Poverty and Health

Poverty is a major cause of ill health and a barrier to accessing health care when needed. This relationship is financial: the poor cannot afford to purchase those things that are needed for good health, including sufficient quantities of quality food and health care. But, the relationship is also related to other factors related to poverty, such as lack of information on appropriate health-promoting practices or lack of voice needed to make social services work for them.
Ill health, in turn, is a major cause of poverty. This is partly due to the costs of seeking health care, which include not only out-of-pocket spending on care (such as consultations, tests and medicine), but also transportation costs and any informal payments to providers. It is also due to the considerable loss of income associated with illness in developing countries, both of the breadwinner, but also of family members who may be obliged to stop working or attending school to take care of an ill relative. In addition, poor families coping with illness might be forced to sell assets to cover medical expenses, borrow at high interest rates or become indebted to the community.
Strong health systems improve the health status of the whole population, but especially of the poor among whom ill health and poor access to health care tends to be concentrated, as well as protect households from the potentially catastrophic effects of out-of-pocket health care costs. In general, poor health is disproportionately concentrated among the poor.
The World Bank’s work in the area of health equity and financial protection is defined by the 2007 Health, Nutrition and Population Strategy . The strategy identifies “preventing poverty due to illness (by improving financial protection)” as one of its four strategic objectives and commits the Bank’s health team, both through its analytical work and its regional operations, to addressing vulnerability that arises from health shocks.
The strategy also stresses the importance of equity in health outcomes in a second strategic objective to "improve the level and distribution of key health, nutrition and population outcomes... particularly for the poor and the vulnerable".
The Bank supports governments to implement a variety of policies and programs to reduce inequalities in health outcomes and enhance financial protection. Generally, this involves mechanisms that help overcome geographic, social and psychological barriers to accessing care and reducing out-of-pocket cost of treatment. Examples include:
- Reducing the direct cost of care at the point of service, e.g. through reducing/abolishing user fees for the poor or expanding health insurance to the poor (including coverage, depth and breadth).
- Increasing efficiency of care to reduce total consumption of care, e.g. by limiting “irrational drug prescribing,” strengthening the referral system, or improving the quality of providers (especially at the lower level).
- Reducing inequalities in determinants of health status or health care utilization, such as reducing distance (through providing services closer to the poor), subsidizing travel costs, targeted health promotion, conditional cash transfers.
- Expanding access to care by using the private sector or public-private partnerships.
The Bank’s health team also promotes the monitoring of equity and financial protection by publishing global statistics on inequalities in health status, access to care and financial protection, as well as training government officials, policymakers and researchers in how to measure and monitor the same.
Examples of how World Bank projects have improved health coverage for the poor and reduced financial vulnerability include:
The Rajasthan Health Systems Development Project resulted in improved access to care for vulnerable Indians. The share of below-poverty line Indians in the overall inpatient and outpatient load at secondary facilities more than doubled between 2006 and 2011, well exceeding targets. In the same period, the share of the vulnerable tribal populations in the overall patient composition tripled.
The Georgia Health Sector Development Project supported the government of Georgia in implementing the Medical Insurance Program for the Poor, effectively increasing the share of the government health expenditure earmarked for the poor from 4% in 2006 to 38% in 2011. It also increased the number of health care visits of both the general population and the poor, but by more for the poor (from 2 per capita per year to 2.6) than for the general population (from 2 to 2.3) over the same time period.
The Mekong Regional Health Support Project helped the government of Vietnam to increase access to (government) health insurance from 29% to 94% among the poor, as well as from 7% to 68% among the near-poor. Hospitalization and consultation rates, at government facilities, also increased among both the poor and near-poor.
Analyzing Health Equity Using Household Survey Data
AdePT Software
- PUBLICATION Health Equity and Financial Protection Datasheets
- PUBLICATION Health Equity and Financial Protection Country Reports (2012)
- ADEPT TRAINING ADePT Training Resource Center
This site uses cookies to optimize functionality and give you the best possible experience. If you continue to navigate this website beyond this page, cookies will be placed on your browser. To learn more about cookies, click here .

- Our history
- Find Your Feet
- Newsletters
- Accounts & reports
- Jobs & tenders

Key Facts: Poverty and Poor Health
On 10th January 2018 by Sorsha Roberts
Poverty and poor health worldwide are inextricably linked.
What links poverty and poor health?
Poverty and poor health worldwide are inextricably linked. The causes of poor health for millions globally are rooted in political, social and economic injustices. Poverty is both a cause and a consequence of poor health. Poverty increases the chances of poor health. Poor health, in turn, traps communities in poverty. Infectious and neglected tropical diseases kill and weaken millions of the poorest and most vulnerable people each year.
What other links are there between poverty and poor health?
- The economic and political structures which sustain poverty and discrimination need to be transformed in order for poverty and poor health to be tackled.
- Marginalised groups and vulnerable individuals are often worst affected, deprived of the information, money or access to health services that would help them prevent and treat disease.
- Very poor and vulnerable people may have to make harsh choices – knowingly putting their health at risk because they cannot see their children go hungry, for example.
- The cultural and social barriers faced by marginalised groups – including indigenous communities – can mean they use health services less, with serious consequences for their health. This perpetuates their disproportionate levels of poverty.
- The cost of doctors’ fees, a course of drugs and transport to reach a health centre can be devastating, both for an individual and their relatives who need to care for them or help them reach and pay for treatment. In the worst cases, the burden of illness may mean that families sell their property, take children out of school to earn a living or even start begging.
- The burden of caring is often taken on by a female relative, who may have to give up her education as a result, or take on waged work to help meet the household’s costs. Missing out on education has long-term implications for a woman’s opportunities later in life and for her own health.
- Overcrowded and poor living conditions can contribute to the spread of airborne diseases such as tuberculosis and respiratory infections such as pneumonia. Reliance on open fires or traditional stoves can lead to deadly indoor air pollution. A lack of food, clean water and sanitation can also be fatal.
Which infectious diseases are the main killers worldwide?
HIV, diarrhoea, tuberculosis and malaria, as well as communicable respiratory diseases such as pneumonia kill the most people. Diarrhoea, pneumonia and malaria account for nearly half of all child deaths globally.
Neglected tropical diseases affect over one billion people, almost all in the poorest and most marginalised communities. You may not have heard of diseases such as leprosy, lymphatic filariasis, onchocerciasis, schistosomiasis, soil-transmitted helminths and trachoma, but they can cause severe pain and life-long disabilities – and mean enormous productivity losses. However, efforts to tackle them have usually taken a back seat to the bigger killers.
Which are the most deadly non-communicable illnesses worldwide?
The biggest non-communicable killers are maternal and newborn deaths and deaths related to poor nutrition, cardiovascular disease and non-communicable respiratory diseases.
How do disease and infection affect economic growth?
- Lives lost mean reduced economic productivity as well as personal tragedy. Productivity is further slowed while people are ill or caring for others. There were 1.7 HIV-related deaths in 2007 and 990 thousand deaths from tuberculosis. Most of these were among young people and adults in their most productive years.
- In heavily affected countries billions of dollars of economic activity are lost each year as a result of illness and death from HIV, TB and malaria. This can seriously reduce economic growth in countries that are already struggling. Malaria reduces economic growth by 1.3% in heavily affected countries, and costs around $12 billion in lost GDP across Africa. TB costs around 7% of GDP in the worst affected countries.
How has the global community responded?
World leaders and international organisations have slowly woken up to the impact of the most prevalent infectious diseases. The World Health Organisation has declared TB, HIV and malaria global emergencies. Reducing the spread and treating HIV, TB, malaria, and other diseases is also one of the Millennium Development Goals.
However, as well as tackling specific diseases, it is crucial that leaders also address the underlying causes. It is widely accepted that the key reason for the increase in life expectancy in wealthy countries in the late 19th and early 20th century was less to do with the leaps forward in medical science, and more to do with the arrival of better nutrition, clean water and sanitation.
Reducing poverty, improving nutrition and making sure people have access to safe water and sanitation, as well as strengthening national health systems, is of the utmost importance. Otherwise tackling one particular threat simply leaves people open to another deadly disease soon afterward.
Tackling the structural causes of poverty and poor health, for example calling for measures to tackle inequality and injustices such as corporate tax evasion, are central to what is needed from the global community.
How poverty is created
The cycle of poverty and poor health, health systems.

Keep in touch
Be part of the global movement for better health, almost there....
Sign up to be a part of our global movement for health justice, including how you can get involved in our work through campaigning and fundraising. On average you may receive an email once every two weeks, and you can unsubscribe at any time.
For more information on how we process your data, you can read Health Poverty Action’s privacy notice here .
Sign up to be kept up to date on the global movement for better health, including how you can get involved in our work through campaigning and fundraising.
Privacy policy
Causes Of Poor Health Essay

