Essay on the HIV/Aids Health Issue in South Africa
The Human immunodeficiency virus and acquired immunodeficiency syndrome (HIV/AIDS) is one of the major health challenges affecting public health in South Africa. Despite South Africa’s efforts to avail medications for controlling and reducing viral transmission, HIV/AIDS still poses a significant health challenge to the public. The disease has already devastated thousands of families across the country. Deaths resulting from HIV/AIDS have orphaned millions of children and disrupted the normal structure of the community. HIV/AIDS has affected almost every sector of life. The pandemic has largely contributed to the increase in health expenditures in South Africa. The critical level of care required by the patients is forcing the government to divert resources that would otherwise be used to finance other development projects. Apart from overburdening the overall health and social support expenditures in the country, the virus is claiming the lives of hundreds of health practitioners in South Africa. The HIV/AIDS pandemic in South Africa is a complicated public health issue that requires a strategic approach from the national governmental organizations, non-governmental organizations, and international organizations.
Historical Context of HIV/AIDS in South Africa
South Africa reported its first HIV case in 1982, a time when the country was fighting to end the apartheid system (Hodes, 2018). The government ignored the HIV/AIDS problem as the country was facing other serious challenges such as political unrest. The media outlets did not react to the pandemic immediately (Hodes, 2018). Politics dominated major headlines at the time and the public was not immediately made aware of the pandemic. HIV silently began to take hold mostly among the gay population of South Africa and the black population.
Three years after the first case was reported, the department of health initiated a public awareness campaign. The campaign included the use of coffins and skeletons to convey messages about HIV/AIDS in the country (Hodes, 2018). The campaign however did not convey messages on the mode of transmission. In 1987, the apartheid government sought to restrict the civil liberties of infected persons (Hodes, 2018). South Africans diagnosed with HIV were quarantined while immigrants who had the disease or were suspected to have been infected were deported back to their countries.
By 1990, HIV/AIDS prevalence in South Africa had reached an all-time high. The country was at this time transitioning from apartheid to democracy and the government was facing a myriad of challenges which included corruption and abuse of power (Hodes, 2018). There was no elaborate plan by the government to handle the HIV/AIDS issue. The department of health was unable to take the appropriate measures to curb the spread of the disease. Infected people could not access the life-saving antiretroviral treatment (Hodes, 2018). These factors led to the rise of public health activist movements in the country. Members of these movements sought to compel the government to enable public access to testing and treatment of the virus. The movements further sought to force the government to undertake the necessary steps to curb the spread of the virus.
The efforts of the activists saw the formation of The National Aids Convention of South Africa (NACOSA) in 1991 (Geffen and Welte, 2018). This organization sought to strengthen partnerships among civil groups, health workers, and development agencies in a bid to curb the spread of HIV on the. In 1993, the South Africa government published its first plan to intervene HIV/AIDS pandemic issue (Hodes, 2018). Despite all these activities, the response to the pandemic remained inadequate and ineffective. Cultural challenges impeded the government’s efforts in addressing the HIV/AIDS issue. For instance, it was a taboo among some South African communities to talk openly about sex.
Current Developments of HIV/AIDS Pandemic Issue
Currently, South Africa has the highest HIV prevalence rate in the world. Out of the 58 million people in the country, 7.7 million are estimated to have contracted the virus (Avert, 2020). In the Southern Africa region, South Africa alone accounts for 30% of all new HIV infections. Of the 240,000 new infections in 2018, 71,000 were from South Arica (Avert, 2020). The burden of the pandemic has profound implications on the development of South Africa. The high rates of HIV-related infections and deaths have compromised household stability and investments in children.
The government of South Africa has made commendable efforts to address the HIV/AIDS issue. Steps undertaken by the government include enhanced clinical testing and financing the anti-retroviral program (ART) (Avert, 2020). Today, South Africa has the largest antiretroviral treatment in the world (Avert, 2020). This program is largely financed from domestic resources. As a result of the ART program, the national life expectancy in the country has increased from 56 to 63 years.
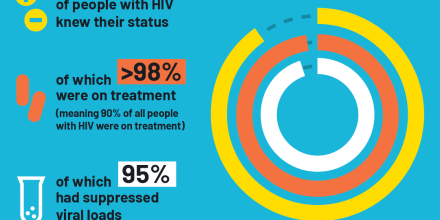
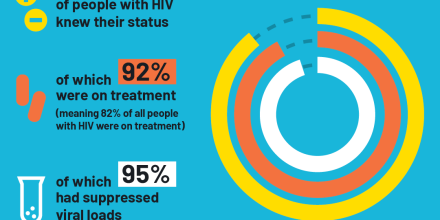
There has been notable progress in the testing and suppression of the virus. A report by the world health organization indicates that 90% of the people living with HIV have so far been tested and 87% of them have enrolled in the treatment program (Avert, 2020). The prevalence, however, remains high especially in the Western Cape and in KwaZulu-Natal areas.
HIV/AIDS Health and Social Policies in South Africa and a Comparative Analysis with the United States
Access to Testing
The government of South Africa has launched a number of HIV testing and care programs. The two recent nationwide testing initiatives are the National HIV testing and the National HIV/AIDS counseling campaign (Avert, 2020). These initiatives were part of the government’s policy to have people working in the private sector and the higher education sector get tested for the virus. As a result of this policy, more than 10 million people have since been tested (Avert, 2020). There have however been discrepancies in the number of women when compared to that of men who present themselves for testing. More women are tested as compared to men. Men are reportedly worried about queuing outside the testing facilities.
Access to HIV testing is a priority in many other countries. In the United States, for instance, the government has undertaken measures to include annual HIV testing for people aged between 15-65 years (Avert, 2019). Such measures include the expansion of the national health insurance program. The rate of people who turn in for HIV testing in the United States of America is however low as compared to that of South Africa. In the United States, people have a low disease risk perception while others are afraid of being stigmatized after diagnosis.
Access to Care and Treatment
The United Nations program introduced the 90-90-90 targets to mitigate the adverse effects of HIV/AIDS (UNAIDS, 2017). In line with the UN’s program, South Africa guarantees free and reliable access to anti-retroviral treatment (ART) (Avert, 2020). At least 4.8 million people in the country are receiving HIV/AIDS treatment as a result of the free access to care and treatment policy (Masquillier et al., 2020). Studies reveal that more women than men are more likely to enroll for ART in South Africa and as a result, the mortality rate of men is twice that of women.
Just like in South Africa, there is free access to care and treatment policy for the people living with HIV/AIDS in the United States (Avert, 2020). Testing for HIV/AIDS in the United States has become widespread over time. However, more than half of the adult population are were yet to turn out for testing as at 2012 (Rizza et al., 2012). The number of people who turn in for these services in the United States is, however, lower when compared with that of South Africa. This can be attributed to lack of awareness and misconceptions related to the HIV/AIDS virus in the United States.
Education and Awareness
The government of South Africa has made numerous efforts to educate the masses and create awareness of the HIV/AIDS pandemic (Avert 2020). The government is determined to use the education policy to provide comprehensive sexuality education in both public and private schools. By the end of the year 2016, only 5% of the schools were offering sexuality education in South Africa (Avert 2020). The government is planning to introduce a system of education that will assist learners to prevent and report incidents of sexual violence.
In the United States, the status of sexual health education is insufficient in most areas. There are claims that sexual education is not taken seriously and in some cases, it does not start early enough for the learners. The number of schools where students are supposed to get advice on HIV prevention keeps decreasing in the United States. Offering HIV/AIDS education and creating awareness has not been taken seriously in the United States. According to the Centers for Diseases Control and Prevention (2016), many Americans have become complacent about HIV/AIDS and at least a quarter of the patients are not aware of their statuses.
Legislation
Through legislation, the government of South Africa has managed to minimize cases of discrimination on an HIV status basis. Section 6(1) of the constitution requires the public especially those at the workplace to desist from any form of unfair discrimination based on a person’s HIV status (Mubangizi, 2009). The constitution bars employees from dismissing employees who turn out to be HIV positive. These laws aim to promote a non-discriminatory work environment and curb the stigmatization of HIV patients.
HIV/AIDS Pandemic issue in the Context of Social Divisions in South Africa
Apart from HIV/AIDS being a medical problem in South Africa, it is a social problem. This is demonstrated by the virus’s widespread, ineffectiveness and the inability of the medical department to control HIV expansion in the country. South Africa is one of the world’s countries that have experienced gross social inequalities (Gordon, Booysen and Mbonigaba, 2020). Such inequalities are mostly based on racial, class, and gender factors. Apartheid for instance has for a long time shaped the social profile and as a result, derailed the efforts to deal with the HIV/AIDS pandemic.
Social divisions and issues related to it have been the major setback in the fight against the virus. Whereas anyone regardless of their social status can get infected with HIV/AIDS, certain groups of people are at a higher risk of getting the infection (Avert, 2020). These groups of people engage in high-risk behaviors while others experience stigma and discrimination. Stigma and discrimination are among the major hindrances for people to seek HIV testing and treatment. If the social issues are well understood and dealt with, the government and international organizations could effectively roll out prevention programs to the people at high risks.
Women in South African society have an unequal cultural, social, and economic status. This is largely a result of inequitable laws and harmful cultural practices that empower men and disempower women. Women are at a higher risk of contracting the virus as compared to men. By 2017, the percentage of women infected stood at 26% while that of men stood at 15% (Avert, 2020). Gender-based violence, poverty, and the low status of women in South Africa are largely to blame for the high disease prevalence among women. A third of women in the country have at one time experienced intimate partner violence.
A report by the world health organization indicated that the HIV prevalence among young women was much higher than that of young men in the year 2018. Intergeneration relationships between older men and young women were understood to be the major force behind this disparity. Discriminative social attitude towards women makes it harder for them to access testing and treatment services.
South Africa is among the countries with the highest unequal distribution of resources (Gordon, Booysen and Mbonigaba, 2020). The HIV/AIDS epidemic in the country has brought about huge demands for medical care in the public health sector. As a result, the disease is more prevalent among the middle class and lower class population.
Preventing early deaths arising from HIV-related infections requires a household member to first identify the infection through testing, and enroll in the treatment program. Though testing is free in South Africa, there are other related expenses such as transport fees. People of the lower class may have problems in financing such expenses. People of the lower social class report lower rates of HIV testing as compared to those of high social class.
Being of a lower social class in South Africa is associated with reduced or no food security, lack of food diversity, and increased chances of skipping meals. Poor women are forced to adopt behaviors that increase their risk of getting infected. These behaviors include commercial sex and early marriages. HIV patients require a balanced diet to boost their immune response to opportunistic infections. In addition, Low-class people may have difficulties accessing protection equipment such as condoms due to their reduced financial capability.
Globally, racial inequalities play a significant role in escalating the HIV/AIDS pandemic. Some ethnic groups are at a higher risk of acquiring and transmitting HIV when compared to other ethnic groups. This is because, in some places such as South Africa, some population groups have higher rates of HIV/AIDS prevalence. The risk of acquiring the infection in these groups is high.
In South Africa, Black African males have high HIV/AIDS prevalence as compared to their counterparts from other races (Avert, 2020). The high prevalence among blacks is created by historical social injustices and unequal social and economic status. The apartheid particularly has contributed significantly to the HIV prevalence among the black community in South Africa (Hodes, 2018). In a country where blacks are the majority, apartheid perpetuated HIV through denial of health services and access to quality education to the black community. Apartheid policies mostly addressed the social and economic advances for the minority white communities at the expense of the black race. Up to date, the black community is yet to recover from the burden of high HIV prevalence which would otherwise not be there had it not for the apartheid system.
Cultural Issues
The high prevalence of HIV/AIDS in South Africa has prompted speculations regarding risk factors that may be unique to the country. Some cultural practices increase the risk of HIV/AIDS in the region. These factors include polygamy, early marriages, and virginity testing. All these vices characterize most South African societies.
Polygamy is not primarily a harmful practice that can directly lead to the spreading of HIV/AIDS. However, how people in polygamous marriages conduct themselves ends up facilitating the spread of the virus. Wives in a polygamous marriage have little or no control over the sexual behaviors of their husbands or co-wives. Infidelity for instance could be a catalyst for the spread if the cheating partner gets infected. In the KwaZulu-Natal community of South Africa, there has been a resurgence of virginity testing (Ngubane, 2020). The public identification of a young girl as a virgin increases her risk of sexual abuse.
Age and Family Status
By 2018, the number of HIV-infected children in South Africa stood at 260,000 and 63% of them were on treatment. These were children of age 0-14 (Avert, 2020). The rate of infection among young children is lower as compared to that of people aged 15 years and above. The decline in new infections among children is attributed to the government’s efforts in preventing mother-to-child HIV transmission. Children are however mostly affected by the HIV pandemic through the loss of their parents and guardians. HIV/AIDS pandemic has orphaned At least 1.2 million children in South Africa (Avert, 2020). This creates another problem as these children lose their providers. They become insecure and vulnerable to HIV due to economic and social insecurities. Such children become targets of sexual predators who force them to have sex in exchange for support.
The Role of International Organizations and Aid Agencies in Addressing the HIV/AIDS Issue
There are many international organizations involved in the fight against the spread of the HIV/AIDS pandemic. These organizations engage in a coordinated effort to stop new HIV infections and ensure that everyone living with the virus has unrestricted access to testing and quality treatment. International Organizations such as the Joint United Program on HIV/AIDS (UNAIDS) are responsible for promoting human rights for the patients and producing data for decision making. Some of the prominent international organizations involved in this fight include The Global Fund, The World Health Organization (WHO), and UNAIDS. These organizations undertake the international role of policy formulation and legislation in matters concerning the HIV/AIDS pandemic.
Formulation of Policies
One of the policies adopted by international organizations is the creation of awareness about HIV/AIDS. Kaiser Family Foundation for instance focuses on the provision of the latest data and information about the virus (Kaiser Family Foundation, 2016). The organization conducts research and data analysis on regular basis. In addition, Kaiser Family Foundation works with major news organizations across the world to enable easy access to information. Its information is provided free of charge.
International health organizations aim to build a better and healthier future for people living with HIV/AIDS across the world. These organizations advocate for equality and preservation of human rights regardless of their health status. The World Health Organization particularly provides evidence-based technical support to countries across the world. The organization supports its members in the quest to scale up the treatment of the virus and slow down its spread. The mission of such organizations is to lead collective action on the global HIV response.
The United Nations General Assembly fully recognizes human rights and freedoms. The organization has formulated a number of international regulations and guidelines meant to protect HIV patients across the world. Following a global outcry against the high cost of HIV treatment, the ministerial council in 2001 made a regulation prompting its members to take measures to protect public health (Patterson and London, 2002). The United Nations members were required to allow easier access to medications for people living with the virus.
International organizations have made numerous efforts to form and support national organizations. These national organizations comprise professionals and HIV/AIDS victims who are united in advocating for the rights of patients. With the support of the United Nations Development Programme, many countries have been able to form law associations meant to oversee the implementation of the rights of patients. Organizations such as legal clinics promote laws and policies on human rights and freedom.
Global Issues in the Fight against HIV/AIDS
The global economic crisis is a major hindrance to the international fight against HIV/AIDS. The UNAIDS faces a greater challenge in ensuring that UN agencies heed their call of supporting developing countries that are severely affected by the pandemic. Financing a sustainable response to the disease is a hard task especially for developing nations. With the emergence of other pandemics that require huge financing, international organizations face a challenge in financing the HIV/AIDS control measures.
The emergence of other infections has derailed the international fight against HIV/AIDS. Currently, the world is battling a new virus. The COVID-19 pandemic has a serious impact on the most vulnerable communities and impedes the progress of the fight against HIV/AIDS. World resources are now redirected to the new virus. At the moment, there is no single country that is immune to the increasing economic cost of the new pandemic.
The HIV/AIDS pandemic poses a significant health threat to South Africa. The complex nature of the disease makes it even harder for the government and other international organizations to develop a comprehensive approach to addressing it. The government and other organizations, however, have made numerous efforts to intensify testing, treatment, and provision of care to HIV patients. All these efforts have been derailed by other social factors such as class differences, gender inequalities, ethnicity, and cultural issues. In its efforts to slow the spread of the disease and mitigate its adverse effects, the government has enacted a number of policies. The policies include free access to HIV testing, education, and the creation of public awareness. International organizations have made numerous efforts to help South Africa and other developing nations in fighting the virus. These include financing the war against the disease and developing policies meant to address the HIV/AIDS issue.
Avert. 2019. HIV and AIDS in the United States of America (USA). [Online] Available at: <https://www.avert.org/professionals/hiv-around-world/western-central-europe-north-america/usa> [Accessed 17 April 2021].
Avert. 2020. HIV and AIDS in South Africa. [Online] Available at: <https://www.avert.org/professionals/hiv-around-world/sub-saharan-africa/south-africa> [Accessed 17 April 2021].
Centers for Disease Control and Prevention. 2016. Challenges in HIV Prevention . [Online] Available at: <https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/challenges-508.pdf> [Accessed 6 May 2021].
UNAIDS. 2017. Ending Aids; Progress towards the 90-90-90 targets. [Online] Available at: <https://www.unaids.org/sites/default/files/media_asset/Global_AIDS_update_2017_en.pdf> [Accessed 17 April 2021].
Geffen, N. and Welte, A., 2018. Modeling the human immunodeficiency virus (HIV) epidemic: A review of the substance and role of models in South Africa. Southern African Journal of HIV Medicine , 19(1).
Gordon, T., Booysen, F. and Mbonigaba, J., 2020. Socio-economic inequalities in the multiple dimensions of access to healthcare: the case of South Africa. BMC Public Health, 20(1).
Hodes, R, 2018. ‘HIV/AIDS in South Africa’, Oxford Research Encyclopedia of African History .
Kaiser Family Foundation. 2016. HIV Awareness and Testing. [Online] Available at: <https://www.kff.org/slideshow/hiv-awareness-and-testing/> [Accessed 17 April 2021
Masquillier, C., Knight, L., Campbell, L., Sematlane, N., Delport, A., Dube, T., and Wouters, E., 2020. Sinako, a study on HIV competent households in South Africa: a cluster-randomized controlled trial protocol. Trials, 21(1).
Mubangizi, J., 2009. HIV/AIDS and the South African Bill of Rights, with specific reference to the approach and role of the courts. African Journal of AIDS Research , 3(2), pp.113-119.
Ngubane, L., 2020. Traditional Practices and Human Rights: An Insight on a Traditional Practice in Inchanga Village of Kwazulu-Natal, South Africa. The Oriental Anthropologist: A Bi-annual International Journal of the Science of Man , 20(2), pp.315-331.
Patterson, D. and London, L., 2002. International law, human rights, and HIV/AIDS. [Online] Global Public Health and International Law. Available at: <https://www.who.int/bulletin/archives/80(12)964.pdf> [Accessed 17 April 2021].
Rizza, S., MacGowan, R., Purcell, D., Branson, B. and Temesgen, Z., 2012. HIV Screening in the Health Care Setting: Status, Barriers, and Potential Solutions. Mayo Clinic Proceedings , 87(9), pp.915-924.

