
- Previous Article
- Next Article

Case Presentation
Case study: a patient with uncontrolled type 2 diabetes and complex comorbidities whose diabetes care is managed by an advanced practice nurse.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Geralyn Spollett; Case Study: A Patient With Uncontrolled Type 2 Diabetes and Complex Comorbidities Whose Diabetes Care Is Managed by an Advanced Practice Nurse. Diabetes Spectr 1 January 2003; 16 (1): 32–36. https://doi.org/10.2337/diaspect.16.1.32
Download citation file:
- Ris (Zotero)
- Reference Manager
The specialized role of nursing in the care and education of people with diabetes has been in existence for more than 30 years. Diabetes education carried out by nurses has moved beyond the hospital bedside into a variety of health care settings. Among the disciplines involved in diabetes education, nursing has played a pivotal role in the diabetes team management concept. This was well illustrated in the Diabetes Control and Complications Trial (DCCT) by the effectiveness of nurse managers in coordinating and delivering diabetes self-management education. These nurse managers not only performed administrative tasks crucial to the outcomes of the DCCT, but also participated directly in patient care. 1
The emergence and subsequent growth of advanced practice in nursing during the past 20 years has expanded the direct care component, incorporating aspects of both nursing and medical care while maintaining the teaching and counseling roles. Both the clinical nurse specialist (CNS) and nurse practitioner (NP) models, when applied to chronic disease management, create enhanced patient-provider relationships in which self-care education and counseling is provided within the context of disease state management. Clement 2 commented in a review of diabetes self-management education issues that unless ongoing management is part of an education program, knowledge may increase but most clinical outcomes only minimally improve. Advanced practice nurses by the very nature of their scope of practice effectively combine both education and management into their delivery of care.
Operating beyond the role of educator, advanced practice nurses holistically assess patients’ needs with the understanding of patients’ primary role in the improvement and maintenance of their own health and wellness. In conducting assessments, advanced practice nurses carefully explore patients’ medical history and perform focused physical exams. At the completion of assessments, advanced practice nurses, in conjunction with patients, identify management goals and determine appropriate plans of care. A review of patients’ self-care management skills and application/adaptation to lifestyle is incorporated in initial histories, physical exams, and plans of care.
Many advanced practice nurses (NPs, CNSs, nurse midwives, and nurse anesthetists) may prescribe and adjust medication through prescriptive authority granted to them by their state nursing regulatory body. Currently, all 50 states have some form of prescriptive authority for advanced practice nurses. 3 The ability to prescribe and adjust medication is a valuable asset in caring for individuals with diabetes. It is a crucial component in the care of people with type 1 diabetes, and it becomes increasingly important in the care of patients with type 2 diabetes who have a constellation of comorbidities, all of which must be managed for successful disease outcomes.
Many studies have documented the effectiveness of advanced practice nurses in managing common primary care issues. 4 NP care has been associated with a high level of satisfaction among health services consumers. In diabetes, the role of advanced practice nurses has significantly contributed to improved outcomes in the management of type 2 diabetes, 5 in specialized diabetes foot care programs, 6 in the management of diabetes in pregnancy, 7 and in the care of pediatric type 1 diabetic patients and their parents. 8 , 9 Furthermore, NPs have also been effective providers of diabetes care among disadvantaged urban African-American patients. 10 Primary management of these patients by NPs led to improved metabolic control regardless of whether weight loss was achieved.
The following case study illustrates the clinical role of advanced practice nurses in the management of a patient with type 2 diabetes.
A.B. is a retired 69-year-old man with a 5-year history of type 2 diabetes. Although he was diagnosed in 1997, he had symptoms indicating hyperglycemia for 2 years before diagnosis. He had fasting blood glucose records indicating values of 118–127 mg/dl, which were described to him as indicative of “borderline diabetes.” He also remembered past episodes of nocturia associated with large pasta meals and Italian pastries. At the time of initial diagnosis, he was advised to lose weight (“at least 10 lb.”), but no further action was taken.
Referred by his family physician to the diabetes specialty clinic, A.B. presents with recent weight gain, suboptimal diabetes control, and foot pain. He has been trying to lose weight and increase his exercise for the past 6 months without success. He had been started on glyburide (Diabeta), 2.5 mg every morning, but had stopped taking it because of dizziness, often accompanied by sweating and a feeling of mild agitation, in the late afternoon.
A.B. also takes atorvastatin (Lipitor), 10 mg daily, for hypercholesterolemia (elevated LDL cholesterol, low HDL cholesterol, and elevated triglycerides). He has tolerated this medication and adheres to the daily schedule. During the past 6 months, he has also taken chromium picolinate, gymnema sylvestre, and a “pancreas elixir” in an attempt to improve his diabetes control. He stopped these supplements when he did not see any positive results.
He does not test his blood glucose levels at home and expresses doubt that this procedure would help him improve his diabetes control. “What would knowing the numbers do for me?,” he asks. “The doctor already knows the sugars are high.”
A.B. states that he has “never been sick a day in my life.” He recently sold his business and has become very active in a variety of volunteer organizations. He lives with his wife of 48 years and has two married children. Although both his mother and father had type 2 diabetes, A.B. has limited knowledge regarding diabetes self-care management and states that he does not understand why he has diabetes since he never eats sugar. In the past, his wife has encouraged him to treat his diabetes with herbal remedies and weight-loss supplements, and she frequently scans the Internet for the latest diabetes remedies.
During the past year, A.B. has gained 22 lb. Since retiring, he has been more physically active, playing golf once a week and gardening, but he has been unable to lose more than 2–3 lb. He has never seen a dietitian and has not been instructed in self-monitoring of blood glucose (SMBG).
A.B.’s diet history reveals excessive carbohydrate intake in the form of bread and pasta. His normal dinners consist of 2 cups of cooked pasta with homemade sauce and three to four slices of Italian bread. During the day, he often has “a slice or two” of bread with butter or olive oil. He also eats eight to ten pieces of fresh fruit per day at meals and as snacks. He prefers chicken and fish, but it is usually served with a tomato or cream sauce accompanied by pasta. His wife has offered to make him plain grilled meats, but he finds them “tasteless.” He drinks 8 oz. of red wine with dinner each evening. He stopped smoking more than 10 years ago, he reports, “when the cost of cigarettes topped a buck-fifty.”
The medical documents that A.B. brings to this appointment indicate that his hemoglobin A 1c (A1C) has never been <8%. His blood pressure has been measured at 150/70, 148/92, and 166/88 mmHg on separate occasions during the past year at the local senior center screening clinic. Although he was told that his blood pressure was “up a little,” he was not aware of the need to keep his blood pressure ≤130/80 mmHg for both cardiovascular and renal health. 11
A.B. has never had a foot exam as part of his primary care exams, nor has he been instructed in preventive foot care. However, his medical records also indicate that he has had no surgeries or hospitalizations, his immunizations are up to date, and, in general, he has been remarkably healthy for many years.
Physical Exam
A physical examination reveals the following:
Weight: 178 lb; height: 5′2″; body mass index (BMI): 32.6 kg/m 2
Fasting capillary glucose: 166 mg/dl
Blood pressure: lying, right arm 154/96 mmHg; sitting, right arm 140/90 mmHg
Pulse: 88 bpm; respirations 20 per minute
Eyes: corrective lenses, pupils equal and reactive to light and accommodation, Fundi-clear, no arteriolovenous nicking, no retinopathy
Thyroid: nonpalpable
Lungs: clear to auscultation
Heart: Rate and rhythm regular, no murmurs or gallops
Vascular assessment: no carotid bruits; femoral, popliteal, and dorsalis pedis pulses 2+ bilaterally
Neurological assessment: diminished vibratory sense to the forefoot, absent ankle reflexes, monofilament (5.07 Semmes-Weinstein) felt only above the ankle
Lab Results
Results of laboratory tests (drawn 5 days before the office visit) are as follows:
Glucose (fasting): 178 mg/dl (normal range: 65–109 mg/dl)
Creatinine: 1.0 mg/dl (normal range: 0.5–1.4 mg/dl)
Blood urea nitrogen: 18 mg/dl (normal range: 7–30 mg/dl)
Sodium: 141 mg/dl (normal range: 135–146 mg/dl)
Potassium: 4.3 mg/dl (normal range: 3.5–5.3 mg/dl)
Lipid panel
• Total cholesterol: 162 mg/dl (normal: <200 mg/dl)
• HDL cholesterol: 43 mg/dl (normal: ≥40 mg/dl)
• LDL cholesterol (calculated): 84 mg/dl (normal: <100 mg/dl)
• Triglycerides: 177 mg/dl (normal: <150 mg/dl)
• Cholesterol-to-HDL ratio: 3.8 (normal: <5.0)
AST: 14 IU/l (normal: 0–40 IU/l)
ALT: 19 IU/l (normal: 5–40 IU/l)
Alkaline phosphotase: 56 IU/l (normal: 35–125 IU/l)
A1C: 8.1% (normal: 4–6%)
Urine microalbumin: 45 mg (normal: <30 mg)
Based on A.B.’s medical history, records, physical exam, and lab results, he is assessed as follows:
Uncontrolled type 2 diabetes (A1C >7%)
Obesity (BMI 32.4 kg/m 2 )
Hyperlipidemia (controlled with atorvastatin)
Peripheral neuropathy (distal and symmetrical by exam)
Hypertension (by previous chart data and exam)
Elevated urine microalbumin level
Self-care management/lifestyle deficits
• Limited exercise
• High carbohydrate intake
• No SMBG program
Poor understanding of diabetes
A.B. presented with uncontrolled type 2 diabetes and a complex set of comorbidities, all of which needed treatment. The first task of the NP who provided his care was to select the most pressing health care issues and prioritize his medical care to address them. Although A.B. stated that his need to lose weight was his chief reason for seeking diabetes specialty care, his elevated glucose levels and his hypertension also needed to be addressed at the initial visit.
The patient and his wife agreed that a referral to a dietitian was their first priority. A.B. acknowledged that he had little dietary information to help him achieve weight loss and that his current weight was unhealthy and “embarrassing.” He recognized that his glucose control was affected by large portions of bread and pasta and agreed to start improving dietary control by reducing his portion size by one-third during the week before his dietary consultation. Weight loss would also be an important first step in reducing his blood pressure.
The NP contacted the registered dietitian (RD) by telephone and referred the patient for a medical nutrition therapy assessment with a focus on weight loss and improved diabetes control. A.B.’s appointment was scheduled for the following week. The RD requested that during the intervening week, the patient keep a food journal recording his food intake at meals and snacks. She asked that the patient also try to estimate portion sizes.
Although his physical activity had increased since his retirement, it was fairly sporadic and weather-dependent. After further discussion, he realized that a week or more would often pass without any significant form of exercise and that most of his exercise was seasonal. Whatever weight he had lost during the summer was regained in the winter, when he was again quite sedentary.
A.B.’s wife suggested that the two of them could walk each morning after breakfast. She also felt that a treadmill at home would be the best solution for getting sufficient exercise in inclement weather. After a short discussion about the positive effect exercise can have on glucose control, the patient and his wife agreed to walk 15–20 minutes each day between 9:00 and 10:00 a.m.
A first-line medication for this patient had to be targeted to improving glucose control without contributing to weight gain. Thiazolidinediones (i.e., rosiglitizone [Avandia] or pioglitizone [Actos]) effectively address insulin resistance but have been associated with weight gain. 12 A sulfonylurea or meglitinide (i.e., repaglinide [Prandin]) can reduce postprandial elevations caused by increased carbohydrate intake, but they are also associated with some weight gain. 12 When glyburide was previously prescribed, the patient exhibited signs and symptoms of hypoglycemia (unconfirmed by SMBG). α-Glucosidase inhibitors (i.e., acarbose [Precose]) can help with postprandial hyperglycemia rise by blunting the effect of the entry of carbohydrate-related glucose into the system. However, acarbose requires slow titration, has multiple gastrointestinal (GI) side effects, and reduces A1C by only 0.5–0.9%. 13 Acarbose may be considered as a second-line therapy for A.B. but would not fully address his elevated A1C results. Metformin (Glucophage), which reduces hepatic glucose production and improves insulin resistance, is not associated with hypoglycemia and can lower A1C results by 1%. Although GI side effects can occur, they are usually self-limiting and can be further reduced by slow titration to dose efficacy. 14
After reviewing these options and discussing the need for improved glycemic control, the NP prescribed metformin, 500 mg twice a day. Possible GI side effects and the need to avoid alcohol were of concern to A.B., but he agreed that medication was necessary and that metformin was his best option. The NP advised him to take the medication with food to reduce GI side effects.
The NP also discussed with the patient a titration schedule that increased the dosage to 1,000 mg twice a day over a 4-week period. She wrote out this plan, including a date and time for telephone contact and medication evaluation, and gave it to the patient.
During the visit, A.B. and his wife learned to use a glucose meter that features a simple two-step procedure. The patient agreed to use the meter twice a day, at breakfast and dinner, while the metformin dose was being titrated. He understood the need for glucose readings to guide the choice of medication and to evaluate the effects of his dietary changes, but he felt that it would not be “a forever thing.”
The NP reviewed glycemic goals with the patient and his wife and assisted them in deciding on initial short-term goals for weight loss, exercise, and medication. Glucose monitoring would serve as a guide and assist the patient in modifying his lifestyle.
A.B. drew the line at starting an antihypertensive medication—the angiotensin-converting enzyme (ACE) inhibitor enalapril (Vasotec), 5 mg daily. He stated that one new medication at a time was enough and that “too many medications would make a sick man out of me.” His perception of the state of his health as being represented by the number of medications prescribed for him gave the advanced practice nurse an important insight into the patient’s health belief system. The patient’s wife also believed that a “natural solution” was better than medication for treating blood pressure.
Although the use of an ACE inhibitor was indicated both by the level of hypertension and by the presence of microalbuminuria, the decision to wait until the next office visit to further evaluate the need for antihypertensive medication afforded the patient and his wife time to consider the importance of adding this pharmacotherapy. They were quite willing to read any materials that addressed the prevention of diabetes complications. However, both the patient and his wife voiced a strong desire to focus their energies on changes in food and physical activity. The NP expressed support for their decision. Because A.B. was obese, weight loss would be beneficial for many of his health issues.
Because he has a sedentary lifestyle, is >35 years old, has hypertension and peripheral neuropathy, and is being treated for hypercholestrolemia, the NP performed an electrocardiogram in the office and referred the patient for an exercise tolerance test. 11 In doing this, the NP acknowledged and respected the mutually set goals, but also provided appropriate pre-exercise screening for the patient’s protection and safety.
In her role as diabetes educator, the NP taught A.B. and his wife the importance of foot care, demonstrating to the patient his inability to feel the light touch of the monofilament. She explained that the loss of protective sensation from peripheral neuropathy means that he will need to be more vigilant in checking his feet for any skin lesions caused by poorly fitting footwear worn during exercise.
At the conclusion of the visit, the NP assured A.B. that she would share the plan of care they had developed with his primary care physician, collaborating with him and discussing the findings of any diagnostic tests and procedures. She would also work in partnership with the RD to reinforce medical nutrition therapies and improve his glucose control. In this way, the NP would facilitate the continuity of care and keep vital pathways of communication open.
