मानसिक स्वास्थ्य पर निबंध | Essay on Mental Health in Hindi | 10 Lines on Mental Health in Hindi
By निशा ठाकुर
Published on: December 30, 2023
Essay on Mental Health in Hindi : इस लेख में हमने मानसिक स्वास्थ्य के बारे में जानकारी प्रदान की है। यहाँ पर दी गई जानकारी बच्चों से लेकर प्रतियोगी परीक्षाओं के तैयारी करने वाले छात्रों के लिए उपयोगी साबित होगी।
मानसिक स्वास्थ्य पर निबंध: मानसिक स्वास्थ्य में किसी का मनोवैज्ञानिक, भावनात्मक और सामाजिक कल्याण शामिल होता है – किसी का मानसिक स्वास्थ्य उसके सोचने, महसूस करने और कार्य करने के तरीके को प्रभावित करता है। यह यह निर्धारित करने में भी मदद करता है कि कोई व्यक्ति तनाव को कैसे संभालता है, चुनाव करता है और दूसरों से संबंधित होता है। मानसिक स्वास्थ्य किसी के दैनिक जीवन की गतिविधियों, संबंधों और शारीरिक स्वास्थ्य को प्रभावित कर सकता है।
मानसिक स्वास्थ्य से तात्पर्य संज्ञानात्मक और व्यवहारिक कल्याण की स्थिति से है। कभी-कभी ‘मानसिक स्वास्थ्य’ शब्द का प्रयोग मानसिक विकार की अनुपस्थिति को निर्धारित करने के लिए किया जाता है। यह भलाई की स्थिति है जिससे प्रत्येक व्यक्ति अपनी क्षमता का एहसास करता है और जीवन में परिवर्तन और अनिश्चितता से निपट सकता है।
आप लेखों, घटनाओं, लोगों, खेल, तकनीक के बारे में और निबंध पढ़ सकते हैं ।
- 1.1 मानसिक स्वास्थ्य पर लंबा निबंध(500 शब्द)
- 1.2 मानसिक स्वास्थ्य पर लघु निबंध( 150 शब्द)
- 2 मानसिक स्वास्थ्य पर 10 पंक्तियाँ
- 3 मानसिक स्वास्थ्य पर अक्सर पूछे जाने वाले प्रश्न

मानसिक स्वास्थ्य पर लंबा और छोटा निबंध
हम छात्रों को संदर्भ के लिए मानसिक स्वास्थ्य विषय पर 500 शब्दों के लंबे निबंध और 150 शब्दों के एक छोटे निबंध पर निबंध के नमूने प्रदान करते हैं।
मानसिक स्वास्थ्य पर लंबा निबंध(500 शब्द)
मानसिक स्वास्थ्य पर लंबा निबंध आमतौर पर कक्षा 7, 8, 9 और 10 को दिया जाता है।
मानसिक स्वास्थ्य महत्वपूर्ण है और स्वास्थ्य के एक घटक को एकीकृत करता है। मानसिक स्वास्थ्य में एक व्यक्ति की मनोवैज्ञानिक, भावनात्मक और सामाजिक भलाई शामिल होती है। उचित मानसिक स्वास्थ्य के परिणामस्वरूप उचित मानसिक कार्य होता है जिसके परिणामस्वरूप गतिविधियों में उत्पादक होता है, अन्य लोगों के साथ स्वस्थ और पूर्ण संबंध होते हैं और प्रतिकूल परिस्थितियों का सामना करने और अनुकूलन करने की क्षमता होती है।
बचपन और किशोरावस्था से लेकर वयस्कता तक – जीवन के हर चरण में उचित मानसिक स्वास्थ्य आवश्यक है। जीवन भर, एक व्यक्ति किसी भी समय मानसिक स्वास्थ्य के मुद्दे का अनुभव कर सकता है। यह न केवल उनके मनोदशा और व्यवहार को प्रभावित करता है बल्कि उनके सोचने, जीवन को देखने और चुनौतियों का सामना करने के तरीके को भी बदलता है।
भले ही मानसिक स्वास्थ्य एक अत्यधिक व्यक्तिगत चीज है, जो एक व्यक्ति को प्रभावित करता है वह दूसरे व्यक्ति को प्रभावित कर सकता है या नहीं भी कर सकता है; हालांकि, कुछ महत्वपूर्ण कारक मानसिक स्वास्थ्य समस्याओं में योगदान करते हैं। इन कारकों में जीवन के अनुभव जैसे आघात या दुर्व्यवहार, मस्तिष्क के जीन या रसायन विज्ञान जैसे जैविक कारक और यहां तक कि मानसिक स्वास्थ्य समस्याओं का पारिवारिक इतिहास भी किसी व्यक्ति को प्रभावित कर सकता है। खराब मानसिक स्वास्थ्य तनावपूर्ण कार्य परिस्थितियों, तेजी से सामाजिक परिवर्तन, लिंग भेदभाव, लिंग भेदभाव, सामाजिक बहिष्कार, शारीरिक बीमारी और मानवाधिकारों के उल्लंघन से भी जुड़ा हुआ है।
मानसिक स्वास्थ्य समस्याएं आम हैं, लेकिन सबसे लंबे समय तक, लोगों ने इसकी पूरी अवधारणा से परहेज किया है और मानसिक स्वास्थ्य को हल्के में लिया है। एक समय में, मानसिक स्वास्थ्य को वर्जित माना जाता था, और मदद मांगने वाले को मानसिक रूप से बीमार करार दिया जाता था। मानसिक स्वास्थ्य और मानसिक बीमारी समान चीजें नहीं हैं।
लंबे समय से, मानसिक स्वास्थ्य को चिंता और अवसाद जैसी मानसिक बीमारियों की अनुपस्थिति के रूप में परिभाषित किया गया है। मानसिक बीमारी आमतौर पर सभी निदान योग्य मानसिक विकारों को संदर्भित करती है – स्वास्थ्य की स्थिति जो बिगड़ा हुआ कामकाज या संकट से जुड़े मूड, सोच और व्यवहार में बदलाव की विशेषता है।
मानसिक स्वास्थ्य और मानसिक रोग साथ-साथ चलते हैं। इष्टतम मानसिक स्वास्थ्य स्थितियों वाले व्यक्ति भी मानसिक बीमारी का सामना कर सकते हैं, जहां जिन लोगों को कोई मानसिक बीमारी नहीं है, उनका मानसिक स्वास्थ्य भी खराब हो सकता है। हाल के दिनों में, लोगों ने मानसिक स्वास्थ्य को गंभीरता से लेना शुरू कर दिया है और किसी भी मानसिक स्वास्थ्य समस्या से निपटने के लिए उचित कदम उठाने शुरू कर दिए हैं।
मानसिक स्वास्थ्य के मुद्दों से पीड़ित लोग विभिन्न लक्षण दिखाते हैं जैसे कि कम या कोई ऊर्जा, लोगों को दूर करना और नियमित गतिविधियों से खुद को वापस खींचना, नींद की कमी या खाने की इच्छा, धूम्रपान, शराब पीना या ड्रग्स करना, असहाय महसूस करना, चिल्लाना और लड़ना, बहुत जल्दी आपा खोना, खुद को और बहुतों को नुकसान पहुँचाना।
मानसिक स्वास्थ्य की देखभाल करना न केवल जरूरत पड़ने पर पेशेवरों की मदद लेना है, बल्कि दूसरे से जुड़ना, शारीरिक गतिविधियों में शामिल होना, दूसरों की मदद करना, पर्याप्त नींद लेना और सकारात्मक रहना है कि कोई रास्ता है। सकारात्मक मानसिक स्वास्थ्य लोगों को अपनी पूरी क्षमता का एहसास करने, जीवन में तनाव का सामना करने, उत्पादक रूप से काम करने और समुदाय में सार्थक योगदान करने की अनुमति देता है। लोगों के जीवन में विभिन्न कारक जैसे कि अंतर्वैयक्तिक संबंध, शारीरिक कारक, बचपन का आघात और कई अन्य स्थितियां मानसिक स्वास्थ्य की स्थिति को बाधित कर सकती हैं। अपने मानसिक स्वास्थ्य की देखभाल और देखभाल करने से व्यक्ति के जीवन का आनंद लेने की क्षमता बनी रहती है।
मानसिक स्वास्थ्य पर लघु निबंध( 150 शब्द)
मानसिक स्वास्थ्य पर लघु निबंध आमतौर पर कक्षा 1, 2, 3, 4, 5 और 6 को दिया जाता है।
मानसिक स्वास्थ्य न केवल एक व्यक्ति का मनोवैज्ञानिक और भावनात्मक कल्याण है, बल्कि यह कल्याण की स्थिति भी है जहां एक व्यक्ति अपनी भावनात्मक और संज्ञानात्मक क्षमताओं का उपयोग रोजमर्रा की जिंदगी की मांगों को पूरा करने और समाज में योगदान करने के लिए कर सकता है। बचपन से किशोरावस्था से लेकर वयस्कता तक, जीवन के हर चरण में मानसिक स्वास्थ्य आवश्यक है।
हर साल 10 अक्टूबर को विश्व मानसिक स्वास्थ्य दिवस के रूप में मनाया जाता है। यह मानसिक स्वास्थ्य के लिए उस समय यूएनओ (संयुक्त राष्ट्र संगठन) के उप महासचिव द्वारा विश्व महासंघ द्वारा वार्षिक गतिविधि के रूप में शुरू किया गया था।
हर देश में मानसिक स्वास्थ्य के संसाधन अलग-अलग होते हैं। वहीं, पश्चिमी दुनिया के विकसित देश हर आयु वर्ग के लिए मानसिक स्वास्थ्य कार्यक्रम प्रदान करते हैं। तीसरी दुनिया के देशों में जहां परिवारों की बुनियादी जरूरतों को पूरा करने के लिए संघर्ष करना पड़ता है, वहां उचित मानसिक स्वास्थ्य सहायता प्रदान करने को ज्यादा महत्व नहीं दिया जाता है।
मानसिक स्वास्थ्य पर 10 पंक्तियाँ
- मानसिक स्वास्थ्य मनोवैज्ञानिक कल्याण की स्थिति है, या जहाँ मानसिक बीमारी अनुपस्थित है।
- भारतीय वयस्कों में से एक मानसिक स्वास्थ्य समस्याओं का सामना करता है।
- दस में से एक युवा ने महत्वपूर्ण अवसाद की अवधि का अनुभव किया है।
- मानसिक स्वास्थ्य की स्थिति जैसे चिंता, अवसाद और तनाव जीवन बदलने वाली शारीरिक स्वास्थ्य समस्याओं जैसे मधुमेह, कैंसर या दर्द के कारण विकसित हो सकते हैं।
- निदान योग्य मानसिक स्वास्थ्य समस्याओं वाले 20% से कम किशोरों और बच्चों को उचित उपचार मिलता है जिसकी उन्हें आवश्यकता होती है।
- एक जीन होने से जो मानसिक स्वास्थ्य विकार जैसे कि अवसाद या सिज़ोफ्रेनिया से जुड़ा होता है, इसका मतलब यह नहीं है कि स्थिति विकसित हो जाएगी।
- उचित मानसिक स्वास्थ्य मनोवैज्ञानिक और मानसिक कल्याण से जुड़ा हुआ है।
- दुनिया के 5 में से लगभग 1 बच्चे और किशोर मानसिक विकार से पीड़ित हैं।
- डिप्रेशन विकलांगता के प्रमुख कारणों में से एक है, जो 246 मिलियन लोगों को प्रभावित करता है।
- 14 साल की उम्र में मानसिक स्वास्थ्य संबंधी विकार होने लगते हैं।
मानसिक स्वास्थ्य पर अक्सर पूछे जाने वाले प्रश्न
प्रश्न 1. कुछ सामान्य मानसिक स्वास्थ्य विकारों के नाम लिखिए।
उत्तर: चिंता विकार, मनोदशा संबंधी विकार और सिज़ोफ्रेनिया विकार कुछ सामान्य मानसिक स्वास्थ्य विकार हैं।
प्रश्न 2. मानसिक स्वास्थ्य समस्याओं में योगदान देने वाले कारक कौन से हैं?
उत्तर: जैविक कारक जैसे जीन, जीवन बदलने वाले अनुभव जैसे आघात, दुर्व्यवहार या पुरानी बीमारी और यहां तक कि मानसिक स्वास्थ्य समस्याओं का पारिवारिक इतिहास।
प्रश्न 3. मानसिक स्वास्थ्य को किस प्रकार सुधारा जा सकता है?
उत्तर: कैसा महसूस होता है, इसके बारे में बात करना, सक्रिय रहना, अच्छा खाना और स्वस्थ रहना, उचित आराम करना और कभी-कभी मदद मांगना भी।
मैं इतिहास विषय की छात्रा रही हूँ I मुझे विभिन्न विषयों से जुड़ी जानकारी साझा करना बहुत पसंद हैI मैं इस मंच बतौर लेखिका कार्य कर रही हूँ I
Related Post
उपभोक्तावाद पर निबंध | consumerism essay in hindi, भारत में महिलाओं के सशक्तिकरण में बाधाओं पर निबंध | barriers to empowerment of women in india essay in hindi, उपभोक्ता अधिकारों पर निबंध | consumer rights essay in hindi, भिखारी पर निबंध | essay on beggars in hindi | beggars essay in hindi, leave a comment cancel reply.
Save my name, email, and website in this browser for the next time I comment.
Recent Posts
सेबरटूथ बाघ विलुप्त क्यों हो गए?

मैमथ विलुप्त क्यों हो गए?

डोडो पक्षी विलुप्त क्यों हो गया?
इस मंच के माध्यम से हमारा लक्ष्य विभिन्न विषयों से जुड़ी महत्वपूर्ण जानकारी अपने पाठकों तक पहुँचाना है
Quick Links
- Short Videos
- वेब स्टोरीज
- बीएमआई जांचें
- Dabur Vedic Tea
- शुगर-फ्री लाइफ
- स्वास्थ्य और बीमारियां
- डाइट और फिटनेस
- ग्रूमिंग टिप्स
- बच्चों के नाम
मानसिक स्वास्थ्य
- Causes and Symptoms
- Mental Health Disorders
- Tips for good mental health
Mental Health in Hindi (मेंटल हेल्थ), Mansik Swasthya in Hindi (मानसिक स्वास्थ्य): किसी भी व्यक्ति के लिए शारीरिक और मानसिक स्वास्थ्य दोनों ही बहुत जरूरी हैं। अगर कोई व्यक्ति शारीरिक रूप से स्वस्थ है लेकिन उसका मानसिक स्वास्थ्य खराब है तो उसे अपने जीवन में कई प्रकार की दिक्कतों का सामना करना पड़ेगा। मानसिक स्वास्थ्य से एक व्यक्ति को अपनी क्षमताओं का पता चलता है, उसके भीतर आत्मविश्वास आता कि वे जीवन में तनाव से सामना कर सकता है और अपने काम या कार्यों से अपने समुदाय के विकास में योगदान दे सकता है। मानसिक विकार व्यक्ति के स्वास्थ्य-संबंधी व्यवहार, फैसले, नियमित व्यायाम, पर्याप्त नींद, सुरक्षित यौन व्यवहार आदि को प्रभावित करता है और शारीरिक रोगों के खतरे को बढ़ाता है। मानसिक अस्वस्थता के कारण ही व्यक्ति को बेरोजगार, बिखरे हुए परिवार, गरीबी, नशीले पदार्थों का सेवन और संबंधित अपराध का सहभागी बनना पड़ता है। अगर किसी व्यक्ति का मानसिक स्वास्थ्य सही रहेगा तो उसका जीवन भी सही रहेगा। इसलिए हम आपको अपने इस खंड में मानसिक विकारों से जुड़ें हर पहलू के बारे में विस्तार से बताएंगे, जो आपके मानसिक स्वास्थ्य को बेहतर बनाने में मदद करेगा। पर आइए सबसे पहले जान लेते हैं, मानसिक स्वास्थ्य से जुड़ी कुछ जरूरी बातें।
मानसिक बीमारियों का कारण - Causes of Mental Illness
मानसिक स्वास्थ्य में हमारे भावनात्मक, मनोवैज्ञानिक और सामाजिक कल्याण (emotional, psychological, and social well-being) शामिल हैं। यह प्रभावित करता है कि हम कैसे सोचते हैं, महसूस करते हैं और कार्य करते हैं। आपका मानसिक स्वास्थ्य उम्र बढ़ने के साथ बदलता चला जाता है। अपने जीवन के दौरान, अगर आप मानसिक स्वास्थ्य समस्याओं का अनुभव करते हैं तो इसके बारें में जानना, डॉक्टर की मदद लेना और इलाज करवाना बेहद जरूरी है क्योंकि ये आपकी सोच, मनोदशा और व्यवहार को प्रभावित कर सकते हैं। ऐसे कई अन्य कारण भी हैं, जो कि मानसिक स्वास्थ्य समस्याओं में योगदान करते हैं, जिनमें शामिल हैं:
- -जैविक कारक (Biological factors), जैसे कि जीन या मस्तिष्क रसायन
- -मानसिक स्वास्थ्य समस्याओं का पारिवारिक इतिहास (Family history of mental health problems)
- -जीवन के अनुभव, जैसे आघात या तकलीफ (Life experiences, such as trauma or abuse)
- -जीवन में अवसाद रूपी वातावरण के कारण (Depressive Environment)
- -बचपन का आघात लगने के कारण (Childhood trauma)
- -तनावपूर्ण घटनाएं जैसे किसी प्रियजन को खोने के कारण (Stressful events of life)
- -नकारात्मक विचारों के बढ़ने के कारण (Negative thoughts)
- - अनहेल्दी आदतों जैसे कि पर्याप्त नींद न लेना या खराब खान-पान की वजह से (unhealthy lifestyle)
- - ड्रग्स और अल्कोहल का दुरुपयोग से( Abusing drugs and alcohol)
- -एक लंबी बीमारी के उपचार के बाद (treatment with a chronic disease)
मानसिक बीमारी के लक्षण - Symptoms of Mental Illness
प्रत्येक मानसिक बीमारी के अपने-अपने लक्षण होते हैं। हालांकि, कुछ सामान्य चेतावनी संकेत या लक्षण हैं जो आपको सचेत कर सकते हैं कि आपको किसी को पेशेवर मदद की आवश्यकता है। जैसे कि
- -ज्यादा सोचना (Over thinking)
- -एंग्जायटी और घबराहट (Anxiety)
- - व्यक्तित्व परिवर्तन (marked personality change)
- --खाने या सोने के पैटर्न में बदलाव (changes in eating or sleeping patterns)
- -समस्याओं और दैनिक गतिविधियों को करने में असमर्थता (inability to cope with problems and daily activities)
- -ज्यादा चिंता करना (excessive anxieties)
- -लंबे समय तक अवसाद और उदासीनता (prolonged depression and apathy)
- - ज्यादा गुस्सा करना या हिंसक व्यवहार करना (excessive anger or violent behavior)
- -आत्महत्या के बारे में सोचना या खुद को नुकसान पहुंचाना (thinking or talking about suicide)
- -बहुत ज्यादा मूड स्विंग्स होना (extreme mood swings)
- -शराब या ड्रग्स का दुरुपयोग (abuse of alcohol or drugs)
मानसिक स्वास्थ्य से जुड़ी बीमारियां -Mental Health Disorders
1. एंग्जायटी डिसऑर्डर (anxiety disorders).
एंग्जायटी डिसऑर्डर (Anxiety Disorders) मानसिक बीमारी का सबसे आम प्रकार है। इन स्थितियों वाले लोगों में गंभीर भय या चिंता होती है, जो कुछ वस्तुओं या स्थितियों से संबंधित होती है। एंग्जायटी डिसऑर्डर के प्रकार (Types of Anxiety Disorders) भी हैं, जैसे कि
a. सामान्यीकृत चिंता विकार (Generalized anxiety disorder)
सामान्यीकृत चिंता विकार में लगातार और अत्यधिक चिंता शामिल होती है जो दैनिक गतिविधियों में हस्तक्षेप करती है। यह चल रही चिंता और तनाव शारीरिक लक्षणों के साथ हो सकता है, जैसे कि बेचैनी, किनारे पर महसूस करना या आसानी से थकावट, ध्यान केंद्रित करने में कठिनाई, मांसपेशियों में तनाव या नींद की समस्या।
b. घबराहट की समस्या (Panic Disorder)
पैनिक डिसऑर्डर का मुख्य लक्षण बार-बार होने वाले पैनिक अटैक, शारीरिक और मनोवैज्ञानिक संकट का एक जबरदस्त संयोजन है। इसके कई लक्षण हैं जैसे कि
- -तेज दिल की धड़कन
- -थरथर कांपना या हिलाना
- -सांस की तकलीफ महसूस करना
- -छाती में दर्द
- -चक्कर आना, हल्का-फुल्का या बेहोश होना
- -घुटन का अहसास
- -स्तब्ध हो जाना या झुनझुनी
- -ठंड लगना
- -मतली या पेट में दर्द
- -मरने का डर
c. फोबिया (Phobias)
फोबिया एक विशिष्ट वस्तु, स्थिति या गतिविधि का अत्यधिक और लगातार भय है जो आमतौर पर हानिकारक नहीं होता है। मरीजों को पता है कि उनका डर अत्यधिक है, लेकिन वे इसे दूर नहीं कर सकते।
d. भीड़ से डर लगना (Agoraphobia)
एगोराफोबिया उन स्थितियों में होने का डर है जहां से बचना मुश्किल या शर्मनाक हो सकता है। ये डर वास्तविक स्थिति बहुत परेशान करता है और कामकाज में समस्याएं पैदा करता है। एग्रोफोबिया से पीड़ित व्यक्ति इस डर का अनुभव कई स्थितियों में करता है। जैसे कि
- -सार्वजनिक परिवहन का उपयोग करना
- -खुले स्थानों में होने पर
- - भीड़ वाले स्थानों में होना
- -लाइन में खड़ा होने पर
- -घर के बाहर अकेले रहने पर
e. सोशल एंग्जायटी डिसऑर्डर (Social Anxiety Disorder)
सामाजिक चिंता विकार वाले व्यक्ति को शर्मिंदगी, अपमानित, अस्वीकार किए जाने या सामाजिक संबंधों में कमी देखने के बारे में ज्यादा चिंता और असुविधा होती है। इस विकार वाले लोग स्थिति से बचने के लिए सार्वजनिक स्थानों पर जानें, बोलने, नए लोगों से मिलने और सार्वजनिक रूप से खाने पीने से अत्यधिक डरते हैं।
f. अलगाव की चिंता (Separation Anxiety Disorder)
अलगाव चिंता विकार वाले लोगों को अपने लोगों से बिछड़ने का डर रहता है। ऐसे लोग घर से बाहर जाने या उस व्यक्ति के बिना बाहर जाने से इनकार कर सकते है, या अलगाव के बारे में बुरे सपने का अनुभव कर सकते हैं। ये परेशानी बचपन में विकसित होते हैं, लेकिन लक्षण वयस्क होने के बाद भी रह सकते हैं।
2. मूड डिसऑर्डर (Mood disorders)
मूड डिसऑर्डर को भी भावात्मक विकारों या अवसादग्रस्तता विकारों के रूप में संदर्भित किया जा सकता है। इन स्थितियों वाले लोगों के मनोदशा में बहुत जल्दी बदलाव आता रहता है। इसके भी कई प्रकार होते हैं, जैसे कि
a. मेजर डिप्रेशन (Major depression)
इस अवसाद के साथ एक व्यक्ति लगातार लो फिल करता है और उसका मूड हमेशा खराब रहता है और उन गतिविधियों और घटनाओं में रुचि खो देता है जो पहले से आनंद लेते थे। वे लंबे समय तक निराश या अत्यधिक उदास महसूस करता है।
b. बाइपोलर डिसऑर्डर (Bipolar disorder)
बाइपोलर डिसऑर्डर या द्विध्रुवी विकार वाला व्यक्ति अपने मनोदशा, ऊर्जा के स्तर, गतिविधि के स्तर और दैनिक जीवन को जारी रखने की क्षमता में असामान्य परिवर्तन का अनुभव करता है। अच्छा महसूस करने पर वो बहुत ज्यादा एनर्जेटिक हो जाते हैं, जबकि लो मूड होने पर अवसाद में चले जाते हैं।
c. मौसमी भावात्मक विकार (Seasonal affective disorder )
सर्दियों और शुरुआती वसंत महीनों के दौरान जब दिन का छोटा होता है या ज्यादा अंधेरा होता है, तो ये कुछ लोगों को डिप्रेशन में डाल सकता है। ऐसे लोगों के लिए सबसे ज्यादा जरूरी है एक बेहतर लाइटिंग या सूर्य की रोशनी वाले कमर में रहना।
3. सिजोफ्रेनिया (Schizophrenia disorders)
सिजोफ्रेनिया एक या कई मानसिक बीमारियों का एक समूह है जिसे समझना काफी मुश्किल है। सिजोफ्रेनिया के लक्षण आमतौर पर 16 से 30 साल की उम्र के बीच विकसित होते हैं। ऐसे व्यक्ति के विचार कई बार टूटे हुए और खोए हुए से होते हैं। ये लोग उन चीजों को भी अपने आस पास महसूस करते हैं, जो कि सच में दुनिया में है ही नहीं। सिजोफ्रेनिया के नकारात्मक और सकारात्मक लक्षण हैं। सकारात्मक लक्षणों में भ्रम, विचार विकार और मतिभ्रम शामिल हैं। नकारात्मक लक्षणों में प्रेरणा की कमी और खराब मनोदशा शामिल हैं।
मानसिक स्वास्थ्य को बेहतर बनाने के उपाय- Tips for good mental health
- -दूसरों से जुड़े रहें और अपने आप को अलग न समझें।
- -पॉजिटिव सोचें
- -शारीरिक रूप से सक्रिय रहें।
- -दूसरों की मदद करते रहें।
- -पर्याप्त नींद लें और समय पर सोएं और समय से जागें
- -हेल्दी डाइट लें खास कर मूड को बेहतर बनाने वाली चीजों को खाएं।
- -शराब, धूम्रपान और ड्रग्स से बचें।
- -खूब धूप लें।
- -तनाव ज्यादा न लें।
- -बहुत ज्यादा सोचना बंद करें।
- -एक्सरसाइज और योग करें।
- -ऐसा कुछ करें जिससे आपका मन लगा रहे और आप खुश रहें।
- - मिलनसार बनें।
इस तरह आप मानसिक स्वास्थ्य से जुड़ी सभी परेशानियों, बीमारियों, उनके लक्षण, उपचार और बचाव के लिए एक्सपर्ट टिप्स और जानकारियां यहां पा सकते हैं। तो पढ़ते रहें ऑनली माय हेल्थ का ये खंड 'मानसिक स्वास्थ्य -Mental health in hindi' और अपने मानसिक स्वास्थ्य का रखें खास ख्याल।
Source: American Psychiatric Association
WHO and CDC
https://www.ncbi.nlm.nih.go
Related Articles

टाइट पैंटी पहनने से इंटिमेट हेल्थ पर क्या असर पड़ता है? एक्सपर्ट से समझें

40 साल की उम्र के बाद हर महिला को जरूर करवाने चाहिए ये टेस्ट, समय पर होगा बीमारियों का निदान

किडनी को हेल्दी रखने के लिए डाइट में शामिल करें ये 5 फल

क्या बाईं ओर करवट लेकर सोना हार्ट के लिए नुकसानदायक होता है? डॉक्टर से जानें

वजाइना में असुविधा क्यों महसूस होती है? एक्सपर्ट से जानें कारण

Anteverted Uterus: क्या एंटेवर्टेड गर्भाशय वाली महिलाएं प्रेग्नेंट हो सकती हैं? डॉक्टर से जानें

महिलाओं में अंडे की गुणवत्ता को प्रभावित कर सकते हैं ये 6 कारक, एक्सपर्ट से जानें

गर्मियों में प्रेग्नेंट महिलाएं पिएं ये 5 हेल्दी और टेस्टी स्मूदी, सेहत को मिलेंगे कई फायदे