Show More Poor health causes Health is the most important thing in one person’s life. But in the last fifty years the whole world is facing problems with health. This problem became huge, especially in the United States of America. People and the Government are trying to solve this problem, but it is getting bigger and bigger. Every year the Government spends 150 billion dollars for solving this problem, but maybe they do not know where the core of this problem is. We can find obesity within young people and children. The question is: “What are the causes of this and is it too late for solving this problem?” Obesity is one of the poor health causes. A lot of children in middle school and in high school are obese. Almost every teacher will say this: “Parents are buying what the kids want, rather than what may be healthy for them” (fourth-grade teacher 1). We can say that their parents are responsible for their children’s health but the question is, can parents do something about it? I do not think so because the problem is in the food and ingredients we can find in food. A lot of scientists will say that there is a …show more content… To be healthy people have to put some effort in. Or maybe they do not. Just carefully choose what are you eating and stay away from fast food. I did not mention physical activity which is very important in every human’s life. Physical activity on a daily basis should be everybody’s routine. A lot people will say that you are what you eat, but just a minority will actually do that, which means be careful with food. So I think that all these problems with overweight and obesity can be solved, starting in people’s heads. I want to say that it is all on us, because at the end of the day we choose what are we going to eat and nobody is forcing us to eat something that we do not want to. There are big chances for us to get out of this big problem, but we should do something about it right
Related Documents
Persuasive essay on school lunches.
Childhood obesity is the beginning of obesity so we need to control it at a young age. “What a horrible place we've come to in this country. We're in the throes of an obesity crisis, and diet-related illness is on the rise. The CDC has stated that of children born in the year 2000-- those ten-year-old kids in fourth or fifth grade this year, one out of every three Caucasians and almost one out of every two African American and Hispanics will contract diabetes in their lifetime, most before they graduate high school. This means that one-third-- yes, one third-- of all children will become overweight or obese.…
Eating In-N-Out: Right
I believe that since children are incapable of balancing their diet and exercise it is up to the parent. If we rely on government intervention we will be sacrificing our civil…
Liberty High School Research Paper
Every year people die due to diseases caused by obesity. According to Ryan Masters of the Robert Wood Johnson Foundation Health & Society Scholar, "Obesity accounts for 18 percent of deaths among Americans between the ages of 40 and 85". That is a large group of people who die due to obesity diseases. To solve this problem we have to change the school system.…
Persuasive Speech: Gull Lake High School
Thank you ladies and gentlemen of the Gull Lake School board for being here. What if I told you I could sufficiently reduce the amount of stress and increase social and academic ability for students here at Gull Lake High School? While also providing long-term benefits of decreasing the risk of cancer, diabetes, high blood pressure, and high cholesterol. By making one annual physical education course mandatory for high school students here at GL. This proposition administers an immense amount of health benefits as well as stress relief, social development, and escalation in academic performance.…
Tp1 Application Of Effective Communication Paper
Application of Effective Communication – TJP1 Mallory McLean Western Governors University Student ID # 000596676 I. Introduction 1. Hook: Most adults in our country obese. This is also an alarming statistic showing in our children. Research shows that when you have obese parents their children are more likely to be overweight as well. This trend needs to change.…
Analysis Of Being Fat Is Ok By Paul Campos
Being Fat Is Not Ok Most of Americans are currently realizing that obesity is bad but being fat does not related on their health condition. Thus far, According to Paul Campos, the author of the essay “Being Fat Is Ok” for Americans, being fat is considered to be ok because he said that there is not enough evidence to show that this condition is a problem. The continuous condition of being overweight can lead to obesity for many people which will result in the obesity epidemic which affects people’s health. In facts, obesity has negative health effect such as diabetes, high blood pressure, and increase the likelihood of a stroke.…
Childhood Obesity Proposal
Being overweight is a matter that is continuously increasing. Actions towards childhood obesity need to be taken, and parents, schools, the government, and physicians need to be involved. The main goal for these groups should be to get children eating healthier and being more active. Unfortunately, there is no special solution to this issue, but if people take the time and make life changes to improve the well-being of children and themselves, then positive outcomes will be the ending result. It will not only improve the child’s life now, but it could reduce the risks of complications in their adulthood.…
Obesity Epidemic In America
The obesity epidemic in the United States is now three decades old, continuing to worsen over the years. Many Americans are fearful of being categorized as obese because of the risk of other developing health conditions that come along with it, including: heart disease, cancer, diabetes or sleep apnea, just to name a few. Obesity is looked at as a simplistic issue because being larger than others automatically means that one is lazy right? This is the attitude taken towards this subject. Many people do not understand the complexity of obesity, but medical professionals and other researchers are starting to take a look into why the number of people being diagnosed as obese is increasing.…
The Controversy Of Obesity In The United States
The Controversy of Obesity Obesity is a major problem in America. The numbers of obese people in the United States have steadily increased since the 1970’s. Over a fourth of the population in America is obese, leading it to be the among the most obese countries in the world. Obesity can be solved.…
Childhood Obesity In America Essay
In the United States, childhood obesity rates have more than tripled since the 1970s, with roughly one in six children aged six to nineteen suffering from obesity according to an article from Gale, a Cengage Company (GCC). Furthermore, overweight or obese preschoolers are 5 times more likely than normal-weight children to be overweight or obese as adults, according to an article published by the Obesity Society (OS). This rapid increase in obesity is not the product of changing biology or genes; it is the product of an obesogenic environment that promotes inactivity and overeating, according to an article published by the American Psychological Association (Johnson). There are many reasons for this dramatic increase that happen every day.…
Factors Of Childhood Obesity
They prefer to take their children out for dinner instead of making an effort and cooking a homemade meal. In today’s household most parents work full time, this gives parents little time to prepare proper meals for their family. This, in part due to the hectic and fast pace lives of dual income families. The core problem of childhood obesity is due to the lack of understanding and education that parents have, parents need to equip themselves with the necessary skills, in order to maintain their children’s well being so that the unhealthy risk factors can be avoided. Unhealthy weight gain due to poor diet and lack of exercise is responsible for over 300,000 deaths each year.…
Possible Solutions To The Obesity Problem In America
Obesity in America becomes a more relevant issue as time progresses and people develop terrible habits. Yvette C. Terrie, a writer from U.S. News Health states, “In the past two decades in the United States, there 's been an alarming increase in obesity rates among all age groups, even children. It 's estimated that more than one-third of adults and 17 percent of children and adolescents are obese.” These numbers are alarming because of the massive amounts of health problems that obesity causes such as diabetes, Coronary artery disease, and cancer (Terrie). Although it may not seem like it, some obese people have diseases or health complications that result in excessive overweight.…
How To Prevent Childhood Obesity Essay
Abstract This paper will be discussing childhood obesity and gives ways to improve one’s lifestyle. I will be giving information all about this topic that is accurate based on official websites and readings. I will be giving ways to change children’s lifestyles that are healthy and explain how it will benefit them and help prevent childhood obesity. I have also interviewed a high school teacher of mine that will give her input on this topic.…
Analysis: The Fight Against Childhood Obesity
The Fight Against obesity Childhood obesity is causing a broad range of health problems that previously weren’t seen until adulthood. There are several causes for obesity in America, including fast- food restaurants and their marketing. Childhood obesity in America is a growing disease that has become an epidemic that has health risk effects. Parents should take the lead in fighting against childhood obesity. In order to protect our children, parents should have a better understanding about obesity; encourage active lifestyle for their children and why fast food contributes to obesity.…
Argumentative Essay About Obesity
Our world, due to various reasons, is filled with all types of diseases. The latest of them all is the one called obesity. This word is presently the talking point of people all around the globe. Rising obesity rates have now become a major public health concern around the world. Prolonged obesity has implications for health at older ages, and these health effects may increase the costs of health care for individuals and governments.…
Related Topics
- Hypertension
Ready To Get Started?
- Create Flashcards
- Mobile apps
- Cookie Settings
Poverty and Health - The Family Medicine Perspective (Position Paper)
Introduction
Poverty is a complex and insidious determinant of health caused by systemic factors that can persist for generations in a family. Beginning before birth and continuing throughout an individual’s life, poverty can significantly impact health and health outcomes. The vision of the American Academy of Family Physicians (AAFP) is to transform health care to achieve optimal health for everyone. Primary care physicians and public health professionals continue to collaborate on a shared vision of improving population health. As the integration of primary care and public health continues, this shared vision becomes even more relevant, focused, and clear. Success in this new era means achieving better outcomes by transforming health care to overcome obstacles related to the social, environmental, and community determinants of health – including poverty. 1,2,3,4
Family physicians have a unique perspective on local population’s health challenges because we serve generations of families and follow individual patients through different life stages. We are privileged to share the complex stories of individuals and families in sickness and health over long periods and across different care settings. Rather than viewing a single snapshot of a patient during an episode of illness, we know the patient’s whole story. We know the environmental, patient, and family factors that lead to illness and disease – and the patient’s need to manage their condition effectively. As lifelong collaborators in care, family physicians are well-positioned to understand each patient’s unique obstacles to better health and help overcome them.
Call to Action
The AAFP urges its members to become informed about the impact of poverty on health. Achieving the vision of optimal health for everyone requires a culturally proficient care team and a well-resourced medical neighborhood that supplies readily accessible solutions. Family physicians play a critical role in community health and can contribute through bold efforts in many areas. When these solutions are incorporated seamlessly into everyday practice workflows, family physicians and care teams can be true to the AAFP’s vision by achieving positive change for individuals, families, and communities, and improve population health.
The AAFP calls for action in the following areas:
Physician Level
- Become more informed about the impact of the social determinants of health (SDoH) and identify tangible next steps you can take to address and reduce health inequities
- Be aware of, and sensitive to, your patient’s specific circumstances to help them achieve their health goals
Practice Level
- Identify critical factors that impact patient health, leveraging The EveryONE Project and data collection on SDoH in electronic health records (EHRs)
- Understand each patient’s unique challenges and coping strategies and know what community resources are available
Community-Leadership Level
- Promote alignment with other private and public community resources to help advance the integration of primary care and public health
- Partner with other health care and social service organizations to connect directly to resources that mitigate poverty’s effect on health
Educational Level
- Drive change in undergraduate and graduate medical education to ensure future physicians are adequately prepared to prevent and address disparities caused by SDoH
Advocacy Level
- Work with local, state, and national governments to adopt a Health in All Policies approach that prioritizes health within goals and agenda-setting
- Advocate for regulatory frameworks and economic incentives to ensure public health and population health are critical to individual health care efforts
Understanding Poverty and Low-income Status
Poverty occurs when an individual or family lacks the resources to provide life necessities, such as food, clean water, shelter, and clothing. It also includes a lack of access to such resources as health care, education, and transportation. 5 In the United States, federal poverty is expressed as an annual pre-tax income level indexed by the size of household and age of household members. For example, in 2020, the federal poverty income level was $12,760 for an individual younger than 65 years and $26,200 for a family of four. 6 In 2019, approximately 10.5% of Americans were living below the poverty line. While overall poverty rates had been declining in the past several years, inequalities remain by SDoH, including race and racism, ethnicity, educational attainment, and disability status. 7
The term “low income” generally describes individuals and families whose annual income is less than 130-150% of the federal poverty income level. For example, the Supplemental Nutrition Assistance Program (SNAP) is available to individuals with a gross monthly income of 130% of the federal poverty income level. 8 Medicaid is open to families with an income of 138% of the poverty income level. 9
Poverty and low-income status are associated with various adverse health outcomes, including shorter life expectancy, higher infant mortality rates, and higher death rates for the 14 leading causes of death. 10,11 Individual- and community-level mechanisms mediate these effects. 12 For individuals, poverty restricts the resources used to avoid risks and adopt healthy behaviors. 13 Poverty also affects the built environment (i.e., the human-made physical parts of the places where people live, work, and play, including buildings, open spaces, and infrastructure), services, culture, and communities’ reputation, all of which have independent effects on health outcomes. 14
Location matters, and there are often dramatic differences in health care delivery and health outcomes between communities that are only a few miles apart. For example, the Robert Wood Johnson Foundation (RWJF) found a 25-year difference in average life expectancy in New Orleans, LA, between inner city and suburban neighborhoods. Similarly, there is a 14-year difference in average life expectancy between two Kansas City, MO, neighborhoods that are roughly three miles apart. 15
A study by The Commonwealth Fund assessed 30 indicators of access, prevention, quality, potentially avoidable hospital use, and health outcomes. The study found that populations with low-income status suffer disparities in every state. However, it also identified significant differences among states’ performances. For top-performing states, many health care measures of populations with low income were better than average and better than those for individuals with higher income or more education in lagging states. These findings indicate that low-income status does not have to determine poor health or poor care experience. Interventions seen in top-performing states, such as expanded insurance coverage, access, and coordination of social and medical services, can help mitigate poverty’s effects on health. 16
Poverty and Health
SDoH are the conditions under which people are born, grow, live, work, and age, and include factors such as socioeconomic status, education, employment, social support networks, and neighborhood characteristics. 4 These social factors have a more significant collective impact on health and health outcomes than health behavior, health care, and the physical environment. 17,18 SDoH, especially poverty, structural racism, and discrimination, are the primary drivers of health inequities. 19,20
Economic prosperity can provide individuals access to resources to avoid or buffer exposure to health risks. 21 Research shows that individuals with higher incomes consistently experience better health outcomes than individuals with low incomes and those living in poverty. 22 Poverty affects health by limiting access to proper nutrition and healthy foods; shelter; safe neighborhoods to learn, live, and work; clean air and water; utilities; and other elements that define an individual’s standard of living. Individuals who live in low-income or high-poverty neighborhoods are likely to experience poor health due to a combination of these factors. 23,24
Violence is also more prevalent in areas with greater poverty. From 2008 to 2012, individuals in households at or below the poverty level experienced more than double the rate of violent victimization than individuals in high-income households. 25 This pattern of victimization by violent behavior was consistent for both Black and white individuals. It significantly impacts the victim’s family and perpetrator’s family (through incarceration).
Because they intersect with so many SDoH, poverty and low-income status dramatically affects life expectancy. 26 Education and its socioeconomic status correlate to income and wealth. These have powerful associations with life expectancy for both sexes and all races at all ages. Students from families with low income are five times more likely to drop out of high school than students from families with high income. 27 In 2008, the life expectancy among U.S. adult men and women with fewer than 12 years of education was not much better than the life expectancy among all adults in the 1950s and 1960s. 28
Poverty affects individuals insidiously in other ways that we are just beginning to understand. Mental illness, chronic health conditions, and substance use disorders are all more prevalent in populations with low income. 29 Poor nutrition, toxic exposures (e.g., lead), and elevated levels of the stress hormone cortisol are factors associated with poverty that may have lasting effects on children beginning before birth and continuing after birth. These effects, which can influence cognitive development and chronic disease development, are dose-dependent (i.e., the duration of exposure matters). 30,31,32 For example, the greater the number of years a child spends living in poverty, the more elevated the child’s overnight cortisol level and the more dysregulated the child’s cardiovascular response to acute stressors. 31 Impaired development of the nervous system affects cognitive and socioemotional development and increases the risk of behavioral challenges, adverse health behaviors, and poor school performance. 31,32 Recent studies have even identified a strong association between pediatric suicide and county-level poverty rates. 33
However, the effects of poverty are not predictably uniform. Longitudinal studies of health behavior describe positive (e.g., tobacco use cessation) and negative (e.g., decrease in physical activity) health behavior trends in populations with lower and higher socioeconomic status. However, there is a socioeconomic gradient in health improvement. In other words, populations with lower socioeconomic status lag behind populations with higher socioeconomic status in positive gains from health behavior trends. Health behaviors are important in that they account for differences in mortality. 34 The fact that positive changes in health behaviors are possible despite the challenges of poverty points to the importance of developing and implementing interventions that promote healthy behaviors in populations with low income.
Risk Regulators and Intervention
Poverty affects health in many different ways through complex mechanisms that we are just beginning to understand and describe. Living in poverty does not necessarily predetermine poor health. 35 Poverty will not “cause” a disease. Instead, poverty affects both the likelihood that an individual will have risk factors for disease and its ability and opportunity to prevent and manage disease. An individual’s health outcomes (a physiologic expression) ultimately will be influenced by genetic and environmental factors, as well as health behaviors – all of which may be affected by poverty. Material conditions, discriminatory practices, neighborhood conditions, behavioral norms, work conditions, as well as laws, policies, and regulations associated with poverty make it a “risk regulator.” 35 This means that poverty functions as a control parameter at a system level to influence the probability of exposure to key risk factors (e.g., behaviors, environmental risks) that lead to disease (Figure 1).
Figure 1: An Illustration of Risk Regulators in Social and Biological Context
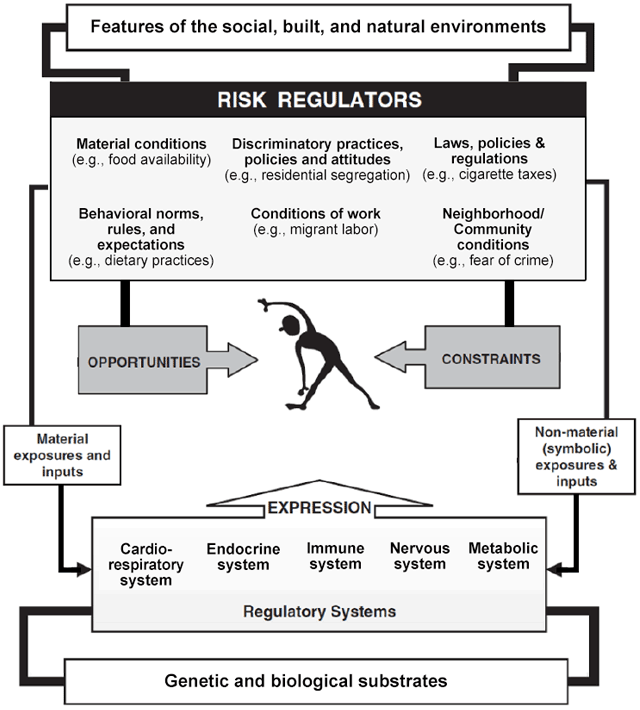
Reprinted with permission from Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Soc Sci Med. 2006;62(7):1650-1671.
Thinking of poverty as a risk regulator rather than a rigid determinant of health allows family physicians to relinquish the feeling of helplessness when providing medical care to families and individuals with low income.
Family physicians are uniquely positioned to devise solutions to mitigate the development of risk factors that lead to disease and the conditions unique to populations with low income that interfere with effective disease prevention and management. They can boost an individual or family’s “host resistance” to the health effects of poverty and tap into a growing array of aligned resources that provide patients and families with tangible solutions so that health maintenance can be a realistic goal.
Role of the Family Physician
Community-Oriented Primary Care (COPC)
Strong primary care teams are critical in the care of patients with low income. These populations often have higher rates of chronic disease and difficulty navigating health care systems. They benefit from care coordination and team-based care that addresses medical and socioeconomic needs.
In the United States, there is a move toward increased payment from government and commercial payers to offset the cost of providing coordinated and team-based care. Some payment models provide shared savings or care coordination payments in addition to traditional fee-for-service reimbursement. The practice transformations from COPC and payment models based on targets and meaningful use alter how we approach patient panels and communities. 36 The rationale behind alternative payment models – particularly regarding the care of lower socioeconomic populations – is that significant cost savings can be realized when care moves toward prevention and self-management and away from crisis-driven, fragmented care provided in the emergency department or a hospital setting. By recognizing and treating disease earlier – and actively partnering with local public health services like health educators, community health workers, and outreach services – family physicians can help prevent costly, avoidable complications and reduce the total cost of care.
Community Responsive Care
Care team members can positively affect the health of patients with low income by creating a welcoming, nonjudgmental environment that supports a long-standing therapeutic relationship built on trust. Familiarity with the National Standards for Culturally and Linguistically Appropriate Services (CLAS) in Health and Health Care can prepare practices and institutions to provide care in a manner that promotes health equity. 37
Patients with low income may be unintentionally shamed by the care team when their behaviors are seen as evidence of being “noncompliant” (e.g., missing appointments, not adhering to a medical regimen, not getting tests done). These patients may not be comfortable sharing information about the challenges that lead to their “noncompliant” behaviors. For example, a patient with low income may arrive 15 minutes late to an appointment because they have to rely on someone else for transportation. A patient may not take prescribed medication because it is too expensive. A patient may not get tests done because their employer will not allow time off from work. A patient may not understand printed care instructions because of low-literacy skills. Such patients may be turned away by staff because their tardiness disrupts the schedule, or they may even be dismissed from the practice altogether because of repeated noncompliance. Physicians and care team members should learn why the patient was noncompliant and promote an atmosphere of tolerance and adaptation.
Patients with low socioeconomic status and other marginalized populations rarely respond well to dictation from health care professionals. Instead, interventions that rely on peer-to-peer storytelling or coaching are more effective in overcoming cognitive resistance to positive health behavior changes. 38 Physicians and care team members can identify local groups that provide peer-to-peer support. Such activities are typically hosted by local hospitals, faith-based organizations, health departments, or senior centers.
Screen for Socioeconomic Challenges
Family physicians regularly screen for risk factors for disease. Screening to identify patients’ socioeconomic challenges and other SDoH can be incorporated into practices using EveryONE Project tools. Once socioeconomic challenges are identified, physicians and their care teams can work with patients to design achievable, sustainable treatment plans. The simple question, “Do you (ever) have difficulty making ends meet at the end of the month?” has a sensitivity of 98% and specificity of 60% in predicting poverty. 39 A casual inquiry about the cost of a patient’s medications is another way to start a conversation about socioeconomic obstacles to care.
A patient’s home and neighborhood affect health. 40 The care team should ask the patient whether their home is adequate to support healthy behaviors. For example, crowding, infestations, and lack of utilities are all risk factors for disease. Knowing that a patient is homeless or has poor, inadequate housing will help guide care.
Set Priorities and Make a Realistic Plan of Action
Family physicians direct the therapeutic process by working with the patient and care team to identify priorities so treatment goals are clear and achievable. In many cases, suspending a “fix everything right now” agenda in favor of a treatment plan of small steps that incorporate shared decision making can help this process. It is likely that a patient with low income will not have the resources (e.g., on-demand transportation, forgiving work schedule, available child care) to comply with an ideal treatment plan. Formulating a treatment plan that makes sense for the patient’s life circumstances is vital to success.
For example, for a patient with limited means and multiple chronic conditions – including hypertension and diabetes – start by addressing these conditions. Colon cancer screening or a discussion about beginning statin therapy can come later. It may be easier for this patient to adhere to an insulin regimen involving vials and syringes instead of insulin pens, which are much more expensive. The “best” medication for a patient with low income is the one that the patient can afford and self-administer reliably. Celebrate success with each small step that takes a patient closer to disease control and improved self-management.
Help Newly Insured Patients Navigate the Health Care System
In many states, the expansion of Medicaid has allowed individuals and families with low income to become insured – perhaps for the first time. A newly insured individual with low income will not necessarily know how or when to make, keep, or reschedule an appointment; develop a relationship with a family physician; manage medication refills; or obtain referrals. They may be embarrassed to reveal this lack of knowledge to the care team. Physicians and care team members can help by providing orientation to newly insured patients within the practice. For example, ensure that all patients know where to pick up medication, how to take it and why, when to return for a follow-up visit and why, and how to follow their treatment plan from one appointment to the next. Without this type of compassionate intervention, patients may revert to an old pattern of seeking crisis-driven care often provided by the emergency department or a local hospital.
Provide Material Support to Families with Low Income
