- Patient Care & Health Information
- Diseases & Conditions
- Pancreatic cancer
- What is pancreatic cancer? A Mayo Clinic expert explains
Learn more about pancreatic cancer from Mayo Clinic surgical oncologist Chee-Chee Stucky, M.D.
Hi. I'm Dr. Chee-Chee Stucky, a surgical oncologist at Mayo Clinic. In this video, we'll cover the basics of pancreatic cancer: What is it? Who gets it? What are the symptoms, diagnosis and treatment? Whether you're looking for answers for yourself or someone you love, we're here to give you the best information available. Understanding pancreatic cancer starts with understanding the pancreas. This small, fish-shaped organ sits behind the stomach, producing enzymes that aid digestion and hormones that regulate blood sugar. Pancreatic cancer typically starts in the ducts of the pancreas. Small changes in the cellular DNA result in uncontrolled multiplication and accumulation of cells in clusters called tumors. If untreated, these cancer cells can spread outside of the pancreas to other parts of the body.
While anyone can get pancreatic cancer, there are certain risk factors to be aware of. Most pancreatic cancer is diagnosed after age 65. Smoking, diabetes, chronic pancreatitis or inflammation of the pancreas, family history of pancreatic cancer, and certain genetic syndromes are all known risk factors. Carrying extra weight that is unhealthy for your body may also be a contributing factor. New research has found that the specific combination of smoking, diabetes and poor diet increases the risk of pancreatic cancer the most beyond any one factor alone.
Unfortunately, we don't usually see the signs of pancreatic cancer until it's in more advanced stages. When present, symptoms may include: Abdominal pain that radiates to the back. A loss of appetite or unintentional weight loss. Jaundice, which is the yellowing of your skin or eyes. Light colored stools. Dark colored urine. Particularly itchy skin. Diabetes that's becoming unusually difficult to control. Blood clots or fatigue.
If your doctors think you may have pancreatic cancer, they may recommend one or more diagnostic tests. For instance, imaging tests like an ultrasound, CT scan, MRI, or PET scan, can help your doctor see a clearer picture of your internal organs. An endoscopic ultrasound, or EUS, is when the doctor passes a tiny camera down the esophagus and into the stomach to get a close-up view of the pancreas. During the EUS, the doctor might collect a biopsy of the tissue for further testing. Sometimes pancreatic cancer can shed specific proteins called tumor markers in your blood. So your doctors may request blood tests to identify elevation of these markers, one of which is called CA 19-9. If a diagnosis is confirmed, the next step is to determine the extent or stage of the cancer. The stages are numbered one through four and may need to be determined by additional testing. Feel free to ask lots of questions during this process. Or get a second opinion to feel the most confident and empowered moving into treatment.
When recommending treatment for pancreatic cancer, your doctor is considering many factors, including your overall health and personal preferences. They may recommend one or a combination of the following treatments: Chemotherapy uses drugs that release chemicals that enter the body and kill cancerous cells that may be throughout. Radiation, similarly kills the cancer cells, but with high-energy beams directed at the tumor. Surgery is used to physically remove the cancer and the immediate surrounding area. Ask your doctor if you qualify for clinical trials that test new treatments. And lastly, there is palliative care. This care is provided by a team of doctors, nurses, social workers, and other trained professionals who specialize in providing much needed relief from the pain and unpleasant symptoms of a serious illness.
Getting diagnosed with a life-threatening illness can be devastating to both the patient and their loved ones. But we have some of the following suggestions that may help patients cope: Learn about your condition. Knowledge is power and information can make you feel more confident in your treatment decisions. Find support. This can mean a support system of family and friends, a cancer support group of people going through the same experience, or qualified counselor like your therapist or religious leader. Lean on those around you when you're feeling helpless, overwhelmed, or uncertain. You may want to consider hospice care, which provides comfort and support to terminally ill patients and their loved ones. If you'd like to learn even more about pancreatic cancer, watch our other related videos or visit mayoclinic.org. We wish you well.
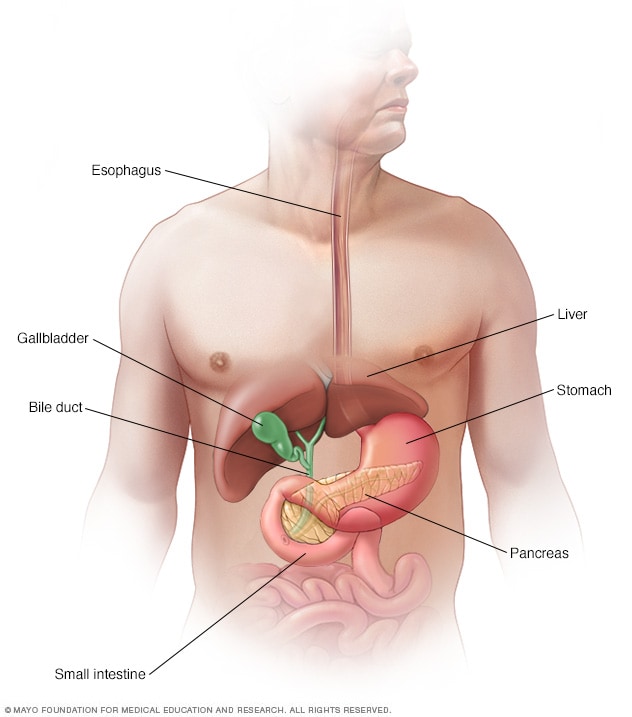

The pancreas in the digestive system
The pancreas is a long, flat gland that lies horizontally behind your stomach. It has a role in digestion and in regulating the level of sugar in your blood.
Pancreatic cancer is cancer that forms in the cells of the pancreas.
Pancreatic cancer is a type of cancer that begins as a growth of cells in the pancreas. The pancreas lies behind the lower part of the stomach. It makes enzymes that help digest food and hormones that help manage blood sugar.
The most common type of pancreatic cancer is pancreatic ductal adenocarcinoma. This type begins in the cells that line the ducts that carry digestive enzymes out of the pancreas.
Pancreatic cancer rarely is found at its early stages when the chance of curing it is greatest. This is because it often doesn't cause symptoms until after it has spread to other organs.
Your health care team considers the extent of your pancreatic cancer when creating your treatment plan. Treatment options may include surgery, chemotherapy, radiation therapy or a mix of these.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- A Book: Mayo Clinic on Digestive Health
- Assortment of Pill Aids from Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Pancreatic cancer often doesn't cause symptoms until the disease is advanced. When they happen, signs and symptoms of pancreatic cancer may include:
- Belly pain that spreads to the sides or back.
- Loss of appetite.
- Weight loss.
- Yellowing of the skin and the whites of the eyes, called jaundice.
- Light-colored or floating stools.
- Dark-colored urine.
- New diagnosis of diabetes or diabetes that's getting harder to control.
- Pain and swelling in an arm or leg, which might be caused by a blood clot.
- Tiredness or weakness.
When to see a doctor
Make an appointment with a health care professional if you have symptoms that worry you.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
Get Mayo Clinic cancer expertise delivered to your inbox.
Subscribe for free and receive an in-depth guide to coping with cancer, plus helpful information on how to get a second opinion. You can unsubscribe at any time. Click here for an email preview.
Error Select a topic
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing
Your in-depth coping with cancer guide will be in your inbox shortly. You will also receive emails from Mayo Clinic on the latest about cancer news, research, and care.
If you don’t receive our email within 5 minutes, check your SPAM folder, then contact us at [email protected] .
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
It's not clear what causes pancreatic cancer. Doctors have found some factors that might raise the risk of this type of cancer. These include smoking and having a family history of pancreatic cancer.
Understanding the pancreas
The pancreas is about 6 inches (15 centimeters) long and looks something like a pear lying on its side. It releases hormones, including insulin. These hormones help the body process the sugar in the foods you eat. The pancreas also makes digestive juices to help the body digest food and take in nutrients.
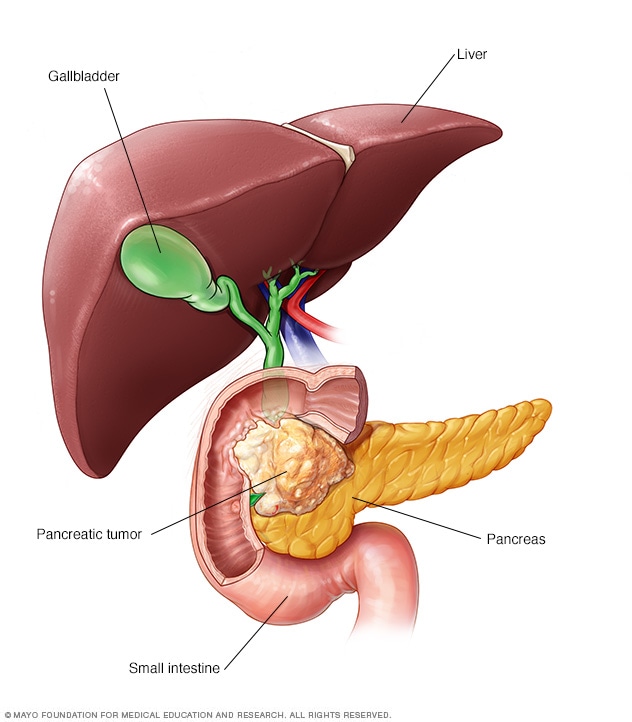
How pancreatic cancer forms
Pancreatic cancer happens when cells in the pancreas develop changes in their DNA. A cell's DNA holds the instructions that tell a cell what to do. In healthy cells, the instructions tell the cells to grow and multiply at a set rate. The cells die at a set time. In cancer cells, the changes give different instructions. The changes tell the cancer cells to make many more cells quickly. Cancer cells can keep living when healthy cells would die. This causes there to be too many cells.
The cancer cells might form a mass called a tumor. The tumor can grow to invade and destroy healthy body tissue. In time, cancer cells can break away and spread to other parts of the body.
Most pancreatic cancer begins in the cells that line the ducts of the pancreas. This type of cancer is called pancreatic ductal adenocarcinoma or pancreatic exocrine cancer. Less often, cancer can form in the hormone-producing cells or the neuroendocrine cells of the pancreas. These types of cancer are called pancreatic neuroendocrine tumors or pancreatic endocrine cancer.
Risk factors
Factors that might raise the risk of pancreatic cancer include:
- Type 2 diabetes.
- Chronic inflammation of the pancreas, called pancreatitis.
- Family history of DNA changes that can increase cancer risk. These include changes in the BRCA2 gene, Lynch syndrome and familial atypical multiple mole melanoma (FAMMM) syndrome.
- Family history of pancreatic cancer.
- Older age. Most people with pancreatic cancer are over 65.
- Drinking a lot of alcohol.
Complications
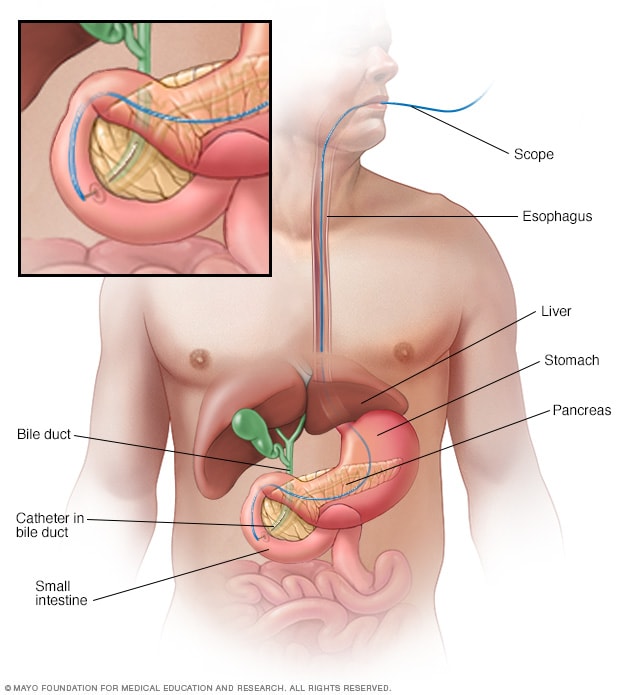
Endoscopic retrograde cholangiopancreatography
Endoscopic retrograde cholangiopancreatography (ERCP) uses a dye to highlight the bile ducts and pancreatic duct on X-ray images. A thin, flexible tube with a camera on the end, called an endoscope, is passed down your throat and into your small intestine. The dye enters the ducts through a small hollow tube, called a catheter, passed through the endoscope. Tiny tools passed through the catheter also can be used to remove gallstones.
As pancreatic cancer progresses, it can cause complications such as:
- Weight loss. People with pancreatic cancer might lose weight as the cancer uses more of the body's energy. Nausea and vomiting caused by cancer treatments or a cancer pressing on the stomach might make it hard to eat. Sometimes the body has trouble getting nutrients from food because the pancreas isn't making enough digestive juices.
Jaundice. Pancreatic cancer that blocks the liver's bile duct can cause jaundice. Signs include yellowing of the skin and the whites of the eyes. Jaundice can cause dark-colored urine and pale-colored stools. Jaundice often occurs without belly pain.
If the bile duct is blocked, a plastic or metal tube called a stent can be put inside it. The stent helps hold the bile duct open. This is done using a procedure called endoscopic retrograde cholangiopancreatography, also called ERCP.
During ERCP , a health care professional puts a long tube with a tiny camera, called an endoscope, down the throat. The tube goes through the stomach and into the upper part of the small intestine. The health professional puts a dye into the pancreatic ducts and bile ducts through a small tube that fits through the endoscope. The dye helps the ducts show up on imaging tests. The health professional uses those images to place a stent at the right spot in the duct to help hold it open.
Pain. A growing tumor may press on nerves in your abdomen, causing pain that can become severe. Pain medications can help you feel more comfortable. Treatments, such as radiation and chemotherapy, might help slow tumor growth and provide some pain relief.
When medicines aren't helping, a health care professional might suggest a celiac plexus block. This procedure uses a needle to put alcohol into the nerves that control pain in the belly. The alcohol stops the nerves from sending pain signals to the brain.
Bowel blockage. Pancreatic cancer can grow into or press on the first part of the small intestine, called the duodenum. This can block the flow of digested food from the stomach into the intestines.
A health care professional might suggest putting a tube called a stent in the small intestine to hold it open. Sometimes, it might help to have surgery to place a feeding tube. Or surgery can attach the stomach to a lower part of the intestines where the cancer isn't causing a blockage.
Screening for people with a high risk of pancreatic cancer
Screening uses tests to look for signs of pancreatic cancer in people who don't have symptoms. It might be an option if you have a very high risk of pancreatic cancer. Your risk might be high if you have a strong family history of pancreatic cancer or if you have an inherited DNA change that increases the risk of cancer.
Pancreatic cancer screening might involve imaging tests, such as MRI and ultrasound. These tests are generally repeated every year.
The goal of screening is to find pancreatic cancer when it's small and most likely to be cured. Research is ongoing, so it's not yet clear whether screening can lower the risk of dying of pancreatic cancer. There are risks to screening. This includes the chance of finding something that requires surgery but later turns out to not be cancer.
Talk about the benefits and risks of pancreatic cancer screening with your health care team. Together you can decide whether screening is right for you.
Genetic testing for cancer risk
If you have a family history of pancreatic cancer, discuss it with a health care professional. The health professional can review your family history and help you understand whether genetic testing might be right for you.
Genetic testing can find DNA changes that run in families and increase the risk of cancer. If you're interested in genetic testing, you might be referred to a genetic counselor or other health care professional trained in genetics.
Ways to lower risk
You might reduce your risk of pancreatic cancer if you:
- Stop smoking. If you smoke, talk to a member of your health care team about ways to help you stop. These might include support groups, medicines and nicotine replacement therapy.
- Maintain a healthy weight. If you are at a healthy weight, work to maintain it. If you need to lose weight, aim for a slow, steady weight loss of 1 to 2 pounds (0.5 to 1 kilogram) a week. To help you lose weight, exercise most days of the week. Slowly increase the amount of exercise you get. Choose a diet rich in vegetables, fruit and whole grains with smaller portions.
Pancreatic cancer care at Mayo Clinic
Living with pancreatic cancer?
Connect with others like you for support and answers to your questions in the Pancreatic Cancer support group on Mayo Clinic Connect, a patient community.
Pancreatic Cancer Discussions

1117 Replies Sat, Apr 06, 2024

144 Replies Sat, Apr 06, 2024

12 Replies Wed, Apr 03, 2024
- AskMayoExpert. Pancreatic cancer (adult). Mayo Clinic; 2022.
- Groggins M, et al. Management of patients with increased risk for familial pancreatic cancer: Updated recommendations from the International Cancer of the Pancrease Screening (CAPS) Consortium. Gut. 2020; doi:10.1136/gutjnl- 2019- 319352.
- Debouk M, et al. The Multicenter Cancer of Pancreas screening study: Impact on stage and survival. Journal of Clinical Oncology. 2022; doi:10.1200/JCO.22.00298.
- Pancreatic adenocarcinoma. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1455. Accessed April 27, 2023.
- De la Fuente J, et al. How I approach screening for pancreatic cancer. American Journal of Gastroenterology. 2021; doi:10.14309/ajg.0000000000001305.
- Fernandez-del Castillo C. Clinical manifestations, diagnosis and staging of exocrine pancreatic cancer. https://www.uptodate.com/contents/search. Accessed April 26, 2023.
- Pancreatic cancer treatment (PDQ) — Health professional version. National Cancer Institute. https://www.cancer.gov/types/pancreatic/hp/pancreatic-treatment-pdq. Accessed April 26, 2023.
- Distress management. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1455 Accessed April 27, 2023.
- Ryan DP. Initial systemic chemotherapy for metastatic exocrine pancreatic cancer. https://www.uptodate.com/contents/search. Accessed April 26, 2023.
- AskMayoExpert. Pancreas ductal adenocarcinoma: Diagnosis and treatment (adult). Mayo Clinic; 2022.
- Fernandez-del Castillo C, et al. Overview of surgery in the treatment of exocrine pancreatic cancer and prognosis. https://www.uptodate.com/contents/search. Accessed April 26, 2023.
- NPF Centers of Excellence. National Pancreas Foundation. https://pancreasfoundation.org/patient-resources/npf-centers-of-excellence/. Accessed April 27, 2023.
- Niederhuber JE, et al., eds. Carcinoma of the pancreas. In: Abeloff's Clinical Oncology. 6th ed. Elsevier; 2020. http://www.clinicalkey.com. Accessed April 28, 2023.
- Sugumar A, et al. Distinguishing pancreatic cancer from autoimmune pancreatitis. Current Gastroenterology Reports. 2010;12:91.
- Ami T. Allscripts EPSi. Mayo Clinic. Feb. 28, 2022.
- Pancreatic Cancer Genetic Epidemiology (PACGENE) Study. ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT00526578. Accessed April 26, 2023.
- Thind K et al. Immunotherapy in pancreatic cancer treatment: A new frontier. Therapeutic Advances in Gastroenterology. 2017;10:168.
- Tee MC, et al. Laparoscopic pancreaticoduodenectomy: Is it an effective procedure for pancreatic ductal adenocarcinoma? Advances in Surgery. 2015;49:143.
- Merrell KW, et al. Predictors of locoregional failure and impact on overall survival in patients with resected exocrine pancreatic cancer. International Journal of Radiation Oncology. 2016;doi:10.1016/j.ijrobp.2015.11.003.
- Moris M, et al. Risk factors for malignant progression of intraductal papillary mucinous neoplasms. Digestive and Liver Disease. 2015;47:495.
- Pancreatic cancer: Symptoms and signs. Cancer.Net. https://www.cancer.net/cancer-types/pancreatic-cancer/symtpms-and-signs. Accessed May 2, 2023.
- Loncle C, et al. The pancreatitis-associated protein VMP1, a key regulator of inducible autophagy, promotes KRAS-G12D-mediated pancreatic cancer initiation. Cell Death and Disease. 2016;7:32295.
- Thiels CA, et al. Outcomes of pancreaticoduodenectomy for pancreatic neuroendocrine tumors: Are combined procedures justified? Journal of Gastrointestinal Surgery. 2016;20:891.
- Dr. Mark Truty (surgery, MN) better outcomes with chemo
- Dr. Wallace Video
- Infographic: Pancreatic Cancer: Minimally Invasive Surgery
- Infographic: Pancreatic Cancers-Whipple
- Pancreatic Cancer Survivor
- Pancreatic ultrasound
- Whipple procedure
Associated Procedures
- Chemotherapy
- Endoscopic ultrasound
- Integrative medicine
- Needle biopsy
- Palliative care
- Positron emission tomography scan
- Proton therapy
- Radiation therapy
News from Mayo Clinic
- Researchers make unexpected discovery in how pancreatic cancer spreads Dec. 15, 2023, 03:00 p.m. CDT
- Mayo Clinic's AI innovation inspires hope in early detection of pancreatic cancer Oct. 02, 2023, 03:25 p.m. CDT
- Long-term pancreatic cancer survivors report excellent post-surgery quality of life Aug. 28, 2023, 01:30 p.m. CDT
- Staging pancreatic cancer early with minimally invasive surgery shows positive results in patient prognosis, Mayo Clinic study finds June 29, 2023, 05:16 p.m. CDT
- Mayo Clinic to lead new radiotracer trial for detecting pancreatic cancer Jan. 30, 2023, 05:55 p.m. CDT
- Helpful guidelines if you test positive or negative for COVID-19 Nov. 30, 2022, 05:00 p.m. CDT
- Identifying inherited gene mutations in pancreatic cancer can lead to targeted therapies, better survival Nov. 24, 2022, 03:30 p.m. CDT
- 5 things to know about pancreatic cancer Nov. 18, 2022, 05:00 p.m. CDT
- Mayo Clinic Q and A: Pancreatic cancer risk, symptoms and treatment Nov. 10, 2022, 04:00 p.m. CDT
- Advances in treating pancreatic cancer mean options and hope--2022 Nov. 01, 2022, 04:30 p.m. CDT
- Mayo Clinic Researchers ID Potential Gene Marker for Treating Pancreatic Cancer Sept. 22, 2022, 04:08 p.m. CDT
- AI applied to prediagnostic CTs may help diagnose pancreatic cancer at earlier, more treatable stage July 14, 2022, 02:01 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

