- Search Menu
- Themed Collections
- Editor's Choice
- Ilona Kickbusch Award
- Supplements
- Author Guidelines
- Submission Online
- Open Access Option
- Self-Archiving Policy
- About Health Promotion International
- Editorial Board
- Advertising and Corporate Services
- Journals on Oxford Academic
- Books on Oxford Academic


Article Contents
Introduction, supplementary material.
- < Previous
Promoting lung cancer awareness, help-seeking and early detection: a systematic review of interventions
- Article contents
- Figures & tables
- Supplementary Data
Mohamad M Saab, Serena FitzGerald, Brendan Noonan, Caroline Kilty, Abigail Collins, Áine Lyng, Una Kennedy, Maidy O’Brien, Josephine Hegarty, Promoting lung cancer awareness, help-seeking and early detection: a systematic review of interventions, Health Promotion International , Volume 36, Issue 6, December 2021, Pages 1656–1671, https://doi.org/10.1093/heapro/daab016
- Permissions Icon Permissions
Lung cancer (LC) is the leading cause of cancer death. Barriers to the early presentation for LC include lack of symptom awareness, symptom misappraisal, poor relationship with doctors and lack of access to healthcare services. Addressing such barriers can help detect LC early. This systematic review describes the effect of recent interventions to improve LC awareness, help-seeking and early detection. This review was guided by the Cochrane Handbook for Systematic Reviews of Interventions. Electronic databases MEDLINE, CINAHL, ERIC, APA PsycARTICLES, APA PsycInfo and Psychology and Behavioral Sciences Collection were searched. Sixteen studies were included. Knowledge of LC was successfully promoted in most studies using educational sessions and campaigns. LC screening uptake varied with most studies successfully reducing decision conflicts using decision aids. Large campaigns, including UK-based campaign ‘Be Clear on Cancer’, were instrumental in enhancing LC awareness, promoting help-seeking and yielding an increase in chest X-rays and a decrease in the number of individuals diagnosed with advanced LC. Multimodal public health interventions, such as educational campaigns are best suited to raise awareness, reduce barriers to help-seeking and help detect LC early. Future interventions ought to incorporate targeted information using educational resources, face-to-face counselling and video- and web-based decision aids.
Lung cancer (LC) is the leading cause of cancer incidence and mortality in men and women globally, with 2.1 million new cases (11.6% of the total cancer cases) and 1.8 million deaths (18.4% of the total cancer deaths) in the year 2018 alone ( Bray et al. , 2018 ). More than half of LC cases (53%) are diagnosed among men and women aged 55–74 years (median age = 70 years) ( Torre et al. , 2016 ). In contrast to the increase in survival rates for most cancers, LC is typically diagnosed at advanced stages with a five‐year survival rate of 5% ( Siegel et al. , 2018 ).
Screening individuals at risk for LC with low dose computed tomography (LDCT) has been shown to reduce LC mortality by up to 20% ( National Lung Screening Trial Research Team, 2011 ; Marcus et al. , 2016 ). The European Union stressed the importance of starting LC screening using LDCT throughout Europe ( Oudkerk et al. , 2017 ). However, to date, very few countries possess screening programs for LC ( Siegel et al. , 2018 ), and the uptake of LC screening in countries like the United States of America (USA) remains low, with only 4% of 6.8 million eligible individuals reporting having undergone LDCT ( Jemal and Fedewa, 2017 ). This highlights the importance of raising awareness of LC, supporting at-risk individuals in making a decision regarding LC screening and promoting early presentation for symptoms indicative of LC.
A persistent cough, a change in a pre-existing cough, and shortness of breath are common symptoms of early-stage LC ( Chowienczyk et al. , 2020 ). Haemoptysis remains the strongest symptom predictor of LC, yet it occurs in only a fifth of patients ( Walter et al. , 2015 ). Patients with LC can also be asymptomatic until systemic symptoms, such as unexplained weight loss and fatigue occur, signalling advanced disease ( American Cancer Society, 2019 ). Therefore, the symptom signature of LC is considered to be broad ( Koo et al. , 2018 ) in comparison to cancers that have a narrow symptom signature with single identifiable symptoms, such as breast ( O'Mahony et al. , 2013 ) and testicular ( Saab et al. , 2017a ) cancers. This may lead to delay in early presentation and LC diagnosis ( Holmberg et al. , 2010 ).
Early help-seeking for symptoms indicative of LC is key for timely and early diagnosis and improved survivorship. However, patients diagnosed with LC experience, on average, a 6-month delay between symptom onset and initiation of treatment ( Ellis and Vandermeer, 2011 ). This is known to have detrimental effects on early diagnosis, quality of life, cost of healthcare, and patients’ eligibility for curative treatment ( Walter et al. , 2015 ; World Health Organisation, 2020 ). Several barriers to help-seeking and early detection of LC exist, such as lack of symptom awareness, poor relationship with physicians and lack of healthcare access ( Carter‐Harris, 2015 ; Koo et al. , 2018 ; Cassim et al. , 2019 ; Cunningham et al. , 2019 ). Symptom misappraisal is another key contributor to help-seeking delay, especially in the presence of risk factors like smoking ( Smith et al. , 2016 ) and comorbidities, such as chronic obstructive pulmonary disease (COPD) ( Cunningham et al. , 2019 ). For instance, a survey of 2042 participants found that being a smoker was associated with a reduced likelihood of help-seeking for symptoms indicative of LC, potentially due to pre-existing respiratory symptoms associated with chronic smoking ( Smith et al. , 2016 ). Similarly, in their qualitative study, Cunningham et al. (2019) found that individuals with COPD attributed changes in their respiratory symptoms to their COPD and failed to mention LC, despite having a significantly greater risk for LC. LC stigma also impacts negatively on help-seeking for LC ‘alarm’ symptoms. Indeed, a survey of 93 symptomatic individuals found that higher levels of perceived LC stigma were associated with a median waiting time of 41 days prior to seeking medical help for symptoms of concern ( Carter‐Harris, 2015 ). Therefore, raising awareness and promoting early presentation for symptoms indicative of LC can help detect LC early and improve survival.
The international literature has highlighted the importance of interventions that target awareness, symptom evaluation and early help-seeking for LC ( Dlamini et al. , 2019 ). For example, a national campaign in the UK entitled ‘Be Clear on Cancer’ resulted in a significant increase in LC awareness, respiratory consultations, number of physician-prescribed chest X-rays and CT scans, and number of LC cases diagnosed at early stages ( Ironmonger et al. , 2015 ). Interventions often vary in terms of modalities, intended mechanisms, theoretical basis and target area/groups. This systematic review aims to describe the effect of recent interventions to improve (i) knowledge and/or awareness of LC; (ii) help-seeking intentions and/or behaviours for LC and (iii) early detection of LC.
This systematic review was guided by the Cochrane Handbook for Systematic Reviews of Interventions ( Higgins et al. , 2019 ) and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist ( Moher et al. , 2009 ).
Eligibility criteria
The review eligibility criteria were predetermined using the PICO (Population, Intervention, Comparison, Outcomes) framework ( Moher et al. , 2009 ). Population: conducted among individuals of any age including at-risk populations; Intervention: included any intervention, programme, or campaign; Comparison: incorporated within- or between-group comparison; and Outcomes: reported on at least one of the review outcomes (i.e. knowledge/awareness of LC, help-seeking intentions/behaviours for LC and/or early detection of LC). Studies were excluded if they included patients with LC, used LC screening as the intervention, did not incorporate a comparator, and used any nonexperimental design.
Search strategy
A search was conducted using the electronic databases MEDLINE, CINAHL, ERIC, APA PsycARTICLES, APA PsycInfo and Psychology and Behavioral Sciences Collection. Keywords were truncated and combined using Boolean operators ‘OR’ and ‘AND’ and the proximity indicator ‘N.’ The following keywords were searched on title or abstract: (lung* OR pulmo*) N3 (cancer* OR neoplas* OR malignan* OR tumo*) AND (know* OR aware* OR detect* OR help-seek*) AND (interven* OR program* OR campaign* OR trial* OR experiment* OR educat*).
The search was conducted on 15 January 2020 and, for pragmatic reasons, was limited to studies published in English between January 2015 and January 2020. Of note, there is no gold standard for limiting the search by year of publication, though studies published within a 10-year timeframe are broadly considered to be recent ( Wilhelm and Kaunelis, 2005 ). However, knowledge decay is common in public health interventions and is one of the reasons researchers frequently develop and refine health promotion interventions, whilst older interventions and campaigns become increasingly obsolete over time ( Nimmons et al ., 2017 ; Saab et al ., 2018 ). Therefore, it had been agreed a priori to limit the current search to evidence published within a five-year timeframe in order to source and synthesize the most up-to-date evidence relating to the latest interventions and educational LC campaigns.
Study selection
Records were transferred to Covidence, an online software used to produce systematic reviews of interventions ( The Cochrane Collaboration, 2020 ). Titles and abstracts were screened, and irrelevant records were excluded. The full text of potentially eligible records was then screened and reasons for exclusion were recorded. Title, abstract and full-text screenings were conducted in pairs. For a screening decision to be made, each record was screened twice by two independent reviewers. Screening conflicts were resolved by a third reviewer.
Data extraction and synthesis
Data were extracted using a standardized data extraction table ( Supplementary Table 1S ) as follows: author(s); year; country; aim(s); design; theoretical underpinning; sample; setting; relevant outcomes; intervention; procedures; instruments; follow-up times and findings. Data extraction was conducted by one reviewer. Each extracted study was then cross-checked by the rest of the review team.
A meta-analysis with summary measures of intervention effect requires that the included studies be sufficiently homogenous ( Higgins et al. , 2019 ). Therefore, given the heterogeneity of the studies in terms of design, outcomes and outcome measures, a meta-analysis was not plausible. Instead, a narrative synthesis of study findings was conducted, and findings were synthesized and discussed according to the review aims under the headings (i) knowledge and awareness, (ii) help-seeking and (iii) early detection.
Quality and level of evidence
The Mixed Methods Appraisal Tool (MMAT) helps appraise the methodological quality of five study categories: qualitative studies, randomized controlled trials (RCTs), nonrandomized studies, quantitative descriptive studies and mixed methods studies ( Hong et al. , 2018 ). In line with the current review aim and eligibility criteria, the methodological quality of three study categories was appraised, namely RCTs (seven quality appraisal items), nonrandomized studies (seven quality appraisal items) and mixed methods studies (17 quality appraisal items). Each of the quality appraisal items was judged on a ‘Yes’, ‘No’ and ‘Can’t tell’ basis. The clarity of research questions and the use of appropriate data collection methods to address those were assessed for all study categories. For RCTs and nonrandomized studies, sample representativeness and similarities between participant groups at baseline were assessed. Other items related to blinding the outcome assessor, reporting of complete outcome data, accounting for confounders, and ensuring that interventions have been administered as intended. For mixed methods studies, additional items assessed the integration of quantitative and qualitative methods and explored whether divergences and inconsistencies between quantitative and qualitative results have been adequately addressed.
The Scottish Intercollegiate Guidelines Network’s ( Scottish Intercollegiate Guidelines Network, 2019 ) guidelines were used to assess the level of evidence per study. This assesses the study design and how well a study was carried out and helps judge whether research conclusions are accurate. Level of evidence scores range from 1 ++ , 1 + , 1 – , 2 ++ , 2 + , 2 – , 3, to 4. A score of 1 ++ corresponds to high quality meta-analyses, systematic reviews of RCTs, or RCTs with a very low risk of bias, whereas a score of 4 is assigned to expert opinions ( Scottish Intercollegiate Guidelines Network, 2019 ).
Level of evidence and quality assessments were conducted by one reviewer and verified independently by the review team. Discrepancies in quality appraisal ratings and level of evidence assessment scores were then discussed among the review team until consensus was reached. When consensus was not reached between two reviewers, a third reviewer was asked to resolve conflicts. Studies were included in the present review regardless of their methodological quality and level of evidence to minimize the risk of study selection and reporting bias ( Higgins et al. , 2019 ).
Database searching yielded 4362 records. Following deletion of duplicates, 3270 records were screened on title and abstract and 3222 irrelevant records were excluded. Full texts of the remaining 48 records were screened. Of those, 16 studies were included in this review ( Figure 1 ).