Advanced practice nurses are ideally suited to play an integral role in the education and medical management of people with diabetes. 15 The combination of clinical skills and expertise in teaching and counseling enhances the delivery of care in a manner that is both cost-reducing and effective. Inherent in the role of advanced practice nurses is the understanding of shared responsibility for health care outcomes. This partnering of nurse with patient not only improves care but strengthens the patient’s role as self-manager.
Geralyn Spollett, MSN, C-ANP, CDE, is associate director and an adult nurse practitioner at the Yale Diabetes Center, Department of Endocrinology and Metabolism, at Yale University in New Haven, Conn. She is an associate editor of Diabetes Spectrum.
Note of disclosure: Ms. Spollett has received honoraria for speaking engagements from Novo Nordisk Pharmaceuticals, Inc., and Aventis and has been a paid consultant for Aventis. Both companies produce products and devices for the treatment of diabetes.
Email alerts
- Advanced Practice Care: Advanced Practice Care in Diabetes: Epilogue
- Advanced Practice Care: Advanced Practice Care in Diabetes: Preface
- Online ISSN 1944-7353
- Print ISSN 1040-9165
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
- Reference Manager
- Simple TEXT file
People also looked at
Hypothesis and theory article, type 2 diabetes mellitus: a pathophysiologic perspective.

- Department of Medicine, Duke University, Durham, NC, United States
Type 2 Diabetes Mellitus (T2DM) is characterized by chronically elevated blood glucose (hyperglycemia) and elevated blood insulin (hyperinsulinemia). When the blood glucose concentration is 100 milligrams/deciliter the bloodstream of an average adult contains about 5–10 grams of glucose. Carbohydrate-restricted diets have been used effectively to treat obesity and T2DM for over 100 years, and their effectiveness may simply be due to lowering the dietary contribution to glucose and insulin levels, which then leads to improvements in hyperglycemia and hyperinsulinemia. Treatments for T2DM that lead to improvements in glycemic control and reductions in blood insulin levels are sensible based on this pathophysiologic perspective. In this article, a pathophysiological argument for using carbohydrate restriction to treat T2DM will be made.
Introduction
Type 2 Diabetes Mellitus (T2DM) is characterized by a persistently elevated blood glucose, or an elevation of blood glucose after a meal containing carbohydrate ( 1 ) ( Table 1 ). Unlike Type 1 Diabetes which is characterized by a deficiency of insulin, most individuals affected by T2DM have elevated insulin levels (fasting and/or post glucose ingestion), unless there has been beta cell failure ( 2 , 3 ). The term “insulin resistance” (IR) has been used to explain why the glucose levels remain elevated even though there is no deficiency of insulin ( 3 , 4 ). Attempts to determine the etiology of IR have involved detailed examinations of molecular and intracellular pathways, with attribution of cause to fatty acid flux, but the root cause has been elusive to experts ( 5 – 7 ).
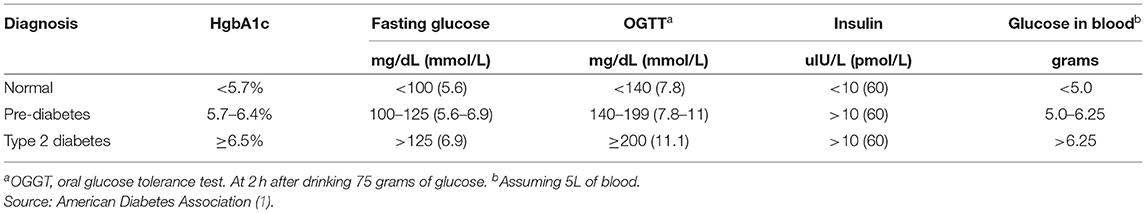
Table 1 . Definition of type 2 diabetes mellitus.
How Much Glucose Is in the Blood?
Keeping in mind that T2DM involves an elevation of blood glucose, it is important to understand how much glucose is in the blood stream to begin with, and then the factors that influence the blood glucose—both exogenous and endogenous factors. The amount of glucose in the bloodstream is carefully controlled—approximately 5–10 grams in the bloodstream at any given moment, depending upon the size of the person. To calculate this, multiply 100 milligrams/deciliter × 1 gram/1,000 milligrams × 10 deciliters/1 liter × 5 liters of blood. The “zeros cancel” and you are left with 5 grams of glucose if the individual has 5 liters of blood. Since red blood cells represent about 40% of the blood volume, and the glucose is in equilibrium, there may be an extra 40% glucose because of the red blood cell reserve ( 8 ). Adding the glucose from the serum and red blood cells totals about 5–10 grams of glucose in the entire bloodstream.
Major Exogenous Factors That Raise the Blood Glucose
Dietary carbohydrate is the major exogenous factor that raises the blood glucose. When one considers that it is common for an American in 2021 to consume 200–300 grams of carbohydrate daily, and most of this carbohydrate is digested and absorbed as glucose, the body absorbs and delivers this glucose via the bloodstream to the cells while attempting to maintain a normal blood glucose level. Thinking of it in this way, if 200–300 grams of carbohydrates is consumed in a day, the bloodstream that holds 5–10 grams of glucose and has a concentration of 100 milligrams/deciliter, is the conduit through which 200,000–300,000 milligrams (200 grams = 200,000 milligrams) passes over the course of a day.
Major Endogenous Factors That Raise the Blood Glucose
There are many endogenous contributors that raise the blood glucose. There are at least 3 different hormones that increase glucose levels: glucagon, epinephrine, and cortisol. These hormones increase glucose levels by increasing glycogenolysis and gluconeogenesis ( 9 ). Without any dietary carbohydrate, the normal human body can generate sufficient glucose though the mechanism of glucagon secretion, gluconeogenesis, glycogen storage and glycogenolysis ( 10 ).
Major Exogenous Factors That Lower the Blood Glucose
A reduction in dietary carbohydrate intake can lower the blood glucose. An increase in activity or exercise usually lowers the blood glucose ( 11 ). There are many different medications, employing many mechanisms to lower the blood glucose. Medications can delay sucrose and starch absorption (alpha-glucosidase inhibitors), slow gastric emptying (GLP-1 agonists, DPP-4 inhibitors) enhance insulin secretion (sulfonylureas, meglitinides, GLP-1 agonists, DPP-4 inhibitors), reduce gluconeogenesis (biguanides), reduce insulin resistance (biguanides, thiazolidinediones), and increase urinary glucose excretion (SGLT-2 inhibitors). The use of medications will also have possible side effects.
Major Endogenous Factors That Lower the Blood Glucose
The major endogenous mechanism to lower the blood glucose is to deliver glucose into the cells (all cells can use glucose). If the blood glucose exceeds about 180 milligrams/deciliter, then loss of glucose into the urine can occur. The blood glucose is reduced by cellular uptake using glut transporters ( 12 ). Some cells have transporters that are responsive to the presence of insulin to activate (glut4), others have transporters that do not require insulin for activation. Insulin-responsive glucose transporters in muscle cells and adipose cells lead to a reduction in glucose levels—especially after carbohydrate-containing meals ( 13 ). Exercise can increase the glucose utilization in muscle, which then increases glucose cellular uptake and reduce the blood glucose levels. During exercise, when the metabolic demands of skeletal muscle can increase more than 100-fold, and during the absorptive period (after a meal), the insulin-responsive glut4 transporters facilitate the rapid entry of glucose into muscle and adipose tissue, thereby preventing large fluctuations in blood glucose levels ( 13 ).
Which Cells Use Glucose?
Glucose can used by all cells. A limited number of cells can only use glucose, and are “glucose-dependent.” It is generally accepted that the glucose-dependent cells include red blood cells, white blood cells, and cells of the renal papilla. Red blood cells have no mitochondria for beta-oxidation, so they are dependent upon glucose and glycolysis. White blood cells require glucose for the respiratory burst when fighting infections. The cells of the inner renal medulla (papilla) are under very low oxygen tension, so therefore must predominantly use glucose and glycolysis. The low oxygen tension is a result of the countercurrent mechanism of urinary concentration ( 14 ). These glucose-dependent cells have glut transporters that do not require insulin for activation—i.e., they do not need insulin to get glucose into the cells. Some cells can use glucose and ketones, but not fatty acids. The central nervous system is believed to be able to use glucose and ketones for fuel ( 15 ). Other cells can use glucose, ketones, and fatty acids for fuel. Muscle, even cardiac muscle, functions well on fatty acids and ketones ( 16 ). Muscle cells have both non-insulin-responsive and insulin-responsive (glut4) transporters ( 12 ).
Possible Dual Role of an Insulin-Dependent Glucose-Transporter (glut4)
A common metaphor is to think of the insulin/glut transporter system as a key/lock mechanism. Common wisdom states that the purpose of insulin-responsive glut4 transporters is to facilitate glucose uptake when blood insulin levels are elevated. But, a lock serves two purposes: to let someone in and/or to keep someone out . So, one of the consequences of the insulin-responsive glut4 transporter is to keep glucose out of the muscle and adipose cells, too, when insulin levels are low. The cells that require glucose (“glucose-dependent”) do not need insulin to facilitate glucose entry into the cell (non-insulin-responsive transporters). In a teleological way, it would “make no sense” for cells that require glucose to have insulin-responsive glut4 transporters. Cells that require glucose have glut1, glut2, glut3, glut5 transporters—none of which are insulin-responsive (Back to the key/lock metaphor, it makes no sense to have a lock on a door that you want people to go through). At basal (low insulin) conditions, most glucose is used by the brain and transported by non-insulin-responsive glut1 and glut3. So, perhaps one of the functions of the insulin-responsive glucose uptake in muscle and adipose to keep glucose OUT of the these cells at basal (low insulin) conditions, so that the glucose supply can be reserved for the tissue that is glucose-dependent (blood cells, renal medulla).
What Causes IR and T2DM?
The current commonly espoused view is that “Type 2 diabetes develops when beta-cells fail to secrete sufficient insulin to keep up with demand, usually in the context of increased insulin resistance.” ( 17 ). Somehow, the beta cells have failed in the face of insulin resistance. But what causes insulin resistance? When including the possibility that the environment may be part of the problem, is it possible that IR is an adaptive (protective) response to excess glucose availability? From the perspective that carbohydrate is not an essential nutrient and the change in foods in recent years has increased the consumption of refined sugar and flour, maybe hyperinsulinemia is the cause of IR and T2DM, as cells protect themselves from excessive glucose and insulin levels.
Insulin Is Already Elevated in IR and T2DM
Clinical experience of most physicians using insulin to treat T2DM over time informs us that an escalation of insulin dose is commonly needed to achieve glycemic control (when carbohydrate is consumed). When more insulin is given to someone with IR, the IR seems to get worse and higher levels of insulin are needed. I have the clinical experience of treating many individuals affected by T2DM and de-prescribing insulin as it is no longer needed after consuming a diet without carbohydrate ( 18 ).
Diets Without Carbohydrate Reverse IR and T2DM
When dietary manipulation was the only therapy for T2DM, before medications were available, a carbohydrate-restricted diet was used to treat T2DM ( 19 – 21 ). Clinical experience of obesity medicine physicians and a growing number of recent studies have demonstrated that carbohydrate-restricted diets reverse IR and T2DM ( 18 , 22 , 23 ). Other methods to achieve caloric restriction also have these effects, like calorie-restricted diets and bariatric surgery ( 24 , 25 ). There may be many mechanisms by which these approaches may work: a reduction in glucose, a reduction in insulin, nutritional ketosis, a reduction in metabolic syndrome, or a reduction in inflammation ( 26 ). Though there may be many possible mechanisms, let's focus on an obvious one: a reduction in blood glucose. Let's assume for a moment that the excessive glucose and insulin leads to hyperinsulinemia and this is the cause of IR. On a carbohydrate-restricted diet, the reduction in blood glucose leads to a reduction in insulin. The reduction in insulin leads to a reduction in insulin resistance. The reduction in insulin leads to lipolysis. The resulting lowering of blood glucose, insulin and body weight reverses IR, T2DM, AND obesity. These clinical observations strongly suggest that hyperinsulinemia is a cause of IR and T2DM—not the other way around.
What Causes Atherosclerosis?
For many years, the metabolic syndrome has been described as a possible cause of atherosclerosis, but there are no RCTs directly targeting metabolic syndrome, and the current drug treatment focuses on LDL reduction, so its importance remains controversial. A recent paper compared the relative importance of many risk factors in the prediction of the first cardiac event in women, and the most powerful predictors were diabetes, metabolic syndrome, smoking, hypertension and BMI ( 27 ). The connection between dietary carbohydrate and fatty liver is well-described ( 28 ). The connection between fatty liver and atherosclerosis is well-described ( 29 ). It is very possible that the transport of excess glucose to the adipose tissue via lipoproteins creates the particles that cause the atherosclerotic damage (small LDL) ( Figure 1 ) ( 30 – 32 ). This entire process of dietary carbohydrate leading to fatty liver, leading to small LDL, is reversed by a diet without carbohydrate ( 26 , 33 , 34 ).
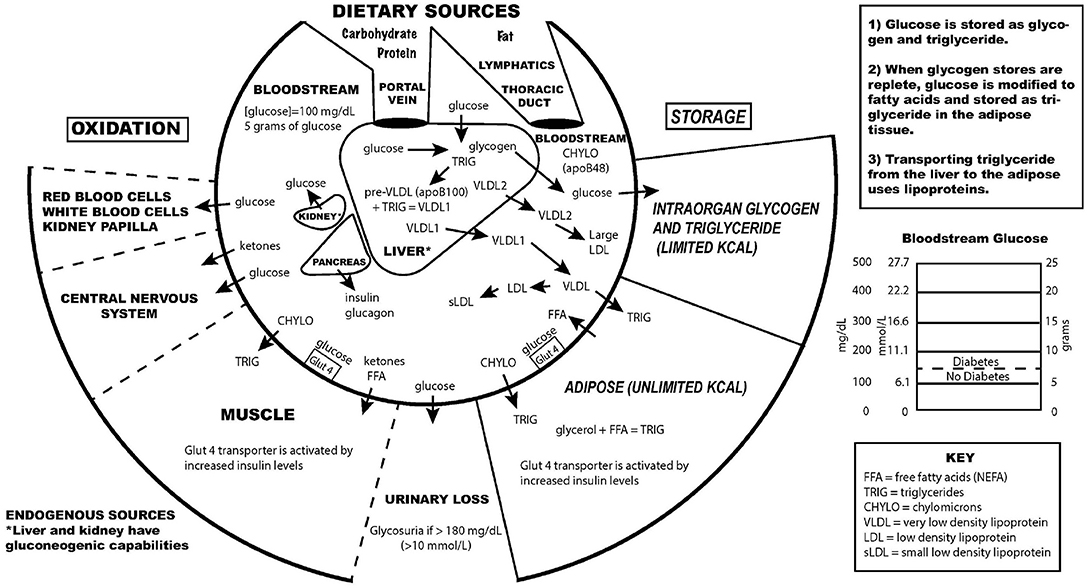
Figure 1 . Key aspects of the interconnection between glucose and lipoprotein metabolism.
Reducing dietary carbohydrate in the context of a low carbohydrate, ketogenic diet reduces hyperglycemia and hyperinsulinemia, IR and T2DM. In the evaluation of an individual for a glucose abnormality, measure the blood glucose and insulin levels. If the insulin level (fasting or after a glucose-containing meal) is high, do not give MORE insulin—instead, use an intervention to lower the insulin levels. Effective ways to reduce insulin resistance include lifestyle, medication, and surgical therapies ( 23 , 35 ).
