183 Schizophrenia Essay Topics & Examples
Welcome to our list of schizophrenia essay topics! Here, you will discover the most interesting research topics on schizophrenia, project ideas to write about, and titles for argumentative papers. Check them out below!

🔝 Top 10 Schizophrenia Research Topics for 2024
🏆 best schizophrenia topic ideas & essay examples, 👍 good essay topics on schizophrenia, ⭐ simple & catchy schizophrenia titles, 💡 interesting topics research topics on schizophrenia, ❓ research questions about schizophrenia, 🎓 schizophrenia research questions for dissertations, ✅ schizophrenia project ideas for students.
- Brain Abnormalities in Schizophrenia
- Risk Factors of Adolescent Schizophrenia
- Cognitive Impairment in Schizophrenia Patients
- Family Support in Schizophrenia Management
- Ways of Enhancing Social Skills in Schizophrenia
- Schizophrenia and Comorbid Medical Conditions
- Early Detection and Intervention in Schizophrenia
- Genetic and Environmental Factors in Schizophrenia
- The Relationship between Schizophrenia and Substance Use
- Efficacy of Antipsychotic Medicines and Side Effects
- Schizophrenia: An Informative View It discusses the symptoms of the disorder, the cause, and the impact it has on both the individual suffering from it and the people surrounding the victim, both within and outside the family unit.
- Schizophrenia Explained by “A Beautiful Mind” It is a disease which can emotionally devastate the [patient as well as the relatives and the loved ones of the patient causes the patients to have hallucinations as well as delusions and even in […]
- The Movie “A Beautiful Mind” and Display of Schizophrenia This paper offers an in-depth analysis of the movie A Beautiful Mind to ascertain its display of schizophrenia as well as societal and cultural attitudes towards the disorder.
- Schizophrenia in ‘A Beautiful Mind’ Film The main symptom of a schizophrenic patient depicted in the film is the patient’s inability to distinguish between the real world and the subconscious pattern created within the imaginations of his mind.
- The Current Concept of Schizophrenia Is Neither Valid and Useful The primary research question is ‘Is the current concept of schizophrenia valid and useful?’ Hence, it is crucial to evaluate the empirical basis to answer the question and discuss the alternative system.
- Schizophrenia in The Center Cannot Hold by Elyn Saks Nevertheless, in college, Saks faced stress due to the need to study, communicate, and care about herself and was left without the support of the Center, which led to the first episode of acute psychosis.
- Paranoid Schizophrenia in “A Beautiful Mind” The film A Beautiful Mind depicts the impact of progressive paranoid schizophrenia on the mathematician John Nash and the burden that it places on social and personal relationships.
- Schizophrenia: Case Analysis Paper The purpose is to inform the reader about a comprehensive case study with a schizophrenia diagnosis and the rationale for a nursing care plan.
- Freud’s Psychoanalysis for Schizophrenia Patients In this paper, the author’s approaches to this ailment are considered, and the ways of applying the specific observations of human behavior are discussed. Freud’s contribution to the development of psychoanalysis is significant, and his […]
- Schizophrenia and the Reduction of Readmissions Thus, this research will be rather useful because it will discuss the effectiveness of self-management programs for people with schizophrenia and their influence on the reduction of readmissions.
- Schizophrenia and Its Functional Limitation The situation advances in severity with the age of the patient. This condition may affect work, social, training, and interpersonal relations and skills among people with the schizophrenia condition.
- Schizophrenia Patients Using Atypical Medication The research procedure follows a timed experiment with several trials beginning with a fixation point displayed in the middle of the black rectangle. A participant’s task is to identify accurate locations of the stimuli after […]
- Schizophrenia and Its Effects on the Brain This shows that functional variations are not a product of long consequences of the condition or therapy for the disorder, just like the structural alterations in gray matter and white matter.
- Negative versus Positive Symptoms of Schizophrenia Schizophrenia is a condition that hinders the ability of a person to think, feel, and act. In Schizophrenia, a decrease or absence of normal motivational and interest-related behaviors or expressions are referred to as negative […]
- The Brief Psychotic Disorder, Schizophreniform Disorder, and Schizophrenia People with “delusions, hallucinations, and disorganized behavior, with a return to normal functioning over a short time span” are diagnosed with a brief psychotic disorder.
- Schizophrenia and Schizoaffective Disorder He is calm and cooperative. There is no evidence of any suicidal or homicidal ideation, and he denies them as well.
- Schizophrenia: Causes and Symptoms People with this condition can live full lives and perform independently because of the accessibility of medicine, counseling, and support. Additionally, the ideal way to perceive Schizophrenia is when it is promptly diagnosed and treated.
- Schizophrenia: Neurochemical Theories and Medications The dopamine theory regarding schizophrenia, the serotonin theory of depression, and the glutamate theory will get discussed in detail in this paper. The dopamine hypothesis of schizophrenia holds that the overall neurotransmitters associated with dopamine […]
- Schizophrenia and Bipolar Disorder Portrayal in Mass Media Thus, the portrayal of the disorder in the media is the mix of symptoms that belong to bipolar I and II disorders in the textbook.
- Indian, Chinese, and American Approaches to Treating Schizophrenia Thus, the perception of mental illnesses in Chinese traditional medicine should be discussed it will benefit the patients and reduce the destructive effects such disorders as schizophrenia may have on one’s life.
- Health Information: Schizophrenia The critical components that I used to evaluate the sites are the owners, mission, references, and information review. The benefits of WebMD are that it mentions the author’s name and the person who medically reviewed […]
- Schizophrenia Spectrum and Psychosis Disorders Management The psychopharmacology of risperidone shows the correlation between the drug’s impact on the brain and the behavior of patients. The FDA addresses the management of risperidone based on its class and its mechanism of action.
- Plan for Management of Patient with Schizophrenia and Heart Disease About 1% of the world’s population suffers from schizophrenia About 0. 7% of the UK population suffers from schizophrenia Schizophrenia can manifest any time from early adulthood onwards, but rarely when a person is below […]
- Quality of Life With Schizophrenia The main difference between the former and new guidelines in patients’ professional and personal life will only be that people with schizophrenia will have to consider the symptoms of their illness and maintain a distance […]
- Schizophrenia: The Etiology Analysis Disrupted epigenomic regulation in response to environmental triggers leads to decreased brain function and the onset of schizophrenia. The Khavari & Cairns, article focuses on the epigenomic factors that contribute to the development of the […]
- Schizophrenia as a Chronic Mental Disorder The first signs of the disease began to appear at the age of 28, which, according to his friend, coincided with the patient’s loss of a loved one.
- Schizophrenia and Its Effects on the Lives of Patients Schizophrenia is a mental disorder that affects the lives of patients diagnosed with the condition on multiple levels, as evident from the individual in question.
- Schizophrenia Diagnostics and Its Challenges In addition to the core symptoms of hallucinations, delusions, or persistent disorganized speech, schizophrenia may be manifested through psychosis, which accounts for the majority of acute admissions to the inpatient setting.
- Schizophrenia: Symptoms and Therapy Schizophrenia is a complex condition involving a number of cognitive, behavioral and emotional symptoms, all of which can present differently depending on the person. In addition, there are a number of symptoms that can help […]
- Schizophrenia Disorder: Definition, Treatment, and Medication Schizophrenia is linked to anatomical and functional alterations in the pallium, the layer of the unmyelinated neurons, as well as variations in the networks in the middle of cortical areas.
- Schizophrenia: Cause, Consequence, Care Considering the assessment above, the diagnosis of paranoid schizophrenia can be established due to Caroline’s concerns about being a target for her social environment.
- Social Risk Factors for Schizophrenia However, genetic predisposition is not the only risk factor for psychoses in general and schizophrenia in particular. One of them is possibly social isolation, as most patients used to be somewhat reserved in their childhood […]
- Analysis of Article Related to Schizophrenia Treatment The objective of the study is to evaluate the effectiveness and safety application of cannabidiol as an adjunctive treatment for patients with schizophrenia.
- Neuroscience: Schizophrenia and Neurotransmitters From the definition of neurotransmitters, it is clear that schizophrenia is caused by the irregular functioning of neurotransmitters. Physical abnormalities in the brain have been suspected to be causes of schizophrenia.
- Treatment Plan For Schizophrenia Patient Bill will fully recover and be in a position to perform the activities of the daily living on his own. Bill complies with the treatment regimen because treatment will help him recover and be in […]
- Mental Health: Analysis of Schizophrenia In the early years, signs related to the disease were said to be resulting from possession of evil spirits. The history of development in respect to mental health can be traced to antiquity.
- Paranoid Schizophrenia: Psychosocial Rehabilitation The behavior of being a social loner is reinforced by the indoor equipments that motivate his stay in the house. Barhof et al, explains that recognition of the value or importance of change is wholly […]
- Principles and Practice of Psychosocial Rehabilitation: Schizophrenia The objective of this study was to evaluate the literature accumulated so far and address the issues surrounding the principles and practice of Psychosocial Rehabilitation.
- Schizophrenia and Primary Care in Britain The illness causes distress in the form of severe suffering for the patient, his family and friends. The annual costs for care and treatment of schizophrenia in the United Kingdom in the 1990s were 397 […]
- Impact of Drug Use on Schizophrenia and Its Treatment The basis for the behaviors exhibited by schizophrenics, described in particular in the current case: paranoia, severe excitation coupled with periods of gloom and darkness, and a desire to commit suicide, are signs of drug […]
- The Schizophrenia Drugs: Lithium and Abilify Lithium overdose affects primarily two systems of the human body: the central nervous system and the kidneys since it is through the latter that the drug is excreted from the body.
- Collaborative Care in a Schizophrenia Scenario For example, the social worker will be in a position to emphasize the human dimensions of the problem, such as Simon’s preferences and social aspirations.
- Alcoholism and Schizophrenia: Interconnection In addition to its physical effects on the chronic drinker’s body, alcohol is associated with a variety of mental impairments. Alcoholic dementia and Wernicke-Korsakoff syndrome are among the most prominent concerns in the matter. The former is a blanket term for a variety of cognitive deficiencies caused by the substance. The latter is a two-stage […]
- “Schizophrenia: A Sibling’s Tale” by Stephan Kirby The primary purpose of this article seems to inform the readers about the effective strategies that can be implemented in order to help the families of the affected people to go through a number of […]
- Schizophrenia and Workplace Behaviors Besides, their condition and performance at work may be significantly improved in case of a proper help from the company’s leadership.
- Schizophrenia and Health Strategy Proposal The use of qualitative analysis is thus justified, since the amount of detail and quality of information required would only be provided using this method.
- Schizophrenia and Biological Therapeutic Approach The level of social stigma associated with this condition has been identified as a major obstacle to the recovery of patients from this condition.
- Schizophrenia: An Abnormal Human Behavior Despite there not being a cure for the disorder as yet, there are current treatments available and meant to eliminate the majority of symptoms associated with the disorder thus enabling such individuals to live healthy […]
- Schizophrenia & Neurosis and Lifespan Development The learning objectives are to comprehend worrying conduct in the scope of the growth missions, series, and procedures that show human development.
- Schizophrenia Diagnostic Assessment As is mentioned above, the client does not understand or is not able to see the original appearance of objects and people around her.
- Analyzing Psychological Disorders: Schizophrenia Nevertheless, the damage to the brain as a result of this disorder seems to target two main areas: the frontal lobe, and the parietal cortex.
- Schizophrenia Study and Rehabilitation Outcome In fact, the results of this prospective study can reasonably be projected to the universe of Germans with mental disorders only if Rehabilitation Psychisch Kranker in the city of Halle is a kind of secondary […]
- Theme of Schizophrenia in “Slaughterhouse-Five” by Kurt Vonnegut The Tralfamadorian subplot includes a vision of the end of the world and the perpetuation of war, but these seem distant threats compared with the miseries of battlefield.
- Schizophrenia in Adults: Causes, Diagnosis, and Management Among the usual characteristics of schizophrenia is low motivation; which consequently makes the victim withdraw from other members of the society.”Although studies have shown that, women are equally likely to develop the mental disorder as […]
- Schizophrenia Causes, Symptoms, and Risk Factors This paper aims to research and analyze the causes, symptoms and the risk factors associated with the mental disease and discuss some of the prevention measures of the disease.
- Haldol and Negative Symptoms of Schizophrenia Very often this disease is treated with the help of haloperidol, a kind of injection used as a medicine against brain disorders and psychotic states.
- Schizophrenia: The Role of Family and Effect on the Relations The role of family members and other social support is essential and form part of the management of this illness. The illness causes the others in the family to have stress.
- Schizophrenia as a Common Mental Disorder Before a patient is diagnosed to have schizophrenia, the person must have two or more of the following symptoms for at least a month according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth […]
- Delusional “Pseudotranssexualism” in Schizophrenia But it was in the middle of the twentieth century that the name transsexualism was fixed for this disorder for the first time by Cauldwell and after a few years Benjamin in the US and […]
- Schizophrenia Symptoms, Etiology, and Treatment The treatment as well as the prognosis for recovery is highly dependent on the stage in which schizophrenia is diagnosed and the age of first onset.
- Schizophrenia Causes and Treatment Analysis There exist several theories about the causes of schizophrenia, the most convincing of them are: the theory of genetic predispositions, the theory of prenatal or vital antecedents and the theory of social and environmental causes.
- Schizophrenia: Characteristics, Types and Symptoms This disease is a type of brain disease which if remain unnoticed affects the entire personality and life of the patient.
- Schizophrenia: Biological & Environmental Causes The indications of schizophrenia are varied but the results are the same, causing a breakdown of individuality and the consequent inability of the personage to purpose in reality.
- Schizophrenia and Its Special Symptoms Talking to the patients in a way that could enhance their hopes in life and activities they usually engage in is one way of reducing patients’ overwhelmed, as well as keeping them with the hope […]
- Can Cannabis Cause Schizophrenia? Regarding this assignment, I am going to address the importance of this topic in the field of addiction and healthcare, assessing the research that suggests that cannabis plays a role in schizophrenia and the strengths […]
- People With Schizophrenia Diagnosis in Prisons As a result, the behavior of the individuals with the condition is a threat to the members of the family and the society.
- Schizophrenia Symptoms and Treatment Complications Schizophrenia is one of the most complex examples of these disorders because it leads to the inability to live independently and hold a job.
- Schizophrenia: History and Diagnosis The process of diagnosing involves a comprehensive assessment of the patient’s symptoms, in which a specialist searches for the symptoms of schizophrenia and other disorders, which need to be ruled out for the diagnosis to […]
- Schizophrenia Diagnosis, Planning and Treatment Peter is 18 years old He lives at home with his parents. The patient has gained 20 pounds without any diet changes His glucose is at 145 He has not been taking his Olanzapine […]
- Schizophrenia Research: Ethical Principles and Steps The issue of beneficence is also put into consideration to ensure the research is done to improve the well being of the subjects and the society at large.
- Prevention of Suicide in People with Schizophrenia As a strategy to prevent suicide in schizophrenic patients, the drugs are aimed at controlling the symptoms associated with the condition.
- Readmissions in Schizophrenia and Reduction Methods After this, the regression model will be developed applying the variables associated with predictors of readmission and the dichotomous variable as the outcome.
- Schizophrenia Therapy: “People Matter” by Marley The study indicates how the targeted respondents supported the “use of different interpersonal interactions towards reducing the symptoms associated with schizophrenia”. This author supports the use of interpersonal interactions in every patient with schizophrenia.
- Schizophrenia Effects on Patient Development This essay explores schizophrenia in a bid to understand what it really is, how it affects the development and relational abilities of its victims, and why these effects qualify it as a mental disorder.
- Courtesy Stigma: Relatives of Schizophrenia Patients The quota sampling method was used in the research survey. In regards to the analytic strategy, the inductive formation of categories was used to analyze the transcripts.
- Schizophrenia Symptomatology and Misdiagnosis Although it was previously believed that the incidence and prevalence of schizophrenia in men and women were approximately the same, newer studies point out that the use of more restrictive criteria for diagnosis results in […]
- Schizophrenia and Cognitive Therapy Interventions The onset of the mental disorder usually occurs in the first half of life; however, many episodes of schizophrenia have been registered beyond the age of 60 years.
- Schizophrenia and Bipolar Disorder in Children and Adolescents It is acknowledged by the researchers that the symptoms indicate the possibility of bipolar disease and not schizophrenia. Psychiatric and physiological factors, among others, contribute to the prevalence of self-harm in children and young people.
- Schizophrenia Drugs’ Mechanism of Action In the case of M.Y.is can be useful to prescribe a second-generation antipsychotic, and if it proves to be ineffective, clozapine can be used.
- Schizophrenia Treatment: 25-Year-Old Male Patient The symptom of social isolation also contributes to the development of schizophrenia in Mr. Dashiell to identify the cause of the condition.
- Schizophrenia Hypothesis and Treatment The dopamine theory hypothesizes that the activation of post-synaptic dopamine receptors in the mesolimbic pathway of the brain increases dopaminergic activity, resulting in positive symptoms delusions and hallucinations.
- The Diagnostic Concept of Schizophrenia Cultural and historical contexts have largely influenced the perception of this mental disorder, and the assessment of this disease and its features in different cultures is not the same.
- Schizophrenia: Diagnosis and Treatment Approaches A detailed analysis of the factors that affect the patient’s condition, including the internal and the external ones, must be mentioned as one of the essential strengths of the studies that have been conducted on […]
- Schizophrenia in Young Men and Women Thus, the research of the problem among the young people is the primary task. The feelings of people with schizophrenia are contradictory and uncertain.
- Paranoid Schizophrenia in “A Beautiful Mind” Movie John Nash is the protagonist in the movie, A Beautiful Mind. The movie did a good job of depicting the disorder in John Nash.
- Schizophrenia, Ethical and Multicultural Issues For instance, the assumption that the absence of evidence implies the same outcomes as the actual absence of the disorder symptoms often hinders the process of determining and addressing schizophrenia in patients.
- Schizophrenia, Its Symptoms, Prevalence, Causes Noteworthy, hallucinations and delusions are reflections of the distortions of the human mind, which in turn causes distortions of the person’s perceptions and interpretations of reality.
- Pharmacological & Psychotherapeutic Schizophrenia Interventions The use of clozapine is a medical intervention that targets the biological functioning of patients by blocking serotonin receptors and thus bringing about the release of dopamine receptors in specific parts of the brain.
- Schizophrenia Effects on Patient, Caregiver, Society The purpose of this paper is to discuss the effects of schizophrenia on the victim, caregiver, as well as the society.
- Self-Management Programs for Schizophrenia Therefore, the significance of the problem that is reviewed in this paper consists in the fact that the approaches to the treatment of schizophrenia can be optimized.
- Schizophrenia and Frequent Readmission Rates This literature review is focused on the exploration of self-management programs for patients with schizophrenia and their effectiveness in terms of the reduction readmission rates and the overall management of the condition.
- Schizophrenia and Self-Management Programs In order to collect the data for further analysis that will help to answer the defined research question, it will be necessary to conduct the study allowing the researchers to track changes in behavior and […]
- Schizophrenia Readmissions Reduction: Data Analysis A simple random sampling technique will be used to select participants, and it implies that each respondent will be randomly chosen to take part in the study to avoid bias and ensure the validity of […]
- Readmission Rates in Schizophrenia Patients The purpose of this paper is to propose a research analyzing the frequency of admission rates among patients with schizophrenia treated with long-acting injectable antipsychotics or with oral antipsychotics.
- Eating Disorders, Insomnia, and Schizophrenia Of course, this readiness does not exclude the necessity to identify such people and provide the necessary treatment to them, which is proved to be effective.
- Schizophrenia as an Extreme Form of Schizotypy The use of Meehl’s model to expose extreme forms of schizotypy as a manifestation of schizophrenia also informs the findings of this paper. Nonetheless, the similarities between schizophrenia and schizotypy do not show that one […]
- Schizophrenia: Psychiatric Evaluation and Treatment Plan The purpose of this paper is to examine the symptoms characteristic for Oscar in order to determine whether it is necessary to conduct the psychiatric evaluation for the young man and propose the plan of […]
- Schizophrenia – Mental Health Disorder The neurotransmitters at the ending of the nerve cells transmit messages from one area to another nerve cell in the body.
- Schizophrenia: Symptoms and Treatment The positive symptoms of the disease incorporate hallucinations associated with hearing, illusions, and disordered language and behavior. The symptoms of schizophrenia captured in the DSM IV TR includes illusions, hallucinations, and disordered language.
- Undifferentiated Schizophrenia: Sally’s Case Sally could have inherited some patterns of the disease from her maternal grandfather and her mother’s continued smoking patterns and flu during her pregnancy.
- Schizophrenia Patients Biochemical and Behavioral Changes It is also important to note that microscopic studies on the tissues of brain have shown slight variations in the number of cells of the brain and their distribution patterns. Biochemical changes in the brain […]
- Schizophrenia and Delusional Disorder For example, a range of scholars have attempted to identify schizophrenia and the delusional disorder as phenomena. Therefore, the instances of delirium must be viewed as possible indicators of schizophrenia.
- Psychiatric Issues: Schizophrenia’s Demystify The web is an internet community that is dedicated to the provision of high-quality data, elucidation, and assistance to the kin, providers, and persons that have been impacted by the condition.
- Non-Clinical Indicators in Patients with Schizophrenia The collaboration between the clinicians and the family is beneficial to the patient especially in administering the daily routines of the patient.
- Schizophrenia: Pathophysiology and Treatment The treatment methods commonly in the application are based on a clinical research that has been conducted on the disease as well as on the experience of the physician on the treatment of the disease.
- Schizophrenia: Description, Development and Treatment According to Van Dyke, schizophrenia begins to develop in the early adulthood years of the victim from the age of 15 to 30 years.
- A Critical Examination of the Link between Nicotine Dependence and Schizophrenia Over the years, there have been strong indications that heavy cigarette smoking can be linked to schizophrenia and that smoking may have a connection to the neurobiology of schizophrenic illness.
- Schizophrenia Genetic and Environmental Factors The research paper explores schizophrenia by providing a general overview, a comprehensive discussion of clinical synopsis, genetics and environmental factors in relation to schizophrenia, limitations of the methods of analyses, and a clear demonstration of […]
- Childhood Schizophrenia: Causes and Management of This Mental Disorder Hardman et al.are of the view that the risk of a child suffering from this condition is one percent when there are no recorded cases of the condition in the family.
- Dimensional Approaches to Schizophrenia and their Inclusion in the DSM-V The inclusion of the dimensional diagnosis of schizophrenia and other disorders to DSM-V will help to avoid some of the problems that are currently faced by the system.
- Smoking as Activity Enhancer: Schizophrenia and Gender Once learning the effects which nicotine has on people’s health and the relation between gender and schizophrenia, one can possibly find the ways to prevent the latter and to protect the people in the high-risk […]
- Clinical and Neuropsychological Characteristics in Subjects With Schizophrenia The need to understand the complex interplay between a number of variables, including genetics, environmental factors, clinical, psychological and social processes, in the development of brain disorders and the resultant behavioural and cognitive deficiencies informed […]
- Psychological Classification of Schizophrenia The paper is composed of a matrix that gives detailed information on the major DSM IV-TR categories of schizophrenia and psychosis, and lifespan development as well as the various classifications of schizophrenia and psychosis, and […]
- Cognitive Behavioural Therapy in Schizophrenia The basic idea in cognitive therapy is the fact that the cognitive aspect of esteem, the way we perceive problems, the world, and other mundane aspects of life like expectations and beliefs are chief determinants […]
- Schizophrenia a Psychological Disorder The main purpose of this research study was to investigate the relationship between Schizophrenia and reading impairments that are usually experienced by individuals when assessed in terms of Oculomotor Control and phonological Processing The research […]
- Homelessness and Schizophrenia It is essential to consider that lack of a proper home can exert pressure in an individual, to the extent of mental burdening.
- Should Persons Suffering From Schizophrenia Be Forced to Take Medications? Though many studies have pointed out that its causes are poorly understood, Dora is of the view that it results from the interplay of the immediate environment that a person is exposed to and the […]
- A Beautiful Mind: Understanding Schizophrenia and Its Impact on the Individual and the Family The psychological disorder presented in the movie refer to one of the most common of schizophrenia paranoia. The disorder, however, is still subjected to experimental treatments by means of medications and psychotherapy.
- Bipolar Disorder and Schizophrenia Genetically, an alteration in the serotonin, dopamine and glutamate genes may be the cause of the disease. Therefore, the close interactions of genetic, psychological and environmental factors lead to severe cases of bipolar disorder.
- Schizophrenia, Psychosis and Lifespan Development Schizophrenia is a complicated condition not only due to its nature but also due to the fact that it results from a wide range of factors.
- Diagnosis and Treatment of the Schizophrenia The prevalence rate of the disease is around 1% in the whole world and despite the fact that its rate is higher among the poor; there is no much difference from one culture to another. […]
- Physical Health and Its Relations to Schizophrenia Smith is the fact that the disease got him at a time in life when he wanted to settle in marriage and due to the changes brought about by the mental disorder, he lost his […]
- Neurological Disorder: Effects of Schizophrenia on the Brain and Behavior Furthermore, as identified earlier, the neurological basis of the disorder may also involve abnormalities in the structure of the forebrain, the hindbrain and the limbic system.
- What Makes Schizophrenia One of the Worst Mental Illnesses?
- Are Bipolar Disorder and Schizophrenia Neuroanatomically Distinct?
- What Predicts Stigmatization About Schizophrenia?
- How and Why Affective and Reactive Virtual Agents Will Bring New Insights on Social Cognitive Disorders in Schizophrenia?
- What Do Visual Illusions Teach Us About Schizophrenia?
- Can Neurostimulation Prevent the Risk of Alzheimer’s Disease in Elderly Individuals With Schizophrenia?
- How Can Nurses Deal With a Patient With Paranoid Schizophrenia?
- What Is Connection Between Schizophrenia and Social Isolation?
- Are Continuum Beliefs About Psychotic Symptoms Associated With Stereotypes About Schizophrenia?
- What Is the Link Between Drug Addiction and Underdiagnosed Schizophrenia?
- How Does Gray Matter Effect Schizophrenia and Bipolar?
- What Is Schizophrenia Disorder?
- Can N-Methyl-D-Aspartate Receptor Hypofunction in Schizophrenia Be Localized to an Individual Cell Type?
- How Should People With Schizophrenia Be Treat?
- Are Patients With Schizophrenia Impaired in Processing Non-emotional Features of Human Faces?
- How Does Schizophrenia Affect Development and Aging?
- Did Andrea Yates Have Schizophrenia?
- How Does Schizophrenia Affect the Lifespan?
- Are Patients With Schizophrenia Spectrum Disorders More Prone to Manifest Nocebo-Like-Effects?
- How Does the Environment Influence Schizophrenia and Possible Prevention?
- Does Co-morbid Obsessive-compulsive Disorder Modify the Abnormal Language Processing in Schizophrenia Patients?
- How Will the Mild Encephalitis Hypothesis of Schizophrenia Influence Stigmatization?
- Are People With Schizophrenia Dangerous and Unpredictable?
- Does Non-adherence Increase Treatment Costs in Schizophrenia?
- What Are the Major Main Barriers to Treatment of Schizophrenia?
- Is Schizophrenia an Incurable Mental Illness?
- How Do Genetic Factors Contribute to the Development of Schizophrenia?
- Is Any Particular Race More Vulnerable to Schizophrenia?
- How Does Schizophrenia Affect People Who Live In States That Opted Out of the State Healthcare Exchanges?
- Is Schizophrenia a Genetically Transmittable Illness?
- How Do Environmental Factors Contribute to the Development of Schizophrenia?
- What Are the Most Effective Pharmacological Interventions for Managing Positive and Negative Symptoms of Schizophrenia?
- How Does Early Intervention Impact the Long-Term Outcomes of Individuals with Schizophrenia?
- What Are the Most Common Cognitive Deficits Experienced by Schizophrenia Patients?
- How Can Dual Diagnosis Treatments for Substance Use and Schizophrenia Be Optimized?
- What Are the Treatment Considerations for Managing Schizophrenia in Young Adults?
- How Can Family Psychoeducation and Support Programs Help Improve Treatment and Outcomes in Schizophrenia?
- What Are the Social Functioning Difficulties Faced by Individuals with Schizophrenia?
- How Can Holistic Care Approaches Help Address Physical Health Comorbidities Associated with Schizophrenia?
- How Can Neuroimaging and Brain Research Advancements Contribute to Our Understanding of Schizophrenia?
- A Multimedia Presentation Explaining the Neurobiological Basis of Schizophrenia
- An infographic that Educates the Public about Early Warning Signs and Symptoms of Schizophrenia.
- A Survey Assessing the Awareness and Understanding of Schizophrenia in the School Community.
- Video Simulation Demonstrating the Experiences of Individuals Living with Schizophrenia
- Plan of a Mental Health Awareness Event to Reduce the Stigma Surrounding Schizophrenia
- Research Paper on the Impact of Family Support on Improving Outcomes of Schizophrenia Patients
- Interviews with Schizophrenia Patients and Their Families
- A Classroom Presentation on the Connection Between Creativity and Schizophrenia
- Literature Review on the Effectiveness of Cognitive Remediation Interventions for Schizophrenia
- Mental Health Awareness Campaign Focused on Schizophrenia
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, February 29). 183 Schizophrenia Essay Topics & Examples. https://ivypanda.com/essays/topic/schizophrenia-essay-topics/
"183 Schizophrenia Essay Topics & Examples." IvyPanda , 29 Feb. 2024, ivypanda.com/essays/topic/schizophrenia-essay-topics/.
IvyPanda . (2024) '183 Schizophrenia Essay Topics & Examples'. 29 February.
IvyPanda . 2024. "183 Schizophrenia Essay Topics & Examples." February 29, 2024. https://ivypanda.com/essays/topic/schizophrenia-essay-topics/.
1. IvyPanda . "183 Schizophrenia Essay Topics & Examples." February 29, 2024. https://ivypanda.com/essays/topic/schizophrenia-essay-topics/.
Bibliography
IvyPanda . "183 Schizophrenia Essay Topics & Examples." February 29, 2024. https://ivypanda.com/essays/topic/schizophrenia-essay-topics/.
- Abnormal Psychology Paper Topics
- Mental Disorder Essay Topics
- Developmental Psychology Essay Ideas
- Bipolar Disorder Research Ideas
- Dissociative Identity Disorder Essay Topics
- Mental Health Essay Ideas
- Cognitive Dissonance Research Topics
- BPD Research Ideas
- Mental Illness Research Topics
- Cognitive Psychology Topics
- Neuropsychology Topics
- Cognitive Therapy Essay Topics
- Psychopathology Paper Topics
- Cognitive Behavioral Therapy Topics
- Therapeutics Research Ideas