Resources that make it easier for busy physicians to provide support to families with low income include the following:
● Reach Out and Read is a program that helps clinicians provide books for parents to take home to read to their children. Studies have shown that Reach Out and Read improve children’s language skills. 41
● 2-1-1 is a free, confidential service that patients or staff can access 24 hours a day by phone. 2-1-1 is staffed by community resource specialists who can connect patients to resources such as food, clothing, shelter, utility bill relief, social services, and even employment opportunities. Follow-up calls are made to ensure clients connect successfully with the resource referrals.
● The National Domestic Violence Hotline is staffed 24 hours a day by trained advocates who provide confidential help and information to patients who are experiencing domestic violence.
Local hospitals, health departments, and faith-based organizations often are connected to community health resources that offer services such as installing safety equipment in homes; providing food resources; facilitating behavioral health evaluation and treatment; and providing transportation, vaccinations, and other benefits to individuals and families with low income.
Practices can make a resource folder of information about local community services that can be easily accessed when taking care of patients in need. This simple measure incorporates community resources into the everyday workflow of patient care, thus empowering the care team.
Participate in Research that Produces Relevant Evidence
Much of the research about the effects of poverty on health is limited to identifying health disparities. This is insufficient. Research that evaluates specific interventions is needed to gain insight into what effectively alleviates poverty’s effects on health care delivery and outcomes. Family physicians can serve a critical role in this research because we have close relationships with patients with low income. 42
Advocate on Behalf of Neighborhoods and Communities with Low Income
Family physicians are community leaders, so we can advocate effectively for initiatives that improve the quality of life in neighborhoods with low income. Some forms of advocacy are apparent, such as promoting a state’s expansion of Medicaid. Other efforts may be specific to the community served. For example, a vacant lot can be converted to a basketball court or soccer field. A community center can expand programs that involve peer-to-peer health coaching. A walking program can be started among residents in a public housing unit. Collaboration with local law enforcement agencies can foster the community’s trust and avoid the potential for oppression. 43
Family physicians have local partners in advocacy, so we do not have to act in isolation. As a result of the Patient Protection and Affordable Care Act (ACA), nonprofit hospitals regularly report community needs assessments and work with local health departments to establish action plans that address identified needs. A Community Health Needs Assessment (CHNA) reflects a specific community’s perception of need, and each action plan outlines multi-sectoral solutions to meet local health needs. Local CHNAs are typically available online, as are the associated action plans. Family physicians can use information in the CHNA to access local health care leadership and join aligned forces in the communities we serve, thereby supporting the AAFP’s vision of achieving optimal health for everyone.
1. Sherin K, Adebanjo T, Jani A. Social determinants of health: family physicians’ leadership role. Am Fam Physician . 2019;99(8):476-477.
2. Commission on Social Determinants of Health. Closing the gap in a generation. Health equity through action on the social determinants of health. World Health Organization (WHO). Accessed March 22, 2021. www.who.int/social_determinants/final_report/csdh_finalreport_2008.pdf
3. Kovach KA, Reid K, Grandmont J, et al. How engaged are family physicians in addressing the social determinants of health? A survey supporting the American Academy of Family Physician’s health equity environmental scan. Health Equity . 2019;3(1):449-457.
4. American Academy of Family Physicians (AAFP). Advancing health equity by addressing the social determinants of health in family medicine (position paper). Accessed March 22, 2021.
5. World Vision. What is poverty? It’s not as simple as you think. Accessed March 22, 2021. www.worldvision.ca/stories/child-sponsorship/what-is-poverty#:~:text=1.-,What%20is%20the%20definition%20of%20poverty%3F,care%2C%20education%20and%20even%20transportation
6. Office of the Assistant Secretary for Planning and Evaluation. 2020 poverty guidelines. Accessed March 22, 2021. https://aspe.hhs.gov/2020-poverty-guidelines
7. United States Census Bureau. Income, poverty and health insurance coverage in the United States: 2019. Accessed March 22, 2021. www.census.gov/newsroom/press-releases/2020/income-poverty.html
8. United States Department of Agriculture. SNAP special rules for the elderly or disabled. Accessed March 22, 2021. www.fns.usda.gov/snap/eligibility/elderly-disabled-special-rules
9. U.S. Centers for Medicare & Medicaid Services. Federal poverty level (FPL). Accessed March 22, 2021. www.healthcare.gov/glossary/federal-poverty-level-fpl/
10. Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav . 1995;Spec No:80-94.
11. Brooks-Gunn J, Duncan GJ. The effects of poverty on children. Future Child . 1997;7(2):55-71.
12. Berkman LF, Kawachi I. A historical framework for social epidemiology. In: Berkman LF, Kawachi I, eds. Social Epidemiology . New York, NY: Oxford University Press; 2014.
13. Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav . 2010;51 Suppl:S28-S40.
14. Macintyre S, Ellaway A, Cummins S. Place effects on health: how can we conceptualise, operationalise and measure them? Soc Sci Med . 2002;55(1):125-139.
15. Robert Wood Johnson Foundation. Mapping life expectancy. Short distances to large gaps in health. Accessed March 22, 2021. www.rwjf.org/en/library/articles-and-news/2015/09/city-maps.html
16. Schoen C, Radley D, Riley P, et al. Health care in the two Americas. Findings from the Scorecard on State Health System Performance for Low-Income Populations, 2013. Accessed March 22, 2021. www.commonwealthfund.org/sites/default/files/documents/___media_files_publications_fund_report_2013_sep_1700_schoen_low_income_scorecard_full_report_final_v4.pdf
17. Booske BC, Athens JK, Kindig DA, Park H, Remington PL. County health rankings working paper. Different perspectives for assigning weights to determinants of health. University of Wisconsin Population Health Institute. Accessed March 22, 2021. www.countyhealthrankings.org/sites/default/files/differentPerspectivesForAssigningWeightsToDeterminantsOfHealth.pdf
18. County Health Rankings & Roadmaps. County Health Rankings model. Accessed March 22, 2021. www.countyhealthrankings.org/explore-health-rankings/measures-data-sources/county-health-rankings-model
19. Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav . 2010;51 Suppl:S28-S40.
20. National Academies of Sciences, Engineering, and Medicine. Communities in action. Pathways to health equity. Accessed March 22, 2021. www.nap.edu/catalog/24624/communities-in-action-pathways-to-health-equity
21. Anderson LM, Scrimshaw SC, Fullilove MT, Fielding JE, Task Force on Community Preventive Services. The Community Guide’s model for linking the social environment to health. Am J Prev Med . 2003;24(3 Suppl):12-20.
22. Berkman LF, Kawachi I, eds. Social Epidemiology . New York, NY: Oxford University Press; 2000.
23. Riste L, Khan F, Cruickshank K. High prevalence of type 2 diabetes in all ethnic groups, including Europeans, in a British inner city: relative poverty, history, inactivity, or 21st century Europe? Diabetes Care . 2001;24(8):1377-1383.
24. Healthy People 2030. Social determinants of health. Accessed March 22, 2021. https://health.gov/healthypeople/objectives-and-data/social-determinants-health
25. Bureau of Justice Statistics. Household poverty and nonfatal violent victimization, 2008-2012. Accessed March 24, 2021. www.bjs.gov/index.cfm?ty=pbdetail&iid=5137
26. Chetty R, Stepner M, Abraham S, et al. The association between income and life expectancy in the United States, 2001–2014. JAMA . 2016;315(16):1750-1766.
27. National Center for Education Statistics. Trends in high school dropout and completion rates in the United States: 1972–2009. Accessed March 24, 2021. https://nces.ed.gov/pubs2012/2012006.pdf
28. Olshansky SJ, Antonucci T, Berkman L, et al. Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Aff (Millwood). 2012;31(8):1803-1813.
29. Walker ER, Druss BG. Cumulative burden of comorbid mental disorders, substance use disorders, chronic medical conditions, and poverty on health among adults in the United States. Psychol Health Med . 2017;22(6):727-735.
30. Evans GW, Kim P. Childhood poverty and health: cumulative risk exposure and stress dysregulation. Psychol Sci . 2007;18(11):953-957.
31. Lipina SJ, Colombo JA. Poverty and Brain Development During Childhood: An Approach from Cognitive Psychology and Neuroscience . Human Brain Development Series. Washington, DC: American Psychological Association; 2009.
32. Farah MJ, Noble KG, Hurt H. Poverty, privilege, and brain development: empirical findings and ethical implications. In: Illes J, ed. Neuroethics: Defining the Issues in Theory, Practice, and Policy . New York: Oxford University Press; 2005.
33. Hoffmann JA, Farrell CA, Monuteaux MC, et al. Association of pediatric suicide with county-level poverty in the United States, 2007-2016. JAMA Pediatr . 2020;174(3):287-294.
34. Stringhini S, Sabia S, Shipley M, et al. Association of socioeconomic position with health behaviors and mortality. JAMA . 2010;303(12):1159-1166.
35. Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Soc Sci Med . 2006;62(7):1650-1671.
36. American Academy of Family Physicians. Integration of primary care and public health (position paper). Accessed March 24, 2021. www.aafp.org/about/policies/all/integration-primary-care.html
37. U.S. Department of Health and Human Services. National CLAS Standards. Accessed March 24, 2021. https://thinkculturalhealth.hhs.gov/clas
38. Houston TK, Allison JJ, Sussman M, et al. Culturally appropriate storytelling to improve blood pressure: a randomized trial. Ann Intern Med . 2011;154(2):77-84.
39. Brcic V, Eberdt C, Kaczorowski J. Development of a tool to identify poverty in a family practice setting: a pilot study. Int J Family Med . 2011;2011:812182.
40. Braveman P, Dekker M, Egerter S, Sadegh-Nobari T, Pollack C. Housing and health. Robert Wood Johnson Foundation. Accessed March 24, 2021. www.dhss.delaware.gov/dhss/dph/mh/files/housingandhealth.pdf
41. Zuckerman B. Promoting early literacy in pediatric practice: twenty years of Reach Out and Read. Pediatrics. 2009;124(6):1660-1665.
42. O’Campo P, Dunn JR, eds. Rethinking Social Epidemiology: Towards a Science of Change . New York, NY: Springer; 2012.
43. President's Task Force on 21st Century Policing. Interim report of the President's Task Force on 21st Century Policing. Office of Community-Oriented Policing Services. Accessed March 21, 2021. https://cdpsdocs.state.co.us/ccjj/meetings/2015/2015-03-13_CCJJ_Presidents-21CentCommPolicingTF-InterimReport.pdf
(2015 COD) (January 2022 COD)
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Three Essays on the Causes and Consequences of Poor Health and Nutrition in the Developing World
Stress and Its Effects on Health Essay
Introduction, physical effects, psychological effects, behavioral effects.
Stress is the emotional strain or tension experienced by an individual due to a reaction toward various demanding and influential situations. The challenging or compelling situations are termed stressors. Stressors can be internal or external and include life changes such as losing a significant figure, low socioeconomic status, relationship problems, occupational challenges, and familial or environmental factors. An individual’s response to stressors influences the outcome of their life. Health is a state of complete social, emotional, and physical well-being and not merely the absence of disease. Stress is a common risk factor for negative health status secondary to negative adaptation and coping with the stressors. Stressors can create a strain on one’s physical, psychological and behavioral well-being, leading to lasting effects that are detrimental to one’s health.
Stress is associated with various physical health impacts on an individual. In an online cross-sectional survey by Keech et al. (2020) to determine the association between stress and the physical and psychological health of police officers, the findings illustrate that stress negatively impacts physical and psychological well-being. One hundred and thirty-four police officers were involved in the study (Keech et al., 2020). The findings demonstrate that stress resulted in various short and long-term physical effects that included increased heart rates, sweating, high blood pressure, and long-term development of the cardiac condition. In addition, stress resulted in the development of gastrointestinal disorders such as peptic ulcer and irritable bowel syndrome. Keech et al. (2020) note that stress’s associated physical health effects are explained by various mechanisms that include overstimulation of the sympathetic nervous system and the hypothalamic-pituitary-adrenocortical axis.
Overstimulation of the sympathetic nervous system results in increased sympathetic actions on the peripheral body organs leading to increased sweat production, heart rate, respiration rate, and urinary and bowel elimination. The study notes that chronic stress without positive adaptation measures results in the progressive development of hypertension, peptic ulcers, and irritable bowel syndrome as long-term effects (Keech et al., 2020). Within the gastrointestinal tract, chronic stress activity on the sympathetic nervous system results in increased parietal cell action. Overactivity of the parietal cells results in excessive gastric acid production, gradually eroding the mucosa, and ulceration occurs.
The effects of stress on the cardiovascular system are explained in a review by Kivimäki & Steptoe (2017) to determine the impact of stress on the development and progression of cardiovascular diseases. In the review, stress is identified to cause cardiovascular conditions secondary to the effects of sustained sympathetic action on heart contractility and peripheral vascular resistance (Kivimäki & Steptoe, 2017). The sympathetic nervous system contributes to normal heart and blood vessel contractility. However, when the system is overstimulated, a surge in contractility above the normal limits ensues, leading to the progressive development of heart conditions.
Psychological well-being incorporates a positive mental health status evidenced by an individual’s satisfaction with life, happiness, rational thinking and decision-making, and positive mood patterns. Stress has been associated with alterations in an individual’s psychological wellness. An explanation for alteration in an individual’s psychological well-being secondary to stress is negative adaptation. Keech et al. (2020) note that an individual’s response to a stressor determines whether stress results in positive or negative effects. In the online cross-sectional survey by Keech et al. (2020), the findings illustrate that pressure resulted in the development of anxiety, depression, and bipolar disorders as long-term effects among the participants. Exposure to stressful situations resulted in progressively developing anxiety among the individual secondary to persistent worry over the issue. The anxiety results in other physical manifestations, including increased heart rate, palpitations, sweating, and altered mobility. Depression and bipolar conditions were also associated with chronic stress secondary to the impacts of stress on neurotransmitter function and nerves.
Similar findings are noted in a cross-sectional study by Zhang et al. (2020) to compare the prevalence and severity of stress-associated mental health symptoms, including anxiety, depression, and insomnia among healthcare workers during the COVID pandemic. Five hundred and twenty-four healthcare workers were involved in the study. The study findings illustrate that 31.3% of the participants developed depression secondary to the stressful working environment, 41.2% reported anxiety, and 39.3% reported sleep disturbances (Zhang et al., 2020). The scientific explanation for the relationship between stress and depression was attributed to the effects of stressful periods on neurotransmitter homeostasis. Chronic stress results in the altered regulation of neurotransmitters in the central nervous system. Alterations in serotonin, norepinephrine, and dopamine resulted in the progressive development of depression and anxiety. Sleep disturbances reported by the participants are attributed to alterations in cortisol hormone homeostasis secondary to overstimulation of the hypothalamic-pituitary-adrenocortical axis.
Stressful situations can also lead to alterations in the behavioral patterns of an individual. The most common behavioral effects secondary to stress include the development of eating disorders, altered sleeping patterns, impaired concentration, and drug abuse especially alcohol. Alterations in sleep and eating patterns are linked to stress’s effects on the hypothalamic-pituitary-adrenocortical axis (HPA). Exposure to stressful events leads to increased activation of the HPA axis with a net effect of increased catecholamine production (adrenaline and noradrenaline) (Moustafa et al., 2018). Increased adrenaline and noradrenaline production results in dysregulation in the eating and sleeping patterns. Sustained high levels of cortisol results in difficulty falling asleep and increased metabolic processes. The biological clock regulates the typical sleeping pattern that relies on producing the sleep hormone melatonin. Melatonin production by the pineal gland is regulated indirectly by the concentration of serum cortisol levels and directly by light perception. Imbalances in the serum concentration cycle secondary to stress results in imbalanced melatonin production and concentration with a net effect of sleeping difficulties.
The emotional strain caused by stress increases the risk of alcohol and other illicit drug use and dependence. Moustafa et al. (2018) conducted an integrative literature review to determine the relationship between childhood trauma, early-life stress, alcohol and drug use, addiction, and abuse. The review findings illustrate that stress increases the risk of alcohol and drug use, addiction, and abuse among the victims. An explanation for the increased risk is the individuals’ lack of identification and implementation of effective coping strategies (Moustafa et al., 2018). Lack of effective coping strategies results in maladaptive measures such as illicit drug use and alcohol consumption. Extensive use of the maladaptive measures results in progressive addiction and drug abuse among individuals with an increased predisposition to other health effects. Alcohol consumption and other illicit drug use over time increase the risk of developing cardiac, respiratory, and liver conditions.
Stress is the emotional strain or tension experienced by an individual due to a reaction toward various demanding and influential situations. Individual response to stressors influences their health. Maladaptive response to stress results in various physical, psychological, and behavioral negative effects. Negative effects of stress on physical health include increased heart rates, sweating, high blood pressure, and long-term development of the cardiac condition. Psychological effects include the development of anxiety, depression, and bipolar disorders. The behavioral effects of stress on an individual include the development of eating disorders, altered sleeping patterns, impaired concentration, and abuse of alcohol and other drugs. Based on the research findings, it is essential for healthcare providers to identify strategic measures and health initiatives to educate and sensitize the community members on effective stress management approaches in all settings to aid in combating the health effects.
Keech, J. J., Cole, K. L., Hagger, M. S., & Hamilton, K. (2020). The association between stress mindset and physical and psychological well being: Testing a stress beliefs model in police officers . Psychology & Health , 35 (11), 1306-1325. Web.
Kivimäki, M., & Steptoe, A. (2017). Effects of stress on the development and progression of cardiovascular disease . Nature Reviews Cardiology , 15 (4), 215–229. Web.
Moustafa, A. A., Parkes, D., Fitzgerald, L., Underhill, D., Garami, J., Levy-Gigi, E., Stramecki, F., Valikhani, A., Frydecka, D., & Misiak, B. (2018). The relationship between childhood trauma, early-life stress, and alcohol and drug use, abuse, and addiction: An integrative review . Current Psychology , 40 (2), 579–584. Web.
Zhang, X., Zhao, K., Zhang, G., Feng, R., Chen, J., Xu, D., Liu, X., Ngoubene-Italy, A. J., Huang, H., Liu, Y., Chen, L., & Wang, W. (2020). Occupational Stress and Mental Health: A comparison between frontline medical staff and non-frontline medical staff during the 2019 novel Coronavirus Disease outbreak . Frontiers in Psychiatry , 11 . Web.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2023, December 19). Stress and Its Effects on Health. https://ivypanda.com/essays/stress-and-its-effects-on-health/
"Stress and Its Effects on Health." IvyPanda , 19 Dec. 2023, ivypanda.com/essays/stress-and-its-effects-on-health/.
IvyPanda . (2023) 'Stress and Its Effects on Health'. 19 December.
IvyPanda . 2023. "Stress and Its Effects on Health." December 19, 2023. https://ivypanda.com/essays/stress-and-its-effects-on-health/.
1. IvyPanda . "Stress and Its Effects on Health." December 19, 2023. https://ivypanda.com/essays/stress-and-its-effects-on-health/.
Bibliography
IvyPanda . "Stress and Its Effects on Health." December 19, 2023. https://ivypanda.com/essays/stress-and-its-effects-on-health/.
- History and Concept of the Psychoneuroimmunology
- Insomnia: Cause and Effect
- Genes, Neurotransmitters, and Emotions
- Post-Traumatic Stress Disorder and Its Theories
- Effect of Stress Hormones on Brain Cells
- Pathophysiology of Stress, Processed Foods, and Risky Alcohol Consumption
- Coronary Heart Disease Caused by Stress
- Mood and Stress Psychology: Causes, Effects and Treatments
- Adrenocorticotropic Hormone Regulation
- Jessie as the Most Sympathetic Character of “Night, Mother” by Marsha Norman
- Intergenerational Trauma and Traumatic Memory
- The Lifespan Theory Applied to a Grieving Case
- Psychological Conditions in Addition to Highly Superior Autobiographical Memory
- Self-Control: Individual Development Plan
- Arachnophobia: Systematic Desensitization Project
- Essay Editor
Mental Health Essay
Revolutionize your writing process: our AI rewrite tool is here to help
Introduction
Mental health, often overshadowed by its physical counterpart, is an intricate and essential aspect of human existence. It envelops our emotions, psychological state, and social well-being, shaping our thoughts, behaviors, and interactions. With the complexities of modern life—constant connectivity, societal pressures, personal expectations, and the frenzied pace of technological advancements—mental well-being has become increasingly paramount. Historically, conversations around this topic have been hushed, shrouded in stigma and misunderstanding. However, as the curtains of misconception slowly lift, we find ourselves in an era where discussions about mental health are not only welcomed but are also seen as vital. Recognizing and addressing the nuances of our mental state is not merely about managing disorders; it's about understanding the essence of who we are, how we process the world around us, and how we navigate the myriad challenges thrown our way. This essay aims to delve deep into the realm of mental health, shedding light on its importance, the potential consequences of neglect, and the spectrum of mental disorders that many face in silence.
Importance of Mental Health
Mental health plays a pivotal role in determining how individuals think, feel, and act. It influences our decision-making processes, stress management techniques, interpersonal relationships, and even our physical health. A well-tuned mental state boosts productivity, creativity, and the intrinsic sense of self-worth, laying the groundwork for a fulfilling life.
Negative Impact of Mental Health
Neglecting mental health, on the other hand, can lead to severe consequences. Reduced productivity, strained relationships, substance abuse, physical health issues like heart diseases, and even reduced life expectancy are just some of the repercussions of poor mental health. It not only affects the individual in question but also has a ripple effect on their community, workplace, and family.
Mental Disorders: Types and Prevalence
Mental disorders are varied and can range from anxiety and mood disorders like depression and bipolar disorder to more severe conditions such as schizophrenia.
- Depression: Characterized by persistent sadness, lack of interest in activities, and fatigue.
- Anxiety Disorders: Encompass conditions like generalized anxiety disorder, panic attacks, and specific phobias.
- Schizophrenia: A complex disorder affecting a person's ability to think, feel, and behave clearly.
The prevalence of these disorders has been on the rise, underscoring the need for comprehensive mental health initiatives and awareness campaigns.
Understanding Mental Health and Its Importance
Mental health is not merely the absence of disorders but encompasses emotional, psychological, and social well-being. Recognizing the signs of deteriorating mental health, like prolonged sadness, extreme mood fluctuations, or social withdrawal, is crucial. Understanding stems from awareness and education. Societal stigmas surrounding mental health have often deterred individuals from seeking help. Breaking these barriers, fostering open conversations, and ensuring access to mental health care are imperative steps.
Conclusion: Mental Health
Mental health, undeniably, is as significant as physical health, if not more. In an era where the stressors are myriad, from societal pressures to personal challenges, mental resilience and well-being are essential. Investing time and resources into mental health initiatives, and more importantly, nurturing a society that understands, respects, and prioritizes mental health is the need of the hour.
- World Leaders: Several influential personalities, from celebrities to sports stars, have openly discussed their mental health challenges, shedding light on the universality of these issues and the importance of addressing them.
- Workplaces: Progressive organizations are now incorporating mental health programs, recognizing the tangible benefits of a mentally healthy workforce, from increased productivity to enhanced creativity.
- Educational Institutions: Schools and colleges, witnessing the effects of stress and other mental health issues on students, are increasingly integrating counseling services and mental health education in their curriculum.
In weaving through the intricate tapestry of mental health, it becomes evident that it's an area that requires collective attention, understanding, and action.
Short Essay about Mental Health
Mental health, an integral facet of human well-being, shapes our emotions, decisions, and daily interactions. Just as one would care for a sprained ankle or a fever, our minds too require attention and nurture. In today's bustling world, mental well-being is often put on the back burner, overshadowed by the immediate demands of life. Yet, its impact is pervasive, influencing our productivity, relationships, and overall quality of life.
Sadly, mental health issues have long been stigmatized, seen as a sign of weakness or dismissed as mere mood swings. However, they are as real and significant as any physical ailment. From anxiety to depression, these disorders have touched countless lives, often in silence due to societal taboos.
But change is on the horizon. As awareness grows, conversations are shifting from hushed whispers to open discussions, fostering understanding and support. Institutions, workplaces, and communities are increasingly acknowledging the importance of mental health, implementing programs, and offering resources.
In conclusion, mental health is not a peripheral concern but a central one, crucial to our holistic well-being. It's high time we prioritize it, eliminating stigma and fostering an environment where everyone feels supported in their mental health journey.
Frequently Asked Questions
- What is the primary focus of a mental health essay?
Answer: The primary focus of a mental health essay is to delve into the intricacies of mental well-being, its significance in our daily lives, the various challenges people face, and the broader societal implications. It aims to shed light on both the psychological and emotional aspects of mental health, often emphasizing the importance of understanding, empathy, and proactive care.
- How can writing an essay on mental health help raise awareness about its importance?
Answer: Writing an essay on mental health can effectively articulate the nuances and complexities of the topic, making it more accessible to a wider audience. By presenting facts, personal anecdotes, and research, the essay can demystify misconceptions, highlight the prevalence of mental health issues, and underscore the need for destigmatizing discussions around it. An impactful essay can ignite conversations, inspire action, and contribute to a more informed and empathetic society.
- What are some common topics covered in a mental health essay?
Answer: Common topics in a mental health essay might include the definition and importance of mental health, the connection between mental and physical well-being, various mental disorders and their symptoms, societal stigmas and misconceptions, the impact of modern life on mental health, and the significance of therapy and counseling. It may also delve into personal experiences, case studies, and the broader societal implications of neglecting mental health.

