- Open access
- Published: 09 November 2023

To vaccinate or not to vaccinate? The interplay between pro- and against- vaccination reasons
- Marta Caserotti 1 ,
- Paolo Girardi 2 ,
- Roberta Sellaro 1 ,
- Enrico Rubaltelli 1 ,
- Alessandra Tasso 3 ,
- Lorella Lotto 1 &
- Teresa Gavaruzzi 4
BMC Public Health volume 23 , Article number: 2207 ( 2023 ) Cite this article
1919 Accesses
1 Altmetric
Metrics details
By mid 2023, European countries reached 75% of vaccine coverage for COVID-19 and although vaccination rates are quite high, many people are still hesitant. A plethora of studies have investigated factors associated with COVID-19 vaccine hesitancy, however, insufficient attention has been paid to the reasons why people get vaccinated against COVID-19. Our work aims to investigate the role of reasons in the decision to get vaccinated against COVID-19 in a representative sample of 1,689 adult Italians (March–April 2021) balanced in terms of age, gender, educational level and area of residence.
Through an online questionnaire, we asked participants to freely report up to three reasons for and against COVID-19 vaccination, and the weight each had in the decision to get vaccinated. We first investigated the role of emotional competence and COVID-19 risk perception in the generation of both reasons using regression models. Next, we studied the role that the different reasons had in the vaccination decision, considering both the intention to vaccinate (using a beta regression model) and the decision made by the participants who already had the opportunity to get vaccinated (using a logistic regression model). Finally, two different classification tree analyses were carried out to characterize profiles with a low or high willingness to get vaccinated or with a low or high probability to accept/book the vaccine.
High emotional competence positively influences the generation of both reasons (ORs > 1.5), whereas high risk perception increases the generation of positive reasons (ORs > 1.4) while decreasing reasons against vaccination (OR = 0.64). As pro-reasons increase, vaccination acceptance increases, while the opposite happens as against-reasons increase (all p < 0.001). One strong reason in favor of vaccines is enough to unbalance the decision toward acceptance of vaccination, even when reasons against it are also present ( p < 0.001). Protection and absence of distrust are the reasons that mostly drive willingness to be vaccinated and acceptance of an offered vaccine.
Conclusions
Knowing the reasons that drive people’s decision about such an important choice can suggest new communication insights to reduce possible negative reactions toward vaccination and people's hesitancy. Results are discussed considering results of other national and international studies.
Peer Review reports
Introduction
By mid 2023 the European Union reached nearly 75% vaccine coverage for the primary vaccine cycle against COVID-19, with countries such as Croatia, Slovakia, and Poland falling short of 60% and others such as France, Portugal, and Italy close to 90% [ 1 ]. Although vaccination rates are, on average, quite high, many people are still hesitant. Vaccine hesitancy indicates the delay or refusal of a vaccine despite availability in vaccine services [ 2 , 3 ] and is a multidimensional construct, resulting from the interaction between individual, social, and community aspects [ 4 ]. In the last two years, a plethora of studies have investigated factors associated with COVID-19 vaccine hesitancy showing, for example, that vaccine hesitancy is higher in women [ 5 , 6 ], in young people [ 5 , 7 , 8 ], in people with low education [ 8 , 9 ], low trust in authorities [ 10 , 11 ], and strong conspiracy beliefs [ 5 , 12 , 13 ]. However, to the best of our knowledge no one has investigated the interplay that pro- and against- vaccination reasons may play in the choice to get vaccinated, namely what happens when a person has both pro- and against-vaccine considerations. Trying to fill this gap in the literature, our work aims to investigate how different reasons and the importance people place on them are likely to influence the decision to get vaccinated against COVID-19.
In line with the vaccine hesitancy continuum defined by SAGE [ 2 ], while extremely pro-vax people are likely to express only reasons pro-vaccination and extremely no-vax people are likely to express only reasons against vaccination, individuals who fall between the two extreme end-points are likely to feel some doubts. This large number of people offer us the unique opportunity to assess which category of reasons (pro- vs. against- vaccination) is more impactful in driving people's vaccination decisions. As it is reasonable to imagine, among the reasons for choosing to get (or not) vaccinated some reasons are more rational, while others are more related to affect. For example, there are people who rationally recognize the importance of vaccines but at the same time are frightened by the side effects. Thus, the decision to get (or not) vaccinated is the result of a complex process, in which costs and benefits are weighed more or less rationally. Indeed, while several studies have pointed out that the decision to vaccinate is due to cognitive rather than emotional processes [ 14 , 15 , 16 , 17 ], others have highlighted the role of affect and risk perception in the vaccination decision [ 18 , 19 , 20 ]. Thus, the intention to accept the vaccine is driven by emotional and affective feelings as much as by cognitive and rational judgments. Particular attention to what people feel and think about vaccine-preventable diseases and vaccination in general is paid in the model developed by the “Measuring Behavioral and Social Drivers of Vaccination” (BeSD), a global group of experts established by the World Health Organization [ 21 ]. This model encompasses two groups of proximal antecedents of vaccination, namely, what people think and feel (e.g., perceived risk, worry, confidence, trust and safety concerns) and social processes (e.g., provider recommendation, social norms and rumors). Antecedents affect vaccination motivation (i.e., vaccination readiness, willingness, intention, hesitancy), which can then be strengthened or weakened by practical issues (such as vaccine availability, convenience and cost but also requirements and incentives), resulting in acceptance, delay or refusal of vaccination (vaccination behavior).
Although some studies have considered whether the cognitive or affective component has greater weight in determining the intention to vaccinate, no one, to the best of our knowledge, has studied the interplay between pro- and against- vaccination reasons, nor the weight these have in the choice to vaccinate. In addition to the drivers already studied in the literature [ 5 , 6 , 7 , 8 , 11 , 12 ], we believe that the focus on this interaction may be relevant to better understand the complex phenomena related to vaccine hesitancy. Few recent studies have attempted to investigate the complexity of vaccination choice by studying the reasons why people choose to get (or not) vaccinated against COVID-19. Fieselmann and colleagues [ 22 ] highlighted that among the reasons that reduce adherence to vaccination are a low perception of its benefits, a low perception of the risk of contracting COVID-19, health concerns, lack of information, distrust of the system, and spiritual or religious reasons. Another study, instead, shed light on the reasons that encourage hesitant people to consider vaccination, such as protecting themselves, their family, friends and community from COVID-19, and being able to return to normal life [ 23 ].
In the present study we asked the participants to spontaneously come up with their own reasons to get (or not) vaccinated, without limiting or influencing them with a set of predefined options to choose from, thus aiming to obtain more genuine answers that may better capture the intuitive aspect of people’s opinions (for a similar reasoning see [ 24 ]). The procedure we used has been implemented by Moore et al. [ 23 ], the only study, as far as we know, that asked for reasons with an open-ended question. Critically, in their study, participants were asked to report only reasons in favor of vaccination (e.g., "What are your reasons for getting the COVID-19 vaccine?"), excluding reasons against. By contrast, we asked participants to freely report up to three reasons in favor and up to three reasons against COVID-19 vaccination and to rate on a 5-point Likert scale their weight in the decision about getting (or not) vaccinated.
From a theoretical point of view, the reasons pro- and against vaccination may be seen within the framework of prospect theory [ 25 , 26 ] which suggests that people evaluate the outcome of a choice based on a reference point, against which losses and gains are determined: the former below this point, the latter above this point. Importantly, especially in this specific context, losses and negative consequences are weighted more than gains and benefits, making us hypothesize that if a person has one reason for and one reason against the vaccine, which are of equal importance, they will more likely lean toward choosing not to vaccinate. Consistently, it is known that negative experiences have a greater impact than neutral or positive ones (i.e., the negativity bias [ 27 ]).
Besides delving into the reasons that may influence the choice to get (or not) vaccinated, it would be interesting to also look at the individual differences that may determine the reporting of pro- and against- vaccination reasons and their valence. In this regard, the literature suggests that risk perception and emotion regulation can both have a great impact in the decision to get vaccinated. For instance, studies conducted during H1N1 influenza have shown that perception of disease-related risk is one of the strongest predictors of vaccine adherence [ 28 , 29 ]. Additional insights have been provided by more recent studies investigating the role of COVID-19 risk perception in the decision to get vaccinated against COVID-19. Viswanath and colleagues [ 30 ] showed that people are more willing to vaccinate themselves and those under their care to the extent to which they feel more vulnerable to COVID-19 and rate the consequences of a possible infection as severe. Such a relationship between COVID-19 risk perception and intention to vaccinate was confirmed by another study using a cross-sectional design, which focused on the early months of the pandemic [ 31 ]. This study also examined how risk perception changed during the pandemic phases and showed that during the lockdown, compared to the pre-lockdown phase, also those who reported some hesitancy were more likely to get vaccinated when they perceived a strong COVID-19 risk.
With regard to emotion regulation, the literature suggests that people react differently to affective stimuli [ 32 ] and that their decisions are influenced by their abilities to regulate emotions [ 33 , 34 ]. Recent works investigating the relationship between hesitancy in pediatric vaccinations and the emotional load associated with vaccinations, have shown that a negative affective reaction is one of the factors leading to lower vaccine uptake [ 35 , 36 ]. Specifically, Gavaruzzi and colleagues [ 36 ] showed that concerns about vaccine safety and extreme views against vaccines are associated with vaccine refusal. Interestingly, they also showed that parents' intrapersonal emotional competences, i.e., their ability to manage, identify, and recognize their own emotions, is critical to vaccine acceptance for their children. Therefore, in our study we measured people's risk perception and emotional competencies to assess their possible role in the production of reasons in favor and against vaccination.
As described in Fig. 1 , the relationship between different domains of interest can be hierarchically structured, using a directed acyclic graph, starting from the risk perception and emotion regulation, to the generation of pro- and against- vaccination reasons and their valence, and finally to the vaccination willingness/adherence. With respect to the mentioned structure, we are interested to investigate the following research hypotheses:
The number and weight associated with reasons pro- and against-vaccination should be influenced by individual differences in the ability to regulate emotions;
The number and weight associated with pro-vaccination reasons should be influenced by individual differences in COVID-19 risk perception;
A higher number of strong (i.e., with high weight) reasons pro- (vs. against-) vaccination should correspond to a more (vs. less) likelihood to accept the vaccination.
Generating an equal number of reasons in favor and against vaccination should lead to a weaker likelihood to accept the vaccination.
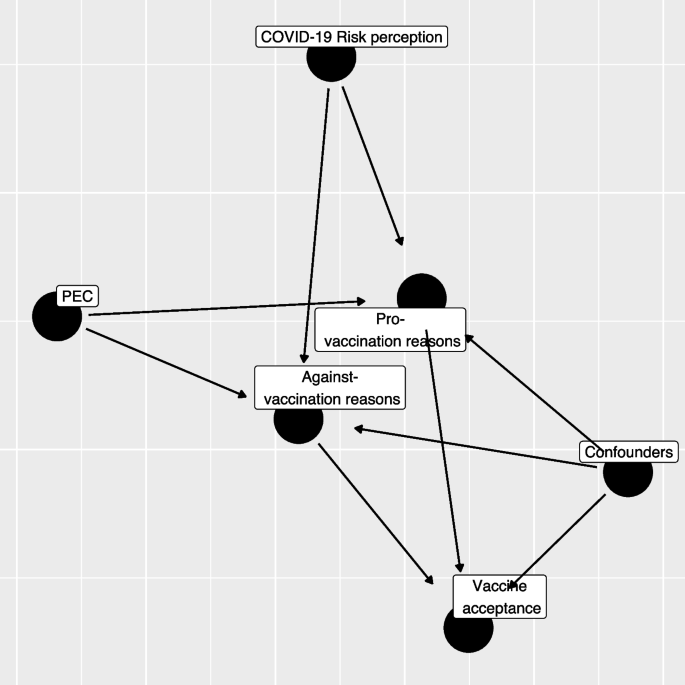
Directed Acyclic Graph (DAG) between variables considered in the study (PEC: Short Profile of Emotional Competence scale)
As we conducted the study between March and April 2021, a time when vaccinations were being progressively rolled out, we decided to consider the role of personal reasons on both the intention to get vaccinated (for those who had not yet had the opportunity to get vaccinated) and the choice already made (e.g., vaccine received or booked vs. refused).
Finally, through a non-parametric classification analysis, we will explore how specific pro- and against-vaccination reasons impact the decision to get (or not) vaccinated. Specifically, we will investigate the role that different categories of reasons play in the choice to vaccinate.
Participants
Data collection was commissioned to a survey and market research agency (Demetra Opinions.net), with the aim of securing a representative sample of the adult (+ 18) Italian population, estimated at 49.8 million [ 37 ]. The sample was balanced in terms of age, gender, educational level (middle school or lower, high school, degree or higher), and area of residence (North, Center, South, and Islands). The agency distributed via email the survey link to its panelists, who freely decided whether to participate in the study in exchange for financial compensation. Out of 1,833 participants who started the questionnaire, 77 (4%) were excluded because they did not complete the survey and 16 (0.9%) were excluded since they reported offensive content in open-ended questions. Finally, 124 (6.8%) participants were excluded because of missing information. Thus, the final sample consisted of 1,689 participants. The project was approved by the ethical committee for Psychology Research of the University of Padova (Italy), with protocol number 3911/2020 and informed consent was obtained for all participants.
We developed an ad-hoc questionnaire including a series of open-ended and closed questions (see Additional file 1 : Appendix 2 for the full material). We first investigated the vaccination status of the participants, asking whether they already had received at least the first dose, whether they had booked it or were still ineligible, and finally whether they had refused the vaccination. Those not yet eligible were asked to rate how likely they would be to get vaccinated at the time they responded (0 = Not at all likely , 100 = Extremely likely ). Then, we asked participants to report a maximum of three reasons both in favor of the COVID-19 vaccine and against it (in counterbalanced order) and to rate how much each of the reported reasons weighed in their choice to vaccinate or not, on a 5-point likert scale (1 = Not at all , 5 = Extremely ). Due to the sparsity on the rate and the number of provided reasons we re-coded the provided information into two semi-quantitative variables, one for pro- and one for against- vaccination reasons, as following: missing/invalid reasons, low average rating (answers 1–3 on the Likert scale) and 1–3 reasons, high rating (answers 4–5 points on the Likert scale) and 1 reason, and high average rating (answer 4–5 points on the Likert scale) and 2–3 reasons.
The questionnaire also included the 20-item Short Profile of Emotional Competence scale (S-PEC; [ 38 ]) to measure intra- and inter-personal emotional competences separately. The intra-personal scale (10 items) refers to emotional competences related to oneself and it includes items such as "In my life I never make decisions based on my emotions'' or "I don't always understand why I react in a certain way". The inter-personal scale (10 items) refers to emotional competences related to other people and it includes items such as “If I wanted, I could easily make someone feel uneasy” or “Most of the time, I understand why the people feel the way they do”. All items are answered on a 7-point likert scale (1 = Not at all agree , 7 = Completely agree ). The internal consistency of the S-PEC scale, measured by means of Cronbach’s α, was adequate (α = 0.81). Further, we measured participants' risk perception of COVID-19 by asking them to indicate how scared they felt of the virus, how serious they think the disease is, how likely they think they are to get sick, and how worried they feel about the various mutations [ 10 , 31 ]. We then asked participants to report their age, gender, educational level, their occupation (health workers, white-collar workers, entrepreneurs, other non-health-related contract forms, and the unemployed), whether they already had COVID-19 (No or don't know, Yes asymptomatic, Yes with few symptoms, and Yes with severe symptoms). The questionnaire was pilot tested by 30 participants who filled the questionnaire first then were asked to discuss and comment on the comprehension of the wording of questions and answer options. Two questions were slightly reworded to improve clarity.
Scoring of reasons
In the first instance, a bottom-up process from reasons to categories was followed by reading a sample of both types of reasons, with the aim of constructing initial categorizing patterns. Examples of pro-vaccination reasons include protection of personal and public health, return to normality, and civic duty; while reasons against vaccination include fears for one's health, sociopolitical perplexity, and distrust of science and institutions (see Additional file 1 : Appendix 1). At this stage, response information was added to the categorizations indicating whether the responses were valid or missing/invalid. Specifically, valid responses had both a reason and the respective weight; missing/invalid responses were those where reason, weight or both were missing or with utterly unrelated concepts or meaningless strings or letters. Finally, by applying a top-down process, we constructed macro categories by merging specific conceptually assimilated categories, so as to avoid the dispersion of data into too many ramifications (see Table S 5 ).
Statistical analysis
Descriptive analysis.
All the analyses were performed only on respondents with no missing observations on the variables of interest (1,681, 92%) excluding also a limited number of those with a non-valid set of pro- or against-vaccination reasons (Table S 1 ; 0.9%). The study variables were summarized in frequency tables and figures (frequency for categorical variables, median and Interquartile Range (IQR) for continuous variables). Kruskal–Wallis tests were computed to compare the distribution of continuous variables across the categories of vaccine status. Categorical variables were compared using chi-squared or Fisher's exact test where expected frequencies in any combination were less than 10. Statistical significance was assumed at the 5% level.
COVID-19 Perceived risk—exploratory factor analysis
An Exploratory Factorial Analysis (EFA) was performed on groups of variables related to COVID-19 perceived risk: scare, severity, contagiousness, and the likelihood of mutation. Since the presence of limited support (0–100 scale) and non-normal marginal distribution, the EFA was performed using a weighted least square mean and variance adjusted (WLSMV) estimator. We extracted from the EFA only the first factor, which explained the highest percentage of variance (Table S 2 ; 61%). The estimated loadings were then used to calculate the regression factor scores. The number and the name of items included, their internal consistency (Cronbach’s α), the estimated loadings, and the proportion of deviance explained are reported in Table S 2 .
Propensity score weighting
At the time of data collection (March–April 2021), the vaccine offer was not opened to the entire population. To adjust the estimates of the following regression models for the propensity to receive the vaccine, we estimated a logistic regression model in which the dependent variable was the response to the question about a previous vaccination offer (Yes/No), while all the factors that can influence the vaccine proposal served as independent variables: age-class (young ≤ 25, young adult 26–45, adult 46–65, elderly 66–84), gender (male, female), occupational status (health worker, not at work, not health worker-employer, not health worker-entrepreneur, not health worker-other), educational level (low = middle school or lower, medium = high school, high = degree or higher), key worker status (yes, no, I don’t know), past COVID-19 contagion (no, yes asymptomatic, yes low symptoms, yes severe symptoms), and familiar status (single/in a relation, married/cohabitant, divorced/separated/other). The predicted probability was used to estimate the weights for the following regression models using a framework based on an inverse probability of treatment weighting (IPTW; for further details, see [ 39 ]).
Regression models
Our research questions can be summarized by trying to describe the relationship exploited by the directed acyclic graph in Fig. 1 . The first step regression model aims to assess how S-PEC scores (inter- and intra-personal) and COVID-19 risk perception influenced the reasons pro- and against-vaccination produced by participants while considering the presence of a set of confounders (age-class, gender, occupational status, educational level, key worker status, and familial status).
Since both the pro- and against-vaccination reasons are formed by a categorical variable with 4 levels (missing/invalid, low 1/2/3 reasons, high 1 reason, high 2/3 reasons), we evaluated whether S-PEC and COVID-19 risk perception scores influenced the distribution of pro- and against-vaccination reasons employing two different multinomial regression models including all the previously mentioned variables (S-PEC, COVID-19 risk perception, and confounders). The overall significance of a variable in the model was tested using an analysis of the variance (ANOVA).
The second step in the analyses was taken to investigate whether the generation of pro- and/or against-vaccination reasons affected the willingness to be vaccinated or the vaccine acceptance. Each participant reported their willingness to get vaccinated on a 0–100 scale or, in case a COVID-19 vaccine had been already offered, their vaccination status (done, booked, or refused). For respondents who had not yet been contacted for booking/getting the vaccination, we evaluated whether pro- and/or against vaccination reasons influenced the willingness to be vaccinated by employing a beta regression model in which the respondent variable scale (0–100) was rescaled to be a relative frequency [ 40 ]. The full models included the semi-quantitative pro- and against-vaccination reasons variables and, even if non-statistically significant, all the confounders in order to adjust for age class, gender, educational level, occupational status, familial status, and key worker status. Beta regression coefficients were estimated using a maximum likelihood estimator (MLE). Results were presented in terms of Odds Ratios (ORs) by exponentiating the estimated coefficients and producing a relative 95% Confidence Interval (95% CI).
A further regression analysis was conducted through a logistic regression model to explain which factors influenced vaccine acceptance (done/booked vs. refused) among those who already received the vaccine offers. The full model included the same variables considered in the previous beta regression model, after recoding the variables related to pro- and against-vaccination reasons into a binary form (missing/invalid vs. presence of at least one valid reason) due to low sample size and the sparsity of the response variable. As a consequence, we tested a simplified version of Hypothesis 3, considering the presence (vs. missing/invalid) of pro- or against-vaccination reasons in order to test their influence on the probability of having accepted/booked the vaccination.
Results were reported employing ORs and relative 95% Confidence Interval (95% CI).
Both the beta regression and logistic regression were weighed using an IPTW scheme to take into account the presence of a different probability of a vaccine offer among respondents.
The presence of an interaction between pro- and against-vaccination reasons was tested by means of a likelihood ratio test. The regression models were estimated through the R 4.0 program (R Core Team, 2021), and for the beta regression we employed the betareg package [ 41 ].
Classification tree analysis
Two different classification tree analyses were carried out to characterize profiles with a low or high willingness to get vaccinated (respondents who had not yet been offered a vaccine) or with a low or high probability to accept/book the vaccine (respondents who had already received a vaccine offer).
Although the dependent variables were non-normally distributed (scale 0–100 or binary 0/1), we considered them continuously distributed adopting a splitting criterion based on the analysis of the variance (ANOVA). We tested the inclusion in the model considering the type of pro- or against-vaccination reasons. A tree pruning strategy was adopted to reduce classification tree overfitting considering the overall determination coefficient (R 2 ) as an indicator and fixing that at each classification step in the tree if the R 2 did not increase by 0.5% the tree should be stopped. Classification tree analysis was performed using the rpart package [ 42 ] on R environment [ 43 ].