- Adolescent and Young Adult Cancer
- Bile Duct Cancer
- Bladder Cancer
- Brain Cancer
- Breast Cancer
- Cervical Cancer
- Childhood Cancer
- Colorectal Cancer
- Endometrial Cancer
- Esophageal Cancer
- Head and Neck Cancer
- Kidney Cancer
- Liver Cancer
- Lung Cancer
- Mouth Cancer
- Mesothelioma
- Multiple Myeloma
- Neuroendocrine Tumors
- Ovarian Cancer
- Pancreatic Cancer
- Prostate Cancer
- Skin Cancer/Melanoma
- Stomach Cancer
- Testicular Cancer
- Throat Cancer
- Thyroid Cancer
- Prevention and Screening
- Diagnosis and Treatment
- Research and Clinical Trials
- Survivorship

Request an appointment at Mayo Clinic

People with pancreatic cancer are living longer, thanks to improved approaches
Share this:.
By Jessica Saenz
A diagnosis of pancreatic cancer is almost synonymous with hopelessness. As the least survivable type of cancer, the perception is understandable. "As soon as patients were diagnosed, they were often told by their physician to start making arrangements," says Mark Truty, M.D. , a surgical oncologist at Mayo Clinic who specializes in pancreatic surgery.
But the tides are turning, thanks to new and improved treatment methods that are helping people with pancreatic cancer live longer. Dr. Truty and Robert McWilliams, M.D. , a medical oncologist at Mayo Clinic, talk about Mayo Clinic's approach to pancreatic cancer care , and how it's leading to improved survival and quality of life.
Capturing the full picture from the time of diagnosis and beyond
Before moving forward with treatment, Dr. Truty says it's critical to understand as much about each person's cancer as possible. "When a patient is first diagnosed, they need really good imaging and molecular testing to see, not just where the tumor is, but if there's any evidence of spread. We do a lot of tests at the beginning and throughout to make sure that the cancer is truly localized and has not spread."
In most instances, a CT scan or MRI scan is used to identify the location of the cancer and possible spread, but Dr. Truty says standard scans are just one piece of the puzzle. "Historically, patients have gotten a scan where the tumor appears to be localized, and then they underwent surgery. But that paradigm has not resulted in the outcomes we wanted."
This is where PET scans and additional molecular testing play an important role.
Dr. Truty says that PET scans and newer genetic testing are key to staging the cancer and assessing its behavior accurately. They can help determine if treatment is working effectively to shrink the tumor, whereas traditional CT scans have distinct limitations in assessing response in pancreatic primary tumors. "If we see a response we’re anticipating on the PET scan, those are the patients that do very well. If we're not seeing a response, then we have to pivot and switch their therapy to see if we can achieve a better outcome," he says. "We've also been using novel genetic testing developed at Mayo Clinic to test the blood of patients, as well as the fluid of the abdomen through laparoscopy , to see if we can pick up some cancer DNA."
This method is helping cancer experts at Mayo Clinic determine who might be at risk for pancreatic cancer recurrence and individualize their treatment to reduce the risk of the cancer returning. "We're the first center to do this routinely for every single patient we see," Dr. Truty says.
Tailoring testing and treatment for each person
Initial testing and staging of pancreatic cancer can help uncover weaknesses or potential threats for each unique pancreatic cancer case. "As we've learned more about the genetics of pancreatic cancer — and how to find patients who can benefit — we've been able to tailor therapies according to the patient's genetics and their DNA, or the DNA changes that are specific to the cancer itself," says Dr. McWilliams.
In a study led by Mayo Clinic Center for Individualized Medicine , researchers found that nearly 1 in 6 people diagnosed with pancreatic cancer had an inherited cancer-related gene mutation that may have predisposed them to pancreatic cancer. The most common genetic mutation in those patients was the BRCA2 gene, which is linked to breast cancer.
Niloy Jewel Samadder, M.D. , a Mayo Clinic gastroenterologist and hepatologist, and the study's senior author, said that patients with mutations had a 50% longer survival. Data from this study and others have led to recent changes in guidelines that advocate for genetic testing for all pancreatic cancer patients, regardless of their cancer stage or family history of cancer.
Though the majority of people with pancreatic cancer do not have a germline mutation, Dr. McWilliams says it's important to use all the tools available for each patient. While it may not achieve a cure, it can help select therapies to improve quality of life so patients can live longer and more comfortably.
"There's a national trial, called the POLO Trial , which showed that patients on chemotherapy with BRCA1 or BRCA2 mutations are eligible for a maintenance therapy with just a pill, rather than IV chemotherapy, which is really good from a side effects standpoint," says Dr. McWilliams.
Redefining what is considered inoperable
Dr. Truty says patients who are able to have surgery to remove their pancreatic cancer can live significantly longer, but in cases where the tumor has grown outside of the pancreas to encase critical blood vessels, pancreatic cancer has been considered inoperable.
About one-third of pancreatic cancer tumors grow to surround blood vessels outside the pancreas. "Those patients have historically not been considered for surgery," he says. "Theoretically, 50% of patients with diagnosed pancreatic cancer have the potential to undergo an operation. The question is: How do we get them to surgery? And how do we optimize their outcomes to make sure that they live as long as they possibly can?"
Drs. Truty, McWilliams and pancreatic cancer experts at Mayo Clinic use an approach called neoadjuvant therapy, which delivers chemotherapy — or a combination of chemotherapy and radiation — to destroy microscopic cancer cells in the body before surgery. By combining this method with personalized surgery for each patient's anatomy, they can remove tumors entirely and reconstruct blood vessels as needed. This has resulted in the ability to operate on patients who previously did not have that option, leading to better results than ever before.
"We're creating custom surgeries for each patient that aren't being done anywhere else on the planet. That's why so many people come to us after they've been told their tumors are inoperable," says Dr. Truty.
Though surgery can lead to the best outcomes in many cases, Dr. Truty emphasizes that the goal of pancreatic cancer treatment is not surgery. "The goal for anyone with cancer is to extend their life and maintain a reasonable quality of life. Sometimes an operation is necessary to achieve this, and sometimes it will decrease the likelihood of one or the other, or both. That's why before we even consider an operation, we have to make sure that operation has the highest probability that we'll achieve both of those goals."
Pancreatic cancer continues to have the highest mortality rate, but Dr. McWilliams says there's plenty of reason for patients to be hopeful. "It's a very serious cancer. It's something that is life-threatening for a lot of people, but it's not necessarily a death sentence," he says. "It's something that we have treatments for, and our treatments are only getting better."
And this progress, he says, is driven by clinical trials. "Clinical trials are how we advance the science. For patients who are looking for the latest and greatest, and want to help advance the options for their cancer, participation in clinical trials is crucial."
Dr. Truty says he hopes more people with pancreatic cancer seek out second opinions from cancer centers who are leveraging new approaches and providing patients more options. "Historically, it's been such a nihilistic disease, but things have really changed. We have not settled for the standard of care — this results in standard outcomes which have not been good. We have to treat patients differently — starting from the beginning," he says. "And if you can do that all the way through treatment, then those patients really do have exceptional outcomes."
Learn more about panc r eatic cancer and find a pancreatic cancer clinical trial at Mayo Clinic.
Read these articles:
- " 5 things to know about pancreatic cancer "
- " PET/MRI biomarkers guide personalized treatment for people with pancreatic cancer, study finds "
- " Identifying inherited gene mutations in pancreatic cancer can lead to targeted therapies, better survival "
- " Aggressive Approach to Pancreatic Cancer Yields Outstanding Outcome "
Also watch this video: " Mayo Clinic Minute: Advances in pancreatic cancer treatment extending lives
Related Posts

They identified a cell-signaling protein that drives pancreatic cancer cell growth that could be a potential therapeutic target.

Researchers built a highly accurate artificial intelligence model for fully automated cancer detection, including small and otherwise difficult-to-detect tumors.

Rita Krueger shares the lessons she has learned from her experience with pancreatic cancer diagnosis, treatment and survivorship.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 29 June 2021
Advancing on pancreatic cancer
Nature Reviews Gastroenterology & Hepatology volume 18 , page 447 ( 2021 ) Cite this article
7774 Accesses
13 Citations
9 Altmetric
Metrics details
- Pancreatic cancer
Pancreatic cancer is a notoriously lethal condition characterised by aggressive malignancy and dismal outcomes. However, translational advances are showing us that hope is on the horizon.
The global burden of pancreatic ductal adenocarcinoma (PDAC), the most common form of pancreatic cancer, has doubled in the last quarter century and is projected to be the second leading cause of cancer deaths in the USA in the next 20–30 years 1 . Outcomes in PDAC make for grim reading: 5-year survival has only just reached double digits in some regions 2 ; current chemotherapeutics lead to survival in the range of months; and ~50% of new diagnoses are the metastatic form of PDAC, with an average survival of less than a year 1 . Such bleak statistics are driven by a disease that often has non-specific symptoms until it is too late; most diagnoses are made once the opportunity for surgical intervention has passed.
Despite this situation, there are reasons to be hopeful. Research investment in pancreatic cancer in the USA has increased more than any other cancer site, driving cutting-edge translational research that aims to enhance strategies towards PDAC detection and treatment 3 . In this Focus Issue of Nature Reviews Gastroenterology & Hepatology , we provide an overview of some of these advances in a series of Reviews and commentaries, which are also available online in a Collection . Each of these articles features a different aspect of PDAC that highlights the inherent challenges of the disease, but each also reveals how advancements are paving the way for improved patient care.
A key feature of the PDAC microenvironment is its dense, hypoxic and immunosuppressive stroma that limits infiltration by immune cells and therapeutics. Adding to our understanding of the mechanisms underlying the stroma, Encarnación-Rosado and Kimmelman explain how it mediates a reprogramming of PDAC metabolism to facilitate tumour survival. By understanding how metabolism is rewired in PDAC and by identifying the metabolic dependencies, new strategies for targeted therapeutic interventions could be revealed.
PDAC is one of the most aggressive and chemoresistant forms of cancer, largely due to the diversity of genetic mutations that give rise to a highly heterogenic disease. Hayashi, Hong and Iacobuzio-Donahue examine the PDAC genome and discuss how our understanding has advanced beyond the common driver genes and major hereditary components. By examining genomic PDAC studies in the context of its cellular origins and evolutionary growth dynamics, they show how distinct genomic events are associated with phenotypes that indicate therapeutic vulnerabilities.
The low prevalence of PDAC in the general population presents further challenges towards a feasible, cost-effective solution to population screening. In their Review, Klein summarises the epidemiology of pancreatic cancer, including modifiable risk factors as well as those that could help identify high-risk individuals and focus screening procedures. Other efforts aiming to improve detection of the disease early in its natural history are detailed by Singhi and Wood . They discuss the precursor lesions of pancreatic cancer and approaches and challenges to their early detection using DNA-based molecular techniques, which demonstrate the promise of technology for overcoming the fundamental problem of late presentation in PDAC.
Another technological advancement, single-cell RNA sequencing, forms the basis of a Comment by Han, DePinho and Maitra . The authors explore how in-depth cellular profiling in PDAC has furthered our understanding of the molecular underpinnings of the disease but also the potential mechanisms responsible for therapeutic resistance. A final reason to be hopeful comes in the form of immunotherapy. Although this field seems poised to revolutionise cancer treatment, PDAC is known to be resistant to many current approaches. However, as discussed in a Comment by Rojas and Balachandran , promising strategies to unlock the potential of immunotherapy in PDAC are underway.
There is encouraging progress towards improving the lives of patients and families affected by PDAC
There is encouraging progress towards improving the lives of patients and families affected by PDAC. However, more investment in both data repositories such as biobanks and high-visibility research is urgently needed, particularly in Europe where pancreatic cancer is relatively neglected 4 despite the increasing burden. Improved awareness of the early signs and risk factors of PDAC will be crucial to increase early diagnosis, as will coordinated cooperation between academia, patient organisations, scientific societies and advocacy groups. Leveraging these stakeholders will be critical in maintaining the momentum needed to translate these hopeful advances to the clinic, where their benefits can be seen.
Mizrahi, J. D. et al. Pancreatic cancer. Lancet 395 , 2008–2020 (2020).
Article CAS Google Scholar
Siegel, A. et al. Cancer Statistics, 2021. CA: a cancer journal for clinicians 71 , 7–33 (2021).
Google Scholar
Abudu, R. Trends in International Cancer Research Investment 2006-2018. JCO Glob. Oncol. 7 , 602–610 (2021).
Article Google Scholar
Prades, J. et al. Bratislava Statement: consensus recommendations for improving pancreatic cancer care. ESMO Open 5 , e001051 (2020).
Download references
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Advancing on pancreatic cancer. Nat Rev Gastroenterol Hepatol 18 , 447 (2021). https://doi.org/10.1038/s41575-021-00479-5
Download citation
Published : 29 June 2021
Issue Date : July 2021
DOI : https://doi.org/10.1038/s41575-021-00479-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Autophagy inhibition improves the targeted radionuclide therapy efficacy of 131i-fap-2286 in pancreatic cancer xenografts.
- Jianming Cai
Journal of Translational Medicine (2024)
SMAD4 endows TGF-β1-induced highly invasive tumor cells with ferroptosis vulnerability in pancreatic cancer
- Hai-di Chen
Acta Pharmacologica Sinica (2024)
KIF15 is essential for USP10-mediated PGK1 deubiquitination during the glycolysis of pancreatic cancer
- Jianxin Jiang
Cell Death & Disease (2023)
Cost-effectiveness of open pancreaticoduodenectomy with or without Heidelberg TRIANGLE operation for pancreatic cancer in China
- Mengdie Zhang
- Haixia Ding
Journal of Cancer Research and Clinical Oncology (2023)
Analysis of cuproptosis-related lncRNA signature for predicting prognosis and tumor immune microenvironment in pancreatic cancer
- Hong-Fei Yao
- Jun-Feng Zhang
Apoptosis (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Open access
- Published: 07 December 2022
Landmarks in pancreatic cancer studies
- Min Huang 2 ,
- Yun Bai 1 ,
- Xueshi Yin 3 ,
- Jingzhe Yan 4 ,
- Fangfang Liu 5 ,
- Jie Chen 6 , 7 &
- Xiechuan Weng 8
Cancer Cell International volume 22 , Article number: 383 ( 2022 ) Cite this article
2629 Accesses
1 Citations
8 Altmetric
Metrics details
Pancreatic cancer is a rare but fatal disease. Patients present advanced disease due to the lack of or typical symptoms when the tumor is still localized. A high-quality image processing system has been in practice to detect the pancreatic tumor and determine the possibility of surgery, and preoperative methods, such as ERCP are increasingly used to complement the staging modality. Pancreaticoduodenectomy is one of the complicated surgeries with potential morbidity. The minimally invasive pancreatic resections, both robot-assisted and laparoscopic, have become a part of standard surgical practice worldwide over the last decade. Moreover, advancements in adjuvant chemotherapy have improved the long-term outcomes in current clinical practice. The systemic conservative treatment, including targeted agents, remains the mainstay of treatment for patients with advanced disease. An increasing number of studies are focused on modulating the pancreatic tumor microenvironment to improve the efficacy of the immunotherapeutic strategies. Herein, the role of preoperative therapy, the novel surgical strategy, and individualized systemic treatment in pancreatic cancer is investigated. Also, the randomized controlled studies that have defined the neoadjuvant and surgical management of pancreatic cancer have been summarized.
Introduction
Pancreatic cancer is an intractable digestive system malignancy. Based on GLOBOCAN 2020 estimate [ 1 ], pancreatic cancer accounts for almost as many deaths (466,000) as cases (496,000). It is the seventh leading cause of cancer deaths in both sexes. A study of 28 European countries showed that because the rates of pancreatic cancer are stable relative to the declining rates of breast cancer, pancreatic cancer will surpass breast cancer as the third leading cause of cancer deaths by 2025 [ 2 ]. The survival rates for pancreatic cancer are extremely low, despite improvements in the overall 5-year survival from < 5% (1990s) to about 9% (2019) in the USA and Europe. The low survival rates could be partially attributed to the advanced stage at diagnosis in most cases, with only 20% of patients presenting early-stage, surgically resectable disease [ 3 ].
Data from China Pancreatic Disease Big Data Center showed that pancreatic cancer has three characteristics: low early diagnosis rate, low surgical resection rate, and low drug efficiency. In addition, it imposes a huge financial burden on the family and society. Cerullo et al. assessed the financial burden associated with the treatment options for resectable pancreatic cancer and reported that the median cumulative cost of gemcitabine with nab-paclitaxel was $74,051 (interquartile range: $38,929–$133,603) [ 4 ]. The cause of pancreatic cancer is complex and multifactorial, and an unhealthy lifestyle increases the incidence of the disease. Nonetheless, smoking remains a major cause of pancreatic cancer. Also, increased rates of diabetes and obesity may contribute to the high rates of pancreatic cancer [ 3 ]. Accumulating evidence suggested that heavy drinking increases the risk of pancreatic cancer [ 5 , 6 ]. The genetic factors might explain 22–33% predisposition to the risk of pancreatic cancer risk [ 3 ].
This review outlines the current progress in pancreatic cancer in terms of the conservative treatment strategy, including immunotherapy and elucidates the immune cell modulation in tumor progression and surgical development for cancer treatment.
Hallmarks of the histological and molecular characteristics
Histological.
Pancreatic tumors include cancers that arise from the endocrine or exocrine components of the pancreas with pancreatic adenocarcinoma. Most pancreatic cancers are pancreatic ductal adenocarcinomas (PDACs) (> 90%) [ 7 ]. PDAC is characterized by invasive, widely separated small tubular (ductal) structures embedded in fibroinflammatory (desmoplastic) stroma, which creates a scirrhous ill-defined lesion that renders difficulty in distinguishing PDAC from chronic pancreatitis both radiologically and pathologically. The infiltration pattern is characteristically subtle, which does not allow the formation of a well-defined mass; however, a highly insidious infiltration leads to peritoneal carcinomatosis with numerous small clusters, whereas the primary tumor may be small.
Nonetheless, it should be remembered that there is an array of other cancer types that occur in the pancreas. These cancers are classified by their cellular lineage: acinar cell carcinomas (acinar differentiation), neuroendocrine neoplasms (arising from the islets), solid-pseudopapillary neoplasms (showing no discernible cell lineage), and pancreatoblastomas (characterized by multiphenotypic differentiation, including acinar endocrine and ductal). Mesenchymal neoplasms, such as gastrointestinal stromal tumors and lymphomas, also occur in the pancreas [ 8 ].
In patients with hereditary germline and spontaneous somatic mutations, the pathogenesis of pancreatic cancer is well-defined in terms of precursor lesions that include pancreatic intraepithelial neoplasia (PanIN), intraductal papillary mucinous neoplasm (IPMN), and mucinous cystic neoplasm (MCN) [ 9 ].
Molecular classification
Historically, pancreatic cancer was viewed as a single disease entity; however, it became clear that similar to other malignancies, such as breast cancer, it is molecularly diverse, and treatments are tailored to the biology of the tumor. The first landmark study to assess the global pancreatic cancer genome pattern was published in 2008, which included a genetic analysis of 24 patients with advanced pancreatic cancer and found that pancreatic cancer contained > 60 genetic changes, equivalent to disruptions in 12 core cell signaling pathways. The study confirms the genetic diversity of pancreatic cancer and lays the foundation for future research [ 10 ]. Advances in sequencing technology in recent years have greatly improved our understanding of pancreatic cancer at the molecular level.
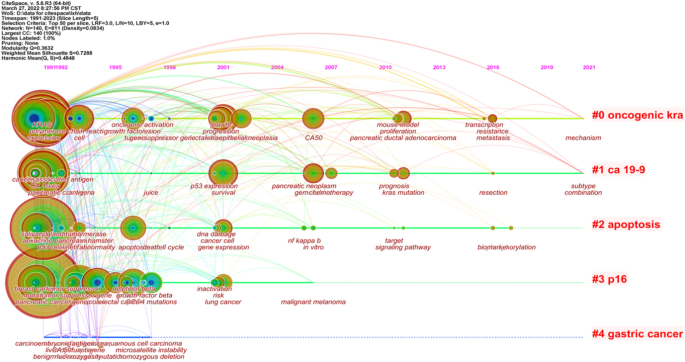
Collisson et al. [ 11 ] analyzed the transcriptional profiles of primary PDAC samples from several studies along with human and mouse PDAC cell lines and defined three subtypes, including classical, quasi-mesenchymal, and exocrine-like, according to specific gene expression. In addition, the study found that two genes associated with subtypes, GATA binding protein 6 ( GATA6 ) and v-ki-ras2 kirsten rat sarcoma viral oncogene homolog ( KRAS ), implicated in both aspects of normal development and cancer pathophysiology (Fig. 1 ).
General genes in studies of pancreatic cancer
Pancreatic cancer is mesenchymal-rich, which makes capturing precise tumor-specific molecular information challenging [ 12 ]. Moffitt et al. have overcome this problem by applying blind source separation to diverse PDAC gene expression microarray data from primary, metastatic, and normal samples. A total of 50 genes related to the development of pancreatic cancer were screened based on tumor epithelial tissue and classified into two tumor-specific subtypes, including classical and basal-like, that have poor outcomes and are molecularly similar to basal tumors in bladder and breast cancers. Furthermore, 48 genes related to the development of PDAC were extracted from tumor stroma and defined as normal and activated stromal subtypes, which are independently prognostic.
Bailey et al. [ 13 ] performed whole-gene sequencing analysis on 456 pancreatic cancer samples. A total of 32 important cyclic mutation motifs and 10 key genetic signaling pathways were identified: KRAS , TGF-β , WNT , NOTCH , ROBO/SLIT signaling, G1/S transition, SWI-SNF , chromatin modification, DNA repair, and RNA processing. The expression analysis defined four subtypes, including squamous, pancreatic progenitor, immunogenic, and aberrantly differentiated endocrine-exocrine (ADEX). Squamous tumors are enriched in TP53 and KDM6A mutations and have a poor prognosis. Pancreatic progenitor tumors expressed genes involved in early pancreatic development ( FOXA2/3 , PDX1 , and MNX1 ). Immunogenic tumors consisted of upregulated immune networks, including acquired immune suppression pathways. ADEX tumors displayed upregulation of genes that regulate networks involved in KRAS activation, exocrine ( NR5A2 and RBPJL ), and endocrine differentiation ( NEUROD1 and NKX2-2 ). The comprehensive evolution landmarks of genetic discovery in pancreatic cancer are displayed in Fig. 1 .
The comparison of different genotypes revealed that 37/62 tumor cell genes analyzed by Collisson et al. and 32/50 tumor cell genes analyzed by Moffitt et al. comprised 707 tumor cell genes analyzed by Bailey et al. Furthermore, Collisson et al. identified 8 genes in tumor cells analyzed by Moffitt et al. Whether the genes were analyzed by Collisson et al. or Bailey et al., there was only a little overlap with the stromal genes analyzed by Moffitt et al. Despite a low gene overlap, all classifications were associated with pathological grade, a critical prognostic feature that reflects the intrinsic molecular characteristics of tumors.
Clinical staging
Accurate staging is the basis for guiding the diagnosis and treatment of malignant tumors and evaluating the prognosis, especially for pancreatic cancer, which is highly malignant and is challenging for diagnosis and treatment. The cancer staging system introduced by the American Joint Council on Cancer (AJCC) has become the gold standard for malignant tumor staging. Presently, clinical staging of pancreatic cancer is based on the eighth edition of the TNM staging system.
van Roessel et al. [ 14 ] reported that the eighth edition of the TNM staging system displays an equal distribution among stages and a modestly increased prognostic accuracy in patients with resected PDAC compared to the seventh edition. The revised T stage remains poorly associated with survival, whereas the revised N stage is highly prognostic. Taniuchi et al. [ 15 ] demonstrated that the combination of PODXL with ITGB1 and that of BCL7B with ITGB1 accurately predicted the postoperative outcomes of pancreatic cancer patients; these predictors were superior compared to the TNM staging system. The combination of PODXL with ITGB1 was rather beneficial as it was the most highly correlated with the postoperative outcomes.
Screening and early diagnosis of pancreatic cancer
The United States Preventive Medicine Task Force (USPSTF) indicated that the potential benefits of screening for pancreatic cancer in asymptomatic adults do not outweigh the potential risks, and screening for pancreatic cancer in asymptomatic adults is not recommended. Since early screening is crucial to improve the overall prognosis of patients with pancreatic cancer, it should be performed in high-risk groups.
Development of imaging technology
The diagnosis of pancreatic cancer depends on traditional imaging examination. With the rapid development of imaging technology and equipment, medical imaging, including transabdominal ultrasound (TAUS), computed tomography (CT), magnetic resonance imaging (MRI), and endoscopic ultrasonography (EUS), plays a critical role in the diagnosis of PDAC, which has different capabilities for the detection of early pancreatic cancer [ 16 ].
Diffusion MRI technology, including diffusion-weighted imaging (DWI) and intravoxel incoherent motion imaging (IVIM), has shown superior diagnostic efficacy [ 17 ]. Due to the limited diffusion of water molecules in pancreatic cancer focus, DWI sequences showed significantly high signal and significantly decreased diffusion coefficient and perfusion fraction of IVIM sequence, which can distinguish pancreatic cancer from other mass pancreatitis and autoimmune pancreatitis. Compared to CT, EUS can detect smaller solid lesions and has the added advantage of not using ionizing radiation, not requiring contrast agents, and obtaining cytopathological results sequentially. Especially, the endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) is the gold standard for the diagnosis of pancreatic cancer [ 18 ]. Additionally, radiomics is a new approach for image analysis, combined with artificial intelligence (AI) and computer-aided diagnosis system that facilitates radiographical diagnosis and step into the era of mass data and precision [ 19 ].
Discovery of new serum marker
Serum cancer antigen 19 − 9 (CA 19 − 9) is the only marker approved by the United States Food and Drug Administration for use in the routine management of pancreatic cancer [ 20 ]. The low positive predictive value means that CA19-9 has no role in the mass screening of asymptomatic patients and is only appropriate for monitoring the response to treatment and as a marker of recurrent disease [ 21 ].
New serum markers combined with clinically common tumor marker detection improves the early diagnosis rate of pancreatic cancer. CA50 combined with tissue polypeptide antigen detection improves the detection rate of pancreatic cancer [ 22 ], and CA19-9 combined with CA125 detection significantly improves the diagnostic sensitivity of pancreatic cancer [ 23 ]. With the development of protein molecular technology and proteomics, several serum protein molecules characteristic of early pancreatic cancer have been identified, including matrix metalloproteinase MMP-2, MMP-9, [ 24 ] and serum galactoagglutinin-3 [ 25 ].
In recent years, the study on non-coding RNA (ncRNA) has developed rapidly and achieved a series of breakthrough results, which have established characteristic models with a strong diagnostic efficiency. In addition, the application of liquid biopsy involving circulating tumor cells (CTCs), circulating tumor DNA (ctDNA), and exosomes provides a new research direction for the early diagnosis of pancreatic cancer.
Landmark of treatment
Resectable pancreatic cancer.
Pancreaticoduodenectomy (Whipple’s procedure), distal or total pancreatectomy, is the surgical option for the resection of pancreatic cancer. Trendelenberg performed a distal pancreatectomy to remove a tumor of the pancreas. Despite a poor postoperative outcome, this procedure marked the birth of pancreatic surgery [ 26 ]. In 1898, The first recorded attempt at a partial pancreaticoduodenectomy was by Alessandro Codivilla. After 21 days, the patient died of cachexia (2009). In 1909, Walter Kausch performed the first successful two-stage partial pancreaticoduodenectomy, and the patient survived for 9 months until dying of cholangitis, without evidence of visible tumor recurrence at autopsy [ 27 ]. About three decades later, Allen Whipple published his series of three patients with ampullary cancer, which marked the first report of a two-stage complete pancreaticoduodenectomy [ 28 ]. In 1942, Whipple reported the modification of this operation to a one-staged procedure and further modified it in 1946 [ 29 ]. The operative mortality of pancreaticoduodenectomy was > 30% at its inception and did not improve significantly. The median OS of patients with resectable pancreatic cancer was approximately 12 months in the 1960s, leading to questions about the curative intent of the procedure [ 30 ]. Thanks to advanced development in surgical robot, more and more patients in this disease benefit from the minor wounds, less infection and longer survival periods. The landmarks in surgical operation pattern against pancreatic cancer, from bottom to up, the complex manual operation to robot assistant operation. More details, the complex manual operation usually need more length wounds, see below part. Then thanks to the second generation technology celioscope, the area and length of wounds become smaller and smaller, see middle part. Recently, the AI and robot technology developing sharply, the robot assistant operation can save more time, conduct more complex operation, see above part, Fig. 2 .

