the obvious as a conclusion raises the question about the goals or aims of the article by Saha et al. [1]. Does any clinician need “an up-to-date list of studies that have examined comorbidity between broadly defined mood- and anxiety-related disorders and to meta-analyze the risk estimates according to key design features related to types of prevalence estimates for the two disorders” [sic]? The article by Goodwin [3] does not really provide anything new, or even a synthesis of previous data. It does not mention monoamine oxidase inhibitors as a treatment for coexisting anxiety and depression. This article also lists only one antidepressant – agomelatine - by its name among key words and in Key Summary Points, which considered together with the funding sources for the article may raise question about the article purpose. Cosci and Fava [2], in their “Innovation,” remind us of the complexity of clinical psychiatry and point out that: “Reviews generally base their conclusions on randomized controlled trials that refer to the average [italics mine] patient and may thus clash with the variety of clinical presentation.” They emphasize that diagnostic criteria “do not include patterns of symptoms, severity of illness, effects of comorbid conditions, timing of phenomena, rate of progression of illness, response to previous treatments that demarcate major prognostic and therapeutic differences among patients who otherwise seem to be deceptively similar since they share the same psychiatric diagnosis” (p. 309). They apply this discussion to coexisting anxiety and depression symptomatology. They call for a renaissance of psychopathology as the basic neglected method of clinical psychiatry and dimensional psychopathology that needs to be integrated into the diagnostic process. They also warn about the limits of existing guidelines that refer to a hypothetic or average patient, a strategy that is not always helpful in more or even less complicated clinical cases. This article is based on a new model of reviewing literature which integrates details of both biology and biography with the ultimate goal of “precision medicine” [5]. Yet their article [2] feels more as an “opinion piece” rather than solid review article.
Thus, in my opinion, out of three articles dealing with a similar topic, only one seems to be useful to clinicians [2]. Two of these articles [2, 3] would probably not fulfill usual journals’ criteria for a review article (see below), and one is not really clinically useful [1]. The utility of another one [3] is also doubtful. I am not saying that all review articles are not useful or do not fit what some envision as a review article. The goals of two of these articles [1, 3], though stated, are not very clear. These three examples [1-3] demonstrate the wide variety of what could be considered a review article, and that the utility of these types of articles can questionable. Thus, it seems that the review article and its attributes and goals require a closer look.
There is no one generally accepted definition of a review article. We all have certain ideas of how a review should look like and what it should accomplish. Some authors and organizations have formulated definitions of a review article. For instance, Ketcham and Crawford [6] note that in pragmatic terms the Institute of Scientific Information (ISI) Web of Knowledge Science Citation Index categorizes a paper as a review if it has more than 100 references, or if it appears in a review journal or the review section of a research journal, or if the paper states in the abstract that it is a review paper. That does not seem like a definition of what most readers and editors expect from a review paper, as, based on this definition, a review article could be just a simple listing of the main findings of a number of papers. Maggio et al. [7] provide a definition that is probably closest to an acceptable definition of a review: “A synthetic review and summary of what is known and unknown regarding the topic of a scholarly body of work, including the current work’s place within the existing knowledge.” They also point out that a literature review should provide context, inform methodology, help maximize innovation, and help avoid duplications. Some outline attributes of a good review article, proposing that such a review should provide synthesis and critical evaluation of available knowledge in a clear and concise way, while using rigorous and consistent methodology. A good review should also be even-handed in presenting various views and interpretations with a focus on answering a clinical or research question(s) in a clear and useful fashion. A solid review article should be sharply focused on a well-defined issue(s).
Though there is not one widely accepted precise definition of a review article, especially in view of newer variations and types of review articles, there seems to be a general notion of what a review article is and what the attributes of a good review article should be. Nevertheless, that is not the only factor that should be considered and addressed in writing a good and useful review. Other factors to be considered in writing are the type of review article, its purpose, intended audience, journal (general, clinical, educational, research), and the expertise of the author(s), their experience, and conflict(s) of interest (COI). In considering the author(s’) COI, one needs to pay attention to all possibilities of COI, and not just the relationship with pharmaceutical companies, but also for instance the author(s’) intellectual “investment,” such as patents, grants, and theoretical orientation (e.g., cognitive behavioral vs. psychodynamic orientation). Some journals also provide their own definition of what a review article should be. Some journals are focused only on reviewing and synthetizing the existing literature (e.g., UpToDate) or on reviews providing continuing medical education.
Types of Review Article
As noted, there is a growing number of permutations of what is called a review article. These include historical review, narrative review, systematic review with or without meta-analysis, integrated review, qualitative research synthesis, and viewpoints, to more specialized ones such as scoping review, rapid review, umbrella reviews, mapping review, meta-synthesis, mixed-method review, overview of reviews, diagnostic accuracy review, review of complex interventions, and network meta-analysis. The discussion of all these types is beyond the scope of this editorial; however, this list illustrates the complexity and confusion regarding review articles.
In their Editorial, Conn and Coon Sells [8] provide a brief outline of some of the more commonly known and used reviews. Narrative reviews “describe primary studies without using an integrated, meta-analysis, or meta-synthesis approach to examine results of various studies; historical review s trace development of an area of science by assessing the chronological order of studies and focus on possible temporal patterns; meta-analysis is the synthesis of previous quantitative studies and involves statistical approaches to aggregate effect size across primary studies to determine patterns of differences across studies related to key concepts; and umbrella reviews summarize findings of previous reviews. Scoping reviews are characterized as identifying the extent and range of previous studies by creating a profile of existing studies but placing little emphasis on study findings or methodological features [9]. However, in my view it seems that scoping reviews are rather preliminary and short reviews, clarifying concepts and identifying gaps, and are limited in their time and scope. Systematic reviews may or may not use meta-analysis and are focused on systematically analyzing studies related to a certain topic/question with particular attention to the methodology of studies, and synthetizing results using strategies to reduce bias and random errors.
It is important to realize that all types of reviews have their strengths and weaknesses and do have a different place in the evidence hierarchy. For instance, some may feel that meta-analyses provide a great systematic and statistically sound summary of available information, yet others point out their weaknesses, and the fact that meta-analyses of the same subject could provide different results [9] and could be of little clinical use [ 10, 11 ]. Meta-analyses rely on published data, do not necessarily include non-statistically significant results, select non-uniform statistical approaches, may have weak inclusion standards, and frequently have an agenda-driven bias. Contrary to the frequent perception that meta-analyses and systematic reviews are relatively free of COI after the financial COI related to the pharmaceutical industry is addressed, these articles may also be biased by non-financial COI [ 12 ]. It is also important to realize that the magic of the term systematic review fades away when one considers the clinical usefulness of this type of review article. As noted [ 13 ], systematic reviews require increasingly complicated and cumbersome procedures, and expert clinicians and expert critical clinical advice are not always part of the systematic review enterprise.
Purpose, Goals, and Attributes of a Review Article
The overall purpose of a review article should be to provide a valuable, solid, informative, critical summary of a well-defined topic/area to the reader . I am emphasizing the reader, as some (e.g., Ketcham and Crawford [6]) discuss the value of the review article for the author and for journals, and the reader is left out. The issue of value, though not always easy, is also important. It is related to the question that we may frequently have: Does the world need yet another review article on this topic?
Related to the reader is the audience. The audience is related to the reader, but not the same. Is the targeted audience a clinician, researcher, educator, student, resident, patient, families, or others?
Similarly important is the topic, or the question to be “answered,” or explored. The topic should always be clearly stated in the abstract and at the beginning of the text, to help the reader (and before him/her the editor and reviewers) to decide whether this article is of his/her interest. The topic should be as simple and narrow as possible, remembering that “less is more.” Nevertheless, while the topic should be narrow, the final product should be complex (not complicated), nuanced, and consider various opinions, views, and interpretations. The complexity and nuances are especially important in clinically oriented articles, as current clinical thinking is frequently superficial and reductionistic (as demonstrated for instance by the article by Goodwin [3]).
The next attribute to consider is what type of review article should one select. That is somewhat intertwined with the type of audience and journal. A general audience would probably still most appreciate either the classic narrative (a better term would be critical narrative review ) or historical review, followed by a solid systematic review. Most of the other types of review articles (e.g., mapping review, scoping review) are for more specialized audiences and journals. However, narrative reviews should not be the present-day summary of conclusions of research studies and case-reports. They should provide a critical, practical view of highly intellectual content/writing. These articles, especially in clinical medicine, should be written by real experts in the field who could appropriately and skillfully mix so-called evidence-based literature data, their clinical significance and application, and real-life experience and examples.
Selection of the journal is another issue, important for both the reader and the author. Some journals publish only or mostly review articles, some journals have a dedicated section for reviews, and some journals publish review articles occasionally. The reputation of the journal (including the magical and not always useful Impact Factor) should be considered, though it is not the most important factor. Journals with a great reputation can publish mediocre and not very useful reviews, while some journals with not such a great reputation may publish a very useful review(s).
Finally, the issue of usefulness is significant, namely for the reader. It is difficult to gauge easily. The reader (and author and editor) should consider this, especially in clinically oriented review articles. It is connected to the type of reader and the topic and scope. The reader should ask: what did I learn, and how can I use it.