एक पैर में सुन्नपन क्यों हो जाता है? जानें इसके कारण और बचाव के उपाय

सेहत के लिए फायदेमंद है ये एंटी-इंफ्लेमेटरी डिटॉक्स ड्रिंक, जानें रेसिपी और फायदे
- सामग्री और उपयोग
- घरेलू उपचार
- त्वचा की देखभाल
- बालों की देखभाल
Home » हिंदी » घरेलू उपचार
मानसिक स्वास्थ्य क्या है, लक्षण और उपाय – Mental Health in Hindi
Expertise: विशेषज्ञ- होम रेमेडिज एंड हेल्थ
सरल जैन ने श्री रामानन्दाचार्य संस्कृत विश्वविद्यालय, राजस्थान से संस्कृत ... more
मानसिक स्वास्थ्य का व्यक्ति की दिनचर्या पर काफी असर पड़ता है। जब व्यक्ति मानसिक रूप से स्वस्थ होता है, तो उसका हर काम काफी अच्छे से होता है। लेकिन, मानसिक स्वास्थ्य संबंधी परेशानी होने पर व्यक्ति दिनभर चिड़चिड़ा महसूस कर सकता है। ऐसे में मानसिक समस्याओं से बचाव करना जरूरी है और इसके लिए सबसे पहले यह समझना होगा कि मानसिक स्वास्थ्य क्या है। इसी उद्देश्य के साथ स्टाइलक्रेज इस लेख में मानसिक स्वास्थ्य को प्रभावित करने वाले कारक के साथ ही मानसिक स्वास्थ्य बिगड़ने के लक्षण की जानकारी लेकर आया है।
चलिए, सबसे पहले विस्तार से समझते हैं कि मानसिक स्वास्थ्य क्या है।
मानसिक स्वास्थ्य क्या होता है?
किसी भी व्यक्ति के मानसिक स्वास्थ्य का संबंध उसकी भावनात्मक (इमोशनल), मनोवैज्ञानिक (साइकोलॉजिकल) और सामाजिक (सोशल) स्थिति से जुड़ा होता है। मानसिक स्वास्थ्य से व्यक्ति के सोचने, समझने, महसूस करने और कार्य करने की क्षमता प्रभावित होती है। इसका असर व्यक्ति के तनाव को संभालने और जीवन से जुड़े जरूरी विकल्प के चयन पर भी पड़ सकता है। मानसिक स्वास्थ्य जीवन के प्रत्येक चरण अर्थात बचपन, किशोरावस्था, वयस्कता और बुढ़ापे में महत्वपूर्ण भूमिका निभाता है ( 1 )।
विश्व स्वास्थ्य संगठन (WHO) के अनुसार, मानसिक स्वास्थ्य एक ऐसी स्थिति है, जिसमें व्यक्ति को अपनी क्षमताओं का एहसास होता है। इस स्थिति में व्यक्ति दूसरों के साथ सकारात्मक तरीके से बातचीत कर सकता है। साथ ही तनाव की समस्या से निपटने की क्षमता भी रखता है ( 2 )।
स्क्रॉल करें
अब हम आगे बताएंगे कि मानसिक स्वास्थ्य कितना महत्वपूर्ण है।
मानसिक स्वास्थ्य क्यों महत्वपूर्ण है?
मानसिक स्वास्थ्य महत्वपूर्ण इसलिए है, क्योंकि इसके बिना जीवन के सभी कार्य प्रभावित होते हैं । मानसिक स्वास्थ्य का उद्देश्य यानी मेंटल हेल्थ किन कामों में सहायक भूमिका निभाता है, यह आगे जानिए ( 1 ):
- तनाव से जूझने
- शारीरिक रूप से स्वस्थ रहने
- लोगों से अच्छे संबंध बनाए रखने
- सामाजिक कार्य में योगदान देने
- प्रोडक्टीव काम करने के लिए
- अपनी क्षमता को जानने में
- स्ट्रोक, टाइप 2 मधुमेह और हृदय रोग के जोखिम से बचने के लिए
अब हम कुछ सामान्य मानसिक स्वास्थ्य विकार के बारे में बता रहे हैं।
सामान्य मानसिक स्वास्थ्य विकार – Common Mental health disorders in Hindi
वैसे तो मानसिक स्वास्थ्य विकार कई प्रकार के होते हैं। इनमें से कुछ सामान्य मानसिक स्वास्थ्य के प्रकार में ये शामिल हैं ( 3 ) ( 4 ):
- चिंता (एंग्जायटी) – मानसिक स्वास्थ्य संबंधी एक विकार चिंता भी है। चिंता के कारण वास्तविक या काल्पनिक स्थितियों में अत्यधिक चिंता या भय उत्पन्न हो सकता है।
- अवसाद (डिप्रेशन) – यह मानसिक समस्या सामान्य उदासी या दुख से अलग होती है। इसमें व्यक्ति को काफी दुख, क्रोध, निराश या फ्रस्टेशन हो सकती है।
- बाइपोलर डिसऑर्डर – बाइपोलर विकार को पहले मैनिक डिप्रेशन कहा जाता था। इस समस्या से जूझ रहे व्यक्ति को बारी-बारी से मेनिया (असामान्य रूप से भावनाओं को प्रकट करना) और अवसाद होता है।
- ईटिंग डिसऑर्डर – यह विकार भोजन और शरीर की छवि से संबंधित जुनूनी व्यवहार होता है। इस समस्या में व्यक्ति बहुत कम खाता है या फिर जरूरत से ज्यादा खाने लगता है।
- पोस्ट ट्रॉमेटिक स्ट्रेस डिसऑर्डर – मानसिक स्वास्थ्य संबंधी यह विकार ऐसी घटनाओं के बाद उत्पन्न होता है, जिसकी कभी आशा न की गई हो। इसमें किसी तरह की लड़ाई , किसी अपने की मृत्यु या गंभीर दुर्घटना शामिल है। इस समस्या की चपेट में आने वाला व्यक्ति तनाव और डर महसूस करता है।
- सिजोफ्रेनिया और सायकोटिक विकार – यह एक गंभीर मानसिक रोग है। इसमें लोग ऐसी चीजों को देखने, सुनने और विश्वास करने लगते हैं, जो वास्तविक में हैं ही नहीं।
- अटेंशन डेफिसिट हाइपरएक्टिविटी डिसऑर्डर (एडीएचडी) – यह बच्चों में पाए जाने वाले सबसे आम मानसिक विकारों में से एक है। इस समस्या से जूझ रहे व्यक्ति को अपने व्यवहार को नियंत्रित रखने में परेशानी होती है।
- एडिक्टिव डिसऑर्डर – इस मानसिक समस्या के अंतर्गत व्यक्ति को शराब या ड्रग्स जैसे नशीले पदार्थों की लत लग सकती है। इस लत के कारण व्यक्ति की जान को भी जोखिम हो जाता है।
- पर्सनालिटी डिसऑर्डर – इस स्थिति में व्यक्ति की पर्सनालिटी यानी बिहेवियर में पूरी तरह बदलाव हो जाता है। इससे व्यक्ति के सोचने-समझने, खाने-पीने और सोने के समय में भी बदलाव होता है, जिसका असर व्यक्ति के रिश्तों पर भी पड़ सकता है। इससे व्यक्ति को तनाव होना भी काफी आम हो जाता है ( 5 )।
नीचे जरूरी जानकारी है
इसके बाद आगे पढ़िए बिगड़ते मानसिक स्वास्थ्य के लक्षण क्या-क्या हैं।
बिगड़ते मानसिक स्वास्थ्य के लक्षण- Mental health symptoms in Hindi
यदि किसी को मानसिक स्वास्थ्य से जुड़ी समस्या होती है, तो उनमें इसके लक्षण पहले ही दिखाई देना शुरू हो जाते हैं। मानसिक स्वास्थ्य के लक्षण कुछ इस तरह के हो सकते हैं ( 1 ):
- खाने या सोने की आदतों में बदलाव
- पसंदीद लोगों और गतिविधियों से दूरी बनाना
- ऊर्जा हीन या लो एनर्जी का एहसास होना
- सुन्न महसूस करना जैसे कि कुछ भी मायने नहीं रखता है
- अजीब सा दर्द महसूस होना
- असहाय या निराश महसूस करना
- धूम्रपान, शराब पीना और ड्रग्स का अधिक उपयोग करना
- कन्फ्यूज्ड होना, चीजों को भूलना और गुस्सा आना
- परेशान, चिंतित या डरा हुआ महसूस करना
- मूड स्विंग्स के कारण रिश्तों में दरार पड़ना
- दिमाग में बार-बार उन यादों का आना, जिन्हें भूलना चाह रहे हैं
- ऐसी आवाजें सुनना और बातों पर विश्वास करना जो सच नहीं हैं
- खुद को या दूसरों को नुकसान पहुंचाने की सोच
- दैनिक कार्य को ठीक से न कर पाना
पढ़ना जारी रखें
चलिए, अब पढ़ते हैं मानसिक स्वास्थ्य की स्थिति के कारण क्या-क्या हैं।
मानसिक स्वास्थ्य की स्थिति के कारण और जोखिम कारक- Causes and Risk factors of mental health conditions in Hindi
वैसे तो मानसिक बीमारी के कारण स्पष्ट नहीं हैं। हां, कुछ कारक मानसिक बीमारी के जोखिम उत्पन्न कर सकते हैं। मानसिक स्वास्थ्य को प्रभावित करने वाले कारक में ये शामिल हैं ( 3 ):
- परिवार में पहले किसी को मानसिक समस्या होना
- तनाव और बचपन में हुए दुर्व्यवहार के कारण
- मस्तिष्क में रासायनिक असंतुलन (केमिकल इम्बेलेंस)
- मस्तिष्क की चोट (ब्रेन इंजरी)
- गर्भावस्था के दौरान वायरस और जहरीले रसायनों के संपर्क में आना
- शराब और ड्रग्स का उपयोग
- कैंसर जैसी गंभीर समस्या होना।
- अकेलापन महसूस होना
लेख के अगले हिस्से में मानसिक स्वास्थ्य को बेहतर करने के तरीके जानिए।
मानसिक स्वास्थ्य को कैसे बेहतर बनाए रखें – Home Remedies to cope up with Mental Health in Hindi
मानसिक स्वास्थ्य को बनाए रखने के लिए कई तरीकों को आजमाया जा सकता है। उन तरीकों के बारे में हम नीचे विस्तार से बता रहे हैं।
1. व्यायाम (एक्सरसाइज)
मानसिक स्वास्थ्य के उपाय के तौर पर व्यायाम कर सकते हैं। दरअसल, व्यायाम के दौरान होने वाली शारीरिक गतिविधि से तनाव और अवसाद कम होता है । साथ ही यह मूड में सुधार करने का भी काम कर सकता है। इसलिए, शारीरिक एवं मानसिक स्वास्थ्य के लिए व्यायाम करना जरूरी है ( 6 )।
2. मेडिटेशन
यह मन और शरीर का अभ्यास होता है, जिसे ध्यान केंद्रित करने के लिए किया जाता है। इससे मानसिक स्वास्थ्य बेहतर हो सकता है। मेडिटेशन के कई तरीके होते हैं, जिसे दिनचर्या में शामिल किया जा सकता है। इनमें माइंडफुलनेस मेडिटेशन और ट्रांसेंडेंटल मेडिटेशन भी शामिल हैं। ये दोनों ध्यान करने की तकनीक हैं, जिनके माध्यम से मन को शांत रखा जा सकता है ( 6 )।
3. रिलैक्सेशन तकनीक
रिलैक्सेशन एक्सरसाइज के माध्यम से पूरे शरीर को आराम दिया जा सकता है। इस तकनीक के मदद से रक्तचाप और मांसपेशियों में तनाव व मानसिक तनाव को कम करने में सहायता मिल सकती है। इससे मानसिक स्वास्थ्य भी बेहतर हो सकता है ( 6 )।
4. लिखना (राइटिंग)
कई सारी चीजों को दिमाग में रखने से टेंशन हो सकती है। इससे मानसिक स्वास्थ्य धीरे-धीरे बिगड़ते जाता है। ऐसे में लेखन की मदद से चीजों को दिमाग से निकालने से मन को हल्का महसूस हो सकता है । इससे मूड बेहतर करने में भी सहायता मिल सकती है ( 7 )।
5. टाइम मैनेजमेंट स्ट्रेटेजीज
एनसीबीआई (National Center for Biotechnology Information) की वेबसाइट पर प्रकाशित वैज्ञानिक परीक्षण में मानसिक स्वास्थ्य के लिए टाइम मैनेजमेंट ट्रेनिंग को प्रभावी बताया गया है। टाइम मैनेजमेंट स्ट्रेटेजी चिंता, अवसाद, नींद की गुणवत्ता में सुधार करने के साथ ही नकारात्मक भावनाओं से बचाने का काम कर सकता है। इस ट्रेनिंग के दौरान यह खास ध्यान दिया जाता है कि व्यक्ति का ध्यान परेशान करने वाली बातों में न जाए और उसका दिमाग किसी-न-किसी कार्य में व्यस्त रहे ( 8 )।
6. अरोमाथेरेपी (लैवेंडर तेल)
अरोमाथेरेपी की मदद से मानसिक स्वास्थ्य में सुधार हो सकता है। इस बात की पुष्टि के लिए हुए वैज्ञानिक रिसर्च में दिया है कि लैवेंडर का तेल कई न्यूरोलॉजिकल (मस्तिष्क से संबंधित) विकारों के उपचार में प्रभावी औषधि का काम करता है। इससे चिंता, तनाव और अवसाद सभी को कम किया जा सकता है ( 9 )।
7. कैनाबिडियोल ऑयल
एनसीबीआई की वेबसाइट पर प्रकाशित रिसर्च पेपर से मिली जानकारी के अनुसार, कैनाबिडियोल ऑयल के इस्तेमाल से चिंता की समस्या कम हो सकती है। साथ ही इस तेल के उपयोग से नींद की गुणवत्ता में भी सुधार हो सकता है। इसी वजह से माना जाता है कि मानसिक स्वास्थ्य को बेहतर करने में यह तेल अच्छी भूमिका निभाता है ( 10 )।
8. हर्बल टी (कैमोमाइल टी)
मानसिक स्वास्थ्य में सुधार करने के लिए कैमोमाइल को लेकर कई शोध किए गए है। उन परीक्षणों से पता चलता है कि कैमोमाइल टी में एंटी-डिप्रेसेंट और एंटी एंग्जायटी प्रभाव होते हैं। इन दोनों गतिविधियों के कारण अवसाद और चिंता की समस्या दूर रहती है और मानसिक स्वास्थ्य बेहतर हो सकता है ( 11 )।
9. ओमेगा -3 फैटी एसिड
ओमेगा -3 फैटी एसिड मानसिक स्वास्थ्य के लिए जरूरी होता है । इस बात को प्रमाणित करने के लिए किए गए अध्ययन में दिया हुआ है कि ओमेगा -3 फैटी एसिड अवसाद और सिजोफ्रेनिया की समस्या को कम करने का काम कर सकता है। इससे मानसिक स्वास्थ्य को लाभ मिलता है ( 12 )।
10. माका रूट
माका रूट का उपयोग भी मानसिक स्वास्थ्य को बेहतर बनाए रखने के लिए किया जा सकता है। वैज्ञानिक रिसर्च के अनुसार, माका रूट में एंटी-डिप्रेसेंट गतिविधि होती है। इसके कारण अवसाद से राहत मिल सकती है। साथ ही मूड को बेहतर और चिंता को कम करने में भी यह प्रभावी हो सकता है ( 13 )।
11. वेलेरियन
वेलेरियन एक तरह का औषधीय पौधा है, जिसे मानसिक स्वास्थ्य में सुधार करने के लिए उपयोग किया जा सकता है। दरअसल, नींद ठीक तरह से पूरी न होने से मानसिक स्वास्थ्य पर असर पड़ सकता है। ऐसे में वेलेरियन नींद का समय और गुणवत्ता में सुधार करने का काम कर सकता है ( 14 )। इसी वजह से वेलेरियन को मानसिक स्वास्थ्य के लिए अच्छा माना गया है।
12. दोस्तों और परिवार के सदस्यों के साथ समय बिताना
मानसिक स्वास्थ्य को बेहतर रखने में दोस्तों और परिवार के सदस्यों की भी अहम भूमिका होती है। सोशल सपोर्ट और लोगों से मजबूत रिश्ता होने पर इंसान अपने मन की सारी बातें खुलकर एक दूसरे से एक कर सकता है, जिससे मानसिक स्वास्थ्य बेहतर रह सकता है। साथ ही तनाव, चिंता जैसे मानसिक विकार दूर रहते हैं ( 6 )।
13. पेट्स के साथ समय बिताना
मानसिक स्वास्थ्य के लिए पेट्स थेरेपी को भी आजमाया जा सकता है । एनसीबीआई की वेबसाइट पर पब्लिश वैज्ञानिक रिसर्च के अनुसार, पेट्स मूड को अच्छा करने का काम कर सकते हैं। इससे व्यक्ति को सकारात्मक तरीके से सोचने में भी मदद मिल सकती है ( 15 )।
लेख में बने रहें
आगे जानिए मानसिक स्वास्थ्य का इलाज किस तरह से किया जाता है।
अन्य मानसिक स्वास्थ्य इलाज – Other Mental Health Treatments
मानसिक स्वास्थ्य को बेहतर करने के लिए कुछ इलाज का भी सहारा लिया जा सकता है, जिसमें ये शामिल हैं:
1. मनोचिकित्सा (Psychotherapy)
मानसिक स्वास्थ्य के इलाज के लिए मनोचिकित्सक की मदद लेना एक अच्छा उपाय है। मनोचिकित्सक के द्वारा दी जाने वाली थरेपी से मानसिक स्वास्थ्य में सुधार हो सकता है। इस बात की जानकारी एनसीबीआई की वेबसाइट पर प्रकाशित मेडिकल रिसर्च में भी दी हुई है। व्यक्ति की स्थिति के हिसाब से मनोचिकित्सक इन थेरेपी को अपना सकते हैं ( 16 ) ( 17 ):
- कॉग्निटिव बिहेवियर थेरेपी – इस थेरेपी में व्यक्ति के बर्ताव और भावनाओं को समझा जाता है और उसी के अनुसार समस्या का समाधान किया जाता है।
- सिस्टमिक थेरेपी – इस प्रक्रिया के दौरान डॉक्टर एक सिस्टम तैयार करता है, जिसमें रोगी के परिवार के लोगों को शामिल किया जाता है। उसके बाद किसी स्थिति या फिर धारणाओं के बारे में उन्हें चर्चा करने के लिए कहा जाता है। इस थेरेपी से यह समझा जाता है कि सब लोग आपस में किस तरह से संवाद करते हैं। साथ ही परिवार संबंधी विवाद को भी सुलझाया जाता है।
- पर्सन सेंटर्ड थेरेपी – इस थेरेपी में व्यक्ति के पर्सनल अप्रोच के आधार पर इलाज की प्रक्रिया को निर्धारित किया जाता है।
- चिंता (एंग्जायटी) – इस इलाज की प्रक्रिया के दौरान ब्रेन केमिस्ट्री में बदलाव किया जाता, जिससे कि अवसाद और सायकोटिक लक्षण में सुधार होता है। यह प्रक्रिया गंभीर अवसाद से गुजर रहे लोगों को ही कराने की सलाह दी जाती है।
- ट्रांसक्रेनियल मेग्नेटिक स्टिम्युलेशन – इस थेरेपी के माध्यम से मस्तिष्क के नर्व सेल्स को उत्तेजित किया जाता है, जिससे अवसाद के लक्षण कम हो सकते हैं।
2. मेडिकेशन (दवाइयां)
मानसिक स्वास्थ्य में सुधार करने के लिए कई दवाइयों का भी उपयोग किया जा सकता है। डॉक्टर व्यक्ति की परेशानी को समझकर उसे दवा बताते हैं ( 18 )।
आगे और जानकारी है
अब आप मानसिक स्वास्थ्य के निदान के संबंध में जानेंगे।
मानसिक स्वास्थ्य का निदान – Mental health diagnosis in Hindi
मानसिक स्वास्थ्य के बारे में जानने के लिए डॉक्टर कई तरह के टेस्ट कर सकते हैं। इन परीक्षणों में ये शामिल हैं ( 3 ):
- व्यक्ति की मेडिकल हिस्ट्री – मानसिक स्वास्थ्य के बारे में जानने के लिए डॉक्टर पहले मरीज की मेडिकल हिस्ट्री यानी पुरानी बीमारियों और उसके द्वारा ली जा रही दवाओं की जानकारी लेते हैं।
- शारीरिक परीक्षण और लैब टेस्ट – मेडिकल हिस्ट्री के बारे में जानने के बाद अगर विशेषज्ञ को लगेगा कि किसी बीमारी के कारण मानसिक समस्या हो रही है, तो डॉक्टर शारीरिक परीक्षण कर सकते हैं। उसके बाद जरूरी लैब टेस्ट का सुझाव देते हैं।
- मनोवैज्ञानिक मूल्यांकन (साइकोलॉजिकल इवेलुएशन) – इस निदान के दौरान विशेषज्ञ व्यक्ति से उसकी सोच, भावनाओं और व्यवहार से जुड़े सवाल करते हैं। फिर उन सवालों के जवाब के आधार पर इस नतीजे पर पहुंचते हैं कि व्यक्ति मानसिक समस्या से जूझ रहा है या नहीं।
अंत तक पढ़ें
यहां हम बता रहे हैं कि मेंटल हेल्थ से जूझ रहे व्यक्ति को क्या खाना चाहिए और क्या नहीं।
मानसिक स्वास्थ्य के लिए आहार – Diet while dealing with Mental Health in Hindi
मानसिक स्वास्थ्य पर खानपान का काफी असर पड़ता है। यही वजह है कि मानसिक स्वास्थ्य को बनाए रखने और इससे जुड़ी समस्याओं से निपटने के लिए सही आहार खाना और गलत खानपान से परहेज करना जरूरी है। इन आहार के बारे में हम नीचे दो भाग में जानकारी दे रहे हैं ( 19 )।
क्या खाना चाहिए
- ओमेगा -3 फैटी एसिड से समृद्ध खाद्य पदार्थ, जैसे – मछली और मांस ।
- अमीनो एसिड, मिनरल्स और बी विटामिन्स से भरपूर खाद्य पदार्थ को आहार में शामिल करें। जैसे कि साबुत अनाज, अंडा, दही, बीन्स, हरी पत्ते वाली
- सब्जियां और मकई।
- सभी तरह के फल।
- फोलिक एसिड युक्त खाद्य पदार्थ का सेवन कर सकते हैं ( 16 )। इसके लिए केल (Kale), बीन्स और फलियां जैसे सब्जियां आदि का सेवन कर सकते हैं ( 20 )।
- मस्तिष्क स्वास्थ्य को बेहतर करने के लिए फलियां, पत्तेदार सब्जी, जैतून का तेल (मोनोअनसैचुरेटेड फैट), दही, नट्स का सेवन करना भी अच्छा माना जाता है ( 20 )।
क्या नहीं खाना चाहिए
- फास्ट फूड के सेवन से बचना चाहिए।
- अधिक तले हुए और मसालेदार खाद्य पदार्थ का सेवन न करें।
- शराब और सिगरेट न पिएं ।
- मिठाई, कुकीज, स्नैक्स से परहेज करें।
मानसिक स्वास्थ्य बेहतर रहे, तो ही व्यक्ति अपने सभी कार्य अच्छे तरीके से कर पाता है। इसी वजह से शारीरिक स्वास्थ्य की तरह ही मानसिक स्वास्थ्य पर भी गौर करना जरूरी है। इसमें ऊपर बताए गए टिप्स मदद कर सकते हैं। साथ ही मेंटल हेल्थ बेहतर बनाने के लिए सही आहार को डाइट में जगह दें, जिनका जिक्र लेख में किया गया है। इन सबके अलावा, योग और व्यायाम को भी अपनी दिनचर्या का हिस्सा बनाएं। इससे मानसिक स्वास्थ्य संबंधी समस्या से बचे रहने में मदद मिल सकती है।
अक्सर पूछे जाने वाले सवाल
मानसिक बीमारी के 4 प्रकार कौन-कौन से हैं?
मानसिक स्वास्थ्य के प्रकार चार से ज्यादा हैं, जिसमें चिंता, डिप्रेशन, फोबिया और तनाव को शामिल किया जा सकता है ( 3 )।
बिगड़ते मानसिक स्वास्थ्य के पहले लक्षण क्या हैं?
बिगड़ते मानसिक स्वास्थ्य के पहला लक्षण बेवजह खाने और सोने की आदतों में परिवर्तन होना हो सकता है ( 1 )।
मानसिक स्वास्थ्य के 7 घटक (कॉम्पोनेन्ट) क्या हैं?
मानसिक स्वास्थ्य के 7 घटक में शारीरिक, बौद्धिक, व्यावसायिक, सामाजिक, भावनात्मक, पर्यावरणीय और आध्यात्मिक स्वास्थ्य शामिल हैं।
मैं अपने मानसिक स्वास्थ्य को कैसे सुधार सकता हूं?
आप मानसिक स्वास्थ्य में सुधार लाने के लिए व्यायाम, योग और स्वस्थ खाद्य पदार्थ को दिनचर्या में शामिल कर सकते हैं।
मैं अपने मानसिक स्वास्थ्य का परीक्षण कैसे कर सकता हूं?
मानसिक स्वास्थ्य का परीक्षण करने के लिए मनोचिकित्सक से संपर्क करना होगा। उनकी सलाह पर लैब टेस्ट और व्यवहार परीक्षण होता है, जिससे मानसिक संबंधी समस्या का पता लगता है।
पागलपन किस तरह की बीमारी है?
पागलपन एक तरह की मानसिक बीमारी है, जिसमें व्यक्ति के सोचने और समझने की क्षमता कमजोर हो जाती है।
क्या ओवररिएक्टिंग मानसिक बीमारी है?
ओवररिएक्टिंग मानसिक बीमारी न होकर किसी बीमारी का लक्षण हो सकता है।
क्या मुझे कोई मानसिक बीमारी है या मैं सिर्फ आलसी हूं?
इसमें कोई दो राय नहीं कि मानसिक बीमारी के कारण आलसीपन होता है ( 21 )। लेकिन, आप सिर्फ आलसी हैं या किसी मानसिक बीमारी से जूझ रहे हैं, इसका पता लगाने के लिए डॉक्टर से संपर्क करना जरूरी है।
मानसिक स्वास्थ्य और मानसिक बीमारी के बीच क्या अंतर है?
मानसिक स्वास्थ्य दैनिक जीवन में होने वाले तनाव से निपटने की क्षमता है। वहीं, मानसिक बीमारी की वजह से मानसिक स्वास्थ्य नकारात्मक रूप से प्रभावित होता है।
मानसिक स्वास्थ्य का उद्देश्य क्या है।
मानसिक स्वास्थ्य का उद्देश्य मस्तिष्क को स्वस्थ रखना और इससे जुड़ी समस्याओं को दूर करना है।
Articles on StyleCraze are backed by verified information from peer-reviewed and academic research papers, reputed organizations, research institutions, and medical associations to ensure accuracy and relevance. Read our editorial policy to learn more.
- Mental Health , https://medlineplus.gov/mentalhealth.html
- Mental Health Disorders: The Deserted Illnesses, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5390222/
- Mental Disorders , https://medlineplus.gov/mentaldisorders.html
- Mental Health Screening, https://medlineplus.gov/lab-tests/mental-health-screening/
- Personality Disorders , https://medlineplus.gov/personalitydisorders.html
- How to Improve Mental Health , https://medlineplus.gov/howtoimprovementalhealth.html
- Therapeutic writing, https://www.ncbi.nlm.nih.gov/books/NBK355724/
- Effect of Time Management Training on Anxiety, Depression, and Sleep Quality, https://pubmed.ncbi.nlm.nih.gov/30788296/
- Lavender and the Nervous System, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3612440/
- Medicinal cannabis for psychiatric disorders: a clinically-focused systematic review, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6966847/
- Chamomile (Matricaria recutita) May Have Antidepressant Activity in Anxious Depressed Humans – An Exploratory Study , https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3600408/
- Effects of Omega-3 Fatty Acids on Mental Health: Summary, https://www.ncbi.nlm.nih.gov/books/NBK11853/
- A Double-Blind Placebo-Controlled Trial of Maca Root as Treatment for Antidepressant-Induced Sexual Dysfunction in Women, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4411442/
- Effects of Valerian on Sleep in Healthy Older Adults, https://clinicaltrials.gov/ct2/show/NCT00097604
- Paws for Thought: A Controlled Study Investigating the Benefits of Interacting with a House-Trained Dog on University Students Mood and Anxiety , https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6826684/
- Urgent Need for Improved Mental Health Care and a More Collaborative Model of Care , https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5593510/
- Psychotherapy: A World of Meanings , https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6448000/
- Improving the Quality of Health Care for Mental and Substance-Use Conditions: Quality Chasm Series, https://www.ncbi.nlm.nih.gov/books/NBK19817/
- Food and Mental Health: Relationship between Food and Perceived Stress and Depressive Symptoms among University Students in the United Kingdom, https://www.researchgate.net/publication/265791820_Food_and_Mental_Health_Relationship_between_Food_and_Perceived_Stress_and_Depressive_Symptoms_among_University_Students_in_the_United_Kingdom
- Food, Mood, and Brain Health: Implications for the Modern Clinician, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6170050/
- Public Stigma of Mental Illness in the United States: A Systematic Literature Review, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3835659/
Saral Jain हेल्थ एंड वेलनेस राइटर
35+ best ways to forget someone you love - अपने प्यार को कैसे भूलें | apne pyar ko kaise bhule, 50+ सगाई शायरी - engagement quotes and wishes in hindi, टाइगर नट्स के फायदे और नुकसान - tiger nuts benefits and side effects in hindi, थायराइड के लिए बेहद आसान और फायदेमंद योग - 15 best yoga for thyroid in hindi, संतरे का फेस पैक लगाने के फायदे और बनाने का तरीका – orange face pack in hindi, दही फेस पैक के फायदे और बनाने का तरीका - benefits of curd (dahi) face pack in hindi, ग्रीन टी फेस पैक के फायदे और बनाने का तरीका - benefits of green tea face pack in hindi, काले अंगूर के फायदे और नुकसान – black grapes benefits and side effects in hindi, कब्ज दूर करने के लिए अरंडी के तेल का उपयोग - castor oil for constipation in hindi, काली किशमिश के 7 फायदे और नुकसान - black raisins benefits and side effects in hindi, वजन कम करने के लिए एलोवेरा जूस के फायदे और उपयोग – aloe vera juice for weight loss in hindi, क्या बेकिंग सोडा से पिम्पल्स कम होते हैं – baking soda for acne in hindi.
StyleCraze believes in credibility and giving our readers access to authentic and evidence-based content. Our stringent editorial guidelines allow us to only cite from reputed research institutions, academic journals, and medically established studies. If you discover any discrepancy in our content, you may contact us .

मानसिक स्वास्थ्य
- सजगता का अभ्यास करें
सजगता वह स्थिति है जिसमें हम अपने मस्तिष्क में और हमारे आस-पास चल रही चीजों के बारे में जागरुक रहते हैं लेकिन इसको ले कर कोई प्रतिक्रिया नहीं करते। हर पल को हम पूर्णता के साथ और उसका पूरा उपयोग करते हुए जीते हैं। इसका अभ्यास करने के लिए अपने पूरे ध्यान को ‘इस समय’ या ‘वर्तमान’ पर लगाएं। आपके जेहन से गुजर रहे सभी विचारों को ले कर जागरुक रहें और इन पर कोई फैसला कायम नहीं करें। साक्ष्य बताते हैं कि अगर हम अपने दैनंदिन जीवन में इस सजगता का अभ्यास करें तो भावनात्मक उथल-पुथल लानी वाली घटनाओं से निपट पाने में, अपनी भावनात्मक स्थिति पर नियंत्रण रखने में और चिंता व तनाव संबंधी लक्षणों को कम करने में काफी अधिक सक्षम हो पाते हैं।
- प्रणायाम या सांस संबंधी आसन सीखें
जब कभी तनाव में हों, लंबी और गहरी सांस लें! “सजग श्वसन प्रक्रिया” को आसानी से सीखा जा सकता है। सामान्य गति से सांस लें और अपनी हर आती-जाती सांस के साथ शरीर में होने वाली संवेदना को महसूस करें। प्रणायाम या सजग श्वसन प्रक्रिया पर शोध कर हम अपनी भावनाओं और तनाव पर काबू रख सकते हैं। सजग श्वसन का एक अहम तरीका विकेंद्रीकरण भी है। इसमें हम अपने मस्तिष्क में चल रहे नकारात्मक विचारों को महसूस करना सीखते हैं और उस दौरान हम उसको ले कर कोई निष्कर्ष नहीं निकालते। इस तरह हम नकारात्मक भावों से खुद अपने आप को अलग रख पाने में कामयाब हो पाते हैं।
- ध्यान लगाएं
ध्यान बहुत आसान प्रक्रिया है और इसके लिए सिर्फ कुछ मिनट ही चाहिए होते हैं! इससे शांति मिलती है, नकारात्मक भावनाएं कम होती हैं, तनाव से निपटने की शक्ति मिलती है और सहनशक्ति बढ़ती है। सजग ध्यान में आप अपने शरीर, सांस और विचारों को ले कर सजग रहते हैं, लेकिन कोई नकारात्मक भाव आए तो बिना उससे किसी निष्कर्ष पर पहुंचे ही आगे बढ़ जाते हैं और उसका प्रभाव स्वयं पर नहीं होने देते। ध्यान में आपकी सहायता के लिए ऑनलाइन और ऑफलाइन असंख्य सामग्री उपलब्ध हैं। इस खंड के अंत में भी ऐसे कई स्रोत उपलब्ध करवाए गए हैं।
- समाचार के लिए सिर्फ भरोसेमंद स्रोतों का ही उपयोग करें
कोविड-19 के बारे में सटीक और समय पर जानकारी प्राप्त करना बहुत जरूरी है। लेकिन इसके लिए सेंटर फॉर डिजीज कंट्रोल (सीडीसी), विश्व स्वास्थ्य संगठन (डब्ल्यूएचओ) और स्वास्थ्य मंत्रालय जैसे विश्वस्त सूत्रों की ओर से जारी सलाह पर ही भरोसा करना चाहिए। इस वायरस के बारे में बहुत अधिक खबरें देखने से भय और चिंता की भावनाएं बढ़ सकती हैं। खास तौर पर नवीनतम वैज्ञानिक शोध आदि के बारे में आ रही जानकारी आपके दिन-प्रतिदिन के प्रयोग के लिए प्रासंगिक नहीं होती हैं। समाचार पढ़ने और देखने या सोशल मीडिया पर समय व्यतीत करने की बजाय पढ़ने, संगीत सुनने, दूसरों से बात करने या किसी सकारात्मक गतिविधि में समय लगाएं।
- सोशल मीडिया का सजग उपयोग
हम में से बहुत से लोग सोशल मीडिया पर सूचना साझा करने को ले कर चिंतित रहते हैं, लेकिन झूठी और भ्रामक सूचना हमारे जीवन पर गंभीर प्रभाव डाल सकती है। सोशल मीडिया पर कुछ भी पोस्ट करते समय दो बार सोचें। खुद से पूछें- क्या वह सामग्री सच्ची, लोगों की मदद करने वाली, प्रेरणा देने वाली, आवश्यक या सहृदयतापूर्ण है? कोविड-19 के दौरान सोशल मीडिया के अधिक सजग उपयोग के संबंध में और जानकारी के लिए यहां क्लिक करें ।
- दूसरों के लिए दयालु और उदार रहें
मौजूदा परिस्थिति में अक्सर ऐसा होगा कि लोग अपने और अपने परिवार के लिए ही सोचें। हम खाने-पीने के समान और दवाओं की कमी की आशंका में इन्हें बड़े पैमाने पर जमा करने लगते हैं जिसकी वजह से इनकी कमी हो जाती है। ऐसे मौकों पर खाद्य और आवश्यक सामग्री की उपलब्धता सुनिश्चित करना जरूरी है, लेकिन ऐसे में दूसरे लोगों का भी ध्यान रखें और यह नहीं भूलें कि उन्हें भी इनकी जरूरत हो सकती है। ऐसी उदारता और दया का भाव हमारे अंदर सामुदायिक भाव को जागृत कर सकता है और इससे यह भी सुनिश्चित होगा कि सभी को इन चीजों की समान उपलब्धता हो।
- किसी को कलंकित ना करें और सभी के लिए सहानुभूति रखें
वायरस किसी से भेद-भाव नहीं करता तो फिर हम ऐसा क्यों करें! कोविड-19 के प्रसार के साथ लोगों में जो भय और चिंता का माहौल बना है, उससे कुछ लोगों, स्थानों या समुदायों के बारे में दुर्भावना पैदा हो सकती है। इससे प्रभावित व्यक्तियों के मानसिक स्वास्थ्य पर गंभीर कुपरिणाम हो सकते हैं, अविश्वास का माहौल पैदा हो सकता है और साथ ही इससे संबंधित लोगों को ऐसे किसी मामले के बारे में बताने या जांच करवाने में भय हो सकता है। कलंक के इस भाव से हम निपट सकते हैं, इसके लिए हमें यह समझना होगा कि वायरस सामाजिक वर्ग, नस्ल, समुदाय या राष्ट्रीयता को नहीं देखता। ऐसे मामलों में हमें दूसरे व्यक्ति या समुदाय की जगह खुद को रख कर देखना चाहिए और उन लोगों या समुदायों के प्रति उदारता दिखानी चाहिए। इनके बारे में किसी तरह के भेद-भाव या कट्टरता पैदा करने वाली सूचना को प्रसारित करने से रोकना चाहिए।
कुछ उपयोगी स्रोत
- Center for Disease Control: Mental Health and Coping During COVID-19
- World Health Organization: Mental health and psychosocial considerations during the COVID-19 outbreak
- Minding our minds during COVID 19
- Mental health of children
- Mental health of elderly
- Psychosocial issues among migrants
- Harvard T.H. Chan School of Public Health: Tips for Coping with Stress
- Harvard University Health Services: Managing Fear and Anxiety Around Corona Virus
- Center for Health & Happiness: Harvard T. H. Chan School of Public Health
- Thrive Global: 5 Ways to Manage Your Coronavirus Stress

My Coaching
मानसिक स्वास्थ्य – अर्थ, परिभाषा, स्वरूप, कारण और निवारण, mental health in hindi.