The search for a single cause of a complex problem is fraught with difficulty and controversy. I am not hypothesizing that excessive dietary carbohydrate is the only cause of IR and T2DM, but that it is a cause, and quite possibly the major cause. How did such a simple explanation get overlooked? I believe it is very possible that the reductionistic search for intracellular molecular mechanisms of IR and T2DM, the emphasis on finding pharmaceutical (rather than lifestyle) treatments, the emphasis on the treatment of high total and LDL cholesterol, and the fear of eating saturated fat may have misguided a generation of researchers and clinicians from the simple answer that dietary carbohydrate, when consumed chronically in amounts that exceeds an individual's ability to metabolize them, is the most common cause of IR, T2DM and perhaps even atherosclerosis.
While there has historically been a concern about the role of saturated fat in the diet as a cause of heart disease, most nutritional experts now cite the lack of evidence implicating dietary saturated fat as the reason for lack of concern of it in the diet ( 36 ).
The concept of comparing medications that treat IR by insulin-sensitizers or by providing insulin itself was tested in the Bari-2D study ( 37 ). Presumably in the context of consuming a standard American diet, this study found no significant difference in death rates or major cardiovascular events between strategies of insulin sensitization or insulin provision.
While lifestyle modification may be ideal to prevent or cure IR and T2DM, for many people these changes are difficult to learn and/or maintain. Future research should be directed toward improving adherence to all effective lifestyle or medication treatments. Future research is also needed to assess the effect of carbohydrate restriction on primary or secondary prevention of outcomes of cardiovascular disease.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Conflict of Interest
EW receives royalties from popular diet books and is founder of a company based on low-carbohydrate diet principles (Adapt Your Life, Inc.).
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. American Diabetes Association. Classification and diagnosis of diabetes. Diabetes Care . (2016) 39 (Suppl. 1):S13–22. doi: 10.2337/dc16-S005
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Bogardus C, Lillioja S, Howard BV, Reaven G, Mott D. Relationships between insulin secretion, insulin action, and fasting plasma glucose concentration in nondiabetic and noninsulin-dependent diabetic subjects. J Clin Invest. (1984) 74:1238–46. doi: 10.1172/JCI111533
3. Reaven GM. Compensatory hyperinsulinemia and the development of an atherogenic lipoprotein profile: the price paid to maintain glucose homeostasis in insulin-resistant individuals. Endocrinol Metab Clin North Am. (2005) 34:49–62. doi: 10.1016/j.ecl.2004.12.001
4. DeFronzo RA, Ferrannini E. Insulin resistance. A multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care. (1991) 14:173–94. doi: 10.2337/diacare.14.3.173
5. Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. (2005) 365:1415–28. doi: 10.1016/S0140-6736(05)66378-7
6. Yaribeygi H, Farrokhi FR, Butler AE, Sahebkar A. Insulin resistance: review of the underlying molecular mechanisms. J Cell Physiol. (2019) 234:8152–61. doi: 10.1002/jcp.27603
7. Shulman GI. Cellular mechanisms of insulin resistance. J Clin Invest. (2000) 106:171–6. doi: 10.1172/JCI10583
8. Guizouarn H, Allegrini B. Erythroid glucose transport in health and disease. Pflugers Arch. (2020) 472:1371–83. doi: 10.1007/s00424-020-02406-0
9. Petersen MC, Vatner DF, Shulman GI. Regulation of hepatic glucose metabolism in health and disease. Nat Rev Endocrinol. (2017) 13:572–87. doi: 10.1038/nrendo.2017.80
10. Tondt J, Yancy WS, Westman EC. Application of nutrient essentiality criteria to dietary carbohydrates. Nutr Res Rev. (2020) 33:260–70. doi: 10.1017/S0954422420000050
11. Colberg SR, Hernandez MJ, Shahzad F. Blood glucose responses to type, intensity, duration, and timing of exercise. Diabetes Care. (2013) 36:e177. doi: 10.2337/dc13-0965
12. Mueckler M, Thorens B. The SLC2 (GLUT) family of membrane transporters. Mol Aspects Med. (2013) 34:121–38. doi: 10.1016/j.mam.2012.07.001
13. Bryant NJ, Govers R, James DE. Regulated transport of the glucose transporter GLUT4. Nat Rev Mol Cell Biol. (2002) 3:267–77. doi: 10.1038/nrm782
14. Epstein FH. Oxygen and renal metabolism. Kidney Int. (1997) 51:381–5. doi: 10.1038/ki.1997.50
15. Cahill GF. Fuel metabolism in starvation. Annu Rev Nutr. (2006) 26:1–22. doi: 10.1146/annurev.nutr.26.061505.111258
16. Murashige D, Jang C, Neinast M, Edwards JJ, Cowan A, Hyman MC, et al. Comprehensive quantification of fuel use by the failing and nonfailing human heart. Science. (2020) 370:364–8. doi: 10.1126/science.abc8861
17. Skyler JS, Bakris GL, Bonifacio E, Darsow T, Eckel RH, Groop L, et al. Differentiation of diabetes by pathophysiology, natural history, and prognosis. Diabetes. (2017) 66:241–55. doi: 10.2337/db16-0806
18. Westman EC, Yancy WS, Mavropoulos JC, Marquart M, McDuffie JR. The effect of a low-carbohydrate, ketogenic diet versus a low-glycemic index diet on glycemic control in type 2 diabetes mellitus. Nutr Metab. (2008) 5:36. doi: 10.1186/1743-7075-5-36
CrossRef Full Text | Google Scholar
19. Allen F. The treatment of diabetes. Boston Med Surg J. (1915) 172:241–7. doi: 10.1056/NEJM191502181720702
20. Osler W, McCrae T. The Principles and Practice of Medicine . 9th ed. New York and London: Appleton & Company (1923).
21. Lennerz BS, Koutnik AP, Azova S, Wolfsdorf JI, Ludwig DS. Carbohydrate restriction for diabetes: rediscovering centuries-old wisdom. J Clin Invest. (2021) 131:e142246. doi: 10.1172/JCI142246
22. Steelman GM, Westman EC. Obesity: Evaluation and Treatment Essentials . 2nd ed. Boca Raton: CRC Press, Taylor & Francis Group (2016). 340 p.
23. Athinarayanan SJ, Adams RN, Hallberg SJ, McKenzie AL, Bhanpuri NH, Campbell WW, et al. Long-term effects of a novel continuous remote care intervention including nutritional ketosis for the management of type 2 diabetes: a 2-year non-randomized clinical trial. Front Endocrinol. (2019) 10:348. doi: 10.3389/fendo.2019.00348
24. Lim EL, Hollingsworth KG, Aribisala BS, Chen MJ, Mathers JC, Taylor R. Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia. (2011) 54:2506–14. doi: 10.1007/s00125-011-2204-7
25. Isbell JM, Tamboli RA, Hansen EN, Saliba J, Dunn JP, Phillips SE, et al. The importance of caloric restriction in the early improvements in insulin sensitivity after Roux-en-Y gastric bypass surgery. Diabetes Care. (2010) 33:1438–42. doi: 10.2337/dc09-2107
26. Bhanpuri NH, Hallberg SJ, Williams PT, McKenzie AL, Ballard KD, Campbell WW, et al. Cardiovascular disease risk factor responses to a type 2 diabetes care model including nutritional ketosis induced by sustained carbohydrate restriction at 1 year: an open label, non-randomized, controlled study. Cardiovasc Diabetol. (2018) 17:56. doi: 10.1186/s12933-018-0698-8
27. Dugani SB, Moorthy MV, Li C, Demler OV, Alsheikh-Ali AA, Ridker PM, et al. Association of lipid, inflammatory, and metabolic biomarkers with age at onset for incident coronary heart disease in women. JAMA Cardiol. (2021) 6:437–47. doi: 10.1001/jamacardio.2020.7073
28. Duwaerts CC, Maher JJ. Macronutrients and the adipose-liver axis in obesity and fatty liver. Cell Mol Gastroenterol Hepatol. (2019) 7:749–61. doi: 10.1016/j.jcmgh.2019.02.001
29. Zhang L, She Z-G, Li H, Zhang X-J. Non-alcoholic fatty liver disease: a metabolic burden promoting atherosclerosis. Clin Sci Lond Engl. (1979) 134:1775–99. doi: 10.1042/CS20200446
30. Horton TJ, Drougas H, Brachey A, Reed GW, Peters JC, Hill JO. Fat and carbohydrate overfeeding in humans: different effects on energy storage. Am J Clin Nutr. (1995) 62:19–29. doi: 10.1093/ajcn/62.1.19
31. Packard C, Caslake M, Shepherd J. The role of small, dense low density lipoprotein (LDL): a new look. Int J Cardiol. (2000) 74 (Suppl. 1):S17–22. doi: 10.1016/S0167-5273(99)00107-2
32. Borén J, Chapman MJ, Krauss RM, Packard CJ, Bentzon JF, Binder CJ, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease: pathophysiological, genetic, and therapeutic insights: a consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. (2020) 41:2313–30. doi: 10.1093/eurheartj/ehz962
33. Yancy WS, Olsen MK, Guyton JR, Bakst RP, Westman EC. A low-carbohydrate, ketogenic diet versus a low-fat diet to treat obesity and hyperlipidemia: a randomized, controlled trial. Ann Intern Med. (2004) 140:769. doi: 10.7326/0003-4819-140-10-200405180-00006
34. Tendler D, Lin S, Yancy WS, Mavropoulos J, Sylvestre P, Rockey DC, et al. The effect of a low-carbohydrate, ketogenic diet on nonalcoholic fatty liver disease: a pilot study. Dig Dis Sci. (2007) 52:589–93. doi: 10.1007/s10620-006-9433-5
35. Pories WJ, Swanson MS, MacDonald KG, Long SB, Morris PG, Brown BM, et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg. (1995) 222:339–50. doi: 10.1097/00000658-199509000-00011
36. Astrup A, Magkos F, Bier DM, Brenna JT, de Oliveira Otto MC, Hill JO, et al. Saturated fats and health: a reassessment and proposal for food-based recommendations: JACC state-of-the-art review. J Am Coll Cardiol. (2020) 76:844–57. doi: 10.1016/j.jacc.2020.05.077
37. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med . (2009) 360:2503–15. doi: 10.1056/NEJMoa0805796
Keywords: type 2 diabetes, insulin resistance, pre-diabetes, carbohydrate-restricted diets, hyperinsulinemia, hyperglycemia
Citation: Westman EC (2021) Type 2 Diabetes Mellitus: A Pathophysiologic Perspective. Front. Nutr. 8:707371. doi: 10.3389/fnut.2021.707371
Received: 09 May 2021; Accepted: 20 July 2021; Published: 10 August 2021.
Reviewed by:
Copyright © 2021 Westman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eric C. Westman, ewestman@duke.edu
This article is part of the Research Topic
Carbohydrate-restricted Nutrition and Diabetes Mellitus
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Best practice in the delivery of diabetes care in the primary care network. 2021. http://www.diabetesonthenet.com/wp-content/uploads/Diabetes-in-the-Primary-Care-Network-Structure-April-2021.pdf (accessed 14 July 2022)
Dose Adjustment For Normal Eating (DAFNE). 2020. https://dafne.nhs.uk/ (accessed 14 July 2022)
Diabetes Education and Self Management for Ongoing and Newly Diagnosed (DESMOND). 2020. https://www.desmond.nhs.uk/ (accessed 14 July 2022)
Best practice for commissioning diabetes services: An integrated care framework. 2013. http://www.diabetes-resources-production.s3-eu-west-1.amazonaws.com/diabetes-storage/migration/pdf/best-practice-commissioning-diabetes-services-integratedcare-framework-0313.pdf (accessed 14 July 2022)
Diabetes Competency Framework. 2015. https://tinyurl.com/4y974ns8 (accessed 14 July 2022)
Improving the delivery of adult diabetes care through integration. 2016. https://tinyurl.com/b46vnppp (accessed 14 July 2022)
Annual report. 2016. https://diabetes-resources-production.s3-eu-west-1.amazonaws.com/diabetes-storage/2017-08/Annual_Report_2016.pdf (accessed 14 July 2022)
Us, diabetes and a lot of facts and stats. 2019. https://www.diabetes.org.uk/resources-s3/2019-11/facts-stats-update-oct-2019.pdf (accessed 14 July 2022)
Delivering the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed Type 2 diabetes: cost effectiveness analysis. 2010. https://doi.org/10.1136/bmj.c4093
The case for diabetes population health improvement: evidence-based programming for population outcomes in diabetes. 2017. https://doi.org/10.1007/s11892-017-0875-223
Diabetes specialist nurses and role evolvement: a survey by Diabetes UK and ABCD of specialist diabetes services. 2007. https://doi.org/10.1111/j.1464-5491.2009.02716
Halfyard C, McGowan D, Whyte M Diabetes rapid access clinic: a bridge between primary and secondary care (Diabetes UK poster presentation). Diabetic Medicine. 2010; 27
Health and Social Care (HSC). DoH Diabetes Nurse Education Group, Diabetes Competency Nursing Tool. 2017. https://tinyurl.com/ycxj5hnd (accessed 14 July 2022)
Diabetes specialist nursing in the UK: the judgement call? A review of existing literature. 2011. https://doi.org/10.1002/edn.190
What Is Population Health?. 2003. https://doi.org/10.2105/AJPH.93.3.366
Population health management in diabetes care: combining clinical audit, risk stratification, and multidisciplinary virtual clinics in a community setting to improve diabetes care in a geographically defined population. an integrated diabetes care pilot in the north east locality, Oxfordshire, UK. 2020. https://doi.org/10.5334/ijic.5177
Point-of-care testing in primary cae needs: needs and attitudes of Irish GPs, BJGP Open. 2018. https://doi.org/10.3399/bjgpopen17X101229
Leading Change. The Atlas of Shared Learning. 2019. https://www.england.nhs.uk/atlas_case_study/improving-insulin-administration-in-a-community-setting/ (accessed 14 July 2022)
Prevalence and correlates of diagnosed and undiagnosed type 2 diabetes mellitus and pre-diabetes in older adults: Findings from the Irish Longitudinal Study on Ageing (TILDA). 2015. https://doi.org/10.1016/j.diabres.2015.10.015
Improving risk factor management for patients with poorly controlled type 2 diabetes: a systematic review of healthcare interventions in primary care and community settings. 2017. https://doi.org/10.1136/bmjopen-2016-015135
Organisation of services for people with cardiovascular disorders in primary care: transfer to primary care or to specialist-generalist multidisciplinary teams?. 2014. https://doi.org/10.1186/1471-2296-15-158
Public Health Skills and Knowledge Framework. User guide. 2016. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/545011/Public_Health_Skills_and_Knowledge_Framework_2016_User_Guide.pdf (accessed 14 July 2022)
Improving quality of care for persons with diabetes: an overview of systematic reviews – what does the evidence tell us?. 2013. https://doi.org/10.1186/2046-4053-2-26
World Health Organisation. Global Report on Diabetes. 2016. https://www.who.int/publications/i/item/9789241565257
Nurses' role in diabetes management and prevention in community care
Sinéad O'Flynn
Nurse and Nutritional Practitioner, Health 4 U, Cork, Ireland
View articles · Email Sinéad

Diabetes care—particularly in a community setting as a form of prevention and management, is a growing requirement across England and Ireland. Self-management skills are an essential part of diabetes management and nurses in the community setting are one of the first points of care to ensure this. It is therefore imperative that nurses working within these primary and community care settings have the knowledge and skills necessary to support those in the community setting to effectively manage their condition, improve their health outcomes and their quality of life. Primary care has been tasked with providing both routine and more complex diabetes care and highlights a risk of adverse outcomes if people with diabetes are transferred to general practices without adequate support. Developing an approach for effective and efficient joint collaboration for primary care and specialists to manage the population of people with diabetes under their care is vital in its prevention and management. So how can this be achieved and what resources are required? This article will discuss current research into clinical practice and pilots which can contribute to supporting a more holistic multi-disciplinary approach to diabetes management and prevention, and hence, a provision of community based services aimed at health prevention.