A few more words about review articles. The articles should always have some educational value, no matter what the topic and audience is. Second, the language used should be clear and concise. Many of us have been dismayed by the lack of clarity, coherence, lucidity, and simplicity of psychoanalytic articles in the past. However, concerning language attributes, the language of some neuroscience articles seems even worse than the language of those old articles to me.
Review articles are a significant, vital part of medical literature. They have various formats and different goals. Review articles should be meaningful, and not just for improvement of the impact factor or H-index. That would be “l’art pour l’art.” Review articles should provide state-of-the-art critical reviews of particular topics, and should target specific readers. They should provide high educational value to readers. Journal editors should pay more attention to what review articles are and whether they are of value to their readership, and the readership should carefully consider what is worth reading and useful for one’s education.
The author declares no conflicts of interest.
There were no funding sources for this work.
Richard Balon, MD, is the sole author of this editorial.
Email alerts
Citing articles via, suggested reading.
- Online ISSN 1423-0348
- Print ISSN 0033-3190
INFORMATION
- Contact & Support
- Information & Downloads
- Rights & Permissions
- Terms & Conditions
- Catalogue & Pricing
- Policies & Information
- People & Organization
- Stay Up-to-Date
- Regional Offices
- Community Voice
SERVICES FOR
- Researchers
- Healthcare Professionals
- Patients & Supporters
- Health Sciences Industry
- Medical Societies
- Agents & Booksellers
Karger International
- S. Karger AG
- P.O Box, CH-4009 Basel (Switzerland)
- Allschwilerstrasse 10, CH-4055 Basel
- Tel: +41 61 306 11 11
- Fax: +41 61 306 12 34
- Email: [email protected]
- Experience Blog
- Privacy Policy
- Terms of Use
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Review Articles
Validation of biomarkers of aging
Robust validation of biomarkers of aging will be critical to their clinical translation; here, authors review the key challenges and propose recommendations to overcome them.
- Mahdi Moqri
- Chiara Herzog
- Luigi Ferrucci
The landscape of cancer research and cancer care in China
The authors discuss how screening strategies, treatment approaches and precision oncology are evolving in China and outline trends and priorities in the drug development and regulatory landscape.


Coproducing health research with Indigenous peoples
This Review explores how research coproduction with Indigenous peoples is evolving; it discusses the challenges and complexities and makes recommendations for researchers wishing to pursue coproduction with Indigenous peoples in responsive and effective ways.
- Chris Cunningham
- Monica Mercury

Recent successes in heart failure treatment
Recent years have seen major advances in heart failure treatment, but gaps in implementation and disparities in care remain; this Review outlines the current state of the field.
- Carolyn S. P. Lam
- Kieran F. Docherty
- Torbjørn Omland

Emerging diagnostics and therapeutics for Alzheimer disease
This Review summarizes recent advances in biomarkers and therapies for Alzheimer disease—the products of decades of research—and discusses the challenges, gaps and clinical implications.
- Wade K. Self
- David M. Holtzman
Considerations for patient and public involvement and engagement in health research
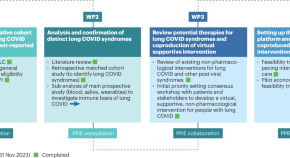
The authors generate a checklist of key considerations to guide patient and public involvement and engagement in future research, informed by lessons from the TLC study, which evaluated therapies for long COVID.
- Olalekan Lee Aiyegbusi
- Christel McMullan
- David C. Wraith
Climate change and health: three grand challenges
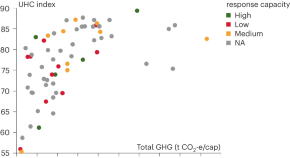
This Review outlines three ‘grand challenges’ to protect and promote health in the face of climate change, and discusses the role of the health community in driving change within and beyond the health sector.
- Diarmid Campbell-Lendrum
- Tara Neville
- Maria Neira
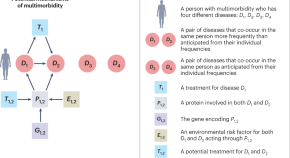
Biological and functional multimorbidity—from mechanisms to management
Multimorbidity is increasing globally, and addressing it requires a shift in the prevailing clinical, educational and scientific thinking. This Review discusses emerging mechanisms, research challenges and the implications for patients and healthcare systems.
- Claudia Langenberg
- Aroon D. Hingorani
- Christopher J. M. Whitty

Adverse childhood experiences and lifelong health
Adverse childhood experiences can negatively impact lifelong health; this Review discusses the underlying mechanisms and potential solutions, advocating for multisectoral interventions and implementation research.
- Zulfiqar A. Bhutta
- Supriya Bhavnani
- Vikram Patel
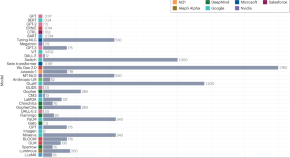
Large language models in medicine
This review explains how large language models (LLMs), such as ChatGPT, are developed and discusses their strengths and limitations in the context of potential clinical applications.
- Arun James Thirunavukarasu
- Darren Shu Jeng Ting
- Daniel Shu Wei Ting
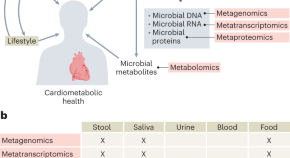
Cardiometabolic health, diet and the gut microbiome: a meta-omics perspective
Cardiometabolic health is tightly linked to diet and the gut microbiome. This Review explains how meta-omics technologies are revealing the intricate links between them and discusses the most promising paths to clinical translation.
- Mireia Valles-Colomer
- Cristina Menni
- Nicola Segata
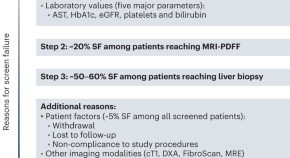
Challenges and opportunities in NASH drug development
This Review surveys the NASH clinical trial landscape and the main challenges to drug approval, and discusses new approaches to overcoming these, including innovative trial designs, non-invasive tests and biomarkers.
- Stephen A. Harrison
- Alina M. Allen
- Naim Alkhouri
Comorbidities, multimorbidity and COVID-19
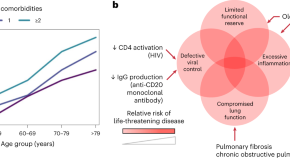
This Review discusses the effect of comorbidities and multimorbidity on the three mechanistically distinct phases of COVID-19, evaluating the evidence in the context of confounding factors and our evolving understanding of the disease.
- Clark D. Russell
- Nazir I. Lone
- J. Kenneth Baillie

New and emerging approaches to treat psychiatric disorders
This Review provides a timely overview of new technological advances and treatment approaches, with a particular emphasis on brain-circuit-based interventions for precision psychiatry.
- Katherine W. Scangos
- Matthew W. State
- Leanne M. Williams

The landscape of mRNA nanomedicine
The COVID-19 mRNA vaccines have transformed the field of mRNA nanomedicine, but this new class of therapeutics has the potential to treat many other diseases. This Review profiles the latest advances and challenges.
- Xiangang Huang
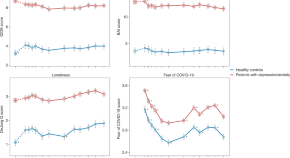
How COVID-19 shaped mental health: from infection to pandemic effects
This Review discusses the impact of COVID-19 on mental health, from pandemic-related societal effects to direct infection-related neuropsychiatric sequelae, highlighting the lessons learned and outstanding knowledge gaps.
- Brenda W. J. H. Penninx
- Michael E. Benros
- Christiaan H. Vinkers

Multimodal biomedical AI
Multimodal artificial intelligence models could unlock many exciting applications in health and medicine; this Review outlines the most promising uses and the technical pitfalls to avoid.
- Julián N. Acosta
- Guido J. Falcone
- Eric J. Topol
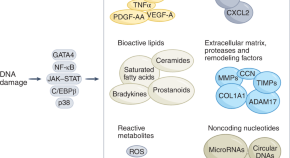
Cellular senescence and senolytics: the path to the clinic
Cellular senescence has emerged as a promising therapeutic target for disorders across the lifespan; this Review highlights the most promising strategies for translating senescence-targeting interventions into clinical use in the near future.
- Selim Chaib
- Tamar Tchkonia
- James L. Kirkland
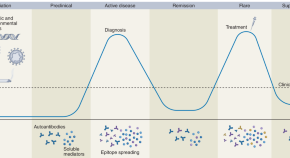
The promise of precision medicine in rheumatology
Precision medicine for rheumatic diseases is still in its infancy, but recent advances are enabling comprehensive profiling and mechanistic insights. This Review outlines the progress, promises, and challenges of translating these findings into the clinic.
- Joel M. Guthridge
- Catriona A. Wagner
- Judith A. James
Regenerative and restorative medicine for eye disease
Restoration of visual function in degenerative retinal disease may be an attainable goal, thanks to advances in cell-based therapy, gene therapy, and prosthetics. This Review discusses the most promising strategies that will probably reach clinical use in the next decade.