Presentations made painless
- Get Premium
108 Schizophrenia Essay Topic Ideas & Examples
Inside This Article
Schizophrenia is a complex and often misunderstood mental disorder that affects millions of people worldwide. As a student studying psychology or mental health, you may be tasked with writing an essay on schizophrenia. To help you get started, we have compiled a list of 108 schizophrenia essay topic ideas and examples to inspire your writing.
The history of schizophrenia research and treatment
The prevalence of schizophrenia in different populations
The genetic and environmental factors that contribute to schizophrenia
The role of neurotransmitters in the development of schizophrenia
The impact of schizophrenia on brain structure and function
The stigma associated with schizophrenia and its effects on individuals
The relationship between schizophrenia and substance abuse
The challenges of diagnosing schizophrenia in adolescents
The effectiveness of antipsychotic medications in treating schizophrenia
The benefits and risks of long-term antipsychotic treatment for schizophrenia
The impact of schizophrenia on social and occupational functioning
The role of family therapy in treating schizophrenia
The challenges of managing schizophrenia in a community setting
The relationship between schizophrenia and other mental health disorders
The potential for early intervention in preventing the onset of schizophrenia
The impact of schizophrenia on cognitive functioning and memory
The relationship between schizophrenia and violence
The experiences of individuals living with schizophrenia
The impact of cultural beliefs and practices on the treatment of schizophrenia
The challenges of providing care for individuals with treatment-resistant schizophrenia
The role of trauma in the development of schizophrenia
The impact of childhood adversity on the risk of developing schizophrenia
The relationship between schizophrenia and homelessness
The challenges of treating schizophrenia in the criminal justice system
The role of peer support in helping individuals with schizophrenia
The impact of schizophrenia on family dynamics and relationships
The benefits and risks of electroconvulsive therapy in treating schizophrenia
The relationship between schizophrenia and suicide
The challenges of managing schizophrenia in older adults
The impact of schizophrenia on physical health and well-being
The potential for personalized medicine in treating schizophrenia
The role of exercise and nutrition in managing symptoms of schizophrenia
The benefits and risks of cognitive-behavioral therapy in treating schizophrenia
The relationship between schizophrenia and creativity
The challenges of providing culturally competent care for individuals with schizophrenia
The impact of social support on the recovery of individuals with schizophrenia
The role of vocational rehabilitation in helping individuals with schizophrenia
The benefits and risks of clozapine in treating treatment-resistant schizophrenia
The relationship between schizophrenia and sleep disorders
The challenges of providing care for individuals with co-occurring schizophrenia and substance use disorders
The impact of schizophrenia on parenting and family dynamics
The role of mindfulness and meditation in managing symptoms of schizophrenia
The benefits and risks of peer-led support groups for individuals with schizophrenia
The relationship between schizophrenia and trauma-related disorders
The challenges of providing care for individuals with schizophrenia in rural communities
The impact of stigma on the treatment and recovery of individuals with schizophrenia
The role of supported housing in helping individuals with schizophrenia
The benefits and risks of mobile health technologies in managing symptoms of schizophrenia
The relationship between schizophrenia and metabolic disorders
The challenges of providing care for individuals with schizophrenia in low-resource settings
The impact of schizophrenia on quality of life and well-being
The role of occupational therapy in helping individuals with schizophrenia
The benefits and risks of mindfulness-based interventions in managing symptoms of schizophrenia
The relationship between schizophrenia and social isolation
The challenges of providing care for individuals with schizophrenia in the LGBTQ+ community
The impact of schizophrenia on academic achievement and educational attainment
The role of peer support specialists in helping individuals with schizophrenia
The benefits and risks of exercise interventions in managing symptoms of schizophrenia
The relationship between schizophrenia and cognitive impairment
The challenges of providing care for individuals with schizophrenia in the foster care system
The impact of schizophrenia on decision-making and problem-solving skills
The role of animal-assisted therapy in helping individuals with schizophrenia
The benefits and risks of group therapy in managing symptoms of schizophrenia
The relationship between schizophrenia and personality disorders
The challenges of providing care for individuals with schizophrenia in the military
The impact of schizophrenia on social relationships and friendships
The role of peer support in helping individuals with schizophrenia stay engaged in treatment
The benefits and risks of art therapy in managing symptoms of schizophrenia
The relationship between schizophrenia and post-traumatic stress disorder
The challenges of providing care for individuals with schizophrenia in the criminal justice system
The impact of schizophrenia on sexual health and relationships
The role of supported employment in helping individuals with schizophrenia
The benefits and risks of dialectical behavior therapy in managing symptoms of schizophrenia
The relationship between schizophrenia and personality traits
The challenges of providing care for individuals with schizophrenia in the workplace
The impact of schizophrenia on self-esteem and self-concept
The role of peer support in helping individuals with schizophrenia navigate the healthcare system
The benefits and risks of music therapy in managing symptoms of schizophrenia
The relationship between schizophrenia and eating disorders
The challenges of providing care for individuals with schizophrenia in the school system
The impact of schizophrenia on spirituality and religious beliefs
The role of peer support in helping individuals with schizophrenia build social connections
The benefits and risks of family therapy in managing symptoms of schizophrenia
The relationship between schizophrenia and obsessive-compulsive disorder
The challenges of providing care for individuals with schizophrenia in the aging population
The impact of schizophrenia on emotional regulation and coping skills
The role of peer support in helping individuals with schizophrenia develop self-advocacy skills
The benefits and risks of mindfulness-based stress reduction in managing symptoms of schizophrenia
The relationship between schizophrenia and autism spectrum disorders
The challenges of providing care for individuals with schizophrenia in the juvenile justice system
The impact of schizophrenia on social skills and communication abilities
The role of peer support in helping individuals with schizophrenia build a sense of community
The benefits and risks of animal-assisted therapy in managing symptoms of schizophrenia
The relationship between schizophrenia and borderline personality disorder
From exploring the biological underpinnings of schizophrenia to examining the social and cultural factors that influence its treatment and management, there are countless avenues for investigation in this field. By choosing a topic that resonates with your interests and expertise, you can delve deep into the complexities of schizophrenia and contribute to a better understanding of this challenging mental disorder. Good luck with your essay writing!
Want to create a presentation now?
Instantly Create A Deck
Let PitchGrade do this for me
Hassle Free
We will create your text and designs for you. Sit back and relax while we do the work.
Explore More Content
- Privacy Policy
- Terms of Service
© 2023 Pitchgrade
90 Schizophrenia Essay Topics
🏆 best essay topics on schizophrenia, 🔎 easy schizophrenia research paper topics, 👍 good schizophrenia research topics & essay examples, 🎓 most interesting schizophrenia research titles, 💡 simple schizophrenia essay ideas.
- Nash’s Schizophrenia in “A Beautiful Mind” Film
- Schizophrenia in “A Beautiful Mind” Film by Howard
- A Mental Health Nursing Social Interventions for Patients With Schizophrenia
- Schizophrenia of John Nash in “A Beautiful Mind”
- Case Study of Schizophrenia: Symptoms, Misconceptions and Diagnosis
- Schizophrenia. Abnormal Psychology
- Schizophrenia: Definition and Symptomps
- The Portrayal of Schizophrenia in a Beautiful Mind A Beautiful Mind by Ron Howard managed to portray the schizophrenia diagnosis accurately but not without a shred of Hollywood exaggeration.
- Deleuze’s “A Thousand Plateaus” and Guattari’s “Capitalism and Schizophrenia” The book “A Thousand Plateaus” written by the French philosopher Gilles Deleuze and the psychoanalyst Felix Guattari is the second part of the project “Capitalism and Schizophrenia”.
- Case Presentation: Schizophrenia The client’s name for this case presentation is Clara Hunters. She is a thirty-three-year-old woman. She is white and has been married for five years.
- Evaluation of the Symptoms of Schizophrenia in “A Beautiful Mind” In this study, the “Diagnostic and Statistical Manual of Mental Disorder” was used to evaluate the symptoms of the main character of the movie called “A Beautiful Mind”.
- Schizophrenia Treatment With Approved Drug Schizophrenia is one of the most common mental disorders in the US. Treatment of schizophrenia is critical since patients stand as dangers to themselves and society.
- Schizophrenia: Non- and Pharmacological Treatment There are effective pharmacological approaches to treating Schizophrenia, such as Clozapine, and non-medical methods, such as psychoeducation.
- Psychiatry: The Multi-Dimensional Nature of Schizophrenia Schizophrenia is a psychological condition in which patients suffer from disabling chronic mental disorders that adversely affect the normal functioning of the brain.
- Schizophrenia: Chapters 15-16 of Psychology by Spielman et al. This research will focus on schizophrenia, a psychological disorder discussed in chapters 15 and 16 of the book Psychology by Spielman, Jenkins, and Lovett.
- Advancements in Schizophrenia Research The article’s primary goal is to review the dopamine hypothesis and study and analyze new targets invented in recent years.
- A Cognitive-Behavioural Therapy Utility of Schizophrenia The paper describes how cognitive-behavioral therapies may be utilized in mental health settings to aid schizophrenic patients in overcoming mental health problems.
- Consciousness and Psychedelic Sciences in Managing Schizophrenia Behavioral management is emerging as a significant intervention in psychiatric treatment, focusing mainly on preserving order for those with clinical mental illness.
- Gender Differences in Schizophrenia The study sheds light on the gender differences in schizophrenia onset. Schizophrenia in women and men manifests itself at different ages.
- Schizophrenia Disorder Diagnosis The main reason for the patient’s visit entails experiences and behavior out of touch with reality. It is the duty of a practitioner to enhance optimal Medicare for a patient.
- Schizophrenia Diagnosis, Treatment, and Prognosis This study evaluates the diagnosis of schizophrenia in a high school teenager, focusing on their background history to assert the prevalence of a different disorder.
- Variables Impacting a Patient With Schizophrenia The mother brought Demetri, her 39-year-old son previously diagnosed with schizophrenia, because of his deteriorating mental well-being.
- Medical Terminology of Treating Schizophrenia The article Clinical relevance of paliperidone palmitate 3-monthly in treating schizophrenia discusses how the mentioned injectable antipsychotic (PP3M) improves non-adherence.
- Gender Differences in Development of Schizophrenia Schizophrenia has varied effects on men’s and women’s sexual life. These effects could be due to variances in the start of schizophrenia at different ages.
- Aspects of Schizophrenia Schizophrenia is a severe mental disorder that demands a specific response. It is vital to diagnose it by using available criteria.
- Schizophrenia in Young Women and Men Schizophrenia, according to several researches, affects both men and women. However, men show high vulnerability as the development of this disorder is concerned.
- Schizophrenia Treatment With Fluphenazine Decanoate The present paper suggests Fluphenazine Decanoate as a medicine useful for decreasing the patient’s paranoid behavior.
- Schizophrenia: Fundamentals and Possible Causes The medicinal approach involves taking drugs based on histone deacetylases, as they improve the condition of certain parts of histones’ acetylation.
- Schizophrenia: Diagnosis and Treatment The presence of signs such as hallucinations, delusions, cognitive issues, and negative symptoms is a marker of developing schizophrenia.
- Schizophrenia: A Comprehensive Explanation Schizophrenia is a severe concern of the modern health care system because it is highly complicated and associated with mental and physical health and reduced life expectancy.
- Schizophrenia: Myths, Causes, and Impacts Schizophrenia is a major mental condition characterized by a combination of unusual behaviors such as hallucinations, delusion, and abnormal thinking.
- Schizophrenia: Causes and Symptoms The leading causes of the development of schizophrenia include heredity, an unfavorable environment, and negative social conditions.
- Schizophrenia and Dopamine Level It is essential to examine the role of dopamine to understand whether the level of this neurotransmitter is high or low in schizophrenia.
- Factors That Caused Schizophrenia Schizophrenia is a common mental disorder among the young males and females, therefore, the paper finds out the various effects of disorder on the young adults.
- Schizophrenia Depicted in “A Beautiful Mind” Film Schizophrenia affects millions of people worldwide, and one of them is John Nash, a mathematician played by Russell Crowe in the film “A Beautiful Mind” by Ron Howard.
- Schizophrenia: Diagnosis, Prevention, and Treatment Articles included in the annotated bibliography describe the causes, diagnosis, prevention, and treatment of schizophrenia.
- Schizophrenia Symptoms and Diagnosis: Patient Interview This article proposes an interview with a patient with schizophrenia, gives his reactions to the questions of the interviewer and describes the symptoms of the disease.
- Biological Strategies for Studying Schizophrenia This paper analyzes several major current approaches to studying schizophrenia. It specifically focuses on several streams of research.
- Schizophrenia as Dangerous Mental Disease Schizophrenia is a very dangerous mental disease, which affects a human mind in numerous ways. It warps a person’s perception of reality.
- Schizophrenia as the Most Challenging Psychological Disorder Despite its relatively low prevalence, schizophrenia ranks among the most impairing and debilitating psychological conditions in people
- Neuroscience of Schizophrenia: The Thinking Patterns The journey to understanding the neuroscience of schizophrenia continues, and firsthand stories like that of John Nash and Lewis continue to play a central role in this process.
- Features of Schizophrenia as Neurodegenerative Disorder This paper describes schizophrenia as a neurodegenerative disorder and tries to understand the key underlying elements linked with the clinical aspect of schizophrenia.
- Gerontology Nursing: Schizophrenia This paper discusses schizophrenia: Its definition, statistics, signs and symptoms, types, risk factors, diagnostic criteria, pharmacological and non-pharmacological interventions.
- Schizophrenia and Folate Status Correlation The research is designed to clarify the relationship between folate status and schizophrenia with an effort to avoid methodological pitfalls during the investigation.
- The Concept of Symptoms in Schizophrenia The essay will delve into the concept of symptoms in schizophrenia and underline the implications for the patient’s treatment.
- Drugs for Treating Schizophrenia and Mood Disorders Schizophrenia and mood disorders are serious mental illnesses, which are challenging to treat. Millions of people suffer from adverse effects on all aspects of life.
- Schizophrenia Versus Schizoaffective Disorders Schizophrenia and schizoaffective are two distinct disorders, each having its way of diagnosis and treatment. However, they share almost similar psychotic characteristics.
- Schizophrenia Treatment: Biopsychological Approaches This paper is aimed at discussing schizophrenia as a mental illness from the perspective of various biopsychological approaches.
- Schizophrenia: Causes, Symptoms, Treatments, and Myths This paper will discuss the causes and symptoms of schizophrenia, the ways of its treatment, and the myths that surround this mental illness.
- Connection Between Schizophrenia and Neurotransmitters Neurotransmitters do the visible impact on the development of schizophrenia, although it manifests when they are inflamed.
- Influence of Sexual Dysfunction and Schizophrenia on Human The paper examines the causes, problems and manifestations of mental problems that affect the physical condition of a person.
- Schizophrenia Disorder: Causes and Treatment Schizophrenia is a mental disease, which affects the thinking capacity of an individual. A considerable number of populations around the globe are affected by this disease.
- An Accurate Portrayal of Schizophrenia This paper will analyze the Schizophrenia along with its symptoms. It will also analyze an important scene in the movie “a beautiful mind” which was directed by Ron Howard.
- Understanding Mental Illness: Aspects of Schizophrenia There is a significant social stigma surrounding severe mental illness such as schizophrenia which leads to discrimination of not just the patient, but the whole family.
- Family Psychoeducation for Schizophrenia Patients This work reviews a meta-analysis on FPE conducted, focusing on the effectiveness of the educational approach in treating patients with schizophrenia and supporting their families.
- Schizophrenia in a First-Year College Student The paper studies a case of schizophrenia, which manifested in a 39-year-old woman during her first year at college in the form of prodromal symptoms, which caused her to drop out.
- Schizophrenia Features Among African American Men Schizophrenia is a serious mental disorder that may occur at any age. African Americans usually have severe psychotic symptoms regarding the scope and quality of hallucinations.
- Schizophrenia and QT Prolongation The paper considers the case of a 62-year-old woman with a history of psychiatric diagnoses, which indicates her predisposition to delusions.
- Schizophrenia: Approaches and Behavior It is hypothesized the symptoms of schizophrenia can be attributed to the increased dopaminergic activities in such brain areas as striatum and thalamus.
- Schizophrenia: Physiological Basis of a Mental Illness Schizophrenia is mental illness with a genetic basis and its complexity is presents in form of chronic psychosis and the cognitive ability of the individual becomes impaired.
- Difficulties That the Person With Schizophrenia Goes Through
- Altered Cerebral Blood Flow Covariance Network in Schizophrenia
- Broader Visual Orientation Tuning in Patients With Schizophrenia
- Imaging Schizophrenia With Voxel-Based Morphometry
- Antipsychotics, Metabolic Adverse Effects, and Cognitive Function in Schizophrenia
- Chronicity and Sex Affect Genetic Risk Prediction in Schizophrenia
- Correlation Between Child Abuse and Schizophrenia
- Genetic and Environmental Factors of Schizophrenia
- Complex Gastrointestinal and Endocrine Sources of Inflammation in Schizophrenia
- Environmental and Genetic Effects and Schizophrenia
- Current Controversial Issues During Treatment of Schizophrenia
- Environmental Factors and the Development of Schizophrenia
- Cognitive Behavioral Therapy for Schizophrenia
- Biological and Cognitive Approaches for the Treatment of Schizophrenia
- Antigliadin Antibodies Relation to Neurochemistry in Schizophrenia
- Considering Brexpiprazole and Its Role in Managing Schizophrenia
- Disrupted Thalamic Resting-State Functional Networks in Schizophrenia
- Demystifying Common Misconceptions About Schizophrenia
- Implementing Evidence-Based Practice With Schizophrenia
- Altered Volume and Functional Connectivity of the Habenula in Schizophrenia
- Causes and Key Symptoms of Paranoid Schizophrenia
- Definitions and Social Perceptions of Schizophrenia
- Decreasing Social Interaction Anxiety for Schizophrenia
- Identifying Modifiable Risk Factors for Relapse in Patients With Schizophrenia in China
- Family Education and Management of Schizophrenia
- Creativity and Schizophrenia Spectrum Disorders Across the Arts and Sciences
- Diagnosing and Treating Schizophrenia
- Drug Abuse and Schizophrenia
- Critical Diagnostic Review of Schizophrenia
- Disorganized Schizophrenia and Its Effects on Children
Cite this post
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2022, May 10). 90 Schizophrenia Essay Topics. https://studycorgi.com/ideas/schizophrenia-essay-topics/
"90 Schizophrenia Essay Topics." StudyCorgi , 10 May 2022, studycorgi.com/ideas/schizophrenia-essay-topics/.
StudyCorgi . (2022) '90 Schizophrenia Essay Topics'. 10 May.
1. StudyCorgi . "90 Schizophrenia Essay Topics." May 10, 2022. https://studycorgi.com/ideas/schizophrenia-essay-topics/.
Bibliography
StudyCorgi . "90 Schizophrenia Essay Topics." May 10, 2022. https://studycorgi.com/ideas/schizophrenia-essay-topics/.
StudyCorgi . 2022. "90 Schizophrenia Essay Topics." May 10, 2022. https://studycorgi.com/ideas/schizophrenia-essay-topics/.
These essay examples and topics on Schizophrenia were carefully selected by the StudyCorgi editorial team. They meet our highest standards in terms of grammar, punctuation, style, and fact accuracy. Please ensure you properly reference the materials if you’re using them to write your assignment.
This essay topic collection was updated on January 9, 2024 .
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 24 February 2022
Systematic literature review of schizophrenia clinical practice guidelines on acute and maintenance management with antipsychotics
- Christoph U. Correll ORCID: orcid.org/0000-0002-7254-5646 1 , 2 , 3 ,
- Amber Martin 4 ,
- Charmi Patel 5 ,
- Carmela Benson 5 ,
- Rebecca Goulding 6 ,
- Jennifer Kern-Sliwa 5 ,
- Kruti Joshi 5 ,
- Emma Schiller 4 &
- Edward Kim ORCID: orcid.org/0000-0001-8247-6675 7
Schizophrenia volume 8 , Article number: 5 ( 2022 ) Cite this article
14k Accesses
45 Citations
14 Altmetric
Metrics details
- Schizophrenia
Clinical practice guidelines (CPGs) translate evidence into recommendations to improve patient care and outcomes. To provide an overview of schizophrenia CPGs, we conducted a systematic literature review of English-language CPGs and synthesized current recommendations for the acute and maintenance management with antipsychotics. Searches for schizophrenia CPGs were conducted in MEDLINE/Embase from 1/1/2004–12/19/2019 and in guideline websites until 06/01/2020. Of 19 CPGs, 17 (89.5%) commented on first-episode schizophrenia (FES), with all recommending antipsychotic monotherapy, but without agreement on preferred antipsychotic. Of 18 CPGs commenting on maintenance therapy, 10 (55.6%) made no recommendations on the appropriate maximum duration of maintenance therapy, noting instead individualization of care. Eighteen (94.7%) CPGs commented on long-acting injectable antipsychotics (LAIs), mainly in cases of nonadherence (77.8%), maintenance care (72.2%), or patient preference (66.7%), with 5 (27.8%) CPGs recommending LAIs for FES. For treatment-resistant schizophrenia, 15/15 CPGs recommended clozapine. Only 7/19 (38.8%) CPGs included a treatment algorithm.
Similar content being viewed by others

Interim analyses of a first-in-human phase 1/2 mRNA trial for propionic acidaemia
Dwight Koeberl, Andreas Schulze, … Stephanie Grunewald

Long COVID: major findings, mechanisms and recommendations
Hannah E. Davis, Lisa McCorkell, … Eric J. Topol