Recent articles
Essay - what it is and how to write it with an ai aithor.
Writing concise and persuasive texts is a skill required in many professional settings. One of the ways we learn this skill is by writing essays. However, essays require lots of preparation and research, so they can be hard to write, especially if you struggle to understand how to make your essay better. In this article, you’ll learn what an essay is and how to use the Aithor AI essay generator for writing essays. What is an essay? In a broad sense, an essay is a genre of writing that allows ...
Artificial Intelligence: Evolution of Essay Writing
We live in the age when each new year brings more innovations than the previous one. One of the most debated topics of recent time is AI writing software. Not only did users get a handy helper for composing emails, but a tireless machine for writing pages of text on a variety of topics. It’s only natural that students who often have to write long essays as homework started using it too. This article will dissect how artificial intelligence will change the future essays and if AI generation tool ...
Join the writing revolution: subscribe to our AI article generator tool
Poor Nutrition

Measure Breastfeeding Practices and Eating Patterns
Support breastfeeding in the hospital and community, offer healthier food options in early care and education facilities and schools, offer healthier food options in the workplace, improve access to healthy foods in states and communities, support lifestyle change programs to reduce obesity and type 2 diabetes risk.
Good nutrition is essential to keeping current and future generations healthy across the lifespan. A healthy diet helps children grow and develop properly and reduces their risk of chronic diseases. Adults who eat a healthy diet live longer and have a lower risk of obesity, heart disease, type 2 diabetes, and certain cancers. Healthy eating can help people with chronic diseases manage these conditions and avoid complications.
However, when healthy options are not available, people may settle for foods that are higher in calories and lower in nutritional value. People in low-income communities and some racial and ethnic groups often lack access to convenient places that offer affordable, healthier foods.
Most people in the United States don’t eat a healthy diet and consume too much sodium, saturated fat, and sugar, increasing their risk of chronic diseases. For example, fewer than 1 in 10 adolescents and adults eat enough fruits or vegetables. In addition, 6 in 10 young people aged 2 to 19 years and 5 in 10 adults consume at least one sugary drink on any given day.
CDC supports breastfeeding and works to improve access to healthier food and drink choices in settings such as early care and education facilities, schools, worksites, and communities.
In the United States:

3 IN 4 INFANTS
are not exclusively breastfed for 6 months.

9 IN 10 AMERICANS
consume too much sodium.

1 in 6 PREGNANT WOMEN
have iron levels that are too low.

NEARLY $173 BILLION
a year is spent on health care for obesity.
The Harmful Effects of Poor Nutrition
Overweight and obesity.
Eating a healthy diet, along with getting enough physical activity and sleep, can help children grow up healthy and prevent overweight and obesity. In the United States, 20% of young people aged 2 to 19 years and 42% of adults have obesity, which can put them at risk of heart disease, type 2 diabetes, and some cancers.
Heart Disease and Stroke

Two of the leading causes of heart disease and stroke are high blood pressure and high blood cholesterol. Consuming too much sodium can increase blood pressure and the risk for heart disease and stroke . Current guidelines recommend getting less than 2,300 mg a day, but Americans consume more than 3,400 mg a day on average.
Over 70% of the sodium that Americans eat comes from packaged, processed, store-bought, and restaurant foods. Eating foods low in saturated fats and high in fiber and increasing access to low-sodium foods, along with regular physical activity, can help prevent high blood cholesterol and high blood pressure.
Type 2 Diabetes
People who are overweight or have obesity are at increased risk of type 2 diabetes compared to those at a healthybecause, over time, their bodies become less able to use the insulin they make. Of US adults, 96 million—more than 1 in 3—have prediabetes , and more than 8 in 10 of them don’t know they have it. Although the rate of new cases has decreased in recent years, the number of adults with diagnosed diabetes has nearly doubled in the last 2 decades as the US population has increased, aged, and become more overweight.
An unhealthy diet can increase the risk of some cancers. Consuming unhealthy food and beverages, such as sugar-sweetened beverages and highly processed food, can lead to weight gain, obesity and other chronic conditions that put people at higher risk of at least 13 types of cancer, including endometrial (uterine) cancer, breast cancer in postmenopausal women, and colorectal cancer. The risk of colorectal cancer is also associated with eating red and processed meat.
CDC’s Work to Promote Good Nutrition
CDC’s Division of Nutrition, Physical Activity, and Obesity uses national and state surveys to track breastfeeding rates and eating patterns across the country, including fruit, vegetable, and added sugar consumption. The division also reports data on nutrition policies and practices for each state. Data from these surveys are used to understand trends in nutrition and differences between population groups.
CDC partners use this information to help support breastfeeding and encourage healthy eating where people live, learn, work, and play, especially for populations at highest risk of chronic disease.

Breastfeeding is the best source of nutrition for most infants. It can reduce the risk of some short-term health conditions for infants and long-term health conditions for infants and mothers. Maternity care practices in the first hours and days after birth can influence whether and how long infants are breastfed.
CDC funds programs that help hospitals use maternity care practices that support breastfeeding . These programs have helped increase the percentage of infants born in hospitals that implement recommended practices 1. CDC also works with partners to support programs designed to improve continuity of care and community support for breastfeeding mothers.

Nearly 56 million US children spend time in early care and education (ECE) facilities or public schools. These settings can directly influence what children eat and drink and how active they are—and build a foundation for healthy habits.
CDC is helping our nation’s children grow up healthy and strong by:
- Creating resources to help partners improve obesity prevention programs and use nutrition standards.
- Investing in training and learning networks that help child care providers and state and local child care leaders meet standards and use and share best practices .
- Providing technical assistance, such as training school staff how to buy, prepare, and serve fruits and vegetables or teach children how to grow and prepare fruits and vegetables.
The CDC Healthy Schools program works with states, school systems, communities, and national partners to promote good nutrition . These efforts include publishing guidelines and tips on how schools and parents can model healthy behaviors and offer healthier school meals, smart snacks , and water access.
CDC also works with national groups to increase the number of salad bars in schools. As of 2021, the Salad Bars to School program has delivered almost 6,000 salad bars to schools across the nation, giving over 2.9 million children and school staff better access to fruits and vegetables.
Millions of US adults buy foods and drinks while at work. CDC develops and promotes food service guidelines that encourage employers and vendors to increase healthy food options for employees. CDC-funded programs are working to make healthy foods and drinks (including water) more available in cafeterias, snack shops, and vending machines. CDC also partners with states to help employers comply with the federal lactation accommodation law and provide breastfeeding mothers with places to pump and store breast milk, flexible work hours, and maternity leave benefits.