Study identification, screening and selection process.
Study characteristics
Most studies were conducted in the USA ( n = 8) and the UK ( n = 6), with the majority being uncontrolled before–after studies ( n = 8) and RCTs ( n = 4). Half of the studies ( n = 8) used multiple researcher-designed instruments to collect data and collected data from rural/underprivileged areas. Five studies were underpinned by theory including the Health Belief Model ( Fung et al. , 2018 ; Williams et al. , 2021 ); elements of Self-Regulation Theory, Theory of Planned Behaviour, and Implementation Intentions ( Emery et al. , 2019 ); Ottawa Decision Support Framework ( Lau et al. , 2015 ) and Theory of Planned Behaviour ( Mueller et al. , 2019 ). Six studies used large or national multimodal campaigns as their intervention with three studies reporting on the same campaign namely the ‘Be Clear on Cancer’ UK-based campaign ( Ironmonger et al. , 2015 ; Moffat et al. , 2015 ; Power and Wardle, 2015 ) ( Table 1 ).
Study characteristics ( n = 16)
n = 5 studies underpinned by theory.
n = number of times an outcome was measured.
n = number of times an instrument was used.
All 16 studies had clear research questions and used appropriate data collection methods. RCTs ( n = 4) performed appropriate randomization, had comparable groups at baseline, presented complete data outcomes, and had participants adhere to the assigned intervention; however, only one RCT reported on blinding the outcome assessor ( Emery et al. , 2019 ) ( Supplementary Table 2S ). As for non-RCTs ( n = 11), only three studies reported that participants were representative of the target population ( Power and Wardle, 2015 ; Sakoda et al. , 2020 ; Williams et al. , 2021 ), and one study accounted for confounders ( Williams et al. , 2021 ). Otherwise, all non-RCTs met the remaining MMAT criteria ( Supplementary Table 3S ). The only mixed methods study ( Cardarelli et al. , 2017 ) met most of the MMAT criteria; however, it was unclear as to how data were synthesized and whether there were divergences and inconsistencies between quantitative and qualitative results ( Supplementary Table 4S ).
Half of the studies ( n = 8) scored 2 + on the SIGN level of evidence criteria, indicating well-conducted non-RCTs with a low risk of confounding or bias and a moderate probability that the relationship is causal. Only one RCT ( Emery et al. , 2019 ), and one non-RCT ( Williams et al. , 2021 ) had a low risk of bias.
Findings from individual studies are reported in Table 2 .
Findings from individual studies ( n = 16)
CG, control group; CI, confidence interval; CT, computed tomography; CXR, chest X-ray; DA, decision aid; GP, general practitioner; IG, intervention group; LC, lung cancer; LCS, lung cancer screening; LDCT, low dose computed tomography; M, mean; MD, mean difference; NR, not reported; O, objective; ODSF, Ottawa decision support framework; RCT, randomized controlled trial; RR, relative rate; SD, standard deviation; SRT, self-regulation theory; TPB, theory of planned behaviour; UK, United Kingdom; USA, United States of America; χ 2 , chi-square test.
Findings according to review objectives: O1: knowledge and/or awareness of LC; O2: help-seeking intentions and/or behaviours for LC; O3: early detection of LC, including clinical outcomes.
Knowledge and awareness
Subjective and objective knowledge of LC were promoted in 12 studies using approaches, such as decision aids ( Lau et al. , 2015 ; Mazzone et al. , 2017 ; Housten et al. , 2018 ); film and booklet ( Ruparel et al. , 2019 ) and educational sessions ( Williams et al. , 2021 ; Sakoda et al. , 2020 ). Lau et al. (2015) evaluated the effectiveness of a web-based decision aid ( www.shouldiscreen.com ) among 60 at-risk individuals and found that knowledge of risk factors, benefits and harms of screening, screening eligibility and percentage of benign lumps increased significantly 4 months post-test [pre-test: mean = 7.52/14, standard deviation (SD) = 1.89; post-test: mean = 10.93/14, SD = 2.19; p < 0.001]. A second study used the same decision aid and also reported statistically significant increases in knowledge of screening-eligible ages ( p < 0.0001), smoking history eligibility criteria ( p < 0.0001), benefits ( p = 0.03) and harms ( p < 0.0001) of LC screening 1 month post-test ( Mazzone et al. , 2017 ).
An information film and booklet (intervention group [IG]) compared with booklet only (control group [CG]) yielded a statistically significant increase in knowledge in both groups, with a greater improvement among IG ( p < 0.001) ( Ruparel et al. , 2019 ). Educational interventions in the form of LC screening classes ( Sakoda et al. , 2020 ) and a 4-week educational intervention ( Williams et al. , 202 1) were also instrumental in increasing objective knowledge of LC screening immediately post-test and 3 months post-test (both p < 0.001).
As for knowledge of LC signs, symptoms, and risk factors, a 90-min educational session significantly increased awareness of warning signs for LC and LC risk factors 1 month, 3 months and 6 months post-test ( p < 0.001) ( Meneses-Echávez et al. , 2018 ). Three before–after studies evaluated the impact of the UK campaign ‘Be Clear on Cancer’ on knowledge of LC signs and symptoms ( Ironmonger et al. , 2015 ; Moffat et al. , 2015 ; Power and Wardle, 2015 ). The campaign was successful in increasing awareness of cough ( p < 0.001), breathlessness ( p = 0.024), haemoptysis ( p < 0.001), chest pain ( p = 0.015) and unexplained weight loss ( p < 0.001) as symptoms of LC ( Ironmonger et al. , 2015 ). Recall and recognition of a persistent cough or hoarseness as signs of LC also increased significantly from 67% pre-campaign to 78% post-campaign ( p < 0.001) ( Power and Wardle, 2015 ). The increase in unprompted awareness of cough/hoarseness was significantly lower among men as compared with women (45% vs 55%; p = 0.001) ( Moffat et al. , 2015 ), and there was no statistically significant change in pre- and post-campaign results for individuals aged 75 years or more ( p = 0.721) as compared with 11% increase for the 55–74 years age group ( p = 0.001). As for prompted awareness, the proportion of participants identifying a ‘cough for 3 weeks or more that doesn’t go away’ as definite warning sign of LC increased from 18% pre-campaign to 33% post-campaign ( p < 0.001), with no statistically significant difference between men and women pre-campaign ( p = 0.389) and post-campaign ( p = 0.587) ( Moffat et al. , 2015 ).
In contrast, a spirometry, self-help manual, action and coping plans and tailored monthly prompts (SMS, emails, post-cards, phone calls, and fridge magnets) (IG) yielded no statistically significant changes in knowledge in comparison to spirometry and brief general discussion about lung health (CG) 1 and 12 months post-test (mean difference = -0.2, p = 0.3954 vs. mean Difference = –0.1, p = 0.6083, respectively) ( Emery et al. , 2019 ). Similarly, a four-day research education seminar on cancer prevention (IG) and biospecimen collection (CG) did not yield a statistically significant increase in awareness of LC early detection immediately post-education ( p = 0.18 and p = 0.49, respectively; group comparison p = 0.13) ( Fung et al. , 2018 ).
Help-seeking
Ten studies addressed help-seeking for LC including seeking help from a General Practitioner (GP) and deciding to undertake LC screening. Spirometry, self-help manual, action and coping plans, and tailored monthly prompts which initially failed to raise LC awareness, were successful in increasing respiratory consultations by 40% among the IG [95% Confidence Interval (CI) IG 0.57 (0.47–0.70), CG 0.41 (0.32–0.52), Relative Rate 1.40 (1.08–1.82); p = 0.0123] ( Emery et al. , 2019 ).
Mueller et al. (2019) conducted a feasibility RCT with block randomization to four groups: tailored information and Theory of Planned Behaviour components (IG); untailored information with Theory of Planned Behaviour components; tailored information without Theory of Planned Behaviour components; and usual care (CG). It was found that the four groups differed significantly in scores on the help-seeking intention variable, ( χ 2 (3) = 8.14, p = 0.04), with the highest intention reported in the IG ( Mueller et al. , 2019 ). In contrast, an uncontrolled before–after study using the Health Belief Model reported no statistically significant changes in intent and cue to action immediately and 3 months following a 4-week educational intervention ( Williams et al. , 2021 ).
The campaign ‘Be Clear on Cancer’ was instrumental in increasing help-seeking for LC symptoms and reducing barriers to help-seeking ( Ironmonger et al. , 2015 ; Moffat et al. , 2015 ; Power and Wardle, 2015 ). Help-seeking for cough increased by 63% during the campaign and by 46% 8 weeks later among at-risk groups ( p < 0.001) ( Ironmonger et al. , 2015 ). The campaign was also associated with a 63% increase in GP attendances for symptoms linked to the campaign, with no difference between genders ( p = 0.107) ( Moffat et al. , 2015 ). The largest increase was seen in the 50–59-year age group in comparison to older age groups (88%, p < 0.001). As for perceived barriers to help-seeking, there was no statistically significant change in barriers targeted by the campaign, such as being ‘worried about wasting the doctor’s time’ (26% in 2010 and 24% in 2012, p = 0.158) or believing that the ‘doctor would be difficult to talk to’ (14% in 2010 and 13% in 2012, p = 0.617). However, barriers not targeted by the campaign, such as being ‘too scared’ ( p = 0.016), being ‘worried about what the doctor might find’ ( p = 0.002), ‘difficulty arranging transport’ ( p = 0.002), ‘difficulty making an appointment’ ( p = 0.025) and being ‘too busy’ ( p = 0.009) were less endorsed post-campaign ( Power and Wardle, 2015 ).
In terms of screening decisions, Cardarelli et al. (2017) conducted a multimodal campaign titled ‘Terminate Lung Cancer’ and found that, out of 145 high-risk individuals, 73 (50.3%) came across the campaign. Of those, 5 (3.4%) thought about getting an LDCT and 2 (1.4%) sought information about LDCT. Three studies used the Decision Conflict Scale ( Lau et al. , 2015 ; Ruparel et al. , 2019 ; Sakoda et al. , 2020 ). A web-based decision aid yielded a decrease in Decision Conflict Scale scores indicating lower decisional conflict (pre-test mean = 46.33, SD = 29.69; post-test mean = 15.08, SD = 25.78; p < 0.001) ( Lau et al. , 2015 ). In contrast, participants who watched an information film and read a booklet (IG) had higher decisional conflict (mean = 8.5/9, SD = 1.3) in comparison to those who read a booklet only (CG) (mean = 8.2/9, SD = 1.5; p = 0.007) ( Ruparel et al. , 2019 ). Moreover, an LC screening class led to a decrease in the proportion of at-risk participants who wanted to be screened from 80% pre-test to 65% immediately post-test ( Sakoda et al. , 2020 ).
Early detection
The effect of interventions on early detection of LC (i.e. screening uptake and clinical outcomes) was addressed in seven studies. LDCT uptake varied widely between 38% after a 4-week educational intervention ( Williams et al. , 2021 ) and 94.6% following face-to-face counselling and shared web-based decision-making ( Mazzone et al. , 2017 ). The multimodal ‘Terminate Lung Cancer’ campaign yielded a significant uptake of LDCT in the two intervention regions as compared with the control region ( p -value not reported) ( Cardarelli et al. , 2017 ). Another social media-based campaign was linked to a 3% increase in LDCT per week immediately post-campaign and a further 5.8% increase a week later ( p = 0.001) ( Jessup et al. , 2018 ). In contrast, LDCT completion rates showed no statistical significance between those who watched an information film and read a booklet (IG) and those who read a booklet only (CG) ( p = 0.66) ( Ruparel et al. , 2019 ).
Clinical outcomes reported following large campaigns included the number of chest X-rays and CT scans ordered, new LC cases, stage at diagnosis and LC treatments ( Ironmonger et al. , 2015 ; Kennedy et al. , 2018 ). The ‘Be Clear on Cancer’ campaign was associated with an increase in GP-referred chest X-rays and CT scans by 18.6% and 15.7%, respectively ( p < 0.001) ( Ironmonger et al. , 2015 ). Moreover, LC diagnosis increased by 9.1% ( p < 0.001) for IG and 1.5% for the CG ( p = 0.373) and the proportion of nonsmall cell LC diagnosed at stage I increased from 14.1% to 17.3% ( p < 0.001) and decreased from 52.5% to 49% ( p < 0.001) for stage IV. As for treatments, there was a 2.3%-point increase ( p < 0.001) in resections for patients seen (IG), with no evidence that these proportions changed in CG pre-campaign ( p = 0.404) and post-campaign ( p = 0.425) ( Ironmonger et al. , 2015 ). A local UK campaign which overlapped with ‘Be Clear on Cancer’ also resulted in an 80.8% increase in community-ordered chest X-rays between the 3 years pre-campaign and 3 years post-campaign and yielded an 8.8% increase in patients diagnosed with stage I/II LC as opposed to a 9.3% reduction in cases of stage III/IV LC ( χ 2 (1) = 32.2, p < 0.0001) ( Kennedy et al. , 2018 ).
A wide range of educational interventions were implemented across the reviewed studies, with several studies testing large national and multimodal campaigns. Most interventions explored knowledge and awareness of LC and its screening, while others examined help-seeking behaviours and early detection of LC, including screening uptake and clinical outcomes, such as stage of LC at diagnosis and treatments received.
Overall, participants were poorly informed about LC at baseline. However, web-based decision aids ( Lau et al. , 2015 ; Mazzone et al. , 2017 ; Housten et al. , 2018 ), information resources ( Ruparel et al. , 2019 ) and educational sessions ( Sakoda et al. , 2020 ; Williams et al. , 2021 ) yielded a significant increase in knowledge and awareness of LC risk factors, warning signs, benefits and harms of screening, and screening eligibility. Notably, tailored monthly prompts (i.e. SMS, emails, post-cards, phone calls, fridge magnets) did not significantly increase LC awareness, detection, or screening uptake ( Emery et al. , 2019 ).
In terms of participants’ sociodemographic profiles, men demonstrated lower awareness than women ( Moffat et al. , 2015 ). Gender disparity in knowledge is well documented in other malignancies including colorectal ( Clarke et al. , 2016 ) and skin ( Christoph et al. , 2016 ) cancers. Age also played a role in increased LC awareness, with a significant improvement in unprompted awareness in the 55–74 years age group ( Moffat et al. , 2015 ). This finding is encouraging since LC is mainly diagnosed in older generations. In the USA, for example, LC is most common among those aged 65 years or older, with a median age of 71 years at diagnosis ( National Cancer Institute, 2020 ). In an Irish study, Ryan et al. (2015) emphasized the importance of age as a significant risk factor in cancer diagnosis and highlighted that, even though age is a nonmodifiable risk factor, researchers must target information to increase LC awareness and promote consultation among at-risk age groups ( McCutchan et al. , 2019 ).
In keeping with high-risk groups, half of the studies were conducted in rural/underprivileged areas. A pooled analysis of case–control studies found that socioeconomic deprivation and lack of healthcare access among at-risk populations were associated with advanced LC at diagnosis ( Hovanec et al. , 2018 ). Therefore, McCutchan et al. (2019) identified the need for multi-faceted community-based interventions to encourage high-risk individuals, living in deprived areas, to seek LC information outside of the GP setting. This may promote better relationships between high-risk groups and trained intervention facilitators, subsequently improving engagement in LC screening and help-seeking ( McCutchan et al. , 2019 ).
Interventions aiming to increase help-seeking intentions ought to consider incorporating tailored information based on, for example, the components of the Theory of Planned Behaviour ( Mueller et al. , 2019 ). Such theory-based interventions should address individuals’ attitudes, social norms, and perceived behaviour control as well as integrating measures to ensure effective decision-making skills ( Ruparel et al. , 2019 ). Moreover, at-risk individuals should be encouraged to consider the benefits and harms of health screening in order to make informed decisions and improve health outcomes ( Bell et al. , 2017 ). Current evidence suggests that the use of decision aids can increase knowledge of the benefits and harms of LC screening, whilst providing a better understanding of the nature of screening ( Reuland et al. , 2018 ). Therefore, methods to help dissipate LC screening decisional conflicts, such as video- and web-based decision aids should be considered ( Lau et al. , 2015 ; Mazzone et al. , 2017 ; Housten et al. , 2018 ). Notably, the use of such aids proved successful in reducing decision conflict and cancer-related distress among individuals at risk for breast ( Metcalfe et al. , 2017 ), prostate ( Reidy et al. , 2018 ) and colorectal ( Perestelo-Perez et al. , 2019 ) cancers, inclusive of those with low literacy and health literacy levels.
Three studies reported on a successful national campaign in the UK titled ‘Be Clear on Cancer’ which resulted in a significant increase in awareness of LC symptoms ( Ironmonger et al. , 2015 ; Moffat et al. , 2015 ; Power and Wardle, 2015 ). This campaign also helped reduce barriers to help-seeking, increase GP consultations for at-risk individuals, increase in individuals requesting chest X-rays, and increase in GP-referred chest X-rays and CT scans. Moreover, there was an encouraging increase in early-stage LC diagnosis as a result of this campaign ( Ironmonger et al. , 2015 ). Alternative strategies, such as the use of social media campaigns could be modified to drive engagement with health services in people with minor/early symptoms ( Jessup et al. , 2018 ). Freeman et al. (2015) reported on lessons learned from the use of social media in public health campaigns and identified positive changes in motivation and action. The use of social media makes it easier to connect with specific population cohorts, increase information visibility, and potentially deliver successful health promotion campaigns. It is worth noting, however, the age profile of at-risk individuals and the learning strategies that appeal to high-risk age groups ( Chelf et al. , 2002 ; Saab et al. , 2017b ).
There are several complex barriers that can affect an individual’s understanding of a disease and impede decision-making and help-seeking. It is evident from this review that multimodal public health campaigns would best suit high-risk populations. Approaching health from a population perspective, future interventions and campaigns should consider including a structured theoretical framework, such as the Theory of Planned Behaviour ( Ajzen and Manstead, 2007 ). Moreover, future interventions ought to incorporate targeted information through the use of educational resources, face-to-face counselling, and video- and web-based decision aids, while being cognizant of the preferred learning strategies and the key characteristics of health-promoting messages that would appeal to at-risk groups.
Limitations
Rigour was sought in the conduct and reporting of this systematic review. However, several threats to generalizability are worthy of note. While some of the review team members were multilingual, none of the languages used in non-English language papers was spoken by the research team and no resources were available to professionally translate non-English papers to English, which resulted in excluding those. Moreover, while the five-year search limit helped source the latest evidence, older interventions were omitted. Generalizability of findings is also hindered by the small number of studies included and the fact that almost half of the reviewed studies ( n = 7) did not meet two key quality assessment criteria namely ‘participants representative of target population’ and ‘confounder accounted for in the design and analysis’ and only two studies had a low risk of bias ( Emery et al. , 2019 ; Williams et al. , 2021 ). Study selection bias could have occurred, since only outcomes that were in line with the review aims were reported and no records were sought from the grey literature.
Despite this being a systematic review of interventions, a meta‐analysis was not plausible primarily due to heterogeneity in study designs, outcomes and outcome measures. The reliability and generalizability of the review results are limited further by the presence of three sources of bias: (i) study designs: the included studies used six different study designs; (ii) study instruments: half of the studies ( n = 8) used researcher-designed instruments and failed to report on the validity and reliability of those instruments and (iii) follow-up periods: diverse follow-up periods of data collection were evident, with some studies not having baseline data and others measuring outcomes either immediately post-test or at multiple points post-test. The implication is that findings relating to subjective data measured objectively would change over time and repeat measures at different points in time give different results. Hence, a consistent prepost repeat measures approach is key to minimizing this bias in future research.
Supplementary material is available at Health Promotion International online.
This study was funded by the National Cancer Control Programme, Health Service Executive, Ireland.
Ajzen I. , Manstead A. S. ( 2007 ) 4 Changing health-related behaviours . The Scope of Social Psychology , 43- , 43 – 63 .
Google Scholar
American Cancer Society ( 2019 ) Signs and symptoms of lung cancer. https://www.cancer.org/cancer/lung-cancer/detection-diagnosis-staging/signs-symptoms.html (last accessed 7 June 2020).
Bell N. R. , Grad R. , Dickinson J. A. , Singh H. , Moore A. E. , Kasperavicius D. et al. ( 2017 ) Better decision making in preventive health screening: balancing benefits and harms . Canadian Family Physician Medecin de Famille Canadien , 63 , 521 – 524 .
Bray F. , Ferlay J. , Soerjomataram I. , Siegel R. L. , Torre L. A. , Jemal A. ( 2018 ) Cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries . CA: A Cancer Journal for Clinicians , 68 , 394 – 424 .
Cardarelli R. , Roper K. L. , Cardarelli K. , Feltner F. J. , Prater S. , Ledford K. M. et al. ( 2017 ) Identifying community perspectives for a lung cancer screening awareness campaign in Appalachia Kentucky: the Terminate Lung Cancer (TLC) study . Journal of Cancer Education , 32 , 125 – 134 .
Carter‐Harris L. ( 2015 ) Lung cancer stigma as a barrier to medical help‐seeking behavior: practice implications . Journal of the American Association of Nurse Practitioners , 27 , 240 – 245 .
Cassim S. , Chepulis L. , Keenan R. , Kidd J. , Firth M. , Lawrenson R. ( 2019 ) Patient and carer perceived barriers to early presentation and diagnosis of lung cancer: a systematic review . BMC Cancer , 19 , 25 .
Chelf J. H. , Deshler A. , Thiemann K. , Dose A. M. , Quella S. K. , Hillman S. ( 2002 , June) Learning and support preferences of adult patients with cancer at a comprehensive cancer center . Oncology Nursing Forum , 29 , 863 – 867 .
Chowienczyk S. , Price S. , Hamilton W. ( 2020 ) Changes in the presenting symptoms of lung cancer from 2000–2017: a serial cross-sectional study of observational records in UK primary care . British Journal of General Practice , 70 , e193 – e199 .
Christoph S. , Cazzaniga S. , Hunger R. E. , Naldi L. , Borradori L. , Oberholzer P. A. ( 2016 ) Ultraviolet radiation protection and skin cancer awareness in recreational athletes: a survey among participants in a running event . Swiss Medical Weekly , 146, w14297 .
Clarke N. , Gallagher P. , Kearney P. M. , McNamara D. , Sharp L. ( 2016 ) Impact of gender on decisions to participate in faecal immunochemical test‐based colorectal cancer screening: a qualitative study . Psycho-oncology , 25 , 1456 – 1462 .
Cunningham Y. , Wyke S. , Blyth K. G. , Rigg D. , Macdonald S. , Macleod U. et al. ( 2019 ). Lung cancer symptom appraisal among people with chronic obstructive pulmonary disease: A qualitative interview study . Psycho‐oncology , 28 , 718 – 725 .
Dlamini S. B. , Sartorius B. , Ginindza T. ( 2019 ) Mapping the evidence on interventions to raise awareness on lung cancer in resource poor settings: a scoping review protocol . Systematic Reviews , 8 , 1 – 5 .
Ellis P. M. and , Vandermeer R. ( 2011 ) Delays in the diagnosis of lung cancer . Journal of Thoracic Disease , 3 , 183 .
Emery J. D. , Murray S. R. , Walter F. M. , Martin A. , Goodall S. , Mazza D. et al. ( 2019 ) The Chest Australia Trial: a randomised controlled trial of an intervention to increase consultation rates in smokers at risk of lung cancer . Thorax , 74 , 362 – 370 .
Freeman B. , Potente S. , Rock V. , McIver J. ( 2015 ) Social media campaigns that make a difference: what can public health learn from the corporate sector and other social change marketers . Public Health Research & Practice , 25 , e2521517 .
Fung L. C. , Nguyen K. H. , Stewart S. L. , Chen , Jr M. S. , Tong E. K. ( 2018 ) Impact of a cancer education seminar on knowledge and screening intent among Chinese Americans: results from a randomized, controlled, community‐based trial . Cancer , 124 , 1622 – 1630 .
Higgins J. P. , Thomas J. , Chandler J. , Cumpston M. , Li T. , Page M. J. , Welch V. A. (eds) ( 2019 ). Cochrane Handbook for Systematic Reviews of Interventions . John Wiley & Sons, Chichester UK .
Google Preview
Holmberg L. , Sandin F. , Bray F. , Richards M. , Spicer J. , Lambe M. et al. ( 2010 ) National comparisons of lung cancer survival in England, Norway and Sweden 2001–2004: differences occur early in follow-up . Thorax , 65 , 436 – 441 .
Hong Q. N. , Fàbregues S. , Bartlett G. , Boardman F. , Cargo M. , Dagenais P. et al. ( 2018 ) The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers . Education for Information , 34 , 285 – 291 .
Housten A. J. , Lowenstein L. M. , Leal V. B. , Volk R. J. ( 2018 ) Responsiveness of a brief measure of lung cancer screening knowledge . Journal of Cancer Education , 33 , 842 – 846 .
Hovanec J. , Siemiatycki J. , Conway D. I. , Olsson A. , Stücker I. , Guida F. et al. ( 2018 ) Lung cancer and socioeconomic status in a pooled analysis of case–control studies . PLoS One , 13 , e0192999 .
Ironmonger L. , Ohuma E. , Ormiston-Smith N. , Gildea C. , Thomson C. S. , Peake M. D. ( 2015 ) An evaluation of the impact of large-scale interventions to raise public awareness of a lung cancer symptom . British Journal of Cancer , 112 , 207 – 216 .
Jemal A. , Fedewa S. A. ( 2017 ) Lung cancer screening with low-dose computed tomography in the United States—2010 to 2015 . JAMA Oncology , 3 , 1278 – 1281 .
Jessup D. L. , Glover , IV M. , Daye D. , Banzi L. , Jones P. , Choy G. et al. ( 2018 ) Implementation of digital awareness strategies to engage patients and providers in a lung cancer screening program: retrospective study . Journal of Medical Internet Research , 20 , e52 .
Kennedy M. P. , Cheyne L. , Darby M. , Plant P. , Milton R. , Robson J. M. et al. ( 2018 ) Lung cancer stage-shift following a symptom awareness campaign . Thorax , 73 , 1128 – 1136 .
Koo M. M. , Hamilton W. , Walter F. M. , Rubin G. P. , Lyratzopoulos G. ( 2018 ) Symptom signatures and diagnostic timeliness in cancer patients: a review of current evidence . Neoplasia , 20 , 165 – 174 .
Lau Y. K. , Caverly T. J. , Cao P. , Cherng S. T. , West M. , Gaber C. et al. ( 2015 ) Evaluation of a personalized, web-based decision aid for lung cancer screening . American Journal of Preventive Medicine , 49 , e125 – e129 .
Marcus P. M. , Doria-Rose V. P. , Gareen I. F. , Brewer B. , Clingan K. , Keating K. et al. ( 2016 ) Did death certificates and a death review process agree on lung cancer cause of death in the National Lung Screening Trial? Clinical Trials: Journal of the Society for Clinical Trials , 13 , 434 – 438 .
Mazzone P. J. , Tenenbaum A. , Seeley M. , Petersen H. , Lyon C. , Han X. et al. ( 2017 ) Impact of a lung cancer screening counseling and shared decision-making visit . Chest , 151 , 572 – 578 .
McCutchan G. , Hiscock J. , Hood K. , Murchie P. , Neal R. D. , Newton G. et al. ( 2019 ) Engaging high-risk groups in early lung cancer diagnosis: a qualitative study of symptom presentation and intervention preferences among the UK’s most deprived communities . BMJ Open , 9 , e025902 .
Meneses-Echávez J. F. , Alba-Ramírez P. A. , Correa-Bautista J. E. ( 2018 ) Raising awareness for lung cancer prevention and healthy lifestyles in female scholars from a low-income area in Bogota, Colombia: evaluation of a national framework . Journal of Cancer Education , 33 , 1294 – 1300 .
Metcalfe K. A. , Dennis C. L. , Poll A. , Armel S. , Demsky R. , Carlsson L. et al. ( 2017 ) Effect of decision aid for breast cancer prevention on decisional conflict in women with a BRCA1 or BRCA2 mutation: a multisite, randomized, controlled trial . Genetics in Medicine , 19 , 330 – 336 .
Moffat J. , Bentley A. , Ironmonger L. , Boughey A. , Radford G. , Duffy S. ( 2015 ) The impact of national cancer awareness campaigns for bowel and lung cancer symptoms on sociodemographic inequalities in immediate key symptom awareness and GP attendances . British Journal of Cancer , 112 , S14 – S21 .
Moher D. , Liberati A. , Tetzlaff J. , Altman D. G. , Grp P. ( 2009 ) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement (Reprinted from Annals of Internal Medicine) . Physical Therapy , 89 , 873 – 880 .
Mueller J. , Davies A. , Jay C. , Harper S. , Blackhall F. , Summers Y. et al. ( 2019 ) Developing and testing a web‐based intervention to encourage early help‐seeking in people with symptoms associated with lung cancer . British Journal of Health Psychology , 24 , 31 – 65 .
National Cancer Institute ( 2020 ) Cancer stat facts: lung and bronchus cancer. https://seer.cancer.gov/statfacts/html/lungb.html (last accessed 5 June 2020).
National Lung Screening Trial Research Team ( 2011 ) Reduced lung-cancer mortality with low-dose computed tomographic screening . New England Journal of Medicine , 365 , 395 – 409 .
Nimmons K. , , Beaudoin C. E. and , St. John J. A. ( 2017 ) The outcome evaluation of a CHW cancer prevention intervention: testing individual and multilevel predictors among hispanics living along the Texas-Mexico Border . Journal of Cancer Education , 32 , 183 – 189 .
O'Mahony M. , McCarthy G. , Corcoran P. , Hegarty J. ( 2013 ) Shedding light on women's help seeking behaviour for self discovered breast symptoms . European Journal of Oncology Nursing , 17 , 632 – 639 .
Oudkerk M. , Devaraj A. , Vliegenthart R. , Henzler T. , Prosch H. , Heussel C. P. et al. ( 2017 ) European position statement on lung cancer screening . The Lancet Oncology , 18 , e754 – e766 .
Perestelo-Perez L. , Rivero-Santana A. , Torres-Castaño A. , Ramos-Garcia V. , Alvarez-Perez Y. , Gonzalez-Hernandez N. et al. ( 2019 ) Effectiveness of a decision aid for promoting colorectal cancer screening in Spain: a randomized trial . BMC Medical Informatics and Decision Making , 19 , 8 .
Power E. , Wardle J. ( 2015 ) Change in public awareness of symptoms and perceived barriers to seeing a doctor following Be Clear on Cancer campaigns in England . British Journal of Cancer , 112 , S22 – S26 .
Reidy M. , Saab M. M. , Hegarty J. , Von Wagner C. , O’Mahony M. , Murphy M. et al. ( 2018 ) Promoting men’s knowledge of cancer risk reduction: a systematic review of interventions . Patient Education and Counseling , 101 , 1322 – 1336 .
Reuland D. S. , Cubillos L. , Brenner A. T. , Harris R. P. , Minish B. , Pignone M. P. ( 2018 ) A pre-post study testing a lung cancer screening decision aid in primary care . BMC Medical Informatics and Decision Making , 18 , 5 .
Ruparel M. , Quaife S. L. , Ghimire B. , Dickson J. L. , Bhowmik A. , Navani N. et al. ( 2019 ) Impact of a lung cancer screening information film on informed decision-making: a randomized trial . Annals of the American Thoracic Society , 16 , 744 – 751 .
Ryan A. M. , Cushen S. , Schellekens H. , Bhuachalla E. N. , Burns L. , Kenny U. et al. ( 2015 ) Poor awareness of risk factors for cancer in Irish adults: results of a large survey and review of the literature . The Oncologist , 20 , 372 – 378 .
Saab M. M. , , Landers M. , , Cooke E. , , Murphy D. , , Davoren M. and , Hegarty J. ( 2018 ) Enhancing men’s awareness of testicular disorders using a virtual reality intervention . Nursing Research , 67 , 349 – 358 .
Saab M. M. , Landers M. , Hegarty J. ( 2017a ) Exploring awareness and help-seeking intentions for testicular symptoms among heterosexual, gay, and bisexual men in Ireland: a qualitative descriptive study . International Journal of Nursing Studies , 67 , 41 – 50 .
Saab M. M. , Landers M. , Hegarty J. ( 2017b ) Exploring men's preferred strategies for learning about testicular disorders inclusive of testicular cancer: a qualitative descriptive study . European Journal of Oncology Nursing , 26 , 27 – 35 .
Sakoda L. C. , Meyer M. A. , Chawla N. , Sanchez M. A. , Blatchins M. A. , Nayak S. et al. ( 2020 ) Effectiveness of a patient education class to enhance knowledge about lung cancer screening: a quality improvement evaluation . Journal of Cancer Education , 35 , 897 – 890 .
Scottish Intercollegiate Guidelines Network ( 2019 ) SIGN 100: a handbook for patients and carer representatives. https://www.sign.ac.uk/assets/sign100.pdf (last accessed 7 June 2020).
Siegel R. L. , Miller K. D. , Jemal A. ( 2018 ) Cancer statistics, 2018 . CA: A Cancer Journal for Clinicians , 68 , 7 – 30 .
Smith C. F. , Whitaker K. L. , Winstanley K. , Wardle J. ( 2016 ) Smokers are less likely than non-smokers to seek help for a lung cancer ‘alarm’ symptom . Thorax , 71 , 659 – 661 .
The Cochrane Collaboration ( 2020 ) About Covidence. https://community.cochrane.org/help/tools-and-software/covidence/about-covidence (last accessed 6 June 2020).
Torre L. A. , Siegel R. L. , Jemal A. ( 2016 ) Lung cancer statistics . Advances in Experimental Medicine and Biology , 893 , 1 – 19 .
Walter F. M. , Rubin G. , Bankhead C. , Morris H. C. , Hall N. , Mills K. et al. ( 2015 ) Symptoms and other factors associated with time to diagnosis and stage of lung cancer: a prospective cohort study . British Journal of Cancer , 112 , S6 – S13 .
Wilhelm W. J. , Kaunelis D. ( 2005 ) Literature reviews: analysis, planning, and query techniques . Delta Pi Epsilon Journal , 47- , 91 – 106 .
Williams L. B. , Looney S. W. , Joshua T. , McCall A. , Tingen M. S. ( 2021 ) Promoting community awareness of lung cancer screening among disparate populations: results of the cancer-community awareness access research and education project . Cancer Nursing, , 44, 89–97.
World Health Organisation ( 2020 ) WHO report on cancer: setting priorities, investing wisely and providing care for all. https://www.who.int/publications-detail/who-report-on-cancer-setting-priorities-investing-wisely-and-providing-care-for-all (last accessed 20 October 2020).
Supplementary data
Email alerts, citing articles via.
- Recommend to Your Librarian
- Journals Career Network
Affiliations
- Online ISSN 1460-2245
- Print ISSN 0957-4824
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Lung Cancer Prevention (PDQ®)–Patient Version
What is prevention.
Cancer prevention is action taken to lower the chance of getting cancer. By preventing cancer, the number of new cases of cancer in a group or population is lowered. Hopefully, this will lower the number of deaths caused by cancer.
To prevent new cancers from starting, scientists look at risk factors and protective factors . Anything that increases your chance of developing cancer is called a cancer risk factor; anything that decreases your chance of developing cancer is called a cancer protective factor.
Some risk factors for cancer can be avoided, but many cannot. For example, both smoking and inheriting certain genes are risk factors for some types of cancer, but only smoking can be avoided. Regular exercise and a healthy diet may be protective factors for some types of cancer. Avoiding risk factors and increasing protective factors may lower your risk but it does not mean that you will not get cancer.
Different ways to prevent cancer are being studied, including:
- Changing lifestyle or eating habits.
- Avoiding things known to cause cancer.
- Taking medicines to treat a precancerous condition or to keep cancer from starting.
General Information About Lung Cancer
Lung cancer is a disease in which malignant (cancer) cells form in the tissues of the lung., lung cancer is the leading cause of cancer death in both men and women..