- Russell N. Van Gelder
- Michael F. Chiang
- Clive N. Svendsen
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Download PDF
- CME & MOC
- Share X Facebook Email LinkedIn
- Permissions
A Dynamical Systems View of Psychiatric Disorders—Theory : A Review
- 1 Wageningen University, Wageningen, the Netherlands
- 2 Amsterdam UMC, Amsterdam, the Netherlands
- 3 University of Amsterdam, Amsterdam, the Netherlands
- 4 Donders Institute, Nijmegen, the Netherlands
- 5 University of Melbourne, Melbourne, Victoria, Australia
- 6 Virginia Commonwealth University, Richmond
- 7 Johns Hopkins University, Baltimore, Maryland
- 8 Orygen, Parkville, Victoria, Australia
- Review A Dynamical Systems View of Psychiatric Disorders—Practical Implications Marten Scheffer, PhD; Claudi L. Bockting, PhD; Denny Borsboom, PhD; Roshan Cools, PhD; Clara Delecroix, MSc; Jessica A. Hartmann, PhD; Kenneth S. Kendler, MD; Ingrid van de Leemput, PhD; Han L. J. van der Maas, PhD; Egbert van Nes, PhD; Mark Mattson, PhD; Pat D. McGorry, PhD; Barnaby Nelson, PhD JAMA Psychiatry
Importance Psychiatric disorders may come and go with symptoms changing over a lifetime. This suggests the need for a paradigm shift in diagnosis and treatment. Here we present a fresh look inspired by dynamical systems theory. This theory is used widely to explain tipping points, cycles, and chaos in complex systems ranging from the climate to ecosystems.
Observations In the dynamical systems view, we propose the healthy state has a basin of attraction representing its resilience, while disorders are alternative attractors in which the system can become trapped. Rather than an immutable trait, resilience in this approach is a dynamical property. Recent work has demonstrated the universality of generic dynamical indicators of resilience that are now employed globally to monitor the risks of collapse of complex systems, such as tropical rainforests and tipping elements of the climate system. Other dynamical systems tools are used in ecology and climate science to infer causality from time series. Moreover, experiences in ecological restoration confirm the theoretical prediction that under some conditions, short interventions may invoke long-term success when they flip the system into an alternative basin of attraction. All this implies practical applications for psychiatry, as are discussed in part 2 of this article.
Conclusions and Relevance Work in the field of dynamical systems points to novel ways of inferring causality and quantifying resilience from time series. Those approaches have now been tried and tested in a range of complex systems. The same tools may help monitoring and managing resilience of the healthy state as well as psychiatric disorders.
Read More About
Scheffer M , Bockting CL , Borsboom D, et al. A Dynamical Systems View of Psychiatric Disorders—Theory : A Review . JAMA Psychiatry. Published online April 03, 2024. doi:10.1001/jamapsychiatry.2024.0215
Manage citations:
© 2024
Artificial Intelligence Resource Center
Psychiatry in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Materials Advances
Plant-derived selenium nanoparticles: investigating unique morphologies, enhancing therapeutic uses, and leading the way in tailored medical treatments.
Selenium (Se) stands as a paramount micronutrient, indispensable for the holistic health of humans, animals, and microorganisms. At its core, Se is instrumental for the genesis of selenocysteine, an exclusive amino acid vital for the assembly of selenoproteins, critical actors in human physiology. While the health dividends of Se are profound, its therapeutic potential is intricately tethered to a precise dosage window, underlining the imperativeness of meticulous calibration. Emerging from this backdrop, Selenium nanoparticles (SeNPs) have ascended as the gold standard in nanomaterials, distinguished by their unparalleled immunomodulatory prowess, superior biocompatibility, and enhanced bioavailability. Their reduced toxicity further consolidates their preeminence in biomedical applications. Synthesis methodologies for SeNPs span a spectrum from physical and chemical to biological approaches. Yet, it is the phyto-synthesized SeNPs that reign supreme, characterized by their singular morphological and biochemical attributes, which impart an unmatched compatibility with human tissues. Strikingly, despite their evident superiority, plant-derived SeNPs remain conspicuously underrepresented in the pharmaceutical arena. Contemporary research not only extols the therapeutic potency of SeNPs but also underscores their formidable efficacy against formidable adversaries like cancer cells, microbial pathogens, and viral threats, as well as their robust antioxidant capabilities. This review embarks on a rigorous exposition of the vanguard in plant-mediated SeNPs synthesis, traversing the diverse botanical landscape. It further ventures into the frontier of SeNPs functionalization, illuminating prospects for precision-targeted drug delivery. Conclusively, the review furnishes a comprehensive elucidation of the intricate therapeutic mechanisms harnessed by SeNPs, charting a blueprint for the future of personalized medical interventions.
- This article is part of the themed collection: Recent Review Articles
Article information
Download Citation
Permissions.
A. V. Puri, P. Mohite, Y. Ansari, N. Mukerjee, H. M. Alharbi, A. Upaganlawar and N. D. Thorat, Mater. Adv. , 2024, Accepted Manuscript , DOI: 10.1039/D3MA01126G
This article is licensed under a Creative Commons Attribution 3.0 Unported Licence . You can use material from this article in other publications without requesting further permissions from the RSC, provided that the correct acknowledgement is given.
Read more about how to correctly acknowledge RSC content .
Social activity
Search articles by author.
This article has not yet been cited.
Advertisements
- Open access
- Published: 29 March 2024
Plant a seed series: the impact of an online outreach package on school pupils’ knowledge, skills, and attitudes to medicine
- Nadin Hawwash 1 , 2 &
- Enam Haque 1
BMC Medical Education volume 24 , Article number: 347 ( 2024 ) Cite this article
180 Accesses
5 Altmetric
Metrics details
Medicine is one of the most inaccessible professions in the United Kingdom (UK). The Plant a Seed (PAS) series was created to address this; it is an online pre-recorded three-part video series to “Inspire”, “Educate” and “Motivate” pupils from widening participation backgrounds on Medicine. We explored the impact of PAS on pupils’ knowledge, skills and attitude to Medicine.
We conducted a national pretest-posttest study of Years 7–9 pupils in the UK. 503 schools were invited to PAS, following ethics approval. Consented pupils viewed all three episodes asynchronously and completed a pre-and post-series Likert scale confidence questionnaire, which evaluated their knowledge, skills and attitudes to a medical career. A Shapiro-Wilk test showed the lack of a normal distribution ( p < 0.05); therefore, a Wilcoxon signed-rank test statistically compared pretest-posttest results of each pupil.
70 pupils in Years 7–9 from 2 schools participated in this study. PAS was shown to significantly increase pupils’ knowledge of the role and life of a doctor, medicine as a degree, admissions requirements, and careers in medicine ( p < 0.05). There was a significant increase in pupils believing they could study medicine. The intervention did not significantly increase the desire for pupils to study medicine ( p = 0.187).
PAS significantly improved pupils’ knowledge, skills and confidence demonstrating the need and benefit to enrolment of the programme at scale. It did not significantly increase the number of pupils wishing to study medicine. Analysis at scale is required to evaluate the effectiveness of PAS as a key intervention to break down barriers to medicine.
Peer Review reports
Medicine is one of the most inaccessible professions to enter given the application demands, financial requirements and limited opportunities available to students from working-class backgrounds [ 1 ]. According to the 2016 Social Mobility in the UK Report, just 4% of doctors in the UK come from a working-class background [ 2 ]. The 2013 General Medical Council (GMC)’s National Training Survey found that only 25% of medical trainees were from state schools, only 8% had received free school meals and only 6% grew up in the most deprived areas of the UK [ 3 ]. It is evident there is a longstanding skew in medicine towards more socio-economically advantaged pupils. Although most medical schools in the UK seek triple A A-level results, factors primarily considered beyond this which may disadvantage students from working-class backgrounds include the requirement for high achieving scores in the University Clinical Aptitude Test (UCAT) or BioMedical Admissions Test (BMAT), evidence of volunteering over a specific period in a healthcare setting and evidence of undertaking extra-curricular activities [ 4 , 5 ]. Pupils may not be aware of such requirements generally or in a timely manner to allow for preparation. Pupils from working-class backgrounds may not have support networks within or outside of their academic institution to raise awareness on application requirements or provide support, guidance and opportunities [ 6 ]. Additionally, such preparation or engagement may have associated costs that not all students can afford, for example, a 6-day Medical Summer school costing £3,249 or online admissions preparation packages costing £595 [ 7 , 8 ].
Widening participation (WP) aims to address the underrepresentation in medicine. WP describes attempts to increase pupils entering higher education, particularly from under-represented groups such as (i) low-income backgrounds, (ii) pupils from schools with low performance compared to the national average, (iii) from areas with limited higher education participation and (iv) first-generation higher education students [ 9 ]. Attempts to diversify medicine included the establishment of the National Medical Schools WP Forum (National Forum) in 2015, an organisation of 24 UK medical schools. A key highlight of their work was developing UKWPMed, a collaborative initiative consisting of 6 medical schools providing WP students aspiring to study medicine with an automatic interview and contextual offer in any of the partner institutions [ 10 ]. The National Forum identified a challenge to delivering WP initiatives was the lack of sustainable funding, which was needed for reimbursing travel costs and food expenses for pupils to attend outreach activities [ 10 ]. It made sense, therefore, to develop an WP initiative delivered at a minimal cost.