People living in low-income urban neighborhoods, rural areas, and tribal communities often have little access to affordable, healthy foods such as fruits and vegetables. CDC’s State Physical Activity and Nutrition Program , High Obesity Program , and Racial and Ethnic Approaches to Community Health program fund states and communities to improve food systems in these areas through food hubs, local stores, farmers’ markets, and bodegas.
These programs, which also involve food vendors and distributors, help increase the variety and number of healthier foods and drinks available and help promote and market these items to customers.
CDC’s National Diabetes Prevention Program (National DPP) is a partnership of public and private organizations working to build a nationwide delivery system for a lifestyle change program proven to prevent or delay type 2 diabetes in adults with prediabetes. Participants in the National DPP lifestyle change program learn to make healthy food choices, be more physically active, and find ways to cope with stress. These changes can cut their risk of developing type 2 diabetes by as much as 58% (71% for those over 60).
Social_govd
Get Email Updates
To receive email updates about this page, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- NEWS FEATURE
- 03 April 2024
Why loneliness is bad for your health
- Saima May Sidik 0
Saima May Sidik is a freelance science journalist based in Somerville, Massachusetts.
You can also search for this author in PubMed Google Scholar
Some data challenge the popular notion that older people experience the highest rates of loneliness. Credit: Richard Baker/In Pictures Ltd/Corbis via Getty
You have full access to this article via your institution.
In 2010, Theresa Chaklos was diagnosed with chronic lymphocytic leukaemia — the first in a series of ailments that she has had to deal with since. She’d always been an independent person, living alone and supporting herself as a family-law facilitator in the Washington DC court system. But after illness hit, her independence turned into loneliness .
Loneliness, in turn, exacerbated Chaklos’s physical condition. “I dropped 15 pounds in less than a week because I wasn’t eating,” she says. “I was so miserable, I just would not get up.” Fortunately a co-worker convinced her to ask her friends to help out, and her mood began to lift. “It’s a great feeling” to know that other people are willing to show up, she says.
Many people can’t break out of a bout of loneliness so easily. And when acute loneliness becomes chronic, the health effects can be far-reaching. Chronic loneliness can be as detrimental as obesity, physical inactivity and smoking according to a report by Vivek Murthy , the US surgeon general. Depression, dementia, cardiovascular disease 1 and even early death 2 have all been linked to the condition. Worldwide, around one-quarter of adults feel very or fairly lonely, according to a 2023 poll conducted by the social-media firm Meta, the polling company Gallup and a group of academic advisers (see go.nature.com/48xhu3p ). That same year, the World Health Organization launched a campaign to address loneliness, which it called a “pressing health threat” .
But why does feeling alone lead to poor health? Over the past few years, scientists have begun to reveal the neural mechanisms that cause the human body to unravel when social needs go unmet. The field “seems to be expanding quite significantly”, says cognitive neuroscientist Nathan Spreng at McGill University in Montreal, Canada. And although the picture is far from complete, early results suggest that loneliness might alter many aspects of the brain, from its volume to the connections between neurons.
Subjective and contagious
Loneliness is a slippery concept. It’s not the same as social isolation, which occurs when someone has few meaningful social relationships, although “they’re two sides of the same coin”, says old-age psychiatrist Andrew Sommerlad at University College London. Rather, loneliness is a person’s subjective experience of being unsatisfied with their social relationships.
The list of health conditions linked to loneliness is long and sobering 1 (see ‘Loneliness and health’). Some of these make intuitive sense — people who feel lonely are often depressed, for example, sometimes to the point of being at risk of suicide. Other links are more surprising. Lonely people are at greater risk of high blood pressure and immune-system dysfunction compared with those who do not feel lonely, for example. There’s also a startling connection between loneliness and dementia, with one study reporting that people who feel lonely are 1.64 times more likely to develop this type of neurodegeneration than are those who do not 3 .
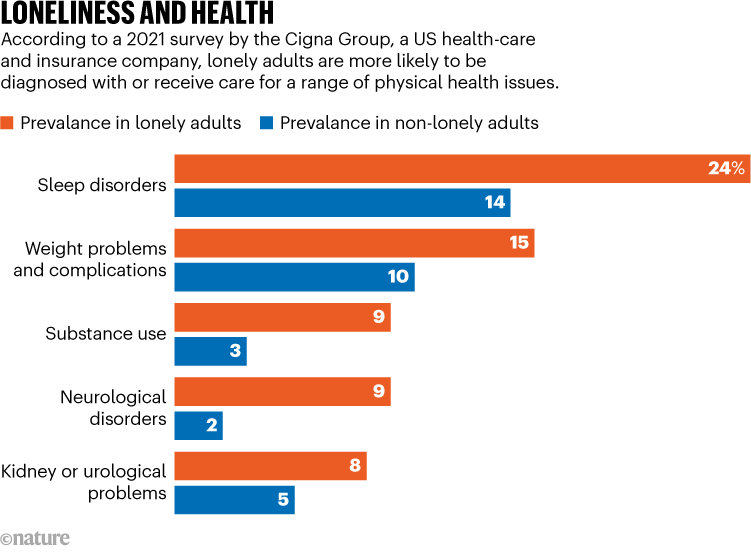
Source: The Cigna Group
A number of physiological effects, including the ability to sleep, increased stress-hormone levels and increased susceptibility to infections, could link loneliness with health problems. But the way in which these factors interact with one another makes it difficult to disentangle the effects of loneliness from the causes, cautions cognitive neuroscientist Livia Tomova at Cardiff University, UK. Do people’s brains start functioning differently when they become lonely, or do some people have differences in their brains that make them prone to loneliness? “We don’t really know which one is true,” she says.
Whatever the cause, loneliness seems to have the biggest effect on people who are in disadvantaged groups. In the United States, Black and Hispanic adults, as well as people who earn less than US$50,000 per year, have higher rates of loneliness than do other demographic groups by at least 10 percentage points, according to a 2021 survey by the Cigna Group, a US health-care and insurance company (see go.nature.com/43eakds ). That’s not surprising because “loneliness, by definition, is an emotional distress that wants us to adapt our social situations”, says geriatrician and palliative-care physician Ashwin Kotwal at the University of California, San Francisco. Without financial resources, adapting is harder.
The COVID-19 pandemic might have exacerbated loneliness by forcing people to isolate for months or years, although “that data is still emerging”, Kotwal says. Older adults have long been thought of as the demographic most heavily affected by loneliness, and indeed it is a major problem faced by many of the older people that Kotwal works with. But the Cigna Group’s data suggest that loneliness is actually highest in young adults — 79% of those between the ages of 18 and 24 reported feeling lonely, compared with 41% of people aged 66 and older.
Loneliness eats at you
A growing amount of research is exploring what happens in the brain when people feel lonely. Lonely people tend to view the world differently from those who aren’t, says cognitive neuroscientist Laetitia Mwilambwe-Tshilobo at Princeton University in New Jersey. In a 2023 study, researchers asked participants to watch videos of people in a variety of situations — for example, playing sports or on a date — while inside an magnetic resonance imaging scanner 4 . People who did not report being lonely all had similar neural responses to each other, whereas the responses in people who felt lonely were all different — from the other group and from each other. The authors hypothesized that lonely people pay attention to different aspects of situations from non-lonely people, which causes those who feel lonely to perceive themselves as being different from their peers.
Feeling lonely in research? You’re not alone
This would mean that loneliness can feed back on itself, becoming worse over time. “It’s almost like a self-fulfilling prophecy,” Mwilambwe-Tshilobo says. “If you think that you’re lonely, you’re perceiving or interpreting your social world more negatively. And that makes you move further and further away.” Some studies have shown that this effect can spread through social networks, giving loneliness a contagious quality 5 .
Historically, staying close to others was probably a good survival strategy for humans. That’s why scientists think that temporary loneliness evolved — to motivate people to seek company, just as hunger and thirst evolved to motivate people to seek food and water.
In fact, the similarities between hunger and loneliness go right down to the physiological level. In a 2020 study, researchers deprived people of either food or social connections for ten hours. They then used brain imaging to identify areas that were activated by images of either food — such as a heaping plate of pasta — or social interactions, such as friends laughing together. Some of the activated regions were unique to images either of food or of people socializing, but a region in the midbrain known as the substantia nigra lit up when hungry people saw pictures of food and when people who felt lonely saw pictures of social interactions 6 . That’s “a key region for motivation — it’s known to be active whenever we want something”, says Tomova, who is an author on the study.
More links are emerging between loneliness and how the brain processes feelings of reward. In mice, loneliness sensitizes certain midbrain neurons to a neurotransmitter called dopamine 7 , which can also cause people to cave in to cravings, such as for food and drugs. Likewise, isolation might make humans more sensitive to rewards and more eager to seek them out. In 2023, Tomova and her colleagues published a preprint 8 for a study in which they isolated adolescents from social contact for up to four hours. After isolation, participants were offered the chance to earn a monetary reward. The isolated participants agreed more quickly than did those who were not isolated, suggesting that isolation had made them more responsive to rewarding actions.
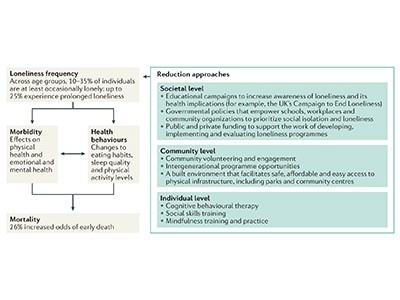
Loneliness and health
Although research on dopamine and loneliness is still emerging, scientists have also long recognized the connection between loneliness and another type of chemical signal — stress hormones called glucocorticoids. Humans need some level of glucocorticoids “to function; to wake up”, says neurophysiologist John-Ioannis Sotiropoulos at the National Centre for Scientific Research ‘Demokritos’ in Athens. But persistent loneliness leads to chronically high levels.
These chemicals could provide a link between loneliness and dementia. In a mouse model of Alzheimer’s disease, for example, glucocorticoids increased the levels of two proteins that are involved in the main hallmark of the condition, the protein plaques that tangle around neurons and interfere with memory and cognition 9 .
Stress is an extra assault on brains that are already wearing out as people get older, Mwilambwe-Tshilobo says, but she wants to see more research before committing to an opinion on exactly what part stress-related chemicals play in neurodegeneration. “It could accelerate the rate of ageing, but there hasn’t been work that explicitly looks at that,” she says.
Tomova says that although high levels of stress hormones probably contribute to dementia, it’s also likely that people who feel lonely miss out on the mental exercise that social interactions provide. And just as a muscle needs exercise to stay fit, so does the brain. In fact, loneliness has been associated with a smaller volume of grey matter in the brain 10 . “This is all hypothesis, really, at this stage,” Sommerlad says, but the idea is that socializing maintains neural connections that might otherwise be lost.
Turning inward
Researchers looking for the neural signature of loneliness have also found differences that could help to explain some of the correlations between loneliness and dementia. Previous research has suggested that there are changes in the connectivity between brain areas in people who feel lonely 11 . A 2020 study 12 examined an area of the brain called the default network — so called because it’s active by default when a person isn’t engaged in a particular task and turns their attention inward — in older people who reported being lonely.
The hurt of loneliness and social isolation
Previous work had suggested that young people who feel lonely have high neural cross-talk between the default network and other networks associated with vision, attention and executive control 13 , possibly because they’re on high alert for social cues, says Spreng, one of the authors on the 2020 study of older people. But his team found the opposite in brain scans from the UK Biobank cohort of people aged 40 to 69. Loneliness weakened connections between the default network and the visual system and instead strengthened connections within the default network.
That could be because older people remedy loneliness by retreating into memories of past social experiences, Spreng says. In doing so, they strengthen the default network.
The default network is one of many networks in the brain that accrues damage during Alzheimer’s disease. Spreng and his colleagues are investigating whether strong default networks can indeed be linked to neurodegeneration — and if so, why. He wonders whether robust neural connections might allow pathologies to spread more readily in the network. The idea is far from proven, but it’s a plausible explanation and “an interesting hypothesis”, says cognitive neuroscientist Anastasia Benedyk at the Central Institute of Mental Health in Mannheim, Germany.
The study “lays the foundation for us to be able to test some hypotheses a little bit more empirically”, says Mwilambwe-Tshilobo, who was also involved in the work linking the default network with loneliness.
Finding solutions
Some remedies for loneliness will come as no surprise. Increasing access to social activities, for example by housing people in communities with common areas, can help, Sommerlad says. Some researchers are also finding ways to tap into the neural mechanisms underlying loneliness directly, through exercise, for instance.
Walking 4–5 kilometres over the course of an hour completely reversed feelings of low mood associated with loneliness in some people, Benedyk and her colleagues found 14 . What’s more, people with high connectivity in their default networks — the same area Spreng studied, which is also known to be affected by depression — were among those who benefited from exercise the most.
One possible explanation for this observation is that people with depression are “stuck in rumination” — a behaviour that draws heavily on the default network, Benedyk says. Exercise could force them to use other parts of their brain by interrupting neural processes that are associated with self-reflection and shifting activity to areas associated with physical activities — freeing them from a cycle of negative thoughts.
Exercising is also a great excuse to socialize. These days, Chaklos is retired, but she now leads the Boston branch of a US programme called ‘Walk with a Doc’, in which physicians invite community members to walk with them. At the group’s February walk, about 14 people chatted and strolled inside the Prudential Center mall in Boston, Massachusetts, where they could avoid New England’s winter weather. The activity “just uplifts a person’s mood”, Chaklos says. “Even if you’re still going back home to be by yourself, you don’t feel totally alone any more.”
Nature 628 , 22-24 (2024)
doi: https://doi.org/10.1038/d41586-024-00900-4
Park, C. et al. Psychiatry Res. 294 , 113514 (2020).
Article PubMed Google Scholar
Wang, F. et al. Nature Hum. Behav. 7 , 1307–1319 (2023).
Holwerda, T. J. et al. J. Neurol. Neurosurg. Psychiatry 85 , 133-134 (2013).
PubMed Google Scholar
Baek, E. C. et al. Psychol. Sci. 34 , 683–695 (2023).
Cacioppo, J. T., Fowler, J. H. & Christakis, N. A. J. Pers. Soc. Psychol. 97 , 977–991 (2009).
Tomova, L. et al. Nature Neurosci. 23 , 1597–1605 (2020).
Matthews, G. A. et al. Cell 164 , 617–631 (2016).
Tomova, L., Towner, E., Thomas, K. & Blakemore, S.-J. Preprint at Research Square https://doi.org/10.21203/rs.3.rs-2718114/v1 (2023).
Green, K. N., Billings, L. M., Roozendaal, B., McGaugh, J. L. & LaFerla, F. M. J. Neurosci. 26 , 9047–9056 (2006).
van der Velpen, I. F. et al. Biol. Psychiatry. Cogn. Neurosci. Neuroimaging 7 , 659–668 (2022).
Feng, C., Wang, L., Li, T. & Xu, P. Soc. Cogn. Affect. Neurosci. 14 , 353–365 (2019).
Spreng, R. N. et al. Nature Commun. 11 , 6393 (2020).
Mwilambwe-Tshilobo, L. et al. Soc. Cogn. Affect. Neurosci. 14 , 423–433 (2019).
Benedyk, A. et al. Nature Mental Health 2 , 337–342 (2024).
Article Google Scholar
Download references
Reprints and permissions
Related Articles

- Neuroscience

A brain-specific angiogenic mechanism enabled by tip cell specialization
Article 03 APR 24

Ancestral allele of DNA polymerase gamma modifies antiviral tolerance

Formation of memory assemblies through the DNA-sensing TLR9 pathway
Article 27 MAR 24
Adopt universal standards for study adaptation to boost health, education and social-science research
Correspondence 02 APR 24
Allow researchers with caring responsibilities ‘promotion pauses’ to make research more equitable

Is IVF at risk in the US? Scientists fear for the fertility treatment’s future
News 02 APR 24
Diabetes drug slows development of Parkinson’s disease
News 03 APR 24

Interim analyses of a first-in-human phase 1/2 mRNA trial for propionic acidaemia
Faculty Positions, Aging and Neurodegeneration, Westlake Laboratory of Life Sciences and Biomedicine
Applicants with expertise in aging and neurodegeneration and related areas are particularly encouraged to apply.
Hangzhou, Zhejiang, China
Westlake Laboratory of Life Sciences and Biomedicine (WLLSB)
Faculty Positions in Chemical Biology, Westlake University
We are seeking outstanding scientists to lead vigorous independent research programs focusing on all aspects of chemical biology including...
School of Life Sciences, Westlake University
Faculty Positions in Neurobiology, Westlake University
We seek exceptional candidates to lead vigorous independent research programs working in any area of neurobiology.
Head of the histopathology and imaging laboratory
GENETHON recruits: Head of the histopathology and imaging laboratory (H/F)
Evry-Sud, Evry (FR)
Seeking Global Talents, the International School of Medicine, Zhejiang University
Welcome to apply for all levels of professors based at the International School of Medicine, Zhejiang University.
Yiwu, Zhejiang, China
International School of Medicine, Zhejiang University
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Mol Cell Biol
- v.13(7); 2021 Jul