There are two types of lung cancer: small cell lung cancer and non-small cell lung cancer .
For more information about lung cancer, see the following:
- Lung Cancer Screening
- Non-Small Cell Lung Cancer Treatment
- Small Cell Lung Cancer Treatment
- Cigarette Smoking: Health Risks and How to Quit
Lung cancer causes more deaths per year in the United States than do colon cancer , breast cancer , and prostate cancer combined.
Lung cancer rates are highest in Black men, while lung cancer deaths are highest among Black, American Indian, and Alaska Native men, compared with other racial and ethnic groups in the United States.
Lung Cancer Prevention
Avoiding risk factors and increasing protective factors may help prevent lung cancer., cigarette, cigar, and pipe smoking, secondhand smoke, family history, hiv infection, environmental risk factors, beta carotene supplements in heavy smokers, not smoking, quitting smoking, lower exposure to workplace risk factors, lower exposure to radon, physical activity, beta carotene supplements in nonsmokers, vitamin e supplements, cancer prevention clinical trials are used to study ways to prevent cancer., new ways to prevent lung cancer are being studied in clinical trials..
Avoiding cancer risk factors may help prevent certain cancers. Risk factors include smoking, having overweight , and not getting enough exercise. Increasing protective factors such as quitting smoking and exercising may also help prevent some cancers. Talk to your doctor or other health care professional about how you might lower your risk of cancer.
The following are risk factors for lung cancer:
Tobacco smoking is the most important risk factor for lung cancer . Cigarette , cigar , and pipe smoking all increase the risk of lung cancer. Tobacco smoking causes about 9 out of 10 cases of lung cancer in men and about 8 out of 10 cases of lung cancer in women.
Studies have shown that smoking low tar or low nicotine cigarettes does not lower the risk of lung cancer.
Studies also show that the risk of lung cancer from smoking cigarettes increases with the number of cigarettes smoked per day and the number of years smoked. People who smoke have about 20 times the risk of lung cancer compared to those who do not smoke.
Being exposed to secondhand tobacco smoke is also a risk factor for lung cancer. Secondhand smoke is the smoke that comes from a burning cigarette or other tobacco product, or that is exhaled by smokers. People who inhale secondhand smoke are exposed to the same cancer -causing agents as smokers, although in smaller amounts. Inhaling secondhand smoke is called involuntary or passive smoking.
Having a family history of lung cancer is a risk factor for lung cancer. People with a relative who has had lung cancer may be twice as likely to have lung cancer as people who do not have a relative who has had lung cancer. Because cigarette smoking tends to run in families and family members are exposed to secondhand smoke, it is hard to know whether the increased risk of lung cancer is from the family history of lung cancer or from being exposed to cigarette smoke.
Being infected with the human immunodeficiency virus (HIV), the cause of acquired immunodeficiency syndrome (AIDS), is linked with a higher risk of lung cancer. People infected with HIV may have more than twice the risk of lung cancer than those who are not infected. Since smoking rates are higher in those infected with HIV than in those not infected, it is not clear whether the increased risk of lung cancer is from HIV infection or from being exposed to cigarette smoke.
- Atomic bomb radiation: Being exposed to radiation after an atomic bomb explosion increases the risk of lung cancer.
- Radiation therapy: Radiation therapy to the chest may be used to treat certain cancers, including breast cancer and Hodgkin lymphoma . Radiation therapy uses x-rays , gamma rays , or other types of radiation that may increase the risk of lung cancer. The higher the dose of radiation received, the higher the risk. The risk of lung cancer following radiation therapy is higher in patients who smoke than in nonsmokers.
- Imaging tests: Imaging tests, such as CT scans , expose patients to radiation. Low-dose spiral CT scans expose patients to less radiation than higher dose CT scans. In lung cancer screening , the use of low-dose spiral CT scans can lessen the harmful effects of radiation.
- Radon: Radon is a radioactive gas that comes from the breakdown of uranium in rocks and soil. It seeps up through the ground, and leaks into the air or water supply. Radon can enter homes through cracks in floors, walls, or the foundation, and levels of radon can build up over time.
Studies show that high levels of radon gas inside the home or workplace increase the number of new cases of lung cancer and the number of deaths caused by lung cancer. The risk of lung cancer is higher in smokers exposed to radon than in nonsmokers who are exposed to it. In people who have never smoked, about 26% of deaths caused by lung cancer have been linked to being exposed to radon.
- Tar and soot.
These substances can cause lung cancer in people who are exposed to them in the workplace and have never smoked. As the level of exposure to these substances increases, the risk of lung cancer also increases. The risk of lung cancer is even higher in people who are exposed and also smoke.
- Air pollution: Studies show that living in areas with higher levels of air pollution increases the risk of lung cancer.
Taking beta carotene supplements (pills) increases the risk of lung cancer, especially in smokers who smoke one or more packs a day. The risk is higher in smokers who have at least one alcoholic drink every day.
The following are protective factors for lung cancer:
The best way to prevent lung cancer is to not smoke.
Smokers can decrease their risk of lung cancer by quitting. In smokers who have been treated for lung cancer, quitting smoking lowers the risk of new lung cancers. Counseling , the use of nicotine replacement products, and antidepressant therapy have helped smokers quit for good.
In a person who has quit smoking, the chance of preventing lung cancer depends on how many years and how much the person smoked and the length of time since quitting. After a person has quit smoking for 10 years, the risk of lung cancer decreases 30% to 60%.
Although the risk of dying from lung cancer can be greatly decreased by quitting smoking for a long period of time, the risk will never be as low as the risk in nonsmokers. This is why it is important for young people not to start smoking.
See the following for more information on quitting smoking:
- Tobacco (includes help with quitting)
Laws that protect workers from being exposed to cancer-causing substances, such as asbestos, arsenic, nickel, and chromium, may help lower their risk of developing lung cancer. Laws that prevent smoking in the workplace help lower the risk of lung cancer caused by secondhand smoke.
Lowering radon levels may lower the risk of lung cancer, especially among cigarette smokers. High levels of radon in homes may be reduced by taking steps to prevent radon leakage, such as sealing basements.
It is not clear if the following decrease the risk of lung cancer:
Some studies show that people who eat high amounts of fruits or vegetables have a lower risk of lung cancer than those who eat low amounts. However, since smokers tend to have less healthy diets than nonsmokers, it is hard to know whether the decreased risk is from having a healthy diet or from not smoking.
Some studies show that people who are physically active have a lower risk of lung cancer than people who are not. However, since smokers tend to have different levels of physical activity than nonsmokers, it is hard to know if physical activity affects the risk of lung cancer.
The following do not decrease the risk of lung cancer:
Studies of nonsmokers show that taking beta carotene supplements does not lower their risk of lung cancer.
Studies show that taking vitamin E supplements does not affect the risk of lung cancer.
Cancer prevention clinical trials are used to study ways to lower the risk of developing certain types of cancer. Some cancer prevention trials are conducted with healthy people who have not had cancer but who have an increased risk for cancer. Other prevention trials are conducted with people who have had cancer and are trying to prevent another cancer of the same type or to lower their chance of developing a new type of cancer. Other trials are done with healthy volunteers who are not known to have any risk factors for cancer.
The purpose of some cancer prevention clinical trials is to find out whether actions people take can prevent cancer. These may include eating fruits and vegetables, exercising, quitting smoking, or taking certain medicines , vitamins , minerals , or food supplements.
Information about clinical trials supported by NCI can be found on NCI’s clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
About This PDQ Summary
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish .
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government’s center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about lung cancer prevention. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Screening and Prevention Editorial Board .
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website . For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary].”
The best way to cite this PDQ summary is:
PDQ® Screening and Prevention Editorial Board. PDQ Lung Cancer Prevention. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/lung/patient/lung-prevention-pdq . Accessed <MM/DD/YYYY>. [PMID: 26389497]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online . Visuals Online is a collection of more than 3,000 scientific images.
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s E-mail Us .
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Hosted content
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 57, Issue 11
- Lung cancer • 1: Prevention of lung cancer
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- G E Goodman
- Correspondence to: G E Goodman, Fred Hutchinson Cancer Research Center, Swedish Medical Center Cancer Institute, Seattle, Washington, USA; gary.goodman{at}swedish.org
Cancer of the lung causes more deaths from cancer worldwide than at any other site. The environmental, genetic, and dietary risk factors are discussed and progress in chemoprevention is reviewed. A better understanding of the molecular events that occur during carcinogenesis has opened up new areas of research in cancer prevention and a number of biochemical markers of high risk individuals have been identified. It is predicted that greater success in chemoprevention will be achieved in the next decade than in the last.
- lung cancer
- risk factors
- biochemical markers
https://doi.org/10.1136/thorax.57.11.994
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
THE PROBLEM
In 1990 cancer caused an estimated six million deaths worldwide and, of these, lung cancer was the most frequent site with an estimated 945 000 deaths. 1 In 2002 the death rate from lung cancer in the USA in both men and women is estimated at 134 900, exceeding the combined total for breast, prostate, and colon cancer. 2 Lung cancer is also the leading cause of cancer death in all European countries and is rapidly increasing in the developing world. Of 40 countries worldwide, the countries with the highest rates are Hungary (81.6/100 000 person years), the Czech Republic, the Russian Federation, Poland, and Denmark. 3 Among women the highest rates were in the US (25.6/100 000 person years), Denmark, Canada, the UK, and New Zealand.
ENVIRONMENTAL RISK FACTORS
In addition to being the biggest cancer killer, lung cancer is one of the few cancers with a well defined aetiology—namely, the inhalation of tobacco smoke. In the USA the death rate from lung cancer parallels the 1965 peak and subsequent decline in cigarette smoking rates. The incidence of lung cancer peaked in 1990 with 41.4 deaths per 1000 person years and has since fallen, reaching a rate of 39.8 in 1995. 4 Shopland et al 5 determined the prevalence of smoking in each of the 50 states from surveys conducted in 1992 and compared these rates with 1985. Kentucky and West Virginia were the highest rates with 32.29% and 30.59% of the adult population 20 years or older being current smokers. Utah had the lowest rate at 17.1%. Forty nine of the 51 areas had a decrease in smoking between 1985 and 1992–93. Rhode Island experienced the greatest decline at –30.7%. Only Utah (+16.3%) and Wisconsin (+1.9%) showed increases. Nationally, the prevalence of smoking declined 17% overall from 1985 to 1992–93. Among subgroups, African American men experienced the highest rates (31.3%) followed by White men (26.4%) and Hispanic mens (25.0%). Among women, Whites and African Americans were similar (22.9% and 22.5%, respectively) whereas smoking among Hispanic women was significantly less (12.7%).
While there have been similar declines in the incidence of smoking in Canada and western Europe, there is concern about the rising rates of smoking in developing countries. 6– 8 China, the world’s most populous country, has tripled cigarette consumption between 1978 and 1987. 9 It is estimated that 70% of Chinese men and 2% of women smoke. 10 Given the 20–30 year lag between exposure and peak incidence of cancer, the potential coming epidemic stresses the urgent need to develop effective prevention strategies.
In addition to the hazard of first hand smoke, the 1986 US Surgeon General’s report concluded that cigarette smoke was a health risk to non-smokers. This has subsequently been supported by over 24 studies showing that exposed non-smokers have an increased relative risk of developing cancer ranging from 1.41 to 2.01. 11– 14
Clearly, cigarette smoking remains the most prevalent and uncontrolled environmental carcinogen in our society. The continued burden of current and ex-smokers in the US and western Europe (the majority of Americans developing lung cancer are ex-smokers 15– 17 ), the increasing incidence of smokers in Asia, and the recruitment of new smokers worldwide guarantee that lung cancer will remain the major cause of cancer death worldwide for the next 25–50 years.
Over the past 10 years there have been advances in our understanding of the epidemiology and genetics of nicotine addiction. 18 These findings have opened new areas of smoking prevention and cessation research using pharmacological interventions with both pharmacological agents and nicotine replacement. 19 As health professionals concerned about lung cancer, we must vigorously support smoking prevention and cessation programmes. 20 We must champion efforts to make tobacco abuse a socially and culturally unacceptable habit and support all governmental actions 21 to eliminate tobacco as an environmental carcinogen.
GENETIC RISK FACTORS
Not all cigarette smokers go on to develop lung cancer. Investigators are working to identify factors which can predict individual susceptibility. 22 One area of study is the family of enzymes responsible for carcinogen activation, degradation, and subsequent DNA repair. 23 These enzymes display gene deletions and polymorphisms which can affect enzyme activity. It has been hypothesised that an individual’s enzyme profile is associated with lung cancer risk. This profile could be used to counsel individuals and could be used to select high risk individuals for specific chemoprevention agents. These enzymes and the metabolic pathways they regulate also have the potential to become targets for preventive agents.
To illustrate this point, benzo[a]pyrene, one of the many carcinogens found in cigarette smoke, is metabolically activated by the P450 family of hepatic enzymes (mainly CYP1A1). 24– 27 The intermediate metabolites are chemically active and can bind to DNA and cause gene dysfunction. Glutathione-S-transferase (GST), epoxide hydrolase (EH) and N-acetytransferase (NAT) detoxify these products. Polymorphisms and/or gene deletions result in modified metabolic activity. 18, 28– 32 Enzymes responsible for DNA repair also display polymorphisms. 33– 35 Studies suggest that genetic alterations in each of these enzyme families can have small effects on an individual’s risk of developing lung cancer.
Gene-diet interaction will also require careful investigation. Studies suggest that low levels of vitamin E can increase the GSTM1 associated risk. 36 Interactions with dietary enzyme factors such as folate and subsequent folate metabolism have also been suggested. 37 Although it is possible that a single polymorphism or dietary interactions may significantly alter the relative risk, it is likely that many interactions, each having a subtle effect, can result in synergistic interactions that greatly affect the overall risk. Determining the risk profile of an individual based on their inherited polymorphisms and their potential dietary interaction will be a complex undertaking. Testing these hypotheses will require studies with a very large sample size to achieve the statistical power.
DIETARY RISK FACTORS
Numerous studies have shown that the incidence of cancer can be inversely related to the intake of many food groups. 38– 41 The serum concentration of many micronutrients is also inversely related to the incidence of cancer. 42– 46 Based on these epidemiological studies, it has been suggested that micronutrients and macronutrients present in our diet may act as cancer inhibiting substances.
Dietary carotenoids were one of the first micronutrients suggested as risk factors for lung cancer. 38 Epidemiological studies reported that individuals with a diet low in β-carotene-rich foods had a higher incidence of lung cancer. 39, 40, 47, 48 Retrospective case-control trials of serum obtained from individuals who later developed lung cancer confirmed that the serum concentrations of β-carotene were lower in cases than in controls. 43, 48 Those in the highest category had a relative risk of 0.5–0.7 compared with those in the highest. Another carotenoid, lycopene, a simple hydrocarbon precursor of β-carotene, has been studied. 49 Lycopene is an effective antioxidant (25% better than β-carotene) and is the second most common dietary carotenoid. The most common source of lycopene in the diet is cooked or processed tomatoes which contain about 30 mg/kg. Like β-carotene, epidemiological studies of the dietary intake or serum concentration of lycopene found an inverse relationship with cancer of the bladder, lung and prostate. 49, 50
Other dietary micronutrients may also be associated with lung cancer risk. Knekt et al reported that dietary flavonoids (found in high concentration in apples) were a strong predictor of lung cancer risk. In a population of 9959 Finnish men and women, those with the highest intake of dietary flavonoids had an incidence of lung cancer that was 59% of those in the lowest quartile. 51 Isothiocyanates, which are widely distributed in cruciferous vegetables, have also been shown to have an inverse relationship with the incidence of lung cancer. 52, 53 In vivo animal model systems have shown that isothiocyanates have activity in decreasing the incidence of cancer of the lung, oesophagus, liver, colon, and bladder.
CHEMOPREVENTION
The pragmatic acceptance that tobacco abuse cannot be easily and rapidly eliminated has given emphasis to the field of lung cancer chemoprevention. Chemoprevention is defined as the use of agents to prevent, inhibit, or reverse the process of carcinogenesis. 54 The underlying hypothesis of prevention is that carcinogenesis is the stepwise accumulation of genetic and epigenetic changes that result in a cell with a malignant phenotype. The goal of cancer prevention scientists is to develop interventions that can interrupt, arrest, or reverse this process. 55
Historically, two major categories of compounds have been investigated for cancer prevention activity. One group consists of naturally occurring dietary micronutrients and their synthetic analogues which have been discussed above. Although epidemiological associations cannot prove a cause and effect relationship, they show strong associations and suggest hypotheses to be tested. The goal is to determine which, if any, of these dietary substances (or combination of substances) are important factors in modifying the incidence of cancer, 56 and whether supplementation of the diet with these micronutrients is an effective method of cancer prevention.