In the UK national curriculum, Key Stage 3 is defined as Years 7–9 and occurs prior to GCSE exams sittings in Year 10 and 11 and A-level sittings are in Year 12 and 13 [ 11 ]. WP initiatives in medicine mainly focus on primary school pupils (Year 1–6) or pupils in Year 9 to Year 13 [ 12 , 13 , 14 ]; however, we hypothesised that Years 7–9 was a critical age for raising awareness of medicine as a career as it was the timepoint when pupils consider choosing their GCSE subjects. In the UK, medical schools determine admission to their programmes based on the subjects chosen and grades obtained by applicants. For instance, a pivotal decision to be made during Year 7–9 for medicine includes studying the three sciences Chemistry, Biology and Physics separately as opposed to the BTEC qualifications whereby the latter limits the number of Medical Schools the student may be eligible to apply for. On applying to medicine, evidencing transferrable skills such as communication, leadership, teamwork and problem solving is essential as these are skills required during in the medical programme and for a career as a doctor [ 15 ]. Communication skills such as empathy, gathering information and listening are crucial skills to practice and use as a doctor to create a positive doctor-patient relationship to aid the provision of the best patient care [ 16 ].
A study by Martin et al. (2018) demonstrated that Year 9 pupils had minimal awareness of medicine and the breadth of medical careers [ 14 ]. McHarg et al. (2007), conducted semi-structured interviews with 15 medical students who felt that school support and raising their aspirations helped pupils from WP backgrounds to be motivated to apply to medicine [ 17 ]. McHarg et al. (2007) also found early exposure to medicine to be an important aspect in WP allowing time for the idea to “flourish” [ 17 ]. Gore et al. (2018) highlighted the importance of creating sustained outreach in primary and secondary schools [ 18 ].
The Plant a Seed (PAS) series, a low-cost sustained secondary school outreach package for Year 7–9 pupils, was created to address these points and provide early insight into medical school and medical careers. PAS is an online pre-recorded three-part video series, with each video mapping to one of the themes, “Inspire”, “Educate” and “Motivate”. Pupils had opportunity to view the three sessions over the academic year and thus had the time to reflect after each video. The low cost associated with running this fully asynchronous programme at scale highlights its sustainability. The PAS series shares similarities with the Social Cognitive Theory established by Albert Bandura in the 1960s. Bandura’s Social Cognitive Theory highlights the influence of interactions between personal factors such as knowledge and attitudes, environmental factors such as access in community and behaviours such as skills and self-efficacy [ 19 , 20 ]. Consequently, we hypothesise that having the opportunity to observe and learn from positive role models through the PAS series will impact on a pupil’s knowledge, attitude and career aspirations thereby enhancing their self-efficacy, inspire and motivate them to consider medicine as a viable career prospect [ 19 ]. This study aimed to assess the impact the PAS online outreach package had on the knowledge, skills and attitude to Medicine as a degree and career of pupils in Years 7–9 from WP backgrounds.
Participants
To be eligible for this study, pupils had to (i) be in Years 7–9 at a secondary school in the UK, (ii) from a secondary school in a WP-flagged location and (iii) have completed the whole PAS series.
Recruitment
We performed a national pretest-posttest study of PAS. We recruited UK secondary school pupils in Years 7–9, by emailing 503 schools located in WP postcode areas and inviting them to take part in the study. This information was obtained using the Higher Education Access Tracker (HEAT) database [ 21 ]. Schools that expressed interest were provided with an in-depth letter explaining the study and the PAS series. Schools committed to participating were then sent a link to the PAS webpage which included pupil assent forms, participant information sheets and parent consent forms. Schools that posted back completed forms for each participating pupil were recruited to the study. Printed forms and pre-paid postage envelopes were provided on request. Eligible schools were invited between June 2022 and December 2022 to complete the PAS series in their own time from the date they enrol onto the series till April 2023. Almost a year was provided to complete the PAS series to ensure the PAS sessions were conducted at 3 points over the academic year at times most suitable for schools that would not impact on learning the school curriculum or preparing for exams. This study was conducted as a series to allow time for consolidation of the knowledge gained from each part in the series. Pupils that did not provide signed consent and assent forms could not partake in the PAS series. Teachers were advised to arrange for alternative education sessions during school hours for pupils that did not provide consent, to ensure their education was not impacted by not participating in the series.
Three PAS video sessions were available in the PAS series. Each PAS video session lasted 30 to 60 min and began with a clip of the day in the life of a doctor or surgeon. The “Inspire” recording began with the day in the life of a GP, followed by the history of heart surgery and the development of vaccines. These topics aimed to inspire pupils to consider medicine as a career. The “Educate” session began with the day in a life of a foundation year doctor followed by the teaching on the anatomy of the lungs, as well as the pathophysiology, diagnosis, and treatment of asthma. This was developed to provide insight into the learning undertaken by medical students. The “Motivate” video looked at a day in a life of a surgeon, followed by the journey of a medical student through higher education. This was to make pupils believe they could follow a similar journey. All the PAS content including videos and worksheets, questionnaires, consent and participant information forms were validated by the University of Manchester ethics committee and Access and Success Team to ensure easy language was used that was accessible to all pupils. Additionally, all videos contained subtitles to ensure accessibility to pupils that are deaf or hard of hearing.
Study design
Teachers were invited to watch a briefing video before starting the series, which explained how to navigate the videos and the specific tasks for pupils to complete in the workbook. Teachers then asked pupils to complete the pre-test study paper questionnaire with the pupil’s name on it before they started watching the first video. Teachers were asked to securely store the paper questionnaires in a secure place, to maintain confidentiality. They then accessed the PAS videos through a secure website link, hosted by the University of Manchester. This was accessible to them throughout the study period. Teachers downloaded the worksheets for each session and then handed them to pupils to complete during each session. After viewing all three videos in the PAS series, pupils were handed back their pre-study questionnaire. Pupils were instructed to first input their pre-study paper questionnaire results onto the online version of the questionnaire and then complete the post-test study questionnaire. This enabled the anonymous collection and pairing of pre-and post-series questionnaire feedback from the same pupil. Pupils were made aware in the participant information form that questionnaires submitted would be anonymous and that paper questionnaires would be destroyed.
Questionnaire
The PAS questionnaire consisted of 11 questions with a five-point Likert scale (“Strongly Agree” to “Strongly Disagree”) that measured pupil confidence in knowledge, skills and attitudes towards medicine as a degree and career (Table 1 ). There was a paired analysis of pre-and post-study results for each pupil. Pre- and post-series questionnaires were identical except for the additional inclusion of a comments section. Pupils could complete this section to provide written feedback on the question “If you feel more informed about a career and how to study medicine, what has changed and why?”.
Statistical analysis
A Shapiro-Wilk test was used to assess whether there was a normal distribution in the data, and therefore the type of statistical analysis to use. Given the lack of a normal distribution ( p < 0.05), a Wilcoxon signed-rank test was used to statistically compared pre- and post-series questionnaire results for each pupil to identify any significant differences in knowledge, skills and attitudes on attending the series.
70 pupils in Years 7–9 from two participating schools located in Derbyshire were included in this study. On completion of the PAS series, there was a significant increase in pupils’ knowledge of what a doctor did ( p = 0.002). The proportion of pupils that strongly agreed to the increase in their knowledge of what a doctor did rose from 17% before the session, to 39% after the session (Fig. 1 ). Pupils’ knowledge of medicine as a degree significantly increased ( p < 0.0001). Overall, 2% of pupils strongly agreed that they know about the medicine degree pre-series which increased to 29% post-series (Fig. 1 ). Additionally, a significant increase was found in the knowledge of medicine undergraduate admissions requirements ( p < 0.0001), as well as subject entry requirements ( p < 0.0001). The PAS series also increased the knowledge in pupils’ understanding of life as a doctor ( p < 0.0001). The proportion of pupils strongly agreeing to knowing about life as a doctor increased from 4% pre-series to 29% post-series. Furthermore, the proportion of pupils strongly agreeing with their awareness of the different careers in medicine more than doubled upon completion of the PAS series (Fig. 1 ).