Cite this page
Similar essay samples.
- Essay on the Sisters, Araby, and an Encounter
- Essay on Universalism
- Essay on Compare and Contrast Antigen Receptors With Pattern Recogniti...
- Collective Bargaining Gives Employees a Voice
- Essay on the Collapse of Communism and the Dissection of Bicycle Thiev...
- Essay on Performance Appraisal
Programs submenu
Regions submenu, topics submenu, strengthening australia-u.s. defence industrial cooperation: keynote panel, cancelled: strategic landpower dialogue: a conversation with general christopher cavoli, china’s tech sector: economic champions, regulatory targets.
- Abshire-Inamori Leadership Academy
- Aerospace Security Project
- Africa Program
- Americas Program
- Arleigh A. Burke Chair in Strategy
- Asia Maritime Transparency Initiative
- Asia Program
- Australia Chair
- Brzezinski Chair in Global Security and Geostrategy
- Brzezinski Institute on Geostrategy
- Chair in U.S.-India Policy Studies
- China Power Project
- Chinese Business and Economics
- Defending Democratic Institutions
- Defense-Industrial Initiatives Group
- Defense 360
- Defense Budget Analysis
- Diversity and Leadership in International Affairs Project
- Economics Program
- Emeritus Chair in Strategy
- Energy Security and Climate Change Program
- Europe, Russia, and Eurasia Program
- Freeman Chair in China Studies
- Futures Lab
- Geoeconomic Council of Advisers
- Global Food and Water Security Program
- Global Health Policy Center
- Hess Center for New Frontiers
- Human Rights Initiative
- Humanitarian Agenda
- Intelligence, National Security, and Technology Program
- International Security Program
- Japan Chair
- Kissinger Chair
- Korea Chair
- Langone Chair in American Leadership
- Middle East Program
- Missile Defense Project
- Project on Fragility and Mobility
- Project on Nuclear Issues
- Project on Prosperity and Development
- Project on Trade and Technology
- Renewing American Innovation Project
- Scholl Chair in International Business
- Smart Women, Smart Power
- Southeast Asia Program
- Stephenson Ocean Security Project
- Strategic Technologies Program
- Transnational Threats Project
- Wadhwani Center for AI and Advanced Technologies
- All Regions
- Australia, New Zealand & Pacific
- Middle East
- Russia and Eurasia
- American Innovation
- Civic Education
- Climate Change
- Cybersecurity
- Defense Budget and Acquisition
- Defense and Security
- Energy and Sustainability
- Food Security
- Gender and International Security
- Geopolitics
- Global Health
- Human Rights
- Humanitarian Assistance
- Intelligence
- International Development
- Maritime Issues and Oceans
- Missile Defense
- Nuclear Issues
- Transnational Threats
- Water Security
The World’s Largest HIV Epidemic in Crisis: HIV in South Africa