The other group of compounds currently being investigated are synthetic agents. 57 These include a large number of compounds with varying mechanisms including, for example, the non-steroidal anti-inflammatory agents (NSAIDS) which are potent in vivo inhibitors of colon carcinogenesis 58– 60 and agents such as DFMO (difluoromethyl ornithine), a polyamine synthase inhibitor, which has a broad spectrum of preventive activity in vitro and in vivo. 61– 63
Vitamin A and its family of compounds (the retinoids) were the first dietary constituents to have extensive in vitro and in vivo evidence of chemopreventive activity. 64 The retinoids have been found to be active in many animal model systems using different organ sites as well as different inducing carcinogens. 65 When Sporn et al first discussed the concept of chemoprevention, his work focused on the retinoids. 54
Retinol, its palmitic acid ester, the trace retinoids all-trans-retinoic acid and 13-cis-retinoic acid, together with the synthetic retinoids etretinate and 4-hydroxy phenyl retinamide have all been studied in vitro as well as in human intervention trials. Trials with these agents were started in the early 1980s and a number of them have matured and reported results.
One of the earliest reported positive trials was that by Hong et al who studied the effects of 13-cis-retinoic acid on the incidence of recurrence and second primaries in patients with each stage primary squamous cell carcinomas of the head and neck. 66 This tobacco-associated malignancy has many analogies to lung cancer. Although there was no decrease in the incidence of recurrence, second primaries which, in general, consisted of other tobacco related cancers (head and neck, oesophageal, and lung) were significantly fewer (p<0.05). This study is now undergoing confirmation in a large intergroup trial being conducted within the USA.
The European Organization for Cancer (EORTC) studied a population of patients with resected stage I non-small cell lung cancer. Like patients with early primary cancers of the head and neck, this group has a 60–70% cure rate of their primary cancer with surgery alone. Retinyl palmitate (300 000 IU/day) plus N -acetylcysteine (600 g/day) were given for two years. Their end points were recurrence and second primaries. This trial reported some early encouraging results although a final report in 2000 reported no benefit in survival, relapse free survival, or incidence of second primaries. 67
A US intergroup trial of similar design tested 13-cis-retinoic acid (30 mg/day) for 3 years in a similar population of subjects with stage I lung cancer. This phase III trial completed accrual in 1997 and reported an increase in death rate in patients receiving 13-cis-retinoic acid. After a median follow up of 3.5 years there was no effect of the supplements on the time to second primaries, recurrence, or mortality. There was a smoking-treatment interaction, with current smokers on the active arm having increased recurrence and mortality. 68
13-cis-retinoic acid has also been tested using bronchial metaplasia as the end point. 69 This double blind, randomised trial showed no decrease in the incidence of metaplasia in the active treatment arm. The positive results of the clinical trial in head and neck cancers using cancer as an end point and these negative results help to emphasise that intermediate end points need to be clearly linked to cancer incidence before they can be acceptable as a surrogate end point.
The retinoids as a family continue to be investigated for chemoprevention. It is likely that additional synthetic retinoids which block or activate specific retinoid receptors (RXR) will be developed and tested in the clinic. 70 Lung cancer will remain a prime target for these agents.
Beta-carotene
Epidemiological trials, together with an influential science editorial in 1981, suggested that β-carotene was the most promising lung cancer prevention agent. 6 In spite of only limited in vitro and in vivo animal studies suggesting that β-carotene had preventive activity, human intervention trials were started in the early 1980s. Two of these trials focused on lung cancer—the Alpha Tocopherol Beta Carotene Trial (ATBC) in Finland 71 and the Carotene and Retinol Efficacy Trial (CARET) in the USA. 72
CARET tested the combination of 30 mg β-carotene and 25 000 IU retinyl palmitate daily in 18 314 men and women aged 50–69 years at high risk for developing lung cancer. 73 The high risk groups consisted of 14 254 cigarette smokers with a 20-pack year smoking history, either current smokers or ex-smokers who had quit within 6 years, and 4060 men with extensive occupational asbestos exposure who were current or ex-smokers (up to 15 years since quitting). The intervention was stopped 21 months early because of evidence of no benefit and possible harm (mean follow up 4 years). There were 28% more lung cancers (p=0.02) and 17% more deaths (p=0.02) in the active intervention group. Because CARET administered a combination of β-carotene and retinyl palmitate it was not possible to distinguish whether the adverse effects were due to β-carotene, retinyl palmitate, or the combination.
These results were remarkably similar to the ATBC trial which was completed in Finland in a similar high risk population and reported in 1994, before CARET. 74 This NCI sponsored 2 × 2 placebo controlled trial administered 20 mg β-carotene with or without 50 mg α-tocopherol for 5–8 years (mean 6.1 years) to 29 133 Finnish men aged 50–69 who smoked five or more cigarettes daily. There was no overall effect of α-tocopherol on the incidence of lung cancer (relative risk (RR) 0.99, 95% confidence interval (CI) 0.87 to 1.13, p=0.86). On the other hand, β-carotene supplementation was associated with an increase in lung cancer risk (RR 1.16, 95% CI 1.02 to 1.33, p=0.02). The adverse effect of β-carotene appeared to be stronger in those who were heavy smokers of at least 20 cigarettes per day (RR 1.25, 95% CI 1.07 to 1.46) than in those who smoked 19 cigarettes or less per day (RR 0.97, 95% CI 0.76 to 1.23). These two trials clearly established that β-carotene supplements are harmful to cigarette smokers causing an increase in the incidence of lung cancer and mortality.
Another smaller intervention trial has reported encouraging results in lung and other cancer. It has long been known that there is an inverse relationship between the incidence of cancer and the selenium content of the soil (and hence locally grown foods) and cancer. 75 Based on this finding, Clark et al 76 conducted a skin cancer prevention trial in individuals previously diagnosed as having skin cancer. Participants were randomised to receive 200 μg/day selenium rich brewer yeast or placebo. An analysis in 1997 reported that selenium supplementation did not change the primary end point of new skin cancers but did reduce the incidence of other primaries (lung, p=0.05; prostate, p=0.001; colorectal, p=0.03). This study will require confirmation since the population consisted of patients with previous skin cancer and the encouraging results were seen only in the secondary analysis. A primary intervention trial of selenium and α-tocopherol with a sample size of 32 000 with the primary end point of prostate cancer and secondary end points of lung cancer and colon cancer (SELECT) began recruitment in 2001.
The findings of CARET and ATBC were a surprise since they conflicted with the epidemiological data. However, both CARET and ATBC administered high doses of β-carotene (20–30 times the average daily intake). These results emphasise the importance of carefully controlled intervention trials in determining the role of dietary supplements or any intervention agent. Because of the discouraging results of the large intervention trials as well as a rapidly expanding understanding of lung cancer, there has been a shift in focus to small clinical trials evaluating the effect of potential intervention agents on biomarkers of carcinogenesis.
BIOMARKERS OF CARCINOGENESIS
A better understanding of the molecular events that occur during carcinogenesis has opened new areas of research in cancer prevention. Currently, pre-neoplasia is diagnosed based on histological examinations. However, for lung cancer, bronchial metaplasia or dysplasia is not always a good predictor of future cancer risk. Ex-smokers can have improvement in metaplasia/dysplasia but their cancer risk remains increased. 77– 79 It is hoped that testing bronchial mucosa or bronchial epithelial cells for the presence of genetic or epigenetic changes will better predict the risk of cancer. Patients with documented changes may be more appropriate for treatment with chemoprevention agents. In addition, chemoprevention trials can be based on these molecular markers. Patients can be recruited to a trial by the presence of one or more of these markers. Those agents which cause an improvement in marker profile can then be further investigated for cancer prevention activity. These scenarios remain hypotheses to be tested since none of the molecular markers described has been shown to be a reliable predictor of cancer incidence. Their natural history in high risk populations is unknown, and it is also unknown if an agent which causes an improvement in marker status will ultimately decrease the incidence of cancer.
Numerous candidate markers are being investigated. Alterations in the p53 tumour suppressor gene are commonly acquired genetic lesions observed in lung cancer. 80– 82 Mutations affect approximately 90% of small cell lung cancers and 50–60% of non-small cell lung cancers. 83– 91 Lonardo et al 92 studied the expression of p53 in bronchial epithelium and squamous cell carcinomas and found that 61% of the squamous cell carcinomas, 54% of high grade dysplasias, and only 6% with atypia overexpressed p53. p53 expression was not seen in squamous metaplasia or low grade dysplasia. Rusch et al 93 had similar findings with 56% of non-small cell and 16% of bronchial lesions exhibiting aberrant p53 immunohistochemical staining.
Mao et al 94 studied the sputum of high risk individuals and followed them for cancer incidence. They found that 10 of 15 patients who developed adenocarcinoma had mutations in the ras or p53 gene. They then examined sputum collected prior to diagnosis and found that eight of the 10 patients had the identical mutation detected in at least one sputum sample. Mao et al 95 later reported the detection of abnormalities in bronchoscopic epithelial biopsy specimens in 40 current smokers and 14 former smokers. They determined DNA sequence losses involving microsatellite DNA at three loci (3p14, 9p21, and 17p13). DNA losses at 3p14, 9p21, and 17p13 were detected in 27 (75%), 21 (57%), and six (18%), respectively, of the informative subjects (those who could be evaluated at that specific loci). Only one abnormality, loss of 3p14, was seen in five of nine of the informative non-smokers. These sites of DNA loss are known to be localised to chromosomal sites important in cancer. The tumour suppressor gene p53 is located at 17p13. 96 The other two loci contain the tumour suppressor genes FHIT (3p14) and p16 (9p21). 97– 99 This study showed that relevant genetic abnormalities can be seen in histologically normal bronchial epithelial cells of smokers and are compatible with the hypothesis of a stepwise accumulation of genetic abnormalities leading to cancer.
Inactivation of the p16 tumour suppressor gene resulting from either allelic loss or mutation of p16 or hypermethylation of CpG islands in its promoter region 100 is also a promising marker in lung cancer. 101– 103 Belinsky’s group used methylation-specific polymerase chain reaction (MSP) 104, 105 to determine the frequency of p16 methylation in premalignant lesions, carcinoma in situ lesions, squamous cell carcinomas, and sputum samples. The frequency increased during disease progression from basal cell hyperplasia (17%) to squamous metaplasia (24%) to carcinoma in situ (50%) lesions. He further showed that aberrant p16 methylation could be detected in sputum samples from three of seven patients with lung cancer and five of 26 cancer-free individuals at high risk (smokers). Ahrendt 101 found methylated p16 alleles in prospectively collected bronchoalveolar lavage (BAL) fluid from 63% of patients (12/19) with a primary resectable non-small cell lung cancer that had p16 methylation in the cancer. Palmisano et al 106 found that aberrant methylation of the p16 and/or O6-methyl-guanine-DNA methyltransferase (MGMT) promoter regions can be detected in DNA from sputum in all 10 patients with squamous cell lung carcinoma at the time of diagnosis and also in sputum samples of all 11 patients up to 3 years before clinical diagnosis. Only five of these 21 patients had sputum cytologies positive for cancer. Furthermore, methylated p16 and MGMT sputum markers were detected in 12–19% and 16–36%, respectively, of cancer-free individuals at high risk (exposure to tobacco and/or radon) for developing lung tumours.
The cyclins are a family of nuclear factors that are expressed and control the progression of the cell through the cell cycle. Inappropriate expression or activity has been found in cancer and it has been suggested that the expression of these proteins may be a marker of early carcinogenesis. Lonardo et al 92 studied cyclin D1 and E in a series of bronchial biopsies ranging from metaplasia to low grade dysplasia, high grade dysplasia, and squamous cell carcinoma. They found that cyclin D1 was detected in 7% with squamous metaplasia, 15% with atypia, 18% with low grade dysplasia, 47% with high grade dysplasia, and 42% with squamous cell carcinoma. Findings were similar with cyclin E which was not detected in normal epithelium, squamous metaplasia, or low grade dysplasia but occurred in 9% with atypia, 33% with high grade dysplasia, and 54% with squamous cell carcinomas. Papadimitrakopoulou et al 107 studied 27 patients with biopsy specimens of the upper aerodigestive tract and found 50% expression of cyclin D.
Cyclo-oxygenase (COX) is a constitutively expressed enzyme which is one of the rate limited steps in the conversion of arachadonic acid to prostaglandins. An alternative form of COX, COX-2, is inducible and is expressed in response to growth factors and to other stimuli. It appears that COX-2 is expressed in many lung cancer cell line model systems and tumours obtained from patients. Overexpression of COX-2 occurs in all cell types but appears more prominent in well differentiated cancers. It is also found in premalignant stages and invasive cancers. 108– 112 Many COX-2 inhibitors have inhibitory effects on cell lines. 113, 114 It has been proposed that the expression of COX-2 may be an early marker of a genetically altered epithelial cell destined to become cancer. Wolff et al 111 found expression of COX-2 in 19 of 21 adenocarcinomas. Well differentiated adenocarcinomas appeared to have more COX-2 staining than poorly differentiated tumours. Expression of COX-2 was also seen in 11 squamous cell carcinomas.
Epidermal growth factor receptor (EGFR) is a member of the erbB gene family of transmembrane tyrosine kinase. Activation plays an important role in cell division and differentiation. Abnormalities of EGFR have been found in patients with lung cancer and those at high risk. 115– 118 While EGFR is expressed in normal epithelium, increased expression has been in found metaplastic lesions 119, 120 and in 70% of squamous cell carcinomas and around 50% of adenocarcinomas.
These markers are just a few of the many which have been described that may serve as intermediate end points in identifying high risk individuals. Currently, many are acting as end points for an intervention trial. Although each marker is firmly established as important in the carcinogenesis of lung cancer, modulation of these markers by preventive agents does not guarantee that the agent will have activity in reducing the incidence of lung cancer. Trials are currently being conducted to evaluate multiple markers.
A better understanding of carcinogenesis has also fostered the development of agents specifically targeting the epigenetic and genetic changes which develop in neoplastic cancer cells. Specific agents are now available that block the COX-2 enzyme (Celecoxib). EGFR is activated in lung cancer and is expressed in pre-neoplasia. ZD1839 is a specific inhibitor of the EGF activated tyrosine kinase. These compounds are examples of agents currently being tested in the treatment of patients with established lung cancer and have good potential as preventive agents.
Chemoprevention is a new field. Analogous to the development of cancer chemotherapy in the 1940s and 1950s, this field is in its infancy. As we gain a better understanding of carcinogenesis our development and use of agents will become based in modifying underlying mechanisms. Although the past 10–15 years have been disappointing, we have established a strong foundation for future clinical trials. There is every reason to believe that greater success will be achieved in the next 10–15 years.
- ↵ Murray C , Lopez A. Mortality by cause for eight regions of the world. Lancet 1997 ; 349 : 1269 –76. OpenUrl CrossRef PubMed Web of Science
- ↵ Jemal A , Thomas A, Murray T, et al . Cancer statistics. CA Cancer J Clin 2002 ; 52 : 23 –47. OpenUrl CrossRef PubMed Web of Science
- ↵ Levi F , LaVecchia, Lucchini F. Cancer mortality in Europe 1990–1992. Eur J Cancer Prev 1995 ; 4 : 389 –417. OpenUrl CrossRef PubMed
- ↵ Cole P , Rodu B. Declining cancer mortality in the United States. Cancer 1996 ; 78 : 2045 –8. OpenUrl CrossRef PubMed Web of Science
- ↵ Shopland DR , Hartman AM, Gibson J, et al . Cigarette smoking among U.S. adults by state and region: estimates from the current population survey. J Natl Cancer Inst 1996 ; 88 : 1748 –58. OpenUrl Abstract / FREE Full Text
- ↵ Peto R , Lopez A, Boreman J. Mortality from smoking worldwide. Br Med Bull 1996 ; 52 : 12 –21. OpenUrl Abstract / FREE Full Text
- Parkin D , Whelan S, Ferlay J, et al . Cancer incidents in five continents . Lyon, France: IARC Scientific Publication, No 143, Vol 7, 1997.
- ↵ Stellman SD , Takezaki T, Wang L-E, et al . Smoking and lung cancer risk in American and Japanese men: an international case-control study. Cancer Epidemiol Biomarkers Prevent 2001 ; 10 : 1193 –9. OpenUrl Abstract / FREE Full Text
- ↵ Chollat-Traquet C . Tobacco or health: a WHO programme. Eur J Cancer 1992 ; 28 : 311 –5. OpenUrl PubMed
- ↵ Gong YL , Koplan J, Feng W. Cigarette smoking in China. Prevalence, characteristics, and attitudes in Minhang District. JAMA 1995 ; 274 : 1232 –4. OpenUrl CrossRef PubMed Web of Science
- ↵ National Research Council . Environmental tobacco smoke: Measuring exposures and assessing health effects . Washington DC: National Academy, 1986.
- Wald NJ , Nanchahal K, Thompson S. Does breathing other people’s tobacco smoke cause lung cancer? BMJ Clin Res Ed 1986 ; 293 : 1217 –22. OpenUrl Abstract / FREE Full Text
- Spitzer WO , Lawrence V, Dales R. Links between passive smoking and disease: a best-evidence synthesis. A report of the Working Group on Passive Smoking. Clin Invest Med 1990 ; 13 : 17 –42; discussion 43–6. OpenUrl PubMed Web of Science
- ↵ Cardenas VM , Thun M, Austin H. Environmental tobacco smoke and lung cancer mortality in the American Cancer Society’s Cancer Prevention Study. II. Cancer Causes Control , 1997 ; 8 : 57 –64; erratum Cancer Causes Control 1997; 8 :675. OpenUrl CrossRef PubMed Web of Science
- ↵ Halpern MT , Gillespie B, Warner K. Patterns of absolute risk of lung cancer mortality in former smokers. J Natl Cancer Inst 1993 ; 85 : 457 –64. OpenUrl Abstract / FREE Full Text
- Lubin JH , Blot W. Lung cancer and smoking cessation: patterns of risk. J Natl Cancer Inst 1993 ; 85 : 422 –3. OpenUrl FREE Full Text
- ↵ Strauss G , DeCamp M, Dibiccaro E. Lung cancer diagnosis is being made with increasing frequency in former cigarette smokers! Clin Oncol 1995 ; 14 : 362 . OpenUrl
- ↵ Nazar-Stewart V , Motulsky AG, Eaton DL, et al . The glutathione S-transferase u polymorphism as a marker for susceptibility to lung carcinoma. Cancer Res 1993 ; 53 : 2313 –8. OpenUrl Abstract / FREE Full Text