Landmarks in surgical operation pattern against pancreatic cancer (Drawn by FFL)
The Gastrointestinal Tumor Study Group (GITSG) trial heralded a new era of adjuvant therapy, and operative mortality declined to < 3%, as reported in the reviews in 1980s [ 30 ]. Subsequent clinical trials over the next several decades have pushed the boundaries of treatment of resectable pancreatic cancer, resulting in significant improvements in OS. The JASPAC 01 and PRODIGE-24 trials [ 31 ],[ 32 ] in the 2010s demonstrated significant improvements in median OS of resectable pancreatic cancer with adjuvant S-1 and FOLFIRINOX (a combination chemotherapy regimen consisting of oxaliplatin, irinotecan, fluorouracil, and leucovorin). In 2019, PREOPANC-1, the first phase III clinical trial of neoadjuvant therapy, showed benefits in disease-free survival, R0 removal, and decreasing pathologic lymph node rate, perineural infiltration, and venous infiltration as secondary endpoints [ 33 ]. However, a meta-analysis about the preoperative/neoadjuvant therapy in pancreatic cancer found that estimated median survival following resection was 23.3 (range 12–54) mouths for initially resectable tumors patients and 20.5 (range 9–62) mouths for and initially non-resectable tumors patients, and concluded that in patients with resectable tumor, survival after neoadjuvant therapy were similar to those of patients with primarily resected tumors and adjuvant therapy [ 34 ]. Therefore, neoadjuvant chemotherapy for the treatment of resectable pancreatic cancer remains controversial. According to the guidelines of the National Comprehensive Cancer Network (NCCN) and the Pancreatic Surgery Group of the Surgery Society of the Chinese Medical Association, the indications of neoadjuvant chemotherapy are: (1) Suspicious metastases are found in imaging examination; (2) Serum CA19-9 level increase significantly; (3) The primary tumor is large; (4) Regional lymph nodes are larger.
There is a growing interest in minimally invasive techniques for pancreatic surgery. Laparoscopic distal pancreatectomy was the first minimally invasive pancreatectomy. A meta-analysis demonstrated that laparoscopic and open distal pancreatectomy had comparable morbidity and mortality, with reduced blood loss and length of hospital stay in the minimally invasive group. Also, no difference in the positive rate of resection margins [ 35 ]. Further meta-analysis suggested that laparoscopic distal pancreatectomy is similar to open surgery, but the lack of primary evidence indicated that it could not be sup [ 36 ].
Interestingly, robotics has been applied to improve Whipple’s surgery. A meta-analysis of a retrospective cohort study found a lower incidence of complications and less margin involvement in the robotic group compared to open pancreatectomy [ 37 ]. However, these studies lack randomization, which makes them vulnerable to selection bias. Robotic surgery also requires significant capital investment; the cost-effectiveness assessments were not included in any of the articles.
Borderline resectable pancreatic cancer and locally advanced unresectable pancreas
For borderline resectable and locally advanced unresectable pancreatic cancer, the 2020 version of the US NCCN guidelines has clearly defined neoadjuvant therapy as the clinical diagnosis and treatment standard that affirms the clinical application value of neoadjuvant therapy for such diseases and provides patients with the opportunity of surgical resection after receiving tumor transformation therapy. A single-arm phase II clinical trial investigated the effects of adjuvant chemoradiotherapy combined with FOLFIRINOX and the angiotensin II receptor antagonist losartan in patients with locally advanced unresectable pancreatic cancer. Consequently, this treatment plan provided a downstaging of locally advanced pancreatic ductal adenocarcinoma and was associated with an R0 resection rate of 61% [ 38 ]. Our previous systemic review and meta-analysis described the clinical efficacy of radiotherapy in neoadjuvant therapy for borderline resectable pancreatic cancer and local advanced unresectable pancreatic cancer; however, the treatment-related toxicity might significantly reduce the life quality of patients [ 39 ].
Metastatic pancreatic cancer
The management of metastatic pancreatic cancer involves symptom control and management of jaundice, and gemcitabine is the therapeutic drug. A phase III randomized clinical study of 342 patients with untreated metastatic pancreatic cancer demonstrated that the median OS in the FOLFIRONOX group was 11.1 months compared to 6.8 months in the gemcitabine group. However, the incidence of adverse effects within the group receiving FOLFIRONOX was increased [ 40 ]. Another first-line phase III clinical study showed that the median progression-free survival was 5.5 months in the nab-paclitaxel-gemcitabine group (Gnp) compared to 3.7 months in the gemcitabine group; however, the rates of peripheral neuropathy and myelosuppression were increased [ 41 ]. FOLFIRINOX and Gnp are options for the treatment of patients with metastatic pancreatic cancer and a satisfactory performance status.
Other treatment strategies
Pancreatic cancer has unique characteristics, including dense stroma and tumor microenvironment filled with immunosuppressive intermediates, which form a solid barrier against pancreatic cancer immune cell and drug infiltrations. Immunotherapy is active against melanoma, kidney cancer, non-small cell lung cancer, and other malignant tumors. Presently, the immunotherapy effect of pancreatic cancer is not optimal, but as more immune mechanisms are being revealed and clinical studies are underway, significant progress is expected in the future.
With the understanding of the mechanism of pancreatic cancer, additional targets for PDAC therapy are being discovered. The POLO research on gBRCAm [ 42 ], phase I and II clinical trials on epidermal growth factor receptor (EGFR) target drugs, and the study on PARP-1/2 inhibitors [ 43 ] are exploring the value of these drugs in the treatment of pancreatic cancer.
Pancreatic cancer is a devastating malignancy disease with a restricted approach to treatment. Thus, improving OS and treatment outcomes in the patient will rely on multidisciplinary cooperation in imaging, surgical procedures, radiation, and personalized therapies. Since the clinical progress is gradual, our insight into the molecular biology of PDAC and the tumor and inflammatory microenvironment needs further exploration.
The tumor and inflammatory microenvironment is characterized by an abundance of immunosuppressive cells and a highly fibrotic stroma that prevents infiltration of immune effector cells. The ablative techniques have the potential to overcome these factors. It has been hypothesized that ablation induces anti-tumor immune responses by increasing the availability of tumor-specific neoantigens in an inflammatory context. Numerous preclinical studies demonstrated that radiation therapy, thermal ablation, and IRE induce systemic anti-tumor immune responses in multiple tumor types. The current data showed improved OS in the postoperative therapies after surgery. Nonetheless, monitoring the tumor response to postoperative treatment is challenging. Thus, it is essential to improve the sensitivity of pancreatic cancer to immunotherapy and improve the outcomes.
We are stepping towards an exciting era where a better understanding of tumor biology, novel therapeutic targets, and innovative clinical trial designs and protocols will fetch data to illuminate the treatment and termination of pancreatic cancer.
Availability of data and materials
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
Sung H, Siegel FJ, Laversanne RL, Soerjomataram M, Jemal I, Bray AF. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Article Google Scholar
Arnold M, Neale AC, Vignat RE, Giovannucci J, McGlynn EL, Bray KAF. Global burden of 5 major types of gastrointestinal cancer. Gastroenterology. 2020;159(1):335–49.
Klein AP. Pancreatic cancer epidemiology: understanding the role of lifestyle and inherited risk factors. Nat Rev Gastroenterol Hepatol. 2021;18(7):493–502.
Cerullo M, Gani F, Chen SY, Canner JK, Herman JM, Laheru D, Pawlik TM. Assessing the financial burden associated with treatment options for resectable pancreatic cancer. Ann Surg. 2018;267(3):544–51.
Jiao L, Schairer SD, Thiébaut C, Hollenbeck AC, Leitzmann AR, Schatzkin MF, Stolzenberg-Solomon A. Alcohol use and risk of pancreatic cancer: the NIH-AARP diet and health study. Am J Epidemiol. 2009;1(9):1053–51.
Google Scholar
Genkinger JM, Spiegelman D, Anderson KE, Bergkvist L, Bernstein L, van den Brandt PA, English DR, Freudenheim JL, Fuchs CS, Giles GG, Giovannucci E, Hankinson SE, Horn-Ross PL, Leitzmann M, Männistö S, Marshall JR, McCullough ML, Miller AB, Reding DJ, Robien K, Rohan TE, Schatzkin A, Stevens VL, Stolzenberg-Solomon RZ, Verhage BA, Wolk A, Ziegler RG, Smith-Warner SA. Alcohol intake and pancreatic cancer risk:a pooled analysis of fourteen cohort studies. Cancer Epidemiol Biomarkers Prev. 2009;18(3):765–76.
Article CAS Google Scholar
Wood LD, Hruban RH. Pathology and molecular genetics of pancreatic neoplasms. Cancer J. 2012;18(6):492–501.
Kearney JF, Adsay V, Yeh JJ. Pathology and molecular characteristics of pancreatic cancer. Surg Oncol Clin N Am. 2021;30(4):609–19.
Basturk O, Hong SM, Wood LD, Adsay NV, Albores-Saavedra J, Biankin AV, Brosens LA, Fukushima N, Goggins M, Hruban RH, Kato Y, Klimstra DS, Klöppel G, Krasinskas A, Longnecker DS, Matthaei H, Offerhaus GJ, Shimizu M, Takaori K, Terris B, Yachida S, Esposito I, Furukawa T, Baltimore Consensus Meeting. A revised classification system and recommendations from the baltimore consensus meeting for neoplastic precursor lesions in the pancreas. Am J Surg Pathol. 2015;39(12):1730–41.
Jones S, Parsons ZX, Lin DW, Leary JC, Angenendt RJ, Mankoo P, Carter P, Kamiyama H, Jimeno H, Hong A, Fu SM, Lin B, Calhoun MT, Kamiyama ES, Walter M, Nikolskaya K, Nikolsky T, Hartigan Y, Smith J, Hidalgo DR, Leach M, Klein SD, Jaffee AP, Goggins EM, Maitra M, Iacobuzio-Donahue A, Eshleman C, Kern JR, Hruban SE, Karchin RH, Papadopoulos R, Parmigiani N, Vogelstein G, Velculescu B, Kinzler VE. KW Core signaling pathways in human pancreatic cancers revealed by global genomic analyses. Science. 2008;26(5897):1801–6.
Collisson EA, Sadanandam A, Olson P, Gibb WJ, Truitt M, Gu S, Cooc J, Weinkle J, Kim GE, Jakkula L, Feiler HS, Ko AH, Olshen AB, Danenberg KL, Tempero MA, Spellman PT, Hanahan D, Gray JW. Subtypes of pancreatic ductal adenocarcinoma and their differing responses to therapy. Nat Med. 2011;17(4):500–3.
Moffitt RA, Marayati R, Flate EL, Volmar KE, Loeza SG, Hoadley KA, Rashid NU, Williams LA, Eaton SC, Chung AH, Smyla JK, Anderson JM, Kim HJ, Bentrem DJ, Talamonti MS, Iacobuzio-Donahue CA, Hollingsworth MA, Yeh JJ. Virtual microdissection identifies distinct tumor-and stroma-specific subtypes of pancreatic ductal adenocarcinoma. Nat Genet. 2015;47(10):1168–78.
Bailey P, Nones CD, Johns K, Patch AL, Gingras AM, Miller MC, Christ DK, Bruxner AN, Quinn TJ, Nourse MC, Murtaugh C, Harliwong LC, Idrisoglu I, Manning S, Nourbakhsh S, Wani E, Fink S, Holmes L, Chin O, Anderson V, Kazakoff MJ, Leonard S, Newell C, Waddell F, Wood N, Xu S, Wilson Q, Cloonan PJ, Kassahn N, Taylor KS, Quek D, Robertson K, Pantano A, Mincarelli L, Sanchez L, Evers LN, Wu L, Pinese J, Cowley M, Jones MJ, Colvin MD, Nagrial EK, Humphrey AM, Chantrill ES, Mawson LA, Humphris A, Chou J, Pajic A, Scarlett M, Pinho CJ, Giry-Laterriere AV, Rooman M, Samra I, Kench JS, Lovell JG, Merrett JA, Toon ND, Epari CW, Nguyen K, Barbour NQ, Zeps A, Moran-Jones N, Jamieson K, Graham NB, Duthie JS, Oien F, Hair K, Grützmann J, Maitra R, Iacobuzio-Donahue A, Wolfgang CA, Morgan CL, Lawlor RA, Corbo RT, Bassi V, Rusev C, Capelli B, Salvia P, Tortora R, Mukhopadhyay G, Petersen DGM, Munzy DM, Fisher WE, Karim SA, Eshleman JR, Hruban RH, Pilarsky C, Morton JP, Sansom OJ, Scarpa A, Musgrove EA, Bailey UM, Hofmann O, Sutherland RL, Wheeler DA, Gill AJ, Gibbs RA, Pearson JV, Waddell N, Biankin AV, Grimmond SM, Australian Pancreatic Cancer Genome Initiative. Genomic analyses identify molecular subtypes of pancreatic cancer. Nature. 2016;531(7592):47–52.
van Roessel S, Kasumova GG, Verheij J, Najarian RM, Maggino L, de Pastena M, Malleo G, Marchegiani G, Salvia R, Ng SC, de Geus SW, Lof S, Giovinazzo F, van Dam JL, Kent TS, Busch OR, van Eijck CH, Koerkamp BG, Abu Hilal M, Bassi C, Tseng JF, Besselink MG. International validation of the eighth edition of the American Joint Committee on Cancer (AJCC) TNM staging system in patients with resected pancreatic cancer. JAMA Surg. 2018;153(12):e183617.
Taniuchi K, Naganuma FM, Sakaguchi S, Saibara M. T., Overexpression of PODXL/ITGB1 and BCL7B/ITGB1 accurately predicts unfavorable prognosis compared to the TNM staging system in postoperative pancreatic cancer patients. PLoS One. 2019 Jun;5(6):e0217920. . 14 .
Chen X, Liu F, Xue Q, Weng X, Xu F. Metastatic pancreatic cancer: mechanisms and detection (review). Oncol Rep. 2021;46(5):231.
Chen J, Liu S, Tang Y, Zhang X, Cao M, Xiao Z, Ren M, Chen X. Diagnostic performance of diffusion MRI for pancreatic ductal adenocarcinoma characterisation: a meta-analysis. Eur J Radiol. 2021;139:109672.
Yang J, Xu R, Wang C, Qiu J, Ren B, You L. Early screening and diagnosis strategies of pancreatic cancer: a comprehensive review. Cancer Commun (Lond). 2021;41(12):1257–74.
Bartoli M, Barat M, Dohan A, Gaujoux S, Coriat R, Hoeffel C, Cassinotto C, Chassagnon G, Soyer P. CT and MRI of pancreatic tumors: an update in the era of radiomics. Jpn J Radiol. 2020;38(12):1111–24.
Kim JE, Lee KT, Lee JK, Paik SW, Rhee JC, Choi KW. Clinical usefulness of carbohydrate antigen 19–9 as a screening test for pancreatic cancer in an asymptomatic population. J Gastroenterol Hepatol. 2004;19(2):182–6.
McGuigan A, Kelly P, Turkington RC, Jones C, Coleman HG, McCain RS. Pancreatic cancer: a review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol. 2018;24(43):4846–61.
Pasanen PA, Eskelinen M, Partanen K, Pikkarainen P, Penttilä I, Alhava E. A prospective study of serum tumour markers carcinoembryonic antigen, carbohydrate antigens 50 and 242, tissue polypeptide antigen and tissue polypeptide specific antigen in the diagnosis of pancreatic cancer with special reference to multivariate diagnostic score. Br J Cancer. 1994;69(3):562–5.
Skulimowski A, Durczyński A, Strzelczyk J, Hogendorf P. Comparison of clinical usefulness of serum Ca125 and CA19-9 in pancreatic adenocarcinoma diagnosis: meta-analysis and systematic review of literature. Biomarkers. 2021;26(4):287–95.
Dranka-Bojarowska D, Lewinski A, Lekstan A, Gajda M, Ciosek J, Mrowiec S. The assessment of serum and diagnostic peritoneal lavage concentration of matrix metalloproteinase-2, matrix metalloproteinase-9, carbohydrate antigen 19–9, and carcinoembryonic antigen in patients with pancreatic cancer and chronic pancreatitis. J Physiol Pharmacol. 2020. https://doi.org/10.26402/jpp.2020.5.09 .
Yi N, Zhao X, Ji J, Xu M, Jiao Y, Qian T, Zhu S, Jiang F, Chen J, Xiao M. Serum galectin-3 as a biomarker for screening, early diagnosis, prognosis and therapeutic effect evaluation of pancreatic cancer. J Cell Mol Med. 2020;24(19):11583–91.
Griffin JF, Poruk KE, Wolfgang CL. Pancreatic cancer surgery: past, present, and future. Chin J Cancer Res. 2015;27(4):332–48.
CAS Google Scholar
Kausch W (1990) Das Carcinom der Papilla duodeni und seine radikale Entfernung. In: Schmiedebach H-P, Winau R, Häring R(eds) Erste Operationen Berliner Chirurgen 1817–1931, De Gruyter, Berlin, Boston, pp 40–51. https://doi.org/10.1515/9783110864731-008
Chapter Google Scholar
Whipple AO, Mullins PW. Treatment of carcinoma of the ampulla of vater Ann Surg. 1935;102(4):763–79.
O WA. Present-day surgery of the pancreas. N Engl J Med. 1942;226(13):515–26.
Torphy RJ, Fujiwara Y, Schulick RD. Pancreatic cancer treatment: better, but a long way to go. Surg Today. 2020;50(10):1117–25.
Uesaka K, Fukutomi BN, Okamura A, Konishi Y, Matsumoto M, Kaneoka I, Shimizu Y, Nakamori Y, Sakamoto S, Morinaga H, Kainuma S, Imai O, Sata K, Hishinuma N, Ojima S, Yamaguchi H, Hirano R, Sudo S, Ohashi T. Y; JASPAC 01 Study Group., Adjuvant chemotherapy of S-1 versus gemcitabine for resected pancreatic cancer: a phase 3, open-label, randomised, non-inferiority trial (JASPAC 01). Lancet, 2016 Jul 16. 388 (10041): 248–57.
Conroy T, Hebbar HP, Ben Abdelghani M, Wei M, Raoul AC, Choné JL, Francois L, Artru E, Biagi P, Lecomte JJ, Assenat T, Faroux E, Ychou R, Volet M, Sauvanet J, Breysacher A, Di Fiore G, Cripps F, Kavan C, Texereau P, Bouhier-Leporrier P, Khemissa-Akouz K, Legoux F, Juzyna JL, Gourgou B, O’Callaghan S, Jouffroy-Zeller CJ, Rat C, Malka P, Castan D, Bachet F, Canadian Cancer trials Group and the Unicancer-GI–PRODIGE Group. FOLFIRINOX or gemcitabine as adjuvant therapy for pancreatic cancer. N Engl J Med. 2018;20(25):2395–406.
Versteijne E, Groothuis SM, Akkermans-Vogelaar K, Besselink JM, Bonsing MG, Buijsen BA, Busch J, Creemers OR, van Dam GM, Eskens RM, Festen FALM, de Groot S, Groot Koerkamp JWB, de Hingh B, Homs IH, van Hooft MYV, Kerver JE, Luelmo ED, Neelis SAC, Nuyttens KJ, Paardekooper J, Patijn GMRM, van der Sangen GA, de Vos-Geelen MJC, Wilmink J, Zwinderman JW, Punt AH, van Eijck CJ, van Tienhoven CH, Dutch pancreatic Cancer Group. Preoperative chemoradiotherapy versus immediate surgery for resectable and borderline resectable pancreatic cancer: results of the dutch randomized phase III PREOPANC trial. J Clin Oncol. 2020;1(18):1763–73.
Gillen S, Schuster T, Büschenfelde CMZ, Friess H, Kleeff J. Preoperative/neoadjuvant therapy in pancreatic cancer: a systematic review and meta-analysis of response and resection percentages. PLoS Med. 2010;20(4):e1000267.
Venkat R, Edil BH, Schulick RD, Lidor AO, Makary MA, Wolfgang CL. Laparoscopic distal pancreatectomy is associated with significantly less overall morbidity compared to the open technique: a systematic review and meta-analysis. Ann Surg. 2012;255(6):1048–59.
Pericleous S, Middleton N, McKay SC, Bowers KA, Hutchins RR. Systematic review and meta-analysis of case-matched studies comparing open and laparoscopic distal pancreatectomy: is it a safe procedure? Pancreas. 2012;41(7):993–1000.
Zhang J, Wu WM, You L, Zhao YP. Robotic versus open pancreatectomy: a systematic review and meta-analysis. Ann Surg Oncol. 2013;20(6):1774–80.
Murphy JE, Ryan WJ, Clark DP, Jiang JW, Yeap W, Drapek BY, Ly LC, Baglini L, Blaszkowsky CV, Ferrone LS, Parikh CR, Weekes AR, Nipp CD, Kwak RD, Allen EL, Corcoran JN, Ting RB, Faris DT, Zhu JE, Goyal AX, Berger L, Qadan DL, Lillemoe M, Talele KD, Jain N, DeLaney RK, Duda TF, Boucher DG, Fernández-Del Castillo Y, Hong C. Total neoadjuvant therapy with FOLFIRINOX in combination with Losartan followed by chemoradiotherapy for locally advanced pancreatic cancer: a phase 2 clinical trial. JAMA Oncol. 2019;1(7):1020–7.
Chen J, Yu CL, Xu J, Wang Y, Zeng X, Liu Z, Xu N, Yang FS. Meta-analysis of current chemotherapy regimens in advanced pancreatic cancer to prolong survival and reduce treatment–associated toxicities. Mol Med Rep. 2019;19(1):477–89.
Conroy T, Ychou DF, Bouché M, Guimbaud O, Bécouarn R, Adenis Y, Raoul A, Gourgou-Bourgade JL, de la Fouchardière S, Bennouna C, Bachet J, Khemissa-Akouz JB, Péré-Vergé F, Delbaldo D, Assenat C, Chauffert E, Michel B, Montoto-Grillot P, Ducreux C, Groupe Tumeurs Digestives of Unicancer; PRODIGE Intergroup. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;12(19):1817–25.
Von Hoff DD, Ervin T, Arena FP, Chiorean EG, Infante J, Moore M, Seay T, Tjulandin SA, Ma WW, Saleh MN, Harris M, Reni M, Dowden S, Laheru D, Bahary N, Ramanathan RK, Tabernero J, Hidalgo M, Goldstein D, Van Cutsem E, Wei X, Iglesias J, Renschler MF. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med. 2013;369(18):1691–703.
Barnard ZR, Alexander MJ. Device profile of the Wingspan Stent System for the treatment of intracranial atherosclerotic disease: overview of its safety and efficacy. Expert Rev Med Devices. 2020;17(3):167–71.
Tuli R, Shiao SL, Nissen N, Tighiouart M, Kim S, Osipov A, Bryant M, Ristow L, Placencio-Hickok V, Hoffman D, Rokhsar S, Scher K, Klempner SJ, Noe P, Davis MJ, Wachsman A, Lo S, Jamil L, Sandler H, Piantadosi S, Hendifar A. A phase 1 study of veliparib, a PARP-1/2 inhibitor, with gemcitabine and radiotherapy in locally advanced pancreatic cancer. EBioMedicine. 2019;40:375–81.
Download references
This study was supported by the National Natural Science Foundation of China (82073833) and the Chengdu Science and Technology Bureau Focuses on Research and Development Support Plan (2019-YF09-00097-SN).
Author information
Fan Xu, Min Huang and Yun Bai are contributed equally to this study
Authors and Affiliations
Department of Public Health, Chengdu Medical College, Chengdu, 610500, Sichuan, China
Fan Xu & Yun Bai
Department of Physiology, Chengdu Medical College, Chengdu, 610500, Sichuan, China
Department of Clinic Medicine, Chengdu Medical College, Chengdu, 610500, Sichuan, China
Department of Abdominal Oncosurgery-2, Jilin Province Tumor Hospital, Changchun, 130012, China
Jingzhe Yan
Art college, Southwest Minzu University, Chengdu, 610041, Sichuan, China
Fangfang Liu
Department of Orthopedics, Shanghai Institute of Traumatology and Orthopaedics, Ruijin Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, 200025, China
School of Chinese Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, 999077, China
Department of Neuroscience, Beijing Institute of Basic Medical Sciences, Beijing, 100850, China
Xiechuan Weng
You can also search for this author in PubMed Google Scholar
Contributions
XF, HM and BY screened the literature, presented data, and drafted the manuscript. LFF drew the images, YXS performed citespace analysis for keyword evaluation. XF ensured the general workflow, and CJ and WXC proofread the manuscript. All authors contributed to the study and approved the submitted version of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Jie Chen or Xiechuan Weng .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Xu, F., Huang, M., Bai, Y. et al. Landmarks in pancreatic cancer studies. Cancer Cell Int 22 , 383 (2022). https://doi.org/10.1186/s12935-022-02803-8
Download citation
Received : 27 April 2022
Accepted : 23 November 2022
Published : 07 December 2022
DOI : https://doi.org/10.1186/s12935-022-02803-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Pancreatic cancer
Cancer Cell International
ISSN: 1475-2867
- General enquiries: [email protected]
Home — Essay Samples — Nursing & Health — Oncology — Pancreatic Cancer
Essay Examples on Pancreatic Cancer
Ethical dilemmas in end-of-life decision making, a look at the root, impact, and remedy for pancreatic cancer, made-to-order essay as fast as you need it.
Each essay is customized to cater to your unique preferences
+ experts online
Looking at The Biography of The 39th President of The United States, James Earl Carter Jr
The origin and effect of blood pressure on my family, research of pancreatic cancer, the best treatment for pancreatic cancer, let us write you an essay from scratch.
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
The Overview of Pancreatic Cancer
Relevant topics.
- Breast Cancer
- Prostate Cancer
- Ovarian Cancer
- Skin Cancer
- Lung Cancer
- Cervical Cancer
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Pancreatic Cancer Research Results and Study Updates
See Advances in Pancreatic Cancer Research for an overview of recent findings and progress, plus ongoing projects supported by NCI.
A new study finds that pancreatic cancer cells have a ready way to overcome a lack of glucose, a frequent occurrence in this disease. They use another fuel source: a molecule called uridine. Findings from a related study suggest other cancers do as well.
An experimental drug, MRTX1133, shrank tumors or halted their growth in several mouse models of human pancreatic cancer with KRAS G12D mutations, a new study shows. The models included one that is genetically engineered to closely mimic the human disease.
Abnormal collagen that is formed only by pancreatic cancer cells ramps up activity that increases tumor growth and survival, a study found. In mice, blocking production or effects of the abnormal collagen made treatment for pancreatic cancer more effective.
FDA has approved belzutifan (Welireg) to treat adults with von Hippel-Lindau disease (VHL) who have tumors of the kidney, brain, nervous system, or pancreas. The drug may help these patients avoid or delay surgery by shrinking their tumors.
Numerous studies have pointed to a link between new-onset diabetes and pancreatic cancer. Now, several large NCI-supported studies are testing ways to pick out those people whose diabetes might be a sign of early pancreatic cancer, when treatments may be more effective.
The number of dendritic cells in a tumor may explain why immunotherapies work for some cancers but not others, a new study suggests. In mice, boosting dendritic cells triggered an immune response that slowed pancreatic tumor growth.
In people with pancreatic cancer, the makeup of bacteria that populate their tumors could predict how long they live, results from a new study suggest. Experiments in mice suggested that altering the tumor microbiome could play a role in treatment.
Olaparib (Lynparza) may be beneficial for some people with advanced pancreatic cancer who have inherited mutations in the BRCA1 or BRCA2 genes, according to results from the POLO trial.
Three research groups have found a potential way to kill cancer cells in pancreatic tumors by simultaneously blocking the activity of proteins that interact with KRAS proteins and disrupting an energy-creating process called autophagy.
Results from two clinical trials are expected to improve the outlook for some people with early-stage pancreatic cancer. Altering the chemotherapy drugs used and the timing of treatment substantially improved survival.
People with cancerous neuroendocrine tumors (NETs) that affect the digestive tract now have a new treatment option. On January 29, FDA approved the targeted treatment lutetium Lu 177 dotatate (Lutathera®) for adult patients with advanced NETs that affect the pancreas or gastrointestinal tract.
A new blood test that measures levels of two specific proteins may be able to accurately detect pancreatic cancer at its earliest stages, when it is most likely to respond to treatment, findings from a new study suggest.
In 2011, based on initial findings from two clinical trials, the Food and Drug Administration approved sunitinib and everolimus for patients with pancreatic neuroendocrine tumors. Updated results from the everolimus trial were published in September 2016.
Pancreatic cancer cells instruct healthy cells around them to provide nutrients they need to survive and grow, a new study suggests.
Pancreatic cancer cells and neighboring normal cells engage in a two-way molecular conversation that helps drive malignant behavior in the cancer cells, according to new study results.
Patients with metastatic pancreatic cancer that has progressed after receiving gemcitabine-based chemotherapy now have a new treatment option: irinotecan liposome in combination with fluorouracil and leucovorin.
A protein attached to vesicles circulating in the blood could be a biological marker for detecting early signs of pancreatic cancer.
Essay On Pancreatic Cancer
What is pancreatic cancer? Pancreatic cancer is an aggressive form of cancer that develops in the tissues of the pancreas. Located in the abdomen behind the lower part of the stomach, the pancreas aids in digestion. It contains both exocrine glands (which produce enzymes that help the body digest food) and endocrine glands (which produce hormones, including insulin, that help control blood sugar levels in the body).
Pancreatic cancer is hard to diagnose and once it is found it has usual spread to other places in the body pancreatic cancer typically spreads rapidly to nearby organs. It is seldom detected in its early stages. But for people with pancreatic cysts or a family history of pancreatic cancer, some screening steps might help detect a problem early. One sign of pancreatic cancer is diabetes, especially when it occurs with weight loss, jaundice or pain in the upper abdomen that spreads to the back.
Symptoms Signs and symptoms of pancreatic cancer often don’t occur until the disease is advanced. They may include: • Pain in the upper abdomen that radiates to your back • Loss of appetite or unintended weight loss • Depression • New-onset diabetes • Blood clots Fatigue Yellowing of your skin and the whites of your eyes (jaundice) In 2017, the American Cancer Society predicts that about 53,670 people will be diagnosed with pancreatic cancer and about 43,090 people will die from pancreatic cancer.
Symptoms of pancreatic cancer may not appear until it is “too late” or when total removal of the pancreas is not possible, but some of the symptoms include; loss of appetite, jaundice(yellowing of the skin or whites of the eyes), blood clots, or pain that begins in the upper abdomen and radiates to the back. Many of the symptoms of pancreatic cancer, however, are similar to those of other diseases or cancers. Obviously, if one is experiencing unexplained weight loss or begins to develop jaundice, a doctor should be contacted immediately.
Pancreatic cancer forms once cells in your pancreas develop mutations in their DNA. The cells continue to multiply and grow uncontrollably and can eventually form a tumor. Pancreatic adenocarcinoma or also known as pancreatic exocrine cancer begins in the cells that line the Pancreatic Cancer ducts of the pancreas. This is the most common form of cancer. Islet cell cancer, pancreatic endocrine cancer, or pancreatic neuroendocrine tumors are the more rare types of this cancer, and they begin in the hormone producing or neuroendocrine cells of the pancreas.
As with any disease, there are always things that people can do to prevent or reduce the risk of getting the disease. With pancreatic cancer, the risk factors are being over weight, diabetes, family history of cancers or genetic mutations that may cause cancer, personal or family history of specifically pancreatic cancer, and smoking. There is a 2. 5 to 3. 6 time increased rate of a person who smokes or uses tobacco developing pancreatic cancer rather than someone who does not (Dr. Hidalgo 2010). The risk is also increased in those who are drink alcohol more often compared to those who drink less or not at all.
Now, doctors or researchers are not saying that if a person does, is or has any of these, that they are going to get pancreatic cancer, they are just at a more elevated risk rather than somebody who has a clean background or somebody who does not smoke, for example. Pancreatic Cancer the patient has a type of pancreatic cancer that presses into the small intestine, that is when digested food going to the intestines from the stomach is blocked. If a patient is experiencing severe or unusual symptoms, that person should contact their doctor immediately.
Doctors may use CT scans, ultrasound, MRI, or occasionally PET scan to diagnose pancreatic ancer. The doctors could also use an endoscopic ultrasound, which makes images of your pancreas. The EUS uses a tube that oasses through the esophagus and down into the stomach to gather the images. Also, a doctor may simply order a blood test from a patient. The doctor may be looking for tumour markers that may be shed by pancreatic cancer cells. Once a diagnosis is confirmed, the doctor will determine the extent of the cancer by determining the stage. By determining the stage, the doctor can then determine the next step in determining the treatment. In each stage, there is something different occurring as the cancer progresses.
Stage 1 of pancreatic cancer is when the cancer is first identified and the cancerous portion of the pancreas can be removed during surgery. The cancer has spread to organs and tissues that are nearby in Stage II. The cancer may have also spread to the lymph nodes. Surgery at this point may still be possible. By Stage III, surgery still is a possibility but at the same time, it may not be a possibility. The cancer has spread past the pancreas to videal blood vessels and possibly to the lymph nodes. Once a cancer hits Stage IV, surgery is no longer an option.
This is the stage where the cancer has spread to nearby locations of the body including the lungs or the liver or organs that are adjacent to the pancreas such as the stomach and the spleen. There are, however, two groups of Stage IV pancreatic cancer; Stage IVA and Stage IVB. Stage IVA involves organs that are adjacent to the pancreas and nearby blood vessels, but the cancer is contained into a small Pancreatic Cancer 4 area. Even though it is confined to one area, that makes it more difficult for surgery. This stage of cancer is also known as locally advanced or localized. Stage IVB most commonly involves the liver.
In this stage, the cancer has spread to distant organs, such as the liver. This stage is also known as metastatic. The treatment for pancreatic cancer depends on where the cancer is found and what stage the cancer is discovered at, as well as the patient’s health and the personal preferences of the patient and the family. Overall, the goal is to eliminate or remove the cancer when it is first discovered. However, that may not always be possible, depending on the stage or the location. The next focus may to improve the patient’s quality of life or to prevent the cancer from spreading any further and causing more harm to the patient.
Treatment could include surgery, radiation, or chemotherapy, or a combination of chemotherapy and radiation. If the cancer is found too late, the doctor will often palliative care to make the patient as comfortable as possible. There are many different types of surgery for the different areas where the cancer can be located on the pancreas. The Whipple procedure is used when the cancer is located on the head of the pancreas. The Whipple procedure removes the gallbladder, the head of the pancreas, the first part of the small intestine, and part of the bile duct.
There are some cases in which part of the stomach and the lymph nodes that are nearby must also be removed. The surgeon will then reconnect the pancreas, the intestines, and the stomach together, allowing the patient to digest food. Surgery to completely remove the whole pancreas in known as total pancreatectomy. This option is only for those patients whose pancreas is completely compromised by the cancer. Once the Pancreatic Cancer 5 pancreas is removed, the patient will be put on a insulin and enzyme replacement that will be lifelong, due to the fact that the organ that used to do that job will now be out of the body.
Chemotherapy is a treatment that uses drugs to kill cancer cells. The treatment will either be injected into the vein or distributed orally. Chemotherapy can also be delivered with radiation. When chemo is delivered, that normally means that the cancer has spread beyond the pancreas, but it is controlled to nearby organs and has not spread to distal parts of the body. In patients who have advanced cancer, chemo is used to control the growth of the cancer and increased the survival time. Radiation therapy is a type of treatment that uses high-energy beams, similar to those that X-Rays are made from, that are used to kill cancer cells.
Radiation may be delivered before or after surgery is performed. If the cancer cannot be removed by surgery, radiation may be combined with chemo. The radiation is delivered by a machine that rotates around the patient, directing the radiation at specific spots of the body. Pancreatic cancer is the leading cause of cancer deaths. Once it is spotted, often times it is too late to do anything about it. Typically, more men than women are diagnosed with this cancer, however, more women die from this cancer. This cancer is normally diagnosed in older patients, but it is not picky and will attack anybody of any age.
More Essays
- Argumentative Essay: Starving Cancer With Nutrition
- Describe The Process Of Homeostasis Essay
- Chemotherapy: The Cause Of Cancer Essay
- Ovarian Cancer: A Short Story Essay
- Cancer-Related Pain: A Literature Review Essay
- Melanoma – skin cancer
- Why Are Heart Surgery Important Essay
- Cancer Alternative Treatments: Documentary Analysis Essay
- Persuasive Essay On Gene Therapy
- Personal Narrative: Stoned My Life Essay
There's still no standard test to detect pancreatic cancer early. Scientists are working to change that
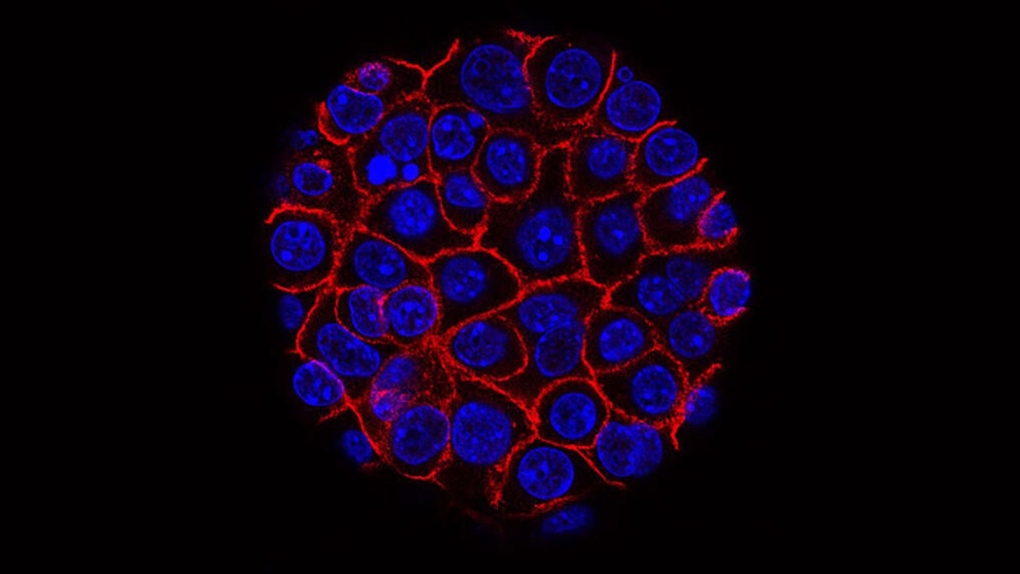
To spot breast cancer early, there are mammograms. To find colon cancer early, there are colonoscopies. But there is no standard test to detect early cases of pancreatic cancer, before cancer cells have spread and when surgery is more likely to be helpful.
Finding pancreatic cancer early could help increase a patient’s chances of survival. Although pancreatic accounts for just about 3% of all new cancer cases in the United States, it’s the third leading cause of cancer deaths and is projected to become the second leading cause of cancer deaths by the end of this decade.
- Top health headlines, all in one place
Across the United States, research teams are investigating ways to spot early cases, with many turning to blood-based liquid biopsy tests.
"This term ‘liquid biopsy,’ essentially, is trying to find markers in the blood that signify a tumor is present – and there are many different ways to do that. There are a lot of different features of a tumor that can end up in the blood that you could use,” said Dr. Brian Wolpin, director of the Gastrointestinal Cancer Center at Dana-Farber Cancer Institute, whose laboratory has done work in this area.
But many studies investigating the potential of liquid biopsy tests for the early detection of pancreatic cancer are still in the early phases. And the US Preventive Services Task Force recommends against screening for pancreatic cancer in adults who are not showing symptoms, especially because there is no established method or test to detect this form of the disease early in the general population.
Although there currently is no single recommended blood test to find early pancreatic cancers, “there is a large scientific community working to try to change this and to identify a screening test that we can use in the clinic, but it’s quite hard,” Wolpin said. “There’s still more work that needs to be done to get there.”
One team presented its research Monday at an annual meeting of the American Association for Cancer Research, detailing the development of a liquid biopsy test that was found to detect 97% of stage I and stage II pancreatic cancers in hundreds of volunteers. The researchers are from the City of Hope Comprehensive Cancer Center and other institutions around the world.
Their study, which has not been published in a peer-reviewed journal, included 984 people, some healthy and others with pancreatic cancer, based in Japan, the United States, South Korea and China.
The researchers collected blood samples from each person and tested the expression of a set of small genes called microRNAs within the blood and encapsulated within exosomes found in the blood. Exosomes are small vesicles that are shed by both cancerous and healthy cells in the blood.
“Cancer cells tend to release many, many more exosomes compared to our healthy cells because our healthy cells do not multiply as fast as cancer cells do,” said Dr. Ajay Goel, senior author of the study and the chair of the Department of Molecular Diagnostics and Experimental Therapeutics at City of Hope. “And once these exosomes are released by the tumor cells, they circulate in our bloodstream.”
Goel and his colleagues identified eight microRNAs found in exosomes that are shed by cancerous cells in the pancreas and five microRNAs in blood. They used those markers to develop an approach for determining whether a person’s exosomes are associated with pancreatic cancer.
The researchers found that their liquid biopsy approach detected 93% of pancreatic cancers among the US volunteers in their study, 91% of pancreatic cancers in the South Korean cohort and 88% of pancreatic cancers in the Chinese cohort.
The researchers ran their tests again and, this time, not only used their exosome-based markers but also tested for a key protein called CA19-9, known to be associated with pancreatic cancer. When they combined their approach with CA19-9 testing, they were able to accurately detect 97% of stage I and stage II pancreatic cancers in the US volunteers.
“That’s what we are excited about: that not only this test worked beautifully in all stages, but it is 97% accurate in finding those who have either stage I or stage II disease,” Goel said.
He added that the test presented false positive results for stage I and II pancreatic cancers at a rate of less than 5%, the study data showed.
- The information you need to know, sent directly to you: Download the CTV News App
“It’s very important to diagnose the disease at the earliest possible stage, like stage I or II disease, which means there is a higher chance that the cancer is operable surgically,” Goel said. “The best cure for a pancreas patient is not chemotherapy or drugs but to take the cancer out.”
Surgeons may be “very reluctant” to operate when someone has stage III or IV pancreatic cancer, he said. That’s sometimes because of the complexity of such a procedure, the long-term complications and the likelihood that surgery at that advanced stage may not be enough to prevent the cancer from coming back.
“That’s why it is very important that this blood test is so good that it can, 97% of the time, find the cancers at the earliest possible stages where we can intercept the cancer, where we can intervene, and we can surgically remove this cancer effectively,” Goel said.
'We need to do something'
There are blood-based tests for pancreatic cancer that are used in medicine, but they’re often used in people who have already been diagnosed with the disease. Doctors might repeat blood tests during and after treatment to determine how the cancer is responding. But there is no blood test that can detect early pancreatic cancer.
Goel and his colleagues wrote in their abstract that their approach “can potentially be further validated for clinical use in the near future,” specifically for the early detection of pancreatic cancer.
“We were generally excited about these particular data, because the cancer type we’re looking at here is extremely lethal,” Goel said.
“The number of people who are going to be affected with this disease or this cancer is going to continue to go up,” he said. “So we need to do something about it, and that is why we were extremely excited that we have a blood-based liquid biopsy for early detection of pancreatic cancer with this high sensitivity.”
The liquid biopsy test study that Goel and his colleagues presented is “interesting,” Wolpin said, and describes one approach to possibly developing a test for early detection – where there is a big need.
Definitively diagnosing someone with pancreatic cancer can involve a series of scans, blood tests and biopsies, which are typically performed only once someone has symptoms, which may include jaundice or yellowing of the eyes and skin, weight loss, belly or back pain, or tiredness and weakness. But by that point, the cancer is probably advanced.
“The vast majority of patients who present with pancreatic cancer have advanced disease at the time of their diagnosis. So 80% or more of patients present with advanced disease where we know at the time of their presentation, we’re very unlikely to be able to cure the cancer,” Wolpin said.
“That’s very different than many other of the major cancer types like breast cancer or colorectal cancer, where the vast majority of patients actually present with early disease,” he said. “The symptoms from pancreatic cancer are generally less specific, like some abdominal discomfort or sometimes weight loss – things that often don’t immediately trigger people to go to their doctor.”
- Follow the CTV News channel on WhatsApp
But some experts warn that mass testing of average-risk healthy people who are not showing symptoms could lead to false positive results, doing more harm than good.
'The pancreas is a very weird organ'
The City of Hope researchers are not the only scientists hoping to develop a reliable test to diagnose pancreatic cancer patients as early as possible.
In 2020, a study from the University of Pennsylvania found that a blood test to screen for certain biomarkers associated with pancreatic cancer was 92% accurate in its ability to detect disease.
In 2022, a pilot study from researchers at UC San Diego and other institutions found that a blood test to detect proteins associated with cancer cells was able to identify 95.5% of stage I pancreatic cancers among a sample of more than 300 volunteers, among whom 139 were cancer patients and 184 were healthy people.
In general, the field of pancreatic cancer is an area where there has not been much advancement when it comes to either early-stage or advanced disease, said Dr. Al Neugut, a medical oncologist at Columbia University’s Herbert Irving Comprehensive Cancer Center and professor of epidemiology at Columbia University Mailman School of Public Health, who was not involved in any of the liquid biopsy testing research.
“Pancreatic cancer is the poster child for cancers we’ve gotten nowhere with,” Neugut said.
“The pancreas is a very weird organ, and it’s just different than every other organ in the body,” he said. “It’s behind the abdomen, so it’s hard to get to. It’s not easy for a surgeon. It’s not easy for an oncologist. It makes it very difficult even to approach. You can’t examine it physically. It’s hard to get to radiologically. It’s hidden.”
Although pancreatic cancer is rare, people can lower their risk by eating a healthy diet, maintaining a healthy weight, getting regular exercise, avoiding alcohol, limiting exposures to carcinogens and not smoking.
“Smoking is the most important avoidable risk factor for pancreatic cancer,” according to the American Cancer Society.
Still, having some form of test to detect pancreatic cancer early would “dramatically change the landscape” for patients, Wolpin said, adding that he hopes the medical field can achieve developing such a tool.
“The more patients we can find early, the greater the chance we have to cure patients of pancreatic cancer and start to reverse the statistics that are pretty tough – almost 90% of patients who get pancreatic cancer die from their cancer,” Wolpin said. “We really need to change those numbers, and finding the cancer earlier would be a dramatic way to do that.”
CTVNews.ca Top Stories

