- Patient Care & Health Information
- Diseases & Conditions
- Teen depression
Teen depression is a serious mental health problem that causes a persistent feeling of sadness and loss of interest in activities. It affects how your teenager thinks, feels and behaves, and it can cause emotional, functional and physical problems. Although depression can occur at any time in life, symptoms may be different between teens and adults.
Issues such as peer pressure, academic expectations and changing bodies can bring a lot of ups and downs for teens. But for some teens, the lows are more than just temporary feelings — they're a symptom of depression.
Teen depression isn't a weakness or something that can be overcome with willpower — it can have serious consequences and requires long-term treatment. For most teens, depression symptoms ease with treatment such as medication and psychological counseling.

Products & Services
- A Book: A Practical Guide to Help Kids of All Ages Thrive
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Teen depression signs and symptoms include a change from the teenager's previous attitude and behavior that can cause significant distress and problems at school or home, in social activities, or in other areas of life.
Depression symptoms can vary in severity, but changes in your teen's emotions and behavior may include the examples below.
Emotional changes
Be alert for emotional changes, such as:
- Feelings of sadness, which can include crying spells for no apparent reason
- Frustration or feelings of anger, even over small matters
- Feeling hopeless or empty
- Irritable or annoyed mood
- Loss of interest or pleasure in usual activities
- Loss of interest in, or conflict with, family and friends
- Low self-esteem
- Feelings of worthlessness or guilt
- Fixation on past failures or exaggerated self-blame or self-criticism
- Extreme sensitivity to rejection or failure, and the need for excessive reassurance
- Trouble thinking, concentrating, making decisions and remembering things
- Ongoing sense that life and the future are grim and bleak
- Frequent thoughts of death, dying or suicide
Behavioral changes
Watch for changes in behavior, such as:
- Tiredness and loss of energy
- Insomnia or sleeping too much
- Changes in appetite — decreased appetite and weight loss, or increased cravings for food and weight gain
- Use of alcohol or drugs
- Agitation or restlessness — for example, pacing, hand-wringing or an inability to sit still
- Slowed thinking, speaking or body movements
- Frequent complaints of unexplained body aches and headaches, which may include frequent visits to the school nurse
- Social isolation
- Poor school performance or frequent absences from school
- Less attention to personal hygiene or appearance
- Angry outbursts, disruptive or risky behavior, or other acting-out behaviors
- Self-harm — for example, cutting or burning
- Making a suicide plan or a suicide attempt
What's normal and what's not
It can be difficult to tell the difference between ups and downs that are just part of being a teenager and teen depression. Talk with your teen. Try to determine whether he or she seems capable of managing challenging feelings, or if life seems overwhelming.
When to see a doctor
If depression signs and symptoms continue, begin to interfere in your teen's life, or cause you to have concerns about suicide or your teen's safety, talk to a doctor or a mental health professional trained to work with adolescents. Your teen's family doctor or pediatrician is a good place to start. Or your teen's school may recommend someone.
Depression symptoms likely won't get better on their own — and they may get worse or lead to other problems if untreated. Depressed teenagers may be at risk of suicide, even if signs and symptoms don't appear to be severe.
If you're a teen and you think you may be depressed — or you have a friend who may be depressed — don't wait to get help. Talk to a health care provider such as your doctor or school nurse. Share your concerns with a parent, a close friend, a spiritual leader, a teacher or someone else you trust.
Suicide is often associated with depression. If you think you may hurt yourself or attempt suicide, call 911 or your local emergency number immediately.
Also consider these options if you're having suicidal thoughts:
- Call your mental health professional.
- In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline , available 24 hours a day, seven days a week. Or use the Lifeline Chat . The Spanish language phone line is 1-888-628-9454 (toll-free). Services are free and confidential.
- Or contact a crisis service for teenagers in the U.S. called TXT 4 HELP : Text the word "safe" and your current location to 4HELP (44357) for immediate help, with the option for interactive texting.
- Seek help from your primary care doctor or other health care provider.
- Reach out to a close friend or loved one.
- Contact a minister, spiritual leader or someone else in your faith community.
If a loved one or friend is in danger of attempting suicide or has made an attempt:
- Make sure someone stays with that person.
- Call 911 or your local emergency number immediately.
- Or, if you can do so safely, take the person to the nearest hospital emergency room.
Never ignore comments or concerns about suicide. Always take action to get help.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
It's not known exactly what causes depression, but a variety of issues may be involved. These include:
- Brain chemistry. Neurotransmitters are naturally occurring brain chemicals that carry signals to other parts of your brain and body. When these chemicals are abnormal or impaired, the function of nerve receptors and nerve systems changes, leading to depression.
- Hormones. Changes in the body's balance of hormones may be involved in causing or triggering depression.
- Inherited traits. Depression is more common in people whose blood relatives — such as a parent or grandparent — also have the condition.
- Early childhood trauma. Traumatic events during childhood, such as physical or emotional abuse, or loss of a parent, may cause changes in the brain that increase the risk of depression.
- Learned patterns of negative thinking. Teen depression may be linked to learning to feel helpless — rather than learning to feel capable of finding solutions for life's challenges.
Risk factors
Many factors increase the risk of developing or triggering teen depression, including:
- Having issues that negatively impact self-esteem, such as obesity, peer problems, long-term bullying or academic problems
- Having been the victim or witness of violence, such as physical or sexual abuse
- Having other mental health conditions, such as bipolar disorder, an anxiety disorder, a personality disorder, anorexia or bulimia
- Having a learning disability or attention-deficit/hyperactivity disorder (ADHD)
- Having ongoing pain or a chronic physical illness such as cancer, diabetes or asthma
- Having certain personality traits, such as low self-esteem or being overly dependent, self-critical or pessimistic
- Abusing alcohol, nicotine or other drugs
- Being gay, lesbian, bisexual or transgender in an unsupportive environment
Family history and issues with family or others may also increase your teenager's risk of depression, such as:
- Having a parent, grandparent or other blood relative with depression, bipolar disorder or alcohol use problems
- Having a family member who died by suicide
- Having a family with major communication and relationship problems
- Having experienced recent stressful life events, such as parental divorce, parental military service or the death of a loved one
Complications
Untreated depression can result in emotional, behavioral and health problems that affect every area of your teenager's life. Complications related to teen depression may include, for example:
- Alcohol and drug misuse
- Academic problems
- Family conflicts and relationship difficulties
- Suicide attempts or suicide
There's no sure way to prevent depression. However, these strategies may help. Encourage your teenager to:
- Take steps to control stress, increase resilience and boost self-esteem to help handle issues when they arise
- Practice self-care, for example by creating a healthy sleep routine and using electronics responsibly and in moderation
- Reach out for friendship and social support, especially in times of crisis
- Get treatment at the earliest sign of a problem to help prevent depression from worsening
- Maintain ongoing treatment, if recommended, even after symptoms let up, to help prevent a relapse of depression symptoms
Teen depression care at Mayo Clinic
- Depressive disorders. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. American Psychiatric Association; 2013. https://dsm.psychiatryonline.org. Accessed May 4, 2021.
- Bipolar and related disorders. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. American Psychiatric Association; 2013. https://dsm.psychiatryonline.org. Accessed May 4, 2021.
- Brown AY. Allscripts EPSi. Mayo Clinic. April 9, 2021.
- Teen depression. National Institute of Mental Health. https://www.nimh.nih.gov/health/publications/teen-depression/. Accessed March 30, 2022.
- Depression in children and teens. American Academy of Child and Adolescent Psychiatry. https://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/The-Depressed-Child-004.aspx. Accessed May 4, 2021.
- Psychotherapy for children and adolescents: Different types. American Academy of Child and Adolescent Psychiatry. https://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/Psychotherapies-For-Children-And-Adolescents-086.aspx. Accessed May 4, 2021.
- Suicidality in children and adolescents being treated with antidepressant medications. U.S. Food and Drug Administration. https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/suicidality-children-and-adolescents-being-treated-antidepressant-medications. Accessed May 4, 2021.
- Depression medicines. U.S. Food and Drug Administration. https://www.fda.gov/consumers/free-publications-women/depression-medicines. Accessed May 4, 2021.
- Building your resilience. American Psychological Association. https://www.apa.org/topics/resilience. Accessed May 4, 2021.
- Psychiatric medications for children and adolescents: Part I ― How medications are used. American Academy of Child and Adolescent Psychiatry. https://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/Psychiatric-Medication-For-Children-And-Adolescents-Part-I-How-Medications-Are-Used-021.aspx. Accessed May 4, 2021.
- Psychiatric medications for children and adolescents: Part II ― Types of medications. American Academy of Child and Adolescent Psychiatry. https://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/Psychiatric-Medication-For-Children-And-Adolescents-Part-II-Types-Of-Medications-029.aspx. Accessed May 5, 2021.
- Weersing VR, et al. Evidence-base update of psychosocial treatments for child and adolescent depression. Journal of Clinical Child and Adolescent Psychology. 2017; doi:10.1080/15374416.2016.1220310.
- Zuckerbrot RA, et al. Guidelines for adolescent depression in primary care (GLAD-PC): Part I. Practice preparation, identification, assessment, and initial management. Pediatrics. 2018; doi:10.1542/peds.2017-4081.
- Cheung AH, et al. Guidelines for adolescent depression in primary care (GLAD-PC): Part II. Treatment and ongoing management. Pediatrics. 2018; doi:10.1542/peds.2017-4082.
- Resilience guide for parents and teachers. American Psychological Association. https://www.apa.org/topics/resilience/guide-parents-teachers. Accessed May 4, 2021.
- Rice F, et al. Adolescent and adult differences in major depression symptoms profiles. Journal of Affective Disorders. 2019; doi:10.1016/j.jad.2018.09.015.
- Haller H, et al. Complementary therapies for clinical depression: An overview of systemic reviews. BMJ Open. 2019; doi:10.1136/bmjopen-2018-028527.
- Ng JY, et al. Complementary and alternative medicine recommendations for depression: A systematic review and assessment of clinical practice guidelines. BMC Complementary Medicine and Therapeutics. 2020; doi:10.1186/s12906-020-03085-1.
- American College of Obstetricians and Gynecologists. Practice Bulletin No. 92: Use of psychiatric medications during pregnancy and lactation. Obstetrics & Gynecology. 2008; doi:10.1097/AOG.0b013e31816fd910. Reaffirmed 2019.
- Neavin DR, et al. Treatment of major depressive disorder in pediatric populations. Diseases. 2018; doi:10.3390/diseases6020048.
- Vande Voort JL (expert opinion). Mayo Clinic. June 29, 2021.
- Safe Place: TXT 4 HELP. https://www.nationalsafeplace.org/ txt-4-help. Accessed March 30, 2022.
- Antidepressants for children and teens
Associated Procedures
- Acupuncture
- Cognitive behavioral therapy
- Psychotherapy
News from Mayo Clinic
- Mayo Clinic Minute: Know the difference between adult and teen depression April 15, 2022, 04:00 p.m. CDT
Mayo Clinic in Rochester, Minnesota, has been recognized as one of the top Psychiatry hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Let’s celebrate our doctors!
Join us in celebrating and honoring Mayo Clinic physicians on March 30th for National Doctor’s Day.
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Verywell Mind Insights
- 2023 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
Depression in Teens
Barbara Poncelet, CRNP, is a certified pediatric nurse practitioner specializing in teen health.
Steven Gans, MD is board-certified in psychiatry and is an active supervisor, teacher, and mentor at Massachusetts General Hospital.
:max_bytes(150000):strip_icc():format(webp)/steven-gans-1000-51582b7f23b6462f8713961deb74959f.jpg)
Verywell / Jo Zixuan Zhou
As much as 8% of teens experience depression each year, according to one survey. By the time young adults reach age 21, one study found that nearly 15% have had at least one episode of a mood disorder. Depression can cause problems such as difficulties in school, difficulties with relationships, and decreased enjoyment of life. At its worst, depression can lead to suicide, one of the leading causes of death for teens in the United States.
Depression is an illness with many causes and many forms. It is a disorder of a person’s moods or emotions—not an attitude that someone can “control” or “snap out of.” But it is treatable with psychotherapy and/or medication, which is why it's especially important for parents and caregivers to educate themselves about the disorder.
Adults sometimes don’t recognize symptoms of depression in teens because the disorder can look quite different from that in adults. A teenager with depression might have some or all of these signs of the illness:
- Sad or depressed mood
- Feelings of worthlessness or hopelessness
- Loss of interest in things they used to enjoy
- Withdrawal from friends and family
- Inability to sleep or sleeping too much
- Loss of appetite or increased appetite
- Aches and pains that don’t go away, even with treatment
- Irritability
- Feeling tired despite getting enough sleep
- Inability to concentrate
- Thoughts of suicide, talk of suicide, or suicide attempts
Types of Teen Depression
The National Institute of Mental Health states that there are two common forms of depression found in teens: major depressive disorder and dysthymic disorder (now known as persistent depressive disorder).
- Major depressive disorder , also called major depression, is characterized by a combination of symptoms that interfere with a person's ability to work, sleep, study, eat, and enjoy once pleasurable activities. Major depression is disabling and prevents a person from functioning normally. An episode of major depression may occur only once in a person's lifetime, but more often, it recurs throughout a person's life.
- Dysthymic disorder , also called dysthymia, is characterized by long-term (two years or longer) but less severe symptoms that may not disable a person but can prevent one from functioning normally or feeling well. People with dysthymia may also experience one or more episodes of major depression during their lifetimes.
There are thought to be many causes of depression . There are most likely many factors behind who develops depression and who doesn’t, and these factors are no different for teens.
- Traumatic life event, such as the loss of a loved one or pet, divorce, or remarriage. Any event that causes distress or trauma, or even just a major change in lifestyle, can trigger depression in a vulnerable individual.
- Social situation/family circumstances. Unfortunately, there are teens who live in difficult circumstances. Domestic violence, substance abuse, poverty or other family issues can cause stress and contribute to depression in a teen.
- Genetics/biology. It has been found that depression runs in families and that there is a genetic basis for depression. Keep in mind, though, that teens who have depression in their family will not necessarily get the illness, and teens without a history of depression in their family can still get the disorder.
- Medical conditions. Occasionally, symptoms of depression can be a sign of another medical illness, such as hypothyroidism, or other disorders.
- Medications/illegal drugs. Some legal, prescription medications can have depression as a side effect. Certain illegal drugs (street drugs) can also cause depression.
Depression in teens is most often diagnosed by a primary care physician.
Researchers suggest that teen depression is often underdiagnosed and undertreated.
If teen depression is suspected, a doctor will often start with a physical exam that may include blood tests. Your teen's pediatrician will want to rule out any other medical illnesses that may be causing or contributing to your teen's symptoms.
Your child will also be given a psychological evaluation. This often involves a depression questionnaire as well as a discussion about the severity and duration of their symptoms.
The Guidelines for Adolescent Depression in Primary Care (GLAD-PC) recommend the following in the management of teen depression:
- Educating teens and families about treatment options that are available
- Developing a treatment plan that includes specific treatment goals that address functioning at home and school
- Collaborating with other mental health resources in the community
- Creating a safety plan with steps that should be taken if the teen's symptoms become worse or if they experience suicidal thinking
- Considering active support and monitoring before beginning other treatments
- Consulting a mental health specialist if symptoms are moderate or severe
- Incorporating evidence-based treatments such as cognitive-behavioral therapy, interpersonal therapy, and antidepressants
- Continuing to monitor symptoms and functioning during antidepressant treatment; doctors and family member should watch for signs that symptoms are worsening and for suicidal thinking or behaviors
Talk to your teen about your concerns. There may be a specific cause for why they are acting a certain way. Opening up the lines of communication lets your teenager know you care and that you are available to talk about the situation and provide support.
Other things that may help your teen manage symptoms of depression include:
- Talking about concerns with family and friends
- Having a healthy support system
- Using good stress management techniques
- Eating a healthy diet
- Getting regular exercise
- Finding new things to look forward to
- Joining a support group, either offline or online
Also, talk to your pediatrician or family physician if you have concerns about your teen regarding depression. Your provider may be able to discuss the situation with your teen, rule out a medical reason for the behavior, recommend a psychotherapist, or prescribe medication .
Lastly, never ignore the signs or symptoms of depression. Depression is treatable and there is help available for both you and your teen. If left untreated, depression can lead to thoughts of suicide or even the act itself.
If your teen talks about suicide or attempts suicide, get help immediately. The Centers for Disease Control and Prevention (CDC) cites suicide as the third leading cause of death for people between the ages of 10 and 24.
If a teen is in immediate danger of suicide, call 911. If you or a loved one is having thoughts of suicide, call the National Suicide Prevention Lifeline at 988 to get support from a trained counselor in your area.
For more mental health resources, see our National Helpline Database .
Kessler RC, Avenevoli S, Costello EJ, Georgiades K, Green JG, et al. Prevalence, persistence, and sociodemographic correlates of DSM-IV disorders in the National Comorbidity Survey Replication Adolescent Supplement . Arch Gen Psychiatry . 2012; 69(4): 372-80. doi:10.1001/archgenpsychiatry.2011.160
Copeland W, Shanahan L, Costello EJ, Angold A. Cumulative prevalence of psychiatric disorders by young adulthood: A prospective cohort analysis from the Great Smoky Mountains Study . J Am Acad Child Adolesc Psychiatry . 2011; 50(3): 252-261. doi:10.1016/j.jaac.2010.12.014
Cheung AH, Kozloff N, Sacks D. Pediatric depression: An evidence-based update on treatment interventions . D. Curr Psychiatry Rep. 2013; 15: 381. doi:10.1007/s11920-013-0381-4
Zuckerbrot RA, Cheung A, Jensen PS, Stein REK, Larague D, GLAD-PC Steering Group. Guidelines for adolescent depression in primary care (GLAD-PC): Part II. Treatment and ongoing management . Pediatrics . 2018; 141(3). pii: e20174082. doi:10.1542/peds.2017-4082
By Barbara Poncelet Barbara Poncelet, CRNP, is a certified pediatric nurse practitioner specializing in teen health.
Parent’s Guide to Teen Depression
Are you feeling suicidal, coping with depression.
- Premenstrual Dysphoric Disorder (PMDD): How to Cope with Severe PMS
- I Feel Depressed: 9 Ways to Deal with Depression
- Depression Types and Causes: Clinical, Major, and Others
- Electroconvulsive Therapy (ECT): How it Works and What to Expect
Depression Symptoms and Warning Signs
- Online Therapy: Is it Right for You?
- Mental Health
- Health & Wellness
- Children & Family
- Relationships
Are you or someone you know in crisis?
- Bipolar Disorder
- Eating Disorders
- Grief & Loss
- Personality Disorders
- PTSD & Trauma
- Schizophrenia
- Therapy & Medication
- Exercise & Fitness
- Healthy Eating
- Well-being & Happiness
- Weight Loss
- Work & Career
- Illness & Disability
- Heart Health
- Childhood Issues
- Learning Disabilities
- Family Caregiving
- Teen Issues
- Communication
- Emotional Intelligence
- Love & Friendship
- Domestic Abuse
- Healthy Aging
- Aging Issues
- Alzheimer’s Disease & Dementia
- Senior Housing
- End of Life
- Meet Our Team
What is teen depression?
Signs and symptoms of teen depression, coping with suicidal thoughts, why am i depressed, overcoming teen depression tip 1: talk to an adult you trust, tip 2: try not to isolate yourself—it makes depression worse, tip 3: adopt healthy habits, tip 4: manage stress and anxiety, how to help a depressed teen friend, dealing with teen depression.
No matter how despondent life seems right now, there are many things you can do to start feeling better today. Use these tools to help yourself or a friend.