- ↵ Yoshida K , Hamajima N, Kozaki K, et al . Association between the dopamine de receptor A2/A2 genotype and smoking behaviour in the Japanese. Cancer Epidemiol Biomarkers Prevent 2001 ; 10 : 403 –5. OpenUrl Abstract / FREE Full Text
- ↵ Risser NL . Prevention of lung cancer: the key is to stop smoking. Semin Oncol Nursing 1996 ; 12 : 260 –9. OpenUrl CrossRef PubMed
- ↵ Koh HK . An analysis of the successful 1992 Massachusetts tobacco tax initiative. Tobacco Control 1996 ; 5 : 220 –5. OpenUrl Abstract
- ↵ Spitz MR , Bondy M. Genetic susceptibility to cancer. Cancer 1993 ; 72 (3 Suppl): 991 –5. OpenUrl CrossRef PubMed Web of Science
- ↵ Perera F . Molecular epidemiology: insights into cancer susceptibility, risk assessment, and prevention. J Natl Cancer Inst 1996 ; 88 : 496 –509. OpenUrl Abstract / FREE Full Text
- ↵ Li D , Firozi P, Wang L-E, et al . Sensitivity to DNA damage induced by benzo(a)pyrene diol epoxide and risk of lung cancer: A case-control analysis. Cancer Res 2001 ; 61 : 1445 –50. OpenUrl Abstract / FREE Full Text
- Wu X , Shi H, Jiang H, et al . Associations between cytochrome P4502E1 genotype, mutagen sensitivity, cigarette smoking and susceptibility to lung cancer. Carcinogenesis 1997 ; 18 : 967 –73. OpenUrl Abstract / FREE Full Text
- Kato S , Shields P, Caporaso N, et al . Analysis of cytochrome P450 2E1 genetic polymorphisms in relation to human lung cancer. Cancer Epidemiol Biomarkers Prevent 1994 ; 3 : 515 –8. OpenUrl Abstract
- ↵ Nakachi K , Imai K, Hayashi S, et al . Polymorphisms of the CYP1A1 and glutathione S-transferase genes associated with susceptibility to lung cancer in relation to cigarette dose in a Japanese population. Cancer Res 1993 ; 53 : 2994 –9. OpenUrl Abstract / FREE Full Text
- ↵ Heckbert S , Weiss NS, Hornung SK, et al . Glutathione S-transferease and epoxide hydrolase activity in human leukocytes in relation to risk of lung cancer and other smoking-related cancers. J Natl Cancer Inst 1992 ; 84 : 414 –22. OpenUrl Abstract / FREE Full Text
- Zhou W , Liu G, Thurston SW, et al . Genetic polymorphisms in N-acetyltransferase-2 and microsomal epoxide hydrolase, cumulative cigarette smolking, and lung cancer. Cancer Epidemiol Biomarkers Prevent 2002 ; 11 : 15 –21. OpenUrl Abstract / FREE Full Text
- Hou S-M , Falt S, Yang K, et al . Differential interactions between GSTM1 and NAT1 genotypes on aromatic DNA adduct level and HPRT mutant frequency in lung cancer patients and population controls. Cancer Epidemiol Biomarkers Prevent 2001 ; 10 : 133 –40. OpenUrl Abstract / FREE Full Text
- Frazier ML , O’Donnell FT, Kong S, et al . Age-associated risk of cancer among individuals with N-acetyltransferase 2 (NAT2) mutations and mutations in DNA mismatch repair genes. Cancer Res 2001 ; 61 : 1269 –71. OpenUrl Abstract / FREE Full Text
- ↵ Zhou W , Thurston SW, Liu G, et al . The interaction between microsomal epoxide hydrolase polymorphisms and cumulative cigarette smoking in different histological subtypes of lung cancer. Cancer Epidemiol Biomarkers Prevent 2001 ; 10 : 461 –6. OpenUrl Abstract / FREE Full Text
- ↵ Ratnzsinghe D , Yao S-X, Tangrea JA, et al . Polymorphisms of the DNA repair gene XRCC1 and lung cancer risk. Cancer Epidemiol Biomarkers Prevent 2001 ; 10 : 119 –23. OpenUrl Abstract / FREE Full Text
- David-Beabes GL , Lunn RM, London SJ. No association between the XPD (Lys751G1n) polymorphism or the XRCC3 (Thr241Met) polymorphism and lung cancer risk. Cancer Epidemiol Biomarkers Prevent 2001 ; 10 : 911 –2. OpenUrl FREE Full Text
- ↵ Park JY , Lee SY, Jeon H-S, et al . Polymorphism of the DNA repair gene XRCC1 and risk of primary lung cancer. Cancer Epidemiol Biomarkers Prevent 2002 ; 11 : 23 –7. OpenUrl Abstract / FREE Full Text
- ↵ Woodson K , Stewart C, Barrett M, et al . Effect of vitamin intervention on the relationship between GSTM1, smoking, and lung cancer risk among male smokers. Cancer Epidemiol Biomarkers Prevent 1999 ; 8 : 965 –70. OpenUrl Abstract / FREE Full Text
- ↵ Shen H , Spitz MR, Wang L-E, et al . Polymorphisms of methylene-tetrahydrofolate reductase and risk of lung cancer: a case-control study. Cancer Epidemiol Biomarkers Prevent 2001 ; 10 : 397 –401. OpenUrl Abstract / FREE Full Text
- ↵ Ziegler R , Colavito E, Hartge P. Importance of alpha-carotene, beta-carotene, and other phytochemicals in the etiology of lung cancer. J Natl Cancer Inst 1996 ; 88 : 612 –5. OpenUrl FREE Full Text
- ↵ Colditz GA , Stampfer MJ, Willett WC. Diet and lung cancer. A review of the epidemiologic evidence in humans. Arch Intern Med 1987 ; 147 : 157 –60. OpenUrl CrossRef PubMed Web of Science
- ↵ Byers T . Diet as a factor in the etiology and prevention of lung cancer. In: Samet J, ed. Epidemiology of lung cancer . New York: Marcel Dekker, 1994: 335–52.
- ↵ Block G . Fruit, vegetables, and cancer prevention: a review of the epidemiological evidence. Nutr Cancer 1992 ; 18 : 1 –29. OpenUrl CrossRef PubMed Web of Science
- ↵ Stahelin H , Gey K, Eichholzer M. Plasma anti-oxidant vitamins and subsequent cancer mortality in the 12-year follow-up of the prospective Basel study. Am J Epidemiol 1991 ; 133 : 766 –75. OpenUrl Abstract / FREE Full Text
- ↵ Nomura AM , Stemmermann G, Heilbrun L. Serum vitamin levels and the risk of cancer of specific sites in men of Japanese ancestry in Hawaii. Cancer Res 1985 ; 45 : 2369 –72. OpenUrl Abstract / FREE Full Text
- Wald NJ , Thompson S, Densem J, et al . Serum beta-carotene and subsequent risk of cancer: results from the BUPA study. Br J Cancer 1988 ; 57 : 428 –33. OpenUrl PubMed Web of Science
- Virtamo J , Valkeila E, Alfthan G. Serum selenium and risk of cancer. A prospective follow-up of nine years. Cancer 1987 ; 60 : 145 –8. OpenUrl CrossRef PubMed Web of Science
- ↵ Connett JE , Kuller L, Kjelsberg M. Relationship between carotenoids and cancer. The Multiple Risk Factor Intervention Trial (MRFIT) study. Cancer 1989 ; 64 : 126 –34. OpenUrl CrossRef PubMed Web of Science
- ↵ Greenwald P . NCI cancer prevention and control research. Prevent Med 1993 ; 22 : 642 –60. OpenUrl CrossRef PubMed
- ↵ Willett WC , Polk B, Underwood B, et al . Relation of serum vitamins A and E and carotenoids to the risk of cancer. N Engl J Med 1984 ; 310 : 430 –4. OpenUrl PubMed Web of Science
- ↵ Stahl W , Sies H. Lycopene: a biologically important carotenoid for humans? Arch Biochem Biophys 1996 ; 336 : 1 –9. OpenUrl CrossRef PubMed Web of Science
- ↵ Clinton SK , Emenhiser C, Schwartz S. cis-trans lycopene isomers, carotenoids, and retinol in the human prostate. Cancer Epidemiol Biomarkers Prevent 1996 ; 5 : 823 –33. OpenUrl Abstract
- ↵ Knekt P , Jarvinen R, Seppanen R. Dietary flavonoids and the risk of lung cancer and other malignant neoplasms. Am J Epidemiol 1997 ; 146 : 223 –30. OpenUrl Abstract / FREE Full Text
- ↵ Hecht SS . Chemoprevention of lung cancer by isothiocyanates. Advan Exp Med Biol 1996 ; 401 : 1 –11. OpenUrl
- ↵ Stoner GD , Morse M. Isothiocyanates and plant polyphenols as inhibitors of lung and esophageal cancer. Cancer Lett 1997 ; 114 : 113 –9. OpenUrl CrossRef PubMed Web of Science
- ↵ Sporn MB , Dunlop N, Newton D. Prevention of chemical carcinogenesis by vitamin A and its synthetic analogs (retinoids). Fed Proc 1976 ; 35 : 1332 –8. OpenUrl PubMed Web of Science
- ↵ Bertram JS . Rationale and strategies for chemoprevention of cancer in humans. Cancer Res 1987 ; 47 : 3012 –31. OpenUrl Abstract / FREE Full Text
- ↵ Goodman GE . Cancer prevention: chemoprevention vs dietary modifications. Prevent Med 1993 ; 22 : 689 –92. OpenUrl CrossRef PubMed
- ↵ Kelloff GJ , Hawk E, Crowell J, et al . Strategies for identification and clinical evaluation of promising chemoprevention agents. Oncology 1996 ; 10 : 1471 –84. OpenUrl PubMed
- ↵ Giardiello FM , Hamilton S, Krush A. Treatment of colonic and rectal adenomas with sulindac in familial adenomatous polyposis. N Engl J Med 1993 ; 328 : 1313 –6. OpenUrl CrossRef PubMed Web of Science
- Kelloff GJ , Crowell J, Boone C. Clinical development plan: piroxicam. J Cell BiochemSuppl 1994 ; 20 : 219 –30. OpenUrl
- ↵ Kelloff GJ , Crowell J, Boone C. Clinical development plan: sulindac. J Cell Biochem Suppl 1994 ; 20 : 240 –51. OpenUrl PubMed
- ↵ McCann P , Pegg A, Sjoeerdsma A. Inhibition of polyamine metabolism: biological significance and basis for new therapies . New York: Academic Press, 1987.
- Meyskens FL Jr , Emerson S, Pelot D. Dose de-escalation chemoprevention trial of alpha-difluoromethylornithine in patients with colon polyps. J Natl Cancer Inst 1994 ; 86 : 1122 –30. OpenUrl Abstract / FREE Full Text
- ↵ Kelloff GJ , Crowell J, Boone C. Clinical development plan: 2-difluoromethylornithine (DFMO). J Cell Biochem Suppl 1994 ; 20 : 147 –65. OpenUrl PubMed
- ↵ Bollag W , Hartmann H. Prevention and therapy of cancer with retinoids in animals and man. Cancer Surv 1983 ; 2 : 293 –314. OpenUrl
- ↵ Lippman SM , Benner SE, Hong WK. Cancer chemoprevention. J Clin Oncol 1994 ; 12 : 851 –73. OpenUrl Abstract
- ↵ Hong WK , Lippman SM, Itri L. Prevention of second primary tumors with isotretinoin in squamous-cell carcinoma of the head and neck. N Engl J Med 1990 ; 323 : 795 –801. OpenUrl CrossRef PubMed Web of Science
- ↵ van Zandwijk N , Dalesio O, Pastorino U, et al . EUROSCAN, a randomized trial of vitamin A and N-acetylcysteine in patients with head and neck cancer or lung cancer. J Natl Cancer Inst 2000 ; 92 : 977 –86. OpenUrl Abstract / FREE Full Text
- ↵ Lippman SM , Lee JJ, Karp DD, et al . Randomized phase III intergroup trial of isotretinoin to prevent second primary tumors in stage I non-small-cell lung cancer. J Natl Cancer Inst 2001 ; 93 : 605 –18. OpenUrl Abstract / FREE Full Text
- ↵ Lee JS , Lippman SM, Benner SE. Randomized placebo-controlled trial of isotretinoin in chemoprevention of bronchial squamous metaplasia. J Clin Oncol 1994 ; 12 : 937 –45. OpenUrl Abstract / FREE Full Text
- ↵ Dragney K , Rigas J, Dmitrovsky E. The retinoids and cancer prevention mechanisms. Oncologist 2000 ; 5 : 361 –8. OpenUrl Abstract / FREE Full Text
- ↵ Alpha Tocopherol Beta Carotene Trial Group . The effect of vitamin E and beta-carotene on the incidence of lung cancer and other cancers in male smokers. N Engl J Med 1994 ; 330 : 1029 –35. OpenUrl CrossRef PubMed Web of Science
- ↵ Omenn GS , Goodman GE, Thornquist M, et al . The beta-Carotene and Retinol Efficacy Trial (CARET) for chemoprevention of lung cancer in high-risk populations: smokers and asbestos-exposed workers. Cancer Res 1994 ; 54 : 2038 –43S. OpenUrl
- ↵ Omenn GS , Goodman GE, Thornquist M, et al . Risk factors for lung cancer and for intervention effects in CARET, the beta-Carotene and Retinol Efficacy Trial. J Natl Cancer Inst 1996 ; 88 : 1550 –9. OpenUrl Abstract / FREE Full Text
- ↵ Albanes D , Heinonen OP, Taylor PR, et al . Alpha-tocopherol and beta-carotene supplements and lung cancer incidence in the alpha-tocopherol, beta-carotene cancer prevention study: effects of base-line characteristics and study compliance. J Natl Cancer Inst 1996 ; 88 : 1560 –70. OpenUrl Abstract / FREE Full Text
- ↵ van den Brandt PA , Goldbohm RA, van ‘t Veer P, et al . A prospective cohort study on selenium status and the risk of lung cancer. Cancer Res 1993 ; 53 : 4860 –5. OpenUrl Abstract / FREE Full Text
- ↵ Clark LC , Combs G, Turnbull B. Effects of selenium supplementation for cancer prevention in patients with carcinoma of the skin. A randomized controlled trial. Nutritional Prevention of Cancer Study Group. JAMA 1996 ; 276 : 1957 –63; erratum appears in JAMA 1997; 277 :1520. OpenUrl CrossRef PubMed Web of Science
- ↵ Melamed MR , Zaman M, Flehinger B. Radiologically occult in situ and incipient invasive epidermoid lung cancer: detection by sputum cytology in a survey of asymptomatic cigarette smokers. Am J Surg Pathol 1977 ; 1 : 5 –16. OpenUrl PubMed
- Topping DC , Griesemer R, Nettesheim P. Quantitative assessment of generalized epithelial changes in tracheal mucosa following exposure to 7,12-dimethylbenz(a)anthracene. Cancer Res 1979 ; 39 : 4823 –8. OpenUrl Abstract / FREE Full Text
- ↵ Ono J , Auer G, Caspersson T, et al . Reversibility of 20-methylcholanthrene-induced bronchial cell atypia in dogs. Cancer 1984 ; 54 : 1030 –7. OpenUrl CrossRef PubMed
- ↵ Greenblatt MS , Bennett WP, Hollstein M, et al . Mutations in the p53 tumor suppressor gene: clues to cancer etiology and molecular pathogenesis. Cancer Res 1994 ; 54 : 4855 –78. OpenUrl FREE Full Text
- Harris CC . p53: at the crossroads of molecular carcinogenesis and risk assessment. Science 1993 ; 262 : 1980 –1. OpenUrl FREE Full Text
- ↵ Hollstein M , Sidransky D, Vogelstein B, et al . p53 mutations in human cancers. Science 1991 ; 253 : 49 –53. OpenUrl Abstract / FREE Full Text
- ↵ Bennett WP . Molecular epidemiology of human cancer risk: gene-environment interactions and p53 mutation spectrum in human lung cancer. J Pathol 1999 ; 187 : 8 –18. OpenUrl CrossRef PubMed Web of Science
- Tammemagi MC , McLaughlin J, Bull S. Meta-analyses of p53 tumor suppressor gene alterations and clinicopathological features in resected lung cancers. Cancer Epidemiol Biomarkers Prevent 1999 ; 8 : 625 –34. OpenUrl Abstract / FREE Full Text
- Salgia R , Skarin A. Molecular abnormalities in lung cancer. J Clin Oncol 1998 ; 16 : 1207 –17. OpenUrl Abstract
- Minna JD . The molecular biology of lung cancer pathogenesis. Chest 1993 ; 103 (4 Suppl): 449 –56S. OpenUrl CrossRef PubMed
- Chiba I , Takahashi T, Nau M, et al . Mutations in the p53 gene are frequent in primary, resected non-small cell lung cancer. Lung Cancer Study Group. Oncogene 1990 ; 5 : 1603 –10. OpenUrl PubMed Web of Science
- D’Amico D , Carbone D, Mitsudomi T, et al . High frequency of somatically acquired p53 mutations in small-cell lung cancer cell lines and tumors. Oncogene 1992 ; 7 : 339 –46. OpenUrl PubMed Web of Science
- Takahashi T , Nau M, Chiba I, et al . p53: a frequent target for genetic abnormalities in lung cancer. Science 1989 ; 246 : 491 –4. OpenUrl Abstract / FREE Full Text
- Kishimoto Y , Murakami Y, Shiraishi M, et al . Aberrations of the p53 tumor suppressor gene in human non-small cell carcinomas of the lung. Cancer Res 1992 ; 52 : 4799 –804. OpenUrl Abstract / FREE Full Text
- ↵ Gazdar AF . The molecular and cellular basis of human lung cancer. Anticancer Res 1994 ; 14 (1B): 261 –7. OpenUrl PubMed Web of Science
- ↵ Lonardo F , Rusch V, Langenfield J, et al . Overexpression of cyclins D1 and E is frequent in bronchial preneoplasia and precedes squamous cell carcinoma development. Cancer Res 1999 ; 59 : 2470 –6. OpenUrl Abstract / FREE Full Text
- ↵ Rusch V , Klimstra D, Linkov I, et al . Aberrant expression of p53 or the epidermal growth factor receptor is frequent in early bronchial neoplasia and coexpression precedes squamous cell carcinoma development. Cancer Res 1995 ; 55 : 1365 –72. OpenUrl Abstract / FREE Full Text
- ↵ Mao L , Hruban R, Boyle J, et al . Detection of oncogen mutations in sputum precedes diagnosis of lung cancer. Cancer Res 1994 ; 54 : 1634 –7. OpenUrl Abstract / FREE Full Text
- ↵ Mao L , Lee J, Kurie J. Clonal genetic alterations in the lungs of current and former smokers. J Natl Cancer Inst 1997 ; 89 : 857 –62. OpenUrl Abstract / FREE Full Text
- ↵ Isobe M , Emanuel B, Givol D. Localization of gene for human p53 tumour antigen to band 17p13. Nature 1986 ; 320 : 84 –5. OpenUrl CrossRef PubMed Web of Science
- ↵ Ohta M , Inoue M, Cotticelli M. The FHIT gene, spanning the chromosome 3p14.2 fragile site and renal carcinoma-associated t(3;8) breakpoint, is abnormal in digestive tract cancers. Cell 1996 ; 84 : 587 –97. OpenUrl CrossRef PubMed Web of Science
- Kamb A , Gruis N, Weaver-Feldhaus J. A cell cycle regulator potentially involved in genesis of many tumor types. Science 1994 ; 264 : 436 –40. OpenUrl Abstract / FREE Full Text
- ↵ Nobori T , Muira K, Wu D. Deletions of the cyclin-dependent kinase-4 inhibitor gene in multiple human cancers. Nature 1994 ; 368 : 753 –6. OpenUrl CrossRef PubMed Web of Science
- ↵ Shapiro GI , Park J, Edwards C, et al . Multiple mechanisms of p16INK4A inactivation in non-small cell lung cancer cell lines. Cancer Res 1995 ; 55 : 6200 –9. OpenUrl Abstract / FREE Full Text
- ↵ Ahrendt SA . Molecular detection of tumor cells in bronchoalveolar lavage fluid from patients with early stage lung cancer. J Natl Cancer Inst 1999 ; 91 : 332 –9. OpenUrl Abstract / FREE Full Text
- Belinsky SA . Aberrant methylation of p16(INK4a) is an early event in lung cancer and a potential biomarker for early diagnosis. Proc Natl Acad Sci USA 1998 ; 95 : 11891 –6. OpenUrl Abstract / FREE Full Text
- ↵ Merlo A , Herman J, Mao L, et al . 5‘ CpG island methylation is associated with transcriptional silencing of the tumour suppressor p16/CDKN2/MTS1 in human cancers. Nature Med 1995 ; 1 : 686 –92. OpenUrl CrossRef PubMed Web of Science
- ↵ Swafford DS , Middleton S, Palmisano W, et al . Frequent aberrant methylation of p16INK4a in primary rat lung tumors. Mol Cell Biol 1997 ; 17 : 1366 –74. OpenUrl Abstract / FREE Full Text
- ↵ Herman JG , Graff J, Myohanen S, et al . Methylation-specific PCR: a novel PCR assay for methylation status of CpG islands. Proc Natl Acad Sci USA 1996 ; 93 : 9821 –6. OpenUrl Abstract / FREE Full Text
- ↵ Palmisano WA, Divine KK, Saccomanno G et al . Predicting lung cancer by detecting aberrant promoter methylation in sputum. Cancer Res 2000 ; 60 : 5954 –8. OpenUrl Abstract / FREE Full Text
- ↵ Papadimitrakopoulou VA , Izzo J, Mao L, et al . Cyclin D1 and p16 alterations in advanced premalignant lesions of the upper aerodigestive tract: role in response to chemoprevention and cancer development. Clin Cancer Res 2001 ; 7 : 3127 –34. OpenUrl Abstract / FREE Full Text
- ↵ Soslow RA , Dannenberg A, Rush D, et al . COX-2 is expressed in human pulmonary, colonic, and mammary tumors. Cancer 2000 ; 89 : 2637 –45. OpenUrl CrossRef PubMed Web of Science
- Hosomi Y , Yokose T, Hirose Y, et al . Increased cyclooxygenase 2 (COX-2) expression occurs frequently in precursor lesions of human adenocarcinoma of the lung. Lung Cancer 2000 ; 30 : 73 –81. OpenUrl CrossRef PubMed Web of Science
- Watkins DN , Lenzo J, Segal A, et al . Expression and localization of cyclo-oxygenase isoforms in non-small cell lung cancer. Eur Respir J 1999 ; 14 : 412 –8. OpenUrl Abstract / FREE Full Text
- ↵ Wolff H , Saukkonen K, Anttila S, et al . Expression of cyclooxygenase-2 in human lung carcinoma. Cancer Res 1998 ; 58 : 4997 –5001. OpenUrl Abstract / FREE Full Text
- ↵ Hida T , Yatabe Y, Achiwa H, et al . Increased expression of cyclooxygenase 2 occurs frequently in human lung cancers, specifically in adenocarcinomas. Cancer Res 1998 ; 58 : 3761 –4. OpenUrl Abstract / FREE Full Text
- ↵ Hung WC , Chang H, Pan M, et al . Induction of p27(KIP1) as a mechanism underlying NS398-induced growth inhibition in human lung cancer cells. Mol Pharmacol 2000 ; 58 : 1398 –403. OpenUrl PubMed Web of Science
- ↵ Eli Y , Przedecki F, Levin G, et al . Comparative effects of indomethacin on cell proliferation and cell cycle progression in tumor cells grown in vitro and in vivo. Biochem Pharmacol 2001 ; 61 : 565 –71. OpenUrl CrossRef PubMed Web of Science
- ↵ Brabender J , Danenberg K, Metzger R, et al . Epidermal growth factor receptor and HER2-neu mRNA expression in non-small cell lung cancer is correlated with survival. Clin Cancer Res 2001 ; 7 : 1850 –5. OpenUrl Abstract / FREE Full Text
- Hendler FJ , Ozanne B. Human squamous cell lung cancers express increased epidermal growth factor receptors. J Clin Invest 1984 ; 74 : 647 –51. OpenUrl CrossRef PubMed Web of Science
- Cerny T , Barnes D, Hasleton P, et al . Expression of epidermal growth factor receptor (EGF-R) in human lung tumours. Br J Cancer 1986 ; 54 : 265 –9. OpenUrl CrossRef PubMed Web of Science
- ↵ Veale D , Ashcroft T, Marsh C, et al . Epidermal growth factor receptors in non-small cell lung cancer. Br J Cancer 1987 ; 55 : 513 –6. OpenUrl CrossRef PubMed Web of Science
- ↵ Ozanne B , Richards C, Hendler F J, et al . Over-expression of the EGF receptor is a hallmark of squamous cell carcinomas. J Pathol 1986 ; 149 : 9 –14. OpenUrl CrossRef PubMed Web of Science
- ↵ Berger MS . Epidermal growth factor receptors in lung tumours. J Pathol 1987 ; 152 : 297 –307. OpenUrl CrossRef PubMed Web of Science
Read the full text or download the PDF:
You are using an outdated browser. Please upgrade your browser to improve your experience.
Skip to Site Navigation Skip to Page Content
- Physician Referrals
- Patient Resources
- Why UT Southwestern
Refine your search: Find a Doctor Search Conditions & Treatments Find a Location