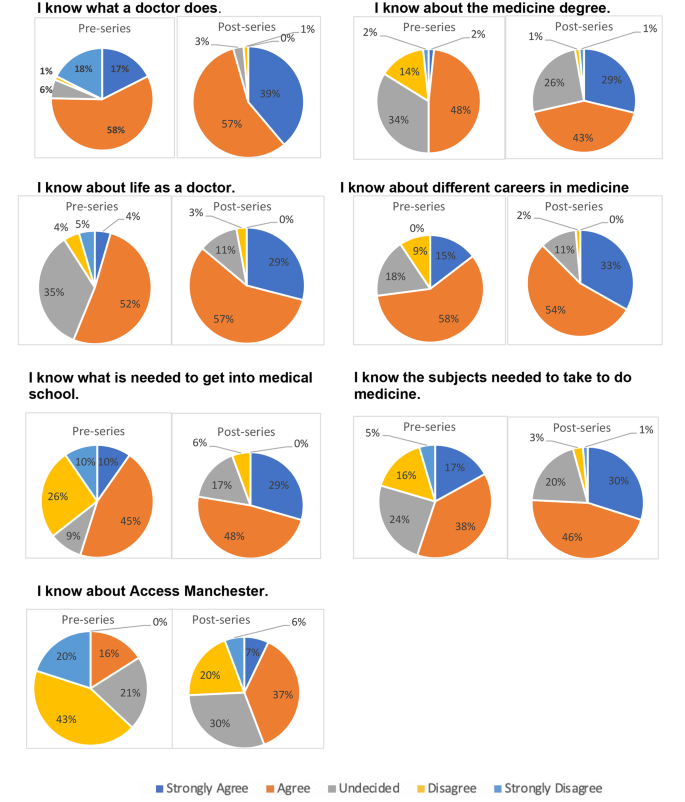
Pupil knowledge of medicine as a degree and career pre- and post-series
The PAS series significantly increased pupils’ beliefs that they had the necessary skills to apply to medicine ( p < 0.0001) and that they had the necessary communication skills to study medicine ( p < 0.0001) (Fig. 2 ).
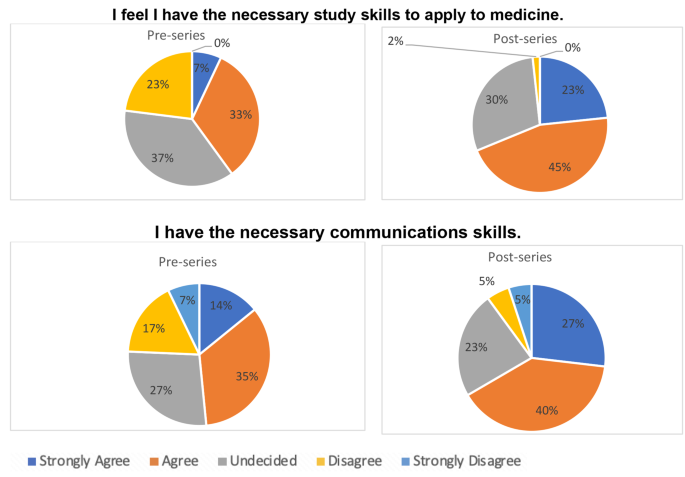
Pupil knowledge of the skills required in medicine pre- and post-series
On analysis of pupils’ attitudes towards medicine, this study found a significant improvement in pupils’ confidence in applying to medical school after completing the PAS series ( p < 0.0001). There was an improvement in pupils that wished to study medicine, but this was not statistically significant ( p = 0.187). The proportion of pupils strongly agreeing to want to study medicine only rose from 7 to 9% upon completion of the PAS series; however, few pupils strongly disagreed or disagreed with wanting to study medicine after the series (Fig. 3 ).
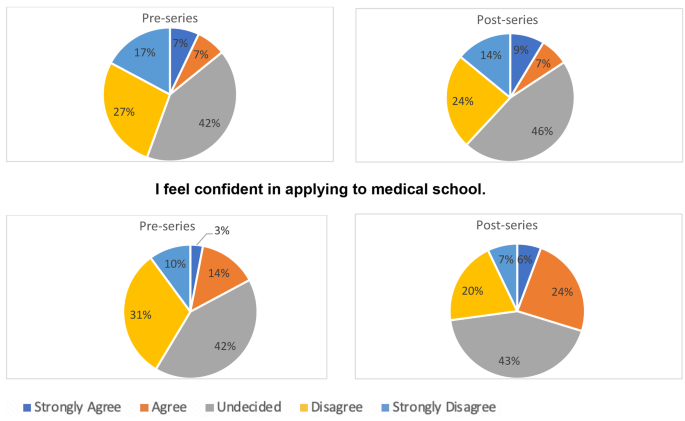
Pupils’ attitude towards medicine pre- and post-series
Pupils’ perceptions
To gain further insight in understanding factors that contributed to the changes in pupils’ perceptions in time regarding medicine as a degree and career, qualitative results were also collected. This provided opportunities to explore pivotal domains to consider and address when planning WP initiatives like PAS. A thematic analysis of open-ended comments provided by pupils on their perceptions of medicine as a degree and career on completing the PAS series is shown in Table 2 . Many pupils mentioned they felt more informed after the series “I feel more informed about a career and how to study medicine because I have been told what I could take for GCSE and the steps and layout there is for applying to Medical School, which gives me a brief outline, therefore, I feel more confident”.
Other pupils felt they were now more aware of the different options within Medicine “The Plant a Seed series has definitely made me more aware of the options within the Medicine degree, but I couldn’t say one hundred per cent that I would go into medicine”. Some pupils expressed the PAS series did not change their perception of medicine.
The PAS series appeared to change some pupils’ perception of what a medical career entailed “ I’m now reconsidering medicine if my other job doesn’t work out because I didn’t know that medicine was like a puzzle, and you have to try and figure out what is wrong with them and give them the right treatment”.
This study aimed to explore the impact of a low-cost online WP initiative on pupils’ knowledge, skills and attitudes toward a career in medicine. It found significant improvements in all three domains, demonstrating the effectiveness of the PAS series. Findings from this study emphasises the impact Universities can have and outlines the importance of prioritising widening participation at an early stage. PAS demonstrates the impact low-cost interventions can have and prioritisation of Government support through funding and measures such as annual social mobility league tables to encourage University involvement is key to bridge the gap and enable equal opportunities for all pupils [ 22 ].
However, the PAS study did not find that the intervention significantly increased pupils’ desire to study medicine. It is hard to gauge why this discrepancy took place. The written comments provided in the post-series survey suggested pupils’ knowledge of medicine as an undergraduate degree and career increased but they were still not sure if medicine was a career for them. This suggests that the PAS series may have allowed pupils to make informed decisions on their future. It is imperative to note that WP initiatives do not pressure pupils into applying to medicine but provide them with the level of knowledge and the necessary support to allow them to make an informed decision about their future degrees and careers. The pupils feedback suggested that this goal was achieved. On the other hand, other unknown factors may have contributed to the lack of significant change in pupils’ attitudes, which would need to be explored using qualitative methods. A potential factor that may have contributed to this could be the costs associated with an undergraduate medicine degree in the UK and the minimum five-year duration of the undergraduate degree before working and receiving a salary. Costs associated with undergraduate medicine for a UK student include tuition fee costs at £9,250 per year, living costs at an average £11,484 in year one and £12,350 for the following years, travel costs associated placements, equipment costs such as a stethoscope and costs for elective placements [ 23 , 24 ]. This gives an estimated minimum required cost of £107,134 for tuition fees and living costs alone without the added interest and additional expenses mentioned. Thus, although pupils are now more aware of the programme through PAS, studying a medicine degree may not be a sustainable option for those in particular from lower socioeconomic backgrounds. Additionally, although PAS provides a deeper understanding of medicine as a degree and career at an early stage, support for more specific preparations for medicine applications such as the University Clinical Aptitude Test (UCAT) or BioMedical Admissions Test (BMAT) is still required depending on the universities applied for [ 4 , 5 ]. Career barriers which may deter pupils from pursuing a career in medicine includes the debt associated with the medical degree, costs associated with training, long working hours and the salary in foundation training. A survey published by the British Medical Association in February 2023 found junior doctors financially struggling with over 50% of their utility bills and the current level of pay being among the top reasons for the consideration of leaving their role [ 25 ].
On the whole, the PAS series could adapt to having a focus on promoting medicine as a career. One suggestion would be to offer interactive Q&A sessions, as an additional component of the series, with the opportunity for pupils to ask a panel of doctors, academics and medical students any pressing questions they had about a medical career. A study found interaction during online sessions resulted in behavioural and emotional engagement with online learning and encouraged learning outside of the session [ 26 ]. However, the incorporation of live sessions would prevent the provision of a fully asynchronous programme and would need adequate resourcing.
Strengths and limitations
A key strength of the study was the novelty of the intervention in its focus on Years 7–9 pupils from WP postcodes. As an online asynchronous intervention, PAS was delivered at a low cost to both schools and the university with no financial cost to pupils. This suggests a sustainable future for the intervention. We maintained an inclusive approach to recruitment, by ensuring the series was delivered during school hours. This meant that all pupils could access the videos. Pupils may not have access to the appropriate technology to run the series at home, given the known digital divide in the UK, with a recently estimated over 700,000 pupils having limited access to online learning outside school hours [ 27 ].
A key limitation was the small sample size given out of the 503 WP schools invited only 2 schools participated in the series. Contributing factors included the significant delay with ethics approval, which resulted in a short time to advertise and recruit schools. Another factor was that schools may have been put off by the need for pupils to view three 30–60-minute videos over the course of the academic year. This challenge was worsened by reduced teaching time, due to the national teachers’ strikes in 2023. Another barrier was the administrative burden of the study for each school, with paper consent forms and questionnaires adding to the high level of paperwork. Attempts to overcome this included the provision of a prepaid envelope and an offer to provide printed forms to avoid the need to scan in the signed forms. However, we did not have a solution for reducing the time to collect all consent/assent forms from pupils.