Photo: STEPHANE DE SAKUTIN/AFP/Getty Images
Commentary by Sara M. Allinder and Janet Fleischman
Published April 2, 2019
In some communities of KwaZulu-Natal Province, South Africa, 60 percent of women have HIV. Nearly 4,500 South Africans are newly infected every week; one-third are adolescent girls/young women (AGYW) ages 15-24. These are staggering figures, by any stretch of the imagination. Yet, the HIV epidemic is not being treated like a crisis. In February, we traveled to South Africa, to understand what is happening in these areas with “hyper-endemic” HIV epidemics, where prevalence rates exceed 15 percent among adults. We were alarmed by the complacency toward the rate of new infections at all levels and the absence of an emergency response, especially for young people.
This is no time for business as usual from South Africa or its partners, including the U.S. government through the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR). The epidemic is exacerbated by its concentration in 15-49-year-olds, those of reproductive and working age who are the backbone of South Africa. Without aggressive action to reduce the rate of new infections in young people, HIV will continue to take a tremendous toll on the country for years and generations to come. Collective action is needed to push beyond the complacency and internal barriers to implement policies and interventions that directly target HIV prevention and treatment for young people. PEPFAR should ensure its programs support those efforts.
South Africa remains the epicenter of the HIV pandemic as the largest AIDS epidemic in the world—20 percent of all people living with HIV are in South Africa, and 20 percent of new HIV infections occur there too. The country also faces a high burden of tuberculosis (TB), including multi-drug resistant TB, which amplifies its HIV epidemic. Of particular concern are South Africa’s hyper-epidemics , many in KwaZulu-Natal and Mpumalanga provinces, and the concentration in specific populations like AGYW. Of the estimated 7.2 million South Africans living with HIV, nearly 60 percent are women over the age of 15. HIV prevalence in other key populations—female sex workers, men who have sex with men, transgender women, and people who inject drugs—remains unacceptably high, in some cases double the national prevalence rate of approximately 19 percent .
After the early years of denial, the South African government now finances close to 80 percent of the HIV response, an unparalleled commitment in sub-Saharan Africa, and provides more than 4 million people with life-prolonging anti-retroviral treatment (ART). In 2018, President Cyril Ramaphosa called for an increase of 2 million South Africans on ART by December 2020 through increased testing and treatment.
The problem facing South Africa’s HIV response is that treatment scale-up has stalled, and while new infections have gone down by 42 percent, the rate is not fast enough to bend the curve of the epidemic. New infections in young men and women remain alarmingly high (nearly 87 percent of the total) and viral suppression rates, a key to preventing those living with the virus from passing it on, are under 50 percent for those 15-24 years old. With approximately 45 percent of the population under the age of 25 , the sheer numbers of those becoming infected and overall prevalence of HIV will stay alarmingly high without a massive decline in the new HIV infection rate.
The central question is how to interrupt HIV transmission in young adults, and where and whom to target. One answer is to target AGYW who are at higher risk for HIV acquisition in South Africa, as they are elsewhere in sub-Saharan Africa. The reasons are both biological and social, including high rates of teenage pregnancy, an epidemic of gender-based and interpersonal violence; lack of quality education; and widespread poverty and unemployment. High rates of sexually transmitted infections (STIs) increase the risk of HIV acquisition, and mental health issues can lead to risky behaviors. Professor Olive Shisana, special adviser on social policy to President Cyril Ramaphosa, emphasized the urgency: “New infections are the highest in adolescent girls/young women. We need to close the tap. If we get to them early, we’ll reduce the load on the nation and globally.”
Addressing the range of social, economic, and health issues that put AGYW at risk is one approach. PEPFAR’s DREAMS program—Determined, Resilient, Empowered, Aids-Free, Mentored, and Safe—includes a package of multisectoral interventions to be “layered” for a comprehensive benefit to the young woman. The importance of this layered approach led to DREAMS being adapted by the Global Fund to Fight AIDS, Tuberculosis, and Malaria and the South African government in its She Conquers campaign. However, tracking the layering of those services has proven to be a challenge, as has widespread scale up.
Another important approach is to reach young men. The Centre for the Aids Programme of Research in South Africa (Caprisa) has demonstrated that a particularly complicated cycle of transmission involves men ages 25-34 infecting adolescent girls/young women ages 15-24, who then go on to infect their longer-term male partners ages 24-35, and the cycle continues. Prevalence among 20-24-year-old women is three times higher than in men their age. Promoting prevention through behavior and voluntary medical male circumcision (VMMC) and getting those men who are already living with HIV on treatment and virally suppressed so they can’t pass the virus to their partners are critical interventions.
The challenge is reaching the men. “Services are not geared for men and young people,” acknowledged Dr. Yogan Pillay, the deputy director general for the National Department of Health. While adult women come to clinics when they are pregnant or for their children, young men rarely interact with the health system unless they have suffered a major injury. In general, men are less likely to know their HIV status than women or to seek care and treatment if they test positive. Health services seen as not “male friendly” and gender norms around masculinity that equate seeking health care with weakness are two factors. As a result, men 25-34 years old have the lowest viral suppression rates (41.5 percent) of any gender/age band in South Africa. Community outreach is one way to reach AGYW and their male partners, especially those out-of-school who have a substantially higher HIV risk and men older than 25 years, by bringing information and services to where they are. “If you think you can intervene by using the current approach to health delivery, it won’t work,” noted professor Quarraisha Abdool Karim, Caprisa associate scientific director.
For many young adults, HIV is often not seen as a crisis because they have bigger worries: extreme poverty, unemployment and lack of jobs, crumbling school infrastructure. When they live in a community with such high HIV rates, there is a fatalistic feeling that getting infected with HIV is inevitable. Girls and women also face an epidemic of rape and gender-based violence; many young women express more concerns about getting raped or getting pregnant than getting HIV. At one site we visited, the girls stated that getting raped was their number one fear.
Pre-exposure prophylaxis (PrEP) offers a tool to help break the transmission cycle. Oral PrEP taken once a day can reduce vulnerability to infection by 99 percent. In areas where there is so much HIV circulating, every sexual encounter is high risk, and widespread PrEP could be a prevention lynchpin. However, PrEP rollout has been slow and inadequate in South Africa since it was approved in national guidelines in 2016. There have been issues with messaging, health worker sensitization and training, and availability. PrEP scale-up will require extensive outreach to create demand, ensure adherence, and negate any stigma to ensure that all those at high risk can have access. Only an estimated 12,000 people are currently on PrEP at approximately 50 clinics nationwide—shy of the national target of more than 18,000. To put that in further perspective, 12,000 equates to only 5 percent of the 231,000 presumed to be at risk for new infections based on the 2017 rates.
Lack of knowledge can impact young adults’ informed prevention and treatment choices. There has been an associated decline in HIV and treatment literacy, which means that young people often don’t understand how the virus affects the body and the impact of lifelong ART. The most recent national survey data from 2017 shows the same low level of condom use among 15-24-year-olds as the last survey in 2012, an increase in sexual debut before the age of 15 for boys, and an increase in multiple sexual partnerships for women under 24.
One barrier is the provision of basic health education and service delivery in schools. While South Africa has a national policy on school-based health education, some provincial officials, school governing boards, and other gatekeepers often prevent services from being provided, even though the age of consent for health services is 12. Schools are an important entry point because there is a high rate of school retention in South Africa and, once out of school, it is difficult to reach young people.
While we met many dedicated HIV champions across South Africa, and there are commitments from national and provincial officials and existing national strategies, the health and education systems are not providing the necessary information and services for young people, and not enough investment is being made to empower communities and civil society organizations to launch more effective and sustainable responses. There is an absence of targeted outreach, media campaigns, and high-profile champions. Young South Africans told us repeatedly that they wanted more leadership and information on HIV and to see role models of healthy living that make HIV prevention and staying negative cool and demonstrate how to live positively with HIV.
The critical gap in South Africa is not between evidence and policy, but between policy and implementation. While the government is committed to supporting the national HIV treatment program and has issued enabling guidelines, it faces significant challenges to effective implementation. It lacks the resources for an overhaul of the public health infrastructure and to scale up and increase coverage of prevention programs like PrEP and broader programs to address the needs of young adults. In addition, health worker shortages and a rising non-communicable disease (NCD) burden are crippling already overstretched health facilities, and the decentralized health system requires political will at the provincial and district levels to implement services effectively.
Many politicians and local government officials are preoccupied with other issues, such as the economic crisis that has gripped the country in recent years, a legacy of corruption that has crippled the energy sector, and upcoming elections in May. The president’s 2019 State of the Nation address called attention to corruption and gender-based violence, but in stark contrast to last year’s treatment pledge, he did not once mention HIV.
South Africa’s HIV epidemic needs to be treated as a public health emergency. After the elections in May, there is an opportunity for the government to re-commit to fighting HIV, at national, provincial, and district levels. Business as usual is not bringing down new infections or getting patients onto treatment. The government should go beyond strategies and push through barriers to actual implementation, get services into school, and re-educate South Africans about HIV. Enabling nationwide scale-up of PrEP for young adults and all who are at high risk would go along way toward protecting South Africa’s future.
For South Africa’s HIV partners, like PEPFAR, the post-election period also provides an opportunity to re-engage with the new government and focus on how to best support targeted interventions toward adolescents and young people. That includes listening to young people and communities, making sure services are available away from clinics in communities and schools, supporting provinces in service provision, and elevating prevention and treatment for young people. Turning the tide on the epidemic will require more than increasing the number of people on treatment; PEPFAR can provide unique support to South Africa to implement a multipronged strategy for young people as an urgent priority.
Sara M. Allinder is executive director and senior fellow and Janet Fleischman is senior associate with the Global Health Policy Center at the Center for Strategic and International Studies in Washington, D.C. This commentary is based on their visit to South Africa in February 2019.
Commentary is produced by the Center for Strategic and International Studies (CSIS), a private, tax-exempt institution focusing on international public policy issues. Its research is nonpartisan and nonproprietary. CSIS does not take specific policy positions. Accordingly, all views, positions, and conclusions expressed in this publication should be understood to be solely those of the author(s).
© 2019 by the Center for Strategic and International Studies. All rights reserved.