मानसिक स्वास्थ्य का अर्थ Meaning of Mental Health
बालकों में मानसिक स्वास्थ्य से सम्बन्धित व्यवहार की अनेक समस्याएँ देखी जाती हैं। इससे परिवार तथा विद्यालय का वातावरण अव्यवस्थित हो जाता है। जिस बालक का व्यवहार असामान्य है, वह अवश्य ही मानसिक रूप से रुग्ण होगा।
स्वस्थ शरीर में स्वस्थ मस्तिष्क निवास करता है। उदाहरण के लिये, कोई बालक प्रतिभाशाली या बुद्धि का तेज है, किन्तु वह थोड़ी-थोड़ी बात पर झुंझला जाता है तो वह बालक अवश्य ही मानसिक रूप से अस्वस्थ होगा अथवा ऐसा बालक शारीरिक रूप से विक्रत होगा।
मानसिक अस्वस्थता की दशा में कोई बालक सामान्य व्यवहार नहीं करता। न ही वह विभिन्न जटिल परिस्थितियों से समायोजन कर पाता है, जबकि मानसिक रूप से स्वस्थ बालक कठिनतम परिस्थितियों में सामंजस्य स्थापित कर लेता है, कठिन स्थिति में निदान का पथ खोज लेता है तथा उसका मन अध्ययन में लगता है।
मानसिक रूप से अस्वस्थ बालक अपने विद्यालय, साथी तथा शिक्षकों के लिये सिर दर्द बन जाता है। बालक के मानसिक रूप से अस्वस्थ होने के अनेक कारण होते हैं। अत: बालक के मानसिक रूप से अस्वस्थ होने के कारणों का पता लगाकर उनका निदान करना अध्यापक का प्रमुख कार्य होता है।
बाल विकास तथा शिक्षा के विकास के लिये शिक्षक तथा बालक का मानसिक रूप से स्वस्थ रहना शिक्षण प्रक्रिया का प्रथम कार्य है।
राष्ट्रीय मानसिक स्वास्थ्य संगठन , न्यूयार्क के अनुसार, “ मानसिक स्वास्थ्य का अर्थ है कि बालक अपने कार्य में, शाला में, परिवार में, सहयोगियों तथा समुदाय के साथ ठीक प्रकार से रहे। इसका अभिप्राय प्रत्येक व्यक्ति के उस तरीके से हैं, जिसके द्वारा वह अपनी इच्छाओं, महत्त्वाकांक्षाओं, विचारों, भावनाओं और अन्तरात्मा का समन्वय करता है जिससे वह जीवन की उन माँगों को पूरा कर सके, जिनका उसे सामना करना है। ”
मानसिक स्वास्थ्य की परिभाषाएँ Definitions of Mental Health
डॉ. सरयूप्रसाद चौबे के शब्दों में मानसिक स्वास्थ्य की परिभाषा- “ मानसिक रूप से स्वस्थ न रहने पर बालक का विकास कुण्ठित हो जाता है। मानसिक अस्वस्थता के कारण अनेक बालक समाज पर बोझ बने दिखायी देते हैं। इसीलिये हमारे जीवन में मानसिक स्वास्थ्य का महत्त्व शारीरिक स्वास्थ्य से कहीं कम नहीं है। ”
अन्य विद्वानों के अनुसार मानसिक स्वास्थ्य की परिभाषा-
- हेड फील्ड ने कहा है, “सम्पूर्ण व्यक्ति की सम्पूर्ण एवं समन्वित कार्यशीलता को मानसिक स्वास्थ्य कहा जाता है।”
- क्रो एवं क्रो का कथन है, “मानसिक स्वास्थ्य विज्ञान वह विज्ञान है, जिसका सम्बन्ध मानव कल्याण से है और जो मानव सम्बन्धों के सभी क्षेत्रों को प्रभावित करता है।”
- ड्रेवर के शब्दों में, “मानसिक स्वास्थ्य के नियमों की खोज करना और उसके संरक्षण के उपाय करना।”
- लेडेन के अनुसार, “मानसिक स्वास्थ्य का अर्थ है-वास्तविकता के धरातल पर वातावरण से सामंजस्य स्थापित करना।”
मानसिक स्वास्थ्य का स्वरूप Nature of Mental Health
हमारा मुख्य ध्येय बालकों के मानसिक स्वास्थ्य को ठीक बनाये रखना है। अच्छे मानसिक स्वास्थ्य के बिना बालकों की योग्यताओं का उचित विकास सम्भव नहीं है। जिन बालकों में भय, चिन्ता, निराशा तथा अन्य समायोजन दोषों का विकास हो जाता है। उनका मन पढ़ने में नहीं लगता और सीखने में उन्नति नहीं हो पाती।
इसके अतिरिक्त समायोजन दोष वाले बालक अनेक प्रकार की समस्याएँ रखते हैं जिनको समझने और समाधान के लिये प्रत्येक अध्यापक एवं अभिभावक को मानसिक स्वास्थ्य विज्ञान का ज्ञान अति आवश्यक है।
एक समय था जबकि बच्चे की बुद्धि, रुचि एवं मानसिक स्थिति की ओर कोई ध्यान नहीं दिया जाता था। उस समय शिक्षा पूर्णतया अध्यापक केन्द्रित थी और शिक्षा का मुख्य उद्देश्य बच्चों को ‘ थ्री आर ‘ का ज्ञान देना था।
किन्तु अब शिक्षा का केन्द्र बालक बन गया है, उसकी मानसिक स्थति, रुचि एवं अन्य योग्यताओं को आधार मानकर ही पाठ्यक्रम का निर्माण किया जाता है।

मानसिक स्वास्थ्य में बाधक तत्त्व
बालक के मानसिक स्वास्थ्य को जो तत्त्व क्षीण कर देते हैं अथवा प्रभाव डालते हैं, वे निम्न हैं-
1. वंशानुक्रम तत्त्व का प्रभाव
वंशानुक्रम दोषपूर्ण होने के कारण बालक मानसिक दुर्बलता, अस्वस्थता तथा एक विशेष प्रकार की मानसिक अस्वस्थता प्राप्त करता है। अत: वंशानुक्रम प्रभाव का प्रमुख घटक है। इस प्रकार बालक समायोजन करने में कठिनाई का अनुभव करता है।
2. शारीरिक अस्वस्थता का प्रभाव
जो बालक शारीरिक रूप से अस्वस्थ रहते हैं, वे सामान्य जीवन में सामंजस्य स्थापित नहीं कर पाते। अत: शारीरिक अस्वस्थता का घटक मानसिक स्वास्थ्य को प्रभावित करता है। शारीरिक स्वास्थ्य अनुकूल होने की दशा में ही मानसिक स्वास्थ्य ठीक रहता है।
3. शारीरिक दोषों का प्रभाव
बालक के शारीरिक दोष विकलांगता अथवा किसी प्रकार शारीरिक विकृतियाँ बालक के मानसिक स्वास्थ्य को प्रभावित करते हैं। ऐसे बालक हीनता तथा कुण्ठा ओं से ग्रसित होते हैं। इस प्रकार वे समाज से समायोजन नहीं कर पाते।
4. पारिवारिक परिस्थितियों का प्रभाव
इसमें पारिवारिक विघटन, परिवार की अनुशासनहीनता, निर्धनता, संघर्ष , माता-पिता का परस्पर दुर्व्यवहार इत्यादि अनेक घटक आते हैं। इन बाधक तत्त्वों के कारण बालकों का मानसिक स्वास्थ्य ठीक नहीं रहता।
कुछ माता-पिता अपने बालकों को बहुत लाड़-दुलार देते हैं। उन्हें अधिक विलासी साधन उपलब्ध कराते हैं। इससे उनकी मनोवृत्ति असामान्य हो जाती है।
कुछ नौकरी तथा व्यवसाय से अधिक व्यस्त रहने के कारण भली प्रकार ध्यान नहीं दे पाते अथवा बालकों को छात्रावासों में भर्ती कर देते हैं। प्यार के अभाव में भी बालकों का मानसिक स्वास्थ्य बिगड़ जाता है
इन सभी बाधक तत्त्वों के कारण बालक असामान्य हो जाते हैं। इस कारण वे परिस्थितियों से सामंजस्य स्थापित नहीं कर पाते।
5. विद्यालयी वातावरण का प्रभाव
विद्यालयी वातावरण; जैसे-भेद-भाव, छुआछूत, अभिव्यक्ति की स्वतन्त्रता का अभाव, इच्छा, दमन, पाठ्यक्रम-सहगामी क्रियाओं का अभाव, भय,आतंक आदि तत्त्व बालक के मानसिक स्वास्थ्य को खराब करते हैं।
अनुशासन की कठोरता, दोषपूर्ण पाठ्यक्रम, नीरस शिक्षण विधियाँ, अमनोवैज्ञानिक प्रणालियाँ, परीक्षा प्रणाली का दोषपूर्ण होना, पुरस्कार वितरण में भेद-भाव, कक्षा का दूषित वातावरण, जलवायु एवं प्रकाश व्यवस्था का अभाव, छोटी-छोटी त्रुटियों पर भारी दण्ड की व्यवस्था, शिक्षक का नीरस एवं कठोर व्यवहार एवं पक्षपातपूर्ण रवैया आदि बाधक तत्त्व बालक के मानसिक स्वास्थ्य को खराब कर देते हैं एवं उनकी उन्नति में बाधक होते हैं।
बालक की रुचियाँ चूंकि प्रमुख होती हैं अत: रुचि के अनुसार कार्य न देना भी मानसिक स्वास्थ्य की विकृति का प्रतीक है।
6. मनोरंजन तथा सांस्कृतिक क्रिया कलापों के अभाव का प्रभाव
बालक मनोरंजन, जिज्ञासा तथा खेलप्रिय होते हैं। यदि उनको यह साधन उपलब्ध नहीं कराये जाते तो मानसिक रूप से अस्वस्थता का अनुभव करते हैं। वे निराश तथा नीरस हो जाते हैं। उनका मानसिक सन्तुलन बिगड़ जाता है। अत: यह बिन्दु भी विचारणीय हैं।

मानसिक स्वास्थ्य सुधार के उपाय (निराकरण)
बालक के मानसिक रूप से स्वस्थ न रहने के कारण उसके अन्दर असमायोजन उत्पन्न हो जाता है। इससे बालक पर बुरा प्रभाव पड़ता है। वह समायोजन उचित रूप से नहीं कर पाता। उसकी क्षमता में कमी आ जाती है।
छात्र के मानसिक स्वास्थ्य की रक्षा हेतु निम्न उपाय करने चाहिये-
1. शारीरिक स्वास्थ्य पर ध्यान : अच्छे मानसिक स्वास्थ्य के लिये अच्छे शारीरिक स्वास्थ्य का होना भी आवश्यक है। इसलिये बालक को सदैव अपने शारीरिक स्वास्थ्य का ध्यान रखना चाहिये।
2. मानसिक स्वास्थ्य विज्ञान की शिक्षा : प्रत्येक बालक को मानसिक स्वास्थ्य विज्ञान की शिक्षा दी जानी चाहिये। ऐसा करने से वह अपनी कठिनाइयों को समझकर उनका उचित उपचार कर सकेगा, जिससे उसका समायोजन भी ठीक बना रहेगा।
3. आर्थिक कठिनाइयों को दूर करना : बालक में समायोजन का मुख्य कारण उसकी आर्थिक स्थिति होती है। घर की आर्थिक दशा ठीक होने पर ही वह आर्थिक चिन्ता से मुक्त होगा और उसका समायोजन भी अच्छा होगा।
4. उचित मात्रा में गृह तथा कक्षा कार्य प्रदान करना : बालक के मानसिक स्वास्थ्य को ठीक बनाये रखने के लिये उसे विद्यालय में उचित मात्रा में गृह तथा कक्षा कार्य दिया जाय। कार्य की अधिकता एवं कार्य की कमी दोनों ही बालक में असमायोजन उत्पन्न कर देती हैं।
5. भविष्य में व्यवसाय की प्राप्ति : अधिक आयु के बालकों को यह चिन्ता रहती है कि पढ़-लिखकर जब तैयार हो जायेंगे तो हमें नौकरी कहाँ मिलेगी? हम क्या करेंगे? आज के बेरोजगारी के समय यह चिन्ता रहती है। उनको नौकरी या व्यवसाय चयन की चिन्ता न होगी तो वे मन लगाकर विद्याध्ययन करेंगे तथा उनका मानसिक स्वास्थ्य भी अच्छा रहेगा।
6. मनोरंजन की व्यवस्था : बालकों के मनोरंजन की भी उचित व्यवस्था होनी चाहिये। कठिन परिश्रम के कारण बालकों को मानसिक थकान हो जाती है। अत: समायोजन प्रभावित होता है।
7. सदाचरण वाले मित्र बनाना : बालकों को चरित्रवान एवं विश्वास पात्र मित्र बनाने चाहिये, ताकि संकट के समय वे काम आ सकें। अच्छे मित्रों के अभाव में आपत्ति के समय मानसिक सन्तुलन बिगड़ जाता है।
8. शिक्षण सामग्री की सुविधा : बालकों को अध्ययन हेतु पर्याप्त मात्रा में शिक्षण सामग्री उपलब्ध होनी चाहिये।
9. विद्यालय का वातावरण : विद्यालय में सहयोग एवं सहानुभूति का वातावरण होना चाहिये। छात्रों, अध्यापकों तथा प्रधानाध्यापक आदि के बीच तनाव नहीं होना चाहिये।
10. छात्र संघ की स्थापना : बालकों का मानसिक स्वास्थ्य प्राय: दोषपूर्ण शिक्षा प्रणाली, बेरोजगारी एवं तानाशाही रवैया के कारण खराब हो जाता है। अत: इन समस्त कारणों के निवारण हेतु छात्र संघों की प्रान्तीय एवं राष्ट्रीय स्तर पर स्थापना होनी चाहिये। इससे छात्रों का मानसिक स्वास्थ्य ठीक रहेगा।
घर, विद्यालय और समाज का मानसिक स्वास्थ्य सुधार में योगदान
बालक के सुधार तथा परिवर्तन में घर, विद्यालय तथा समाज की प्रमुख भूमिका रहती है। समाज तथा विद्यालय उसके विकास को प्रभावित करते हैं। बालक इन संस्थाओं से प्रत्यक्ष रूप से सम्बन्धित रहता है। अत: ये उसके विकास को किसी न किसी रूप में प्रभावित करती रहती हैं।
घर का मानसिक स्वास्थ्य सुधार में योगदान
विद्यालय का मानसिक स्वास्थ्य सुधार में योगदान, समाज या समूह का मानसिक स्वास्थ्य सुधार में योगदान.
तीनों स्थानों में जो मानसिक स्वास्थ्य में योगदान होता है उसका वर्णन नीचे है-
घर में मानसिक स्वास्थ्य सबसे अधिक प्रभावित होता है। यदि घर का वातावरण अच्छा है तो घर में मानसिक स्वास्थ्य शीघ्र ही अच्छा हो जाता है। घर बालक के मानसिक स्वास्थ्य सुधार में निम्नलिखित योगदान करते हैं-
1. घर का प्रभाव
बालक घर में जन्म लेता है और उसका विकास भी घर में ही होता है। अत: घर का वातावरण बालक को सबसे अधिक प्रभावित करता है।
2. शान्तिमय वातावरण
जिन घरों का वातावरण शान्तिमय तथा कलह से मुक्त होता है वहाँ बालकों का संवेगात्मक विकास भी स्वाभाविक रूप में होता है। कलहयुक्त वातावरण में पले बालक झगड़ालू तथा संवेगात्मक दृष्टि से अस्थिर होते हैं।
3. भाषा का विकास
बालक बोलचाल का प्रशिक्षण घर से ही सीखता है। माता -पिता की भाषा बालको को सबसे अधिक प्रभावित करती है।
4. माता-पिता का व्यवहार
माता-पिता का बालकों के प्रति व्यवहार भी उनके विकास को प्रभावित करता है। यदि माता-पिता अपने सभी बालकों को समान दृष्टि से प्यार करते हैं, तो बालकों का मानसिक विकास भी ठीक प्रकार से होगा।
इसके विपरीत पक्षपातपूर्ण व्यवहार बालकों में द्वन्द्व उत्पन्न करता है। जो माता-पिता किसी विशेष बालक पर लाड़-प्यार अधिक करते हैं, उसके बिगड़ने की अधिक सम्भावना रहती है।
5. सदस्यों का व्यवहार
परिवार के सदस्यों का परस्पर व्यवहार भी बालक के व्यवहार को प्रभावित करता है। जिन परिवारों के सदस्य शिष्ट तथा नियम से जीवन व्यतीत करने वाले होते हैं, वहाँ बालक भी शिष्ट व्यवहार करने वाले तथा नियमबद्ध जीवन व्यतीत करने वाले होते हैं।
6. आर्थिक दशा
परिवार की आर्थिक दशा भी बालकों के विकास को प्रभावित करती है। जिन परिवारों की आर्थिक दशा अच्छी होती है, वहाँ बालकों को पर्याप्त पौष्टिक भोजन मिलता है। अत: इनका शारीरिक विकास भी उचित दशा में होता है।
परन्तु आवश्यकता से अधिक गरिष्ठ भोजन बालकों के स्वास्थ्य पर बुरा प्रभाव डालता है। प्रायः अमीरों के बालक इसी कारण पेट के रोगी होते हैं। दूसरी ओर निर्धन परिवारों के बालक धनाभाव के कारण पौष्टिक भोजन प्राप्त नहीं कर पाते।
अत: उनका शारीरिक विकास भी ठीक प्रकार से नहीं हो पाता। धनाभाव के कारण निर्धन परिवार के बालकों की शैक्षिक आवश्यकताओं की पूर्ति नहीं हो पाती। अत: वे कक्षा में भी पढ़ने से पिछड़ जाते हैं।
7. सामान्य बुद्धि का विकास
जिन परिवारों में अच्छी पुस्तकें होती हैं तथा अच्छी पत्रिकाएँ आती हैं, वहाँ के बालकों की सामान्य बुद्धि का विकास तीव्रता से होता है।
8. अनुशासन का प्रशिक्षण
जिन परिवारों में अनुशासन की भावना आवश्यकता से अधिक कठोर होती है तथा माता-पिता बात-बात पर बालकों को कठोर दण्ड देते हैं, वहाँ के बालक विद्रोही होते हैं या चोरी छिपे अपराध करने लगते हैं। उनके मस्तिष्क में एक प्रकार की विकृति उत्पन्न हो जाती है।
घर के वातावरण में सुधार के सुझाव
घर के वातावरण में मानसिक स्वास्थ्य सुधार के सुझाव निम्न हैं-
- घर का वातावरण पूर्णतया, शान्तिमय होना चाहिये। बात-बात पर माता-पिता को लड़ना-झगड़ना नहीं चाहिये।
- अभिभावकों को लालन पालन करने का प्रशिक्षण लेना चाहिये।
- बालकों की विभिन्न शैक्षिक आवश्यकताओं की पूर्ति की जाय।
- बालकों के साथ मनोवैज्ञानिक व्यवहार किया जाय तथा उन्हें बात-बात में डाँटना-डपटना नहीं चाहिये।
- निर्धन परिवार के बालकों को सरकार द्वारा पर्याप्त आर्थिक सहायता प्रदानकी जाय।
- अभिभावकों का कर्तव्य है कि वे अपने बालकों को खेलने-कूदने की स्वतन्त्रता दें।
- परिवार के समस्त सदस्यों का आचरण नैतिकतापूर्ण होना चाहिये।
विद्यालय बालक के मानसिक स्वास्थ्य सुधार में निम्नलिखित योगदान करते हैं-
- विद्यालय बालक के लिये स्वास्थ्यप्रद और शिक्षाप्रद वातावरण प्रदान करते हैं। इस प्रकार के वातावरण में उनका शारीरिक विकास और मानसिक विकास उचित प्रकार से होता है।
- विद्यालय बालकों को विभिन्न सामाजिक गतिविधियों में भाग लेने का अवसर प्रदान करते हैं, इस प्रकार उनमें सामाजिकता का विकास करते हैं।
- जिन बालकों के घर का वातावरण शैक्षिक नहीं होता, वे बालक विद्यालय में इस अभाव की पूर्ति कर लेते हैं।
- वाद-विवाद, कविता प्रतियोगिता तथा अन्य साहित्यिक गतिविधियों में भाग लेकर बालक अपना साहित्यिक विकास करते हैं।
- विद्यालय सामूहिक खेल-कूद तथा व्यायाम-शालाओं का आयोजन करके छात्रों के शारीरिक विकास में एक महत्त्वपूर्ण योग प्रदान करते हैं।
- विद्यालयों में बालकों की रचनात्मक शक्ति तथा प्रतिभा का विकास होता है।
- स्वशासन जैसी योजनाओं में भाग लेकर बालक प्रजातन्त्र का पाठ सीखते हैं।
- बुनियादी विद्यालय बालकों को विभिन्न प्रकार के हस्त-शिल्प का प्रशिक्षण देकर व्यावसायिक क्षमताओं का विकास करते हैं।
समूह एक प्रकार से समाज की इकाई होती है। बालक किसी न किसी समूह के सदस्य होते हैं और उसके प्रति निष्ठावान होते हैं। बालकों के खेलने-कूदने की विभिन्न क्रियाएँ समूह में ही होती हैं। ऐसी दशा में बालक का समूह द्वारा प्रभावित होना स्वाभाविक हो जाता है। अत: समूह बालक के विकास को अवश्य प्रभावित करता है। समाज बालक में सामाजिकता की भावना का विकास करता है।
बालक के मानसिक स्वास्थ्य सुधार में समाज या समूह के योगदान निम्न प्रकार से होता है-
- समाज में रहकर बालक परस्पर सहयोग और सहकारिता की भावना सीखते हैं तथा नेतृत्व की भावना का जन्म होता है।
- समाज बालकों को संगठन और नेतृत्व का प्रशिक्षण देता है।
- यदि समाज के सदस्य दुराचारी और भ्रष्ट हैं तो अच्छे बालक भी भ्रष्ट और दुसचारी हो जाते हैं।
- समाज बालकों में प्रतियोगिता की भावना उत्पन्न करता है। वह प्रतियोगिता अच्छी भी हो सकती है और बुरी भी।
- बुद्धिमान मित्रों के समूह में बालक का मानसिक विकास होता है।
- समाज में न रहने पर बालक एकान्तप्रिय तथा असामाजिक हो जाता है।
- समाज में रहकर बालक अपनी रुचियों, क्षमताओं तथा योग्यताओं का विकास कर लेता है।
मानसिक स्वास्थ्य क्या है? मानसिक स्वास्थ्य का अर्थ है कि व्यक्ति अपने कार्य में, शाला में, परिवार में, सहयोगियों तथा समुदाय के साथ ठीक प्रकार से रहना। मानसिक रूप से स्वस्थ न रहने पर व्यक्ति का विकास कुण्ठित हो जाता है। मानसिक अस्वस्थता के कारण अनेक व्यक्ति समाज पर बोझ बने दिखायी देते हैं। इसीलिये हमारे जीवन में मानसिक स्वास्थ्य का महत्त्व शारीरिक स्वास्थ्य से कहीं कम नहीं है।
कुछ सामान्य मानसिक स्वास्थ्य विकार क्या हैं? कुछ सामान्य मानसिक स्वास्थ्य विकारों में चिंता विकार, अवसाद, द्विध्रुवी विकार, सिज़ोफ्रेनिया, खाने के विकार और व्यक्तित्व विकार आदि शामिल हैं।
खराब मानसिक स्वास्थ्य के कुछ लक्षण क्या हैं? विकार के आधार पर खराब मानसिक स्वास्थ्य के लक्षण अलग-अलग हो सकते हैं, लेकिन इसमें उदासी या निराशा की भावना, भूख या नींद न आना , ऊर्जा या प्रेरणा की कमी, ध्यान केंद्रित करने में कठिनाई, या खुद को नुकसान पहुंचाने या आत्महत्या करने के विचार शामिल हो सकते हैं।
मानसिक स्वास्थ्य को बेहतर बनाने के कुछ तरीके क्या हैं? मानसिक स्वास्थ्य को बेहतर बनाने के कुछ तरीकों में पर्याप्त नींद लेना, संतुलित आहार खाना, नियमित शारीरिक गतिविधि में शामिल होना, तनाव प्रबंधन तकनीकों जैसे ध्यान या ध्यान का अभ्यास करना और जरूरत पड़ने पर मानसिक स्वास्थ्य सलाहकार से सहायता लेना शामिल है।
मानसिक स्वास्थ्य के संबंध में लांछन क्या है? लांछन मानसिक बीमारी के आसपास के नकारात्मक दृष्टिकोणों और विश्वासों को संदर्भित करता है जो भेदभाव, पूर्वाग्रह और सामाजिक बहिष्कार का कारण बन सकता है। लांछन व्यक्तियों के लिए सहायता प्राप्त करना कठिन बना सकता है और शर्म और शर्मिंदगी की भावनाओं में योगदान कर सकता है।
मैं मानसिक स्वास्थ्य विकार वाले किसी व्यक्ति की सहायता कैसे कर सकता हूँ? आप समझदार और गैर-न्यायिक बनकर मानसिक स्वास्थ्य विकार वाले किसी व्यक्ति का समर्थन कर सकते हैं, सुनने की पेशकश कर सकते हैं और भावनात्मक समर्थन प्रदान कर सकते हैं, उन्हें पेशेवर मदद लेने के लिए प्रोत्साहित कर सकते हैं, और उन्हें अपने समुदाय में संसाधनों और सहायता समूहों को खोजने में मदद कर सकते हैं।
मुझे अपने मानसिक स्वास्थ्य के लिए सलाहकार से मदद कब लेनी चाहिए? यदि आप मानसिक स्वास्थ्य विकार के लगातार या गंभीर लक्षणों का अनुभव कर रहे हैं, यदि आपके लक्षण आपके दैनिक जीवन या रिश्तों में हस्तक्षेप कर रहे हैं, या यदि आपके मन में खुद को नुकसान पहुंचाने या आत्महत्या करने के विचार आ रहे हैं, तो आपको अपने मानसिक स्वास्थ्य सलाहकार से मदद लेनी चाहिए।
- मानसिक स्वास्थ्य
You may like these posts
विषय-वस्तु विश्लेषण के सिद्धांत, शिक्षण बिन्दुओं का निर्धारण.
विषय-वस्तु विश्लेषण के सिद्धान्त (Principles of Contents Matter Analysis) विषय-वस्तु का निर्माण करते समय सामान्यतया शिक्षक, शिक्षार्थी से सम्बन्धित मनोवैज्ञानिक, दार्शनिक, सामाजिक एवं राष्ट्रीय दृष्टिकोण को ध्यान में रखना आवश्यक... Read more !
अपेक्षित अधिगम स्तर (Expected Learning Outcome) – शिक्षा शास्त्र
अपेक्षित अधिगम स्तर की संकल्पना Concept of Expected Learning Outcome राष्ट्रीय शिक्षा नीति, 1986 की संस्तुति के अनुसार विद्यालयीन शिक्षा के प्रत्येक स्तर हेतु अधिगम के न्यूनतम स्तर निर्धारित किये... Read more !
समुदाय या वातावरण का बालक के अधिगम या विकास में योगदान
समुदाय या वातावरण का बालक के अधिगम या विकास में योगदान– अधिगम को प्रभावित करने वाले वातावरण से सम्बन्धित कारक अथवा बालक के अधिगम या विकास में समुदाय का योगदान... Read more !
माई कोचिंग डॉट इन ने आपके ब्राउज़र में जावास्क्रिप्ट अवरोधक का पता लगाया है। कृपया साइट की सामग्री देखने के लिए जावास्क्रिप्ट सक्षम करें।
We have detected the javascript blocker in your browser. Please enable javacript to visit content of site.
धन्यवाद

- Submit Your Post
- English ( English )
- हिन्दी ( हिन्दी )
मानसिक स्वास्थ्य में सुधार कैसे करे
Mental Health in Hindi: आपका मानसिक स्वास्थ्य आपके सम्पूर्ण स्वास्थ्य का एक महत्वपूर्ण पहलू है। वास्तव में, यह आपके शारीरिक स्वास्थ्य जितना ही महत्वपूर्ण है। आपका मानसिक स्वास्थ्य डिप्रेशन जैसी चिकित्सीय स्थितियों से प्रभावित हो सकता है। आपका भावनात्मक स्वास्थ्य आपके सामाजिक जीवन, आपके रोमांटिक जीवन और आपकी अपनी मानसिकता से संबंधित हो सकता है। आपकी स्थिति कैसी भी हो, आप अपने मानसिक और भावनात्मक स्वास्थ्य को और बेहतर बना सकते हैं। सबसे पहले अपनी मानसिक स्वास्थ्य (Mental health in Hindi) को प्राथमिकता दें। आप अपने परिवार और दोस्तों से भी बेहतर मानसिक स्वास्थ्य की दिशा में आपकी मदद करने के लिए कह सकते हैं।
Table of Contents
- 1.1 1. खुद को महत्व दें
- 1.2 2. अपने मानसिक स्वास्थ्य को प्राथमिकता बनाए
- 1.3 3. अपने सामने एक लक्ष्य रखो
- 1.4 4. अपनी भावनाओं को संसाधित करें
- 1.5 5. स्वस्थ गतिविधियों का चयन
- 1.6 6. स्वस्थ आहार लें
- 1.7 7. पर्याप्त नींद ले
- 1.8 8. दोस्तों और परिवार से बात करें
- 1.9 9. अपनी नियमित दिनचर्या बदलें
- 1.10 10. अपने वर्तमान समय में रहे
मानसिक स्वास्थ्य में सुधार के उपाय – Ways to Improve Mental Health in Hindi
मानसिक स्वास्थ्य होने का मतलब है कि दैनिक जीवन के दौरान कार्य करने में सक्षम होना और मौका मिलने पर चुनौतियों से निपटने के लिए आत्मविश्वास महसूस करना। जो लोग भावनात्मक रूप से स्वस्थ होते हैं वे अक्सर अपनी भावनाओं, व्यवहार, यहां तक कि शारीरिक स्वास्थ्य के नियंत्रण में होते हैं।
निचे दिए गए तरीकों से आप अपने मानसिक स्वास्थ्य में सुधार कर सकते हैं –
1. खुद को महत्व दें
अच्छे मानसिक स्वास्थ्य (Mental health in Hindi) के अच्छी तरह कार्य करने के लिए स्वयं के मूल्य को स्वीकार करना आवश्यक है। यह आपको अपनी ताकत और कमजोरियों का आकलन करने में मदद करेगा, और आपको उन्हें प्रभावी ढंग से संतुलित करने की क्षमता प्रदान करेगा। अपने आप को सम्मान और दया के साथ व्यवहार करें, और आत्म-आलोचना से बचें।
2. अपने मानसिक स्वास्थ्य को प्राथमिकता बनाए
अपनी प्राथमिकताओं को सूची तैयार करें। क्या आपके जीवन के ऐसे क्षेत्र हैं जहाँ आप जानते हैं कि आप सुधार कर सकते हैं? अपना कुछ समय यह पता लगाने में भी लगाएं कि इनमें से कौन सा क्षेत्र या कार्य आपके लिए सबसे महत्वपूर्ण है। उदाहरण के लिए , आपकी प्राथमिकताओं में से एक आपके किसी के साथ अधिक सकारात्मक संबंध विकसित करना भी हो सकता है।
एक प्राथमिकता यह भी हो सकती है कि कैसे एक कार्य जीवन में संतुलन बनाए, एक अच्छा स्वास्थ्य, रिश्तों में संतुलन और कैसे एक संतोषजनक आध्यात्मिक जीवन बनाए रखा जाए।
3. अपने सामने एक लक्ष्य रखो
अपना कुछ लक्ष्य रखो जीवन में जिसे आप पूरा करना चाहते हो । ये लॉन्ग टर्म और शॉर्ट टर्म दोनों तरह के लक्ष्य हो सकते हैं। उदाहरण के लिए, जैसे कि आप प्रतिदिन 10 मिनट ध्यान करने का लक्ष्य निर्धारित कर सकते हैं। यह एक शॉर्ट टर्म लक्ष्य है। अपने लक्ष्यों को लिखें। इससे आपको उन्हें मजबूत करने में मदद मिलेगी और आपको प्रतिबद्ध होने की अधिक संभावना होगी।
4. अपनी भावनाओं को संसाधित करें
अपनी भावनात्मक भलाई में सुधार करने का एक महत्वपूर्ण हिस्सा अपनी भावनाओं को स्वीकार करना सीख रहा है। कभी-कभी असहज भावना को दूर करना आसान लग सकता है। हालांकि, अपनी भावनाओं को संसाधित करना महत्वपूर्ण है। अपनी भावनाओं को संसाधित करना एक बहु-चरणीय प्रक्रिया है।
इसमें शामिल है –
- संवेदना: यह तब होती है जब आप कुछ महसूस कर रहे होते हैं उसे नोटिस करते हैं। इस भावना से जुड़ी कोई शारीरिक अनुभूति हो सकती है। उदाहरण के लिए, आप उदास महसूस कर सकते हैं और अपने सीने में भारीपन या जकड़न महसूस कर सकते हैं।
अपने ट्रिगर्स को पहचानने और उनसे निपटने का तरीका जानें। हर किसी के अलग-अलग ट्रिगर होते हैं। इन ट्रिगर्स में कुछ निश्चित लोग, परिस्थितियाँ या स्थान भी हो सकते हैं। अपने ट्रिगर्स से निपटने के लिए, यह पता लगाने के लिए कुछ समय लें कि वे क्या हैं और उनसे निपटने के लिए योजनाएँ बनाये।
- जानकारी इकट्ठा करें: इस चीज से बचें कि मानसिक स्वास्थ्य (Mental health in Hindi) के मुद्दे किसी भी तरह “वास्तविक” समस्याएं नहीं हैं। आपका मानसिक और भावनात्मक स्वास्थ्य उतना ही महत्वपूर्ण है जितना कि आपका शारीरिक स्वास्थ्य। अपने मानसिक स्वास्थ्य के महत्व के बारे में जानने के लिए कुछ समय निकालें।
अपनी भावनात्मक भलाई को बेहतर बनाने के लिए विभिन्न तरीकों पर शोध करें। उदाहरण के लिए, आप किसी योग क्लास में जाकर उनसे योग का अभ्यास करने के मानसिक लाभों के बारे में पूछ सकते हैं।
5. स्वस्थ गतिविधियों का चयन
- रचनात्मक (क्रिएटिव) बनो: अपने अंदर के कलाकार को पहचानिये। कलात्मक पक्ष से संपर्क करने का प्रयास करें। रचनात्मक गतिविधियाँ मानसिक स्वास्थ के लिए बहुत लाभदायक होती हैं, और मूड बूस्टर के रूप में भी काम कर सकती हैं। उदाहरण के लिए, स्केचिंग। संगीत सुनें या एक वाद्य बजाना सीखें। आप एक समूह कक्षा ढूंढ सकते हैं या एक व्यक्तिगत शिक्षक को नियुक्त कर सकते हैं।
- दूसरों की मदद करे: दूसरों की मदद करना खुद को अच्छा महसूस कराने का एक शानदार तरीका है। यह आपके मूड को बढ़ावा दे सकता है और आपके भावनात्मक स्वास्थ्य में सुधार कर सकता है।
- बाहर समय बिताएं: प्रकृति हमारी प्राकृतिक मनोदशा को बढ़ावा देती है। बाहर समय बिताने से आप अच्छा महसूस करेंगे, जो आपके मानसिक स्वास्थ्य के लिए बहुत अच्छा है। प्रकृति के साथ समय बिताए।
- काम से ब्रेक लें: समय समय पर काम से ब्रेक ले कर बाहर घूमने जाये। यह आपके मूड को अच्छा करता है साथ ही साथ मानसिक स्वास्थ्य को भी बूस्ट करने में भी मदद होती है।
- ध्यान करना सीखें: ध्यान चिंता और तनाव को कम करने का एक अचूक तरीका है। ध्यान को प्रतिदिन अपनी दिनचर्या में शामिल करने का संकल्प लें। यदि आप इसे रोजाना करने में असमर्थ है , तो सप्ताह में दो से तीन दिन के लिए जरूर करें। आप कम समय से भी शुरुवात कर सकते हैं – 5 से 10 मिनट का ध्यान भी सहायक होता है। इसमें आप “ओम” मंत्र का जाप भी कर सकते हैं।
ध्यान करने के लिए सुबह और रात दोनों ही समय आप चुन सकते हैं। बस एक शांत जगह चुनना और आरामदायक कपड़े पहनना सुनिश्चित करें। अपनी सांस पर ध्यान दें। अपनी नाक से और अपने मुंह से धीरे-धीरे और जानबूझकर सांस लें। यह अक्सर तनाव के कारण होने वाली हृदय गति को धीमा करने में मदद करेगा।
पढ़े: ध्यान के फायदे
- व्यायाम : शारीरिक गतिविधि एंडोर्फिन पैदा करती है, जो आपके मूड को बूस्ट करती है। नियमित व्यायाम आपके तनाव को प्रबंधित करने, अधिक आत्मविश्वास महसूस करने और आपके स्वास्थ्य में सुधार करने में मदद करता है। सप्ताह के अधिकांश दिनों में कम से कम 30 मिनट का व्यायाम करने का प्रयास करें। शारीरिक गतिविधियां मस्तिष्क को ऑक्सीजन प्रदान करती हैं, जिससे यह डिप्रेशन और तनाव को कम करने में मदद करता है।
एक ऐसी गतिविधि चुने जिसमे आपकी रूचि हो। उदारण के लिए, अगर आपको डांस पसंद है तो आप ज़ुम्बा क्लास ट्राई करें।
6. स्वस्थ आहार लें
भोजन निश्चित रूप से आपके मूड और आपके संपूर्ण मानसिक स्वास्थ्य (Mental health in Hindi) को प्रभावित करता है। इसलिए अपने आहार का चयन सही से करे। हर दिन खूब सारे फल और सब्जियां खाएं। कुछ खाद्य पदार्थ मूड बूस्टर हैं। अपने आहार में सैल्मन, अखरोट और एवोकाडो को शामिल करने का प्रयास करें।
- आपको ब्लूबेरी और पत्तेदार सब्जियों का भी इस्तेमाल कर सकते हैं।
- ऐसे खाद्य पदार्थों से बचें जो आपके मूड को नकारात्मक रूप से प्रभावित कर सकते हैं। मीठे स्नैक्स और तले हुए भोजन से दूर रहने की कोशिश करें।
- शराब का सेवन करने से बचे।
- ज्यादा से ज्यादा पानी पिए।
- कम से कम 10 मिनट सुबह – सुबह धुप में बैठे।
7. पर्याप्त नींद ले
यदि आपको पर्याप्त आराम नहीं मिलता है तो आप अच्छा महसूस नहीं करेंगे। रात की अच्छी नींद को प्राथमिकता दें। अधिकांश वयस्कों को रोजाना सात से नौ घंटे के बीच की नींद की आवश्यकता होती है। हर दिन एक ही समय पर सोने और उठने की कोशिश करें। यह आपके शरीर को नियमित नींद के समय में समायोजित करने में मदद करेगा।
सोने से पहले इलेक्ट्रॉनिक्स सीमित करें। सोने से लगभग एक घंटे पहले लैपटॉप और टेलीविजन को बंद कर दें। देर रात तक ई-मेल या सोशल मीडिया चेक करने से बचें। नींद की कमी आपको चिड़चिड़ी, चिंतित और ध्यान केंद्रित करने में असमर्थ बनाती है।
8. दोस्तों और परिवार से बात करें
अपने जीवन में उन लोगों से जुड़े जो आपके लिए महत्वपूर्ण हैं। जब आप किसी क्षेत्र में फेल होते हैं तो आपके प्रियजन आपका समर्थन कर सकते हैं, और कुछ अच्छा होने पर आप के साथ जश्न मना सकते हैं। किसी ऐसे व्यक्ति से संपर्क करें जिसे आपने कुछ समय से नहीं देखा है। जरूरत पड़ने पर प्रियजनों के सामने झुक जाएं। खुल कर उनसे बातें करे।
9. अपनी नियमित दिनचर्या बदलें
यदि आप गतिरोध से जूझ रहे हैं, तो दैनिक दिनचर्या में कुछ छोटे-छोटे बदलाव करें, जैसे नाश्ते के लिए कुछ नया, कार्यस्थल के लिए एक नया रास्ता बदलना, टीवी देखने के बजाय एक नई किताब पढ़ना आदि। वहां छोटी चीजें आपके वर्तमान जीवन में बहुत अधिक उत्तेजना और आवश्यक विविधता जोड़ सकती हैं, कौन जानता है, वे कुछ बड़े बदलाव भी ला सकते हैं।
10. अपने वर्तमान समय में रहे
बहुत से लोग वर्तमान का अनुभव करने के बजाय या तो अतीत के बारे में सोचते है या भविष्य की योजना बनाने में खोये रहते है। भावनाओं और विचारों, शरीर और आसपास की दुनिया से युक्त वर्तमान समय के बारे में अधिक ध्यान दें। कुछ लोग इस जागरूकता को “माइंडफुलनेस” नाम देते हैं।
डॉक्टर की सलाह ले: कभी-कभी आपको ऐसा महसूस हो सकता है कि आप जो कोशिश कर रहे हैं वह काम नहीं कर रहा है। अगर आपको लगता है कि आपको मानसिक स्वास्थ्य (Mental health in Hindi) की स्थिति ठीक नहीं है , तो एक चिकित्सकीय पेशेवर से परामर्श लेने पर विचार करें। उदाहरण के लिए,
यदि आप चिंता या डिप्रेशन से झूज रहे हैं तो थेरेपी वास्तव में मददगार हो सकती है।
अन्य उपयोगी लेख : एप्रीकॉट फ्रूट के फायदे
अलसी के फायदे
गिलोय के फायदे
आंवला के फायदे
चिंता के लक्षण
मानसिक स्वास्थ्य में सुधार कैसे करे
डिप्रेशन के लक्षण और उपाय
महिलाओं के लिए स्वस्थ आहार
बच्चों के लिए स्वस्थ आहार
How useful was this post?
Click on a star to rate it!
Average rating 5 / 5. Vote count: 1
No votes so far! Be the first to rate this post.