The main characteristics of the respondents by vaccination status (received, booked, not yet, and refused) were reported in Table 1 . Among respondents, 23.3% were offered the vaccination and, among them, 13.8% refused it (Fig. S 1 ). Among those not yet eligible, willingness to be vaccinated showed a median value of 80 points (average: 68.7). The distribution of gender was almost equal (51% females, 49% male), and the median age was 47 years old (IQR: 34–57 years). Educational level was low in 41% of the sample, while the most represented employment status was not at work (39%) followed by employed (37%), and entrepreneur (9.8%). A quarter (26%) of respondents classified themselves as key workers during the COVID-19 pandemic. The predominance of respondents (63%) were married or living with a partner, while only 9% had had a COVID-19 infection.
COVID-19 risk perception and the S-PEC score (intra- and inter-personal) were categorized into three categories according to empirical tertiles (low:1 st tertile, medium: 2 nd tertile, high: 3 rd tertile). The level of COVID-19 risk perception differed across vaccination status ( p < 0.001). The reasons pro- and against-vaccination have a different distribution according to COVID-19 vaccination status (Table 2 ). The highest frequency of pro-vaccination reasons was reported by those who received the COVID-19 vaccination; conversely the lowest frequency of pro-vaccination reasons was generated by those who refused the vaccine, whereas, intermediate frequencies were shown by people who were not yet offered the vaccination and those who had booked the vaccine, who reported a comparable distribution of the number of pro-vaccination reasons. A reverse pattern was exhibited for against-vaccination reasons, which were generated with the highest percentage by respondents who refused the vaccine (in particular high and multiple reasons). Conversely those who have booked/done the COVID-19 vaccine showed the lowest frequency of reasons against vaccination, while respondents without a vaccine offer reported an intermediate frequency of reasons against vaccination.
The estimated results of the propensity score model for the vaccine offer are shown in Table S 3 . Respondents older than 65 years exhibited a nearly four-fold increase in the probability to be contacted for the vaccination with respect to the reference age-class (≤ 25 years). All non-health employees showed a high drop in the probability of having received the vaccination offer, while the probability increased as the educational level increased. Being a key worker during pandemic resulted in an increased probability of having received the vaccination proposal while no statistical significant influence was observed for the past COVID-19 contagion or for familial status. The distribution of the propensity score by vaccine status obtained by the model is reported in Fig. S 1 , in which it is shown that the distribution is different by vaccine offer, but the two density functions partially overlap. The discriminant power of the propensity score estimated was only discrete (ROC analysis, AUC: 71.8%).
The results of the multinomial regression models which investigated the effect of emotional competences and risk perception on the generation and the predictors of pro- and against-vaccination reasons with respect to missing/invalid level and the reference categories are presented in Table 3 (see also Fig. 1 ). Compared to the reference category (missing/invalid), high values of S-PEC-self were associated with a higher probability to report pro- and against-vaccination reasons (all ORs > 1.5), while high values of S-PEC-others were associated with a mild probability to report multiple pro-vaccination reasons (all ORs > 1.42). A high (vs. low) COVID-19 risk perception increased the frequency of one strong pro-vaccination reason while it had a null or low decremental effect on the frequency of against weak vaccination reasons. Further, medium (vs. low) COVID-19 risk perception only increased the strong pro-vaccination. Compared to the reference age-class (young), adults and elderly showed a higher probability to generate a strong unique pro-vaccination reason (adults vs. young OR: 1.72, 95%CI: 1.07–2.77); elderly vs. young OR: 2.24, 95%CI: 1.26–4.00), while lower probability to generate against vaccination reasons was observed for elderly compared to young respondents (OR: 0.48, 95%CI: 0.26–0.90). Female participants generated fewer strong pro-vaccination reasons (ORs < 0.73), and also fewer multiple weak against-vaccination reasons (OR: 0.68, 95%CI: 0.51–0.91) compared to male participants. Overall, the occupational status did not affect the generation of pro- and against-vaccination reasons (ANOVA test p > 0.05); however an increased frequency of low 1/2/3 against-vaccination reasons emerged among the category “Other—not health workers” compared to the reference group represented by health workers (OR: 2.52, 95%CI:1.09–5.86). Pro-vaccination reasons are more frequent as the educational level becomes higher, while the relation of the educational level with against- vaccination reasons appears weaker and significantly increased only for the presence of multiple weak reasons against vaccination (High vs. Low educational level, OR: 2.10, 95%CI: 1.45–3.03). Not being a key worker is related to a higher frequency of multiple strong both pro- and against vaccination reasons. The familiar status did not seem to be related to the frequency or the strength of the reasons, except for the status of divorced/separate/other that, with respect to the reference category single/in a relation, showed a twofold increase in the frequency of a strong unique against vaccination reason.
Through a beta regression model we investigated the predictors of willingness to be vaccinated for the participants who had not yet received the vaccination offer. As shown in Table 4 , the generation of pro- and against-vaccination reasons strongly influences the willingness to be vaccinated. The predicted probability from the combination of pro- and against-vaccination reasons is shown in Fig. 2 (and Table S 4 ): respondents who did not report any reasons had an average predicted probability above 60%, while the presence of at least one reason against vaccination decreased the willingness to be vaccinated, in particular in the case of strong multiple against vaccination reasons. On the other hand, the presence of at least one pro-vaccination reason strongly increased the probability. In the end, the presence of both strong multiple pro and against vaccination reasons resulted in a high probability of getting the vaccine. Regression models adjusted by propensity score weighting allowed us to comment the influence of potential confounders: males reported an increased willingness to be vaccinated (vs. females; OR: 1.26, 95%CI: 1.11–1.42), and so did those with a high educational level (vs. low; OR: 1.22, 95%CI: 1.04–1.44) while the opposite was true among no key workers (vs. key workers; OR: 0.85, 95%CI: 0.72–0.99).
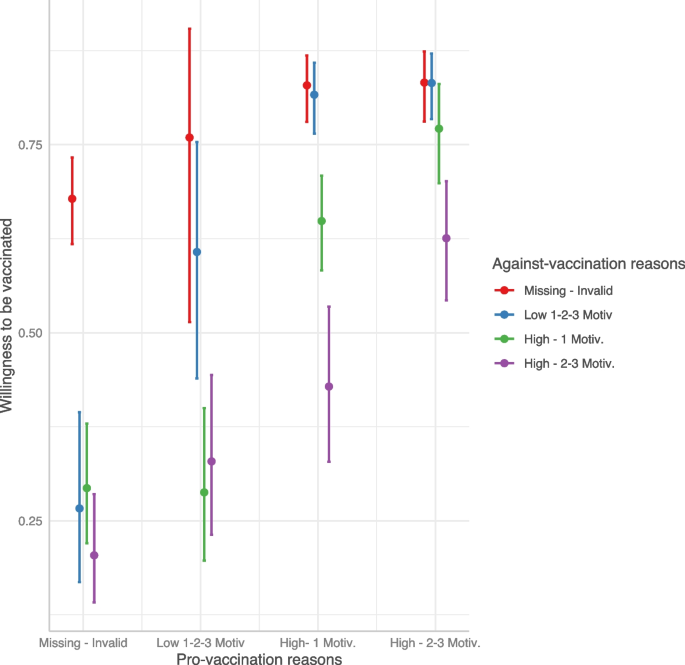
Predicted willingness to get vaccinated by interaction between pro- and against-vaccination reasons
Finally, with a logistic model we investigated the predictors of vaccine acceptance\booking. As shown in Table 5 , people who accepted or booked the COVID-19 vaccine were more likely to show pro-vaccination reasons and less likely to show against-vaccination reasons. Interestingly, when both kinds of reasons were provided, the probability of getting/booking the vaccine remained nevertheless very high (Fig. 3 ). Compared to the age class [46-65], younger age classes reported a strong reduction in the probability to have accepted/booked the vaccine. Male participants (OR: 1.53, 95%CI: 1.10–2.12) and those with a high educational level (OR: 2.65, 95%CI: 1.60–4.54) showed an increased probability of vaccine acceptance/booking when compared to females and participants with medium educational level, respectively. Being a health worker had a strong and positive influence on the probability of getting/booking the vaccine with respect to those employed as no health workers (OR: 6.61, 95%CI: 2.10–30.9).
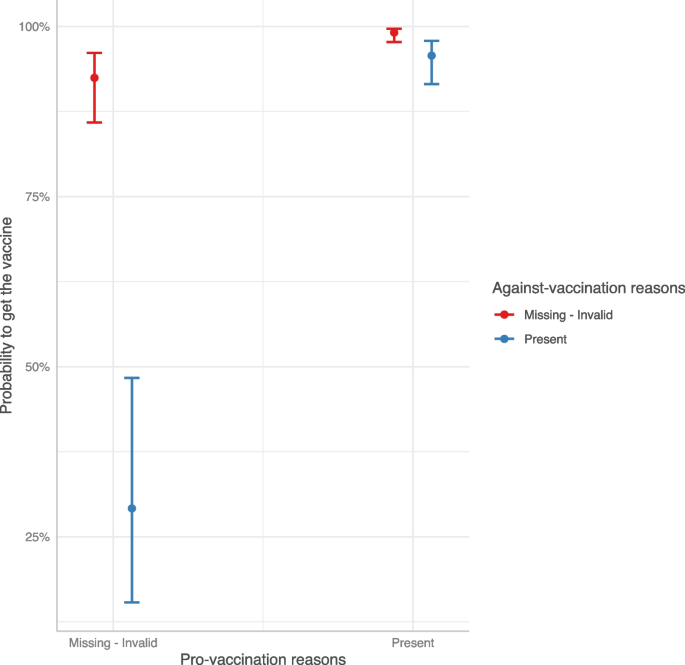
Predicted COVID-19 vaccine acceptance/booking probability by interaction between pro- and against-vaccination reasons
Two regression tree models were estimated separately on the willingness to be vaccinated for those who had not yet received the vaccine offer and on the booking/acceptance of the vaccination in case of vaccine offer. Results are shown in Fig. 4 . Considering the willingness to be vaccinated, the presence of distrust in the vaccination was the most discriminant variable; this latter in conjunction with reasons related to protection, herd immunity, and the absence of no clinical trials guided the willingness to be vaccinated. In particular, the combination of the absence of reasons related to distrust and the presence of protection reasons showed the highest values on the intention to get vaccinated (average value = 83 points, 22% of the sample). On the other side, the presence of at least one reason related to distrust without any positive reasons concerning protection, herd immunity, and trust predicted the lowest willingness to be vaccinated (average value = 29 points, 6% of the sample).
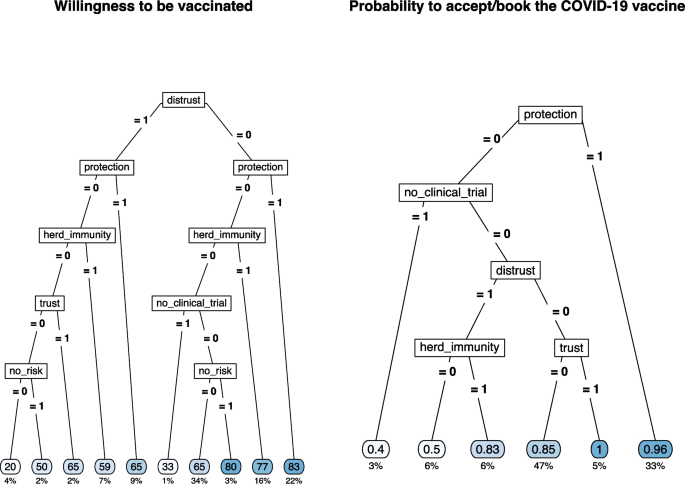
Regression tree for the willingness to be vaccinated (left) and for COVID-19 vaccine acceptance/booking (right) by selected type of pro- and against-vaccination reasons
The sense of protection given by the vaccine or the trust in the vaccination was the main reason for vaccination acceptance/booking (average probability = 0.96 and 1.00, 33% and 5% of the sample, respectively). The combination of the absence of protective reasons and the presence of doubts about the lack of clinical studies results in the lowest likelihood of accepting/booking the vaccination (average probability = 0.40, 3% of the sample). The presence of distrust and the belief in herd immunity were the other discriminant reasons with intermediate results in terms of the probability to accept/book the vaccination.
The frequency of each category of pro- and against-vaccination reasons by COVID-19 vaccine status is shown in Table S 5 .
In the present study we aimed to investigate the reasons behind the decision to get (or not) vaccinated against COVID-19 by asking participants to report up to three reasons in favor and three reasons against the COVID-19 vaccination and to indicate the weight these reasons had in their decision. Although some researchers discourage categorization, the sparsity of the responses related to the number of reasons and their weight implies a semi-quantitative solution since a simple variable multiplication between rating and frequency (recoding to zero in case of zero reasons) is not feasible. In this case, this approach was not satisfactory as such coding would not allow differences underlying identical scores to emerge. For example, only 1 strong motivation (rating 5) would be coded in the same way as three motivations with weights 1, 2, and 2. Instead, we decided to categorize the combination of frequency-weight reasons as categorical variables (missing/invalid, low 1/2/3 reasons, high 1 reason, high 2/3 reasons) in which rating and number of reasons are combined into a single variable. This categorization allows us not only to study the weight that different categories have on the decision to get vaccinated but also to overcome the risk of imputing a specific value for missing responses.
As shown in Fig. 1 , analyses were run in two steps. The first step aimed to assess how emotional competences and risk perception impacted the generation of reasons pro- and against-vaccination (Hypotheses 1A and 1B), whereas the second step investigated how different reasons affected the intention to get vaccinated (Hypotheses 2 and 3). The results support the hypotheses that emotional competences and risk perception play a significant role. Regarding emotional competence as measured by the S-PEC, the results show that high intra-personal emotional competence positively influences the production of stronger and more numerous pro-vaccination and against-vaccination reasons (confirming Hypothesis 1A). This result suggests that greater awareness of one's emotions and of what one is feeling promotes higher fluency in the production of reasons about the vaccination. Research has shown that people can be ambivalent about vaccines and hold both positive and negative reasons [ 2 , 44 ]. It is reasonable to assume that, compared to people with low intra-personal emotional competences, those with high intra-personal emotional competences are more likely to have higher awareness of these contrasting attitudes and to embrace them without suppressing one of the two stances. Furthermore, the results showed that only high inter-personal emotional competences influence the generation of multiple strong reasons in favor of vaccination, and this appears to be related to the perception of vaccines as a public good and a tool to protect others. As for risk perception, a moderate to high perception of risk associated with COVID-19 influences the generation of strong pro-vaccination reasons (confirming Hypothesis 1B). These results are in line with the literature showing that a high perception of risk associated with COVID-19 positively influences the decision to get vaccinated [ 30 , 31 , 45 , 46 , 47 ]. In particular, perceiving a medium/high risk leads to generating a high number of reasons strongly in favor of vaccination, while reducing the number and weight of the reasons against the vaccine. The main premise of the psychological literature examining the relationship between risk perception and affect is that one’s behaviors are affected by rapid and intuitive evaluations, either positive or negative, people make while assessing things happening around them [ 48 , 49 ]. Thus, an event is evaluated not only on the basis of objective information, but also on the basis of the experienced feelings. Emotional competence, which is clearly related to affect, also modulates how we perceive and process the emotional component underlying our judgments [ 36 ].
The results also show that, compared with younger people, those over 45 more frequently produce reasons in favor of vaccines while those over 65 produce fewer reasons against vaccination. These results are in line with the fact that younger people are at lower risk of severe consequences than older people [ 50 ], but can also be explained by considering that age was particularly salient during the period of the data collection, as the vaccination campaign was phased out by age groups, starting from the elderly. As for gender, women produced less strong pro-vaccine and weak-against vaccine reasons than men. These results are congruent with the general findings in the literature on vaccine hesitancy showing that females are more hesitant than males [ 5 , 51 , 52 ]. Furthermore, medium and high educational levels favored the production of both pro- and against-vaccination reasons, whereas not being in a relationship or being divorced/separated increased the generation of a strong reason against vaccination. Consistent with previous work [ 53 ], we confirmed that non-health professionals participants or non-key workers categories showed a lower intention to get vaccinated and a higher likelihood of having refused the vaccine compared to health care and key workers.
Once the role of demographics aspects and individual differences on the generation of reasons pro and/or against vaccination had been established, we ran two additional models to assess the role that those reasons have on the decision to accept the vaccination (see Fig. 1 ). More specifically, we tested the hypothesis that a higher number of pro- (vs. against-) vaccination reasons, connoted by a higher weight, corresponded to a stronger (vs. weaker) acceptance of vaccination (Hypothesis 2). Since data collection took place between March and April 2021, when the vaccination campaign had already started in Italy, we developed two different regression models, with the first investigating the willingness to be vaccinated in participants who were not yet offered the vaccine and the second investigating the likelihood of accepting/booking or refusing the vaccine in those who already received the offer. In particular, thanks to the propensity score weighting technique, we managed to reduce the estimates bias, especially for those factors (age, occupational status, and educational level) that influenced the vaccine offer the most [ 54 ]. The results of the two models are very similar, as the intention to get vaccinated and the likelihood of having accepted/booked the vaccine are predicted by the same factors. Specifically, the production of strong positive reasons increases either the intention to get vaccinated or having accepted/booked the vaccination. In contrast, generating strong negative reasons reduces vaccination intention and predicts the refusal of the vaccination. Hypothesis 2 is thus confirmed.
Results on the interactions between reasons, pro- and against-vaccination, and vaccination intention or vaccination choice are particularly worthy of attention. The third hypothesis was derived from the literature on prospect theory [ 25 , 26 ], suggesting that at equal intensity subjective losses are more important in determining a decision than subjective gains. We therefore expected that negative reasons would count more than positive reasons in deciding whether to get vaccinated or to accept the vaccine. However, in contrast to our hypothesis, the results showed that just the generation of a single positive reason with a strong weight was enough to shift behavior and attitude in favor of the vaccination, regardless of the number and weight of negative reasons. In other words, vaccine refusal is predicted by the absence of any positive strong reasons, while when people generate both positive and negative reasons, the positive ones seem to yield a particularly important role when having a strong weight. According to prospect theory, people evaluate their goals depending on the reference point they focus on. During the pandemic, the vaccination offered an opportunity to be safer, reduced the risk of infection, and more generally appeared as the best way to re-open and get back to life as it was before COVID-19. After a year of pandemic characterized by periods of lockdown and some re-opening attempts, people were likely feeling in a state of loss (e.g., the lost freedom to go out and meet with friends and family, the lost freedom of traveling) and were looking forward to whatever chance available to recover and return to their previous lifestyle and habits. Just as those who gamble are willing to do anything to make up for a loss, so probably those who were not entirely certain about the vaccine were more willing to take risks to recover the loss in quality of life. It follows that the pandemic emergency made people forgo some of their doubts about the vaccine when, at the same time, they had reasons to get their shot. In addition, several studies [ 19 , 55 , 56 ] have highlighted the relationship between anticipated regret and vaccination, showing that anticipated regret is associated with an increased likelihood of adhering, or having one's children adhere, to vaccine offerings. Trusting that the vaccine would work, focusing less on its potential side effects, made sense for people who were looking forward to recovering what was perceived (and was indeed) a loss of quality of life and freedom, because they desired to be back doing the things had ever enjoyed doing (e.g., going to restaurants, movies, etc.). This finding is also interesting from a communicative perspective: providing positive reasons that resonate well with people and have therefore a strong weight for them could offset their doubts, yielding to a greater acceptance of COVID-19 vaccination.
Therefore, it is crucial to consider what kind of reasons drive the decision toward or against vaccination. Allowing participants to openly report their reasons pro- or against- vaccination can facilitate a freer exploration of the concerns and reservations of the most hesitant individuals [ 24 ], thus providing valuable insights for shaping future vaccine-related communications. In fact, thanks to the regression tree on vaccination intention, it emerges that positive attitudes toward vaccines are strongly determined by "Protection" and "Community Protection" reasons. The fact that the sense of individual and collective protection is among the principal determinants of the decision with respect to COVID-19 vaccines suggests that in general vaccination is seen as a means of avoiding nefarious clinical consequences. The effect of the sense of communal protection as the reason favoring vaccination and of other-oriented S-PEC in determining the generation of multiple pro-vaccine motivations confirms previous results suggesting that people often are more willing to get vaccinated primarily to protect their loved ones [ 57 , 58 , 59 ], especially when they have a good understanding of how community immunity works [ 60 , 61 ]. However, it is worth mentioning that, at the time the study was conducted (March–April 2021), there was still uncertainty about whether COVID-19 vaccines could provide sterilizing immunity (i.e., could prevent the transmission of the infection) in addition to protecting the individual. To foster people's willingness to get vaccinated, it is crucial from a public health perspective that people understand that even when vaccines do not yield sterilizing immunity, vaccination can still increase protection of others by reducing the circulation of the virus.
The reasons that influenced the willingness to be vaccinated or the vaccination acceptance/booking were generally in line with the existing literature, although they differed depending on whether respondents had already been offered a vaccine or not: among those who did not received a vaccination offer, the main reasons promoting vaccination acceptance were protection against COVID-19 for oneself, one's family, friends, and community [ 23 ], while among the main reasons that reduced vaccination adherence for those who got the vaccine offer we found the lack of clinical trials [ 62 , 63 ], as well as the distrust of institutions and science [ 22 ]. This latter emerged as the most reported negative reason by those who have refused the vaccine and those who have not yet received the vaccine offer. Thus, effective communication aimed at defusing the perception of risk regarding vaccines themselves should focus on enhancing trust in the scientific process and experimental rigor. Indeed, these reasons were deemed as very important not only by those who refused the vaccination, but also by those who had not yet been offered the vaccine, and even by those who held mixed feelings but eventually chose to get vaccinated. While it is unlikely that individuals firmly against vaccination will be persuaded by simple interventions [ 64 ], we should keep in mind that vaccine hesitancy is a dynamic process. As such, reducing hesitancy or enhancing ambivalence, for example through motivational interviewing (e.g., [ 65 , 66 ]), could potentially lead to small shifts towards greater vaccine acceptance.