Sara M. Allinder

Janet Fleischman
Programs & projects.
- Health Security
- Understanding The HIV Epidemic
At a glance: HIV in South Africa
The biggest HIV epidemic in the world
Key statistics: 2021
- 7.5 million people with HIV
- 18.3% adult HIV prevalence
- 210,000 new HIV infections
- 51,000 AIDS-related deaths
- 5.5 million people on antiretroviral treatment
Progress towards targets
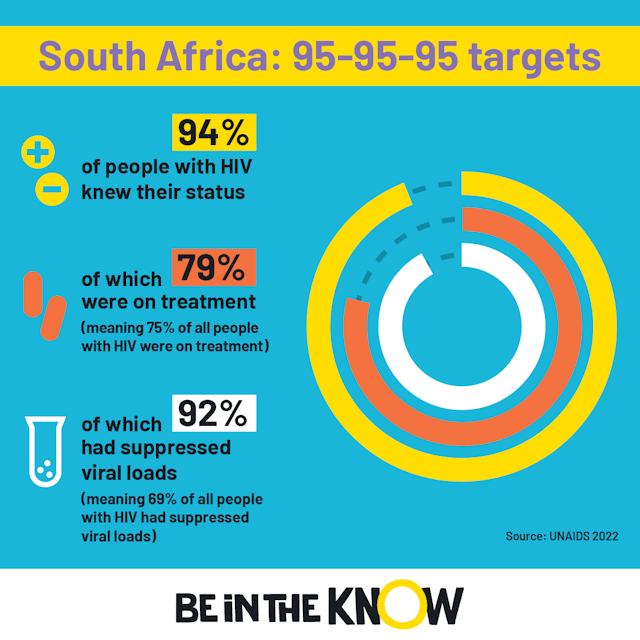
The current targets for HIV testing and treatment are called the 95-95-95 targets and must be reached by 2025 in order to end AIDS by 2030.
In 2021 in South Africa:
Did you know?
South Africa has made huge improvements in getting people to test for HIV in recent years and met the 2020 target of 90% of people with HIV knowing their status in 2018. But it is behind on increasing access to HIV treatment, hampered by the need to provide HIV treatment for more people than any other country in the world.
Preventing HIV in South Africa focuses on:
- prevention of mother-to-child transmission
- distributing condoms, including male and female condoms
- voluntary medical male circumcision
- PrEP – a daily pill that can prevent HIV (vaginal ring and injectable being trialled)
- management of sexually transmitted infections, including partner infections
- linking closely to HIV testing services.
South Africa was the first country in sub-Saharan Africa to fully approve PrEP, which is now being made available to people at high risk of infection, such as sex workers. The country has remained focused on increasing PrEP access in recent years by introducing things such as mobile PrEP clinics, despite the challenges of the COVID-19 pandemic.
Testing for HIV is lower among:
- people with a lower socio-economic background
- people living in rural areas.
It is possible to self-test for HIV at home in South Africa, which is popular among young people and people from key affected populations.
Treatment for HIV is:
- started as soon as someone tests positive
- usually a three-in-one tablet
- received by more people with HIV than any other country in the world.
The South African government changed the usual first-line treatment regimen it offers in 2017, to a Dolutegravir-containing fixed dose combination, which has been found to have fewer side effects.
Local context
Women continue to bear a disproportionate burden of the HIV epidemic, with women twice as likely to have HIV than men . Around one-third of women are likely to experience intimate partner violence in South Africa – and this has increased in recent years, linked to the fallout of the COVID-19 pandemic. Violence against women and girls is a huge issue, and can prevent women from testing for HIV and starting and staying on treatment. It also helps drive transmission.
Men in South Africa are less likely than women to use HIV services, including HIV testing and starting and staying on antiretroviral treatment.
It is estimated that around 58% of sex workers have HIV. Female sex workers with HIV are consistently less likely to know their HIV status than other adult women.
Gay men and other men who have sex with men with HIV are much less likely to know their HIV status compared with other men. However, when they do know their HIV status, they are more likely to receive HIV treatment and be virally suppressed.
HIV-related stigma remains an issue – around 17% of people hold discriminatory attitudes towards people with HIV, according to UNAIDS data. But this is lower compared to other countries in the region.
Get the latest news
Keep up-to-date with new developments, research breakthroughs and evidence for what works in sexual health and the HIV response, with our news service.
Explore more
At a glance: HIV in Kenya
At a glance: HIV in Lesotho
At a glance: HIV in Malawi
At a glance: HIV in Nigeria
At a glance: HIV in Uganda
Still can't find what you're looking for, share this page.
- Last updated: 31 March 2023
- Last full review: 01 March 2025
- Next full review: 01 March 2025
HIV and AIDS Prevalence in South Africa Essay
Introduction, podcast overview, information learned.
Countries of the African continent continue to be disproportionately burdened by HIV/AIDS. South Africa has the highest HIV prevalence rates in the world, both among adults and children. In the Africa Science Focus podcast episode, the host and guests, including UNAIDS representatives, discuss the causes of South Africa’s HIV burden (Africa Science Focus, 2022). The podcast was selected as it addresses a disease that remains a critical health and social problem worldwide.
The podcast focuses primarily on the discussion of inequalities in access to treatment and preventative measures in high-risk South African society. According to Africa Science Focus (2022), despite effective HIV/AIDS treatments available around the world, there is a distinct inequality in the ability of South Africa to access them. This disparity is attributed to supply chain complexities, health system shortcomings, poverty, and lingering prejudices (Africa Science Focus, 2022). Although the country made great strides in reducing new infections and the mortality rate, the 90-90-90 UNAID targets of decreasing HIV incidence in the country by 2020 have not been met (Johnson et al., 2020). Overall, many people in South Africa are unaware of their HIV status, have no access to treatment, or are vulnerable to infection due to life circumstances.
The podcast under consideration shed light on some new information concerning approaches to addressing HIV/AIDS and preventing the spread of the disease. According to Africa Science Focus (2022), vulnerable populations should be reached through community work rather than medical facilities. HIV-positive people in South Africa experience concurrent mental health problems, stigma, and breakdown of relationships. Before listening to the podcast, I knew that HIV/AIDS is a significant health problem in South Africa. However, I did not realize how it can be attributed to inequality in the global arena. The condition is on the World Health Organization (WHO) agenda, with the organization working closely with UNAIDS (World Health Organization, 2022). Thus, many community and health organizations are working on reducing HIV incidence in the country.
In summary, HIV/AIDS presents a substantial health problem for South Africa. The Africa Science Focus podcast notes that as the country with the highest HIV prevalence in the world, South Africa does not have the same access to effective HIV treatments as developed countries. Furthermore, the podcast suggests that failure to prevent new infections and reduce transmission can be attributed to the inequality between developing and developed countries.
Africa Science Focus. (2022). Inequality still hampers Africa’s HIV fightback . Sub-Saharan Africa. Web.
Johnson, L. F., Patrick, M., Stephen, C., Patten, G., Dorrington, R. E., Maskew, M., Jamieson, L., & Davies, M.-A. (2020). Steep declines in pediatric aids mortality in South Africa, despite poor progress toward pediatric diagnosis and treatment targets . Pediatric Infectious Disease Journal , 39 (9), 843–848. Web.
World Health Organization. (2022). HIV . World Health Organization. Web.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, January 31). HIV and AIDS Prevalence in South Africa. https://ivypanda.com/essays/hiv-and-aids-prevalence-in-south-africa/
"HIV and AIDS Prevalence in South Africa." IvyPanda , 31 Jan. 2024, ivypanda.com/essays/hiv-and-aids-prevalence-in-south-africa/.
IvyPanda . (2024) 'HIV and AIDS Prevalence in South Africa'. 31 January.
IvyPanda . 2024. "HIV and AIDS Prevalence in South Africa." January 31, 2024. https://ivypanda.com/essays/hiv-and-aids-prevalence-in-south-africa/.
1. IvyPanda . "HIV and AIDS Prevalence in South Africa." January 31, 2024. https://ivypanda.com/essays/hiv-and-aids-prevalence-in-south-africa/.
Bibliography
IvyPanda . "HIV and AIDS Prevalence in South Africa." January 31, 2024. https://ivypanda.com/essays/hiv-and-aids-prevalence-in-south-africa/.
- Acquired Immunodeficiency Syndrome Pathophysiology
- Segregation of HIV-Positive Prisoners
- HIV Prevention Programs in Africa
- HIV/AIDS and International Health Community
- COVID-Related Depression: Lingering Signs of Depression
- Podcasts: Definition and Functions
- HIV-Positive Women's Mental Health Problems
- Deadlocks in Concurrent Computing
- How podcasts differ from radio
- Concurrent Engineering with 3D Printer
- The US and Brazil’s Response to COVID-19
- Epidemiological Study on Salmonella in the Caribbean
- COVID-19 Outbreak and Effectiveness of Vaccines
- The Spread of Monkeypox as a Topic in Healthcare
- The West Africa Ebola Outbreak of 2014-2016
- Society and Politics
- Art and Culture
- Biographies
- Publications
HIV/Aids in South Africa
HIV/Aids is a deadly disease, which is currently not curable. The United Nations AIDS agency (UNAIDS) says the evidence that HIV is the underlying cause of AIDS is ‘irrefutable’. HIV was isolated and identified as the source of what came to be defined as AIDS in 1983/84. HIV destroys blood cells called CD4+ T cells, which are crucial to the normal function of the human immune system. Studies of thousands of people have revealed that most people infected with HIV carry the virus for years before enough damage is done to the immune system for AIDS to develop.
Statistics:
On 21 November 2007, a new UN report said more than three-quarters of Aids-related deaths occurred in sub-Saharan Africa and South Africa was officially the country with the highest prevalence of HIV in the world. The consequences of HIV and AIDS for the economy in the countries in southern Africa are terrible. HIV/Aids is becoming the most devastating disease humankind has ever faced.
In the same UN report on 2007 (UN 2008 Global Report on the HIV and AIDS Epidemic) around 5.7 million South Africans were estimated as having HIV or Aids, including 300 000 children under the age of 15 years. 350 000 people died from AIDS in South Africa in 2007. Women face a greater risk of HIV infection. On average in South Africa there are three women infected with HIV for every two men who are infected. The difference is greatest in the 15-24 age group, where three young women for every one young man are infected.
One of the most significant damages caused by this disease is the number of children orphaned as a result of AIDS. Obtaining accurate statistics on the number of children orphaned is problematic. If orphans are defined as children from birth up to the age of 17 whose mothers have died, UNAIDS estimates that there were 1 400 000 children orphaned due to AIDS living in South Africa at the end of 2007. This figure is higher than for any other country. However, it is estimated that Zimbabwe has 1 000 000 children orphaned due to AIDS among a total population of fewer than 13 million.
How does South Africa celebrate World Aids day? In South Africa, this day was first celebrated in 1996 when the Department of Health organised a special event called the National World AIDS Day in Bloemfontein, Free State, and in Pretoria, Gauteng... read more
Estimates of the numbers of people infected with HIV and dying of AIDS are based on surveys and models. Most people in South Africa do not know their HIV status. Therefore, researchers and statisticians use the prevalence of HIV among groups whose status is known (such as pregnant women attending antenatal classes) to work out the likely prevalence rate in the general population. They also "project" how many people are likely to become infected and die in future, based on what is already known about infection and mortality rates.
Many factors contribute to the spread of HIV. These include: poverty; inequality and social instability; high levels of sexually transmitted infections; the low status of women; sexual violence; high mobility (particularly migrant labour); limited and uneven access to quality medical care; a history of poor leadership in the response to the epidemic and society leaders dying and leaving a generation of children growing up without the care and role models they will normally have. In addition many people in South Africa do not know their HIV status because as a predominantly sexually transmitted disease, its discussion is often taboo. Education, testing, counseling and living positively after being infected play a role in reducing the numbers of infection.
This is a war, it has killed more people than has been the case in all previous wars, we must not continue to be debating, to be arguing, when people are dying and I have no doubt that we have a reasonable and intelligent government, and that if we intensify this debate inside, they will be able to resolve it” - Former South African President, Nelson Mandela, Sunday Times, Sunday 10 Aug 2003
HIV can be transmitted from one person to another through:
Transmission and symptoms:
- Unprotected vaginal or anal intercourse with an infected person
- A mother's infection passing to her child during pregnancy, birth or breastfeeding (called vertical transmission)
- Injections with contaminated needles, which may occur when intravenous drug users share needles, or when health care workers are involved in needle prick accidents
- Use of contaminated surgical instruments, for example during traditional circumcision
- Blood transfusion with infected blood
The only way to know if you are infected is to be tested for HIV infection; you may not have any symptoms for many years.
There are some symptoms that are common warning signs of infection with HIV:
- rapid weight loss
- recurring fever or night sweats
- severe, unexplained fatigue
- swollen glands in the armpits, groin, or neck
- diarrhoea that lasts for more than a week
- white spots or unusual blemishes on the tongue, or in the mouth or throat
- red, brown, pink, or purplish blotches on or under the skin or inside the mouth, nose, or eyelids
- memory loss, depression, and other neurological disorders
However, each of these symptoms can be related to other illnesses so the only way to be sure of HIV infection is to get tested.
Aids Foundation, South Africa [online], available at: www.aids.org.za [accessed 15 April 2009]| History and Science of HIV and Aids [online], available at: www.avert.org [accessed 15 April 2009]|Mandela, N (1998), Keynote Address at a Rally on World AIDS Day. |Mandela, N (2000), Closing Address at the 13th International AIDS Conference .|Bazilli, S., Bond, J., McPhedran, M. and Sherret, L. (2006) Prognosis for the Inequality Virus, Gender, Democracy, Reconstruction & HIV/AIDS in Southern Africa , Concept Paper for the Commonwealth Secretariat, Gender Section, Social Transformation Programmes Division.|Van Wyk, B. (2003). Dark side of the rainbow: the impact of HIV/AIDS on the African renaissance. Centre for the Study of AIDS|Van Wyk, B. (2003). A brief history of a global effort to fund the Campaign against Aids, Centre for the Study of AIDS . Centre for the Study of AIDS.|Van Wyk, B. (2003). The New Drug War. Centre for the Study of AIDS.|Van Wyk, B. (2003). Bringing out the best but mostly the worst in people: addressing HIV/AIDS-related stigma in South Africa.| The SAHARA archive , SAHARA is an alliance of partners established to conduct, support and use social sciences research to prevent the further spread of HIV and mitigate the impact of its devastation in sub-Saharan Africa. The website houses many research papers and publications on HIV/Aids in sub-Saharan Africa| NAM Aids Map , NAM is an award-winning community based HIV information provider. The team at NAM is based in London, in the UK, but their information is known and used across the world. This is a good resource.| TAC, Treatment action Campaign , campaigning for the rights of those living with HIV/Aids in South Africa.|Cameron, E (date unknown) Legal and Human Rights responses to the Hiv/Aids epidemic , prepared for a Court of Appeal exposition.
World Aids Day is internationally observed for the first time The birth of the Treatment Action Campaign
Collections in the Archives
Know something about this topic.
Towards a people's history
The macro-economic impact of HIV/AIDS in South Africa
Journal title, journal issn, volume title, description, collections.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Croat Med J
- v.49(3); 2008 Jun
HIV Infection and AIDS Among Young Women in South Africa
This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Young women in South Africa are at great risk of being infected with HIV. In 2005, HIV infection prevalence in the age group 15-24 years was 16.9% in women and 4.4% in men ( 1 ). The high HIV prevalence in this country is a result of a number of factors which include the following: poverty, violence against women, cultural limitations that promote intergenerational sex, non-condom use and preference for “dry sex,” political factors and challenges that possibly prevented an aggressive response against HIV, recreational drug use, and biological factors such as high prevalence of sexually transmitted infections (STI). This essay will present and discuss the prevalence of HIV among young women in South Africa and the reasons for such a high prevalence in the country. I will also give an overview of the intervention programs that are currently under way with an aim to reduce the vulnerability of young women in South Africa. Finally, I will suggest what further interventions need to be provided in order to prevent and control HIV spread in South Africa and other southern African countries.
HIV prevalence among young women in South Africa
HIV prevalence among young women aged 15 years to 24 years in South Africa is estimated at between 15 to 25 percent ( 2 - 4 ). Shisana et al ( 1 ) estimated an estimate of 16.9 percent in 2005. HIV prevalence of about 4 to 6% among young men, although high in comparison with Western countries, is still lower than the prevalence among women ( 3 ). There are also significant racial differences as shown in Table 1 .
Prevalence of HIV infection among South African 2 years or older in 2005*
*Data from Shisana et al ( 1 )
Although there is high HIV prevalence among young women, the distribution is not uniform across the country. Kleinschmidt et al ( 2 ) have reported that lowest levels of infection are found in inland rural areas of the Western Cape and the highest in northwestern parts of KwaZulu Natal, southern Mpumalanga, and eastern Free State. The major metropolitan areas of Johannesburg and Cape Town have intermediate levels of between 7 and 11%.