Related Article
No Related Article
- स्वास्थ्य और फिटनेस
- स्वस्थ भोजन और फल
- योगा और मेडिटेशन
- मानसिक स्वास्थ्य
- महिला स्वास्थ्य
- मस्तिष्क रोग
- बच्चों का स्वास्थ्य
Trending Posts
- Depression Meaning in Hindi – डिप्रेशन क्या है और जानिए इसके लक्षण, कारण और इलाज
- Quinoa in Hindi – क्विनोआ क्या है और इसके स्वास्थ्य लाभ हिंदी में
- Apricot Fruit Meaning in Hindi – एप्रीकॉट फ्रूट क्या है और जानिए इसे खाने के फायदे
- A to Z Tablet Uses in Hindi – A to Z टेबलेट के फायदे, उपयोग, डोज और दुष्प्रभाव
- High Blood Pressure in Hindi – हाई ब्लड प्रेशर कब और क्यों होता है?
Login access is disabled
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.15(7); 2023 Jul
- PMC10460242

A Comprehensive Analysis of Mental Health Problems in India and the Role of Mental Asylums
Vanee r meghrajani.
1 Community Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Education and Research, Wardha, IND
Manvi Marathe
2 Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Education and Research, Wardha, IND
Ritika Sharma
3 Medicine and Surgery, Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Education and Research, Wardha, IND

Ashwini Potdukhe
4 Medical Surgical Nursing, Smt. Radhikabai Meghe Memorial College of Nursing, Datta Meghe Institute of Higher Education and Research, Wardha, IND
Mayur B Wanjari
5 Research Scientist, Department of Research and Development, Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Education and Research, Wardha, IND
Avinash B Taksande
6 Physiology, Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Education and Research, Wardha, IND
This review article provides a comprehensive overview of the current state of mental health in India, highlighting the challenges faced, the existing initiatives, and the future directions for improving mental healthcare delivery. India is grappling with a high prevalence of mental health disorders, including depression, anxiety disorders, bipolar disorder, schizophrenia, and substance use disorders. The burden of mental health issues on individuals, families, and society is immense, leading to reduced quality of life, impaired functioning, and significant economic and social consequences. Various social and cultural factors, such as stigma, discrimination, gender inequalities, poverty, rapid urbanization, and cultural beliefs surrounding mental illness, further exacerbate the challenges of addressing mental health problems. Access to mental healthcare remains a significant concern, with considerable gaps in access to and quality of treatment and limited availability of mental health professionals, especially in rural areas. Inadequate infrastructure, a lack of awareness, and insufficient integration into primary healthcare systems hinder access to appropriate care. The historical development of mental asylums in India is examined, highlighting their establishment, purpose, and evolution over time. Critiques and challenges associated with mental asylums are discussed, including stigmatization, human rights concerns, the absence of human center approaches, quality of care, and the need for alternative approaches to mental healthcare.
Introduction and background
With its vast population and diverse demographics, India confronts a substantial mental health burden that warrants urgent attention [ 1 ]. Mental disorders cut across various age groups, socioeconomic backgrounds, and geographical regions, impacting individuals from all walks of life [ 1 ]. The repercussions of these conditions encompass personal suffering, impaired daily functioning, and extensive societal costs [ 1 ]. The prevalence of mental health disorders in India has risen steadily in recent years, contributing to the escalating public health concern. Estimates suggest that nearly 15% of the Indian population grapples with some form of mental health issue. This figure encompasses many disorders, including anxiety disorders, depression, bipolar disorder, schizophrenia, substance use disorders, and neurodevelopmental disorders [ 2 ].
The consequences of these mental health challenges reverberate throughout society. Firstly, individuals struggling with mental health problems face immense personal anguish and distress, as these conditions often impede their ability to lead fulfilling lives. They may encounter difficulties maintaining relationships, pursuing education or employment opportunities, and participating in social activities [ 3 ]. Moreover, mental health problems substantially affect the overall functioning of communities and the nation. Decreased productivity, both in the workplace and within households, is a significant economic consequence. Mental health issues often lead to absenteeism, reduced work efficiency, and long-term disability, negatively impacting workforce productivity and economic growth [ 4 , 5 ].
The financial burden associated with mental health problems cannot be overlooked. Increased healthcare expenditure is incurred due to the need for mental healthcare services, including diagnosis, treatment, medication, and therapy [ 6 ]. The indirect costs, such as lost productivity and an increased burden on caregivers, further exacerbate the economic impact [ 6 ]. Beyond the economic aspect, mental health problems in India also have far-reaching social implications. Stigma and discrimination surrounding mental disorders persist in many communities, hindering individuals from seeking help and support. This leads to delays in diagnosis and treatment, perpetuating the cycle of suffering and exacerbating the long-term consequences [ 7 ].
The rising prevalence of mental health disorders in India and their multifaceted impacts necessitate a comprehensive understanding of the challenges. Addressing mental health issues becomes crucial not only for the well-being of affected individuals but also for the overall progress and development of the nation. By investigating the role of mental asylums in this context, this review article aims to shed light on potential strategies to tackle mental health problems and improve the lives of individuals grappling with these conditions in India [ 1 , 2 , 6 ]. This review article aims to comprehensively analyze mental health problems in India and explore the role of mental asylums in addressing these challenges. By examining the historical and current context, this review aims to shed light on the strengths, limitations, and potential future directions of mental asylums in the Indian mental health landscape.
Methodology
The literature search strategy involved a comprehensive approach to identifying relevant studies on mental health problems in India. Multiple databases, including PubMed, PsycINFO, and Google Scholar, were searched using a combination of keywords such as "mental health," "India," "prevalence," "burden," "access to care," and "mental health disorders." The search was conducted without any language or date restrictions to ensure the inclusion of a wide range of studies. In addition to academic literature, reports from government agencies, international organizations, and non-governmental organizations were reviewed to capture a holistic understanding of the topic. To ensure the selection of appropriate studies, specific inclusion and exclusion criteria were applied. Inclusion criteria included studies on mental health problems in India, prevalence rates, types of mental health disorders, access to mental healthcare, social and cultural factors influencing mental health, and mental health policies and initiatives in India. Both quantitative and qualitative studies were considered. Studies that provided insights into the challenges, current practices, and future directions for mental healthcare in India were prioritized. Exclusion criteria involved studies that were not specific to mental health or did not pertain to the Indian context. Studies with insufficient data, case reports, editorials, and opinion pieces were also excluded. The focus was primarily on peer-reviewed articles, systematic reviews, meta-analyses, and research reports that provided substantial evidence and analysis of mental health problems in India. The selection of studies involved a two-step process. Initially, titles and abstracts were screened to assess their relevance to the research topic. Subsequently, full-text articles were reviewed based on the inclusion and exclusion criteria. Any discrepancies or uncertainties during the study selection process were resolved through discussion and consensus among the research team members.
Mental health problems in India
Prevalence and Types of Mental Health Disorders
In India, mental health disorders have a high prevalence, impacting a considerable proportion of the population. Epidemiological studies report prevalence rates for psychiatric disorders varying from 9.5 to 370 per 1000 people in India [ 8 ]. This prevalence encompasses a broad spectrum of mental health disorders, reflecting the diverse challenges individuals face in the country [ 8 ]. The prevalence rates of mental health disorders in India highlight the need for effective interventions and support systems to address the mental well-being of the population. Conditions such as depression, anxiety disorders, bipolar disorder, schizophrenia, and substance use disorders are commonly observed mental health disorders in India [ 8 ].
Depression: Depression is a common mental health disorder characterized by persistent sadness, hopelessness, and a loss of interest or pleasure in activities. At the population level, 3.5% of deaths were attributable to anxiety or depression [ 9 ]. It can negatively impact an individual's mood, thoughts, behavior, and physical well-being. Symptoms of depression may include fatigue, changes in appetite, sleep disturbances, difficulty concentrating, and thoughts of self-harm or suicide. Depression can significantly impair a person's daily functioning, interpersonal relationships, and overall quality of life [ 9 ].
Anxiety disorders: Anxiety disorders are characterized by excessive and persistent worry, fear, or anxiety that significantly interfere with daily functioning. Generalized anxiety disorder involves chronic and excessive worry about various aspects of life. Panic disorder is characterized by recurrent panic attacks, which are intense periods of overwhelming fear and physical symptoms such as heart palpitations and shortness of breath. Phobias involve an intense fear of specific objects, situations, or activities. Obsessive-compulsive disorder (OCD) is characterized by intrusive thoughts (obsessions) and repetitive behaviors (compulsions) performed to alleviate anxiety. Anxiety disorders can cause significant distress, avoidance behaviors, and impaired functioning [ 10 ].
Bipolar disorder: Bipolar disorder is characterized by alternating periods of elevated mood (mania or hypomania) and episodes of depression. During manic episodes, individuals may experience heightened energy levels, decreased sleep, racing thoughts, inflated self-esteem, impulsive behavior, and an exaggerated sense of self-importance. Depressive episodes are marked by sadness, loss of interest, fatigue, and changes in appetite and sleep patterns. Bipolar disorder can profoundly impact an individual's emotions, behavior, relationships, and overall functioning [ 11 ].
Schizophrenia: Schizophrenia is a chronic and severe mental disorder that affects a person's perception of reality, thinking processes, emotions, and behavior. Common symptoms include hallucinations (perceiving things that are not there), delusions (false beliefs), disorganized speech and behavior, reduced emotional expression, and social withdrawal. Individuals with schizophrenia may experience difficulties in cognitive functioning, such as problems with memory, attention, and executive functioning. Schizophrenia can significantly impair an individual's ability to think, interact with others, and function in society [ 12 ].
Substance use disorders: Substance use disorders involve the excessive and compulsive use of substances, such as alcohol or drugs, despite negative consequences. These disorders can have significant impacts on mental health. Substance abuse can lead to addiction, dependence, and withdrawal symptoms when the substance is unavailable. Substance use disorders can cause various mental health issues, including mood disorders, anxiety disorders, psychosis, cognitive impairments, and social and occupational problems. The associated problems may include financial difficulties, legal issues, relationship conflicts, and physical health complications [ 13 ].
Social and cultural factors influencing mental health in India
Societal Stigma and Discrimination
Mental illness carries a significant social stigma in Indian society, leading to discrimination and social exclusion for individuals with mental health problems. The stigma surrounding mental illness often stems from misconceptions, fear, and a lack of awareness. This stigma creates barriers to seeking help and support, as individuals may fear judgment, rejection, or negative consequences. Consequently, individuals may delay or avoid seeking treatment, resulting in inadequate or delayed care and further exacerbating their condition [ 14 ].
Gender Inequalities
Gender inequalities in India have a profound impact on mental health. Women, in particular, face unique challenges and are more vulnerable to mental health problems. Factors such as domestic violence, sexual abuse, unequal power dynamics, limited access to education and employment opportunities, and societal expectations can contribute to increased stress, anxiety, and depression among women. The intersectionality of gender with other factors, such as socioeconomic status and caste, further compounds mental health disparities [ 15 ].
Poverty and Socioeconomic Factors
Poverty and socioeconomic disparities play a crucial role in developing and exacerbating mental health disorders in India. Limited resources, including access to quality healthcare, mental health services, and essential social support systems, significantly impact mental well-being. Stressful living conditions, financial instability, and a lack of opportunities for upward mobility contribute to heightened psychological distress and the risk of mental health problems [ 16 ].
Rapid Urbanization and Migration
India's rapid urbanization and migration patterns have significant implications for mental health. Urban areas often present challenges such as social dislocation, loss of social support networks, increased competition, and higher stress levels. The migration process, whether from rural to urban areas or within urban areas, can disrupt social cohesion, traditional support systems, and stability, leading to an increased risk of mental health problems [ 17 ].
Family Dynamics and Societal Pressure
Family dynamics and societal expectations pressure individuals, impacting their mental well-being. Expectations related to education, career success, marriage, and gender roles can create significant stress and anxiety. Interpersonal conflicts, strained relationships, and dysfunctional family dynamics can also contribute to developing mental health issues. In some cases, the stigma associated with mental illness within families can lead to a lack of understanding and support, further hindering the individual's ability to seek help [ 18 ].
Cultural Beliefs Surrounding Mental Illness
Cultural beliefs and traditional practices related to mental illness vary across different regions and communities in India. These beliefs can influence help-seeking behaviors, treatment approaches, and perceptions of mental health. Sometimes, cultural beliefs may stigmatize mental illness, discourage open discussions, and promote harmful practices or ineffective remedies. This can hinder access to evidence-based care and perpetuate the cycle of mental health-related challenges [ 19 ].
The Burden of Mental Health Issues on Individuals and Society
Mental health problems substantially burden individuals and society as a whole in India. Individuals with mental health disorders often experience a reduced quality of life, impaired functioning in various domains (such as work, relationships, and education), and an increased risk of suicide [ 20 ]. Societally, mental health problems lead to significant productivity losses due to absenteeism, decreased work performance, and disability. The economic impact includes increased healthcare costs and decreased productivity, impeding social and economic development [ 21 ]. Additionally, mental health problems contribute to the overall burden on the healthcare system, straining resources and diverting attention from other areas of healthcare.
Access to mental healthcare in India
Shortage of Mental Health Professionals
The availability of mental health professionals, including psychiatrists, psychologists, and psychiatric nurses, is insufficient to meet the growing demand for mental healthcare in India. The shortage is particularly prominent in rural areas, where access to mental health professionals is limited. This uneven distribution of services creates a significant barrier for individuals seeking timely and appropriate mental healthcare [ 22 - 23 ].
Inadequate Infrastructure and Resources
Mental healthcare facilities, especially in rural areas, often lack the necessary infrastructure, equipment, and resources to provide comprehensive care. There is a shortage of psychiatric hospitals, outpatient clinics, and community-based services. The lack of appropriate infrastructure hinders the delivery of mental healthcare services and limits the capacity to meet the diverse needs of individuals with mental health disorders [ 24 ].
Lack of Awareness and Stigma
Limited awareness and pervasive stigma surrounding mental health issues in India contribute to the underutilization of mental healthcare services. The stigma associated with mental illness leads to discrimination, social isolation, and prejudice against individuals seeking help. This stigma discourages individuals from openly discussing their mental health concerns and seeking timely treatment [ 25 ].
Insufficient Integration into Primary Healthcare
Mental health services are not adequately integrated into primary healthcare systems in India. This lack of integration results in a fragmented approach to mental healthcare, hindering early detection, timely intervention, and continuity of care for individuals with mental health problems. The separation of mental health from primary healthcare reinforces the notion that mental health is separate from physical health, perpetuating the treatment gap [ 26 ].
Historical development of mental asylums in India
Establishment and Purpose of Mental Asylums
Mental asylums were established in India during the colonial era, primarily under British rule. The first mental asylum in India, the Indian Lunatic Asylum, was established in 1745 in Calcutta (now Kolkata). These institutions were initially established to confine and segregate individuals with mental illness from the rest of society. The focus was primarily on custodial care, with little emphasis on therapeutic interventions [ 27 ].
The main objectives of mental asylums were to provide a secure and controlled environment for those deemed "insane" and to manage and control perceived threats posed by individuals with mental illness. Asylums were often located in remote areas away from urban centers and were designed to isolate individuals with mental illness from the general population [ 28 ].
Changes and Evolution of Mental Asylums Over Time
Over time, mental asylums in India have undergone significant changes and evolution. With advancements in medical understanding and changes in societal attitudes towards mental illness, the approach to care within mental asylums shifted from custodial confinement to a more humane and therapeutic approach [ 29 ].
In the mid-19th century, mental asylums began adopting moral treatment principles influenced by European reform movements. Moral treatment aims to provide a more humane and respectful environment for individuals with mental illness. It focused on promoting moral and spiritual development, engaging patients in meaningful activities, and creating a supportive therapeutic milieu [ 30 ].
In the 20th century, developing psychiatric research institutes and training centers in India further contributed to the evolution of mental healthcare practices. These institutions played a crucial role in advancing the understanding, diagnosis, and treatment of mental health disorders. They also provided opportunities to train mental health professionals and conduct research to improve care [ 31 ].
Role of Mental Asylums in Addressing Mental Health Problems
Mental asylums significantly addressed mental health problems in India, particularly when alternative options were limited. They provided a place of refuge for individuals with mental illness, offering shelter, basic care, and some level of treatment. The asylums acted as custodial institutions, ensuring the containment and management of individuals considered "insane" by societal standards [ 32 ].
Although mental asylums' quality of care and conditions varied widely, some asylums did strive to provide treatment and rehabilitation to their residents. Occupational therapy, recreation, and vocational training were introduced to promote functional improvement and reintegration into society. Some mental asylums also contributed to the understanding and treatment of mental health disorders through research and training initiatives [ 33 ].
However, it is important to acknowledge that mental asylums face significant criticism and challenges. Stigmatization, abuse, overcrowding, a lack of resources, and inadequate staff training were pervasive issues. These concerns led to an evaluation of the asylum model and the recognition of the need for broader reforms in mental healthcare delivery [ 34 ]. The role of mental asylums has evolved, and today, the focus is shifting towards community-based care, deinstitutionalization, and integrating mental health services into mainstream healthcare systems.
Critiques and challenges of mental asylums in India
Stigmatization and Social Attitudes Towards Mental Asylums
Mental asylums in India have historically faced stigmatization and negative societal attitudes. They have been associated with neglect, abuse, and human rights violations. The perception of mental asylums as places of confinement and isolation perpetuates the stigma surrounding mental health and hampers efforts to promote community-based care. This stigma often prevents individuals from seeking help and reinforces the idea that mental health conditions should be dealt with in isolation rather than as part of a broader community [ 35 ].
Human Rights Concerns and Ethical Considerations
Human rights concerns have been raised regarding mental asylums in India. Reports have documented overcrowding, a lack of privacy, and inadequate living conditions in some institutions. Patients' rights, including dignity, autonomy, and privacy, can be compromised in these settings. Additionally, the ethical considerations of involuntary admissions, the use of restraints, and the need for informed consent in psychiatric treatment are critical issues that must be addressed to protect individuals' rights and well-being [ 36 ].
Quality of Care and Treatment Modalities
The quality of care provided in mental asylums varies widely across India. While some institutions adhere to evidence-based treatments, rehabilitation programs, and a multidisciplinary approach, others struggle with resource constraints, inadequate staffing, and outdated practices. Using outdated treatments and over-reliance on medications without adequate psychosocial support services remain challenges within the mental asylum system. Improving the quality of care requires a focus on the training and capacity-building of mental health professionals, ensuring access to evidence-based treatments, and promoting holistic approaches that address the individual's social, psychological, and emotional needs [ 37 ].
Alternative Approaches to Mental Healthcare
The criticisms and challenges surrounding mental asylums have spurred the exploration of alternative approaches to mental healthcare in India. Community-based care has gained recognition as a more humane and effective approach that emphasizes the involvement of families, communities, and social support networks. Integrating mental health into primary healthcare settings allows for early detection, timely intervention, and holistic management of mental health problems. Other alternative approaches include mobile mental health units to reach underserved populations, telemedicine for remote consultations, and the implementation of psychosocial interventions that prioritize individual empowerment, resilience, and well-being. These alternative approaches promote a shift towards person-centered care and community support, reducing reliance on institutionalized care and enhancing India's overall mental health ecosystem [ 38 ].
Current mental health initiatives in India
Government Programs and Policies
The Government of India has implemented several programs and policies to address mental health issues. The National Mental Health Program (NMHP) is a flagship initiative to improve mental healthcare services. The program aims to provide accessible and affordable mental healthcare, promote community participation, train mental health professionals, and raise awareness about mental health. It also emphasizes integrating mental health into primary healthcare systems [ 39 ].
In addition, the Mental Healthcare Act of 2017 is significant legislation that prioritizes the rights and dignity of individuals with mental illness. It provides a legal framework for delivering mental healthcare, protects the rights of individuals with mental illness, decriminalizes suicide, and promotes community-based care [ 40 ].
Community-Based Mental Health Services
Community-based mental health services have gained prominence in India as a strategy to bridge the treatment gap and improve access to mental healthcare. These services adopt a decentralized approach, delivering mental healthcare at the community level through trained professionals. Community mental health programs involve outreach activities, awareness campaigns, counseling services, and support for individuals with mental health disorders and their families. The aim is to reduce stigma, enhance accessibility, and provide holistic care sensitive to communities' cultural context [ 38 ].
Integration of Mental Health into Primary Healthcare
Integrating mental health into primary healthcare is a key strategy to improve access to mental healthcare services. The District Mental Health Program (DMHP) is a notable initiative. The DMHP focuses on strengthening mental health services at the primary care level by training primary healthcare workers to identify and manage common mental health conditions. It involves capacity building, the provision of essential psychotropic medications, referral systems, and community-based rehabilitation services. This integration ensures that mental health is given equal importance to physical health, leading to early detection, timely intervention, and continuity of care [ 41 ].
Awareness Campaigns and Advocacy Efforts
Awareness campaigns and advocacy efforts are critical to promoting mental health literacy, reducing stigma, and raising public awareness about mental health issues. Non-governmental organizations (NGOs), mental health professionals, and community groups actively engage in advocacy, education, and destigmatization initiatives. These efforts aim to challenge stereotypes, provide accurate information about mental health, promote help-seeking behaviors, and create supportive environments for individuals with mental health disorders. Awareness campaigns often utilize various media platforms, community events, and workshops to reach a wide audience and promote positive attitudes toward mental health [ 42 ]. These current mental health initiatives in India demonstrate a multifaceted approach that combines government policies, community-based services, integration into primary healthcare, and awareness campaigns. Such comprehensive efforts are crucial in addressing the complex challenges of mental health and improving the overall mental well-being of individuals in the country.
Future directions for mental health in India
Increasing the Number of Mental Health Professionals
Addressing the shortage of mental health professionals requires a multi-pronged approach. One strategy is to increase the number of psychiatrists, psychologists, psychiatric nurses, and other mental health specialists. This can be achieved through expanded training programs that attract more individuals to the field and provide them with the necessary skills and knowledge to practice effectively. Scholarships and incentives can also be offered to encourage professionals to work in underserved areas where the shortage is more pronounced. By increasing the workforce in mental health, access to care can be improved [ 43 ].
Enhancing Training and Capacity-Building
To ensure the delivery of high-quality mental healthcare, it is crucial to provide comprehensive and specialized training to mental health professionals. This includes continuous professional development programs that keep professionals updated with the latest evidence-based practices. Professionals can provide more effective and targeted interventions by enhancing their knowledge and skills in diagnosing and treating mental health disorders. Training programs should focus on culturally sensitive approaches and address the specific needs of diverse populations [ 44 ].
Decentralizing Mental Health Services
To bridge the gap in mental healthcare between urban and rural areas, it is essential to strengthen mental healthcare infrastructure and services at the district and community levels. This involves establishing mental health facilities, outpatient clinics, and community-based services in rural and remote areas. By bringing mental health services closer to where people live, access to care can be improved, and individuals can receive timely interventions. This also helps reduce the burden on tertiary care centers and psychiatric hospitals [ 45 ].
Integrating Mental Health into Primary Healthcare
Recognizing the importance of early detection and intervention, integrating mental health services into primary healthcare settings is crucial. This integration involves training primary healthcare providers to identify and manage common mental health conditions. It also includes establishing referral systems between primary care and specialized mental health services. Individuals can receive timely support and treatment by integrating mental health into primary healthcare, and the stigma associated with seeking mental healthcare can be reduced [ 46 ].
Strengthening Referral Systems
To ensure seamless transitions between different levels of care, robust referral systems must be developed. Effective communication and coordination between primary healthcare providers, specialized mental health services, and other relevant sectors (such as education and employment) are essential. Referral systems should ensure that individuals with mental health problems receive continuous support and follow-up care as they move through different stages of their treatment journey. This helps maintain continuity of care and address individuals' holistic needs [ 47 ].
Public-Private Partnerships and Leveraging Technology
To improve mental healthcare delivery, collaborations between the public and private sectors can be fostered through public-private partnerships. Such partnerships can enhance resource allocation, capacity-building, and the development of innovative approaches to mental health. Private sector involvement can bring additional expertise and resources to complement public sector efforts. Furthermore, leveraging technology can significantly improve access to mental healthcare, particularly in remote and underserved areas. Telemedicine, mobile health applications, and online platforms can facilitate virtual consultations, remote monitoring, and self-help interventions, expanding the reach of mental health services [ 48 ].
By implementing these recommendations, India can make significant strides in improving mental healthcare delivery, addressing workforce shortages, enhancing training and capacity-building, decentralizing services, integrating mental health into primary care, strengthening referral systems, and harnessing the potential of public-private partnerships and technology. These strategies contribute to a more comprehensive and accessible mental health system that meets the diverse needs of individuals nationwide.
Policy reforms and resource allocation
Allocating Adequate Resources
Increasing budgetary allocations specifically for mental health is essential. Sufficient funds should be allocated to support infrastructure development, including the establishment of mental health facilities, outpatient clinics, and community-based services. Adequate resources are also necessary to recruit and train mental health professionals, implement training programs for primary healthcare providers, conduct research, and address mental health disparities across regions [ 49 ].
Prioritizing Mental Health in the Healthcare Agenda
Recognizing mental health as a priority area within the broader healthcare system is essential for effective reform. This involves integrating mental health into national health policies, strategic plans, and programs. Setting measurable targets and indicators for improving mental healthcare outcomes helps ensure that progress is monitored and interventions are evidence-based [ 50 ].
Developing a Robust Regulatory Framework
Establishing and implementing a comprehensive regulatory framework is crucial for ensuring quality standards, ethics, and guidelines for mental health services. This includes developing licensing and accreditation processes for mental healthcare providers, monitoring compliance with professional standards, and enforcing ethical guidelines. Additionally, monitoring and evaluation mechanisms should be in place to assess the quality and effectiveness of mental healthcare delivery, identify areas for improvement, and ensure accountability [ 51 ].
Ensuring Policy Implementation
Strengthening coordination and collaboration among government departments responsible for mental health, social welfare, education, and employment is necessary for effective policy implementation. Intersectoral collaboration facilitates a holistic approach to addressing mental health issues and ensures that policies and initiatives are coordinated. This coordination can include sharing resources, data, and expertise, as well as joint planning and monitoring of mental health programs [ 52 ].
Holistic and multidisciplinary approaches to mental health
Integrating Psychological, Social, and Biological Perspectives
Recognizing that mental health disorders have complex causes and manifestations, it is essential to adopt an integrated approach that addresses mental health's biological, psychological, and social determinants. This means acknowledging the interplay between genetic factors, brain chemistry, individual experiences, and social contexts in developing and managing mental health disorders [ 53 ].
Collaborative Care Models
Collaborative care models involve a coordinated and team-based approach to mental healthcare delivery. These models bring together multiple stakeholders, including mental health professionals, primary healthcare providers, social workers, and community organizations, to work collaboratively to address the needs of individuals with mental health disorders [ 54 ].
Promoting community participation and support systems
Engaging Community Leaders and Organizations
Collaborating with community leaders, religious and cultural organizations, and community-based groups is crucial for promoting mental health awareness, reducing stigma, and improving access to care. Community leaders and organizations have significant influence and reach within their communities. By partnering with them, it is possible to conduct awareness campaigns, organize educational events, and disseminate accurate information about mental health. This collaboration can help create supportive environments where individuals feel comfortable seeking help and accessing mental healthcare services. Community-based organizations can also play a role in identifying individuals in need of support and connecting them with appropriate resources [ 55 ].
Involving Individuals with Lived Experience
It is essential to involve individuals with personal experience with mental health problems in decision-making, service planning, and advocacy efforts. Their unique insights and perspectives can contribute to more person-centered and recovery-oriented mental healthcare services. These individuals can provide valuable input on the challenges they faced, the types of support that were helpful to them, and the gaps in existing services. Their involvement can help shape policies, programs, and interventions more responsive to the needs and preferences of individuals with mental health disorders. It also empowers them to become advocates for mental health and reduce stigma through sharing their stories and experiences [ 56 ].
Peer Support Networks and Community-Based Rehabilitation
Establishing peer support networks, self-help groups, and community-based rehabilitation programs is essential for fostering a sense of belonging and support among individuals with mental health disorders. Peer support networks provide a platform for individuals to connect, share experiences, and offer mutual support. These networks can help reduce feelings of isolation and provide a sense of community, which is particularly beneficial during recovery. Self-help groups allow individuals to share coping strategies, provide emotional support, and learn from each other's experiences. Community-based rehabilitation programs empower individuals with mental health disorders to develop skills, reintegrate into society, and participate in meaningful activities. These initiatives promote social inclusion, recovery, and well-being [ 57 ]. By implementing these recommendations, India can significantly improve its mental healthcare delivery, ensure better access and quality of care, reduce stigma, and promote holistic well-being for individuals with mental health disorders.
Conclusions
Addressing mental health problems in India holds immense significance, considering the scale of human value impact involved. The country's population size gives added weight to the importance of tackling these barriers. It is crucial to recognize that mental health issues affect a significant portion of the population and can lead to severe consequences if left unaddressed. Therefore, concerted efforts are essential to combating these challenges effectively. Reducing the stigma surrounding mental illness is critical to addressing mental health problems in India. Stigma creates barriers that hinder individuals from seeking the necessary help and support they require. To overcome this, public awareness campaigns and educational initiatives are vital in combating stigma and promoting understanding and empathy toward those with mental health conditions. A comprehensive and compassionate approach is necessary to tackle India's complex mental health challenges. By reducing stigma, improving accessibility, enhancing the quality of services, shifting towards community-based care, protecting human rights, and integrating mental health into mainstream healthcare systems, India can make significant progress in addressing mental health issues. The benefits will extend beyond individuals, contributing to society's overall development and well-being.
The authors have declared that no competing interests exist.
- Essay Editor
Mental Health Essay
Revolutionize your writing process: our AI rewrite tool is here to help
Introduction
Mental health, often overshadowed by its physical counterpart, is an intricate and essential aspect of human existence. It envelops our emotions, psychological state, and social well-being, shaping our thoughts, behaviors, and interactions. With the complexities of modern life—constant connectivity, societal pressures, personal expectations, and the frenzied pace of technological advancements—mental well-being has become increasingly paramount. Historically, conversations around this topic have been hushed, shrouded in stigma and misunderstanding. However, as the curtains of misconception slowly lift, we find ourselves in an era where discussions about mental health are not only welcomed but are also seen as vital. Recognizing and addressing the nuances of our mental state is not merely about managing disorders; it's about understanding the essence of who we are, how we process the world around us, and how we navigate the myriad challenges thrown our way. This essay aims to delve deep into the realm of mental health, shedding light on its importance, the potential consequences of neglect, and the spectrum of mental disorders that many face in silence.
Importance of Mental Health
Mental health plays a pivotal role in determining how individuals think, feel, and act. It influences our decision-making processes, stress management techniques, interpersonal relationships, and even our physical health. A well-tuned mental state boosts productivity, creativity, and the intrinsic sense of self-worth, laying the groundwork for a fulfilling life.
Negative Impact of Mental Health
Neglecting mental health, on the other hand, can lead to severe consequences. Reduced productivity, strained relationships, substance abuse, physical health issues like heart diseases, and even reduced life expectancy are just some of the repercussions of poor mental health. It not only affects the individual in question but also has a ripple effect on their community, workplace, and family.
Mental Disorders: Types and Prevalence
Mental disorders are varied and can range from anxiety and mood disorders like depression and bipolar disorder to more severe conditions such as schizophrenia.
- Depression: Characterized by persistent sadness, lack of interest in activities, and fatigue.
- Anxiety Disorders: Encompass conditions like generalized anxiety disorder, panic attacks, and specific phobias.
- Schizophrenia: A complex disorder affecting a person's ability to think, feel, and behave clearly.
The prevalence of these disorders has been on the rise, underscoring the need for comprehensive mental health initiatives and awareness campaigns.
Understanding Mental Health and Its Importance
Mental health is not merely the absence of disorders but encompasses emotional, psychological, and social well-being. Recognizing the signs of deteriorating mental health, like prolonged sadness, extreme mood fluctuations, or social withdrawal, is crucial. Understanding stems from awareness and education. Societal stigmas surrounding mental health have often deterred individuals from seeking help. Breaking these barriers, fostering open conversations, and ensuring access to mental health care are imperative steps.
Conclusion: Mental Health
Mental health, undeniably, is as significant as physical health, if not more. In an era where the stressors are myriad, from societal pressures to personal challenges, mental resilience and well-being are essential. Investing time and resources into mental health initiatives, and more importantly, nurturing a society that understands, respects, and prioritizes mental health is the need of the hour.
- World Leaders: Several influential personalities, from celebrities to sports stars, have openly discussed their mental health challenges, shedding light on the universality of these issues and the importance of addressing them.
- Workplaces: Progressive organizations are now incorporating mental health programs, recognizing the tangible benefits of a mentally healthy workforce, from increased productivity to enhanced creativity.
- Educational Institutions: Schools and colleges, witnessing the effects of stress and other mental health issues on students, are increasingly integrating counseling services and mental health education in their curriculum.
In weaving through the intricate tapestry of mental health, it becomes evident that it's an area that requires collective attention, understanding, and action.
Short Essay about Mental Health
Mental health, an integral facet of human well-being, shapes our emotions, decisions, and daily interactions. Just as one would care for a sprained ankle or a fever, our minds too require attention and nurture. In today's bustling world, mental well-being is often put on the back burner, overshadowed by the immediate demands of life. Yet, its impact is pervasive, influencing our productivity, relationships, and overall quality of life.
Sadly, mental health issues have long been stigmatized, seen as a sign of weakness or dismissed as mere mood swings. However, they are as real and significant as any physical ailment. From anxiety to depression, these disorders have touched countless lives, often in silence due to societal taboos.
But change is on the horizon. As awareness grows, conversations are shifting from hushed whispers to open discussions, fostering understanding and support. Institutions, workplaces, and communities are increasingly acknowledging the importance of mental health, implementing programs, and offering resources.
In conclusion, mental health is not a peripheral concern but a central one, crucial to our holistic well-being. It's high time we prioritize it, eliminating stigma and fostering an environment where everyone feels supported in their mental health journey.
Frequently Asked Questions
- What is the primary focus of a mental health essay?
Answer: The primary focus of a mental health essay is to delve into the intricacies of mental well-being, its significance in our daily lives, the various challenges people face, and the broader societal implications. It aims to shed light on both the psychological and emotional aspects of mental health, often emphasizing the importance of understanding, empathy, and proactive care.
- How can writing an essay on mental health help raise awareness about its importance?
Answer: Writing an essay on mental health can effectively articulate the nuances and complexities of the topic, making it more accessible to a wider audience. By presenting facts, personal anecdotes, and research, the essay can demystify misconceptions, highlight the prevalence of mental health issues, and underscore the need for destigmatizing discussions around it. An impactful essay can ignite conversations, inspire action, and contribute to a more informed and empathetic society.
- What are some common topics covered in a mental health essay?
Answer: Common topics in a mental health essay might include the definition and importance of mental health, the connection between mental and physical well-being, various mental disorders and their symptoms, societal stigmas and misconceptions, the impact of modern life on mental health, and the significance of therapy and counseling. It may also delve into personal experiences, case studies, and the broader societal implications of neglecting mental health.
Recent articles
Essay - what it is and how to write it with an ai aithor.
Writing concise and persuasive texts is a skill required in many professional settings. One of the ways we learn this skill is by writing essays. However, essays require lots of preparation and research, so they can be hard to write, especially if you struggle to understand how to make your essay better. In this article, you’ll learn what an essay is and how to use the Aithor AI essay generator for writing essays. What is an essay? In a broad sense, an essay is a genre of writing that allows ...
Artificial Intelligence: Evolution of Essay Writing
We live in the age when each new year brings more innovations than the previous one. One of the most debated topics of recent time is AI writing software. Not only did users get a handy helper for composing emails, but a tireless machine for writing pages of text on a variety of topics. It’s only natural that students who often have to write long essays as homework started using it too. This article will dissect how artificial intelligence will change the future essays and if AI generation tool ...
Join the writing revolution: subscribe to our AI article generator tool
- Essay On Mental Health In Hindi
- Mental Health
Featured Example Essay
This featured Essay On Mental Health In Hindi is one of many example essays available on this topic.
Sample Essay Examples