Diabetes is a well known condition which can result in significant morbidity and mortality. The World Health Organisation ( WHO, 2016 ) recommends sharing the care of diabetes between primary and specialist teams, using referrals through primary to secondary to tertiary care. Research clearly highlights that an early diagnosis, along with effective management of care can determine the clinical course and outcome of diabetes. Health services worldwide are finding it challenging to provide systematic, ongoing and skilled care due to a growing prevalence of diabetes ( Worswick, 2013 ). Diabetes UK (2019) report that diabetes continues to be a growing health concern, with 4.7 million people in the UK known to have this condition; this number signifies an exponential increase, having doubled over the last 20 years. Mortality rates remain high due to the macrovascular complications of the condition, with over 500 diabetics dying prematurely. It is also reported by Gillet et al (2013) that self-management is often difficult due to the rising number of older people developing diabetes who already have other conditions such as dementia and arthritis. This results in community care having to administer insulin, adding pressure to already constrained services ( Leading Change, 2019 ). Leahy et al (2015) report from The Irish LongituDinal Study on Ageing (TILDA) that type 2 diabetes is the leading cause of death and disability in Ireland, and it is well known that diabetes increases risk of heart attacks, heart failure and kidney disease, resulting in a loss of independence and early mortality. They further note that diabetes accounts for 10% expenditure in the Health Service Executive (HSE), the Irish public healthcare system. The 2015 report also highlighted diabetes being more common in men than women and that those with diabetes are more likely to be obese with low levels of physical activity and suffering with other ailments such as high cholesterol and high blood pressure. The TILDA study provided, and continues to provide, the first Irish national prevalence in diagnosed, undiagnosed and pre–diabetes in older Irish adults, shaping the future for evidence based prevention programmes.
To increase prevention of diabetes and to decrease the burden to healthcare services in the long term, leading change across the community setting is a vital component of reducing mortality and morbidity with diabetes. Health and Social Care ( HSC, 2017 ) states district/community nurses are well placed to support people living with diabetes in the community. As nurses are members of a multi-disciplinary team (MDT), they can be part of a provision of services with a management strategy of a preventative holistic approach in community nursing and primary care to effectively manage the care of diabetes. It is important that care is not solely focused on treatment and management; diabetes prevention and its integration across MDT in community settings also needs to be part of this change ( Ali et al, 2021 ). So what does the research indicate regarding nursing and the community?
Nurses role – diabetes management and prevention
The crucial role of the diabetes specialist nurses (DSNs) in the provision of good patient care and promoting self-care management cannot be underestimated. They are often the first point of contact for people newly diagnosed with diabetes, and care can be employed in a variety of settings ( Gosden et al, 2007 ). Their work in the provision of education, training and support helps achieve the MDT approach with promoting self-care in diabetes and through screening and prevention of type 2 diabetes ( James, 2011 ).
All nursing staff have an important role in the treatment, management and prevention of diabetes through the promotion of dietary and lifestyle adaptations ( Halfyard et al, 2010 ). The risk factors associated with diabetes are well-researched; these include lack of physical activity, a poor diet, high blood pressure, high cholesterol, smoking and excessive alcohol consumption. According to Murphy et al (2017) , healthcare professionals can promote the adaptation of lifestyle and dietary changes, which can often lead to the reduction of incidence rates in type 2 diabetes. While type 1 diabetes cannot be prevented, advice on taking steps to prevent further health conditions can help reduce the need for further care by ensuring that treatment is provided as early as detection.
Diabetes UK (2013) highlight the vital role practice nurses have as they are often the people who carry out the annual diabetes and foot checks. Practice nurses also play a clinical role in screening, maintaining and supporting people with diabetes.
This brings into discussion another very important aspect of diabetes management and risk reduction. Using equipments such as point of care testing (POCT) can play an extremely important role in diabetes prevention and management. Practice nurses and community nurses are well placed to provide this type of non-invasive fingertip testing. These tests provide instant results, meaning dietary and lifestyle advice can be offered on the spot, tailored to the individual's health needs. POCT is defined as a laboratory service using small analytical devices conducted in a patient consultation setting rather than in a traditional central laboratory, thus providing results in real time with faster decision making. This makes it a convenient test with rapidly available results, providing immediate impact for the patients, with a potential change to their care and the appropriate advice provided at the appointment consult. Laima et al (2019) state that POCT facilitates efficient clinical management, reducing patient morbidity and mortality in primary care. POCT also contributes to cost savings in an overburdened healthcare system, enhances patients' quality of life and increases patient satisfaction. The increased utilisation of POCTs in primary health care is likely to play a significant role in the future (Laima et al, 2019). When used appropriately, POCT can lead to more efficient, effective medical treatments and improved quality of medical care. The author of this article, a nurse and nutritional practitioner, utilises POCT in their healthcare service where health promotion and prevention are the main goals. POCT is expected to continue to expand, changing the way healthcare is delivered, meaning more patient-driven and focused care (Laima et al, 2019).
Leading Change (2019) reports another area which proved successful in diabetes management in the community. They reported a previous audit by specialist diabetes nurses resulting in a modular training programme being developed to upskill both community nurses and non-registered practitioners in diabetes care. The programme was supported by the Department of Health's Knowledge and Skills Framework (2016) and by the Diabetes National Workforce Competence Framework (2015) . It provided classroom teaching with written and oral competency assessments consisting of three modules: 1) diabetes awareness 2) expansion of diabetes knowledge and 3) insulin administration for a non-registered practitioner.
Another area explored through research and which needs further evidence of the outcomes, is a population health approach ( Kindig and Stoddart, 2003 ). A population health approach has the potential to improve the quality of care of individuals by introducing solutions targeting groups and sub-groups at risk of developing complications from diabetes ( Golden et al, 2017 ). Golden et al (2017) state this approach is a whole system effort which can systematically identify, reach and improve care for all individual patients from groups which are identified as being at risk of poor outcomes. Golden et al (2017) highlight that the steps in the process involve measuring health status of a defined group of people and the distribution of health outcomes within each group. Identifying determinants of health then occurs, with designing and implementing of interventions occurring after and lastly, measuring their effectiveness.
Research recognises that good diabetes care pathways address the needs of the local service and is underpinned by a multidisciplinary team. Koslowska et al's (2020) pilot of virtual clinics in diabetes care highlighted that MDT virtual clinics in the community are one of the options for joint collaboration with primary care staff being supported by the specialist team. They argue that virtual clinics are associated with improved outcomes and show a positive impact on care processes following the success of their pilot study on a population health approach in diabetes care. The pilot enabled the service to discuss the outcomes of audit, taking into consideration the characteristics of the population and plan for improvement, proactively identify groups of patients at risk of complications from diabetes, and then plan their care together. They also reported that unnecessary referrals were avoided by the encouragement of shared responsibility and decision making for changes in treatment.
Other areas where resources for diabetes help to shape diabetes care within the community are resources provided by Diabetes UK such as DAFNE (2020) -a working collaborative of 75 diabetes services across the UK and Ireland, which is an intensive insulin therapy for type 1 diabetes. Another example of care pathways is DESMOND (2020) – a group of self-management education models and toolkits for the management of type 2 diabetes.
Diabetes UK (2013) state how planning and organising for the future has never been more important. With an ageing population compounded by people having increasingly complex health and social needs, the NHS and the Health Service Executive (HSE - the Irish public healthcare service) face financial and workforce challenges. Considering the current restraints in healthcare environments, Kozlowska's (2020) recommendations on care management-requiring a coordinated MDT approach, with a focus on effective early care in primary and community settings to reduce pressure on acute services (and reduce the onset of diabetes complications) is more important than ever. Price et al (2014) report that collaborative working is fundamental to the delivery of diabetes care in primary care networks and a multidisciplinary approach is essential to ensuring all core elements of care are met. Primary care has historically struggled with insufficient staffing and capacity to meet rising patient demands and complexity. Utilising POCT for prevention of diabetes, education programmes for HCP's and a population health approach are all areas reporting the success of diabetes management and prevention and are areas which need to be further developed and implemented.

Self-Management of Type 2 Diabetes Comprehensive Nursing Essay Example
- Rachel R.N. R.N.
- October 14, 2023
- Samples for MSN students
Introduction
Individuals with type 2 diabetes require proper disease management that includes control of their blood sugar levels, adopting healthy eating, exercises, medication, or insulin. Many people can effectively manage type 2 diabetes with adequate resources and support. If the condition is not properly managed, it can affect other body organs, leading to complications like bacterial and fungal infections and skin problems. Worst case scenario, lack of proper management increase patient mortality rates. Conducting a needs assessment is critical to help an organization identify gaps that prevent it from achieving the desired goals, in this case, proper type 2 diabetes self-management. The gaps can exist in the organization’s knowledge, practices, or skills regarding the problem. The assessment helps the organization determine effective strategies and interventions to accomplish its objectives. The purpose of this paper is to identify an organizational gap and associate interventions that can help fill the gap for better patient outcomes. The paper includes a practice gap description, a summary of the organizational needs, and the development of the practice question (PICOT).(Self-Management of Type 2 Diabetes Comprehensive Nursing Essay Example)

The problem affects the endocrinology unit that specializes in treating patients with diabetes. The endocrinologists working in the unit are the key stakeholders responsible for informing and advising major decisions regarding diabetes. The hospital leaders and administrators are also responsible for making major decisions to address the gap identified and support intervention implementation through resource mobilization. The problem identified is self-management among the rising number of type 2 diabetes patients(Self-Management of Type 2 Diabetes Comprehensive Nursing Essay Example). Limited access to diabetes self-management education at the hospital affects the patients’ ability to manage their condition effectively. The endocrinologists are responsible for treating people with diabetes and are directly affected by the identified problem. They understand what is best for their patients, and the needs assessment informs the need for diabetes self-management education (DSME/S). The leadership and administration are responsible for supporting the recommended interventions, and their decisions directly impact the unit’s efficiency in addressing the gap.(Self-Management of Type 2 Diabetes Comprehensive Nursing Essay Example)
Practice Gap
The identified gap is the lack of proper practice guidelines that support type 2 diabetes self-managemen t at the practice site. Specifically, the needs assessment identified a lack of diabetes self-management education to guide the patient in managing their condition. Many barriers prevent the implementation of a proper patient education platform or means, including limited funding and staff members, workload and time pressures, patients’ access issues, and uncoordinated relationships and communication with other specialist teams. (Self-Management of Type 2 Diabetes Comprehensive Nursing Essay Example)The lack of education means patients have inadequate knowledge and behavioral guidelines and support to manage their condition. DSME/S is crucial as it helps and motivates patients to adjust to lifestyles after diagnoses and during the treatment process. The identified intervention is face-to-face and telephone-based family-oriented education in type 2 diabetes management (Hemmati et al., 2017). The use of mhealth mobile applications is also an intervention that can help patients live healthily by sending patients adherence and treatment guidelines through messages (Boels et al., 2019). However, the hospital lacks practice guidelines for mobile applications used in type 2 diabetes management. The rising number of type 2 diabetes patients requires more effort from the care team to educate the patients to adhere to treatment and management guidelines. (Self-Management of Type 2 Diabetes Comprehensive Nursing Essay Example)

Practice Question
For patients with type 2 diabetes, does the implementation of face-to-face and telephone-based family-oriented education and mhealth mobile applications compared to written patient education materials improve self-management of type 2 diabetes among patients after diagnosis and during the treatment period?(Self-Management of Type 2 Diabetes Comprehensive Nursing Essay Example)
The purpose of the paper was to identify a research gap in the practice site and appropriate interventions to address it. The problem identified affects the endocrinology unit that specializes in treating people with diabetes. The unit presents a lack of clinical guidelines in the implementation of diabetes self-management education initiatives like mhealth mobile applications or face-to-face and telephone-based family-oriented education. Effective communication competencies help support patient education because it is essential to deliver information quickly and accurately to bolster patient understanding. Effective communication also allows DNP-prepared nurses to collaborate with other staff members and understand the patients’ concerns to address them appropriately for better patient outcomes(Self-Management of Type 2 Diabetes Comprehensive Nursing Essay Example)

Boels, A. M., Vos, R. C., Dijkhorst-Oei, L. T., & Rutten, G. E. (2019). Effectiveness of diabetes self-management education and support via a smartphone application in insulin-treated patients with type 2 diabetes: Results of a randomized controlled trial (TRIGGER study). BMJ Open Diabetes Research and Care, 7(1), e000981(Self-Management of Type 2 Diabetes Comprehensive Nursing Essay Example)
Hemmati Maslakpak, M., Razmara, S., & Niazkhani, Z. (2017). Effects of Face-to-Face and Telephone-Based Family-Oriented Education on Self-Care Behavior and Patient Outcomes in Type 2 Diabetes: A Randomized Controlled Trial. Journal of diabetes research, 2017, 8404328. https://doi.org/10.1155/2017/8404328(Self-Management of Type 2 Diabetes Comprehensive Nursing Essay Example)
https://www.ncbi.nlm.nih.gov/

Working On an Assignment With Similar Concepts Or Instructions?
A Page will cost you $12, however, this varies with your deadline.
We have a team of expert nursing writers ready to help with your nursing assignments. They will save you time, and improve your grades.
Whatever your goals are, expect plagiarism-free works, on-time delivery, and 24/7 support from us.
Here is your 15% off to get started. Simply:
- Place your order ( Place Order )
- Click on Enter Promo Code after adding your instructions
- Insert your code – Get20
All the Best,
Get A 100% Plagiarism-Free Nursing Paper
Related samples.
- Medical Safety Competency Comprehensive Nursing Essay Example
- Descriptive Analytics in Organizations Comprehensive Solved Nursing Essay Example
- Interventions in the Management of Elderly Persons Comprehensive Solved Nursing Essay Example
- Final Care Coordination Plan Comprehensive Solved Nursing Essay Example
- Developmental Assessment and the School-Aged Child Comprehensive Solved Nursing Essay Example
Nursing Topics
- Academic Writing Guides
- Advanced Cardiac Care Nursing
- Advanced Community Health Nursing
- Advanced Critical Care Nursing
- Advanced Health Assessment
- Advanced Mental Health Nursing
- Advanced Nursing Ethics
- Advanced Nursing Informatics
- Advanced Occupational Health Nursing
- Advanced Pathophysiology
- Advanced Pediatric Nursing
- Advanced Pharmacology
- Gerontological Nursing
- Healthcare Policy and Advocacy
- Healthcare Quality Improvement
- Nurse Practitioner
- Nursing Education and Curriculum Development
- Nursing Leadership and Management
- Nursing Research and Evidence-Based Practice
- Nursing Theories
- Nursing Topics and Ideas
- Population Health and Epidemiology
- Assignment Help
- Chamberlain University
- Grand Canyon University (GCU)
- MSN Nursing Papers Examples
- APA NURSING PAPER EXAMPLE
- capstone project
- community health nursing assignments
- comprehensive assessment
- graphic organizer
- Nursing Care Plan
- Nursing Case study
- nursing informatics assignments
- Nursing Leadership Essay
- Shadow Health
- tina jones shadow health
- Windshield Survey Examples
- Nursing Essays
- PICOT Paper Examples
- Walden University
- Women's Health Nursing
Important Links
Knowledge base, utilize our guides & services for flawless nursing papers: custom samples available.