Our findings are also in line with the results of other international studies that have used a qualitative approach to examine reasons for and against vaccinations. For example, Hamilton and colleagues [ 67 ] employed a qualitative content analysis to extract the main motivations for and concerns about COVID-19 vaccination from medical records obtained by 102 consults in Australia. The study was conducted in June 2021, and revealed that most consults were driven by doubts about the vaccine available and recommended at that time (i.e., ChAdOx1-S, also known as Vaxzevria), followed by need for further information regarding vaccines and vaccination, also considering specific comorbidities. Notwithstanding the peculiarity of the Australian context in which a very low number of COVID-19 infections was observed, the analysis performed by Hamilton et al. [ 67 ] revealed a set of themes that largely overlaps with the reasons identified in our study. Indeed, among the reason to get vaccinated, 5 themes emerged: a) Protection, b) Occupational or facility responsibility or requirement, c) Trust in primary healthcare physician, d) Autonomy, and e) Civic duty, likewise, concerns about vaccination were mainly in terms of: a) Perceived vaccine risks, b) Perceived vaccine performance, c) Uncertainty, d) Autonomy, and e) Fairness in access. An aspect worth noting is that after the consultation, 81% of participants received the vaccination, 19% did not. Consistent results were observed in another study by Purvis and colleagues [ 68 ] conducted in the USA, which focused specifically on “hesitant adopters”, i.e. those who accepted vaccination but showed some level of hesitancy. To note that in this study the focus was on factors influencing the decision to get the COVID-19 vaccine, not on reasons against it. The authors interviewed 49 participants as a follow up of a larger study ( N = 2022) conducted from mid-September 2021 through mid-October 2021, to explore factors that influenced their decision-making process about COVID-19 vaccination [ 68 ]. Two main themes emerged, each with four subthemes: 1) sociocultural context (political, cultural, health professionals, employment, and media environment) and 2) individual and group influences (attitudes and beliefs related to vaccines, family and social networks, free to return to normal, and COVID-19 outcomes).
As for the Italian context, to the best of our knowledge, only one study (i.e., [ 69 ]) attempted to provide a qualitative examination of the concept associated with vaccination in general, through open-ended and closed questions. Notably, this study was conducted a year later than our own study (April–May 2022) and was administered to a non-representative sample of Italians. The authors used a combination of closed and open-ended questions to assess concepts associated with vaccination in general. Consistent with our findings, Boragno et al. reported that participants who had been vaccinated against COVID-19 (92% of the sample) frequently mentioned concepts related to protection and salvation, whereas those who were not vaccinated frequently mentioned mistrust and ambivalence as concepts associated with vaccination [ 69 ].
This study has some limitations. First, COVID-19 perceived risk score was obtained only with respect to the disease and a similar score should be of interest for the COVID-19 vaccine. Second, data were collected during a vaccine offer limited to a well-defined slice of the population and the investigation on the vaccine acceptance/booking has, as a consequence, a limited sample size. Finally, the lack of a longitudinal perspective does not allow us to evaluate how strong the association is between the willingness to get vaccinated, vaccine acceptance and potential changes in risk perception. Thus, we cannot generalize our results beyond the period of data collection and to other countries or health systems. Since the dynamics have now changed, results may not apply to the decision to get a booster shot or not or an annual shot, however it might be interesting to study what motivations are most relevant now. Likewise, it remains to be established whether our results are generalisable to other populations.
Future studies could consider how the interaction between perceived risk associated with the disease and perceived risk associated with the vaccine influences the choice to get the shot. Furthermore, it would be important to explore how we can harness the reasons that most hold back vaccination in a specific communication strategy for the most hesitant people. Moreover, at the time of data collection, the vaccination campaign was still at an early stage, and only a small portion of the population had already received their shot. Therefore, we believe that it might be of particular interest to know more in detail, with a larger sample, what are the reasons that to date, almost 2 years after the release of the vaccine, still make some people reject the vaccine. Only by knowing these reasons will it be possible to develop appropriate vaccination campaigns.
In conclusion, our work examined pro- and against-vaccination reasons and how these, and their interaction, influence the decision to get vaccinated or not. Specifically, high emotional competence and risk perception influence the generation of pro- and against-vaccination reasons and that the presence of a strong pro-vaccination reason shifts intention toward vaccination. We also highlighted the category of reasons that influence intention to vaccinate. That said, given that the discussion about the next doses is still open and that in any case the next pandemic is a matter of when and not if [ 70 ], it is of paramount importance to know the best way to counteract vaccine hesitancy, fostering more effective communication strategies.
Availability of data and materials
Raw data are available on https://osf.io/dpn2q/?view_only=af05427467634411b471af7a8475ffab .
European Centre for Disease Prevention and Control. Cumulative uptake (%) of the primary course among adults (+18) in EU/EEA countries as of 2023–09–07. https://vaccinetracker.ecdc.europa.eu/public/extensions/COVID-19/vaccine-tracker.html#uptake-tab . Accessed 12 Sept 2023.
MacDonald NE. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015; https://doi.org/10.1016/j.vaccine.2015.04.036.
Bedford H, Attwell K, Danchin M, Marshall H, Corben P, Leask J. Vaccine hesitancy, refusal and access barriers: the need for clarity in terminology. Vaccine. 2018; https://doi.org/10.1016/j.vaccine.2017.08.004.
Paul KT, Zimmermann BM, Corsico P, Fiske A, Geiger S, Johnson S, Kuiper JM, Lievevrouw E, Marelli L, Prainsack B, Spahl W. Anticipating hopes, fears and expectations towards COVID-19 vaccines: a qualitative interview study in seven European countries. SSM-Qual Res Health. 2022; https://doi.org/10.1016/j.ssmqr.2021.100035.
Murphy J, Vallières F, Bentall RP, Shevlin M, McBride O, Hartman TK, McKay R, Bennett K, Mason L, Gibson-Miller J, Levita L. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021; https://doi.org/10.1038/s41467-020-20226-9.
Soares P, Rocha JV, Moniz M, Gama A, Laires PA, Pedro AR, Dias S, Leite A, Nunes C. Factors associated with COVID-19 vaccine hesitancy. Vaccines. 2021; https://doi.org/10.3390/vaccines9030300.
Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of US adults. Ann Internal Med. 2020; https://doi.org/10.7326/M20-3569.
Robertson E, Reeve KS, Niedzwiedz CL, Moore J, Blake M, Green M, Katikireddi SV, Benzeval MJ. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav Immun. 2021; https://doi.org/10.1016/j.bbi.2021.03.008.
Caserotti M, Gavaruzzi T, Girardi P, Tasso A, Buizza C, Candini V, Zarbo C, Chiarotti F, Brescianini S, Calamandrei G, Starace F. Who is likely to vacillate in their COVID-19 vaccination decision? Free-riding intention and post-positive reluctance. Prev Med. 2022; https://doi.org/10.1016/j.ypmed.2021.106885.
Caserotti M, Girardi P, Tasso A, Rubaltelli E, Lotto L, Gavaruzzi T. Joint analysis of the intention to vaccinate and to use contact tracing app during the COVID-19 pandemic. Sci Rep. 2022; https://doi.org/10.1038/s41598-021-04765-9 .
Pereira B, Fehl AG, Finkelstein SR, Jiga‐Boy GM, Caserotti M. Scarcity in COVID‐19 vaccine supplies reduces perceived vaccination priority and increases vaccine hesitancy. Psychol Mark. 2022; https://doi.org/10.1002/mar.21629 .
Đorđević JM, Mari S, Vdović M, Milošević A. Links between conspiracy beliefs, vaccine knowledge, and trust: Anti-vaccine behavior of Serbian adults. Soc Sci Med. 2021; https://doi.org/10.1016/j.socscimed.2021.113930 .
Candini V, Brescianini S, Chiarotti F, Zarbo C, Zamparini M, Caserotti M, Gavaruzzi T, Girardi P, Lotto L, Tasso A, Starace F. Conspiracy mentality and health-related behaviour during the COVID-19 pandemic: a multi-wave survey in Italy. Public Health. 2023, https://doi.org/10.1016/j.puhe.2022.11.005 .
Asch DA, Baron J, Hershey JC, Kunreuther H, Meszaros J, Ritov I, Spranca M. Omission bias and pertussis vaccination. Medic Decis Mak. 1994; https://doi.org/10.1177/0272989X9401400204 .
Meszaros JR, Asch DA, Baron J, Hershey JC, Kunreuther H, Schwartz-Buzaglo J. Cognitive processes and the decisions of some parents to forego pertussis vaccination for their children. J Clin Epidemiol. 1996; https://doi.org/10.1016/0895-4356(96)00007-8 .
Bell RA, McGlone MS, Dragojevic M. Vicious viruses and vigilant vaccines: Effects of linguistic agency assignment in health policy advocacy. J Health Commun. 2014; https://doi.org/10.1080/10810730.2013.81133 .
Nan X, Madden K. HPV vaccine information in the blogosphere: how positive and negative blogs influence vaccine-related risk perceptions, attitudes, and behavioral intentions. Health Commun. 2012; https://doi.org/10.1080/10410236.2012.661348 .
Christy SM, Winger JG, Raffanello EW, Halpern LF, Danoff-Burg S, Mosher CE. The role of anticipated regret and health beliefs in HPV vaccination intentions among young adults. J Behav Med. 2016; https://doi.org/10.1007/s10865-016-9716-z .
Chapman GB, Coups EJ. Emotions and preventive health behavior: worry, regret, and influenza vaccination. Health Psychol. 2006; https://doi.org/10.1037/0278-6133.25.1.82 .
Klasko-Foster LB, Przybyla S, Orom H, Gage-Bouchard E, Kiviniemi MT. The influence of affect on HPV vaccine decision making in an HPV vaccine naïve college student population. Prev Med Rep. 2020; https://doi.org/10.1016/j.pmedr.2020.101195.
World Health Organization = Organisation mondiale de la Santé. Understanding the behavioural and social drivers of vaccine uptake WHO position paper – May 2022 – Comprendre les facteurs comportementaux et sociaux de l’adoption des vaccins Note de synthèse de l’OMS – mai 2022. Weekly Epidemiological Record = Relevé épidémiologique hebdomadaire, 97 (20), 209 - 224. World Health Organization = Organisation mondiale de la Santé. 2022; https://apps.who.int/iris/handle/10665/354460 .
Fieselmann J, Annac K, Erdsiek F, Yilmaz-Aslan Y, Brzoska P. What are the reasons for refusing a COVID-19 vaccine? A qualitative analysis of social media in Germany. BMC Public Health. 2022; https://doi.org/10.1186/s12889-022-13265-y .
Moore R, Purvis RS, Hallgren E, Willis DE, Hall S, Reece S, CarlLee S, Judkins H, McElfish PA. Motivations to vaccinate among hesitant adopters of the COVID-19 vaccine. J Commun Health. 2022; https://doi.org/10.1007/s10900-021-01037-5 .
Cassels TG, Birch SA. Comparisons of an open-ended vs. forced-choice ‘mind reading’task: Implications for measuring perspective-taking and emotion recognition. PLoS One. 2014; https://doi.org/10.1371/journal.pone.0093653 .
Kahneman D, & Tversky A. On the interpretation of intuitive probability: A reply to Jonathan Cohen. 1979; https://doi.org/10.1016/0010-0277(79)90024-6 .
Tversky A, Kahneman D. Advances in prospect theory: Cumulative representation of uncertainty. J Risk Uncertain. 1992; https://doi.org/10.1007/BF00122574 .
Baumeister RF, Bratslavsky E, Finkenauer C, Vohs KD. Bad is stronger than good. Review of general psychology. 2001; https://doi.org/10.1037/1089-2680.5.4.323 .
Chor JS, Ngai KL, Goggins WB, Wong MC, Wong SY, Lee N, Leung TF, Rainer TH, Griffiths S, Chan PK. Willingness of Hong Kong healthcare workers to accept pre-pandemic influenza vaccination at different WHO alert levels: two questionnaire surveys. BMJ. 2009; https://doi.org/10.1136/bmj.b3391 .
Pareek M, Clark T, Dillon H, Kumar R, Stephenson I. Willingness of healthcare workers to accept voluntary stockpiled H5N1 vaccine in advance of pandemic activity. Vaccine. 2009; https://doi.org/10.1016/j.vaccine.2008.12.006 .
Viswanath K, Bekalu M, Dhawan D, Pinnamaneni R, Lang J, McLoud R. Individual and social determinants of COVID-19 vaccine uptake. BMC Public Health. 2021; https://doi.org/10.1186/s12889-021-10862-1 .
Caserotti M, Girardi P, Rubaltelli E, Tasso A, Lotto L, Gavaruzzi T. Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc Sci Med. 2021; https://doi.org/10.1016/j.socscimed.2021.113688 .
Finucane ML, Peters E, & Slovic P. (2003). Judgment and decision making: The dance of affect and reason. In: S. L. Schneider & J. Shanteau, editors. Emerging Perspectives on Judgment and Decision Research Cambridge. University Press; 2003. 327–364. https://doi.org/10.1017/CBO9780511609978.012 .
Pittarello A, Conte B, Caserotti M, Scrimin S, Rubaltelli E. Emotional intelligence buffers the effect of physiological arousal on dishonesty. Psychonomic Bull Rev. 2018; https://doi.org/10.3758/s13423-017-1285-9 .
Scrimin S, Rubaltelli E. Dehumanization after terrorism: the role of psychophysiological emotion regulation and trait emotional intelligence. Curr Psychol. 2021; https://doi.org/10.1007/s12144‐019‐00189‐x .
Tomljenovic H, Bubic A, Erceg N. It just doesn’t feel right–the relevance of emotions and intuition for parental vaccine conspiracy beliefs and vaccination uptake. Psychol Health. 2020; https://doi.org/10.1080/08870446.2019.1673894 .
Gavaruzzi T, Caserotti M, Leo I, Tasso A, Speri L, Ferro A, Fretti E, Sannino A, Rubaltelli E, Lotto L. The role of emotional competences in parents’ vaccine hesitancy. Vaccines. 2021; https://doi.org/10.3390/vaccines9030298 .
ISTAT. Resident population on 1st January: By age. http://dati.istat.it/?lang=en&SubSessionId=d7024c9e-239b-455d-924b-df19345a27b2 . Accessed Sept 25, 2023.
Mikolajczak M., Brasseur S, & Fantini-Hauwel C. Measuring intrapersonal and interpersonal EQ: The short profile of emotional competence (S-PEC). Pers Individ Differ. 2014; https://doi.org/10.1016/j.paid.2014.01.023 .
Olmos A, Govindasamy P. A practical guide for using propensity score weighting in R. Pract Assess Res Eval. 2015; https://doi.org/10.7275/jjtm-r398 .
Smithson M, Verkuilen J. A better lemon squeezer? Maximum-likelihood regression with beta-distributed dependent variables. Psychological methods. 2006; https://doi.org/10.1037/1082-989X.11.1.54 .
Ferrari S, Cribari-Neto F. Beta regression for modelling rates and proportions. Journal of applied statistics. 2004; https://doi.org/10.1080/0266476042000214501 .
Thernau T, Atkinson B, Ripley B. Rpart: Recursive Partitioning. R Package 4.1–0. http://CRAN.R-project.org/package=rpart .
RC Team. R Core Team R: A language and environment for statistical computing. R. . Foundation for Statistical Computing. 2014. https://www.r-project.org .
Freeman D, Loe BS, Chadwick A, Vaccari C, Waite F, Rosebrock L, ... & Lambe S. COVID-19 vaccine hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol Med. 2022; https://doi.org/10.1017/S0033291720005188 .
Caserotti M, Gavaruzzi T, Girardi P, Sellaro R, Rubaltelli E, Tasso A, Lotto L. People’s perspectives about COVID-19 vaccination certificate: Findings from a representative Italian sample. Vaccine. 2022; https://doi.org/10.1016/j.vaccine.2022.08.016 .
MacDonald NE, Comeau J, Dubé È, Graham J, Greenwood M, Harmon S, McElhaney J, Meghan McMurtry C, Middleton A, Steenbeek A, Taddio A. Royal society of Canada COVID-19 report: Enhancing COVID-19 vaccine acceptance in Canada. Facets. 2021; https://doi.org/10.1139/facets-2021-0037 .
Schwarzinger M, Watson V, Arwidson P, Alla F, Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. 2021; https://doi.org/10.1016/S2468-2667(21)00012-8 .
Slovic P, Finucane M, Peters E, MacGregor DG. Rational actors or rational fools: Implications of the affect heuristic for behavioral economics. J Socio-Econ. 2002; https://doi.org/10.1016/S1053-5357(02)00174-9 .
Slovic P, Finucane ML, Peters E, MacGregor DG. Risk as analysis and risk as feelings: Some thoughts about affect, reason, risk and rationality. In The feeling of risk 2013 Mar 7 (pp. 21–36). Routledge.
Bhopal SS, Bagaria J, Olabi B, Bhopal R. Children and young people remain at low risk of COVID-19 mortality. Lancet Child Adolesc Health. 2021; https://doi.org/10.1016/S2352-4642(21)00066-3 .
Lazarus JV, Wyka K, Rauh L, Rabin K, Ratzan S, Gostin LO, Larson HJ, El-Mohandes A. Hesitant or not? The association of age, gender, and education with potential acceptance of a COVID-19 vaccine: a country-level analysis. J Health Commun. 2020; https://doi.org/10.1080/10810730.2020.1868630 .
Seale H, Heywood AE, Leask J, Sheel M, Durrheim DN, Bolsewicz K, Kaur R. Examining Australian public perceptions and behaviors towards a future COVID-19 vaccine. BMC Infect Dis. 2021; https://doi.org/10.1186/s12879-021-05 .
Butter S, McGlinchey E, Berry E, Armour C. Psychological, social, and situational factors associated with COVID‐19 vaccination intentions: A study of UK key workers and non‐key workers. Br J Health Psychol. 2022; https://doi.org/10.1111/bjhp.12530 .
Freedman DA, Berk RA. Weighting regressions by propensity scores. Eval Rev. 2008; https://doi.org/10.1177/0193841X08317586 .
Lagoe C, Farrar KM. Are you willing to risk it? The relationship between risk, regret, and vaccination intent. Psychol Health Med. 2015; https://doi.org/10.1080/13548506.2014.911923 .
Ziarnowski KL, Brewer NT, Weber B. Present choices, future outcomes: anticipated regret and HPV vaccination. Prev Med. 2009; https://doi.org/10.1016/j.ypmed.2008.10.006 .
Betsch C, Böhm R, Korn L, Holtmann C. On the benefits of explaining herd immunity in vaccine advocacy. Nat Hum Behav. 2017; https://doi.org/10.1038/s41562-017-0056 .
Loomba S, de Figueiredo A, Piatek SJ, de Graaf K, Larson HJ. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat Hum Behav. 2021; https://doi.org/10.1038/s41562-021-01056-1 .
Pfattheicher S, Petersen MB, Böhm R. Information about herd immunity through vaccination and empathy promote COVID-19 vaccination intentions. Health Psychol. 2022;41(2):85.
Article PubMed Google Scholar
Hakim H, Provencher T, Chambers CT, Driedger SM, Dube E, Gavaruzzi T, ... & Witteman HO. Interventions to help people understand community immunity: a systematic review. Vaccine. 2019; https://doi.org/10.1016/j.vaccine.2018.11.016 .
Hakim H, Bettinger JA, Chambers CT, Driedger SM, Dubé E, Gavaruzzi T, Giguere AMC, Kavanagh É, Leask J, MacDonald SE, Orji R, Parent E, Paquette J, Roberge J, Sander B, Scherer AM, Tremblay-Breault M, Wilson K, Reinharz D, Witteman HO. A Web Application About Herd Immunity Using Personalized Avatars: Development Study. Journal of medical Internet research. 2020; https://doi.org/10.2196/20113 .
Callaghan T, Moghtaderi A, Lueck JA, Hotez P, Strych U, Dor A, Fowler EF, Motta M. Correlates and disparities of intention to vaccinate against COVID-19. Soc Sci Med (1982). 2021; https://doi.org/10.1016/j.socscimed.2020.113638 .
Griffith J, Marani H, Monkman H. COVID-19 vaccine hesitancy in Canada: Content analysis of tweets using the theoretical domains framework. Journal of medical Internet research. 2021; https://doi.org/10.2196/26874 .
Attwell K, Lake J, Sneddon J, Gerrans P, Blyth C, & Lee J. Converting the maybes: Crucial for a successful COVID-19 vaccination strategy. PLoS One. 2021; https://doi.org/10.1371/journal.pone.0245907 .
Breckenridge LA, Burns D, & Nye C. The use of motivational interviewing to overcome COVID‐19 vaccine hesitancy in primary care settings. Public Health Nurs. 2022; https://doi.org/10.1111/phn.13003 .
Gabarda A, & Butterworth SW. Using best practices to address COVID-19 vaccine hesitancy: The case for the motivational interviewing approach. Health Promot Pract, 2021; https://doi.org/10.1177/152483992110164 .
Hamilton EM, Oversby S, Ratsch A, & Kitchener S.COVID-19 vaccination: An exploratory study of the motivations and concerns detailed in the medical records of a regional Australian population. Vaccines. 2022; https://doi.org/10.3390/vaccines10050657 .
Purvis RS, Moore R, Willis DE, Hallgren E, & McElfish PA. Factors influencing COVID-19 vaccine decision-making among hesitant adopters in the United States. Human Vaccines Immunother. 2022; https://doi.org/10.1080/21645515.2022.2114701 .
Boragno P, Fiabane E, Taino I, Maffoni M, Sommovigo V, Setti I, Gabanelli P. Perceptions of COVID-19 Vaccines: Protective Shields or Threatening Risks? A Descriptive Exploratory Study among the Italian Population. Vaccines. 2023; https://doi.org/10.3390/vaccines11030642 .