The teenage years can be really tough and it’s perfectly normal to feel sad or irritable every now and then. But if these feelings don’t go away or become so intense that you feel overwhelmingly hopeless and helpless, you may be suffering from depression.
Teen depression is much more than feeling temporarily sad or down in the dumps. It’s a serious and debilitating mood disorder that can change the way you think, feel, and function in your daily life, causing problems at home, school, and in your social life. When you’re depressed, you may feel hopeless and isolated and it can seem like no one understands. But depression is far more common in teens than you may think. The increased academic pressures, social challenges, and hormonal changes of the teenage years mean that about one in five of us suffer with depression in our teens. You’re not alone and your depression is not a sign of weakness or a character flaw.
Even though it can feel like the black cloud of depression will never lift, there are plenty of things you can do to help yourself deal with symptoms, regain your balance and feel more positive, energetic, and hopeful again.
If you’re a parent or guardian worried about your child…
While it isn’t always easy to differentiate from normal teenage growing pains, teen depression is a serious health problem that goes beyond moodiness. As a parent, your love, guidance, and support can go a long way toward helping your teen overcome depression and get their life back on track. Read Parent’s Guide to Teen Depression .
It can be hard to put into words exactly how depression feels—and we don’t all experience it the same way. For some teens, depression is characterized by feelings of bleakness and despair. For others, it’s a persistent anger or agitation, or simply an overwhelming sense of “emptiness.” However depression affects you, though, there are some common symptoms that you may experience:
- You constantly feel irritable, sad, or angry.
- Nothing seems fun anymore—even the activities you used to love—and you just don’t see the point of forcing yourself to do them.
- You feel bad about yourself—worthless, guilty, or just “wrong” in some way.
- You sleep too much or not enough.
- You’ve turned to alcohol or drugs to try to change the way you feel .
- You have frequent, unexplained headaches or other physical pains or problems.
- Anything and everything makes you cry.
- You’re extremely sensitive to criticism.
- You’ve gained or lost weight without consciously trying to.
- You’re having trouble concentrating, thinking straight, or remembering things. Your grades may be plummeting because of it.
- You feel helpless and hopeless.
- You’re thinking about death or suicide. (If so, talk to someone right away!)
If your negative feelings caused by depression become so overwhelming that you can’t see any solution besides harming yourself or others, you need to get help right away . Asking for help when you’re in the midst of such strong emotions can be really difficult, but it’s vital you reach out to someone you trust—a friend, family member, or teacher, for example. If you don’t feel that you have anyone to talk to, or think that talking to a stranger might be easier, call a suicide helpline . You’ll be able to speak in confidence to someone who understands what you’re going through and can help you deal with your feelings.
Whatever your situation, it takes real courage to face death and step back from the brink. You can use that courage to help you keep going and overcome depression.
There is ALWAYS another solution, even if you can’t see it right now. Many people who have survived a suicide attempt say that they did it because they mistakenly felt there was no other solution to a problem they were experiencing. At the time, they couldn’t see another way out, but in truth, they didn’t really want to die. Remember that no matter how badly you feel, these emotions will pass.
Having thoughts of hurting yourself or others does not make you a bad person. Depression can make you think and feel things that are out of character. No one should judge you or condemn you for these feelings if you are brave enough to talk about them.
If your feelings are uncontrollable, tell yourself to wait 24 hours before you take any action. This can give you time to really think things through and give yourself some distance from the strong emotions that are plaguing you. During this 24-hour period, try to talk to someone—anyone—as long as they are not another suicidal or depressed person. Call a hotline or talk to a friend. What do you have to lose?
If you’re afraid you can’t control yourself, make sure you are never alone. Even if you can’t verbalize your feelings, just stay in public places, hang out with friends or family members, or go to a movie—anything to keep from being by yourself and in danger.
If you're thinking about suicide…
Please read Are You Feeling Suicidal? or call a helpline:
- In the U.S.: 988
- UK: 116 123
- Australia: 13 11 14
- To find a helpline in other countries, visit IASP or Suicide.org .
Remember, suicide is a “permanent solution to a temporary problem.” Please take that first step and reach out now.
Despite what you may have been told, depression is not simply caused by a chemical imbalance in the brain that can be cured with medication. Rather, depression is caused by a combination of biological, psychological, and social factors . Since the teenage years can be a time of great turmoil and uncertainty, you’re likely facing a host of pressures that could contribute to your depression symptoms. These can range from hormonal changes to problems at home or school or questions about who you are and where you fit in.
As a teen, you’re more likely to suffer from depression if you have a family history of depression or have experienced early childhood trauma, such as the loss of a parent or physical or emotional abuse .
Risk factors for teen depression
Risk factors that can trigger or exacerbate depression in teens include:
- Serious illness, chronic pain, or physical disability .
- Having other mental health conditions, such as anxiety, an eating disorder , learning disorder , or ADHD.
- Alcohol or drug abuse.
- Academic or family problems.
- Trauma from violence or abuse.
- Recent stressful life experiences, such as parental divorce or the death of a loved one.
- Coping with your sexual identity in an unsupportive environment.
- Loneliness and lack of social support.
- Spending too much time on social media .
If you’re being bullied…
The stress of bullying—whether it’s online, at school, or elsewhere—is very difficult to live with. It can make you feel helpless, hopeless, and ashamed: the perfect recipe for depression.
If you’re being bullied, know that it’s not your fault. No matter what a bully says or does, you should not be ashamed of who you are or what you feel. Bullying is abuse and you don’t have to put up with it . You deserve to feel safe, but you’ll most likely need help. Find support from friends who don’t bully and turn to an adult you trust—whether it’s a parent, teacher, counselor, pastor, coach, or the parent of a friend.
Whatever the causes of your depression, the following tips can help you overcome your symptoms, change how you feel, and regain your sense of hope and enthusiasm.
Depression is not your fault, and you didn’t do anything to cause it. However, you do have some control over feeling better. The first step is to ask for help.
Speak to a Licensed Therapist
BetterHelp is an online therapy service that matches you to licensed, accredited therapists who can help with depression, anxiety, relationships, and more. Take the assessment and get matched with a therapist in as little as 48 hours.
Talking to someone about depression
It may seem like there’s no way your parents will be able to help, especially if they are always nagging you or getting angry about your behavior. The truth is, parents hate to see their kids hurting. They may feel frustrated because they don’t understand what is going on with you or know how to help.
- If your parents are abusive in any way, or if they have problems of their own that makes it difficult for them to take care of you, find another adult you trust (such as a relative, teacher, counselor, or coach). This person can either help you approach your parents, or direct you toward the support you need.
- If you truly don’t have anyone you can talk to, there are many hotlines, services, and support groups that can help.
- No matter what, talk to someone, especially if you are having any thoughts of harming yourself or others. Asking for help is the bravest thing you can do, and the first step on your way to feeling better.
The importance of accepting and sharing your feelings
It can be hard to open up about how you’re feeling—especially when you’re feeling depressed, ashamed, or worthless. It’s important to remember that many people struggle with feelings like these at one time or another—it doesn’t mean that you’re weak, fundamentally flawed, or no good. Accepting your feelings and opening up about them with someone you trust will help you feel less alone.
Even though it may not feel like it at the moment, people do love and care about you. If you can muster the courage to talk about your depression, it can—and will—be resolved. Some people think that talking about sad feelings will make them worse, but the opposite is almost always true. It is very helpful to share your worries with someone who will listen and care about what you say. They don’t need to be able to “fix” you; they just need to be good listeners.
Depression causes many of us to withdraw into our shells. You may not feel like seeing anybody or doing anything and some days just getting out of bed in the morning can be difficult. But isolating yourself only makes depression worse. So even if it’s the last thing you want to do, try to force yourself to stay social. As you get out into the world and connect with others, you’ll likely find yourself starting to feel better.
Spend time face-to-face with friends who make you feel good —especially those who are active, upbeat, and understanding. Avoid hanging out with those who abuse drugs or alcohol, get you into trouble, or make you feel judged or insecure.
Get involved in activities you enjoy (or used to). Getting involved in extracurricular activities seem like a daunting prospect when you’re depressed, but you’ll feel better if you do. Choose something you’ve enjoyed in the past, whether it be a sport, an art, dance or music class, or an after-school club. You might not feel motivated at first, but as you start to participate again, your mood and enthusiasm will begin to lift.
Volunteer. Doing things for others is a powerful antidepressant and happiness booster. Volunteering for a cause you believe in can help you feel reconnected to others and the world, and give you the satisfaction of knowing you’re making a difference.
Cut back on your social media use. While it may seem that losing yourself online will temporarily ease depression symptoms, it can actually make you feel even worse. Comparing yourself unfavorably with your peers on social media , for example, only promotes feelings of depression and isolation. Remember: people always exaggerate the positive aspects of their lives online, brushing over the doubts and disappointments that we all experience. And even if you’re just interacting with friends online, it’s no replacement for in-person contact. Eye-to-eye contact, a hug, or even a simple touch on the arm from a friend can make all the difference to how you’re feeling.
Making healthy lifestyle choices can do wonders for your mood. Things like eating right, getting regular exercise, and getting enough sleep have been shown to make a huge difference when it comes to depression.
Get moving! Ever heard of a “runner’s high”? You actually get a rush of endorphins from exercising, which makes you feel instantly happier. Physical activity can be as effective as medications or therapy for depression, so get involved in sports, ride your bike, or take a dance class. Any activity helps! If you’re not feeling up to much, start with a short daily walk, and build from there.
Be smart about what you eat. An unhealthy diet can make you feel sluggish and tired, which worsens depression symptoms. Junk food , refined carbs, and sugary snacks are the worst culprits! They may give you a quick boost, but they’ll leave you feeling worse in the long run. Make sure you’re feeding your mind with plenty of fruits, vegetables, and whole grains. Talk to your parents, doctor, or school nurse about how to ensure your diet is adequately nutritious.
Avoid alcohol and drugs. You may be tempted to drink or use drugs in an effort to escape from your feelings and get a “mood boost,” even if just for a short time. However, as well as causing depression in the first place, substance use will only make depression worse in the long run. Alcohol and drug use can also increase suicidal feelings. If you’re addicted to alcohol or drugs , seek help. You will need special treatment for your substance problem on top of whatever treatment you’re receiving for your depression.
Aim for eight hours of sleep each night. Feeling depressed as a teenager typically disrupts your sleep. Whether you’re sleeping too little or too much, your mood will suffer. But you can get on a better sleep schedule by adopting healthy sleep habits.
For many teens, stress and anxiety can go hand-in-hand with depression. Unrelenting stress, doubts, or fears can sap your emotional energy, affect your physical health, send your anxiety levels soaring, and trigger or exacerbate depression.
If you’re suffering from an anxiety disorder , it can manifest itself in a variety of ways. Perhaps you endure intense anxiety attacks that strike without warning, get panicky at the thought of speaking in class, experience uncontrollable, intrusive thoughts, or live in a constant state of worry. Since anxiety makes depression worse (and vice versa), it’s important to get help for both conditions.
Tips for managing stress
Managing the stress in your life starts with identifying the sources of that stress:
- If exams or classes seem overwhelming, for example, talk to a teacher or school counselor, or find ways of improving how you manage your time.
- If you have a health concern you feel you can’t talk to your parents about—such as a pregnancy scare or drug problem —seek medical attention at a clinic or see a doctor. A health professional can guide you towards appropriate treatment (and help you approach your parents if that’s necessary).
- If you’re struggling to fit in or dealing with relationship, friendship, or family difficulties, talk your problems over with your school counselor or a professional therapist. Exercise, meditation , muscle relaxation, and breathing exercises are other good ways to cope with stress.
- If your own negative thoughts and chronic worrying are contributing to your everyday stress levels, you can take steps to break the habit and regain control of your worrying mind.
If you’re a teenager with a friend who seems down or troubled, you may suspect depression. But how do you know it’s not just a passing phase or a bad mood? Look for common warning signs of teen depression:
- Your friend doesn’t want to do the things you guys used to love to do.
- Your friend starts using alcohol or drugs or hanging with a bad crowd.
- Your friend stops going to classes and after-school activities.
- Your friend talks about being bad, ugly, stupid, or worthless.
- Your friend starts talking about death or suicide.
Teens typically rely on their friends more than their parents or other adults, so you may find yourself in the position of being the first—or only—person that your depressed friend confides in. While this might seem like a huge responsibility, there are many things you can do to help :
Get your friend to talk to you. Starting a conversation about depression can be daunting, but you can say something simple: “You seem like you are really down, and not yourself. I really want to help you. Is there anything I can do?”
You don’t need to have the answers. Your friend just needs someone to listen and be supportive. By listening and responding in a non-judgmental and reassuring manner, you are helping in a major way.
Encourage your friend to get help. Urge your depressed friend to talk to a parent, teacher, or counselor. It might be scary for your friend to admit to an authority figure that they have a problem. Having you there might help, so offer to go along for support.
Stick with your friend through the hard times. Depression can make people do and say things that are hurtful or strange. But your friend is going through a very difficult time, so try not to take it personally. Once your friend gets help, they will go back to being the person you know and love. In the meantime, make sure you have other friends or family taking care of you. Your feelings are important and need to be respected, too.
Speak up if your friend is suicidal. If your friend is joking or talking about suicide, giving possessions away, or saying goodbye, tell a trusted adult immediately. Your only responsibility at this point is to get your friend help , and get it fast. Even if you promised not to tell, your friend needs your help. It’s better to have a friend who is temporarily angry at you than one who is no longer alive.
Depression support, suicide prevention help
Depression support.
Find DBSA Chapters/Support Groups or call the NAMI Helpline for support and referrals at 1-800-950-6264
Find Depression support groups in-person and online or call the Mind Infoline at 0300 123 3393
Call the SANE Help Centre at 1800 18 7263
Call Mood Disorders Society of Canada at 519-824-5565
Call the Vandrevala Foundation Helpline (India) at 1860 2662 345 or 1800 2333 330
Suicide prevention help
Call 988 Suicide and Crisis Lifeline at 988
Call Samaritans UK at 116 123
Call Lifeline Australia at 13 11 14
Visit IASP or Suicide.org to find a helpline near you
More Information
- Depression: What You Need to Know - Depression in teenagers, including symptoms, remedies, and how to talk to your parents. (TeensHealth)
- Depression in Teens - Recognizing and treating adolescent depression. (Mental Health America)
- How to Talk to Your Parents About Getting Help - Speaking up for yourself is the first step to getting better. (Child Mind Institute)
- Petito, A., Pop, T. L., Namazova-Baranova, L., Mestrovic, J., Nigri, L., Vural, M., Sacco, M., Giardino, I., Ferrara, P., & Pettoello-Mantovani, M. (2020). The Burden of Depression in Adolescents and the Importance of Early Recognition. The Journal of Pediatrics, 218, 265-267.e1. Link
- Hallfors, D. D., Waller, M. W., Ford, C. A., Halpern, C. T., Brodish, P. H., & Iritani, B. (2004). Adolescent depression and suicide risk: Association with sex and drug behavior. American Journal of Preventive Medicine, 27(3), 224–231. Link
- Merikangas, K. R., He, J., Burstein, M., Swanson, S. A., Avenevoli, S., Cui, L., Benjet, C., Georgiades, K., & Swendsen, J. (2010). Lifetime Prevalence of Mental Disorders in U.S. Adolescents: Results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 49(10), 980–989. Link
- Bhatia, S. K., & Bhatia, S. C. (2007). Childhood and Adolescent Depression. American Family Physician, 75(1), 73–80. Link
- NIMH » Major Depression. (n.d.). Retrieved July 26, 2021, from Link
- Depressive Disorders. (2013). In Diagnostic and Statistical Manual of Mental Disorders . American Psychiatric Association. Link
More in Depression
Recognizing the signs and symptoms, and helping your child

How to deal with suicidal thoughts and feelings

Tips for overcoming depression one step at a time

Premenstrual Dysphoric Disorder (PMDD)
Coping with severe PMS

I Feel Depressed
9 Ways to Deal with Depression

Depression Types and Causes
What type of depression do you have and what’s causing it?

Electroconvulsive Therapy (ECT)
How it works and how to decide if it’s the right treatment for you

Recognizing depression and getting the help you need

Professional therapy, done online
BetterHelp makes starting therapy easy. Take the assessment and get matched with a professional, licensed therapist.
Help us help others
Millions of readers rely on HelpGuide.org for free, evidence-based resources to understand and navigate mental health challenges. Please donate today to help us save, support, and change lives.
- Share full article
Advertisement
Supported by
‘It’s Life or Death’: The Mental Health Crisis Among U.S. Teens
Depression, self-harm and suicide are rising among American adolescents. For one 13-year-old, the despair was almost too much to take.

By Matt Richtel
Photographs by Annie Flanagan
Matt Richtel spent more than a year interviewing adolescents and their families for this series on the mental health crisis.
One evening last April, an anxious and free-spirited 13-year-old girl in suburban Minneapolis sprang furious from a chair in the living room and ran from the house — out a sliding door, across the patio, through the backyard and into the woods.
Moments earlier, the girl’s mother, Linda, had stolen a look at her daughter’s smartphone. The teenager, incensed by the intrusion, had grabbed the phone and fled. (The adolescent is being identified by an initial, M, and the parents by first name only, to protect the family’s privacy.)
Linda was alarmed by photos she had seen on the phone. Some showed blood on M’s ankles from intentional self-harm. Others were close-ups of M’s romantic obsession, the anime character Genocide Jack — a brunette girl with a long red tongue who, in a video series, kills high school classmates with scissors.
In the preceding two years, Linda had watched M spiral downward: severe depression, self-harm, a suicide attempt. Now, she followed M into the woods, frantic. “Please tell me where u r,” she texted. “I’m not mad.”
American adolescence is undergoing a drastic change. Three decades ago, the gravest public health threats to teenagers in the United States came from binge drinking, drunken driving, teenage pregnancy and smoking. These have since fallen sharply, replaced by a new public health concern: soaring rates of mental health disorders.
In 2019, 13 percent of adolescents reported having a major depressive episode , a 60 percent increase from 2007 . Emergency room visits by children and adolescents in that period also rose sharply for anxiety, mood disorders and self-harm. And for people ages 10 to 24, suicide rates, stable from 2000 to 2007, leaped nearly 60 percent by 2018, according to the Centers for Disease Control and Prevention.

Emergency room visits for self-harm by children and adolescents rose sharply over the last decade, particularly among young women.
600 E.R. visits
per 100,000
Emergency room visits
for self-inflicted injuries
Ages 10–19

Emergency room visits for self-harm by children and adolescents rose sharply over the last decade, particularly for young women.
room visits
for self-harm
The decline in mental health among teenagers was intensified by the Covid pandemic but predated it, spanning racial and ethnic groups, urban and rural areas and the socioeconomic divide. In December, in a rare public advisory, the U.S. surgeon general warned of a “devastating” mental health crisis among adolescents. Numerous hospital and doctor groups have called it a national emergency , citing rising levels of mental illness, a severe shortage of therapists and treatment options, and insufficient research to explain the trend.
“Young people are more educated; less likely to get pregnant, use drugs; less likely to die of accident or injury,” said Candice Odgers, a psychologist at the University of California, Irvine. “By many markers, kids are doing fantastic and thriving. But there are these really important trends in anxiety, depression and suicide that stop us in our tracks.”
“We need to figure it out,” she said. “Because it’s life or death for these kids.”
Read about how Matt Richtel reported this series .
The crisis is often attributed to the rise of social media , but solid data on the issue is limited, the findings are nuanced and often contradictory and some adolescents appear to be more vulnerable than others to the effects of screen time. Federal research shows that teenagers as a group are also getting less sleep and exercise and spending less in-person time with friends — all crucial for healthy development — at a period in life when it is typical to test boundaries and explore one’s identity. The combined result for some adolescents is a kind of cognitive implosion: anxiety, depression, compulsive behaviors, self-harm and even suicide.
This surge has raised vexing questions. Are these issues inherent to adolescence that merely went unrecognized before — or are they being overdiagnosed now? Historical comparisons are difficult, as some data around certain issues, like teen anxiety and depression, began to be collected relatively recently. But the rising rates of emergency-room visits for suicide and self-harm leave little doubt that the physical nature of the threat has changed significantly.
As M descended, Linda and her husband realized they were part of an unenviable club: bewildered parents of an adolescent in profound distress. Linda talked with parents of other struggling teenagers; not long before the night M fled into the forest, Linda was jolted by the news that a local girl had died by suicide.
“You have no control over what they’re thinking,” Linda said. “I just want to tell people what can happen.”
‘A typical outpatient’

M is one of dozens of teenagers who spoke to The New York Times for a yearlong project exploring the changing nature of adolescence in the United States. The Times was given permission by M and the family to speak with M’s school counselor; M’s medical records were shared with The Times and, with the family’s permission, reviewed by outside experts not involved in M’s care.
“This is a typical outpatient,” said Emily Pluhar, a child and adolescent psychologist at Harvard University, describing M as “an internalizer.”
M, now 14, is tall, with red hair and blue eyes, and has a younger sister and older half brother. By turns shy and outspoken, M has thought extensively about pronouns and currently prefers “they.” At the beginning of seventh grade, M also asked to be called by the name of a popular Japanese anime character, whose first name starts with M. “I think we’re similar in that she’s, like, quiet and smart and plays electric bass, and I really like bass and guitars,” M said.
When M was 4, a psychologist the family consulted to assess M’s school readiness concluded that their “intellectual ability is in the very superior range,” according to the report. M enrolled in kindergarten as one of the younger class members.
At 10, M got a smartphone. Linda and her husband, Tony, both of whom had busy work schedules, worried that the device might lead to heavy screen time, but they felt it was necessary to stay in touch. At 11, M hit another adolescent milestone: puberty.
Over the last century, the age of puberty onset has dropped markedly for girls, to 12 years old today from 14 years old in 1990; the age of onset for boys has followed a similar path. Experts say this shift probably now plays a role in the adolescent mental health crisis, although it is just one of many factors that researchers are still working to understand.
When puberty hits, the brain becomes hypersensitive to social and hierarchical information, even as media flood it with opportunities to explore one’s identity and gauge self-worth. Laurence Steinberg, a psychologist at Temple University, said that ability to maturely grapple with the resulting questions — Who am I? Who are my friends? Where do I fit in? — typically lags behind.
The falling age of puberty, he said, has created a “widening gap” between incoming stimulation and what the young brain can process:
“They’re being exposed to this deluge at a much earlier age.”
M’s first hint of trouble came in sixth grade, with challenges focusing in class. The school called a meeting with M’s parents. One teacher suggested testing M for attention deficit hyperactivity disorder, but Linda and Tony were skeptical. The number of A.D.H.D. diagnoses in the United States rose 39 percent from 2003 to 2016 , according to the C.D.C., and M’s parents, both scientists in biomedical fields, were concerned that consulting an A.D.H.D. specialist would tilt the scales toward that diagnosis.
Instead, Linda tried to help M stay organized with an app that parents and students used to track assignments, test scores and grades. M felt put under a microscope.
“She would say, ‘Can you bring me your iPad so we can check Schoology?’” M recalled about Linda. “I would literally have an anxiety attack because I was so scared.”
By the fall of 2019 — seventh grade — M was struggling socially, too. A close friend got popular, while M often came home from school and got into bed. “I felt like a plus one,” M said. “I just wanted to be unconscious.” Other times, M said, “I just sat in my room and cried.”
The behavior seemed alien to Tony, who had lived a different childhood. As an adolescent in Vermont in the 1980s, he fished and played outdoors. By 15, he had his first serious girlfriend; in 1990, the summer before their senior year, he got her pregnant. Their son was born that December, and Tony and the mother shared custody.
Times have changed. Federal research shows that 38 percent of high-school-age teenagers report having had sex at least once, compared with roughly 50 percent in 1990. The teen birthrate has plummeted.
So has cigarette and alcohol use . In 2019, 4 percent of high school seniors reported having a cigarette in the last 30 days, down from 26.5 percent in 1997 . Alcohol use by high schoolers hit 30-year lows at the same time. Use of OxyContin and other illicit drugs among high schoolers is down sharply over the last 20 years. Vaping of both nicotine and marijuana has risen in recent years, although both dropped sharply during the pandemic .

Rates of smoking, drugs, alcohol and sex declined among high school students over the last decade, continuing trends that started over two decades ago.
One notable exception was a rise in excessive smartphone and computer use over the last decade.
Use a smartphone ,
tablet, computer or
game console at least
3 hours a day, not
including school work
Recently drank
Watch television
3 hours a day
Last sex was
unprotected
Get at least
8 hours of sleep
Feelings of sadness and hopelessness rose over the same decade, and suicidal thoughts increased.
Persistently felt
sad or hopeless
Made a suicide plan
Attempted suicide
Injured in a suicide
attempt and needed
medical treatment

Feelings of sadness and hopelessness rose, and suicidal thoughts increased.