Attempting to explore the factors that are associated with high HIV prevalence among South African young women is a daunting task, mostly because of the following reasons:
a) Research may examine only a limited scope of factors. For instance, studies designed to explore the role of individual-level determinants of infection (eg, lifetime number of sexual partners, concurrent partners, history of STIs) may not give due recognition to group-level factors, such as percentage of the population living in poverty within a community, racial distribution,, the role of legislation on intimate partner violence, contraceptive use, or availability of health services;
b) limitation in access to communities: much of the studies conducted in South Africa have been conducted in large metropolitan zones or at least in settings which are easily accessible;
c) contradictions arising from studies reporting different effect estimates and different key factors important in the transmission of HIV in a particular setting. For instance, in most of Africa, there is evidence that education level of an individual may be associated with the risk of HIV infection. However, education may be an important factor in one setting but not in another, or the effect of education as an explanatory factor may change over time in the same setting (depending on the stage of the epidemic, a factor such as education may have different associations), or a variable may be measured differently from study to study. For instance, when education is the main variable some studies measure the number of years of schooling completed while other study measure the level of education attained. Certainly, these two measurements may not always measure the same constructs.
d) data on potential confounding variables may not be available from studies conducted in South Africa. It is not always possible to have available data on all aspects of HIV that may potentially affect HIV transmission. For instance, data on injecting drug use in many parts of Africa are lacking. This does not necessarily mean that the practice does not contribute to HIV transmission in these settings. So if injecting illicit drug use and men having sex with men facilitate HIV spread in South Africa, the extent of their contribution to HIV spread is not fully known, as these behaviors are not often studied.
Despite these limitations and potentially many other, there is still a need to explore the “risk factors” of HIV infection and transmission in South Africa, a country which has the largest number of HIV infected persons in the world – an estimated 5 500 000 (95% confidence interval; 4 900 000-6,100,000) ( 5 ).
Biological susceptibility to HIV infection among young women
Pettifor et al ( 4 ) have reported the high efficiency of HIV transmission from men to women in South Africa. They reported that, contrary to previous findings, many HIV infected young women in South Africa had not had significantly more sexual partners than women of similar age in the developed nations. Mean number of lifetime sexual partners was 2.3, but HIV infection prevalence was 21.2%. In many developed countries, infection prevalence estimates are below 1% ( 4 ). Although the results by Pettifor et al may have been affected by under-reporting, there is no reason to believe that South African women would under-report more than the women elsewhere. The finding that many HIV-infected South African young women reported relatively low-risk sexual behaviors is not unusual ( 4 ). A report by Moyo et al ( 6 ) suggests that young people who were in a relationship for at least a year and had sex in the past month were less likely to have used condoms consistently. HIV-infected women in North Carolina ( 7 ) reported that a third of them did not report any known “high risk” behaviors.
The high HIV man to woman transmission rate may be a manifestation of the efficiency of the male “transmitter” and the susceptibility of the woman ( 4 ). Sexually transmitted infections in a male sex partner are important facilitators of HIV transmission ( 8 , 9 ). Furthermore, the immature cervix of the young female is particularly susceptible to the entry of HIV. Other biological factors that have been studied and possibly modulate the susceptibility of young women are the use of hormonal contraceptives, pregnancy, and abnormal vaginal flora ( 10 - 12 ).
South African women may be exposed to HIV infection due to the following reasons: limited treatment opportunities for sexually transmitted infections; young women having sex with young men who are likely to have recent infection; and high pregnancy rates. McPhail et al ( 13 ) surveyed 3618 sexually active young women, 52% of which reported the use of contraceptives in the last 12 months. However, no definitive conclusion has been reached regarding the role of contraception and HIV transmission.
The role of the CCR gene
In the past several years, there has been a growing interest in genetic factors that may help to explain the large differences in HIV prevalence between Africa as opposed to Europe and North America. This resulted in a search for possible genetic differences among races; although race-ethnicity itself is a social and not genetic construct ( 14 ). The CCR5 gene, relatively more common among Caucasians but almost not present among people of African descent, has been suggested to partly be responsible for the differences in HIV prevalence between Africa and Europe and North America ( 15 - 18 ). Iqbal et al ( 19 ) have postulated that the protection from HIV infection in sex workers in Nairobi, Kenya, may be explained by the CCR5 gene. However, the CCR5 gene is not that prevalent even among Caucasians and so its role in the epidemic nature of HIV transmission in southern Africa remains unclear.
Poverty and low status of women
Poverty, both at the individual and the societal level, has been associated with HIV prevalence ( 20 - 23 ). Poor neighborhoods do not have the necessary social infrastructure, which may promote HIV spread. Poor individuals, due to lack of alternatives for earning a livelihood, may be more likely to engage in sex work or other forms of transactional sex. Lopman et al ( 24 ) have reported that HIV prevalence is lower among higher socio-economic classes in that country. As a consequence of Apartheid and the associated racial segregation and discrimination, many South African young women, especially black ones are not educated. Their earning potential within the job market is, therefore, compromised. South Africa has high rates of poverty and unemployment (almost 40% of unemployed).
Transactional sex has been associated with high risk of HIV acquisition in both the developing and developed nations ( 25 ). The most common nationally representative survey of sexual behaviors and HIV infection is the Demographic Health Survey, which is conducted periodically with funding from the United States Agency for International Development of ORC Macro (Maryland) and developing nations’ governments. Survey respondents are simply asked whether men have either provided money or material resources to their non-marital partner. Women are also asked whether they have received money or material gifts from a sexual partner. Any person who reports “yes” to this question is classified as having offered or obtained transactional sex.
Transactional sex has consistently been associated with a high risk of sexually transmitted infections and HIV. While “transactional sex” may be also understood as sex work from the western standpoint, some reports from Africa suggest that exchange of money and material resources may be a different cultural practice ( 26 ). Maganja et al ( 27 ) have reported that in Tanzania, committed sexual partnerships among youth are associated with the expectation that the male will provide material and financial resources to the female partner. The ability of the male partner to provide financial and material resources affects both the duration and the exclusivity of the relationship.
Poulin ( 28 ) has also explored the role of money transfers among youth in a rural southern district of Malawi. This author found that monetary transfers were expected in male-female sexual relationships. Women were described as gauging the marriage potential of a prospective partner by assessing how much money transfers he was able to make. On the other hand, young men perceived such women as ”gold diggers” and not really committed to marriage.
Despite the fact that there are forms of transactional sex that may not carry higher HIV transmission potential, in general though, transactional sex is more likely to be associated with risk behavior. An individual is less likely to insist on “safer sex” when if she or he were to benefit materially or financially from the sexual transaction. Transactional sex is also associated with casual sex and concurrent sexual partnerships, which are then associated with high likelihood of HIV transmission. The power imbalance that may exist between the person providing the money and the person receiving the money facilitates HIV transmission, since partners are not selected on the basis on criteria other than money.
The role of migrant labor
The role that labor migration has played in the spread of HIV in Southern Africa has been discussed elsewhere ( 29 , 30 ). During the Apartheid period, South Africa had been a major recipient of migrant labor from neighboring countries such as Zimbabwe, Botswana, Swaziland, and even from Zambia and Malawi. Some authors have also described the process of “circular migration” where individuals cycle through urban and rural areas in search of jobs in urban areas and living a subsistence livelihood in rural areas. South African authors have ascribed the spread of HIV to and from South Africa to the way migrant labor camps were run. Adult men (laborers) that are employed in the mines are confined to migrant labor camps. Men are not allowed to come to the mines with their spouses, so a vibrant sex industry and an environment that encourages men having sex with men are probably created. This has at least three important implications. First, the men would transmit HIV and other sexually transmitted infections to their sex partners back home during their holidays or upon the return. Second, these men would also bring sexually transmitted infections acquired in their homeland to the migrant labor camps. Finally, disturbed sex ratios may stimulate the relationships with multiple and concurrent partners and transactional sex. Labor migration within South Africa, where mostly men leave their rural areas in search of employment in urban areas is probably a main driver of HIV spread in South Africa ( 31 , 32 ). Migrant labor movement still continues in South Africa, as people work in large farms and in the mines.
Intergenerational sex
Doherty et al ( 33 ) have reported that dissortative sex, ie, sexual partnerships between individuals from high risk and from low risk groups (mixing of risk groups) is an important driving force of the HIV epidemic. This is contrasted to assortative sexual mixing, ie, sexual partnerships between individuals of similar HIV risk, which would not foster the spread of HIV.
Intergenerational sex, where young women have sex with older men (more than 5 years age difference), is one of the different forms of dissortative sex. Young people, who have had less exposure to sex, are sexually connected with adults, whose HIV infection rates are likely to be higher.
The mechanisms by which inter-generational sex may facilitate HIV transmission are as follows: there is likely to be significant power differentials when the ages of the partners are so much different; condoms are less likely to be used in these relationships; likelihood of HIV discordancy at start of relationship likely to be high.
Research on intergenerational sex suggested that all intergenerational sex is associated with power imbalances, no condom use, manipulation, poverty and the sheer need for economic survival. While such factors may be at play in many intergenerational partnerships, exceptions do exist. Nkosana and Rosenthal’s qualitative research showed that some relationship between young girls and older men were associated with desire for pleasure, enjoyment and sense of equal partnership by the younger partner ( 34 ). However, young women involved in such kind of relationship may fail to appreciate the precarious nature of such relationships.
High risk intergenerational sex may also occur when older men, who know they are infected with HIV, seek unprotected sex with younger women or children ( 35 , 36 ). In South Africa, and many parts of southern Africa, there is a belief that having sex with a virgin is a cure for HIV. The extent to which such practices could be driving the HIV epidemic in South Africa is likely to be small though.
Alcohol and other recreational drug use
There is growing research interest in the role of alcohol and other recreational drugs in the spread of HIV in South Africa ( 37 , 38 ).The growth of the number of taverns and shebeens in poor peri-urban South Africa and its associated lifestyles are a consequence of segregation and discrimination during the Apartheid era. Such places, located largely in the poor neighborhoods, also very often associated with sex work ( 39 ).
Violence against women and rape
Violence against women, and especially rape, are significant problems in South Africa, where it is estimated that more than one woman is raped each second. Jewkes and Abrahams ( 40 ) report that representative community-based surveys have found that among women in the 17-48 age group, there were 2070 such incidents of rape per 100 000 women per year. Compared to consensual sex, rape is a rare event. However, the fact that rape is unsolicited, and is likely to be unsafe (no condom use, tears), makes it an important aspect of the HIV transmission in South Africa. The risk of HIV infection may be minimized by the provision of drug prophylaxis, which may not be readily available, especially in remote rural parts of South Africa ( 41 , 42 ).
Lack of male circumcision
From the mid 1980s, evidence has been accumulating that male circumcision could be associated with lower transmission of HIV ( 43 - 47 ). Countries with high prevalence of circumcision are also likely to have lower prevalence of HIV infection ( 48 , 49 ). However, most of these studies were cross-sectional and, therefore, could not estimate causation ( 50 ). Therefore, randomized controlled trials were conducted in Orange Farm (South Africa), Kisumu (Kenya), and Rakai (Uganda). These studies have demonstrated a protective efficacy of circumcision against HIV acquisition among men of about 60% ( 51 - 53 ).
South Africa’s male circumcision prevalence is below 30% and the majority of men were traditionally circumcised as a rite of passage from childhood into adulthood ( 54 ). Circumcision protects against HIV acquisition potentially through many mechanisms, as has been discussed elsewhere ( 55 ). In brief however, the reduced surface area of potential exposure to HIV, the prevention of sexually transmitted diseases (other than HIV), and the keratinization of the glans penis are all postulated as mechanisms through which circumcision prevents HIV transmission among men. In a community where men are less likely to be infected with HIV (as a consequence of circumcision) women are also likely not to be infected. The fact that a small percent of men in South Africa is circumcised ( 56 ) could at least in part explain the high HIV prevalence among women.
There is already interest to provide circumcision to adolescents and young men in South Africa in order to prevent HIV transmission. Rennie et al ( 57 ) have discussed the operational and ethical issues that may need to be considered in such a scaling-up. These issues include the age of circumcision, consent and assent issues, safety of the procedure within a health system with limited supplies and human resources, and stigma that may be associated with circumcision.
“Dry sex” preference
In many parts of Southern Africa, women insert detergents, antiseptic powders into their vagina in order to make them “dry” or “tight” ( 58 , 59 ). In these settings, it is believed that a highly lubricated vagina diminishes sexual pleasure during insertive penile vaginal sex. A dry vagina or a dry vagina with herbal particles is likely to suffer lesions during sex which may either facilitate transmission of HIV or acquisition of the virus.
While the practice may be blamed for the spread of HIV, its prevalence is not known. Much of the data on this practice has come from studies with small sample size and among selected groups such as sex workers.
The role of AIDS “denialists”
The claim by South Africa’s president Thabo Mbeki and his minister for health that HIV is not the cause of AIDS may have derailed many prevention, treatment, care, and support efforts by various stakeholders in South Africa ( 60 , 61 ). It was not until the South African government lost in courts that significant progress started to be made in the country ( 62 , 63 ).
To what extent the government’s response to HIV has facilitated the rapid spread of infection or not can be debated. This is because South Africa has continued to attract both domestic and international resources in the fight against the virus. There is no doubt, though, that AIDS treatment programs, including the prevention of mother to child transmission through the use of nevirapine, were all delayed because of the government’s reluctance. How this may have affected HIV infection prevalence estimates among young women is probably not known.
Education and HIV infection
South Africa, as a middle-income country, has a much better education system than many other southern African nations. However, educational opportunities are not evenly shared among the provinces and among the different racial groups (blacks, Asian, coloreds or mixed race, and whites). The blacks are less likely to receive education than the whites or Asians. Education has been reported to be associated with HIV infection, either negatively or positively, depending on the setting and circumstances. In a study in India, Radhakrishna et al reported that individuals with low education were more likely to be infected with HIV ( 64 ). In a study in Zambia, however, Gabrysch et al reported that high education was a risk factor for HIV infection ( 20 ). Bärnighausen et al ( 65 ) have reported a 7% reduction in the hazard of acquiring HIV infection in a general population in South Africa.