'Like magic': Total solar eclipse moves across parts of Canada, crowds in awe
Earth-bound audiences turned skyward as the sun moved directly behind the moon on Monday, plunging parts of Canada into the darkness of a total solar eclipse and a moment of shared celestial awe.
4 arrested in connection with murder of 22-year-old in Penticton, B.C.
Police investigating the 2021 murder of a man in Penticton, B.C., have arrested four people in connection with the case, including three who were youths at the time of the killing.
Canada's new 'Our North, Strong and Free' defence policy explained
Announced Monday by Prime Minister Justin Trudeau at Canadian Forces Base Trenton in Ontario, the spending is expected to total just over $8 billion over the next five years and $73 billion in the next two decades for new equipment and infrastructure, including improvements to Canadian air and sea fleets, communications technologies and services for military personnel.
Deportation hearing set for truck driver in deadly Humboldt Broncos bus crash
A deportation hearing for the truck driver who caused the deadly Humboldt Broncos bus crash six years ago has been scheduled for next month.
Alberta minor hockey volunteer charged with alleged sexual offences involving teenage boys
A volunteer with the Sundre Minor Hockey Association faces several charges related to an alleged sexual assault involving teenagers.
WATCH | Time-lapse video shows the solar eclipse across North America
Watch time-lapse video of the solar eclipse as it occurred from Mexico to Canada.
2 dead after daylight shooting in south Edmonton residential neighbourhood
Police are investigating a shooting in south Edmonton over the noon hour on Monday.
Killer Nathaniel Veltman appealing his conviction
Convicted of murdering a London, Ont. Muslim family with his pickup truck, Nathaniel Veltman, 23, has filed an Inmate Notice of Appeal with the court in an attempt to overturn the jury’s verdict.
Here are some highlights from the total solar eclipse in Ontario
Hundreds of people across Ontario looked up to the skies to view the total solar eclipse on Monday – a rare celestial event that will not return for another 120 years.