Experts cite multiple factors: public awareness campaigns, antismoking laws, parental oversight and a changing social lifestyle that is no longer strictly in-person.
Dr. Nora Volkow, director for the National Institute on Drug Abuse, described drug and alcohol use as “very much of a group dynamic.” She added: “To the extent that kids are not in the same place, one would expect a decrease in the behavior.”
A virtual crush
In the spring of 2020, M retreated further. Bewildered by online classes, M lied about participating, felt guilty and watched YouTube instead, devouring an anime series called “Danganronpa.” It is set in a high school where students learn from the evil headmaster, a bear, that the only way to graduate is to kill a peer.
M became enamored of one of the characters, Genocide Jack (sometimes known as Genocide Jill), who is described on one fan site as a witty “murderous fiend” who “kills handsome men” using scissors.
One night after dinner, M was upstairs and used scissors to cut both ankles. “I was mad at myself for not doing homework,” M said. “I was kind of thinking, ‘Oh, the pain feels good,’ like it was better than being stressed.” M couldn’t recall where the idea came from: “I wanted to hurt myself with anything.”
M’s parents noticed superficial scratches on M’s thighs that resembled cuts but did not raise the subject. Linda worried about the screen time but “it was pandemic,” she said.
When school ended for summer break, M’s mood improved. Over the summer, M discovered the mobile version of the “Danganronpa” video game and how to override the parental screen limits. M played all day.
“I was in front of my screen staring at Jack,” M said. “Then I was playing ‘Trigger Happy Havoc,’ and I was, like, more in love.”
“I was kind of just lonely,” M said. M fantasized about the future with Jack: “I’d want her to almost kill me but not, and then we could spend the rest of our lives together.”
An obsession with a virtual character is not uncommon, experts said. “This is a kid who is a bit lonely, a bit caught up in these narratives,” said Nick Allen, a psychologist at the University of Oregon. “There’s nothing new in coming up with stuff that freaks out their parents.”
Nonetheless, he added, “extremely powerful” online experiences like these can encourage users to think, “That is going to be my identity, my sense of the future, my sense of where I belong socially,” at a time when one’s identity is a work in progress.
Dr. Pluhar of Harvard noted that “the challenge and the progress” of modern adolescence “is there are so many types of identity” — more choices and possibilities, which in turn could be overwhelming. Among the factors shaping mental health, Dr. Pluhar said, is the mind’s churning and obsessing: “Rumination is a big piece of it.”
M had a name for the main source of their mental health challenges: “Loneliness.”
Health experts note that, for all its weight, the adolescent crisis at least is unfolding in a more accepting environment. Mental health issues have shed much of the stigma they carried three decades ago, and parents and adolescents alike are more at ease when discussing the subject among themselves and seeking help.
Indeed, Linda had begun having conversations with other parents who wondered whether the challenges their adolescents were facing represented typical moody teen behavior or something pathological. A colleague told Linda about her daughter’s eating disorder. A mother named Sarah confided that her middle-school-age daughter was in therapy for anxiety and depression. “I told her, ‘I understand where you’re at way better than you think,’” Sarah recalled.
In a nearby suburb, the parents of Elaniv Burnett were struggling to understand their daughter’s desperation. As a young child, Elaniv had been joyful, an eager student and graceful gymnast, her father, Dr. Tatnai Burnett, a gynecological surgeon at the Mayo Clinic, recalled: “The kind of kid where you go, ‘Huh, we should have more kids.’”
But in 2014, when Elaniv was 9, her parents’ marriage began to fracture, and Elaniv injured her ankle; she developed chronic pain, which sidelined her from gymnastics, and she went through a dark period. Then, in 2016, Dr. Burnett, who is Black, was held at gunpoint at home by the police, in full view of the family, after officers responded to a call of a possible intruder.
Recent research has found that wealth, education and opportunity do not shield Black families from mental health issues to the same degree they do for white families. From 1991 to 2017, suicide attempts by Black adolescents rose 73 percent , compared with an 18 percent rise among white adolescents . (The overall suicide rate remains higher among white adolescents.) The suicide rate leaped particularly for Black girls, up 6.6 percent per year on average from 2003 to 2017, new research shows .
In the fall of 2019, Elaniv was diagnosed with major depressive disorder. In a poem in her journal, she wrote: “Thoughts like racecars zoom constant in my head/ Self-hate and worthlessness/ Perpetual, they speed ahead.”
Elaniv began therapy, took medications and enrolled in an outdoor inpatient program in Utah. “We worked on ourselves, worked on our parenting, we changed so many things to try to help meet Elaniv where she was,” Dr. Burnett said. “We controlled electronics, monitored friendships.”
Elaniv’s mother, Tania Gainza, a clinical social worker, saw a generational trend. She had counseled an adolescent for years who was terrified of not meeting expectations. She heard about a local boy who killed himself seemingly without warning.
“There’s something different about this era or generation that makes them much more susceptible or vulnerable,” Ms. Gainza said. “There’s not that community, I guess.”
A rise in loneliness is a key factor, experts said. Recent studies have shown that teenagers in the United States and worldwide increasingly report feeling lonely , even in a period when their internet use has exploded .
“They’re hanging out with friends, but no friends are there,” said Bonnie Nagel, a psychologist at the Oregon Health & Science University. “It’s not the same social connectedness we need and not the kind that prevents one from feeling lonely.”
Often, she said, online social connections amount to seeing “pictures of people hanging out, flaunting it, as if to say, ‘Hey, I’m very socially connected,’ and ‘Hey, look at you by yourself.’”
The pandemic factor
One day in the autumn of 2020, with the pandemic in full swing and eighth grade having gone fully remote, Linda found M sobbing in bed. M confessed to wanting to die.
Linda found an online therapist. After several sessions, “the therapist broke confidentiality,” Linda said. “She said, ‘You need to know about the knife.’”
In M’s night stand, Tony found a pocketknife and a box knife with a cat’s paw image on the handle that M had surreptitiously bought on Amazon and was using to self-harm. One night, M went further, tightening a red hair tie around their neck. “I was trying to see how far I could take it,” M said.
The following February, M entered full-day group therapy. A psychiatrist at the clinic notified the family that M had admitted to being unable to stop cutting, medical records show. Linda “de-knived the house,” she said, and hid all the pills. Then M engaged in a different kind of self-harm: hitting their head with an eight-pound workout barbell.
Linda recalled feeling stunned: “Oh, now I have to get rid of the blunt objects, too.”
M was discharged with a diagnosis of depression and a prescription for antidepressants. From 2015 to 2019, prescriptions for antidepressants rose 38 percent for teenagers compared with 15 percent for adults, according to Express Scripts, a major mail-order pharmacy.
Subsequently, M also received a diagnosis of attention deficit disorder, not A.D.H.D., and given a prescription for methylphenidate, the generic name for medications including Ritalin and Concerta. “I’m still not sure I believe it,” Linda said.
M’s middle school has a trained mental health counselor. In March 2021, M visited him for the first time. During that visit, on a scale of 0 to 10, M ranked hopelessness and anxiety at 9, expressing terror at returning to school, a fear of falling behind and a wish to die.
But M’s mood improved; at a meeting a month later, M ranked hopelessness and sadness at 5 and anxiousness at 2. M felt therapy was crucial but wasn’t sure the medications helped; the school counselor credited M’s improvement to family support and getting back to school. He cautioned the parents, though, that the pendulum could swing back.
Into the forest
Around that time, Linda heard through the grapevine that a girl named Elaniv Burnett had died following an overdose. “I’m sorry, I can’t take it anymore,” Elaniv wrote in a note. Her mother rushed her, still conscious, to the hospital, where Elaniv expressed regret at the overdose and described her terror. She died four days later, at age 15 .
The news was still on Linda’s mind a few weeks later when M fled into the forest.
M’s family had recently returned from visiting both sets of grandparents. One set criticized M’s pronouns, the other M’s heavy screen use. Linda said she felt judged. She stole a look at M’s phone and saw the troubling photos.
“Let’s go for a walk,” she said to M and went upstairs briefly. When she returned, M had vanished, so she followed them into the woods, texting as she frantically looked for flashes of M’s white dress.
Finally M texted back: “I don’t want to talk to you.”
Linda returned home, and Tony went out. He found M along a commonly used trail. They walked, mostly in silence. “Then they were ready to come home,” he recalled.
The school year ended, and M improved, the anxiety ebbing. M took joy spending time with a friend, in person, walking home, strolling the forest.
But a few weeks later, a hurtful text from the friend plunged M into despair again, “like I was back to having no friends.”
M used an exfoliating blade to cut both ankles. “I don’t know how to stop it,” M said. “I can bet $20 that I’ll be in the hospital next year.”
When Linda saw the cuts, she confronted M, who handed over the blade. M let Linda examine the wounds.
“I think that’s good,” Linda said. “They let me look.”
How Matt Richtel spoke to adolescents and their parents for this series
In mid-April, I was speaking to the mother of a suicidal teenager whose struggles I’ve been closely following. I asked how her daughter was doing.
Not well, the mother said: “If we can’t find something drastic to help this kid, this kid will not be here long term.” She started to cry. “It’s out of our hands, it’s out of our control,” she said. “We’re trying everything.”
She added: “It’s like waiting for the end.”
Over nearly 18 months of reporting, I got to know many adolescents and their families and interviewed dozens of doctors, therapists and experts in the science of adolescence. I heard wrenching stories of pain and uncertainty. From the outset, my editors and I discussed how best to handle the identities of people in crisis.
The Times sets a high bar for granting sources anonymity; our stylebook calls it “a last resort” for situations where important information can’t be published any other way. Often, the sources might face a threat to their career or even their safety, whether from a vindictive boss or a hostile government.
In this case, the need for anonymity had a different imperative: to protect the privacy of young, vulnerable adolescents. They have harmed themselves and attempted suicide, and some have threatened to try again. In recounting their stories, we had to be mindful that our first duty was to their safety.
If The Times published the names of these adolescents, they could be easily identified years later. Would that harm their employment opportunities? Would a teen — a legal minor — later regret having exposed his or her identity during a period of pain and struggle? Would seeing the story published amplify ongoing crises?
As a result, some teenagers are identified by first initial only; some of their parents are identified by first name or initial. Over months, I got to know M, J and C, and in Kentucky, I came to know struggling adolescents I identified only by their ages, 12, 13 and 15. In some stories, we did not publish precisely where the families lived.
Everyone I interviewed gave their own consent, and parents were typically present for the interviews with their adolescents. On a few occasions, a parent offered to leave the room, or an adolescent asked for privacy and the parent agreed.
In these articles, I heard grief, confusion and a desperate search for answers. The voices of adolescents and their parents, while shielded by anonymity, deepen an understanding of this mental health crisis.
Matt Richtel is a best-selling author and Pulitzer Prize-winning reporter based in San Francisco. He joined The Times in 2000, and his work has focused on science, technology, business and narrative-driven storytelling around these issues. More about Matt Richtel
Our website uses cookies to offer you the most relevant experience and optimal performance.
By clicking ‘Accept’ you agree to the storing of cookies on your device. Cookie Policies.
- Free Essays
- Article Critique
- Article Review
- Article Writing
- Synopsis Writing
- Book Report
- Book Review
- Business Plan
- Business Report
- Marketing Plan
- Capstone Project
- Dissertation
- Interview Essay
- Grant Proposal
- Literary Analysis
- PhD Dissertation
- Presentation and Poster
- Research Proposal
- Research Paper
- Thesis Proposal
- Thesis Statement
- Essay Questions
- Excel Homework
- Extended Essay IB
- Film Analysis
- Movie Review
- Proofreading
- Reaction Paper
- White Paper
- Questionnaire
- Annotated Bibliography
- VIP Services
- Discussion Board Post
- Depression in Adolescents Psychology Essay Example
- Free Essays Online >
- Psychology Essay Examples >
- Depression in Adolescents Psychology Essay... >
Depression by definition is simply the mood or emotional state manifested by feelings of low self-worth or guilt and a compact incapacity to relish life. It is deemed to be a common issue among many people in our society today. Every human being experiences periods when they face hardships. Stress and mood changes that follow the difficulties fit the emotional state that marks depression. Sadness, pessimism, and hopelessness become naturally incorporated. The resulting mental symptoms include disturbed sleep and slowing of the thinking process or actions. Depression may be caused by genetic factors that are hereditary. Cases of depression vary depending on the individual; however, in order to make the diagnosing of the problem easier, it has been split into many categories. The examples of these are an acute vs. chronic and mild vs. severe depression.
Main Causes of Depression Among the Teenagers
Adolescence is the period of evolution from infancy to maturity, a stage of significant growth and development, in which substantial physiological, cognitive, psychological, and behavioral deviations take place. Adolescence is a phase of delight and anxiety; of happiness and troubles; of discovery and perplexity (Garber, 2006). It seems that the age peak of depression correlates with the peak years of low self-esteem, which is the early and middle adolescence with the peak period between the age of thirteen and fourteen (Garber, 2006). There may rise a question whether low self-esteem is a precursor for depression and other mood disorders, and if a low self-esteem curtails the resilience of the adolescent, thus making him or her more susceptible to depression.
24/7 Support
Have you got any questions?
Experts have analyzed and estimated that 5% of all teenagers suffer from depression. (Abramson, 1988). Only a small part of this portion is well-diagnosed and treated. There are some factors correlated with the depression among adolescents. Some of them include the proper process of maturing and the stress involved in the process: the influence of sex hormones, conflicts at home, and the loss of close friends and family members through death. This paper investigates the causes of depression in teenagers, the treatments taken to diagnose depression and its prevention. Female adolescents display higher levels of depression-related symptoms as compared to males. There are three main forms of treatment for depression: counseling and psychotherapy; electroconvulsive therapy (ECT); and antidepressant medications. The adolescent depression signs and symptoms vary from changes in emotions and behavior (Abramson, 1988). Emotional changes include such feelings as sadness, frustration over small matters, loss of interest, and frequent suicidal thoughts. Behavioral changes include insomnia, appetite changes, alcohol and substance abuse, agitation, and slowed body movements. Other changes may include poor school performance, absence from school, and self-harm such as tattooing excessively and adopting a risky behavior.
When depression symptoms persist, it is advisable to seek medical attention. A good family doctor or pediatrician is to be consulted to assist the teenager. If the depression symptoms are untreated, they continue getting worse day by day, and this may lead to the risk of the adolescent committing suicide (Begley, 2010). The teenagers should approach someone they trust in case they do not feel comfortable sharing their situation with anyone.
The main causes of depression among the teenagers are induced by a variety of factors. These are the changes in the body balance of hormones, early childhood traumas such as physical abuse, the loss of a parent, which may cause brain changes that may trigger depression (Beck T, 2009). Depression could also result from the inherited traits from one’s bloodline. The teenagers may be linked to learning patterns that make them feel helpless. Neurotransmitters in the human brain cells also seem to play a role in depression. When the brain chemicals are out of balance, this may lead to depression (Begley, 2010). According to rational behavior counselors, it is not essentially nerve-wracking events and positions but rather a propensity toward negative understanding of these events that initiates and upholds despair (Calles J. 2007). When a contrary incident befalls, the depressed adolescent often comprehends the reason for the event as something steady, internal, and global. For example, if a young person does not receive good grades at school, he or she may attribute this disappointment to his or her being “stupid.” This cause is steady (unlikely to change), internal (his or her fault), and global (affecting everything he or she does). There is also an indication of the genomic tendency in the causes of adolescent depression as the depressed adolescents often have high rates of depression among their family members (Springer & Beevers, 2011).
Many factors trigger depression in teenagers. Having issues, such as peer problems, academic problems, and obesity, impacts negatively one’s self-esteem. When an individual is a victim or witness of any form of violence, sexual or physical, this may make them susceptible to depression (Richardson, 2005). If a person has chronic illnesses, such as cancer, asthma or diabetes, this individual is at high risk of contracting depression. The gender of an adolescent may also be a leading cause of their depression. If a person is lesbian, gay, bisexual, or transgender, he or she feels isolated in the social setting, thus increasing the risk of depression. Drug abuse and alcohol consumption are also another risk factor for depression. The family history can trigger depression in an individual through things such as having a parent or relative who has depression. Passing through stressful life events, such as the parental divorce or death of the loved one, may also be a trigger for depression (Springer & Beevers, 2011).
Don't waste your time on boring tasks!
Save your time for something pleasant!
Description of Counseling Related to Depression in Adolescents
Depression is one of the most common reasons why people seek therapy sessions from their trusted doctors and counselors. However, the condition is successfully treatable. A trusted therapist is preferred in the treatment of the depressed adolescent as the person is likely to feel shame expressing himself/herself to people. They fear the consequences of disclosing their conditions to their friends, families, and even health care providers (Birmaher, 1998). Various therapeutic approaches have demonstrated to be effective in the treatment of depression. Cognitive behavioral therapy (CBT) is amongst the acclaimed therapies for handling depression. It frequently involves self-help books and sessions with a therapist, but specific methods will depend on the type of depression and concentration of symptoms. The primary purpose of counseling is to help people apprehend their illness and its causes. Counselors will work with clients to unearth and discover the fundamental reasons that have added to symptoms of depression while assisting them in changing their feelings and learning to manage them more efficiently. Counseling is essential in handling low self-esteem, relationship issues, or persistent negative thinking that may be propagating the illness. Many counseling sessions for depression usually comprise 12 to 20 weekly sessions of one or two hours. These are undertaken in the form of one-on-one sessions with a counselor or the kind of group counseling, depending on the circumstances (Mental Health Foundation of Australia,2007).
The other methods include mindfulness, based on the cognitive and psychodynamic therapy. A psychodynamic counselor assists people in assessing emotions, thoughts, early-life experiences, and beliefs to gain awareness of their lives and their present-day problems and appraise the trends that they have developed over time. Identifying repeated patterns helps individuals appreciate the ways in which they dodge distress or develop resistance mechanisms as a method of surviving so that they can take steps to modification of those patterns (Wagner, 2003). The mindfulness-based cognitive therapy happens through an eight-week program of therapy sessions as well as home audio prompts that instill people with the art of mindfulness meditation. People gain an aptitude to realign themselves away from their thoughts and feelings and focus instead on the occurring changes in their body and mind through yoga, breathing, and meditation. In this therapy, the adolescents are instructed to recognize their sense of being and see themselves as separate from their thoughts and moods (Abramson, 1988). Despite the approach used by the counselor, he/she can help a teenager visualize his/her depression state with curiosity and without judgment. This is to comprehend and heal the depression source. Counselors can treat the adolescents mainly by identifying the core source of the depression. The therapy sessions help people be aware of their strengths, willpower, and capacity for change (Birmaher, 1998). Counseling is also used in group therapies and other young support groups. This social group helps the adolescents in the alleviation of the symptoms of isolation and loneliness.

Stages of Depression and Their Implications
At the initial stages, the teenager will behave as usual without any signs of depression. The only symptoms are night dreams and insomnia. During moderate depression, the person continues with the same behavior. However, one can notice that something is happening to the teenager. The person will show the change in reactions and speech tones toward being sarcastic and ironic. Anything that relates to death, illness, and problems often triggers an impulse of emotional response in the individual (Wagner, 2003).
The next stage is the intermediate stage. The neurohormonal and biochemical processes start depression amongst teenagers on a psychological level. The youth will feel socially fenced off from the world, and they stop communicating. They change their moods and attitudes toward everything. The teenagers will put on a mask of gaiety unconsciously to hide their feelings and emotions. The most extreme level of depression is the withdrawal, when the teenagers completely alienate themselves from the rest of the people (Birmaher, 1998). They tend to withdraw from their families and relatives. They become rude and aggressive to anything that comes their way. The condition, if not diagnosed at this point, will lead to mental deterioration, and suicidal thoughts can hit the teenager’s mind. Depression affects the teenagers socially, emotionally, academically, and physically. Depression has always been a problem in adolescents; however, in the past few decades it has grown to a significant percentage. The teenagers’ mental health is affected since childhood, and this has an impact on their mind biology. Adolescents are also affected physically, socially, and spiritually. They tend to lose interest in some of the activities they used to love and experience incidences of weight fluctuations (Mental Health Foundation of Australia,2007). The issues affect the psychosocial behavior that eventually causes deviations, even from the religious beliefs.
Our Benefits
- Deadline Guarantee
- Total Confidentiality
- Great Pricing System
- Plagiarism Free Papers
- VIP Writing Services
- Free Revision on Demand
Treatment of Depression
Many types of treatment are available. A doctor can sometimes prescribe medications that will help relieve the depression symptoms. It is recommendable that teenagers see a psychiatrist or psychologist or any other psychological counselor. The combination of counseling and medications are very useful for treatment and diagnosis of depression in teenagers (Springer & Beevers, 2011). Numerous classes of drugs are designed to minimize the symptoms of depression. The medical drugs used comprise Selective serotonin reuptake inhibitors, Selective Serotonin and Norepinephrine Reuptake Inhibitors, and Tricyclic Antidepressants among others. The SSRIs are the most prescribed antidepressants. They are preferred as they have fewer side effects than other medications. The drugs work on neurotransmitter serotonin that is associated with mood regulation. The drugs help prevent the body from absorbing serotonin. The most common side effects of the drugs are nausea, diarrhea, headache, and sexual problems. SNRIs also avoid the re-absorption of serotonin and norepinephrine that help in mood regulation. The side effects are constipation, nausea, insomnia, vomiting, anxiety, and headache. TCAs work on serotonin, norepinephrine, and dopamine. The side effects are diverse. They include weight gain, sexual dysfunction, dry mouth, dizziness, constipation, and sleepiness (Begley & Kliff, 2010).
Exercise is another substitute to using antidepressants. Injuries are the most common side effect of exercise. However, according to Richard Lee (2010), combining different weight bearing activities with weight training reduces the risk of injury from repetitive stresses on particular joints and muscles. The parents can come to rescue of the depressed teenagers. They should take the time to understand and listen to their problems. They should keep the communication lines open for the teenagers.
Education would be of value to both parents and teachers and aid them in ascertaining the depression “indicators” and not taking for granted that it is just another “teenage phase.” This would allow for timely diagnosis and several treatment choices to be considered. It is the age when teenagers have a tendency to resort to the world of social media and the Internet, and interactions with parents are narrowed to the bare necessities. Yet, their stress with school work, peer pressure, and other challenges do not diminish, which probably only adds to the possible causes for the onset of depression. Once depression has been diagnosed, treatment options need to be carefully assessed as there are very real suicide risks associated with antidepressant use in adolescents.
Why not to check your price right now?
Related essays:.
- The Speed of Our Life Essay Example
- Effects of Long Hours Flight on Aircrew Essay Sample
- Psychological Aspects of Organ Donation and Transplant Essay Sample
- Wilhelm Wundt and Experimental Psychology Essay Example
- Bipolar Disorder Psychology Essay Example
How to make peace with academic deadlines?
Use our writing service!