Adults who microdose psychedelics report health related motivations and lower levels of anxiety and depression compared to non-microdosers
Joseph M. Rootman, Pamela Kryskow, … Zach Walsh
Introduction
Schizophrenia is an often debilitating, chronic, and relapsing mental disorder with complex symptomology that manifests as a combination of positive, negative, and/or cognitive features 1 , 2 , 3 . Standard management of schizophrenia includes the use of antipsychotic medications to help control acute psychotic episodes 4 and prevent relapses 5 , 6 , whereas maintenance therapy is used in the long term after patients have been stabilized 7 , 8 , 9 . Two main classes of drugs—first- and second-generation antipsychotics (FGA and SGA)—are used to treat schizophrenia 10 . SGAs are favored due to the lower rates of adverse effects, such as extrapyramidal effects, tardive dyskinesia, and relapse 11 . However, pharmacologic treatment for schizophrenia is complicated because nonadherence is prevalent, and is a major risk factor for relapse 9 and poor overall outcomes 12 . The use of long-acting injectable (LAI) versions of antipsychotics aims to limit nonadherence-related relapses and poor outcomes 13 .
Patient treatment pathways and treatment choices are determined based on illness acuity/severity, past treatment response and tolerability, as well as balancing medication efficacy and adverse effect profiles in the context of patient preferences and adherence patterns 14 , 15 . Clinical practice guidelines (CPG) serve to inform clinicians with recommendations that reflect current evidence from meta-analyses of randomized controlled trials (RCTs), individual RCTs and, less so, epidemiologic studies, as well as clinical experience, with the goal of providing a framework and road-map for treatment decisions that will improve quality of care and achieve better patients outcomes. The use of clinical algorithms or other decision trees in CPGs may improve the ease of implementation of the evidence in clinical practice 16 . While CPGs are an important tool for mental health professionals, they have not been updated on a regular basis like they have been in other areas of medicine, such as in oncology. In the absence of current information, other governing bodies, healthcare systems, and hospitals have developed their own CPGs regarding the treatment of schizophrenia, and many of these have been recently updated 17 , 18 , 19 . As such, it is important to assess the latest guidelines to be aware of the changes resulting from consideration of updated evidence that informed the treatment recommendations. Since CPGs are comprehensive and include the diagnosis as well as the pharmacological and non-pharmacological management of individuals with schizophrenia, a detailed comparative review of all aspects of CPGs for schizophrenia would have been too broad a review topic. Further, despite ongoing efforts to broaden the pharmacologic tools for the treatment of schizophrenia 20 , antipsychotics remain the cornerstone of schizophrenia management 8 , 21 . Therefore, a focused review of guideline recommendations for the management of schizophrenia with antipsychotics would serve to provide clinicians with relevant information for treatment decisions.
To provide an updated overview of United States (US) national and English language international guidelines for the management of schizophrenia, we conducted a systematic literature review (SLR) to identify CPGs and synthesize current recommendations for pharmacological management with antipsychotics in the acute and maintenance phases of schizophrenia.
Systematic searches for the SLR yielded 1253 hits from the electronic literature databases. After removal of duplicate references, 1127 individual articles were screened at the title and abstract level. Of these, 58 publications were deemed eligible for screening at the full-text level, from which 19 were ultimately included in the SLR. Website searches of relevant organizations yielded 10 additional records, and an additional three records were identified by the state-by-state searches. Altogether, this process resulted in 32 records identified for inclusion in the SLR. Of the 32 sources, 19 primary CPGs, published/issued between 2004 and 2020, were selected for extraction, as illustrated in the PRISMA diagram (Fig. 1 ). While the most recent APA guideline was identified and available for download in 2020, the reference to cite in the document indicates a publication date of 2021.
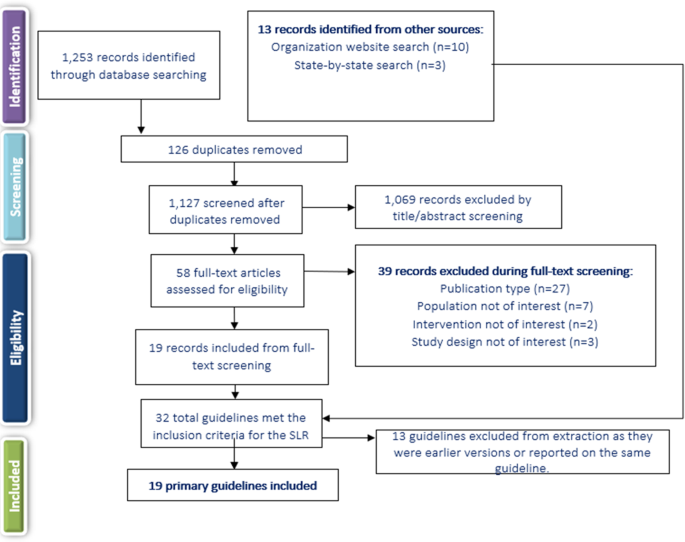
SLR systematic literature review.
Of the 19 included CPGs (Table 1 ), three had an international focus (from the following organizations: International College of Neuropsychopharmacology [CINP] 22 , United Nations High Commissioner for Refugees [UNHCR] 23 , and World Federation of Societies of Biological Psychiatry [WFSBP] 24 , 25 , 26 ); seven originated from the US; 17 , 18 , 19 , 27 , 28 , 29 , 30 , 31 , 32 three were from the United Kingdom (British Association for Psychopharmacology [BAP] 33 , the National Institute for Health and Care Excellence [NICE] 34 , and the Scottish Intercollegiate Guidelines Network [SIGN] 35 ); and one guideline each was from Singapore 36 , the Polish Psychiatric Association (PPA) 37 , 38 , the Canadian Psychiatric Association (CPA) 14 , the Royal Australia/New Zealand College of Psychiatrists (RANZCP) 39 , the Association Française de Psychiatrie Biologique et de Neuropsychopharmacologie (AFPBN) from France 40 , and Italy 41 . Fourteen CPGs (74%) recommended treatment with specific antipsychotics and 18 (95%) included recommendations for the use of LAIs, while just seven included a treatment algorithm Table 2 ). The AGREE II assessment resulted in the highest score across the CPGs domains for NICE 34 followed by the American Psychiatric Association (APA) guidelines 17 . The CPA 14 , BAP 33 , and SIGN 35 CPGs also scored well across domains.
Acute therapy
Seventeen CPGs (89.5%) provided treatment recommendations for patients experiencing a first schizophrenia episode 14 , 17 , 18 , 19 , 22 , 23 , 24 , 28 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 39 , 40 , 41 , but the depth and focus of the information varied greatly (Supplementary Table 1 ). In some CPGs, information on treatment of a first schizophrenia episode was limited or grouped with information on treating any acute episode, such as in the CPGs from CINP 22 , AFPBN 40 , New Jersey Division of Mental Health Services (NJDMHS) 32 , the APA 17 , and the PPA 37 , 38 , while the others provided more detailed information specific to patients experiencing a first schizophrenia episode 14 , 18 , 19 , 23 , 24 , 28 , 33 , 34 , 35 , 36 , 39 , 41 . The American Association of Community Psychiatrists (AACP) Clinical Tips did not provide any information on the treatment of schizophrenia patients with a first episode 29 .
There was little agreement among CPGs regarding the preferred antipsychotic for a first schizophrenia episode. However, there was strong consensus on antipsychotic monotherapy and that lower doses are generally recommended due to better treatment response and greater adverse effect sensitivity. Some guidelines recommended SGAs over FGAs when treating a first-episode schizophrenia patient (RANZCP 39 , Texas Medication Algorithm Project [TMAP] 28 , Oregon Health Authority 19 ), one recommended starting patients on an FGA (UNHCR 23 ), and others stated specifically that there was no evidence of any difference in efficacy between FGAs and SGAs (WFSBP 24 , CPA 14 , SIGN 35 , APA 17 , Singapore guidelines 36 ), or did not make any recommendation (CINP 22 , Italian guidelines 41 , NICE 34 , NJDMHS 32 , Schizophrenia Patient Outcomes Research Team [PORT] 30 , 31 ). The BAP 33 and WFBSP 24 noted that while there was probably no difference between FGAs and SGAs in efficacy, some SGAs (olanzapine, amisulpride, and risperidone) may perform better than some FGAs. The Schizophrenia PORT recommendations noted that while there seemed to be no differences between SGAs and FGAs in short-term studies (≤12 weeks), longer studies (one to two years) suggested that SGAs may provide benefits in terms of longer times to relapse and discontinuation rates 30 , 31 . The AFPBN guidelines 40 and Florida Medicaid Program guidelines 18 , which both focus on use of LAI antipsychotics, both recommended an SGA-LAI for patients experiencing a first schizophrenia episode. A caveat in most CPGs was that physicians and their patients should discuss decisions about the choice of antipsychotic and that the choice should consider individual patient factors/preferences, risk of adverse and metabolic effects, and symptom patterns 17 , 18 , 19 , 22 , 24 , 28 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 39 , 41 .
Most CPGs recommended switching to a different monotherapy if the initial antipsychotic was not effective or not well tolerated after an adequate antipsychotic trial at an appropriate dose 14 , 17 , 18 , 19 , 22 , 23 , 24 , 28 , 32 , 33 , 35 , 36 , 39 . For patients initially treated with an FGA, the UNHCR recommended switching to an SGA (olanzapine or risperidone) 23 . Guidance on response to treatment varied in the measures used but typically required at least a 20% improvement in symptoms (i.e. reduction in Positive and Negative Syndrome Scale or Brief Psychiatric Rating Scale scores) from pre-treatment levels.
Several CPGs contained recommendations on the duration of antipsychotic therapy after a first schizophrenia episode. The NJDMHS guidelines 32 recommended nine to 12 months; CINP 22 recommended at least one year; CPA 14 recommended at least 18 months; WFSBP 25 , the Italian guidelines 41 , and NICE 34 recommended 1 to 2 years; and the RANZCP 39 , BAP 33 , and SIGN 35 recommended at least 2 years. The APA 17 and TMAP 28 recommended continuing antipsychotic treatment after resolution of first-episode symptoms but did not recommend a specific length of therapy.
Twelve guidelines 14 , 18 , 22 , 24 , 28 , 30 , 31 , 33 , 34 , 35 , 36 , 39 , 40 (63.2%) discussed the treatment of subsequent/multiple episodes of schizophrenia (i.e., following relapse). These CPGs noted that the considerations guiding the choice of antipsychotic for subsequent/multiple episodes were similar to those for a first episode, factoring in prior patient treatment response, adverse effect patterns and adherence. The CPGs also noted that response to treatment may be lower and require higher doses to achieve a response than for first-episode schizophrenia, that a different antipsychotic than used to treat the first episode may be needed, and that a switch to an LAI is an option.
Several CPGs provided recommendations for patients with specific clinical features (Supplementary Table 1 ). The most frequently discussed group of clinical features was negative symptoms, with recommendations provided in the CINP 22 , UNHCR 23 , WFSBP 24 , AFPBN 40 , SIGN 35 , BAP 33 , APA 17 , and NJDMHS guidelines; 32 negative symptoms were the sole focus of the guidelines from the PPA 37 , 38 . The guidelines noted that due to limited evidence in patients with predominantly negative symptoms, there was no clear benefit for any strategy, but that options included SGAs (especially amisulpride) rather than FGAs (WFSBP 24 , CINP 22 , AFPBN 40 , SIGN 35 , NJDMHS 32 , PPA 37 , 38 ), and addition of an antidepressant (WFSBP 24 , UNHCR 23 , SIGN 35 , NJDMHS 32 ) or lamotrigine (SIGN 35 ), or switching to another SGA (NJDMHS 32 ) or clozapine (NJDMHS 32 ). The PPA guidelines 37 , 38 stated that the use of clozapine or adding an antidepressant or other medication class was not supported by evidence, but recommended the SGA cariprazine for patients with predominant and persistent negative symptoms, and other SGAs for those with full-spectrum negative symptoms. However, the BAP 33 stated that no recommendations can be made for any of these strategies because of the quality and paucity of the available evidence.
Some of the CPGs also discussed treatment of other clinical features to a limited degree, including depressive symptoms (CINP 22 , UNHCR 23 , CPA 14 , APA 17 , and NJDMHS 32 ), cognitive dysfunction (CINP 22 , UNHCR 23 , WFSBP 24 , AFPBN 40 , SIGN 35 , BAP 33 , and NJDMHS 32 ), persistent aggression (CINP 22 , WFSBP 24 , CPA 14 , AFPBN 40 , NICE 34 , SIGN 35 , BAP 33 , and NJDMHS 32 ), and comorbid psychiatric diagnoses (CINP 22 , RANZCP 39 , BAP 33 , APA 17 , and NJDMHS 32 ).
Fifteen CPGs (78.9%) discussed treatment-resistant schizophrenia (TRS); all defined it as persistent, predominantly positive symptoms after two adequate antipsychotic trials; clozapine was the unanimous first choice 14 , 17 , 18 , 19 , 22 , 23 , 24 , 28 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 39 . However, the UNHCR guidelines 23 , which included recommendations for treatment of refugees, noted that clozapine is only a reasonable choice in regions where white blood cell monitoring and specialist supervision are available, otherwise, risperidone or olanzapine are alternatives if they had not been used in the previous treatment regimen.
There were few options for patients who are resistant to clozapine therapy, and evidence supporting these options was limited. The CPA guidelines 14 therefore stated that no recommendation can be given due to inadequate evidence. Other CPGs discussed options (but noted there was limited supporting evidence), such as switching to olanzapine or risperidone (WFSBP 24 , TMAP 28 ), adding a second antipsychotic to clozapine (CINP 22 , NICE 34 , TMAP 28 , BAP 33 , Florida Medicaid Program 18 , Oregon Health Authority 19 , RANZCP 39 ), adding lamotrigine or topiramate to clozapine (CINP 22 , Florida Medicaid Program 18 ), combination therapy with two non-clozapine antipsychotics (Florida Medicaid Program 18 , NJDMHS 32 ), and high-dose non-clozapine antipsychotic therapy (BAP 33 , SIGN 35 ). Electroconvulsive therapy was noted as a last resort for patients who did not respond to any pharmacologic therapy, including clozapine, by 10 CPGs 17 , 18 , 19 , 22 , 24 , 28 , 32 , 35 , 36 , 39 .
Maintenance therapy
Fifteen CPGs (78.9%) discussed maintenance therapy to various degrees via dedicated sections or statements, while three others referred only to maintenance doses by antipsychotic agent 18 , 23 , 29 without accompanying recommendations (Supplementary Table 2 ). Only the Italian guideline provided no reference or comments on maintenance treatment. The CINP 22 , WFSBP 25 , RANZCP 39 , and Schizophrenia PORT 30 , 31 recommended keeping patients on the same antipsychotic and at the same dose on which they had achieved remission. Several CPGs recommended maintenance therapy at the lowest effective dose (NJDMHS 32 , APA 17 , Singapore guidelines 36 , and TMAP 28 ). The CPA 14 and SIGN 35 defined the lower dose as 300–400 mg chlorpromazine equivalents or 4–6 mg risperidone equivalents, and the Singapore guidelines 36 stated that the lower dose should not be less than half the original dose. TMAP 28 stated that given the relapsing nature of schizophrenia, the maintenance dose should often be close to the original dose. While SIGN 35 recommended that patients remain on the same antipsychotic that provided remission, these guidelines also stated that maintenance with amisulpride, olanzapine, or risperidone was preferred, and that chlorpromazine and other low-potency FGAs were also suitable. The BAP 33 recommended that the current regimen be optimized before any dose reduction or switch to another antipsychotic occurs. Several CPGs recommended LAIs as an option for maintenance therapy (see next section).
Altogether, 10/18 (55.5%) CPGs made no recommendations on the appropriate duration of maintenance therapy, noting instead that each patient should be considered individually. Other CPGs made specific recommendations: Both the Both BAP 33 and SIGN 35 guidelines suggested a minimum of 2 years, the NJDMHS guidelines 32 recommended 2–3 years; the WFSBP 25 recommended 2–5 years for patients who have had one relapse and more than 5 years for those who have had multiple relapses; the RANZCP 39 and the CPA 14 recommended 2–5 years; and the CINP 22 recommended that maintenance therapy last at least 6 years for patients who have had multiple episodes. The TMAP was the only CPG to recommend that maintenance therapy be continued indefinitely 28 .
Recommendations on the use of LAIs
All CPGs except the one from Italy (94.7%) discussed the use of LAIs for patients with schizophrenia to some extent. As shown in Table 3 , among the 18 CPGs, LAIs were primarily recommended in 14 CPGs (77.8%) for patients who are non-adherent to other antipsychotic administration routes (CINP 22 , UNHCR 23 , RANZCP 39 , PPA 37 , 38 , Singapore guidelines 36 , NICE 34 , SIGN 35 , BAP 33 , APA 17 , TMAP 28 , NJDMHS 32 , AACP 29 , Oregon Health Authority 19 , Florida Medicaid Program 18 ). Twelve CPGs (66.7%) also noted that LAIs should be prescribed based on patient preference (RANZCP 39 , CPA 14 , AFPBN 40 , Singapore guidelines 36 , NICE 34 , SIGN 35 , BAP 33 , APA 17 , Schizophrenia PORT 30 , 31 , AACP 29 , Oregon Health Authority 19 , Florida Medicaid Program 18 ).
Thirteen CPGs (72.2%) recommended LAIs as maintenance therapy 18 , 19 , 24 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 39 , 40 . While five CPGs (27.8%), i.e., AFPBN 40 , RANZCP 39 , TMAP 28 , NJDMHS 32 , and the Florida Medicaid Program 18 recommended LAIs specifically for patients experiencing a first episode. While the CPA 14 did not make any recommendations regarding when LAIs should be used, they discussed recent evidence supporting their use earlier in treatment. Five guidelines (27.8%, i.e., Singapore 36 , NICE 34 , SIGN 35 , BAP 33 , and Schizophrenia PORT 30 , 31 ) noted that evidence around LAIs was not sufficient to support recommending their use for first-episode patients. The AFPBN guidelines 40 also stated that LAIs (SGAs as first-line and FGAs as second-line treatment) should be more frequently considered for maintenance treatment of schizophrenia. Four CPGs (22.2%, i.e., CINP 22 , UNHCR 23 , Italian guidelines 41 , PPA guidelines 37 , 38 ) did not specify when LAIs should be used. The AACP guidelines 29 , which evaluated only LAIs, recommended expanding their use beyond treatment for nonadherence, suggesting that LAIs may offer a more convenient mode of administration or potentially address other clinical and social challenges, as well as provide more consistent plasma levels.
Treatment algorithms
Only Seven CPGs (36.8%) included an algorithm as part of the treatment recommendations. These included decision trees or flow diagrams that map out initial therapy, durations for assessing response, and treatment options in cases of non-response. However, none of these guidelines defined how to measure response, a theme that also extended to guidelines that did not include treatment algorithms. Four of the seven guidelines with algorithms recommended specific antipsychotic agents, while the remaining three referred only to the antipsychotic class.
LAIs were not consistently incorporated in treatment algorithms and in six CPGs were treated as a separate category of medicine reserved for patients with adherence issues or a preference for the route of administration. The only exception was the Florida Medicaid Program 18 , which recommended offering LAIs after oral antipsychotic stabilization even to patients who are at that point adherent to oral antipsychotics.
Benefits and harms
The need to balance the efficacy and safety of antipsychotics was mentioned by all CPGs as a basic treatment paradigm.
Ten CPGs provided conclusions on benefits of antipsychotic therapy. The APA 17 and the BAP 33 guidelines stated that antipsychotic treatment can improve the positive and negative symptoms of psychosis and leads to remission of symptoms. These CPGs 17 , 33 as well as those from NICE 34 and CPA 14 stated that these treatment effects can also lead to improvements in quality of life (including quality-adjusted life years), improved functioning, and reduction in disability. The CPA 14 and APA 17 guidelines noted decreases in hospitalizations with antipsychotic therapy, and the APA guidelines 17 stated that long-term antipsychotic treatment can also reduce mortality. The UNHCR 23 and the Italian 41 guidelines noted that early intervention increased positive outcomes. The WFSBP 24 , AFPBN 40 , CPA 14 , BAP 33 , APA 17 , and NJDMHS 32 affirmed that relapse prevention is a benefit of continued/maintenance treatment.
Some CPGs (WFSBP 24 , Italian 41 , CPA 14 , and SIGN 35 ) noted that reduced risk for extrapyramidal adverse effects and treatment discontinuation were potential benefits of SGAs vs. FGAs.
The risk of adverse effects (e.g., extrapyramidal, metabolic, cardiovascular, and hormonal adverse effects, sedation, and neuroleptic malignant syndrome) was noted by all CPGs as the major potential harm of antipsychotic therapy 14 , 17 , 18 , 19 , 22 , 23 , 24 , 28 , 29 , 30 , 31 , 32 , 34 , 35 , 36 , 37 , 39 , 40 , 41 , 42 . These adverse effects are known to limit long-term treatment and adherence 24 .
This SLR of CPGs for the treatment of schizophrenia yielded 19 most updated versions of individual CPGs, published/issued between 2004 and 2020. Structuring our comparative review according to illness phase, antipsychotic type and formulation, response to antipsychotic treatment as well as benefits and harms, several areas of consistent recommendations emerged from this review (e.g., balancing risk and benefits of antipsychotics, preferring antipsychotic monotherapy; using clozapine for treatment-resistant schizophrenia). On the other hand, other recommendations regarding other areas of antipsychotic treatment were mostly consistent (e.g., maintenance antipsychotic treatment for some time), somewhat inconsistent (e.g., differences in the management of first- vs multi-episode patients, type of antipsychotic, dose of antipsychotic maintenance treatment), or even contradictory (e.g., role of LAIs in first-episode schizophrenia patients).
Consistent with RCT evidence 43 , 44 , antipsychotic monotherapy was the treatment of choice for patients with first-episode schizophrenia in all CPGs, and all guidelines stated that a different single antipsychotic should be tried if the first is ineffective or intolerable. Recommendations were similar for multi-episode patients, but factored in prior patient treatment response, adverse effect patterns, and adherence. There was also broad consensus that the side-effect profile of antipsychotics is the most important consideration when making a decision on pharmacologic treatment, also reflecting meta-analytic evidence 4 , 5 , 10 . The risk of extrapyramidal symptoms (especially with FGAs) and metabolic effects (especially with SGAs) were noted as key considerations, which are also reflected in the literature as relevant concerns 4 , 45 , 46 , including for quality of life and treatment nonadherence 47 , 48 , 49 , 50 .
Largely consistent with the comparative meta-analytic evidence regarding the acute 4 , 51 , 52 and maintenance antipsychotic treatment 5 effects of schizophrenia, the majority of CPGs stated there was no difference in efficacy between SGAs and FGAs (WFSBP 24 , CPA 14 , SIGN 35 , APA 17 , and Singapore guidelines 36 ), or did not make any recommendations (CINP 22 , Italian guidelines 41 , NICE 34 , NJDMHS 32 , and Schizophrenia PORT 30 , 31 ); three CPGs (BAP 33 , WFBSP 24 , and Schizophrenia PORT 30 , 31 ) noted that SGAs may perform better than FGAs over the long term, consistent with a meta-analysis on this topic 53 .
The 12 CPGs that discussed treatment of subsequent/multiple episodes generally agreed on the factors guiding the choices of an antipsychotic, including that the decision may be more complicated and response may be lower than with a first episode, as described before 7 , 54 , 55 , 56 .
There was little consensus regarding maintenance therapy. Some CPGs recommended the same antipsychotic and dose that achieved remission (CINP 22 , WFSBP 25 , RANZCP 39 , and Schizophrenia PORT 30 , 31 ) and others recommended the lowest effective dose (NJDMHS 32 , APA 17 , Singapore guidelines 36 , TMAP 28 , CPA 14 , and SIGN 35 ). This inconsistency is likely based on insufficient data as well as conflicting results in existing meta-analyses on this topic 57 , 58 , 59 .
The 15 CPGs that discussed TRS all used the same definition for this condition, consistent with recent commendations 60 , and agreed that clozapine is the primary evidence-based treatment choice 14 , 17 , 18 , 19 , 22 , 23 , 24 , 28 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 39 , reflecting the evidence base 61 , 62 , 63 . These CPGs also agreed that there are few options well supported by evidence for patients who do not respond to clozapine, with a recent meta-analysis of RCTs showing that electroconvulsive therapy augmentation may be the most evidence-based treatment option 64 .
One key gap in the treatment recommendations was how long patients should remain on antipsychotic therapy after a first episode or during maintenance therapy. While nine of the 17 CPGs discussing treatment of a first episode provided a recommended timeframe (varying from 1 to 2 years) 14 , 22 , 24 , 32 , 33 , 34 , 35 , 39 , 41 , the APA 17 and TMAP 28 recommended continuing antipsychotic treatment after resolution of first-episode symptoms but did not recommend a specific length of therapy. Similarly, six of the 18 CPGs discussing maintenance treatment recommended a specific duration of therapy (ranging from two to six years) 14 , 22 , 25 , 32 , 39 , while as many as 10 CPGs did not point to a firm end of the maintenance treatment, instead recommending individualized decisions. The CPGs not stating a definite endpoint or period of maintenance treatment after repeated schizophrenia episodes or even after a first episode of schizophrenia, reflects the different evidence types on which the recommendation is based. The RCT evidence ends after several years of maintenance treatment vs. discontinuation supporting ongoing antipsychotic treatment; however, naturalistic database studies do not indicate any time period after which one can safely discontinue maintenance antipsychotic care, even after a first schizophrenia episode 8 , 65 . In fact, stopping antipsychotics is associated not only with a substantially increased risk of hospitalization but also mortality 65 , 66 , 67 . In this sense, not stating an endpoint for antipsychotic maintenance therapy should not be taken as an implicit statement that antipsychotics should be discontinued at any time; data suggest the contrary.
A further gap exists regarding the most appropriate treatment of negative symptoms, such as anhedonia, amotivation, asociality, affective flattening, and alogia 1 , a long-standing challenge in the management of patients with schizophrenia. Negative symptoms often persist in patients after positive symptoms have resolved, or are the presenting feature in a substantial minority of patients 22 , 35 . Negative symptoms can also be secondary to pharmacotherapy 22 , 68 . Antipsychotics have been most successful in treating positive symptoms, and while eight of the CPGs provided some information on treatment of negative symptoms, the recommendations were generally limited 17 , 22 , 23 , 24 , 32 , 33 , 35 , 40 . Negative symptom management was a focus of the PPA guidelines, but the guidelines acknowledged that supporting evidence was limited, often due to the low number of patients with predominantly negative symptoms in clinical trials 37 , 38 . The Polish guidelines are also one of the more recently developed and included the newer antipsychotic cariprazine as a first-line option, which although being a point of differentiation from the other guidelines, this recommendation was based on RCT data 69 .
Another area in which more direction is needed is on the use of LAIs. While all but one of the 19 CPGs discussed this topic, the extent of information and recommendations for LAI use varied considerably. All CPGs categorized LAIs as an option to improve adherence to therapy or based on patient preference. However, 5/18 CPGs (27.8%) recommended the use of LAI early in treatment (at first episode: AFPBN 40 , RANZCP 39 , TMAP 28 , NJDMHS 32 , and Florida Medicaid Program 18 ) or across the entire illness course, while five others stated there was not sufficient evidence to recommend LAIs for these patients (Singapore 36 , NICE 34 , SIGN 35 , BAP 33 , and Schizophrenia PORT 30 , 31 ). The role of LAIs in first-episode schizophrenia was the only point where opposing recommendations were found across CPGs. This contradictory stance was not due to the incorporation of newer data suggesting benefits of LAIs in first episode and early-phase patients with schizophrenia 70 , 71 , 72 , 73 , 74 in the CPGs recommending LAI use in first-episode patients, as CPGs recommending LAI use were published between 2005 and 2020, while those opposing LAI use were published between 2011 and 2020. Only the Florida Medicaid CPG recommended LAIs as a first step equivalent to oral antipsychotics (OAP) after initial OAP response and tolerability, independent of nonadherence or other clinical variables. This guideline was also the only CPG to fully integrate LAI use in their clinical algorithm. The remaining six CPGs that included decision tress or treatment algorithms regarded LAIs as a separate paradigm of treatment reserved for nonadherence or patients preference rather than a routine treatment option to consider. While some CPGs provided fairly detailed information on the use of LAIs (AFPBN 40 , AACP 29 , Oregon Health Authority 19 , and Florida Medicaid Program 18 ), others mentioned them only in the context of adherence issues or patient preference. Notably, definitions of and means to determine nonadherence were not reported. One reason for this wide range of recommendations regarding the placement of LAIs in the treatment algorithm and clinical situations that prompt LAI use might be due to the fact that CPGs generally favor RCT evidence over evidence from other study designs. In the case of LAIs, there was a notable dissociation between consistent meta-analytic evidence of statistically significant superiority of LAIs vs OAPs in mirror-image 75 and cohort study designs 76 and non-significant advantages in RCTs 77 . Although patients in RCTs comparing LAIs vs OAPs were less severely ill and more adherent to OAPs 77 than in clinical care and although mirror-image and cohort studies arguably have greater external validity than RCTs 78 , CPGs generally disregard evidence from other study designs when RCT evidence exits. This narrow focus can lead to disregarding important additional data. Nevertheless, a most updated meta-analysis of all 3 study designs comparing LAIs with OAPs demonstrated consistent superiority of LAIs vs OAPs for hospitalization or relapse across all 3 designs 79 , which should lead to more uniform recommendations across CPGs in the future.
Only seven CPGs included treatment algorithms or flow charts to guide LAI treatment selection for patients with schizophrenia 17 , 18 , 19 , 24 , 29 , 35 , 40 . However, there was little commonality across algorithms beyond the guidance on LAIs mentioned above, as some listed specific treatments and conditions for antipsychotic switches, while others indicated that medication choice should be based on a patient’s preferences and responses, side effects, and in some cases, cost effectiveness. Since algorithms and flow charts facilitate the reception, adoption and implementation of guidelines, future CPGs should include them as dissemination tools, but they need to reflect the data and detailed text and be sufficiently specific to be actionable.
The systematic nature in the identification, summarization, and assessment of the CPGs is a strength of this review. This process removed any potential bias associated with subjective selection of evidence, which is not reproducible. However, only CPGs published in English were included and regardless of their quality and differing timeframes of development and publication, complicating a direct comparison of consensus and disagreement. Finally, based on the focus of this SLR, we only reviewed pharmacologic management with antipsychotics. Clearly, the assessment, other pharmacologic and, especially, psychosocial interventions are important in the management of individuals with schizophrenia, but these topics that were covered to varying degrees by the evaluated CPGs were outside of the scope of this review.
Numerous guidelines have recently updated their recommendations on the pharmacological treatment of patients with schizophrenia, which we have summarized in this review. Consistent recommendations were observed across CPGs in the areas of balancing risk and benefits of antipsychotics when selecting treatment, a preference for antipsychotic monotherapy, especially for patients with a first episode of schizophrenia, and the use of clozapine for treatment-resistant schizophrenia. By contrast, there were inconsistencies with regards to recommendations on maintenance antipsychotic treatment, with differences existing on type and dose of antipsychotic, as well as the duration of therapy. However, LAIs were consistently recommended, but mainly suggested in cases of nonadherence or patient preference, despite their established efficacy in broader patient populations and clinical scenarios in clinical trials. Guidelines were sometimes contradictory, with some recommending LAI use earlier in the disease course (e.g., first episode) and others suggesting they only be reserved for later in the disease. This inconsistency was not due to lack of evidence on the efficacy of LAIs in first-episode schizophrenia or the timing of the CPG, so that other reasons might be responsible, including possibly bias and stigma associated with this route of treatment administration. Lastly, gaps existed in the guidelines for recommendations on the duration of maintenance treatment, treatment of negative symptoms, and the development/use of treatment algorithms whenever evidence is sufficient to provide a simplified summary of the data and indicate their relevance for clinical decision making, all of which should be considered in future guideline development/revisions.
The SLR followed established best methods used in systematic review research to identify and assess the available CPGs for pharmacologic treatment of schizophrenia with antipsychotics in the acute and maintenance phases 80 , 81 . The SLR was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, including use of a prespecified protocol to outline methods for conducting the review. The protocol for this review was approved by all authors prior to implementation but was not submitted to an external registry.
Data sources and search algorithms
Searches were conducted by two independent investigators in the MEDLINE and Embase databases via OvidSP to identify CPGs published in English. Articles were identified using search algorithms that paired terms for schizophrenia with keywords for CPGs. Articles indexed as case reports, reviews, letters, or news were excluded from the searches. The database search was limited to CPGs published from January 1, 2004, through December 19, 2019, without limit to geographic location. In addition to the database sources, guideline body websites and state-level health departments from the US were also searched for relevant CPGs published through June 2020. A manual check of the references of recent (i.e., published in the past three years), relevant SLRs and relevant practice CPGs was conducted to supplement the above searches and ensure and the most complete CPG retrieval.
This study did not involve human subjects as only published evidence was included in the review; ethical approval from an institution was therefore not required.
Selection of CPGs for inclusion
Each title and abstract identified from the database searches was screened and selected for inclusion or exclusion in the SLR by two independent investigators based on the populations, interventions/comparators, outcomes, study design, time period, language, and geographic criteria shown in Table 4 . During both rounds of the screening process, discrepancies between the two independent reviewers were resolved through discussion, and a third investigator resolved any disagreement. Articles/documents identified by the manual search of organizational websites were screened using the same criteria. All accepted studies were required to meet all inclusion criteria and none of the exclusion criteria. Only the most recent version of organizational CPGs was included for data extraction.
Data extraction and synthesis
Information on the recommendations regarding the antipsychotic management in the acute and maintenance phases of schizophrenia and related benefits and harms was captured from the included CPGs. Each guideline was reviewed and extracted by a single researcher and the data were validated by a senior team member to ensure accuracy and completeness. Additionally, each included CPG was assessed using the Appraisal of Guidelines for Research and Evaluation II (AGREE II) tool. Following extraction and validation, results were qualitatively summarized across CPGs.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The data that support the findings of the SLR are available from the corresponding author upon request.
Correll, C. U. & Schooler, N. R. Negative symptoms in schizophrenia: a review and clinical guide for recognition, assessment, and treatment. Neuropsychiatr. Dis. Treat. 16 , 519–534 (2020).
Article PubMed PubMed Central Google Scholar
Kahn, R. S. et al. Schizophrenia. Nat. Rev. Dis. Prim. 1 , 15067 (2015).
Article PubMed Google Scholar
Millan, M. J. et al. Altering the course of schizophrenia: progress and perspectives. Nat. Rev. Drug Discov. 15 , 485–515 (2016).
Article CAS PubMed Google Scholar
Huhn, M. et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and network meta-analysis. Lancet 394 , 939–951 (2019).
Article CAS PubMed PubMed Central Google Scholar
Kishimoto, T., Hagi, K., Nitta, M., Kane, J. M. & Correll, C. U. Long-term effectiveness of oral second-generation antipsychotics in patients with schizophrenia and related disorders: a systematic review and meta-analysis of direct head-to-head comparisons. World Psychiatry 18 , 208–224 (2019).
Leucht, S. et al. Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis. Lancet 379 , 2063–2071 (2012).
Carbon, M. & Correll, C. U. Clinical predictors of therapeutic response to antipsychotics in schizophrenia. Dialogues Clin. Neurosci. 16 , 505–524 (2014).
Correll, C. U., Rubio, J. M. & Kane, J. M. What is the risk-benefit ratio of long-term antipsychotic treatment in people with schizophrenia? World Psychiatry 17 , 149–160 (2018).
Emsley, R., Chiliza, B., Asmal, L. & Harvey, B. H. The nature of relapse in schizophrenia. BMC Psychiatry 13 , 50 (2013).
Correll, C. U. & Kane, J. M. Ranking antipsychotics for efficacy and safety in schizophrenia. JAMA Psychiatry 77 , 225–226 (2020).
Kane, J. M. & Correll, C. U. Pharmacologic treatment of schizophrenia. Dialogues Clin. Neurosci. 12 , 345–357 (2010).
Kane, J. M., Kishimoto, T. & Correll, C. U. Non-adherence to medication in patients with psychotic disorders: epidemiology, contributing factors and management strategies. World Psychiatry 12 , 216–226 (2013).
Correll, C. U. et al. The use of long-acting injectable antipsychotics in schizophrenia: evaluating the evidence. J. Clin. Psychiatry 77 , 1–24 (2016).
Remington, G. et al. Guidelines for the pharmacotherapy of schizophrenia in adults. Can. J. Psychiatry 62 , 604–616 (2017).
American Psychiatric Association. Treatment recommendations for patients with schizophrenia. Am. J. Psychiatry 161 , 1–56 (2004).
Institute of Medicine (US) Committee to Advise the Public Health Service on Clinical Practice Guidelines, Field, M. J., & Lohr, K. N. (Eds.). Clinical Practice Guidelines: Directions for a New Program. (National Academies Press (US), 1990).
American Psychiatric Association. Practice Guideline for the Treatment of Patients With Schizophrenia , 3rd edn. (2021). https://doi.org/10.1176/appi.books.9780890424841 .
Florida Medicaid Drug Therapy Management Program. 2019–2020 Florida Best Practice Psychotherapeutic Medication Guidelines for Adults . (2020). Available at: https://floridabhcenter.org/wp-content/uploads/2021/04/2019-Psychotherapeutic-Medication-Guidelines-for-Adults-with-References_06-04-20.pdf .
Mental Health Clinical Advisory Group, Oregon Health Authority. Mental Health Care Guide for Licensed Practitioners and Mental Health Professionals. (2019). Available at: https://sharedsystems.dhsoha.state.or.us/DHSForms/Served/le7548.pdf .
Krogmann, A. et al. Keeping up with the therapeutic advances in schizophrenia: a review of novel and emerging pharmacological entities. CNS Spectr. 24 , 38–69 (2019).
Fountoulakis, K. N. et al. The report of the joint WPA/CINP workgroup on the use and usefulness of antipsychotic medication in the treatment of schizophrenia. CNS Spectr . https://doi.org/10.1017/S1092852920001546 (2020).
Leucht, S. et al. CINP Schizophrenia Guidelines . (CINP, 2013). Available at: https://www.cinp.org/resources/Documents/CINP-schizophrenia-guideline-24.5.2013-A-C-method.pdf .
Ostuzzi, G. et al. Mapping the evidence on pharmacological interventions for non-affective psychosis in humanitarian non-specialised settings: A UNHCR clinical guidance. BMC Med. 15 , 197 (2017).
Hasan, A. et al. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for Biological Treatment of Schizophrenia, Part 1: Update 2012 on the acute treatment of schizophrenia and the management of treatment resistance. World J. Biol. Psychiatry 13 , 318–378 (2012).
Hasan, A. et al. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for Biological Treatment of Schizophrenia, Part 2: Update 2012 on the long-term treatment of schizophrenia and management of antipsychotic-induced side effects. World J. Biol. Psychiatry 14 , 2–44 (2013).
Hasan, A. et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of schizophrenia - a short version for primary care. Int. J. Psychiatry Clin. Pract. 21 , 82–90 (2017).
Moore, T. A. et al. The Texas Medication Algorithm Project antipsychotic algorithm for schizophrenia: 2006 update. J. Clin. Psychiatry 68 , 1751–1762 (2007).
Texas Medication Algorithm Project (TMAP). Texas Medication Algorithm Project (TMAP) Procedural Manual . (2008). Available at: https://jpshealthnet.org/sites/default/files/inline-files/tmapalgorithmforschizophrenia.pdf .
American Association of Community Psychiatrists (AACP). Clinical Tips Series, Long Acting Antipsychotic Medications. (2017). Accessed at: https://drive.google.com/file/d/1unigjmjFJkqZMbaZ_ftdj8oqog49awZs/view .
Buchanan, R. W. et al. The 2009 schizophrenia PORT psychopharmacological treatment recommendations and summary statements. Schizophr. Bull. 36 , 71–93 (2010).
Kreyenbuhl, J. et al. The Schizophrenia Patient Outcomes Research Team (PORT): updated treatment recommendations 2009. Schizophr. Bull. 36 , 94–103 (2010).
New Jersey Division of Mental Health Services. Pharmacological Practice Guidelines for the Treatment of Schizophrenia . (2005). Available at: https://www.state.nj.us/humanservices/dmhs_delete/consumer/NJDMHS_Pharmacological_Practice_Guidelines762005.pdf .
Barnes, T. R. et al. Evidence-based guidelines for the pharmacological treatment of schizophrenia: updated recommendations from the British Association for Psychopharmacology. J. Psychopharmacol. 34 , 3–78 (2020).
National Institute for Health and Care Excellence (NICE). Psychosis and schizophrenia in adults: prevention and management. (2014). Available at: http://www.nice.org.uk/guidance/cg178 .
Scottish Intercollegiate Guidelines Network (SIGN). Management of Schizophrenia: A National Clinical Guideline . (2013). Available at: https://www.sign.ac.uk/assets/sign131.pdf .
Verma, S. et al. Ministry of Health Clinical Practice Guidelines: Schizophrenia. Singap. Med. J. 52 , 521–526 (2011).
CAS Google Scholar
Szulc, A. et al. Recommendations for the treatment of schizophrenia with negative symptoms. Standards of pharmacotherapy by the Polish Psychiatric Association (Polskie Towarzystwo Psychiatryczne), part 1. Rekomendacje dotyczace leczenia schizofrenii z. objawami negatywnymi. Stand. farmakoterapii Polskiego Tow. Psychiatrycznego, czesc 1. 53 , 497–524 (2019).
Google Scholar
Szulc, A. et al. Recommendations for the treatment of schizophrenia with negative symptoms. Standards of pharmacotherapy by the Polish Psychiatric Association (Polskie Towarzystwo Psychiatryczne), part 2. Rekomendacje dotyczace leczenia schizofrenii z. objawami negatywnymi. Stand. farmakoterapii Polskiego Tow. Psychiatrycznego, czesc 2. 53 , 525–540 (2019).
Galletly, C. et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the management of schizophrenia and related disorders. Aust. N. Z. J. Psychiatry 50 , 410–472 (2016).
Llorca, P. M. et al. Guidelines for the use and management of long-acting injectable antipsychotics in serious mental illness. BMC Psychiatry 13 , 340 (2013).
De Masi, S. et al. The Italian guidelines for early intervention in schizophrenia: development and conclusions. Early Intervention Psychiatry 2 , 291–302 (2008).
Article Google Scholar
Barnes, T. R. Evidence-based guidelines for the pharmacological treatment of schizophrenia: recommendations from the British Association for Psychopharmacology. J. Psychopharmacol. 25 , 567–620 (2011).
Correll, C. U. et al. Efficacy of 42 pharmacologic cotreatment strategies added to antipsychotic monotherapy in schizophrenia: systematic overview and quality appraisal of the meta-analytic evidence. JAMA Psychiatry 74 , 675–684 (2017).
Galling, B. et al. Antipsychotic augmentation vs. monotherapy in schizophrenia: systematic review, meta-analysis and meta-regression analysis. World Psychiatry 16 , 77–89 (2017).
Pillinger, T. et al. Comparative effects of 18 antipsychotics on metabolic function in patients with schizophrenia, predictors of metabolic dysregulation, and association with psychopathology: a systematic review and network meta-analysis. Lancet Psychiatry 7 , 64–77 (2020).
Rummel-Kluge, C. et al. Second-generation antipsychotic drugs and extrapyramidal side effects: a systematic review and meta-analysis of head-to-head comparisons. Schizophr. Bull. 38 , 167–177 (2012).
Angermeyer, M. C. & Matschinger, H. Attitude of family to neuroleptics. Psychiatr. Prax. 26 , 171–174 (1999).
CAS PubMed Google Scholar
Dibonaventura, M., Gabriel, S., Dupclay, L., Gupta, S. & Kim, E. A patient perspective of the impact of medication side effects on adherence: results of a cross-sectional nationwide survey of patients with schizophrenia. BMC Psychiatry 12 , 20 (2012).
McIntyre, R. S. Understanding needs, interactions, treatment, and expectations among individuals affected by bipolar disorder or schizophrenia: the UNITE global survey. J. Clin. Psychiatry 70 (Suppl 3), 5–11 (2009).
Tandon, R. et al. The impact on functioning of second-generation antipsychotic medication side effects for patients with schizophrenia: a worldwide, cross-sectional, web-based survey. Ann. Gen. Psychiatry 19 , 42 (2020).
Zhang, J. P. et al. Efficacy and safety of individual second-generation vs. first-generation antipsychotics in first-episode psychosis: a systematic review and meta-analysis. Int. J. Neuropsychopharmacol. 16 , 1205–1218 (2013).
Zhu, Y. et al. Antipsychotic drugs for the acute treatment of patients with a first episode of schizophrenia: a systematic review with pairwise and network meta-analyses. Lancet Psychiatry 4 , 694–705 (2017).
Kishimoto, T. et al. Relapse prevention in schizophrenia: a systematic review and meta-analysis of second-generation antipsychotics versus first-generation antipsychotics. Mol. Psychiatry 18 , 53–66 (2013).
Leucht, S. et al. Sixty years of placebo-controlled antipsychotic drug trials in acute schizophrenia: systematic review, Bayesian meta-analysis, and meta-regression of efficacy predictors. Am. J. Psychiatry 174 , 927–942 (2017).
Samara, M. T., Nikolakopoulou, A., Salanti, G. & Leucht, S. How many patients with schizophrenia do not respond to antipsychotic drugs in the short term? An analysis based on individual patient data from randomized controlled trials. Schizophr. Bull. 45 , 639–646 (2019).
Zhu, Y. et al. How well do patients with a first episode of schizophrenia respond to antipsychotics: a systematic review and meta-analysis. Eur. Neuropsychopharmacol. 27 , 835–844 (2017).
Bogers, J. P. A. M., Hambarian, G., Michiels, M., Vermeulen, J. & de Haan, L. Risk factors for psychotic relapse after dose reduction or discontinuation of antipsychotics in patients with chronic schizophrenia. A systematic review and meta-analysis. Schizophr. Bull. Open 46 , Suppl 1 S326 (2020).
Tani, H. et al. Factors associated with successful antipsychotic dose reduction in schizophrenia: a systematic review of prospective clinical trials and meta-analysis of randomized controlled trials. Neuropsychopharmacology 45 , 887–901 (2020).
Uchida, H., Suzuki, T., Takeuchi, H., Arenovich, T. & Mamo, D. C. Low dose vs standard dose of antipsychotics for relapse prevention in schizophrenia: meta-analysis. Schizophr. Bull. 37 , 788–799 (2011).
Howes, O. D. et al. Treatment-resistant schizophrenia: treatment response and resistance in psychosis (TRRIP) working group consensus guidelines on diagnosis and terminology. Am. J. Psychiatry 174 , 216–229 (2017).
Masuda, T., Misawa, F., Takase, M., Kane, J. M. & Correll, C. U. Association with hospitalization and all-cause discontinuation among patients with schizophrenia on clozapine vs other oral second-generation antipsychotics: a systematic review and meta-analysis of cohort studies. JAMA Psychiatry 76 , 1052–1062 (2019).
Siskind, D., McCartney, L., Goldschlager, R. & Kisely, S. Clozapine v. first- and second-generation antipsychotics in treatment-refractory schizophrenia: systematic review and meta-analysis. Br. J. Psychiatry 209 , 385–392 (2016).
Siskind, D., Siskind, V. & Kisely, S. Clozapine response rates among people with treatment-resistant schizophrenia: data from a systematic review and meta-analysis. Can. J. Psychiatry 62 , 772–777 (2017).
Wang, G. et al. ECT augmentation of clozapine for clozapine-resistant schizophrenia: a meta-analysis of randomized controlled trials. J. Psychiatr. Res. 105 , 23–32 (2018).
Tiihonen, J., Tanskanen, A. & Taipale, H. 20-year nationwide follow-up study on discontinuation of antipsychotic treatment in first-episode schizophrenia. Am. J. Psychiatry 175 , 765–773 (2018).
Taipale, H. et al. Antipsychotics and mortality in a nationwide cohort of 29,823 patients with schizophrenia. Schizophr. Res . 197 , 274–280 (2018).
Taipale, H. et al. 20-year follow-up study of physical morbidity and mortality in relationship to antipsychotic treatment in a nationwide cohort of 62,250 patients with schizophrenia (FIN20). World Psychiatry 19 , 61–68 (2020).
Carbon, M. & Correll, C. U. Thinking and acting beyond the positive: the role of the cognitive and negative symptoms in schizophrenia. CNS Spectr. 19 (Suppl 1), 38–52 (2014).
PubMed Google Scholar
Krause, M. et al. Antipsychotic drugs for patients with schizophrenia and predominant or prominent negative symptoms: a systematic review and meta-analysis. Eur. Arch. Psychiatry Clin. Neurosci. 268 , 625–639 (2018).
Kane, J. M. et al. Effect of long-acting injectable antipsychotics vs usual care on time to first hospitalization in early-phase schizophrenia: a randomized clinical trial. JAMA Psychiatry 77 , 1217–1224 (2020).
Schreiner, A. et al. Paliperidone palmitate versus oral antipsychotics in recently diagnosed schizophrenia. Schizophr. Res. 169 , 393–399 (2015).
Subotnik, K. L. et al. Long-acting injectable risperidone for relapse prevention and control of breakthrough symptoms after a recent first episode of schizophrenia. A randomized clinical trial. JAMA Psychiatry 72 , 822–829 (2015).
Tiihonen, J. et al. A nationwide cohort study of oral and depot antipsychotics after first hospitalization for schizophrenia. Am. J. Psychiatry 168 , 603–609 (2011).
Zhang, F. et al. Efficacy, safety, and impact on hospitalizations of paliperidone palmitate in recent-onset schizophrenia. Neuropsychiatr. Dis. Treat. 11 , 657–668 (2015).
Kishimoto, T., Nitta, M., Borenstein, M., Kane, J. M. & Correll, C. U. Long-acting injectable versus oral antipsychotics in schizophrenia: a systematic review and meta-analysis of mirror-image studies. J. Clin. Psychiatry 74 , 957–965 (2013).
Kishimoto, T. et al. Effectiveness of long-acting injectable vs oral antipsychotics in patients with schizophrenia: a meta-analysis of prospective and retrospective cohort studies. Schizophr. Bull. 44 , 603–619 (2018).
Kishimoto, T. et al. Long-acting injectable vs oral antipsychotics for relapse prevention in schizophrenia: a meta-analysis of randomized trials. Schizophr. Bull. 40 , 192–213 (2014).
Kane, J. M., Kishimoto, T. & Correll, C. U. Assessing the comparative effectiveness of long-acting injectable vs. oral antipsychotic medications in the prevention of relapse provides a case study in comparative effectiveness research in psychiatry. J. Clin. Epidemiol. 66 , S37–41 (2013).
Kishimoto, T., Hagi, K., Kurokawa, S., Kane, J. M. & Correll, C. U. Long-acting injectable versus oral antipsychotics for the maintenance treatment of schizophrenia: a systematic review and comparative meta-analysis of randomised, cohort, and pre-post studies. Lancet Psychiatry 8 , 387–404 (2021).
Cook, D. J., Mulrow, C. D. & Haynes, R. B. Systematic reviews: synthesis of best evidence for clinical decisions. Ann. Intern. Med. 126 , 376–380 (1997).
Higgins, J. P. T. & Green, S. Cochrane Collaboration Handbook for Systematic Reviews of Interventions . (The Cochrane Collaboration and John Wiley & Sons, Ltd, 2008).
Download references
Acknowledgements
This study received financial funding from Janssen Scientific Affairs.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
The Zucker Hillside Hospital, Department of Psychiatry, Northwell Health, Glen Oaks, NY, USA
- Christoph U. Correll
Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Department of Psychiatry and Molecular Medicine, Hempstead, NY, USA
Charité Universitätsmedizin Berlin, Department of Child and Adolescent Psychiatry, Berlin, Germany
Evidera, Waltham, MA, USA
Amber Martin & Emma Schiller
Janssen Scientific Affairs, LLC, Titusville, NJ, USA
Charmi Patel, Carmela Benson, Jennifer Kern-Sliwa & Kruti Joshi
Goulding HEOR Consulting Inc., Vancouver, BC, Canada
Rebecca Goulding
Biohaven Pharmaceuticals, New Haven, CT, USA
You can also search for this author in PubMed Google Scholar
Contributions
C.C., A.M., R.G., C.P., C.B., K.J., J.K.S., E.S. and E.K. contributed to the conception and the design of the study. A.M., R.G. and E.S. conducted the literature review, including screening, and extraction of the included guidelines. All authors contributed to the interpretations of the results for the review; A.M. and C.C. drafted the manuscript and all authors revised it critically for intellectual content. All authors gave their final approval of the completed manuscript.
Corresponding author
Correspondence to Christoph U. Correll .
Ethics declarations
Competing interests.
C.C. has received personal fees from Alkermes plc, Allergan plc, Angelini Pharma, Gedeon Richter, Gerson Lehrman Group, Intra-Cellular Therapies, Inc, Janssen Pharmaceutica/Johnson & Johnson, LB Pharma International BV, H Lundbeck A/S, MedAvante-ProPhase, Medscape, Neurocrine Biosciences, Noven Pharmaceuticals, Inc, Otsuka Pharmaceutical Co, Inc, Pfizer, Inc, Recordati, Rovi, Sumitomo Dainippon Pharma, Sunovion Pharmaceuticals, Inc, Supernus Pharmaceuticals, Inc, Takeda Pharmaceutical Company Limited, Teva Pharmaceuticals, Acadia Pharmaceuticals, Inc, Axsome Therapeutics, Inc, Indivior, Merck & Co, Mylan NV, MedInCell, and Karuna Therapeutics and grants from Janssen Pharmaceutica, Takeda Pharmaceutical Company Limited, Berlin Institute of Health, the National Institute of Mental Health, Patient Centered Outcomes Research Institute, and the Thrasher Foundation outside the submitted work; receiving royalties from UpToDate; and holding stock options in LB Pharma. A.M., R.G., and E.S. were all employees of Evidera at the time the study was conducted on which the manuscript was based. C.P., C.B., K.J., J.K.S., and E.K. were all employees of Janssen Scientific Affairs, who hold stock/shares, at the time the study was conducted.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information, reporting summary, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Correll, C.U., Martin, A., Patel, C. et al. Systematic literature review of schizophrenia clinical practice guidelines on acute and maintenance management with antipsychotics. Schizophr 8 , 5 (2022). https://doi.org/10.1038/s41537-021-00192-x
Download citation
Received : 26 February 2021
Accepted : 02 November 2021
Published : 24 February 2022
DOI : https://doi.org/10.1038/s41537-021-00192-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Psychosis superspectrum ii: neurobiology, treatment, and implications.
- Roman Kotov
- William T. Carpenter
- Katherine G. Jonas
Molecular Psychiatry (2024)
Delphi panel to obtain clinical consensus about using long-acting injectable antipsychotics to treat first-episode and early-phase schizophrenia: treatment goals and approaches to functional recovery
- Celso Arango
- Andrea Fagiolini
BMC Psychiatry (2023)
Machine learning methods to predict outcomes of pharmacological treatment in psychosis
- Lorenzo Del Fabro
- Elena Bondi
- Paolo Brambilla
Translational Psychiatry (2023)
Comparison of clinical outcomes in patients with schizophrenia following different long-acting injectable event-driven initiation strategies
- Carmela Benson
- Panagiotis Mavros
Schizophrenia (2023)
Early Non-Response to Antipsychotic Treatment in Schizophrenia: A Systematic Review and Meta-Analysis of Evidence-Based Management Options
- Jose M. Rubio
- Daniel Guinart
CNS Drugs (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Call to +1 844 889-9952
110 Schizophrenia Research Topics & Essay Examples
📝 schizophrenia research papers examples, 🏆 best schizophrenia essay titles, 🎓 simple research topics about schizophrenia, ❓ schizophrenia research questions, 📣 schizophrenia discussion questions.
- Clozapine Treatment for Paranoid Schizophrenia Clozapine would be an effective choice for Caitlyn since this medication is prescribed for individuals suffering from severe forms of schizophrenia.
- Adult Psychiatry: Schizophrenia in Quadruplets Four Genain quadruplets developed schizophrenia, but the course of the disease was different for each of them.
- Geriatric Mental Health: Dementia & Schizophrenia This paper reviews the case study of a 67-year-old patient admitted to a hospital with agitation, hallucinations, and paranoia after a medication course.
- Different Methods of Treating Schizophrenia Schizophrenia is a disorder that disables the brain in a severe and chronic manner. This paper examine the different treatments of Schizophrenia and their effectiveness and side effects.
- Schizophrenia: Cause, Consequence, Care Being one of the most widespread mental disorders in terms of identifying major symptoms, schizophrenia still remains quite complicated when it comes to the etiology examination.
- Positive and Negative Symptoms of Schizophrenia
- Dysregulated but Not Decreased Salience Network Activity in Schizophrenia
- Treatment Intervention for Paranoid Schizophrenia
- Biological and Cognitive Approaches for the Treatment of Schizophrenia
- Schizophrenia, Psychosis and Lifespan Development It can easily be assumed that schizophrenia, psychosis, and childhood and lifespan developmental disorders do not have much in common.
- Schizophrenia and Its Effects on the Way People Interpret
- Schizophrenia and Cortical Blindness: Protective Effects and Implications for Language
- Treatment-Resistant Schizophrenia: Genetic and Neuroimaging Correlates
- Definitions and Social Perceptions of Schizophrenia
- Hippocampus and Schizophrenia Causes
- Death Penalty Mitigation Assessment The results of the assessments might be used to evaluate the defendant and obtain mitigation evidence to reduce the degree of guilt.
- Disorganized Schizophrenia and Its Effects on Children
- Disorganized Schizophrenia and Methodist Unity Point
- Schizophrenia, Substance Abuse, and Violent Crime
- Functional Connectivity Density Alterations in Schizophrenia
- Schizophrenia and Its Effects on Young Children and Adolescents
- Psychological Disorders: Schizophrenia Schizophrenia is a condition that severely affects person’s thought process, speech, perception of reality, emotions, and actions.
- Hispanic and Urban Black Populations and Schizophrenia
- Attention and Multisensory Integration of Emotions in Schizophrenia
- Negative Symptoms and Hypofrontality in Chronic Schizophrenia
- Resilience and Cognitive Function in Patients With Schizophrenia and Bipolar Disorder, and Healthy Controls
- Schizophrenia and Family Interventions
- Schizophrenia and Anti-Social Personality Disorder
- White Matter Measures and Cognition in Schizophrenia
- Clinical Practice on Schizophrenia Family Work
- Neurocognitive Decrements Are Present in Intellectually Superior Schizophrenia
- Altered Cerebral Blood Flow Covariance Network in Schizophrenia
- Schizophrenia and Its Effects on the Development of Schizophrenia
- Schizophrenia, Bipolar Disorder and Antidepressants The variety of mental disorders may often confuse terms of disease differentiation due to the lack of proper education. Schizophrenia and bipolar disorder are examples of such confusion.
- Dopamine, Psychosis and Schizophrenia: The Widening Gap Between Basic and Clinical Neuroscience
- Psychosocial Rehabilitation for Schizophrenia
- Psychology: Schizophrenia and Widely Used Treatments
- Chronicity and Sex Affect Genetic Risk Prediction in Schizophrenia
- Paranoid Schizophrenia and Nursing Interventions
- Perinatal Factors and Schizophrenia
- Altered Basal Ganglia Network Integration in Schizophrenia
- Schizophrenia Stigmas, Causes, and Brain Activity Differences
- Schizophrenia: Psychological and Psychiatric Views Schizophrenia is a chronic severe brain disorder characterized by altered perception and the manner of expression of reality. The effects are manifested as hearing voices.
- Antipsychotics, Metabolic Adverse Effects, and Cognitive Function in Schizophrenia
- Schizoaffective Disorder: The Bridge Between Schizophrenia and Bipolar
- Dysfunctional Brain Networks and Genetic Risk for Schizophrenia
- Demystifying Common Misconceptions About Schizophrenia
- Schizophrenia and Emergency Room Costs
- Schizophrenia and Causes for This Complex and Puzzling Illness
- Antigliadin Antibodies Relation to Neurochemistry in Schizophrenia
- How Do Gray Matter Effects Schizophrenia and Bipolar Disorder?
- What Is the Role of Brexpiprazole in the Management of Schizophrenia?
- Can Exercise Increase Fitness and Reduce Weight in Patients With Schizophrenia and Depression?
- How Is Near Cognitive Correction for Schizophrenia Performed?
- How Does Smoking Affect Schizophrenia?
- How Can Nurses Deal With a Patient With Paranoid Schizophrenia?
- Are People With Schizophrenia Dangerous and Unpredictable?
- Are Patients With Schizophrenia Impaired in Processing Non-emotional Features of Human Faces?
- What Is the Relationship Between Schizophrenia and Crime?
- Schizophrenia and Medication Adherence and Health Care?
- Is Early Intervention Occupational Therapy Effective for Schizophrenia?
- How Will the Mild Encephalitis Hypothesis of Schizophrenia Influence Stigmatization?
- What Are the Major Main Barriers to Treatment That Someone With Schizophrenia?
- How Do Environmental Factors Affect the Development of Schizophrenia?
- How To Reduce Social Interaction Anxiety in Schizophrenia?
- What Are the Environmental and Genetic Effects of Schizophrenia?
- What Is the Diagnosis of the Etiology of Schizophrenia?
- What Is the Relationship Between Violence and Schizophrenia?
- Biological and Environmental Factors for Schizophrenia?
- What Are the Current Controversies in the Treatment of Schizophrenia?
- Non-pharmacological Interventions for Schizophrenia: How Much Can Be Achieved and How?
- How Is Schizophrenia Imaging With Voxel-based Morphometry?
- What Are the Genetic Risk Factors for Schizophrenia?
- Subjective and Objective Cognitive Dysfunction in Schizophrenia Is There a Link?
- What Is the Modified Volume and Functional Connectivity of the Habenula in Schizophrenia?
- What Are False Memories of Affective Information in Schizophrenia?
- How Schizophrenia Affects the Lifespan?
- What Mechanism Underlies Schizophrenia?
- Are Bipolar Disorder and Schizophrenia Neuroanatomically Distinct?
- Does Non-adherence Increase Treatment Costs in Schizophrenia?
- Why Is Schizophrenia Considered a Complex and Multifaceted Disorder?
- How Do Genetic Factors Contribute to the Risk of Developing Schizophrenia?
- What Are the Subtypes of Schizophrenia?
- Are There Gender Differences in the Prevalence and Manifestation of Schizophrenia?
- At What Age Do the Symptoms of Schizophrenia Appear?
- What Are the Primary Positive Symptoms of Schizophrenia, and How Do They Manifest?
- How Is Schizophrenia Diagnosed and Treated?
- Why Is the Age of Onset of Schizophrenia an Important Factor in Understanding Its Course?
- Can Electrical Stimulation Improve Cognition in People Living with Schizophrenia?
- Is It Possible to Prevent Schizophrenia?
- What Is the Relationship Between Substance Abuse and the Development of Schizophrenia?
- Can Schizophrenia Be Caused by Trauma?
- What Challenges Do Clinicians Face in Diagnosing Schizophrenia Accurately?
- What Therapy Is Best for Schizophrenia?
- Does Schizophrenia Get Worse with Age?
- What Role Do Psychosocial Interventions Play in the Overall Treatment of Schizophrenia?
- Can Schizophrenia Be Treated Without Medication?
- Are Antipsychotic Medications Effective in Addressing the Symptoms of Schizophrenia?
- Can Schizophrenia Cause Memory Loss?
- How Does Schizophrenia Impact Family Dynamics and Relationships?
- Can a Blood Test Detect Schizophrenia?
- What Ethical Considerations Arise in the Treatment of Individuals with Schizophrenia?
- Can Brain Surgery Cure Schizophrenia?
- How Do Cultural Factors Influence the Experience and Perception of Schizophrenia?
- Does Schizophrenia Cause Brain Damage?
- Is There a Correlation Between Schizophrenia and Violent Behavior?
- Why Is Schizophrenia More Common in Males?
- How Does Schizophrenia Impact Employment and an Individual’s Ability to Maintain Work?
- What Is the Latest Treatment for Schizophrenia?
- Why Are Peer Support Programs Valuable for Individuals Living With Schizophrenia?
Cite this page
Select style
- Chicago (A-D)
- Chicago (N-B)
NursingBird. (2023, October 5). 110 Schizophrenia Research Topics & Essay Examples. https://nursingbird.com/topics/schizophrenia-research-topics/
"110 Schizophrenia Research Topics & Essay Examples." NursingBird , 5 Oct. 2023, nursingbird.com/topics/schizophrenia-research-topics/.
NursingBird . (2023) '110 Schizophrenia Research Topics & Essay Examples'. 5 October.
NursingBird . 2023. "110 Schizophrenia Research Topics & Essay Examples." October 5, 2023. https://nursingbird.com/topics/schizophrenia-research-topics/.
1. NursingBird . "110 Schizophrenia Research Topics & Essay Examples." October 5, 2023. https://nursingbird.com/topics/schizophrenia-research-topics/.
Bibliography
NursingBird . "110 Schizophrenia Research Topics & Essay Examples." October 5, 2023. https://nursingbird.com/topics/schizophrenia-research-topics/.
- Human Papillomavirus
Explore 185+ Schizophrenia Research Paper Topics for In-Depth Analysis
Nov 12, 2023