Related Essay Topics
- Mental Health Essay
- Social Media And Mental Health Essay
- Mental Health Essay Outline
- Mental Health Persuasive Essay
- Persuasive Essay Topics On Mental Health
- Mental Health Awareness Persuasive Essay
- Mental Health Introduction Essay
- Mental Health Reflection Essay
- Mental Health Topics For Essays
- Persuasive Essay On Mental Health
- Abortion And Mental Health Essay
- Argumentative Essay Topics Mental Health
- Importance Of Mental Health Essay
- Recovery In Mental Health Essay
- Examples Of Reflective Essays In Mental Health Nursing
- Mental Health Discursive Essay
- Mental Health Essay In Kannada
- Mental Health Essay Introduction
- Mental Health Essay Questions
- Mental Health Essays Uk
- Mental Health Nursing Care Plan Essay
- Mental Health Nursing Essays
- Social Media And Mental Health Essay Outline
- What Does Mental Health Mean To You Essay
- Argumentative Essay Topics About Mental Health
- Essay On Mental Health Pdf
- How Social Media Affects Mental Health Essay
- Medical Model Of Mental Health Essay
- Mental Health And Crime Essay
- Mental Health Persuasive Essay Topics
- My Mental Health Essay
- Reflective Essay On Mental Health Placement
- Why Is Mental Health Important Essay
- Expository Essay On Mental Health
- How Does Social Media Affect Mental Health Essay
- Importance Of Mental Health Awareness Essay
- Mental Health Argumentative Essay
- Mental Health Argumentative Essay Topics
- Mental Health Awareness Essay
- Mental Health Case Study Essay
- Mental Health Conclusion Essay
- Mental Health Essay Competition
- Mental Health Essay Titles
- Persuasive Essay About Mental Health Awareness
- Social Media Impact On Mental Health Essay
- An Essay On Mental Health
- Argumentative Essay Topics On Mental Health
- Care Plan Essay Mental Health
- Cause And Effect Essay Topics Mental Health
- Communication In Mental Health Nursing Essay
- Essay About Mental Health An Important Aspect Of Life
- Essay About Mental Health Of Students
- Essay About Your Mental Health
- Essay On Mental Health Awareness
- Essay On Social Media And Mental Health
- Essay On World Mental Health Day
- Essay Questions About Mental Health
- Essay Stigma Mental Health
- Exercise And Mental Health Essay
- Good Mental Health Essay
- How Does Music Affect Mental Health Essay
- Human Rights And Mental Health Essay
- Mental Health And Wellbeing Essay
- Mental Health Assessment Essay
- Mental Health Care Plan Essay
- Mental Health Essay Conclusion
- Mental Health Essay Contest
- Mental Health Essay Examples
- Mental Health Essay Free
- Mental Health Essay Pdf
- Mental Health Essay Sample
- Mental Health Essay Samples
- Mental Health Essay Thesis
- Mental Health Essay Topics
- Mental Health In College Students Essay
- Mental Health In Prisons Essay
- Mental Health In Schools Essay
- Mental Health Is More Important Than Physical Health Essay
- Mental Health Issues Essay
- Mental Health Nursing Essay
- Mental Health Photo Essay
- Mental Health Promotion Essay
- Mental Health Proposal Essay
- Mental Health Sociology Essay
- Mental Health Stigma Essay
- Mental Health Stigma Persuasive Essay
- Narrative Essay About Mental Health
- Negative Effects Of Social Media On Mental Health Essay
- Personal Essay On Mental Health
- Persuasive Essay Topics About Mental Health
- Persuasive Essay Topics Mental Health
- Physical And Mental Health Essay
- Reflective Essay Mental Health Nursing
- Sample Essay About Mental Health
- Short Essay About Mental Health
- Social Media Affects Mental Health Essay
- Social Media Effects On Mental Health Essay
- Social Media Mental Health Essay
- Social Media On Mental Health Essay
- Open access
- Published: 12 December 2023
Examining the role of community resilience and social capital on mental health in public health emergency and disaster response: a scoping review
- C. E. Hall 1 , 2 ,
- H. Wehling 1 ,
- J. Stansfield 3 ,
- J. South 3 ,
- S. K. Brooks 2 ,
- N. Greenberg 2 , 4 ,
- R. Amlôt 1 &
- D. Weston 1
BMC Public Health volume 23 , Article number: 2482 ( 2023 ) Cite this article
1772 Accesses
21 Altmetric
Metrics details
The ability of the public to remain psychologically resilient in the face of public health emergencies and disasters (such as the COVID-19 pandemic) is a key factor in the effectiveness of a national response to such events. Community resilience and social capital are often perceived as beneficial and ensuring that a community is socially and psychologically resilient may aid emergency response and recovery. This review presents a synthesis of literature which answers the following research questions: How are community resilience and social capital quantified in research?; What is the impact of community resilience on mental wellbeing?; What is the impact of infectious disease outbreaks, disasters and emergencies on community resilience and social capital?; and, What types of interventions enhance community resilience and social capital?
A scoping review procedure was followed. Searches were run across Medline, PsycInfo, and EMBASE, with search terms covering both community resilience and social capital, public health emergencies, and mental health. 26 papers met the inclusion criteria.
The majority of retained papers originated in the USA, used a survey methodology to collect data, and involved a natural disaster. There was no common method for measuring community resilience or social capital. The association between community resilience and social capital with mental health was regarded as positive in most cases. However, we found that community resilience, and social capital, were initially negatively impacted by public health emergencies and enhanced by social group activities.
Several key recommendations are proposed based on the outcomes from the review, which include: the need for a standardised and validated approach to measuring both community resilience and social capital; that there should be enhanced effort to improve preparedness to public health emergencies in communities by gauging current levels of community resilience and social capital; that community resilience and social capital should be bolstered if areas are at risk of disasters or public health emergencies; the need to ensure that suitable short-term support is provided to communities with high resilience in the immediate aftermath of a public health emergency or disaster; the importance of conducting robust evaluation of community resilience initiatives deployed during the COVID-19 pandemic.
Peer Review reports
For the general population, public health emergencies and disasters (e.g., natural disasters; infectious disease outbreaks; Chemical, Biological, Radiological or Nuclear incidents) can give rise to a plethora of negative outcomes relating to both health (e.g. increased mental health problems [ 1 , 2 , 3 , 4 ]) and the economy (e.g., increased unemployment and decreased levels of tourism [ 4 , 5 , 6 ]). COVID-19 is a current, and ongoing, example of a public health emergency which has affected over 421 million individuals worldwide [ 7 ]. The long term implications of COVID-19 are not yet known, but there are likely to be repercussions for physical health, mental health, and other non-health related outcomes for a substantial time to come [ 8 , 9 ]. As a result, it is critical to establish methods which may inform approaches to alleviate the longer-term negative consequences that are likely to emerge in the aftermath of both COVID-19 and any future public health emergency.
The definition of resilience often differs within the literature, but ultimately resilience is considered a dynamic process of adaptation. It is related to processes and capabilities at the individual, community and system level that result in good health and social outcomes, in spite of negative events, serious threats and hazards [ 10 ]. Furthermore, Ziglio [ 10 ] refers to four key types of resilience capacity: adaptive, the ability to withstand and adjust to unfavourable conditions and shocks; absorptive, the ability to withstand but also to recover and manage using available assets and skills; anticipatory, the ability to predict and minimize vulnerability; and transformative, transformative change so that systems better cope with new conditions.
There is no one settled definition of community resilience (CR). However, it generally relates to the ability of a community to withstand, adapt and permit growth in adverse circumstances due to social structures, networks and interdependencies within the community [ 11 ]. Social capital (SC) is considered a major determinant of CR [ 12 , 13 ], and reflects strength of a social network, community reciprocity, and trust in people and institutions [ 14 ]. These aspects of community are usually conceptualised primarily as protective factors that enable communities to cope and adapt collectively to threats. SC is often broken down into further categories [ 15 ], for example: cognitive SC (i.e. perceptions of community relations, such as trust, mutual help and attachment) and structural SC (i.e. what actually happens within the community, such as participation, socialising) [ 16 ]; or, bonding SC (i.e. connections among individuals who are emotionally close, and result in bonds to a particular group [ 17 ]) and bridging SC (i.e. acquaintances or individuals loosely connected that span different social groups [ 18 ]). Generally, CR is perceived to be primarily beneficial for multiple reasons (e.g. increased social support [ 18 , 19 ], protection of mental health [ 20 , 21 ]), and strengthening community resilience is a stated health goal of the World Health Organisation [ 22 ] when aiming to alleviate health inequalities and protect wellbeing. This is also reflected by organisations such as Public Health England (now split into the UK Health Security Agency and the Office for Health Improvement and Disparities) [ 23 ] and more recently, CR has been targeted through the endorsement of Community Champions (who are volunteers trained to support and to help improve health and wellbeing. Community Champions also reflect their local communities in terms of population demographics for example age, ethnicity and gender) as part of the COVID-19 response in the UK (e.g. [ 24 , 25 ]).
Despite the vested interest in bolstering communities, the research base establishing: how to understand and measure CR and SC; the effect of CR and SC, both during and following a public health emergency (such as the COVID-19 pandemic); and which types of CR or SC are the most effective to engage, is relatively small. Given the importance of ensuring resilience against, and swift recovery from, public health emergencies, it is critically important to establish and understand the evidence base for these approaches. As a result, the current review sought to answer the following research questions: (1) How are CR and SC quantified in research?; (2) What is the impact of community resilience on mental wellbeing?; (3) What is the impact of infectious disease outbreaks, disasters and emergencies on community resilience and social capital?; and, (4) What types of interventions enhance community resilience and social capital?
By collating research in order to answer these research questions, the authors have been able to propose several key recommendations that could be used to both enhance and evaluate CR and SC effectively to facilitate the long-term recovery from COVID-19, and also to inform the use of CR and SC in any future public health disasters and emergencies.
A scoping review methodology was followed due to the ease of summarising literature on a given topic for policy makers and practitioners [ 26 ], and is detailed in the following sections.
Identification of relevant studies
An initial search strategy was developed by authors CH and DW and included terms which related to: CR and SC, given the absence of a consistent definition of CR, and the link between CR and SC, the review focuses on both CR and SC to identify as much relevant literature as possible (adapted for purpose from Annex 1: [ 27 ], as well as through consultation with review commissioners); public health emergencies and disasters [ 28 , 29 , 30 , 31 ], and psychological wellbeing and recovery (derived a priori from literature). To ensure a focus on both public health and psychological research, the final search was carried across Medline, PsycInfo, and EMBASE using OVID. The final search took place on the 18th of May 2020, the search strategy used for all three databases can be found in Supplementary file 1 .
Selection criteria
The inclusion and exclusion criteria were developed alongside the search strategy. Initially the criteria were relatively inclusive and were subject to iterative development to reflect the authors’ familiarisation with the literature. For example, the decision was taken to exclude research which focused exclusively on social support and did not mention communities as an initial title/abstract search suggested that the majority of this literature did not meet the requirements of our research question.
The full and final inclusion and exclusion criteria used can be found in Supplementary file 2 . In summary, authors decided to focus on the general population (i.e., non-specialist, e.g. non-healthcare worker or government official) to allow the review to remain community focused. The research must also have assessed the impact of CR and/or SC on mental health and wellbeing, resilience, and recovery during and following public health emergencies and infectious disease outbreaks which affect communities (to ensure the research is relevant to the review aims), have conducted primary research, and have a full text available or provided by the first author when contacted.
Charting the data
All papers were first title and abstract screened by CH or DW. Papers then were full text reviewed by CH to ensure each paper met the required eligibility criteria, if unsure about a paper it was also full text reviewed by DW. All papers that were retained post full-text review were subjected to a standardised data extraction procedure. A table was made for the purpose of extracting the following data: title, authors, origin, year of publication, study design, aim, disaster type, sample size and characteristics, variables examined, results, restrictions/limitations, and recommendations. Supplementary file 3 details the charting the data process.
Analytical method
Data was synthesised using a Framework approach [ 32 ], a common method for analysing qualitative research. This method was chosen as it was originally used for large-scale social policy research [ 33 ] as it seeks to identify: what works, for whom, in what conditions, and why [ 34 ]. This approach is also useful for identifying commonalities and differences in qualitative data and potential relationships between different parts of the data [ 33 ]. An a priori framework was established by CH and DW. Extracted data was synthesised in relation to each research question, and the process was iterative to ensure maximum saturation using the available data.
Study selection
The final search strategy yielded 3584 records. Following the removal of duplicates, 2191 records remained and were included in title and abstract screening. A PRISMA flow diagram is presented in Fig. 1 .
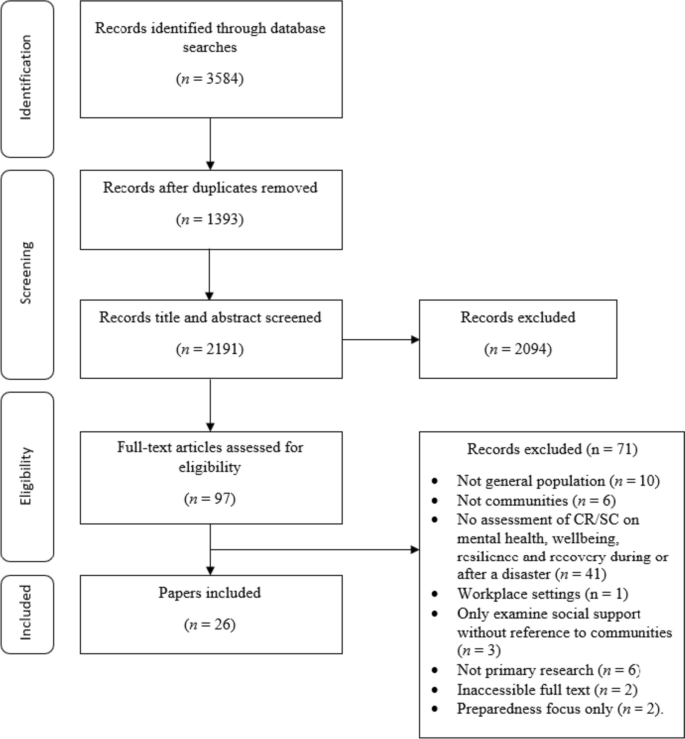
PRISMA flow diagram
At the title and abstract screening stage, the process became more iterative as the inclusion criteria were developed and refined. For the first iteration of screening, CH or DW sorted all records into ‘include,’ ‘exclude,’ and ‘unsure’. All ‘unsure’ papers were re-assessed by CH, and a random selection of ~ 20% of these were also assessed by DW. Where there was disagreement between authors the records were retained, and full text screened. The remaining papers were reviewed by CH, and all records were categorised into ‘include’ and ‘exclude’. Following full-text screening, 26 papers were retained for use in the review.
Study characteristics
This section of the review addresses study characteristics of those which met the inclusion criteria, which comprises: date of publication, country of origin, study design, study location, disaster, and variables examined.
Date of publication
Publication dates across the 26 papers spanned from 2008 to 2020 (see Fig. 2 ). The number of papers published was relatively low and consistent across this timescale (i.e. 1–2 per year, except 2010 and 2013 when none were published) up until 2017 where the number of papers peaked at 5. From 2017 to 2020 there were 15 papers published in total. The amount of papers published in recent years suggests a shift in research and interest towards CR and SC in a disaster/ public health emergency context.
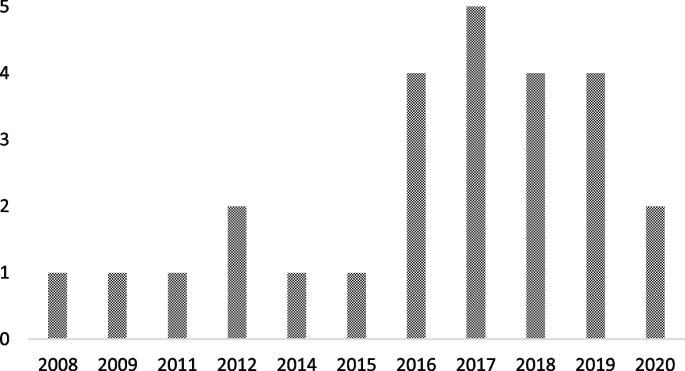
Graph to show retained papers date of publication
Country of origin
The locations of the first authors’ institutes at the time of publication were extracted to provide a geographical spread of the retained papers. The majority originated from the USA [ 35 , 36 , 37 , 38 , 39 , 40 , 41 ], followed by China [ 42 , 43 , 44 , 45 , 46 ], Japan [ 47 , 48 , 49 , 50 ], Australia [ 51 , 52 , 53 ], The Netherlands [ 54 , 55 ], New Zealand [ 56 ], Peru [ 57 ], Iran [ 58 ], Austria [ 59 ], and Croatia [ 60 ].
There were multiple methodological approaches carried out across retained papers. The most common formats included surveys or questionnaires [ 36 , 37 , 38 , 42 , 46 , 47 , 48 , 49 , 50 , 53 , 54 , 55 , 57 , 59 ], followed by interviews [ 39 , 40 , 43 , 51 , 52 , 60 ]. Four papers used both surveys and interviews [ 35 , 41 , 45 , 58 ], and two papers conducted data analysis (one using open access data from a Social Survey [ 44 ] and one using a Primary Health Organisations Register [ 56 ]).
Study location
The majority of the studies were carried out in Japan [ 36 , 42 , 44 , 47 , 48 , 49 , 50 ], followed by the USA [ 35 , 37 , 38 , 39 , 40 , 41 ], China [ 43 , 45 , 46 , 53 ], Australia [ 51 , 52 ], and the UK [ 54 , 55 ]. The remaining studies were carried out in Croatia [ 60 ], Peru [ 57 ], Austria [ 59 ], New Zealand [ 56 ] and Iran [ 58 ].
Multiple different types of disaster were researched across the retained papers. Earthquakes were the most common type of disaster examined [ 45 , 47 , 49 , 50 , 53 , 56 , 57 , 58 ], followed by research which assessed the impact of two disastrous events which had happened in the same area (e.g. Hurricane Katrina and the Deepwater Horizon oil spill in Mississippi, and the Great East Japan earthquake and Tsunami; [ 36 , 37 , 38 , 42 , 44 , 48 ]). Other disaster types included: flooding [ 51 , 54 , 55 , 59 , 60 ], hurricanes [ 35 , 39 , 41 ], infectious disease outbreaks [ 43 , 46 ], oil spillage [ 40 ], and drought [ 52 ].
Variables of interest examined
Across the 26 retained papers: eight referred to examining the impact of SC [ 35 , 37 , 39 , 41 , 46 , 49 , 55 , 60 ]; eight examined the impact of cognitive and structural SC as separate entities [ 40 , 42 , 45 , 48 , 50 , 54 , 57 , 59 ]; one examined bridging and bonding SC as separate entities [ 58 ]; two examined the impact of CR [ 38 , 56 ]; and two employed a qualitative methodology but drew findings in relation to bonding and bridging SC, and SC generally [ 51 , 52 ]. Additionally, five papers examined the impact of the following variables: ‘community social cohesion’ [ 36 ], ‘neighbourhood connectedness’ [ 44 ], ‘social support at the community level’ [ 47 ], ‘community connectedness’ [ 43 ] and ‘sense of community’ [ 53 ]. Table 1 provides additional details on this.
How is CR and SC measured or quantified in research?
The measures used to examine CR and SC are presented Table 1 . It is apparent that there is no uniformity in how SC or CR is measured across the research. Multiple measures are used throughout the retained studies, and nearly all are unique. Additionally, SC was examined at multiple different levels (e.g. cognitive and structural, bonding and bridging), and in multiple different forms (e.g. community connectedness, community cohesion).
What is the association between CR and SC on mental wellbeing?
To best compare research, the following section reports on CR, and facets of SC separately. Please see Supplementary file 4 for additional information on retained papers methods of measuring mental wellbeing.
- Community resilience
CR relates to the ability of a community to withstand, adapt and permit growth in adverse circumstances due to social structures, networks and interdependencies within the community [ 11 ].
The impact of CR on mental wellbeing was consistently positive. For example, research indicated that there was a positive association between CR and number of common mental health (i.e. anxiety and mood) treatments post-disaster [ 56 ]. Similarly, other research suggests that CR is positively related to psychological resilience, which is inversely related to depressive symptoms) [ 37 ]. The same research also concluded that CR is protective of psychological resilience and is therefore protective of depressive symptoms [ 37 ].
- Social capital
SC reflects the strength of a social network, community reciprocity, and trust in people and institutions [ 14 ]. These aspects of community are usually conceptualised primarily as protective factors that enable communities to cope and adapt collectively to threats.
There were inconsistencies across research which examined the impact of abstract SC (i.e. not refined into bonding/bridging or structural/cognitive) on mental wellbeing. However, for the majority of cases, research deems SC to be beneficial. For example, research has concluded that, SC is protective against post-traumatic stress disorder [ 55 ], anxiety [ 46 ], psychological distress [ 50 ], and stress [ 46 ]. Additionally, SC has been found to facilitate post-traumatic growth [ 38 ], and also to be useful to be drawn upon in times of stress [ 52 ], both of which could be protective of mental health. Similarly, research has also found that emotional recovery following a disaster is more difficult for those who report to have low levels of SC [ 51 ].
Conversely, however, research has also concluded that when other situational factors (e.g. personal resources) were controlled for, a positive relationship between community resources and life satisfaction was no longer significant [ 60 ]. Furthermore, some research has concluded that a high level of SC can result in a community facing greater stress immediately post disaster. Indeed, one retained paper found that high levels of SC correlate with higher levels of post-traumatic stress immediately following a disaster [ 39 ]. However, in the later stages following a disaster, this relationship can reverse, with SC subsequently providing an aid to recovery [ 41 ]. By way of explanation, some researchers have suggested that communities with stronger SC carry the greatest load in terms of helping others (i.e. family, friends and neighbours) as well as themselves immediately following the disaster, but then as time passes the communities recover at a faster rate as they are able to rely on their social networks for support [ 41 ].
Cognitive and structural social capital
Cognitive SC refers to perceptions of community relations, such as trust, mutual help and attachment, and structural SC refers to what actually happens within the community, such as participation, socialising [ 16 ].
Cognitive SC has been found to be protective [ 49 ] against PTSD [ 54 , 57 ], depression [ 40 , 54 ]) mild mood disorder; [ 48 ]), anxiety [ 48 , 54 ] and increase self-efficacy [ 59 ].
For structural SC, research is again inconsistent. On the one hand, structural SC has been found to: increase perceived self-efficacy, be protective of depression [ 40 ], buffer the impact of housing damage on cognitive decline [ 42 ] and provide support during disasters and over the recovery period [ 59 ]. However, on the other hand, it has been found to have no association with PTSD [ 54 , 57 ] or depression, and is also associated with a higher prevalence of anxiety [ 54 ]. Similarly, it is also suggested by additional research that structural SC can harm women’s mental health, either due to the pressure of expectations to help and support others or feelings of isolation [ 49 ].
Bonding and bridging social capital
Bonding SC refers to connections among individuals who are emotionally close, and result in bonds to a particular group [ 17 ], and bridging SC refers to acquaintances or individuals loosely connected that span different social groups [ 18 ].
One research study concluded that both bonding and bridging SC were protective against post-traumatic stress disorder symptoms [ 58 ]. Bridging capital was deemed to be around twice as effective in buffering against post-traumatic stress disorder than bonding SC [ 58 ].
Other community variables
Community social cohesion was significantly associated with a lower risk of post-traumatic stress disorder symptom development [ 35 ], and this was apparent even whilst controlling for depressive symptoms at baseline and disaster impact variables (e.g. loss of family member or housing damage) [ 36 ]. Similarly, sense of community, community connectedness, social support at the community level and neighbourhood connectedness all provided protective benefits for a range of mental health, wellbeing and recovery variables, including: depression [ 53 ], subjective wellbeing (in older adults only) [ 43 ], psychological distress [ 47 ], happiness [ 44 ] and life satisfaction [ 53 ].
Research has also concluded that community level social support is protective against mild mood and anxiety disorder, but only for individuals who have had no previous disaster experience [ 48 ]. Additionally, a study which separated SC into social cohesion and social participation concluded that at a community level, social cohesion is protective against depression [ 49 ] whereas social participation at community level is associated with an increased risk of depression amongst women [ 49 ].
What is the impact of Infectious disease outbreaks / disasters and emergencies on community resilience?
From a cross-sectional perspective, research has indicated that disasters and emergencies can have a negative effect on certain types of SC. Specifically, cognitive SC has been found to be impacted by disaster impact, whereas structural SC has gone unaffected [ 45 ]. Disaster impact has also been shown to have a negative effect on community relationships more generally [ 52 ].
Additionally, of the eight studies which collected data at multiple time points [ 35 , 36 , 41 , 42 , 47 , 49 , 56 , 60 ], three reported the effect of a disaster on the level of SC within a community [ 40 , 42 , 49 ]. All three of these studies concluded that disasters may have a negative impact on the levels of SC within a community. The first study found that the Deepwater Horizon oil spill had a negative effect on SC and social support, and this in turn explained an overall increase in the levels of depression within the community [ 40 ]. A possible explanation for the negative effect lays in ‘corrosive communities’, known for increased social conflict and reduced social support, that are sometimes created following oil spills [ 40 ]. It is proposed that corrosive communities often emerge due to a loss of natural resources that bring social groups together (e.g., for recreational activities), as well as social disparity (e.g., due to unequal distribution of economic impact) becoming apparent in the community following disaster [ 40 ]. The second study found that SC (in the form of social cohesion, informal socialising and social participation) decreased after the 2011 earthquake and tsunami in Japan; it was suggested that this change correlated with incidence of cognitive decline [ 42 ]. However, the third study reported more mixed effects based on physical circumstances of the communities’ natural environment: Following an earthquake, those who lived in mountainous areas with an initial high level of pre-community SC saw a decrease in SC post disaster [ 49 ]. However, communities in flat areas (which were home to younger residents and had a higher population density) saw an increase in SC [ 49 ]. It was proposed that this difference could be due to the need for those who lived in mountainous areas to seek prolonged refuge due to subsequent landslides [ 49 ].
What types of intervention enhance CR and SC and protect survivors?
There were mixed effects across the 26 retained papers when examining the effect of CR and SC on mental wellbeing. However, there is evidence that an increase in SC [ 56 , 57 ], with a focus on cognitive SC [ 57 ], namely by: building social networks [ 45 , 51 , 53 ], enhancing feelings of social cohesion [ 35 , 36 ] and promoting a sense of community [ 53 ], can result in an increase in CR and potentially protect survivors’ wellbeing and mental health following a disaster. An increase in SC may also aid in decreasing the need for individual psychological interventions in the aftermath of a disaster [ 55 ]. As a result, recommendations and suggested methods to bolster CR and SC from the retained papers have been extracted and separated into general methods, preparedness and policy level implementation.
General methods
Suggested methods to build SC included organising recreational activity-based groups [ 44 ] to broaden [ 51 , 53 ] and preserve current social networks [ 42 ], introducing initiatives to increase social cohesion and trust [ 51 ], and volunteering to increase the number of social ties between residents [ 59 ]. Research also notes that it is important to take a ‘no one left behind approach’ when organising recreational and social community events, as failure to do so could induce feelings of isolation for some members of the community [ 49 ]. Furthermore, gender differences should also be considered as research indicates that males and females may react differently to community level SC (as evidence suggests males are instead more impacted by individual level SC; in comparison to women who have larger and more diverse social networks [ 49 ]). Therefore, interventions which aim to raise community level social participation, with the aim of expanding social connections and gaining support, may be beneficial [ 42 , 47 ].
Preparedness
In order to prepare for disasters, it may be beneficial to introduce community-targeted methods or interventions to increase levels of SC and CR as these may aid in ameliorating the consequences of a public health emergency or disaster [ 57 ]. To indicate which communities have low levels of SC, one study suggests implementing a 3-item scale of social cohesion to map areas and target interventions [ 42 ].
It is important to consider that communities with a high level of SC may have a lower level of risk perception, due to the established connections and supportive network they have with those around them [ 61 ]. However, for the purpose of preparedness, this is not ideal as perception of risk is a key factor when seeking to encourage behavioural adherence. This could be overcome by introducing communication strategies which emphasise the necessity of social support, but also highlights the need for additional measures to reduce residual risk [ 59 ]. Furthermore, support in the form of financial assistance to foster current community initiatives may prove beneficial to rural areas, for example through the use of an asset-based community development framework [ 52 ].
Policy level
At a policy level, the included papers suggest a range of ways that CR and SC could be bolstered and used. These include: providing financial support for community initiatives and collective coping strategies, (e.g. using asset-based community development [ 52 ]); ensuring policies for long-term recovery focus on community sustainable development (e.g. community festival and community centre activities) [ 44 ]; and development of a network amongst cooperative corporations formed for reconstruction and to organise self-help recovery sessions among residents of adjacent areas [ 58 ].
This scoping review sought to synthesise literature concerning the role of SC and CR during public health emergencies and disasters. Specifically, in this review we have examined: the methods used to measure CR and SC; the impact of CR and SC on mental wellbeing during disasters and emergencies; the impact of disasters and emergencies on CR and SC; and the types of interventions which can be used to enhance CR. To do this, data was extracted from 26 peer-reviewed journal articles. From this synthesis, several key themes have been identified, which can be used to develop guidelines and recommendations for deploying CR and SC in a public health emergency or disaster context. These key themes and resulting recommendations are summarised below.
Firstly, this review established that there is no consistent or standardised approach to measuring CR or SC within the general population. This finding is consistent with a review conducted by the World Health Organization which concludes that despite there being a number of frameworks that contain indicators across different determinants of health, there is a lack of consensus on priority areas for measurement and no widely accepted indicator [ 27 ]. As a result, there are many measures of CR and SC apparent within the literature (e.g., [ 62 , 63 ]), an example of a developed and validated measure is provided by Sherrieb, Norris and Galea [ 64 ]. Similarly, the definitions of CR and SC differ widely between researchers, which created a barrier to comparing and summarising information. Therefore, future research could seek to compare various interpretations of CR and to identify any overlapping concepts. However, a previous systemic review conducted by Patel et al. (2017) concludes that there are nine core elements of CR (local knowledge, community networks and relationships, communication, health, governance and leadership, resources, economic investment, preparedness, and mental outlook), with 19 further sub-elements therein [ 30 ]. Therefore, as CR is a multi-dimensional construct, the implications from the findings are that multiple aspects of social infrastructure may need to be considered.
Secondly, our synthesis of research concerning the role of CR and SC for ensuring mental health and wellbeing during, or following, a public health emergency or disaster revealed mixed effects. Much of the research indicates either a generally protective effect on mental health and wellbeing, or no effect; however, the literature demonstrates some potential for a high level of CR/SC to backfire and result in a negative effect for populations during, or following, a public health emergency or disaster. Considered together, our synthesis indicates that cognitive SC is the only facet of SC which was perceived as universally protective across all retained papers. This is consistent with a systematic review which also concludes that: (a) community level cognitive SC is associated with a lower risk of common mental disorders, while; (b) community level structural SC had inconsistent effects [ 65 ].
Further examination of additional data extracted from studies which found that CR/SC had a negative effect on mental health and wellbeing revealed no commonalities that might explain these effects (Please see Supplementary file 5 for additional information)
One potential explanation may come from a retained paper which found that high levels of SC result in an increase in stress level immediately post disaster [ 41 ]. This was suggested to be due to individuals having greater burdens due to wishing to help and support their wide networks as well as themselves. However, as time passes the levels of SC allow the community to come together and recover at a faster rate [ 41 ]. As this was the only retained paper which produced this finding, it would be beneficial for future research to examine boundary conditions for the positive effects of CR/SC; that is, to explore circumstances under which CR/SC may be more likely to put communities at greater risk. This further research should also include additional longitudinal research to validate the conclusions drawn by [ 41 ] as resilience is a dynamic process of adaption.
Thirdly, disasters and emergencies were generally found to have a negative effect on levels of SC. One retained paper found a mixed effect of SC in relation to an earthquake, however this paper separated participants by area in which they lived (i.e., mountainous vs. flat), which explains this inconsistent effect [ 49 ]. Dangerous areas (i.e. mountainous) saw a decrease in community SC in comparison to safer areas following the earthquake (an effect the authors attributed to the need to seek prolonged refuge), whereas participants from the safer areas (which are home to younger residents with a higher population density) saw an increase in SC [ 49 ]. This is consistent with the idea that being able to participate socially is a key element of SC [ 12 ]. Overall, however, this was the only retained paper which produced a variable finding in relation to the effect of disaster on levels of CR/SC.
Finally, research identified through our synthesis promotes the idea of bolstering SC (particularly cognitive SC) and cohesion in communities likely to be affected by disaster to improve levels of CR. This finding provides further understanding of the relationship between CR and SC; an association that has been reported in various articles seeking to provide conceptual frameworks (e.g., [ 66 , 67 ]) as well as indicator/measurement frameworks [ 27 ]. Therefore, this could be done by creating and promoting initiatives which foster SC and create bonds within the community. Papers included in the current review suggest that recreational-based activity groups and volunteering are potential methods for fostering SC and creating community bonds [ 44 , 51 , 59 ]. Similarly, further research demonstrates that feelings of social cohesion are enhanced by general social activities (e.g. fairs and parades [ 18 ]). Also, actively encouraging activities, programs and interventions which enhance connectedness and SC have been reported to be desirable to increase CR [ 68 ]. This suggestion is supported by a recent scoping review of literature [ 67 ] examined community champion approaches for the COVID-19 pandemic response and recovery and established that creating and promoting SC focused initiatives within the community during pandemic response is highly beneficial [ 67 ]. In terms of preparedness, research states that it may be beneficial for levels of SC and CR in communities at risk to be assessed, to allow targeted interventions where the population may be at most risk following an incident [ 42 , 44 ]. Additionally, from a more critical perspective, we acknowledge that ‘resilience’ can often be perceived as a focus on individual capacity to adapt to adversity rather than changing or mitigating the causes of adverse conditions [ 69 , 70 ]. Therefore, CR requires an integrated system approach across individual, community and structural levels [ 17 ]. Also, it is important that community members are engaged in defining and agreeing how community resilience is measured [ 27 ] rather than it being imposed by system leads or decision-makers.
In the aftermath of the pandemic, is it expected that there will be long-term repercussions both from an economic [ 8 ] and a mental health perspective [ 71 ]. Furthermore, the findings from this review suggest that although those in areas with high levels of SC may be negatively affected in the acute stage, as time passes, they have potential to rebound at a faster rate than those with lower levels of SC. Ongoing evaluation of the effectiveness of current initiatives as the COVID-19 pandemic progresses into a recovery phase will be invaluable for supplementing the evidence base identified through this review.
- Recommendations
As a result of this review, a number of recommendations are suggested for policy and practice during public health emergencies and recovery.
Future research should seek to establish a standardised and validated approach to measuring and defining CR and SC within communities. There are ongoing efforts in this area, for example [ 72 ]. Additionally, community members should be involved in the process of defining how CR is measured.
There should be an enhanced effort to improve preparedness for public health emergencies and disasters in local communities by gauging current levels of SC and CR within communities using a standardised measure. This approach could support specific targeting of populations with low levels of CR/SC in case of a disaster or public health emergency, whilst also allowing for consideration of support for those with high levels of CR (as these populations can be heavily impacted initially following a disaster). By distinguishing levels of SC and CR, tailored community-centred approaches could be implemented, such as those listed in a guide released by PHE in 2015 [ 73 ].
CR and SC (specifically cognitive SC) should be bolstered if communities are at risk of experiencing a disaster or public health emergency. This can be achieved by using interventions which aim to increase a sense of community and create new social ties (e.g., recreational group activities, volunteering). Additionally, when aiming to achieve this, it is important to be mindful of the risk of increased levels of CR/SC to backfire, as well as seeking to advocate an integrated system approach across individual, community and structural levels.
It is necessary to be aware that although communities with high existing levels of resilience / SC may experience short-term negative consequences following a disaster, over time these communities might be able to recover at a faster rate. It is therefore important to ensure that suitable short-term support is provided to these communities in the immediate aftermath of a public health emergency or disaster.
Robust evaluation of the community resilience initiatives deployed during the COVID-19 pandemic response is essential to inform the evidence base concerning the effectiveness of CR/ SC. These evaluations should continue through the response phase and into the recovery phase to help develop our understanding of the long-term consequences of such interventions.
Limitations
Despite this review being the first in this specific topic area, there are limitations that must be considered. Firstly, it is necessary to note that communities are generally highly diverse and the term ‘community’ in academic literature is a subject of much debate (see: [ 74 ]), therefore this must be considered when comparing and collating research involving communities. Additionally, the measures of CR and SC differ substantially across research, including across the 26 retained papers used in the current review. This makes the act of comparing and collating research findings very difficult. This issue is highlighted as a key outcome from this review, and suggestions for how to overcome this in future research are provided. Additionally, we acknowledge that there will be a relationship between CR & SC even where studies measure only at individual or community level. A review [ 75 ] on articulating a hypothesis of the link to health inequalities suggests that wider structural determinants of health need to be accounted for. Secondly, despite the final search strategy encompassing terms for both CR and SC, only one retained paper directly measured CR; thus, making the research findings more relevant to SC. Future research could seek to focus on CR to allow for a comparison of findings. Thirdly, the review was conducted early in the COVID-19 pandemic and so does not include more recent publications focusing on resilience specifically in the context of COVID-19. Regardless of this fact, the synthesis of, and recommendations drawn from, the reviewed studies are agnostic to time and specific incident and contain critical elements necessary to address as the pandemic moves from response to recovery. Further research should review the effectiveness of specific interventions during the COVID-19 pandemic for collation in a subsequent update to this current paper. Fourthly, the current review synthesises findings from countries with individualistic and collectivistic cultures, which may account for some variation in the findings. Lastly, despite choosing a scoping review method for ease of synthesising a wide literature base for use by public health emergency researchers in a relatively tight timeframe, there are disadvantages of a scoping review approach to consider: (1) quality appraisal of retained studies was not carried out; (2) due to the broad nature of a scoping review, more refined and targeted reviews of literature (e.g., systematic reviews) may be able to provide more detailed research outcomes. Therefore, future research should seek to use alternative methods (e.g., empirical research, systematic reviews of literature) to add to the evidence base on CR and SC impact and use in public health practice.
This review sought to establish: (1) How CR and SC are quantified in research?; (2) The impact of community resilience on mental wellbeing?; (3) The impact of infectious disease outbreaks, disasters and emergencies on community resilience and social capital?; and, (4) What types of interventions enhance community resilience and social capital?. The chosen search strategy yielded 26 relevant papers from which we were able extract information relating to the aims of this review.
Results from the review revealed that CR and SC are not measured consistently across research. The impact of CR / SC on mental health and wellbeing during emergencies and disasters is mixed (with some potential for backlash), however the literature does identify cognitive SC as particularly protective. Although only a small number of papers compared CR or SC before and after a disaster, the findings were relatively consistent: SC or CR is negatively impacted by a disaster. Methods suggested to bolster SC in communities were centred around social activities, such as recreational group activities and volunteering. Recommendations for both research and practice (with a particular focus on the ongoing COVID-19 pandemic) are also presented.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Social Capital
Zortea TC, Brenna CT, Joyce M, McClelland H, Tippett M, Tran MM, et al. The impact of infectious disease-related public health emergencies on suicide, suicidal behavior, and suicidal thoughts. Crisis. 2020;42(6):474–87.
Article PubMed PubMed Central Google Scholar
Davis JR, Wilson S, Brock-Martin A, Glover S, Svendsen ER. The impact of disasters on populations with health and health care disparities. Disaster Med Pub Health Prep. 2010;4(1):30.
Article Google Scholar
Francescutti LH, Sauve M, Prasad AS. Natural disasters and healthcare: lessons to be learned. Healthc Manage Forum. 2017;30(1):53–5.
Article PubMed Google Scholar
Jones L, Palumbo D, Brown D. Coronavirus: How the pandemic has changed the world economy. BBC News; 2021. Accessible at: https://www.bbc.co.uk/news/business-51706225 .
Below R, Wallemacq P. Annual disaster statistical review 2017. Brussels: CRED, Centre for Research on the Epidemiology of Disasters; 2018.
Google Scholar
Qiu W, Chu C, Mao A, Wu J. The impacts on health, society, and economy of SARS and H7N9 outbreaks in China: a case comparison study. J Environ Public Health. 2018;2018:2710185.
Worldometer. COVID-19 coronavirus pandemic. 2021.
Harari D, Keep M. Coronavirus: economic impact house of commons library. Briefing Paper (Number 8866); 2021. Accessible at: https://commonslibrary.parliament.uk/research-briefings/cbp-8866/ .
Nabavi N. Covid-19: pandemic will cast a long shadow on mental health, warns England’s CMO. BMJ. 2021;373:n1655.
Ziglio E. Strengthening resilience: a priority shared by health 2020 and the sustainable development goals. No. WHO/EURO: 2017-6509-46275-66939. World Health Organization; Regional Office for Europe; 2017.
Asadzadeh A, Kotter T, Salehi P, Birkmann J. Operationalizing a concept: the systematic review of composite indicator building for measuring community disaster resilience. Int J Disaster Risk Reduct. 2017;25:147.
Sherrieb K, Norris F, Galea S. Measuring capacities for community resilience. Soc Indicators Res. 2010;99(2):227.
Poortinga W. Community resilience and health: the role of bonding, bridging, and linking aspects of social capital. Health Place. 2011;18(2):286–95.
Ferlander S. The importance of different forms of social capital for health. Acta Sociol. 2007;50(2):115–28.
Nakagawa Y, Shaw R. Social capital: a missing link to disaster recovery. Int J Mass Emerge Disasters. 2004;22(1):5–34.
Grootaert C, Narayan D, Jones VN, Woolcock M. Measuring social capital: an integrated questionnaire. Washington, DC: World Bank Working Paper, No. 18; 2004.
Adler PS, Kwon SW. Social capital: prospects for a new concept. Acad Manage Rev. 2002;27(1):17–40.
Aldrich DP, Meyer MA. Social capital and community resilience. Am Behav Sci. 2015;59(2):254–69.
Rodriguez-Llanes JM, Vos F, Guha-Sapir D. Measuring psychological resilience to disasters: are evidence-based indicators an achievable goal? Environ Health. 2013;12(1):115.
De Silva MJ, McKenzie K, Harpham T, Huttly SR. Social capital and mental Illness: a systematic review. J Epidemiol Community Health. 2005;59(8):619–27.
Bonanno GA, Galea S, Bucciarelli A, Vlahov D. Psychological resilience after disaster: New York City in the aftermath of the september 11th terrorist attack. Psychol Sci. 2006;17(3):181.
World Health Organization. Health 2020: a European policy framework and strategy for the 21st century. World Health Organization. Regional Office for Europe; 2013.
Public Health England. Community-Centred Public Health: Taking a Whole System Approach. 2020.
SPI-B. The role of Community Champion networks to increase engagement in the context of COVID19: Evidence and best practice. 2021.
Public Health England. Community champions: A rapid scoping review of community champion approaches for the pandemic response and recovery. 2021.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
World Health Organisation. WHO health evidence network synthesis report: what quantitative and qualitative methods have been developed to measure health-related community resilience at a national and local level. 2018.
Hall C, Williams N, Gauntlett L, Carter H, Amlôt R, Peterson L et al. Findings from systematic review of public perceptions and responses. PROACTIVE EU. Deliverable 1.1. 2019. Accessible at: https://proactive-h2020.eu/wp-content/uploads/2021/04/PROACTIVE_20210312_D1.1_V5_PHE_Systematic-Review-of-Public-Perceptions-and-Responses_revised.pdf .
Weston D, Ip A, Amlôt R. Examining the application of behaviour change theories in the context of Infectious disease outbreaks and emergency response: a review of reviews. BMC Public Health. 2020;20(1):1483.
Article PubMed PubMed Central CAS Google Scholar
Patel SS, Rogers MB, Amlôt R, Rubin GJ. What do we mean by ‘community resilience’? A systematic literature review of how it is defined in the literature. PLoS Curr. 2017;9:ecurrents.dis.db775aff25efc5ac4f0660ad9c9f7db2.
PubMed PubMed Central Google Scholar
Brooks SK, Weston D, Wessely S, Greenberg N. Effectiveness and acceptability of brief psychoeducational interventions after potentially traumatic events: a systematic review. Eur J Psychotraumatology. 2021;12(1):1923110.
Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review-a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy. 2005;10(1_suppl):21–34.
Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:1–8.
Bearman M, Dawson P. Qualitative synthesis and systematic review in health professions education. Med Educ. 2013;47(3):252–60.
Heid AR, Pruchno R, Cartwright FP, Wilson-Genderson M. Exposure to Hurricane Sandy, neighborhood collective efficacy, and post-traumatic stress symptoms in older adults. Aging Ment Health. 2017;21(7):742–50.
Hikichi H, Aida J, Tsuboya T, Kondo K, Kawachi I. Can community social cohesion prevent posttraumatic stress disorder in the aftermath of a disaster? A natural experiment from the 2011 Tohoku Earthquake and tsunami. Am J Epidemiol. 2016;183(10):902–10.
Lee J, Blackmon BJ, Cochran DM, Kar B, Rehner TA, Gunnell MS. Community resilience, psychological resilience, and depressive symptoms: an examination of the Mississippi Gulf Coast 10 years after Hurricane Katrina and 5 years after the Deepwater Horizon oil spill. Disaster med. 2018;12(2):241–8.
Lee J, Blackmon BJ, Lee JY, Cochran DM Jr, Rehner TA. An exploration of posttraumatic growth, loneliness, depression, resilience, and social capital among survivors of Hurricane Katrina and the deepwater Horizon oil spill. J Community Psychol. 2019;47(2):356–70.
Lowe SR, Sampson L, Gruebner O, Galea S. Psychological resilience after Hurricane Sandy: the influence of individual- and community-level factors on mental health after a large-scale natural disaster. PLoS One. 2015;10(5):e0125761.
Rung AL, Gaston S, Robinson WT, Trapido EJ, Peters ES. Untangling the disaster-depression knot: the role of social ties after deepwater Horizon. Soc Sci Med. 2017;177:19–26.
Weil F, Lee MR, Shihadeh ES. The burdens of social capital: how socially-involved people dealt with stress after Hurricane Katrina. Soc Sci Res. 2012;41(1):110–9.
Hikichi H, Aida J, Matsuyama Y, Tsuboya T, Kondo K, Kawachi I. Community-level social capital and cognitive decline after a Natural Disaster: a natural experiment from the 2011 Great East Japan Earthquake and Tsunami. Soc Sci Med. 2018;257:111981.
Lau AL, Chi I, Cummins RA, Lee TM, Chou KL, Chung LW. The SARS (severe acute respiratory syndrome) pandemic in Hong Kong: effects on the subjective wellbeing of elderly and younger people. Aging Ment Health. 2008;12(6):746–60.
Sun Y, Yan T. The use of public health indicators to assess individual happiness in post-disaster recovery. Int J Environ Res Public Health. 2019;16(21):4101.
Wong H, Huang Y, Fu Y, Zhang Y. Impacts of structural social capital and cognitive social capital on the psychological status of survivors of the yaan Earthquake. Appl Res Qual Life. 2018;14:1411–33.
Xiao H, Zhang Y, Kong D, Li S, Yang N. Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Med Sci Monit. 2020;26:e923921.
PubMed PubMed Central CAS Google Scholar
Matsuyama Y, Aida J, Hase A, Sato Y, Koyama S, Tsuboya T, et al. Do community- and individual-level social relationships contribute to the mental health of disaster survivors? A multilevel prospective study after the great East Japan earthquake. Soc Sci Med. 2016;151:187–95.
Ozaki A, Horiuchi S, Kobayashi Y, Inoue M, Aida J, Leppold C, Yamaoka K. Beneficial roles of social support for mental health vary in the Japanese population depending on disaster experience: a nationwide cross-sectional study. Tohoku J Exp Med. 2018;246(4):213–23.
Sato K, Amemiya A, Haseda M, Takagi D, Kanamori M, Kondo K, et al. Post-disaster changes in Social Capital and Mental Health: a natural experiment from the 2016 Kumamoto Earthquake. Am J Epidemiol. 2020;189(9):910–21.
Tsuchiya N, Nakaya N, Nakamura T, Narita A, Kogure M, Aida J, Tsuji I, Hozawa A, Tomita H. Impact of social capital on psychological distress and interaction with house destruction and displacement after the great East Japan earthquake of 2011. J Neuropsychiatry Clin Neurosci. 2017;71(1):52–60.
Brockie L, Miller E. Understanding older adults’ resilience during the Brisbane floods: social capital, life experience, and optimism. Disaster Med Pub Health Prep. 2017;11(1):72–9.
Caldwell K, Boyd CP. Coping and resilience in farming families affected by drought. Rural Remote Health. 2009;9(2):1088.
PubMed Google Scholar
Huang Y, Tan NT, Liu J. Support, sense of community, and psychological status in the survivors of the Yaan earthquake. J Community Psychol. 2016;44(7):919–36.
Wind T, Fordham M, Komproe H. Social capital and post-disaster mental health. Glob Health Action. 2011;4(1):6351.
Wind T, Komproe IH. The mechanisms that associate community social capital with post-disaster mental health: a multilevel model. Soc Sci Med. 2012;75(9):1715–20.
Hogg D, Kingham S, Wilson TM, Ardagh M. The effects of spatially varying earthquake impacts on mood and anxiety symptom treatments among long-term Christchurch residents following the 2010/11 Canterbury Earthquakes, New Zealand. Health Place. 2016;41:78–88.
Flores EC, Carnero AM, Bayer AM. Social capital and chronic post-traumatic stress disorder among survivors of the 2007 earthquake in Pisco, Peru. Soc Sci Med. 2014;101:9–17.
Rafiey H, Alipour F, LeBeau R, Salimi Y, Ahmadi S. Exploring the buffering role of social capital in the development of posttraumatic stress symptoms among Iranian earthquake survivors. Psychol Trauma. 2019;14(6):1040–6.
Babcicky P, Seebauer S. The two faces of social capital in private Flood mitigation: opposing effects on risk perception, self-efficacy and coping capacity. J Risk Res. 2017;20(8):1017–37.
Bakic H, Ajdukovic D. Stability and change post-disaster: dynamic relations between individual, interpersonal and community resources and psychosocial functioning. Eur J Psychotraumatol. 2019;10(1):1614821.
Rogers RW. A protection motivation theory of fear appeals and attitude change. J Psychol. 1975;91(1):93–114.
Lindberg K, Swearingen T. A reflective thrive-oriented community resilience scale. Am J Community Psychol. 2020;65(3–4):467–78.
Leykin D, Lahad M, Cohen O, Goldberg A, Aharonson-Daniel L. Conjoint community resiliency assessment measure-28/10 items (CCRAM28 and CCRAM10): a self-report tool for assessing community resilience. Am J Community Psychol. 2013;52:313–23.
Sherrieb K, Norris FH, Galea S. Measuring capacities for community resilience. Soc Indic Res. 2010;99:227–47.
Ehsan AM, De Silva MJ. Social capital and common mental disorder: a systematic review. J Epidemiol Community Health. 2015;69(10):1021–8.
Pfefferbaum B, Van Horn RL, Pfefferbaum RL. A conceptual framework to enhance community resilience using social capital. Clin Soc Work J. 2017;45(2):102–10.
Carmen E, Fazey I, Ross H, Bedinger M, Smith FM, Prager K, et al. Building community resilience in a context of climate change: the role of social capital. Ambio. 2022;51(6):1371–87.
Humbert C, Joseph J. Introduction: the politics of resilience: problematising current approaches. Resilience. 2019;7(3):215–23.
Tanner T, Bahadur A, Moench M. Challenges for resilience policy and practice. Working paper: 519. 2017.
Vadivel R, Shoib S, El Halabi S, El Hayek S, Essam L, Bytyçi DG. Mental health in the post-COVID-19 era: challenges and the way forward. Gen Psychiatry. 2021;34(1):e100424.
Article CAS Google Scholar
Pryor M. Social Capital Harmonised Standard. London: Government Statistical Service. 2021. Accessible at: https://gss.civilservice.gov.uk/policystore/social-capital/ .
Public Health England NE. A guide to community-centred approaches for health and wellbeing. 2015.
Hawe P. Capturing the meaning of ‘community’ in community intervention evaluation: some contributions from community psychology. Health Promot Int. 1994;9(3):199–210.
Uphoff EP, Pickett KE, Cabieses B, Small N, Wright J. A systematic review of the relationships between social capital and socioeconomic inequalities in health: a contribution to understanding the psychosocial pathway of health inequalities. Int J Equity Health. 2013;12:1–12.
Download references
Acknowledgements
Not applicable.
This study was supported by the National Institute for Health Research Research Unit (NIHR HPRU) in Emergency Preparedness and Response, a partnership between Public Health England, King’s College London and the University of East Anglia. The views expressed are those of the author(s) and not necessarily those of the NIHR, Public Health England, the UK Health Security Agency or the Department of Health and Social Care [Grant number: NIHR20008900]. Part of this work has been funded by the Office for Health Improvement and Disparities, Department of Health and Social Care, as part of a Collaborative Agreement with Leeds Beckett University.
Author information
Authors and affiliations.
Behavioural Science and Insights Unit, Evaluation & Translation Directorate, Science Group, UK Health Security Agency, Porton Down, Salisbury, SP4 0JG, UK
C. E. Hall, H. Wehling, R. Amlôt & D. Weston
Health Protection Research Unit, Institute of Psychology, Psychiatry and Neuroscience, King’s College London, 10 Cutcombe Road, London, SE5 9RJ, UK
C. E. Hall, S. K. Brooks & N. Greenberg
School of Health and Community Studies, Leeds Beckett University, Portland Building, PD519, Portland Place, Leeds, LS1 3HE, UK
J. Stansfield & J. South
King’s Centre for Military Health Research, Institute of Psychology, Psychiatry and Neuroscience, King’s College London, 10 Cutcombe Road, London, SE5 9RJ, UK
N. Greenberg
You can also search for this author in PubMed Google Scholar
Contributions
DW, JSo and JSt had the main idea for the review. The search strategy and eligibility criteria were devised by CH, DW, JSo and JSt. CH conducted the database searches. CH and DW conducted duplicate, title and abstract and full text screening in accordance with inclusion criteria. CH conducted data extraction, CH and DW carried out the analysis and drafted the initial manuscript. All authors provided critical revision of intellectual content. All authors approved the final manuscript.
Authors’ information
Corresponding author.
Correspondence to D. Weston .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., additional file 2., additional file 3., additional file 4., additional file 5., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hall, C.E., Wehling, H., Stansfield, J. et al. Examining the role of community resilience and social capital on mental health in public health emergency and disaster response: a scoping review. BMC Public Health 23 , 2482 (2023). https://doi.org/10.1186/s12889-023-17242-x
Download citation
Received : 04 April 2022
Accepted : 16 November 2023
Published : 12 December 2023
DOI : https://doi.org/10.1186/s12889-023-17242-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Community cohesion
- Public health emergency
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Talk to our experts
1800-120-456-456
- Mental Health Essay