Join our Affiliate Program today and receive a Comission from Your Friend’s Orders!
- Questions Answers
- Presentation/Poster
- Research Papers
- Term Papers
on your first order
code: prime15
- Business essays
- history essays
- literature essays
- management essays
- medicine essays
- psychology essays
- Open access
- Published: 02 October 2020
Depression in adolescence: a review
- Diogo Beirão ORCID: orcid.org/0000-0001-5612-8941 1 ,
- Helena Monte 1 ,
- Marta Amaral 1 ,
- Alice Longras 1 ,
- Carla Matos 1 , 2 &
- Francisca Villas-Boas 1
Middle East Current Psychiatry volume 27 , Article number: 50 ( 2020 ) Cite this article
48k Accesses
15 Citations
13 Altmetric
Metrics details
Depression is a common mental health disease, especially in mid to late adolescence that, due to its particularities, is a challenge and requires an effective diagnosis. Primary care providers are often the first line of contact for adolescents, being crucial in identifying and managing this pathology. Besides, several entities also recommend screening for depression on this period. Thus, the main purpose of this article is to review the scientific data regarding screening, diagnosis and management of depression in adolescence, mainly on primary care settings.
Comprehension of the pathogenesis of depression in adolescents is a challenging task, with both environmental and genetic factors being associated to its development. Although there are some screening tests and diagnostic criteria, its clinical manifestations are wide, making its diagnosis a huge challenge. Besides, it can be mistakenly diagnosed with other psychiatric disorders, making necessary to roll-out several differential diagnoses. Treatment options can include psychotherapy (cognitive behavioural therapy and interpersonal therapy) and/or pharmacotherapy (mainly fluoxetine), depending on severity, associated risk factors and available resources. In any case, treatment must include psychoeducation, supportive approach and family involvement. Preventive programs play an important role not only in reducing the prevalence of this condition but also in improving the health of populations.
Depression in adolescence is a relevant condition to the medical community, due to its uncertain clinical course and underdiagnosis worldwide. General practitioners can provide early identification, treatment initiation and referral to mental health specialists when necessary.
Adolescence is an important period in developing knowledge and skills, learning how to manage emotions and relationships and acquiring attributes and abilities for adulthood. Depression in adolescence is a common mental health disease with a prevalence of 4–5% in mid to late adolescence [ 1 ]. It is a major risk factor for suicide and can also lead to social and educational impairments. Consequently, identifying and treating this disorder is crucial.
General practitioners and primary care providers are frequently the first line of contact for adolescents in times of distress and can be crucial to identify mental health issues amongst these patients. They can facilitate early identification of depression, initiate treatment and refer the adolescents for mental health specialists [ 2 ]. It is vital to make a timely and accurate diagnosis of depression in adolescence and a correct differential diagnosis from other psychiatric disorders, due to the recurrent nature of this condition and its association with poor academic performance, functional impairment and problematic relationships with parents, siblings and peers. Furthermore, depression at this age is strongly related to suicidal ideation and attempts [ 2 ].
The US Preventive Services Task Force (USPSTF) recommends screening adolescents for depressive disorder by the General Practitioners [ 2 , 3 ]. Guidelines from the American Academy of Pediatrics (AAP) state that adolescent patients should be screened annually for depression in Primary Care with a formal self-report screening tool [ 4 ]. AAP recommends that Primary Care clinicians should evaluate for depression in those who screen positive on the screening tool, in those who present with any emotional problem as the chief complaint and in those in whom depression is highly suspected despite a negative screen result [ 4 ].
The present work consists of a review on the depression in the adolescent, summarizing data published in scientific papers in the last years, regarding the epidemiology of the disease, its pathogenesis and risk factors, screening and diagnosis tools and its management and treatment. Our research focused on research papers published between January 2010 and March 2020 in the area. Other research papers not included in this first search were included due to their interest and value to the subject. The keywords, used in different permutations and combinations, included the following: depression, adolescence, overview, pathophysiology, diagnosis and treatment.
Epidemiology
The prevalence of depression is significantly linked to age, being low in children (< 1%) and increasing throughout childhood and adolescence. Nevertheless, the prevalence of depression in adolescence varies significantly between studies and reports. A reported prevalence in Great Britain was 4%, whereas in the USA was 2.1% and in France was 11.0% [ 5 , 6 , 7 ]. Nevertheless, a systematic review from 2013 stated the life prevalence of depression varies from 1.1 to 14.6% [ 8 ].
A possible factor for the reported increase during adolescence is the set of social and biological changes characteristic of post-pubertal phase, such as enhanced social understanding and self-awareness, brain circuits changes involved in responses to reward and danger and increased reported stress levels [ 9 , 10 , 11 ].
Regarding differences between genders, while no significant differences are found in depression during childhood, depression during adolescence has a strong female preponderance, similar to adulthood [ 12 , 13 , 14 ]. This difference is still observed between distinct epidemiological and clinical samples and across various methods of assessment. As such, it is unlikely due to differences in help-seeking or reporting of symptoms and more closely tied to female hormonal changes, which suggests a direct link to hormone-brain relations [ 15 ].
Pathogenesis
Comprehension of the pathogenesis of depression in adolescents is a challenging task, due to its heterogeneous clinical presentation and diverse causes.
Putative risk factors, potentially modifiable during adolescence without professional intervention, are substance use (alcohol, cannabis and other illicit drugs, tobacco), diet and weight [ 16 ].
Alcohol use is known to have neurotoxic effects during this developmentally sensitive period. Cannabis and other illicit drugs can have an impact on serotonin and other neurotransmitters causing an increase in depressive symptoms. Furthermore, alcohol, cannabis and other illicit drug use have various deleterious social and academic consequences for the adolescent which could increase their risk for depression [ 16 ].
The relationship between tobacco use and depression is unclear. However, it has been proposed that this linkage may arise from the effects of nicotine on neurotransmitter activity in the brain, causing changes to neurotransmitter activity [ 17 ]. Overweight can have a negative impact on self-image which elevates the risk for depression. Moreover, depressed people may lead a less healthy lifestyle and suffer from deregulation in the stress response system, which may contribute to weight gain [ 16 ].
Association between depression and environmental factors, such as exposures to acute stressful events (personal injury, bereavement) and chronic adversity (maltreatment, family discord, bullying by peers, poverty, physical illness), has been subject of papers. Stressful life events seem more strongly associated with first onset rather than recurrence, and risk is considerably greater in girls and in adolescents who have multiple negative life events. The most important factors are chronic and severe relationship stressors [ 18 ]. A significant interaction was found between exposure to maternal threatening behaviours and deficits in emotional clarity in relation to depressive symptom severity [ 19 ].
Genetic factors can also play a very important role in the pathogenesis. Many reports suggest that a variant (5-HTTLPR) in the serotonin transporter gene might increase the risk of depression, but only in the presence of adverse life stressors or early maltreatment. The findings are less robust in adolescent boys than girls. This gene variant has also been reported to affect fear-related and danger-related brain circuitry, which is altered in depression. However, such findings seem to vary not only by genotype but also by age, sex, and severity of symptoms, and are also reliant on good quality measures of adversity and depression [ 18 , 20 ].
Two interrelated neural circuits and associated modulatory systems have been closely linked to risk for depression. One circuit connects the amygdala to the hippocampus and ventral expanses of the prefrontal cortex (PFC) and is linked to hypothalamic-pituitary-adrenal (HPA) axis activity. Disruption of this circuit links depression to stress-related enhancements in HPA-stress systems, such as higher than expected cortisol concentrations, and activity in the serotonergic system. Psychosocial stress, sex hormones and development have also been linked to changing activity in this circuit, with evidence that this circuit matures after adolescence. High concentrations of sex steroid receptors have been identified within this circuit and might provide a biological mechanism for why girls have higher risk of depression than boys. The other key circuit implicated in depression encompasses the striatum and its connection to both the PFC and ventral dopamine-based systems. Like the first circuit, this one also continues to mature through adolescence. Sex differences emerge in both circuits. Research into this reward circuit implies that reduced activity is linked with expression of and risk for depression. Reduced striatal and PFC activity during tasks involving rewards has been recorded both in individuals with major depression and in those with depressed parents. Both inherited factors and stress-related perturbations seem to contribute to these changes [ 18 , 21 ].
Temperament and character traits are also important factors in the pathogenesis of depression in adolescence. According to Cloninger, temperament is responsible for automatic and emotional responses to environmental stimuli and encompasses four dimensions: novelty seeking, exploratory activity, harm avoidance, reward dependence and persistence [ 22 ]. In contrast, character develops across the lifespan and is influenced by social and cultural experiences. Three dimensions are distinguished: self-directedness, cooperativeness and self-transcendence [ 23 ]. Studies showed that depressed patients present higher novelty seeking, harm avoidance and lower reward dependence, persistence, self-directedness and cooperativeness compared to healthy individuals [ 23 , 24 ].
Primary care providers are frequently the first contact during times of distress and can be crucial to identify mental health issues allowing for an earlier depression diagnosis, treatment and referral [ 2 ].
The symptoms can differ from the adult population. In comparison to it, adolescents tend to have more frequently somatic symptoms, anxiety, disruptive behaviour and personality disorders [ 25 ].
The fact that these symptoms are common in other disorders such as hypothyroidism, anaemia, sleep apnoea or other chronic diseases makes the diagnosis more challenging to establish in these subjects [ 26 ].
Screening tools
The screening of adolescents for depression is an essential tool for early detection of this disorder. USPSTF and AAP recommend the screening of adolescents in primary care settings [ 2 , 3 , 4 , 25 , 26 , 27 ].
The Beck Depression Inventory (BDI) and Patient Health Questionnaire for Adolescents (PHQ-A) are the most commonly used, outperforming other screening tools in the identification of major depressive disorder among adolescents [ 2 , 28 ].
Originally developed as a depression symptom rating scale for the adult population, BDI is widely used among adults and adolescents and mainly in research. It is a 21-item self-report measure of depressive symptoms, scored from “0” to “3”. Participants are asked to respond to each item based on their experiences within the past 2 weeks. The total score can range from 0 to 63, with higher scores meaning higher levels of depressive symptoms [ 29 ]. In primary care settings, an adapted version (BDI-PC) is often used, which consists of a 7-item self-report instrument, with a cut-off of 4 points for major depression [ 30 ]. Good performance has also been shown using BDI, with sensitivity ranging from 84 to 90% and specificity ranging from 81 to 86% [ 3 ].
The PHQ-A is the depression module of a 67-item questionnaire that can be used to screen for depression among adolescent primary care patients. Composed of 9 questions, it can be entirely self-administered by the patient and evaluates symptoms experienced in the 2 weeks prior. It measures functional impairment and inquiries about suicidal ideation and suicide attempts [ 31 ]. The PHQ-A study had the highest positive predictive value, as well as a sensitivity and specificity of 73% and 94%, respectively [ 3 ].
Diagnostic tools
Diagnosis of depression in adolescents is established through the criteria described in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) [ 32 ]. The evaluation of patients should be made through interviews, alone and with the patient’s family and/or caregivers and should include an assessment of functional impairment in different domains and other existing psychiatric conditions [ 4 ].
DSM-5 establishes the diagnosis of major depressive disorder as a period of at least 2 weeks during which there is a depressed mood or the loss of interest or pleasure in nearly all activities, and, additionally, at least four additional symptoms from a list that includes changes in weight, sleep disturbances, changes in psychomotor activity, fatigue, feelings of worthlessness or guilt, impaired concentration or ability to make decisions, or suicidal ideation. Additionally, it states that, in adolescents, depressed mood can be replaced by irritability or crankiness, a sign that can be neglected during assessment or by caregivers. This presentation should be differentiated from a pattern of irritability when frustrated [ 33 ]. Children diagnosed with disruptive mood dysregulation disorder, a new diagnosis referring persistent irritability and frequent episodes of extreme behaviour, typically develop unipolar depressive or anxiety disorders as they mature into adolescence [ 32 ]. Clinical presentation differs between genders, with female adolescents reporting feelings of sadness, loneliness, irritability, pessimism, self-hatred and eating disorders, while males present with somatic complaints, reduced ability to think or concentrate, lacking decision making skills, restlessness and anhedonia [ 34 , 35 ].
The severity of depressive disorders can be based on symptom count or intensity, and/or level of impairment. Mild depression can be defined as 5 to 6 symptoms that are mild in severity, with mild impairment in functioning. Severe depression exists when a patient experiences all depressive symptoms listed in the DSM-5 or severe impairment in functioning and, also, with at least 5 criteria and a specific suicide plan, clear intent or recent suicide attempt, psychotic symptoms or family history of first-degree relatives with bipolar disorder. Moderate depression falls between these two categories [ 4 ].
Differential diagnosis
Despite its well-defined diagnostic criteria, depression during adolescence can often be misdiagnosed, with the main differential diagnoses being adjustment disorder, dysthymic disorder, bipolar disorder and schizophrenia. However, it is crucial to establish the correct diagnosis as different psychiatric disorders involve distinct treatment and prognosis.
Adjustment disorder is classified as depressed mood in response to an identifiable psychosocial stressor. It arises within 3 months of the onset of a stressor and persists up to 6 months after stressor resolution. It is characterized by low mood, tearfulness, or hopelessness associated with a significant distress that exceeds what would be expected given the nature of the stressor, or impaired social or occupational functioning. On the other hand, dysthymic disorder is a pattern of chronic symptoms of depression that are present for most of the time on most days with a minimum duration of 1 year for children and adolescents [ 32 ].
Bipolar disorder and schizophrenia are much less common in adolescents compared to depression disorder. However, they have different prognosis and require different treatments. Consequently, when establishing the diagnosis of depressive disorder in adolescence, it is important to bear in mind that the first symptomatic episode may also represent the beginning of a bipolar disorder [ 36 , 37 ].
Management and treatment
The treatment of depression in adolescence can include psychotherapy, pharmacotherapy or both [ 38 ]. Treatment should be selected based on the severity of the condition, the preference of the patient/family, associated risk factors, family support and the availability of each therapy [ 39 , 40 ]. On first approach, it is essential to comprehensively explain the therapeutic strategy and involve both patients and family members to assure close follow-up of progress, treatment adjustment according to symptoms and prevention of relapse [ 41 ]. Adolescents with moderate to severe depression, substance abuse, psychiatric disorders, suicidal ideation or resistance to treatment should be referred for specialized evaluation [ 42 ].
Treatment may be divided into three phases: acute (obtain response and remission), continuation (consolidate the response) and maintenance (avoid recurrences) [ 39 ]. Each of them must include psychoeducation, supportive approach and family involvement [ 39 , 40 ].
In mild depression, psychotherapy may be the first option, complemented with pharmacotherapy if there is no response [ 42 , 43 ]. The AAP recommends starting with active support, symptom monitoring and close follow-up for 6–8 weeks [ 44 ]. These measures are also useful when patients refuse more interventional treatments. The National Institute for Health and Care Excellence (NICE) has a slightly stricter approach, in which it recommends psychotherapy after absence of improvement after 2 weeks of watchful waiting [ 45 ]. In adolescents with moderate to severe depression, treatment is based on combined psychotherapy and pharmacotherapy [ 42 , 43 ]. NICE recommends psychotherapy for the minimum of 3 months, followed by fluoxetine if necessary. AAP has a similar approach [ 44 , 45 ]. Other strategies such as physical exercise, sleep hygiene and adequate nutrition have been referred as treatment adjuvants [ 44 , 46 , 47 ].
Both NICE and AAP recommend treatment for at least 6 months after remission of symptoms to consolidate the response and prevent relapse (continuation phase). In addition, both organizations also recommend maintaining follow-up during 1 year or, in cases of recurrent depression, 2 years [ 44 , 45 ].
Psychotherapy
In this area, Cognitive Behavioural Therapy (CBT) and Interpersonal Therapy (IPT) have shown effectiveness [ 40 , 48 ].
CBT is a brief psychotherapy, carried out individually or in groups, based on the relationship between thoughts, feelings and behaviours [ 40 ]. CBT focuses on cognitive distortions associated with depressive mood and the development of behavioural activation techniques, coping strategies and problem solving [ 42 ]. When used in acute depression, it has been shown to have a moderate effect [ 40 ]. CBT seems to be useful in preventing relapses and suicidal ideation, in the treatment of resistant depression and in adolescents with long-term physical conditions [ 49 , 50 , 51 ]. Moreover, the combination of psychotherapy and pharmacotherapy, in particular fluoxetine, has shown promising results [ 52 ]. Within the different psychotherapy approaches, behavioural activation, challenging thoughts and involvement of caregivers have a higher success rate [ 53 ].
IPT assumes depression association with disruptive relationships, based on the negative impact of symptoms on interpersonal relationships and vice-versa [ 40 ]. This approach may be useful especially when there is a well-established relational factor as the cause of the depressive condition [ 54 ]. Most studies have compared only IPT with placebo groups or with other psychotherapy, showing favourable results for IPT [ 48 , 55 ].
Psychotherapy should be considered first line of treatment in adolescents afraid of or with contraindications for medication, with identified stress factors or those with poor response to other approaches [ 56 ]. There are no contraindications to psychotherapy, though it has a limited effect in cases of cognitive delay [ 40 ].
Pharmacotherapy
Even though psychotherapy is an important component, pharmacotherapy can be used as an addition. When psychotherapy is not available or cannot be applied, pharmacotherapy can be an alternative [ 39 , 41 ].
Fluoxetine is widely regarded as the first-line drug for this age group given its efficacy [ 2 , 38 , 57 , 58 , 59 ]. Besides fluoxetine, escitalopram has also shown to be particularly effective, especially for ages between 12 and 17 years [ 38 , 60 , 61 , 62 ]. The main side effects of selective serotonin receptor inhibitors (SSRIs) include abdominal pain, agitation, jitteriness, restlessness, diarrhoea, headache, nausea and changes in sleep patterns. However, these effects are dose dependent and tend to decrease over time [ 39 ].
Given the efficacy of fluoxetine and escitalopram, many studies have focused on other SSRIs, such as sertraline, citalopram, paroxetine and fluvoxamine. Citalopram must be carefully evaluated as side effects include prolongation of the QT interval, which can lead to arrhythmia [ 63 , 64 ]. Paroxetine and fluvoxamine are not commonly used due to a lack of efficacy in this age group [ 65 , 66 ]. Regarding serotonin noradrenaline receptor inhibitors (SNRIs), venlafaxine appears to have a similar efficacy to SSRIs in resistant depression and no significant differences in adverse effects [ 49 ]. However, because hypertension is a possible side effect, this parameter must be periodically evaluated [ 41 , 64 ]. In Table 1 , the main drugs used in the treatment of depression in adolescents are displayed.
Bupropion and duloxetine have also been studied as alternatives but the evidence of its use in adolescents is limited. Bupropion can be useful in the treatment of overweight patients or those who intend to quit smoking. The main side effects are insomnia, agitation and seizures [ 41 ]. Bupropion is contraindicated in patients suffering from eating disorders. Duloxetine can be used for comorbid depression and pain in adolescents [ 67 ].
Tricyclic antidepressants do not have any demonstrated benefit in the treatment of depression in adolescents [ 42 , 68 , 69 ]. This drug class has significant side effects such as dry mouth, orthostatic hypotension, tremors and vertigo and can increase PR interval and QRS duration. Moreover, it is highly lethal in overdose [ 69 ].
At the time of writing, only fluoxetine (ages 8 years and older) and escitalopram (ages 12 years and older) are approved by the Food and Drug Administration for the treatment of depression in children and adolescents [ 70 , 71 ].
Several studies suggest an association between antidepressants and increased suicidal risk [ 18 , 58 ]. However, the risks and benefits of this strategy should be evaluated. Adolescents should be closely monitored, and, if suicidal thoughts arise during treatment, parents should seek care as soon as possible, to adjust dosage, change antidepressant or discontinue it [ 42 ].
Finally, the treatment strategies proposed in this age group are illustrated in Fig. 1 .
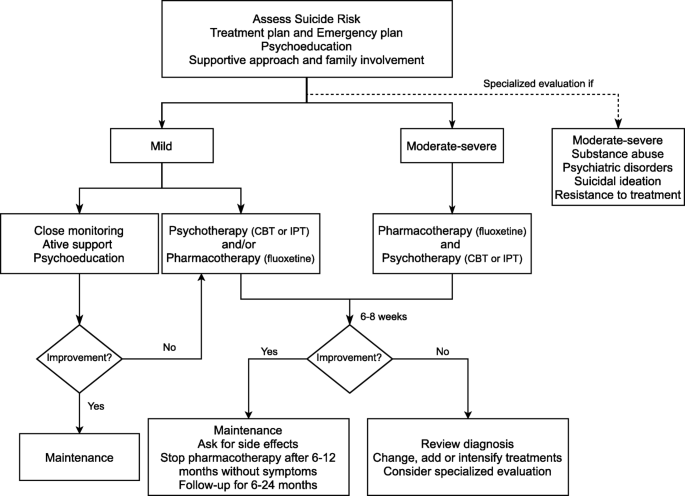
Algorithm for the management and treatment of depression in adolescents
Prevention is crucial to depression management, consequence of the impact on the population and inequal quality health care access [ 72 ]. In addition, it prevents the onset of other possible comorbidities, as well as reduces the impact on the patient and their families [ 73 , 74 , 75 ].
It is important to understand which different risk factors and protective factors intervene in the development of the disease. The risk factors can be divided into specific and non-specific for depression. Regarding the specific ones, parent depression history increases the risk between 2 and 4 times [ 76 ]. Among the non-specific, poverty, domestic violence and child abuse also increase the risk. On the other hand, protective factors are good family support, emotional skills or coping ability [ 77 ].
Depression prevention can be divided into 3 types: universal, selective and indicated. Universal interventions target the adolescent population group in general. Selective interventions target adolescents who are at risk for developing depression. Finally, indicated interventions target adolescents with subclinical symptoms of depression [ 78 ].
With regard to universal interventions, the efficacy of prevention programs through therapy for problem solving and overcoming traumatic situations has been demonstrated in multiple studies [ 79 , 80 ]. Although it has been shown that adolescents under these programs experience decreased depressive symptoms, the long-term usefulness of these programs was not unanimous. The inclusion of parents to these programs provided no additional advantage [ 81 ]. Furthermore, no significant difference between adolescents who received an intervention program and those who did not was found, although improvements in school environment were reported [ 82 ].
Concerning selective interventions, interpersonal communication skills and optimistic thinking programs have shown to be effective in decreasing anxiety and depression [ 83 ]. Contrary to universal interventions, the inclusion of parents in programs was demonstrated as beneficial [ 83 , 84 , 85 ]. However, it had no benefit to adolescents, but improved the parents’ perception of children’s behaviour [ 86 ].
Finally, in indicated interventions, psychoeducation and skill development programs to overcome interpersonal issues and role disputes among adolescents have been carried out [ 87 , 88 ]. It was shown that symptoms improved significantly compared at the end of the program [ 87 ]. Additionally, the number of adolescents with suicidal ideations decreased.
Comparing different groups of programs, various meta-analyses have found that selective and indicated programs are more effective than universal ones [ 89 , 90 ]. These prevention programs are more effective when started between the ages of 11 and 15 [ 78 ]. However, their superiority is not unanimous [ 91 ].
Depression in adolescence can be a complex diagnosis and requires individual and oriented treatment. For this reason, early identification, treatment initiation and prompt referral to mental health specialists is crucial for the prognosis of these patients.
Due to the variety of its main clinical manifestations and the lack of diagnostic tests that fully and accurately establish the definite diagnosis, this process can be particularly challenging. Additionally, several differential diagnoses must be made to provide an accurate course of treatment.
Treatment options can include both psychotherapy (CBT or IPT) and pharmacotherapy. The most promising results are observed with the combination of psychotherapy and pharmacotherapy, mainly fluoxetine.
Nevertheless, the authors would like to highlight certain aspects that require improvement and implementation in daily practice in comparison with the presented recommendations in this publication. First, although Cognitive Behavioral Therapy is one of the most studied therapeutic orientations, the reproducibility of performance among professionals is limited and relies on the relationship established between the mental health professional and the patient, in a deeper way compared to pharmacotherapy. The scarce number of professionals and the absence of choice by the user may not allow the development of this interpersonal bond. This limitation is particularly important in the case of children and adolescents, who are in a period of transition in their physical and mental development, and whose psychological intervention can have a significant positive or negative impact with potential future repercussions. Second, most of the prevention programs described in the literature are not currently implemented. Finally, approaching the family environment is essential in the implementation of effective long-term therapeutic interventions, especially in the presence of a dysfunctional structure. Although recommended, its practical application is often difficult due to the need of active participation of family members, inside and outside the clinical office. Prevention, early diagnosis and treatment of depression in adolescence should be considered worldwide objectives, and the implementation of straightforward, effective and cost-conscious strategies for achieving such purposes is essential. Amongst these objectives, prevention is of utter importance and must be a priority when defining political strategies and governmental programs related to mental health.
Availability of data and materials
Not applicable.
Abbreviations
US Preventive Services Task Force
American Academy of Pediatrics
Prefrontal cortex
Hypothalamic-pituitary-adrenal
Beck Depression Inventory
Patient Health Questionnaire for Adolescents
Beck Depression Inventory for Primary Care
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
Cognitive Behavioral Therapy
Interpersonal Therapy
Selective Serotonin Reuptake Inhibitors
Costello EJ, Egger H, Angold A (2005) 10-year research update review: the epidemiology of child and adolescent psychiatric disorders: I. Methods and public health burden. J Am Acad Child Adolesc Psychiatry 44(10):972–986. https://doi.org/10.1097/01.chi.0000172552.41596.6f
Article PubMed Google Scholar
Forman-Hoffman V, McClure E, McKeeman J, Wood CT, Middleton JC, Skinner AC, Perrin EM, Viswanathan M (2016) Screening for major depressive disorder in children and adolescents: a systematic review for the US preventive services task force. Ann Intern Med 164(5):342. https://doi.org/10.7326/m15-2259
Siu AL, USPSTF (2016) Screening for depression in children and adolescents: US preventive services task force recommendation statement. Pediatrics 137(3). https://doi.org/10.1542/peds.2015-4467
Zuckerbrot RA, Cheung A, Jensen PS, Stein REK, Laraque D (2018) Guidelines for adolescent depression in primary care (GLAD-PC): part I - practice preparation, identification, assessment, and initial management. Pediatrics 141 (3):pii:e20174081. https://doi.org/10.1542/peds.2017-4081
Costello EJ, Foley DL, Angold A (2006) 10-year research update review: the epidemiology of child and adolescent psychiatric disorders: II. Developmental epidemiology. J Am Acad Child Adolesc Psychiatry 45(1):8–25. https://doi.org/10.1097/01.chi.0000184929.41423.c0
Green H, McGinnity A, Meltzer H, Ford T, Goodman R (2005) Mental health of children and young people in Great Britain, 2004. Palgrave Macmillan, Hampshire
Book Google Scholar
Perou R, Bitsko RH, Blumberg SJ, Pastor P, Ghandour RM, Gfroerer JC, Hedden SL, Crosby AE, Visser SN, Schieve LA, Parks SE, Hall JE, Brody D, Simile CM, Thompson WW, Baio J, Avenevoli S, Kogan MD, Huang LN (2013) Mental health surveillance among children - United States, 2005-2011. MMWR Suppl 62(2):1–35
PubMed Google Scholar
Wesselhoeft R, Sorensen MJ, Heiervang ER, Bilenberg N (2013) Subthreshold depression in children and adolescents - a systematic review. J Affect Disord 151(1):7–22. https://doi.org/10.1016/j.jad.2013.06.010
Blakemore SJ (2008) The social brain in adolescence. Nat Rev Neurosci 9(4):267–277. https://doi.org/10.1038/nrn2353
Article CAS PubMed Google Scholar
Nelson EE, Leibenluft E, McClure EB, Pine DS (2005) The social re-orientation of adolescence: a neuroscience perspective on the process and its relation to psychopathology. Psychol Med 35(2):163–174. https://doi.org/10.1017/s0033291704003915
Patton GC, Viner R (2007) Pubertal transitions in health. Lancet 369(9567):1130–1139. https://doi.org/10.1016/s0140-6736(07)60366-3
Avenevoli S, Swendsen J, He JP, Burstein M, Merikangas KR (2015) Major depression in the national comorbidity survey-adolescent supplement: prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry 54 (1):37-44.e32. https://doi.org/10.1016/j.jaac.2014.10.010
Hyde JS, Mezulis AH, Abramson LY (2008) The ABCs of depression: integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychol Rev 115(2):291–313. https://doi.org/10.1037/0033-295x.115.2.291
Seedat S, Scott KM, Angermeyer MC, Berglund P, Bromet EJ, Brugha TS, Demyttenaere K, de Girolamo G, Haro JM, Jin R, Karam EG, Kovess-Masfety V, Levinson D, Medina Mora ME, Ono Y, Ormel J, Pennell BE, Posada-Villa J, Sampson NA, Williams D, Kessler RC (2009) Cross-national associations between gender and mental disorders in the world health organization world mental health surveys. Arch Gen Psychiatry 66(7):785–795. https://doi.org/10.1001/archgenpsychiatry.2009.36
Article PubMed PubMed Central Google Scholar
Angold A, Costello EJ, Erkanli A, Worthman CM (1999) Pubertal changes in hormone levels and depression in girls. Psychol Med 29(5):1043–1053. https://doi.org/10.1017/s0033291799008946
Cairns KE, Yap MB, Pilkington PD, Jorm AF (2014) Risk and protective factors for depression that adolescents can modify: a systematic review and meta-analysis of longitudinal studies. J Affect Disord 169:61–75. https://doi.org/10.1016/j.jad.2014.08.006
Boden JM, Fergusson DM, Horwood LJ (2010) Cigarette smoking and depression: tests of causal linkages using a longitudinal birth cohort. Br J Psychiatry 196(6):440–446. https://doi.org/10.1192/bjp.bp.109.065912
Thapar A, Collishaw S, Pine DS, Thapar AK (2012) Depression in adolescence. Lancet 379(9820):1056–1067. https://doi.org/10.1016/S0140-6736(11)60871-4
Trent ES, Viana AG, Raines EM, Woodward EC, Storch EA, Zvolensky MJ (2019) Parental threats and adolescent depression: the role of emotion dysregulation. Psychiatry Res 276:18–24. https://doi.org/10.1016/j.psychres.2019.04.009
Risch N, Herrell R, Lehner T, Liang KY, Eaves L, Hoh J, Griem A, Kovacs M, Ott J, Merikangas KR (2009) Interaction between the serotonin transporter gene (5-HTTLPR), stressful life events, and risk of depression: a meta-analysis. JAMA 301(23):2462–2471. https://doi.org/10.1001/jama.2009.878
Article CAS PubMed PubMed Central Google Scholar
Forbes EE, Dahl RE (2005) Neural systems of positive affect: relevance to understanding child and adolescent depression? Dev Psychopathol 17(3):827–850. https://doi.org/10.1017/s095457940505039x
Cloninger CR, Svrakic DM, Przybeck TR (1993) A psychobiological model of temperament and character. Arch Gen Psychiatry 50(12):975–990. https://doi.org/10.1001/archpsyc.1993.01820240059008
Nogueira BS, Fraguas R Júnior, Benseñor IM, Lotufo PA, Brunoni AR (2017) Temperament and character traits in major depressive disorder: a case control study. Sao Paulo Med J 135 (5)469-74. https://doi.org/10.1590/1516-3180.2017.0063250517
Zappitelli MC, Bordin IA, Hatch JP, Caetano SC, Zunta-Soares G, Olvera RL, Soares JC (2013) Temperament and character traits in children and adolescents with major depressive disorder: a case-control study. Compr Psychiatry 54(4):346–353. https://doi.org/10.1016/j.comppsych.2012.10.009
Nardi B, Francesconi G, Catena-Dell'Osso M, Bellantuono C (2013) Adolescent depression: clinical features and therapeutic strategies. Eur Rev Med Pharmacol Sci 17(11):1546–1551
CAS PubMed Google Scholar
Bilello JA (2016) Seeking an objective diagnosis of depression. Biomark Med 10(8):861–875. https://doi.org/10.2217/bmm-2016-0076
Mäki M, Mustalahti K, Kokkonen J, Kulmala P, Haapalahti M, Karttunen T, Ilonen J, Laurila K, Dahlbom I, Hansson T, Höpfl P, Knip M (2003) Prevalence of Celiac disease among children in Finland. N Engl J Med 348(25):2517–2524. https://doi.org/10.1056/NEJMoa021687
Maurer DM, Raymond TJ, Davis BN (2018) Depression: screening and diagnosis. Am Fam Physician 98(8):508–515
Stockings E, Degenhardt L, Lee YY, Mihalopoulos C, Liu A, Hobbs M, Patton G (2015) Symptom screening scales for detecting major depressive disorder in children and adolescents: a systematic review and meta-analysis of reliability, validity and diagnostic utility. J Affect Disord 174:447–463. https://doi.org/10.1016/j.jad.2014.11.061
Beck AT, Guth D, Steer RA, Ball R (1997) Screening for major depression disorders in medical inpatients with the beck depression inventory for primary care. Behav Res Ther 35(8):785–791. https://doi.org/10.1016/s0005-7967(97)00025-9
Johnson JG, Harris ES, Spitzer RL, Williams JBW (2002) The patient health questionnaire for adolescents: validation of an instrument for the assessment of mental disorders among adolescent primary care patients. J Adolesc Health 30(3):196–204. https://doi.org/10.1016/s1054-139x(01)00333-0
American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 5th edition: DSM-5 (2013). 5th edn. American Psychiatric Publishing, Arlington.
Orchard F, Pass L, Marshall T, Reynolds S (2017) Clinical characteristics of adolescents referred for treatment of depressive disorders. Child Adolesc Ment Health 22(2):61–68. https://doi.org/10.1111/camh.12178
Kovacs M, Obrosky DS, Sherrill J (2003) Developmental changes in the phenomenology of depression in girls compared to boys from childhood onward. J Affect Disord 74(1):33–48. https://doi.org/10.1016/s0165-0327(02)00429-9
Price RB, Rosen D, Siegle GJ, Ladouceur CD, Tang K, Allen KB, Ryan ND, Dahl RE, Forbes EE, Silk JS (2016) From anxious youth to depressed adolescents: prospective prediction of 2-year depression symptoms via attentional bias measures. J Abnorm Psychol 125(2):267–278. https://doi.org/10.1037/abn0000127
Lewinsohn PM, Klein DN, Seeley JR (1995) Bipolar disorders in a community sample of older adolescents: prevalence, phenomenology, comorbidity, and course. J Am Acad Child Adolesc Psychiatry 34(4):454–463
Article CAS Google Scholar
Thapar A, Pine D, Leckman JF, Scott S, Snowling MJ, Taylor EA (2017) Rutter’s child and adolescent psychiatry, 6th edn. Wiley-Blackwell, Oxford, UK
Google Scholar
Selph SS, McDonagh MS (2019) Depression in children and adolescents: evaluation and treatment. Am Fam Physician 100(10):609–617
Birmaher B, Brent D (2007) Practice parameter for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry 46(11):1503–1526. https://doi.org/10.1097/chi.0b013e318145ae1c
Cheung AH, Kozloff N, Sacks D (2013) Pediatric depression: an evidence-based update on treatment interventions. Curr Psychiatry Rep 15(8):381. https://doi.org/10.1007/s11920-013-0381-4
Richardson LP, Katzenellenbogen R (2005) Childhood and adolescent depression: the role of primary care providers in diagnosis and treatment. Curr Probl Pediatr Adolesc Health Care 35(1):6–24. https://doi.org/10.1016/j.cppeds.2004.09.001
Clark MS, Jansen KL, Cloy JA (2012) Treatment of childhood and adolescent depression. Am Fam Physician 86(5):442–448
Lewandowski RE, Acri MC, Hoagwood KE, Olfson M, Clarke G, Gardner W, Scholle SH, Byron S, Kelleher K, Pincus HA, Frank S, Horwitz SM (2013) Evidence for the management of adolescent depression. Pediatrics 132(4):e996–e1009. https://doi.org/10.1542/peds.2013-0600
Cheung AH, Zuckerbrot RA, Jensen PS, Laraque D, Stein REK (2018) Guidelines for adolescent depression in primary care (GLAD-PC): part II - treatment and ongoing management. Pediatrics 141(3):e20174082. https://doi.org/10.1542/peds.2017-4082
National Institute for Health and Care Excellence (2019) Depression in children and young people: identification and management (NICE Guideline 134). Available at: https://www.nice.org.uk/guidance/ng134 [].
Bailey AP, Hetrick SE, Rosenbaum S, Purcell R, Parker AG (2018) Treating depression with physical activity in adolescents and young adults: a systematic review and meta-analysis of randomised controlled trials. Psychol Med 48(7):1068–1083. https://doi.org/10.1017/s0033291717002653
Radovic S, Gordon MS, Melvin GA (2017) Should we recommend exercise to adolescents with depressive symptoms? A meta-analysis. J Paediatr Child Health 53(3):214–220. https://doi.org/10.1111/jpc.13426
Zhou X, Hetrick SE, Cuijpers P, Qin B, Barth J, Whittington CJ, Cohen D, Del Giovane C, Liu Y, Michael KD, Zhang Y, Weisz JR, Xie P (2015) Comparative efficacy and acceptability of psychotherapies for depression in children and adolescents: a systematic review and network meta-analysis. World Psychiatry 14(2):207–222. https://doi.org/10.1002/wps.20217
Brent D, Emslie G, Clarke G, Wagner KD, Asarnow JR, Keller M, Vitiello B, Ritz L, Iyengar S, Abebe K, Birmaher B, Ryan N, Kennard B, Hughes C, DeBar L, McCracken J, Strober M, Suddath R, Spirito A, Leonard H, Melhem N, Porta G, Onorato M, Zelazny J (2008) Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: the TORDIA randomized controlled trial. JAMA 299(8):901–913. https://doi.org/10.1001/jama.299.8.901
Thabrew H, Stasiak K, Hetrick SE, Donkin L, Huss JH, Highlander A, Wong S, Merry SN (2018) Psychological therapies for anxiety and depression in children and adolescents with long-term physical conditions. Cochrane Database Syst Rev 12:CD012488. https://doi.org/10.1002/14651858.CD012488.pub2
Vitiello B, Brent DA, Greenhill LL, Emslie G, Wells K, Walkup JT, Stanley B, Bukstein O, Kennard BD, Compton S, Coffey B, Cwik MF, Posner K, Wagner A, March JS, Riddle M, Goldstein T, Curry J, Capasso L, Mayes T, Shen S, Gugga SS, Turner JB, Barnett S, Zelazny J (2009) Depressive symptoms and clinical status during the treatment of adolescent suicide attempters (TASA) study. J Am Acad Child Adolesc Psychiatry 48(10):997–1004. https://doi.org/10.1097/CHI.0b013e3181b5db66
March J, Silva S, Petrycki S, Curry J, Wells K, Fairbank J, Burns B, Domino M, McNulty S, Vitiello B, Severe J (2004) Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. JAMA 292(7):807–820. https://doi.org/10.1001/jama.292.7.807
Oud M, de Winter L, Vermeulen-Smit E, Bodden D, Nauta M, Stone L, van den Heuvel M, Taher RA, de Graaf I, Kendall T, Engels R, Stikkelbroek Y (2019) Effectiveness of CBT for children and adolescents with depression: a systematic review and meta-regression analysis. European psychiatry 57:33–45. https://doi.org/10.1016/j.eurpsy.2018.12.008
Brunstein-Klomek A, Zalsman G, Mufson L (2007) Interpersonal psychotherapy for depressed adolescents (IPT-A). Isr J Psychiatry Relat Sci 44(1):40–46
Mufson L, Dorta KP, Wickramaratne P, Nomura Y, Olfson M, Weissman MM (2004) A randomized effectiveness trial of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry 61(6):577–584. https://doi.org/10.1001/archpsyc.61.6.577
Tompson MC, McNeil FM, Rea MM, Asarnow JR (2000) Identifying and treating adolescent depression. West J Med 172(3):172–176. https://doi.org/10.1136/ewjm.172.3.172
Cipriani A, Zhou X, Del Giovane C, Hetrick SE, Qin B, Whittington C, Coghill D, Zhang Y, Hazell P, Leucht S, Cuijpers P, Pu J, Cohen D, Ravindran AV, Liu Y, Michael KD, Yang L, Liu L, Xie P (2016) Comparative efficacy and tolerability of antidepressants for major depressive disorder in children and adolescents: a network meta-analysis. Lancet 388(10047):881–890. https://doi.org/10.1016/S0140-6736(16)30385-3
Hetrick SE, Merry SN, McKenzie J, Sindahl P, Proctor M (2007) Selective serotonin reuptake inhibitors (SSRIs) for depressive disorders in children and adolescents. Cochrane Database Syst Rev 3:CD004851. https://doi.org/10.1002/14651858.CD004851.pub2
Article Google Scholar
Ignaszewski MJ, Waslick B (2018) Update on randomized placebo-controlled trials in the past decade for treatment of major depressive disorder in child and adolescent patients: a systematic review. J Child Adolesc Psychopharmacol 28(10):668–675. https://doi.org/10.1089/cap.2017.0174
Bridge JA, Iyengar S, Salary CB, Barbe RP, Birmaher B, Pincus HA, Ren L, Brent DA (2007) Clinical response and risk for reported suicidal ideation and suicide attempts in pediatric antidepressant treatment: a meta-analysis of randomized controlled trials. JAMA 297(15):1683–1696. https://doi.org/10.1001/jama.297.15.1683
Findling RL, Robb A, Bose A (2013) Escitalopram in the treatment of adolescent depression: a randomized, double-blind, placebo-controlled extension trial. J Child Adolesc Psychopharmacol 23(7):468–480. https://doi.org/10.1089/cap.2012.0023
Mullen S (2018) Major depressive disorder in children and adolescents. Ment Health Clin 8(6):275–283. https://doi.org/10.9740/mhc.2018.11.275
Czaja AS, Valuck RJ, Anderson HD (2013) Comparative safety of selective serotonin reuptake inhibitors among pediatric users with respect to adverse cardiac events. Pharmacoepidemiol Drug Saf 22(6):607–614. https://doi.org/10.1002/pds.3420
DeFilippis M, Wagner KD (2014) Management of treatment-resistant depression in children and adolescents. Pediatric Drugs 16(5):353–361. https://doi.org/10.1007/s40272-014-0088-y
Hetrick SE, McKenzie JE, Cox GR, Simmons MB, Merry SN (2012) Newer generation antidepressants for depressive disorders in children and adolescents. Cochrane Database Syst Rev 11:CD004851. https://doi.org/10.1002/14651858.CD004851.pub3
Walkup JT, Labellarte MJ, Riddle MA, Pine DS, Greenhill L, Klein R, Davies M, Sweeney M, Abikoff H, Hack S (2001) Fluvoxamine for the treatment of anxiety disorders in children and adolescents. N Engl J Med 344(17):1279–1285. https://doi.org/10.1056/NEJM200104263441703
Meighen KG (2007) Duloxetine treatment of pediatric chronic pain and co-morbid major depressive disorder. J Child Adolesc Psychopharmacol 17(1):121–127. https://doi.org/10.1089/cap.2006.0042
Hazell P, Connell D, Heathcote D, Robertson J, Henry D (1995) Efficacy of tricyclic drugs in treating child and adolescent depression: a meta-analysis. BMJ 310(6984):897. https://doi.org/10.1136/bmj.310.6984.897
Hazell P, Mirzaie M (2013) Tricyclic drugs for depression in children and adolescents. Cochrane Database Syst Rev 6:CD002317. https://doi.org/10.1002/14651858.CD002317.pub2
Eli Lilly and Company. Prozac (Fluoxetina) [Capsules]. U.S. Food and Drug Administration website https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/018936s108lbl.pdf . Revised 2017. Accessed 20 July, 2020.
H. Lundbeck A/S. Lexapro (Escitalopram) [Tablets]. U.S. Food and Drug Adminstration website https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/021323s047lbl.pdf . Revised 2017. Accessed 20 July, 2020.
Kakuma R, Minas H, Van Ginneken N, Dal Poz MR, Desiraju K, Morris JE, Saxena S, Scheffler RM (2011) Human resources for mental health care: current situation and strategies for action. The Lancet 378(9803):1654–1663. https://doi.org/10.1016/S0140-6736(11)61093-3
Cuijpers P, van Straten A, Smit F, Mihalopoulos C, Beekman A (2008) Preventing the onset of depressive disorders: a meta-analytic review of psychological interventions. Am J Psychiatry 165(10):1272–1280. https://doi.org/10.1176/appi.ajp.2008.07091422
Judd LL (1997) The clinical course of unipolar major depressive disorders. Arch Gen Psychiatry 54(11):989–991. https://doi.org/10.1001/archpsyc.1997.01830230015002
Panel DG (1994) Depression in primary care: detection, diagnosis, and treatment. J Am Assoc Nurse Pract 6(5):224–238. https://doi.org/10.1111/j.1745-7599.1994.tb00946.x
Evans DL, Andrews LW (2005) Adolescent mental health initiative. In: If your adolescent has depression or bipolar disorder: an essential resource for parents. Press, Oxford University
England MJ, Sim LJ, Council NR (2009) The etiology of depression. In: Depression in parents, parenting, and children: opportunities to improve identification, treatment, and prevention. National Academies Press (US), pp 73-118
O’Connell ME, Boat T, Warner KE (2009) Preventing mental, emotional, and behavioral disorders among young people: progress and possibilities, vol 7. National Academies Press, Washington, DC
Spence SH, Sheffield JK, Donovan CL (2003) Preventing adolescent depression: an evaluation of the problem solving for life program. J Clin Child Psychol 71(1):3–13. https://doi.org/10.1037//0022-006x.71.1.3
Spence SH, Sheffield JK, Donovan CL (2005) Long-term outcome of a school-based, universal approach to prevention of depression in adolescents. J Consult Clin Psychol 73(1):160–167. https://doi.org/10.1037/0022-006X.73.1.160
Shochet IM, Dadds MR, Holland D, Whitefield K, Harnett PH, Osgarby SM (2001) The efficacy of a universal school-based program to prevent adolescent depression. J Clin Child Psychol 30(3):303–315. https://doi.org/10.1207/S15374424JCCP3003_3
Sawyer MG, Pfeiffer S, Spence SH, Bond L, Graetz B, Kay D, Patton G, Sheffield J (2010) School-based prevention of depression: a randomised controlled study of the beyondblue schools research initiative. J Child Psychol Psychiatry 51(2):199–209. https://doi.org/10.1111/j.1469-7610.2009.02136.x
Gillham JE, Reivich KJ, Freres DR, Lascher M, Litzinger S, Shatté A, Seligman ME (2006b) School-based prevention of depression and anxiety symptoms in early adolescence: a pilot of a parent intervention component. Sch Psychol Q 21(3):323–348. https://doi.org/10.1521/scpq.2006.21.3.323
Gillham JE, Brunwasser SM, Freres DR (2008) Preventing depression in early adolescence: the penn resiliency program. In: Handbook of depression in children and adolescents. The Guilford Press, New York, NY, US, pp 309–322
Gillham JE, Hamilton J, Freres DR, Patton K, Gallop R (2006a) Preventing depression among early adolescents in the primary care setting: a randomized controlled study of the Penn Resiliency Program. J Abnorm Child Psychol 34(2):203–219. https://doi.org/10.1007/s10802-005-9014-7
Roberts C, Ballantyne F, Van Der Klift P (2003) Aussie optimism. Curtin University of Technology, Perth, Australia, Social life skills. Teacher resource
Thompson EA, Eggert LL, Herting JR (2000) Mediating effects of an indicated prevention program for reducing youth depression and suicide risk behaviors. Suicide Life Threat Behav 30(3):252–271. https://doi.org/10.1111/j.1943-278X.2000.tb00990.x
Young JF, Mufson L, Davies M (2006) Efficacy of interpersonal psychotherapy-adolescent skills training: an indicated preventive intervention for depression. J Child Psychol Psychiatry 47(12):1254–1262. https://doi.org/10.1111/j.1469-7610.2006.01667.x
Horowitz JL, Garber J (2006) The prevention of depressive symptoms in children and adolescents: a meta-analytic review. J Consult Clin Psychol 74(3):401–415. https://doi.org/10.1037/0022-006X.74.3.401
Stice E, Shaw H, Bohon C, Marti CN, Rohde P (2009) A meta-analytic review of depression prevention programs for children and adolescents: factors that predict magnitude of intervention effects. J Consult Clin Psychol 77(3):486–503. https://doi.org/10.1037/a0015168
Merry SN, Hetrick SE, Cox GR, Brudevold-Iversen T, Bir JJ, McDowell H (2011) Psychological and educational interventions for preventing depression in children and adolescents. Cochrane Database Syst Rev 7(12):CD003380. https://doi.org/10.1002/14651858.CD003380.pub3
Download references
Acknowledgments
The authors would like to thank Dilermando Sobral, MD, Sónia Almeida, MD and Paula Assunção, MD for their guidance.
No sources of funding were required.
Author information
Authors and affiliations.
Family Health Unit of Ramalde, Health Centres Grouping of Porto Ocidental, Porto, Portugal
Diogo Beirão, Helena Monte, Marta Amaral, Alice Longras, Carla Matos & Francisca Villas-Boas
FP-ENAS-Energy, Environment and Health Research Unit/CEBIMED- Centro de Estudos em Biomedicina, Fernando Pessoa University, Porto, Portugal
Carla Matos
You can also search for this author in PubMed Google Scholar
Contributions
DB conceived the original idea of this work and took the lead in writing the manuscript. All authors contributed equally in the literature review and writing of the manuscript. DB was responsible for the section on epidemiology and comorbidities. HM was responsible for the sections on the background and pharmacological treatment. MA was responsible for the abstract, non-pharmacological treatment and the conclusion. AL was responsible for the sections on methods and pathogenesis. CM was responsible for the sections on diagnosis and background, and FVB for the section on prevention. DB and HM were responsible for the construction of the final version of the manuscript which was reviewed and approved by all co-authors.
Corresponding author
Correspondence to Diogo Beirão .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Beirão, D., Monte, H., Amaral, M. et al. Depression in adolescence: a review. Middle East Curr Psychiatry 27 , 50 (2020). https://doi.org/10.1186/s43045-020-00050-z
Download citation
Received : 12 June 2020
Accepted : 21 August 2020
Published : 02 October 2020
DOI : https://doi.org/10.1186/s43045-020-00050-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adolescence
Loyola University > Center for Digital Ethics & Policy > Research & Initiatives > Essays > Archive > 2018 > The Role of Social Media in Adolescent/Teen Depression and Anxiety
The role of social media in adolescent/teen depression and anxiety, april 3, 2018.
The adolescent and teen years have always been a challenging time. Peer pressure, insecurity and hormones are just some of the issues facing those in these age groups. But does social media exacerbate these problems?
For example, researchers from the Alberta Teachers’ Association, the University of Alberta, Boston Children’s Hospital and Harvard Medical School released a study that found significant changes in students at every grade level as a result of digital technology. In the past three to five years, 90 percent of teachers at the University of Alberta saw increases in emotional challenges, 85 percent saw social challenges and 77 percent observed cognitive challenges. Also, 56 percent of teachers report an increase in the number of kids sharing stories about online harassment and/or cyberbullying. There are increases in other areas as well. The majority of teachers say there has been an increase in students diagnosed with the following conditions: anxiety disorders (85 percent), ADD and ADHD (75 percent), and such mood disorders as depression (73 percent).
Also, a recent study by researchers at the Royal Society for Public Health and Young Health Movement found that 91 percent of those between the ages of 16 and 24 said Instagram was the worst social media platform as it relates to mental health. Instagram was most likely to cause negative effects such as poor body image, fear of missing out and sleep deprivation. Snapchat came in second place, followed by Facebook, Twitter and YouTube. The researchers theorize that Instagram and Snapchat are image-focused platforms and users compare themselves to others.
A review of 36 social media studies, published in JAMA Pediatrics, found that 23 percent of kids are victims of cyberbullying. The review also found that cyberbullying results in low self-esteem, depression, self-harm and behavioral problems — in both the victims and the bullies. In addition, cyberbullying was more likely to produce suicidal thoughts than traditional bullying.
Another study , conducted by researchers at Glasgow University found that kids (some of whom were pre-teens) were on social media until the wee morning hours, and some were on more than one device (for example, a phone and a tablet) so they could simultaneously view multiple sites. These individuals reported lower sleep quality rates in addition to higher levels of depression and anxiety.
In a survey by the National Campaign to Support Teen and Unplanned Pregnancy, almost 20 percent of teens admitted to participating in "sexting" or sending nude photos.
The pressure these adolescents and teens feel can be intensified by the time they get to college. Stanford University coined the phrase “ Duck syndrome ” to describe the erroneous attitude of incoming freshmen that they’re struggling while everyone else is gliding along smoothly — but in reality, the gliders are also “paddling furiously under the water just to keep up.” Adolescents and teens become accustomed to creating the impression that everything is perfect to match the equally perfect posts of their friends. But it becomes too difficult to maintain this façade, resulting in suicide among college students who appear to be well-adjusted, but are actually experiencing mental and emotional problems.
Another report , published in the American Journal of Preventive Medicine, reveals that among young adults between the ages of 19 and 32, those with high social media usage (those logging on for more than 2 hours a day and checking their accounts 58 times a week) were more likely to deal with feelings of isolation than those with low social media use (they logged on for 30 minutes and checked their accounts 9 times a week).
In light of these studies, who is responsible for the role of social media in adolescent/teen depression and anxiety?
Many tech leaders seem to understand the unhealthy, addictive nature of technology in general and social media in particular. As far back as 2010, New York Times reporter Nick Bilton interviewed the late Steve Jobs of Apple. Jobs told Bilton that he limited the amount of technology that his kids use. Bill Gates shared that he didn’t let his kids have mobile devices until they were 14 years old, and he sets a time for them to turn off the devices at night.
Evan Williams, one of the founders of Twitter, Medium and Blogger, told Bilton that his kids read physical books instead of using iPads. Dick Costolo, former CEO of Twitter, told Bilton that his teenagers had to be in the living room when they used their tech devices.
But, perhaps the most shocking revelation came from Sean Parker, former president of Facebook, in an interview with Axios. Referring to Facebook, Parker said, “God only knows what it’s doing to our children’s brains.”
But there’s more. Parker also said, “ . . . How do we consume as much of your time and conscious attention as possible? . . . And that means that we need to sort of give you a little dopamine hit every once in a while, because someone liked or commented on a photo or a post or whatever . . . And that's going to get you to contribute more content, and that's going to get you ... more likes and comments . . . It's a social-validation feedback loop ... exactly the kind of thing that a hacker like myself would come up with, because you're exploiting a vulnerability in human psychology . . . The inventors, creators — it's me, it's Mark [Zuckerberg], it's Kevin Systrom on Instagram, it's all of these people — understood this consciously . . . And we did it anyway.”
So, if Parker confessed that social media was designed to be addictive, should social media companies be responsible for depression, anxiety, bullying and other issues among adolescents and teens?
Donna Shea, director of The Peter Pan Center for Social and Emotional Growth, and Nadine Briggs, director of Simply Social Kids , are passionate about helping kids make and keep friends, and together have formed How to Make and Keep Friends, LLC. Shea and Briggs both lead community-based social groups at their centers in Massachusetts and have also formed the Social Success in School initiative. The two have also written several books for kids and teens, including, “Tips for Teens on Life and Social Success” .
Both Shea and Briggs believe that it is the job of parents to monitor their kid’s social media activity. “You wouldn’t allow your teen to put a lock on their bedroom door, but your teen is not only now interacting with peers at school or in your neighborhood, they are interacting with the entire world,” Shea said. “It is a parent’s job to be as involved in their teen’s online life as they are in their offline life.”
In fact, she is not in favor of giving adolescents and teens a phone as a gift. “Mobile devices belong to the parent and the teen is being allowed to use it,” Shea said. “A contract can be a useful tool before putting a device in the hands of your teen which would allow parents to have access to the phone.”
She believes that parents should monitor their adolescent/teen’s activity — and teens should know this is being done. “Parents do not need to be sneaky about that — tell your child to hand over the phone,” she said. Shea also recommends that parents use subscription services to view all of their teens’ activities. “Teens should be prepared to be monitored until they are of legal adult age,” she said.
However, Briggs admits that apps change so quickly that it’s almost impossible to keep up with them. “Other than doing your best to monitor your teen’s activity — and it won’t be 100% effective - it’s important from the very beginning that you teach your child and teen to be good consumers of what is available to them,” Briggs said. “This is the new norm, and we think it’s the parent’s responsibility to be involved in their teen’s online life.”
She compares giving kids a phone or device to putting them behind the wheel of a car. “Both can be dangerous in their own way, but teens can learn the responsibilities that go along with these more adult activities.”
But, do parents bear sole responsibility? For example, everyone knows that tobacco is bad for your health, and people consume it willingly; however, they continue to sue and win lawsuits against tobacco companies. In 2014, one plaintiff was awarded $23.6 billion when her husband died of lung cancer as a result of smoking up to three packs of cigarettes a day. He started smoking at the age of 13 and died at the age of 36. The plaintiff (his widow) argued that the tobacco company willfully deceived consumers with addictive products.
How is this scenario different from what social media companies are doing? And speaking of willful deception, what about companies that make secretive apps that allow teens to hide their sexting?
If someone trips and falls on your property, you could be sued. If someone gets harmed at your nightclub, you could be held liable for not having “adequate security.” If one of your employees sexually harasses a colleague, you would be held responsible — even if you didn’t know about it. If you sell alcohol, you’re responsible for making sure it doesn’t get into the hands of a minor. In fact, according to the Dram Shop Law, if you let an adult have too many drinks and this individual is involved in an accident, you could be responsible.
However, if kids become addicted to a communication platform that was designed to be addictive, if they’re bullied online, if there are no safeguards to stop them from utilizing the types of secretive apps that encourage risky behavior, shouldn’t these companies be held responsible?
I think they should be, but this is not likely to happen until society holds them responsible. Since most adults are also addicted to social media — and some of them are internet bullies and engage in sexting, it seems unlikely that they would advocate for changes.
In the aforementioned study by the Royal Society for Public Health and Young Health Movement, researchers offered several ways to reduce some of the problems adolescents and teens face online. For example, one of the reasons kids feel so much pressure to look perfect is because of the doctored photos they see. The researchers recommend that social media companies include some sort of notification, such as a watermark, when photos have been digitally manipulated (68 percent of surveyed students support this action).
Another suggestion is to create a social media cap. Users would be logged out if they went over a pre-determined usage level (30 percent of surveyed students agree with this suggestion).
The majority of surveyed students (84 percent) approve of schools having classes on safe social media.
Another suggestion by the researchers (which did not include student responses) was to use social media posts to identify kids and teens who might be at risk for mental health problems. However, problems have already been identified with using Facebook to identity potential problem drinkers .
In addition, it was suggested that youth workers be trained in digital media.
These are nice Band-Aid solutions. But they don’t address the addictive nature of social media and the incredible amount of peer pressure that it involves. Parents can provide guidance, but history has shown that their values rarely outweigh the pressure of peers.
Albert Einstein once said, “We can’t solve our problems with the same thinking we used to create them.” But in this situation, the social media giants can solve these problems with the exact same thinking they used to create them. Just as they figured out what it would take to make these platforms addictive, they can figure out what it would take to make the platforms less addictive. But don’t hold your breath because the person who creates the problem and profits from the problem has no incentive to solve the problem.
Terri Williams writes for a variety of clients including USA Today , Yahoo , U.S. News & World Report , The Houston Chronicle , Investopedia , and Robert Half . She has a Bachelor of Arts in English from the University of Alabama at Birmingham. Follow her on Twitter @Territoryone .
Research & Initiatives
Return to top.
- Support LUC
- Directories
- Symposia Archive
- Upcoming Events
- Past Events
- Publications
- CDEP in the News
© Copyright & Disclaimer 2024
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Psychiatry (Edgmont)
Adolescent Depression
Mary n. cook.
Dr. Cook is Medical Director of Clinical Services, Psychiatry and Behavioral Sciences Department, The Children’s Hospital, Denver, Colorado, and Assistant Professor, Department of Psychiatry, University of Colorado, School of Medicine, Denver, Colorado
John Peterson
Dr. Peterson is Director, Child/Adolescent Psychiatry, Denver Health Medical Center, and Associate Professor, Department of Psychiatry, University of Colorado, School of Medicine, Denver, Colorado
Christopher Sheldon
Dr. Sheldon is Chief Psychologist and Training Director, Denver Health Medical Center, and Assistant Professor, Department of Psychiatry, University of Colorado, School of Medicine, Denver, Colorado
Depression in adolescence and adulthood is common, afflicting up to 20 percent of these populations. It represents a significant public health concern and is associated with considerable suffering and functional impairment. Adolescent-onset depression tends to be a particularly malignant and recalcitrant condition, increasing the likelihood of recurrence and chronicity in adulthood. Clinical presentations for various medical and psychiatric conditions, as well as reactions to psychosocial stressors, can mimic or confound the picture of depression in adolescents. Therefore, careful assessment and differential diagnosis is essential. Effective treatments, both pharmacological and psychosocial in nature, exist, and so early detection and intervention is paramount. This article presents an overview of optimal prevention, assessment, and clinical decision-making strategies for managing depression in adolescents.
A Case Vignette
(This is a composite case and is not based on an actual patient in treatment.) Julia was a 16-year-old girl who reported difficulty sleeping, an irritable mood, low energy, and declining grades for the past several months. She was accompanied by her mother who was very worried. The mother reported that Julia quit the tennis team, which she used to enjoy, and lost weight. Julia initially said these problems were “not that bad” and that her mother needed to “stop hassling me.”
Introduction
Depression is one of the most costly and debilitating medical conditions afflicting our society. 1 It is a leading cause of absenteeism and compromised productivity in adults, costing the US economy billions of dollars per year. 2 It also worsens the course and increases the cost of numerous medical illnesses. It contributes to premature death by suicide. 3 The impact of depression reverberates well beyond its victims, affecting family and friends. Recognizing and treating major depression and its variants in the early stages is important in reducing future negative impact.
Depression in adolescence significantly impairs functioning and may derail normal psychosocial development. Moreover, it often recurs or persists into adulthood. Rates of depression rise considerably during adolescence with as many as one in five teenagers developing major depression at some point. In adolescence, depression can be mistaken for adolescent angst or for hormone-related moodiness although it is a disorder associated with serious consequences. Youth with depression are likely to suffer broad functional impairment across social, academic, family, and occupational domains. 4 Adolescents with depression are at higher risk for substance abuse and other psychiatric comorbidities. 4 In addition, depression disorders with a pediatric onset tend to be more chronic and debilitating than depression beginning in adulthood. 5 Fortunately, we now have an array of evidence-based pharmacological and psychotherapeutic treatments for depression.
The literature on prevention of depression in youth has grown substantially in the past decade but has been plagued by methodological limitations; therefore, identification of effective preventive strategies remains in its early stages. Programs that have been universally applied to community samples have been largely, but not entirely, ineffectual. In general, programs with interventions delivered by the research team, psychologists, or extensively trained group leaders, have been associated with the greatest success. 6 Skill sets taught in some of the more effective interventions have included cognitive restructuring, problem solving, stress management, and accessing social support. Programs that have offered less training or for which interventions were delivered by nonmental health professionals (e.g., teachers) have tended to produce less favorable outcomes.
The most successful strategy identified thus far involves both targeting at-risk cohorts and utilizing expert clinicians to deliver treatments. Research has repeatedly documented increased prevalence of major depression in the offspring of depressed parents. 7 Programs that specifically target children of depressed parents have been more effective. 8 , 9 An alternative strategy for identifying risk involves screening adolescents for depression and applying interventions specifically to teens with subsyndromal depression. 10 This strategy has been associated with reduced risk for depression onset, as well as a significant delay in onset of depression. Selecting a well-established risk factor (parental depression, subsyndromal depression), examining the mechanisms by which risk is imposed, and attempting to augment protective factors is a sound model for conducting prevention research.
Epidemiology
Depressive symptoms are common in pediatric clinical settings, with 5 to 10 percent of children and adolescents presenting with subsyndromal symptoms of major depressive disorder (MDD). 11 MDD is estimated to affect two percent of children aged 6 to 12 years and 4 to 8 percent of adolescents aged 13 to 17 years. In children, the ratio of boys to girls is 1:1, but in teens, the ratio changes to 1:2. Dysthymic disorder (DD), which constitutes a more chronic, milder form of depression, has been reported to afflict 0.6 to 1.7 percent of children and 1.6 to 8 percent of adolescents. The risk of depression increases significantly after puberty (particularly in girls), and by age 18, the cumulative incidence is 20 percent. 12
Risk Factors
A family history of depression has consistently been found as a risk factor for the disorder. High-risk, adoption, and twin studies have demonstrated that MDD is caused by the interaction of genetic and environmental risk factors, with an interplay between life stressors and a serotonic transporter polymorphism reported as one causal pathway. 13 – 16 Subsyndromal symptoms of depression, low self esteem, and anxiety have all been found to increase the probability of developing depression. Academic struggles and family turmoil are also prospective predictors of depression for teenagers. 17 Consistent with cognitive models of depression, a negative attributional style in combination with negative life events can lead to the development of depression. 18
Screening and Assessment
Primary care providers should screen all youth for depression by asking about key symptoms, including sad or irritable mood and anhedonia or the inability to experience pleasure and have fun. In youngsters, readily observable changes associated with onset of depression might include deteriorating academic performance, weight or appetite loss or gain, social withdrawal, changes in sleep, increased defiance (related to irritability), and discontinuation of previously preferred activities. Teenagers with increased negative moods should be further assessed for changes in thinking to a more negative view of themselves, the world, and the future. Asking about suicidal ideation and screening for safety are also important parts of the interview.
The clinical presentation of depression in youth resembles that in adults with some differences stemming from developmental considerations. For instance, children are more likely than adults to exhibit mood lability or irritability and display indirect or behavioral manifestations of disturbed mood, such as temper outbursts, somatic complaints, social withdrawal, or diminished frustration tolerance. They are less likely than adults to explicitly complain of feeling depressed and unlikely to exhibit melancholic symptoms, including depressed mood worse in the morning, early morning awakening, marked psychomotor retardation, significant weight loss, and excessive guilt.
Depression in youth may be accompanied by hallucinations or delusions, although rarely. Psychotic depression in children has been associated with a family history of bipolar and depression with psychotic features, more severe depression, greater long-term risk, resistance to antidepressants, and increased risk of future onset of bipolar disorder. 19 , 20 Youth with seasonal affective disorder (SAD) mainly have symptoms of depression during seasons with less daylight. SAD should be differentiated from depression triggered by school stress because both usually coincide with the school calendar.
A diagnosis of a depressive disorder would be considered if the youth demonstrated markedly impaired functioning in social, academic, or family domains. Functionality can be readily and objectively assessed using the Children’s Global Assessment Scale or Global Assessment of Functioning. Complaints of significant emotional distress in the child would also merit further investigation for depressive symptoms. Screening can be facilitated by using depressive symptom checklists derived from the Diagnostic and Statistical manual of Mental Disorders, Fourth Edition, Text Revision ( DSM-IV-TR ) 21 or the International Classification of Diseases, Tenth Revision ( ICD-10 ), 22 clinician-based instruments, or youth or parent self reports. Examples of widely used and well-validated screening checklists include the Child Depression Inventory, as well as the Reynold’s Adolescent Depression Scale. 12
Youth do not always readily report on emotional or behavioral manifestations of psychiatric disorders. They might deny the existence of these symptoms or behaviors or simply have difficulty articulating their thoughts and feelings. The use of open-ended or indirect questions is recommended in pediatric interviews, as the information collected is likely to be more comprehensive and reliable. Direct or closed-ended questions tend to elicit more limited and potentially biased responses from children and teens, due to their leading nature and the tendency of youth to be suggestible. Collateral information from parents, alternative caregivers, and teachers is often essential for confirming or ruling out depression or other psychiatric or behavioral disorders. The onset and course of a mood disorder may be determined through the use of a mood diary or timeline, using significant life events as anchors. A mood timeline can enable the provider, child, and parents to identify environmental triggers, as well as comorbid conditions.
Diagnostic Criteria
Depression is manifested as a spectrum disorder, ranging from subsyndromal to syndromal. Criteria for the full syndrome of MDD are met when a child or adolescent presents with at least two weeks of a persistent change in mood, depressed or irritable, plus at least five of the nine symptoms listed in Table 1 . The symptoms must be impairing, represent a change from baseline functioning, and not be attributable to another psychiatric or medical etiology, bereavement, or substance abuse. MDD can be manifested with atypical symptoms, such as increased reactivity to rejection, lethargy (leaden paralysis), increased appetite, craving for carbohydrates, and hypersomnia.
Criteria for major depressive episode and dysthymic disorder *
Dysthymic disorder consists of a persistent, long-term change in mood that generally is less intense but more chronic than in MDD. Due to its more subtle and chronic nature, DD is often overlooked or misdiagnosed. Although the symptoms of dysthymia are not as severe as in MDD, they nonetheless typically cause as much or more psychosocial impairment. Criteria for DD are met when a child or adolescent presents with at least one year of a depressed or irritable mood most of the time, and at least two other symptoms from the group listed in Table 1 .
Differential Diagnosis
There are a myriad of psychiatric conditions with significant symptomatic overlap with depression, such as anxiety and disruptive, psychotic, and substance use disorders, to name a few. Bereavement and depressive reactions to environmental stressors can likewise present with predominately depressive symptomatology. Youths with SAD, by definition, develop depressive symptoms coincident with seasons having diminished daylight. SAD can be confused with depression precipitated by school stress as both conditions coincide with the school calendar.
Various medical conditions, including hypothyroidism, anemia, autoimmune diseases, and chronic fatigue syndrome may mimic or occur coincidentally with depression. Symptoms shared between these conditions and depression might include fatigue, low energy, sleep and appetite disturbances, and impaired concentration. Demoralization and low self esteem commonly manifest as part of the aforementioned disorders and so, too, are expected symptoms of depression. Therefore, physical examination and screening for such conditions may be warranted.
Practitioners must be mindful of the extensive list of medications that can produce depressive symptoms. For instance, stimulants, corticosteroids, and contraceptives are often associated with worsening mood lability or irritability. They likewise can disturb sleep and appetite as well as induce weight changes.
Children presenting for treatment are often experiencing their first episode of depression, making it difficult to ascertain whether or not they are experiencing unipolar depression or the first episode of a bipolar disorder. A strong family history of bipolar disorder, symptoms of psychosis in the child, and a history of pharmacologically induced mania or hypomania increase the likelihood of future onset of a bipolar disorder. 19 , 20 It is prudent for clinicians to systematically screen for a history of manic or hypomanic symptoms because such a history predicts which youth are more likely to experience medication-induced mania when treated with antidepressants.
It is important to note, however, that not all children who become “activated” or hypomanic while receiving antidepressants have bipolar disorder. A common side effect of serotonergic agents is akathisia or extreme restlessness and agitation. This reaction is likely to occur early in treatment (within a few days) and consists of extreme motoric overactivity without concomitant mood symptoms. Mania or hypomania induced by serotonergic agents might also include a hyperactive motor component, but this generally occurs later in treatment (after 2 or more weeks) and would be accompanied by elevated, euphoric, or irritable mood, grandiosity, decreased need for sleep, and hypersexuality.
Case Vignette, Continued
When Julia was interviewed separately, the clinician was able to establish a therapeutic alliance with the teenager. Julia described her problems in more detail with the clinician. Julia described thoughts of suicide over the past several weeks, although she did not have any specific plan and she had not attempted to harm herself.
Suicidality
Suicide remains the third leading cause of death in US adolescents, claiming almost 2,000 lives each year among youth aged 12 to 19 years. 3 Almost 1 in 5 (17%) of US high school students had suicidal thoughts in a given year, and almost 1 in 10 (8%) have attempted suicide. Current suicidal ideation is a risk factor for suicide, and having made a suicide attempt is the strongest predictor of future suicidal behavior. 23 , 24 Suicidal ideation is common among depressed youth, with an estimated 60 percent reporting having had suicidal thoughts and 30 percent reporting a suicide attempt. 12
Acutely suicidal, psychotic, self-harming, or severely depressed children and adolescents should have an emergency psychiatric consultation. A comprehensive approach is outlined in Table 2 . The thorough assessment of teens who are suicidal should involve interviewing the adolescent separately from the family and obtaining collateral information from parents, therapists, teachers, caseworkers, and others, as needed. The teen will likely respond best to an empathic, nonjudgmental demeanor, and the clinician should ask about current and past self-harming behaviors. Inquiring about suicidal thoughts (frequency, duration, plans, and “triggers”), suicide intent (intensity of the desire to die), and past suicide attempts (number of attempts, methods, consequences) is essential. Targeted questions about suicidality have not been associated with precipitating increased suicidal thinking in youth, and, in fact, literature on this topic has suggested such questioning tends to bring relief to troubled teens. Questions should be asked about acute stressors (e.g., break up, loss or rejection, conflict with parents), presence of psychotic symptoms or homicidal thoughts, and the extent of any substance abuse. Parents or guardians should be involved in the evaluation, safety planning, and treatment process.
The suicidal/self-harming adolescent
Psychiatric hospitalization is appropriate for youth with active suicidal thoughts or recent suicidal or self-injurious behaviors. It might also be indicated for patients presenting with acute psychiatric disorders, significant substance abuse problems, serious medical issues, poor social supports, or an inability to be safely managed on an outpatient basis. A comprehensive approach is outlined in Table 2 .
As the interview progressed, Julia seemed to open up more, describing her increased use of alcohol and marijuana since she and her boyfriend broke up three months previously. Since the break up, Julia felt she was not able to “bounce back” the way that she had before.
Comorbidity
Both MDD and DD are commonly associated with other psychiatric and medical conditions. In addition, they often occur concurrently, a condition termed double depression . Epidemiological studies have estimated that 40 to 90 percent of youth presenting with depression also met criteria for an additional psychiatric disorder, with up to 50 percent manifesting two or more comorbid psychiatric diagnoses. 25 , 26 The most frequent comorbid diagnoses are anxiety disorders, followed by disruptive behavior disorders, including attention deficit hyperactivity disorder, and, in adolescents, substance use disorders. MDD and DD usually onset later than anxiety, but prior to other psychiatric conditions, including conduct and substance abuse disorders.
Situational Problems
Depression is theorized as stemming from an interaction between a depressive diathesis and psychosocial stressors. 27 , 28 Therefore, careful assessment for current and past stressors is indicated, including interpersonal or family conflict; verbal, physical, and sexual abuse; neglect, or poverty. It is also important to assess for symptoms consistent with posttraumatic stress disorder, which can develop in response to traumatic events. Depression often occurs against a backdrop of interpersonal and family conflict. Depression tends to increase irritability, leading to increased interpersonal tension and estrangement of others. Patients with depression consequently often perceive diminishing social support and increasing loneliness, limiting opportunities for pleasure and further exacerbating depression. Involvement in deviant peer groups may lead to antisocial behavior, generating more stressful life events and increasing the likelihood of depression. 29 , 30
The family should be evaluated for psychiatric illness to facilitate establishing a definitive diagnosis and treatment plan for the child, because parental psychopathology often predicts adherence with treatment, course of illness, and outcome. It is essential to assess for marital and family discord, impaired attachment, inadequate parent support, and controlling parent-child relationships, because these factors can increase risk for substance abuse and conduct disorder.
Clinical Course
Clinically referred youth with major depression will have a median episode duration of eight months, whereas community samples experience a median duration of 1 to 2 months. 31 Nearly all children and adolescents will recover from their first depressive episode, but long-term clinical and epidemiological studies have demonstrated probability rates of recurrence ranging from 20 to 60 percent by 1 to 2 years after remission and rising to 70 percent after five years. A significant proportion of youth with MDD will continue to suffer from MDD during adulthood. 19 , 32 Between 20 and 40 percent of pediatric patients presenting with depression will develop bipolar disorder at some point. 19 , 20 Those especially at risk include patients presenting with concomitant psychotic features and family histories of bipolar and those with histories of pharmacologically induced mania or hypomania.
Childhood depression appears to be more heterogeneous than its adult counterpart. Children with significant genetic loading for mood disorders are at particular risk for recurrences whereas others are likely to develop bipolar disorder. Some youth presenting with symptoms and behaviors that initially resemble depression develop behavior problems and substance abuse rather than depression.
Poor outcomes are associated with greater severity, chronicity or recurrence, comorbid conditions, hopelessness, residual subsyndromal symptoms, pessimism, family discord, low socioeconomic status, and chronic environmental stressors (abuse, family conflict). 11 , 25 Children with DD are likely to experience a prolonged course of illness, with a mean episode length of 3 to 4 years for clinical and community samples. 26 In addition, this disorder is further associated with increased risk of subsequent development of MDD and substance abuse.
Long-term Prognosis
Untreated depression in children is likely to derail their emotional, cognitive, and social development, in addition to impairing family relationships. The most devastating consequences of MDD are suicide attempts and completions. Approximately 60 percent of depressed youth report having thought about suicide and 30 percent actually attempt suicide. 3 The risk of suicidality is increased by a history of suicide attempts, comorbid psychiatric disorders (e.g., disruptive disorders, substance abuse), impulsivity, aggression, access to lethal methods (e.g., firearms), exposure to negative events (e.g., physical or sexual abuse, violence), and a family history of suicidal behavior. 23 , 24 , 33 , 34
Pediatric patients with depression are additionally at particularly high risk for substance abuse (including nicotine dependence), legal problems, adverse events, physical illness, early pregnancy, and poor work, academic, and psychosocial outcomes. 25 , 19 , 32 , 35
Psychosocial functioning is likely to gradually improve after an acute depressive episode except, of course, in the face of relapse. However, psychosocial difficulties typically persist even after remission of a depressive episode, highlighting the need for ongoing monitoring and treatment that targets psychosocial and environmental issues.
After a physical exam and laboratory studies showed no significant abnormalities, Julia was diagnosed with MDD and there was a discussion of treatment options. When antidepressant medication was mentioned, Julia and her mother expressed concerns that antidepressants can cause suicide. They also wanted to know whether medication or psychotherapy was better as a treatment approach.
Pharmacological Treatment
The use of pharmacologic agents to treat pediatric depression has been shrouded in controversy in recent years. The controversy stems from a relative paucity of controlled data documenting efficacy for antidepressants in youth and some data demonstrating a small but significant signal of increased suicidality associated with the initiation of some antidepressants. Numerous studies have examined the utility of tricyclic antidepressants (TCAs) to treat pediatric depression, all of which have been negative. 4 This data, together with a relatively high potential for lethality in overdose, have led to the consensus that TCAs are contraindicated for treating youth with depression. Until recently, the only agent to receive US Food and Drug Administration (FDA) approval for the indication of major depression in 8- to 17-year-olds was fluoxetine. Recently, escitalopram was approved by the FDA for the treatment of depression in adolescents. 36 , 37 Other antidepressants are frequently still used for pediatric depression, but their use is considered off label.
Efficacy data. The results of randomized, controlled trials comparing selective serotonin reuptake inhibitor (SSRI)-treatment of MDD in adolescents are shown in Table 3 . The efficacy of fluoxetine for pediatric MDD has been demonstrated in several controlled trials. 39 – 41 The results of three paroxetine trials 42 , 43 and two sertraline trials 44 suggest equivocal or weakly positive efficacy. Likewise, efficacy of citalopram was supported by one published trial, but not by an unpublished one. 38 For venlafaxine and mirtazapine, two unpublished trials for each compound did not demonstrate efficacy. 45 , 38
Primary outcome results for acute (8–12 week), placebo-controlled, pediatric studies of SSRIs and related serotonergic drugs in major depression
A landmark study, the Treatment for Adolescents with Depression Study (TADS), was a National Institute of Mental Health (NIMH)-sponsored, multisite trial comparing fluoxetine, cognitive behavioral therapy (CBT), their combination, and placebo in 439 adolescents with a primary diagnosis of major depression. 47 After 12 weeks of treatment, fluoxetine alone was shown to be effective in treating adolescent depression. However, the combination of fluoxetine and CBT was statistically superior to placebo, CBT, and fluoxetine alone. While fluoxetine may help initiate a faster treatment response, extending the study to 36 weeks showed further support for the use of the combination treatment in adolescents with moderate to severe depression. 47
Based upon these clinical trials, fluoxetine and escitalopram appear to have efficacy in the treatment of pediatric depression, with the majority of the trials demonstrating positive results. Some support for efficacy also exists for sertraline and citalopram. However, the efficacy signal for these drugs is weaker and inconsistent. It is possible the variability in outcome is similar to what is seen in adult literature, where antidepressants approved by the FDA for the treatment of adult MDD frequently have as many negative as they do positive trials. No evidence of efficacy exists for venlafaxine, paroxetine, or mirtazapine. Whether the discrepancies in treatment efficacy between the SSRIs is better explained by methodological factors or by substantive pharmacological differences continues to be debated.
Relapse prevention. Rates of recurrence of depression in youth have been found to be strikingly high among clinical and community samples, reaching 20 to 60 percent by 1 to 2 years and 70 percent after five years. 19 , 32 At least one controlled trial demonstrated a significant reduction in the risk of relapse, from 69 to 42 percent, when fluoxetine was continued beyond the acute phase of treatment, through the “continuation” phase, which extended an additional 6 to 9 months. 48 Adult studies have similiarly shown a significant reduction in relapse rates when antidepressants were continued for 6 to 9 months beyond acute treatment. As has also been reported with adults, there is a significant reduction in relapse rates for patients who receive CBT as a continuation treatment. 49
Relapse in both pediatric and adult populations is much less likely in patients who exhibit a complete response to acute treatment. On the other hand, patients with persistent residual depressive symptoms, even after meeting threshold for response to treatment criteria, are at a significantly higher risk for recurrence. 10 Thus, the goal of treatment has increasingly become total wellness or complete response. Furthermore, even subsyndromal, residual depressive symptoms are associated with meaningful impairment.
Safety data. In September 2004, when the FDA presented results of their meta-analysis of 25 trials plus TADS, safety data were presented along with efficacy data. 38 An independent team of experts utilized an approach developed by researchers at Columbia University to evaluate and recode all adverse events for suicidal and self-injurious behaviors (suicide attempt, preparatory acts, suicidal ideation, and so forth). Following reclassification, 78 of the approximately 4,400 subjects from these datasets (1.7%) were coded as experiencing either suicidal behavior (n=33) or suicidal ideation (n=45). There were no completed suicides, and only venlafaxine and fluoxetine in the TADS study exhibited a statistically significant signal for suicidality (suicide attempts or suicidal ideation). The overall relative risk (RR) for suicidality was 1.66 (95% CI; 1.02, 2.68) for MDD trials and 1.95 (1.28, 2.98) for all medication trials, for all indications. 38 The authors of the analysis concluded, “Although the difference is small, it seems likely that the effect is real, because the findings were statistically significant in aggregate and are consistent across multiple studies of various agents.” 38 The overall risk difference for the SSRIs in the MDD trials is approximately two percent. In other words, two patients of 100 treated with an SSRI for major depression would be expected to have an increase in suicidality during short-term treatment, attributable specifically to the drug. The relative risk of suicidality by specific antidepressant is listed in Table 4 . Suicidality, when it did occur, was primarily ideation, with only a minority of events involving actual suicide attempts (27 suicide attempts, 6 “preparatory actions,” and 45 suicidal ideation events).
Overall relative risks of suicidal behavior or ideation by drugs in MDD trials as defined by the Columbia University Reclassification Project 50
In addition to an increase in the risk of suicidality, SSRIs are almost twice as likely as placebo to cause increased agitation and hostility during acute treatment, with the relative risk by specific antidepressant listed in Table 5 . It remains unclear whether the increased risk for suicidality associated with these medications is mediated by the agitation and hostility symptoms. Nonetheless, it is important for patients and families to be aware of this potential.
SSRIs and pediatric depression overall relative risk of treatment emergent agitation or hostility by drug in MDD trials 50
The advisory committee to the FDA concluded that the adverse events reported voluntarily during clinical trials in aggregate indicated an increased risk of treatment-emergent suicidality. Although there was variability in the adverse event data, the committee was unable to conclude that any single antidepressant was without risk. Since the FDA’s October 2004 “black box” warning and additional recommendations regarding antidepressant use in children, other regulatory bodies in Europe and Canada have also released warnings.
TADS provided a systematic approach to collecting data on suicidality, beginning at baseline and continuing to all subsequent endpoints, allowing for a longer-term assessment of the role of various treatments on suicide. At baseline, clinically significant suicidal thinking was present in 29 percent of the sample. Suicidality declined significantly in all four treatment groups with fluoxetine plus CBT showing the greatest reduction ( p =0.02). There were no completed suicides in the course of the study, but 24 (5.5%) of the 439 TADS patients experienced a suicide-related event. Seven (7) of the 24 suicide-related events were suicide attempts (1.6% of the total sample). Four (4) of the attempts were by patients assigned to fluoxetine and CBT, two to fluoxetine alone, and one to CBT alone. None of the subjects taking placebo attempted suicide.
Harm-related events, which included thoughts or behaviors related to harm of self as well as harm to others, occurred in 11.9 percent of those assigned to fluoxetine alone, 8.4 percent fluoxetine with CBT, 4.5 percent CBT alone, and 5.4 percent placebo. Overall, suicidality decreased with treatment. Improvement was greatest for those receiving combination treatment and least for those receiving fluoxetine alone. It is important to note that, though fluoxetine did not appear to increase suicidal ideation, the harm-related adverse events did occur more frequently in fluoxetine-treated patients. The TADS data indicated that the addition of CBT enhanced the safety of depression treatment over medication alone. 51
Epidemiological and observational data. Whereas the pediatric use of antidepressants had been substantially increasing throughout the previous decade, youth suicide rates had been declining. During 1992 to 2001, for example, the overall suicide rate among persons 10 to 19 years of age declined from 6.2 to 4.6 per 100,000 population. 52 Each one-percent increase in antidepressant use was associated with a decrease of 0.23 suicides per 100,000 adolescents per year. 53 , 54 A review of National Vital Statistics from the Centers for Disease Control and Prevention analyzed records of all US individuals at the county level who committed suicide between 1996 and 1998, examining the association between antidepressant prescription and suicide rate. 55 The data demonstrated lower suicide rates in association with increased use of SSRIs and new-generation non-SSRIs, compared to TCA use. A study of suicide in more than 5,000 adults found that, most often, antidepressants had not been taken immediately before death, even though the majority of the persons had been depressed. A study of 14,857 suicides and 26,422 other deaths in Sweden found that none of the 15 suicides below the age of 15 years had an SSRI detected on toxicology. 56 In a study of 49 adolescent suicides in Utah, 24 percent had been prescribed antidepressants, but none had tested positive for SSRIs at the time of death. 57 Most postmortem studies in adults have found that more than 80 percent of depressed patients at the time of suicide are not on antidepressants. 58
In October 2003, the FDA issued a public health advisory or “black box” warning about the risk of suicidality in pediatric patients taking SSRIs. From 1999 to 2004, pediatric diagnoses of depression increased from 3 to 5 per 1,000. After the FDA advisory, the rates decreased back to 1999 levels, a trend which deviated from historical patterns. Most of the reduction was accounted for by a decrease in depressive diagnoses made by primary care physicians. Among youth diagnosed with depression, the proportion who received no antidepressants increased to three times the rate predicted by the preadvisory trend. SSRI prescription rates were 58-percent lower than predicted by preadvisory trends. However, there was no evidence of any increase in the use of nonantidepressant treatment alternatives. In sum, the advisory was associated with significant reductions in the rates of diagnosis and treatment of pediatric depression. In the US, suicide rates among youth 19 years and younger, increased 18.2 percent between 2003 and 2004, the first significant rise in teen suicide in more than a decade and the largest one-year change in suicide rate in a quarter century. 52
Risk of nontreatment. While considering the potential risks and benefits of treatment, it is also important to reflect on the risk of not treating MDD. Suicide is the third-leading cause of death among adolescents 15 to 19 years of age, and fourth-leading cause of death among 10 to 14 year olds. 3 One study, which followed depressed pediatric subjects into adulthood, demonstrated a suicide risk of 2.45 percent, with 44.3 percent of the sample attempting suicide at least once in their lives. 32 Other studies have also demonstrated an elevated risk of suicide and psychiatric comorbidity in long-term follow-up studies of depression. 11 , 19 , 23 During a period spanning 10 years between adolescence and early adulthood, one group of researchers estimated a five-fold increased likelihood of suicide attempts associated with pediatric depression as well as a high rate of completed suicide (7.7%). 7 Prepubertal children with an earlier age of MDD onset are also at increased risk for substance abuse, conduct disorder, impaired functioning, and need for long-term psychiatric and medical services. 5 Since the “black box” warning issued by the FDA in October 2004, prescription rates for SSRIs have fallen dramatically while concurrently youth suicides have significantly increased. 54
Summary of risk-benefit analysis of pharmacologic treatment. Analyses of suicidality adverse events collected in the pediatric antidepressant trials have demonstrated an elevation in suicidality when placebo was compared to active medication. 38 Systematic and repeated assessments of suicidality using symptom rating scales, however, have not supported this finding. 59 In fact, when these data were collected in TADS at baseline, 6 weeks, and 12 weeks, all four treatment groups demonstrated a decline in suicidality, with the greatest decline occurring in the group receiving fluoxetine with CBT. Also of interest are the epidemiological and observational data, which demonstrate an increase in the use of SSRIs in the pediatric population but no corresponding increase in completed suicides. 60 In fact, studies have generally identified an inverse correlation, both nationally and regionally, with suicide and antidepressant usage.
Psychosocial Treatments
CBT . CBT is an umbrella term for a number of psychotherapeutic strategies based on the assumption that depression is caused or maintained by negative and distorted cognitions and dysfunctional behaviors. The theoretical framework for CBT maintains that thoughts, feelings, and behavior are interrelated. Treatment is generally here-and-now focused and often includes teaching psychosocial and relaxation skills in addition to the analysis of cognition and behavior. CBT for depression is based on the presumption that depressive symptoms will decrease through interventions that modify dysfunctional thought and behavior patterns. Meta-analyses of randomized, controlled trials of CBT for depressed adolescents have concluded that there is strong evidence supporting efficacy of CBT to treat pediatric depression, 61 – 63 with effect sizes generally in the moderate to large range, ranging from 1.02 to 1.27, at the end of the acute treatment Additionally, higher rates of remission from depression have been associated with CBT 64 compared to other types of psychotherapy. There is also data suggesting that CBT has a protective effect against suicide attempts in teens. 65
Several groups have directly compared CBT to other forms of psychotherapy. 66 , 67 These studies have consistently demonstrated superiority of CBT over other forms of treatment, which have included supportive therapy, relaxation training, and family therapy. Studies that have examined CBT delivered in group format have shown comparable efficacy to CBT administered individually. A meta-analysis of psychotherapy in general for child and adolescent depression revealed a modest mean effect size of 0.34, suggesting that perhaps noncognitive treatments have effects less robust than cognitive treatments.
TADS compared CBT with medication. At the end of the 12-week, blinded, acute phase, CBT alone was less effective than fluoxetine but CBT and fluoxetine alone were equivalent at 18 and at 36 weeks. A combination of medication and CBT performed best at all three time intervals. 51 In this study, medication appeared to accelerate the treatment response, with the addition of CBT enhancing the overall efficacy of the treatment over time as well as to the safety of the patients. Possible explanations for the relatively poor early showing of CBT in TADS is the high severity of psychopathology in subjects and the fact that comorbid DD was nearly three times higher in the CBT-alone group than in the fluoxetine-alone group. Other explanations are that the CBT was highly structured and mainly emphasized skill acquisition, whereas in previous studies the treatments were more flexible and emphasized behavioral changes and cognitive restructuring to a greater degree. Finally, CBT outcomes varied significantly between sites, with the site responsible for developing the CBT manuals experiencing the most success, perhaps suggesting inconsistent levels of therapist expertise among sites.
Interpersonal psychotherapy for adolescents (IPT-A). IPT-A is a psychotherapeutic intervention developed for depressed teens based on a well-established, time-limited, focused treatment for depressed nonbipolar adult outpatients. A central tenet of IPT-A is that clinical depression occurs in an interpersonal context and that response to treatment is influenced by the interpersonal relations between the patient and significant others. The goals of IPT-A are to reduce depressive symptoms and improve interpersonal functioning. IPT-A has been noted to be efficacious in the acute treatment of depressed adolescents in several controlled trials. 68 , 69 There is evidence of the maintenance of improvement at one year follow up, with associated reduction in hospitalization rates and suicidality. 70
A recent effectiveness study has compared IPT-A with treatment as usual in the school-based health clinics in New York City as delivered by the clinicians employed in school-based clinics. 71 Treatment as usual consisted of the psychological treatment the adolescents would have received had the study not been in place (generally supportive, individual counseling). Adolescents treated with IPT-A compared with treatment as usual showed greater symptom reduction, significantly better social functioning, and greater decrease in clinical severity of depression and improvement in overall functioning. In addition, the study demonstrated the ability to train community clinicians to deliver IPT-A effectively, thereby demonstrating the transportability of IPT-A from the university lab setting to the community. 35
IPT-A also has been adapted to a group format (IPT-AG). Mufson et al 72 recently completed a pilot, controlled, clinical trial demonstrating the feasibility and efficacy of IPT-AG for the treatment of adolescents with depressive disorders. Group IPT-AG offers the potential for increasing access while simultaneously optimizing utilization of resources and cost effectiveness.
Family therapy. Few family-based therapies exist for adolescent depression, and their results are inconsistent. One research group reported that children who participated in monthly family meetings as an adjunctive to their individual CBT had a greater reduction in depressive symptoms, compared with the control group. 73 Other research has demonstrated that an adjunctive multifamily psychoeducation group for families of children with mood disorders increased knowledge, improved family relations, increased child-perceived support from the parents, and increased treatment adherence. 74 Family psychoeducation has been shown to have positive effects on family interactions, which have been postulated to mediate the clinical course of MDD in youth. 75 In contrast, other authors have found no additional benefits to adding a parent-training group to a CBT skills-training group for adolescents. 67 Systemic behavioral family therapy was no better than supportive therapy in reducing depression symptoms in pediatric patients.
Treatment of suicidal behavior and ideation. CBT and dialectical behavioral therapy (DBT) have been found to be effective in reducing suicide attempts among adults. 76 , 77 Until recently, suicidal adolescents have been excluded from clinical trials. Even when suicidal adolescents were included in samples, few of the studies assessed suicidal ideation and behavior as an outcome.
One group of researchers found that permitting adolescents to immediately rehospitalize themselves if needed was not associated with a significant reduction in suicide attempts at one-year follow up. 78 Other research compared adolescent suicide attempters treated with brief cognitive-behavioral family therapy, either alone or in combination with a emergency room intervention designed to increase adherence. 79 The combination of the family and emergency room intervention resulted in lower rates of depression and suicidality, as well as improved adherence, lower maternal depression, and improved family interaction compared with the family-intervention alone.
In one large-scale study of depressed adolescents, 35 to 40 percent of teens had significant suicidal ideation with a plan or a recent attempt at intake across the three treatments (individual CBT, family therapy, supportive therapy). 65 A substantial reduction in suicidal ideation occurred across the three treatments but there was no differential reduction by treatment.
In TADS, 29 percent of the depressed subjects had clinically significant suicidal ideation upon study entry. 59 Combined treatment (fluoxetine and CBT) was found to be superior to both monotherapies and to placebo in treating depression, whereas neither monotherapy was different from the other or from placebo in reducing suicidal ideation.
Julia and her mother chose to begin antidepressant medication along with CBT-focused psychotherapy. They also agreed to have some additional family therapy sessions in order to improve their relationship and the way they communicate with each other. As Julia began to feel better, she stopped using alcohol and marijuana. Concerned about the rest of the family, Julia’s mother asked whether there are ways to prevent depression.
Depression and suicidality in youth are significant public health issues. Prevention strategies targeting at-risk youth have demonstrated greater success than interventions applied universally, suggesting a role for routine screening of depression in primary care settings. Fluoxetine and, most recently, escitalopram have accumulated adequate efficacy and safety data to merit FDA-approved indication for the treatment of pediatric depression. The psychotherapeutic treatments shown to be most effective for adolescent depression include CBT and IPT-A. While there have been few empirical studies on the treatment of suicidal behavior among adolescents, the current data suggest that reduced suicidality is associated with successful treatment of depression. When contemplating the risks and benefits of the various treatments, one must also consider the risks on nontreatment, which are likely to be substantial.
Contributor Information
Mary N. Cook, Dr. Cook is Medical Director of Clinical Services, Psychiatry and Behavioral Sciences Department, The Children’s Hospital, Denver, Colorado, and Assistant Professor, Department of Psychiatry, University of Colorado, School of Medicine, Denver, Colorado.
John Peterson, Dr. Peterson is Director, Child/Adolescent Psychiatry, Denver Health Medical Center, and Associate Professor, Department of Psychiatry, University of Colorado, School of Medicine, Denver, Colorado.
Christopher Sheldon, Dr. Sheldon is Chief Psychologist and Training Director, Denver Health Medical Center, and Assistant Professor, Department of Psychiatry, University of Colorado, School of Medicine, Denver, Colorado.
End the Phone-Based Childhood Now
The environment in which kids grow up today is hostile to human development.