Appointment New Patient Appointment or Call 214-645-8300
Lung Cancer
Lung Cancer Awareness and Prevention
Appointment New Patient Appointment or 214-645-8300
Explore Lung Cancer
Lung cancer is often diagnosed in the late stages of the disease, largely because there are few or no symptoms in the early stages. Having an awareness of the risks and reducing them, plus early detection, can change a person’s outcome.
Reducing the Risk of Lung Cancer
The most common cause of lung cancer is cigarette smoking, which is linked to 80 to 90 percent of lung cancer cases. People who quit smoking have a lower risk of lung cancer than if they had continued to smoke, but their risk is higher than the risk for people who never smoked. Quitting smoking at any age can lower the risk of lung cancer.
UT Southwestern offers a nicotine cessation program to help anyone quit smoking or stop using other nicotine products. Our program offers a supportive, non-judgmental environment that can help people overcome nicotine addiction. Call 833-722-6237 for details.
Secondhand smoke also contributes to lung cancer and should be avoided.
Inhaling chemicals such as radon at a workplace can also cause lung cancer. People who work around chemicals should take safety precautions and use breathing equipment or masks.
The odds for developing lung cancer are higher for those who have a family history of lung cancer or a history of lung disease.
Early Detection
Early detection and diagnosis of lung cancer are major factors in treatment strategy and can improve a person’s chances for a successful outcome.
For those at high risk for lung cancer, UT Southwestern, in partnership with MD Anderson Cancer Center, offers a computed tomography (CT) screening test , possibly at no cost to the patient, that can detect lung cancer early.
This screening program is for patients who:
- Are 50 years of age or older
- History of smoking one pack a day for 20 years
- No other lung disease issues
- Currently smoke or have quit within the past 15 years
Alicia's Story
Alicia Ford-Anderson has seen up close and personal what lung cancer can do. She lost her husband to the disease and wondered whether her own long history of smoking – begun during the “glam” days of the ’60s – had damaged her singing voice and perhaps taken years from her own life. A CT screening for lung cancer gave her the answers she sought, and now she’s singing its praises.
Lung Cancer Awareness
This animated infographic shows the positive changes the body experiences over time after quitting smoking.
You can lower your lung cancer risk in several ways.
Don’t Smoke
The most important thing you can do to prevent lung cancer is to not start smoking, or to quit if you smoke. Smoking can cause cancer and then block your body from fighting it. Nearly 9 out of 10 lung cancers are caused by smoking cigarettes. Treatments are getting better for lung cancer, but it still kills more men and women than any other type of cancer.
For help quitting, visit smokefree.gov, call 1 (800) QUIT-NOW (784-8669), or text “QUIT” to 47848. It’s never too late to quit!
Stay Away from Secondhand Smoke
Smoke from other people’s cigarettes, pipes, or cigars is called secondhand smoke. Secondhand smoke causes lung cancer in adults who have never smoked. People who have never smoked but are exposed to secondhand smoke at home or at work increase their risk of getting lung cancer by 20% to 30%.
Get Your Home Tested for Radon
This video explains what radon is, how it can enter your home and cause lung cancer, and how to fix a radon problem if needed.
Radon is a gas that you cannot smell, taste, or see. It comes naturally from rocks and soil, and can dissolve in groundwater. Radon is thought to be the second leading cause of lung cancer in the United States, responsible for more than 20,000 lung cancer deaths each year.
People can be exposed to radon mainly from breathing radon in air that comes through cracks and gaps in the foundation of buildings and homes. One out of 15 homes has a high level of radon. Testing your home is the only way to find out if you have a radon problem. If you do, then you can fix it.
Is Lung Cancer Screening Right for You?
The U.S. Preventive Services Task Force recommends yearly lung cancer screening with low-dose computed tomography (CT scan) for people who—
- Have a 20 pack-year or more smoking history, and
- Smoke now or have quit within the past 15 years, and
- Are between 50 and 80 years old.
A pack-year is smoking an average of one pack of cigarettes per day for one year. For example, a person could have a 20 pack-year history by smoking one pack a day for 20 years or two packs a day for 10 years.
Lung cancer screening is not without risks. That is why lung cancer screening is recommended only for adults who are at high risk for developing the disease because of their smoking history and age.
If you are thinking about getting screened, learn more and talk to your doctor. Lung cancer screening is not a substitute for quitting smoking.
- Lung cancer is the leading cause of cancer death among both men and women in the United States.
- Each year, about 197,000 people in the United States are told they have lung cancer, and about 136,000 people die from this disease.
- Different people have different symptoms for lung cancer. Most people with lung cancer don’t have symptoms until the cancer is advanced.