MSNSTUDY.com helps students cope with college assignments and write papers on various topics. We deal with academic writing, creative writing, and non-word assignments.
All the materials from our website should be used with proper references. All the work should be used per the appropriate policies and applicable laws.
Our samples and other types of content are meant for research and reference purposes only. We are strongly against plagiarism and academic dishonesty.
We Accept:

Diabetes Type 2
Diabetes mellitus, normal physiology of the pancreas, case in point.
Diabetes mellitus is a metabolic disorder characterised by persistent high glucose levels in blood. The hyperglycaemia persists due to either failure of insulin production or tissues resistance to insulin (Yorek et al., 2015; Barron, 2010). Insulin is produced by the pancreas. Diabetes mellitus can subdivided into three types; type 1 diabetes mellitus, type 2 diabetes mellitus, and gestational diabetes mellitus (Habtewold, Tsega & Wale, 2016; Yorek et al., 2015; Barron, 2010). This assignment will primarily focus on a patient with type 2 diabetes mellitus.

Type 2 diabetes results from the body failing to effectively utilize the insulin produced by the pancreas. The malfunction is referred is known as insulin resistance. The result is hyperglycaemia that is associated with the presenting symptoms of diabetes (Stoian et al., 2015; Lazo et al., 2014)
The alpha cells comprise about 20% of all the islet’s cells. They secrete the hormone named glucagon which increases blood sugar to maintain normal levels so that glucose can get broken down once sugar levels drop (Waters, 2014; TAO, 2014). The making and release of glucagon in the pancreas is controlled by chemoreceptors through the body that are sensitive to the levels of sugar in the blood. When the blood sugar levels drop too low, the chemoreceptors signal the alpha cells in the pancreas to release the hormone glucagon which is transported via blood to the liver. Glucagon acts on hepatocytes hepatocytes to break down glycogen into the glucose through a process referred to as glycogenesis (Barron, 2010; DeWit, Stromberg & Dallred, 2017).
1. Barron, J., 2010. The Endocrine System: The Pancreas & Diabetes. [Online] Available at: https://jonbarron.org/diabetes-blood-sugar-levels/endocrine-system-pancreas-diabetes. [Accessed 21 October 2016].
2. Chin, Y, Huang, T, & Hsu, BR 2013, ‘Impact of action cues, self-efficacy and perceived barriers on daily foot exam practice in type 2 diabetes mellitus patients with peripheral neuropathy’, Journal of Clinical Nursing, vol. 22, no. 1/2, pp. 61-68. Available from: 10.1111/j.1365-2702.2012.04291.x. [8 February 2017].
3. DeWit, S. C., Stromberg, H., & Dallred, C. (2017). Medical-surgical nursing: Concepts & practice.
4. Habtewold, TD, Tsega, WD, & Wale, BY 2016, ‘Diabetes Mellitus in Outpatients in Debre Berhan Referral Hospital, Ethiopia’, Disease Markers, pp. 1-6. Available from: 10.1155/2016/3571368. [8 February 2017].
5. HINKLE, J. L., & CHEEVER, K. H. (2014). Brunner & Suddarth’s textbook of medical-surgical nursing.
6. Lazo, MA, Bernabé-Ortiz, A, Pinto, ME, Ticse, R, Malaga, G, Sacksteder, K, Miranda, JJ, & Gilman, RH 2014, ‘Diabetic Peripheral Neuropathy in Ambulatory Patients with Type 2 Diabetes in a General Hospital in a Middle Income Country: A Cross-Sectional Study’, PLoS ONE, vol. 9, no. 5, pp. 1-5. Available from: 10.1371/journal.pone.0095403. [7 February 2017].
7. Li, G, Sun, C, Wang, Y, Liu, Y, Gang, X, Gao, Y, Li, F, Xiao, X, & Wang, G 2014, ‘A Clinical and Neuropathological Study of Chinese Patients with Diabetic Peripheral Neuropathy’, PLoS ONE, vol. 9, no. 3, pp. 1-5. Available from: 10.1371/journal.pone.0091772. [8 February 2017].
8. Park, H, Park, C, Quinn, L, & Fritschi, C 2015, ‘Glucose control and fatigue in type 2 diabetes: the mediating roles of diabetes symptoms and distress’, Journal of Advanced Nursing, vol. 71, no. 7, pp. 1650-1660. Available from: 10.1111/jan.12632. [8 February 2017].
9. Stoian, A, Bănescu, C, Bălaşa, RI, Moţăţăianu, A, Stoian, M, Moldovan, VG, Voidăzan, S, & Dobreanu, M 2015, ‘Influence of GSTM1, GSTT1, and GSTP1 Polymorphisms on Type 2 Diabetes Mellitus and Diabetic Sensorimotor Peripheral Neuropathy Risk’, Disease Markers, vol. 2015, pp. 1-10. Available from: 10.1155/2015/638693. [6 February 2017].
10. Syngle, A, Verma, I, Krishan, P, Garg, N, & Syngle, V 2014, ‘Minocycline improves peripheral and autonomic neuropathy in type 2 diabetes: MIND study’, Neurological Sciences, vol. 35, no. 7, pp. 1067-1073. Available from: 10.1007/s10072-014-1647-2. [7 February 2017].
11. TAO, Y.-X. (2014). Glucose homeostatis and the pathogenesis of diabetes mellitus.
12. Won, JC, Kwon, HS, Kim, CH, Lee, JH, Park, TS, Ko, KS, & Cha, BY 2012, ‘Prevalence and clinical characteristics of diabetic peripheral neuropathy in hospital patients with Type 2 diabetes in Korea’, Diabetic Medicine: A Journal Of The British Diabetic Association, vol. 29, no. 9, pp. e290-e296. Available from: 10.1111/j.1464-5491.2012.03697.x. [8 February 2017].
13. Yorek, MS, Obrosov, A, Shevalye, H, Holmes, A, Harper, MM, Kardon, RH, & Yorek, MA 2015, ‘Effect of diet-induced obesity or type 1 or type 2 diabetes on corneal nerves and peripheral neuropathy in C57Bl/ 6J mice’, Journal of the Peripheral Nervous System, vol. 20, no. 1, pp. 24-31. Available from: 10.1111/jns.12111. [6 February 2017].
- Alzheimer Disease
- Anger Management

Type 2 Diabetes: Nursing Change Project Essay
Problem statement, purpose of the change proposal, literature search strategy employed, evaluation of the literature, applicable nursing theory utilized, proposed implementation plan, potential barriers and answers.
Type 2 diabetes is a dangerous but treatable disease that manifests as high blood sugar, low insulin, and general insulin resistance. It results from living habits rather than any form of a pathogen, and people can develop it spontaneously as long as they are in a risk group. It generally does not require hospitalization unless the issue is severe, and most patients continue their daily lives. However, its symptoms are not immediately apparent to an untrained observer and can come on slowly, preventing the person from noticing. People can be trained in noticing and measuring their symptoms, but they remain fallible and can fail to see a potential cause for alarm. As such, medical workers are trying to develop more reliable and efficient methods of monitoring patients with the condition.
Most patients with diabetes live their lives with some specific accommodations that manage the condition, such as lifestyle and diet changes alongside specific medications. However, their symptoms require monitoring, and professionals are preferable to the patients for the purpose. Currently, this matter is being resolved through regular clinic visits, with specialists receiving the patients and assessing their condition. However, the procedure takes considerable time and effort on the part of both medical workers and patients. The former have to take time away from their other patients, and the latter have to travel to the clinic and wait to be assessed. With the recent advancements in technology, such an inefficient approach may be outdated and require a replacement.
Telemedicine is emerging as an alternative approach to the monitoring of remote patients whose issues do not warrant hospitalization. It can take a variety of forms, from regular videoconferences that confirm the patient’s condition to specialized medical tools that link with a smartphone app and submit data to the hospital automatically. Its primary advantage is that the patient no longer needs to come to the clinic physically, which is particularly relevant for seniors. The patients can also be more independent, with the medical workers supporting their judgment with their expertise. Telemedicine has already been successfully applied to various aspects of type 2 diabetes management. As such, it may be prudent to adopt it as a standard and outfit care institutions with telemedicine facilities to improve outcomes.
Geriatric patients who have type 2 diabetes are the population for this proposal. The use of telemedicine to monitor symptoms is the intervention, and it is compared to the standard practice of regular clinic visits. The expected outcome is a decrease in the concomitant effects of the condition as a result of continuous monitoring. The time is 12 months, which should be sufficient to see a significant change without taking overly long. With these aspects outlined, it is possible to create the following PICOT question:
In geriatric patients who have type 2 diabetes (P), will the implementation of telemedicine to communicate cares and concerns and conduct continuous symptom monitoring (I) instead of traditional regular clinic visits (C) reveal a reduction in the concomitant effects of the condition (O) over a 12-month period (T)?
The author searched several platforms that host peer-reviewed scholarly nursing literature: Google Scholar, JSTOR, and NCBI PubMed. The process focused on the keywords ‘type 2 diabetes,’ ‘symptoms,’ and ‘telemedicine.’ Only articles that had been published in the last five years were eligible due to the requirement for relevance. Overall, the search yielded approximately 3,000 articles, not all of which applied to the purpose of this proposal. Some were rejected because they did not discuss the relevant topic but mentioned it. Most were omitted due to time concerns, as this proposal only needed several supporting works and was not intended as a literature review. Ultimately, three articles that discuss the advantages of telemedicine and its applicability to various symptom categories passed the inspection.
The three articles selected for this paper discuss various aspects of telemedicine and their relevance to the ultimate choice of one approach or the other. Rasmussen, Lauszus, Lokke, and Jensen (2017) claim that the new method is more cost-effective than clinic visits and yields better results, particularly with regards to blood glucose. Fox, Kronenberg, and Weiskopf (2019) highlight the relationship between diabetes and preventable blindness and propose a telemedicine strategy to screen patients for the issue. Finally, Huang, Tao, Meng, and Jing (2015) show a significant improvement in patient glycemic control as a result of telemedicine usage. Overall, the literature appears to promote the view that the new method can improve the quality of current diabetes care and create opportunities for new treatments that enhance patient quality of life further.
Martha E. Rogers’s Theory of Unitary Human Beings is the most applicable for this proposal, as it discusses both scientific progress and the application of the findings in ways that help patients. Past findings have demonstrated that telemedicine is appropriate to nursing as a whole, helping medical workers manage various conditions. Now, nurses should use the art of nursing to find creative applications of the approach that help diabetes patients improve their well-being. As the literature review demonstrates, it is possible to use telemedicine to address various aspects of the condition and prevent side complications. Medical workers should work on ways to further enhance health by using the new tool at their disposal for various purposes and choosing the best ideas for implementation.
The implementation will consist of three separate parts: planning, purchase and installation, and training. First, the nursing staff will determine the specific devices and software they will use for telemedicine and outline the requirements. Second, the facility will purchase the necessary equipment, construct a telemedicine room, and configure it so that it becomes operable. Third, the staff will be trained in the operation of the telemedicine equipment and in teaching seniors how to use the tools to communicate. The three steps will have to happen successively because a plan is necessary before purchase and because the room will be required for practical staff training.
Some seniors may not be able to afford the equipment required for successful telemedicine usage. The nursing staff should find inexpensive devices that have the required functions and are easy to use. They can then suggest these options to the people in question as cheaper alternatives that still have the benefits. Additionally, seniors may not be receptive to the new technology and its usage, especially if the method chosen requires their active participation. They will require extensive explanations and reminders before they get used to the regular communication or other monitoring methods used.
Fox, C. R., Kronenberg, K., & Weiskopf, E. S. (2019). Using telemedicine to increasing eye care screening & referral for people with diabetes. Journal of Public Health Issues and Practices , 3 . Web.
Huang, Z., Tao, H., Meng, Q., & Jing, L. (2015). Effects of telecare intervention on glycemic control in type 2 diabetes: A systematic review and meta-analysis of randomized controlled trials. European Journal of Endocrinology , 172 (3), R93-R101.
Rasmussen, O. W., Lauszus, F. F., Lokke, M., & Jensen, M. S. (2017). Telemedicine is cost effective compared with standard care in type 2 diabetes mellitus – A randomized trial with an economic analysis in an outpatient clinic. Biotechnology Health Science , 4 (2). Web.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, February 28). Type 2 Diabetes: Nursing Change Project. https://ivypanda.com/essays/type-2-diabetes-nursing-change-project/
"Type 2 Diabetes: Nursing Change Project." IvyPanda , 28 Feb. 2024, ivypanda.com/essays/type-2-diabetes-nursing-change-project/.
IvyPanda . (2024) 'Type 2 Diabetes: Nursing Change Project'. 28 February.
IvyPanda . 2024. "Type 2 Diabetes: Nursing Change Project." February 28, 2024. https://ivypanda.com/essays/type-2-diabetes-nursing-change-project/.
1. IvyPanda . "Type 2 Diabetes: Nursing Change Project." February 28, 2024. https://ivypanda.com/essays/type-2-diabetes-nursing-change-project/.
Bibliography
IvyPanda . "Type 2 Diabetes: Nursing Change Project." February 28, 2024. https://ivypanda.com/essays/type-2-diabetes-nursing-change-project/.
- Telemedicine as an Effective Tool of the Health Care
- Telemedicine as a Form of Healthcare Delivery
- Trend in Canada: Care at a Distance (Telemedicine)
- Legal State of Telemedicine
- Telemedicine: Development, Opportunities and Obstacles
- Anchor Hospital's Telemedicine Services
- Implementing Telemedicine Solutions: Grand Hospital
- Implementing Telemedicine Technology
- Telemedicine for Chronic Diseases: PICOT (Research) Question
- Dermatology and Telemedicine in Dubai
- Type 2 Diabetes in Geriatric Patients
- Cultural Empowerment. Diabetes in Afro-Americans
- Hypothyroidism Diagnosis and Treatment Plan
- Thalassemia: Pharmacotherapy for Hematologic Disorders
- Diagnosis and Classification of Diabetes Mellitus
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.26(8); 2021 Dec

A nurse-led conceptual model to inform patient-centred, type 2 diabetes mellitus management in public clinical settings
Globally, there is an increased need to provide patient-centred care for people diagnosed with type 2 diabetes mellitus. In Nigeria, a poorly financed health system has worsened the difficulties associated with managing type 2 diabetes mellitus in clinical settings, causing a detrimental effect on patient-centred care.
We aimed to develop a conceptual model to promote patient-centred type 2 diabetes mellitus care in clinical settings. We explored nurses’ contextual perceptions of clinical practices and operations in light of type 2 diabetes mellitus management across public hospitals in Lagos, Nigeria. Identifying a nurse-led intervention is critical to care optimisation for people diagnosed with type 2 diabetes mellitus.