Centers for Disease Control and Prevention. Why it matters: The pandemic threat. Retrieved December. 2020;1:2020.
Download references
Acknowledgements
Not applicable.
Open access funding provided by Università degli Studi di Padova. The project was developed thanks to institutional research funding of TG and AT.
Author information
Authors and affiliations.
Department of Developmental Psychology and Socialization, University of Padova, Padua, Italy
Marta Caserotti, Roberta Sellaro, Enrico Rubaltelli & Lorella Lotto
Department of Environmental Sciences, Informatics and Statistics, Ca’ Foscari University of Venezia, Venice, Italy
Paolo Girardi
Department of Humanities, University of Ferrara, Ferrara, Italy
Alessandra Tasso
Department of Medical and Surgical Sciences, University of Bologna, Bologna, Italy
Teresa Gavaruzzi
You can also search for this author in PubMed Google Scholar
Contributions
MC: Conceptualization, Formal analysis, Visualization, Writing—original draft and Writing—review & editing. PG: Conceptualization, Formal analysis, Visualization, Writing—original draft. RS: Conceptualization, Writing—review & editing. ER: Conceptualization, Writing—review & editing. AT: Conceptualization, Writing—review & editing. LL: Conceptualization, Writing—review & editing. TG: Conceptualization, Visualization, Writing—review & editing.
Corresponding author
Correspondence to Marta Caserotti .
Ethics declarations
Ethics approval and consent to participate.
The project was approved by the ethical committee for Psychology Research of the University of Padova (Italy), with protocol number 3911/2020, and informed consent was obtained for all participants.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: appendix 1..
Scoring for pro- and against-vaccination reasons. Appendix 2. Structure of the questionnaire. Table S1. Selection criteria. Table S2. Number of items, internal consistency (Cronbach’s α), name of the items and their estimated loadings, total deviance explained by the loadings and proportion of variance explained by EFA for COVID-19 perceived risk. Table S3. Odds ratios (ORs) estimated by the logistic model for the propensity score weighting for the COVID-19 vaccine offer. Table S4 . Predicted willingness to get vaccinated by combination of pro- and against-vaccination reasons by category of reference. Table S5. Frequency of reported categories of pro- and against-vaccination reasons overall, and by COVID-19 vaccine status. Figure S1. Distribution of the propensity scores by vaccine offer.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Caserotti, M., Girardi, P., Sellaro, R. et al. To vaccinate or not to vaccinate? The interplay between pro- and against- vaccination reasons. BMC Public Health 23 , 2207 (2023). https://doi.org/10.1186/s12889-023-17112-6
Download citation
Received : 12 December 2022
Accepted : 30 October 2023
Published : 09 November 2023
DOI : https://doi.org/10.1186/s12889-023-17112-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Pro-and against-reasons
- Vaccination intention
- Risk perception
- Emotional competences
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
An Overview of the Vaccine Debate
Looking at Both Sides of the Argument
There is a wealth of research demonstrating the efficacy and safety of vaccines —including how some have virtually eradicated infectious diseases that once killed millions. However, this has done little to sway those who believe that untold harms are being hidden from the American public.
The vaccine debate—including the argument as to whether vaccines are safe, effective, or could cause conditions like autism —has received a lot of attention from the media in recent years. With so much conflicting information being publicized, it can be a challenge to discern what is true and what is not. Therefore, it is important to learn the facts before making health decisions.
Claims and Controversy
Those who are part of the anti-vaccination movement include not only non-medical professionals but several scientists and healthcare providers who hold alternative views about vaccines and vaccination in general.
Some notable examples include:
- British healthcare provider Andrew Wakefield, who in 1998 published research linking the MMR vaccine and autism . That study has since been retracted, and he was later removed from the medical registry in the United Kingdom for falsifying scientific data.
- Pediatrician Bob Sears, who wrote the bestseller "The Vaccine Book: Making the Right Decision for your Child ," which suggested that many essential childhood vaccines were "optional." However, he was subsequently put on probation by the Medical Review Board of California in 2018 for alleged medical negligence and the inappropriate writing of medical exemptions for vaccinations.
- Dr. Jane M. Orient, director of the Association of American Healthcare Providers and Surgeons, who was among the leading opponents of the COVID-19 vaccine and one of the leading proponents of using hydroxychloroquine to treat COVID-19 during the pandemic.
These opposing views and claims, along with other information promoted by the news and social media, have led some people to question whether they know everything they need to know about vaccines.
Common Concerns Regarding Vaccines
The arguments made against vaccines are not new and have been made well before the first vaccine was developed for smallpox back in the 18th century.
The following are some of the common arguments against vaccines:
- Vaccines contain "toxic" ingredients that can lead to an assortment of chronic health conditions such as autism.
- Vaccines are a tool of "Big Pharma," in which manufacturers are willing to profit off of harm to children.
- Governments are "pharma shills," meaning they are bought off by pharmaceutical companies to hide cures or approve drugs that are not safe.
- A child’s immune system is too immature to handle vaccines , leading the immune system to become overwhelmed and trigger an array of abnormal health conditions.
- Natural immunity is best , suggesting that a natural infection that causes disease is "better" than receiving a vaccine that may cause mild side effects.
- Vaccines are not tested properly , suggesting a (highly unethical) approach in which one group of people is given a vaccine, another group is not, and both are intentionally inoculated with the same virus or bacteria.
- Infectious diseases have declined due in part to improved hygiene and sanitation , suggesting that hand-washing and other sanitary interventions are all that are needed to prevent epidemics.
- Vaccines cause the body to "shed" virus , a claim that is medically true, although the amount of shed virus is rarely enough to cause infection.
The impact of anti-vaccination claims has been profound. For example, it has led to a resurgence of measles in the United States and Europe, despite the fact that the disease was declared eliminated in the U.S. back in 2000.
Studies have suggested that the anti-vaccination movement has cast doubt on the importance of childhood vaccinations among large sectors of the population. The added burden of the COVID-19 pandemic has led to further declines in vaccination rates.
There is also concern that the same repercussions may affect COVID-19 vaccination rates—both domestically and abroad. Ultimately, vaccine rates must be high for herd immunity to be effective.
According to a study from the Centers for Disease Control and Prevention (CDC), the rate of complete recommended vaccination among babies age 5 months has declined from 66.6% in 2016 to 49.7% by May 2020. Declines in vaccination coverage were seen in other age groups as well.
Benefits of Vaccination
Of the vaccines recommended by the CDC, the benefits of immunization are seen to overwhelmingly outweigh the potential risks. While there are some people who may need to avoid certain vaccines due to underlying health conditions, the vast majority can do so safely.
According to the U.S. Department of Health and Human Services, there are five important reasons why your child should get the recommended vaccines:
- Immunizations can save your child’s life . Consider that polio once killed up to 30% of those who developed paralytic symptoms. Due to polio vaccination, the disease is no longer a public health concern in the United States.
- Vaccination is very safe and effective . Injection site pain and mild, flu-like symptoms may occur with vaccine shots. However, serious side effects , such as a severe allergic reaction, are very rare.
- Immunization protects others . Because respiratory viruses can spread easily among children, getting your child vaccinated not only protects your child but prevents the further spread of disease.
- Immunizations can save you time and money . According to the non-profit Borgen Project, the average cost of a measles vaccination around the world is roughly $1.76, whereas the average cost of treating measles is $307. In the end, the cost of prevention is invariably smaller than the cost of treatment.
- Immunization protects future generations . Smallpox vaccinations have led to the eradication of smallpox . Rubella (German measles) vaccinations have helped eliminate birth defects caused by infection of pregnant mothers in the developed world. With persistence and increased community uptake, measles could one day be declared eliminated (again) as well.
A Word From Verywell
If you have any questions or concerns about vaccinations, do not hesitate to speak with your healthcare provider or your child's pediatrician.
If a vaccine on the immunization schedule has been missed, speak to a healthcare provider before seeking the vaccination on your own (such as at a pharmacy or clinic). In some cases, additional doses may be needed.
Vaccines Healthcare Provider Discussion Guide
Get our printable guide for your next healthcare provider's appointment to help you ask the right questions.
Sign up for our Health Tip of the Day newsletter, and receive daily tips that will help you live your healthiest life.
Thank you, {{form.email}}, for signing up.
There was an error. Please try again.
Eggerton L. Lancet retracts 12-year-old article linking autism to MMR vaccines . CMAJ . 2010 Mar 9; 182(4):e199-200. doi:10.1503/cmaj.109-3179
Park A. Doctor behind vaccine-autism link loses license . Time .
Offit PA, Moser CA. The problem with Dr Bob's alternative vaccine schedule . Pediatrics. 2009 Jan;123 (1):e164-e169. doi:10.1542/peds.2008-2189
Before the Medical Board of California, Department of Consumer Affairs, State of California. In the Matter of the Accusation Against Robert William Sears, M.D., Case No. 800-2015-012268 .
Stolberg SG. Anti-vaccine doctor has been invited to testify before Senate committee . The New York Times.
Wolfe RM, Sharp LK. Anti-vaccinationists past and present . BMJ. 2002;325(7361):430-2. doi:10.1136/bmj.325.7361.430
Agley J, Xiao Y. Misinformation about COVID-19: Evidence for differential latent profiles and a strong association with trust in science . BMC Public Health. 2021;21:89. doi:10.1186/s12889-020-10103-x
Centers for Disease Control and Prevention. Measles history .
Hussain A, Ali S, Ahmed M, Hussain S. The anti-vaccination movement: a regression in modern medicine . Cureus . 2018;10(7): e2919. doi:10.7759/cureus.2919
Bramer CA, Kimmins LM, Swanson R, et al. Decline in child vaccination coverage during the COVID-19 pandemic — Michigan Care Improvement Registry, May 2016–May 2020 . MMWR. 2020 May;69(20):630-1. doi:10.15585/mmwr.mm6920e1
Centers for Disease Control and Prevention. Why vaccinate .
Centers for Disease Control and Prevention. Poliomyelitis .
Centers for Disease Control and Prevention. Making the vaccine decision .
Borgen Project. What is the cost of measles in the developed world? .
By Vincent Iannelli, MD Vincent Iannelli, MD, is a board-certified pediatrician and fellow of the American Academy of Pediatrics. Dr. Iannelli has cared for children for more than 20 years.
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Attitudes on voluntary and mandatory vaccination against COVID-19: Evidence from Germany
Roles Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing
Affiliation DIW Berlin / SOEP, Berlin, Germany
* E-mail: [email protected] (CSP); [email protected] (CS)
Affiliation Karlsruhe Institute of Technology, Karlsruhe, Germany
Affiliations DIW Berlin / SOEP, Berlin, Germany, Freie Universität Berlin, Berlin, Germany
- Daniel Graeber,
- Christoph Schmidt-Petri,
- Carsten Schröder

- Published: May 10, 2021
- https://doi.org/10.1371/journal.pone.0248372
- Reader Comments
Several vaccines against COVID-19 have now been developed and are already being rolled out around the world. The decision whether or not to get vaccinated has so far been left to the individual citizens. However, there are good reasons, both in theory as well as in practice, to believe that the willingness to get vaccinated might not be sufficiently high to achieve herd immunity. A policy of mandatory vaccination could ensure high levels of vaccination coverage, but its legitimacy is doubtful. We investigate the willingness to get vaccinated and the reasons for an acceptance (or rejection) of a policy of mandatory vaccination against COVID-19 in June and July 2020 in Germany based on a representative real time survey, a random sub-sample (SOEP-CoV) of the German Socio-Economic Panel (SOEP). Our results show that about 70 percent of adults in Germany would voluntarily get vaccinated against the coronavirus if a vaccine without side effects was available. About half of residents of Germany are in favor, and half against, a policy of mandatory vaccination. The approval rate for mandatory vaccination is significantly higher among those who would get vaccinated voluntarily (around 60 percent) than among those who would not get vaccinated voluntarily (27 percent). The individual willingness to get vaccinated and acceptance of a policy of mandatory vaccination correlates systematically with socio-demographic and psychological characteristics of the respondents. We conclude that as far as people’s declared intentions are concerned, herd immunity could be reached without a policy of mandatory vaccination, but that such a policy might be found acceptable too, were it to become necessary.
Citation: Graeber D, Schmidt-Petri C, Schröder C (2021) Attitudes on voluntary and mandatory vaccination against COVID-19: Evidence from Germany. PLoS ONE 16(5): e0248372. https://doi.org/10.1371/journal.pone.0248372
Editor: Valerio Capraro, Middlesex University, UNITED KINGDOM
Received: October 19, 2020; Accepted: February 25, 2021; Published: May 10, 2021
Copyright: © 2021 Graeber et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: Our analyses rely on the German Socio-Economic Panel (SOEP), an independent scientific data infrastructure established in 1984. We, as users, cannot send the data to the journal and make them publicly available, as this is against SOEP's statutes (and most likely against the statutes of all providers of micro data). However, this should not be a hurdle, as researchers from scientific institutions around the globe can access the data (free of costs) once they have signed a user contract. The scientific use file of the SOEP with anonymous microdata is made available free of charge to universities and research institutes for research and teaching purposes. The direct use of SOEP data is subject to the provisions of German data protection law. Therefore, signing a data distribution contract is the single precondition for working with SOEP data. The data distribution contract can be requested with a form which can be downloaded from: http://www.diw.de/documents/dokumentenarchiv/17/diw_01.c.88926.de/soep_application_contract.pdf .
Funding: The data collection of the SOEP-CoV Study was financially supported by the German Federal Ministry of Education and Research. We acknowledge support by the KIT-Publication Fund of the Karlsruhe Institute of Technology. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Great efforts have been made worldwide to develop a vaccine against COVID-19. When we first drafted this article, in October 2020, 35 different potential vaccines were in clinical trials and 145 were still in the pre-clinical stage. In February 2021, several vaccines have been approved in many countries and are being rolled out, 74 are in clinical trials, and 182 are in the pre-clinical stage [ 1 ].
These developments are very encouraging, as a wide availability of vaccines is seen by many as a prerequisite for a return to a “normal” pre-COVID-19 type of social and economic life. With the growing availability of vaccines comes the hope that coercive measures such as restrictions on international trade, contact restrictions, and travel bans, etc., which cause enormous economic and social costs, may soon be removed and will not need to be reimplemented.
Of course, any vaccine is only an effective contribution to a return to normal life if a sufficiently high number of people are actually vaccinated, yielding herd immunity. If so, vaccination secures a public good: protection from COVID-19 for everyone. From a microeconomic perspective, this raises a well-known problem, free-riding: If the vaccination is freely available but not obligatory, then citizens’ individual decisions determine the extent to which this public good is made available. In order to make that decision, they will weigh their own costs and benefits. These costs include the time sacrificed, physical unpleasantness, possible side effects of a vaccination, etc. The benefits to a particular individual are primarily, but not necessarily exclusively, the reduction in risk to that person’s own health or material well-being. From a welfare perspective, if individuals do not take into account the positive externalities on third parties that their own vaccination triggers, there will be an undersupply of the public good. Following [ 2 , 3 ], individuals’ utility function may also include other-regarding preferences and hence yield a direct benefit from contributions to a public good. In our context, people could therefore benefit from a ‘warm glow of vaccinating’, because by vaccinating themselves they also reduce the risks of others. But even so there is certainly no guarantee that the social optimum will be reached [ 4 ] or that a sufficiently high number of people will freely choose to get vaccinated.
It is frequently argued that vaccination should be made mandatory because of the free-rider problem [ 5 ]: While vaccinated individuals have incurred private costs in terms of discomfort or money and receive the private benefit of a reduced risk of getting the disease, the major collective benefit, the reduced incidence of disease, is public. If enough other people produce the public benefit, and the circulation of the virus decreases accordingly, an individual might rationally decide to free-ride on others’ decisions. A policy of mandatory vaccination would prevent this.
[ 6 ] argue that such a policy would not be necessary: “If vaccinations are perfect, then if one is vaccinated he or she does not care whether others are vaccinated, so there is no longer any public good problem” ([ 6 ], p. 70). Hence there would not be a case in favor of mandatory vaccination, as under such a policy, individuals who would have favored not to be vaccinated are made worse off, while those who anyway would get vaccinated are not better off.
However, by definition, ‘perfect’ vaccination means that everyone vaccinated is perfectly immune [ 6 ]. In the current situation, it can neither be taken for granted that a perfect vaccination is being or will be provided soon, nor that everyone who wants to also will have the possibility to be vaccinated (both financially and in terms of health). If perfect vaccination is not feasible, however, mandatory vaccination is not dominated by a laissez faire solution [ 6 ].
Extensions of this theoretical public good analysis emphasize the relevance of behavioral aspects not typically considered in classical models. The empirical literature also highlights a number of factors that matter for vaccine uptake. For instance [ 7 ], show that social norms matter for an individual’s willingness to get a vaccination and that such norms can suppress vaccine uptake even in the presence of frequent disease outbreaks. Further [ 8 ], show that the design of public vaccination policies should also take intergroup interactions into account. Other-regarding preferences can explain voluntary vaccination uptake, as argued by [ 9 ]. For example [ 10 ], show that the presence of individuals who cannot get vaccinated, like babies and the elderly, increases the willingness to get vaccinated. The static model in [ 6 ] also does not reflect interactive processes [ 9 , 11 ]. show that vaccination is the individually best response until a certain vaccination rate is reached in the population and becomes a social dilemma only from this vaccination rate until herd immunity is maximized. Communicating the social benefits of vaccination can have positive effects, particularly when this protects vulnerable groups, but it can also invite free-riding [ 12 ]. Those people who cannot get vaccinated themselves for medical reasons are particularly vulnerable: they cannot protect themselves even if they wanted to and, hence, depend on their fellow citizens to protect them by preventing the spread of the virus through their vaccination. Children, too, need to be considered separately. Since they cannot give informed consent to a voluntary vaccination themselves, they might have to be protected from their parents (who might be unwilling to get them vaccinated) in case of particularly serious diseases (see [ 13 , 14 ]).
There is, in summary, hope that the public goods problem may be overcome, as social and behavioral science offers a wide array of potential policy options to influence people’s perceptions and reactions to the pandemic (for an extensive up-to-date overview, see [ 15 ]). It is not clear, however, how the research on well-established vaccines carries over to the current pandemic, and recent developments seem to indicate that the willingness to get vaccinated against the novel coronavirus is currently rather low. We therefore chose to investigate two fundamental questions at the opposite extremes of the spectrum of policy options: would a sufficient number of people voluntarily undergo vaccination to achieve herd immunity? Or would a mandatory vaccination against COVID-19 be acceptable to achieve herd immunity?
A legal duty to be vaccinated against COVID-19 could be an alternative to other coercive measures if one assumes that a high-risk, unregulated, laissez faire approach is not a realistic policy option: it seems irresponsible to lift all restrictions because the virus would soon spread through the entire population. Coercive measures of some kind therefore seem inevitable. Mandatory vaccination could be preferable to other coercive measures, provided the interference with bodily integrity would be considered less socially costly in the long run than the effects of prolonged lockdowns. Emotions run high where vaccination policies are concerned, but because mandatory vaccination might become a realistic scenario, it is worth investigating what the general population thinks about such a policy.
It is important to emphasize that a legal duty to vaccinate against COVID-19 would not imply a legal (or even moral) duty to vaccinate against other diseases. The novel coronavirus is a special case in many respects: In contrast to influenza, for example, the population does not have a background immunity from past infections. In addition, many infected people do not show symptoms (a recent meta-study estimates this to be one in six infected [ 16 ]) and, hence, cannot protect others from being infected through voluntary self-quarantining. Thus, people with COVID-19 represent a much higher risk of infection for others than, for example, people who come down with influenza, assuming that these would normally stay at home. Therefore, a vaccination against COVID-19 is much more important from the social perspective than e.g. a vaccination against influenza: not for self-protection, but to protect other people from unintentional infection. Although classic liberal positions (cf. [ 17 ]) would reject a paternalist legal obligation to protect oneself through vaccination, they plausibly would favor a policy of mandatory vaccination in the case of COVID-19 to protect others from being harmed. In modern philosophical discussions, even some libertarians are in favor of mandatory vaccination against serious diseases for similar reasons (see [ 18 ] and for an overview [ 19 ]).
Though there are philosophical reasons supporting a policy of mandatory vaccination, we want to emphasize that we are not advocating it as a concrete policy option for Germany at this moment. Our aim is to understand whether the general public would consider such a policy acceptable, or which sections of the population, and why. To this end, we study the willingness to get vaccinated and the acceptance of a policy of mandatory vaccination against COVID-19 in June and July 2020 in Germany. We use unique real time survey data from a sub-sample (SOEP-CoV) of the German Socio-Economic Panel (SOEP, see [ 20 ]). A set of questions about vaccination was part of the later stages of SOEP-CoV, an ongoing research project initiated in April 2020. This so-called ‘vaccination module’ included questions on the willingness to get vaccinated voluntarily and the acceptance of a policy of mandatory vaccination against COVID-19. In addition, individuals could indicate reasons for their preference regarding the second question. Using the rich data of the SOEP, pre-pandemic income, education, household context, personality, political preferences etc., which can be directly linked with SOEP-CoV, we are able to provide a detailed picture on who intends to get vaccinated and who does not.
The most important result of our study is that about 70 percent of adults in Germany would get vaccinated voluntarily against COVID-19 if a vaccine without significant side effects was available. Further, about half of adults in Germany are in favor, and half against, a policy of mandatory vaccination against COVID-19. The approval rate for mandatory vaccination is significantly higher among those who would get vaccinated voluntarily (around 60 percent) than among those who would not get vaccinated voluntarily (27 percent). However, 22 percent of the individuals would disapprove of both a voluntary and a mandatory vaccination and 8 percent can be characterized as ‘passengers’ (they are not willing to get vaccinated but do support a policy of mandatory vaccination, but they might not all be ‘free-riders’ in the standard sense). In this group, surprisingly, 86 percent state that, without a mandatory vaccination, too few individuals would get vaccinated and about 87 percent indicate that most people underestimate how dangerous COVID-19 is. In general, the willingness to get vaccinated is significantly lower for female, younger, and less educated respondents as well as those with lower income. A policy of mandatory vaccination is rejected with higher probability by women and favored by older people and those living in the eastern federal states.