Racial and urban-rural differences
In a study on HIV infected persons receiving care in rural and urban South Africa, Lurie et al ( 66 ) reported that urban residents were more likely to use condoms with both regular and casual sex partners. Furthermore, HIV prevalence is associated with ethnicity, urban status, and unemployment. According to Shisana et al, HIV prevalence in 2005 was 9.1% in urban formal sector; 17.6% in urban informal sector; 11.6% in rural informal sector, and 9.9% in rural formal sector. These estimates may also need to be viewed in the light of the findings that showed that 13.3% of the blacks were infected, as opposed to 0.6% of the whites, 1.9% of coloreds, and 1.6% of Indian ( 1 ).
The racial and rural-urban divide in HIV prevalence estimates in South Africa is likely to be associated with the distribution of poverty, access to health care, unemployment, migrant labor and crime. Black South Africans in general are more likely to be exposed to these social ill than the other racial/ethnicity group. I doubt that the differences have to do with genetic differences at all.
Openness about sexuality and HIV among young people
South Africa, like many countries in southern Africa, has experienced enormous social changes in the past two decades. Harrison ( 67 ) has explored the experience of sexuality among South African young people within an environment that emphasizes “good behavior,” conformity with traditional norms, and where it is considered to be “wrong” that young unmarried women have sex. Relationships, especially in rural areas, are conducted in secrecy, and risk being of stigmatized when discovered by society militates against an open discussion of adolescent sexuality and decision making. Kennedy et al ( 68 ) has reported that adolescent African American men were likely to assume that they know the sexual risk behaviors of their partners.
Orphanhood and HIV
In a study of 200 girls in a peri-urban area of Zimbabwe, maternal orphans were more likely to be sexually active, to have had an STI, to have been pregnant, and to have been infected with HIV. Paternal orphans were more likely to have ever been homeless and to be out of school ( 69 ). Birdthistle et al ( 70 ) have also reported higher HIV infection prevalence among orphan girls and women aged 15 to 19 years (17%), as opposed to non-orphan girls (14%). These authors also found that orphans had an earlier age of sexual debut and were likely to have had multiple sexual partners. Herpes simplex virus type 2, an indicator of sexual experiences, was higher among orphan than non-orphan children.
The high HIV prevalence among orphans could be explained by exposure to sexual risk factors for the acquisition of HIV. Another plausible explanation would be that orphaned children were infected from their mother by vertical HIV transmission. However, this alternative explanation cannot be applicable in Zimbabwe, where antiretroviral therapy has not been used long enough to affect the survival of infants and children who may have acquired HIV vertically. The importance of such a possibility, though, is likely to be increasingly reasonable as HIV treatment possibilities expand in southern Africa and more HIV infected children survive to reach into adolescence.
Orphans are likely to be exposed to HIV risk behavior via a number of mechanisms. First, due to death of their parents and losing their source of livelihood, they may be more likely to engage in transactional sex. Multiple sex partnerships are also likely as one may need more than a single partner to satisfy the diverse economic needs. Second, orphan children may miss the guidance and supervision that parents normally provide within the community. Previous data on adolescents’ tobacco use have suggested that adolescents who are often supervised by adults are less likely to engage in cigarette smoking and illicit drug use.
Incarceration and HIV
Violent crime is fairly rampant in South Africa, largely as a consequence of years of Apartheid. The blacks are more likely to be incarcerated than the whites. The South African Department of Correctional Services reported 5285 HIV cases in the prison system in 2002, compared with 623 in 1995. Between 1996 and 2000, departmental statistics show that the system has experienced a 40% increase in the number of HIV/AIDS cases. It is estimated that HIV prevalence among the prison population was 41%, much higher than the national adult average prevalence estimates ( 71 ).
There are limited data on the epidemiology of HIV among incarcerated populations in South Africa. HIV infection in correctional settings is, therefore, a relatively neglected issue in southern Africa ( 72 ). However, emerging data from the United States suggest that the role of incarceration in the spread of HIV has been under-recognized.
Wherever data are available, the HIV infection prevalence estimates of incarcerated populations are higher than in the general population ( 73 ). In Malawi, Chimphambano et al ( 74 ) estimated an HIV prevalence rate 36.6%; 29.9% among men and 50% among women in a prison population. This estimate was also three-times the prevalence of the general adult population ( 75 ). This may not necessarily imply that HIV transmission or incidence in jails and prisons is higher than in the general population. One important reason for the high HIV prevalence within jails and prisons is that the incarcerated people already had background HIV risk factors while they were still in the general community. Many are likely to be injecting drug users ( 76 ), procure or provide transactional sex, be poor, have limited education, and multiple sexual partners. Individuals living “in the margins” of society are likely to be incarcerated just as they are likely to be infected. Furthermore, while incarcerated, and in a high HIV prevalence environment, any sexual penetrative sexual activity is likely to be of high risk.
Incarceration also affects HIV transmission via the associated societal disruption and encouragement of high risk partnerships ( 77 ). In South Africa, just like in many other settings, the jail and prison population is largely male. A disruption of the male to female ratio through the disproportionate incarceration of men leads to a limited choice of sexual partners for women (in heterosexual terms). The remaining and available men are, therefore, likely to be “shared” by the women. Furthermore, as the man is usually the main bread-winner in the family, his incarceration lead to a loss of earnings for the household and an increased likelihood for the woman to engage in transactional sex. The incarcerated man may also be exposed to multiple same-sex encounters within prison or jail.
The effects of incarceration on the transmission of HIV do not only manifest while an individual is in jail or prison. Even after release, people who had been incarcerated more often have multiple sexual partners than before the incarceration and so do their sexual partners ( 78 , 79 ). Stephenson et al ( 80 ) have reported that upon release from prisons, individuals were more likely to have unprotected sex with their regular partners. In Zambia, it is believed that unsafe tattooing practices in correctional facilities could be responsible for the spread of HIV ( 81 ).
Like many other countries in southern Africa, South Africa has devoted significant resources to the scaling-up of HIV treatment, care, and support. Treatment with highly active antiretroviral therapy is provided for free to incarcerated people. There are several ways how incarceration can influence HIV treatment. First, individuals who were on HIV treatment outside jail or prison are likely to miss treatment, as they may not have taken their medications with them. Even those who may have had their medications with them may be unwilling to take their medications in the prison as their HIV status may be revealed to the fellow inmates or warders. In a study from North Carolina ( 82 ), 93% of prison officers and 94% of medical staff agreed with the statement: “If an inmate is taking medications in jail, other inmates will know about it.”
Then, there are those who may start HIV treatment during a long-term stay in prison. Such persons may have well-controlled HIV infection while incarcerated due to the availability of medications and reasonable nutrition. Such quality of care may not be available when they are released. As has been reported elsewhere ( 82 , 83 ), individuals who had received reasonable medical attention with adequate HIV viral suppression while incarcerated may not be able to access it when released, which results in a rebound of the HIV viral load. High viral load is an important determinant of HIV transmission, ie, the higher the viral load the greater are the chances that HIV will be transmitted via penetrative or insertive sex.
Unlike other African countries where same sex intercourse is outlawed ( 84 ), in South Africa there is no such legal practice. This gives the opportunity for public health intervention programs to be provided with the correctional facilities without much legal hurdles. Condoms are therefore provided routinely in South African facilities. However, for condoms to make an impact on HIV transmission, they need to be used correctly and consistently.
Limited human resources for intervention programs
As is the case in many southern African countries, South Africa has an inadequate number and uneven spread of health sector workers, especially in HIV treatment programs ( 85 , 86 ),. It is, therefore, neccesary that prevention programs face human resources challenges as the country scales-up HIV prevention efforts.
Treatment of STIs
STIs other than HIV facilitate HIV transmission. Some of these infections manifest as ulcerative lesions which may act as portals of entry of HIV ( 87 , 88 ). An STI results in an increase in genital HIV viral load, which means that having sex with a person with an STI implies an exposal to a higher viral load ( 88 ). Furthermore, STIs also result in the recruitment of macrophages and lymphocytes which are virotrophic ( 87 - 92 ). A person with STI and exposed to HIV infection through sex is likely to acquire the infection due to the breached epithelium and/or increase in white cells to which HIV will get attached for entry.
In an over-stretched health system, especially in rural areas, prompt and effective treatment of STIs may not be always available and untreated STIs are likely to fuel HIV transmission.
What can be done to reduce HIV in South Africa
There are many interventions being implemented to reduce the HIV transmission. Some of the programs aim to delay sexual debut, prevent intergenerational sex, and promote condom use ( 4 ). Other programs are structured within the ABC (abstinence, being faithful to one’s partner, and condom use) guidelines. However, evaluating the impact of any of these programs is fraught with methodological challenges, including the fact that there is a multiplicity of programs and adolescents are simultaneously exposed to many of them. However, these interventions should be scaled-up, as not all geographical areas of the country have been equally included. Furthermore, as new challenges emerge, eg, injecting drug use and men having sex with men, there is a need to adapt these interventions.
Many factors affect the prevalence and incidence of HIV in a country. The following measures, many of which are already been employed within South Africa, are suggested: delaying age at sexual debut among adolescents; promoting consistent and correct condom use (encouraging distribution and training on correct use); promoting mutual monogamy; prompting treatment for sexually transmitted infections; providing sterile needles; promoting formal education, especially among the blacks; introducing employment programs to reduce poverty; preventing rape and sexual violence, and promoting safe male circumcision.
Acknowledgments
A previous draft of this paper was submitted to fulfill course requirements for AIDS, Principles and Politics (PUBH 420) at the University of North Carolina at Chapel Hill, United States.
Poverty and HIV/AIDS in Africa: Specifying the connections
- Original Article
- Published: 29 October 2014
- Volume 13 , pages 1–29, ( 2015 )
Cite this article
- Pempelani Mufune 1
2503 Accesses
11 Citations
1 Altmetric
Explore all metrics
There is an increasing recognition that poverty in Africa is a critical factor in the transmission of HIV/AIDS. To this end, at a macro level some theorists have described HIV/AIDS as one of the diseases of poverty. ‘Diseases of poverty’ are those that primarily affect the poor, and which worsen the toll of poverty. Many if not most countries severely affected by HIV/AIDS are also in the global south and poverty stricken, but this does not necessarily mean poverty leads to HIV infection. In fact, evidence on the relationship between HIV transmission and poverty remains mixed. While some macro and micro studies find a positive relationship between poverty and HIV, others do not. Although efforts have been made to tackle the issue of poverty as a way of dealing with HIV/AIDS, the role played by poverty in HIV/AIDS remains poorly understood. There are several impediments to understanding the poverty and HIV/AIDS nexus. First, researchers who investigate the poverty and HIV relationship have failed to take into account conceptual and theoretical advances in the literature on poverty. In the process they have failed to specify what aspects of poverty might be related to HIV/AIDS. Second, there is little agreement on how poverty should be measured. Choice of the poverty measure is much more than just a technical detail, and is reflective of social concerns and values inherent in debates over poverty. Third, researchers in this area use different definitions of poverty, but different definitions of poverty lead to different measures of poverty, yielding different groups of people. This article evaluates studies in Africa that look at the role played by poverty in HIV/AIDS transmission at both macro and micro level. It examines the conceptual and methodological obstacles that prevent a clear sociological understanding of the poverty–HIV/AIDS behaviour dynamic. In this article we develop a framework for conceptualizing poverty and its relationship to HIV/AIDS. We look to common and well-formulated ideas in the literature on poverty to develop the framework. We suggest material deprivation (relative and absolute), vulnerability and social exclusion as the core ideas in recent advances in the literature on poverty. We then identify possible social, structural and behavioural pathways between these aspects of poverty and link them to HIV/AIDS.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
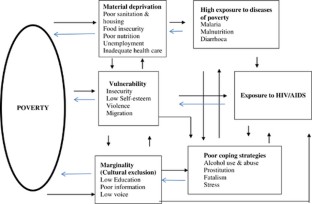
Similar content being viewed by others