Future work
Future analysis at scale and over a longer period of follow-up will be undertaken to fully capture the impact of this series on pupil’s knowledge, skills and attitudes to medicine as a degree and career and quantify the number of pupils who applied to and were successful on the medicine programme. We propose to use HEAT tracking to establish the long-term impact of the PAS series. HEAT tracking would enable them to see how many of the pupils who completed PAS entered medical school [ 21 ]. However, the team accept that PAS would only be one contributing factor to a pupil deciding on a career in medicine. Analysis at scale would also enable a sufficient sample size for sub-group analysis of the impact of gender, age, ethnicity, parental occupation and socioeconomic status on the overall questionnaire score. We suggest a future study should incorporate rigorous qualitative analysis with qualitative comments [ 28 ]. This data could be obtained through ethics-approved focus groups of pupils that participated in the study.
We also plan to discuss PAS with schools to explore how they can make the process easier for the teachers and administrative staff. This would increase uptake and help increase the generalisability of study findings to areas across the UK. Although a strength of the study included enrolment through schools and not pupils, a limitation was that it meant that pupils potentially interested in PAS could not enrol without interest from their school. Future work could include recruiting pupils directly. However, pupils from WP backgrounds may not have access to facilities at home to view the videos, and it may be cumbersome obtaining consent for them.
Findings from this study underscore the impact low-cost and effective WP interventions like PAS can have on significantly improving pupils’ knowledge, skills and confidence in considering a degree and career in medicine and evidences the need for government and academic institutions to invest in and award such interventions. PAS will be delivered on a national scale to schools in deprived areas of the UK to allow pupils to make more informed decisions about their future and will improve inclusivity and diversity in the healthcare workforce.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
Higher Education Access Tracker
Plant a Seed
- Widening participation
Reference list
Martin AJ, Beska BJ, Wood G, Wyatt N, Codd A, Vance G, et al. Widening interest, widening participation: factors influencing school students’ aspirations to study medicine. BMC Med Educ. 2018;18(1):1–13.
Article Google Scholar
Social mobility in the UK. state of the nation 2016 report - GOV.UK [Accessed 2023 May 24]. Available from: https://www.gov.uk/government/publications/state-of-the-nation-2016
GMC. National training survey 2013: socioeconomic status questions October 2013 | 2 at any point during your school years, did your household receive income support? 2013.
UKCAT. About the University Clinical Aptitude Test (UCAT) | UCAT Consortium [Accessed 2024 Jan 24]. University Clinical Aptitude Test. 2021. Available from: https://www.ucat.ac.uk/
BMAT | Cambridge Assessment Admissions Testing [Accessed. 2024 Jan 24]. Available from: https://www.admissionstesting.org/for-test-takers/bmat/
Joseph J, Dao D, Hwang SM, Dotzler SM, Chesak SS, Weiskittel TM, et al. Perceptions of barriers and facilitators to becoming a Medical Professional among underrepresented undergraduate and Postbaccalaureate Learners. Mayo Clin Proc Innov Qual Outcomes. 2021;5(2):347–58.
6-day Medical Summer School – Medic Mentors [Accessed. 2024 Jan 25]. Available from: https://medicmentor.co.uk/6-day-medical-summer-school/
UCAT Courses | In-Person or Online. | Trusted by 150 + Schools - The Medic Portal [Accessed 2024 Jan 25]. Available from: https://www.themedicportal.com/courses/ucat-courses/?gad_source=1&gclid=Cj0KCQiAqsitBhDlARIsAGMR1Ri6hUIdwNuPWHlG7KREq8VuCh2k99p-W3cBG-VbrvXVRbgMWmhmpi4aAmtCEALw_wcB
Widening participation | The University of Manchester [Accessed. 2023 Aug 3]. Available from: https://www.manchester.ac.uk/discover/social-responsibility/social-inclusion/widening-participation/
Haque E, Spencer A, Alldridge L. Developing a UK widening participation forum. Clin Teach. 2021;18(5):482–4.
The national curriculum: Overview - GOV.UK [Accessed 2024 Jan 24]. 2023. Available from: https://www.gov.uk/national-curriculum
Medics. in Primary Schools – Sentinus [Accessed 2024 Jan 25]. Available from: https://www.sentinus.co.uk/programmes/medics-in-primary-schools/
Ryan B, Auty C, Maden M, Leggett A, Staley A, Haque E. Widening participation in medicine: The impact of medical student-led conferences for year 12 pupils. Adv Med Educ Pract. 2021;12:937–43.
Martin AJ, Beska BJ, Wood G, Wyatt N, Codd A, Vance G et al. Widening interest, widening participation: factors influencing school students’ aspirations to study medicine. BMC Med Educ. 2018;18(1).
Transferable skills whilst at medical school | Health Careers [Accessed. 2024 Jan 25]. Available from: https://www.healthcareers.nhs.uk/explore-roles/doctors/medical-school/transferable-skills-whilst-medical-school
Biglu M-H, Nateqv F, Ghojazadeh M, Asgharzadeh A. Communication skills of Physicians and patients’ satisfaction. Mater Socio Med. 2017;29(3):192.
McHarg J, Mattick K, Knight LV. Why people apply to medical school: implications for widening participation activities. Med Educ. 2007;41(8):815–21.
Gore J, Patfield S, Holmes K, Smith M. Widening participation in medicine? New insights from school students’ aspirations. Med Educ. 2018;52(2):227–38.
Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Adv Behav Res Ther. 1978;1(4):139–61.
Bandura A, McClelland D. Social Foundations of Thought and Action: A social cognitive theory. Social Learning Theory. 1977. p. 12–29.
Higher Education Access Tracker [Accessed. 2023 Aug 4]. Available from: https://heat.ac.uk/how-it-works/tracking-research-and-evidence/
White C. Just 4% of UK doctors come from working class backgrounds. BMJ. 2016;355:i6330.
Intercalation | Medicine MBChB | University of Manchester [Accessed. 2024 Feb 7]. Available from: https://www.bmh.manchester.ac.uk/study/medicine/finance/
Studying Medicine. A Guide To Medical Student Finance [Accessed 2024 Feb 7]. Available from: https://www.bmj.com/careers/article/studying-medicine-a-guide-to-medical-student-finance
BMA. A perfect storm of poor conditions and pay [Accessed 2024 Jan 25]. 2023. Available from: https://www.bma.org.uk/news-and-opinion/a-perfect-storm-of-poor-conditions-and-pay?_gl=1*pqbgnj*_up*MQ.*_ga*MTE2MDIxNzgwNi4xNzA2MTk2NTU2*_ga_F8G3Q36DDR*MTcwNjE5NjU1NS4xLjAuMTcwNjE5NjU1NS4wLjAuMA
Gherghel C, Yasuda S, Kita Y. Interaction during online classes fosters engagement with learning and self-directed study both in the first and second years of the COVID-19 pandemic. Comput Educ. 2023;200:104795.
Homeschooling BBC. Lack of internet putting some children at a disadvantage say MPs - CBBC Newsround [Accessed 2023 Aug 4]. 2020. Available from: https://www.bbc.co.uk/newsround/53047270
Roberts K, Dowell A, Nie JB. Attempting rigour and replicability in thematic analysis of qualitative research data; a case study of codebook development. BMC Med Res Methodol. 2019;19(1):1–8.
Download references
Acknowledgements
We would like to acknowledge the pupils and schools involved in PAS for their commitment to the series. We would also like to acknowledge Annie Baldwin and Lior Saad for their contribution to the creation of the PAS series online content. We would also like to acknowledge Albert Jennings and Hannah Thomas for the administrative support related to the PAS series and would like to thank all staff that contributed to supporting the creation of the PAS webpage.
This research study received no external funding.
Author information
Authors and affiliations.
School of Medical Sciences, Faculty of Biology, Medicine and Health, University of Manchester, Manchester, UK
Nadin Hawwash & Enam Haque
Cancer Research UK Manchester Cancer Research Centre, Manchester, UK
Nadin Hawwash
You can also search for this author in PubMed Google Scholar
Contributions
N.H. and E.H. designed the research study (conceptualisation, methodology, project administration). N.H. wrote the original draft, which was then critically reviewed by E.H. The work reported in the paper has been performed by the authors, unless clearly specified in the text.
Corresponding author
Correspondence to Nadin Hawwash .
Ethics declarations
Ethics approval and consent to participate.
Proportionate ethics approval for this study was granted by the University of Manchester ethics committee (Reference ID: 2022-13648-22673). Only consented participants were included in this study. This study involved minors. Informed consent was obtained from a parent and/or legal guardian for study participation.