Nov 12, 2023 | Topics
Embarking on a journey into the world of schizophrenia research paper topics is like stepping into a puzzle with many pieces waiting to be explored. Wondering about the complexities of this mental health condition and what it means for those affected? Well, you’re not alone. In my experience, delving into schizophrenia topics typically involves unraveling various facets, from understanding its symptoms to exploring potential treatment avenues. Have you ever questioned how genetics might play a role in schizophrenia or perhaps pondered the impact of environmental factors? Investigating these aspects not only broadens our understanding but also opens the door to discussions about stigma and support for those facing this challenge. So, let’s dive into the diverse realm of schizophrenia research, where every topic holds the potential to shed light on this intricate condition.
People Also Read
- Explore 171+ Anthropology Research Topics | Uncover the Secrets of Human Culture
- 88+ Western Civilization Research Paper Topics | Expert Recommendations
- 100+ Public Administration Research Paper Topics You Can Use
Best Schizophrenia Research Paper Topics
- Genetic Factors in the Development of Schizophrenia: Unraveling the Complex Puzzle
- Exploring the Onset of Schizophrenia: Early Signs and Predictors
- Psychosis Beyond Perception: Understanding the Various Facets
- The Etiology of Schizophrenia: An In-Depth Examination
- Risk Factors Associated with the Development of Schizophrenia
- Psychiatry and Schizophrenia: A Holistic Approach to Treatment
- Hallucination in Schizophrenia: Examining the Distorted Realities
- Delusions in Patients with Schizophrenia: A Comprehensive Analysis
- The Spectrum Disorder: Navigating the Complexity of Schizophrenia
- Negative Symptoms in Schizophrenia: Impact on Daily Functioning
- Positive Symptoms of Schizophrenia: Unmasking the Manifestations
- Treatment Approaches for People with Schizophrenia: Current Perspectives
- Psychotic Disorders Within the Schizophrenia Spectrum: Distinguishing Characteristics
- The Role of Mental Disorders in Shaping Schizophrenia: A Multifaceted Exploration
- Understanding Schizophrenic Individuals: Bridging the Gap of Misconceptions
- Exploring Different Therapeutic Avenues in the Treatment of Schizophrenia
- Schizophrenia and Its Impact on the Social Lives of Individuals
- The Relationship Between Developmental Factors and Schizophrenia Onset
- Addressing Negative Stigmas Surrounding People with Schizophrenia
- The Interplay of Genetic and Environmental Factors in Schizophrenia Risk
Interesting Schizophrenia Research Paper Topics
- Examining the Onset of Schizophrenia: Early Indicators and Predictors
- The Heterogeneous Nature of Schizophrenia: A Comprehensive Overview
- Impact of Schizophrenia on Daily Life: Unraveling the Challenges Faced by Individuals
- Etiology of Schizophrenia: Investigating the Underlying Causes
- Schizophrenia Spectrum Disorders: Navigating the Diverse Manifestations
- Understanding the Abnormalities Associated with Schizophrenia
- The Chronic Nature of Schizophrenia: Long-Term Implications for Patients
- Bipolar Disorder and Schizophrenia: Overlapping Symptoms and Distinctions
- Therapeutic Approaches for Schizophrenia: Current Trends and Innovations
- Exploring the Future of Schizophrenia Research: Emerging Areas of Interest
- Impact of Schizophrenia on Social and Interpersonal Relationships
- Diagnosing Schizophrenia: Challenges and Advances in Clinical Practice
- Integrating Psychotherapy into the Treatment of Individuals with Schizophrenia
- Investigating Psychotic Symptoms in Schizophrenia: Beyond Hallucinations
- The Role of Therapy in Alleviating Schizophrenia Symptoms
- Schizophrenia as a Serious Mental Health Challenge: Bridging Gaps in Understanding
- Unveiling the Abnormalities in Brain Functioning in Schizophrenia Patients
- Exploring Novel Approaches in Treating Schizophrenia: From Pharmacology to Psychotherapy
- The Intersection of Genetics and Environmental Factors in Schizophrenia Development
- Shifting Perspectives: Redefining the Diagnosis and Treatment of Schizophrenia
Simple Schizophrenia Research Paper Topics
- The Impact of Schizophrenia on Daily Life: Simple Insights into Everyday Challenges
- Treatment Approaches for Individuals Developing Schizophrenia: Simplifying Complex Solutions
- Unraveling the Chronic Nature of Schizophrenia: A Basic Understanding
- How Schizophrenia Affects Relationships: A Simple Exploration
- A Primer on Schizophrenia Development: Understanding the Basics
- Simplifying the Treatment Maze: Navigating Therapeutic Options for Schizophrenia
- Schizophrenia and Its Long-term Effects: Breaking Down the Basics
- Addressing Misconceptions: Schizophrenia’s Impact on Cognitive Abilities
- A Closer Look at the Chronicity of Schizophrenia: Basic Concepts
- The Simple Facts: Treatment Modalities for Individuals with Schizophrenia
- Exploring the Emotional Impact of Schizophrenia on Individuals and Families
- Schizophrenia Development: Early Warning Signs Simplified
- Treatment Strategies for Managing Schizophrenia: Simplified Approaches
- Breaking Down the Basics: How Schizophrenia Affects Social Functioning
- A Simple Guide to Understanding the Chronic Nature of Schizophrenia
- Simplifying the Concept of Chronic Schizophrenia: Key Points for Awareness
- The Basics of Schizophrenia: Addressing Common Myths and Realities
- Exploring the Psychological Impact of Schizophrenia on Patients
- Basic Insights into the Chronicity of Schizophrenia: A Layman’s Perspective
- Simplifying Treatment Discussions: What Works for Schizophrenia?
Controversial Schizophrenia Research Paper Topics
- The Controversy Surrounding Treatment for Schizophrenia: Examining Divergent Perspectives
- Mental Disorder that Affects Emotional Expression: A Controversial Exploration
- Schizophrenia and Social Functioning: Debating the Impact on Interpersonal Relationships
- The Age Factor: Controversies in the Onset of Schizophrenia between 16 and 30
- Debunking Myths: Dispelling Misconceptions About How Schizophrenia Affects Thinking
- Controversial Approaches to Treating Schizophrenia: Beyond Traditional Methods
- Hallucinations and Delusions in Schizophrenia: A Contested Landscape
- The United States and Schizophrenia: Analyzing Controversial Trends and Patterns
- Schizophrenia’s Impact on Emotional Expression: A Debate in the Mental Health Community
- Evidence-Based Controversies: Assessing the Validity of Research on Schizophrenia
- Schizophrenia Patients’ Experience: Unraveling the Controversial Subjectivity
- Genetic and Environmental Influences on Schizophrenia: A Contested Interaction
- Controversial Perspectives on Schizophrenia Treatment: Clashes Between Researchers and Clinicians
- Social Functioning in Individuals with Schizophrenia: A Controversial Paradigm
- Exploring Non-Traditional Approaches: Controversies in How Schizophrenia Is Treated
- Navigating Stigmas: Debates on the Social Perception of People with Schizophrenia
- Between Science and Society: The Controversy of Schizophrenia Research Funding
- Schizophrenia in Adolescents: Controversies Surrounding Diagnosis and Treatment
- The National Institute of Mental Health’s Role in Shaping Controversial Narratives on Schizophrenia
- Debunking Stereotypes: Controversies in How People with Schizophrenia May Seem to Others
Schizophrenia Research Paper Topics for Middle School
- Understanding Schizophrenia: What Middle Schoolers Need to Know
- Brain Basics: Exploring How Schizophrenia Affects a Person’s Thinking
- The Mystery of Voices: Hallucinations in Individuals with Schizophrenia
- Ages 16 to 30: Why is Schizophrenia More Common During This Time?
- The United States and Schizophrenia: How Many People Are Affected?
- Peer Perspectives: What It’s Like for Someone Suffering from Schizophrenia
- Comics and Facts: Breaking Down the Myths Around Schizophrenia
- Inside the Mind: Neurobiological Insights into Schizophrenia
- Coping with Schizophrenia: Strategies for Individuals and their Friends
- Talking About Mental Health: Why Understanding Schizophrenia Matters
Schizophrenia Research Paper Topics for High School
- The Neurobiology of Schizophrenia: A High School Exploration
- Social Stigma Surrounding Schizophrenia: Breaking Down Misconceptions
- Early Warning Signs: Recognizing Symptoms of Schizophrenia
- Treatment Modalities: Examining Therapeutic Approaches for Schizophrenia
- The Genetic Puzzle: Understanding Family Links to Schizophrenia
- Impact on Academic Performance: Schizophrenia’s Effect on High School Students
- Adolescence and Schizophrenia: Exploring the Vulnerability of this Age Group
- Innovative Therapies: Breakthroughs in Schizophrenia Treatment Research
- Media Representation: How Movies and TV Portray Schizophrenia
- Youth Advocacy: Raising Awareness and Support for Teens with Schizophrenia
Schizophrenia Research Paper Topics for College
- Exploring Genetic Markers in Schizophrenia: A Comprehensive Analysis
- Schizophrenia Spectrum Disorders: Examining Variations and Classifications
- The Impact of Environmental Factors on Schizophrenia Development
- Early Intervention Strategies: Enhancing Outcomes for Individuals at Risk
- Novel Therapeutic Approaches: Beyond Traditional Medications
- Social Stigma and Schizophrenia: Breaking Down Misconceptions
- Cognitive Impairment in Schizophrenia: Understanding and Addressing Challenges
- Technology and Mental Health: Innovations in Schizophrenia Research
- Integrating Psychotherapy into Schizophrenia Treatment Plans
- Cross-Cultural Perspectives on Schizophrenia: Examining Global Trends
- Neuroimaging Studies in Schizophrenia: Advancements and Applications
- The Role of Inflammation in Schizophrenia: A Contemporary Focus
- Trauma and Schizophrenia: Unraveling the Complex Relationship
- Assessing Social Functioning in Individuals with Schizophrenia
- The Intersection of Substance Use and Schizophrenia: Implications for Treatment
- Gender Differences in Schizophrenia: An In-depth Exploration
- Pharmacogenomics in Schizophrenia Treatment: Tailoring Medications to Individuals
- Psychosocial Rehabilitation Programs: Enhancing Quality of Life
- Schizophrenia Prevention Strategies: Addressing Early Warning Signs
- Ethical Considerations in Schizophrenia Research: Balancing Progress and Participant Well-being
Schizophrenia Research Paper Topics for Grad School
- Future Research Horizons in Schizophrenia: Emerging Frontiers and Paradigms
- Integrative Approaches to Therapy for Schizophrenia: Beyond Medication
- The Interface of Schizophrenia and Bipolar Disorder: Overlapping Features and Distinctions
- Mental Illnesses Comorbidity: Navigating Complex Clinical Presentations
- Understanding the Lived Experience: Insights from Someone with Schizophrenia
- Assessing the Risk of Schizophrenia: A Comprehensive Epidemiological Perspective
- The Evolution of the Diagnostic and Statistical Manual of Mental Disorders in Schizophrenia Research
- Serious Mental Illness and Schizophrenia: Defining Severity and Implications for Treatment
- Unraveling the Neural Mechanisms: Exploring Schizophrenia as a Brain Disorder
- The Phenomenon of Hearing Voices in Schizophrenia: Neuroscientific and Clinical Perspectives
- Advances in Psychopharmacology: Novel Targets and Drug Development for Schizophrenia
- From Genetics to Epigenetics: A Multilayered Exploration of Schizophrenia Etiology
- Cognitive Rehabilitation in Schizophrenia: Enhancing Neurocognitive Functioning
- Integrating Digital Health Solutions: Technology’s Role in Schizophrenia Management
- Schizophrenia and Social Cognition: Implications for Therapeutic Interventions
- Beyond Symptomatology: Investigating the Neurobiological Basis of Schizophrenia
- Early Intervention Strategies: Reducing the Long-Term Impact of Schizophrenia
- The Neurochemistry of Schizophrenia: Targeting Neurotransmitter Dysregulation
- Examining Schizophrenia in the Criminal Justice System: Challenges and Ethical Considerations
- Psychosocial Factors in Schizophrenia Treatment: Holistic Approaches for Optimal Outcomes
📝 Schizophrenia Research Papers Examples
- Exploring the Impact of Age on Rates of Schizophrenia Diagnosis in Clinical Settings
- The Prevalence of Schizophrenia in the United States: A Comprehensive Epidemiological Study
- Diagnostic Challenges: Unraveling the Characteristics of Schizophrenia in Patients Ages 16 to 30
- Schizophrenia and Mental Health Disorders: A Dual Analysis of Prevalence and Comorbidity
- Neurocognitive Dysfunction in Schizophrenic Patients: Implications for Treatment Strategies
- Understanding How Schizophrenia Affects Cognitive Processes: Insights from Clinical Research
- The Journal of Clinical Approaches to Schizophrenia: An Overview of Recent Research
- Unveiling the Interplay of Environmental Factors Involved in Schizophrenia Development
- Examining the Neurobiological Basis of Schizophrenia: Insights from Imaging Studies
- Gender Disparities in Rates of Schizophrenia Diagnosis: A Critical Examination
- Dissecting the Socioeconomic Factors Involved in the Prevalence of Schizophrenia
- A Comprehensive Analysis of Prevalence Rates and Clinical Profiles in Schizophrenia
- The Dynamics of Schizophrenia in Diagnosed Patients: A Longitudinal Study
- Investigating the Link Between Substance Use and the Onset of Schizophrenia
- Neurodevelopmental Perspectives on Schizophrenia: Insights into Early Manifestations and Interventions
🏆 Best Schizophrenia Essay Titles
- “Unraveling Minds: Navigating the Complexities of Schizophrenia”
- “Beyond Hallucinations: A Comprehensive Look at Schizophrenia Symptoms”
- “Breaking the Silence: Understanding the Impact of Schizophrenia”
- “Cognitive Conundrum: Exploring Neurological Aspects of Schizophrenia”
- “Shattered Perceptions: Social Stigma and Misunderstanding in Schizophrenia”
- “From Diagnosis to Treatment: A Journey Through Schizophrenia”
- “Ties That Bind: Investigating Genetic Influences on Schizophrenia”
- “Balancing Act: Addressing Schizophrenia’s Impact on Academic Performance”
- “Minds in Transition: Adolescence and the Vulnerability to Schizophrenia”
- “Beyond Medication: Exploring Holistic Approaches to Schizophrenia Treatment”

❓ Schizophrenia Research Questions
- What are the genetic factors contributing to the development of schizophrenia?
- How do environmental factors influence the onset and progression of schizophrenia?
- What are the most effective therapeutic approaches for managing schizophrenia symptoms?
- How does schizophrenia impact the cognitive functioning of affected individuals?
- Are there gender disparities in the prevalence and manifestation of schizophrenia?
- What role does social stigma play in shaping the experiences of people with schizophrenia?
- How can early warning signs of schizophrenia be recognized and addressed?
- What are the neurobiological mechanisms underlying hallucinations and delusions in schizophrenia?
- What innovative research is being conducted to improve the treatment of schizophrenia?
- How can societal attitudes and understanding of schizophrenia be improved to support affected individuals?
🎓 Simple Research Topics about Schizophrenia
- Neurobiology of Schizophrenia: Simplifying the Complexities
- Recognizing Early Warning Signs: A Simple Guide for Families
- Understanding Schizophrenia’s Impact on Daily Life
- Exploring Therapeutic Approaches: What Works Best for Patients?
- Family Connections: Investigating Genetic Links to Schizophrenia
- Social Stigma: Breaking Down Misconceptions About Schizophrenia
- The Role of Environmental Factors in Schizophrenia Development
- Navigating Adolescence: How Schizophrenia Affects Teens
- Media Influence: How Movies Portray Schizophrenia
- Coping Strategies for Individuals Living with Schizophrenia
Get Help With Your Schizophrenia Research Paper
Struggling with your schizophrenia research paper? Fret not! Essay Freelance Writers stands out as the go-to source for top-notch assistance. Wondering why we claim to be the best? Well, our expert writers are seasoned professionals well-versed in the complexities of schizophrenia. Need help sorting through the research or crafting a compelling thesis statement? We’ve got you covered! Just hit that ORDER NOW button above, and let’s embark on the journey of crafting an exceptional research paper together. Your success is just a click away!
What are some interesting topics about schizophrenia? There are diverse and engaging research topics about schizophrenia, ranging from exploring its genetic factors to examining innovative treatment approaches and societal perceptions.
What is the latest research on schizophrenia? As of my last knowledge update in January 2023, I don’t have specific details on the absolute latest research on schizophrenia. However, staying updated with reputable journals and academic sources is the best way to access current research in 2023.
What is the latest research for schizophrenia in 2023? For the most recent and specific research on schizophrenia in 2023, it is recommended to check the latest publications in reputable scientific journals or visit the websites of organizations such as the National Institute of Mental Health for up-to-date information.
What kind of research is being done on schizophrenia? Research on schizophrenia encompasses a broad spectrum, including studies on its genetic and environmental origins, novel treatment modalities, the impact on social functioning, and efforts to combat the stigma associated with the disorder.