Essay on Mental Health
According to WHO, there is no single 'official' definition of mental health. Mental health refers to a person's psychological, emotional, and social well-being; it influences what they feel and how they think, and behave. The state of cognitive and behavioural well-being is referred to as mental health. The term 'mental health' is also used to refer to the absence of mental disease.
Mental health means keeping our minds healthy. Mankind generally is more focused on keeping their physical body healthy. People tend to ignore the state of their minds. Human superiority over other animals lies in his superior mind. Man has been able to control life due to his highly developed brain. So, it becomes very important for a man to keep both his body and mind fit and healthy. Both physical and mental health are equally important for better performance and results.
Importance of Mental Health
An emotionally fit and stable person always feels vibrant and truly alive and can easily manage emotionally difficult situations. To be emotionally strong, one has to be physically fit too. Although mental health is a personal issue, what affects one person may or may not affect another; yet, several key elements lead to mental health issues.
Many emotional factors have a significant effect on our fitness level like depression, aggression, negative thinking, frustration, and fear, etc. A physically fit person is always in a good mood and can easily cope up with situations of distress and depression resulting in regular training contributing to a good physical fitness standard.
Mental fitness implies a state of psychological well-being. It denotes having a positive sense of how we feel, think, and act, which improves one’s ability to enjoy life. It contributes to one’s inner ability to be self-determined. It is a proactive, positive term and forsakes negative thoughts that may come to mind. The term mental fitness is increasingly being used by psychologists, mental health practitioners, schools, organisations, and the general population to denote logical thinking, clear comprehension, and reasoning ability.
Negative Impact of Mental Health
The way we physically fall sick, we can also fall sick mentally. Mental illness is the instability of one’s health, which includes changes in emotion, thinking, and behaviour. Mental illness can be caused due to stress or reaction to a certain incident. It could also arise due to genetic factors, biochemical imbalances, child abuse or trauma, social disadvantage, poor physical health condition, etc. Mental illness is curable. One can seek help from the experts in this particular area or can overcome this illness by positive thinking and changing their lifestyle.
Regular fitness exercises like morning walks, yoga, and meditation have proved to be great medicine for curing mental health. Besides this, it is imperative to have a good diet and enough sleep. A person needs 7 to 9 hours of sleep every night on average. When someone is tired yet still can't sleep, it's a symptom that their mental health is unstable. Overworking oneself can sometimes result in not just physical tiredness but also significant mental exhaustion. As a result, people get insomnia (the inability to fall asleep). Anxiety is another indicator.
There are many symptoms of mental health issues that differ from person to person and among the different kinds of issues as well. For instance, panic attacks and racing thoughts are common side effects. As a result of this mental strain, a person may experience chest aches and breathing difficulties. Another sign of poor mental health is a lack of focus. It occurs when you have too much going on in your life at once, and you begin to make thoughtless mistakes, resulting in a loss of capacity to focus effectively. Another element is being on edge all of the time.
It's noticeable when you're quickly irritated by minor events or statements, become offended, and argue with your family, friends, or co-workers. It occurs as a result of a build-up of internal irritation. A sense of alienation from your loved ones might have a negative influence on your mental health. It makes you feel lonely and might even put you in a state of despair. You can prevent mental illness by taking care of yourself like calming your mind by listening to soft music, being more social, setting realistic goals for yourself, and taking care of your body.
Surround yourself with individuals who understand your circumstances and respect you as the unique individual that you are. This practice will assist you in dealing with the sickness successfully. Improve your mental health knowledge to receive the help you need to deal with the problem. To gain emotional support, connect with other people, family, and friends. Always remember to be grateful in life. Pursue a hobby or any other creative activity that you enjoy.
What does Experts say
Many health experts have stated that mental, social, and emotional health is an important part of overall fitness. Physical fitness is a combination of physical, emotional, and mental fitness. Emotional fitness has been recognized as the state in which the mind is capable of staying away from negative thoughts and can focus on creative and constructive tasks.
He should not overreact to situations. He should not get upset or disturbed by setbacks, which are parts of life. Those who do so are not emotionally fit though they may be physically strong and healthy. There are no gyms to set this right but yoga, meditation, and reading books, which tell us how to be emotionally strong, help to acquire emotional fitness.
Stress and depression can lead to a variety of serious health problems, including suicide in extreme situations. Being mentally healthy extends your life by allowing you to experience more joy and happiness. Mental health also improves our ability to think clearly and boosts our self-esteem. We may also connect spiritually with ourselves and serve as role models for others. We'd also be able to serve people without being a mental drain on them.
Mental sickness is becoming a growing issue in the 21st century. Not everyone receives the help that they need. Even though mental illness is common these days and can affect anyone, there is still a stigma attached to it. People are still reluctant to accept the illness of mind because of this stigma. They feel shame to acknowledge it and seek help from the doctors. It's important to remember that "mental health" and "mental sickness" are not interchangeable.
Mental health and mental illness are inextricably linked. Individuals with good mental health can develop mental illness, while those with no mental disease can have poor mental health. Mental illness does not imply that someone is insane, and it is not anything to be embarrassed by. Our society's perception of mental disease or disorder must shift. Mental health cannot be separated from physical health. They both are equally important for a person.
Our society needs to change its perception of mental illness or disorder. People have to remove the stigma attached to this illness and educate themselves about it. Only about 20% of adolescents and children with diagnosable mental health issues receive the therapy they need.
According to research conducted on adults, mental illness affects 19% of the adult population. Nearly one in every five children and adolescents on the globe has a mental illness. Depression, which affects 246 million people worldwide, is one of the leading causes of disability. If mental illness is not treated at the correct time then the consequences can be grave.
One of the essential roles of school and education is to protect boys’ and girls' mental health as teenagers are at a high risk of mental health issues. It can also impair the proper growth and development of various emotional and social skills in teenagers. Many factors can cause such problems in children. Feelings of inferiority and insecurity are the two key factors that have the greatest impact. As a result, they lose their independence and confidence, which can be avoided by encouraging the children to believe in themselves at all times.
To make people more aware of mental health, 10th October is observed as World Mental Health. The object of this day is to spread awareness about mental health issues around the world and make all efforts in the support of mental health.
The mind is one of the most powerful organs in the body, regulating the functioning of all other organs. When our minds are unstable, they affect the whole functioning of our bodies. Being both physically and emotionally fit is the key to success in all aspects of life. People should be aware of the consequences of mental illness and must give utmost importance to keeping the mind healthy like the way the physical body is kept healthy. Mental and physical health cannot be separated from each other. And only when both are balanced can we call a person perfectly healthy and well. So, it is crucial for everyone to work towards achieving a balance between mental and physical wellbeing and get the necessary help when either of them falters.