Consent for publication
Participants consented for the publication of this study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hawwash, N., Haque, E. Plant a seed series: the impact of an online outreach package on school pupils’ knowledge, skills, and attitudes to medicine. BMC Med Educ 24 , 347 (2024). https://doi.org/10.1186/s12909-024-05300-w
Download citation
Received : 18 December 2023
Accepted : 12 March 2024
Published : 29 March 2024
DOI : https://doi.org/10.1186/s12909-024-05300-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Widening access
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Trending News
Related Practices & Jurisdictions
- Biotech, Food, Drug
- Health Law & Managed Care
- Communications, Media & Internet
- Administrative & Regulatory
- All Federal

Industry Seeks Global Regulatory Certainty and Consistency
AI stands to transform medical product development by creating efficiencies that shrink timelines and costs, and by producing insights. In fact, according to a Berkeley Research Group (BRG) report, the AI health care market is expected to grow by nearly 500% to $187 billion between 2024 and 2030.
However, while regulators in 60 countries, including the European Union, South Korea, the United States, and China, have begun to develop their own regulatory frameworks in response to the rapid proliferation of AI tools, global regulators are attempting to build AI infrastructure and technical expertise. 1 Consequently, while regulatory agencies build their respective AI infrastructures and technical expertise, they should also proactively collaborate with their international counterparts to harmonize these efforts and ensure the responsible use of AI.
FDA Prioritizes AI Use in Development of Medical Products
Following a series of AI-related publications 2 in recent years, on March 15, 2024, the FDA’s Center for Biologics Evaluation and Research (CBER), Center for Drug Evaluation and Research (CDER), Center for Devices and Radiological Health (CDRH), and Office of Combination Products (OCP) (the Centers) jointly published a paper—“ Artificial Intelligence & Medical Products: How CBER, CDER, CDRH, and OCP are Working Together ”—detailing the Centers’ four high-level priorities for a patient-centered, risk-based regulatory approach that strikes a balance between fostering responsible and ethical innovation and upholding quality, safety, and effectiveness. The priorities are listed and elaborated below:
OMB Memorandum Defines Parameters for Advancing Governance, Innovation, and Risk Management for Agency Use of AI
In the paper, FDA also noted its intention to use AI to streamline regulatory processes. However, FDA now must abide by the government-wide policy published by OMB March 28, 2024, that seeks to protect the rights and safety of the public when agencies use AI to inform, influence, decide, or execute agency decisions or actions by:
Opportunities for Agency Engagement and Collaboration
Because AI regulation is in its infancy, stakeholders should dialogue with regulators to inform how FDA crafts its regulatory framework. Stakeholders should be prepared to provide robust information about how AI functions in their medical products and potential limitations to the technology, including monitoring and mitigation of risks related to cybersecurity, bias, safety, transparency, and privacy, among other elements, and AI’s impact on product quality and patient outcomes.
Stakeholders should keep a close eye on regulatory developments in a cross-border context, including any guidance or requests for comment as well as any opportunities to participate in demonstration projects or RFIs. For example, in addition to the planned guidance above, OMB plans to issue proposed regulations relating to responsible use of AI in federal procurement standards later this year. 3 Moreover, at an April 25, 2024, public meeting, FDA plans to release more information about its recently established Quantitative Medicine (QM) Center of Excellence, which will oversee ML and AI approaches. In the meeting, FDA plans to solicit public feedback on education, outreach, and policy needs and to provide an update on the QM Center of Excellence’s status and objectives.
Current Legal Analysis
More from greenberg traurig, llp, upcoming legal education events.

Sign Up for e-NewsBulletins
Inside the ruins of Gaza’s al-Shifa Hospital
GAZA CITY — Gaza’s largest hospital has been gutted. Combat bulldozers have moved sand into the courtyards. The buildings are scorched. It smells like death. Israeli commandos pulled out before dawn on Monday.
A sprawling medical campus that housed maternity wards, surgery suites and emergency rooms has been mostly destroyed after two weeks of intense assault by Israeli troops battling Hamas militants who Israel said were barricading themselves inside the complex.
Spokesmen for the Israel Defense Forces brought a handful of foreign journalists into the compound Sunday afternoon, just hours before the last special forces troops withdrew. A reporter and photographer from The Washington Post were there.
The IDF offered a narrow view — a pinhole, really — but what we saw was destruction on a massive scale. Military censors did not review our words or photos.
It is hard to overstate the importance of al-Shifa , where the dueling narratives of this war have converged.
The hospital has served as a beacon of refuge and resilience for Palestinians. The Israelis described it as a mustering point and command center for terrorists who used the doctors and patients as human shields.
The staff who have toiled at al-Shifa said they just wanted to care for the sick and wounded. “We are doctors: Our job is to treat people. We have nothing to do with this,” said Amr Fawzi Jedbah, a 31-year-old vascular surgeon, who spoke to The Post in the early days of the raid.
As we emerged from the windowless armored personnel carriers that brought us to the site, the first view was sand, and, for a moment, there was silence. Gaza City, more rubble now than city, was quiet.
Then we heard small-arms fire.
The compound smelled of bodies. And rot. Everything that could be broken, smashed or twisted, was, after 14 days of fighting. Dozens of fighters had been killed, the IDF said, but said it could not provide a precise count. Some desperately ill patients had been evacuated; others, aid groups said, died during the siege.
Before this second offensive against al-Shifa, the hospital was still functioning, if just barely, after a first raid by Israel soldiers in November. When the March assault began two weeks ago, there were 6,000 people sheltering on the grounds, according to the IDF — patients, medical staff and displaced families.
On Sunday, we didn’t see a single Palestinian.
In the central quad, there were new sand dunes shaped by bulldozers. Israeli armor and personnel carriers encircled the complex; troops moved quickly from spot to spot.
We were told that Palestinian snipers remained in the area and that a handful of Hamas operatives might still be moving around the hospital buildings, based on night-vision sweeps of the compound.
We saw only Israeli soldiers. In one darkened room, a platoon of commandos slept on the floor beside hallways strewn with trash.
There were sporadic bursts of automatic rifle fire in the distance and what we guessed were heavier rounds being fired. It was unclear who was shooting, or at what.
The Israeli special forces described close-quarter combat with desperate fighters from Hamas who had been taken by surprise and barricaded themselves in emptied hospital wards, including elevator shafts and operating rooms.
The Israelis said two Palestinian militants, in confrontations, used grenades to kill themselves, in what would be the first reported suicide bombings of this latest Gaza war . This could not be confirmed.
We were hustled into a mid-rise medical office building seized by Israeli Navy SEALs, our masked escorts who guided us to the top floors to see the destruction below.
All of the main structures of al-Shifa were blasted and blackened, walls missing, shards of cement flooring pulling against twisted rebar.
These buildings were not pancaked by big bombs, but targeted by Israel’s air force strikes, artillery fire and small arms. The building that housed the Israeli commandos was also pocked by bullet holes and shattered glass.
What the Israeli military described at the outset as a “precise operation” looked more like all-out urban warfare.
We were not given access to the last 140 Palestinians — staff and patients — who the IDF said were sheltering in a nearby building, waiting to be evacuated. The rest of the civilians had already been sent to other medical facilities, the military said, or were told to head south.
“There was no medical care or drinking water or food” for the first three days of the raid, according to Mohamed al-Sikafi, 18, who texted with The Post last Tuesday after making it out of al-Shifa to a nearby hospital, one of the few still functioning in the north. “There are many patients whose health conditions declined.”
Tedros Adhanom Ghebreyesus, the director general of the World Health Organization, wrote on X late Sunday that 21 patients had died at al-Shifa “since the hospital came under siege.” The IDF said no medical staff or patients died as a “direct result” of the Israeli raid, adding that some may have died of “natural causes.”
Reporters were led to an unlit room for a briefing by a top officer in the navy special operations unit called Flotilla 13, one the most secretive in the Israeli forces, famous since the founding of the Jewish state.
Col. “E” — we were not allowed to name him or photograph his face — described his mission: Kill or capture Hamas fighters and spare the innocents.
The colonel said that after the Israeli forces left the hospital after the first raid in November, Hamas fighters streamed back into the complex to take up arms, seek shelter and mix with civilians.
“They go where they know,” the colonel said, suggesting that in bombed-out Gaza City, the al-Shifa complex offered shelter, food, water, electricity and internet service.
Earlier in the war, the IDF made much of the tunnels it found on the hospital grounds. The IDF described a vast underground command and control center, a virtual city. But definitive evidence was lacking . There were clearly tunnels. But where was Hamas?
As it turns out, the Israeli commando colonel stressed that the tunnel system may not have been as important as the IDF once thought. Instead, the colonel said, the Hamas operatives in recent months were working above ground, inside offices and wards. The IDF showed pictures of what it said were cash, rifles, RPGs, grenades, mortars and some Hamas documents found on-site.
Basem Naim, a Hamas official, denied Sunday that militants were using the hospital as a staging ground, telling The Post it was “propaganda to justify the attack on our people.”
“Even if some Hamas members were present in the hospital as refugees,” he continued, “does this justify destroying hospitals?”
Medical staff stated repeatedly that the complex was not used for military purposes. Ghassan Abu Sitta , a British Palestinian doctor who spent several weeks tending to the wounded at al-Shifa late last year, said Monday that his friend and colleague Ahmad Maqadmeh, “a beautiful soul and a great surgeon,” was among the dead.