Data, measures, and methods
Data: soep and soep-cov.
The German Socio-economic Panel (SOEP) is among the largest and longest-running representative panel surveys worldwide and is recognized for maintaining the highest standards of data quality and research ethics [ 20 ]. In 2020, the survey covers about 30,000 adults in 20,000 households. Since the same individuals and households participate in the study every year, life courses of the respondents can be tracked and intertemporal analyses can be carried out at the individual and at the household level. The data contain information on the respondents’ household situation, education, labor market outcomes, and health, among others (see [ 20 , 21 ]).
To better understand the effects of the corona pandemic, a special survey called SOEP-CoV was conducted within the framework of the SOEP, which consisted of a random sample of about 6,700 SOEP respondents, (see [ 21 , 22 ]). SOEP-CoV was surveyed in nine staggered tranches from early April to the end of July 2020 and collected data on the following topics: a) Prevalence, health behavior, and health inequality; b) Labor market and gainful employment; c) Social life, networks, and mobility; d) Mental health and well-being; and e) Social cohesion. Over time, some new question modules were introduced within these five thematic complexes. These included the ‘vaccination module’ (see questionnaires available under www.soep-cov.de/Methodik/ ).
Measures: Preferences toward vaccination against COVID-19
The ‘vaccination module’ went into the field with tranches 7 to 9, in June and July 2020, and covered a total of 851 persons aged 19 years and older. At that moment, major research efforts were being undertaken, but it was not clear whether any vaccine would actually be found. The module hence starts with a question on the hypothetical willingness to get vaccinated against COVID-19:
- “Let us assume that a vaccine against the novel coronavirus that is shown to have no significant side effects is found. Would you get vaccinated?” The response categories are ’Yes’, ’No’, and ‘no answer’. The module contains a further question about mandatory vaccination with the same response categories:
- “Would you be in favor of a policy of mandatory vaccination against the coronavirus?” In addition, the interviewees were asked about their reasons for or against a policy of mandatory vaccination. For this purpose, a filter was used to adapt the arguments according to the respondents’ answers to question (B). The arguments given were as follows:
Argument 1: Others’ willingness to get vaccinated without mandatory vaccination
- Against mandatory vaccination: “Enough people would get vaccinated even without a policy of mandatory vaccination.”
- In favor of mandatory vaccination: “Only with a policy of mandatory vaccination would enough people get vaccinated.”
Argument 2: Misperception of risks
- Against mandatory vaccination: “Most people overestimate the dangerousness of the virus.”
- In favor of mandatory vaccination: “Most people underestimate the dangerousness of the virus.”
Argument 3: Legitimacy of a policy of mandatory vaccinations in general
- Against mandatory vaccination: “A policy of mandatory vaccination is never permissible, even in the case of very dangerous diseases.”
- In favor of mandatory vaccination: “A policy of mandatory vaccinations would make sense also for less dangerous diseases.”
Argument 4: Other reasons (without listing these reasons explicitly)
The first three arguments are of particular relevance for political decision-making. Although there is quite a lot of research on the reasons people have not to get vaccinated themselves, there is much less research on what people think about policies of mandatory vaccinations, and up to present–at least to our knowledge–none on the application to the special case of the novel coronavirus. As the reasons for the individual decision need not carry over to the policy assessment, and given the previously discussed particularities of the coronavirus, we focused on factors that are both of theoretical importance and under discussion in the general public. It would be interesting, for instance, if many people did not have the intention to get vaccinated themselves, yet believed that enough other people would get vaccinated so that mandatory vaccination would not be required. Similarly, it would be surprising if people wanted to get vaccinated yet believed that others overestimated the dangerousness of the virus. Finally, we wanted to see whether people considered mandatory vaccinations potentially legitimate at all.
Sample selection, weighting, and item non-response
Since SOEP-CoV is a random sample from the SOEP population, the SOEP-CoV data 2020 can be linked with the regular SOEP data of previous years. Thus, attitudes toward vaccination against COVID-19 that were collected during the pandemic can be linked to the characteristics of the respondents before the outbreak of the pandemic (e.g., income or educational level). Since these characteristics were collected before the pandemic, they can be considered unaffected by the pandemic event and, hence, exogenous ( S1 File provides definitions of all dependent and independent variables used in the empirical analyses).
The response rate in the vaccination module was high. Altogether, only 4.58 percent of the 851 respondents did not answer the question about voluntary vaccination and 3.41 percent did not answer the question about mandatory vaccination. Of those who supported (objected to) mandatory vaccination, 0.26 (1.82) percent did not provide at least one motive in the follow-up question. Hence, bias from item non-response should be small and we did not correct for it. As the focal variables are coded dichotomously (yes = 1; no = 0), there was no need to remove outliers in them from the database.
To derive population-wide estimates, the SOEP-CoV data is equipped with frequency weights. The weighting of SOEP-CoV follows the standard weighting used in SOEP [ 23 , 24 ]. Based on the SOEP household weights, weights for all persons in the participating households were generated via a marginal adjustment step and corrected for selection effects. Furthermore, the data were corrected for the fact that some SOEP subsamples were excluded from the SOEP-CoV study from the outset. To address potential selection effects and adjust frequency weights accordingly, we followed the two-step procedure recommended in [ 25 ]:
- Step 1: Estimation of a logistic regression model where the dependent variable is a dummy variable indicating whether respondents belong to the working sample of tranches 7 to 9 (dummy is equal to one) or not (dummy is zero). All variables included in the following analyses serve as explanatory variables.
- Step 2: If at least one analysis variable shows a significant (i.e., p -value below 0.05) and at the same time meaningful effect (i.e., coefficient above 0.01) with respect to the assignment to the analysis population, a correction of the SOEP-CoV weights is performed by multiplying the frequency weights by the inverse estimated probability. In other words, multiplying the SOEP-CoV weights belonging to the analysis set by the inverse predicted probability yields the sought adjusted weight that can be used to calculate population statistics. In the present case, an adjustment using the following variables is indicated: Extraversion and whether respondents live in a household in which at least one household member was tested for COVID-19. Overall, selection on observables is very minor. Unless otherwise stated, our results are weighted with the adjusted probability weights.
Statistical framework
Since the vaccination questions are answered once by each respondent, our empirical strategy is between-person. Uni- and bivariate results for our focal variable, attitudes toward vaccination, are presented as weighted means or percentages. Assessments of differences in attitudes or characteristics between-groups rely on two-tailed t-tests, with statistical significance evaluated at p <0.01, p <0.05, and p <0.10 using the survey weights explained above. Our empirical strategy involves multiple between-group tests. This raises the question of whether a correction is necessary for multiple hypotheses testing. We do not implement such a correction because we seek to compare a certain attitude or characteristic between groups and not to draw, at the end of the test series, a concluding summary of all tests results.
Willingness to get vaccinated and attitudes toward a policy of mandatory vaccination
For the questions on voluntary vaccination (A) and mandatory vaccination (B), four groups in the population may be distinguished:
- Anti-vaccination: interviewees who would not get vaccinated voluntarily against the coronavirus and who also oppose a policy of mandatory vaccination.
- Anti-duty: interviewees who would get vaccinated voluntarily but oppose a policy of mandatory vaccination.
- Passengers: interviewees who would not get vaccinated voluntarily but are in favor of mandatory vaccination. We refer to this group as ‘passengers’ because they apparently want to see the public good of herd immunity provided by mandatory vaccination, yet would not voluntarily contribute to this good. Some of these passengers might be free-riders in the standard sense, trying to benefit from the decisions of others while not voluntarily contributing themselves, while others might not be able to get vaccinated for medical reasons. If mandatory vaccination were introduced, the first group, but not the second, would also get vaccinated, of course. Neither group would actually free-ride, but the first might initially have wanted to.
- Pro-vaccination: interviewees who would get vaccinated voluntarily and are also in favor of mandatory vaccination.
Overall, 70 percent of adults in Germany would voluntarily get vaccinated against the coronavirus, provided a vaccine without significant side effects was available ( Table 1 : groups 2 and 4). This value corresponds exactly to the results of [ 26 ]. From May till September 2020, the COVID-19 snapshot monitoring (COSMO) at the University of Erfurt showed relatively constant values of between 60 and 66 percent; it was only in April that it showed an exceptionally high value of 79 percent, and it has now decreased further (cf. [ 27 ], p. 76; an overview of previous studies on the willingness to get vaccinated in Germany is provided in S2 File .). Overall, these studies paint a consistent picture, with a slight decline in the willingness in the second half of 2020.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0248372.t001
Approximately half of the interviewees are against, and half are in favor of, a policy of mandatory vaccination (against: 51%, groups 1 and 2, in favor: 49%, groups 3 and 4). These values, too, coincide almost exactly with those of the COSMO monitoring since May 2020 (cf. [ 27 ], p. 78), which in April showed an approval rate for mandatory vaccination of 73 percent, but later discontinued this question (till July 2020, and it has been decreasing since; see S2 File ). The agreement with a policy of mandatory vaccination is clearly higher, namely almost 60 percent (41/(41+29) = 0.59) among those who would get vaccinated voluntarily than with those who would not let themselves be vaccinated voluntarily, i.e. approximately 27 percent (8/(8+22) = 0.27).
Attitudes toward a policy of mandatory vaccination
The four groups differ noticeably in how they assess the arguments presented to them. This is shown in Table 2 , which gives the group-specific approval rate for each argument in combination with the p-values of t-tests in S3.1 Table in S3 File .
https://doi.org/10.1371/journal.pone.0248372.t002
Argument 1.
The groups differ markedly in how likely they think it is that others will get vaccinated. Among the two groups that are against a policy of mandatory vaccination, 56 percent of the ‘anti-vaccination’ group (who would not get vaccinated voluntarily) think that their fellow citizens would get vaccinated sufficiently frequently such that mandatory vaccinations would not be necessary. Almost 80 percent of the ‘anti-duty’ group (the members of which would get vaccinated voluntarily) think the same. Among the two groups that are in favor of mandatory vaccination, 85 percent of the ‘passengers’ (who would not voluntarily get vaccinated) think that the others would not voluntarily get vaccinated either, as do slightly more than 90 percent of the ‘pro-vaccination’ group (who would also get vaccinated voluntarily).
Argument 2.
These results run in parallel with the assessment of the dangerousness of the virus. Even though the analysis is not causal, we can see that about 50 percent of the ‘anti-vaccination’ group and 30 percent of the ‘anti-duty’ group think that most people overestimate the dangerousness of SARS-CoV-2. Exactly the opposite, that most people underestimate the dangerousness, is believed by nearly 90 percent of the ‘passenger’ group and by slightly more than 80 percent of the ‘pro-vaccination’ group. Summarizing the numbers differently, one could say that groups 2 and 4, who would voluntarily get vaccinated, probably have similar opinions about whether their fellow citizens correctly assess the danger posed by the virus. About 80 percent of the members of the ‘pro-vaccination’ group think that most people underestimate the danger. Of the members of the ‘anti-duty’ group, we only know with certainty that 30 percent of them believe that most people overestimate the danger–we do not know, however, how the remaining 70 percent are divided between ’underestimate’ and ’correctly estimate’. The difference between the corresponding values for groups 1 and 3 is significantly higher.
Looking at arguments 1 and 2, we may conclude that there is a high level of disagreement among the population about the dangerousness of the virus. This disagreement probably explains why people have such different attitudes toward getting vaccinated and toward the necessity (or not) of a policy of mandatory vaccination.
The position of the group of the ‘passengers’ is hard to understand. On the one hand, they favor a policy of mandatory vaccination, presumably because, as they do believe, the dangerousness of the virus is often underestimated. On the other hand, they probably assume that they themselves do not underestimate that dangerousness, but nevertheless would not get vaccinated voluntarily. One reason for this could be their medical condition: they might be willing but unable to get vaccinated for medical reasons. If so, they would not be trying to free-ride. It is unclear, however, how much weight the appeal to such a hypothetical medical contraindication should have, given that at the time of the interviews, no vaccine was even available. Some, but not all, of the ‘passengers’ are probably free-riders in the standard sense.
Argument 3.
Approximately 40 percent of both the ‘anti-vaccination’ group and the ‘anti-duty’ group agree with the statement that a mandatory vaccination is never permissible, not even with very dangerous diseases. Since these two groups reject mandatory vaccination against COVID-19, this means that for the remaining 60 percent of the group, mandatory vaccination may well be permissible–but apparently only for diseases that they would have to consider as even more dangerous than COVID-19. Conversely, well over 60 percent of the ‘passenger’ group and just over 70 percent of the ‘pro-vaccination’ group agree with the statement that a policy of mandatory vaccination would also make sense for less dangerous diseases. In combination with the results for argument 2, these two groups could therefore believe that their fellow citizens also underestimate the danger of such other diseases. It is interesting to note that, overall, people in Germany estimate the probability that the novel coronavirus will cause a life-threatening disease within the next twelve months to be high (cf. [ 20 ]). This probability is around 25 percent across our four groups. In group 1 it is 20 percent, in group 2 around 27 percent, in group 3 it is 30 percent and in group 4 it is 25 percent (see Table 3 ).
https://doi.org/10.1371/journal.pone.0248372.t003
Other reasons (which were not further broken down in the questionnaire for capacity reasons) are important primarily among those respondents who would not themselves get vaccinated and also oppose mandatory vaccination. Although questions (A) and (B) explicitly assume that a vaccine would not have any significant side effects, this could be due to a deeper skepticism about vaccination, which we hope to be able to explore in future research (on ’vaccine denialism’ see [ 28 ]).
Characteristics of the ‘anti-vaccination’, ‘anti-duty’, ‘passenger’, and ‘pro-vaccination’ groups
Description of the individual characteristics of the groups..
We would like to know in more detail who is in favor of a policy of mandatory vaccination against COVID-19 and who is opposing it, as well as what the socio-economic characteristics of those who would get vaccinated and of those who would not are. Table 3 shows how the four groups defined above differ across various socio-demographic characteristics (measured before the pandemic), personality (measured before the pandemic), health (before and during the pandemic), and political orientation (measured before the pandemic). Statistical t-tests for the significance of differences in characteristics between groups are shown in S3.2 Table in S3 File assuming equal variances across groups. S3.3 Table in S3 File provides supporting evidence: tests for equality of variance across groups provides support for this assumption in about 90% of the cases, and as S3.4 Table in S3 File . shows, relaxing the equality of variances assumption does not change our conclusions.
Socio-demographic characteristics . Almost 60 percent of the ‘anti-vaccination’ group are female, they are on average 48 years old, 12 percent of them have a university degree and their monthly net household income in 2019 averaged just under EUR 2,800. Around 27 percent have children under 16 and around 17 percent live in the eastern German states. ‘Passengers’ do not differ in their characteristics statistically significantly from this group. The members of the ‘anti-duty’ group, by contrast, are much more likely to be male and more often have a university degree. In comparison to the ‘anti-vaccination’ group, the members of the ‘pro-vaccination’ group are also more often male and older, and are also more likely to have a university degree. In particular, older interviewees are more likely to be in groups that favor mandatory vaccination and persons with a university education in groups comprising those who would get vaccinated voluntarily.
Personality traits . SOEP collects the personality traits of the respondents using a battery of questions that measure the five dimensions of the so-called ’Big Five’ [ 29 ]. The Big Five are the five most important groups of character traits in personality research: ’openness’, ’conscientiousness’, ’extraversion (sociability)’, ’tolerance’, and ’neuroticism’. Furthermore, risk attitude is surveyed. We see that members of the ‘anti-vaccination’ group tend to be more sociable but less open than the other groups. Their willingness to take risks is similar to that of the members of the ‘anti-duty’ and of the ‘pro-vaccination’ groups, but is significantly higher than that of ‘passengers’. Members of the ‘anti-duty’ group are particularly unsociable compared to the other groups, but open to new experiences. The ‘passengers’ are, like the members of the ‘pro-vaccination’ group, less neurotic. They are particularly tolerable and the least willing to take risks of the four groups.
Health . As far as the health of those surveyed is concerned, statistically significant differences are only evident in the number of illnesses: Members of the ‘anti-vaccination’ group have significantly fewer risk diseases than ‘passengers’ and members of the ‘pro-vaccination’ group. ‘Anti-duty’ members, on the other hand, have significantly fewer diseases than the ‘passengers’. Thus, overall, it may be said that those who refuse a policy of mandatory vaccination have fewer risk diseases at the time of the survey. There are no differences between the groups in terms of whether a member of the respondent’s household has already undergone a test for an infection with corona. It should be noted, however, that the number of cases of those tested for an infection is comparatively small.
Political orientation . As far as the political orientation of the respondents is concerned, no systematic significant differences between the four groups are identified. Only the members of the ‘anti-vaccination’ group seem to be positioned somewhat more to the right in the party spectrum than the members of the ‘anti-duty’ group.
Multivariate description of the characteristics of the four groups.
The differences and similarities with regard to group composition described above always refer to a single characteristic, i.e. they are univariate. Additionally, the relationships between individual characteristics of the respondents–after taking other characteristics into account–and their attitude toward mandatory or voluntary vaccination are explained below using a multivariate model (logistic estimation; see Eq ( 1 )). The dependent variable is either an indicator that describes the respondent’s own willingness to get vaccinated voluntarily (value 1 = yes; 0 = no; Table 4 ) or an indicator (value 1 = yes; 0 = no) that describes whether the respondents favors a policy of mandatory vaccination ( Table 5 ). As our interest is the explanation of data structures, we do not use survey weights in the multivariate analysis.
https://doi.org/10.1371/journal.pone.0248372.t004
https://doi.org/10.1371/journal.pone.0248372.t005
With regard to the willingness to voluntarily get vaccinated ( Table 4 ), some significant differences in socio-demographic characteristics are observed. If all other characteristics are kept constant, the willingness to vaccinate is about 10 percentage points lower in women than in men. It is positively associated with age (0.4 percentage points per year of life), education (13 percentage points if respondents have a university degree compared to the other education categories), and household income (2.5 percentage points per 1,000 euros). The personality traits of the Big Five do not correlate with the respondents’ willingness to vaccinate; only openness is slightly positively associated with the willingness to vaccinate. In the health block, there is also only one significant variable that correlates with the willingness to get vaccinated: The higher the respondents estimate the probability that the virus could trigger a life-threatening disease in them, the more willing they are to be vaccinated.
A policy of mandatory vaccination ( Table 5 ) is also rejected with higher probability by women, but favored by older people and those living in the eastern federal states, ceteris paribus . Approval is negatively associated with neuroticism, i.e. emotional instability, and positively associated with the subjective probability of contracting life-threatening COVID-19.
The tables presenting the logit estimations include an initial model diagnostic: the Pseudo- R 2 . In S4 File , we present two additional model diagnostics: First, the linktest for both logit models does not find any evidence for model misspecifications. Second, a receiver operator characteristic (ROC) analysis provides evidence that the predictive power of our two models is acceptable. In addition, to assess multicollinearity, we have computed variance inflation factors (VIF) in S5 File . As a rule of thumb, a variable whose VIF values exceeds 10 may merit further investigation. In both regressions, the VIF of none of the explanatory variable exceeds 7.7 and the average VIF over all variables is below 2.1. It should also be noted that the two separate logit models do not model correlation and heteroscedasticity between the two outcomes (vaccinate voluntarily or obligatorily). Hence, in S6 File , as a robustness check, we have estimated a multivariate probit model using Stata’s mvprobit command that relies on simulated maximum likelihood [ 30 ]. S6.1-S6.6 Tables in S6 File compare the coefficients of the multivariate probit with the two separate models. Overall, there are some changes in the magnitude of the coefficients, but no changes in the signs of the regression coefficients or significance levels.
It is possible that respondents who did not give an answer about their vaccination preferences–for example, because they are still undecided–would decide to vaccinate or support mandatory vaccination after an adequate vaccination campaign. In a robustness check, we followed this argument by assigning respondents who refused to answer the question about voluntary or mandatory vaccination to the ‘yes’ category and repeated the logit estimation. This does not change our results (see S7.1 and S7.2 Tables in S7 File , S8 File provides our Stata code, which prepares the data and conducts all the statistical analyses, as well as the outputs of the multivariate estimations).
Finally, Table 6 provides a statistical comparison of the marginal effects from the model on willingness to get vaccinated ( Table 4 ) and attitudes toward mandatory vaccinations ( Table 5 ). We find no significant differences in marginal effects between the two models except for two variables: tertiary education and eastern federal states. The marginal effect for tertiary education is significantly larger for the willingness to get vaccinated model while the opposite is true for eastern federal states.
https://doi.org/10.1371/journal.pone.0248372.t006
Politicians must make decisions which are based on incomplete information yet have far-reaching consequences for public health, personal freedom, and economic prosperity. It seems that many citizens are prepared to behave responsibly in the sense that they are prepared to endure a ‘little sting’ for the good of all: a vast majority of the German population (70 percent) state that they would get vaccinated as soon as a vaccine against COVID-19 was available. This means that under favorable conditions, a legal duty to get vaccinated to achieve herd immunity might not be necessary. It should, however, be noted that the question was asked in a stylized context: Potential side effects or ineffectiveness of the then hypothetical vaccine were assumed away. Though there is no reason to believe the vaccines currently being administered are more problematic in this respect than any other vaccines in use, neither can strictly be guaranteed in reality. In addition, the time required for a vaccination, the process of the vaccination itself (i.e. the injection), bureaucratic administration (e.g. making an appointment with the family doctor) or any necessary co-payment should de facto reduce the willingness to get vaccinated. Furthermore, at the time of writing, not only is it still unclear how quickly a vaccine can even be produced in the quantity required and administered to enough people, it is also unclear how long its effect will last. It is not even clear what percentage of the population would have to be vaccinated to achieve herd immunity, as this also depends on individual behavior and legal (or ethical) norms which are likely to continue to change (e.g. an explicit or implicit obligation to wear a mask of a specific variety in public transport or a testing obligation for people returning from trips abroad) [ 31 , 32 ]. Hence, a sufficiently high willingness to get vaccinated in the ‘best case’ scenario investigated here is an idealization and in any case only one relevant factor among many.