A Geographical Analysis of the African COVID-19 Paradox: Putting the Poverty-as-a-Vaccine Hypothesis to the Test
Tolulope Osayomi, Richard Adeleke, … Ayobami Abayomi Popoola
Does poverty increase COVID-19 in Africa? A cross-country analysis
Etayibtalnam Koudjom, Sévérin Tamwo & Koffi D. Kpognon

Food Insecurity, Poverty, and HIV/AIDS
Abrahams, N., Jewkes, R., Laubscher, R. and Hoffman, M. (2006) Intimate partner violence: Prevalence and risk factors for men in Cape Town, South Africa. Violence and Victims 21: 247–264.
Article Google Scholar
Agyei-Mensah, S. (2006) Poverty and HIV prevalence in Ghana: A geographical perspective. GeoJournal 66 (4): 311–324.
Alcock, P. (1997) Understanding Poverty. London: Palgrave Macmillan.
Book Google Scholar
Anglewicz, P. (2012) Migration, marital change, and HIV infection in Malawi. Demography 49 (1): 239–265.
Baral, S. et al (2009) HIV prevalence, risks for HIV infection, and human rights among men who have sex with men (MSM) in Malawi, Namibia, and Botswana. PLoS ONE 4 (3): e4997.
Beaulier, S. (2003) Explaining Botswana’s success: The critical role of post-colonial policy. Cato Journal 23 (2): 227–240.
Google Scholar
Beckfield, J. (2004) Does income inequality harm health? New cross-national evidence. Journal of Health and Social Behavior 45 (3): 231–248.
Bernstein, H. (1992) Poverty and the poor. In: H. Bernstein, B. Crow and H. Johnson (eds.) Rural Livelihoods. Oxford: Oxford University Press.
Bloom, D., River Path Associates Sevilla, J. (2002) Health, wealth, AIDS and poverty, Manila, Asian Development Bank, http://www.hivpolicy.org/Library/HPP000622.pdf , accessed 12 December 2012.
Bond, P. (1999) Globalization, pharmaceutical pricing, and South African health policy: Managing confrontation with U.S. firms and politicians. International Journal of Health Service 29 (4): 765–792.
Bond, P. (2008) Social movements and corporate social responsibility in South Africa. Development and Change 39 (6): 1037–1052.
Booysen, F. and Summerton, J. (2002) Poverty, risky sexual behaviour, and vulnerability to HIV infection: Evidence from South Africa. Journal of Health, Population and Nutrition 20 (4): 285–288.
Bradley-Springer, L. (2010) Political ideology, HIV infection, and PEPFAR. Journal of the Association of Nurses in AIDS Care ; 21(5): 377–379.
Brady, D. (2003) Rethinking the sociological measurement of poverty. Social Forces 81 (3): 715–752.
Bradshaw, J. and Finch, N. (2003) Overlaps in dimensions of poverty. Journal of Social Policy 32 (4): 513–525.
Bryceson, D.F. and Fonseca, J. (2006) Risking death for survival: Peasant responses to hunger and HIV/AIDS in Malawi. World Development 34 (9): 1654–1666.
Campbell, C. (1997) Migrancy, masculine identities and AIDS: The psychosocial context of HIV transmission on the South African gold mines. Social Science and Medicine 45 (2): 273–281.
Catley-Carlson, M. and Outlaw, J. (1998) Poverty and population issues: Clarifying the connections. Journal of International Affairs 52 (1): 233–252.
Chambers, R. (1995) Poverty and livelihoods: Whose reality counts? Environment and Urbanization 7 (1): 173–204.
Chambers, R. (2006) Editorial introduction: Vulnerability, coping and policy. IDS Bulletin 37 (4): 33–40.
Chin, B. (2010) Income, health, and well-being in rural Malawi. Demographic Research 23: 997–1030.
de Haan, A. (1998) Social exclusion-an alternative concept for the study of deprivation? IDS Bulletin 29 (1): 10–19.
de Waal, A. (2006) AIDS and Power: Why There is No Political Crisis -Yet. London: Zed Books.
Deane, K., Parkhurst, J. and Johnston, D. (2010) Linking migration, mobility, and HIV. Tropical Medicine and International Health 15 (12): 1458–1463.
Decosas, J., Kane, F., Anarfi, J., Sodji, K. and Wagner, H. (1995) Migration and AIDS. Lancet 346 (8978): 826–828.
Ditmore, M. and Allman, D. (2010) Implications of PEPFAR's anti-prostitution pledge for HIV prevention among organizations working with sex workers. HIV/AIDS Policy & Law Review 15 (1): 63–64.
Ditmore, M.H. and Allman, D. (2013) An analysis of the implementation of PEPFAR’s anti-prostitution pledge and its implications for successful HIV prevention among organizations working with sex workers. Journal of International AIDS Society 16 (March): 17354.
Dunkle, K., Jewkes, R., Brown, H., Gray, G., McIntyre, J. and Harlow, S. (2004) Gender-based violence, relationship power and risk for prevalent HIV infection among women attending antenatal clinics in Soweto, South Africa. Lancet 363 (9419): 1415–1421.
Edwards, J.W., Fisher, D.G. and Reynolds, G.L. (2007) Male-to-female transgender and transsexual clients of HIV service programs in Los Angeles county, California. American Journal of Public Health 97 (6): 1030–1033.
Facey, M. and Eakin, J. (2010) Contingent work and ill-health: Conceptualising the links. Social Theory and Health 8 (4): 326–349.
Fenton, L. (2004) Preventing HIV/AIDS through poverty reduction: The only sustainable solution? Lancet 364 (9440): 1186–1187.
Fitzgerald, E. (1991) Economic Reform and Citizen Entitlements in Eastern Europe. Geneva: UNRISD Discussion Paper No. 27.
Fox, AM (2012) The HIV-poverty thesis re-examined: Poverty, wealth or inequality as a social determinant of HIV infection in Sub-Saharan Africa? Journal of Biosocial Science 44: 459–480.
Gillespie, S. and Greener, R. (2007) Is poverty or wealth driving HIV transmission? AIDS 21 (Suppl 7): S5–S16.
Gillies, P.A., Tolley, K. and Wolstentolme, J. (1996) Is AIDS a disease of poverty? AIDS Care 8 (3): 351–363.
Green, E.C., Halperin, D.T, Nantulya, V. and Hogle, J. (2006) Uganda’s HIV prevention success: The role of sexual behavior change and the national response. AIDS and Behavior 10 (July): 335–346.
Gregson, S. et al (2006) HIV decline associated with behavior change in Eastern Zimbabwe. Science 311 (5761): 664–666.
Haralambos, M. and Holborn, M. (1995) Sociology. Themes and Perspectives. 4th edn. Connecticut: Collins Educational.
Hargreaves, J.R. et al (2008) Systematic review exploring time trends in the association between educational attainment and risk of HIV infection in Sub-Saharan Africa. AIDS 22 (3): 403–414.
Hargreaves, J., Davey, C., Fearon, E. and Krishnaratne, S. (2013) Changes in HIV prevalence among socioeconomic groups in eight African countries: Analysis of sequential cross-sectional surveys. The Lancet 381: S57.
Hope, K.R. (2001) Population mobility and multi-partner sex in Botswana: Implications for the spread of HIV/AIDS. African Journal of Reproductive Health 5 (3): 73–83.
Hunter, M. (2002) The materiality of everyday sex: Thinking beyond ‘prostitution’. African Studies 61 (1): 99–120.
Illife, J. (1987) The African Poor – A History. Cambridge, UK: Cambridge University Press.
IMF (2011) Regional economic outlook: Sub-Saharan Africa, http://www.imf.org/external/pubs/ft/reo/2012/afr/eng/sreo0412.pdf , accessed 7 January 2013.
Jewkes, R.K., Dunkle, K., Nduna, M. and Shai, N. (2010) Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: A cohort study. Lancet 376 (9734): 41–48.
Kabeer, N. (1991) Gender dimensions of rural poverty: Analysis from Bangladesh. Journal of Peasant Studies 18 (2): 241–262.
Kalichman, S. (2000) HIV transmission risk behaviors of men and women living with HIV-AIDS: Prevalence, predictors, and emerging clinical interventions. Clinical Psychology: Science and Practice 7 (1): 32–47.
Kalichman, S., Simbayi, L.C., Jooste, S., Cherry, C. and Caim, D. (2005) Poverty-related stressors and HIV/AIDS transmission risks in two South African communities. Journal of Urban Health 82 (2): 237–249.
Kalichman, S., Simbayi, L., Kagee, A., Toefy, Y., Cain, D. and Cherry, C. (2006) Association of poverty, substance use, and HIV transmission risk behaviors in three South African communities. Social Science and Medicine 62 (7): 1641–1649.
Kishamawe, C. et al (2006) Mobility and HIV in Tanzanian couples: Both mobile persons and their partners show increased risk. AIDS 20 (4): 601–608.
Leclerc-Madlala, S. (2003) Transactional sex and the pursuit of modernity. Social Dynamics 29 (2): 213–233.
Marks, G. (2007) Income Poverty, Subjective Poverty and Financial Stress, Social Policy Research Paper No. 29, Department of Families, Community Services and Indigenous Affairs, Government of Australia.
Mishra, V. et al (2007) HIV infection does not disproportionately affect the poorer in Sub-Saharan Africa. AIDS 21 (Suppl 7): s17–s28.
Morison, L. et al (2001) Commercial sex and the spread of HIV in four cities in Sub-Saharan Africa. AIDS 15 (Suppl 4): S61–S69.
Mufune, P. (2003) African culture and managerial behavior: Clarifying the connections. South African Business Management 34 (3): 17–28.
Natrass, N. (2009) Poverty, sex and HIV. AIDS Behaviour 13 (5): 833–840.
Niemietz, K. (2011) A New Understanding of Poverty. London: Institute of economic affairs.
Panchanadeswaran, S. et al (2008) Intimate partner violence is as important as client violence in increasing street-based female sex workers’ vulnerability to HIV in India. International Journal of Drug Policy 19 (2): 106–112.
Parkhurst, J. (2010) Understanding the correlation between wealth, poverty and human immunodeficiency virus infection in African countries. Bulletin of the World Health Organization 88 (7): 519–526.
Rodrigo, C. and Rajapakse, S. (2010) HIV, poverty and women. International Health 2 (1): 9–16.
Schröder-Butterfill, E. and Marianti, R. (2006) A framework for understanding old-age vulnerabilities. Ageing and Society 26 (1): 9–35.
Sen, A. (1981) Poverty and Famines: An Essay on Entitlement and Deprivation. Oxford: Clarendon Press.
Sen, A. (1984) Resources, Values and Development. Oxford: Basil Blackwell.
Sen, A. (1991) Poverty and Famines: An Essay on Entitlement and Deprivation. Oxford, New York: Clarendon Press Oxford University Press.
Shelton, J.D., Cassell, M.M. and Adetunji, J. (2005) Is poverty or wealth at the root of HIV? Lancet 366 (9491): 1057–1058.
Shisana, O., Rice, K., Zungu, N. and Zuma, K. (2010) Gender and poverty in South Africa in the era of HIV/AIDS: A quantitative study. Journal of Women‘s Health 19 (1): 39–46.
Silberschmidt, M. (2003) AIDS, sexuality and gender in Africa: Collective strategies and struggles in Tanzania and Zambia. Social Science & Medicine 56 (2): 425–427.
Silverman, J.G., Decker, M.R., Saggurti, N. and Balaiah, D. (2008) Intimate partner violence and HIV infection among married Indian women. JAMA 300 (6): 703–710.
Simbayi, L.C., Kalichman, S.C., Jooste, S., Cherry, C., Mfecane, S. and Cain, D. (2005) Risk factors for HIV-AIDS among youth in Cape Town, South Africa. AIDS and Behavior 9 (1): 53–61.
Stillwaggon, E. (2000) HIV transmission in Latin America: Comparisons with Africa and policy implications. South African Journal of Economics. Special Issue: Economics of HIV/AIDS 68 (5): 985–1011.
Stillwaggon, E. (2001) AIDS and poverty in Africa. The Nation 272 (20): 22–25.
Townsend, P. (1993) The International Analysis of Poverty. London: Harvester Wheatsheaf.
UNAIDS World AIDS Day Report. (2012) UNAIDS World AIDS Day Report, http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2012/gr2012/JC2434_WorldAIDSday_results_en.pdf , accessed 7 January 2013.
UNAIDS Report on the Global AIDS Epidemic. (2012) UNAIDS Report on the Global AIDS Epidemic, http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2012/gr2012/20121120_UNAIDS_Global_Report_2012_en.pdf , accessed 7 January 2013.
UNAIDS/WHO (2005) AIDS epidemic update, http://www.who.int/hiv/epi-update2005_en.pdf , accessed 7 January 2013.
Wagle, U. (2002) Rethinking poverty: Definition and measurement. International Social Science Journal 54 (171): 155–165.
Weiser, S. et al (2007) Food insufficiency is associated with high-risk sexual behavior among women in Botswana and Swaziland. PLoS Medicine 4 (10): 1589–1597.
Whiteside, A. (2002) Poverty and HIV/AIDS in Africa. Third World Quarterly 23 (2): 313–332.
Wilkinson, R. (1999) Income inequality, social cohesion, and health: Clarifying the theory: A reply to Muntaner and Lynch. International Journal of Health Services 29 (3): 525–543.
Download references
Author information
Authors and affiliations.
Department of Sociology, University of Namibia, Windhoek, P/Bag 13301, Namibia
Pempelani Mufune
You can also search for this author in PubMed Google Scholar
Rights and permissions
Reprints and permissions
About this article
Mufune, P. Poverty and HIV/AIDS in Africa: Specifying the connections. Soc Theory Health 13 , 1–29 (2015). https://doi.org/10.1057/sth.2014.14
Download citation
Published : 29 October 2014
Issue Date : 01 February 2015
DOI : https://doi.org/10.1057/sth.2014.14
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- material deprivation (relative and absolute)
- vulnerability and social exclusion
- Find a journal
- Publish with us
- Track your research
- Election 2024
- Entertainment
- Newsletters
- Photography
- Personal Finance
- AP Investigations
- AP Buyline Personal Finance
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Election Results
- Delegate Tracker
- AP & Elections
- March Madness
- AP Top 25 Poll
- Movie reviews
- Book reviews
- Personal finance
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
The pioneer of America’s embattled global HIV program recalls the hope after years of despair
FILE - John Nkengasong, head of the U.S. President’s Emergency Plan for AIDS Relief, or PEPFAR, poses for a portrait on Aug. 29, 2023, in Washington. Nkengasong spoke to The Associated Press about his experience, at a period when challenges by anti-abortion groups and House Republican have made the future of PEPFAR uncertain. (AP Photo/Mark Schiefelbein, File)
FILE - John Nkengasong, head of the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR), speaks during an interview on Aug. 29, 2023, in Washington. Nkengasong spoke to The Associated Press about his experience, at a period when challenges by anti-abortion groups and House Republican have made the future of PEPFAR uncertain. (AP Photo/Mark Schiefelbein, File)
FILE - Ambassador-at-Large John Nkengasong, new head of the Bureau of Global Health Security and Diplomacy at the State Department, speaks during the launch of the new bureau, Aug. 1, 2023, at the State Department in Washington. Nkengasong spoke to The Associated Press about his experience, at a period when challenges by anti-abortion groups and House Republican have made the future of PEPFAR, the U.S. President’s Emergency Relief Plan for AIDS Relief, uncertain. (AP Photo/Jacquelyn Martin, File)
- Copy Link copied
WASHINGTON (AP) — Through his office window at what was then one of Africa’s few modern clinics dealing with HIV and AIDS, the man who now oversees the United States’ threatened global AIDS effort used to hear the sound of taxis pulling up throughout the day.
If he turned his head to look out the window, Dr. John Nkengasong said, he knew what he would see: another desperate family carrying a dying loved one — a man or woman already lapsing into a coma, a stick-thin child — and hoping to find help.
It was before the Bush administration started the U.S. President’s Emergency Relief Plan for AIDS Relief, known as PEPFAR , in 2004. There was almost no affordable effective treatment anywhere between South Africa and the Sahara, no rapid HIV tests or high-quality government labs, and few beds for AIDS patients.
Nkengasong has spent decades working in Africa on HIV and AIDS, a career intertwined with the U.S. program that since its introduction 20 years ago has transformed care in some of the hardest-hit countries and saved an estimated 25 million lives. He spoke to The Associated Press during a battle over funding in Congress that imperils the AIDS program’s future.
Opponents say the HIV/AIDS funding could be indirectly supporting abortion abroad, although the Biden administration and PEPFAR’s defenders say there is no evidence that it does. After a handful of conservative lawmakers threatened for months to block the funding unless restrictions were attached, a compromise was struck in late March that extends the funding for a year.
But advocates of the program warn that without the full five-year renewal, its future remains in doubt as the political debate over abortion and reproductive rights only becomes more combative.
Before PEPFAR, in most cases, Nkengasong’s infectious disease clinic in Abidjan, in the Ivory Coast, could offer the families no care. In their loved ones’ last hours, the families who came there often were left to crouch outside, in the parking lot.
They would surround “a skeleton of a human being, with a tinge of flesh over their bodies,” Nkengasong recalled. “They held their loved ones, giving them the best comfort they could.”
Soon enough, the sound of wailing would rise through his windows. The cries signaled another death to HIV/AIDS, one of millions in Africa by the mid-2000s.
The scene would be repeated “nearly hour by hour,” Nkengasong said. Sometimes he would get up and close the curtains, blocking out the misery of an epidemic he could not then stem.
Two decades later, Nkengasong says, his trips to the region from his offices in Washington bring joyous meetings with men, women and children whose lives were saved through PEPFAR, credited as the biggest government effort ever against a single disease.
In all, the U.S. program has spent more than $110 billion on HIV care and treatment, local medical systems and social programs aimed at stemming infection. The U.S. says it has saved 25 million lives in sub-Saharan Africa and other vulnerable regions, including those of 5.5 million children.
‘A THRIVING INDUSTRY OF COFFINS’
Nkengasong, who was born in Cameroon and did his graduate studies in Belgium, worked in Africa in the 1990s, when the AIDS epidemic was raging all but unchecked.
It made for a “thriving industry of coffins,” he said. Visiting cities in Uganda, Rwanda, Kenya and elsewhere for his work on infectious diseases, he would travel streets lined by handmade coffins of all sizes.
Beds of infectious-disease clinics were full of “adults lying there looking like babies, because of what HIV had done. That ugly face,” Nkengasong recalled.
With early retroviral medication averaging $10,000 per patient per year, only 50,000 HIV-infected people in sub-Saharan Africa were estimated to be receiving effective treatment in the mid-to-late 1990s. That was out of what the World Health Organization said was 10 million people there living with HIV and AIDS.
THE ‘AHA’ MOMENT
One day in spring 2002, as he was in his lab conducting tests, a large American delegation suddenly arrived at the clinic in Abidjan.
Health Secretary Tommy Thompson and other leading U.S. health officials crowded into the facility, along with representatives of businesses and members of faith-based organizations.
“I remember opening the door and the first person who walked through was Dr. Fauci,” Nkengasong recounted. Anthony Fauci, a leading HIV researcher, was then a top official at the U.S. National Institutes of Health and a leader in Nkengasong’s field of HIV and AIDS work. “And he said, ‘John, good to see you again.’ And I was so excited.”
Unbeknownst to Nkengasong and his colleagues, national security adviser Condoleeza Rice and other officials privately had been making the case to President George W. Bush that the global HIV epidemic was where the U.S. could make a huge difference.
For the Bush administration, the epidemic presented an opportunity to do good at a time when the U.S. was waging war in Afghanistan and later Iraq as well after the Sept. 11, 2001 attacks.
Nine months after the Americans showed up in his lab, “we’re watching news on CNN, it was the State of the Union address,” Nkengasong recalled. “And President Bush announced the start of PEPFAR.”
That night, the president pledged an initial $15 billion over the next five years to tackle the AIDS epidemic around the world.
Nkengasong called it the “aha moment” for himself and others fighting AIDS in the most vulnerable region of the world.
Two decades later, AIDS deaths globally have fallen nearly 70% from their peak in 2004. Sub-Saharan Africa is still the most vulnerable region and home to two-thirds of the people living with HIV. But the PEPFAR program and others have strengthened health care systems to deal with infectious diseases, made treatment available to millions, and expanded support for the most at-risk populations, including women.
On a trip back to Abidjan, Nkengasong met a healthy 17-year-old girl, one of millions spared from infection at birth thanks to medical treatment that prevented HIV transmission from their infected mothers.
This past summer, he visited a clinic in Namibia where HIV-infected mothers had delivered “super healthy” babies thanks to treatment that saved them from infection.
“I grabbed some of the babies and looked at them,” he said. Holding them, he wondered what would have happened to them without proper care.
“And they just give you that smile,” he said.