Listen to this article
Produced by ElevenLabs and News Over Audio (NOA) using AI narration.
This article was featured in the One Story to Read Today newsletter. Sign up for it here .
S omething went suddenly and horribly wrong for adolescents in the early 2010s. By now you’ve likely seen the statistics : Rates of depression and anxiety in the United States—fairly stable in the 2000s—rose by more than 50 percent in many studies from 2010 to 2019. The suicide rate rose 48 percent for adolescents ages 10 to 19. For girls ages 10 to 14, it rose 131 percent.
The problem was not limited to the U.S.: Similar patterns emerged around the same time in Canada, the U.K., Australia, New Zealand , the Nordic countries , and beyond . By a variety of measures and in a variety of countries, the members of Generation Z (born in and after 1996) are suffering from anxiety, depression, self-harm, and related disorders at levels higher than any other generation for which we have data.
The decline in mental health is just one of many signs that something went awry. Loneliness and friendlessness among American teens began to surge around 2012. Academic achievement went down, too. According to “The Nation’s Report Card,” scores in reading and math began to decline for U.S. students after 2012, reversing decades of slow but generally steady increase. PISA, the major international measure of educational trends, shows that declines in math, reading, and science happened globally, also beginning in the early 2010s.
Read: It sure looks like phones are making students dumber
As the oldest members of Gen Z reach their late 20s, their troubles are carrying over into adulthood. Young adults are dating less , having less sex, and showing less interest in ever having children than prior generations. They are more likely to live with their parents. They were less likely to get jobs as teens , and managers say they are harder to work with. Many of these trends began with earlier generations, but most of them accelerated with Gen Z.
Surveys show that members of Gen Z are shyer and more risk averse than previous generations, too, and risk aversion may make them less ambitious. In an interview last May , OpenAI co-founder Sam Altman and Stripe co-founder Patrick Collison noted that, for the first time since the 1970s, none of Silicon Valley’s preeminent entrepreneurs are under 30. “Something has really gone wrong,” Altman said. In a famously young industry, he was baffled by the sudden absence of great founders in their 20s.
Generations are not monolithic, of course. Many young people are flourishing. Taken as a whole, however, Gen Z is in poor mental health and is lagging behind previous generations on many important metrics. And if a generation is doing poorly––if it is more anxious and depressed and is starting families, careers, and important companies at a substantially lower rate than previous generations––then the sociological and economic consequences will be profound for the entire society.
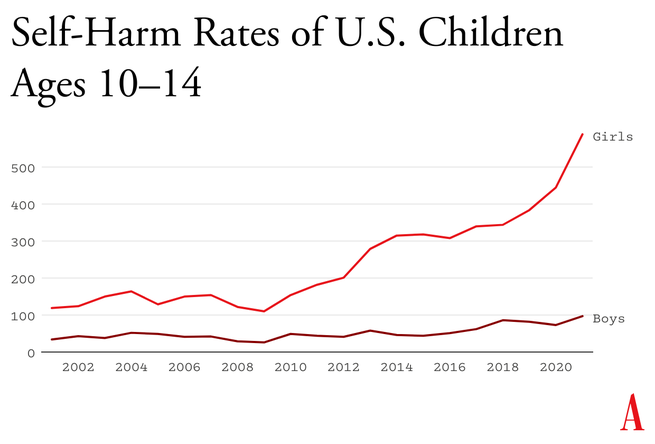
What happened in the early 2010s that altered adolescent development and worsened mental health? Theories abound , but the fact that similar trends are found in many countries worldwide means that events and trends that are specific to the United States cannot be the main story.
I think the answer can be stated simply, although the underlying psychology is complex: Those were the years when adolescents in rich countries traded in their flip phones for smartphones and moved much more of their social lives online—particularly onto social-media platforms designed for virality and addiction . Once young people began carrying the entire internet in their pockets, available to them day and night, it altered their daily experiences and developmental pathways across the board. Friendship, dating, sexuality, exercise, sleep, academics, politics, family dynamics, identity—all were affected. Life changed rapidly for younger children, too, as they began to get access to their parents’ smartphones and, later, got their own iPads, laptops, and even smartphones during elementary school.
Jonathan Haidt: Get phones out of schools now
Related Podcast
As a social psychologist who has long studied social and moral development, I have been involved in debates about the effects of digital technology for years. Typically, the scientific questions have been framed somewhat narrowly, to make them easier to address with data. For example, do adolescents who consume more social media have higher levels of depression? Does using a smartphone just before bedtime interfere with sleep? The answer to these questions is usually found to be yes, although the size of the relationship is often statistically small, which has led some researchers to conclude that these new technologies are not responsible for the gigantic increases in mental illness that began in the early 2010s.
But before we can evaluate the evidence on any one potential avenue of harm, we need to step back and ask a broader question: What is childhood––including adolescence––and how did it change when smartphones moved to the center of it? If we take a more holistic view of what childhood is and what young children, tweens, and teens need to do to mature into competent adults, the picture becomes much clearer. Smartphone-based life, it turns out, alters or interferes with a great number of developmental processes.
The intrusion of smartphones and social media are not the only changes that have deformed childhood. There’s an important backstory, beginning as long ago as the 1980s, when we started systematically depriving children and adolescents of freedom, unsupervised play, responsibility, and opportunities for risk taking, all of which promote competence, maturity, and mental health. But the change in childhood accelerated in the early 2010s, when an already independence-deprived generation was lured into a new virtual universe that seemed safe to parents but in fact is more dangerous, in many respects, than the physical world.
My claim is that the new phone-based childhood that took shape roughly 12 years ago is making young people sick and blocking their progress to flourishing in adulthood. We need a dramatic cultural correction, and we need it now.
Brain development is sometimes said to be “experience-expectant,” because specific parts of the brain show increased plasticity during periods of life when an animal’s brain can “expect” to have certain kinds of experiences. You can see this with baby geese, who will imprint on whatever mother-sized object moves in their vicinity just after they hatch. You can see it with human children, who are able to learn languages quickly and take on the local accent, but only through early puberty; after that, it’s hard to learn a language and sound like a native speaker. There is also some evidence of a sensitive period for cultural learning more generally. Japanese children who spent a few years in California in the 1970s came to feel “American” in their identity and ways of interacting only if they attended American schools for a few years between ages 9 and 15. If they left before age 9, there was no lasting impact. If they didn’t arrive until they were 15, it was too late; they didn’t come to feel American.
Human childhood is an extended cultural apprenticeship with different tasks at different ages all the way through puberty. Once we see it this way, we can identify factors that promote or impede the right kinds of learning at each age. For children of all ages, one of the most powerful drivers of learning is the strong motivation to play. Play is the work of childhood, and all young mammals have the same job: to wire up their brains by playing vigorously and often, practicing the moves and skills they’ll need as adults. Kittens will play-pounce on anything that looks like a mouse tail. Human children will play games such as tag and sharks and minnows, which let them practice both their predator skills and their escaping-from-predator skills. Adolescents will play sports with greater intensity, and will incorporate playfulness into their social interactions—flirting, teasing, and developing inside jokes that bond friends together. Hundreds of studies on young rats, monkeys, and humans show that young mammals want to play, need to play, and end up socially, cognitively, and emotionally impaired when they are deprived of play .
One crucial aspect of play is physical risk taking. Children and adolescents must take risks and fail—often—in environments in which failure is not very costly. This is how they extend their abilities, overcome their fears, learn to estimate risk, and learn to cooperate in order to take on larger challenges later. The ever-present possibility of getting hurt while running around, exploring, play-fighting, or getting into a real conflict with another group adds an element of thrill, and thrilling play appears to be the most effective kind for overcoming childhood anxieties and building social, emotional, and physical competence. The desire for risk and thrill increases in the teen years, when failure might carry more serious consequences. Children of all ages need to choose the risk they are ready for at a given moment. Young people who are deprived of opportunities for risk taking and independent exploration will, on average, develop into more anxious and risk-averse adults .
From the April 2014 issue: The overprotected kid
Human childhood and adolescence evolved outdoors, in a physical world full of dangers and opportunities. Its central activities––play, exploration, and intense socializing––were largely unsupervised by adults, allowing children to make their own choices, resolve their own conflicts, and take care of one another. Shared adventures and shared adversity bound young people together into strong friendship clusters within which they mastered the social dynamics of small groups, which prepared them to master bigger challenges and larger groups later on.
And then we changed childhood.
The changes started slowly in the late 1970s and ’80s, before the arrival of the internet, as many parents in the U.S. grew fearful that their children would be harmed or abducted if left unsupervised. Such crimes have always been extremely rare, but they loomed larger in parents’ minds thanks in part to rising levels of street crime combined with the arrival of cable TV, which enabled round-the-clock coverage of missing-children cases. A general decline in social capital ––the degree to which people knew and trusted their neighbors and institutions–– exacerbated parental fears . Meanwhile, rising competition for college admissions encouraged more intensive forms of parenting . In the 1990s, American parents began pulling their children indoors or insisting that afternoons be spent in adult-run enrichment activities. Free play, independent exploration, and teen-hangout time declined.
In recent decades, seeing unchaperoned children outdoors has become so novel that when one is spotted in the wild, some adults feel it is their duty to call the police. In 2015, the Pew Research Center found that parents, on average, believed that children should be at least 10 years old to play unsupervised in front of their house, and that kids should be 14 before being allowed to go unsupervised to a public park. Most of these same parents had enjoyed joyous and unsupervised outdoor play by the age of 7 or 8.
But overprotection is only part of the story. The transition away from a more independent childhood was facilitated by steady improvements in digital technology, which made it easier and more inviting for young people to spend a lot more time at home, indoors, and alone in their rooms. Eventually, tech companies got access to children 24/7. They developed exciting virtual activities, engineered for “engagement,” that are nothing like the real-world experiences young brains evolved to expect.