- Open access
- Published: 08 April 2024
Preventing workplace mistreatment and improving workers’ mental health: a scoping review of the impact of psychosocial safety climate
- Mustapha Amoadu 1 ,
- Edward Wilson Ansah 1 &
- Jacob Owusu Sarfo 1
BMC Psychology volume 12 , Article number: 195 ( 2024 ) Cite this article
Metrics details
Work environment is rapidly evolving, unfortunately, it is also becoming increasingly hostile for workers due mostly to common psychosocial hazards. This situation is posing significant challenges for organisations to protect the psychological well-being of their workers. Hence, this review aims to map studies to understand the influence of psychosocial safety climate (PSC) on workplace mistreatment and mental health of workers.
The guidelines outlined by Arksey and O’Malley were adopted for this review. PubMed, Scopus, Web of Science, JSTOR, Google and Google Scholar were searched for relevant papers. Only peer-reviewed studies that measured PSC using PSC-12, PSC-8 or PSC-4 were included in this review.
Thirty-eight studies met the inclusion criteria. This review found that PSC has a negative association with workplace mistreatment such as bullying, harassment, violence, discrimination and abuse. Further, PSC has a positive association with psychological well-being, personal resilience and hope. Low level organisational PSC also promotes psychological distress, stress, depression, cognitive weariness and emotional exhaustion. The buffering effect of PSC is well-established. Moreover, PSC mediates the association between health-centric leadership and workers’ psychological health problems. The inverse relationship between PSC and depressive symptoms was stronger for females than males.
Organisations should prioritise training and development of supervisors to enhance their supportive skills, encourage respectful behaviour, encourage the use of resources promote open and bottom-up communication and provide guidance on conflict resolution. By promoting a high PSC context, organisations can create a culture that discourages mistreatment, leading to increased employee well-being, job satisfaction, and productivity.
Peer Review reports
Introduction
Work environment globally is rapidly evolving, but it is also becoming increasingly hostile for workers. Recent evidence from the International Labour Organisation (ILO) indicates that about 23% of workers have experienced violence and harassment at work, encompassing physical, psychological, and sexual abuse [ 1 ]. This disturbing statistic reveals that more than one in five people in employment have encountered workplace violence and harassment, posing significant challenges for organizations to protect the psychological well-being of their workforce. There is also a growing realization of the need to understand the influence of the psychosocial work environment on workplace mistreatment and mental health. The World Health Organisation (WHO) and ILO have jointly reported a global increase in occupational morbidity and mortality resulting from a poor psychosocial work environment [ 2 , 3 ], emphasising the importance of exploring the concept of psychosocial safety climate (PSC).
PSC is an organisational culture that prioritises workers’ psychological health and safety at the workplace [ 4 ]. Thus, PSC refers to the shared perceptions of workers concerning workplace policies, practices, and procedures that are designed to protect and promote their psychological well-being [ 5 ]. It encompasses a range of organisational factors including leadership commitment to workers’ well-being, job design, organisational justice, social support and overall climate of trust and respect at the workplace [ 6 ]. A high PSC context emphasises the importance of fostering a psychologically healthy work environment, where workers feel safe, supported, valued, treated fairly and respected [ 7 ], thus, lowering the tendency of mistreatment of workers.
Workplace mistreatment refers to any form of harmful, abusive, or disrespectful behaviour that occurs in the work environment [ 1 ] This includes but not limited to bullying, harassment, violence, abuse and discrimination [ 1 ]. Workplace mistreatment has gained significant research and policy attention due to its detrimental effects on both workers and organizations [ 1 ]. Victims of workplace mistreatment often experience poor mental health, job dissatisfaction and impaired productivity [ 8 ]. Recognising the crucial role of the PSC in mitigating workplace mistreatment and protecting workers’ mental health has become a pressing concern for researchers, industries and policymakers [ 8 ]. For over a decade of research into PSC, identifying and synthesising studies that have explored PSC in reducing workplace mistreatment and improving mental health is noteworthy. Thus, this scoping review aims at mapping existing studies to provide a comprehensive understanding of the influence of PSC on workplace mistreatment and mental health on workers. The purpose is to make recommendations for future research and systematic reviews. This review will also help organisations, managers and policymakers to develop evidence-based strategies and interventions that promote a PSC work-context that fosters a respectful and supportive work environment and safeguard workers’ psychological well-being. Also, this review aims to provide evidence that is useful in promoting a healthy and decent workplace that eliminates all forms of workplace mistreatment and mental health stressors.
The guidelines outlined by Arksey and O’Malley [ 9 ] were adopted for this scoping review: thus, identifying and stating the research questions, identifying relevant studies, studies selection, data collection, summary and synthesis of results and consultation. Therefore, we formulated research questions based on the Population, Concept and Context (PCC) framework. The following questions guided this scoping review:
What is the relationship between PSC and workplace mistreatment?
What is the relationship between PSC and mental health parameters?
What is the mediating and moderating role of PSC in improving workers’ mental health and reducing workplace mistreatment?
Search for relevant papers was conducted in four main databases (PubMed, Scopus, Web of Science, and JSTOR). Google and Google Scholar were explored for additional papers. Reference lists of eligible records were also checked for relevant papers. The authors created a search technique that used a combination of controlled vocabularies like Medical Subject Headings (MeSH). Keywords for each of the four major electronic databases (PubMed, Scopus, Web of Science and JSTOR) were also created to address the research questions and identify relevant literature. Table 1 presents the search strategy conducted in PubMed and other databases. The search strategies were informed by PCC. The context was not limited to a specific country or region since this review was given a global focus. The search strategy used in PubMed was then modified for search in other databases. The authors used three keywords in their search strategy (1) psychosocial safety climate, (2) workplace abuse and (3) mental health. The search for relevant papers started on March 12, 2023, and ended on July 1, 2023. Chartered librarians at the Sam Jonah Library, University of Cape Coast were consulted.
Mendeley software was used to remove duplicate records. Ten graduate students were trained and supervised by MA to screen titles and abstracts for full-text-eligible records. This was done to enhance efficiency in the screening process and allowed for a more thorough and expedited review of titles and abstracts to identify records eligible for full-text examination. Authors checked the reference list of full-text records to identify additional eligible records. Eligible full-text records were then screened independently by MA and JOS and supervised by EWA using the eligibility criteria presented in Table 2 . Weekly meetings were used to resolve disagreements identified during the screening process.
Data extraction was handled independently by two independent researchers (MA and JOS) and supervised by EWA. This was done to ensure that accurate and reliable data were extracted for this review. Disagreements during the data extraction phase were handled during weekly meetings. Authors extracted data on authors, the country where the study was conducted, year of publication, purpose of the study, study design, population, sample size, measure of PSC and study outcomes. Finally, thematic content analysis was conducted by the authors based on the research questions. The analysis involved identifying recurring themes relevant to the research questions. This process included organising and categorising data to extract meaningful patterns and insights from the extracted information. The search results, characteristics of reviewed studies and thematic analysis were presented.
Search results
Search conducted in the four main databases produced 4,621 records and additional 29 records were retrieved from Google and Google Scholar. The Mendeley software was used to remove 742 duplicate records. After title and abstract screening, 3,820 records were removed because they were not relevant to this review. Additional 5 records were retrieved through reference checking of eligible studies and 93 full-text records were screened for eligibility. Finally, 38 full-text records were included in this scoping review and the remaining 55 full-text records were removed because they did not report on variables of interest. The search results and screening process is presented in Fig. 1 .
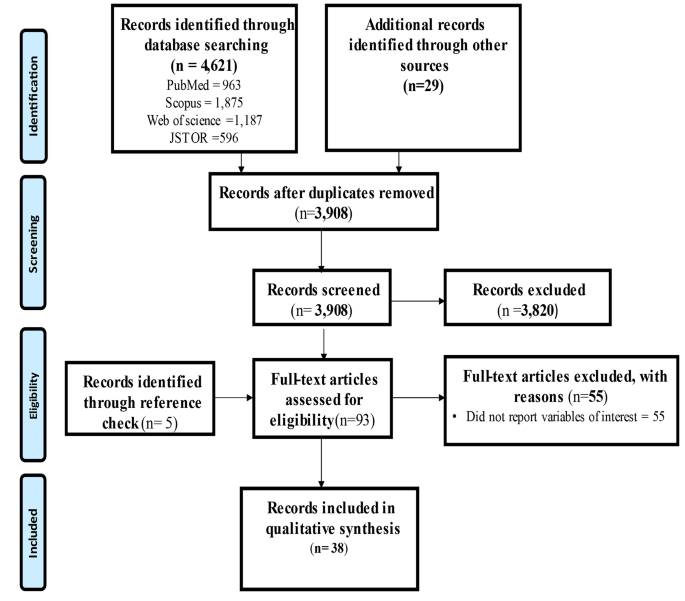
PRISMA flow diagram of search results and screening process
Characteristics of reviewed studies
Reviewed studies collectively sampled 53,733 workers. A cross-sectional survey design was mostly used in conducting these studies (See Fig. 2 for details). A few (6) of the studies were published in 2021 (See Fig. 3 for details), with about half (19) conducted in Australia (See details in Fig. 4 ). Most of the studies we reviewed sampled general working population (16) and healthcare providers (11) (See details in Fig. 5 ). Characteristics of reviewed studies are presented in Supplementary File (Table S1 ).
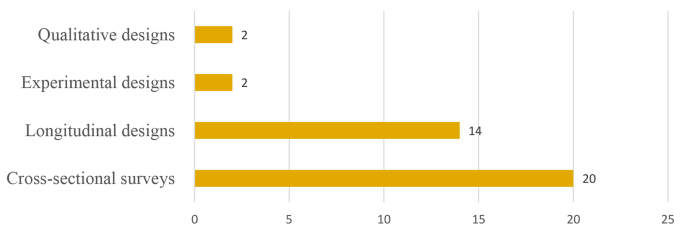
Study designs of reviewed studies
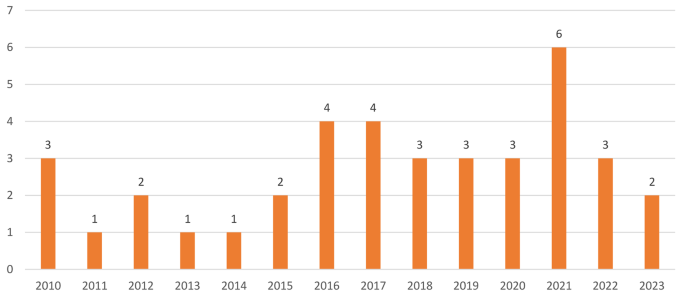
Year of publication of included studies
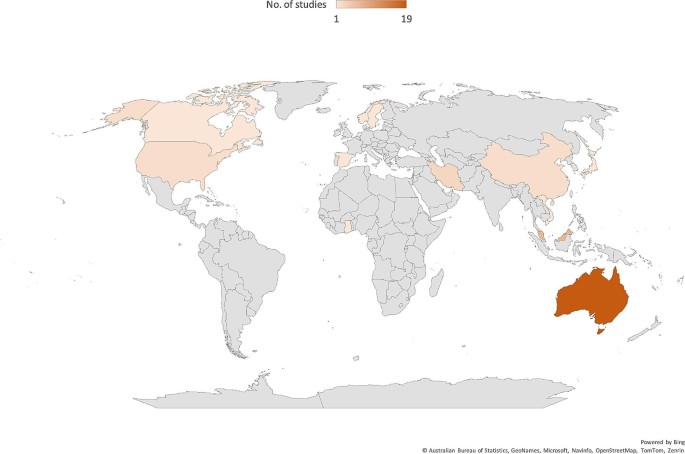
Map showing countries and continents where reviewed studies were conducted
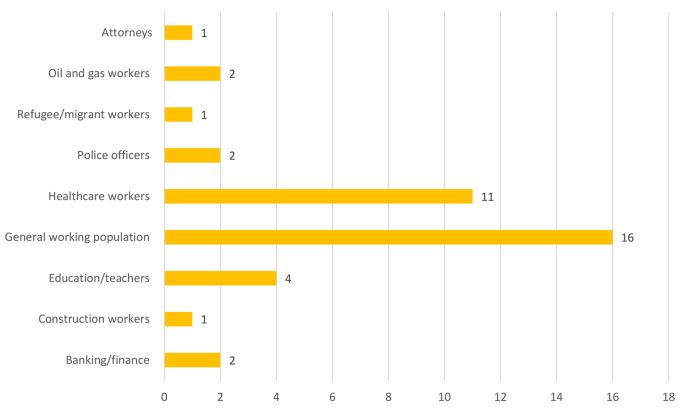
Occupational groups explored by reviewed studies
Influence of PSC on workplace mistreatment
Evidence indicates that PSC has a direct and significant influence on workplace mistreatment. For instance, reviewed studies reported that a high PSC work context provides a favourable work environment that helps eliminates or reduces workplace bullying among workers [ 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 ]. Also, workplace violence [ 8 , 10 ] and abuse [ 18 ] are common in a low PSC context. In addition, studies further highlighted that workplace harassment [ 10 , 11 ] and discrimination [ 18 ] are less common or eliminated in a high PSC context.
Influence of PSC on workers’ mental health
Evidence established that PSC directly improves workers’ mental health. For example, evidence is consistent that high PSC context improves psychological well-being [ 14 , 19 , 20 , 21 ] and reduces psychological distress [ 4 , 18 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 ]. Furthermore, it is indicated that low PSC work exposes workers to emotional exhaustion [ 4 , 16 , 22 , 25 , 30 , 31 , 32 ], stress [ 33 , 34 ], cognitive weariness [ 35 ] and depression [ 23 , 36 , 37 , 38 ]. For instance, a study reported that the inverse relationship between PSC and depressive symptoms was stronger for females than males [ 36 ]. Moreover, a high PSC context makes workers more assertive [ 39 ] and resilient [ 40 ] and presents opportunities for hope [ 40 ]. We present thematic analysis of the influence of PSC on workplace mistreatment and mental health in Table 3 .
Mediation and the buffering effect of PSC
The literature consistently confirms the buffering effect of PSC on various outcomes related to worker well-being and mistreatment. Yulita et al. [ 7 ]for example, found that in a high PSC context, job resources had a stronger impact on reducing psychological distress. Similarly, Lawrie et al. [ 41 ] demonstrated positive impact of job control on worker mindfulness which is enhanced in a high PSC work environment. Besides, Siami et al. [ 40 ] revealed that the association between supportive leadership and personal hope is strengthened in the presence of a high PSC. Hall et al. [ 42 ] showed that the effect of job demands on depression is diminished when workers perceive high PSC. Additionally, Loh et al. [ 43 ] found a negative impact of emotional demands on psychological well-being that is mitigated in a high PSC context.
Furthermore, it is indicated that the adverse association between workplace bullying, harassment, and psychological well-being is attenuated when workers perceive high PSC [ 11 ]. Thus, PSC has the capacity to reduce the impact of workplace bullying on post-traumatic disorder and work engagement [ 12 , 44 ] Kwan et al. [ 39 ] revealed that the positive association between bullying and neglect is diminished when a high PSC is perceived by workers. Moreover, PSC moderates the associations between role conflict and workplace bullying [ 17 ], role ambiguity and workplace bullying [ 17 ] and stigma and workplace bullying [ 15 ]. While a limited research attention is given, a study reported that PSC mediates the association between health-centric leadership and workers’ psychological health problems [ 26 ]. These findings collectively emphasize the crucial role of PSC in mitigating the negative consequences of mistreatment and enhancing workers’ well-being.
Workplace-specific findings
The findings from various studies reveal workplace-specific outcomes related to Psychosocial Safety Climate (PSC). In the education sector in Australia, PSC was associated with a reduction in psychological distress and emotional exhaustion among education workers [ 4 ]. Similarly, in Malaysia, among police officers, PSC buffered the effect of job resources on psychological distress [ 7 ]. Healthcare workers in China experienced a decrease in workplace violence in the presence of a positive PSC [ 8 ]. For the general working population in Australia, PSC was linked to a decrease in harassment, violence, and bullying [ 10 ]. In diverse settings, including police officers, the general working population, and refugees in Australia, PSC demonstrated a consistent negative association with workplace mistreatment such as bullying, harassment, violence, discrimination, and abuse [ 12 , 13 , 18 ]. Healthcare workers in both Australia and Malaysia reported improved psychological well-being in the presence of a high PSC context [ 19 ]. Construction workers in China showed enhanced mental well-being [ 20 ]. Various workplace settings, such as attorneys in the USA and oil and gas workers in Malaysia, exhibited a decrease in psychological distress with a positive PSC [ 27 , 28 ]. Notably, healthcare workers across different countries, including Iran, Australia, and Canada, experienced positive outcomes such as decreased emotional exhaustion and stress, emphasizing the universal impact of PSC in healthcare settings [ 22 , 30 , 35 ].
This review found that PSC has a negative association with workplace mistreatment such as bullying, harassment, violence, discrimination and abuse. Furthermore, we found that PSC has a positive association with psychological well-being, personal resilience and hope. Moreover, PSC has a negative association with psychological distress, stress, depression, cognitive weariness and emotional exhaustion. The buffering effect of PSC is well-established in the literature.
PSC has a negative association with workplace mistreatment. A high PSC work environment indicates that managers and supervisors are perceived as supportive, approachable and caring towards their workers. In such a work context, workers are more likely to feel protected, valued and respected [ 5 ]. Furthermore, such work context acts as a deterrent to workplace mistreatment including bullying and harassment because workers are more assertive at work [ 18 ]. Furthermore, when workers perceive their supervisors as supportive, they are likely to develop trust and respect among workers and towards their supervisors. This trust and respect may lead to positive interpersonal relationships between supervisors and workers, fostering a sense of fairness, partnership, and open communication [ 10 , 11 ]. In such a work context, discrimination and mistreatment are less likely to occur, since they contradict the principles of trust and respect. In a high PSC context, managers and supervisors are expected to exhibit positive behaviours to serve as role models for their colleagues and subordinates. When managers and supervisors exhibit respectful and inclusive behaviours, it serves as precedents for acceptable conduct at the workplace, reducing the occurrence of mistreatment [ 8 , 10 ]. In a high PSC work context, bottom-up communication is encouraged and supervisors are more likely to intervene and address workplace mistreatment, provide training on respectful behaviours and establish mechanisms for reporting incidents [ 5 ]. These communication and conflict resolution mechanisms do not only deter mistreatment but also provide a sense of security for workers.
Influence of PSC on mental health
PSC has a positive association with psychological well-being. In a high PSC context, workers are trained and encouraged to utilise essential resources capable of helping workers to cope effectively with the psychological and emotional demands of work. Furthermore, high PSC implies that supervisors provide emotional support, understanding and validation of their workers which helps buffer against stressors at the workplace [ 5 ]. Besides, the presence of supportive supervisors or management contributes to workers’ mental well-being by reducing feelings of isolation, enhancing self-esteem, and promoting a sense of belongingness [ 7 ]. Moreover, in a high PSC context, supervisors are more likely to be responsive to workers’ needs and concerns, providing workers with essential resources and guidance that alleviate psychological distress [ 33 , 34 ]. Thus, high PSC contexts encourage and empower workers by promoting assertiveness, resilience, and hope [ 39 ]. In such an environment, workers may feel more confident in expressing their needs, standing up for themselves, and seeking solutions to challenges. Consequently, this may lead to increased assertiveness, better coping mechanisms, and a more positive outlook on work-related issues [ 39 ].
The finding that the negative association between PSC and depressive symptoms is stronger for females than males highlight the potential of gender differences in the impact of PSC on mental health outcomes. This finding could be influenced by several variables including differences in socialisation, communication styles, and the importance of supportive relationships for women [ 36 ]. However, further research is needed to explore these gender-specific dynamics in more detail.
The buffering effects of PSC
In a high PSC environment, job resources including job control and supportive leadership, are perceived as more beneficial and impactful [ 5 ]. Thus, PSC acts as an amplifier, enhancing the positive effects of these resources on workers’ mental well-being [ 43 ]. When workers perceive a supportive work environment, they are more likely to utilise job resources that are more effective in reducing psychological distress, increasing mindfulness, fostering personal hope, and mitigating the negative impact of job demands on depression and emotional exhaustion [ 7 ]. A high PSC context would create a sense of psychological safety, where workers feel comfortable expressing their concerns, reporting mistreatment, and seeking essential support [ 5 ]. This situation creates an environment where bullying, harassment, and other forms of workplace mistreatment are less tolerated, and thus, less occur [ 4 ]. The perception of high PSC buffers the adverse effect of workplace mistreatment on psychological well-being, post-traumatic disorder, stress, cognitive weariness and other psychological health problems to improve productivity and organisational image [ 4 ].
PSC in specific workplaces
The workplace-specific findings underscore the intricate interplay between PSC and various professional domains, shedding light on the nuanced dynamics within diverse work settings [ 12 , 35 ]. In the education sector, the observed reduction in psychological distress and emotional exhaustion among education workers in the presence of a positive PSC speaks to the profound impact of a supportive climate on educators’ well-being [ 4 ]. This suggests that cultivating an environment where educators feel psychologically safe translates into not only improved mental health but also potentially enhanced teaching effectiveness. Similarly, the buffering effect of PSC among police officers in Malaysia, mitigating the impact of job resources on psychological distress, implies that the nature of law enforcement work may be less psychologically taxing when embedded in a supportive organisational climate [ 7 ]. This finding holds implications for law enforcement agencies globally, urging a closer examination of the organisational factors influencing officers’ mental well-being.
In healthcare settings across different countries, the consistent positive outcomes, including decreased emotional exhaustion and stress, emphasise the universal importance of PSC in fostering a supportive environment for healthcare professionals [ 22 , 30 , 35 ]. The demanding and often emotionally charged nature of healthcare work makes the role of PSC in enhancing mental well-being particularly crucial. In the context of the general working population, the findings of reduced harassment, violence, and bullying in Australia underscore the broader societal impact of promoting a psychosocially safe work environment [ 10 ]. These results imply that organisational climates that prioritise employee well-being contribute not only to individual flourishing but also to creating healthier workplace cultures that extend beyond specific professions.
The enhanced mental well-being observed among construction workers in China suggests that the positive effects of PSC are not confined to traditional office settings [ 20 ]. In physically demanding and high-risk occupations, cultivating a supportive climate may play a pivotal role in mitigating the adverse psychological impacts of the job. Furthermore, the positive outcomes observed among attorneys in the USA and oil and gas workers in Malaysia highlight the relevance of PSC in diverse and high-pressure work environments [ 27 , 28 ]. The findings imply that irrespective of the industry or professional demands, a psychosocially safe climate can act as a buffer against psychological distress.
Practical implications for managers and organisations
Organisations and managers need to cultivate a supportive leadership style that emphasise open and bottom-up communication, approachability, and empathy towards workers [ 44 ]. Building positive relationships with workers and demonstrating genuine care is enhance PSC which contributes to creating a healthy and decent work environment where the psychological well-being of workers is prioritised. Furthermore, organisations should establish clear policies and procedures that explicitly address workplace mistreatment such as violence, bullying, harassment, discrimination, and abuse. These policies should be effectively communicated to all workers, reinforced and encouraged through training programmess. Organisations emphasising a zero-tolerance approach to workplace violence and harassment, have the potential of promoting a culture of respect and fairness, thereby promoting the health and well-being of their workers [ 45 ].
Managers and supervisors ought to undergo training on the significance of PSC and its relation to preventing mistreatment at the workplace. This training should concentrate on augmenting supportive leadership skills, promoting positive communication, conflict resolution, and creating an awareness of the impact of mistreatment on both individual and the organisation [ 46 ]. It is of utmost importance to institute confidential mechanisms for workers to report incidents of mistreatment without any apprehension of retaliation. Encouraging reporting can help identify and address mistreatment cases expediently. Managers should communicate the existence of reporting channels and ensure that workers feel secure and supported when reporting their concerns and seeking support and resources.
Managers possess a vital function in establishing a culture that highly regards respect, diversity, and inclusion. Through the cultivation of an inclusive work environment, wherein individuals are treated with dignity and fairness, managers can contribute to creating a high PSC context that minimizes the occurrences of mistreatment [ 46 ]. Managers should consistently evaluate and attend to work-related stressors that may lead to psychological distress, cognitive fatigue, emotional exhaustion, and depression. This can encompass the management of workload, provision of resources and support, and promotion of work-life balance. Organisations ought to allocate resources to workers’ well-being initiatives, such as mental health programmess, wellness activities, and workshops that develop resilience [ 46 , 47 ]. Such initiatives may further reinforce psychological well-being, personal resilience, and hope among workers.
Limitations and recommendations for future research
Most of the studies included this study were cross-sectional surveys which are usually affected by response bias, which may also affect the findings of this review. Using only papers published in the English language may affect the volume and depth of evidence retrieved for this review. There is limited evidence from continents such as Africa and South America that may skew the findings. However, authors used robust protocols to retrieve essential papers from 13 countries, screen papers, extract data and thematic analysis which may help in generalisation findings and make recommendations for future research and practice. Authors did not appraise the studies included in this scoping review. This poses a limitation as it may impact the overall quality and reliability of the included studies. Hence, caution should be taken when interpretating the findings and conclusion drawn from this review. Further research is needed to explore gender-specific dynamics in the influence of PSC on workplace mistreatment and mental health. A future systematic review is needed to estimate the practical effect of PSC on psychological well-being and workplace mistreatment.
This review found that PSC has a negative association with workplace mistreatment such as bullying, harassment, violence, discrimination and abuse. Furthermore, the authors found that PSC has a positive association with psychological well-being, personal resilience and hope. PSC also has a negative association with psychological distress, stress, depression, cognitive weariness and emotional exhaustion, strongly establishing the buffering effect of PSC on worker health and well-being. The findings highlight the importance of fostering a supportive work environment and cultivating positive relationships between supervisors and employees. Workplaces or organisations should prioritise the training and development of supervisors to enhance their supportive skills, encourage respectful behaviour, and provide guidance on conflict resolution. By promoting a high PSC context, organizations can create a culture that discourages mistreatment, leading to increased employee well-being, job satisfaction, and productivity. Finally, organizations need to address factors that contribute to low PSC, such as ineffective leadership, lack of open bottom-up communication, or perceived unfairness. By identifying and addressing these issues, organisations can make practical steps towards creating a work environment that minimises mistreatment and promotes a positive workplace culture. Further research is needed to explore gender-specific dynamics in the influence of PSC on workplace mistreatment and mental health. A future systematic review is needed to estimate the practical effect of PSC on psychological well-being and workplace mistreatment in various and diverse organisational settings, especially in settings such as Africa and South America that have received limited research on PSC and its interplay with workplace mistreatment and mental health.
Data availability
All data generated or analysed during this study are included in this article and its supplementary file (Table S1 ).
ILO. Experiences of Violence and Harassment at Work: A first global survey. Experiences of Violence and Harassment at Work: A First Global Survey 2022.
WHO, WHO/ILO ILO. accessed November 16,: Almost 2 million people die from work-related causes each year. WHO/ILO: Almost 2 Million People Die from Work-Related Causes Each Year 2021. https://www.who.int/news/item/16-09-2021-who-ilo-almost-2-million-people-die-from-work-related-causes-each-year (2021).
WHO. ILO. WHO/ILO joint estimates of the work-related burden of disease and injury, 2000–2016: global monitoring report. Geneva: 2021.
Dollard MF, Bakker AB. Psychosocial safety climate as a precursor to conducive work environments, psychological health problems, and employee engagement. J Occup Organ Psychol. 2010;83:579–99. https://doi.org/10.1348/096317909X470690 .
Article Google Scholar
Dollard M, Dormann C, Idris M. Psychosocial Safety Climate. Vol. Eds. Springer International Publishing; 2019. https://doi.org/10.1007/978-3-030-20319-1 .
Hall GB, Dollard MF, Coward J. Psychosocial Safety Climate: development of the PSC-12. Int J Stress Manag. 2010;17:353–83. https://doi.org/10.1037/a0021320 .
Yulita Y, Idris MA, Dollard MF. Effect of psychosocial safety climate on psychological distress via job resources, work engagement and workaholism: a multilevel longitudinal study. Int J Occup Saf Ergon. 2022;28:691–708. https://doi.org/10.1080/10803548.2020.1822054 .
Article PubMed Google Scholar
Pien LC, Cheng Y, Cheng WJ. Psychosocial safety climate, workplace violence and self-rated health: a multi-level study among hospital nurses. J Nurs Manag. 2019;27:584–91. https://doi.org/10.1111/jonm.12715 .
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Social Res Methodology: Theory Pract. 2005;8:19–32. https://doi.org/10.1080/1364557032000119616 .
Bailey TS, Dollard MF, McLinton SS, Richards PAM. Psychosocial safety climate, psychosocial and physical factors in the aetiology of musculoskeletal disorder symptoms and workplace injury compensation claims. Work Stress. 2015;29:190–211. https://doi.org/10.1080/02678373.2015.1031855 .
Law R, Dollard MF, Tuckey MR, Dormann C. Psychosocial safety climate as a lead indicator of workplace bullying and harassment, job resources, psychological health and employee engagement. Accid Anal Prev. 2011;43:1782–93. https://doi.org/10.1016/j.aap.2011.04.010 .
Bond SA, Tuckey MR, Dollard MF. Psychosocial safety climate, workplace bullying, and symptoms of posttraumatic stress. Organ Dev J. 2010;28:37–56.
Google Scholar
Nguyen DTN, Teo STT, Grover SL, Nguyen NP. Psychological safety climate and workplace bullying in Vietnam’s public sector. Public Manage Rev. 2017;19:1415–36. https://doi.org/10.1080/14719037.2016.1272712 .
Dollard MF, Dormann C, Tuckey MR, Escartín J. Psychosocial safety climate (PSC) and enacted PSC for workplace bullying and psychological health problem reduction. Eur J Work Organizational Psychol. 2017;26:844–57. https://doi.org/10.1080/1359432X.2017.1380626 .
Klinefelter Z, Sinclair RR, Britt TW, Sawhney G, Black KJ, Munc A. Psychosocial safety climate and stigma: reporting stress-related concerns at work. Stress Health. 2021;37:488–503. https://doi.org/10.1002/smi.3010 .
Escartín J, Dollard M, Zapf D, Kozlowski SWJ. Multilevel emotional exhaustion: psychosocial safety climate and workplace bullying as higher level contextual and individual explanatory factors. Eur J Work Organizational Psychol. 2021;30:742–52. https://doi.org/10.1080/1359432X.2021.1939412 .
Vaktskjold Hamre K, Valvatne Einarsen S, Notelaers G. Psychosocial safety climate as a moderator in role stressor- bullying relationships: a multilevel approach. Saf Sci. 2023;164:106165. https://doi.org/10.1016/J.SSCI.2023.106165 .
Afsharian A, Dollard M, Miller E, Puvimanasinghe T, Esterman A, De Anstiss H, et al. Refugees at work: the preventative role of psychosocial safety climate against workplace harassment, discrimination and psychological distress. Int J Environ Res Public Health. 2021;18. https://doi.org/10.3390/ijerph182010696 .
Idris MA, Dollard MF, Coward J, Dormann C. Psychosocial safety climate: conceptual distinctiveness and effect on job demands and worker psychological health. Saf Sci. 2012;50:19–28. https://doi.org/10.1016/j.ssci.2011.06.005 .
Xie L, Lin G, Hon C, Xia B, Skitmore M. Comparing the psychosocial safety climate between megaprojects and non-megaprojects: evidence from China. Appl Sci (Switzerland). 2020;10:1–17. https://doi.org/10.3390/app10248809 .
Zinsser KM, Zinsser A. Two Case studies of Preschool Psychosocial Safety climates. Res Hum Dev. 2016;13:49–64. https://doi.org/10.1080/15427609.2016.1141278 .
Afsharian A, Dollard M, Ziaian T. Psychosocial Safety Climate. Psychosocial Saf Clim. 2019. https://doi.org/10.1007/978-3-030-20319-1 .
Owen MS, Bailey TS, Dollard MF. Psychosocial Safety Climate as a Multilevel extension of ERI Theory: evidence from Australia. In: Siegrist J, Wahrendorf M, editors. Work Stress and Health in a globalized economy, aligning perspectives on Health, Safety and Well-Being. Springer International Publishing Switzerland; 2016. pp. 189–217. https://doi.org/10.1007/978-3-319-32937-6_9 .
Dollard MF, Opie T, Lenthall S, Wakerman J, Knight S, Dunn S, et al. Psychosocial safety climate as an antecedent of work characteristics and psychological strain: a multilevel model. Work Stress. 2012;26:385–404. https://doi.org/10.1080/02678373.2012.734154 .
Dollard MF, Karasek RA. Building Psychosocial Safety Climate: evaluation of a socially coordinated PAR risk management stress Prevention Study. Contemp Occup Health Psychology: Global Perspect Res Pract. 2010;1:208–33. https://doi.org/10.1002/9780470661550.ch11 .
Mirza MZ, Memon MA, Dollard M. A time-lagged study on health-centric leadership styles and psychological health: the mediating role of psychosocial safety climate. Curr Psychol 2021:2021–3. https://doi.org/10.1007/s12144-021-02140-5 .
Gazica MW, Powers SR, Kessler SR. Imperfectly perfect: examining psychosocial safety climate’s influence on the physical and psychological impact of perfectionism in the practice of law. Behav Sci Law. 2021;39:741–57. https://doi.org/10.1002/bsl.2546 .
Mirza MZ, Isha ASN, Memon MA, Azeem S, Zahid M. Psychosocial safety climate, safety compliance and safety participation: the mediating role of psychological distress. J Manage Organ. 2022;28:363–78. https://doi.org/10.1017/jmo.2019.35 .
Inoue A, Eguchi H, Kachi Y, Tsutsumi A. Perceived psychosocial safety climate, psychological distress, and work engagement in Japanese employees: a cross-sectional mediation analysis of job demands and job resources. J Occup Health. 2023;65:e12405. https://doi.org/10.1002/1348-9585.12405 .
Article PubMed PubMed Central Google Scholar
Afsharian A, Zadow A, Dollard MF. Psychosocial factors at work in the Asia Pacific. Psychosocial factors at work in the Asia Pacific: from theory to practice. Springer International Publishing Switzerland; 2016. pp. 187–201. https://doi.org/10.1007/978-3-319-44400-0_10 .
Idris MA, Dollard MF, Yulita. Psychosocial safety climate, emotional demands, burnout, and depression: a longitudinal multilevel study in the Malaysian private sector. J Occup Health Psychol. 2014;19:291–302. https://doi.org/10.1037/a0036599 .
Zadow AJ, Dollard MF, Mclinton SS, Lawrence P, Tuckey MR. Psychosocial safety climate, emotional exhaustion, and work injuries in healthcare workplaces. Stress Health. 2017;33:558–69. https://doi.org/10.1002/smi.2740 .
Berthelsen H, Muhonen T, Bergström G, Westerlund H, Dollard MF. Benchmarks for evidence-based risk assessment with the Swedish version of the 4-item psychosocial safety climate scale. Int J Environ Res Public Health. 2020;17:1–18. https://doi.org/10.3390/ijerph17228675 .
Havermans BM, Boot CRL, Houtman ILD, Brouwers EPM, Anema JR, Van Der Beek AJ. The role of autonomy and social support in the relation between psychosocial safety climate and stress in health care workers. BMC Public Health. 2017;17:1–7. https://doi.org/10.1186/s12889-017-4484-4 .
Mansour S, Tremblay DG. How can we decrease burnout and safety workaround behaviors in health care organizations? The role of psychosocial safety climate. Personnel Rev. 2019;48:528–50. https://doi.org/10.1108/PR-07-2017-0224 .
Zadow AJ, Dollard MF, Dormann C, Landsbergis P. Predicting new major depression symptoms from long working hours, psychosocial safety climate and work engagement: a population-based cohort study. BMJ Open. 2021;11. https://doi.org/10.1136/bmjopen-2020-044133 .
Bailey TS, Dollard MF, Richards PAM. A national standard for psychosocial safety climate (PSC): PSC 41 as the benchmark for low risk of job strain and depressive symptoms. J Occup Health Psychol. 2015;20:15–26. https://doi.org/10.1037/a0038166 .
Dormann C, Owen M, Dollard M, Guthier C. Translating cross-lagged effects into incidence rates and risk ratios: the case of psychosocial safety climate and depression. Work Stress. 2018;32:248–61. https://doi.org/10.1080/02678373.2017.1395926 .
Kwan SSM, Tuckey MR, Dollard MF. The role of the psychosocial safety climate in coping with workplace bullying: a grounded theory and sequential tree analysis. Eur J Work Organizational Psychol. 2016;25:133–48. https://doi.org/10.1080/1359432X.2014.982102 .
Siami S, Gorji M, Martin A. Psychosocial safety climate and supportive leadership as vital enhancers of personal hope and resilience during the COVID-19 pandemic. Stress Health. 2022. https://doi.org/10.1002/smi.3192 .
Lawrie EJ, Tuckey MR, Dollard MF. Job design for mindful work: the boosting effect of psychosocial safety climate. J Occup Health Psychol. 2018;23:483–95. https://doi.org/10.1037/ocp0000102 .
Hall GB, Dollard MF, Winefield AH, Dormann C, Bakker AB. Psychosocial safety climate buffers effects of job demands on depression and positive organizational behaviors. Anxiety Stress Coping. 2013;26:355–77. https://doi.org/10.1080/10615806.2012.700477 .
Loh MY, Idris MA, Dollard MF, Isahak M. Psychosocial safety climate as a moderator of the moderators: contextualizing JDR models and emotional demands effects. J Occup Organ Psychol. 2018;91:620–44. https://doi.org/10.1111/joop.12211 .
Laloo E, Coman R, Hanley N, Bakand S. The impact of leadership on the psychosocial safety climate of organizations: a scoping review. Int J Occup Saf Health. 2023;13:258. https://doi.org/10.3126/ijosh.v13i2.43294 .
Zahlquist L, Hetland J, Skogstad A, Bakker AB, Einarsen SV. Job demands as risk factors of exposure to bullying at work: the moderating role of Team-Level Conflict Management Climate. Front Psychol. 2019;10:471375. https://doi.org/10.3389/FPSYG.2019.02017/BIBTEX .
Amoadu M, Ansah EW, Sarfo JO. Influence of psychosocial safety climate on occupational health and safety: a scoping review. BMC Public Health. 2023;23:1344. https://doi.org/10.1186/S12889-023-16246-X/FIGURES/3 .
Amoadu M, Ansah EW, Sarfo JO. Psychosocial work conditions and traffic safety among minibus and long-bus drivers. J Occup Health. 2024;66:1–8. https://doi.org/10.1093/JOCCUH/UIAD019 .
Download references
Acknowledgements
Authors are grateful to graduate students at the Department of Health, Physical Education and Recreation, University of Cape Coast, for their enormous support. Authors are also grateful to the chartered librarians at the research commons and digital library units at the Sam Jonah Library, University of Cape Coast for the support.
This work received no funding support.
Author information
Authors and affiliations.
Department of Health, Physical Education and Recreation, University of Cape Coast, Cape Coast, Ghana
Mustapha Amoadu, Edward Wilson Ansah & Jacob Owusu Sarfo
You can also search for this author in PubMed Google Scholar
Contributions
E.W.A and M.A conceptualisation and design the study. M.A conducted data collection and analysis and initial write-up, M.A and J.O.S independently extracted data for evidence synthesis, reviewed by E.W.A. M.A wrote the first and final draft. M.A and E.W.A examined and oversaw the review process. The final draft of the manuscript was read and authorised for publication by all authors.
Corresponding author
Correspondence to Mustapha Amoadu .
Ethics declarations
Ethical approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Amoadu, M., Ansah, E.W. & Sarfo, J.O. Preventing workplace mistreatment and improving workers’ mental health: a scoping review of the impact of psychosocial safety climate. BMC Psychol 12 , 195 (2024). https://doi.org/10.1186/s40359-024-01675-z
Download citation
Received : 03 July 2023
Accepted : 19 March 2024
Published : 08 April 2024
DOI : https://doi.org/10.1186/s40359-024-01675-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Psychosocial safety climate
- Workplace violence
- Workplace abuse
- Mental health
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
Mental health care is hard to find, especially for people with Medicare or Medicaid
Rhitu Chatterjee