Mayiga lauds Balaam's effort in NUP missing persons quest

The run is scheduled on Sunday 7th April 2024, under the theme “Men are stars in the fight against HIV/AIDS to save the Girl Child”.
Buganda Premier Charles Peter Mayiga has expressed support for Youth Minister Balaam Barugahara's effort in urging President Museveni to release Opposition National Unity Platform (NUP) supporters who were arrested during the 2021 general election campaigns.
Last week, Balaam asked the President to release NUP supporters detained for political reasons.
Katikkiro Mayiga affirmed his support for Barugahara's efforts and stated his willingness to engage with the NUP to facilitate release of the party supporters.
The Buganda Kingdom premier was speaking after meeting members of the Patriotic League of Uganda (PLU) at Bulange Mengo where they had called on Mayiga to buy kits for the Kabaka Birthday Run.
Members of PLU led by the State minister for National Guidance, Godfrey Kabbyanga, bought kits worth Shs20 million.
Minister Kabbyanga expressed gratitude to Buganda for its inclusive hospitality, irrespective of race or political affiliation.
‘’We are so grateful to the Kabaka and the entire kingdom for the open-door policy, welcoming everyone regardless of the religion or political affiliation,’’ Kabbyanga said.
The team had more than 10 members of Parliament from different regions as well as Balaam and Lilian Aber, the minister of state for relief, disaster preparedness and refugee affairs.
The Katikkiro also welcomed Bishop Wilson Kisekka of Luwero Diocese, who led a delegation from Bulemeezi, Katikkiro Mayiga asked leaders there to collaborate and fight defilement, which is so rampant in the area.
They also bough kits for three million Uganda shillings in support of the Kabaka Birthday Run.
Schools and institutions are increasingly visiting Bulange to purchase kits for participation in the run whose proceeds will go toward the HIV/AIDS prevention efforts.
This year's Kabaka birthday run is witnessing unprecedented popularity.
Reader's Comments
Popular this week, ugandans in qatar want pdm cash, adf commander 'baghdad' killed in joint updf-fardc operation, deputy speaker tayebwa commends gov't's multi-billion electricity scale-up project, the role of protests in uganda's political landscape, speculation rises over nrm's role in masaka nup rift, latest stories.

Police launch magazine celebrating women officers

EC conducting civic education in north

Singer Vinka to grace Tusker Malt conversessions season two finale

William Bugeme elected president of Congolese diaspora in Uganda

Government unveils plans for construction of Standard Gauge Railways

Uganda's Batwa People Petition Government for Recognition and Rights

Masaka's Stalled Health Center: A Story of Broken Promises and Mismanagement

New Curriculum in Ugandan Schools: A Tale of Two Realities as Bukomansimbi schools suffer

Besigye: I've been relaxed but now I am back

USMID interventions in Albertine, Rwenzori boost tourism

IMAGES
VIDEO
COMMENTS
Currently, South Africa has the highest HIV prevalence rate in the world. Out of the 58 million people in the country, 7.7 million are estimated to have contracted the virus (Avert, 2020). In the Southern Africa region, South Africa alone accounts for 30% of all new HIV infections.
South Africa remains the epicenter of the HIV pandemic as the largest AIDS epidemic in the world—20 percent of all people living with HIV are in South Africa, and 20 percent of new HIV infections occur there too. The country also faces a high burden of tuberculosis (TB), including multi-drug resistant TB, which amplifies its HIV epidemic.
South Africa is home to the largest HIV seropositive population in the world, with 7·2 million individuals.1 Since the country's first case of HIV in 1982, South Africa has come a long way to reduce HIV/AIDS-related rates of infection, morbidity, and mortality. Some responses to the epidemic fostered improvement, whereas others exacerbated the crisis. As a dramatic lesson, the denialist line ...
South Africa has made huge improvements in getting people to test for HIV in recent years and met the 2020 target of 90% of people with HIV knowing their status in 2018. But it is behind on increasing access to HIV treatment, hampered by the need to provide HIV treatment for more people than any other country in the world.
1. Introduction. The HIV epidemic in South Africa has been measured nationally using surveillance mechanisms and cross-sectional population-based HIV sero-prevalence surveys for more than 15 years [1,2,3,4,5].These surveys, conducted every 3-5 years, help monitor the HIV epidemic, its impact, and its dynamics in the country [1,2,3,4,5,6,7].Among the key findings from the fourth survey in ...
A 2008 study revealed that HIV/AIDS infection in South Africa was distinctly divided along racial lines: 13.6% of Black Africans in South Africa are HIV-positive, whereas only 0.3% of Whites living in South Africa have the disease. False traditional beliefs about HIV/AIDS, which contribute to the spread of the disease, persist in townships due to the lack of education and awareness programmes ...
Countries of the African continent continue to be disproportionately burdened by HIV/AIDS. South Africa has the highest HIV prevalence rates in the world, both among adults and children. In the Africa Science Focus podcast episode, the host and guests, including UNAIDS representatives, discuss the causes of South Africa's HIV burden (Africa ...
Chapter Three. AIDS IN SOUTH AFRICA: EXTENT, IMPLICATIONS, AND RESPONSE. The contemporary HIV/AIDS crisis in South Africa represents an acute example of how infectious diseases can undermine national resilience and regional stability. Roughly 25 percent of the country's adult population is currently infected with HIV, which makes South Africa ...
South Africa, where our study is based, is, possibly, the most important country in which to examine the end of AIDS. It has the world's largest epidemic, with 7.9 million people living with HIV. Among those aged 15-49 years, an estimated 20.6% have HIV (HSRC 2018 ).
In his essays about the AIDS crisis, he addresses the greatly contested statements made by former President Thabo Mbeki, which delayed access to proper treatment for many South Africans. ... 203) argues, the early cases of HIV/AIDS in South Africa were largely connected to the white community but by 1986, the year Cameron found out that he had ...
South Africa now is the country estimated to have the largest number of people (5.3 million hiv positive people as at December 2007) living with hiv / Aids. Despite this, the South African response to the hiv epidemic over the past decade has been characterised by a unique form of denialism in the highest echelons of political power.
However, the numbers of orphans resulting from aids-related deaths in South Africa are predicted to rise to over five million by 2014, making effective community response to the epidemic essential. Responses encompass different levels of care for orphans, community involvement in prevention and awareness efforts and continued advocacy and ...
This essay discusses popular media's presentation of South Africa's response to HIV, especially with respect to care and support of HIV infected persons and the provision of antiretroviral therapy (ART). Attempting to comprehensively discuss all facets associated with this issue may be a lifetime endeavor. However, the most pertinent issues ...
South Africa, are also thought to have contributed to the rapid spread of HIV/AIDS. Mark Horton • 115 0 5 10 15 20 25 30 1990 92 94 96 98 2000 02 Figure 7.1. HIV Prevalence Rates Among Antenatal Clinic Attendees (In percent) Sources: Department of Health (2002 and 2003). 0.7 1.7 2.2 4 7.6 10.4 14.2 17 22.8 22.4 24.5 24.8 26.5
Clinically defined in 1983, HIV/AIDS gained prominence in the international scientific community as a disease of homosexual men. Accordingly, the earliest data on HIV/AIDS (that is, data for the period 1983-1986) in South Africa focuses almost entirely upon homosexual men. In fact, it was only in 1990 that antenatal clinic attendees were tested ...
HIV/Aids is becoming the most devastating disease humankind has ever faced. In the same UN report on 2007 (UN 2008 Global Report on the HIV and AIDS Epidemic) around 5.7 million South Africans were estimated as having HIV or Aids, including 300 000 children under the age of 15 years. 350 000 people died from AIDS in South Africa in 2007.
ENGLISH ABSTRACT: South Africa faces one of the world's most severe HIV/AIDS epidemics. Whereas the disease was initially only regarded as a serious health crisis, it is now clear that the epidemic will also have economic repercussions. The objective of this study is to project the extent of the macro-economic impact of HIV/AIDS in South Africa over the next 10 to 15 years.
infections of 36.7 million people in 2017 (UNAIDS, 2017a; Statistics South Africa, 2017). It is estimated that 19.2 percent of South Africans of ages 15 to 59 were infected with HIV/AIDS in 2015 (UNAIDS, 2015a). In South Africa, Gauteng province had the fifth highest HIV and AIDS prevalence in 2012 (Human Sciences Research Council, 2014).
Young women in South Africa are at great risk of being infected with HIV. In 2005, HIV infection prevalence in the age group 15-24 years was 16.9% in women and 4.4% in men ().The high HIV prevalence in this country is a result of a number of factors which include the following: poverty, violence against women, cultural limitations that promote intergenerational sex, non-condom use and ...
The macroeconomic impact of aids is determined by the demographics of those most affected, the young and economically active, and in the costs of combating the disease. Economic growth will be less than it would be without aids, although the exact reduction is hard to determine. Type. Chapter. Information. HIV/AIDS in South Africa , pp. 417 - 431.
South Africa, with currently 4-6 million people estimated to be HIV-positive, faces. one of the world's most severe HIV/AIDS epidem ics. The economic implications of. HIV/AIDS, which are expected ...
As Catley-Carlson and Outlaw (1998) pointed out, there are several misconceptions among social scientists analysing the effect of poverty in the African context. The first is that poverty (and by extension HIV/AIDS) is a hopelessly difficult problem in African countries. In reality, although Africa lags behind on most development indices, some economies are growing rapidly, and some countries ...
THREE ESSAYS ON HIV/AIDS RELATED ISSUES IN SOUTHERN AFRICA I-Heng Lee A dissertation submitted to the faculty of the University of North Carolina at Chapel Hill in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Department of Health Policy and Management of the Gillings School of Global Public Health.
Of the estimated 7.8 million people living with HIV in South Africa in 2023 (12.6% of the population), just under 5.9 million were on treatment. This translates to treatment coverage of 75%, or one in every four people living with HIV not being on treatment. Antiretroviral treatment is recommended for all people living with the infection.
With early retroviral medication averaging $10,000 per patient per year, only 50,000 HIV-infected people in sub-Saharan Africa were estimated to be receiving effective treatment in the mid-to-late 1990s. That was out of what the World Health Organization said was 10 million people there living with HIV and AIDS. THE 'AHA' MOMENT
The run is scheduled on Sunday 7th April 2024, under the theme "Men are stars in the fight against HIV/AIDS to save the Girl Child". Buganda Premier Charles Peter Mayiga has expressed support for Youth Minister Balaam Barugahara's effort in urging President Museveni to release Opposition National Unity Platform (NUP) supporters who were arrested during the 2021 general election campaigns.