We observed there to be gender differences in the willingness to get vaccinated: women are less willing to get vaccinated, and also less willing to support a policy of mandatory vaccination. This is surprising, given that men are generally less likely to engage in preventive behavior [ 33 ] and women have been shown to be more willing to engage in preventive behavior in the pandemic, for instance by wearing face masks when recommended [ 34 ], and they also seem to be more compliant with other measures in general [ 35 ]. However, men are also more severely affected by the coronavirus [ 36 ] and women generally more skeptical about vaccinations, especially against COVID-19 [ 37 ]. We don’t know whether our interviewees frame their decision to get vaccinated or not as a situation of a social dilemma, but if so, previous results on gender differences in cooperation suggest men and women might have to be addressed differently to influence their decisions [ 38 , 39 ]. We also observed that income and education increase the willingness to get vaccinated voluntarily. It has also been shown recently that the willingness to pay for a vaccine against Covid-19 is positively impacted by, among other variables, income [ 40 ].
A mandatory vaccination would almost certainly achieve herd immunity against COVID-19, since all those for whom there is no medical contraindication would also get vaccinated. About half of the respondents approve and disapprove, respectively, of such a mandatory vaccination policy. In this context, the strong disagreement among the participants of the study regarding the dangerousness of the virus is particularly striking. Many of those who reject a policy of mandatory vaccination assume the dangerousness of the virus is being overestimated by others, while those who approve of a policy of mandatory vaccination seem to believe the exact opposite. This is highly problematic: at most one of the two groups can be right. Plausibly, the interviewees themselves differ in how dangerous they think the virus is. This yields a concrete and important policy recommendation (see also [ 40 , 41 ]): we need more reliable data on the dangerousness of SARS-CoV-2 and to communicate this data more clearly to the general public. Though the ‘knowledge-deficit’ explanation of low vaccine uptake might not work for well-established vaccines [ 42 ], we have found evidence that this might be different for COVID-19.
We are not recommending a policy of mandatory vaccination in this paper, but merely investigating the attitudes of people towards it. A policy of mandatory vaccination would be an extreme solution to solve the potential problem of low vaccine uptake, and a lot may be said in favor of less extreme policies (as outlined in [ 15 ], for instance). Vaccination could also be made mandatory only for certain groups of people (e.g. nurses, physicians, physiotherapists, people working in confined spaces, people travelling on public transport etc.), or only after time has conclusively shown that not enough people actually get vaccinated. It might also turn out that people are unwilling to take the second dose of a two-dose vaccine, or not accept refresher doses, which would further complicate the situation and might require subtle intertemporal strategy choice. Before making any vaccination mandatory, people could also be paid or incentivized in other ways to accept it [ 43 ]. If, as we hope, people take the external effects of their action into account, and a sufficiently high number of people get vaccinated as a result, mandatory vaccination won’t be necessary.
This article investigates the willingness to get vaccinated and the acceptance of a policy of mandatory vaccination against COVID-19 in June and July 2020 in Germany. Our first main result is that a large majority of about 70 percent of adults in Germany would voluntarily get vaccinated against the novel coronavirus if a vaccine without side effects was available. Our second result is that about half of this population is in favor of, and half against, a policy of mandatory vaccination. Our third main result is that the individual willingness to get vaccinated and acceptance of a policy of mandatory vaccination correlates systematically with several socio-demographics (gender, age, education, income) but, overall, not with psychological characteristics of the respondents.
When interpreting the results from our survey, it should be noted that preferences were elicited in an ideal-typical situation: a vaccine which is effective and free of side effects is immediately available for the entire population at zero cost. Future research will have to show how actual vaccination behavior differs in real-life situations that deviate from this ideal-typical situation.
Supporting information
S1 file. variable definitions..
https://doi.org/10.1371/journal.pone.0248372.s001
S2 File. Comparison with further studies in Germany.
https://doi.org/10.1371/journal.pone.0248372.s002
S3 File. Complementary estimation results.
https://doi.org/10.1371/journal.pone.0248372.s003
S4 File. Additional diagnostics for the logit models.
https://doi.org/10.1371/journal.pone.0248372.s004
S5 File. Multicollinearity across explanatory variables.
https://doi.org/10.1371/journal.pone.0248372.s005
S6 File. Functional form assumptions and simultaneity.
https://doi.org/10.1371/journal.pone.0248372.s006
S7 File. Imputation.
https://doi.org/10.1371/journal.pone.0248372.s007
S8 File. Stata code.
https://doi.org/10.1371/journal.pone.0248372.s008
Acknowledgments
We thank Thomas Rieger for his outstanding research assistance.
- 1. WHO. Draft Landscape of COVID-19 candidate vaccines. 2020. Available from: https://www.who.int/publications/m/item/draft-landscape-of-COVID-19-candidate-vaccines (accessed: March 2, 2021).
- View Article
- Google Scholar
- 5. Stiglitz JE. Economics of the public sector. 2nd edn. W.W. Norton & Co.: New York. 1988.
- PubMed/NCBI
- 17. Mill JS. On Liberty. In: Collected Works of John Stuart Mill , ed. Robson J.M. Toronto: University of Toronto Press, London: Routledge and Kegan Paul, 1963–1991). 1859; 33. https://oll.libertyfund.org/titles/165 .
- 19. Giubilini A. The Ethics of Vaccination. Palgrave Studies in Ethics and Public Policy. Open Access. 2019. https://link.springer.com/book/10.1007%2F978-3-030-02068-2 .
- 21. Schröder C, Goebel J, Grabka MM, Graeber D, Kröger H, Kroh M, et al. Vor dem COVID-19-Virus sind nicht alle Erwerbstätigen gleich. DIW aktuell. 2020; 41.
- 23. Siegers R, Belcheva V, Silbermann T. SOEP-Core v35 Documentation of Sample Sizes and Panel Attrition in the German Socio-Economic Panel (SOEP) (1984 until 2018). SOEP Survey Papers. 2020; 826.
- 24. Kroh M, Siegers R, Kühne S. Gewichtung und Integration von Auffrischungsstichproben am Beispiel des Sozio-oekonomischen Panels (SOEP), in Nonresponse Bias: Qualitätssicherung Sozialwissenschaftlicher Umfragen. Eds.: Schupp J. und Wolf . Wiesbaden: Springer Fachmedien Wiesbaden. 2015; C: 409–44.
- 25. Siegers S, Steinhauer HW, Zinn S. Gewichtung der SOEP-CoV-Studie 2020, SOEP Survey Papers, Series C–Data Documentation. 2020; 888.
- 28. Navin M. Values and Vaccine Refusal: Hard Questions in Epistemology, Ethics and Health Care, New York: Routledge. 2016.
MANDATORY VACCINATION: WHY WE STILL GOT TO GET FOLKS TO TAKE THEIR SHOTS
Ben Balding
Class of 2006
April 27, 2006
This paper is submitted in satisfaction of the Food and Drug Law course paper and the Harvard Law School 3L Written Work Requirement
Vaccination is widely considered one of the greatest medical achievements of modern civilization. Childhood diseases that were commonplace less than a generation ago are now increasingly rare because of vaccines. In order to be effective at eliminating communicable diseases, vaccines must be administered to sufficient levels of persons in the community. Because of this, public health officials have mandated vaccination for certain diseases as a condition to school attendance. The overwhelming effectiveness of vaccination programs may lead individuals to ignore the benefits of vaccination and focus more on the risk of side effects. Moreover, some have criticized the coercive nature of these programs. These objections may lead to an unacceptably high number of exemptions, which can compromise vaccination programs and leave the population susceptible to outbreaks.
This paper explores vaccination programs with an eye toward greater public safety without ignoring the reality of a small but committed group of vaccine critics. The paper begins with a discussion of the historical development of mandatory vaccination policies and the issues posed by exemptions. It then addresses some of these issues in the context of vaccine safety. It also seeks solution by framing the discussion in economic terms. It concludes by recommending stricter enforcement of mandatory requirements for most vaccines and greater dissemination of information on the continued importance of vaccination.
TABLE OF CONTENTS
Introduction.
Vaccination is widely considered one of the greatest medical achievements of modern civilization. Childhood diseases that were commonplace less than a generation ago are now increasingly rare because of vaccines. The smallpox vaccine has eradicated a disease that was responsible for centuries of outbreaks and had a 30% fatality rate. [1] Physical handicaps resulting from polio can still be observed on some of those who were children before Jonas Salk developed a vaccine in 1955. Formerly common childhood diseases are now rarely observed. Even ear infections may soon be prevented by vaccination. [2] The widespread success of vaccinations has led one medical report to comment that “[n]ext to clean water, no single intervention has had so profound an effect on reducing mortality from childhood diseases as has the widespread introduction of vaccines.” [3]
The story of modern vaccination begins with Edward Jenner’s development of the vaccine for smallpox, one of the most feared diseases in recent history. At first, vaccination was optional and not everyone chose to vaccinate. [4] In time, states would allow municipalities to mandate vaccination in time of outbreak in order to protect the public from epidemics. [5] A further step was taken when states imposed smallpox vaccination as a prerequisite for attending public schools. [6] These requirements were amended in time as new vaccines were developed. [7] At some point actual outbreaks and epidemics ceased to be the trigger for mandatory vaccination, and prevention became the overriding justification. [8] Most states today require vaccination for a multitude of childhood diseases, including measles, diphtheria, pertussis, polio, and now even chickenpox. [9]
Because of the success and the mandatory nature of vaccination, most people would probably not consider vaccination an optional method of medical treatment. For most parents, the “decision” to vaccinate is equivalent to the “decision” to feed one’s child. [10] Typically, a doctor informs parents of the school vaccination schedule and the parents consent to having their child vaccinated. Since the vaccination schedule usually corresponds to the scheduled doctor visits for infants, full compliance with mandatory vaccination schedules is typically not a problem and can usually be substantially accomplished by age two. [11]
For some parents, however, vaccination is no routine matter. [12] From the time of Jenner’s smallpox vaccine, vaccination has had its critics. [13] In the two centuries since that time, many different types of objections have been raised. Some have questioned the scientific qualifications of mass immunization. [14] Others have focused on the personal liberty interests at stake and have objected to the paternalistic nature of government imposition of what is viewed as a personal medical choice. [15] Still others have opposed vaccination for personal or religious reasons. [16]
Today, some parents raise similar objections. The idea that a potentially harmful substance is being placed directly into the bloodstream raises a red flag for some. Additionally, the decline of many diseases for which vaccination is still mandated may make some parents skeptical of the continued wisdom of subjecting a child to a vaccine, even if the vaccine is considered extremely safe. This skepticism grows when some point to the correlation between vaccinations and conditions such as SIDS and autism. Whether or not such a correlation is scientifically significant, many parents simply wonder if it is wise to vaccinate against a disease unlikely to afflict their child if any chance exists that the vaccine will cause autism, SIDS, or any other side effect. [17]
Since the efficacy of a particular vaccine corresponds directly with the percentage of a given population that has been vaccinated, proponents of mandatory vaccination have sought to convince those with reservations about vaccines that vaccination is the right choice. The Center for Disease Control has attempted to allay possible reservations parents may have with vaccinations by rebutting some of the commonly held fears about vaccines. [18] The CDC has pointed out, for example, that most adverse effects from vaccines are “minor and temporary, such as a sore arm or mild fever.” [19] Because vaccination often involves the introduction of a harmful live (although seriously weakened) organism into the patient, vaccination can never be 100% safe. Serious side effects usually occur only between one per thousands to one per millions of doses, while some serious reactions and death occur so rarely that accurate risk assessment is difficult. [20] The CDC has also responded to many of the other concerns raised about the need for vaccination, and the FDA continually works to ensure vaccine safety and efficacy, but many still harbor reservations toward vaccination.
This paper will endeavor to discuss some of the most common objections to vaccination programs in general while trying to shed light on the veracity and tenability of these objections. Part I will discuss the nature of mandatory vaccination programs in this country; both scientific and historical issues will play a key part in this discussion. Part II will describe the role of the FDA and other governmental bodies in the overall vaccination picture. Part III will attempt to utilize multiple analytical tools in search of possible solutions to the dangers posed by those who may attempt to opt out of vaccination programs. It will first examine vaccination through the lens of an old television show episode. It will then adopt an economic analytical framework to discuss the balance between individual and general welfare in the context of vaccination. Part IV will conclude with some observations on how the goal of greater public health might be achieved without completely neglecting the concerns of many in the community regarding the prudence of using a medical technique that by definition relies on a degree of coercion.
I. MANDATORY VACCINATION
Historical background.
Jenner’s smallpox vaccine led to the research and development of vaccines for other widespread and epidemic diseases. The twentieth century saw the development of vaccines for such diseases as polio, diphtheria, tetanus, pertussis, measles, and others. [21] As with the smallpox vaccine, many of these vaccines soon found their way into vaccination programs mandated by the government, albeit through a somewhat different pathway.
Mandatory smallpox vaccination programs typically arose through state police power legislation authorizing municipalities to deal with outbreaks. [22] Typically, when a local municipality decided that the threat of outbreak was sufficient to exercise this authority it would require vaccination of everyone in the community (with a possible exception for individuals who could demonstrate uncommonly high health risks from receiving the vaccine, although this exception sometimes applied only to children) and fine and/or quarantine those who refused to be vaccinated. [23] When other diseases became preventable by vaccination, outbreak ceased to be the trigger for mandatory vaccination. Rather, because of their cost-efficiency and their ability to reduce and ultimately eliminate disease, vaccination programs became an important part of general public health policy. [24]
Most of the time, vaccination programs are accomplished through the dual efforts of national entities (which tend to develop and recommend vaccines) and state legislatures and local boards of health (which usually implement these recommended vaccines through vaccination programs). [25] It is not entirely accurate to refer to this as “mandatory vaccination,” as typically individual states will not criminally punish parents for not vaccinating their children or forcefully subject individuals to vaccination. [26] Instead, states typically condition school enrollment on proof of vaccination. [27] Though it may be a high price to pay, home schooling is usually an available means parents have if they wish to bypass these vaccination requirements. Moreover, most states grant exemptions to vaccination requirements for religious reasons and some even grant exemptions for philosophical reasons (in addition, every state exempts from school vaccination requirements individuals who cannot be vaccinated for medical reasons). [28]
The connection between school enrollment and vaccination programs may now seem obvious. Public health officials, faced with a means of protecting the general population from the harmful disease smallpox, realized that mass vaccination could lead to a sufficient level of immunity to eliminate the risk of outbreak, even for those in the community unable to vaccinate (because of medical reasons, for instance). [29] Because of the concept of herd immunity, public health officials considering the proper utilization of vaccines were dealing with a medical procedure quite out of the ordinary. Since vaccination itself does not typically provide 100% immunity to a disease, vaccinated individuals can still contract the disease. [30] Yet because of herd immunity, if a sufficient level of vaccination within a population is attained, the entire population will no longer be susceptible to the disease. In this way, vaccination came to be viewed not only as a personal medical choice but also as a step taken to improve the overall health of the population.
With the rise of public schooling in the mid- to late-nineteenth century, cities decided to condition public school attendance on smallpox vaccination. [31] By the latter part of the century, many states had adopted this practice. [32] Such a policy makes sense when one considers the increased risk of infectious disease in public areas like cities in general and schools in particular. By mandating vaccination for school attendance, of course, the state would eventually have ensured the vaccination of the entire population by the time the initially vaccinated generation became the oldest living one.
These vaccination schemes have faced challenges, both legal and social, throughout their existence. [33] The reasons for such challenges have ranged from personal liberty interests to doubts about the efficacy of vaccines. [34] State courts in the nineteenth century typically upheld both the enactment of mandatory vaccination programs and the delegation of power to local authorities. [35] More importantly for the future of mandatory vaccination policy, two important Supreme Court decisions in the early part of the twentieth century affirmed the power of state governments both to mandate vaccination and to delegate a broad degree of authority to local municipalities and health boards to carry out particular vaccination programs.
Judicial Approval
In 1905 the Court held in Jacobson v. Massachusetts [36] that the general police power of states is broad enough to overcome a Due Process claim brought by an individual who claimed his personal liberty interests were unconstitutionally invaded by the mandatory smallpox vaccination program in question. [37] In an opinion by Justice Harlan, the Court ruled that the constitutional guarantee of liberty “does not import an absolute right in each person, to be, at all times and in all circumstances wholly free from restraint.” [38]
This case still represents the initial constitutional basis of most mandatory vaccination legislation. Many states still provide for the governor or a public health official to mandate vaccination for all in the event of an outbreak. [39] Individuals who cannot vaccinate for health reasons or who refuse to vaccinate may be quarantined in order to protect the population in some states. [40] These laws gained greater relevance following the terrorist attacks of 9/11 and the increased public concerns regarding bioterrorism. For the most part, however, mandatory vaccination laws in the name of outbreak control have given way to vaccination requirements as a prerequisite for school attendance.
The issue of school vaccination came before the Court nearly two decades after Jacobson . In Zucht v. King [41] , the plaintiff challenged a general grant of authority from Texas to local boards of health to condition school entry on proof of vaccination. [42] To differentiate the case from Jacobson , the plaintiff noted that the San Antonio ordinances mandated vaccination even in the absence of evidence of outbreak. [43] The Court, speaking this time through Justice Brandeis, upheld the validity of the ordinances as well as the broad grant of authority to local health boards. [44] On the issue of the state’s power to mandate vaccination, he merely cited Jacobson : “[l]ong before this suit was instituted, Jacobson v. Massachusetts...had settled that it is within the police power of a state to provide for compulsory vaccination.” [45] As for entrusting a broad degree of authority on local health officials, he noted that Jacobson and other cases had affirmed that a state may “delegate to a municipality authority to determine under what conditions health regulations shall become operative.” [46] This delegation includes the permission to vest municipal officials with “broad discretion in matters affecting the application and enforcement of a health law.” [47] In summary, the Court found that these ordinances were valid assignments of “that broad discretion required for the protection of the public health.” [48] The language of the opinion emphasizes the importance of the public health as the key justification for mandatory vaccination.
Zucht , along with Jacobson , thus became the legal foundation for the mandatory vaccination laws of the twentieth century. Modern school vaccination laws and policies have grown from early mandatory smallpox vaccination laws:
The early successes of school vaccination laws against most political, legal, and social challenges helped lay the foundation for modern immunization statutes. Since the introduction of smallpox vaccination policies in the mid-to-late 1800s, states have amended them to include additional diseases as new vaccines become available. [49]
Though various amendments and additions have been made to mandatory vaccination laws throughout their history, the past half century has experienced the true culmination of mandatory vaccination policy. Public health officials have been able to institute a scheme for near-universal vaccination:
Many existing school vaccination laws were enacted in response to the transmission of measles in schools in the 1960s and 1970s. State legislatures at that time were influenced by the significantly lower incidence rates of measles among school children in states that strictly enforced vaccination requirements and school exclusions in outbreak situations without significant community opposition. Rather than having health departments require immunization in emergency conditions, legislatures acted to prevent disease by mandatory immunization as a condition of enrollment or attendance in schools or licensed day care facilities. [50]
Moreover, states have not been completely left to implement the recommended immunization schedule. [51] Though school requirements are still a state matter, national public health officials are typically able to enact their recommendations through federally funded immunization plans. [52] These plans require states to implement and enforce federally recommended immunization requirements before the states can receive federal funds. [53] The current recommended vaccination schedule appears below.
Recommended Childhood and Adolescent Immunization Schedule [54]
Challenges and concessions.
While school vaccination requirements have been credited with bringing about the control and elimination of many devastating childhood diseases, critics have continued to voice concerns and raise legal and political challenges to the entire process of mandatory vaccination.
Personal Liberty Concerns
One key argument against mandatory school vaccination has always focused on government intrusion into what is considered a personal medical choice. [55] Just as the government cannot force a person to have surgery to repair a torn ligament, for example, the government should not be able to force parents to vaccinate their children if the parents believe that vaccination is not the best medical decision. One prominent critic of mandatory vaccination has stated her organization’s goal as simply providing parents with choices: “[w]e believe that health care consumers should have the right to choose the type of preventive health care that they want to use – including choosing whether to use one, ten, or no vaccines.” [56] Other objections along similar bases argue that mandatory vaccination violates the medical ethic of informed consent or even that school district control over mandatory vaccination policies amounts to the unlawful practice of medicine without a license. [57]
The typical counterargument given by the public health officials is to point out that one’s decision to vaccinate, unlike one’s decision whether to undergo surgery, affects the health of others in the community. [58] To allow parents the right to choose not to vaccinate is to infringe on the ability of other parents to raise their children in a society free of certain deadly diseases. From a legal standpoint, Jacobson still seems to have settled the issue that at least under some circumstances, the government may force an individual to receive a vaccination.
Although public health officials have the legal authority to mandate vaccination for the public health under Jacobson, they should be very mindful of the personal liberty concerns just stated. Those with such views often cling to them vigorously. [59] As certain vaccine-preventable diseases decline, such concerns become even stronger. For this reason, it is important for public health officials to support their mandatory vaccination programs with justifiable arguments rather than simply citing legal precedent or historical tradition in support of their exercise of power. Fortunately for public health officials, the benefits provided by vaccination programs can be utilized to justify the existence of such programs.