People across the Maritimes take time to observe historic eclipse
Chris Hadfield was one of thousands of people across the Maritimes who observed the celestial event, which won’t repeat in the region until 2079.
B.C. man sentenced for 'horrific, cowardly' beating death of 78-year-old man
A British Columbia man who burned down his father's home and then kicked to death a 78-year-old stranger on the main street of a quiet mountain town has been sentenced to six and a half years in prison for what the judge described as 'a horrific, cowardly and senseless act of violence.'
Vatican's denouncement of gender-affirming surgery is harmful, LGBTQ2S+ advocates say
The Vatican's declaration that gender-affirming surgery and what it calls gender 'ideologies' violate human dignity is disappointing and 'deeply harmful,' LGBTQ2S+ rights advocates in Canada say.
Parts of southern Quebec have front-row seat for total solar eclipse
People gathered across southern Quebec Monday to get a rare view of a total solar eclipse. Parts of the province will have a front-row seat for the phenomenon, which occurs when the moon passes between the Earth and the sun, blocking out sunlight for a brief period.

Iran's foreign minister accuses U.S. of giving Israel 'green light' to attack consulate in Syria
Iran's foreign minister Monday accused the United States of giving Israel the "green light" for a strike on its consulate building in Syria that killed seven Iranian military officials including two generals.

Prosecutors urge U.S. Supreme Court to reject Trump's immunity claims in election subversion case
Special counsel Jack Smith's team urged the U.S. Supreme Court on Monday night to reject former president Donald Trump's claim that he is immune from prosecution in a case charging him with scheming to overturn the results of the 2020 presidential election.
The Security Council revives the Palestinian Authority's UN hopes. The U.S. says not yet
The UN Security Council on Monday revived the Palestinian Authority's hopes of joining the United Nations as a full member.
'Panama Papers' trial starts. 27 people charged in the worldwide money laundering case
The trial of 27 people charged in connection with the worldwide "Panama Papers" money laundering started Monday in a Panamanian criminal court.
The U.S. Army will hold combat training in the Philippines to hone skills as maritime tensions rise
The U.S. Army is introducing a joint battlefield training in the Philippines to improve combat readiness including by ensuring adequate supply of ammunition and other needs in difficult conditions in tropical jungles and on scattered islands, a U.S. general said.
Overcrowded ferry sinks off Mozambique's coast, leaving at least 98 dead, media reports say
A makeshift ferry overcrowded with residents reportedly fleeing a feared cholera outbreak capsized off Mozambique's northern coast, killing at least 98 people including children, local media said Monday.