We adopted a qualitative approach. Using the constant comparison method and semi-structured questions and interviewed practice nurses, with over one year’s experience and who were working in public hospitals across Lagos, Nigeria. The framework method was used to analyse the data obtained.
Nurses provided insight into four areas of patient-centred type 2 diabetes mellitus management in clinical settings: empowering collaboration; empowering flexibility; empowering approach; and empowering practice. Nurses discussed an empowering pathway through which health settings could provide patient-centred care to individuals diagnosed with type 2 diabetes mellitus. The pathway entailed the integration of macro, meso and micro levels for patient management. Nurses’ accounts have informed the development of a conceptual model for the optimisation of patient care.
Conclusions
The model developed from this research sits within the patient-centred care model of healthcare delivery. The research sits within the patient-centred care model of healthcare delivery. inform patient-centred care, not only in countries with poorly financed healthcare systems, but in developed countries with comparatively better healthcare.
Introduction
The prevalence of diabetes mellitus (DM) is increasing across the world and, notably, in low and middle-income countries (LMICs). Type 2 diabetes mellitus (T2DM) is the most prevalent type of DM in Nigeria ( International Diabetes Federation, 2015 ), accounting for 95% of DM cases reported in Nigerian hospitals ( Chinenye et al., 2012 ). However, 70–80% of individuals remain undiagnosed in the community ( International Diabetes Federation, 2014 ). Almost 60% of those diagnosed with T2DM had an early onset of complications such as hypertension ( Anakwue et al., 2013 ; Fasanmade et al., 2013 ) and 90% developed dyslipidaemia ( Chinenye et al., 2012 ). A substantial proportion of patients with T2DM in Nigeria had below intermediate level quality of life, and were physically inactive (Adeniyi et al., 2015). The reported burdens occurred because approximately 70% of Nigerians live in poverty ( National Bureau of Statistics, 2015 ) and there are organisational factors such as poor knowledge and information management that can adversely impact patient care ( Bosun-Arije et al., 2020 ).
The burdens associated with T2DM management in Nigeria are driven by a combination of complex factors such as poverty, lack of health-related knowledge and a fragile healthcare system ( National Bureau of Statistics, 2015 ). For instance, in 2017, only 3.76% of the Nigerian national budget was allocated to the health sector compared to countries such as Sierra Leone (13.42%), South Africa (8.11%) and Malawi (9.65%) ( World Bank, 2017 ).
A systematic review by Bosun-Arije et al. (2019) found six factors influencing T2DM management in Nigerian public hospitals: non-adherence/non-compliance, biosocial, self-care, psychological, as well as cost and drug-related. These factors are detrimental to patient-centredness and optimisation of patient care ( Iwuala et al., 2015 ). Patient-centred care improves patient self-management skills and heightened patient quality of life. Challenges of T2DM management include prolonged hospital stays, high medical costs, microvascular and macrovascular complications ( Arogundade, 2013 ; Olamoyegun et al., 2015 ; Onakpoya et al., 2010 ) and a high mortality rate ( Chijioke et al., 2010 ). These burdens threaten patient-centred care and reduce the optimisation of patient empowerment. Structured recommendations are required to promote patient-centred care. This research aimed to develop a conceptual model to improve patient-centred T2DM management in clinical settings. A model is needed alongside robust approaches and context-driven research to aid surveillance, prevention, early diagnosis and patient-focused T2DM management (World Health Organization, 2016).
This study sits with pragmatism. We adopted the constant comparison as a method ( Charmaz, 2008 ) and not as a methodology as propounded by grounded theory ( Glaser and Strauss, 1967 ). The grounded theory method was combined with the framework method ( Ritchie and Spencer, 2002 ), which we adopted to gather rich and robust data through an iterative process, while the latter facilitated a transparent and systematic data analysis as advised by Merriam (2009) . Interviews commenced after obtaining ethical approval from the university of the last author, and the Lagos State Ministry of Health Ethics Committee (LREC /06/10/682). All participants received a participant information sheet and gave informed consent before participation.
We used a sampling frame that encompassed a list of all the public secondary and tertiary health facilities in Lagos State. Furthermore, we adopted two types of purposive sampling ( Holloway and Galvin, 2016 ). First, we used the maximum variation sampling method when selecting the hospitals. We ensured that we chose at least one hospital from each of the five administrative regions within Lagos State. Second, using expert and typical case sampling methods, we approached participants who had met the inclusion criteria as being qualified for 1–30 years with various work experience, nursing qualifications and educational levels.
Characteristics of the study population and research participants
We selected six hospitals from different urban, suburban and rural regions across Lagos State. We anonymised them as AO1, BO1, CO1, DO1, EO1 and FO1 for confidentiality. Participants were given an alphanumeric label of P1–P8. The label represents the eight grades of the nurses interviewed: nursing officer one (N01), nursing officer two (NO2), sister, principal nursing officer (PNO), matron, assistant chief nursing officers (ACNOs), chief nursing officer (CNO) and apex. In this study, we interviewed nurses of different grades.
N01 and N02 are nurses who have practised for between one year and 10 years. Five nurses from this group participated. PNOs or matrons are more senior nurses. Four nurses from this group were interviewed. One of them had a bachelor’s degree qualification in nursing, and three had a diploma in nursing. Three ACNOs participated; one with BSc and master’s degrees, one with a BSc and one with a nursing diploma; one CNO with BSc and master’s degrees. Finally, we interviewed two apex nurses who are degree holders. Apex oversees the overall leadership and management of other nurses. In total, 17 nurses participated, with modal working experience of 18 years and median work experience of 15 years.
Data collection
We collected data using face-to-face, in-depth semi-structured interviews. A pre-test interview guide was adopted. All participants had several years of work experience and nursing qualifications and were involved in both operational and strategic levels of patient management in public hospitals across Lagos, Nigeria. We engaged with participants to elicit their views for an in-depth understanding of factors to optimise patient-centred T2DM management. We posed three research questions.
- What factors threaten patient-centred T2DM management in clinical settings?
- How do patients with T2DM react to these factors?
- What approaches can inform person-centred T2DM management at a low or no cost?
Each interview was audiotaped, lasted between 45 and 60 minutes and was transcribed verbatim. Throughout the data collection phase, constant comparison ensured the collection of robust data from the nurses through an iterative process. During this process, emerging information from all participants was logically integrated into the interview questions for a deeper exploration of the emerging themes (please see Figure 1 for an NVivo extract). We also adhered to data sufficiency as recommended by Bryman (2012) to ensure that adequate data were obtained to address the research aim. Data collection concluded at the point at which no new information, relevant to the research, was emerging from the participants.

‘Community mobilisation’ as used in context (NVivo extract).
Data analysis
As the study aimed to develop a conceptual model to promote patient-centred T2DM care in clinical settings, we utilised the framework approach ( Ritchie and Spencer, 2002 ) for a transparent and systematic analysis. During the five phases of data analysis: familiarisation; identifying a thematic framework; indexing; charting; and mapping and interpretation, we adopted both manual and NVivo analysis techniques, as recommended by Gale et al. (2013) . Themes emerged from the data through a logical, rigorous, formal review and iteration of the data ( Ritchie et al., 2013 ).
We interviewed a total of 17 practice nurses in six public hospitals across urban, suburban and rural regions of Lagos, Nigeria. Participant responses were analysed and are presented according to the three research questions we posed.
Question one: What factors threaten patient-centred T2DM management in clinical settings?
We asked participants to discuss the factors that they felt threatened patient-centred T2DM management in the clinical settings in which they were working. We elicited from them elements which we interpreted to be unrealistic collaboration, rigid flexibility, uncomfortable approach and unsteady practice. Participants reported that the factors resulted when the organisational policies and decisions did not anchor on holistic patient-centredness.
Unrealistic collaboration
Nurses recounted that not all collaborations between health providers and volunteers, the government and international bodies, patients and traditional leaders, as well as hospitals and media, focused on patient-centred T2DM care. For instance
Some patients are being misled by their pastors or traditional leaders. There was a man that came in he was having a wound on his leg, so they said somebody came in and said that it was the witches and wizards, so he went to a pastor, and the pastor asked him to be burning something and be putting it on the wound for it to heal. P1 (N02)
A collaborative, patient-centred approach is empowering for patients to self-manage their T2DM. A patient-centred collaboration in healthcare is that which supports meaningful partnerships and collaboration with volunteers, international bodies, patients, traditional leaders and media agencies.
Rigid flexibility
Some clinical policies and decisions that aimed at flexible practices were reported by nurses as vague and rigid to achieve in real-world settings. For example, when patients are told to come to clinics for free blood glucose tests and no flexible payment arrangement is in place for them to buy their prescribed medications.
If they (the patients) cannot afford the drugs, we discuss among ourselves and refer the case to the social worker who will take over, but then most hospitals in Nigeria demand upfront payment before treatment meaning there is no flexible billing method. P3 (sister)
When a patient experienced this form of ‘rigid flexibility’, they refused professionals’ advice. The nurses felt that for a policy or decision to be considered flexible, it should be empowering and equity focused. Therefore, the participants suggested that a database needs to be instituted to record and evaluateT2DM cases treated across public hospitals in Nigeria. Participants also discussed the need for a connection between patients, the government, community members and professional bodies to make clinical approaches patient-focused and patient-driven to boost patient compliance.
The patients will then not listen to the health professionals; most of them just run away from the hospital and will come back with a diabetic foot. P4 (PN0) I will just like to say that on the aspect of dietary [advice],… patient[s] do not really comply. Maybe because they are being forced by either their family members or health professionals to avoid some food. P1 (N02)
Uncomfortable approach
The participants expressed their concerns for uncomfortable operational approaches that existed in clinical practice in terms of the scare tactics and educational approaches adopted when counselling patients. An example of an uncomfortable approach is when a health professional uses health education approaches that increase patients’ fears.
By the time most of them are told the story of DM complications, they are always afraid but eager to learn. P1 (N02)
Participants explained that some health professionals found it challenging to communicate effectively, especially with uneducated patients. For instance, advising them to taste their urine for sweetness can be very disturbing for the patients.
Then you will also tell those stack illiterates, when you urinate, try to taste it, it must not taste like you are taking sugar. P4 (PN0)
The patient often felt uncomfortable with some of the strategies used by some health professionals. Some strategies adopted during health education of patients often worsened patients’ fears and worries about their condition.
and some health professional over-scrutinise the patients and screen them about what to eat or take. P3 (sister)
Inconsistent practice
The unsteady practice emerged from the words the participants used to describe inconsistent practices experienced by patients, especially during DM clinic days. Unsteady practices occur at a strategic level. As recounted by the participants, when many patients turned up for clinic appointments, they struggled to have a seat and had no easy access to the essential facility such as functional toilets and toilet access for disabled patients.
We see up to 400 patients in a day, times, 300, 250 on their clinic day and the clinic is not originally structured to accommodate many people. P7 (CNO)
Also, there were reported workforce and diabetes specialist shortages, and these had led to patients spending up to 6 hours waiting when they attended their clinical appointments. There were no consistent monitoring strategies or guidelines to guide practice around how patients were fed and monitored on the wards.
There are no diabetes specialist nurses in the department, and there is a shortage of manpower. P6 (ACNO) We provide food for the patient when on admission. But well at the same time, you know? People still bring in food. For patients in the hospital, for showing that they care and things like that and they sneak in things. I will just like to say that on the aspect of dietary [advice], patients do not really comply. Maybe because they don’t really understand or maybe people, I don’t know, because patients still eat apart from the food given them. P7 (CNO)
Question two: How do patients with T2DM react to these factors?
When participants were asked about patients’ reactions to the above-discussed factors, various burdens were expressed. The burdens described by the participants are linked with the rigid flexibility that results when a patient is advised to come to the hospital for testing and had no money or insurance to pay for their hypoglycaemic medications, as well as the unrealistic collaboration that exists. For instance, between the patients and their religious leaders in the rural areas, usually, some pastors who told individuals that DM was caused by witches or wizards.
The patients become so scared. P6 (ACNO) Most of the patients believe that the witches and wizard cause it. P2 (N01) Yes, out-of-pocket affect the patients because for the patients to come to you, so you have to relieve them of the financial burden so that they will be able to cooperate and when you tell them to come, they will come. DM drugs are expensive so that it will affect the health situation of Nigeria, yes it will. P8 (apex)
Question three: What approaches can inform person-centred T2DM management at a low or no cost?
The participants considered T2DM management strategies that focused on low or no cost as patient-empowering and person-centred. In this section, we discuss the approaches highlighted by participants. Participants’ views are presented under four themes: empowering collaboration; empowering flexibility; empowering approach; and empowering practice.
Empowering collaboration
Nurses recounted that collaboration and partnership need to be driven by patient-centred intentions and not financial gains. The participants narrated that patients felt that collaboration and partnership should be tailored towards patients and their convalescence. However, effective media and platforms must be used to make collaboration empowering for the patients.
Use public address system be it through radio, through every form of… of which you can give the patients information. P5 (matron) You know some of these elites; they have in-depth knowledge of the disease conditions, so we can also involve them to educate the patients. P5 (matron)
The participants reported that only empowering collaboration could provide effective platforms for patients to become more knowledgeable about their DM and self-care to thrive. Such platforms would depend on timely, transparent and accurate cooperation among all key stakeholders. The government, non-governmental organisations (NGOs), patients’ relatives, health professionals, professional organisations, research organisations, religious and community leaders should be educated to educate patients when necessary. Please see Figure 2- A conceptual model for patient-centred type 2 diabetes mellitus management in Nigeria.
The first thing to do is mobilisation, and when I am talking about mobilisation, I am not just talking about ordinary mobilisation, I am talking about community mobilisation. P8 (apex) Open in a separate window Figure 2. A conceptual model for patient-centred type 2 diabetes mellitus management in Nigeria. community enlightenment through outreach programmes. P8 (apex)
Empowering flexibility
The participants acknowledged that flexibility is crucial to patient-centred care, but more importantly pointed out the benefit of empowering flexibility in health service delivery to patients with T2DM. Nurses stressed the empowering benefits of flexible clinic appointments, flexible follow-up care and flexible communication to patient-centredness. Also, nurses felt that flexible health financing would support patient-centredness in care in clinical settings. The link between health financing and health service delivery for patients diagnosed with T2DM was illuminated. The purpose of flexible health financing is to make funding available, as well as set financial incentives for the hospitals, such that individuals diagnosed with T2DM can flexibly access healthcare services and flexibly pay for their hypoglycaemic medicines.
support patients who are poor to have free treatment or flexible payment P8 (apex) funding to make special pharmacy arrangement possible P1 (NO2)
Empowering approach and practice
The participants discussed the need to review clinical approaches to T2DM management in clinical settings frequently. Health professionals should uptake counselling approaches that can uphold patient empowerment, alleviate patients’ fears, correct their misconceptions about the causes of T2DM and heighten patients’ ability to self-manage their condition with less dependency.
most of them believe that DM is caused by the witches and wizard, so I have to tell them that their lifestyles matter. P6 (ACNO)
The nurses we interviewed gave insights on how DM education needs to be objective, evidence-based, informative and be provided concerning patients’ and their relatives’ decisions. Nurses suggested that all health stakeholders should, ‘say it as it is’ and ‘just do it right’. This suggests that health professionals should be honest and open when educating the patients about DM and to talk less and listen more to patients, reduce waiting time in clinics, provide more resources and training for staff, and ensure that DM specialists are available and accessible.
counsel them again one on one, so privacy and confidentiality are very important and so that one we will be able to gain their confident. P2 (N01) Give patients flyers and leaflets to educate them. P3 (sister) Tell patients the truth about their condition. P8 (apex) even when the patients are in the hospital, we allow their relations, and we encourage the care of their relations. We tell their relations to also assist in caring for them. P6 (ACNO)
As explained by the research participants, listening to patients’ views is essential in clinical practice. However, while clinicians must listen more than they talk to patients, nurses stated that sometimes it might be vital to be firm with patients, especially when educating them on diet modification as a way of promoting their compliance. As well as encouraging patient networking for guidance and advice on lifestyle modification, nurses felt that patients who struggled to modify their diets benefitted from a ‘firm’ approach. However, while being firm, the participants suggested the use of jokes could improve effective communication and inform the development of a nurse–patient therapeutic relationship.