Safety Accountability Concerns
A variation on the consumer choice challenge to mandatory school vaccination requirements tends to accuse the public health community of conspiring with or at least willfully acquiescing to powerful vaccine manufacturers at the expense of citizens. [60] Mandatory programs, the argument goes, eliminate any accountability from vaccine manufacturers that the free market might otherwise provide. [61] Both the safety and efficacy of vaccines fail to improve because manufacturers do not have to respond to consumer concerns. [62] Mandatory programs thus prevent better vaccines. A prominent critic of these programs has stated that if mandatory vaccination programs are ended, “we will have the ability to put economic pressure on the drug companies and on the health agencies to do a better job with vaccine safety and efficacy.” [63]
The strength of this argument lies in its apparent lack of hostility toward vaccines per se. Given the historical success of vaccination in eradicating smallpox and in reducing or eliminating the risk of other childhood diseases, any critique of mandatory vaccination programs that focuses on the use of vaccines generally is likely to be dismissed by those in the field of public health. By focusing on the economic drawbacks inherent in a mandatory vaccination program and how those drawbacks can negatively affect the quality of vaccines, this argument may gain more traction. Indeed, all sides of this debate claim to desire both safer and more effective vaccines.
The response to this argument, I would imagine, would be to emphasize the drawbacks of opening up the “market” in this case. Because vaccination programs depend on a sufficient percentage of the community being vaccinated, complete consumer choice carries with it problems that might be absent in a standard market. As for vaccine quality, FDA regulation is in place to ensure a sufficient level of safety and efficacy to accomplish the goals of vaccination. [64] The pressure faced by vaccine manufacturers to obtain and maintain FDA approval should provide a check sufficient to guarantee proper vaccine quality. If not, the answer should be to raise FDA standards, rather than to jettison the entire mandatory vaccination process and with it the likelihood of maintaining a sufficient level of immunity among the population.
This response might be unacceptable to those concerned. If the connection between public health officials entrusted with implementing the mandatory vaccination schedule and FDA regulators entrusted with ensuring the safety and efficacy of vaccines is seen as too close, proposing higher FDA standards as a solution may not allay concerns. The independence and integrity of FDA is therefore critical in this arena, just as it is in other areas of public health.
Concern of Unknown Risks
In what may be a combination of the two challenges previously discussed, many individuals challenge vaccine programs because of a lack of information about vaccines. [65] Many people, for example, legitimately question the wisdom of forced vaccination before long-term effects of a vaccine are studied. One website that purports “to provide a wide range of news and views on vaccination and vaccination policy” has summarized this challenge to vaccines simply as opposing the idea of “a parent, any parent, being forced to do something that has even a remote chance of harming their child.” [66] Since long-term (ten or more years down the road) and low-risk (on the order of one-per-million or less, for example) side effects may truly be unknown, this concern does present a challenge for public health officials. [67]
Unfortunately, even the best studies are unable to fully determine all long-term consequences of vaccination. In addition, “[t]here is no such thing as a ‘perfect’ vaccine which protects everyone who receives it AND is entirely safe for everyone.” [68] Therefore, it is true that mandatory vaccination probably forces some parents to inject their children with a substance that will cause some unknown harm.
As with the other objections to mandatory vaccination, however, this objection suffers from a critical flaw. Mandatory school vaccination requirements are not justified solely on the benefit they provide to the recipient. Instead, it is the benefit they provide to the community as a whole by ensuring a sufficient level of vaccination to prevent outbreak that justifies their intrusive nature on individual medical decision-making. [69] For this reason, if public health officials did not enact the mandatory vaccination program, they would be forcing on parents a system that had at least a “remote chance of harming their child.” [70] Because the decision to enact a community-wide vaccination program must be made at the general level if it is to be made at all, and because some children will undoubtedly suffer some health consequences regardless of which policy is chosen, individuals will always be able to raise this argument against mandatory vaccination programs.
A better critique of these programs would focus on whether mandatory vaccination causes more overall harm than a voluntary system; that is, is it better when viewed at the general, rather than the individual, level? Ironically, the very success of vaccination programs in reducing the incidence of once-prominent diseases has led some to ignore the overall and continuing benefit of community vaccination (herd immunity). [71] But for parents to decry the “remote chance” of harm from vaccination while ignoring the very real chance of outbreak in an under-vaccinated population is to reframe the issue entirely.

Other Concerns
Other challenges to vaccination laws have cited strongly held religious or philosophical positions against vaccination in general. Such challenges require a different type of response from public health officials; often the options are limited to overriding such objections and excluding children of parents adhering to such positions from public schools (which is constitutionally permissible under Jacobson and its progeny) or creating exemptions to vaccination requirements (which is detrimental to the overall goals of mandatory vaccination if a sufficient number of exemptors exist). Reactions to such religious and philosophical concerns vary from state to state, with a general trend toward greater accommodation of objectors.
In response to these and other challenges to mandatory vaccination laws, states have enacted various exemptions to vaccination requirements for school entry. Actual enforcement varies by state.
All states provide exemptions for those with medical risks associated with vaccines. [72] If certain contraindications indicate a likelihood of harm from a particular vaccine, the exemption will be allowed. [73] Because such cases are rare and exemptions relatively easy to enforce, there usually is very little risk of compromising the efficacy of the overall vaccination program by granting these exemptions. [74] The ability to grant medical exemptions while still maintaining sufficient levels of vaccination to provide community-wide immunity is one of the great accomplishments of the vaccination system. [75]
In addition to medical exemptions, almost every state grants religious exemptions for those with sincere religious beliefs opposing vaccination. [76] Individual states tend to vary with regard to the level of religious conviction necessary to obtain a religious exemption. Such exemptions reflect the sometimes uneasy balance between mandatory vaccination programs and First Amendment Free Exercise rights, even though the Supreme Court has validated the right of states to mandate vaccination without providing for such exemptions. [77] West Virginia, for example, does not provide religious exemptions. [78]
Some religious exemption statutes have spurred challenges on Establishment Clause grounds by those who claim they favor organized or recognized religions over the sincerely held religious views of others. [79] These challenges, if successful, would lead to the invalidation of many religious exemption statutes. Rather than decrease the number of religious exemptors, however, this may actually lead to more religious exemptors. The political climate of our day, along with the experience of a few states already (such as Arkansas), suggests that legislatures may respond to invalidation of religious exemption statutes that require adherence to an organized religion by drafting more general and expansive religious exemption statutes. [80] By subjugating religion to compulsory vaccination, courts may actually be helping to bring about a system with even more religious exemptors, thereby harming the very vaccination programs to which religious objections had been subordinated. [81]
Philosophical
The possibility that some parents who strongly oppose vaccination for other than religious reasons has led to other means of exempting from mandatory vaccination programs. In some states, people may avoid vaccination requirements by way of philosophical exemptions. [82] In California, for example, a parent need only “submit a letter or affidavit stating that the immunization is contrary to his or her beliefs” to exempt their child from vaccination requirements. [83] “Where available, parents are taking advantage of such exemptions with growing regularity; and in states offering both exemptions, the number of philosophical exemptions far exceeds the number of religious and medical exemptions.” [84]
States without philosophical exemptions, moreover, are often lax with their enforcement of religious exemptions. [85] Because of this, parents in these states can usually submit insincere affidavits purporting to object to vaccination for religious reasons and local health officials, unconcerned with delving into the sincerity of such affidavits, will widely grant exemptions. [86] In most states, therefore, persistent parents can usually find some way to exempt their children from vaccination requirements. If all else fails and vaccination is still regarded as unacceptable to the parent, the option of home schooling may provide a final avenue of evading these school vaccination requirements.
Dangers of Widespread Exemptions
The ease with which non-medical exemptions can typically be obtained has raised concerns among many that the benefits of widespread immunization are being compromised. [87] Because of the nature of medical exemptions, unvaccinated persons in a community with only medical exemptions would be expected to be few and dispersed. Herd immunity can be attained, and protection is ensured for both the vaccinated majority and the unvaccinated few. [88] Broadly granted philosophical and religious exemptions make herd immunity more difficult to attain and increase the risk to the community. This risk is exacerbated by the fact that many of those who apply for such exemptions “will cluster together in one geographic area.” [89] This cluster effect tends to increase the likelihood of serious outbreaks:
Recent studies have shown that clusters of exemptors, who are significantly more susceptible to contracting vaccine preventable illnesses, pose an increased risk of spread of diseases not only to their unimmunized peers, but also to the surrounding, largely vaccinated population. [90]
Given that many childhood diseases seem to be in decline, exemptors may fail to realize the continued value of vaccination. As the mumps outbreak in Iowa makes clear, however, vaccination programs take time and are at risk if vaccination rates fall. Other diseases are still prevalent in other parts of the world, and outbreaks can still occur in this country due to the prevalence of international travel. Ever though measles is rarely observed in the US, for example, the World Health Organization has reported that nearly 900,000 measles-related deaths occurred in developing countries in 1999. [91] Until diseases are eradicated globally, it may be necessary to continue vaccination.
Because many of the aforementioned risks are frequently underappreciated by those who seek exemptions, some have suggested a combination of stricter enforcement of exemption requirements and increased public knowledge of the reasons underlying childhood vaccination requirements. [92] Knowledge is indeed essential to the resolution of this problem. The easier it is to obtain an exemption, the less likely individuals are to understand and appreciate the importance of widespread participation to the success of a vaccination program. Greater public appreciation of the need for such participation (even for diseases that seem to be in retreat), along with greater information on the safety of vaccines can go a long way toward increasing public health in this area. [93]
Partial Exemptors – A Modern Phenomenon
The availability of exemptions has led to other interesting developments in the vaccination debate. Recently, for example, challenges have been raised against the need for mandatory chickenpox and hepatitis B vaccines. Diseases such as these, which are either not greatly feared (chickenpox) or transmitted primarily through voluntary rather than involuntary contact (hepatitis B), do not fit neatly into the typical justification for mandatory vaccination. [94] Nevertheless, public health officials have decided that recently-developed vaccines for these diseases should be placed on the recommended schedule. This has given rise to a significant number of partial exemptors – those who are not opposed to vaccination requirements per se, but who oppose particular vaccines on the schedule. Such a position may not have been comprehended by those who drafted the religious and philosophical exemptions, which seem to assume that a parent’s opposition is to vaccination generally, rather than to a specific vaccine. [95]
Because the religious exemption is usually constructed to apply to those who oppose vaccination generally because of sincere religious beliefs, would-be partial exemptors have difficulty fulfilling their optimal desires. In states without a philosophical objection, parents must choose either to accept the entirety of the recommended schedule of vaccines or to obtain a religious exemption for all vaccinations. [96] Parents who live in states with a philosophical exemption are much more able to tailor their objection to those vaccines with which they disagree. [97]
From the standpoint of a public health official, this presents two possible worlds. In the world with traditional religious exemptors but no philosophical exemptors, overall percentages of vaccinations would be relatively equal from vaccine to vaccine, and higher vaccination rates would be obtained for diseases associated with more objectionable vaccines at the expense of lower vaccination rates for diseases associated with less objectionable vaccines. [98] By contrast, in the world with philosophical exemptors, the public health official would observe higher vaccination rates for the less objectionable vaccines and lower vaccination rates for the more objectionable vaccines. [99]
The difference between these two worlds can have far-reaching implications. If parents are forced to make the all-or-nothing choice, a significant enough number could choose to forego vaccines (including some which they would otherwise accept) that herd immunity is lost, even for less objectionable vaccinations. On the other hand, a significant enough number could accept the more objectionable vaccinations to bring about herd immunity for those diseases. Though the public health official might prefer a world in which neither religious nor philosophical exemptions exist, such a world may not be possible. Therefore, the official should determine which of the two possible worlds provides a greater overall level of safety for the society. In addition, potential public reaction to a vaccine should cause the public health official to consider the ramifications the addition of a vaccine to the schedule will have on those vaccines already on the schedule.
Because partial exemptors have the potential to sway the balance between herd immunity and vulnerability, public health officials must take account of their concerns. Unlike in years past, today the development of a new vaccine presents public health officials with a choice that can affect other vaccines on the recommended schedule. Though the possibility for a chickenpox- and Hepatitis-B-free nation may seem tempting, officials should now consider the possible consequences of mandating such “borderline” vaccines. Parents who might otherwise vaccinate according to the old schedule might have second thoughts about the new vaccines on the schedule and seek means of avoiding the new requirements. If no means exist for avoiding the new vaccines other than complete exemption on religious grounds, parents who would subsequently pursue such exemptions would bring about a lower level of immunization for older diseases.
Studies may be necessary in the above situation to determine whether herd immunity status could be in jeopardy for those diseases for which vaccines are already on the schedule. While one solution might be to provide parents with greater ability to tailor their individual vaccination desires, such a solution would undermine the efficacy of newly scheduled vaccines. In addition, greater levels of flexibility in vaccination choice would undermine public understanding of the community-based nature of vaccination. I think it might be worth sacrificing the efficacy of the newer vaccines in order to maintain that of the more established ones. The public might be willing to suffer the possibility of chickenpox outbreaks, for example, in order to prevent an even minor epidemic of diphtheria or the measles.
Again, information should play a key role in the resolution of this issue. Many of the websites urging parents to carefully consider the vaccination decision do not inform parents that their decision to vaccinate may affect the overall health of the community. [100] The CDC, for its part, does urge parents to take note of this concern. [101] The very persons who most need to know of this concern (those seeking exemptions), however, are often those most likely to distrust CDC publications. For supposed citizen-oriented websites to urge individuals to make vaccination choices without considering how such decisions affect the community is irresponsible, especially given the scientific stability of the concept of herd immunity.
II. THE ROLE OF THE FEDERAL GOVERNMENT
Some of the problems posed to vaccination programs by exemptors and others could be partially solved through greater public awareness of the stringent safety and efficacy testing done on vaccines before they may enter the market. This section summarizes the role of FDA in the context of vaccination programs. In addition, this section will discuss other ways in which the federal government gets involved in the vaccination issue, concluding with a brief synopsis of the no-fault compensation scheme enacted pursuant to the National Childhood Vaccine Injury Act of 1986. [102]
FDA Regulation
Though state governments determine which vaccinations are mandatory for school attendance, the federal government plays a key role in vaccination. Perhaps most importantly, the federal government regulates the safety and effectiveness of all vaccines. The FDA’s Center for Biologics Evaluation and Research (CBER) is charged with this critical task. [103] The role of CBER ranges from pre-approval testing of potential vaccines to facility inspection to continued oversight and sampling after approval. [104] Regulation of vaccines can be more stringent than for other biologics or drugs. [105] Even after a vaccine is licensed, for example, FDA oversight is prevalent. [106] Since vaccines are derived from living organisms and are particularly susceptible to contamination and other environmental factors, manufacturers usually must submit samples of each vaccine lot for testing before release. [107]
Before a vaccine can even be licensed for distribution and use, it must go through an extensive testing process relatively similar to that of drugs and other biologics. [108] First, a new vaccine must be tested for safety on animals. [109] The vaccine manufacturer next must file an Investigational New Drug application (IND) with the FDA. [110] Studies are then undertaken to ensure safety before any human testing takes place. [111] In addition, the IND must describe the studies intended for humans. [112]
Once these initial steps are completed, proposed vaccines must undergo three phases of clinical trials, in which the vaccine is tested on humans. [113] Phase 1 testing looks only for very serious or very common problems. [114] A small number of subjects (usually less than 100) are closely monitored, usually for only a few months. [115] Testing expands in Phase 2 to begin evaluating efficacy, as well as to further test safety. [116] Phase 2 trials can last up to two years and typically include hundreds of subjects. [117] The final stage of testing, Phase 3, further studies safety and effectiveness. [118] Thousands of people may be involved in this stage of testing, and if successful it can lead to application for FDA licensing. [119]
Once the clinical trials are completed, the FDA can examine the results of the tests to determine whether the vaccine is safe and effective enough to be placed on the market. [120] At any point in the process, the FDA may halt ongoing studies if safety concerns require such action. [121] The FDA also reviews the data from the studies and inspects the manufacturing facility. [122] At this point the vaccine may be licensed.
As stated above, the FDA’s role in protecting the safety and effectiveness of vaccines does not end at the licensing stage. [123] Before any vaccines from a particular lot can be released, the manufacturer must typically submit samples for potency, safety, and purity testing. [124] Periodic facility inspections also continue for the duration of the license. [125] Furthermore, formal post-market studies may be conducted in order to identify problems that would not show up in pre-market clinical testing. [126] These tests are referred to as Phase 4 tests and are not mandatory, but can help identify problems that may only occur very infrequently. [127] Post-marketing surveillance programs are important because manufacturers are “never going to be able to do studies big enough to detect risks that might happen at a level of one in 100,000 or one in 1 million.” [128]
The Vaccine Adverse Event Reporting System (VAERS) is another valuable tool in identifying problems with a vaccine once it has been approved for the market. [129] VAERS was developed following Congress’s enactment of the National Childhood Vaccine Injury Act of 1986 and has become a very useful tool for identifying possible adverse effects that would otherwise escape detection. [130] VAERS allows anyone to report a problem that may be associated with any vaccine. [131]
It is important to keep in mind that VAERS is simply a reporting system. Experts and others use the data in VAERS to attempt to determine whether a vaccine actually causes a particular adverse effect, but the events that VAERS documents are not all caused by vaccines. It is therefore easy to understand why VAERS encourages doctors and others to report any adverse event that may be related to a vaccine. “VAERS is designed to detect signals or warnings that there might be a problem rather than to answer questions about what caused the adverse event.” [132] It is important to keep these facts in mind when looking at VAERS data, as many of the adverse effects may be completely unrelated to the vaccine in question. Often the effects are correlated with, but unrelated to, vaccination simply because many of the problems reported are those usually associated with events happening during the vaccination period (the first few years of life). [133]
Used correctly, VAERS can lead to useful studies and the discovery of potentially rare adverse effects. [134] VAERS can also be used to monitor individual lots of a vaccine. [135] Unfortunately, by encouraging individuals to report any adverse effect that may possibly have been caused by a vaccine, VAERS can provide ammunition for those claiming a definite link between a vaccine and a particular adverse effect, even if the data is silent on whether such a link exists. [136] While VAERS is in place to help identify actual risks associated with vaccines, these risks cannot be accurately assessed solely on the basis of reported incidents of adverse effects. [137]
The real value of VAERS lies in the testing and hypotheses that are developed in response to the data that has been reported. Because of the serious adverse effects already occurring during the typical vaccination period, it will often be easy and convenient to point to the correlation between vaccines and reported adverse events. Lost in the picture is the foundational proposition that VAERS is, at its core, a data collection system. To forego scientific inquiry and point instead to simple correlation may be convenient, but it is unwise. [138]
The recent public discussion surrounding the use of thimerosal as a preservative in vaccines helps to illustrate the importance of the FDA and other factors in furthering the goals of vaccine safety and public confidence in the entire safety regulatory process. Thimerosal is a mercury-containing organic compound that for many years has been used as a preservative in vaccines to help prevent contamination with microbes that could potentially be fatal. [139] Recently, fears that mercury at very low levels may be toxic to the brain have raised concern among many in the public about allowing the use of thimerosal in vaccines. [140] Many began to fear a connection between thimerosal and autism. [141] Standard FDA testing of lots, as well as studies measuring the amount of mercury contained in the standard immunization schedule versus accepted safe amounts, did not lead to safety concerns sufficient to pull thimerosal from the market. [142] Though one committee (the Immunization Safety Review Committee, commissioned by the Institute of Medicine) concluded that a theoretical link between thimerosal and autism was biologically plausible, most health experts continue to assert that there simply is no scientific evidence of a link between the two. [143]
During this time period FDA performed additional tests to verify or refute the supposed link between thimerosal and autism. [144] In 1999, FDA performed a comprehensive study and review of thimerosal use in vaccines for children. This review revealed no risk from thimerosal use, other than “local hypersensitivity reactions.” [145] Indeed, none of the standard safety protocols in place suggested or required that FDA pull thimerosal from the market. This is not to say, however, that no risk existed. As is clear from the foregoing summary of FDA vaccine approval, not all adverse effects will be known from clinical trials. [146] It may take years or longer to assess some of the risks of vaccines, including the risk of thimerosal as a preservative. [147]
Continued public concern over the safety of thimerosal caused FDA to begin to work with vaccine manufacturers in order to reduce or eliminate thimerosal from vaccines as a precautionary measure. [148] About this time, the American Academy of Pediatrics and the Public Health Service urged the removal of thimerosal from vaccines. [149] Today, with the exception of the inactivated influenza vaccine, all recommended childhood vaccines are either thimerosal free or contain only trace amounts of the compound. [150] Even though the risk may not have been as great as feared by the public or even existent at all, if the new vaccines are equally effective, the elimination of thimerosal from vaccines can probably be seen as a safety improvement, albeit at the expense of the added research and development needed to create the new thimerosal-free vaccines.