Obesity: causes, consequences, treatments, and challenges
Obesity has become a global epidemic and is one of today’s most public health problems worldwide. Obesity poses a major risk for a variety of serious diseases including diabetes mellitus, non-alcoholic liver disease (NAFLD), cardiovascular disease, hypertension and stroke, and certain forms of cancer ( Bluher, 2019 ).
Obesity is mainly caused by imbalanced energy intake and expenditure due to a sedentary lifestyle coupled with overnutrition. Excess nutrients are stored in adipose tissue (AT) in the form of triglycerides, which will be utilized as nutrients by other tissues through lipolysis under nutrient deficit conditions. There are two major types of AT, white AT (WAT) and brown AT, the latter is a specialized form of fat depot that participates in non-shivering thermogenesis through lipid oxidation-mediated heat generation. While WAT has been historically considered merely an energy reservoir, this fat depot is now well known to function as an endocrine organ that produces and secretes various hormones, cytokines, and metabolites (termed as adipokines) to control systemic energy balance. Studies over the past decade also show that WAT, especially subcutaneous WAT, could undergo ‘beiging’ remodeling in response to environmental or hormonal perturbation. In the first paper of this special issue, Cheong and Xu (2021) systematically review the recent progress on the factors, pathways, and mechanisms that regulate the intercellular and inter-organ crosstalks in the beiging of WAT. A critical but still not fully addressed issue in the adipose research field is the origin of the beige cells. Although beige adipocytes are known to have distinct cellular origins from brown and while adipocytes, it remains unclear on whether the cells are from pre-existing mature white adipocytes through a transdifferentiation process or from de novo differentiation of precursor cells. AT is a heterogeneous tissue composed of not only adipocytes but also nonadipocyte cell populations, including fibroblasts, as well as endothelial, blood, stromal, and adipocyte precursor cells ( Ruan, 2020 ). The authors examined evidence to show that heterogeneity contributes to different browning capacities among fat depots and even within the same depot. The local microenvironment in WAT, which is dynamically and coordinately controlled by inputs from the heterogeneous cell types, plays a critical role in the beige adipogenesis process. The authors also examined key regulators of the AT microenvironment, including vascularization, the sympathetic nerve system, immune cells, peptide hormones, exosomes, and gut microbiota-derived metabolites. Given that increasing beige fat function enhances energy expenditure and consequently reduces body weight gain, identification and characterization of novel regulators and understanding their mechanisms of action in the beiging process has a therapeutic potential to combat obesity and its associated diseases. However, as noticed by the authors, most of the current pre-clinical research on ‘beiging’ are done in rodent models, which may not represent the exact phenomenon in humans ( Cheong and Xu, 2021 ). Thus, further investigations will be needed to translate the findings from bench to clinic.
While both social–environmental factors and genetic preposition have been recognized to play important roles in obesity epidemic, Gao et al. (2021) present evidence showing that epigenetic changes may be a key factor to explain interindividual differences in obesity. The authors examined data on the function of DNA methylation in regulating the expression of key genes involved in metabolism. They also summarize the roles of histone modifications as well as various RNAs such as microRNAs, long noncoding RNAs, and circular RNAs in regulating metabolic gene expression in metabolic organs in response to environmental cues. Lastly, the authors discuss the effect of lifestyle modification and therapeutic agents on epigenetic regulation of energy homeostasis. Understanding the mechanisms by which lifestyles such as diet and exercise modulate the expression and function of epigenetic factors in metabolism should be essential for developing novel strategies for the prevention and treatment of obesity and its associated metabolic diseases.
A major consequence of obesity is type 2 diabetes, a chronic disease that occurs when body cannot use and produce insulin effectively. Diabetes profoundly and adversely affects the vasculature, leading to various cardiovascular-related diseases such as atherosclerosis, arteriosclerotic, and microvascular diseases, which have been recognized as the most common causes of death in people with diabetes ( Cho et al., 2018 ). Love et al. (2021) systematically review the roles and regulation of endothelial insulin resistance in diabetes complications, focusing mainly on vascular dysfunction. The authors review the vasoprotective functions and the mechanisms of action of endothelial insulin and insulin-like growth factor 1 signaling pathways. They also examined the contribution and impart of endothelial insulin resistance to diabetes complications from both biochemical and physiological perspectives and evaluated the beneficial roles of many of the medications currently used for T2D treatment in vascular management, including metformin, thiazolidinediones, glucagon-like receptor agonists, dipeptidyl peptidase-4 inhibitors, sodium-glucose cotransporter inhibitors, as well as exercise. The authors present evidence to suggest that sex differences and racial/ethnic disparities contribute significantly to vascular dysfunction in the setting of diabetes. Lastly, the authors raise a number of very important questions with regard to the role and connection of endothelial insulin resistance to metabolic dysfunction in other major metabolic organs/tissues and suggest several insightful directions in this area for future investigation.
Following on from the theme of obesity-induced metabolic dysfunction, Xia et al. (2021) review the latest progresses on the role of membrane-type I matrix metalloproteinase (MT1-MMP), a zinc-dependent endopeptidase that proteolytically cleaves extracellular matrix components and non-matrix proteins, in lipid metabolism. The authors examined data on the transcriptional and post-translational modification regulation of MT1-MMP gene expression and function. They also present evidence showing that the functions of MT1-MMP in lipid metabolism are cell specific as it may either promote or suppress inflammation and atherosclerosis depending on its presence in distinct cells. MT1-MMP appears to exert a complex role in obesity for that the molecule delays the progression of early obesity but exacerbates obesity at the advanced stage. Because inhibition of MT1-MMP can potentially lower the circulating low-density lipoprotein cholesterol levels and reduce the risk of cancer metastasis and atherosclerosis, the protein has been viewed as a very promising therapeutic target. However, challenges remain in developing MT1-MMP-based therapies due to the tissue-specific roles of MT1-MMP and the lack of specific inhibitors for this molecule. Further investigations are needed to address these questions and to develop MT1-MMP-based therapeutic interventions.
Lastly, Huang et al. (2021) present new findings on a critical role of puromycin-sensitive aminopeptidase (PSA), an integral non-transmembrane enzyme that catalyzes the cleavage of amino acids near the N-terminus of polypeptides, in NAFLD. NAFLD, ranging from simple nonalcoholic fatty liver to the more aggressive subtype nonalcoholic steatohepatitis, has now become the leading chronic liver disease worldwide ( Loomba et al., 2021 ). At present, no effective drugs are available for NAFLD management in the clinic mainly due to the lack of a complete understanding of the mechanisms underlying the disease progress, reinforcing the urgent need to identify and validate novel targets and to elucidate their mechanisms of action in NAFLD development and pathogenesis. Huang et al. (2021) found that PSA expression levels were greatly reduced in the livers of obese mouse models and that the decreased PSA expression correlated with the progression of NAFLD in humans. They also found that PSA levels were negatively correlated with triglyceride accumulation in cultured hepatocytes and in the liver of ob/ob mice. Moreover, PSA suppresses steatosis by promoting lipogenesis and attenuating fatty acid β-oxidation in hepatocytes and protects oxidative stress and lipid overload in the liver by activating the nuclear factor erythroid 2-related factor 2, the master regulator of antioxidant response. These studies identify PSA as a pivotal regulator of hepatic lipid metabolism and suggest that PSA may be a potential biomarker and therapeutic target for treating NAFLD.
In summary, papers in this issue review our current knowledge on the causes, consequences, and interventions of obesity and its associated diseases such as type 2 diabetes, NAFLD, and cardiovascular disease ( Cheong and Xu, 2021 ; Gao et al., 2021 ; Love et al., 2021 ). Potential targets for the treatment of dyslipidemia and NAFLD are also discussed, as exemplified by MT1-MMP and PSA ( Huang et al., 2021 ; Xia et al., 2021 ). It is noted that despite enormous effect, few pharmacological interventions are currently available in the clinic to effectively treat obesity. In addition, while enhancing energy expenditure by browning/beiging of WAT has been demonstrated as a promising alternative approach to alleviate obesity in rodent models, it remains to be determined on whether such WAT reprogramming is effective in combating obesity in humans ( Cheong and Xu, 2021 ). Better understanding the mechanisms by which obesity induces various medical consequences and identification and characterization of novel anti-obesity secreted factors/soluble molecules would be helpful for developing effective therapeutic treatments for obesity and its associated medical complications.
- Bluher M. (2019). Obesity: global epidemiology and pathogenesis . Nat. Rev. Endocrinol . 15 , 288–298. [ PubMed ] [ Google Scholar ]
- Cheong L.Y., Xu A. (2021). Intercellular and inter-organ crosstalk in browning of white adipose tissue: molecular mechanism and therapeutic complications . J. Mol. Cell Biol . 13 , 466–479. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cho N.H., Shaw J.E., Karuranga S., et al. (2018). IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045 . Diabetes Res. Clin. Pract . 138 , 271–281. [ PubMed ] [ Google Scholar ]
- Gao W., Liu J.-L., Lu X., et al. (2021). Epigenetic regulation of energy metabolism in obesity . J. Mol. Cell Biol . 13 , 480–499. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Huang B., Xiong X., Zhang L., et al. (2021). PSA controls hepatic lipid metabolism by regulating the NRF2 signaling pathway . J. Mol. Cell Biol . 13 , 527–539. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Loomba R., Friedman S.L., Shulman G.I. (2021). Mechanisms and disease consequences of nonalcoholic fatty liver disease . Cell 184 , 2537–2564. [ PubMed ] [ Google Scholar ]
- Love K.M., Barrett E.J., Malin S.K., et al. (2021). Diabetes pathogenesis and management: the endothelium comes of age . J. Mol. Cell Biol . 13 , 500–512. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ruan H.-B. (2020). Developmental and functional heterogeneity of thermogenic adipose tissue . J. Mol. Cell Biol . 12 , 775–784. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Xia X.-D., Alabi A., Wang M., et al. (2021). Membrane-type I matrix metalloproteinase (MT1-MMP), lipid metabolism, and therapeutic implications . J. Mol. Cell Biol . 13 , 513–526. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Home — Essay Samples — Nursing & Health — Mental Health — Understanding Mental Health: Definition, Causes, and Impacts
Understanding Mental Health: Definition, Causes, and Impacts
- Categories: Mental Health
About this sample

Words: 638 |
Published: Jan 29, 2024
Words: 638 | Page: 1 | 4 min read
Table of contents
Definition and understanding of mental health, causes of mental health issues, common mental health disorders, impact of mental health on individuals, stigma surrounding mental health, effective ways to promote positive mental health.
- World Health Organization. (2014). Mental health: a state of well-being. Retrieved from https://www.who.int/features/factfiles/mental_health/en/
- National Institute of Mental Health. (n.d.). Mental Health Information. Retrieved from https://www.nimh.nih.gov/health/publications/mental-health-information/index.shtml

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
7 pages / 3006 words
5 pages / 2449 words
5 pages / 2111 words
2 pages / 834 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Mental Health
However, psychology also uses behavior along with the mapping to the DSM from the checklist survey to separate genuine from faked mental illness and this epistemological problem can be solved using the proven to be successful [...]
Mental health stigma is a pervasive issue that hinders individuals from seeking help, perpetuates myths, and marginalizes those who experience mental health challenges. This essay explores the nature of mental health stigma in [...]
Mental health stigma is a pervasive issue that has long hindered individuals from seeking the help they need and perpetuated damaging stereotypes and misconceptions. In this comprehensive essay, we will delve deeply into the [...]
Mental illness within the criminal justice system is a complex and pressing issue that intersects legal, medical, and ethical considerations. This essay examines the challenges posed by mental illness among individuals in the [...]
“Eat your vegetables! Exercise! Get a good night's sleep!” We’ve all known to take care of our bodies since grade school P. E. class. But what about our mental health, isn’t mental health just as important as physical health? [...]
Arnekrans et al. (2018) state that childhood trauma is also known as developmental trauma and this refers to numerous amounts of stressful experiences in child development. Many of these stressful experiences consist of divorce, [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Could poor sleep hygiene lead to an increased risk of heart attack? Maybe. Here's what to know

How you sleep determines how you feel throughout the day, and science is constantly uncovering increasingly more evidence about why a good night's sleep is at the core of a healthy lifestyle. Some researchers contend it is as important as a good diet and regular exercise.
Unfortunately, as our society gets progressively busier, we are more prone to being sleep-deprived, costing us more than we realize.
Recent research on the quality of sleep in men reported that in the majority, there were sleep problems that ranged from mild to severe sleep disorders. Not surprising. However, what was not expected was the finding that those with a sleep disorder experienced more than twice as many heart attacks. This caught my attention, and I wondered how it is possible that a sleep disorder can exert such a powerful negative influence.
For starters, inadequate sleep can mess with hormones, triggering undesirable outcomes including stoking the appetite, which could cause you to eat more and gain body fat. As males age, fat tends to be gained around the midsection, the worst place to gain fat. This is because excess belly fat promotes insulin resistance, which can contribute to high blood pressure and ultimately lead to Type 2 diabetes .
Thus, poor sleep may contribute to increased heart disease risk via three established heart disease risk factors ― excess body fat , high blood pressure, and Type 2 diabetes.
What can cause sleeping problems?
Next, I shifted my attention to what might be causing sleep problems. For example, obesity can cause sleep apnea . This further increases appetite, which could make you fatter, disrupting sleep even more, and creating a vicious cycle.
Another thing that causes interrupted sleep is worry. Research suggests that those with sleep disorders tend to report having significant social problems, things like a divorce, conflicts at work, a death in the family, etc. These are important events, but is it the event that is most disruptive to sleep, or the reaction to what happened? In other words, when two people confront the same problem, one may be a worry-wart and react very strongly, while the other is more relaxed and less bothered by it. This brings personality into the mix.
Does personality impact your heart health?
Years ago, it was proposed that personality contributes to heart disease. The so-called Type A personality described as competitive, ambitious, aggressive, volatile, and easily upset was thought to be the culprit. However, more research revealed that being Type A isn’t necessarily detrimental to your health. You can be hard-charging in your lifestyle, the opposite of Type B (relaxed, patient, not highly competitive, etc.), and even be a workaholic, and it’s OK.
Additional research revealed the degree of hostility in your personality and approach to life that matters most regarding heart disease risk. A hostile personality suggests an overarching characteristic of taking things too personally as explained in the 1989 book "The Trusting Heart" by psychiatrist Dr. Redford Williams. In a nutshell, a hostile personality constantly promotes psychological stress, and such stress is an established risk factor for heart disease.
The book by Williams also made it clear how to recognize hostility in yourself and what to do about it.
When I first read this book, I thought "goodness gracious, this guy has been following me around 24 hours a day and taking notes." It was enlightening but humbling to realize how my approach to life was too hostile, and how I personalized things to extreme.
For example, it seemed I was always multi-tasking and in a hurry, and at the time I would become angry if anything got in my way. If the car in front of me in the fast lane was going too slow, I’d blow it up in my mind.
“Why is he doing that? I’m going to be late.”
Worse, I’d personalize it, and whatever was happening wasn’t just happening at random. It was happening to “me,” and I resented it, triggering my anger.
Can a personality change impact heart health?
My newfound awareness about hostility inspired me to change, and I realized that although I still had gut reactions to certain situations, I had a choice. I could either allow myself to be frustrated, get angry, and express it, or recognize the feelings and decide not to act out the way I always had. I made this huge and important change with the help of psychologist, Ed Kopp, who helped me greatly in several ways and the impact was remarkable.
As a result, I am a happier person and much easier to get along with. And, just as important, I’m sure my heart health took a big step forward.
If you have excess belly fat, high blood pressure, Type 2 diabetes, and an ongoing high level of psychological stress, you are placing your heart in great danger. Is it possible that these factors can be traced back to poor sleep and your approach to life — your personality? Perhaps. If so, please start today to take some corrective steps.
Reach Bryant Stamford, a professor of kinesiology and integrative physiology at Hanover College, at [email protected] .
- Share full article
Advertisement
Supported by
What Really Causes Poor Performance in School
More from our inbox:, becoming a republican to vote against trump, countering propaganda from the fossil fuel industry.