The first wave came ashore in the 1990s with the arrival of dial-up internet access, which made personal computers good for something beyond word processing and basic games. By 2003, 55 percent of American households had a computer with (slow) internet access. Rates of adolescent depression, loneliness, and other measures of poor mental health did not rise in this first wave. If anything, they went down a bit. Millennial teens (born 1981 through 1995), who were the first to go through puberty with access to the internet, were psychologically healthier and happier, on average, than their older siblings or parents in Generation X (born 1965 through 1980).
The second wave began to rise in the 2000s, though its full force didn’t hit until the early 2010s. It began rather innocently with the introduction of social-media platforms that helped people connect with their friends. Posting and sharing content became much easier with sites such as Friendster (launched in 2003), Myspace (2003), and Facebook (2004).
Teens embraced social media soon after it came out, but the time they could spend on these sites was limited in those early years because the sites could only be accessed from a computer, often the family computer in the living room. Young people couldn’t access social media (and the rest of the internet) from the school bus, during class time, or while hanging out with friends outdoors. Many teens in the early-to-mid-2000s had cellphones, but these were basic phones (many of them flip phones) that had no internet access. Typing on them was difficult––they had only number keys. Basic phones were tools that helped Millennials meet up with one another in person or talk with each other one-on-one. I have seen no evidence to suggest that basic cellphones harmed the mental health of Millennials.
It was not until the introduction of the iPhone (2007), the App Store (2008), and high-speed internet (which reached 50 percent of American homes in 2007 )—and the corresponding pivot to mobile made by many providers of social media, video games, and porn—that it became possible for adolescents to spend nearly every waking moment online. The extraordinary synergy among these innovations was what powered the second technological wave. In 2011, only 23 percent of teens had a smartphone. By 2015, that number had risen to 73 percent , and a quarter of teens said they were online “almost constantly.” Their younger siblings in elementary school didn’t usually have their own smartphones, but after its release in 2010, the iPad quickly became a staple of young children’s daily lives. It was in this brief period, from 2010 to 2015, that childhood in America (and many other countries) was rewired into a form that was more sedentary, solitary, virtual, and incompatible with healthy human development.
In the 2000s, Silicon Valley and its world-changing inventions were a source of pride and excitement in America. Smart and ambitious young people around the world wanted to move to the West Coast to be part of the digital revolution. Tech-company founders such as Steve Jobs and Sergey Brin were lauded as gods, or at least as modern Prometheans, bringing humans godlike powers. The Arab Spring bloomed in 2011 with the help of decentralized social platforms, including Twitter and Facebook. When pundits and entrepreneurs talked about the power of social media to transform society, it didn’t sound like a dark prophecy.
You have to put yourself back in this heady time to understand why adults acquiesced so readily to the rapid transformation of childhood. Many parents had concerns , even then, about what their children were doing online, especially because of the internet’s ability to put children in contact with strangers. But there was also a lot of excitement about the upsides of this new digital world. If computers and the internet were the vanguards of progress, and if young people––widely referred to as “digital natives”––were going to live their lives entwined with these technologies, then why not give them a head start? I remember how exciting it was to see my 2-year-old son master the touch-and-swipe interface of my first iPhone in 2008. I thought I could see his neurons being woven together faster as a result of the stimulation it brought to his brain, compared to the passivity of watching television or the slowness of building a block tower. I thought I could see his future job prospects improving.
Touchscreen devices were also a godsend for harried parents. Many of us discovered that we could have peace at a restaurant, on a long car trip, or at home while making dinner or replying to emails if we just gave our children what they most wanted: our smartphones and tablets. We saw that everyone else was doing it and figured it must be okay.
It was the same for older children, desperate to join their friends on social-media platforms, where the minimum age to open an account was set by law to 13, even though no research had been done to establish the safety of these products for minors. Because the platforms did nothing (and still do nothing) to verify the stated age of new-account applicants, any 10-year-old could open multiple accounts without parental permission or knowledge, and many did. Facebook and later Instagram became places where many sixth and seventh graders were hanging out and socializing. If parents did find out about these accounts, it was too late. Nobody wanted their child to be isolated and alone, so parents rarely forced their children to shut down their accounts.
We had no idea what we were doing.
The numbers are hard to believe. The most recent Gallup data show that American teens spend about five hours a day just on social-media platforms (including watching videos on TikTok and YouTube). Add in all the other phone- and screen-based activities, and the number rises to somewhere between seven and nine hours a day, on average . The numbers are even higher in single-parent and low-income families, and among Black, Hispanic, and Native American families.
These very high numbers do not include time spent in front of screens for school or homework, nor do they include all the time adolescents spend paying only partial attention to events in the real world while thinking about what they’re missing on social media or waiting for their phones to ping. Pew reports that in 2022, one-third of teens said they were on one of the major social-media sites “almost constantly,” and nearly half said the same of the internet in general. For these heavy users, nearly every waking hour is an hour absorbed, in full or in part, by their devices.