MPs clad in eclipse glasses stare at 'surreal' celestial event on Parliament Hill
Not even the vital business of Parliament was enough to keep MPs from slipping outside to glimpse celestial history. Dozens of elected officials, including Conservative Leader Pierre Poilievre, gathered on the Hill to crane their necks skyward.
As Sudan crisis rages, resettlement stalled; groups urge Ottawa to do more to help
Canada has yet to reunite a single family with relatives who are trying to escape conflict-racked Sudan, while diaspora groups are demanding the federal government do more to end a yearlong civil war.

U.S. CDC says bird flu risk low, but asks states to be ready with rapid testing
The U.S. Centers for Disease Control and Prevention said on Monday bird flu risk to the public remains low even as it asked the state public health officials to be prepared to respond.
There's still no standard test to detect pancreatic cancer early. Scientists are working to change that
Finding pancreatic cancer early could help increase a patient’s chances of survival. Across the United States, research teams are investigating ways to spot early cases, with many turning to blood-based liquid biopsy tests.
5 tips for finding the best diet that works for you
With dieting, the conventional wisdom says a person needs to be in calorie-deficit mode to lose weight. If you eat more calories than you burn, you gain weight; if you eat fewer calories, you lose weight.

What an eclipse sounds like -- and why it matters
People will be looking to the sky on Monday to witness a total solar eclipse. Others will be listening to it. And to Harvard University astronomers working to transform the rare sight into sound, the eclipse should create a symphony.
Why this year's eclipse is different from the last one in 2017
In addition to being a rare phenomenon, Monday's total solar eclipse is different than the last one visible from North America in 2017 for a few reasons.
Vancouver-based Hootsuite buys analytics firm Talkwalker as CEO foresees social media disruption
When Irina Novoselsky contemplates social media, she's certain the next decade won't be anything like the last because consumers increasingly allow the online world to shape nearly every aspect of their lives.
Entertainment


Beyonce makes history with 'Country Carter' hitting No. 1
Beyoncé may have proclaimed that her latest project "ain't a country album," but someone forgot to tell the charts that.
'Total Eclipse of the Heart' searches surge on Spotify
A Spotify representative told CNN that searches for Bonnie Tyler's song have soared by nearly 50 per cent in the U.S. over the past week.
Jelly Roll shares update after his jet's emergency landing
Country music star Jelly Roll has recovered from a flight scare over the weekend.

Doug Ford directs LCBO to go back to using single-use paper bags
Paper bags could soon return to the LCBO following a request from Ontario’s premier.
Trump's net worth has tumbled by US$2 billion since Truth Social stock peaked last month
The Truth Social owner dropped by another 8 per cent on Monday, adding to a brutal week that wiped out a third of the stock's value.

This hidden Eden in Mexico won't stay undiscovered forever
The remote landscapes of La Huasteca Potosina – part of the larger La Huasteca region spanning multiple states – include vast desert, lush mountains and rainforest nooks with turquoise rivers and waterfalls. And the attractions within remain unknown to most international travellers – for now, at least.
'You're the chef': Fast-food chains embrace menu hackers' creative combinations
Some are as simple as coating chicken nuggets in a blend of barbecue and ghost pepper sauces — nicknamed "cowboy caviar" — but others take things to a new level, like dropping pie or mini cinnamon sugar doughnuts into a milkshake or ensconcing a hotdog in onion rings.

Toronto Blue Jays defeat Seattle Mariners in home opener at Rogers Centre
The Toronto Blue Jays defeated the Seattle Mariners Monday night in their home opener at the newly renovated Rogers Centre.
Novak Djokovic eclipses Roger Federer's record for oldest man ranked No. 1 in tennis
Novak Djokovic has surpassed another tennis record once held by Roger Federer, becoming the oldest man to be ranked No. 1 in the ATP Tour's computerized rankings.
Canada's swim trials shift to Toronto from Montreal because of fire, pool closure
Canada's Olympic and Paralympic swim trials have been moved from Montreal to Toronto.

Tesla settles case over fatal Autopilot crash of Apple engineer
Tesla has settled a lawsuit over a 2018 car crash that killed an Apple engineer after his Model X, operating on Autopilot, swerved off a highway near San Francisco, court documents showed on Monday.
NEW | What are the chances police can find your stolen car? Canadians believe odds are low
A new poll from Nanos Research for CTV News has found that a majority of Canadians doubt the police are able to recover stolen cars.
Elon Musk announces Tesla will unveil a 'robotaxi' on August 8
Elon Musk has long had an affinity for self-driving vehicles, claiming they will be one of Tesla's most important products. Despite big promises, years have gone by without cars that can, so far, drive on their own.
Local Spotlight

Couple lucky to be alive after piece of Montreal highway crashes into their windshield
A Montreal couple is having a hard time driving without stress and is unhappy with the city's maintenance after a chunk of highway crashed into their windshield while driving on Thursday night.
Star Trek superfan turns his home into a Trekkie’s dream
As many Star Trek fans may know, Friday was “First Contact Day,” but one superfan got to spend the day in his own starship.
'Like an underwater puppy': B.C. woman forms lasting friendship with octopus
When Catherine Dobrowolski began doing daily walks by the water, she never expected to make an eight-legged friend.
Ground-breaking Canadian giraffe researcher Anne Innis Dagg dies at 91
Pioneering Canadian giraffe researcher and feminist activist Anne Innis Dagg has died at the age of 91.
Merlin the Macaw leaving Halifax for Ontario due to depression and stress
According to a news release from the Maritime Museum of the Atlantic, Merlin the Macaw, a resident mascot for the facility, is flying off to Safari Niagara in Fort Erie, Ontario.
Ontario family's car stolen from parking lot of Montreal hotel
A family from Ontario says their SUV was stolen from a hotel parking lot in Montreal while the family was on a March break vacation down south.
Ottawa snowbirds embark on epic bicycle journey back to Canada
Two adventurous snowbirds have embarked on an amazing journey back to Canada, and they're inviting the world to join in on their adventure.
'I'm indebted to these guys': First responder, former cop save N.S. man's life in hockey rink
A first responder and a former police officer saved a Nova Scotia man's life as he suffered a heart attack on ice in March.
'Pretty remarkable': Alberta distillery beats out Ireland, Scotland at international whisky competition
A distillery in Parkland County is being internationally recognized for outstanding whisky production – and one bottle in particular is getting all the attention.

Suspects traded street drugs for safer supply outside B.C. pharmacy, police say
Prince George RCMP say after multiple days of investigation, including surveillance outside one of the city’s pharmacies, officers arrested two people who had been offering illicit drugs in exchange for safer supply opioids.
Concerns about alleged kickback scheme leads to investigation of CleanBC grants
A Merritt-based company that makes electric logging trucks says it hasn't received a CleanBC grant and is raising concerns about the accounting firm tasked with administering them.
Don't let the weather get you down, there will be a total eclipse over B.C. in 2099
A total eclipse was never in the cards for Metro Vancouver on Monday, but it was so overcast that even catching a glimpse of the moon taking a so-called "bite" out of the sun was impossible.
Toronto police officer seriously injured while making an arrest in North York: TPS
A Toronto police officer has been injured while making an arrest in North York on Monday night, say police.

'It does kind of put you in your place': Calgary comes out to catch glimpse of solar eclipse
Thousands of Calgarians flocked to the University of Calgary on Monday to get a glimpse of the solar eclipse.
Stampede Elm comes down after more than 125 years
A big elm tree that had grown in the parking lot of the Calgary Stampede grounds for more than 125 years was cut down on Monday.

SOLAR ECLIPSE | Historic solar eclipse brings breathtaking views across eastern Ontario
Thousands of people gathered as a solar eclipse moved across eastern Ontario Monday afternoon, achieving totality in several communities.
SOLAR ECLIPSE | Scenes from the solar eclipse across eastern Ontario
Thousands are gathering across eastern Ontario in preparation for a solar eclipse that will begin moving through the province at 2 p.m.
Tractor trailer driver seriously injured after crash on Hwy. 417
Ottawa paramedics say the driver of a tractor trailer had to be airlifted to hospital after a crash on Highway 417 Monday afternoon.

No charges in pedestrian's death in St-Michel
A 54-year-old truck driver will not be charged in the death of a pedestrian last June after a Quebec coroner's report and recommendations.
Father of boy killed by dogs calls media attention 'brutal,' urges kindness for dogs' owner
The father of a boy killed by two dogs on Monday says he saw no indication the animals were a danger to his son.
Recovery-based Alberta drug-addiction treatment model limits options: critic
Dan Williams, Alberta's minister of mental health and addiction, defends the recovery community model despite deaths from all substances increasing by 130 per cent since the governing UCP party took office in 2019.
Everything you need to know about solar eclipses
The eclipse moved over a large swath of North America and during the brief period when the moon totally covered the sun, day transformed to night with a show of streamers and magnetic loops dancing around the sun.
New Glasgow police ask for the public’s help locating missing senior
The New Glasgow Regional Police is asking for the public’s help locating 73-year-old Adair Townsend.

'Significant adverse environmental effects’ on Indigenous peoples: Outlet Channels draft report
'magical feeling': manitobans take in partial solar eclipse.
Manitobans gathered to watch a rare celestial event on Monday.
Takeoff: WestJet increasing flights from Winnipeg to Montreal and Ottawa, adds direct Nashville route
If you’re looking to fly out of Winnipeg Richardson International Airport, you’ll now have more flight options.

Sask. RCMP use spike strip to stop stolen vehicle near Edgeley
An investigation into a stolen vehicle ultimately led to RCMP deploying a spike strip to end a pursuit near Edgeley, Sask.
In Pictures | Here's what Monday's solar eclipse looked like in Saskatchewan
Monday's solar eclipse was only partial in Saskatchewan, but with proper eyewear it was still possible to see the moon crossing paths with the sun during the early afternoon hours.
Why did the fish cross the road? Here's why
The Arm River low level crossing was host to a fascinating sight over the weekend — as schools of determined fish made their journey upriver.

Watching the solar eclipse in Waterloo Region and Guelph
People across Waterloo Region - and beyond - had their eyes on the skies for Monday's solar eclipse.
Tributes to Ontario couple killed in Swiss avalanche
Capt. Sean Thomas and Nicole Nagy were snowboarding in Switzerland over the Easter long weekend when both presumably died in an avalanche.
‘EePispe 2024’: Eclipse cake gone wrong in Kitchener, Ont.
A work party in Kitchener, Ont. may not have gotten the eclipse-themed cake they were hoping for.

Saskatchewan residents looked to the skies. Some saw mostly clouds
Crowds of people across Saskatchewan were outside on Monday hoping to catch a glimpse of the rare celestial spectacle that made news across the continent.
Saskatoon property 'crawls' with swarms of maple bugs
Bob Muckalt rarely had to deal with maple bugs before he and his wife Rita bought their home in Confederation Park in 2021.
Northern Ontario

Here's what the total solar eclipse looked like at its peak in Ontario
Though the skies clouded the total solar eclipse as it peaked through Toronto, several onlookers still donned their certified solar shades to view the 'once-in-a-lifetime' celestial event.
Drunk Sudbury man arrested trying to hitchhike on Hwy. 400
A 37-year-old Sudbury man heading to the airport Sunday with his buddies for a trip south ended up in the holding cells of the Southern Georgian Bay OPP detachment.
Men who started Sudbury fire that killed three people testify at murder trial
A murder trial in Sudbury will continue Tuesday with testimony of one of the men who admitted to starting the fire that killed three people.

London, Ont. jury hears disturbing evidence at child abuse case involving parents
A London, Ont. jury heard horrific testimony Monday surrounding the alleged abuse of several children at the hands of their mother and father.
Brief totality reached for solar eclipse in Tillsonburg
According to NASA's calculations, the total eclipse will began to peak in Canada in the minutes before 3:15 p.m. local time for communities near the north shore of Lake Erie in southwestern Ontario

Limo passenger taken to jail rather than airport after arrest on Highway 400
Police say a man on his way to the airport in a limo with his friends wound up in a holding cell over the weekend instead.
Malnourished, frostbitten pups rescued by Barrie organization in dire need of donations
A non-profit animal rescue organization in Barrie that relies on community generosity recently saved a distressed young lab and her 12 puppies from northern Manitoba.
Orillia native looks for hometown support to propel her to next big break
A singer with deep roots in the Sunshine City hopes some hometown support can help propel her to her next big break.

Solar eclipse 2024 impresses crowds in Windsor-Essex
As the total solar eclipse fell over parts of southwestern Ontario Monday, many residents watched online and in person across the region.
Windsorite convicted in grisly 2004 murder of taxicab driver wants early parole
Ali Al-Shammari, 38, has been in prison since 2007 after being convicted of first-degree murder by a jury.
Vancouver Island

Searchers say 21-year-old still missing after empty kayak found on Vancouver Island
Searchers are scouring a remote section of northwestern Vancouver Island after a kayak was recovered over the weekend with no sign of its 21-year-old occupant.
Major redevelopment pitched for Victoria's waterfront around the Capital Iron building
Reliance Properties owns the land spanning from the waterfront, through the Capital Iron building and up to Government Street, and is looking to redevelop it.

Evacuation of Kelowna, B.C., apartment near construction site extended for two weeks
More than 80 residents from a low-income apartment building in Kelowna, B.C., have learned they won't be able to return to their homes for at least another two weeks.
2 men injured after 'road rage' incident with Dodge Ram driver, Kelowna RCMP say
Mounties are investigating a reported "road rage" incident in Kelowna, B.C., that left two men injured last week.
Unstable nearby construction site forces evacuation of apartment in Kelowna, B.C.
More than 80 residents of a low-income apartment building in Kelowna, B.C., have been told they need to leave over a 'significant' risk to life and safety.

'Our place in the universe': Southern Albertans take in partial solar eclipse
Whether through a telescope or solar viewing glasses, southern Albertans were treated to a 30 per cent partial solar eclipse Monday.
'Not pleased with the result': Lethbridge Hurricanes looking ahead to next season after first-round exit
The Lethbridge Hurricanes were bounced out of the playoffs earlier this week by the Swift Current Broncos after a double-overtime thriller.
'Hasn't lost its momentum': Green Shirt Day continues to inspire 6 years after Humboldt Broncos crash
This Saturday marks the sixth anniversary of the Humboldt Broncos bus crash and the start of Green Shirt Day, honouring the legacy of Logan Boulet.
Sault Ste. Marie

After ‘disastrous’ winter, Sault tourism officials hope for strong summer
As we near summer, northern tourism officials are taking stock of the winter that was (or wasn’t) and looking to the next busy season for the industry.
Sault driver clocked at 108 km/h in a 50 km/h zone
On April 5, officers with Sault police charged a 23-year-old resident with stunt driving under the Highway Traffic Act.
SPONSORED | Get your car ready for spring with these 7 tips
While winter car maintenance often takes center stage, neglecting spring preparations can lead to potential issues down the road. Here’s how you can get your car ready for spring while maximizing your savings with a CAA Membership.

On an island off Newfoundland's coast, a solar eclipse is part of history
Lego takes over newfoundland's biggest museum.
Newfoundland's biggest museum has transformed into a giant Lego playground, featuring designs made by creators young and old.
Mysterious Newfoundland shipwreck finally out of the water
It took a few cuts with a chainsaw and the full strength of a 30-ton excavator, but a mysterious Newfoundland shipwreck has finally been pulled out of the water near the small community of Cape Ray.
Shopping Trends
The Shopping Trends team is independent of the journalists at CTV News. We may earn a commission when you use our links to shop. Read about us.
Editor's Picks
14 of the best interactive dog toys to stimulate your dog's mind, if you're ready to dip your toes into spring cleaning, you'll want to order at least one of these amazon products, 15 awesome presents to give if you're tired of gift cards, our guide to the best knee pillows in canada in 2024 (and where to get them), our guide to the best charcoal grills in canada in 2024 (and where to get them), 20 gifts that are so great, you'll want to keep them for yourself, 19 of the best mother's day gifts under $50, if you're on the hunt for a retinol serum, here are 12 that reviewers are loving right now, rosemary oil and 11 other products that reviewers swear by for hair growth, if you hate hate razors and waxing, allow me to introduce you to your new favourite at-home hair removal devices, stay connected.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Cancers (Basel)