To the Editor:
Re “ We’re Not Battling the School Issues That Matter ,” by Nicholas Kristof (column, March 7):
I completely agree with Mr. Kristof’s column. The situation is serious, not only for education but also for our embattled democracy.
I would like to add some nuance. I have been working on a state-by-state analysis of the possible influence of racism, specifically anti-Black racism, on educational achievement.
What I have found so far indicates that some children are taught quite well: those in private schools, of course; Asian American children (particularly those whose families are from India); white children of families prosperous enough to be ineligible for the National School Lunch Program; children of college-educated parents; and Hispanic children who are not English-language learners.
Some students are in groups that are not likely to be taught to read effectively: Native Americans, children who are poor enough to be eligible for the National School Lunch Program and Black children.
None of this will be news to Mr. Kristof. What is surprising to me is the sheer extent and arbitrary nature of the failure by school authorities. Almost everywhere that urban schools, in particular, are failing, socioeconomically similar children are being taught much more effectively in the nearest suburban districts.
Part of the reason is money: Per-student expenditure is associated with educational achievement.
But part of the problem — most of it — is a matter of administrative decisions: placing the best teachers in schools with the “best” students; equipping schools, in effect, in accordance with parental income; offering more gifted and talented classes to white students — all the perhaps unconscious manifestations of everyday racism.
Michael Holzman Briarcliff Manor, N.Y. The writer is a former consultant for the Schott Foundation for Public Education in Cambridge, Mass.
Writers like Nicholas Kristof make a critical mistake when they assume that conservatives’ focus on issues like nudity, diversity and critical race theory in education is just a matter of misplaced priorities. Conservatives’ opposition to substantive improvements in American education is not a bug; it’s a feature.
Do politicians like Ron DeSantis and Donald Trump really want children to grow up with a better grasp of math, when they can instead persuade voters that inflation is an existential threat to their personal financial security, even when wage growth is comfortably outstripping inflation?
Do they want students to become better critical thinkers when they can use photos of migrants massed at the border to convince voters that immigrants are a threat to national security, even though most immigrants will provide needed labor in a rapidly growing economy?
Do they want students to be good readers who can use logic and analysis to evaluate an argument, when politicians can easily use social media platforms, with no evidence, to persuade voters that the 2020 presidential election was rigged?
Why would Republicans want America’s children to be well educated, when the voters with the most education will consistently vote for the other guys?
Lisa Elliott Newark, Del. The writer is a licensed school psychologist.
Nicholas Kristof’s column miseducates by pointing out which states do better with schools.
In Massachusetts, one of the examples Mr. Kristof mentions, parents don’t move there because of the schools. They choose the town or city they think has the best schools — and the one they can afford.
Local property taxes, not the state, provide most educational funding, so the better schools tend to be in the wealthier towns. Per-pupil spending in Massachusetts varies greatly from district to district: According to recent data from the state Department of Education , that figure ranges from about $14,000 in Dracut to almost $37,000 in Cambridge.
More money means smaller classes and better-paid teachers. So Mr. Kristof’s argument about which states have better education mostly misses the mark about what matters.
Michael Jacoby Brown Arlington, Mass. The writer is a community organizer and former high school teacher.
Nicholas Kristof makes some valid points in his column, but I have to wonder why he and most of the media skipped over Donald Trump’s promise that followed his vile remark about denying funding to schools that teach critical race theory.
Mr. Trump announced, “ I will not give one penny to any school that has a vaccine mandate or mask mandate .”
Hello, diphtheria, tetanus, polio, pertussis, measles, mumps, hepatitis, rubella and more.
Surely, any worries over whether teachers choose to focus on phonics or address critical race theory will vanish when these diseases, which vaccinations prevent, invade the schools.
Susan Ohanian Charlotte, Vt. The writer is a retired reading teacher.
Re “ Trump’s Conquest of the Republican Party ” (editorial, March 10):
I’ve been a registered Democrat most of my adult life, except for a brief time with the Green Party. I have campaigned for Bernie Sanders. Earlier this winter I changed my official party affiliation to Republican. I made that change solely as a way to vote against Donald Trump in the primaries.
My plan following Nikki Haley’s exit after Super Tuesday is to cast a protest vote in New York next month. In November, I’ll vote for Joe Biden.
That said, my registration won’t change again. I’m not going anywhere. The G.O.P. will be stuck with this lefty.
The party of Trump needs a new birth of freedom, however belated, within its ranks. That reconstruction must be seeded by individual voters like yours truly.
Donald Mender Rhinebeck, N.Y.
Re “ John Kerry: ‘I Feel Deeply Frustrated,’ ” by David Wallace-Wells (Opinion, March 10):
John Kerry, America’s departing climate envoy, is “pissed off and frustrated” with the fossil fuel industry’s propaganda campaign to obstruct climate action and raise fears about its costs.
Just recently, the American Petroleum Institute launched an eight-figure media campaign intended to “dismantle policy threats” to the fossil fuel industry, with statements such as “Products made from oil and gas … make everyday living more mobile, comfortable and healthier.”
Most Americans — including our policymakers — are unaware that burning fossil fuels produces pollution that causes over eight million deaths a year.
Rather than bemoan the industry’s decades of disinformation, we need to proactively counter it. Exxon and other fossil fuel companies followed Big Tobacco’s playbook. Let’s build on lessons from successful tobacco control campaigns with a “truth” campaign on fossil fuels and health, enforcement of false advertising rules, and a Surgeon General’s Advisory on the Health Harms of Fossil Fuels.
Linda Rudolph Oakland, Calif. The writer is a consultant with the Medical Society Consortium on Climate and Health and on the steering committee of the Fossil Free for Health Coalition.

IMAGES
VIDEO
COMMENTS
Poverty and Health. Context. Poverty is a major cause of ill health and a barrier to accessing health care when needed. This relationship is financial: the poor cannot afford to purchase those things that are needed for good health, including sufficient quantities of quality food and health care. But, the relationship is also related to other ...
For the 6.8 million children living in deep poverty (those with family incomes of less than half of poverty), there are adverse consequences across the life course related to nutrition ...
Poverty has been characterized in the following three ways: (1) economic well-being, commonly linked to income; (2) ability to navigate society as a function of an education or health status of the individual; and/or (3) social exclusion as a result of institutional behaviors, practices, and policies ( 1, 14 ).
The causes of poor health for millions globally are rooted in political, social and economic injustices. Poverty is both a cause and a consequence of poor health. Poverty increases the chances of poor health. Poor health, in turn, traps communities in poverty. Infectious and neglected tropical diseases kill and weaken millions of the poorest ...
Health inequities are unfair and could be reduced by the right mix of government policies. Every day 16 000 children die before their fifth birthday. Maternal mortality is a key indicator of health inequity. Tuberculosis is a disease of poverty. 87% of premature deaths due to noncommunicable diseases occur in low- and middle-income countries.
The question is: "What are the causes of this and is it too late for solving this problem?". Obesity is one of the poor health causes. A lot of children in middle school and in high school are obese. Almost every teacher will say this: "Parents are buying what the kids want, rather than what may be healthy for them" (fourth-grade ...
Abstract. During the past two decades, the public health community's attention has been drawn increasingly to the social determinants of health (SDH)—the factors apart from medical care that can be influenced by social policies and shape health in powerful ways. We use "medical care" rather than "health care" to refer to clinical ...
Because income is a significant, well-documented determinant of health, the effects of low income and income inequality are reflected in population health. Referred to as a "cause of causes" or "fundamental cause" of health outcomes, income shapes the resources at our disposal, the disease risks we are exposed to, and our ability to ...
The social determinants of health that typically make up this field of study are social class, sex, age, race, and ethnicity. In this essay I focus mainly on social class but note that there is a ...
Low quality healthcare is increasing the burden of illness and health costs globally. Poor quality health services are holding back progress on improving health in countries at all income levels, according to a new joint report by the OECD, World Health Organization (WHO) and the World Bank. Today, inaccurate diagnosis, medication errors ...
However, it is very challenging to determine if malnutrition can be considered a cause or consequence of poverty ( Siddiqui et al. ). Individuals living in poverty have limited access to necessities such as clean water, hygiene, and healthy food products. The consequences of poverty on individuals include food insecurity, poor health, and ...
Poverty and Diseases Essay. It is believed that poverty and poor health are correlated, especially in developing countries. Due to various circumstances, marginalized social groups are affected by unhygienic living conditions, thus allowing infections to spread. Moreover, poor people are often stripped of the information or availability of ...
Introduction. Poverty is a complex and insidious determinant of health caused by systemic factors that can persist for generations in a family. Beginning before birth and continuing throughout an ...
Those growing up in poverty are subsequently more likely to suffer poor mental and physical health into adulthood, risking life-limiting, severe, long-term illnesses. Longitudinal studies have ...
to improve health and (2) provides a better understanding of the linkages between poor health and economic outcomes. The three essays that comprise the dissertation investigate separate contexts and linkages involving health and nutrition in the developing world.
Individual response to stressors influences their health. Maladaptive response to stress results in various physical, psychological, and behavioral negative effects. Negative effects of stress on physical health include increased heart rates, sweating, high blood pressure, and long-term development of the cardiac condition. Psychological ...
Mental health, an integral facet of human well-being, shapes our emotions, decisions, and daily interactions. Just as one would care for a sprained ankle or a fever, our minds too require attention and nurture. In today's bustling world, mental well-being is often put on the back burner, overshadowed by the immediate demands of life.
Consuming too much sodium can increase blood pressure and the risk for heart disease and stroke. Current guidelines recommend getting less than 2,300 mg a day, but Americans consume more than 3,400 mg a day on average. Over 70% of the sodium that Americans eat comes from packaged, processed, store-bought, and restaurant foods.
But why does feeling alone lead to poor health? Over the past few years, scientists have begun to reveal the neural mechanisms that cause the human body to unravel when social needs go unmet.
Rich Get Richer, Poor Get Poorer: Rich Vs Poor Pages: 4 (1129 words) Poor Drainage System: Causes, Consequences, and Remedies Pages: 2 (492 words) Filariasis: Causes, Effects and Prevention Pages: 3 (731 words) Understanding Tuberculosis: Causes, Prevention, and Treatment Pages: 5 (1236 words)
The vicious cycle between poor health and poverty is an unwanted gift that keeps on giving. Medical debt degrades health and nutrition, both financially and in terms of stress. Those laboring under the burden of debt have higher blood pressure, worse self-reported health status, poorer mental health, and shorter life expectancy than those with ...
Obesity has become a global epidemic and is one of today's most public health problems worldwide. Obesity poses a major risk for a variety of serious diseases including diabetes mellitus, non-alcoholic liver disease (NAFLD), cardiovascular disease, hypertension and stroke, and certain forms of cancer (Bluher, 2019).Obesity is mainly caused by imbalanced energy intake and expenditure due to a ...
Definition and Understanding of Mental Health. Mental health encompasses a person's emotional, psychological, and social well-being. It affects how individuals think, feel, and act, and helps determine how they handle stress, relate to others, and make choices. Good mental health is essential for functioning well in everyday life, maintaining ...
41%. Percentage of teens with the highest social media use who rate their overall mental health as poor or very poor, compared with 23% of those with the lowest use. For example, 10% of the highest use group expressed suicidal intent or self-harm in the past 12 months compared with 5% of the lowest use group, and 17% of the highest users expressed poor body image compared with 6% of the lowest ...
KU ~ lower deciles have a higher rate of poor health (over 30% in decile 1) no one in decile 10 feels they have very bad health, only about 10% bad health at all > Life expectancy ~ Calton - 54 years ~ Lenzie - 82 ~ at birth boys in the lowest social class almost 6 years shorter than in highest > Marmot Review ~ the more deprived the area the shorter the life expectancy ~ people in poorer ...
Thus, poor sleep may contribute to increased heart disease risk via three established heart disease risk factors ― excess body fat, high blood pressure, and Type 2 diabetes. What can cause ...
Responses to a column by Nicholas Kristof about schools' inadequacies. Also: A lefty in the G.O.P.; countering fossil fuel industry propaganda.