With rates of suicide and opioid deaths rising in the past decade and children's mental health declared a national emergency , the United States faces an unprecedented mental health crisis. But access to mental health care for a significant portion of Americans — including some of the most vulnerable populations — is extremely limited, according to a new government report released Wednesday.
The report, from the Department of Health and Human Services' Office of Inspector General, finds that Medicare and Medicaid have a dire shortage of mental health care providers.
The report looked at 20 counties with people on Medicaid, traditional Medicare and Medicare Advantage plans, which together serve more than 130 million enrollees — more than 40% of the U.S. population, says Meridith Seife , the deputy regional inspector general and the lead author of the report.
Medicaid serves people on low incomes, and Medicare is mainly for people 65 years or older and those who are younger with chronic disabilities.
The report found fewer than five active mental health care providers for every 1,000 enrollees. On average, Medicare Advantage has 4.7 providers per 1,000 enrollees, whereas traditional Medicare has 2.9 providers and Medicaid has 3.1 providers for the same number of enrollees. Some counties fare even worse, with not even a single provider for every 1,000 enrollees.
"When you have so few providers available to see this many enrollees, patients start running into significant problems finding care," says Seife.
The findings are especially troubling given the level of need for mental health care in this population, she says.
"On Medicare, you have 1 in 4 Medicare enrollees who are living with a mental illness," she says. "Yet less than half of those people are receiving treatment."
Among people on Medicaid, 1 in 3 have a mental illness, and 1 in 5 have a substance use disorder. "So the need is tremendous."
The results are "scary" but "not very surprising," says Deborah Steinberg , senior health policy attorney at the nonprofit Legal Action Center. "We know that people in Medicare and Medicaid are often underserved populations, and this is especially true for mental health and substance use disorder care."
Among those individuals able to find and connect with a provider, many see their provider several times a year, according to the report. And many have to drive a long way for their appointments.
"We have roughly 1 in 4 patients that had to travel more than an hour to their appointments, and 1 in 10 had to travel more than an hour and a half each way," notes Seife. Some patients traveled two hours each way for mental health care, she says.
Mental illnesses and substance use disorders are chronic conditions that people need ongoing care for, says Steinberg. "And when they have to travel an hour, more than an hour, for an appointment throughout the year, that becomes unreasonable. It becomes untenable."
"We know that behavioral health workforce shortages are widespread," says Heather Saunders , a senior research manager on the Medicaid team at KFF, the health policy research organization. "This is across all payers, all populations, with about half of the U.S. population living in a workforce shortage."
But as the report found, that's not the whole story for Medicare and Medicaid. Only about a third of mental health care providers in the counties studied see Medicare and Medicaid patients. That means a majority of the workforce doesn't participate in these programs.
This has been well documented in Medicaid, notes Saunders. "Only a fraction" of providers in provider directories see Medicaid patients, she says. "And when they do see Medicaid patients, they often only see a few."
Lower reimbursement rates and a high administrative burden prevent more providers from participating in Medicaid and Medicare, the report notes.
"In the Medicare program, they set a physician fee rate," explains Steinberg. "Then for certain providers, which includes clinical social workers, mental health counselors and marriage and family therapists, they get reimbursed at 75% of that rate."
Medicaid reimbursements for psychiatric services are even lower when compared with Medicare , says Ellen Weber , senior vice president for health initiatives at the Legal Action Center.
"They're baking in those discriminatory standards when they are setting those rates," says Steinberg.
The new report recommends that the Centers for Medicare & Medicaid Services (CMS) take steps to increase payments to providers and lower administrative requirements. In a statement, CMS said it has responded to those recommendations within the report.
According to research by Saunders and her colleagues at KFF, many states have already started to take action on these fronts to improve participation in Medicaid.
Several have upped their payments to mental health providers. "But the scale of those increases ranged widely across states," says Saunders, "with some states limiting the increase to one provider type or one type of service, but other states having rate increases that were more across the board."
Some states have also tried to simplify and streamline paperwork, she adds. "Making it less complex, making it easier to understand," says Saunders.
But it's too soon to know whether those efforts have made a significant impact on improving access to providers.
CMS has also taken steps to address provider shortages, says Steinberg.
"CMS has tried to increase some of the reimbursement rates without actually fixing that structural problem," says Steinberg. "Trying to add a little bit here and there, but it's not enough, especially when they're only adding a percent to the total rate. It's a really small increase."
The agency has also started covering treatments and providers it didn't use to cover before.
"In 2020, Medicare started covering opioid treatment programs, which is where a lot of folks can go to get medications for their substance use disorder," says Steinberg.
And starting this year, Medicare also covers "mental health counselors, which includes addiction counselors, as well as marriage and family therapists," she adds.
While noteworthy and important, a lot more needs to be done, says Steinberg. "For example, in the substance use disorder space, a lot of addiction counselors do not have a master's degree. And that's one of their requirements to be a counselor in the Medicare program right now."
Removing those stringent requirements and adding other kinds of providers, like peer support specialists, is key to improving access. And the cost of not accessing care is high, she adds.
"Over the past two decades, [in] the older adult population, the number of overdose deaths has increased fourfold — quadrupled," says Steinberg. "So this is affecting people. It is causing deaths. It is causing people to go to the hospital. It increases [health care] costs."
- Centers for Medicare & Medicaid Services
- mental health

25,000+ students realised their study abroad dream with us. Take the first step today
Here’s your new year gift, one app for all your, study abroad needs, start your journey, track your progress, grow with the community and so much more.

Verification Code
An OTP has been sent to your registered mobile no. Please verify

Thanks for your comment !
Our team will review it before it's shown to our readers.

- Sahitya (साहित्य) /
Mental Health Quotes in Hindi: पढ़िए मानसिक स्वास्थ्य पर आधारित अनमोल विचार, जो करेंगे आपको प्रेरित
- Updated on
- अक्टूबर 5, 2023

कोरोना महामारी के बाद से ही मानव ने जीवन का सही मूल्य जाना है, लेकिन आज भी विश्व भर में कई लोग मानसिक तौर पर स्वस्थ नहीं होते हैं। मानसिक स्वास्थ्य को जानने वाला इंसान ही सकारात्मक ढंग से लोगों के जीवन को प्रभावित कर सकता है। इस पोस्ट के माध्यम से आप मानसिक स्वास्थ्य पर आधारित अनमोल विचारों के बारे में जान पाएंगे। Mental Health Quotes in Hindi के माध्यम से खुद को मानसिक स्वास्थ्य के लिए खुद को प्रेरित कर सकते हैं, जिसके लिए आपको यह ब्लॉग अंत तक पढ़ना पड़ेगा।
This Blog Includes:
टॉप 10 mental health quotes in hindi, विद्यार्थियों के लिए health is wealth quotes in hindi, स्वास्थ्य के प्रति जागरूक करने वाले विचार, समाज में मानसिक स्वास्थ्य की पैरवी करने वाले विचार, mental health quotes in english .
टॉप 10 Mental Health Quotes in Hindi निम्नवत हैं, जिनके माध्यम से आप अपने मानसिक स्वास्थ्य के लिए खुद को प्रेरित कर सकते हैं;
जिन्दगी चाहे जितनी कठिन लगे, हमेशा कुछ न कुछ होता है जो आप कर सकते हैं और जिसमे सफल हो सकते हैं।

सबसे जरूरी चीज है अपने जीवन का आनंद लेना – खुश रहना – बस यही मायने रखता है।
आपका दिमाग अधिकतर प्रश्नों के उत्तर दे देगा यदि आप विश्राम करना और उत्तर की प्रतीक्षा करना सीख लें।
यदि आप जीवन की चिंताओं से जीतना चाहते हैं तो, इस क्षण में जिएं, इस सांस में जिए।
स्वास्थ्य मानसिकता का भी होता है।
मानसिक स्वास्थ्य को महत्व देना उतना ही महत्वपूर्ण है, जितना कि शारीरिक स्वास्थ्य को देना।

अपने मानसिक स्वास्थ्य का ध्यान रखो, क्योंकि यह ही आपके जीवन की अच्छाई और खुशियों का कुंजी है।
मानसिक रूप से मजबूत रहना व्यक्तिगत विकास का मार्ग है।
मानसिक स्वास्थ्य को नजरअंदाज न करें, बल्कि उसका सही देखभाल करें।
आपका मानसिक स्वास्थ्य आपकी शक्तियों की जद है, इसे बिना किसी शरणागति के बदलें।

विद्यार्थियों के लिए health is wealth quotes in hindi एक अच्छा तरीका होगा, जो उन्हें मानसिक स्वास्थ्य के लिए प्रेरित करेगा। विद्यार्थियों के लिए Mental Health Quotes in Hindi कुछ इस प्रकार हैं-
सब कुछ ठीक नहीं हो सकता, लेकिन अच्छे मानसिक स्वास्थ्य के साथ हर समस्या का समाधान संभव है।

मानसिक स्वास्थ्य का ध्यान रखना एक सबसे महत्वपूर्ण काम है, क्योंकि यह हमारे संपूर्ण जीवन को प्रभावित करता है।
अपने मानसिक स्वास्थ्य को पहचानो और सुरक्षित रखो, क्योंकि यह हमारी सबसे महत्वपूर्ण संपत्ति है।
मानसिक स्वास्थ्य के बिना, हम कुछ भी नहीं कर सकते।
बेहतर मानसिक स्वास्थ्य के लिए योग और व्यायाम पर विशेष ध्यान दें।

मानसिक स्वास्थ्य का समय निकालें, क्योंकि यह सबसे महत्वपूर्ण होता है।
मानसिक बीमारी एक सबक हो सकती है, लेकिन यह कभी भी अंत नहीं होना चाहिए।
आपका मानसिक स्वास्थ्य आपके शारीरिक स्वास्थ्य का हिस्सा है, इसे प्राथमिकता दें।
खुश रहने के लिए हमें सीखना होगा कि कैसे अपने मानसिक स्वास्थ्य का ख्याल रखें।
मानसिक स्वास्थ्य को अच्छी तरह से देखभाल करना, आत्म-समर्पण का एक सबसे महत्वपूर्ण प्रक्रिया है।

Mental Health Quotes in Hindi आपके लिए एक प्रेरणा का काम करेंगे, जिनके माध्यम से आप स्वास्थ्य के प्रति जागरूक करने वाले विचार पढ़ सकेंगे। ऐसे अनमोल विचार निम्नलिखित हैं;
मानसिक स्वास्थ्य हमारे शारीरिक स्वास्थ्य का महत्वपूर्ण हिस्सा है।

अपने मन की देखभाल करना उतना ही महत्वपूर्ण है, जितना कि शारीरिक स्वास्थ्य की देखभाल करना।
मानसिक स्वास्थ्य को समझना और देखभाल करना स्वास्थ्य और खुशी का मार्ग होता है।
अपने मन की सुनो, उसे समझो, और उसकी देखभाल करो।
खुद को प्यार करना मानसिक स्वास्थ्य का पहला कदम है।
मानसिक स्वास्थ्य का ध्यान रखना, सबसे बड़ी धन और सशक्ति का स्रोत हो सकता है।

अपने दिमाग की सुनो, वो तुम्हें बहुत कुछ सिखा सकता है।
मानसिक स्वास्थ्य के बिना, शारीरिक स्वास्थ्य की कोई महत्व नहीं होता।
जब तुम्हारा मन खुश होता है, तो तुम पूरी दुनिया को खुश देखते हो।
मानसिक स्वास्थ्य की सुरक्षा अपने हाथ में होती है।

Mental Health Quotes in Hindi के इस ब्लॉग में आपको समाज में मानसिक स्वास्थ्य की पैरवी करने वाले विचार पढ़ पाएंगे, जो कि निम्नलिखित हैं-
अपने मानसिक स्वास्थ्य की परवाह करना तंग नहीं करता, बल्कि आपको मजबूत बनाता है।

अपने दिमाग की देखभाल करो, क्योंकि वह आपका सबसे महत्वपूर्ण निवेश है।
मानसिक स्वास्थ्य का ध्यान रखने का समय आपके जीवन का सबसे महत्वपूर्ण समय हो सकता है।
जब आप मानसिक तौर पर मजबूत होते हैं, तो आप हर मुश्किल को पार कर सकते हैं।
खुद की देखभाल करना सही होता है, क्योंकि एक स्वस्थ मन खुदी तोड़ देता है।
मानसिक स्वास्थ्य का देखभाल करना उस अहम कदम की शुरुआत है जो आपके खुद के दिल की सुनवाई का हिस्सा हो सकता है।
सबसे पहले अपने दिल की सुनो, फिर अपने दिमाग की।
मानसिक स्वास्थ्य को बढ़ावा देना एक सफल और सुखमय जीवन की शुरुआत है।
समय-समय पर अपने आप को भी देखभाल की आवश्यकता होती है, और यह सही है।
मानसिक स्वास्थ्य का ध्यान रखना आपकी ताकत बना सकता है, आपको सशक्त बना सकता है।
सबसे बड़ी खुशी यह है कि आप खुद के लिए देखभाल कर रहे हैं, अपने मानसिक स्वास्थ्य को महत्व देने के माध्यम से।
मानसिक स्वास्थ्य को देखभाल करना सबसे अच्छा निवेश है, क्योंकि यह आपके जीवन को सुखमय बना सकता है।
मानसिक स्वास्थ्य को संरक्षित रखें, खुद को प्यार करें, और खुश रहें।
मानसिक स्वास्थ्य का सहारा लें, क्योंकि आपकी ताक़त आपके मन में है।
मानसिक स्वास्थ्य की देखभाल स्वस्थ जीवन की कुंजी है।

Mental Health Quotes in Hindi के इस ब्लॉग में आपको लाल बहादुर शास्त्री के कुछ इंग्लिश कोट्स भी पढ़ने को मिल जाएंगे, जो कि निम्नलिखित हैं-
Mental health is also a part of life, take care of it.
Taking care of mental health is a sign of self-love.
Recognize your mental health, enhance its capacity.
First, take care of your mental health, then do all other tasks.
Your mental health is your most valuable asset, always cherish it.
Taking care of mental health is a spiritual dialogue with oneself.
Understanding and accepting your mental health is a salute to your freedom.
Properly caring for mental health is the best way to improve oneself.
Taking care of mental health is the key to happiness in life.
Respect your mental health; it’s your strength.

आशा है कि Mental Health Quotes in Hindi के माध्यम से आप मानसिक स्वास्थ्य के लिए प्रेरित करने वाले विचारों को पढ़ पाए होंगे। इसी प्रकार के कोट्स पढ़ने के लिए हमारी वेबसाइट Leverage Edu के साथ बने रहें।
मयंक विश्नोई
जन्मभूमि: देवभूमि उत्तराखंड। पहचान: भारतीय लेखक । प्रकाश परिवर्तन का, संस्कार समर्पण का। -✍🏻मयंक विश्नोई
प्रातिक्रिया दे जवाब रद्द करें
अगली बार जब मैं टिप्पणी करूँ, तो इस ब्राउज़र में मेरा नाम, ईमेल और वेबसाइट सहेजें।
Contact no. *

Leaving already?
8 Universities with higher ROI than IITs and IIMs
Grab this one-time opportunity to download this ebook
Connect With Us
25,000+ students realised their study abroad dream with us. take the first step today..

Resend OTP in

Need help with?
Study abroad.
UK, Canada, US & More
IELTS, GRE, GMAT & More
Scholarship, Loans & Forex
Country Preference
New Zealand
Which English test are you planning to take?
Which academic test are you planning to take.
Not Sure yet
When are you planning to take the exam?
Already booked my exam slot
Within 2 Months
Want to learn about the test
Which Degree do you wish to pursue?
When do you want to start studying abroad.
September 2024
January 2025
What is your budget to study abroad?
How would you describe this article ?
Please rate this article
We would like to hear more.
There’s a Reason They’re Called ‘Gut’ Feelings

I n the 1800s, a French Canadian named Alexis St. Martin was shot in the stomach while at a fur trading post, when someone’s musket accidentally fired at close range. He survived, but his injuries resulted in a hole in his stomach wall. This provided an early window—literally—into how our emotions and mental health affect the gut. Through careful experiments, the surgeon William Beaumont discovered that St. Martin’s mental state had direct physiological consequences on his stomach’s activity: when he felt irritable, for example, his digestion slowed. Somehow, his emotional states were manifest in the specific, local biology of his gut.
Most people have experienced the gut consequences of their emotional feelings. Nerves before an exam might lead you to feel nauseous or even vomit. Profound sadness might make you lose your appetite, or perhaps cause a hunger impossible to satiate. Gut symptoms are common in mental health conditions, from appetite changes in depression to debilitating “psychosomatic” stomach pains. Many of our feelings are gut feelings.
But the gut doesn’t just respond to emotional feelings: it influences them, too. Take disgust. Disgust is visceral. Our stomach, like our heart, has a regular electrical rhythm; even just seeing something disgusting causes disruptions, called “dysrhythmias,” in this electrical signalling. Although disgust is crucial for survival—helping us avoid disease and stay alive—in many mental health conditions disgust becomes pathological. In obsessive compulsive disorder (OCD), for instance, dirt or germs can preoccupy someone’s thoughts, causing symptoms like compulsive hand-washing. Self-disgust is common in depression and eating disorders. And even post-traumatic disorder can be brought on by profoundly disgusting traumas.
Pathological disgust is particularly hard to treat : exposure therapy and other psychological approaches are much less effective than for fear-based mental health problems. A couple years ago, working as a neuroscientist at the University of Cambridge, I wondered if abnormal signals from the stomach could be causing disgust avoidance. I ran an experiment to test this hypothesis, and found that changing someone’s gut activity with a common anti-nausea drug reduced their disgust avoidance . This could represent a new way of treating pathological disgust in mental health disorders. For example, an anti-nausea drug could be administered just before exposure therapy, enabling patients to engage with therapy under a more optimal gut state.
Read More: How I Learned to Listen to What My Gut Was Telling Me
So gut feelings are not “all in your mind”—but they are not “all in your gut,” either. Sensations from the gut are transmitted to the brain via the vagus nerve, the primary channel of information sent from the body to the brain. A second route to target “gut feelings” is by electrically stimulating this nerve, which changes the electrical rhythm of the stomach . That said, the idea is not new: vagus nerve stimulation for patients with major depression dates back to 2000 .
A new theory published in November 2023 proposes that vagus nerve stimulation amplifies signals from the internal body to the brain, which helps us adapt our behaviour to its current challenges and needs. That could explain why the effects of vagus nerve stimulation are so wide-reaching, altering learning, memory, and motivation. That means amplifying signals from the gut using vagus nerve stimulation might improve mental health in some cases, but in others could be ineffective or even detrimental. Ultimately, we need to consider the state and needs of someone’s internal body before amplifying the body’s influence on the brain.
But the importance of the vagus nerve extends to even more established treatments: evidence from mice suggests that the most common type of antidepressant drugs (SSRIs, or selective serotonin reuptake inhibitors) require the vagus nerve to work. This, too, could begin to provide clues why antidepressants do, or don’t, work for a given person, and even help us understand why they might cause side effects in some people.
If the vagus nerve’s role helps us adapt to our bodily needs, perhaps the most important internal need of all is energy. One function of the gut—together with other organs—is metabolism, converting food to energy the body can use. There are mysterious and wide-ranging connections between our metabolic system and mental health. For example, the prevalence of depression in people with diabetes is two or three times higher than in the general population. It’s not clear why: diabetes could increase depression risk, or vice versa. My lab is currently testing a third possibility: that common metabolic factors might increase your risk of both depression and diabetes because of interactions between the body and the brain. If we’re right, this could open up avenues toward metabolic interventions that improve both physical and mental health.
Our brain and wider nervous system adapts to its circumstances, including the body’s internal, metabolic needs, as well as our experience of the environment around us. Because of this, your gut-brain connection is not static, but rather changes and adapts over time. A fascinating study in 2021 discovered that brain cells can re-activate gut inflammation that an animal has previously experienced. The mere “memory” of gut inflammation, stored in cells in the brain, induced the physical state in the body. So sometimes a “gut feeling” actually originates from the brain. This role of the brain in “gut feelings” means our brain has the capacity to produce dysfunctional gut symptoms via brain changes alone. This ability of the brain could have upsides as well, perhaps explaining why psychological therapy—which causes brain changes —can also treat some gut conditions .
Gut feelings originate from many sources: directly through the gut, through channels of communication between gut and brain, or even through the brain itself. In neuroscience, as we unravel the dynamic communications between gut and brain, we can begin to understand how these processes helped our ancestors survive—and how we could better harness them to improve emotional and mental wellbeing. A gut feeling might have many possible causes, but each of these represent a potential solution for mental health.
More Must-Reads From TIME
- Jane Fonda Champions Climate Action for Every Generation
- Passengers Are Flying up to 30 Hours to See Four Minutes of the Eclipse
- Biden’s Campaign Is In Trouble. Will the Turnaround Plan Work?
- Essay: The Complicated Dread of Early Spring
- Why Walking Isn’t Enough When It Comes to Exercise
- The Financial Influencers Women Actually Want to Listen To
- The Best TV Shows to Watch on Peacock
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]
You May Also Like
- Share full article
Advertisement
Supported by
Guest Essay
Anxious Parents Are the Ones Who Need Help

By Mathilde Ross
Dr. Ross is a senior staff psychiatrist at Boston University Health Services.
This month, across the country, a new cohort of students is being accepted into colleges. And, if recent trends continue, the start of the new school year will kick off another record-breaking season for anxiety on campus.
I’m talking about the parents. The kids are mostly fine.
Let me explain. Most emotions, even unpleasant ones, are normal. But the word is out about increasing rates of mental health problems on campus, and that’s got parents worrying. Fair enough. The statistics are startling — in 2022, nearly 14 percent of 18- to 25-year-olds reported having serious thoughts about suicide.
But parents are allowing their anxiety to take over, and it’s not helping anyone, least of all their children. If a child calls home too much, there must be a crisis! And if a child calls too little, there must be a crisis! Either way, the panicked parent picks up the phone and calls the college counseling center to talk to someone like me.
I am a psychiatrist who has worked at a major university’s mental health clinic for 16 years. Much of next year’s freshman class was born the year before I started working here. Technically, my job is to keep my door open and help students through crises, big and small. But I have also developed a comprehensive approach to the assessment and treatment of anxious parents.
The typical call from a parent begins like this: “I think my son/daughter is suffering from anxiety.” My typical reply is: “Anxiety in this setting is usually normal, because major life transitions like living away from home for the first time are commonly associated with elevated anxiety.” Parents used to be satisfied with this kind of answer, thanked me, hung up, called their children and encouraged them to think long-term: “This too shall pass.” And most everyone carried on.
But these days this kind of thinking just convinces parents that I don’t know what I’m talking about. In the circular logic of mental health awareness, a clinician’s reassurance that situational anxiety is most likely normal and time-limited leads a parent to believe that the clinician may be missing a serious mental health condition.
Today’s parents are suffering from anxiety about anxiety, which is actually much more serious than anxiety. It’s self-fulfilling and not easily soothed by logic or evidence, such as the knowledge that most everyone adjusts to college just fine.
Anxiety about anxiety has gotten so bad that some parents actually worry if their student isn’t anxious. This puts a lot of pressure on unanxious students — it creates anxiety about anxiety about anxiety. (This happens all the time. Well-meaning parents tell their kid to make an appointment with our office to make sure their adjustment to college is going OK.) If the student says she’s fine, the parents worry that she isn’t being forthright. This is the conundrum of anxiety about anxiety — there’s really no easy way to combat it.
But I do have some advice for parents. The first thing I’d like to say, and I mean it in the kindest possible way, is: Get a grip.
As for your kids, I would like to help you with some age-appropriate remedies. If your child calls during the first weeks of college feeling anxious, consider saying any of the following: You’ll get through this; this is normal; we’ll laugh about this phone call at Thanksgiving. Or, say anything that was helpful to you the last time you started something new. Alternatively, you could say nothing. Just listening really helps. It’s the entire basis of my profession.
If the anxiety is connected to academic performance — for instance, if your child is having difficulty following the professor and thinks everyone in class is smarter — consider saying, “Do the reading.” Several times a semester, a student I’ve counseled tells me he or she discovered the secret to college: Show up for class prepared! This is often whispered rather sheepishly, even though my office is private.
Anxiety about oral presentations is also quite common. You know what I tell students? “Rehearse your speech.” Parents, you can say things like this, too. Practice it: “Son, you wouldn’t believe how helpful practice is.”
I can prepare you for advanced topics, too. Let’s say your child is exhausted and having trouble waking up for class; he thinks he has a medical problem or maybe a sleep disorder. Consider telling him to go to bed earlier. Common sense is still allowed.
What if a roommate is too loud or too quiet, too messy or too neat? Advise your kid to talk to the roommate, to take the conversation to the problem’s source.
If your child is worrying about something more serious, like failing out of college: This is quite common in the first few weeks on campus. Truth be told, failing all of one’s classes and being expelled as a result, all within the first semester, is essentially impossible and is particularly rare among those students who are worrying about it. The administrative process simply doesn’t happen that fast. Besides, you haven’t paid enough tuition yet.
I’m making my job sound easy, and it’s not. I’m making kids sound simple, and they’re not. They are my life’s work. Some kids walk through my door in serious pain. But most don’t. Most just need a responsible adult to show them the way. And most of what I do can be handled by any adult who has been through a thing or two, which is to say, any parent.
I worry that the current obsession with mental health awareness is disempowering parents from helping their adult children handle ordinary things. People are increasingly fearful that any normal emotion is a sign of something serious. But if you send your adult children to a mental health professional at the first sign of distress, you deprive yourself of the opportunity to strengthen your relationship with them. This is the beginning of their adult relationship with you. Show them the way.
The transition to college is full of excitement and its cousin, anxiety. I enjoy shepherding young people through this rite of passage. Parents should try enjoying it, too.
Mathilde Ross is a senior staff psychiatrist at Boston University Health Services.
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow The New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .

IMAGES
VIDEO
COMMENTS
Mental Health Essay in Hindi पर 10 लाइन्स नीचे दी गई है: मानसिक स्वास्थ्य व्यक्ति की भावनात्मक, मानसिक और सामाजिक क्षमता का प्रतीक होता है। अच्छा ...
Essay on Mental Health in Hindi : इस लेख में हमने मानसिक स्वास्थ्य के बारे में जानकारी प्रदान की है। यहाँ पर दी गई जानकारी बच्चों से लेकर प्रतियोगी ...
Mental Health in Hindi (मेंटल हेल्थ), Mansik Swasthya in Hindi (मानसिक स्वास्थ्य): मानसिक स्वास्थ्य व ...
इतिहास. 19वीं शताब्दी के मध्य में, विलियम स्वीटजर प्रथम व्यक्ति थे जिन्होंने "मानसिक स्वास्थ्य" को पहली बार स्पष्ट रूप से परिभाषित किया, जिसे सकारात्मक ...
मानसिक स्वास्थ्य के लिए आहार - Diet while dealing with Mental Health in Hindi. ... Articles on StyleCraze are backed by verified information from peer-reviewed and academic research papers, reputed organizations, research institutions, and medical associations to ensure accuracy and relevance.
Center for Disease Control: Mental Health and Coping During COVID-19; World Health Organization: Mental health and psychosocial considerations during the COVID-19 outbreak; NIMHANS with the Ministry of Health & Family Welfare, Government of India: Minding our minds during COVID 19; Mental health of children; Mental health of elderly
मानसिक स्वास्थ्य का अर्थ Meaning of Mental Health. बालकों में मानसिक स्वास्थ्य से सम्बन्धित व्यवहार की अनेक समस्याएँ देखी जाती हैं। इससे परिवार तथा विद्यालय का ...
मानसिक विकार व्यक्ति के स्वास्थ्य-संबंधी बर्तावों जैसे, समझदारी से भोजन करने, नियमित व्यायाम, पर्याप्त नींद, सुरक्षित यौन व्यवहार ...
1 मानसिक स्वास्थ्य में सुधार के उपाय - Ways to Improve Mental Health in Hindi. 1.1 1. खुद को महत्व दें. 1.2 2. अपने मानसिक स्वास्थ्य को प्राथमिकता बनाए. 1.3 3. अपने सामने ...
Today, we are sharing a simple essay on Mental Health in Hindi. This video can help those who are looking for information about Mental Health in Hindi. This ...
Tuesday April 02, 2024 , 3 min Read. Wysa, an AI-driven mental health support provider, has launched its conversational AI therapy app for mental health in Hindi. The aim of this is to enhance the ...
राष्ट्रीय मानसिक स्वास्थ्य कार्यक्रम | national mental health programme hindi me, उद्देश्य, राष्ट्रीय मानसिक स्वास्थ्य नीति, DMHP, लक्ष्य, सिद्धांत जानें!
The role of mental asylums has evolved, and today, the focus is shifting towards community-based care, deinstitutionalization, and integrating mental health services into mainstream healthcare systems. Critiques and challenges of mental asylums in India. Stigmatization and Social Attitudes Towards Mental Asylums.
Mental health, an integral facet of human well-being, shapes our emotions, decisions, and daily interactions. Just as one would care for a sprained ankle or a fever, our minds too require attention and nurture. In today's bustling world, mental well-being is often put on the back burner, overshadowed by the immediate demands of life.
Mental Health; Essay On Mental Health In Hindi; Featured Example Essay Kama Sutra PREFACE IN the literature of all countries there will be found a certain number of works treating especially of love. Everywhere the subject is dealt with differently, and from various points of view. In the present publication it is proposed to give a complete ...
The ability of the public to remain psychologically resilient in the face of public health emergencies and disasters (such as the COVID-19 pandemic) is a key factor in the effectiveness of a national response to such events. Community resilience and social capital are often perceived as beneficial and ensuring that a community is socially and psychologically resilient may aid emergency ...
The state of cognitive and behavioural well-being is referred to as mental health. The term 'mental health' is also used to refer to the absence of mental disease. Mental health means keeping our minds healthy. Mankind generally is more focused on keeping their physical body healthy. People tend to ignore the state of their minds.
Hence, this review aims to map studies to understand the influence of psychosocial safety climate (PSC) on workplace mistreatment and mental health of workers. The guidelines outlined by Arksey and O'Malley were adopted for this review. PubMed, Scopus, Web of Science, JSTOR, Google and Google Scholar were searched for relevant papers.
A report from the Department of Health and Human Services' inspector general finds a dire shortage of mental health care providers in Medicaid and Medicare, which together serve some 40% of Americans.
Mental health is also a part of life, take care of it. Taking care of mental health is a sign of self-love. Recognize your mental health, enhance its capacity. First, take care of your mental health, then do all other tasks. Your mental health is your most valuable asset, always cherish it. Taking care of mental health is a spiritual dialogue ...
A fascinating study in 2021 discovered that brain cells can re-activate gut inflammation that an animal has previously experienced. The mere "memory" of gut inflammation, stored in cells in ...
Beyond centering mental health in their college essays, many prospective students have created and/or participated in clubs that increase awareness of and support for mental and socio-emotional health. We are seeing the creation of new groups to address mental health issues and offer new webs of support for students at the college level as well.
About Sarah: WHO's first digital health promoter. Using cutting edge technology, Sarah has helped fight misinformation about COVID-19 since the beginning of the pandemic. She now also provides information across major health topics, including mental health, and has expertise to help prevent some of the biggest causes of death in the world ...
41%. Percentage of teens with the highest social media use who rate their overall mental health as poor or very poor, compared with 23% of those with the lowest use. For example, 10% of the highest use group expressed suicidal intent or self-harm in the past 12 months compared with 5% of the lowest use group, and 17% of the highest users expressed poor body image compared with 6% of the lowest ...
Fair enough. The statistics are startling — in 2022, nearly 14 percent of 18- to 25-year-olds reported having serious thoughts about suicide. But parents are allowing their anxiety to take over ...
World Health Day 2024 is 'My health, my right'. This year's theme was chosen to champion the right of everyone, everywhere to have access to quality health services, education, and information, as well as safe drinking water, clean air, good nutrition, quality housing, decent working and environmental conditions, and freedom from discrimination.
Latest Jobs in Russia. Below are the latest jobs in Russia. Head of Accounting (International) Online in Russia RateHawk. Full Time. Morning. 1 Year. Admin. Emerging Travel Group, world leader in online travel services, a travel-tech company that owns several international brands: RateHawk, ZenHotels, RoundTrip, Ostrovok and others.12 years ago ...