How did Jackie, who never smoked, develop lung cancer? She is grateful that she found an answer. Read her story.

Smoking tobacco products causes almost nine of every 10 cases of lung cancer, and can cause cancer almost anywhere in your body.

This blog post shares nine caring ways to support someone who has lung cancer.

Stay Informed
Exit notification / disclaimer policy.
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Patient Care & Health Information
- Diseases & Conditions
- Lung cancer
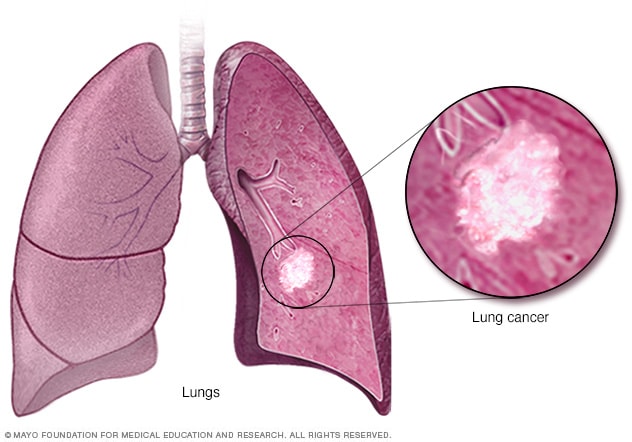
Lung cancer begins in the cells of the lungs.
Lung cancer is a kind of cancer that starts as a growth of cells in the lungs. The lungs are two spongy organs in the chest that control breathing.
Lung cancer is the leading cause of cancer deaths worldwide.
People who smoke have the greatest risk of lung cancer. The risk of lung cancer increases with the length of time and number of cigarettes smoked. Quitting smoking, even after smoking for many years, significantly lowers the chances of developing lung cancer. Lung cancer also can happen in people who have never smoked.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Lung cancer typically doesn't cause symptoms early on. Symptoms of lung cancer usually happen when the disease is advanced.
Signs and symptoms of lung cancer that happen in and around the lungs may include:
- A new cough that doesn't go away.
- Chest pain.
- Coughing up blood, even a small amount.
- Hoarseness.
- Shortness of breath.
Signs and symptoms that happen when lung cancer spreads to other parts of the body may include:
- Losing weight without trying.
- Loss of appetite.
- Swelling in the face or neck.
When to see a doctor
Make an appointment with your doctor or other healthcare professional if you have any symptoms that worry you.
If you smoke and haven't been able to quit, make an appointment. Your healthcare professional can recommend strategies for quitting smoking. These may include counseling, medicines and nicotine replacement products.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
Get Mayo Clinic cancer expertise delivered to your inbox.
Subscribe for free and receive an in-depth guide to coping with cancer, plus helpful information on how to get a second opinion. You can unsubscribe at any time. Click here for an email preview.
Error Select a topic
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing
Your in-depth coping with cancer guide will be in your inbox shortly. You will also receive emails from Mayo Clinic on the latest about cancer news, research, and care.
If you don’t receive our email within 5 minutes, check your SPAM folder, then contact us at [email protected] .
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Lung cancer happens when cells in the lungs develop changes in their DNA. A cell's DNA holds the instructions that tell a cell what to do. In healthy cells, the DNA gives instructions to grow and multiply at a set rate. The instructions tell the cells to die at a set time. In cancer cells, the DNA changes give different instructions. The changes tell the cancer cells to make many more cells quickly. Cancer cells can keep living when healthy cells would die. This causes too many cells.
The cancer cells might form a mass called a tumor. The tumor can grow to invade and destroy healthy body tissue. In time, cancer cells can break away and spread to other parts of the body. When cancer spreads, it's called metastatic cancer.
Smoking causes most lung cancers. It can cause lung cancer in both people who smoke and in people exposed to secondhand smoke. But lung cancer also happens in people who never smoked or been exposed to secondhand smoke. In these people, there may be no clear cause of lung cancer.
How smoking causes lung cancer
Researchers believe smoking causes lung cancer by damaging the cells that line the lungs. Cigarette smoke is full of cancer-causing substances, called carcinogens. When you inhale cigarette smoke, the carcinogens cause changes in the lung tissue almost immediately.
At first your body may be able to repair this damage. But with each repeated exposure, healthy cells that line your lungs become more damaged. Over time, the damage causes cells to change and eventually cancer may develop.
Types of lung cancer
Lung cancer is divided into two major types based on the appearance of the cells under a microscope. Your healthcare professional makes treatment decisions based on which major type of lung cancer you have.
The two general types of lung cancer include:
- Small cell lung cancer. Small cell lung cancer usually only happens in people who have smoked heavily for years. Small cell lung cancer is less common than non-small cell lung cancer.
- Non-small cell lung cancer. Non-small cell lung cancer is a category that includes several types of lung cancers. Non-small cell lung cancers include squamous cell carcinoma, adenocarcinoma and large cell carcinoma.
Risk factors
A number of factors may increase the risk of lung cancer. Some risk factors can be controlled, for instance, by quitting smoking. Other factors can't be controlled, such as your family history.
Risk factors for lung cancer include:
Your risk of lung cancer increases with the number of cigarettes you smoke each day. Your risk also increases with the number of years you have smoked. Quitting at any age can significantly lower your risk of developing lung cancer.
Exposure to secondhand smoke
Even if you don't smoke, your risk of lung cancer increases if you're around people who are smoking. Breathing the smoke in the air from other people who are smoking is called secondhand smoke.
Previous radiation therapy
If you've had radiation therapy to the chest for another type of cancer, you may have an increased risk of developing lung cancer.
Exposure to radon gas
Radon is produced by the natural breakdown of uranium in soil, rock and water. Radon eventually becomes part of the air you breathe. Unsafe levels of radon can build up in any building, including homes.
Exposure to cancer-causing substances
Workplace exposure to cancer-causing substances, called carcinogens, can increase your risk of developing lung cancer. The risk may be higher if you smoke. Carcinogens linked to lung cancer risk include asbestos, arsenic, chromium and nickel.
Family history of lung cancer
People with a parent, sibling or child with lung cancer have an increased risk of the disease.
Complications
Lung cancer can cause complications, such as:
Shortness of breath
People with lung cancer can experience shortness of breath if cancer grows to block the major airways. Lung cancer also can cause fluid to collect around the lungs and heart. The fluid makes it harder for the affected lung to expand fully when you inhale.
Coughing up blood
Lung cancer can cause bleeding in the airway. This can cause you to cough up blood. Sometimes bleeding can become severe. Treatments are available to control bleeding.
Advanced lung cancer that spreads can cause pain. It may spread to the lining of a lung or to another area of the body, such as a bone. Tell your healthcare professional if you experience pain. Many treatments are available to control pain.
Fluid in the chest
Lung cancer can cause fluid to accumulate in the chest, called pleural effusion. The fluid collects in the space that surrounds the affected lung in the chest cavity, called the pleural space.
Pleural effusion can cause shortness of breath. Treatments are available to drain the fluid from your chest. Treatments can reduce the risk that pleural effusion will happen again.
Cancer that spreads to other parts of the body
Lung cancer often spreads to other parts of the body. Lung cancer may spread to the brain and the bones.
Cancer that spreads can cause pain, nausea, headaches or other symptoms depending on what organ is affected. Once lung cancer has spread beyond the lungs, it's generally not curable. Treatments are available to decrease symptoms and to help you live longer.
There's no sure way to prevent lung cancer, but you can reduce your risk if you:
Don't smoke
If you've never smoked, don't start. Talk to your children about not smoking so that they can understand how to avoid this major risk factor for lung cancer. Begin conversations about the dangers of smoking with your children early so that they know how to react to peer pressure.
Stop smoking
Stop smoking now. Quitting reduces your risk of lung cancer, even if you've smoked for years. Talk to your healthcare team about strategies and aids that can help you quit. Options include nicotine replacement products, medicines and support groups.
Avoid secondhand smoke
If you live or work with a person who smokes, urge them to quit. At the very least, ask them to smoke outside. Avoid areas where people smoke, such as bars. Seek out smoke-free options.
Test your home for radon
Have the radon levels in your home checked, especially if you live in an area where radon is known to be a problem. High radon levels can be fixed to make your home safer. Radon test kits are often sold at hardware stores and can be purchased online. For more information on radon testing, contact your local department of public health.
Avoid carcinogens at work
Take precautions to protect yourself from exposure to toxic chemicals at work. Follow your employer's precautions. For instance, if you're given a face mask for protection, always wear it. Ask your healthcare professional what more you can do to protect yourself at work. Your risk of lung damage from workplace carcinogens increases if you smoke.
Eat a diet full of fruits and vegetables
Choose a healthy diet with a variety of fruits and vegetables. Food sources of vitamins and nutrients are best. Avoid taking large doses of vitamins in pill form, as they may be harmful. For instance, researchers hoping to reduce the risk of lung cancer in people who smoked heavily gave them beta carotene supplements. Results showed the supplements increased the risk of cancer in people who smoke.
Exercise most days of the week
If you don't exercise regularly, start out slowly. Try to exercise most days of the week.
Lung cancer care at Mayo Clinic
Living with lung cancer?
Connect with others like you for support and answers to your questions in the Lung Cancer support group on Mayo Clinic Connect, a patient community.
Lung Cancer Discussions

59 Replies Sun, Apr 07, 2024

18 Replies Sun, Apr 07, 2024

107 Replies Mon, Apr 01, 2024
- Non-small cell lung cancer. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1450. Accessed Dec. 4, 2023.
- Small cell lung cancer. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1462. Accessed Dec. 4, 2023.
- Niederhuber JE, et al., eds. Cancer of the lung: Non-small cell lung cancer and small cell lung cancer. In: Abeloff's Clinical Oncology. 6th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Dec. 4, 2023.
- Non-small cell lung cancer treatment (PDQ) – Patient version. National Cancer Institute. https://www.cancer.gov/types/lung/patient/non-small-cell-lung-treatment-pdq. Accessed Dec. 4, 2023.
- Small cell lung cancer treatment (PDQ) – Patient version. National Cancer Institute. https://www.cancer.gov/types/lung/patient/small-cell-lung-treatment-pdq. Accessed Dec. 4, 2023.
- Lung cancer – non-small cell. Cancer.Net. https://www.cancer.net/cancer-types/lung-cancer/view-all. Accessed Dec. 4, 2023.
- Lung cancer – small cell. Cancer.Net. https://www.cancer.net/cancer-types/33776/view-all. Accessed Dec. 4, 2023.
- Detterbeck FC, et al. Executive Summary: Diagnosis and management of lung cancer, 3rd ed.: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013; doi:10.1378/chest.12-2377.
- Palliative care. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=3&id=1454. Accessed Dec. 4, 2023.
- Lung cancer. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/lung-cancer. Accessed Dec. 4, 2023.
- Cairns LM. Managing breathlessness in patients with lung cancer. Nursing Standard. 2012; doi:10.7748/ns2012.11.27.13.44.c9450.
- Warner KJ. Allscripts EPSi. Mayo Clinic. Jan. 13, 2020.
- Brown AY. Allscripts EPSi. Mayo Clinic. July 30, 2019.
- Searching for cancer centers. American College of Surgeons. https://www.facs.org/search/cancer-programs. Accessed Dec. 4, 2023.
- Temel JS, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. New England Journal of Medicine. 2010; doi:10.1056/NEJMoa1000678.
- Dunning J, et al. Microlobectomy: A novel form of endoscopic lobectomy. Innovations. 2017; doi:10.1097/IMI.0000000000000394.
- Leventakos K, et al. Advances in the treatment of non-small cell lung cancer: Focus on nivolumab, pembrolizumab and atezolizumab. BioDrugs. 2016; doi:10.1007/s40259-016-0187-0.
- Dong H, et al. B7-H1, a third member of the B7 family, co-stimulates T-cell proliferation and interleukin-10 secretion. Nature Medicine. 1999;5:1365.
- Aberle DR, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. New England Journal of Medicine. 2011; doi:10.1056/NEJMoa1102873.
- Infographic: Lung Cancer
- Lung cancer surgery
- Lung nodules: Can they be cancerous?
- Super Survivor Conquers Cancer
Associated Procedures
- Ablation therapy
- Brachytherapy
- Bronchoscopy
- Chemotherapy
- Lung cancer screening
- Positron emission tomography scan
- Proton therapy
- Radiation therapy
- Stop-smoking services
News from Mayo Clinic
- Science Saturday: Study finds senescent immune cells promote lung tumor growth June 17, 2023, 11:00 a.m. CDT
- Era of hope for patients with lung cancer Nov. 16, 2022, 03:00 p.m. CDT
- Mayo Clinic Q&A podcast: Survivorship after surgery for lung cancer Nov. 15, 2022, 01:30 p.m. CDT
- Mayo Clinic Minute: Understanding lung cancer Nov. 02, 2022, 04:00 p.m. CDT
- Lung cancer diagnosis innovation leads to higher survival rates Nov. 02, 2022, 02:30 p.m. CDT
Mayo Clinic in Rochester, Minnesota, Mayo Clinic in Phoenix/Scottsdale, Arizona, and Mayo Clinic in Jacksonville, Florida, have been recognized among the top Pulmonology hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Lung Cancer Disease and Prevention Methods Research Paper
Introduction, description of the disease, current statistics of those affected, risk factors, medication and treatment, works cited.
Lung cancer is a common and deadly form of cancer characterized by the development of cancerous cells in the lungs of the individual. This disease is associated with many negative health and social outcomes for the patient. There is no cure for lung cancer, although treatment can be offered to improve the patient’s quality of life and their survival rate. This paper will provide a description of lung cancer and document the risk factors for the disease. The treatment options for the disease and prevention methods will be discussed.
Lung cancer is the type of cancer characterized by the development of cancerous cells in the lungs of the individual. As the disease progresses, the malignant cells can spread to other body organs. The American Cancer Society places cancer as the third most common cancer and it accounts for 13% of new cancer cases.
While it is the third most common cancer, lung cancer is the leading cause of cancer-related deaths in the US (Moyer 330). Zakowski declares that lung cancer “remains the largest cancer killer in the westernized world, with approximately 226000 new cases, and more than 160,000 deaths estimated for 2012 in the US” (1816).
There are several different histological forms of lung cancer and each unique type influences the treatment choice and prognosis. The first main type of lung cancer is non-small cell lung cancer (NSCLC) and it makes up 85% of all the lung cancer cases (Bennett and White 50). The second type is small cell lung cancer (SCLC) and it accounts for 15% of the lung cancer diagnoses. NSCLC is further subdivided into “squamous cell carcinoma, adenocarcinoma, and large cell carcinoma” (Bennett and White 51).
Squamous cell carcinoma is caused by the mutation of the healthy cells found on the lining of the airways into malignant cells. The cancer starts near the center of the chest and spreads to the other parts of the lungs. Squamous cell carcinoma is the most common type of NSCLC and it is closely associated with smoking. Adenocarcinoma develops when cancerous cells develop in the mucus producing cells in the lungs. This type of NSCLC starts from the outer regions of the lungs and it is common in non-smokers.
Lung cancer is more prevalent in men than in women. This high representation of men can be explained by the fact that the smoking population is predominantly male. However, women who smoke are at a greater risk of developing lung cancer since women are more susceptible than men to the carcinogens in tobacco smoke (Bennett and White 51).
There is an increase in the prevalence of lung cancer as individuals get older. A report by the CDC reveals that incidents of lung cancer are most common in adults aged 55 years and above (Moyer 334). Diagnosis for lung cancer peaks between the ages of 74 and 84 years.
The primary risk factor for lung cancer is cigarette smoking and up to 90% of lung cancer cases are caused by using tobacco products. Inhalation of tobacco smoke causes lung cancer since this smoke is comprised of a toxic mixture of thousands of chemicals.
The risk for lung cancer increases with the number of cigarettes and the duration of time that a person smokes. As far back as the 1950s, researchers had identified that the risk of developing lung cancer “increases proportionally to the amount of cigarettes smoked, with those who smoke 25 or more cigarettes each day being 50 times more likely to develop lung cancer compared with non-smokers” (Bennett and White 51).
Exposure to naturally occurring substances such as Radon gas is also a significant risk factor. The Centers for Disease Control and Prevention documents that naturally occurring Radon might be trapped in houses where people become exposed to it (par. 8). Since the gas is odorless and invisible, people might be subjected to high Radon levels without knowing it.
Exposure to toxic substances such as diesel fumes and asbestos dust also significantly increases the chances of an individual developing lung cancer. The Centers for Disease Control and Prevention reports that genes play a minor role in causing lung cancer (par. 15). While this risk factor is rare, there are cases where lung cancer is inherited. An individual from a family with a history of lung cancer is therefore more likely to develop the disease that one who is from a family without a history of this disease.
Lung cancer is detected through screening of a person for the disease. Screening can be done using Low Dose Computed Tomography, chest radiography, and sputum cytologic evaluation. However, screening with Low Dose Computed Tomography (LDCT) is more effective since this method has a greater sensitivity for detecting early stage cancer. Zakowski documents that individuals who are screened with LDC have a 20% lower risk of dying from the disease than those who are screened using chest radiography, and sputum cytologic (1816).
Chemotherapy is the most common treatment for patients with small cell lung cancer. Chemotherapy is chosen over surgery since the cells are too small to be detected through imaging. In addition to this, there is a likelihood that the cells have broken away and started moving to other organs (Bennett and White 55). Chemotherapy is able to treat cancer cells throughout the body since it circulates in the bloodstream.
Patients who respond positively to chemotherapy are offered sequential consolidation chest radiotherapy to improve on the positive results of the chemotherapy. In chest radiotherapy, the beam is directed to the area where the cancerous cells have been detected.
Patients receiving chemotherapy to treat lung cancer often experience a range of physical and psychosocial problems. The physic problems include coughs, pain, fatigue, and decreased functional capacity. Psychologically, lung cancer patients experience increased anxiety and depression levels.
For non-small cell lung cancer, surgery is the mainstay of treatment. Specifically, this treatment is recommended for patients diagnosed with Stage I-IIIa NSCLC. In these stages, the tumor can be up to 7cm and it can be invading the chest wall, diaphragm, or phrenic nerve. Surgery is undertaken to remove the cancerous tumor. Bennett and White state that surgery is a potentially curative treatment since it can lead to the complete elimination of the cancer (55).
Complete excision of the tumor through surgery often leads to complete curing. However, a patient must demonstrate fitness in order to be considered a candidate for surgery. While research is ongoing, there is currently no cure for late stage lung cancer. For patients with advanced lung cancer, there is no hope of cure and the goal of treatment efforts is to improve the patients’ quality of life and possibly keep him alive for longer.
In addition to medication, physical exercise has beneficial effects for cancer patients. Research by Quist reveals that physical exercise for advanced stage lung cancer patients improves the quality of life and reduces symptoms and side effects for the patients (9). Physical exercise has some notable merits, including improving the physical capacity of the lung cancer patient. The patient’s psychological outcomes are also improved as the anxiety and depression levels are decreased through exercising.
The Prognosis for lung cancer is poor since almost all patients suffering from this disease succumb to it in a relatively short time. Moyer documents that about 90% of individuals diagnosed with lung cancer die of the disease (331). The survival rate for lung cancer patients is currently 5 years. This is one of the lowest survival rates of all types of cancers, making lung cancer one of the deadliest cancer forms. The low survival rate of lung cancer patients is attributed to the fact that most patients are unfit for surgery.
Quist reveals that in most cases, surgery is required to manage lung cancer (1). However, most patients are not surgical candidates since the condition is discovered at a late stage. Quist reveals that most patients with lung cancer have reduced physical capacity and functional capacity, making them poor candidates for surgery (1).
The best prognosis is achieved for patients whose cancer is discovered at an early stage. The Early state includes non-small cell lung cancer (NSCLC) states I-IIIa and Small Cell Lung Cancer limited disease. For patients with lung cancer at this stage, treatment is provided with curative intent. Patients with advanced lung cancer have an even lower prognosis.
Quist states that patients with NSCLC IIIb-IV survive for an average of 10-13 months after diagnosis (3). This observation is corroborated by Bennett and White, who document that up to 80% of patients with advanced lung cancer will die within one year of diagnosis (51).
Considering the poor prognosis of lung cancer, the most effective way of dealing with the disease is to prevent it from occurring in the first place. Research clearly shows that smoking is the most important risk factor for lung cancer. The most important prevention method is mitigating or altogether stopping smoking among members of the general population. Moyer documents that smokers should be advised to quit smoking and measures should be taken to prevent non-smokers from being exposed to tobacco smoke (332).
Treatment options to assist in cessation can also be provided by health care service providers and the government. A lot of support is provided for individuals who want to quit smoking. The CDC provides a wide range of resources to assist in smoking cessation, including behavioral counseling and support.
The survival rate for lung cancer patients is significantly higher if the disease is diagnosed at an early stage. The delay in diagnosis is caused by a lack of awareness of the risk of lung cancer as well as the absence of symptoms during the initial stages of the disease. As such, regular screening for high-risk persons is recommended. Through regular screening of high-risk persons, a substantial number of lung-cancer related deaths can be prevented (331).
Bennett, Alison and John White. “Improving care and quality of life for patients with lung cancer.” Nursing Standard 28.9 (2013): 50-58. Web.
Centers for Disease Control and Prevention. Lung Cancer: Basic information. 2013. Web.
Moyer, Virginia. “Screening for Lung Cancer: U.S. Preventive Services Task Force Recommendation Statement.” Annals of Internal Medicine 160.5 (2014): 330-340. Web.
Quist, Morten. “Exhale exercise as a strategy for rehabilitation in advanced stage lung cancer patients: a randomized clinical trial comparing the effects of 12 weeks supervised exercise intervention versus usual care for advanced stage lung cancer patients.” BMC Cancer 13.1 (2013): 1-14. Web.
Zakowski, Maureen. “Lung Cancer in the Era of Targeted Therapy.” Archives of Pathology & Laboratory Medicine 137.12 (2013): 1816-1821. Print.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2020, April 1). Lung Cancer Disease and Prevention Methods. https://ivypanda.com/essays/lung-cancer-disease-and-prevention-methods/
"Lung Cancer Disease and Prevention Methods." IvyPanda , 1 Apr. 2020, ivypanda.com/essays/lung-cancer-disease-and-prevention-methods/.
IvyPanda . (2020) 'Lung Cancer Disease and Prevention Methods'. 1 April.
IvyPanda . 2020. "Lung Cancer Disease and Prevention Methods." April 1, 2020. https://ivypanda.com/essays/lung-cancer-disease-and-prevention-methods/.
1. IvyPanda . "Lung Cancer Disease and Prevention Methods." April 1, 2020. https://ivypanda.com/essays/lung-cancer-disease-and-prevention-methods/.
Bibliography
IvyPanda . "Lung Cancer Disease and Prevention Methods." April 1, 2020. https://ivypanda.com/essays/lung-cancer-disease-and-prevention-methods/.
- The Preliminary Results of Tomotherapy
- Practice of Qualitative Research Report
- Lung Cancer and Cystic Fibrosis: Diagnosis and Care
- Carcinoma in Situ Management Options
- Hepatocellular Carcinoma Diagnosis and Treatment
- Basal Cell Carcinoma - Symptoms and Causes
- Hepatocellular Carcinoma: Case Study Assignment
- Histopathology: Epidermal Changes
- Endocrine System: Fat Necrosis in a Patient
- Fibrocystic Breast Condition or Breast Cancer?
- Opposing Viewpoints on Vaccination
- Lupus – Skin Disease (Discoid)
- Pancreatic Pseudoaneurysm Diagnosis and Management
- The Pathology of Acne
- Healthcare: High Blood Pressure
Home — Essay Samples — Nursing & Health — Lung Cancer — The Prevention and Treatment of the Deadly Lung Cancer
The Prevention and Treatment of The Deadly Lung Cancer
- Categories: Lung Cancer The Dead
About this sample