With a passion for education and student empowerment, I create blog content that speaks directly to the needs and interests of students. From study hacks and productivity tips to career exploration and personal development
- Top 100 Climate Change Research Paper Topics
- Top 100 Cancer Research Paper Topics

Most Popular Articles
Racism thesis statement example, how to rephrase a thesis statement, capstone project topic suggestions, how to write an abortion essay, should students wear school uniforms essay, list causal essay topics write, respect essay, signal words, great synonyms, informative speech examples, essay writing guide, introduction paragraph for an essay, argumentative essay writing, essay outline templates, write an autobiographical essay, personal narrative essay ideas, descriptive essay writing, how to write a reflective-essay, how to write a lab report abstract, how to write a grant proposal, point of view in an essay, debate topics for youth at church, theatre research paper topics, privacy overview.
- Frontiers in Psychiatry
- Schizophrenia
- Research Topics
Reviews In Psychiatry 2023: Schizophrenia
Total Downloads
Total Views and Downloads
About this Research Topic
Frontiers in Psychiatry is delighted to present the ‘Reviews in’ series of article collections. Reviews in Schizophrenia will publish high-quality scholarly review papers on key topics in Schizophrenia. It aims to highlight recent advances in the field, whilst emphasizing important directions and new ...
Keywords : schizophrenia, reviews, mini reviews, systematic reviews
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, recent articles, submission deadlines.
Submission closed.
Participating Journals
Total views.
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
Elimu Centre
Education Centre
Schizophrenia Research Topics
Schizophrenia essay titles, schizophrenia paper topics, schizophrenia research questions.
Schizophrenia Research Topics: Schizophrenia is a complex mental disorder. When writing research topics on Schizophrenia one has to be very careful on the topics since one should be conversant with the topic. Hope the list of schizophrenia research paper topics below will give you a starting point in writing your research paper.
1. Treatment Of People With Schizophrenia
2. The Vicious Cycle Of Schizophrenia
3. The Reality Of Schizophrenia Is A Frightening Menace
4. The Progression Of Development Of Schizophrenia
5. The Mental Illness Of Schizophrenia
6. The Mental Condition Of Schizophrenia
7. The History and Future of Schizophrenia
8. The General Psychiatric Symptoms Of Schizophrenia
9. The Enigma of Schizophrenia
10. The effect on Individuals with Schizophrenia in states that opted out of Medicaid Expansion/The State Healthcare Exchanges under The Affordable Care Act
Read: Argumentative Essay Topics about Mental Health
11. The Diagnostic Criteria Of Schizophrenia
12. The Connection Between Schizophrenia And Violence
13. The Cognitive Behavioral Aetiology Of Schizophrenia
14. The ‘Glutamate Theory’ of the Pathogenesis of Schizophrenia
15. Symptoms And Treatment Of Patients With Schizophrenia
16. Symptoms And Symptoms Of Schizophrenia
17. Schizophrenia, The Schizophrenic Mind Is Not So Much Split As Shattered
18. Schizophrenia Of Children And Adolescents
19. Schizophrenia Is A Serious Disorder
Read: Research Topics on Mental Health
1. Schizophrenia As A Psychotic Disorder
2. Schizophrenia And Treatment Of Schizophrenia
3. Schizophrenia and the Mental Health Consumer Movement
4. Schizophrenia and PET Scan Findings
5. Schizophrenia And Other Psychotic Disorders
6. Schizophrenia and Neuroplasticity
7. Schizophrenia And Its Effects On The Development Of Schizophrenia
8. Schizophrenia And Its Effects On People
9. Schizophrenia And Its Effects On Children
10. Schizophrenia and Homelessness
11. Schizophrenia and Disorder of Lifespan Development
12. Schizophrenia and Aging
13. Schizophrenia – Longitudinal Studies
Read: Policy Topics for Persuasive Speeches
14. Schizophrenia Symptoms And Treatment Of Schizophrenia
15. Schizophrenia A Correlation Between Poverty And Schizophrenia
16. Psychotherapy as a Treatment for Schizophrenia
17. New Treatments for Schizophrenia Currently in Clinical Trials
18. Mental Health Condition Of Schizophrenia
19. Living With Schizophrenia
20. Marijuana and it’s effect on Individuals with Schizophrenia
Read: Research Project Samples for Students
1. Incidence of Schizophrenia Among Healthcare Professionals
2. Genetic Links Between Schizophrenia and Associated Co-morbid Conditions
3. Diagnosis Of Schizophrenia
4. Description and Analysis of Catatonic Schizophrenia
5. Childhood Onset Schizophrenia And Schizophrenia
6. Causes and Treatments of Schizophrenia
7. Bipolar Vs. Schizophrenia Bipolar And Schizophrenia
8. A Depth Report On Schizophrenia
Read: Narrative Essay Topics for College Students
1. Is there an Association between Schizophrenia and Intracellular Pathogens?
2. What are the positives signs of Schizophrenia?
3. Is Schizophrenia A Psychological Or Mental Disorder?
4. How to treat Schizophrenia medically?
5. What to know about Schizophrenia?
6. Is supportive therapy effective in managing Schizophrenia

Betty is a qualified teacher with a Bachelor of Education (Arts). In addition, she is a registered Certified Public Accountant. She has been teaching and offering part-time accounting services for the last 10 years. She is passionate about education, accounting, writing, and traveling.
Everything begins with an idea!
Schizophrenia Research Paper Topics
Schizophrenia is a chronic mental disorder that affects how a person thinks, expresses emotions, acts, and perceives reality. Schizophrenia is among the most complex mental disorder. Due to its complex nature, students have a high chance of struggling with schizophrenia research paper topics. As a student, you should realize that a schizophrenia research paper is quite easy to write if you get a good topic to use. We know that many students don’t have enough time to be brainstorming for topics, which is why we decided to help them with topic ideas. We have listed the best schizophrenia research paper topics below. The topics that we listed below will assist you in making the most out of your research paper. You’ll quickly know what to write about any topic that you choose here after you carry out a little research. We implore you to make attempts to meet some patients with this mental disorder and use your findings in your research paper. By using the topics here for your research paper, you will surely surprise your professors and colleagues. More importantly, these topics will assist you in comprehending the medical issue of schizophrenia fully.
- A Report On Schizophrenia
- Association between Intracellular Pathogens and Schizophrenia
- Diagnosis Of Schizophrenia
- Genetic Links Between Associated Co-morbid Conditions and Schizophrenia
- Schizophrenic Bipolar And Schizophrenia
- Is Schizophrenia A Mental Disorder?
- Living With Schizophrenia
- The Dangers Of Having Schizophrenia
- Causes Of Schizophrenia
- Treatment Of Schizophrenia
- The similarity between bipolar disorder and schizophrenia
- Description Of Catatonic Schizophrenia
- Analysis of Catatonic Schizophrenia
- Childhood-Onset Schizophrenia
- Is Schizophrenia An Incurable Mental Illness?
- New Treatments for Schizophrenia
- Trial Treatments for Schizophrenia
- The Effect Of Medical Marijuana On Individuals with Schizophrenia
- Schizophrenia Among Healthcare Professionals
- Mental Health Condition Of Schizophrenia
- How Do Genetic Factors Contribute To The Development Of Schizophrenia?
- Behavioral Aetiology Of Schizophrenia
- Schizophrenia and Neuroplasticity
- Schizophrenia As A Serious Disorder
- A Person With Schizophrenia
- Schizophrenia and Homelessness
- Schizophrenia and Aging
- Psychotherapy For Treating Schizophrenia
- Schizophrenia – Longitudinal Studies
- Schizophrenia As A Psychotic Disorder
- Schizophrenia and PET Scan Findings
- Symptoms Of Schizophrenia
- Early Signs Of Schizophrenia
- How Schizophrenia Affects Cognitive Ability
- How Schizophrenia Develops
- Symptoms And Treatment Of Schizophrenia
- Correlation Between Schizophrenia And Poverty
- Disorder of Lifespan Development And Schizophrenia
- The Effects Of Schizophrenia On Children
- The Effects Of Schizophrenia On Adults
- Is Any Particular Race More Vulnerable To Schizophrenia?
- Schizophrenia And Other Psychotic Disorders
- The Development Of Schizophrenia
- Schizophrenia Of Children And Adolescents
- The Pathogenesis of Schizophrenia
- How The ‘Glutamate Theory’ Is Related To Schizophrenia
- The Mental Health Consumer Movement And Schizophrenia
- A Detailed Description Of A Schizophrenic Mind
- How Schizophrenia Affects Brain Development In Children With Schizophrenia
- The Diagnostic Criteria Of Schizophrenia
- How Does Schizophrenia Affect People Who Live In States That Opted Out Of The State Healthcare Exchanges?
- The Enigma of Schizophrenia
- The Connection Between Violence And Schizophrenia
- The Mental Illness Of Schizophrenia
- What is Schizophrenia?
- The Mental Condition Of Schizophrenia
- The Vicious Cycle Of Schizophrenia
- Treatment Of People With Schizophrenia
- The History of Schizophrenia
- The Possible Future Of Schizophrenia
- Ia Schizophrenia A Genetically Transmittable Illness?
- Development Of Schizophrenia
- Why The Reality Of Schizophrenia Frightens Many American Citizens
- Medical Solution To Schizophrenia
- How To Prevent The Development Of Schizophrenia In Children
- Are There Effective Drugs Against Schizophrenia?
- Therapy For Schizophrenia
- Schizophrenia And Cognitive Ability
- Non-Genetic Factors That Can Cause Schizophrenia
- What Is The Relationship Between Unhealthy Diet And Schizophrenia?
- How To Reverse The Negative Impacts Of Schizophrenia
- How Do People With Schizophrenia Perceive Their Environment?
- Schizophrenia And Co-morbid Conditions
- Reversible Damages That Schizophrenia Can Cause
- Irreversible Damages That Schizophrenia Can Cause
- What Are The Dangers Associated With Late Treatment Of Schizophrenia?
- How Schizophrenia Affects Mental Health
- Can Schizophrenia Cause The Death Of Brain Cells?
- The Relationship Between Schizophrenia And Loss Of Memory
- How Schizophrenia Affects Consciousness
- Can Schizophrenia Affect Neurons?
- How Schizophrenia Changes Brain Function
- What Makes A Person Vulnerable To Schizophrenia?
- How Schizophrenia Retards Brain Performance
- The Health Risks Associated With Schizophrenia
- What It Take To Treat Schizophrenia
- The Side Effects Of Schizophrenia Treatment On Patients
- The Dangers Of Living With Schizophrenia
- How Can Schizophrenia Reflect On The Physical Health?
- How Schizophrenia Affects Women
Have top experts do your papers.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Custom Essay, Term Paper & Research paper writing services
- testimonials
Toll Free: +1 (888) 354-4744
Email: [email protected]
Writing custom essays & research papers since 2008
Schizophrenia research papers: tips and topics.

Schizophrenia is regarded as one of the most serious psychiatric disorders that exist. It is also one of the most common psychiatric disorders. Symptoms of the disease include disorganized speech behavior, hallucinations, and delusional thoughts. Schizophrenia research as with other research under psychiatric medicine areas of today is tailored towards the industry demand.
Over the years, there has been a massive increase in educational programs, however with little or no increase in schizophrenia research topics. As a result, current research on schizophrenia deals more with the prescribing of newer antipsychotic agents. The implication is that there is a vast array of grey in schizophrenia studies. This article will provide some tips that you might need to write schizophrenia research papers on your own, and to standard.
Writing a Good Research Paper on Schizophrenia
In writing a good schizophrenia paper, here are some steps that you can follow, that would be very helpful.
In some cases, you might be lucky enough to be assigned a topic that makes this step relatively irrelevant. Otherwise, if you are to choose a topic on your own, of all the steps involved in writing your research paper on schizophrenia, this might be the toughest. First, you would have to research schizophrenia to understand what you are going into. After this, you would have to decide if your schizophrenia paper would be on areas of research that have previously been touched. You could also decide to dive into totally new research on schizophrenia.
Whichever topic you choose, a good research topic should not be too broad. A relatively broad topic might capture a general view of the research rather than capture a more specific view. For instance, a topic like “Hard drug dependence in Schizophrenia” can easily be narrowed down to “Nicotine dependence in Schizophrenia patients.”
After you might have selected an article that suits you, the next phase is proper research on your chosen topic. You can use the internet to get yourself a lot of schizophrenia research articles. In achieving this aim, you can make good use of Google Scholar.
A simple search with the words “latest research on schizophrenia” or “new research on schizophrenia” would bring you journals that might be helpful in your research study. After you might have found the schizophrenia research article that you need, do well to write down your sources in a way that you can write your references properly in the end.
Developing an outline will help you come up with ideas as well as order your thoughts appropriately. Without a proper outline, your work might like focus and direction. In creating your schizophrenia research paper outline, you create subheadings that have central themes with the topic you have chosen.
Look at these subheadings as key points that you need to discuss your topic for proper understanding. You’ll need to develop the points using what you have found in your schizophrenia research and in the research articles on schizophrenia that you have read.
In writing your research paper on schizophrenia, you could go through two ways. You could start typing your work directly or you could first have a draft. Having a draft will allow you to create a more error-free schizophrenia research paper. However, making a draft could see you extend the time you have in coming up with your schizophrenia paper.
Schizophrenia Research Journals
To come up with a research article on schizophrenia that is of standard, you’ll need to cite some journals. From these journals, you will find research papers on schizophrenia. From these papers, you’ll find the results of a series of schizophrenia research studies that might be helpful. You can also contact professional writers who are experts in this field. Here is a list of journals that are available at your disposal.
- Schizophrenia Research . The schizophrenia research journal is a journal that contributes to the dissemination of information associated with research on schizophrenia. The schizophrenia research impact factor as of 2018 by Clarivative Analysis is 4.569.
- Schizophrenia Bulletin . In this journal, you will find reviews on recent development in the world of research in schizophrenia. It looks into areas of schizophrenia research study bordering around the etiology and treatment of schizophrenia. The Schizophrenia bulletin impact factor is 7.289.
- World Psychiatry . this journal is published by the world’s Psychiatric association. The Journal deals widely with psychiatric medicine as a whole. However, it could as well provide readers with answers to schizophrenia research questions about significant clinical, service and research developments.
- Proceedings from Conferences . In addition to journals, you can make use of proceedings from conferences. For instance, proceedings from the international congress on schizophrenia research that takes place once in two years.
Sample Schizophrenia Research Paper Topics
Just in case you need a topic to write on for your research paper on Schizophrenia, here are a few topics you can work with:
- The role of alkaloid in schizophrenic psychosis.
- Relationship between schizophrenic psychosis and animate thing Pathogens
- Medical Marijuana and its impact on people with Schizophrenia
- “Schizophrenia and also the psychological state shopper Movement
- Incidence of schizophrenic psychosis Among tending Professionals
- Genetic Links Between schizophrenic psychosis and Associated Co-morbid Conditions”
- Longitudinal Studies on Schizophrenic psychosis
- Schizophrenic psychosis and Aging
- New Treatments for schizophrenic psychosis presently in Clinical Trials
- Schizophrenic psychosis and PET Scan Findings”
- Schizophrenia, Schizophrenic psychosis and Neuroplasticity
- Schizophrenia, Schizophrenic psychosis and Homelessness
- The impact on people with schizophrenic psychosis in states that opted out of health care Expansion/The State tending Exchanges underneath the Affordable Care Act
Having all the necessary information relating to your topic would not necessarily make your schizophrenia research paper a good one. A good research paper in addition to having all the necessary information is one that is free of errors. Amongst other things, make sure to review your work properly for grammatical errors. Finally, look out for the flow, use of logic, sentence structure, the order of paragraphs, and avoid plagiarism.
Home — Essay Samples — Nursing & Health — Psychiatry & Mental Health — Schizophrenia
Essays About Schizophrenia
Understanding schizophrenia: overview, diagnosis, treatment, schizophrenia: definition, symptoms, causes, made-to-order essay as fast as you need it.
Each essay is customized to cater to your unique preferences
+ experts online
Schizophrenia: Symptoms, Treatment, and Stigma
Research of schizophrenia disorder, the history of schizophrenia, analysis of the symptoms of schizophrenia, let us write you an essay from scratch.
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Biopsychosocial Influences on Schizophrenia
An examination of the six mental illnesses and its impact on human life, a case study on the mental illness of mr. nash and the treatment plan for his schizophrenia, the link between drug addiction and under-diagnosed/misdiagnosed schizophrenia, get a personalized essay in under 3 hours.
Expert-written essays crafted with your exact needs in mind
Schizophrenia in Film: an Analysis of The Psychopathology Portrayed in Donnie Darko
Psychosis and schizophrenia in children, schizoaffective disorder: the bridge between schizophrenia and bipolar, connection between schizophrenia and social isolation, alice in wonderland syndrome, psychological evaluation of john nash through analysis of the film a beautiful mind, depiction of john nash’s schizophrenia in the film a beautiful mind, analysis of john nash's life long struggles with schizophrenia in the movie a beautiful mind, critical review of the movie the soloist, art therapy and cognitive-behavioral therapy in schizophrenia treatment, best friends in our lives, schizophrenia and crime: the complex relationship, summary of a beautiful mind.
Schizophrenia is a chronic and severe mental disorder characterized by a profound disruption in thinking, perception, emotions, and behavior. It affects approximately 1% of the global population and typically emerges in late adolescence or early adulthood. Individuals with schizophrenia often experience a range of symptoms that can significantly impair their ability to function in various aspects of life.
Delusions: People with schizophrenia often experience delusions, which are fixed false beliefs that are not based in reality. These delusions can be paranoid, grandiose, or related to persecution. Hallucinations: Another common characteristic of schizophrenia is hallucinations, particularly auditory hallucinations. These involve hearing voices or sounds that are not actually present. Disorganized thinking: Schizophrenia can lead to disorganized thinking, making it difficult for individuals to maintain a logical thought process or communicate coherently. They may jump between unrelated topics or exhibit incoherent speech. Negative symptoms: Negative symptoms refer to a decrease or loss of normal functions. These may include a lack of motivation, decreased emotional expression, social withdrawal, and reduced ability to carry out everyday tasks. Cognitive impairments: Schizophrenia can also impact cognitive abilities such as attention, memory, and problem-solving. This can make it challenging for individuals to focus, learn, and make decisions. Impact on daily functioning: Schizophrenia can significantly interfere with an individual's ability to function in daily life. It can disrupt relationships, work or educational performance, and self-care.
Genetics: There is a strong genetic component to schizophrenia, as individuals with a family history of the disorder have a higher risk of developing it. Certain genes and gene variations are associated with an increased susceptibility to schizophrenia. Brain chemistry and structure: Imbalances in brain chemicals, specifically dopamine and glutamate, have been implicated in schizophrenia. Structural abnormalities in the brain, such as enlarged ventricles and reduced gray matter volume, have also been observed in individuals with the disorder. Environmental factors: Prenatal and early life factors can contribute to the development of schizophrenia. Maternal stress, infections during pregnancy, and birth complications have been linked to an increased risk. Additionally, exposure to certain environmental stressors and substance abuse during adolescence and adulthood may also play a role. Neurodevelopmental abnormalities: Schizophrenia is thought to involve disruptions in brain development during early life stages. Factors such as abnormal neural migration, synaptic pruning, and connectivity between brain regions may contribute to the manifestation of symptoms. Psychological and social factors: Stressful life events, trauma, and dysfunctional family environments may increase the risk of developing schizophrenia or trigger its onset in susceptible individuals.
1. Paranoid Schizophrenia 2. Disorganized Schizophrenia 3. Catatonic Schizophrenia 4. Undifferentiated Schizophrenia 5. Residual Schizophrenia
1. Antipsychotic medications 2. Psychotherapy (i.e. cognitive-behavioral therapy (CBT)) 3. Social support (vocational rehabilitation, housing assistance, and community programs) 4. Self-care (practicing good sleep hygiene, engaging in regular physical activity, maintaining a balanced diet, and avoiding alcohol and drugs) 5. Ongoing management.
"A Beautiful Mind" (Film, 2001): This biographical drama portrays the life of mathematician John Nash, who was diagnosed with schizophrenia. The film depicts his struggle with the illness, showcasing both the challenges and the triumphs he experiences. "One Flew Over the Cuckoo's Nest" (Novel, 1962): This classic novel by Ken Kesey takes place in a psychiatric hospital and features a character named Chief Bromden, who is believed to have schizophrenia. The story explores the institutional treatment of mental illness and challenges the notions of sanity and insanity. "Silver Linings Playbook" (Film, 2012): This romantic comedy-drama revolves around a man named Pat Solitano, who has bipolar disorder but also exhibits symptoms of psychosis, including delusions. While the film primarily focuses on bipolar disorder, it sheds light on the complexities of mental health and the impact it has on relationships. "The Soloist" (Book, 2008; Film, 2009): Based on a true story, "The Soloist" follows the life of Nathaniel Ayers, a gifted musician who becomes homeless and is diagnosed with schizophrenia. The narrative explores the challenges faced by Ayers as he navigates his mental health condition while pursuing his passion for music.
1. Schizophrenia affects approximately 1% of the global population, with no significant variation across different cultures or ethnicities. 2. Schizophrenia typically emerges in late adolescence or early adulthood, although it can occur at any age. 3. Men often experience the onset of schizophrenia earlier than women. Additionally, men tend to have more severe symptoms, while women generally have a better overall prognosis. 4. Research suggests that an imbalance of certain neurotransmitters, such as dopamine and glutamate, may contribute to the development of schizophrenia. 5. Schizophrenia is often stigmatized, leading to discrimination and social isolation for those affected. Education and awareness campaigns aim to combat the stigma and promote understanding.
The topic of schizophrenia is important to write an essay about due to its significant impact on individuals, families, and society as a whole. Understanding schizophrenia is crucial for several reasons. Firstly, it is a complex mental health disorder that affects a considerable portion of the population worldwide, leading to significant personal and societal burdens. Exploring the causes, symptoms, and treatment options for schizophrenia can contribute to advancing knowledge in the field of mental health.
Secondly, addressing the misconceptions and stigma associated with schizophrenia is paramount. By writing an essay on this topic, one can raise awareness and promote empathy, fostering a more inclusive and supportive environment for individuals living with schizophrenia.
Additionally, studying schizophrenia can provide insights into the intricate workings of the human mind and the intricate interplay between genetics, neurobiology, and environment. This knowledge can lead to advancements in early detection, intervention, and treatment strategies.
Lastly, exploring the lived experiences of individuals with schizophrenia and their journeys towards recovery can provide valuable perspectives on resilience, hope, and the human capacity for growth and adaptation.
1. Andreasen, N. C. (1999). A unitary model of schizophrenia: Bleuler's "fragmented phrene" as schizencephaly. Archives of General Psychiatry, 56(9), 781-787. 2. Cannon, T. D., & van Erp, T. G. M. (2003). Bearden CE: Early-onset schizophrenia: a review of recent findings. Current Opinion in Psychiatry, 16(3), 307-312. 3. Hafner, H., Riecher-Rössler, A., & Hambrecht, M. (1993). IRAOS: an instrument for the assessment of onset and early course of schizophrenia. Schizophrenia Research, 9(1-2), 209-223. 4. Javitt, D. C. (2009). When doors of perception close: bottom-up models of disrupted cognition in schizophrenia. Annual Review of Clinical Psychology, 5, 249-275. 5. Kahn, R. S., Sommer, I. E., Murray, R. M., Meyer-Lindenberg, A., Weinberger, D. R., Cannon, T. D., O'Donovan, M., Correll, C. U., Kane, J. M., & van Os, J. (2015). Schizophrenia. Nature Reviews Disease Primers, 1, 15067. 6. Leucht, S., Cipriani, A., Spineli, L., Mavridis, D., Örey, D., Richter, F., Samara, M., Barbui, C., Engel, R. R., Geddes, J. R., Kissling, W., Stapf, M. P., Lässig, B., Salanti, G., & Davis, J. M. (2013). Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. The Lancet, 382(9896), 951-962. 7. McGrath, J., Saha, S., Chant, D., & Welham, J. (2008). Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiologic Reviews, 30(1), 67-76. 8. Millan, M. J., Andrieux, A., Bartzokis, G., Cadenhead, K., Dazzan, P., Fusar-Poli, P., Gallinat, J., Giedd, J., Grayson, D. R., Heinrichs, M., Kahn, R., Krebs, M. O., Leboyer, M., Lewis, D., Marin, O., Marin, P., Meyer-Lindenberg, A., McGorry, P., McGuire, P., ... & Stephan, K. E. (2016). Altering the course of schizophrenia: progress and perspectives. Nature Reviews Drug Discovery, 15(7), 485-515. 9. Sullivan, P. F., Kendler, K. S., & Neale, M. C. (2003). Schizophrenia as a complex trait: evidence from a meta-analysis of twin studies. Archives of General Psychiatry, 60(12), 1187-1192. 10. van Os, J., Kapur, S., & Schizophrenia, C. (2009). Progressive brain changes in schizophrenia? A meta-analysis of longitudinal MRI studies. Schizophrenia Research, 115
Relevant topics
- Mental Health
- Stress Management
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Bibliography
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Schizophrenia Research Paper

This sample schizophrenia research paper features: 6600 words (approx. 22 pages), an outline, and a bibliography with 6 sources. Browse other research paper examples for more inspiration. If you need a thorough research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.
Schizophrenia is a psychotic disorder characterized by disturbances in thought, emotion, and behavior. This research paper discusses the symptoms, etiology, treatment, and other pertinent issues concerning this mental illness.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% off with 24start discount code, i. description and classification, a. symptoms, 1. delusions, 2. hallucinations, 3. disorganized speech, 4. disorganized or catatonic behavior, 5. negative symptoms, b. variability of symptoms among patients, c. subtypes of schizophrenia, ii. history, iii. demographic characteristics of schizophrenia, a. sex differences, b. social class differences, iv. life functioning and prognosis, a. long-term course, b. premorbid characteristics of schizophrenia, v. etiology: theories and research findings, a. brain abnormalities in schizophrenia, b. biochemical factors, c. genetics, d. obstetrical complications, e. viral infection, f. diathesis-stress model, vi. treatment and therapy, a. antipsychotic medication, b. psychological treatment, vii. summary.