Nutritional Interventions in Pancreatic Cancer: A Systematic Review
Aline emanuel.
1 Division of Nutrition Sciences, German University of Applied Sciences for Prevention and Health Management (DHfPG), 66123 Saarbruecken, Germany; ed.asb-gpfhd@leuname-a
Julia Krampitz
2 Division of Psychology and Pedagogy, German University of Applied Sciences for Prevention and Health Management (DHfPG), 66123 Saarbruecken, Germany; ed.asb-gpfhd@ztipmark-j
3 Institute of Psychology, University of Innsbruck, 6020 Innsbruck, Austria
Friederike Rosenberger
4 Department of Medical Oncology, National Center for Tumor Diseases (NCT), Heidelberg University Hospital, 69120 Heidelberg, Germany; [email protected]
5 Division of Health Sciences, German University of Applied Sciences for Prevention and Health Management (DHfPG), 66123 Saarbruecken, Germany; ed.asb-gpfhd@dnik-s
Sabine Kind
Ingeborg rötzer.
6 Clinic for Oncology and Haemotology, Northwest Hospital, UCT-Cancer University Center, 60488 Frankfurt am Main, Germany
Associated Data
Simple summary.
This systematic review investigates the impact of nutritional interventions on cachexia, malnutrition and weight loss in patients with pancreatic cancer. In total, 26 studies were included. Parenteral nutrition is associated with a higher incidence of complications. Enteral nutrition shows positive effects on length of stay in hospital, complications, weight loss and cytokines. Dietary supplements enriched with omega-3 fatty acids improve body weight and lean body mass. Considering the heterogeneous study situation as well as the high bias potential of the included RCTs, a recommendation for enteral nutrition and dietary supplements with omega-3 fatty acids can be given.
(1) Background: Pancreatic cancer (PaCa) is directly related to malnutrition, cachexia and weight loss. Nutritional interventions (NI) are used in addition to standard therapy. The aim of this systematic review is to provide an overview of the types of NI and their effects. (2) Methods: We included RCTs with at least one intervention group receiving an NI and compared them with a control group with no NI, placebo or alternative treatment on cachexia, malnutrition or weight loss in patients with PaCa. Any available literature until 12 August 2021 was searched in the Pubmed and Cochrane databases. RCTs were sorted according to NI (parenteral nutrition, enteral nutrition, dietary supplements and mixed or special forms). (3) Results: Finally, 26 studies with a total of 2720 patients were included. The potential for bias was mostly moderate to high. Parenteral nutrition is associated with a higher incidence of complications. Enteral nutrition is associated with shorter length of stay in hospital, lower rate and development of complications, positive effects on cytokine rates and lower weight loss. Dietary supplements enriched with omega-3 fatty acids lead to higher body weight and lean body mass. (4) Conclusions: Enteral nutrition and dietary supplements with omega-3 fatty acids should be preferred in nutritional therapy of PaCa patients.
1. Introduction
Pancreatic cancer (PaCa) has a poor overall prognosis, with a 5-year survival rate of 9% and a median survival time of 6 months [ 1 ]. However, patients with early tumour resection have a higher chance of remission, with a 5-year survival rate of 25% and a median survival of 14–20 months [ 2 , 3 , 4 ]. Patients often suffer from tumour cachexia [ 5 , 6 ], which is manifested in weight loss [ 7 , 8 ], malnutrition [ 9 , 10 , 11 , 12 ] and systemic inflammation [ 13 ]. A large proportion of patients have already lost 10% of body weight at initial diagnosis [ 7 , 8 ]. There is an association between malnutrition and, among other things, poorer quality of life [ 14 ], postoperative complications [ 15 , 16 ] and higher mortality risk [ 15 ]. A prospective multicentre cohort study showed that 71% of PaCa patients had cachexia at time of diagnosis, but only 56% of them received nutritional counselling [ 17 ]. Therefore, it is an important goal to improve the nutritional status and so prevent or counteract cachexia [ 18 ].
Cachexia is not consistently defined in the literature. It is often defined as weight loss ≥5% in ≤12 months (or body mass index (BMI) <20 kg/m²) and the presence of three of the following five criteria: decreased muscle strength, fatigue, anorexia, low fat-free mass index, abnormal biochemistry (increased inflammatory markers (CRP, IL-6), anaemia (Hb < 12 g/dL), low serum albumin (<3.2 g/dL)) [ 19 ]. Independent of cachexia, a weight loss ≥5% caused by malnutrition is also seen to be significant [ 20 , 21 , 22 , 23 , 24 ]. Malnutrition is defined as a weight loss >5% within past 6 months or 10% beyond 6 months; mild to moderate loss of muscle mass; reduced food intake ≤50% of estimated requirements for >1 week or any reduction of >2 weeks; or the presence of chronic gastrointestinal disease that negatively affects food intake or absorption [ 25 ]. Furthermore, a chronic disease such as cancer or other diseases must be present [ 25 ]. However, the crucial criterion to distinguish cachexia from disease-related malnutrition is the inflammatory process [ 26 ]. The systemic inflammation is triggered by cytokines and tumour-derived factors. Increased serum CRP, IL6 and growth differentiation factor-15 are associated with cachexia [ 19 , 27 ]. Figure S1 shows factors of tumour cachexia. Malnutrition in the preoperative setting of gastrointestinal cancers has been identified as an independent risk factor for mortality [ 28 ]. Weight loss can lead to immunodeficiency, which in turn increases the risk of infection [ 29 ].
Different nutritional interventions (NI) exist to counteract cachexia or malnutrition in patients with PaCa. These are parenteral nutrition (PN), enteral nutrition (EN), dietary supplements (DS) and mixed or special forms. In PN, nutrients are applied directly into the bloodstream, bypassing the digestive tract, thereby supplying them to the metabolism [ 30 ] (p. 555). In EN, a special liquid food mixture is given through a tube into the gastrointestinal tract. DS are pills, capsules, tablets, powder, sip feed nutrition or liquids to supplement diet. The individual components are part of the normal diet and are intended to supplement it if they are not sufficiently available for certain reasons [ 30 ] (p. 128). Mixed or special forms are NI that are composed of different interventions mentioned above or represent special forms such as nutritional counselling or fasting. These are used before (pre), during (peri), after (post) or even without connection to a surgical procedure.
The current data situation regarding NI in cachectic patients is referred to as “wildfire” [ 31 ]. Comprehensive reviews of different types of interventions and their impact on malnutrition and cachexia in PaCa are few and sometimes only address specific nutrients such as omega-3 fatty acids [ 32 , 33 , 34 , 35 ]. A narrative review focusing on the efficacy of NI in cachectic PaCa patients concluded that nutritional counselling, to increase energy and protein intake, should be the first step, followed by DS and PN [ 36 ]. Two reviews in gastrointestinal cancer/PaCa patients examined the development of postoperative infectious complications and the postoperative and immunology outcome parameters and showed a significant reduction in postoperative infectious complications and shorter length of stay in the hospital with preoperative immunonutrition [ 37 , 38 ]. Another systematic review in patients undergoing pancreaticoduodenectomy focused on the perioperative nutritional supplementation concluded that attention should be paid to preoperative nutritional optimization and nutritional support should be delivered in the postoperative period with cyclical enteral nutrition [ 32 ]. A narrative review in patients with cancer-associated cachexia focused on a diet in relation to the treatment of cancer-associated cachexia and shows that a multimodal therapy consisting of a combination of exercise, nutrition and/or other measures seems to be gaining importance [ 39 ]. This interdisciplinary approach is confirmed by another review looking at patients with cancer cachexia and focusing on the diagnostic criteria and therapeutic approaches of cancer cachexia [ 40 ]. The ESPEN Guidelines recommend nutritional assessment for all cancer patients at diagnosis and provision of appropriate nutritional support (preferably nutritional counselling followed by artificial nutrition (EN, PN)) according to need [ 41 ]. Altogether, the body of literature on the effects of different NI in patients with PaCa is complex, heterogeneous and often unclear.
Therefore, the aim of this systematic review was to summarize the effects of different NI (PN, EN, DS, mixed or special forms) in PaCa patients on cachexia, malnutrition and weight loss. Because of the poor data situation regarding NI in PaCa, parameters associated with the nutritional status such as immunology and complications should be included. Furthermore, recommendations for clinical practice should be derived if appropriate.
2. Materials and Methods
This systematic review was prepared following the PRISMA guidelines [ 42 ] as well as the Cochrane collaboration guidelines [ 43 ]. The protocol was registered in PROSPERO database (CRD42021270502) on 29 August 2021.
2.1. Search Strategy
All available literature (from 1957) to 12 August 2021 was searched in Pubmed and Cochrane library databases by two independent researchers. A hand search of the bibliographies of the selected papers was also conducted. The search strategy was defined using the PICO scheme [ 44 ]:
- P(opulation): pancreatic cancer patients;
- I(ntervention): nutrition intervention (PN, EN, DS, mixed or special forms);
- C(omparison): no nutrition intervention or placebo or alternative treatment;
- O(utcome): malnutrition or cachexia or weight loss.
Malnutrition and cachexia were defined as a weight loss or BMI < 20 kg/m². Furthermore, criteria closely related to cachexia or malnutrition (e.g., decreased muscle strength, fatigue, anorexia, low fat-free mass index, abnormal biochemistry (increased inflammatory markers (CRP, IL-6), anaemia (Hb < 12 g/dL), low serum albumin (<3.2 g/dL) [ 19 ]) were also included.
Due to the complex definitions of cachexia, malnutrition and weight loss, surrogate parameters to nutritional status (weight loss and parameters of bioelectrical impedance analysis (BIA)), immunology (cytokines, C-reactive protein (CRP), albumin) and complications (infections, mortality, length of stay in hospital) were used as additional outcomes in order to represent a large database.
The search term was (Nutrition* OR Diet* OR Supplement*) AND ((Pancrea* Cancer) OR (Pancrea* Carcinoma) OR (Pancrea* Tumour) OR (Pancrea* Neoplasm)) AND (Malnutrition OR Cachexia OR (Weight Loss)).
2.2. Eligibility Criteria
We included studies in humans with PaCa (incl. periampullary tumours) or several types of cancer including PaCa. The studies needed to be randomized controlled trials (RCTs) with at least one intervention group receiving an NI and compared with a control group with no NI, placebo or alternative treatment on cachexia, malnutrition or weight loss and their surrogate parameters described above. Further inclusion criteria were: patients ≥ 18 years of age, published in full text in English, of all publication years.
Studies were excluded if pancreatic enzyme replacement therapy was the only NI or just the risk of developing PaCa was investigated. Duplicates were also excluded.
2.3. Study Selection
The studies were imported in Citavi literature management program. The two independent reviewers (A.E. and J.K.) screened the titles and abstracts and in the next step the full texts to filter them against inclusion and exclusion criteria.
2.4. Quality Criteria
Primary endpoints of included RCTs were checked for quality criteria by two independent reviewers (A.E. and J.K.) using the Cochrane Collaboration tool (RoB2) for assessing bias risk [ 43 ]. In case of disagreement, a third reviewer was consulted for assistance (S.K.). No studies were excluded based on quality assessment.
2.5. Data Extraction and Analysis
The following data were extracted from the full texts: entity(ies), sample characteristics, description of nutrition intervention(s), outcome(s), results.
Due to considerable statistical and methodological heterogeneity (e.g., different length and type of intervention), a random-effect meta-analysis could not be performed. The studies were sorted by NI (PN, EN, DS, mixed and special forms). The intervention nutritional counselling was integrated in mixed and special forms, as the current study situation shows a trend towards individualized nutritional counselling.
Outcomes are presented as reported by the authors.
3.1. Overview
A Prisma flow diagram is given in Figure 1 . In Pubmed, 43 trials were found, and in the Cochrane database, 144 trials were found. After a duplicate check, 31 were excluded. Titles of 156 papers were screened, of which 129 were excluded due to inappropriate subject matter. This left 27 trials from which the abstracts were checked. Ten abstracts were excluded because they were thematically unsuitable. Seventeen full texts were reviewed, and two trials were excluded because of the randomization scheme and no difference between NI in intervention and control group. Fifteen trials were included from the database search.

Prisma flow diagram.
Further, 11 trials were included through a manual search of the bibliographies of the searched trials, so that a total of 26 RCTs were considered in the review.
All trials are presented in tabular form. They are described in more detailed in the text and assessed according to risk of bias as described above.
The characteristics of the included studies are given in Table 1 . The systematic review included 2720 patients across the selected studies (PN: n = 277; EN: n = 981; DS: n = 528; mixed/special forms: n = 934). The average age was 65 years (PN: 62 years; EN: 64 years; DS: 68 years; mixed/special forms: 68 years). Of all of the subjects, 57% were male (PN: 56%; EN: 64%; DS: 53%; mixed/special forms: 51%). The average BMI was 22.5 kg/m² (reported in 54% of the included studies) (PN: 26.0 kg/m²; EN: 21.3 kg/m²; DS: 22.3 kg/m²; mixed/special forms: 23.3 kg/m²). In terms of entities, nine studies (35%) looked at PaCa alone. Fourteen studies (54%) were included that looked at other cancer types in addition to PaCa. Three studies (11%) looked at periampullary tumours. Of mixed-entity studies, all results are reported.
Characteristics of included studies.
BMI: body mass index; BW: body weight; CG : control group; CoCa: colon cancer; DHA: docosahexaenoic acid; EN: enteral nutrition; EPA: eicosapentaenoic acid; FO: fish oil; GaCa: gastric cancer; HEN: home-enteral nutrition; IG : intervention group; IN: immunonutrition; LOS: length of stay in hospital; MCT: medium-chain triglyceride; MPL: marine phospholipids; n.a.: data not available; NI: nutritional intervention; OeCa: oesophagus cancer; PaCa: pancreatic cancer; PN: parenteral nutrition; RNA: ribonucleic acid; SAFA: saturated fatty acid; WL: weight loss.
3.2. Parenteral Nutrition
Three RCTs were included that did not have common outcomes (see Table 2 ) [ 51 , 60 , 63 ]. The timing of intervention ranged from 2 days before to 5 days after surgery.
Randomized controlled trials of parenteral nutrition.
BIA: bio impedance analysis; CG: control group; IG : intervention group; LOS: length of stay in hospital; PaCa: pancreatic cancer; TPN: total parenteral nutrition; WL: weight loss.
Regarding effects on our category nutritional status, one RCT investigated the effects of PN adapted with vitamins and trace elements on fasting days vs. an isotonic electrolyte solution on fasting days on body weight and weight gain [ 63 ]. There was no difference in the weight change from hospital admission to discharge between groups when medians were compared ( p = 0.217). However, a multivariate regression analysis adjusted for nine potential influencing factors revealed a significant advantage for the intervention group ( p = 0.027).
Two studies examine the impact of parenteral nutrition on the occurrence of complications according to our definition from Brennan et al. (1994), who compared total parenteral nutrition (TPN) with macro- and micronutrients in an intervention group with dextrose-containing saline (without TPN) to a control group on survival, complications, mortality, reoperation and length of stay in hospital. There was no significant difference in median survival between groups ( p = 0.25). Further, there was no significant difference in minor complications between groups ( p = 0.30). However, major complications and severe complications occurred more often in the intervention group compared to the control group ( p = 0.02 and p = 0.01). PostOP mortality ( p = 0.17) and reoperation rate ( p = 0.18) were not significantly different between groups. The authors concluded that there is no justification for administration of a TPN after pancreatic resection.
The second trial in our category complications investigated the effects of a parenteral amino acid supplement (+glutamine) vs. an isonitrogen parenteral amino acid supplement on patients after pancreaticoduodenectomy [ 60 ]. They concluded that median postOP length of stay in hospital was similar between groups ( p = 0.197). The study was stopped halfway through because the glutamine solution was no longer available.
In summary, parenteral nutrition appears unlikely to lead to weight change and seems to result in a higher chance of postoperative complications.
3.3. Enteral Nutrition
Ten RCTs with EN could be included (see Table 3 ) [ 49 , 52 , 55 , 56 , 58 , 61 , 62 , 64 , 65 , 69 ]. Studies were conducted very differently with regard to the start of the intervention which ranged from 14 days before to 16 weeks after surgery.
Randomized controlled trials of enteral nutrition.
BIA: bio impedance analysis; CG: control group; CoCa: colon cancer; CRP: C-reactive protein; GaCa: gastric cancer; IG: intervention group; LOS: length of stay in hospital; OeCa: oesophagus cancer; PaCa: pancreatic cancer; POD: postoperative day; WL: weight loss.
In our category nutritional status, one trial calculated EN according to Harris and Benedict’s energy requirements vs. nutritional counselling by a dietician with recommendations on energy and protein requirements. The intervention group showed a lower weight loss vs. control group after 2 months ( p =0.0031) [ 56 ].
In our category immunology, two trials looked at cytokines [ 58 , 69 ]. The first trial investigated postoperative enteral immunonutrition with glutamine and arginine vs. standard EN [ 69 ]. They showed higher concentrations of IL-6 (on day 10 postOP p = 0.017), IL-8 (on day 1 postOP: p = 0.01; on day 3, 7, 10 postOP: p < 0.001), IL-10 (on day 3 and 10 postOP: p < 0.001), IL-1RA (on day 7 postOP: p < 0.001; on day 10 postOP: p = 0.002) and a significant increase in total lymphocyte count ( p = 0.003) in the intervention group compared to the control group. The control group showed significantly higher levels of proinflammatory cytokines such as IL-1ß (on day 7 postOP: p < 0.001) and TNF-α (on day 3 postOP: p = 0.006; on day 7 postOP: p < 0.001). The increase in total lymphocyte count indicates a better nutritional status and less malnutrition in the intervention group. The second trial [ 58 ] showed, after 14 days of preoperative standard nutritional supplementation with Fresubin ® vs. immune-boosting nutrition Impact ® , no significant difference in IL-1-α ( p = 0.529) and TNF-α ( p = 0.112) between groups, but a significant decrease in TNF- α in the intervention group over period of 14 days (day 14 preOP until day of OP) ( p = 0.047).
In our category complications, seven RCTs looked at postoperative complications (+length of stay in hospital [ 49 , 52 , 55 ]). Braga (1999) and Daly et al. (1995) compared an enteral formula diet as a standard diet with an enteral formula and a complementary diet. In Braga (1999), this diet was with a supplement of arginine, RNA as well as omega-3 fatty acids. In Daly et al. (1995), this comparison was conducted during hospitalization and afterwards in the outpatient sector compared with no outpatient therapy. Braga (1999) showed that postOP infectious complications occurred more frequently ( p = 0.02) and length of stay in hospital was longer ( p = 0.01) in the control group compared to the intervention group. Daly et al. (1995) showed significant frequent development of major postoperative infections/ wound complications ( p < 0.005) and longer length of stay in hospital ( p <0.05) in the control group. Gade et al. (2016) compared preoperative immunonutrition with no nutritional therapy (clinical standard). There was no significant difference in postoperative complications ( p > 0.05). The authors showed a significantly larger number of participants with more than three postoperative complications in the control group ( p = 0.030). For the second primary outcome, length of stay in hospital, there was no significant difference between groups ( p = 0.549). A further trial with fat-free elemental feeding via a tube ( IG : 3 months postOP vs. CG : until oral intake was achieved) showed that the cumulative readmission rate at 3, 6, 12 and 24 months postOP was significantly lower in the intervention vs. control group ( p = 0.018), which did not receive long-term nutrition therapy [ 65 ]. There was a significant increase in readmission rate in the control group vs. intervention group at 90 days ( p = 0.047), 6 ( p = 0.044) and 12 months ( p = 0.065) postOP. Further trials compared an immunostimulatory EN after surgery with a standardized EN [ 61 , 64 ] (+ isonitrogenous, isocaloric diet [ 64 ]) on postoperative complications/infectious complications. Klek et al. (2008) showed no significant differences in postoperative complications between groups ( p > 0.05). The authors stated that despite adequate patient compliance, immunostimulatory EN had no effect on the primary outcome. Lobo et al. (2006) reported no significant differences in infectious complications ( p = 1.0). The authors conclude that there is no outcome benefit for patients. Klek et al. (2011) [ 62 ] showed a significantly lower rate of infectious complications in the intervention group with enteral immunonutrition compared to standard enteral nutrition ( p = 0.04).
In summary, nutritional status and especially weight loss was significant lower after 2 months of EN vs. a nutritional counselling alone. Cytokine levels significantly differed only in some studies. Infectious complications were lower in some trials when enteral immunonutrition enriched with immunomodulating substances such as omega-3 fatty acids and special amino acids were compared to standardized EN. Some trials could not confirm this and showed no significant differences between groups. Some trials showed significantly lower length of stay in hospital in the intervention group, but not all.
3.4. Dietary Supplements
Seven RCTs in the field of dietary supplements could be included (see Table 4 ) [ 46 , 47 , 50 , 53 , 54 , 66 , 70 ]. The timing of interventions varied from 7 days before until 8 weeks after surgery.
Randomized controlled trials of dietary supplements.
BIA: bio impedance analysis; CG: control group; CoCa: colon cancer; CRP: C-reactive protein; GaCa: gastric cancer; IG: intervention group; NS: not significant; PaCa: pancreatic cancer; POD: postoperative day; WL: weight loss.
In our category nutritional status, five trials were included. They examined the effects of a dietary fortification with omega-3 fatty acids [ 46 , 47 , 54 , 66 , 70 ]. Three RCTs looked at the effects of a dietary supplement with protein and energy and enriched with omega-3 fatty acids compared to a isocaloric isonitrogenous dietary supplement on body weight or change in body weight [ 54 , 66 , 70 ]. One trial [ 54 ] observed that body weight and lean body mass remained stable and did not differ significantly between groups ( p = 0.74, p = 0.88). Furthermore, this study showed a significant correlation between supplement intake and weight gain ( p < 0.001) and increase in lean body mass ( p = 0.036) within the intervention group. Another trial looked at body weight and body composition with a dietary supplement high in protein and energy and enriched with omega-3 fatty acids vs. an isocaloric isonitrogenous supplement without omega-3 fatty acids [ 47 ]. There was no significant difference in weight change during the eight weeks of intervention ( p = 0.052). Another trial looked at weight change [ 70 ] compared to omega-3 fatty acids from fish oil or from marine phospholipids and showed no difference between the groups. Nevertheless, a significant weight stabilization after 6 weeks in comparison to the weight loss before the study within both groups was observed (IG: p = 0.001, CG: p = 0.003). The third trial [ 66 ], which compared dietary supplements with and without omega-3 fatty acids, was also unable to show any significant differences in change in body weight and lean body mass between groups (p reported as NS). One older trial compared a high- with a low-calorie standard diet (IG: 2000 kcal protein enriched diet vs. CG: 1300 kcal) on weight loss/weight change [ 53 ]. They reported that weight loss was lower in the intervention group ( p not reported) when only pancreatic patients were considered but weight change during therapy was higher in the intervention group when all patients were considered, because weight loss in patients with gastric and colorectum cancer were higher ( p not reported).
In our category immunology, two trials were included [ 46 , 50 ]. The first looked at serum concentration of IL-6 with a preOP EPA fortified diet (dietary oral supplement) with 1200 kcal vs. a standard diet, isocaloric, isonitrogenous without EPA, and showed no significant difference ( p = 0.68) between groups after 7 days of intake. The second trial [ 50 ] observed the effects of a preoperative oral supplement containing glutamine, antioxidants and green tea extract vs. a placebo (based on orange juice) on inflammatory response. C-reactive protein levels (postOP) did not change significantly within groups ( p = 0.52; p = 0.13; p = 0.57; p = 0.97) [ 50 ].
Altogether, none of the reported trials showed effects of dietary supplements on weight change. One trial showed a correlation between supplement intake and weight gain and increase in lean body mass. Further trials showed no significant differences in lean body mass. A preOP diet (enriched with EPA or glutamine) showed no significant differences on IL-6 and C-reactive protein levels.
3.5. Mixed and Special Forms of Nutritional Interventions
In the category of mixed and special forms, six RCTs could be included (see Table 5 ) [ 45 , 48 , 57 , 59 , 67 , 68 ]. The timing of the intervention was dependent on the type of nutritional intervention and ranged from 5 days before surgery to 3–4 months of general care during chemotherapy.
Randomized controlled trials of mixed and special forms of nutritional interventions.
BIA: bio impedance analysis; CG: control group; CRP: C-reactive protein; GaCa: gastric cancer; IG: intervention group; LOS: length of stay in hospital; NS: not significant; OeCa: oesophagus cancer; PaCa: pancreatic cancer; POD: postoperative day; WL: weight loss.
In our category nutritional status, all trials looked at weight change, ratio of skeletal muscle mass and the recovery of nutritional state. The first trial [ 67 ] compared EN with total PN on weight change and showed significantly higher BMI on postoperative day 21 ( p = 0.005) in the group with enteral nutrition compared with total PN. However, the BMI preOP was slightly higher in the EN group compared to total PN (EN: 23.8 kg/m²; TPN: 23.5 kg/m²). The second trial investigated a combination of an enteral supplement (enriched with EPA) and three nutritional consultations during radiotherapy vs. a normal diet [ 45 ]. They showed no significant difference in the ratio of skeletal muscle mass and psoas major muscle area ( p = 0.102) after intervention during neoadjuvant chemotherapy. A further trial with two intervention groups and one control group compared a standard EN (+electrolyte solution) (IG1) and a parenteral nutrition with vitamins and trace elements (+electrolyte solution) (IG2) with an oral supportive nutrition (+electrolyte solution) (CG) on the recovery of nutritional status. They showed no significant differences in body weight ( p reported as NS), body fat ( p reported as NS) and lean body mass ( p reported as NS) over the time of 12 months between groups [ 59 ].
In our category immunology, one trial was included [ 57 ] which looked at the difference between preoperative enteral immunonutrition (IG1), enteral immunonutrition plus glycine (IG2) and no preoperative nutritional support in a control group over different time periods on postoperative serum level of C-reactive protein. The authors showed significantly lower levels in both the intervention and control group on postoperative day 7 ( p < 0.05). However, there was a significant increase in C-reactive protein levels in all groups vs. baseline ( p > 0.05).
In our category complications, two trials were included. The first trial looked at the effects of nutritional counselling vs. usual supply on 1-year mortality [ 48 ]. They concluded that there was no significant difference in 1-year mortality between groups ( p = 0.74). The second trial compared PN with EN and showed a significant lower incidence of postoperative complications ( p = 0.040) but no significant difference in incidence of infectious complications ( p = 0.731) in the intervention vs. control group [ 68 ].
In summary, there were beneficial effects of EN compared to PN on body mass index on day 21 postOP but no beneficial effects of EN or PN compared to the electrolyte solution on body weight, body fat and lean body mass when the period of 12 months was considered. A preoperative EN with a supplemental immunonutrition with glycine belongs to significant lower serum levels of C-reactive protein on POD7 vs. no supplement. One trial show significantly lower incidence of postoperative complications in EN vs. PN.
As figured in the overall overview of the RCT studies ( Figure 2 ), the majority of the included RCT studies have a high or moderate risk of bias. Eleven studies were assigned a high risk of bias in the overall assessment. Eleven studies have some concerns/problems and thus an unclear risk (some concerns). Four studies indicate a low risk of bias. Especially in the categories “randomization process” and “missing outcome data”, there was more frequent assessment with a high risk of bias.