In Thoreau’s terms, how much of life is exchanged for all this screen time? Arguably, most of it. Everything else in an adolescent’s day must get squeezed down or eliminated entirely to make room for the vast amount of content that is consumed, and for the hundreds of “friends,” “followers,” and other network connections that must be serviced with texts, posts, comments, likes, snaps, and direct messages. I recently surveyed my students at NYU, and most of them reported that the very first thing they do when they open their eyes in the morning is check their texts, direct messages, and social-media feeds. It’s also the last thing they do before they close their eyes at night. And it’s a lot of what they do in between.
The amount of time that adolescents spend sleeping declined in the early 2010s , and many studies tie sleep loss directly to the use of devices around bedtime, particularly when they’re used to scroll through social media . Exercise declined , too, which is unfortunate because exercise, like sleep, improves both mental and physical health. Book reading has been declining for decades, pushed aside by digital alternatives, but the decline, like so much else, sped up in the early 2010 s. With passive entertainment always available, adolescent minds likely wander less than they used to; contemplation and imagination might be placed on the list of things winnowed down or crowded out.
But perhaps the most devastating cost of the new phone-based childhood was the collapse of time spent interacting with other people face-to-face. A study of how Americans spend their time found that, before 2010, young people (ages 15 to 24) reported spending far more time with their friends (about two hours a day, on average, not counting time together at school) than did older people (who spent just 30 to 60 minutes with friends). Time with friends began decreasing for young people in the 2000s, but the drop accelerated in the 2010s, while it barely changed for older people. By 2019, young people’s time with friends had dropped to just 67 minutes a day. It turns out that Gen Z had been socially distancing for many years and had mostly completed the project by the time COVID-19 struck.
Read: What happens when kids don’t see their peers for months
You might question the importance of this decline. After all, isn’t much of this online time spent interacting with friends through texting, social media, and multiplayer video games? Isn’t that just as good?
Some of it surely is, and virtual interactions offer unique benefits too, especially for young people who are geographically or socially isolated. But in general, the virtual world lacks many of the features that make human interactions in the real world nutritious, as we might say, for physical, social, and emotional development. In particular, real-world relationships and social interactions are characterized by four features—typical for hundreds of thousands of years—that online interactions either distort or erase.
First, real-world interactions are embodied , meaning that we use our hands and facial expressions to communicate, and we learn to respond to the body language of others. Virtual interactions, in contrast, mostly rely on language alone. No matter how many emojis are offered as compensation, the elimination of communication channels for which we have eons of evolutionary programming is likely to produce adults who are less comfortable and less skilled at interacting in person.
Second, real-world interactions are synchronous ; they happen at the same time. As a result, we learn subtle cues about timing and conversational turn taking. Synchronous interactions make us feel closer to the other person because that’s what getting “in sync” does. Texts, posts, and many other virtual interactions lack synchrony. There is less real laughter, more room for misinterpretation, and more stress after a comment that gets no immediate response.
Third, real-world interactions primarily involve one‐to‐one communication , or sometimes one-to-several. But many virtual communications are broadcast to a potentially huge audience. Online, each person can engage in dozens of asynchronous interactions in parallel, which interferes with the depth achieved in all of them. The sender’s motivations are different, too: With a large audience, one’s reputation is always on the line; an error or poor performance can damage social standing with large numbers of peers. These communications thus tend to be more performative and anxiety-inducing than one-to-one conversations.
Finally, real-world interactions usually take place within communities that have a high bar for entry and exit , so people are strongly motivated to invest in relationships and repair rifts when they happen. But in many virtual networks, people can easily block others or quit when they are displeased. Relationships within such networks are usually more disposable.
From the September 2015 issue: The coddling of the American mind
These unsatisfying and anxiety-producing features of life online should be recognizable to most adults. Online interactions can bring out antisocial behavior that people would never display in their offline communities. But if life online takes a toll on adults, just imagine what it does to adolescents in the early years of puberty, when their “experience expectant” brains are rewiring based on feedback from their social interactions.
Kids going through puberty online are likely to experience far more social comparison, self-consciousness, public shaming, and chronic anxiety than adolescents in previous generations, which could potentially set developing brains into a habitual state of defensiveness. The brain contains systems that are specialized for approach (when opportunities beckon) and withdrawal (when threats appear or seem likely). People can be in what we might call “discover mode” or “defend mode” at any moment, but generally not both. The two systems together form a mechanism for quickly adapting to changing conditions, like a thermostat that can activate either a heating system or a cooling system as the temperature fluctuates. Some people’s internal thermostats are generally set to discover mode, and they flip into defend mode only when clear threats arise. These people tend to see the world as full of opportunities. They are happier and less anxious. Other people’s internal thermostats are generally set to defend mode, and they flip into discover mode only when they feel unusually safe. They tend to see the world as full of threats and are more prone to anxiety and depressive disorders.
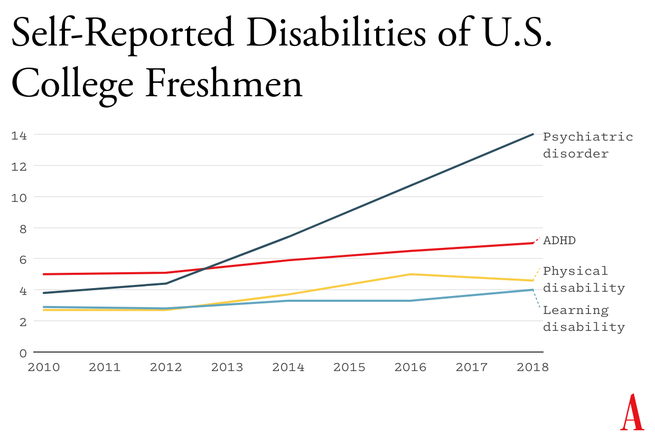
A simple way to understand the differences between Gen Z and previous generations is that people born in and after 1996 have internal thermostats that were shifted toward defend mode. This is why life on college campuses changed so suddenly when Gen Z arrived, beginning around 2014. Students began requesting “safe spaces” and trigger warnings. They were highly sensitive to “microaggressions” and sometimes claimed that words were “violence.” These trends mystified those of us in older generations at the time, but in hindsight, it all makes sense. Gen Z students found words, ideas, and ambiguous social encounters more threatening than had previous generations of students because we had fundamentally altered their psychological development.
Staying on task while sitting at a computer is hard enough for an adult with a fully developed prefrontal cortex. It is far more difficult for adolescents in front of their laptop trying to do homework. They are probably less intrinsically motivated to stay on task. They’re certainly less able, given their undeveloped prefrontal cortex, and hence it’s easy for any company with an app to lure them away with an offer of social validation or entertainment. Their phones are pinging constantly— one study found that the typical adolescent now gets 237 notifications a day, roughly 15 every waking hour. Sustained attention is essential for doing almost anything big, creative, or valuable, yet young people find their attention chopped up into little bits by notifications offering the possibility of high-pleasure, low-effort digital experiences.
It even happens in the classroom. Studies confirm that when students have access to their phones during class time, they use them, especially for texting and checking social media, and their grades and learning suffer . This might explain why benchmark test scores began to decline in the U.S. and around the world in the early 2010s—well before the pandemic hit.
The neural basis of behavioral addiction to social media or video games is not exactly the same as chemical addiction to cocaine or opioids. Nonetheless, they all involve abnormally heavy and sustained activation of dopamine neurons and reward pathways. Over time, the brain adapts to these high levels of dopamine; when the child is not engaged in digital activity, their brain doesn’t have enough dopamine, and the child experiences withdrawal symptoms. These generally include anxiety, insomnia, and intense irritability. Kids with these kinds of behavioral addictions often become surly and aggressive, and withdraw from their families into their bedrooms and devices.
Social-media and gaming platforms were designed to hook users. How successful are they? How many kids suffer from digital addictions?
The main addiction risks for boys seem to be video games and porn. “ Internet gaming disorder ,” which was added to the main diagnosis manual of psychiatry in 2013 as a condition for further study, describes “significant impairment or distress” in several aspects of life, along with many hallmarks of addiction, including an inability to reduce usage despite attempts to do so. Estimates for the prevalence of IGD range from 7 to 15 percent among adolescent boys and young men. As for porn, a nationally representative survey of American adults published in 2019 found that 7 percent of American men agreed or strongly agreed with the statement “I am addicted to pornography”—and the rates were higher for the youngest men.
Girls have much lower rates of addiction to video games and porn, but they use social media more intensely than boys do. A study of teens in 29 nations found that between 5 and 15 percent of adolescents engage in what is called “problematic social media use,” which includes symptoms such as preoccupation, withdrawal symptoms, neglect of other areas of life, and lying to parents and friends about time spent on social media. That study did not break down results by gender, but many others have found that rates of “problematic use” are higher for girls.
Jonathan Haidt: The dangerous experiment on teen girls
I don’t want to overstate the risks: Most teens do not become addicted to their phones and video games. But across multiple studies and across genders, rates of problematic use come out in the ballpark of 5 to 15 percent. Is there any other consumer product that parents would let their children use relatively freely if they knew that something like one in 10 kids would end up with a pattern of habitual and compulsive use that disrupted various domains of life and looked a lot like an addiction?
During that crucial sensitive period for cultural learning, from roughly ages 9 through 15, we should be especially thoughtful about who is socializing our children for adulthood. Instead, that’s when most kids get their first smartphone and sign themselves up (with or without parental permission) to consume rivers of content from random strangers. Much of that content is produced by other adolescents, in blocks of a few minutes or a few seconds.
This rerouting of enculturating content has created a generation that is largely cut off from older generations and, to some extent, from the accumulated wisdom of humankind, including knowledge about how to live a flourishing life. Adolescents spend less time steeped in their local or national culture. They are coming of age in a confusing, placeless, ahistorical maelstrom of 30-second stories curated by algorithms designed to mesmerize them. Without solid knowledge of the past and the filtering of good ideas from bad––a process that plays out over many generations––young people will be more prone to believe whatever terrible ideas become popular around them, which might explain why v ideos showing young people reacting positively to Osama bin Laden’s thoughts about America were trending on TikTok last fall.
All this is made worse by the fact that so much of digital public life is an unending supply of micro dramas about somebody somewhere in our country of 340 million people who did something that can fuel an outrage cycle, only to be pushed aside by the next. It doesn’t add up to anything and leaves behind only a distorted sense of human nature and affairs.
When our public life becomes fragmented, ephemeral, and incomprehensible, it is a recipe for anomie, or normlessness. The great French sociologist Émile Durkheim showed long ago that a society that fails to bind its people together with some shared sense of sacredness and common respect for rules and norms is not a society of great individual freedom; it is, rather, a place where disoriented individuals have difficulty setting goals and exerting themselves to achieve them. Durkheim argued that anomie was a major driver of suicide rates in European countries. Modern scholars continue to draw on his work to understand suicide rates today.
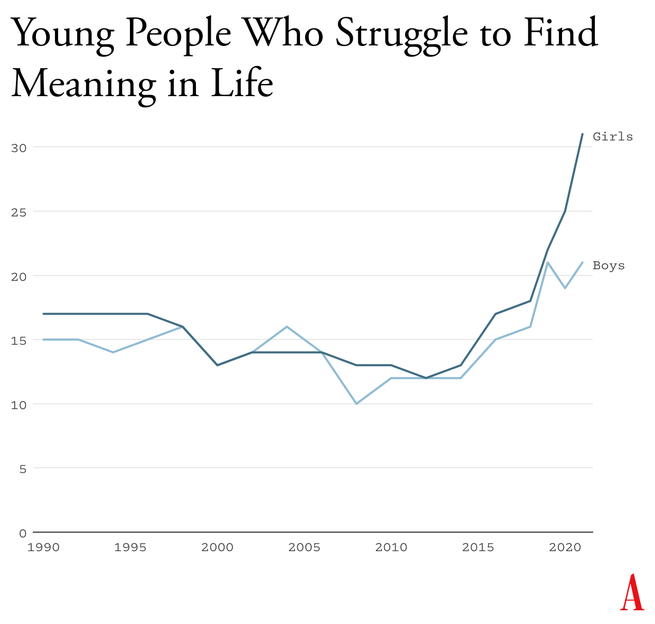
Durkheim’s observations are crucial for understanding what happened in the early 2010s. A long-running survey of American teens found that , from 1990 to 2010, high-school seniors became slightly less likely to agree with statements such as “Life often feels meaningless.” But as soon as they adopted a phone-based life and many began to live in the whirlpool of social media, where no stability can be found, every measure of despair increased. From 2010 to 2019, the number who agreed that their lives felt “meaningless” increased by about 70 percent, to more than one in five.
An additional source of evidence comes from Gen Z itself. With all the talk of regulating social media, raising age limits, and getting phones out of schools, you might expect to find many members of Gen Z writing and speaking out in opposition. I’ve looked for such arguments and found hardly any. In contrast, many young adults tell stories of devastation.
Freya India, a 24-year-old British essayist who writes about girls, explains how social-media sites carry girls off to unhealthy places: “It seems like your child is simply watching some makeup tutorials, following some mental health influencers, or experimenting with their identity. But let me tell you: they are on a conveyor belt to someplace bad. Whatever insecurity or vulnerability they are struggling with, they will be pushed further and further into it.” She continues:
Gen Z were the guinea pigs in this uncontrolled global social experiment. We were the first to have our vulnerabilities and insecurities fed into a machine that magnified and refracted them back at us, all the time, before we had any sense of who we were. We didn’t just grow up with algorithms. They raised us. They rearranged our faces. Shaped our identities. Convinced us we were sick.
Rikki Schlott, a 23-year-old American journalist and co-author of The Canceling of the American Mind , writes ,
The day-to-day life of a typical teen or tween today would be unrecognizable to someone who came of age before the smartphone arrived. Zoomers are spending an average of 9 hours daily in this screen-time doom loop—desperate to forget the gaping holes they’re bleeding out of, even if just for … 9 hours a day. Uncomfortable silence could be time to ponder why they’re so miserable in the first place. Drowning it out with algorithmic white noise is far easier.
A 27-year-old man who spent his adolescent years addicted (his word) to video games and pornography sent me this reflection on what that did to him:
I missed out on a lot of stuff in life—a lot of socialization. I feel the effects now: meeting new people, talking to people. I feel that my interactions are not as smooth and fluid as I want. My knowledge of the world (geography, politics, etc.) is lacking. I didn’t spend time having conversations or learning about sports. I often feel like a hollow operating system.
Or consider what Facebook found in a research project involving focus groups of young people, revealed in 2021 by the whistleblower Frances Haugen: “Teens blame Instagram for increases in the rates of anxiety and depression among teens,” an internal document said. “This reaction was unprompted and consistent across all groups.”
How can it be that an entire generation is hooked on consumer products that so few praise and so many ultimately regret using? Because smartphones and especially social media have put members of Gen Z and their parents into a series of collective-action traps. Once you understand the dynamics of these traps, the escape routes become clear.