Delusions are the primary example of abnormal thought content in schizophrenia. Delusional beliefs conflict with reality and are tenaciously held, despite evidence to the contrary. There are several types of delusions. Delusions of control is the belief that one is being manipulated by an external force, often a powerful individual or organization (e.g., the FBI) that has malevolent intent. Delusions of grancleur refers to patients’ beliefs that they are especially important and have unique qualities or powers (e.g., the capacity to influence weather conditions). In contrast, some patients express the conviction that they are victims of persecution or an organized plot, and these beliefs are referred to as delusions of persecution. Examples of more specific delusions include thought broadcasting, the patient’s belief that his or her thoughts are transmitted so that others know them, and thought withdrawal, the belief that an external force has stolen one’s thoughts.
Hallucinations are among the most subjectively distressing symptoms experienced by schizophrenia patients. These perceptual distortions vary among patients and can be auditory, visual, olfactory, gustatory, or tactile. The majority of hallucinations are auditory in nature and typically involve voices. Examples include the patient hearing someone threatening or chastising him or her, a voice repeating the patient’s own thoughts, two or more voices arguing, and voices commenting. The second most common form of hallucination is visual. Visual hallucinations often entail the perception of distortions in the physical environment, especially in the faces and bodies of other people.
Other perceptual distortions that are commonly reported by schizophrenia patients include feeling as if parts of the body are distorted in size or shape, feeling as if an object is closer or farther away than it actually is, feeling numbness, tingling, or burning, being hypersensitive to sensory stimuli, and perceiving objects as flat and colorless. In addition to these distinctive perceptual abnormalities, persons suffering from schizophrenia often report difficulties in focusing their attention or sustaining concentration on a task.
It is important to note that in order for an unsubstantiated belief or sensory experience to quality as a delusion or hallucination, the individual must experience it within a clear sensorium (e.g., unsubstantiated sensory experiences that occur only upon awaking from sleep or when falling asleep would not qualify as delusions). Thus, for example, if a patient reports hearing something that sounds like voices when alone, but adds that he or she is certain that this is a misinterpretation of a sound, such as the wind blowing leaves, this would not constitute an auditory hallucination.
The DSM uses the term disorganized speech to refer to abnormalities in the form or content of the individual’s verbalizations. It is assumed that these abnormalities reflect underlying distortions in the patient’s thought processes. Thus the term thought disorder is frequently used by researchers and practitioners to refer to the disorganized speech that often occurs in schizophrenia.
Problems in the form of speech are reflected in abnormalities in the organization and coherent expression of ideas to others. One common abnormality of form, incoherent speech, is characterized by seemingly unrelated images or fragments of thoughts that are incomprehensible to the listener. The term loose association refers to the tendency to abruptly shift to a topic that has no apparent association with the previous topic. In general, the overall content of loosely associated speech may be easier to comprehend than incoherent speech. In perseverative speech, words, ideas, or both are continuously repeated, as if the patient is unable to shift to another idea. Clang association is the utterance of rhyming words that follow each other (e.g., “a right, bright kite”). Patients choose words for their similarity in sound rather than their syntax, often producing a string of rhyming words.
The overt behavioral symptoms of schizophrenia fall in two general areas: motor functions and interpersonal behavior. Motor abnormalities, including mannerisms, stereotyped movements, and unusual posture, are common among schizophrenia patients. Other common signs include bizarre facial expressions, such as repeated grimacing or staring, and repeated peculiar gestures that often involve complex behavioral sequences. As with other symptoms of the psychosis, the manifestation of motor abnormalities varies among individuals. Schizophrenia patients sometimes mimic the behavior of others, known as echopraxia, or repeat their own movements, known as stereotyped behaviors. Although a subgroup of patients demonstrate heightened levels of activity, including motoric excitement (e.g., agitation or flailing of the limbs), others suffer from a reduction of movement. At the latter extreme, some exhibit catatonic immobility and assume unusual postures that are maintained for extended periods of time. Some may also demonstrate waxy flexibility, a condition in which patients do not resist being placed into strange positions that they then maintain. Catatonia has decreased dramatically in recent decades, so that it is now rare. Several researchers have attributed this decline to the introduction of antipsychotic medication (described later).
In the domain of interpersonal interactions, schizophrenia patients frequently demonstrate behaviors that are perceived as bizarre or inappropriate by others. For example, it is not uncommon for patients to use socially unacceptable language and unusual tones of voice, or to show overly dependent or intrusive behavior. Another common symptom, inappropriate affect, involves unusual emotional reactions to events and experiences. For example, patients may laugh at a sad or somber occasion, or be enraged by insignificant events. Finally, many patients manifest increasingly poor hygiene as their illness progresses. Their appearance may also be marked by disheveled clothing or inappropriate clothing, such as gloves and coats in the summer.
The symptoms of schizophrenia can be classified into the general categories of positive and negative. Positive symptoms involve behavioral excesses and most of the symptoms described earlier fall in to this category (e.g., delusions, hallucinations, and bizarre behaviors). In contrast, negative symptoms involve behavioral deficits. Examples include fiat affect (blunted expressions of emotion), apathy, and social withdrawal. In the domain of verbal expression, schizophrenia patients who manifest a very low rate of verbal output are described as showing poverty of speech. Patients whose speech is normal in quantity, but lacks meaning, suffer from poverty of content. Recently, some researchers have suggested that positive and negative symptoms may be caused by different neural mechanisms.
It is important to mention that a reduction in overt displays of emotion does not necessarily imply that patients have less intense subjective emotional experiences than the average person. In fact, recent findings indicate that blunted emotional expressions can coexist with intense subjective feelings of emotion.
According to DSM-IV, patients must show two or more of the preceding five symptoms to meet the diagnostic criteria for schizophrenia. Thus, no one of these symptoms is required for the diagnosis. Furthermore, the following four criteria must also be met: (1) the patient shows marked deterioration in occupational, interpersonal, or domestic functioning; (2) the patient manifests continuous signs of symptoms or dysfunction for at least 6 months; (3) the patient does not manifest predominant signs of mood disturbance (e.g., depression or mania); and (4) the symptoms are not caused by substance abuse or a primary medical condition.
Because the diagnostic criteria for schizophrenia are relatively broad, with no one essential symptom, there is a great deal of variability among patients in their symptom profiles. It has therefore been proposed that schizophrenia is a heterogeneous disorder with multiple causes. It is also the case, however, that patients must show a marked and persistent impairment to meet the diagnostic criteria for schizophrenia. Thus, those who meet criteria for the diagnosis are significantly impaired in everyday functioning. For many individuals who are diagnosed with schizophrenia, independent functioning is never achieved.
The DSM lists five subtypes of schizophrenia. In schizophrenia of the paranoid type, delusional concerns about persecution and/or preoccupation with threat dominate the clinical presentation, although delusions of grandeur are also often present. Disorganized schizophrenia is distinguished by extremely incoherent speech and behavior, as well as blunted or inappropriate affect. In catatonic schizophrenia, the clinical picture is dominated by abnormalities in movement and posture, such as those described earlier. Patients classified as having undifferentiated schizophrenia do not meet criteria for any of the previous subtypes. Finally, the diagnosis of residual schizophrenia is applied to patients who have had at least one episode of schizophrenia and who continue to show functional impairment, but who do not currently manifest any positive symptoms.
During the late 1800s and early 1900s, Emil Kraepelin and Eugen Bleuler provided the first conceptualizations of schizophrenia. Kraepelin defined “dementia praecox,” the original term for schizophrenia, as an endogenous psychosis characterized by intellectual deterioration (dementia) and early onset (praecox). Kraepelin included negativism, hallucinations, delusions, stereotyped behaviors, attentional difficulties, and emotional dysfunction as major symptoms of the disorder. Kraepelin’s work focused on description and phenomenology, leaving subsequent researchers to investigate the cause or causes of the disorder.
In contrast to Kraepelin, Eugen Bleuler, a Swiss psychiatrist, proposed a broader view of dementia praecox, with a more theoretical emphasis. Bleuler contested two of Kraepelin’s defining assumptions: specifically, that the psychosis was typically characterized by early onset and intellectual deterioration. Bleuler attempted to identify an underlying commonality among the diverse variations of what Kraepelin referred to as dementia praecox and concluded that all of the patients suffered from a “breaking of associative threads,” causing a disharmony among communicative and thought processes. He believed this abnormality accounted for the problems of thought, emotional expression, decision making, and social interaction associated with schizophrenia. Guided by the defining principle of disharmonious mental structures, Bleuler renamed the disorder “schizophrenia,” meaning “split mind.”
In the early to mid-1900s, American psychiatrists continued to use a broad definition of schizophrenia. The distinction between process and reactive schizophrenia was considered important, however, because it was assumed to distinguish between cases characterized by gradual deterioration (process) and cases that were precipitated by acute stress (reactive).
During this time, some clinicians and researchers viewed the specific diagnostic criteria for the major mental illnesses (schizophrenia, bipolar disorder, major depression) as artificial and discretionary, and used instead flexible and inconsistent standards for diagnoses. Studies that compared the rates of disorder across nations revealed that schizophrenia was diagnosed at a much higher rate in the United States than in Great Britain and some other countries. This national difference resulted from the use of broader criteria for diagnosing schizophrenia in the United States. Many patients who were diagnosed as having depression or bipolar disorder in Britain were diagnosed with schizophrenia in the United States. Because subsequent revisions in the DSM have included more restrictive criteria for schizophrenia, U.S. diagnostic rates are now comparable with other countries.
In addition to a more restrictive definition of schizophrenia, subsequent editions of the DSM have included additional diagnostic categories that contain similar symptoms. Thus the range of “schizophrenia spectrum disorders” continue to broaden with the description of variants of schizophrenia, such as schizoaffective disorder, which is characterized by a mix of affective and psychotic symptoms. The diagnostic category of schizophreniform disorder was also added. This diagnosis is given when the patient shows the typical symptoms of schizophrenia, but does not meet the criterion of 6 months of continuous illness.
Estimates of the prevalence of schizophrenia converge at around 1% of the population. Although there is evidence of cross-national differences in the rate of schizophrenia, the differences are not large (i.e., 1 to 2% difference). It is, in fact, striking that the rate of occurrence is so consistent across cultures.
The modal age at onset of schizophrenia is in early adulthood, usually before 25 years of age. Thus most patients have not had the opportunity to marry or establish a stable work history before the onset of the illness. As a result of this, and the often chronic nature of the illness, many patients never attain financial independence. It is relatively rare for preadolescent children to receive a diagnosis of schizophrenia. Similarly, it is rare for individuals beyond the age of 40 to experience a first episode of the illness.
Although it has traditionally been assumed that there is no sex difference in the rates of schizophrenia, some recent research findings indicate that a somewhat larger proportion of males than females meet the DSM-IV criteria for the disorder. Nonetheless, the overall rates do not differ dramatically for men and women. It is well established, however, that women are more likely to have a later onset of illness, as well as a better prognosis. Women also show a higher level of interpersonal and occupational functioning during the period prior to illness onset. The reasons for this sex difference are not known, but it has been proposed by several theorists that the female sex hormone, estrogen, may function in attenuating the severity of the illness.
Compared with the general population averages, schizophrenia patients tend to have significantly lower incomes and educational levels. Poor urban inner city districts, inhabited by the lowest socioeconomic class, contain the largest proportion of schizophrenia patients. There is a sharp contrast between the rates of schizophrenia in the lowest socioeconomic class and all other levels, including the next higher level. Findings from various cultures suggest that rates of schizophrenia are almost two times higher in the lowest social class group compared with the next lowest.
These social class differences appear to be a partial consequence of the debilitating nature of the illness. The social-drift theory suggests that during the development of schizophrenia, people drift into poverty. When the incomes and educational levels of the parents of patients are compared with those of the general population, the differences are not as striking.
There is, nonetheless, evidence that patients do come from families where the incomes and educational backgrounds of the parents are slightly below the average. These findings have led researchers to conclude that there may be a causal link between social class and risk for the illness. The sociogenic hypothesis posits that situational factors associated with low social class, such as degrading treatment from society, low levels of education, and few opportunities for achievement and reward, produce stress that contributes to the risk for schizophrenia.
Before the introduction of antipsychotic medications in 1950, the majority of patients spent most of their lives in institutional settings. There was little in the way of programs for rehabilitation. But contemporary, multifaceted treatment approaches have made it possible for most patients to live in community settings.
Of course, during active episodes of the illness, schizophrenia patients are usually seriously functionally impaired. They are typically unable to work or maintain a social network, and often require hospitalization. Even when in remission, some patients find it challenging to hold a job or to be self-sufficient. This is partially due to residual symptoms, as well as to the interruptions in educational attainment and occupational progress that result from the illness. However, there are many patients who are able to lead productive lives, hold stable jobs, and raise families. With the development of greater community awareness of mental illness, some of the stigma that kept patients from pursuing work or an education has diminished.
For about one third of patients, the illness is chronic and is characterized by episodes of severe symptoms with intermittent periods when the symptoms subside but do not disappear. For others, there are multiple episodes with periods of substantial symptom remission. About one third of those who receive the diagnosis eventually show a partial or complete recovery after one or two episodes.
Several factors have been linked with a more favorable prognosis for schizophrenia. Early treatment seems to be important in that the shorter the period between the onset of the patient’s symptoms and the first prescribed medication, the better the clinical outcome. Another indicator of better prognosis is a high level of occupational and interpersonal functioning in the premorbid period. Also, as noted earlier, women and patients who have a later onset of symptoms have a better long-term outcome.
Some of the difficulties experienced by individuals with schizophrenia can be observed before the onset of the clinical symptoms. Deficits in social skills, concentration, emotional expression, motivation, and occupational or academic performance often precede the first clinical symptoms. This period of gradual decline in functioning before the first illness episode is referred to as the prodromal phase.
However, there are often more subtle signs of dysfunction long before the onset of the prodromal period. Controlled studies using archival data sources, such as medical and school records or childhood home-movies, indicate that subtle differences are discernible as early as infancy in some patients. Individuals who succumb to schizophrenia in adulthood sometimes have abnormal motor development and show deficits in emotional expression and interpersonal relationships in early childhood. Cognitive impairment and difficult temperament have also been observed. During middle childhood and adolescence, researchers have found evidence of neurological abnormality, poor emotional control, social immaturity, and academic performance deficits. Premorbid behavioral problems often become marked through the adolescent years, and many exhibit behavioral disturbances and cognitive abnormalities that resemble the clinical symptoms of schizophrenia.
The causes of schizophrenia are unknown, but it is now widely accepted by both researchers and clinicians that schizophrenia is biologically determined. This is in striking contrast to the early and mid-1900s, when many subscribed to the theory that faulty parenting, especially cold and rejecting mothers, caused schizophrenia in offspring.
There are several sources of evidence for the assumption that schizophrenia involves an abnormality in brain function. First, studies of schizophrenia patients have revealed a variety of behavioral signs of central nervous system impairment, including motor and cognitive dysfunctions. Second, when the brains of patients are examined with in vivo imaging techniques, such as magnetic resonance imaging (MRI), many show abnormalities in brain structure. Similarly, postmortem studies of brain tissue have revealed irregularities in nerve cell formation and interconnections.
Laboratory studies of schizophrenia patients have revealed a variety of abnormalities, including irregularities in smooth pursuit eye movements, psychophysiological responses to sensory stimuli, and concentration. Research on the neuropsychological performance of schizophrenia patients was first conducted in the 1950s and continues to the present time. Individual neuropsychological tests are designed to measure functions subserved by specific regions or systems of the brain. An early finding in this area was that schizophrenia patients were the one psychiatric group whose performance on neuropsychological tests was indistinguishable from people with known brain damage. The findings suggested a generalized cerebral dysfunction in schizophrenia. However, patients show the most consistent deficits on tests of attention and memory, indicating dysfunction of the frontal and temporal lobes and the hippocampus. Further evidence of dysfunction in these brain regions is derived from poor performance on tests of executive functions: the ability to formulate, maintain, and adapt appropriate responses to the environment.
Brain-imaging studies of schizophrenia have yielded results that mirror those obtained from neuropsychological research. Some relatively consistent findings are that the brains of schizophrenia patients have abnormal frontal lobes and enlarged ventricles. Enlarged ventricles suggest decreased brain mass, particularly in the limbic regions, which are intimately involved in emotional processing. Furthermore, ventricular size correlates with negative symptoms, performance deficits on neuropsychological tests, poor response to medication, and poor premorbid adjustment. These associations between ventricular enlargement and both premorbid and postmorbid characteristics suggest that the brain abnormalities are long-standing, perhaps congenital.
In addition to brain structure, investigators have examined biological indices of brain function in schizophrenia. Functional brain-imaging studies, with procedures such as positron emission tomography (PET) and measurement of regional cerebral blood flow, reveal that schizophrenia patients have decreased levels of blood flow to the frontal lobes, especially while performing cognitive tasks.
Researchers are now pursuing the question of what causes the brain abnormalities observed in schizophrenia. Although as yet there are no definitive answers, investigators have made continuous progress in identifying factors that are associated with risk for the disorder.
The structural brain abnormalities that have been observed in schizophrenia support the assumption that it is a disorder of the central nervous system. But it has also been shown that similar structural abnormalities (i.e., ventricular enlargement and volume reductions) are present in other disorders, both neurological and psychiatric. It is therefore assumed that specific abnormalities in brain biochemistry may play a role in schizophrenia.
The functioning of the central nervous system is dependent on a host of chemicals that serve as the “messenger substances” among neurons. These chemicals or neurotransmitters have been the subject of intense investigation. Among the various neurotransmitters that have been implicated in the neuropathophysiology of schizophrenia is dopamine. Dopamine is viewed as a likely candidate for two main reasons: (1) drugs that act to enhance the release or activity of dopamine can produce psychotic symptoms, and (2) drugs that have been established to have antipsychotic properties (i.e., reduce psychotic symptoms) reduce the activity of dopamine in the brain. Current theories of the role of dopamine in schizophrenia have focused on dopamine receptors. There is evidence that there may be an abnormality in the number or sensitivity of certain dopamine receptors in the brains of schizophrenia patients. To date, however, this evidence remains inconclusive.
Several other neurotransmitters have also been hypothesized to play a role in schizophrenia. Current theories under investigation include a malfunction of the receptors for a neurotransmitter called glutamate and an abnormality in the balance between dopamine and serotonin (another neurotransmitter which, like dopamine, has been implicated in the pathogenesis of schizophrenia). As research findings on the biochemical aspects of schizophrenia accumulate, it increasingly appears that the illness may involve multiple neurotransmitters, with different biochemical profiles for different patients.
A convincing body of research supports the notion of a genetic predisposition to schizophrenia. Behavioral genetic studies of families, twins, and adopted offspring of schizophrenia patients indicate that an inherited vulnerability is involved in at least some cases of the disorder.
There is an elevated risk of schizophrenia for individuals with a biological relative who suffers from the disorder, and the risk rates increase as a function of the genetic closeness of the relationship. For example, it has been estimated that children of schizophrenia patients have a 9 to 15 % likelihood of developing the illness, siblings of patients have an 8 to 14% likelihood, and cousins have a 2 to 6% likelihood of being diagnosed with schizophrenia. Given the general population rate of approximately 1%, relatives of patients are at statistically increased risk. It must be noted, however, that relatives share common experiences as well as common genes. Therefore, examinations of the prevalence of schizophrenia in the relatives of patients cannot elucidate the relative contributions of environmental and genetic factors.
Some investigators have studied the development of adopted children whose biological mothers had schizophrenia. This approach has the potential to provide more conclusive information than family studies. The results of these investigations show that when biological offspring of schizophrenic mothers are reared from infancy in adoptive homes they are more likely to develop schizophrenia than are adopted children from healthy mothers. Furthermore, these children also exhibit a higher rate of other adjustment problems when compared with controls. Studies of this type have clearly illustrated that vulnerability to schizophrenia can be inherited.
Research on twins examines differences in concordance rates between identical (monozygotic or MZ) and fraternal (dizygotic or DZ) twins. Twin studies rely on the fact that MZ twins essentially share 100% of their genes. Thus, environmental influences account for any behavioral differences between MZ twins. In contrast, DZ twins are no more genetically similar than regular siblings; DZ twins do, however, share more similar environmental factors than do nontwin siblings. To date, the results of twin studies have consistently shown that MZ twins are significantly more likely to be concordant for schizophrenia than are DZ twins.
At the same time, it is important to note that in at least 50% of the cases in which one member of an MZ twin pair has schizophrenia, the other does not. Such “discordant” pairs have been the subject of a recent, comprehensive investigation in the United States. Among the most important findings from this research project are those from the MRI scans conducted on the twins. The ill twins in the pairs showed significantly more brain abnormalities than the healthy twins. Most notable were reductions in the volume of certain brain regions, especially the hippocampus, and increases in the size of the ventricles. These results clearly indicate the importance of environmental factors in the etiology of schizophrenia.
As is the case with many other disorders that involve brain dysfunction, there is evidence that schizophrenia is associated with exposure to prenatal and delivery complications. Obstetrical complications (OCs) are defined as physical deviations from the normal course of events during pregnancy, labor, or the neonatal period. Estimates of OCs in schizophrenics have been as high as 67%, significantly higher than the rate of OCs found in normal controls.
Among the prenatal factors that have been found to be associated with increased risk for schizophrenia are prenatal maternal nutritional deficiency, viral infection, bleeding, and toxemia. Complications of delivery that can result in hypoxia have also been linked with heightened risk for the disorder. Hypoxia, a deficiency in the amount of oxygen available to the fetus, can affect the development of various parts of the brain. Some researchers argue that hypoxia results in hippocampal damage, thus contributing to vulnerability for schizophrenia. Low birth weight, a neonatal complication, is another potential early factor contributing to schizophrenia. There is evidence that low birth weight is related to increased ventricular size, which is a common characteristic of schizophrenia patients.
The findings on prenatal complications support the notion that fetal brain development may be disrupted in individuals who later manifest schizophrenia. A central question raised by these findings concerns the nature of the etiologic role of OCs. Some hypothesize that OCs produce the neural predisposition to schizophrenia, whereas others posit that OCs exacerbate or interact with an existing genetic predisposition.
Findings from prospective, high-risk research projects lend support to the hypothesis that OCs interact with genetic vulnerabilities in the etiology of schizophrenia. High-risk studies involve the repeated assessment of children of schizophrenia patients, based on the expectation that a larger percentage of these children will eventually develop the illness than individuals in the general population. The high-risk method offers some advantages when compared with retrospective studies of the precursors of schizophrenia. One advantage is that it allows for the direct assessment of subjects in the premorbid period, as well as the selection and study of variables that are thought to have prognostic relevance. Furthermore, because a significant portion of the data collection takes place during the premorbid period, this reduces confounds that often occur in the study of diagnosed patients (e.g., medication and institutionalization).
Studies using the high-risk method have shown an interactive effect of genetic risk and exposure to OCs in predicting adult psychiatric outcome. In other words, the correlation between OCs and adult psychiatric symptoms was greater for offspring of schizophrenia parents than for children of healthy parents. The same pattern was apparent for the relation between OCs and adult brain morphology, suggesting that pre- and perinatal factors contribute to brain abnormalities.
As noted earlier, prenatal exposure to maternal viral infection has also been linked with schizophrenia. Specifically, the rate of schizophrenia is increased for cohorts who were in the second trimester during flu epidemics. Another source of evidence for the viral hypothesis is the finding that the births of schizophrenia patients do not seem to be randomly distributed throughout the course of the year. Instead, the births of schizophrenia patients occur more frequently in winter months.
Some researchers have suggested that postnatal viral infection may also be relevant to schizophrenia, and that the illness may be caused by a long-acting virus. This hypothesis claims that “slow viruses,” which are active over a long period of time, interact with a genetic predisposition to produce schizophrenia. Various findings are cited in support of this hypothesis. Some researchers have identified a viral infection in fatal catatonia, a disorder characterized by schizophrenia-like symptoms, suggesting that a similar viral infection may be found for schizophrenia. Other researchers have found signs of viral activity in the cerebrospinal fluid of patients with schizophrenia.
The diathesis-stress model has dominated theories about the etiology of schizophrenia for several decades. This model assumes that certain individuals inherit or acquire a vulnerability to schizophrenia (the diathesis), and that the behavioral expression of this vulnerability is determined or triggered by environmental stressors. Although “stress” was originally conceptualized as psychosocial in origin, contemporary versions of this model broaden the definition of stress to include prenatal and postnatal insults to the central nervous system. Thus the diathesis, combined with exposure to environmental stressors, can produce schizophrenia.
Exposure to stress within the context of the family has been the focus of researchers in the field. Families in which there is a schizophrenia patient show more conflict and abnormalities in communication than do other families. However, it has also been shown that there is greater conflict and more abnormalities of communication in families in which any member has a severe debilitating illness. Thus, family communication styles are unlikely to play a unique causal role in schizophrenia.
There is good evidence, however, that exposure to high levels of criticism from family members can increase the likelihood of relapse in schizophrenia patients. The number of critical comments, expressions of hostility, and emotional overinvolvement comprise a construct referred to as expressed emotion (EE). Recovering schizophrenia patients in families high in EE are much more likely to have a relapse compared with patients in families low in EE. There is also evidence from studies of the adopted offspring of schizophrenia patients suggesting that familial stress can hasten the onset of symptoms.
Before 1900, knowledge of the nature and causes of mental disorders was limited. Individuals with psychiatric symptoms, particularly psychotic symptoms, were typically viewed by others with disdain or amusement. However, social trends and advances in medical knowledge converged to produce greater sympathy for those with mental illness. This led, especially during the early part of the century, to the construction of public and private hospitals devoted to the care of the mentally ill.
Today, most schizophrenia patients experience at least one period of inpatient treatment. This is typically precipitated by the first psychotic episode. During this initial hospitalization, an extensive assessment is usually conducted to determine the most appropriate diagnosis. Treatment is then initiated to reduce symptoms and stabilize patients so that they can return to the community as soon as possible.
In the past, periods of hospitalization were longer in duration than they are today. This is due, in part, to the availability today of better medical treatments. Another factor that has contributed to shorter hospital stays is the deinstitutionalization movement. Initially spurred by concerns that too many of the mentally ill were becoming “institutionalized” and were losing their ability to function in the community, financial support for state psychiatric hospitals was gradually cut. But community support services and transitional living arrangements were not readily available to many patients. As a result, former psychiatric inpatients now constitute a substantial proportion of the homeless found in U.S. cities.
Introduced in the 1950s, antipsychotic medication has since become the most effective and widely used treatment for schizophrenia. Research indicated that the “typical” antipsychotics, such as haloperidol, decreased the symptoms of schizophrenia, especially positive symptoms, and reduced the risk of relapse. However, they were not as effective in reducing the negative symptoms. Furthermore, some patients showed no response to antipsychotic drugs.
Chlorpromazine (Thorazine) was among the first antipsychotic commonly used to treat schizophrenia. Since the 1950s, many other antipsychotic drugs have been introduced. Like chlorpromazine, these drugs reduce hallucinations, delusions, and thought disorder, and engender more calm, manageable, and socially appropriate behavior. As mentioned, all currently used antipsychotic drugs block dopamine neurotransmission. Thus it has been assumed that their efficacy is due to their capacity to reduce the overactivation of dopamine pathways in the brain.
Unfortunately, the benefits of standard or typical antipsychotic drugs are often mitigated by side effects. Minor side effects include sensitivity to light, dryness of mouth, and drowsiness. The more severe effects are psychomotor dysfunction, skin discoloration, visual impairment, and tardive dyskinesia (an involuntary movement disorder that can appear after prolonged use of antipsychotics). It is especially unfortunate that tardive dyskinesia is sometimes irreversible when patients are withdrawn from neuroleptics. Many of these physical signs are known to be caused by chronic blockade of dopamine pathways. Although additional medications can counter some of the negative effects of the typical antipsychotics, schizophrenia patients often resist taking them because of an aversion to the side effects.
Within the past decade, some new, “atypical” antipsychotic drugs have been introduced. It was hoped that these drugs would be effective in treating patients who had not responded to standard antipsychotics. Also, researchers hoped to identify medications that had fewer side effects. One example is Clozapine, released in 1990, which seems to reduce negative symptoms more effectively than typical antipsychotic drugs. Clozapine not only offers hope for patients who are nonresponsive to other medications, but it also has fewer side effects than typical antipsychotics. However, clozapine can produce one rare, but potentially fatal, side effect, agranulocytosis, a blood disorder. Consequently, patients who are on this medication must be monitored on a regular basis. It is fortunate that several other new antipsychotic medications have recently become available, and some of these appear to have no serious side effects.
It appears that it is important to begin pharmacological treatment of schizophrenia as soon as possible after the symptoms are recognized. The longer patients go without treatment of illness episodes, the worse the long-term prognosis. Medication also has the benefit of lowering the rate of mortality, particularly suicide, among schizophrenia patients. Patients who are treated with antipsychotic medication generally require maintenance of the medication to obtain continued relief from symptoms. Medication withdrawal often results in relapse. At the same time, the associated long- and short-term side effects of antipsychotics, especially the typical antipsychotics, are of continuing concern to patients, their families, and physicians. It is possible that future research on the neural mechanisms involved in schizophrenia will lead to the development of novel treatments that eliminate the need for maintenance medication.
Many schizophrenia patients also suffer from depression and, as noted, are at elevated risk for suicide. The reason or reasons for the high rate of co-occurance of depression with schizophrenia is not known. Given the debilitating and potentially chronic nature of schizophrenia, however, it is likely that some patients experience depressive symptoms in response to their condition. For others, depressive symptoms may be medication side effects or a manifestation of a biologically based vulnerability to depression.
Clinicians have used various forms of psychological therapy in an effort to treat schizophrenia patients. Early attempts to provide therapy for schizophrenia patients relied on insight-oriented or psychodynamic techniques. The chief goal was to foster introspection and self-understanding in patients. Research findings provided no support for the efficacy of these therapies in the treatment of schizophrenia.
It has been shown, however, that supportive therapy can be a useful adjunct to medication in the treatment of patients. Similarly, psychoeducational approaches that emphasize providing information about symptom management have proven effective in reducing relapse. Among the most beneficial forms of psychological treatment is behavioral therapy. Some psychiatric hospitals have established programs in which patients earn credits or “tokens” for appropriate behavior and then redeem these items for privileges or tangible rewards. These programs can increase punctuality, hygiene, and other socially acceptable behaviors in patients.
In recent years, family therapy has become a standard component of the treatment of schizophrenia. These family therapy sessions are psychoeducational in nature and are intended to provide the family with support, information about schizophrenia, and constructive guidance in dealing with the illness in a family member. In this way, family members become a part of the treatment process and learn new ways to help their loved one cope with schizophrenia.
Another critical component of effective treatment is the provision of rehabilitative services. These services take the form of structured residential settings, independent life-skills training, and vocational programs. Such programs often play a major role in helping patients recover from their illness.
It is now firmly established that schizophrenia is caused by an abnormality of brain function that in most cases has its origin in early brain insults, inherited vulnerabilities, or both. But the identification of the causal agents and the specific neural substrates responsible for schizophrenia must await the findings of future research. There is reason to be optimistic about future research progress. New technologies are available for examining brain structure and function. In addition, dramatic advances in neuroscience have expanded our understanding of the brain and the impact of brain abnormalities on behavior. We are likely to witness great strides in our understanding of the causes of all mental illnesses within the coming decades.
It is hoped that advances will also be made in the treatment of schizophrenia. New drugs are being developed at a rapid pace, and more effective medications are likely to result. At the same time, advocacy efforts on the part of patients and their families have resulted in improvements in services. But a further expansion of services is greatly needed to provide patients with the structured living situations and work environments they need to make the transition into independent community living.
Bibliography:
- Breier, A. (Ed.). (1996). The new pharmacotherapy of schizophrenia. Washington DC: American Psychiatric Press.
- Keefe, R. S., & Harvey, P. (1994). Understanding schizophrenia: A guide to the new research on causes and treatment. New York: Free Press.
- Miller, G. A. (Ed.). (1995). The behavioral high-risk paradigm in psychopathology. New York: Springer.
- Shriqui, C. L., & Nasrallah, H. A. (Eds.). (1995). Contemporary issues in the treatment of schizophrenia. Washington DC: American Psychiatric Press.
- Torrey, E. F. (1994). Schizophrenia and manic-depressive disorder: The biological roots of mental illness as revealed by the landmark study of identical twins. New York: Basic Books.
- Walker, E. F. (1991). Schizophrenia: A life-course developmental perspective. New York: Academic Press.
ORDER HIGH QUALITY CUSTOM PAPER