Risk of bias (RCTs via RoB2 by Cochrane).
4. Discussion
The aim of this systematic review was to describe the effect of a nutritional intervention compared to no nutritional intervention, a placebo or an alternative treatment in PaCa patients on cachexia, malnutrition and the resulting weight loss. The primary outcomes of the included 26 RCTs were highly heterogeneous. The most common primary outcomes were complications and body weight/weight loss.
Some of the included studies were hard to interpret. For example, one RCT in the category PN showed no effect on median weight change but a positive effect in weight change adjusted for nine potential influencing factors in a multivariate regression analysis. In a multivariate analysis, nutritional intervention increased body weight particularly in patients with malignant lesions [ 63 ]. This means that the groups were highly heterogeneous, which reduces the meaningfulness of the trial. Another trial looked at the generic role of total PN and defined this outcome as a summary of survival, complications, mortality (postOP) and reoperation. This complex definition made the interpretation of the study difficult. They showed no effects on survival, minor complications, mortality and reoperation but negative effects on major and severe complications in the intervention group. The authors concluded that routine administration of PN after surgery in patients undergoing pancreatic resection is not justified [ 51 ]. These results are in line with another trial, which showed no effect on length of stay in hospital [ 60 ]. This is also confirmed by the bias assessment, which rated two studies in the category of PN with “some concerns” and one study with a high risk of bias. Based on the present data, we would not recommend routine use of PN because of the frequent complications.
RCTs from the category EN showed that EN and complementary/enriched enteral immunonutrition must be differentiated. Most of the included RCTs in the EN group examined the effects of supplemental immunonutrition [ 49 , 52 , 55 , 58 , 61 , 62 , 64 , 69 ]. Supplements often include arginine, RNA and omega-3 fatty acids. Three studies showed positive effects of supplemental immunonutrition on postoperative complications [ 49 , 52 , 62 ] compared to the control group, while further, three trials found no difference [ 55 , 61 , 64 ]. Two trials showed a positive effect on length of stay in hospital [ 49 , 52 ], while one trial showed no effect [ 55 ]. One trial showed a positive effect on proinflammatory cytokines [ 69 ], and one trial showed no effect between groups but a positive effect on TNF-α in the intervention group over period of 14 days [ 58 ]. The change in cytokine and total lymphocyte is associated with an immunomodelling effect and better nutritional status. One trial showed a positive effect on weight loss [ 56 ]. In summary, some trials showed positive effects and some trials no effect of EN on our outcome categories nutritional status, immunology and complications. There were no trials with a negative effect of EN on our defined outcomes. In the bias assessment, the studies in the category EN were frequently rated as “some concerns” (five times) and “high risk” (four times). Only one study was rated as low risk. Therefore, EN can only be recommended as a possible adjuvant therapy for pancreatic cancer. Further studies of higher quality are necessary in order to derive effects more clearly and to be able to make recommendations.
There were several studies in the category of dietary supplements that investigated an oral supplement that was enriched with omega-3 fatty acids in the intervention group. There was one trial that looked at weight loss which showed a positive effect [ 53 ], and another trial that showed no effect [ 54 ]. One trial showed a positive effect on body weight after 8 weeks [ 47 ], and one trial which showed no effect [ 66 ]. A positive effect on weight gain and lean body mass was shown in correlation to supplement intake [ 54 ]. There were three trials which showed no effect on lean body mass [ 47 , 54 , 66 ]. One trial showed a positive effect of weight stabilization [ 70 ]. One trial showed no effect of a dietary supplement on serum concentration of IL-6 [ 46 ]. A further trial showed no effect on C-reactive protein levels [ 50 ]. The studies show that a heterogeneous picture prevails with regard to dietary supplements. This trend was to be expected in the studies conducted. There was a heterogeneous picture in the bias assessment of studies investigating dietary supplements (two trials with “low”, two trials with “some concerns” and three trials with high risk of bias). The overview of the risk of bias ( Figure 2 ) shows that the studies have different weaknesses. Often there were weaknesses in the randomization process. Further, the results of the trials are dependent on various factors. For example, many studies did not ensure that the intended nutritional target was achieved. The effect of an individual calculation and control of the adherence to the dietary intervention could be investigated in future studies. RCTs comparing different interventions were also included. In three RCTs, EN was compared with PN [ 59 , 67 , 68 ]. One trial that looked at EN vs. PN showed a positive effect on BMI on day 21 postOP [ 67 ]. One trial that looked at a preoperative dietary supplement as immunonutrition (+glycine in second intervention group) compared to no preoperative nutritional support showed a positive effect on serum levels of C-reactive protein at day 7 postOP [ 57 ]. A further trial looked at PN compared to EN and showed a positive effect on the incidence of postOP complications but no effect on infectious complications [ 68 ]. There were further trials which showed no effect on the reported outcomes. In our defined category nutritional status, there was one trial that looked at enteral immunonutrition combined with nutritional counselling vs. a normal diet and showed no effect on the ratio of skeletal muscle mass and psoas major muscle mass [ 45 ]. One trial compared EN in intervention group one and PN in intervention group two with a standard electrolyte solution in a control group and showed no effect on body weight, body fat and lean body mass after 12 months [ 59 ]. One further trial in the category complications compared nutrient supply (energy, protein) combined with nutritional counselling with nutrient supply alone, and showed no effect on 1-year mortality [ 48 ]. The bias assessment of the studies that investigated mixed interventions showed a trend towards high risk for bias (one trial with “low”, two trials with “some concerns” and three trials with high risk of bias). In summary, mixed interventions were hard to interpret and no recommendation can be derived from this. Further trials should focus on simple or multiple nutritional intervention compared with a control group. An evaluation of nutritional intervention is generally difficult and subject to confounding factors, as compliance is often not fully assessed. With regard to nutritional counselling, compliance is very individual and depends on the counsellor–client situation. In the presented studies, the actual total amount of consumed nutrients/food was often not stated. A dose–response relationship therefore cannot be derived.
A comparison of the results of this review with other reviews from this field shows heterogeneous results. A narrative review focusing on the efficacy of nutritional interventions in cachectic PaCa patients concluded that nutritional counselling to increase energy and protein requirements should be the first step, followed by dietary supplements and PN [ 36 ]. This is not in line with our results. We conclude in our review that nutritional counselling should be given as a complementary measure and EN or immunonutrition with dietary supplements should be prioritized. In line with our results are two reviews which showed a positive effect in gastrointestinal cancer/PaCa patients on postoperative infectious complications and shorter length of stay in hospital with preoperative immunonutrition [ 37 , 38 ]. Furthermore, in line with our results is another systematic review in patients undergoing pancreaticoduodenectomy focused on the perioperative nutritional supplementation, which concluded that attention should be paid to preoperative nutritional optimization and nutritional support should be delivered in the postoperative period with cyclical enteral nutrition [ 32 ]. In addition to the results of this review, modern supports through in-app interventions have also shown success in terms of nutritional status in an RCT with PaCa patients [ 71 ]. A further recent analysis demonstrated a clear advantage in median survival of EN or PN over oral nutrition in advanced cancer-related cachexia [ 72 ].
The risk of bias assessment showed a large number of RCTs with high and moderate risk of bias. From 26 studies, 11 were rated as high risk and 11 as medium risk. Only four studies had a low risk of bias according to Cochrane’s RoB2 assessment. The impact of the data is therefore generally difficult. The high number of studies assessed as high risk may be attributable to the high standard of the assessment tool. Due to the impracticability of the meta-analysis and the overall high risk of bias in the quality assessment, the results should be treated with caution. Furthermore, previous studies rarely used placebos in control groups. This can lead to bias because the control group does not expect positive effects and may not receive the same attention by study personnel. Although a large number of studies were included in this review, the sample sizes of the individual studies were very heterogeneous and often very small. Underpowered studies can also lead to bias in results, especially because no meta-analysis could be calculated. Likewise, bias in results can occur because studies with different entities were included if they contained PaCa. A separate analysis was not reported. An analysis of studies that only included PaCa patients would have minimized the risk of bias with regard to the entities but would have greatly minimized the number of studies to be included. Many studies were analysed by intention-to-treat-analysis, which appears appropriate, but it should be noted that the intervention might have larger effects if followed successfully. The timing of the start of the interventions was also heterogeneous. This makes direct comparisons between studies difficult.
There are limitations that should be taken into consideration. The most important limitation lies in the heterogeneous outcomes. Therefore, a meta-analysis could not be calculated. Furthermore, the search in Pubmed did not lead to a complete result. This is shown by the high number of studies that were added to the review by looking at the bibliographies and by hand searching. Searching more databases and using mesh terms could have improved the search. The heterogeneous literature and number of trials with high risk of bias were further limitations.
The greatest strength of our review is that different forms of nutritional interventions were considered. This gives the reader a good overall view regarding the effects of the nutritional interventions. The entire research process of two reviewers followed the Prisma Guidelines and the standards of the Cochrane Handbook in order to conduct systematic reviews throughout the process. In case of discrepancies, a third independent person was consulted.
In addition to certain amino acids and omega-3 fatty acids, in future trials more attention should also be paid to micronutrients via individual blood levels, so that the focus is not only on macronutrients and on calorie balance. This is because micronutrients such as selenium and copper also show a direct influence on the development of PaCa and survival time [ 73 ]. In order to have a larger database in the field of nutrition interventions and to be able to derive evidence-based recommendations, more RCTs on PN, EN and dietary supplements should be conducted. Further, RCTs on anti-inflammatory supplements and anti-inflammatory diets should be planned.
5. Conclusions
This systematic review investigated the effects of different nutritional interventions to treat cachexia, malnutrition and weight loss in patients with PaCa. PN was associated with frequent complications. EN showed positive effects on length of stay in hospital, complications, cytokines and weight loss. Dietary supplements enriched with omega-3 fatty acids maintained and possibly increased body weight and lean body mass. After weighing the advantages and disadvantages of each intervention, an individualized diet should be administered depending on the patient’s condition or whenever possible consisting of EN or dietary supplements as immunonutrition enriched with omega-3 fatty acids and specific amino acids. However, due to the heterogeneity of the data, clear recommendations for these interventions are not possible.
Supplementary Materials
The following supporting information are available online at https://www.mdpi.com/article/10.3390/cancers14092212/s1 , Figure S1: Tumour cachexia [ 29 ].
Funding Statement
This research received no external funding.
Author Contributions
Conceptualization, A.E., F.R. and I.R.; methodology, A.E., F.R., J.K., I.R. and S.K.; validation, A.E., J.K. and S.K.; formal analysis, A.E., J.K. and S.K.; investigation, A.E. and J.K.; resources, F.R.; data curation, A.E.; writing—original draft preparation, A.E.; writing—review and editing, A.E., J.K., F.R., I.R. and S.K.; visualization, A.E.; supervision, F.R., I.R. and J.K.; project administration, F.R. and I.R. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

IMAGES
COMMENTS
INTRODUCTION. The pancreas is an about 15-cm-long, spongy, tube-shaped organ located in the upper abdomen between the stomach and spine[].A normal healthy pancreas consists of acinar cells secreting digestive enzyme, ductal cells secreting bicarbonate, centro-acinar cells that are the transitional region between acinar and ductal cells, endocrine islets secreting hormone, and relatively ...
Symptoms. Pancreatic cancer often doesn't cause symptoms until the disease is advanced. When they happen, signs and symptoms of pancreatic cancer may include: Belly pain that spreads to the sides or back. Loss of appetite. Weight loss. Yellowing of the skin and the whites of the eyes, called jaundice.
Pancreatic ductal adenocarcinoma (PDAC) is a clinically challenging cancer, due to both its late stage at diagnosis and its resistance to chemotherapy. However, recent advances in our understanding of the biology of PDAC have revealed new opportunities for early detection and targeted therapy of PDAC. In this review, we discuss the pathogenesis of PDAC, including molecular alterations in tumor ...
European and international consensus papers have recently been published and are an important point of reference for clinicians dealing with these lesions. However, there is a lack of high-quality population-based studies investigating all premalignant lesions of the pancreas and future work is needed to progress our understanding of aetiology ...
In a study led by Mayo Clinic Center for Individualized Medicine, researchers found that nearly 1 in 6 people diagnosed with pancreatic cancer had an inherited cancer-related gene mutation that may have predisposed them to pancreatic cancer. The most common genetic mutation in those patients was the BRCA2 gene, which is linked to breast cancer.
Essay On Pancreatic Cancer. 525 Words3 Pages. Cancer is a disease where there are uncontrolled division of cells that goes on in the body and invade different tissues. Cancer can also be caused if there is a mutation in the DNA after birth, Things that cause gene mutation is smoking, radiation, viruses, carcinogens, obesity, hormones, and ...
Nature Reviews Gastroenterology & Hepatology 18 , 447 ( 2021) Cite this article. Pancreatic cancer is a notoriously lethal condition characterised by aggressive malignancy and dismal outcomes ...
No common malignancy is as rapidly and inevitably fatal as pancreatic ductal adenocarcinoma (PDA). This grim fact has driven substantial research efforts into this disease in recent decades. Unfortunately, the investment has yet to result in a meaningful increase in 5-year survival. This has prompted many pancreatic cancer researchers and ...
Pancreatic cancer is a rare but fatal disease. Patients present advanced disease due to the lack of or typical symptoms when the tumor is still localized. A high-quality image processing system has been in practice to detect the pancreatic tumor and determine the possibility of surgery, and preoperative methods, such as ERCP are increasingly used to complement the staging modality ...
Essay about Pancreatic Cancer. "Cancer of the pancreas is a genetic disease that is the fifth most common cause of death in both men and women. Pancreatic cancer affects approximately 28,000 Americans each year, or five out of 100,000 people" (Mayo Clinic, 1998). According to physicians at Johns Hopkins Medical Institute, "pancreatic cancer is ...
This paper will provide an overview of pancreatic cancer. Pancreatic cancer is the fourth most common cause of death due to cancer worldwide. Most pancreatic tumors are exocrine tumors, including ductal adenocarcinoma, acinar cell carcinoma, cystadenocarcinoma, adeno-squamous carcinoma, signet ring cell carcinoma, hepatoid carcinoma, colloid ...
Essay Examples on Pancreatic Cancer. Essay examples. Essay topics. 7 essay samples found. Sort & filter. 1 Ethical Dilemmas in End-of-life Decision Making . ... Pancreatic cancer is the king of cancer, and its low survival rate has not changed significantly in the past 40 years. In Europe, pancreatic cancer is the fourth leading cause of cancer ...
Essay about Pancreatic Cancer "Cancer of the pancreas is a genetic disease that is the fifth most common cause of death in both men and women. Pancreatic cancer affects approximately 28,000 Americans each year, or five out of 100,000 people" (Mayo Clinic, 1998).
Approximately 60 430 new diagnoses of pancreatic cancer are anticipated in the US in 2021. 1 The incidence is rising at a rate of 0.5% to 1.0% per year, and pancreatic cancer is projected to become the second-leading cause of cancer death by 2030 in the US. 1,2 Pancreatic ductal adenocarcinoma (PDAC) accounts for the majority (90%)of pancreatic neoplasms, and the other subtypes include acinar ...
Posted: May 16, 2016. Pancreatic cancer cells and neighboring normal cells engage in a two-way molecular conversation that helps drive malignant behavior in the cancer cells, according to new study results. FDA Approves Irinotecan Liposome to Treat Pancreatic Cancer. Posted: November 24, 2015.
Essay On Pancreatic Cancer. Approximately 20% of pancreatic cancer is found to be operable or resectable. The complete resection of the primary lesion is best treatment for patients with localized pancreatic cancer. However the risk of both local and distal recurrence is high in following resection. In early stage pancreatic cancer the complete ...
Pancreatic cancer affects approximately 33,730 Americans each year. The pancreas is a gland found behind the stomach that is shaped a little like a fish. The pancreas is around six inches long and less than two inches wide, and it spans across the abdomen. The pancreas makes enzymes to break down food.…. 514 Words.
Pancreatic Cancer Essay. Pancreatic cancer is an aggressive type of cancer that will be diagnosed in approximately 53,070 Americans this year alone; 41,780 will die of it. (1) The pancreas is an organ essential in maintaining homeostasis in the body, it secretes hormones and enzymes that help us in the digestion of fats.
Pancreatic cancer is an aggressive form of cancer that develops in the tissues of the pancreas. Located in the abdomen behind the lower part of the stomach, the pancreas aids in digestion. It contains both exocrine glands (which produce enzymes that help the body digest food) and endocrine glands (which produce hormones, including insulin, that ...
Papers written and published in the English language in the past five years: Grey literature: Type of intervention included any form of chemotherapy, any combination of chemotherapy and radiotherapy, best supportive care, or another chemotherapy and/or radiotherapy treatment plan. ... Pancreatic cancer is resistant to radiation and chemotherapy ...
1. Essay On Pancreatic Cancer Surgery: Localized Disease Approximately 20% of pancreatic cancer is found to be operable or resectable. The complete resection of the primary lesion is best treatment for patients with localized pancreatic cancer. However the risk of both local and distal recurrence is high in following resection.
Finding pancreatic cancer early could help increase a patient's chances of survival. Across the United States, research teams are investigating ways to spot early cases, with many turning to ...
1. Introduction. Pancreatic cancer (PaCa) has a poor overall prognosis, with a 5-year survival rate of 9% and a median survival time of 6 months [].However, patients with early tumour resection have a higher chance of remission, with a 5-year survival rate of 25% and a median survival of 14-20 months [2,3,4].Patients often suffer from tumour cachexia [5,6], which is manifested in weight loss ...