Crack jokes; get them in the mood and be specific and be precise not boring then let them participate so they will never be bored. P7 (CNO) The hospital is trying. Here they have a club to promote patient networking. P5 (matron) that is when caring for the patients with type 2 diabetes? OK, when you do one on one discussion with them, they try to be nice you explain in the language that they will understand what you are saying so if he is a Yoruba person, you speak Yoruba to them. P3 (sister)
A conceptual model developed from the Nigerian context for patient-centred T2DM management
A conceptual model was logically developed from the data obtained from the nurses. We developed a model from the themes that emerged from the analysis of the interviews. The nurses who participated in this research objected to the idea that a standalone, macro-level factor could promote patient-centred T2DM care in clinical settings. Instead, the participants acknowledged core integration at macro, meso and micro levels was a critical element to patient-focused T2DM management.
At the macro-level (see Figure 2 ), the federal government should provide funds to subsidise hypoglycaemic medications for patients who require them. Furthermore, participants felt that lawmakers should formulate legislation and policies to advocate for patients and coordinate the delivery of valued and quality care to patients. The legislation and policies should be clear, concise and easily accessible and understandable for the people living with T2DM. At macro level, the Federal Ministry of Health should collaborate with frontline clinical staff and seek patients’ inputs regularly in order to formulate new policies and review existing policies for efficiency in light of how clinical practice and approaches can be flexible and empowering for the patients.
Through integration, the macro-level activities should link with the meso: for instance, the hospital board, research institutes and professional bodies to gain empowering collaboration, clinical approach, clinical practice and flexibility to patient care. As nurses in Nigeria recognise, this form of integration is crucial to abolishing unrealistic collaboration, unsteady practice, uncomfortable approaches and rigid flexibility which are detrimental to patient-centred T2DM management. The model shows that a structured and extended network among the government, community, professional bodies, research institutes, members of the public, religious leaders as well as patients and their relations are required to enable coordination and provision of patient-centred care to individuals diagnosed with T2DM. The community sits at the micro level of the model. It encompasses international stakeholders, NGOs, religious leaders, National Insurance Health Scheme providers, community leaders, food and drink companies and advocates, while the media, schools, family members, churches and mosques sit at the core centre of the micro level.
At the micro level, the nurses recognised the usefulness of community mobilisation by giving DM flyers to the people for community enlightenment and effective communication. Having DM specialists within the community to promote patient networking, social welfare, early identification of DM complications as well as providing free tests are models found productive in light of the promotion of patient-centred care to individuals living with T2DM. In addition, subsidised health services, outreach programmes, sharing experiences, timely regimen and group clinic education to patients were recounted as useful strategies to ameliorate patient health and DM outcomes.
To achieve a successful outcome in patient management, health providers who are involved in patient education should focus on health-promoting actions that will encourage patients to achieve realistic DM goals and DM outcomes ( Corser et al., 2007 ; Utz et al., 2008 ). Partnership and collaboration are key elements of a successful strategy ( International Diabetes Federation, 2017 ). Patients can collaborate to share their self-management experiences and discuss their regime and any associated challenges with their family members and friends. By doing this, the patients will be able to receive support from their loved ones. In the same way, health sectors and government can partner and collaborate at national and international levels to improve the effectiveness of T2DM management (World Health Organization, 2016).
Finally, it is paramount that integration is considered as a landmark, collaborative and empowering pathway for the optimisation of patient-centred T2DM management. The macro, meso and micro levels should make a collective alliance to heightening DM care and support to the individuals living with T2DM.
This research sought nurses’ contextual perceptions of clinical practices and operations in light of T2DM management across public hospitals in Lagos, Nigeria, for the development of a conceptual model to optimise patient-centred T2DM care in clinical settings.
Collaboration
The findings of this research support that collaboration is a typical element promoting T2DM management in the clinical setting. Factors such as blame, bureaucracy and mistrust can jeopardise collaboration ( McSherry, 2010 ). The outcome of our research adds that it takes empowering collaboration to heighten patient-centred T2DM management for optimal health outcomes of patients.
Patient-centred care in DM management can be achieved through collaboration ( Inzucchi et al., 2012 ). Katon et al. (2010) found that patient-centred collaboration promoted patient satisfaction for people with diabetes and improved their quality of life. Collaboration curbed depression among low-income individuals with diabetes ( Ell et al., 2010 ). Trief et al. (2011) found that timely telephone intervention promoted collaboration for the patient with T2DM and their partners. Similarly, Lyles et al. (2011) found that mobile phones are useful tools for a web-based collaborative care programme for T2DM. Lyles et al. (2011) showed that benchmarking is a product of a collaboration that has led to improved quality of care in T2DM. At the same time, when patients interact with each other to learn lifestyle-modifying strategies through collaboration, it had a significant impact on improving the glycaemic levels among patients with T2DM ( Hermans et al., 2013 ; Parkinson et al., 2016 ).
The findings of Qi et al. (2015) aligned with what the participants of this research considered as patient networking, a vital component of collaboration for patient-centred care. Several approaches can support patient-centred partnership; however, there is a factor that sums it all up – having a culturally sensitive healthcare delivery system. When healthcare delivery is designed to be culturally appropriate, there is a significant improvement in self-reported diabetes to community health ( Spencer et al., 2011 ). The outcome of our research affirms that integrated care is a suitable approach to promote patient-centred T2DM management as supported by Nuño et al. (2012). Zhang et al. (2015) concur the outcome of our research by demonstrating that patients with diabetes, receiving an integrated model of care, had a reduction in the number of hospitalisations. The findings of the current research align with critical areas of care organisation for patients with T2DM as recommended by the International Diabetes Federation (2017) .
Clinical practice
As highlighted in these research findings, clinical practices that target successful diabetes self-management education (DSME) are essential to promoting patient-centred T2DM management. However, the outcome of our research suggests that empowering clinical practice can optimise DSME. DSME is an innovative approach that helps patients to be independent and self-involved in their care, thus improving patient outcomes. It is crucial to communicate firmly and cautiously with patients because while being firm, poor communication due to linguistic challenges may result in undue tension between clinicians and patients ( Martin, 2014 ).
To improve practice, Ismail-Beigi (2012) supports that clinical decisions should consider cost, side effects of medicines and long-term safety and effects of therapeutic agents on patient management. As suggested in this study, health professionals should address issues relating to patient management in a timely fashion. Timely communication is crucial to reducing treatment delays among physicians ( Christie and Channon, 2014 ; Strain et al., 2014 ). In our research, the nurses added that patients should be allowed to talk more while the clinician interviewing should listen more and talk less, bearing in mind patient-centredness. Clinicians need to choose their words and language carefully ( Sogg et al., 2018 ).
Flexible approach and practice
The research outcome made clear that operational approaches and strategic practices to patient care need to be flexible in many ways which include having adequate staff to care for patients, flexible payment options and flexible counselling strategies. Nigeria has one of the highest out-of-pocket payment plans in the world. About 70% of patients pay for their health directly, and 30% pay for their health through tax-based revenue, donor funding, social health insurance, community-based health insurance and private health insurance ( Uzochukwu et al., 2015 ). The World Health Organization (2016) reiterates health financing as a critical determinant for achieving universal health coverage.
Most public and private hospitals in Nigeria demand upfront payment before they can treat patients (Aregbesola and Khan, 2018). Around 4% of households spend more than half of their total household expenditure on healthcare, and 12% spend more than a quarter. The consequences of this health financing to the management of a long-term condition such as T2DM are substantial, and it can aggravate the poverty of many patients living with T2DM in Nigeria. As revealed by this research, the hospital billing method for patients needs to be flexible and not rigidly flexible for patients to become more compliant with their regimen. It is also imperative to ensure that flexible dietary advice and a subsidised form of pharmaceutical care are provided for people who require it.
In the United Kingdom (UK), for instance, guidelines for the dietary management of patients with T2DM have been modified to accommodate a more flexible approach to weight loss and individualised approaches to patient management ( Dyson et al., 2011 ). Patients with T2DM are educated on the national recommendations for patients with DM who preferred alcohol ( Dyson et al., 2018 ).
Various clinical approaches for patient-centred T2DM management exist. As suggested by the research results, providing useful DM information to patients is a valuable idea for promoting patient-centred T2DM management. However, to do this efficiently, especially in rural areas, telehealth, a technological approach to health education, will be a great asset. Telehealth has proved useful in promoting patient access to DM health education. Nurses and dietitians successfully conducted a one-year remote DSME to an ethnically diverse, rural and underserved population in rural South Carolina. Patients managed through telehealth and had improved metabolic outcomes and reduced cardiovascular complications (Davies et al., 2010). Web-based behavioural interventions integrated with e-research strategies led to favourable outcomes for patients with T2DM ( Ramadas et al., 2011 ).
A patient empowerment programme (PEP) is effective in improving the clinical outcomes and reducing the general outpatient clinic utilisation rate over 12 months ( Wong et al., 2014 ). Empowering T2DM patients on the self-management of their disease can enhance the quality of diabetes care in primary care on clinical outcomes and health service utilisation rates in patients with T2DM, in the primary care setting. It is essential, therefore, that healthcare professionals continue to advocate collaboration and flexibility, as found in this research; also, promoting patient-centred treatment options for the optimisation of patient outcomes in Nigeria ( Bosun-Arije et al., 2017 ). In addition, it is cogent that PEP desists from unpleasant activities that can potentially jeopardise the PEP objectives.
Limitations
None of the participants was a diabetes nurse specialist, from whom a more theory-driven insight could have emerged. As nurses are key clinicians in healthcare settings, other healthcare professionals such as doctors and laboratory scientists could have contributed to the model. If they were included, their views would have contributed to the robustness of the data that informed the model proposed. Patient perspectives would also have added to the data that informed the model. We plan to address these limitations in future research.
Patient-centredness should be a priority in healthcare. The unique nurse-led model can serve as an asset to improve patient outcomes not only in countries with fragile healthcare systems but also in developed countries with flourishing healthcare services. In the context of clinical structure and culture in health settings, nurses are an indispensable part of the health profession and their experiences should continue to inform person-centred T2DM management. The outcome of this research proposes a conceptual model that can inform cost-effective person-centred T2DM management in clinical settings.
Key points for policy, practice and/or research
- Collaboration, flexibility, clinical approach and clinical practice must anchor on empowerment to uphold patient-centred T2DM management and quality health services in clinical settings.
- Nurses’ insights informed an integrated model for the optimisation of patient-centred T2DM management in clinical settings.
- A nurse-led conceptual model can strengthen collaborative and flexible working for care optimisation of patients with T2DM in clinical practice.
Biographies
Stella Foluke Bosun-Arije is an academic and a researcher with a research interest in non-communicable diseases, specifically the remission and management of type 2 diabetes mellitus.
Candidus Chibuzor Nwakasi is an Assistant Professor in Social Gerontology, and has adopted qualitative and quantitative research approaches to improve the lives of people with dementia and chronic conditions.
Mandu Ekpeyong is a research fellow involved in interventional research for the management of communicable and non-communicable diseases.
Laura Serrant is a Professor of Nursing and Head of The Nursing Department at Manchester Metropolitan. She is interested in optimising health equity, personal agency, diversity and inclusive practice in nursing.
Temitope Esther Sunday-Abel is Assistant Chief Nursing Officer at the Federal Medical Centre, Lagos, Nigeria. She is interested in nursing management and leadership-related research.
Jonathan Ling is Professor of Public Health, with interests in public health and health sciences for the promotion of health and wellbeing. His research expertise includes quantitative and mixed methods designs.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical permission: The author(s) obtained ethical approval from the University of Sunderland, and the Lagos State Ministry of Health Ethics Committee (LREC /06/10/682). All participants received a participant information sheet and gave informed consent before participation.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Stella Foluke Bosun-Arije https://orcid.org/0000-0001-7813-9027
Mandu Ekpenyong https://orcid.org/0000-0003-3778-645X
- Adeniyi AF, Ogwumike OO, Oguntola DAet al. >(2015) Interrelationship among physical activity, quality of life, clinical and sociodemographic characteristics in a sample of Nigerian patients with type 2 diabetes . African Journal of Physiotherapy and Rehabilitation Sciences 7 ( 1–2 ): 12–18. [ Google Scholar ]
- Anakwue R, Arodiwe E, Ofoegbu E. (2013) The prevalence and control of hypertension among patients with type 2 diabetes mellitus in Nigeria . Journal of College of Medicine 17 ( 2 ): 11. [ Google Scholar ]
- Aregbeshola BS, Khan SM. (2018) Out-of-pocket payments, catastrophic health expenditure and poverty among households in Nigeria 2010 . International Journal of Health Policy and Management 7 ( 9 ): 798. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Arogundade FA. (2013) Kidney transplantation in a low-resource setting: Nigeria experience . Kidney International Supplements 3 ( 2 ): 241–245. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bosun-Arije FS, Ling J, Graham Yet al. >(2017) Global insights into the clinical management of type 2 diabetes: a context-specific view from Nigeria on drivers and barriers to clinical nursing management . Diabetic Medicine 34 ( Suppl. 1 ): 177. [ Google Scholar ]
- Bosun-Arije FS, Ling J, Graham Yet al. >(2019) A systematic review of factors influencing type 2 diabetes mellitus management in Nigerian public hospitals . International Journal of Africa Nursing Sciences 11 : 100151. [ Google Scholar ]
- Bosun-Arije FS, Ling J, Graham Y, et al. (2020) Organisational factors influencing non-pharmacological management of type 2 diabetes mellitus (T2DM) in public hospitals across Lagos, Nigeria: A qualitative study of nurses' perspectives. Diabetes research and clinical practice 166: p.108288. [ PubMed ]
- Bryman A. (2012) Sampling in qualitative research . Social Research Methods 4: 415–429. Oxford University Press . [ Google Scholar ]
- Charmaz K (2008) Reconstructing grounded theory. In: The Sage handbook of social research methods , Sage, pp. 461–478.