Social media, in contrast, applies a lot more pressure on nonusers, at a much younger age and in a more insidious way. Once a few students in any middle school lie about their age and open accounts at age 11 or 12, they start posting photos and comments about themselves and other students. Drama ensues. The pressure on everyone else to join becomes intense. Even a girl who knows, consciously, that Instagram can foster beauty obsession, anxiety, and eating disorders might sooner take those risks than accept the seeming certainty of being out of the loop, clueless, and excluded. And indeed, if she resists while most of her classmates do not, she might, in fact, be marginalized, which puts her at risk for anxiety and depression, though via a different pathway than the one taken by those who use social media heavily. In this way, social media accomplishes a remarkable feat: It even harms adolescents who do not use it.
From the May 2022 issue: Jonathan Haidt on why the past 10 years of American life have been uniquely stupid
A recent study led by the University of Chicago economist Leonardo Bursztyn captured the dynamics of the social-media trap precisely. The researchers recruited more than 1,000 college students and asked them how much they’d need to be paid to deactivate their accounts on either Instagram or TikTok for four weeks. That’s a standard economist’s question to try to compute the net value of a product to society. On average, students said they’d need to be paid roughly $50 ($59 for TikTok, $47 for Instagram) to deactivate whichever platform they were asked about. Then the experimenters told the students that they were going to try to get most of the others in their school to deactivate that same platform, offering to pay them to do so as well, and asked, Now how much would you have to be paid to deactivate, if most others did so? The answer, on average, was less than zero. In each case, most students were willing to pay to have that happen.
Social media is all about network effects. Most students are only on it because everyone else is too. Most of them would prefer that nobody be on these platforms. Later in the study, students were asked directly, “Would you prefer to live in a world without Instagram [or TikTok]?” A majority of students said yes––58 percent for each app.
This is the textbook definition of what social scientists call a collective-action problem . It’s what happens when a group would be better off if everyone in the group took a particular action, but each actor is deterred from acting, because unless the others do the same, the personal cost outweighs the benefit. Fishermen considering limiting their catch to avoid wiping out the local fish population are caught in this same kind of trap. If no one else does it too, they just lose profit.
Cigarettes trapped individual smokers with a biological addiction. Social media has trapped an entire generation in a collective-action problem. Early app developers deliberately and knowingly exploited the psychological weaknesses and insecurities of young people to pressure them to consume a product that, upon reflection, many wish they could use less, or not at all.
The trap here is that each child thinks they need a smartphone because “everyone else” has one, and many parents give in because they don’t want their child to feel excluded. But if no one else had a smartphone—or even if, say, only half of the child’s sixth-grade class had one—parents would feel more comfortable providing a basic flip phone (or no phone at all). Delaying round-the-clock internet access until ninth grade (around age 14) as a national or community norm would help to protect adolescents during the very vulnerable first few years of puberty. According to a 2022 British study , these are the years when social-media use is most correlated with poor mental health. Family policies about tablets, laptops, and video-game consoles should be aligned with smartphone restrictions to prevent overuse of other screen activities.
The trap here, as with smartphones, is that each adolescent feels a strong need to open accounts on TikTok, Instagram, Snapchat, and other platforms primarily because that’s where most of their peers are posting and gossiping. But if the majority of adolescents were not on these accounts until they were 16, families and adolescents could more easily resist the pressure to sign up. The delay would not mean that kids younger than 16 could never watch videos on TikTok or YouTube—only that they could not open accounts, give away their data, post their own content, and let algorithms get to know them and their preferences.
Most schools claim that they ban phones, but this usually just means that students aren’t supposed to take their phone out of their pocket during class. Research shows that most students do use their phones during class time. They also use them during lunchtime, free periods, and breaks between classes––times when students could and should be interacting with their classmates face-to-face. The only way to get students’ minds off their phones during the school day is to require all students to put their phones (and other devices that can send or receive texts) into a phone locker or locked pouch at the start of the day. Schools that have gone phone-free always seem to report that it has improved the culture, making students more attentive in class and more interactive with one another. Published studies back them up .
Many parents are afraid to give their children the level of independence and responsibility they themselves enjoyed when they were young, even though rates of homicide, drunk driving, and other physical threats to children are way down in recent decades. Part of the fear comes from the fact that parents look at each other to determine what is normal and therefore safe, and they see few examples of families acting as if a 9-year-old can be trusted to walk to a store without a chaperone. But if many parents started sending their children out to play or run errands, then the norms of what is safe and accepted would change quickly. So would ideas about what constitutes “good parenting.” And if more parents trusted their children with more responsibility––for example, by asking their kids to do more to help out, or to care for others––then the pervasive sense of uselessness now found in surveys of high-school students might begin to dissipate.
It would be a mistake to overlook this fourth norm. If parents don’t replace screen time with real-world experiences involving friends and independent activity, then banning devices will feel like deprivation, not the opening up of a world of opportunities.
The main reason why the phone-based childhood is so harmful is because it pushes aside everything else. Smartphones are experience blockers. Our ultimate goal should not be to remove screens entirely, nor should it be to return childhood to exactly the way it was in 1960. Rather, it should be to create a version of childhood and adolescence that keeps young people anchored in the real world while flourishing in the digital age.
In recent decades, however, Congress has not been good at addressing public concerns when the solutions would displease a powerful and deep-pocketed industry. Governors and state legislators have been much more effective, and their successes might let us evaluate how well various reforms work. But the bottom line is that to change norms, we’re going to need to do most of the work ourselves, in neighborhood groups, schools, and other communities.
Read: Why Congress keeps failing to protect kids online
There are now hundreds of organizations––most of them started by mothers who saw what smartphones had done to their children––that are working to roll back the phone-based childhood or promote a more independent, real-world childhood. (I have assembled a list of many of them.) One that I co-founded, at LetGrow.org , suggests a variety of simple programs for parents or schools, such as play club (schools keep the playground open at least one day a week before or after school, and kids sign up for phone-free, mixed-age, unstructured play as a regular weekly activity) and the Let Grow Experience (a series of homework assignments in which students––with their parents’ consent––choose something to do on their own that they’ve never done before, such as walk the dog, climb a tree, walk to a store, or cook dinner).
Even without the help of organizations, parents could break their families out of collective-action traps if they coordinated with the parents of their children’s friends. Together they could create common smartphone rules and organize unsupervised play sessions or encourage hangouts at a home, park, or shopping mall.

P arents are fed up with what childhood has become. Many are tired of having daily arguments about technologies that were designed to grab hold of their children’s attention and not let go. But the phone-based childhood is not inevitable.
We didn’t know what we were doing in the early 2010s. Now we do. It’s time to end the phone-based childhood.
This article is adapted from Jonathan Haidt’s forthcoming book, The Anxious Generation: How the Great Rewiring of Childhood Is Causing an Epidemic of Mental Illness .

When you buy a book using a link on this page, we receive a commission. Thank you for supporting The Atlantic.

COMMENTS
Essay On Teenage Depression. 824 Words4 Pages. Depression is much more common than most of us realize - but the signs of depression are often difficult to detect. This is especially true when it comes to teen depression. The teenage years are already difficult, with emotional, physical, and hormonal changes that often cause confusion and anxiety.
In adolescent depression, the cognitive-behavioral therapy and the Interpersonal Therapy-Adolescent seem to have a well-established efficacy. Weersing et al. , in this same line, state that, although the efficacy of treatments in children is rather weak, cognitive-behavioral therapy is probably the most effective therapy. They also confirm ...
Treating Adolescent Depression. It is extremely important that depressed teens receive prompt, professional treatment. Depression is serious and, if left untreated, can worsen to the point of becoming life-threatening. ... Poems, essays and drawings that refer to death; Giving away belongings; Dramatic change in personality or appearance ...
Teen depression is a serious mental health problem that causes a persistent feeling of sadness and loss of interest in activities. It affects how your teenager thinks, feels and behaves, and it can cause emotional, functional and physical problems. Although depression can occur at any time in life, symptoms may be different between teens and ...
Symptoms. Causes. Diagnosis. Treatment. Coping. As much as 8% of teens experience depression each year, according to one survey. By the time young adults reach age 21, one study found that nearly 15% have had at least one episode of a mood disorder. Depression can cause problems such as difficulties in school, difficulties with relationships ...
Methods: Reviews of relevant papers relating to adolescent depression. Results: Adolescent depression is a common and costly health condition, confounded by a lack of consensus among health professionals regarding evidence-based approaches regarding treatments. Little attention has been paid to the contribution of developmental distress.
Tip 4: Manage stress and anxiety. For many teens, stress and anxiety can go hand-in-hand with depression. Unrelenting stress, doubts, or fears can sap your emotional energy, affect your physical health, send your anxiety levels soaring, and trigger or exacerbate depression.
Epidemiologic Features. Although the prevalence of depression has increased across all age groups, the increase among adolescents has outpaced that among adults. 3 The lifetime prevalence of major ...
Introduction. Unipolar depressive disorder is a common mental health problem in adolescents worldwide, 1 with an estimated 1 year prevalence of 4-5% in mid to late adolescence. 2,3 Depression in adolescents is a major risk factor for suicide, the second-to-third leading cause of death in this age group, 4 with more than half of adolescent suicide victims reported to have a depressive ...
Symptoms of depression in children and adolescents are characterized by persistent feelings of sadness or anxiousness, fatigue and/or insomnia, changes in eating patterns, irritability and restlessness, feelings of guilt or helplessness, and difficulty concentrating and remembering details. Primary prevention involves decreasing the stress of ...
The combined result for some adolescents is a kind of cognitive implosion: anxiety, depression, compulsive behaviors, self-harm and even suicide. This surge has raised vexing questions.
PAGES 5 WORDS 1450. Teen Depression. Stress and modern life are far more ingrained in modern culture, often causing a greater preponderance of mental disorders in almost all population dynamics. The teen population is not eliminated as a candidate for a disorder just because they may be young. In fact, mental disorders affect 1 in 5 teenagers.
Essay about Adolescent Depression. Depression in adolescence related to the school transitional period is a common occurrence according to the research findings of Goodwin, Mrug, Borch, & Cillessen, 2012). in fact according to research adolescents is the peek age for onset of depression during this time (1). There are many causes of depression ...
Depression is a disorder characterized by prolonged periods of sadness and loss of interest in life. The symptoms include irritability, insomnia, anxiety, and trouble concentrating. This disorder can produce physical problems, self-esteem issues, and general stress in a person's life. Difficult life events and trauma are typical causes of ...
Depression affects the teenagers socially, emotionally, academically, and physically. Depression has always been a problem in adolescents; however, in the past few decades it has grown to a significant percentage. The teenagers' mental health is affected since childhood, and this has an impact on their mind biology.
Psychotherapy. When addressing depression in adolescents, the first response for mild symptoms is psychotherapy. Currently, there are three most common psychotherapeutically approved interventions, including cognitive-behavioral therapy (CBT), interpersonal therapy (IPT), and family therapy (Beirão et al., 2020).
Introduction. Over the past several decades, adolescent depression and suicidal behaviours have increased considerably. In the USA, depression diagnoses among youth increased from 8.7% in 2005 to 11.3% in 2014 (Mojtabai, Olfson, & Han, 2016).Additionally, suicide is the second leading cause of death among youth between the ages of 10 and 34 (Centers for Disease Control and Prevention, National ...
Depression is a common mental health disease, especially in mid to late adolescence that, due to its particularities, is a challenge and requires an effective diagnosis. Primary care providers are often the first line of contact for adolescents, being crucial in identifying and managing this pathology. Besides, several entities also recommend screening for depression on this period.
PAGES 8 WORDS 2145. Depression in Adolescents. Roughly nine percent of the population - an estimated 18.8 million Americans -- suffers from depressive disorders, illnesses that affect the body as well as the mind. The effects of depression are magnified in children, who are experiencing depression in greater numbers.
Depression rates in young people have risen sharply in the past decade, especially in females, which is of concern because adolescence is a period of rapid social, emotional, and cognitive development and key life transitions. Adverse outcomes associated with depression in young people include depression recurrence; the onset of other psychiatric disorders; and wider, protracted impairments in ...
"It is a parent's job to be as involved in their teen's online life as they are in their offline life." In fact, she is not in favor of giving adolescents and teens a phone as a gift. "Mobile devices belong to the parent and the teen is being allowed to use it," Shea said. "A contract can be a useful tool before putting a device ...
Abstract. Depression in adolescence and adulthood is common, afflicting up to 20 percent of these populations. It represents a significant public health concern and is associated with considerable suffering and functional impairment. Adolescent-onset depression tends to be a particularly malignant and recalcitrant condition, increasing the ...
Teenage depression is increasing briskly and often being treated erroneously. This is a major problem because depression has fatal effects on adolescents. It was stated by the National Alliance on Mental Illness, that depression is experience by 20% of people during their teen years. Each year, there are stories of thousands of adolescents ...
This pandemic has had a wide range of impacts on children and adolescents, making it an excellent topic for a scoping review (Panchal et al., 2021).With pre-print and peer-reviewed publications on COVID-19 becoming rapidly available, this living approach was timely to identify emerging literature (Ioannidis et al., 2021).Additionally, an interactive evidence map (IEM) is an intuitive and ...
S omething went suddenly and horribly wrong for adolescents in the early 2010s. By now you've likely seen the statistics: Rates of depression and anxiety in the United States—fairly stable in ...