“He refused to leave the north and kept sending me photos of his surgeries,” Abu Sitta wrote on Instagram. “He leaves behind a wife and baby.”
The Israeli colonel — and the IDF spokesman — both repeated that the al-Shifa offensive represented “a success and a tragedy.”
“It is a success that we struck Hamas so hard, that this was a brutal hit against them, that Hamas now tell us that they are ‘out of business’ in the north,” IDF spokesman Daniel Hagari said. But he said it was a tragedy that Israeli soldiers were “forced” to destroy the hospital buildings.
“We had no choice but to fight back,” said the navy special forces commander.
As the journalists looked out at the destruction, one of Hagari’s officers said, “This is what they made us do.”
Since the beginning of the raid, the IDF said it has detained 900 suspected Hamas fighters and that 540 have been sent to Israel.
How many Palestinian fighters were killed here over two weeks of fighting? The IDF did not provide an exact figure. Hagari said “about 40” were killed inside the hospital compound. The commando leader said “a few dozens.” Another 150 suspected militants were killed in the surrounding area, the military said.
No death toll has been provided yet by Palestinian authorities, who gained access to the site again on Monday as the Israelis withdrew. Mahmoud Bassal, spokesman for Gaza’s Civil Defense, said emergency workers entered the compound at dawn.
“The scene here is one of the ugliest we have seen since October 7,” he said. “The hospital has become completely unfit to be a medical center. The situation is tragic in every sense of the word.”
During the offensive, the IDF said it killed Faiq al-Mabhouh, whom Israel called a commander in the Hamas internal security forces. Hamas said he was a police commander charged with coordinating and protecting aid deliveries.
“They consider that everyone who works with the government in Gaza is a Hamas activist and can be killed or arrested, even doctors, nurses, journalists and civilian police,” said Naim, the Hamas official.
The IDF said it also “eliminated” a senior Hamas official named Ra’ad Tabath, whom it described as a leader of the group’s supply lines.
IDF officers have described the raid at al-Shifa as a model for future action in Gaza: intense but focused strikes by commandos. One question, though, is why such a large and destructive operation was required.
The military claimed in late December that it was close to establishing “full operational control” of northern Gaza. More recently, it said it had “dismantled” Hamas’s battalions in the north. It was only natural, the special forces commander said, that Hamas fighters would regroup around al-Shifa.
Now, he said, there was no hospital left for them to return to.
The journalists piled back in armored personnel carriers for the trip back to Israel. We stopped, without warning, along the way. The soldiers told us they had come across a family of four Palestinians: a mother and father and two children. We could not see them.
The soldiers said the family were in an area where they were not allowed to be. They were offered water and a chocolate bar and then detained, we were told; the father would be closely questioned. Hagari, the military spokesman, told us it was the best course of action.
Had the family proceeded in a no-go zone, he said, the IDF soldiers “could have shot them.”
Miriam Berger in Jerusalem, Hajar Harb in London and Hazem Balousha in Amman, Jordan, contributed to this report.
Israel-Gaza war
Israel-Gaza war: Israeli Prime Minister Benjamin Netanyahu said Tuesday that Israel’s military struck civilians in the Gaza Strip in a “ tragic incident ” after the aid organization World Central Kitchen said seven of its workers were killed while distributing food. Meanwhile, an airstrike near Iran’s embassy in Syria’s capital killed a senior Iranian commander and several Iranian diplomats, according to Tehran’s state media, which said it was an Israeli attack.
- Israeli military says strikes that killed Gaza aid workers were ‘grave mistake’ Earlier today Israeli military says strikes that killed Gaza aid workers were ‘grave mistake’ Earlier today
- Israeli strike on Iranian Consulate in Damascus kills key commander, Iran says April 1, 2024 Israeli strike on Iranian Consulate in Damascus kills key commander, Iran says April 1, 2024
- Inside the ruins of Gaza’s al-Shifa Hospital April 1, 2024 Inside the ruins of Gaza’s al-Shifa Hospital April 1, 2024


IMAGES
VIDEO
COMMENTS
McAlister et al. analyzed review articles in 6 medical journals, and disclosed that in less than one fourth of the review articles, methods of description, evaluation or synthesis of evidence had been provided, one third of them had focused on a clinical topic, and only half of them had provided quantitative data about the extend of the ...
How to write and review a review article. In 2016 David Cook wrote an editorial for Medical Education on tips for a great review article. 13 These tips are excellent suggestions for all types of articles you are considering to submit to the CMEJ. First, start with a clear question: focused or more general depending on the type of review you are ...
A review article can also be called a literature review, or a review of literature. It is a survey of previously published research on a topic. It should give an overview of current thinking on the topic. And, unlike an original research article, it will not present new experimental results. Writing a review of literature is to provide a ...
This article presents guidelines for writing an evidence-based clinical review article for American Family Physician. First, the topic should be of common interest and relevance to family practice ...
A good review article provides readers with an in-depth understanding of a field and highlights key gaps and challenges to address with future research. ... within the biological sciences. Its sister site, medRxiv, hosts preprints within the medical sciences. Owned by Cold Spring Harbor Laboratory. Identifying the most important references is a ...
Scientific review articles are common in the medical literature and can serve as definitive references on the topic for other scientists, clinicians, and trainees. The first step in the process of preparing a scientific review article is to select a focused topic. This step is followed by a literature search and critical analysis of the ...
To write an article of any sort is, to some extent, to reveal ourselves. Hence, even a medical article is, in a sense, something of an autobiography. American surgeon J. Chalmers DaCosta (1863-1938) [ 1] Many respected academicians write review articles, for both subscriber-based and controlled-circulation journals .
The best proposals are timely and clearly explain why readers should pay attention to the proposed topic. It is not enough for a review to be a summary of the latest growth in the literature: the ...
The review article is the Rodney Dangerfield of medical writing. Review articles get no respect. Yet, surprisingly, many respected academicians write review articles, for both subscriber-based and controlled-circulation journals. Why do they do so? The answer is that, by writing review articles,
The New England Journal of Medicine (NEJM) is a weekly general medical journal that publishes new medical research and review articles, and editorial opinion on a wide variety of topics of ...
Traditional clinical review articles, also known as updates, discuss a topic broadly and selectively review the medical literature. An excellent structured clinical research article will resolve controversy generated by studies that contradict one another. Before knowing how to structure a clinical review article, you have to know some ...
Three recent articles [1-3] on the seemingly very similar topic of coexistence of anxiety and depression are a case in point of the lack of clarity of what a review article is and what its attributes and goals are The first one by Saha et al. [1] is a systematic review and meta-analysis which "found robust and consistent evidence of comorbidity between broadly defined mood and anxiety disorders.
Takeaway. A systematic review is a form of analysis that medical researchers carry out to synthesize all the available evidence on a particular question, such as how effective a drug is. A meta ...
Peer review is a quality control measure for medical research. It is a process in which professionals review each other's work to make sure that it is accurate, relevant, and significant ...
Review Article 11 Aug 2022. The promise of precision medicine in rheumatology. Precision medicine for rheumatic diseases is still in its infancy, but recent advances are enabling comprehensive ...
Review Article. Mechanisms of long COVID: An updated review. Author links open overlay panel Yan Liu 1 2 #, Xiaoying Gu 3 #, Haibo Li 1, Hui Zhang 1 4, Jiuyang Xu 1. Show more. Add to Mendeley. ... Post-COVID medical complaints following infection with SARS-CoV-2 omicron vs delta variants. Nat Commun, 13 (2022), p. 7363, 10.1038/s41467-022-35240-2.
This narrative review describes a new approach to the diagnosis and treatment of psychiatric disorders that is based on dynamical systems theory, which addresses the concepts of tipping points, cycles, and chaos in complex systems.
Blood Sugar Levels: The tests are conducted to assess the glucose levels in the body, which is very important to diagnose and manage diabetes. Electrolytes: The levels of sodium, potassium, bicarbonate, chloride. These are crucial for maintaining balance and nerve function in the body. Liver Function Tests: They help assess liver function.
It further ventures into the frontier of SeNPs functionalization, illuminating prospects for precision-targeted drug delivery. Conclusively, the review furnishes a comprehensive elucidation of the intricate therapeutic mechanisms harnessed by SeNPs, charting a blueprint for the future of personalized medical interventions.
Medical care costs are up 30% in the past decade — here's what it means for Americans Incredible Health analyzed the increasing costs of medical care and its contributing factors, referencing ...
Medicine is one of the most inaccessible professions in the United Kingdom (UK). The Plant a Seed (PAS) series was created to address this; it is an online pre-recorded three-part video series to "Inspire", "Educate" and "Motivate" pupils from widening participation backgrounds on Medicine. We explored the impact of PAS on pupils' knowledge, skills and attitude to Medicine.
The U.S. Food and Drug Administration (FDA) has outlined its plan to regulate artificial intelligence (AI) in medical products, including building its AI infrastructure and technical expertise ...
A sprawling medical campus that housed maternity wards, surgery suites and emergency rooms has been mostly destroyed after two weeks of intense assault by Israeli troops battling Hamas militants ...