Words: 530 |
Published: Oct 4, 2018
Words: 530 | Page: 1 | 3 min read
Deadly Lung Cancer

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr. Karlyna PhD
Verified writer
- Expert in: Nursing & Health Literature

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 844 words
1 pages / 558 words
3 pages / 1247 words
3 pages / 1206 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
In multiple studies, at both transcript and protein levels, increased expression of biomarkers Rrm1, Rrm2 as well as Tyms were observed in NSCLC patients and suggested for their implications in cancer therapy (Grossi F et al. [...]
Brief overview of breast cancer awareness and its goals Role of breast cancer advocates in raising funds and lobbying for better care The cultural aspect of breast cancer advocacy and pink ribbon culture The [...]
Skin cancer is caused by exposure to the sun. Skin cancer can develop during long term exposure or during short periods of more intense sun exposure. Ultraviolet light in sunlight damages the DNA in our skin cells. Damage can [...]
On February 2nd, 2013 at Chicago Academy High School I participated in the Leukemia Lymphoma walk in the cold walk-a-thon. It was a great experience, and I’m glad I choose it as a service learning project. We walked around the [...]
Leukemia is a psychosocial type of illness that results in the production of a high number of under-developed white blood cells called blasts. The subject is a 27years old Caucasian lady who was diagnosed with chronic Leukemia [...]
Bioethics is the study of ethical problems arising from biological research.. Many people have commented on such subject of how X-rays, plastic from water bottles, and cell phones can cause cancers. This is a very recent [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free

Scientists are making a 'groundbreaking' lung cancer vaccine that could prevent up to 90% of cases
- K nown as 'LungVax', it is being created by researchers in London and Oxford
- READ MORE: The tell-tale lung cancer symptoms to be aware of
Scientists are developing a 'groundbreaking' lung cancer vaccine which research suggests will be effective in preventing up to 90 per cent of cases.
The jab — which will be given to those at highest risk of developing the disease — will train the immune system to spot and attack early signs of disease.
Experts described it as a 'crucial moment' in the fight against the devastating disease, which affects 48,500 in the UK every year.
Known as 'LungVax', it is being created by the University of Oxford , the Francis Crick Institute and University College London .
Lung cancer cells look different from normal cells due to having 'red flag' proteins called neoantigens.
Neoantigens appear on the surface of the cell because of cancer-causing mutations within the cell's DNA.
The LungVax vaccine will carry a strand of DNA which trains the immune system to recognise these neoantigens on abnormal lung cells.
It will then activate the immune system to kill these cells and stop lung cancer.
Professor Tim Eilliot, lead researcher at the University of Oxford, said: 'Cancer is a disease of our own bodies and it's hard for the immune system to distinguish between what's normal and what's cancer.
'Getting the immune system to recognise and attack cancer is one of the biggest challenges in cancer research today.
'This research could deliver an off-the-shelf vaccine based on Oxford's vaccine technology, which proved itself in the Covid pandemic.
'If we can replicate the kind of success seen in trials during the pandemic, we could save the lives of tens of thousands of people every year in the UK alone.'
Researchers have been granted up to £1.7 million from Cancer Research UK and the CRIS Cancer Foundation.
The team will receive funding for the study over the next 2 years to support lab research and initial manufacturing of 3,000 doses of the vaccine at the Oxford Clinical BioManufacturing Facility.
If successful, the vaccine will move straight into a clinical trials, involving those at biggest risk of disease, such as current and former smokers who currently qualify for targeted lung health checks in some parts of the UK.
Fewer than 10 per cent of people with lung cancer survive their disease for 10 years or more.
Professor Mariam Jamal-Hanjani of University College London and the Francis Crick Institute, said: 'We think the vaccine could cover around 90 per cent of all lung cancers, based on our computer models and previous research, and this funding will allow us to take the vital first steps towards trials in patients.
'LungVax will not replace stopping smoking as the best way to reduce your risk of lung cancer.
'But it could offer a viable route to preventing some of the earliest stage cancers from emerging in the first place.'
Lola Manterola, President of CRIS Cancer Foundation, said: 'We are at a crucial moment in the history of cancer research and treatment.
'For the first time, technology and knowledge of the immune system are allowing us to take the first steps towards preventing cancer.
'This groundbreaking study represents a firm step in that direction, and we at CRIS consider it essential to support it.'

- Share full article
Advertisement
Doctors Say Diagnosis of Catherine’s Cancer Is a Familiar Scenario
The Princess of Wales did not reveal the type of cancer she has, but oncologists say the disease is often identified during other procedures.

By Gina Kolata
Gina Kolata previously reported on King Charles III’s cancer diagnosis .
- Published March 22, 2024 Updated March 25, 2024
Although it is not known what type of cancer Princess Catherine has, oncologists say that what she described in her public statement that was released on Friday — discovering a cancer during another procedure, in this case a “major abdominal surgery” — is all too common.
“Unfortunately, so much of the cancer we diagnose is unexpected,” said Dr. Elena Ratner, a gynecologic oncologist at Yale Cancer Center who has diagnosed many patients with ovarian cancer, uterine cancer and cancers of the lining of the uterus.
Without speculating on Catherine’s procedure, Dr. Ratner described situations in which women will go in for surgery for endometriosis, a condition in which tissue similar to the lining of the uterus is found elsewhere in the abdomen. Often, Dr. Ratner says, the assumption is that the endometriosis has appeared on an ovary and caused a benign ovarian cyst. But one to two weeks later, when the supposedly benign tissue has been studied, pathologists report that they found cancer.
In the statement, Princess Catherine said she is getting “a course of preventive chemotherapy.”
That, too, is common. In medical settings, it is usually called adjuvant chemotherapy.
Dr. Eric Winer, director of the Yale Cancer Center, said that with adjuvant chemotherapy, “the hope is that this will prevent further problems” and avoid a recurrence of the cancer.
It also means that “you removed everything” that was visible with surgery, said Dr. Michael Birrer, director of the Winthrop P. Rockefeller Cancer Institute at the University of Arkansas for Medical Sciences. “You can’t see the cancer,” he added, because microscopic cancer cells may be left behind. The chemotherapy is a way to attack microscopic disease, he explained.
Other parts of Catherine’s statement also hit home for Dr. Ratner, particularly her concern for her family.
“William and I have been doing everything we can to process and manage this privately for the sake of our young family,” Catherine said, and “It has taken us time to explain everything to George, Charlotte, and Louis in a way that is appropriate for them, and to reassure them that I am going to be OK.”
Those are sentiments that Dr. Ratner hears on a regular basis and reveal, she says, “how hard it is for women to be diagnosed with cancer.”
“I see this day in and day out,” she said. “Women always say, ‘Will I be there for my kids? What will happen with my kids?’
“They don’t say, ‘What will happen to me?’”
Gina Kolata reports on diseases and treatments, how treatments are discovered and tested, and how they affect people. More about Gina Kolata
The Fight Against Cancer
Colon and rectal cancers are increasing among people younger than 50. Experts have a few ideas about why .
Risk calculators can offer a more personalized picture of an individual patient’s breast cancer risk. But experts warn that the results need to be interpreted with the help of a doctor .
Early detection is a powerful weapon in preventing deaths from colon cancer, but many patients are reluctant to undergo colonoscopies or conduct at-home fecal tests. Doctors see potential in another screening method .
The human papillomavirus vaccine provides powerful protection against the leading cause of cervical cancer and against a strong risk factor for anal cancer. Here’s what to know about the shot.
A recent study adds to growing evidence that exercise is an important part of preventing prostate cancer , the second most common and second most fatal cancer in the United States for men.
No single food can prevent cancer on its own, but experts say that there are some that may help you build the best defense .
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Cancer Control: Knowledge Into Action: WHO Guide for Effective Programmes: Module 4: Diagnosis and Treatment. Geneva: World Health Organization; 2008.

Cancer Control: Knowledge Into Action: WHO Guide for Effective Programmes: Module 4: Diagnosis and Treatment.
A plan for the diagnosis and treatment of cancer is a key component of any overall cancer control plan. Its main goal is to cure cancer patients or prolong their life considerably, ensuring a good quality of life. In order for a diagnosis and treatment programme to be effective, it must never be developed in isolation. It needs to be linked to an early detection programme so that cases are detected at an early stage, when treatment is more effective and there is a greater chance of cure. It also needs to be integrated with a palliative care programme, so that patients with advanced cancers, who can no longer benefit from treatment, will get adequate relief from their physical, psychosocial and spiritual suffering. Furthermore, programmes should include a awareness-raising component, to educate patients, family and community members about the cancer risk factors and the need for taking preventive measures to avoid developing cancer.
Where resources are limited, diagnosis and treatment services should initially target all patients presenting with curable cancers, such as breast, cervical and oral cancers that can be detected early. They could also include childhood acute lymphatic leukaemia, which has a high potential for cure although it cannot be detected early. Above all, services need to be provided in an equitable and sustainable manner. As and when more resources become available, the programme can be extended to include other curable cancers as well as cancers for which treatment can prolong survival considerably.
This module on diagnosis and treatment is intended to evolve in response to national needs and experience. WHO welcomes input from countries wishing to share their successes in diagnosis and treatment. WHO also welcomes requests from countries for information relevant to their specific needs. Evidence on the barriers to diagnosis and treatment in country contexts – and the lessons learned in overcoming them – would be especially welcome (contact at http://www.who.int/cancer ).
All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: tni.ohw@sredrokoob ). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: tni.ohw@snoissimrep ).
- Cite this Page Cancer Control: Knowledge Into Action: WHO Guide for Effective Programmes: Module 4: Diagnosis and Treatment. Geneva: World Health Organization; 2008. CONCLUSION.
- PDF version of this title (3.4M)
Other titles in this collection
- WHO Guidelines Approved by the Guidelines Review Committee
Recent Activity
- CONCLUSION - Cancer Control: Knowledge Into Action CONCLUSION - Cancer Control: Knowledge Into Action
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
COMMENTS
Stay away from tobacco. The best way to reduce your risk of lung cancer is not to smoke and to avoid breathing in other people's smoke. If you stop smoking before a cancer develops, your damaged lung tissue gradually starts to repair itself. No matter what your age or how long you've smoked, quitting will lower your risk of lung cancer and ...
The best prevention for lung cancer is to stop smoking — or never start. In fact, cigarette smoking is the leading cause of preventable diseases in the country, according to the Centers for Disease Control and Prevention. Quitting smoking has immediate health benefits that help minimize a person's risk of developing lung cancer.
1. Introduction. There is a strong link between healthy lifestyle and pathologies such as cancer. Correct nutrition and regular physical activity can induce and/or reduce the molecular mechanism against cancer development and/or progression [].Lung cancer has long been the most common cancer in the world [].The processes leading to lung cancer establishment are different, and there are genetic ...
INTRODUCTION. Lung cancer (LC) is the leading cause of cancer incidence and mortality in men and women globally, with 2.1 million new cases (11.6% of the total cancer cases) and 1.8 million deaths (18.4% of the total cancer deaths) in the year 2018 alone (Bray et al., 2018).More than half of LC cases (53%) are diagnosed among men and women aged 55-74 years (median age = 70 years) (Torre et ...
INTRODUCTION. Lung cancer (LC) is the leading cause of cancer incidence and mortality in men and women globally, with 2.1 million new cases (11.6% of the total cancer cases) and 1.8 million deaths (18.4% of the total cancer deaths) in the year 2018 alone (Bray et al., 2018).More than half of LC cases (53%) are diagnosed among men and women aged 55-74 years (median age = 70 years) (Torre et ...
Lung cancer is a disease in which malignant (cancer) cells form in the tissues of the lung. The lungs are a pair of cone-shaped breathing organs in the chest. The lungs bring oxygen into the body as you breathe in. They release carbon dioxide, a waste product of the body's cells, as you breathe out.Each lung has sections called lobes.The left lung has two lobes.
Despite organized and extensive public health efforts to prevent and reduce cigarette smoking, lung cancer is the no. 1 cause of cancer death among men and women in the United States and worldwide. 1,2 According to the latest National Cancer Institute data, in 2012 lung cancer accounted for 13% of all new cancer diagnoses (1.8 million) and 19.4% of cancer mortality (1.6 million). 3 Higher lung ...
Lung cancer is a type of cancer that starts when abnormal cells grow in an uncontrolled way in the lungs. It is a serious health issue that can cause severe harm and death. Symptoms of lung cancer include a cough that does not go away, chest pain and shortness of breath. It is important to seek medical care early to avoid serious health effects.
Cancer of the lung causes more deaths from cancer worldwide than at any other site. The environmental, genetic, and dietary risk factors are discussed and progress in chemoprevention is reviewed. A better understanding of the molecular events that occur during carcinogenesis has opened up new areas of research in cancer prevention and a number of biochemical markers of high risk individuals ...
Don't smoke. Cigarette smoking causes about 80% to 90% of lung cancer deaths in the United States. The most important thing you can do to prevent lung cancer is to not start smoking, or to quit if you smoke. Avoid secondhand smoke. Smoke from other people's cigarettes, cigars, or pipes is called secondhand smoke. Make your home and car ...
Quitting smoking at any age can lower the risk of lung cancer. UT Southwestern offers a nicotine cessation program to help anyone quit smoking or stop using other nicotine products. Our program offers a supportive, non-judgmental environment that can help people overcome nicotine addiction. Call 833-722-6237 for details.
Smoking can cause cancer and then block your body from fighting it. Nearly 9 out of 10 lung cancers are caused by smoking cigarettes. Treatments are getting better for lung cancer, but it still kills more men and women than any other type of cancer. For help quitting, visit smokefree.gov, call 1 (800) QUIT-NOW (784-8669), or text "QUIT" to ...
PDQ Screening and Prevention Editorial Board. Published online: October 24, 2023. This PDQ cancer information summary has current information about lung cancer prevention. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Signs and symptoms of lung cancer that happen in and around the lungs may include: A new cough that doesn't go away. Chest pain. Coughing up blood, even a small amount. Hoarseness. Shortness of breath. Wheezing. Signs and symptoms that happen when lung cancer spreads to other parts of the body may include: Bone pain.
PDQ Screening and Prevention Editorial Board. Published online: June 8, 2023. This PDQ cancer information summary for health professionals provides comprehensive, peer-reviewed, evidence-based information about lung cancer prevention. It is intended as a resource to inform and assist clinicians in the care of their patients.
Description of the Disease. Lung cancer is the type of cancer characterized by the development of cancerous cells in the lungs of the individual. As the disease progresses, the malignant cells can spread to other body organs. The American Cancer Society places cancer as the third most common cancer and it accounts for 13% of new cancer cases.
Lung cancer is a major cause of mortality and morbidity worldwide. Overall survival has only improved slightly despite advances in surgery, radiotherapy, and chemotherapy. Molecularly targeted agents are currently being studied in all treatment settings including that of chemoprevention, which is defined as the use of natural or synthetic agents to interrupt the process of carcinogenesis and ...
Introduction. Lung cancer is the leading cause of cancer mortality in both men and women with more than 1.8 million deaths a year worldwide. 1 Globally, the five-year net survival for lung cancer is 10% to 20% and is among the lowest of all types of cancer. 2 In 1950, Doll and Hill 3 suggested tobacco smoking and exposure to outdoor pollutants as the two main causes of lung cancer.
Although lung cancer is the leading cause of deaths from cancer in the United States, there remains a chance of survival for patients of it. The survival rate of patients with lung cancer localized in the lungs is 52.6%. Unfortunately, the survival rate of patients with lung cancer that has spread to other organs is only 3.5%.
The 100 most cited articles in lung cancer are listed in Table 1, arranged in descending order according to the number of times cited. The number of citations ranged from 7751 to 889, and the mean number of citations per article was 1879.82 ±1264.78 (range: 7751-889). We found that the most cited article (times cited: 7751) on lung cancer ...
Fish oil-enriched keto diets better for lung nodule prevention. The study found that keto diets, regardless of the type of fats included, were more effective in preventing lung nodules in mice ...
Scientists are making a 'groundbreaking' lung cancer vaccine that could prevent up to 90% of cases. ... Fewer than 10 per cent of people with lung cancer survive their disease for 10 years or more.
The Biology of Cancer. Cancer is a disease that begins with genetic and epigenetic alterations occurring in specific cells, some of which can spread and migrate to other tissues. 4 Although the biological processes affected in carcinogenesis and the evolution of neoplasms are many and widely different, we will focus on 4 aspects that are particularly relevant in tumor biology: genomic and ...
Dr. Eric Winer, director of the Yale Cancer Center, said that with adjuvant chemotherapy, "the hope is that this will prevent further problems" and avoid a recurrence of the cancer.
A plan for the diagnosis and treatment of cancer is a key component of any overall cancer control plan. Its main goal is to cure cancer patients or prolong their life considerably, ensuring a good quality of life. In order for a diagnosis and treatment programme to be effective, it must never be developed in isolation. It needs to be linked to an early detection programme so that cases are ...