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Current Concepts and Treatments of Schizophrenia
Piotr stępnicki.
1 Department of Synthesis and Chemical Technology of Pharmaceutical Substances, Faculty of Pharmacy with Division of Medical Analytics, Medical University of Lublin, 4A Chodzki St., PL-20093 Lublin, Poland; [email protected] (P.S.); [email protected] (M.K.)
Magda Kondej
Agnieszka a. kaczor.
2 School of Pharmacy, University of Eastern Finland, Yliopistonranta 1, P.O. Box 1627, FI-70211 Kuopio, Finland
Schizophrenia is a debilitating mental illness which involves three groups of symptoms, i.e., positive, negative and cognitive, and has major public health implications. According to various sources, it affects up to 1% of the population. The pathomechanism of schizophrenia is not fully understood and current antipsychotics are characterized by severe limitations. Firstly, these treatments are efficient for about half of patients only. Secondly, they ameliorate mainly positive symptoms (e.g., hallucinations and thought disorders which are the core of the disease) but negative (e.g., flat affect and social withdrawal) and cognitive (e.g., learning and attention disorders) symptoms remain untreated. Thirdly, they involve severe neurological and metabolic side effects and may lead to sexual dysfunction or agranulocytosis (clozapine). It is generally agreed that the interactions of antipsychotics with various neurotransmitter receptors are responsible for their effects to treat schizophrenia symptoms. In particular, several G protein-coupled receptors (GPCRs), mainly dopamine, serotonin and adrenaline receptors, are traditional molecular targets for antipsychotics. Comprehensive research on GPCRs resulted in the exploration of novel important signaling mechanisms of GPCRs which are crucial for drug discovery: intentionally non-selective multi-target compounds, allosteric modulators, functionally selective compounds and receptor oligomerization. In this review, we cover current hypotheses of schizophrenia, involving different neurotransmitter systems, discuss available treatments and present novel concepts in schizophrenia and its treatment, involving mainly novel mechanisms of GPCRs signaling.
1. Introduction
Schizophrenia is an important health issue, affecting almost 1% of the population, frequently with significant social and economic implications, as patients often suffer from unemployment and are homeless. Moreover, antipsychotics prescribed to treat schizophrenia are used in bipolar affective disorder, which has a prevalence of 2.3% in the population. Consequently, about 16.5 million patients in the EU need antipsychotics on a daily basis. This generates a significant healthcare costs, as central nervous system (CNS) disorders are among the most costly medical conditions (EUR 386 billion annually in the EU) [ 1 ]. Current treatments of schizophrenia have significant limitations. Firstly, they are efficient for only about half of patients enabling them independent life [ 2 ]. Secondly, they ameliorate mainly positive symptoms (e.g., hallucinations and thought disorders which are the core of the disease) but negative (e.g., flat affect and social withdrawal) and cognitive (e.g., learning and attention disorders) symptoms remain untreated [ 3 ]. Thirdly, they involve severe neurological and metabolic side effects and may lead to sexual dysfunction or agranulocytosis (clozapine) [ 4 ]. The reason for only partial effectiveness of current antipsychotics is the pathomechanism of schizophrenia which is not adequately understood due to its complexity and involvement of many molecular targets.
The current understanding of schizophrenia is constituted by the dopaminergic hypothesis which denotes alterations of dopamine neurotransmission in the mesolimbic system responsible for positive symptoms and mesocortical pathway, causing negative symptoms, complemented by the glutamatergic hypothesis which considers changes in prefrontal neuronal connectivity involving glutamatergic neurotransmission at NMDA receptor [ 5 ]. In particular, increased presynaptic dopamine synthesis is relevant for the pathogenesis of schizophrenia [ 6 ]. The methods of treatment of schizophrenia are classified as the first (mainly dopamine D 2 receptor antagonists), second (multi-target antagonists with greater antagonism at serotonin 5-HT 2A receptor than at dopamine D 2 receptor) and third generation antipsychotics represented, e.g., by aripiprazole, brexpiprazole and cariprazine. Aripiprazole is a partial dopamine D 2 receptor agonist in G α pathway but it can display agonist, partial agonist or antagonist activity at dopamine D 2 receptor upon different signaling readouts [ 7 ]. In particular it is an antagonist or a partial agonist for β-arrestin-2 signaling pathway [ 7 ].
As G protein-coupled receptors (GPCRs) are classical and well-validated targets for antipsychotics, the elaboration of concepts on the nature of GPCR signaling opens novel and unexplored possibilities for more effective and safer antipsychotics. GPCR functioning is conceptualized by the ternary complex model which involves activation of the receptor by an agonist and transmission of the signal to G protein. However, it was reported that many GPCR ligand display high degree of promiscuity which was considered a drawback in GPCR-oriented drug discovery [ 8 ]. In many complex diseases including schizophrenia, the single target drugs turned out a failure, whereas multi-target drugs are much more efficient [ 9 ]. Clozapine has a low nanomolar affinity to several aminergic GPCRs which reflexes the complex pathomechanism of the disease.
Another important breakthrough in the field was discovery that a specific receptor can couple to a few G proteins and can signal independently on G proteins by occurring in an ensemble of conformations which trigger interaction with biased ligands to downstream effectors. This phenomenon is termed the functional selectivity [ 10 , 11 ] and may lead to safer drugs thanks to selective modulation of one pathway over another one. In the field of dopamine D 2 ligands as antipsychotics, it was found that many clinically useful drugs are antagonists of β-arrestin recruitment [ 12 ]. Contrarily, it was also reported that dopamine D 2 receptor ligands which are antagonists of Gα i/o pathway and agonists of β-arrestin pathway may display beneficial antipsychotic properties with diminished extrapyramidal unwanted effects in animal models [ 7 ].
Allosteric modulation of GPCRs has lately been a hot topic in GPCR-oriented drug discovery [ 13 , 14 ] as allosteric mode of action brings important advantages over orthosteric drugs: better receptor or even pathway selectivity and fewer side effects and ceiling effect reducing the risk of overdosage [ 15 ]. This approach has not yet been exploited for antipsychotics, however a positive allosteric modulator (PAM) of dopamine D 2 receptor, a peptidomimetic PAOPA, was proven efficient in attenuating symptoms of schizophrenia in animal models [ 16 ]. Few small molecule negative allosteric modulators (NAMs) of dopamine D 2 receptor are known (SB269,652 [ 17 ]; homocysteine and analogs [ 18 ]) and their usefulness in schizophrenia needs to be further evaluated.
Finally, targeting heterodimers of dopamine D 2 receptor which are distinct pharmacological entities, in particular adenosine A 2A –D 2 and serotonin 5HT 2A –D 2 heterodimers with bivalent ligands, dimer-specific monovalent ligands, compounds causing ligand-induced dimerization and peptides, peptidomimetics or small molecules disrupting dimer interface may lead to better pharmaceutics with higher selectivity and tissue specificity [ 19 , 20 ]. Among compounds targeting these dimers only bivalent ligands (not drug-like due to high molecular weight) are relatively easy to design. Compounds from other groups are not known either for D 2 dimers (dimer-specific monovalent ligands and ligands inducing dimerization) or in the whole GPCR family (small molecules disrupting dimer interface). It was only reported that peptides, corresponding to the dopamine D 2 receptor transmembrane regions TMVI and TMVII, effectively dissociated the dimer [ 21 ].
In this review, we cover current hypotheses of schizophrenia, involving different neurotransmitter systems, discuss available treatments and present novel concepts in schizophrenia and its treatment, involving mainly novel mechanisms of GPCRs signaling.
2. Schizophrenia as a Complex Disease
2.1. dopaminergic hypothesis.
The dopaminergic hypothesis of schizophrenia is the fundament of the investigation and treatment of schizophrenia [ 22 ]. The first version of this hypothesis stressed the role of the excess of dopamine but it was developed into an idea linking prefrontal hypodopaminergia and striatal hyperdopaminergia and then to the current aberrant salience hypothesis [ 22 ].
The dopaminergic hypothesis of schizophrenia was proposed for the first time in the 1960s when chlorpromazine was introduced as the first antipsychotic and proved to treat positive symptoms of the disease [ 23 ]. Subsequently, the discovery that amphetamine produces psychosis was another proof for a role of excessive dopamine in schizophrenia. It was thus proposed that the increased dopamine neurotransmission might be a reason of this disease. The advancement of novel antipsychotics was in accordance with the dopaminergic hypothesis of schizophrenia as it was observed that positive symptoms of the disease can be attenuated with dopamine receptor antagonists. However, some findings contradicted this hypothesis, e.g., clozapine, which is a very effective antipsychotic in patients with resistant schizophrenia, has rather low affinity to dopamine D 2 receptors. Moreover, some patients with schizophrenia also have normal level of dopamine metabolites in cerebrospinal fluid or serum. These contradictions and novel findings from PET studies led Davis et al. [ 24 ] to propose that schizophrenia involves diminished frontal and increased striatal dopaminergic neurotransmission. Moreover, they linked the positive symptoms of the disease with the striatal dopamine D 2 receptor overactivation resulting from hyperactive mesolimbic dopamine projections while negative and cognitive symptoms result from the prefrontal cortex dopamine D 1 receptor hypostimulation due to diminished mesocortical dopamine projections [ 22 , 24 ]. Further reformulation of this hypothesis has been reported [ 25 ].
Nowadays, aberrant salience hypothesis of psychosis most commonly links the dopaminergic system with the symptoms of schizophrenia. It is based on the incentive salience hypothesis [ 26 ] which suggests that the mesolimbic dopaminergic neurotransmission is crucial in the attribution of salience which governs attention and affects decision making and functioning [ 22 ]. The aberrant salience hypothesis assumes that the attribution of salience is disturbed by excessive dopamine firing in psychotic episode, while, in healthy individuals, dopamine is responsible for mediating contextually appropriate saliences [ 27 ]. This revised version of dopaminergic hypothesis of schizophrenia may explain some clinical and pharmacological features of the disease, i.e., why the schizophrenia patients do not develop all symptoms of psychosis at once or why antipsychotics exert their therapeutic effects after weeks [ 22 ]. Moreover, it can also shed new light on the side effect of diminished motivation in patients with antipsychotics medication and on the recurrence of psychosis after drug withdrawal.
As mentioned above, the dopamine D 2 receptor is a drug target for all drugs against schizophrenia currently present on the market. First- and second-generation antipsychotics are dopamine D 2 receptor antagonists while third-generation drugs are partial agonists or biased ligands of this receptor. Many drugs applied to treat schizophrenia are antagonists of D 2 -like (D 2 , D 3 and D 4 ) dopamine receptor subtypes [ 28 ]. As dopamine receptor play a key role in coordination of movement, memory and cognition, emotion and affect, and the regulation of prolactin secretion, blockade D 2 -like receptors may result in side effects linked with the long-lasting antipsychotics medication. This involves parkinsonian-like extrapyramidal symptoms typically resulting from the application of the first-generation antipsychotics and metabolic side effects (weight gain, hyperglycemia, increased risk of diabetes mellitus, dyslipidemia and gynecomastia) linked with the second-generation antipsychotics [ 28 ]. In this regard, there are some reports which indicate that D 3 versus D 2 dopamine receptor selective ligands may be an interesting alternative to treat schizophrenia [ 28 ]. It has also been found that the antagonism of dopamine D 3 receptor may be partially responsible for blonanserin-caused cortical dopamine and acetylcholine efflux and cognitive improvement [ 29 ]. Importantly, selective dopamine D 3 receptor antagonists are not efficient in antipsychotic animal models based on D 2 receptor antagonism [ 30 ]. On the other hand, selective D 3 receptor antagonists influence dopaminergic neurons electrical activity in the ventral tegmental area in the way characteristic for the second-generation antipsychotics, neutralize NMDA glutamate receptor blockade effects, and increase cortical dopamine and acetylcholine in microdialysis [ 30 ]. Contrary to dopamine D 2 receptor antagonists, D 3 antagonists beneficially affect several cognitive and social features in animal models, e.g., cognitive flexibility and executive function, that are deteriorated in patients with schizophrenia [ 30 ].
It was also demonstrated that prolonged dopamine D 2 receptor blockade leads to downregulation of D 1 receptors in the prefrontal cortex and, consequently, results in significant deterioration of working memory [ 31 ]. Thus, agonism at D 1 receptors in the prefrontal cortex can have a key role in working memory and thus D 1 receptor might be a target of choice for treating cognitive deficits in schizophrenia [ 32 ].
It should be stressed that, despite a key role of dopamine in the pathomechanism and clinical practice of schizophrenia, dopamine allows understanding the pathophysiology of the disease but not the reason per se [ 22 ]. In this context, dopamine functions as the common final pathway for a number of contributing environmental and/or genetic factors [ 22 ]. Thus, other neurotransmitters, in particular glutamate, are important for the pathomechanism of schizophrenia.
2.2. Glutamatergic Hypothesis
Glutamate belongs to the main excitatory neurotransmitters and is the most common neurotransmitter in the mammalian brain [ 33 ]. Glutamatergic pathways linking to the cortex, the limbic system, and the thalamus regions are important in schizophrenia [ 34 , 35 ]. Disturbances in the glutamatergic neurotransmission may influence synaptic plasticity and cortical microcircuitry, especially NMDA receptor functioning [ 36 ]. NMDA receptors belong to ligand-gated ion channels, and are important for excitatory neurotransmission, excitotoxicity and plasticity [ 37 , 38 ]. NMDA-receptor antagonists, e.g., phencyclidine and ketamine, can mimic psychosis with similar symptoms as in schizophrenia [ 39 ]. Moreover, in therapeutic trials substances which increase NMDA receptor signaling were reported to attenuate some symptoms in patients with schizophrenia [ 40 ]. Next, in postmortem studies, some disturbances in glutamatergic receptor density and subunit composition in the prefrontal cortex, thalamus, and temporal lobe were found [ 38 , 39 , 40 ] and these are brain regions with distorted stimulation while cognitive actions are performed by schizophrenia patients [ 41 , 42 , 43 , 44 ]. NMDA-receptor hypofunction state can lead to morphological and structural brain changes which can result in the development of psychosis [ 45 , 46 ]. It was hypothesized that levels of glutamate lower with age in healthy people, but it was not determined how they are affected by the chronic illness [ 47 ].
Antipsychotics may influence glutamate transmission by affecting the release of glutamate, by interaction with glutamatergic receptors, or by changing the density or subunit composition of glutamatergic receptors [ 35 ]. It was demonstrated that antipsychotics interacting with dopamine D 2 receptor enhance the phosphorylation of the NR1 subunit of the NMDA receptor, thus reinforce its activation and consequent gene expression [ 48 ]. In this context, dopamine–glutamate interactions occur intraneuronally and intrasynaptically. There are also reports that action of some second-generation antipsychotics on NMDA receptors might be different from the effect of the first generation antipsychotics on this receptor [ 49 ]. Antipsychotics also influence glutamate transmission by acting on serotonin receptors [ 50 ].
Disturbances in glutamate signaling may be an attractive drug target for schizophrenia due to its key role in the pathomechanism of this disease in terms of cognitive impairment and negative symptoms [ 34 , 35 ]. Findings for hypoactivity of NMDA receptors in schizophrenia stimulated the clinical trials with substances activating this receptor [ 35 ]. Classical agonists at the NMDA are not useful here as excessive stimulation of NMDA receptors results in excitotoxicity and neuron damage. The glycine modulatory binding pocket on the NMDA receptor can be considered a more promising target. Similarly, positive allosteric modulators of another family of ionotropic glutamatergic receptors, i.e., α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors [ 51 , 52 ] as well as positive allosteric modulators of metabotropic glutamatergic receptors [ 53 ], might be considered promising new treatments of schizophrenia in accordance with the glutamatergic hypothesis of this disease.
2.3. Serotoninergic Hypothesis of Schizophrenia
The serotonin hypothesis of schizophrenia is derived from the reports about the mechanism of action of the hallucinogenic drug lysergic acid diethylamide (LSD) and its linkage to serotonin [ 54 ]. Consideration of the psychotic effects of LSD and the antipsychotic effects of, e.g., risperidone and clozapine, which are dopamine-serotonin receptor ligands, stimulated the research on connections between these neurotransmitters as a drug target in schizophrenia [ 55 ].
It was suggested that the overload of serotonin from the dorsal raphe nucleus (DRN) resulting from stress can disturb the activity of cortical neurons in schizophrenia [ 56 ]. Moreover, long-lasting extensive stress-derived serotonergic overload in the cerebral cortex in schizophrenia, in particular in the anterior cingulate cortex (ACC) and dorsolateral frontal lobe (DLFL), may be a key reason of this disorder [ 57 ].
Serotonin antagonists improve the extrapyramidal side effects of antipsychotics. Despite the lack of absolute proofs aberrance of serotonin signaling in the pathomechanism of schizophrenia, serotonin receptors, particularly 5-HT 3 and 5-HT 6 , still represent promising drug targets for the discovery of novel multi-receptors antipsychotic agents which can alleviate cognitive and negative symptoms of the disease [ 58 , 59 ].
Serotonin-receptor-based signaling was proposed to have an important role in the action of the atypical antipsychotics [ 60 ]. It was suggested by Meltzer et al. [ 61 ] that significant 5-HT 2A receptor antagonism accompanied by diminished dopamine D 2 receptor antagonism are the key pharmacological attributes which characterize clozapine and other second-generation antipsychotics and differentiate them from first-generation drugs. Several serotonin receptors, including 5-HT 2A / 2C , 5-HT 1A , 5-HT 6 and 5-HT 7 receptors, can be partially responsible for the “atypicality” [ 62 ]. Many studies demonstrated that partial and full 5-HT 1A receptor agonists can diminish antipsychotic-induced catalepsy. Consequently, certain second-generation drugs which display a balance between dopamine D 2 antagonism or partial agonism and 5-HT 1A receptor agonism/partial agonism result in low extrapyramidal side effects, which was demonstrated as low cataleptogenic activity in animal models [ 63 ]. Polymorphism of 5-HT 2C receptor gene is associated with olanzapine-induced weight gain [ 64 ]. Moreover, in meta-analyses, three genetic variants within serotonin genes were found linked to clozapine-associated weight gain: rs6313 and rs6314 within HTR2A gene and rs1062613 within HT3A gene [ 65 ]. Moreover, amisulpride, which has a high affinity for serotonin 5-HT 7 receptors, reversed ketamine-induced social withdrawal in rat models [ 66 ]. Next, the antagonism of 5-HT 7 receptors may be partially responsible for antidepressant and procognitive activity of amisulpride [ 67 ].
2.4. Other Aminergic GPCRs in Schizophrenia
Besides dopamine and serotonin receptors, other aminergic receptors are also linked to schizophrenia, i.e., histamine, muscarinic and adrenergic receptors. Histamine H 3 receptor antagonists can be useful in treating cognitive deficits of schizophrenia [ 68 ].
Muscarinic receptors have a key role in modulating synaptic plasticity in the prefrontal cortex and stimulation of these receptors results in long-term depression at the hippocampo-prefrontal cortex synapse [ 69 ]. Cholinergic neurotransmission is impaired in patients with schizophrenia and in animal models of schizophrenia [ 69 ]. Importantly, muscarinic receptor antagonists deteriorate cognitive and negative symptoms in schizophrenia patients and xanomeline, a muscarinic receptor agonist, ameliorates all symptoms in schizophrenia patients and corresponding animal models [ 69 ].
There are also reports that α adrenergic receptors activity can be crucial for aberrant regulation of cognition, arousal, and valence systems associated with schizophrenia [ 70 ].
2.5. GABAergic Hypothesis of Schizophrenia
Gamma-aminobutyric acid (GABA) is the main inhibitory neurotransmitter in the CNS [ 71 ]. GABAergic interneurons are crucial for suppression of the CNS, key for the synchronization and oscillations of activity of neurons which are vital for perception, learning memory, and cognition [ 72 ]. GABA signaling disturbances cause imbalance between excitation and inhibition in the cerebral cortex which is one of the key factors in the pathomechanism of schizophrenia [ 73 , 74 ]. A role of GABA in schizophrenia was first noticed by Eugene Roberts in 1972 [ 75 ]. It was first suggested that GABA can be applied for the treatment of schizophrenia as it inhibits dopaminergic signaling, however recent evidence demonstrated that, in some models, GABA can have adverse effect on the dopamine activity [ 75 ].
Post-mortem studies supported the hypothesis about a changed GABA transmission in schizophrenia [ 72 ]. Importantly, the reduction of glutamic acid decarboxylase-67, GABA synthetic enzyme was observed in brain parts linked with critical cognitive functions (the dorsolateral prefrontal cortex, anterior cingulate cortex (ACC), motor cortex, visual cortex, and hippocampus) [ 72 ].
The decrease in transmission through the TrkB neurotrophin receptor results in a diminished GABA synthesis in parvalbumin-containing subpopulation of GABA neurons in the dorsolateral prefrontal cortex of schizophrenia patients. Despite both pro- and presynaptic compensative responses, the resulting change in the perisomatic inhibition of pyramidal neurons leads to a reduced capacity for the gamma-frequency synchronized neuronal functioning, which is necessary for the working memory functioning [ 76 ].
Changes in the GABA neurotransmission were found in basic and clinical research on schizophrenia and in animal models. The chandelier subtype of parvalbumin-positive GABA neurons can be particularly altered by, and characteristic for schizophrenia [ 77 ]. GABA interneurons are key to brain rhythm-generating networks, and synchrony of neural oscillations is crucial for the perception, memory and consciousness [ 78 ]. GABA signaling disturbances can result in changes in neural synchrony [ 78 ], abnormal gamma oscillations [ 79 ], and working memory deficits.
In clinical studies, the administration of GABA agonists was demonstrated to attenuate schizophrenia symptoms [ 80 ]. Nevertheless, it is not known how GABA interplays with other neurotransmitter systems which needs further investigation.
2.6. Nicotinic Receptors in Schizophrenia
Many people suffering from schizophrenia smoke. This can be attributed to the disease itself or its treatment [ 81 ]. There are numerous reports about disturbed brain cholinergic transmission in patients with schizophrenia [ 82 ]. Patients communicate that smoking helps them to relieve negative symptoms [ 83 , 84 ] which can be linked to their deficiencies regarding nicotinic receptors.
The high rate of smokers among patients with schizophrenia stimulated the research on the role of nicotinic receptors in this disorder [ 85 ]. Studying of α7 receptors with specific venomous toxins showed that α7 receptors are located in brain regions involved in cognition (e.g., the cortex and hippocampus) [ 85 ]. Deterioration of cognitive abilities such as working memory and cognitive flexibility, as well as attention, anticipate psychotic symptoms and are a prognosticator of functional outcome [ 85 ].
Preclinical and clinical research demonstrated that the diminished suppression of P50 auditory evoked potentials in schizophrenia patients can be linked with a lowered density of α7 nicotinic receptors in the CNS [ 86 ]. Schizophrenia patients display weak inhibition of P50-evoked responses to repeated auditory stimuli, which can result from damaged sensory gating. The influence of smoking, however, on the reversing of lowered auditory sensory gating in schizophrenia may be weakened as a result of the desensitization of the nicotine receptors. This was connected with the chromosome 15q14 locus of the α7 nicotinic receptor gene [ 87 ]. Consequently, nicotinic receptors can be an attractive drug target for the treatment of schizophrenia.
The results of trials with α7 nicotinic receptor agonists or positive allosteric modulators are promising [ 88 ] but require further investigation.
2.7. The Endocannabinoid System in Schizophrenia
The endocannabinoid system is changed in schizophrenia (i.e., elevated density of cannabinoid CB1 receptor binding in corticolimbic regions and increased levels of andamide in cerebrospinal fluid). This results in “cannabinoid hypothesis” of schizophrenia [ 89 ]. Moreover, certain genetic changes of the CNR1 gene may protect against schizophrenia or can promote a better pharmacological response to atypical antipsychotics [ 89 ].
2.8. Role of Inflammation and Oxidative Stress in the Pathomechanism of Schizophrenia
The role of inflammation and oxidative stress in schizophrenia is a focus of many studies [ 34 ]. It was reported that severe infections and immune disorders during the life-time are an additional risk factor for the development of schizophrenia [ 90 , 91 ]. Although prenatal infections alone do not seem to be a definitive risk factor, the neurodevelopmental exposure to infection can facilitate the occurrence of psychosis in offspring. This can be supported by the observation that during influenza epidemics women are more likely to give birth to children who develop schizophrenia [ 92 ]. In this regard, there are inflammatory models of psychotic disorders, e.g., the anti-NMDAR encephalitis syndrome [ 93 ]. In this disease, schizophrenia-liked symptoms are combined with elevated level of NMDA receptor autoantibodies. Immunotherapy is a treatment option for this syndrome. This is also indirect proof of involvement of glutamatergic system in the pathomechanism of schizophrenia.
Another treatable immune model of schizophrenia is gluten sensitivity with the occurrence of anti-tissue transglutaminase or anti-gliadin antibodies [ 94 ]. Indeed, there can be a possible relationship between diet rich in grain products with high gluten content and the occurrence or exacerbation of schizophrenia symptoms [ 95 ].
As a consequence of inflammation role in schizophrenia, antibiotics and anti-inflammatory agents have been tested to treat this disease but with a rather limited success [ 96 ]. However, a trial of 1000 mg per day of aspirin as add on treatment demonstrated improvements in the Positive and Negative Syndrome Scale (PANSS) total and positive symptoms [ 97 ].
The importance of oxidative stress in schizophrenia was suggested in the 1930s but it was for a long time underestimated. Recent studies indicate that the oxidative stress preferentially affects interneurons which can be subjected to antioxidant therapies [ 98 , 99 ]. Next, lipid-rich white matter is also sensitive to oxidative stress which can underlie myelin-associated deficiencies in schizophrenia [ 100 ].
3. Classical Approaches to Treat Schizophrenia
Due to poor understanding of the causes of schizophrenia, the treatment, engaging antipsychotic drugs, focuses mainly on reducing the symptoms of the disease. Although psychotic illnesses include a number of various disorders, the term antipsychotic drugs—also known as neuroleptics, major tranquillizers or anti-schizophrenic drugs—conventionally refers to drugs used to treat schizophrenia. The same drugs are also used to treat brain damage, mania, toxic delirium, agitated depression and other acute behavioral disturbances. In terms of pharmacology, most are antagonists of dopamine receptor, although many of them also have an affinity for other targets, especially serotonin receptors, which may have an impact on their clinical efficacy. Currently available drugs have many drawbacks when it comes to their efficacy and side effects. Even though gradual improvements with newer drugs have been achieved, radical new approaches require a deeper understanding of the pathomechanism and causes of the disorder that are still insufficiently understood [ 101 ].
The purpose of treatment is to reduce the suffering of the patient and to improve functioning in cognitive and social area. Life-long treatment with antipsychotic drugs is required in case of many patients. Neuroleptics relieve positive symptoms of schizophrenia such as thought disorder, delusions and hallucinations, and prevent relapse. Their effectiveness is lesser on negative symptoms, which include social withdrawal and apathy. In many patients, negative symptoms have a tendency to persist between periods of treated positive symptoms, but early begun treatment of schizophrenia may prevent the development of negative symptoms over time. Patients suffering from acute schizophrenia usually respond better to treatment than those with the symptoms of chronic disease. To prevent relapses, long-term treatment is usually necessary after the first episode of the disease. Doses that are effective in acute schizophrenia should ordinarily be continued as prophylaxis [ 102 ].
The clinical effectiveness of antipsychotics in enabling patients suffering from schizophrenia to lead relatively normal lives has been presented in many controlled trials. The patient population of psychiatric hospitals, which was comprised of mainly chronic schizophrenics, declined exponentially in the 1950s and 1960s. It took place due to the introduction of neuroleptics, as well as the changing professional and public attitudes in terms of hospitalization of mentally ill patients. However, antipsychotic drugs suffer severe limitations which include:
- - (1) Some patients lack response to drug treatment. Clozapine is recommended in patients resistant to other neuroleptics. The 30% of patients that do not respond are classified as “treatment resistant” and represent a major problem regarding treatment. It is still unknown what underlies the difference between responsive and unresponsive patients, although there are some presumptions that polymorphisms within the dopamine and serotonin receptors family may be involved.
- - (2) They are effective in relieving the positive symptoms (delusions, hallucinations, thought disorders, etc.) but most of them lack effectiveness in controlling the negative symptoms (social isolation, emotional flattening) and cognitive dysfunctions.
- - (3) They may result in a wide range of side effects including extrapyramidal, sedative and endocrine effects that can limit patient compliance.
- - (4) They may decline survival through pro-arrhythmic effects.
Antipsychotic drugs of second generation were believed to overcome these limitations to some degree. However, according to meta-analysis performed by Leucht and co-workers [ 103 ], only some of the examined second-generation neuroleptics, displayed better overall efficacy. Sudden cessation of administration of antipsychotic drugs may result in a rapid onset of psychotic episode, that are different from the underlying illness [ 101 ].
The antagonism of dopamine D 2 receptors located in the mesolimbic pathway is believed to reduce the positive symptoms of schizophrenia. Unluckily, systemically administered neuroleptics do not distinguish between D 2 receptors in different brain areas and thus D 2 receptors present in other regions of the central nervous system will be blocked as well. As a result of this effect, antipsychotics lead to unwanted motor effects (blocking D 2 receptors in the nigrostriatal pathway), enhanced secretion of prolactin (blocking D 2 receptors in the tuberoinfundibular pathway), reduced pleasure (blocking D 2 receptors in the reward system component in the mesolimbic pathway) and presumably they even exacerbate the negative symptoms of the disease (blocking D 2 receptors located in the prefrontal cortex, although they occur in low abundance–D 1 receptors are expressed at higher density). While all neuroleptics, excluding third generation, act by blocking D 2 receptors and therefore, theoretically, should induce all of these side effects, some exhibit additional pharmacological activity (e.g., antagonism at muscarinic and 5-HT 2A receptor) that, to various degree, reduce unwanted effects. Blockade of 5-HT 2A receptor may also contribute to alleviating the negative and cognitive symptoms of schizophrenia [ 101 ].
The concept that serotonin dysfunction can be involved in the development of schizophrenia has come in and out of favor several times. As already mentioned, originally, it was based on the fact that LSD, which is a 5-HT 2A receptors partial agonist, produces hallucinations. However, nowadays, it is thought that serotonin is not directly associated with the pathogenesis of schizophrenia. Nonetheless, affecting serotonin receptors, combined with antagonism at D 2 receptor, has resulted in development of new drugs with improved pharmacological and therapeutic profiles. These are serotonin 5-HT 2A and 5-HT 1A receptors that play an important role in the treatment of schizophrenia.
5-HT 2A receptors belong to G i /G o -coupled receptors and, being activated, produce neuronal inhibition. In the nigrostriatal pathway, 5-HT 2A receptors control the dopamine release in this way. Drugs that are antagonists to 5-HT 2A (e.g., olanzapine, risperidone) enhance the release of dopamine in the striatum by decreasing the inhibitory effect of serotonin. It will manifest in reducing extrapyramidal side effects. Moreover, in the mesolimbic pathway, combined effects of antagonism at D 2 and 5-HT 2A receptors are suggested to counteract the enhanced dopamine function that cause positive symptoms of schizophrenia. Furthermore, block of 5-HT 2A receptor appears to improve the negative symptoms on account of enhancing the release of both dopamine and glutamate in the mesocortical circuit. 5-HT 1A receptors, which are somatodendritic autoreceptors, inhibit serotonin release. Neuroleptics that are 5-HT 1A receptors agonists or partial agonists (e.g., quetiapine) may act by reducing the release of serotonin and thus increasing dopamine release in prefrontal cortex and the striatum.
Some phenothiazine antipsychotics (e.g., periyazine) have been proven to cause fewer extrapyramidal effects than others, which is thought to be correlated with their antagonist properties to muscarinic receptors. Some second-generation drugs (e.g., olanzapine) also exhibit muscarinic antagonist properties. Dopaminergic nerve terminals in the striatum are suggested to innervate cholinergic interneurons which express inhibitory D 2 receptors [ 104 ]. Normally, there is an equilibrium between activation of dopamine D 2 and muscarinic receptor. Antipsychotic drug that block D 2 receptors in the striatum will lead to increased release of acetylcholine on to muscarinic receptors, producing extrapyramidal side effects, which are neutralized if the antagonist of D 2 receptor also display antagonist activity at muscarinic receptors. Maintaining the balance between dopamine and acetylcholine was also the rationale behind the use of benztropine, the muscarinic antagonist, to reduce extrapyramidal side effects of neuroleptics. However, antagonist activity at muscarinic receptors may result in side effects such as blurred vision, dry mouth and constipation [ 101 ].
The term “atypical” is widely used, although it has not been clearly defined. In result, it refers to the diminished tendency of later drugs to cause motor side effects, but it is also used in describing compounds that have different pharmacological profile from first-generation antipsychotics. In practice, it frequently serves—not very usefully—to distinguish the large group of similar first-generation dopamine antagonists from the group of later compounds, which is characterized by higher degree of diversity. Distinction between first- and second-generation antipsychotic drugs rests on such criteria as: receptor profile, occurrence of extrapyramidal side effects (less in second-generation group), efficacy (especially of clozapine) in resistant to treatment group of patients, and efficacy against negative symptoms [ 101 ].
It is also worth mentioning that nowadays new system of nomenclature for psychotropic medications that is neuroscience-based nomenclature (and its further update neuroscience-based nomenclature-2) is recommended [ 105 ]. This system supplies a pharmacological driven nomenclature which focuses on pharmacology and mode of action, reflecting available knowledge and understanding about the targeted neurotransmitter, molecule, system being modified, and mode/mechanism of action. It also includes four additional dimensions: (1) approved indications; (2) efficacy and side effects; (3) “practical note” which summarizes the clinical knowledge that has been prioritized by “filtering” though the taskforce’s “opinion sieve”; and (4) neurobiology.
3.1. First-Generation Antipsychotics
The first-generation antipsychotic drugs act mainly by blocking dopamine D 2 receptors in the brain. They do not exhibit a selectivity for any of the dopamine pathways in the central nervous system and therefore can lead to a range of side-effects, in particular extrapyramidal symptoms and elevated prolactin. In this and the following sections, the most common adverse effect of antipsychotics are mentioned.
The history of antipsychotic drugs dates to December 1950, when chlorpromazine, the first neuroleptic that belongs to the family of phenothiazines, was synthesized in France by the chemist Paul Charpentier as a result of research on new antihistaminic drugs. Further behavioral experiments confirmed antipsychotic properties of chlorpromazine. The release of chlorpromazine to the market took place in 1953 with the trade name Largactil , which derives from “arge” and “acti”, indicating the broad activity of the drug [ 106 ].
According to chemical structure the first-generation antipsychotics may be divided into several groups, as showed in Table 1 [ 107 ].
Classification of first-generation antipsychotic drugs: examples and their chemical structures.
The prototypical and the largest group of antipsychotic drugs in terms of chemical structure is the group of phenothiazines. It may be divided into three subclasses, which comprise in total more than forty drugs. All of them share three-ring phenothiazine structure but differ with side chains joined to the nitrogen atom (position 10 of phenothiazine) and substituents in position 2, which affects the activity of the drug. The three subgroups of phenothiazines have been distinguished considering the side chain in position 10. They are aliphatic, piperidine, and piperazine phenothiazines. The potency of drugs depends on their side chain and therefore aliphatic and piperidine phenothiazines may be characterized as agents of low to medium potency, whereas the potency of piperazine phenothiazines is described as medium to high [ 108 ].
Aliphatic group of phenothiazine derivatives is generally characterized by explicit sedative effects and moderate extrapyramidal and antimuscarinic side effects. Piperidine phenothiazines have moderate sedative effects, but cause fewer extrapyramidal side effects than other groups. Drugs with side chain containing piperazine exhibit fewer sedative and antimuscarinic effects, but more pronounced extrapyramidal side effects than in case of aliphatic and piperidine phenothiazines [ 102 ].
Another group of typical antipsychotic drugs are butyrophenones (e.g., benperidol, droperidol, and haloperidol) whose pharmacological properties are similar to those of piperazine phenothiazines, although their antidopaminergic effect is probably higher than in the case of phenothiazines, with lower antihistaminic, antiadrenergic and anticholinergic effect. Thioxanthenes exhibit moderate sedative, extrapyramidal and antimuscarinic effects, whereas diphenylbutylpiperidines are characterized by reduced sedative, antimuscarinic and extrapyramidal effects [ 108 ].
The relative potency of typical antipsychotics can be expressed by comparison with chlorpromazine and according to that first-generation neuroleptics can be arranged from low to high potency. The measure of “chlorpromazine equivalence” defines the amount of the drug in mg which allows to achieve the same effect as administration of 100 mg of chlorpromazine. The examples of high potent antipsychotic drugs are haloperidol and fluphenazine, both with chlorpromazine equivalent dose of 2 mg. Thioridazine is an antipsychotic of low potency, according to this classification, and is comparable with chlorpromazine—it must be administered in the dose of 100 mg to achieve similar potency as 100 mg of chlorpromazine [ 101 , 108 ].
Due to affecting wide range of receptors and lack of selectivity to dopamine receptors located in the mesolimbic pathway, antipsychotic drugs result in numerous side effects. The most frequent and severe are extrapyramidal effects, such as dyskinesia, dystonias, akathisia, unwanted movements, muscle breakdown, tremors and rigidity, which occur as a result of blocking dopamine D 2 receptors in the nigrostriatal pathway. High doses of typical antipsychotics may induce negative and cognitive symptoms by antagonism to dopamine receptors in the mesocortical pathway, whereas blocking those receptors in the tuberoinfundibular pathway increases the release of prolactin in the pituitary gland and leads to hyperprolactinemia. Another side effects on the CNS are sedation (resulting from antihistaminic activity), drowsiness, vertigo, disturbed sleep, agitation, nightmares, dementia, loss of memory, and depression. Blockade of α 1 adrenergic receptors may cause hypotension. Side effects on cardiovascular system comprise also tachycardia, palpitation, arrhythmia or chest pain. Antipsychotic drugs affect also liver. They increase the concentration of alkaline aminotransferase in the serum and may cause side effects such as jaundice, reversible liver cell hyperplasia, necrosis and increased level of bilirubin. Some effects from the side of the urinary and reproductive system have also been reported: impotence, increased or decreased libido, priapism, polyuria, delayed and premature ejaculation, galactorrhea and anorgasmia. Side effects related to the gastrointestinal system, such as weight gain, nausea, dry mouth, heartburn, anorexia, epigastric distress, dyspepsia, constipation, increased level of pancreatic enzymes, and abdominal cramps, are also common. Other adverse reactions that may result from the treatment with antipsychotic drugs involve: hot flashes, nasal congestion, numbness, blurred vision, dry throat, neutropenia, leukopenia, agranulocytosis, chills, glaucoma, hyperlipidemia, and depression of the respiratory system [ 101 , 108 ].
3.2. Second-Generation Antipsychotics
The new era in treating schizophrenia has begun when, after almost forty years from the introduction of chlorpromazine, the first antipsychotic, FDA approved the clinical use of clozapine in the cases of treatment-resistant schizophrenia. Clozapine has been synthesized in the laboratories of Sandoz and, after clinical trials were performed, released to the market in such countries as Switzerland, Austria, West Germany and Finland. However, studies on clozapine performed at the same time in the USA resulted in reports of agranulocytosis leading to death in some patients treated with the drug. Thus, clozapine disappeared from the market for a long time, but the interest of the scientists in working on the drug did not diminish. Further studies proved the high efficacy of clozapine in the treatment-resistant forms of schizophrenia, which resulted in the FDA approval for the drug in this disease entity [ 109 ].
Clozapine was the first drug with a stronger ability to reduce negative symptoms and that causes fewer extrapyramidal symptoms than known to date antipsychotics. The discovery of clozapine contributed to the introduction of new drugs with more beneficial pharmacological profile than first generation antipsychotics. Generally, second=generation drugs, in comparison with classical antipsychotics, exhibit higher ability to block serotonin 5-HT 2A receptors than dopamine D 2 receptors. Additionally, antagonism to D 2 receptors is weaker in the case of second-generation antipsychotics comparing to those of first generation, which manifests in lower occurrence of extrapyramidal side effects. There are also hypotheses that suggest that atypical antipsychotics bind to dopamine receptors with high dissociation rates or that they are more likely to block dopamine receptors in cortical and limbic regions than in nigrostriatal pathway, which also contributes to lower risk of extrapyramidal effects [ 110 ].
Besides schizophrenia, atypical antipsychotics are used in other diseases, such as bipolar disorder, anxiety disorder, obsessive-compulsive disorder, agitation associated with dementia and autism spectrum disorder [ 111 ]. This makes searching for novel antipsychotics even more important as there is a significant group of patients who need antipsychotics on a daily basis. Second-generation antipsychotics currently approved for clinical use include: clozapine, olanzapine, quetiapine, risperidone, paliperidone, ziprasidone, and molindone ( Figure 1 ).