- Chijioke A, Adamu AM, Makusidi AM. (2010) Mortality patterns among type 2 diabetes mellitus patients in Ilorin, Nigeria . Journal of Endocrinology, Metabolism and Diabetes of South Africa 15 ( 2 ): 79–82. [ Google Scholar ]
- Chinenye S, Uloko AE, Ogbera AOet al. >(2012) Profile of Nigerians with diabetes mellitus – Diabcare Nigeria study group (2008): results of a multicenter study . Indian Journal of Endocrinology and Metabolism 16 ( 4 ): 558. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Christie D, Channon S. (2014) The potential for motivational interviewing to improve outcomes in the management of diabetes and obesity in paediatric and adult populations: a clinical review . Diabetes, Obesity and Metabolism 16 ( 5 ): 381–387. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Corser W, Holmes-Rovner M, Lein Cet al. >(2007) A shared decision-making primary care intervention for type 2 diabetes . The Diabetes Educator 33 ( 4 ): 700–708. [ PubMed ] [ Google Scholar ]
- Davis RM, Hitch AD, Salaam MMet al. >(2010) TeleHealth improves diabetes self-management in an underserved community: diabetes TeleCare . Diabetes Care 33 ( 8 ): 1712–1717. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dyson PA, Kelly T, Deakin Tet al. >(2011) Diabetes UK evidence-based nutrition guidelines for the prevention and management of diabetes . Diabetic Medicine 28 ( 11 ): 1282–1288. [ PubMed ] [ Google Scholar ]
- Dyson PA, Twenefour D, Breen Cet al. >(2018) Diabetes UK evidence-based nutrition guidelines for the prevention and management of diabetes . Diabetic Medicine 35 ( 5 ): 541–547. [ PubMed ] [ Google Scholar ]
- Ell K, Katon W, Xie Bet al. >(2010) Collaborative care management of major depression among low-income, predominantly Hispanic subjects with diabetes: a randomised controlled trial . Diabetes Care 33 ( 4 ): 706–713. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fasanmade OA, Odeniyi IA, Amira COet al. >(2013) Association of body mass index and abdominal adiposity with atherogenic lipid profile in Nigerians with type 2 diabetes and/or hypertension . Nigerian Medical Journal: Journal of the Nigeria Medical Association 54 ( 6 ): 402. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gale NK, Heath G, Cameron Eet al. >(2013) Using the framework method for the analysis of qualitative data in multi-disciplinary health research . BMC Medical Research Methodology 13 ( 1 ): 1–8. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Glaser BG, Strauss AL. (1967) The discovery of grounded theory , London: Weidenfield and Nicolson. [ Google Scholar ]
- Hermans MP, Elisaf M, Michel Get al. >(2013) Benchmarking is associated with improved quality of care in type 2 diabetes: the OPTIMISE randomised, controlled trial . Diabetes Care 36 ( 11 ): 3388–3395. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Holloway I, Galvin K. (2016) Qualitative Research in Nursing and Healthcare , Hoboken: John Wiley and Sons, Inc. [ Google Scholar ]
- International Diabetes Federation (2014) Regional Fact sheet . Available at: www.idf.org (accessed February 2018).
- International Diabetes Federation (2015) Available at: https://www.diabetesatlas.org/upload/resources/previous/files/7/IDF%20Diabetes%20Atlas%207th.pdf (accessed October 11, 2021).
- International Diabetes Federation (2017) Diabetes Atlas, 8th edition, IDF. https://diabetesatlas.org/upload/resources/previous/files/8/IDF_DA_8e-EN-final.pdf (accessed October 11, 2021).
- Inzucchi SE, Bergenstal RM, Buse JBet al. >(2012) Management of hyperglycaemia in type 2 diabetes: a patient-centred approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) . Diabetologia 55(6 1577–1596. [ PubMed ] [ Google Scholar ]
- Ismail-Beigi F. (2012) Glycemic management of type 2 diabetes mellitus . New England Journal of Medicine 366 ( 14 ): 1319–1327. [ PubMed ] [ Google Scholar ]
- Iwuala SO, Olamoyegun MA, Sabir AAet al. >(2015) The relationship between self-monitoring of blood glucose and glycaemic control among patients attending an urban diabetes clinic in Nigeria . Annals of African Medicine 14 ( 4 ): 182. [ PubMed ] [ Google Scholar ]
- Katon WJ, Lin EH, Von Korff Met al. >(2010) Collaborative care for patients with depression and chronic illnesses . New England Journal of Medicine 363 ( 27 ): 2611–2620. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lyles CR, Harris LT, Le Tet al. >(2011) Qualitative evaluation of a mobile phone and web-based collaborative care intervention for patients with type 2 diabetes . Diabetes Technology and Therapeutics 13 ( 5 ): 563–569. [ PubMed ] [ Google Scholar ]
- McSherry R and Warr J (2010) Factors influencing collaborative working. Implementing Excellence In: Your Health Care Organization: Managing, Leading And Collaborating: managing, leading and collaborating , Jul 1:97.
- Martin G. (2014) “Well I don’t know what to say to that”: Exploring tensions between the voices of Medicine and the lifeworld in the management of diabetes: the case of an immigrant patient . European Journal of Applied Linguistics 2 ( 2 ): 204–232. [ Google Scholar ]
- Merriam SB (2009) Qualitative Research: a Guide to Design and Implementation (rev. and exp. ed.). San Francisco,: Jossey-Bass.
- National Bureau of Statistics (2015) Poverty in Nigeria . Available at: https://www.nigerianstat.gov.ng/ (accessed June 2018).
- Nuño R, Coleman K, Bengoa Ret al. >(2012) Integrated care for chronic conditions: the contribution of the ICCC Framework . Health Policy 105 ( 1 ): 55–64. [ PubMed ] [ Google Scholar ]
- Olamoyegun M, Ibraheem W, Iwuala Set al. >(2015) Burden and pattern of microvascular complications in type 2 diabetes in a tertiary health institution in Nigeria . African Health Sciences 15 ( 4 ): 1136–1141. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Onakpoya OH, Adeoye AO, Kolawole BA. (2010) Determinants of previous dilated eye examination among people with type II diabetes in Southwestern Nigeria . European Journal of Internal Medicine 21 ( 3 ): 176–179. [ PubMed ] [ Google Scholar ]
- Parkinson S, Eatough V, Holmes Jet al. >(2016) Framework analysis: a worked example of a study exploring young people’s experiences of depression . Qualitative Research in Psychology 13 ( 2 ): 109–129. [ Google Scholar ]
- Qi L, Liu Q, Qi Xet al. >(2015) Effectiveness of peer support for improving glycaemic control in patients with type 2 diabetes: a meta-analysis of randomised controlled trials . BMC Public Health 15 ( 1 ): 471. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ramadas A, Quek KF, Chan CKYet al. >(2011) Web-based interventions for the management of type 2 diabetes mellitus: a systematic review of recent evidence . International Journal of Medical Informatics 80 : 389–405. [ PubMed ] [ Google Scholar ]
- Ritchie J and Spencer L (2002) Qualitative data analysis for applied policy research . In: Analyzing qualitative data (pp. 187-208). Routledge.
- Ritchie J, Lewis J, Nicholls CMC, et al. (eds) (2013) Qualitative Research Practises. A Guide for Social Science Students and Researchers . Sage.
- Sogg S, Grupski A, Dixon JB. (2018) Bad words: why language counts in our work with bariatric patients . Surgery for Obesity and Related Diseases 14 ( 5 ): 682–692. [ PubMed ] [ Google Scholar ]
- Spencer MS, Rosland AM, Kieffer ECet al. >(2011) Effectiveness of a community health worker intervention among African American and Latino adults with type 2 diabetes: a randomised controlled trial . American Journal of Public Health 101 ( 12 ): 2253–2260. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Strain WD, Cos X, Hirst Met al. >(2014) Time to do more: addressing clinical inertia in the management of type 2 diabetes mellitus . Diabetes Research and Clinical Practice 105 ( 3 ): 302–312. [ PubMed ] [ Google Scholar ]
- Trief P, Sandberg JG, Ploutz-Snyder Ret al. >(2011) Promoting couples collaboration in type 2 diabetes: the diabetes support project pilot data . Families, Systems, and Health 29 ( 3 ): 253. [ PubMed ] [ Google Scholar ]
- Utz SW, Williams IC, Jones Ret al. >(2008) Culturally tailored intervention for rural African Americans with type 2 diabetes . The Diabetes Educator 34 ( 5 ): 854–865. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Uzochukwu BSC, Ughasoro MD, Etiaba Eet al. >(2015) Health care financing in Nigeria: implications for achieving universal health coverage . Nigerian Journal of Clinical Practice 18 ( 4 ): 437–444. [ PubMed ] [ Google Scholar ]
- Wong CK, Wong WC, Lam CLet al. >(2014) Effects of Patient Empowerment Programme (PEP) on clinical outcomes and health service utilisation in type 2 diabetes mellitus in primary care: an observational matched cohort study . PloS One 9 ( 5 ): e95328. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- World Bank (2017) Current health expenditure (% of GDP) – Sub-Saharan Africa, World . Available at: https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS?locations=ZG-1W (accessed June 2020).
- World Health Organization (2016). Global report on Diabetes. Available at: http://docs.dpaq.de/10605-diabetes_who_embargoed-who-global-report-on-diabetes.pdf (accessed May 2016).
- Zhang J, Donald M, Baxter KAet al. >(2015) Impact of an integrated model of care on potentially preventable hospitalisations for people with type 2 diabetes mellitus . Diabetic Medicine 32 ( 7 ): 872–880. [ PubMed ] [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
What Is Type 2 Diabetes Mellitus Nursing Essay. Type 2 diabetes is the most common form of the disease. Diabetes mellitus is where the body cells cannot use glucose properly for lack of or resistance to the hormone insulin, which is produced by the pancreas. Diabetes can lead to serious complications over time if left untreated.
Diabetes mellitus is an increasingly prevalent condition.[1][2] This condition is characterized by hyperglycemia. The two main types of diabetes are type 1 diabetes mellitus and type 2 diabetes mellitus, with type 2 diabetes accounting for 90% of all cases. Other types of diabetes mellitus include gestational diabetes, drug-induced diabetes, and monogenic diabetes. Complications of diabetes ...
In diabetes, the role of advanced practice nurses has significantly contributed to improved outcomes in the management of type 2 diabetes,5 in specialized diabetes foot care programs,6 in the management of diabetes in pregnancy,7 and in the care of pediatric type 1 diabetic patients and their parents.8,9 Furthermore, NPs have also been ...
Type 2 diabetes is the most common form of the disease. Diabetes mellitus is where the body cells cannot use glucose properly for lack of or resistance to the hormone insulin, which is produced by the pancreas. Diabetes can lead to serious complications over time if left untreated. The high blood sugar levels from uncontrolled diabetes can ...
Introduction. Insulin resistance and β-cell dysfunction are the 2 major hallmarks of type 2 diabetes mellitus (T2DM) that appear as the result of disturbed homeostasis [].Failure of β-cells (∼80% of their β-cell function) and insulin resistance in muscles and the liver is a vicious triumvirate responsible for the core physiological defects.
Type 2 Diabetes Mellitus (T2DM) is characterized by chronically elevated blood glucose (hyperglycemia) and elevated blood insulin (hyperinsulinemia). When the blood glucose concentration is 100 milligrams/deciliter the bloodstream of an average adult contains about 5-10 grams of glucose. Carbohydrate-restricted diets have been used effectively to treat obesity and T2DM for over 100 years ...
Diabetes mellitus is a chronic heterogeneous metabolic disorder with complex pathogenesis. It is characterized by elevated blood glucose levels or hyperglycemia, which results from abnormalities in either insulin secretion or insulin action or both. Hyperglycemia manifests in various forms with a varied presentation and results in carbohydrate ...
Abstract. There are now over four million people living with diabetes in the UK, the majority having type 2 diabetes. The prevalence of type 2 diabetes is rising in line with growing obesity levels. This article will explore prevalence of type 2 diabetes, its prevention and treatment. It also provides guidance on how nurses can work with people ...
Leahy et al (2015) report from The Irish LongituDinal Study on Ageing (TILDA) that type 2 diabetes is the leading cause of death and disability in Ireland, and it is well known that diabetes increases risk of heart attacks, heart failure and kidney disease, resulting in a loss of independence and early mortality. They further note that diabetes ...
Optimisation of this sequence led to the development of JANUVIATM (sitagliptin), a selective DPP-4 inhibitor for treatment of type 2 diabetes (Kumar, Tripathi and Garg, 2013). Sitagliptin was first approved by the FDA for the treatment of type 2 diabetes in 2006 (Drugs.com, 2019). It is available in doses of 25, 50 and 100 mg tablets.
A model for achieving enhanced nursing care of patients with diabetes has been developed according to the findings of this literature. ... Furthermore, this study focuses on both diabetes type 1 and type 2 since our aim is to identify what is the situation in general about diabetes care and whether there is a gap between these two types ...
type 2 diabetes type diabetes assignment brief for case study words) paragraph (300 words) this essay began in an inpatient psychiatric setting, were the. Skip to document. ... will maintain complete anonymity and confidentiality in accordance with Nursing and Midwifery Counsel 2018. Diabetes affects approximately two million within the ...
With the global prevalence of diabetes set to increase over the coming decades from 537 million in 2021 to 783 million in 2045,1 solutions must be found to ensure that both prevention and treatment are guaranteed. A key component to this response will be the strengthening of health systems. Included in the overall health system response is the important role that human resources have in ...
BMJ Open Diabetes Research and Care, 7(1), e000981(Self-Management of Type 2 Diabetes Comprehensive Nursing Essay Example) Hemmati Maslakpak, M., Razmara, S., & Niazkhani, Z. (2017). Effects of Face-to-Face and Telephone-Based Family-Oriented Education on Self-Care Behavior and Patient Outcomes in Type 2 Diabetes: A Randomized Controlled Trial.
Diabetes mellitus is a metabolic disorder characterised by persistent high glucose levels in blood. The hyperglycaemia persists due to either failure of insulin production or tissues resistance to insulin (Yorek et al., 2015; Barron, 2010). Insulin is produced by the pancreas.
Type 2 diabetes mellitus (T2DM) is a chronic health condition whose worldwide prevalence has increased rapidly in recent decades. 1 Individuals with T2DM are responsible for the daily decisions and actions necessary to manage their disease, which makes self-management the cornerstone of diabetes care. 2 Self-management can be defined as an ...
Type 2 diabetes is a dangerous but treatable disease that manifests as high blood sugar, low insulin, and general insulin resistance. It results from living habits rather than any form of a pathogen, and people can develop it spontaneously as long as they are in a risk group. It generally does not require hospitalization unless the issue is ...
Introduction. Type 2 diabetes mellitus (T2DM) has become one of the major causes of burden of disease globally. An estimated 422 million adults were living with the disease in 2014, compared with 108 million in 1980[], representing a nearly quadruple increase within a period of thirty-four years.By 2035 the prevalence of T2DM is expected to increase by about 54% from the 2013 figures to about ...
Although the prognosis for people with type 2 diabetes mellitus is less than favourable, evidence has shown that making major lifestyle changes, such as having a healthy diet, smoking cessation, and increasing activity levels, can reduce the risk of long-term complications (UK Prospective Diabetes Study Group, 1998a).
Introduction. The prevalence of diabetes mellitus (DM) is increasing across the world and, notably, in low and middle-income countries (LMICs). Type 2 diabetes mellitus (T2DM) is the most prevalent type of DM in Nigeria (International Diabetes Federation, 2015), accounting for 95% of DM cases reported in Nigerian hospitals (Chinenye et al., 2012). ...
Essays. Type 2 Diabetes is an example of a metabolic disorder. This disease is caused by high blood sugar and a relative lack of insulin substances in the body system of an individual. This essay provides an analysis of the development of type 2 diabetes in United States, and compares it, to the development of this medical condition in ...