The chemical structures of representatives of second-generation antipsychotic drugs.
Clozapine, as an atypical antipsychotic, is dopamine and serotonin receptor antagonist. It binds to dopamine D 1–5 receptors, with ten times higher affinity to D 4 receptors than to D 2 . Both D 4 and 5-HT 2A antagonist properties contributes to decrease of negative symptoms and lower occurrence of extrapyramidal side effects. The effect of clozapine on 5-HT 2A receptor signaling differs from classic GPCR antagonists, as it also induces 5-HT 2A receptor internalization and activates Akt signaling via a 5-HT 2A receptor-mediated event [ 112 ]. Thus, clozapine may also be considered a functionally selective agonist. At this serotonin receptor, clozapine is also serotonin 5-HT 1A receptor partial agonist, which is thought to have beneficial effect in terms of reducing negative and cognitive symptoms. Muscarinic receptors are also affected by clozapine: it blocks M 1 , M 2 , M 3 and M 5 receptors, while stimulates M 4 receptor (which results in an excessive salivation as a side effect). Clozapine’s metabolite norclozapine is an allosteric modulator of muscarinic M1 and M4 receptors [ 50 ]. The use of clozapine is associated also with sedation, as a result of antagonism to histamine receptors, and side effects from autonomous system, including hypotension and reflex tachycardia, which in turn result from blockade of α 1 adrenergic receptors. Clozapine is currently used mainly in forms of schizophrenia that are resistant to treatment with other drugs, which means that no satisfactory response has been achieved with at least two other drugs. The main limitation of clozapine is its tendency to cause agranulocytosis, which may lead to death. FDA suggests patients to control the number of white blood cells every week during first six months of treatment (it is the period of the highest risk of agranulocytosis). Afterwards, the number of leukocytes should be controlled every two weeks [ 108 ].
Olanzapine is a chemical analog of clozapine with similar pharmacological properties. However, contrary to clozapine, olanzapine causes fewer autonomic side effects and its use is not associated with a risk of agranulocytosis. Affinity of olanzapine to serotonin 5-HT 2 receptors is approximately two times higher than to dopamine D 2 receptors. It also blocks D 3 and D 4 receptors. Antagonism to histamine, muscarinic and α 1 -adrenoreceptors is weaker than in the case of clozapine. Clinical trials showed that efficacy of olanzapine in reducing positive symptoms is comparable with haloperidol, but is much more effective against negative symptoms and causes fewer side effects than haloperidol. The most frequent side effects of olanzapine are sedation and weight gain.
Quetiapine belongs to antipsychotics, which, besides schizophrenia, are used in treating bipolar disorders and major depressive disorders. Its off-label application includes insomnia, Tourette syndrome or anxiety disorders. Quetiapine acts as a dopamine D 1 , dopamine D 2 and serotonin 5-HT 2 receptors antagonist. Quetiapine is also a 5HT 1a receptor partial agonist. Antagonism to α 1 adrenergic and histamine H 1 receptor manifests in occurrence of side effects such as sedation and orthostatic hypotension.
Risperidone is the first novel atypical antipsychotic. It was introduced to the market at the beginning of the 1990s, twenty years after introduction of clozapine [ 113 ]. It is a benzisoxazole derivative ( Figure 1 ). Its pharmacological profile is reminiscent of properties of olanzapine, except that risperidone is thought to cause sedation less frequent and orthostatic hypotension more often than olanzapine. Therapeutic effect of risperidone results from antagonism to both D 2 and 5-HT 2A receptors with 5-HT 2A antagonism significantly stronger than the D 2 antagonism. Moreover, this drug also causes α 1 adrenergic and histamine receptor blockade. Its anticholinergic effects are negligible. In some patients, risperidone may elevate the level of prolactin and cause arrhythmia. The following other adverse effects may occur during treatment with risperidone: insomnia, restlessness, anxiety, headaches, agitation, EPS, headache, rhinitis, sedation, somnia, fatigue, ocular disturbances, orthostatic dizziness, palpitations, weight gain, diminished sexual desire, erectile and ejaculatory dysfunction, orthostatic dysregulation, reflex tachycardia, gastrointestinal complaints, nausea, rash, galactorrhea and amenorrhea [ 113 , 114 ]. Risperidone is efficient not only in treating positive symptoms but also negative and cognitive disturbances as well as has some anti-depressant properties which makes it one of the most commonly prescribed antipsychotics [ 113 ]. The active metabolite of risperidone is paliperidone, which acts on the same range of receptors. It is used in treating schizophrenia, as well as mania and, in lower doses, in bipolar disorder. Paliperidone comes in formulations of extended release, what allows to administer the drug once per day [ 108 ].
Ziprasidone, another second-generation antipsychotic, acts as antagonist of dopamine D 2 and serotonin 5-HT 2A receptors, partial agonist of 5-HT 1A receptor, and partial antagonist of 5-HT 2C and 5-HT 1D receptors. Besides schizophrenia it is used in acute mania or bipolar disorders [ 115 ].
Molindone acts mainly by affecting dopamine transmission in the brain. It is an atypical antipsychotic with unusual profile of pharmacological properties. It rarely causes sedation and autonomic side effects but is thought to lead to extrapyramidal side effects more frequent than other new antipsychotics, although still less frequently than classical neuroleptics. The use of molindone, contrary to other second-generation antipsychotics, rarely results in weight gain. In patients that do not tolerate or respond to other drugs, the treatment with molindone is sometimes effective [ 108 ].
Other second-generation antipsychotics include: lurasidone, iloperidone, asenapine, sertindole and amisulpiride. They are briefly presented below.
Lurasidone is a benzisothiazole derivative with high antagonist activity at serotonin 5-HT 2A and 5-HT 7 receptors and weaker antagonism at dopamine D 2 receptor [ 116 ]. It is also a partial agonist of serotonin 5-HT 1A receptor and has relatively high affinity adrebergic α 2A and weaker affinity to muscarinic receptors [ 116 ]. In general, lurasidone is effective and well-tolerated for treatment of schizophrenia and for acute bipolar depression. It has low probability of side effects such as weight-gain, and metabolic or cardiac abnormalities, but higher risk of akathisia in comparison to other atypicals [ 116 ].
Iloperidone is a benzoxazole derivative with high affinity to serotonin 5-HT 2A and dopamine D 2 receptors [ 117 ]. Iloperidone has also high affinity to α 1 adrenergic receptors and lower affinity to dopamine D 1 receptors, serotonin 5-HT 1A receptors and histamine H 1 receptors and negligible affinity to muscarinic receptors [ 117 ]. This drug has beneficial EPS and akathisia properties which makes it attractive choice for patients whose compliance is limited by these effects [ 117 ].
Asenapine is a dibenzoxepinopyrrole derivative and has a high affinity for the serotonin 5-HT 2A receptor and to a lesser extent to dopamine D 2 receptor [ 118 ] It is an antagonist of 5-HT 2C , H 1 and α2-receptors. It shares a rather complex binding profile with clozapine, olanzapine and quetiapine. The main side effects of asenapine are weight gain and metabolic disorders [ 119 ].
Sertindole is an indole derivative with a high affinity for dopamine D 2 , serotonin 5-HT 2A and 5-HT 2C , and α 1 adrenergic receptors [ 120 ]. It has also some affinity for histamine H 1 and muscarinic receptors. This drug has low probability to cause sedation and EPS and displays an acceptable metabolic profile. However, cardiac safety should be monitored during treatment with sertindole.
Amisulpiride belongs to benzamides and is a specific antagonist for dopamine D 2 and D3 receptors [ 121 ]. It has negligible affinity to serotonin receptors and receptors typically involved in side effects of atypical antipsychotics. EPS is the most common side effect of amisulpiride.
In the past decade, first-generation antipsychotics have been essentially replaced by newer, atypical antipsychotics mainly due to better toleration of second-generation antipsychotics and their more favorable profile of side effects, especially lower risk of extrapyramidal side effects. However, the second-generation antipsychotics have severe metabolic adverse effects, in particular obesity and diabetes. Weight gain and metabolic disfunctions are common in schizophrenia patients. It is attributed to the blockade of adrenergic, cholinergic, and histaminergic postsynaptic receptors by psychotropic agents [ 122 ]. Indeed, antagonism of histamine H 1 receptors is described as a key reason of second-generation antipsychotics-induced obesity [ 123 ]. Moreover, sedation, a common side effect of clozapine treatment, can be connected with clozapine binding to histamine receptors in the CNS [ 124 ]. Type 2 diabetes mellitus is their most often reported output [ 125 ]. Metabolic side effects are mainly associated with clozapine and olanzapine while data are mixed for risperidone and quetiapine [ 125 ]. For other second-generation antipsychotics, there are only few studies which examined their metabolic effects so it is difficult to draw conclusions [ 125 ].
3.3. Third-Generation Antipsychotics
The newest group of antipsychotic drugs, described as the third generation, consists of aripiprazole, brexpiprazole and cariprazine ( Figure 2 ). That group has been individualized on the grounds of their mechanism of action on dopamine receptors. Unlike other neuroleptics, third-generation drugs are not dopamine D 2 receptor antagonists but D 2 partial agonists. The D 2 receptor partial agonist properties of aripiprazole concern inhibition of cAMP accumulation through the dopamine D 2 receptor (i.e., G α signaling) [ 126 , 127 ] and in the presence of high extracellular concentrations of dopamine (e.g., in mesolimbic areas), compete with dopamine and result in partial antagonism leading to clinical benefits. Contrarily, when extracellular dopamine concentration is on a low level (e.g., in dopamine circuits that are involved in working memory), aripiprazole can bind to additional receptors and activate them partially. Hence, aripiprazole is termed as “dopamine stabilizer” [ 128 , 129 , 130 ]. It has also been demonstrated that aripiprazole is an antagonist in GTPγS binding assays with dopamine D 2 receptor [ 127 , 131 ]. Aripiprazole also failed to activate outward potassium currents following activation of dopamine D 2 receptor, which can indicate that it was inactive or an antagonist for Gβγ signaling through this receptor [ 127 ]. Next, aripiprazole, as another clinically efficient antipsychotic, is an antagonist of β-arrestin pathway [ 132 ]. Moreover, aripiprazole was also reported as agonist or antagonist of other GPCRs [ 133 ]. When it comes to serotonin transmission, aripiprazole exhibits partial agonistic properties to 5-HT 1A and 5-HT 2A (much weaker in the second case), which manifests in functional antagonism at this receptor. Contrary to antipsychotic drugs classified as second generation, aripiprazole displays higher affinity for dopamine D 2 receptor than for serotonin 5-HT 2A receptor. Clinical use of aripiprazole includes, besides schizophrenia, bipolar disorder, major depression, obsessive-compulsive disorder, and autism. Effectiveness of treating schizophrenia with aripiprazole is comparable with haloperidol or quetiapine and slightly higher than in the case of chlorpromazine or ziprasidone. Moreover, aripiprazole is characterized by better tolerability comparing to other antipsychotics [ 134 ]. Side effects that may result from treatment with aripiprazole include mainly akathisia [ 135 ] but also weight gain, agitation, insomnia, anxiety, headache, constipation or nausea [ 129 ]. However, aripiprazole results in considerably lower weight gain and lower increase in glucose and cholesterol levels in comparison to clozapine, risperidone, and olanzapine [ 136 ]. Next, aripiprazole led to weaker EPS, less use of antiparkinsonian drugs, and less akathisia, in relation to typical antipsychotic drugs and risperidone [ 136 ].

Antipsychotic drugs categorized as the third generation and their structures.
Brexpiprazole, approved by FDA in 2015, acts as partial agonist to dopamine D 2 , D 3 and serotonin 5-HT 1A receptors, and exhibits also antagonist properties to 5-HT 2A , 5-HT 2B and 5-HT 7 receptors. Its pharmacological profile is very similar to that of aripiprazole. Brexpirazole and aripiprazle are considerably different in potencies at many receptors. Their antipsychotic efficacy is comparable but brexpiprazole causes less akathisia, EPS and activation [ 137 ]. Moreover, brexpiprazole has precognitive properties [ 138 ] in contrast to aripiprazole [ 139 ]. Brexpiprazole, alone or in combination with escitalopram, facilitates prefrontal glutamatergic transmission via a dopamine D 1 receptor-dependent mechanism [ 140 ]. The drug is used in the treatment of schizophrenia and as an adjunct in major depressive disorder (e.g., in combination with fluoxentine [ 141 , 142 ]). The side effects that may result from using brexpiprazol include akathisia, weight gain, infections of upper respiratory tract, somnolence, headache and nasopharyngitis [ 143 ].
Approval of cariprazine, as well as brexpiprazole, took place in 2015. Similar to other antipsychotics from third generation, cariprazine is dopamine D 2 , D 3 and serotonin 5-HT 1A receptors partial agonist. However, its affinity for dopamine D 3 receptor is approximately ten times higher than for D 2 receptors. Cariprazine can be considered a biased agonist at dopamine receptors, with antagonist or partial agonist activity depending on the signaling pathways linked to D 2 /D 3 receptors [ 144 ]. Mean half-life for cariprazine is 2–5 days over a dose range of 1.5–12.5 mg [ 145 ]. Cariprazine has two clinically significant metabolites, desmethyl-cariprazine and didesmethyl-cariprazine, the latter having a longer half-life than cariprazine [ 145 ]. The clinical use of cariprazine includes schizophrenia and manic or mixed episodes associated with bipolar disorder. In particular, cariprazine can be used for the treatment of schizophrenia patients with dominant negative symptoms, a typically difficult to treat group of patients [ 146 ]. The treatment with cariprazine may lead to occurrence of side effects, such as sedation, akathisia, weight gain, nausea, constipation, anxiety, and dizziness [ 147 ]. Metabolic side effects of cariprazine are however negligible [ 148 ]. In summary, a potential for treatment negative symptoms, anti-abuse potential, and a long half-life make cariprazine a promising drug against schizophrenia [ 149 ].
Introduction of newer antipsychotic drugs to the clinical practice has contributed chiefly to lowering extrapyramidal side effects. Patients are less likely to suffer from akathisia, dystonias, parkinsonian symptoms or tardive dyskinesia than in the case of treatment with first generation antipsychotics. However, advantage of atypical over typical drugs when it comes to effectiveness is still discussed. Some patients respond better to newer antipsychotics and in others older drugs are more effective. This issue requires further research, which is problematic, considering schizophrenia as a chronic disease and the fact that the percentage of hospitalization of schizophrenic patients is low. It should be stressed, however, that novel compounds acting on dopaminergic system are still under investigation for the treatment of schizophrenia. Compounds such as BL 1020, ITI-007, and JNJ-37822681 have been thoroughly studied, and compounds such as L-THP, Lu AF35700, S33138, and SB-773812 are under vigorous investigation [ 150 ].
4. Targeting Novel GPCR Signaling Mechanisms in Schizophrenia
4.1. gpcrs and their novel signaling mechanisms as drug targets.
According to the classical ternary complex model, the signaling through GPCRs can be illustrated as the coaction of three main players: a receptor, an agonist and a G protein. However, more and more experimental and computational studies support the view that GPCR functioning can be much more complex than depicted by the ternary complex model.
The discovery that a specific receptor can couple to more than one G protein type and, besides that, that GPCRs could trigger G protein-independent pathways, stimulated a more nuanced characterization of GPCR ligands. Indeed, there are ligands termed biased agonists that are capable of preferentially activating one receptor-associated pathway over another [ 151 ]. This has been connected with the existence of multiple receptor states, with different propensities to couple to G proteins or other signaling partners, and which can be differentially affected by functionally selected ligands. This complex receptor modulation, which has been termed functional selectivity [ 10 , 11 ], has opened a new avenue for the interrogation of specific GPCR-activated pathways and their impact on health and disease, as well as for the subsequent detection of pathway-selective drugs with a refined mechanism of action [ 152 ]. Characterization of the significance of particular pathways associated with a given receptor can provide insight into the optimal functional selectivity profile for the treatment of a particular disease. In particular, targeting β-arrestin signaling pathways can be promising in the case of antipsychotics (see below), however it should be avoided in the case of many other drugs, e.g., antinociceptive compounds targeting the µ opioid receptor [ 153 ].
At present, another hot topic in GPCR-oriented drug discovery is the design of allosteric modulators instead of orthosteric ligands [ 154 ]. Allosteric ligands possess the ability to modulate GPCR function by binding to receptor regions away from the orthosteric binding site. Allosteric modulators usually bind to receptor areas with a low degree of conservation between GPCR subtypes [ 155 ]. This binding specificity could also be the basis for the design of more selective drugs. Additionally, the fact that allosteric modulators can function together with ligands interacting at the orthosteric binding site makes drugs exploiting this phenomenon especially useful when treatment can be achieved by enhancing or decreasing an endogenous signal. Such an approach may make it possible to solve the problem of drug dependence, overdose risk and other adverse effects linked with classical orthosteric drugs. The allosteric mode of action brings several advantages, e.g., a ceiling effect preventing overdosing, high receptor selectivity, and even activation pathway selectivity which may in consequence lead to safer and more efficient drugs [ 15 ].
In addition, the growing body of experimental (cross-linking experiments, BRET and FRET studies) and computational (coarse-grained molecular dynamics simulations) reports suggesting negative and positive cooperativity between receptors, has paved the way to the concept that GPCRs can oligomerize [ 19 , 20 ]. Both homo- and heterodimerization was reported for numerous GPCRs and the resulting protein complexes were in some cases linked to particular functional outcomes. Thus, GPCR dimers, oligomers and receptor mosaics are now considered promising drug targets, which, due to their restricted tissue distribution, can result in tissue-specific drugs. Despite a growing number of functional interactions between dimers, drug discovery targeting GPCR complexes remains a challenge. Thus, a better description of the structural aspects of GPCR oligomerization and of its effect on signaling, accompanied by the developing of original treatment strategies, seems essential for further exploration of this mechanism of GPCR signaling [ 156 ].
4.2. Targeting GPCR Signaling Complexity in Schizophrenia
The GPCR signaling mechanisms described above have been considered as potential drug targets for novel antipsychotics. The most commonly exploited approach is intentional ligand promiscuity for multi-target drugs typical for second- and, to a lesser extent, first-generation antipsychotics which requires separation of the drug targets from the off-targets [ 157 ]. The treatment of complex diseases, such as Alzheimer’s disease, Parkinson’s disease, cancer or schizophrenia, which involve multiple receptors and enzymes in their pathomechanisms, require looking for potential drugs which satisfy the criteria of many pharmacophores, oppositely to acting on a single molecular target. It should be emphasized in schizophrenia and other complex psychiatric disorders, selective single-target drugs have a very limited efficacy. Clozapine with a nanomolar affinity to several aminergic GPCRs is efficient against drug-resistant schizophrenia and reflects the molecular pathomechanism of this disease, involving cross-talk of many neurotransmitter systems (in particular, dopaminergic, serotonergic, adrenergic and glutamatergic). The new paradigm in medicinal chemistry is to look for substances that act on several molecular targets simultaneously. To accomplish that, it is essential to find structural features which combine important classes of drug targets, leading to molecules with desired selectivity profiles. Although recently implement antipsychotics (e.g., cariprazine and brexpiprazole) are the third-generation drugs, efforts are still made to design new multi-target ligands which can be developed into second generation antipsychotics [ 29 , 158 ].
The next approach that is currently under extensive investigation is biased signaling and functional selectivity. D 2 receptors couple to Gα i/o subunits, which leads to a number of signaling events through the release/rearrangement of G proteins, involving inhibition/sensitization of adenylyl cyclase, G βγ potentiation of AC2, and ERK activation as well as β-arrestin pathway [ 159 , 160 ]. Latest reports allow concluding that selective modulation of signaling pathways downstream of the D 2 receptor can lead to development of more efficient and safer antipsychotics [ 161 ]. In particular, blockade of β-arrestin pathway can be considered a common feature of antipsychotics that exhibit either antagonist or partial agonist activity through Gα i/o -cAMP pathways [ 161 ]. This supposes that β-arrestin-biased D 2 antagonists can display unique antipsychotic profiles [ 161 ]. Contrary to that, a study with analogs of aripiprazole concluded that D 2 ligands with Gα i/o antagonist and β-arrestin agonist activity can display antipsychotic properties with diminished extrapyramidal side effects in animal model [ 7 ]. Several series of biased D 2 agonists have been reported [ 7 , 162 , 163 ] as underlying ligand and receptor structural features necessary for biased signaling. Moreover, as has already been mentioned, serotonin 5-HT 2A receptor functional selectivity can be important for the activity of antipsychotics as it was reported for clozapine [ 112 , 164 ].
Allosteric modulation of D 2 receptor as a mechanism for novel antipsychotics has been not sufficiently studied. Only a peptidomimetic PAOPA ( Figure 3 ), a positive allosteric modulator of D 2 receptor, has been proven to be successful in animal models of schizophrenia. Few negative allosteric modulators are known, e.g. SB269,652, homocysteine and analogs, see Figure 3 and their antipsychotic potential needs to be evaluated. A clear finding of antagonist allosteric actions on D 2 receptor has been demonstrated for homocysteine and analogs, which supports the possibility that homocysteine analogs can be developed into an efficient antipsychotic drug, since they reduce in vitro dopamine binding. Allosteric compound SB269,652 seems to act on D 2 receptor dimer [ 165 ], similarly as bivalent D 2 receptor ligands based on agonist or antagonist structures [ 166 , 167 ], which are however not drug-like due to their high molecular weight and are pharmacological tools rather than potential drugs. At present, no dimer-specific monovalent ligands are known for D2 receptor homodimers or heterodimers of this receptor and no ligands inducing or disrupting dimerization are known.

Allosteric modulators of dopamine D 2 receptor with possible application for the treatment of schizophrenia.
In addition to allosteric modulators of dopamine D 2 receptor, positive allosteric modulators of metabotropic glutamate receptors are nowadays studied as possible treatment for schizophrenia [ 168 ]. In particular, PAMs of mGluR1, mGluR2, mGluR3 and mGluR5 are promising. Furthermore, PAMs of muscarinic receptors, e.g., M 1 and M 4 receptor could be also useful [ 168 ].
Targeting D 2 -receptor-containing dimers is a new and yet unexploited strategy for the treatment of schizophrenia. Among heterodimers formed by the D 2 receptor, adenosine A 2A –D 2 and serotonin 5-HT 2A –D 2 heterodimers in particular are implicated in the pathomechanism of schizophrenia [ 169 ]. A possible biochemical alteration in schizophrenia might not only be D 2 receptor sensitization with elevated D 2 receptor signaling, but also decreased A 2A receptor activity or interruption of A 2A –D 2 receptor interactions because of the existence of abnormal A 2A –D 2 receptor heteromers or by their disappearance [ 170 ]. Observations supporting the presence of A 2A –D 2 heteromers with antagonistic A 2A –D 2 interactions in the ventral striatopallidal GABA pathway suggested the use of A 2A receptor agonists as a strategy for the treatment of schizophrenia [ 171 ]. The antipsychotic potential of A 2A receptor agonists is underlined through behavioral analysis in animal models of schizophrenia in which they demonstrated an atypical antipsychotic profile [ 171 ]. Other classes of potential antipsychotics acting through the A 2A –D 2 receptor heteromer may be the heteromer selective D 2 receptor orthosteric or allosteric antagonists or compounds promoting ligand-induced dimerization. The possible involvement of the D 2 –5-HT 2A heterodimer in schizophrenia was proposed by studies on the hallucinogenic 5-HT 2A agonists showing that they probably induce a conformational state of the 5HT 2A protomer different from the one produced by serotonin, leading to facilitating allosteric interactions with the D 2 partner [ 171 ]. This increase in the D 2 receptor signaling in the D 2 –5-HT 2A heterodimer in the nucleus accumbens could be the basis for their psychotic actions [ 171 ]. This fact can also supply a better description of the molecular mechanism of the therapeutic effects of the second-generation antipsychotics, such as risperidone and clozapine, which block the 5-HT 2A receptor with higher potency than the D 2 receptor. It can be postulated that, in some cases of schizophrenia, this pathological facilitating interaction between 5-HT 2A and D 2 receptors has developed in the 5-HT 2A –D 2 heterodimer leading to increased D 2 protomer recognition and signaling [ 171 ]. Interestingly, 5-HT 2A or D 2 receptor antagonists acting selectively on this heterodimer or compounds disrupting the heterodimer interface might be a novel strategy to treat schizophrenia. Regarding other dimers with possible involvement in the pathomechanism of schizophrenia, mGluR2–5-HT 2A heteromer should be mentioned [ 172 ] This complex displays unique signaling when interacting with hallucinogenic drugs and activation of mGluR2 cancels hallucinogenic signaling and related behavioral responses. In postmortem studies of human brains from untreated schizophrenic subjects, the 5-HT 2A receptor is up-regulated and the mGluR2 is down-regulated which can predispose to psychosis.
5. Other Non-Classical Approaches for the Treatment of Schizophrenia
The limitations of current antipsychotics are supplemented by reports about involvement of neurtotransmitter systems other than the dopaminergic system, especially glutamate neurotransmission that contributes to the pathomechanism of schizophrenia. Thus, new drug targets resulting in drugs with novel mechanisms of action have been proposed. In particular, glutamate and nicotinic targets seems promising [ 173 , 174 ]. Selective ligands for metabotropic glutamate receptor, phosphodiesterase, glycine transporter subtype 1 and the alpha7 nicotinic acetylcholine receptor are considered worth further investigation [ 173 , 174 ].
Regarding metabotropic glutamate receptors, potentiation of mGluR2/3 and mGluR5 receptors can be beneficial in schizophrenia [ 175 ]. Although classical orthosteric agonists are still an option, subtype-selective allosteric ligands, including positive allosteric modulators of mGluR2 and mGluR5 can offer numerous advantages brought by allosteric mode of action.
Phosphodiesterase (PDE) inhibitors improve neurotransmission by affecting intracellular second messenger signaling [ 176 ]. In particular, inhibitors of PDE2, PDE4, PDE5 and PDE10 seem promising for treating cognitive symptoms of schizophrenia.
Glycine transporter 1 inhibitors applied in combination with antipsychotics are effective for relieving negative symptoms of the disease. α7 nicotinic receptor agonists and positive allosteric modulators and minocycline may treat negative and cognitive symptoms. Complementary oxytocin may help to ameliorate psychotic symptoms and social cognitive deficits. Complementary erythropoietin might benefit cognitive function [ 174 ].
6. Conclusions and Future Prospects
Although current concept and treatment of schizophrenia are still based on the dopaminergic hypothesis of the disease, novel approaches involving new signaling mechanisms on classical drug targets or completely new targets emerge. Schizophrenia is a complex multi-factor disease and according to the current knowledge it does not seem very probable that all symptoms of the disease can be treated with a single-target drug. Indeed, clozapine, which is used to treat resistant schizophrenia has a nanomolar affinity to a dozen of aminergic GPCRs. Searching for multi-target drugs beyond aminergic GPCRs may be a promising strategy to design better antipsychotics. Moreover, novel signaling mechanisms of GPCRs can lead to safer drugs with fewer side effects, e.g., allosteric modulators or biased ligands or even with tissue specificity (dimer-selective ligands). Current efforts in drug design against schizophrenia focus on searching for compounds to treat negative symptoms and to improve cognitive deficits as well as searching for compounds that are better tolerated by patients who often need life-lasting treatment.
In summary, after over a century of schizophrenia treatment, significant progress has been achieved, starting from lobotomy operations, through discovery of chlorpromazine to current second- and third-generation antipsychotics. Novel approaches, following new findings in the disease mechanisms, will finally result in new generations of drugs.
Author Contributions
P.S. wrote Section 3 ; M.K. wrote Section 2 ; and A.A.K. wrote Section 1 , Section 4 , Section 5 and Section 6 .
The work was performed under OPUS grant from National Science Center (NCN, Poland), grant number 2017/27/B/NZ7/01767.
Conflicts of Interest
The authors declare no conflict of interest.
Education Related Topics
Schizophrenia Research Topics
Schizophrenia Research Topics: Schizophrenia mainly involves a range of problems with thinking (cognition), behavior, and emotions. The signs and symptoms of Schizophrenia may vary.
When choosing schizophrenia as your research topic, it is good to understand the topic in detail.
If you are searching for Schizophrenia Paper Topics , then I am sure one of these topics will inspire you to find an ideal research topic.
Schizophrenia Paper Topics
Schizophrenia essay titles, research topics on schizophrenia, schizophrenia research paper topics.
Acceptance and Commitment Therapy versus Social Support for Smoking Cessation for People with Schizophrenia
Relationship of Corpus Callosum Integrity with Working Memory, Planning, and Speed of Processing in Patients with First-Episode and Chronic Schizophrenia
Schizophrenia And Co-morbid Conditions
Treatment Of Schizophrenia
The Enigma of Schizophrenia
Can Schizophrenia Cause The Death Of Brain Cells?
Schizophrenia and PET Scan Findings
Can Schizophrenia Affect Neurons?
Association between Intracellular Pathogens and Schizophrenia
Is Schizophrenia An Incurable Mental Illness?
How Schizophrenia Affects Cognitive Ability
Schizophrenia As A Psychotic Disorder
A Detailed Description Of A Schizophrenic Mind
How Does Schizophrenia Affect People Who Live In States That Opted Out Of The State Healthcare Exchanges?
How Can Schizophrenia Reflect On The Physical Health?
Description Of Catatonic Schizophrenia
The Diagnostic Criteria Of Schizophrenia
New Treatments for Schizophrenia
The Development Of Schizophrenia
The Vicious Cycle Of Schizophrenia
The Dangers Of Having Schizophrenia
How Schizophrenia Retards Brain Performance
Correlation Between Schizophrenia And Poverty
Treatment Of People With Schizophrenia
How Schizophrenia Affects Brain Development In Children With Schizophrenia
Schizophrenia As A Serious Disorder
Why The Reality Of Schizophrenia Frightens Many American Citizens
Ia Schizophrenia A Genetically Transmittable Illness?
How Schizophrenia Affects Mental Health
What Is The Relationship Between Unhealthy Diet And Schizophrenia?
The Mental Condition Of Schizophrenia
What Makes A Person Vulnerable To Schizophrenia?
The Side Effects Of Schizophrenia Treatment On Patients
Schizophrenic Bipolar And Schizophrenia
Childhood-Onset Schizophrenia
The Mental Health Consumer Movement And Schizophrenia
What is Schizophrenia?
Symptoms Of Schizophrenia
How Schizophrenia Develops
The Connection Between Violence And Schizophrenia
Development Of Schizophrenia
Reversible Damages That Schizophrenia Can Cause
Schizophrenia and Homelessness
Irreversible Damages That Schizophrenia Can Cause
Are There Effective Drugs Against Schizophrenia?
How Do People With Schizophrenia Perceive Their Environment?
Schizophrenia Among Healthcare Professionals
The Mental Illness Of Schizophrenia
The Effect Of Medical Marijuana On Individuals with Schizophrenia
Schizophrenia – Longitudinal Studies
Non-Genetic Factors That Can Cause Schizophrenia
Analysis of Catatonic Schizophrenia
The Dangers Of Living With Schizophrenia
The Pathogenesis of Schizophrenia
How To Prevent The Development Of Schizophrenia In Children
The similarity between bipolar disorder and schizophrenia
Schizophrenia And Cognitive Ability
A Person With Schizophrenia
The Possible Future Of Schizophrenia
Trial Treatments for Schizophrenia
Schizophrenia and Neuroplasticity
Therapy For Schizophrenia
What It Take To Treat Schizophrenia
Symptoms And Treatment Of Schizophrenia
Early Signs Of Schizophrenia
Schizophrenia And Other Psychotic Disorders
How Schizophrenia Changes Brain Function
Mental Health Condition Of Schizophrenia
How To Reverse The Negative Impacts Of Schizophrenia
How The ‘Glutamate Theory’ Is Related To Schizophrenia
The Relationship Between Schizophrenia And Loss Of Memory
Is Any Particular Race More Vulnerable To Schizophrenia?
Living With Schizophrenia
Schizophrenia and Aging
Schizophrenia Of Children And Adolescents
Genetic Links Between Associated Co-morbid Conditions and Schizophrenia
Diagnosis Of Schizophrenia
The Effects Of Schizophrenia On Children
The History of Schizophrenia
Disorder of Lifespan Development And Schizophrenia
How Schizophrenia Affects Consciousness
How Do Genetic Factors Contribute To The Development Of Schizophrenia?
What Are The Dangers Associated With Late Treatment Of Schizophrenia?
How Schizophrenia Affects Women
Causes Of Schizophrenia
The Health Risks Associated With Schizophrenia
A Report On Schizophrenia
Is Schizophrenia A Mental Disorder?
Medical Solution To Schizophrenia
Psychotherapy For Treating Schizophrenia
The Effects Of Schizophrenia On Adults
Behavioral Aetiology Of Schizophrenia

Steve George is Blogger, a marketer and content writer. He has B.A. in Economics from the University of Washington. Read more about Mzuri Mag .
- How Long Is a Dissertation
- Mental Health Topics to Write About
- Ecology Topics for Research Paper
- Mental Health Informative Speech Topics
- Abnormal Psychology Research Topics
- Psychology Capstone Project Ideas

IMAGES
VIDEO
COMMENTS
Schizophrenia in 'A Beautiful Mind' Film. The main symptom of a schizophrenic patient depicted in the film is the patient's inability to distinguish between the real world and the subconscious pattern created within the imaginations of his mind. The Current Concept of Schizophrenia Is Neither Valid and Useful.
As a student studying psychology or mental health, you may be tasked with writing an essay on schizophrenia. To help you get started, we have compiled a list of 108 schizophrenia essay topic ideas and examples to inspire your writing. The history of schizophrenia research and treatment. The prevalence of schizophrenia in different populations.
30 Schizophrenia Research Topics. Schizophrenia is a mental disorder that affects how a person thinks, feels, and behaves. People with schizophrenia may seem like they have lost touch with reality. Although there is no cure for schizophrenia, it can be treated with medication, therapy, and support. In this article, we will provide an overview ...
1. INTRODUCTION. This paper reports a review of outcomes in schizophrenia in the twenty‐first century and is an extension of the work undertaken by the late Dr Richard Warner in his seminal book, "Recovery from Schizophrenia: Psychiatry and Political Economy" (1985 (Warner, 1985); 2004 (Warner, 2004)).The present work was started with Dr Warner's involvement, and the preliminary results ...
👍 Good Schizophrenia Research Topics & Essay Examples. On-time delivery! Get your 100% customized paper done in as little as 1 hour. Let's start. Factors That Caused Schizophrenia. Schizophrenia is a common mental disorder among the young males and females, therefore, the paper finds out the various effects of disorder on the young adults.
Read the latest Research articles from Schizophrenia. The relationship between visual hallucinations, functioning, and suicidality over the course of illness: a 10-year follow-up study in first ...
Schizophrenia is a debilitating disease that presents with both positive and negative symptoms affecting cognition and emotions. Extensive studies have analyzed the different factors that contribute to the disorder. There is evidence of significant genetic etiology involving multiple genes such as dystrobrevin binding protein 1 (DTNBP1) and ...
Schizophrenia is an often debilitating, chronic, and relapsing mental disorder with complex symptomology that manifests as a combination of positive, negative, and/or cognitive features 1,2,3 ...
2. Definitions and Concepts on Schizophrenia. While the cluster of symptoms that clinically define the schizophrenia concept has been noted historically before the 1990s, schizophrenia scientific research was mainly developed following the studies that were carried out by the German psychiatrist Emil Kraeplin (1856-1926) who identified a set of symptoms related to the schizophrenia disease ...
The goal of this special edition Research Topic is to shed light on the progress made in the past decade in the Schizophrenia field, and on its future challenges to provide a thorough overview of the field. This article collection will inspire, inform and provide direction and guidance to researchers in the field.
Schizophrenia is a chronic severe brain disorder characterized by altered perception and the manner of expression of reality. The effects are manifested as hearing voices. Antipsychotics, Metabolic Adverse Effects, and Cognitive Function in Schizophrenia. Schizoaffective Disorder: The Bridge Between Schizophrenia and Bipolar.
The aim of this special issue is to provide a forum of review papers and original studies that address hot topics related to the etiology and emerging treatments of schizophrenia-spectrum disorders. Dr. Andreas Reif. Dr. Blazej Misiak. Dr. Jerzy Samochowiec. Guest Editors. Manuscript Submission Information.
Best Schizophrenia Research Paper Topics. Genetic Factors in the Development of Schizophrenia: Unraveling the Complex Puzzle. Exploring the Onset of Schizophrenia: Early Signs and Predictors. Psychosis Beyond Perception: Understanding the Various Facets. The Etiology of Schizophrenia: An In-Depth Examination.
Abstract. Schizophrenia is a mental disorder characterized by disruptions in thought processes, perceptions, emotional responsiveness, and social interactions. Schizophrenia affects approx. 24 million people or 1 in 300 people (0.32%) worldwide. This rate is 1 in 222 people (0.45%) among adults.
Reviews in Schizophrenia will publish high-quality scholarly review papers on key topics in Schizophrenia. It aims to highlight recent advances in the field, whilst emphasizing important directions and new possibilities for future inquiries. We anticipate the research presented will promote discussion in the Schizophrenia community that will ...
Schizophrenia Research Topics: Schizophrenia is a complex mental disorder. When writing research topics on Schizophrenia one has to be very careful on the topics since one should be conversant with the topic. Hope the list of schizophrenia research paper topics below will give you a starting point in writing your research paper.
Schizophrenia is a highly disabling disorder whose causes remain to be better understood, and treatments have to be improved. However, several recent advances have been made in diagnosis, etiopathology, and treatment. Whereas reliability of diagnosis has improved with operational criteria, including Diagnostic and Statistical Manual of Mental ...
Schizophrenia Research Paper Topics. Schizophrenia is a chronic mental disorder that affects how a person thinks, expresses emotions, acts, and perceives reality. Schizophrenia is among the most complex mental disorder. Due to its complex nature, students have a high chance of struggling with schizophrenia research paper topics.
Sample Schizophrenia Research Paper Topics. Just in case you need a topic to write on for your research paper on Schizophrenia, here are a few topics you can work with: The role of alkaloid in schizophrenic psychosis. Relationship between schizophrenic psychosis and animate thing Pathogens Medical Marijuana and its impact on people with ...
Schizophrenia is a complex and often misunderstood mental health disorder that affects millions of individuals worldwide. This essay aims to provide a comprehensive overview of schizophrenia, including its historical development, prevalence, symptoms, diagnosis, treatment options, impact on daily life and functioning, current research, and future...
Schizophrenia Research Paper. This sample schizophrenia research paper features: 6600 words (approx. 22 pages), an outline, and a bibliography with 6 sources. Browse other research paper examples for more inspiration. If you need a thorough research paper written according to all the academic standards, you can always turn to our experienced ...
Schizophrenia is a debilitating mental illness which involves three groups of symptoms, i.e., positive, negative and cognitive, and has major public health implications. According to various sources, it affects up to 1% of the population. The pathomechanism of schizophrenia is not fully understood and current antipsychotics are characterized by ...
Schizophrenia Research Topics. Updated: January 1, 2024 by Steve George. Schizophrenia Research Topics: Schizophrenia mainly involves a range of problems with thinking (cognition), behavior, and emotions. The signs and symptoms of Schizophrenia may vary.
Schizophrenia is a serious brain disorder marked by positive symptoms (hallucinations and delusions, disorganized speech and thoughts, and agitated or repeated movements) and negative symptoms ...