Rather than quell the existing safety concerns, this action led many of those who had decried the use of thimerosal to accuse FDA of participating in a cover-up to protect vaccine manufacturers. [151] Government agencies, for their part, continue to claim that vaccines with thimerosal are as safe as thimerosal-free vaccines, suggesting that the added development may have been superfluous. [152] While this may be so, the availability and now prevalence of thimerosal-free vaccines does provide the scientific and medical community with a new means of assessing the possible autism-causing effects of thimerosal. Namely, since thimerosal is suspected to cause autism within the first few years of life (the routine vaccination calendar), those who were vaccinated in the years since thimerosal-free vaccines have comprised the overwhelming majority of vaccines (that is, those born after 2001) would be expected to experience lower incidences of autism than the groups vaccinated with thimerosal-containing vaccines. [153]
In spite of the potentially costly decision to encourage the development of thimerosal-free vaccines when there is no sufficient safety concern to pull thimerosal from the market, FDA and other government officials have had little success in assuaging the fears and concerns of thimerosal critics. [154] Scientific arguments often fail to persuade, either because they are inconclusive or because of a perceived bias favoring vaccine manufacturers. [155] To back up their own arguments, thimerosal critics rarely point to scientific studies. [156] Instead, their reasoning seems to stem more from anecdotal evidence and comparison of thimerosal (which contains ethyl-mercury) to methyl-mercury-containing fish. [157] Representative Dan Burton (R-Indiana), a key supporter of the fight against thimerosal, explained that his belief in the toxicity of thimerosal stemmed from a personal episode: “[m]y grandson received nine shots in one day, seven of which contained thimerosal, which is 50 percent mercury as you know, and he became autistic a short time later.” [158] Others point to the rise in autism rates in the past twenty years and put the onus on the medical community to prove that this rise is not due to thimerosal. [159]
The response of health officials has been to ask why the burden should be placed on them to disprove a link between thimerosal and autism; cell phones, ultrasound, or diet soda could just as easily be the culprit. [160] Indeed, the typical response to those charging vaccination with causing many of the adverse effects occurring in life’s first few years is to point out that usually such accusations are based on nothing more than the temporal proximity of the vaccine and the illness. Some have suggested that the rates of autism may be on the rise not because of thimerosal, but because of generally more accurate diagnosis of the affliction. [161] In the past, an autistic child may have been wrongfully diagnosed with other mental disorders. [162] Figures showing a correlation between the rise in autism and the drop in other diagnosed mental disorders bolster such assertions, and suggest that vaccination may simply be a convenient scapegoat. [163]
As the thimerosal issue makes clear, vaccines often provoke strong feelings amongst various segments of the population. [164] Proper consideration of public reaction to its actions is a delicate aspect of FDA regulation of vaccine safety. To complicate matters further, one can easily imagine an equally vehement response and similar claims of conspiracy had the FDA not worked to reduce thimerosal from vaccines as a precautionary measure. Indeed, public confidence in the safety of vaccines is often influenced by factors outside the typical FDA calculus. Though FDA must act in the interests of the general safety regardless of public opinion, it may sometimes be necessary for FDA to consider public opinion, at least when exercising discretionary oversight. After all, the entire VAERS system is to a large extent dependant on public cooperation. Nevertheless, when the choice is between FDA popularity and doing what is right for the safety of Americans, the FDA should not allow itself to be swayed by a misinformed public.
Vaccine Injury Compensation Program
Congressional reaction to safety concerns goes beyond the adverse reporting system VAERS. The National Childhood Vaccine Injury Act of 1986, which created VAERS, also created a no-fault compensation scheme for people injured or killed by vaccines as an alternative to the traditional tort system. [165] This system was intended to efficiently and rapidly compensate those who are actually injured by vaccines while maintaining an environment in which further vaccine research and safety improvement could exist. The situation giving rise to this compensation program sounds remarkably similar to the more recent concerns surrounding thimerosal:
In the early 1980's, reports of harmful side effects following the DTP (diphtheria, tetanus, pertussis) vaccine posed major liability concerns for vaccine companies and health care providers, and caused many to question the safety of the DTP vaccine. Parents began filing many more lawsuits against vaccine companies and health care providers. Vaccination rates among children began to fall and many companies that develop and produce vaccines decided to leave the marketplace, creating significant vaccine shortages and a real threat to the Nation’s health. [166]
Funding for the no-fault compensation scheme initially came from Congressional grants of federal tax dollars totaling $110 million per year. [167] Since October 1, 1988, funding has proceeded from the Vaccine Injury Compensation Trust Fund, which is funded by a $0.75 excise tax on all doses of vaccines covered under the program. [168]
One may wonder what makes vaccines worthy of an alternative dispute resolution system. Perhaps it is the result of the power of the vaccine manufacturing lobby or simply an attempt by Congress to pass some legislation in the face of strong public sentiment. Although these reasons may appear plausible, it seems more likely to me that the Act created this no-fault compensation scheme because of the mandatory nature of vaccination. For those injured by other medical devices or drugs, the traditional tort system or medical insurance seem the proper means of addressing the issue. When people are told to undertake a medical procedure they may not agree with because it helps further a public goal, however, it may make sense to have a system in place whereby they can obtain relief quickly if harmed by the procedure. Moreover, because certain vaccines may be closely associated with particular adverse effects, the efficiency of a no-fault scheme may trump the standard fact-finding processes of the legal system. The government has chosen to enact such a no-fault scheme, and err on the side of compensation.
III. ANALYTICAL MEANS OF ADDRESSING THE ISSUE
The concerns and problems raised in the context of mandatory vaccination programs do not readily suggest a simple answer. In examining the issue, I came across two particularly useful tools for analyzing the problem. The first comes from an old episode of The Andy Griffith Show in which a local farmer refused to accept a vaccination from the local nurse. In addition to providing substantial entertainment to the viewer, the characters can be viewed metaphorically to represent the various parties in the mandatory vaccination debate. The episode’s solution, in turn, sheds some light on the current debate.
This section will also utilize the analytical framework of economic analysis. Though not as enjoyable a topic as The Andy Griffith Show, economic theory helps to reshape the vaccination discussion and greatly facilitates the process of assessing the various positions.
“We got to get folks to take their shots” – Sheriff Andy Taylor [169]
The Andy Griffith Show addressed the concept of popular resistance to universal vaccination over forty years ago. In “The County Nurse,” Sheriff Andy Taylor confronted a local nurse who was trying to bring everyone up to date on their tetanus shots. Not surprisingly, at least to Andy, many of the mountain farmers had not been inoculated. The naïve nurse would soon discover the reason for the low vaccination rate.
Rafe Hollister, one of the leading farmers in Mayberry, had little use for modern medicine or doctors in general. “We don’t need any nurse, nobody gets sick up here.” [170] Thermometers? “I know when I got a fever, I’m hot.” [171] Stethoscopes? “I know my heart’s beating, I’m alive ain’t I?” [172] But his strongest objection was saved for vaccinations: “I ain’t never been jabbed and I ain’t fixin’ to be.” [173] Such were the views that the nurse was up against in her attempt to achieve 100% vaccination rates.
Rafe Hollister
Rafe Hollister’s reasons for opposing vaccination went beyond his desire to avoid getting “jabbed.” He was a farmer who lived off the land, and when he got sick he let his body fight the sickness naturally. His daddy had lived to the age of hundred and he aimed to do the same. [174] The concept of a vaccination was certainly something foreign to him, as was the idea that a health official could force him to do anything. Even in the wake of the nurse’s impassioned plea to accept a shot that could someday save his life, he retorted simply, “I done alright before you come around and I’m doing alright now.” [175]
Although the county nurse was not acting pursuant to a mandatory vaccination program, under the circumstances her attempts to get Rafe inoculated were pretty forceful. The nurse was accompanied by the local sheriff to Rafe’s farm to try to convince him to take the shot, and when he refused, the sheriff and nurse continued to attempt to make him acquiesce. When Deputy Barney Fife heard of Rafe’s stubbornness, he insisted the nurse return to Rafe’s farm with him to force Rafe to take the shot. After all, boasted the deputy, “Rafe Hollister’s like a child and he’s gotta be treated like one...I’ll make him take his shot.” [176] When the deputy arrived at Rafe’s farm yelling that he was forcing Rafe to accept the vaccination, Rafe decided to fight the mandatory vaccination by drawing his rifle and forcing the deputy to leave the farm.
In a classic manifestation of the early spirit of the television series, Sheriff Andy Taylor finally convinced Rafe to take the shot through a little reverse psychology. Andy began by facetiously praising Rafe’s refusal to take the shot as stemming from Rafe’s desire for immortality. Namely, by refusing to take the shot, Rafe was sure to become the impetus for all the other townspeople not to neglect to take their shots. Unfortunately for Rafe, this heroic stature would only be achieved posthumously, as he will have succumbed to a violent and painful death from tetanus. As Andy explained to Rafe, someday, after getting cut by a rusty saw or bitten by an animal, without the shot he’ll “be a cinch to go.” [177] Eschewing the chance to be a dead hero, Rafe finally took the shot.
Sheriff Andy Taylor
Vaccination has changed the modern world. Indeed, it has led to the elimination or significant decline of many diseases that once posed significant and potentially deadly health risks. Public health officials in the United States have managed to institute a program that, though subject to variations on a state by state basis, essentially mandates certain vaccinations as a requirement for school attendance. While these vaccination programs are touted by most public health officials, a significant number of people oppose mandatory vaccination. The County Nurse episode helps illuminate the perspectives of the various sides of the issue, as well as one possible solution.
The nurse herself represents the public health officials. Though she is not implementing a mandatory vaccination program, her stated goal is to inoculate 100% of the population. [178] As mentioned above, she has the assistance of local law enforcement and she is quite persistent. Rafe Hollister, the stubborn farmer, represents those within the community who oppose or resist mandatory vaccination programs. His reasons initially rest on a general reluctance to stray from natural medicine. In this way he represents the contingent of society that scientists and medical researchers will always find difficult to convince of any developments in the medical field. In many ways, he is comparable to the plaintiff in Jacobson . Andy and Barney can be seen as the arms of the state that are entrusted with carrying out the general vaccination plan. Their varying styles can be seen as varying state requirements and enforcement options for vaccination.
Though these comparisons may seem elementary and of little value, the character development that the characters undertake during the episode greatly increases the episode’s usefulness as a surrogate for real world concerns and issues. Rafe resists the shot initially not only because he distrusts medicine in general, but also because he resents the idea that a county nurse can make him do anything. Many who resist mandatory vaccination schemes do so because of personal liberty concerns; they do not want the government to tell them what to do, especially in the context of personal medical decisions. Just as Rafe’s stance becomes more vehement the harder the nurse attempts to convince him, many who oppose mandatory vaccination see the persistence of the medical community as evidence of blind adherence to a potentially dangerous system, or worse yet as an active promotion of the special interests of the vaccine manufacturers. [179] The episode does not paint the nurse in this way at all, however. Rather, after seeing how strongly Rafe opposes vaccination, the nurse passionately pleads with him to reconsider. Her stance truly seems to stem from a genuine concern that he not suffer the potentially terrible effects of the disease. [180] As before, he refuses; this seems to illustrate that the stance of some may be so strong that they will never accept vaccination on the basis of arguments advanced by government officials.
Barney Fife’s insistence that Rafe accept the shot demonstrates the lack of understanding among many in the government and in the general population as to the vehemence with which those opposing mandatory vaccination hold to their views. His paternalistic stand only serves to exacerbate the situation with Rafe. Indeed, Barney Fife helps to illustrate that there cannot be a one-way solution to the issue of mandatory vaccination.
Andy Taylor’s method of convincing, which eventually carried the day, may not be very conducive to real-world implementation. After all, it is unrealistic to think that reverse psychology will convince those currently opposed to vaccination programs to change their minds. What I think is important to notice, however, is the role information can play in this issue. Andy finally convinces Rafe Hollister to take his shot after describing the horrible effects of the disease and how likely Rafe is to contract it. Similarly, any solution to the issue of mandatory vaccination holdouts must rely on increased information dissemination. That the information in the episode came from a trustworthy source may also have been crucial, which seems to imply that public health officials may need to work more closely with local personnel in order to obtain higher vaccination rates.
Because this episode deals with the vaccine for tetanus, a non-communicable disease, the usual community-based arguments in favor of vaccination do not enter the equation. Extra-personal consequences of Rafe’s decision to vaccinate do exist, however. Most importantly, as the unofficial leader of the farming community, his decision will be followed by the other farmers. This is shown both in Andy’s assurances to the nurse that Rafe is the most important of the farmers to convince on the issue and later, after Rafe has decided to get the shot, in his promise to the nurse that all she has to do is come with him and he’ll get all the farmers to take their shots. Perhaps those parents who support vaccination can help bring about higher vaccination rates by being more vocal and persistent with their neighbors who oppose vaccination programs.
Economic Analysis
Economic analysis [181] provides a useful theoretical basis for evaluating the competing sides of the vaccination debate. Arguments regarding the wisdom of the current vaccination policy can often be recast as economic questions involving a cost-benefit analysis.
When an epidemic breaks out, for example, the benefits of vaccination (protection from the disease both for the individual and for society through herd immunity) seem more clearly to outweigh the costs (potential side effects of the vaccine, decreased ability of the immune system to defend the body from variant strands of the disease, or personal or religious objection). Vaccination rates would, therefore, be expected to be highest during such epidemics. Consequently, those few who continue to oppose vaccination during such epidemics would be expected to do so for only the strongest reasons. This is due to the fact that in economic terms, the opponent of vaccination would have to believe that the benefits of vaccination still do not outweigh the costs, even during an epidemic. This might stem from a relative undervaluation of the benefits of vaccination (perhaps due to a belief that contracting the disease would not be so bad) or a relative overvaluation of the costs of vaccination (possibly due to the greater cost to the conscience of the personal or religious opponent of vaccination) or some combination of both. Medical exemptions directly illustrate this cost-benefit analysis: for a person likely to suffer serious side effects from a vaccine, the cost of vaccination is much greater than the cost to the average individual. Even in a time of epidemic, therefore, vaccination might not be rational for such an individual.
This economic analysis of vaccination is well illustrated by the facts of Jacobson v. Massachusetts [182] , the first Supreme Court case addressing the constitutionality of mandatory vaccination legislation. The case involved a Massachusetts statute allowing local authorities to mandate vaccination for smallpox if necessary for the public health and safety. [183] Subsequently, and upon a determination that smallpox was “prevalent to some extent” and “continues to increase,” the city of Cambridge passed a mandatory vaccination ordinance. [184] This ordinance represented the economic determination that the benefit of mandatory vaccination outweighed the cost of supplying vaccines, finding and prosecuting holdouts (such as Jacobson), and the decreased liberty of individuals to be permitted to decide whether to vaccinate.
Jacobson subsequently challenged his prosecution under the ordinance by claiming it to be an unconstitutional denial of his liberty under the 14th Amendment (as well as in violation of the Preamble and the “spirit” of the Constitution, arguments that were summarily dismissed). [185] In economic terms, this may simply indicate that he viewed the cost of accepting a forced vaccination (perhaps of any kind, in any circumstance) as greater than any possible benefit. A closer look at his arguments, however, suggests that he may have performed a more detailed cost-benefit analysis. One can easily convert the various arguments he attempted to advance into economic costs. Among these arguments were the likelihood of vaccination to bring about “serious and permanent injury” and occasional death, the inability of an individual to assess the risk of vaccination in a particular case, and the potential impurity of vaccines and inability to test such impurity, among others. [186] At the very least, it would appear that Jacobson attributed a greater than average cost to vaccination.
The statute also provided that ordinances mandating vaccination provide an exception for “children who present a certificate, signed by a registered physician, that they are unfit subjects for vaccination.” [187] This reflects the state’s determination that the cost of forcing vaccination upon those more likely to suffer adverse side effects outweighed the benefit of completely universal vaccination. Given the determination that near-universal vaccination was required to provide the desired benefit, one would expect that the state expected to grant relatively few medical exemptions (or at least few enough not to seriously compromise the goal of providing protection against smallpox through vaccination).
In rejecting Jacobson’s liberty challenge to the ordinance, the Court endorsed the concept that the State’s cost-benefit analysis can supersede that of the individual, at least in the area of public health. The Court’s decision, in fact, makes irrelevant any individual cost-benefit analysis in the face of a comprehensive mandatory vaccination program.
Various vaccination-related developments in the century since Jacobson can also be cast in an economic analytical framework. Certainly the benefit from vaccination disappears when a disease has been eradicated, which explains why the smallpox vaccine is no longer mandated. Any cost greater than zero (the likely benefit of smallpox vaccination at this point, barring of course a reintroduction of the disease using laboratory samples) will suffice to outweigh this benefit. [188] The success of vaccination policies, however, may lead to an undervaluation of the benefit of continuing to vaccinate due to the lack of visible instances of the disease. [189] This problem may be compounded when vaccines are mandated for diseases which are not associated with high mortality rates, such as chickenpox. A further complication to the cost-benefit analysis arises when assessing vaccination policy for diseases such as Hepatitis B, which is spread typically through voluntary contact. In such a case, an individual who feels highly unlikely to engage in the behavior giving rise to the risk of the disease might rationally see very minimal benefit from vaccination, while the state may view widespread vaccination as the most cost-effective method of dealing with the disease. [190]
Altruism and Free Riding
Given the continuing policy of vaccinating for diseases that have become relatively rare in recent decades, one might expect individual cost-benefit analyses to increasingly come into conflict with the societal policy. Several factors, however, serve to counteract this possibility. Perhaps most significantly, it is likely that many parents defer on the question of vaccination and accept the cost-benefit analysis of the state (communicated to the individual through the vaccination schedule and through doctor’s recommendations) as their own. Along the same lines, many individuals might not strongly consider the pros and cons involved in vaccinating; if the possibility exists for contracting a disease, and a vaccination is available, the decision may already be made. [191] A third possibility implicates a factor that I have not yet mentioned in relation to the individual cost-benefit analysis: altruism.
Some have proposed that altruism may bridge the gap between incompatible cost-benefit analyses of states and individuals. [192] Whereas typical medical decisions affect only the patient making the decision, it is pointed out, medical decisions regarding vaccine-preventable diseases usually implicate outside interests. [193] A patient thinking only of his own interests may forego vaccination if he feels the risk from vaccination outweighs the personal benefit. Altruism, it is argued, may present a separate benefit for such an individual. [194] Though the individual may not consider the risk of contracting the disease high enough by itself to justify vaccination, he may still vaccinate in order to help accomplish the public goal of eliminating the threat of an epidemic. Public health officials hope that comprehensive vaccination will produce herd immunity. [195] Thus the individual who may otherwise forego vaccination might undertake it in order to “do his part” for the community at large. Individuals who cannot vaccinate are particularly dependent on this sort of altruistic behavior, as they often have no other protection from the disease. [196]
Working against this altruistic behavior is the temptation of individuals to enjoy the benefit conferred on them by herd immunity without undertaking the cost of being vaccinated personally. [197] This is widely referred to as “free riding,” and greatly undermines the goal of comprehensive vaccination. Since herd immunity is supposed to create a level of protection sufficient for even those few who are not vaccinated, a small number of free riders might not pose a significant problem. As described earlier in this paper, comprehensive vaccination programs are designed to work even though some members of society cannot be vaccinated. [198] The problem arises when the number of free riders becomes sufficiently high to compromise the ability of the society to achieve herd immunity. Since the average citizen (one with no greater reason to avoid vaccination than any other member of society) could always choose to free ride if immunization were voluntary, herd immunity might never be achieved. This is one of the key arguments advanced in support of government mandated vaccinations. [199]
Ex Ante Versus Ex Post
The concepts of altruism and especially free riding emphasize the importance of ex ante (before the fact) versus ex post (after the fact) decision making in the context of vaccination. One of the main benefits of economic analysis is that it requires decisions to be justified ex ante. Public health officials, for example, are faced with the decision of whether to mandate vaccination for a particular disease at a time when all adverse effects cannot be known. They must weigh the possible consequences of allowing a disease to continue against the possible known and unknown adverse effects of a vaccine that may have just entered the market. When this decision is made properly, the benefit of the vaccination program will have outweighed the cost. The benefit is manifested in lower or no occurrences of the disease, while the cost is seen most directly in those children who have actually experienced adverse effects as a result of the vaccine. If the benefit is greater than the cost from an ex ante perspective, to the economist there should be no second-guessing of the vaccination program. [200]
The economist, of course, is not the parent. Parents who decry mandatory vaccination as the cause of their child’s adverse reaction are typically viewing the situation ex post. That the program has been implemented assumes that the sum of these adverse reactions was an acceptable alternative to non-implementation, and should therefore not be allowed to undermine public confidence in the program. When one surveys the landscape of the vaccination issue, however, objections are usually of the ex post variety. Since it is harder to appreciate the absence of an epidemic than the presence of a child suffering a vaccine-related injury, it is easy to look at the issue solely ex post. In the interests of public safety, such reasoning should be avoided.
This is not to imply that all critics of mandatory vaccination are on unsound theoretical footing. In fact, those whose objections are marked by a distrust of the government authorities in charge of implementing vaccination programs can be seen as questioning only the ex ante judgment of the officials. If this is so, they are actually on firmer ground than those who object to the programs because they feel their child was harmed by the vaccine. Ex ante critiques are valuable because they can bring about change in the system at a time when it can still prove useful.
The National Vaccine Injury Compensation Program represents a theoretically sound program under these criteria. Economically, it represents the idea that some of the costs of mandatory vaccination programs known only ex post will be compensated by all those who share the benefits ex ante. The excise tax, paid ex ante by all who receive the vaccine, is used to compensate anyone who experiences certain adverse effects ex post. This is simply an example of the government distributing the costs of the vaccination program across the spectrum of those who receive the benefit, rather than an ex post complaint by those on whom the costs have fallen.
Other Issues
The modern trend toward more widely-granted exemptions represents government acquiescence toward a certain degree of free riding. Should such exemptions proliferate too widely, herd immunity may indeed be lost and a recalculation of the cost-benefit analysis of individuals will be necessary. In the face of a greater potential to contract disease, the benefit of vaccination grows significantly, while the cost of accepting the vaccine remains the same. Likewise, from the standpoint of the government, the cost of allowing widespread exemptions will eventually overtake the benefit of permitting such exemptions if that cost suddenly includes serious risk of epidemic.
The risks associated with non-vaccination can be illustrated through a rather simplified mathematical example. [201] Suppose a school with 1,000 students is exposed to a measles outbreak. 990 of the students have received all of their measles shots, and so are fully immunized. Suppose further that the measles vaccine is 99% effective; that is, it produces complete immunity in 99% of patients. [202] Therefore, 10 out of the 990 who have been fully immunized will be susceptible to the disease. In addition, all 10 of the 1,000 students who had not been fully immunized will be susceptible to measles. Therefore, 20 out of 1,000 students will get the disease. Although the number of infected students who were vaccinated is equal to the number who were not, this example demonstrates that vaccination can be very effective even if it sometimes does not produce immunity in an individual. If no one had been vaccinated, 980 more students would probably have caught the measles. It is also important to note that this example assumes an epidemic; in reality, herd immunity would probably be attained at this level of inoculation and none of the 1,000 students would have caught the disease.
IV. CONCLUSION
Vaccines have immeasurably improved our quality of life. They have led to the eradication of deadly diseases like smallpox and the near elimination of diseases such as diphtheria, polio, and measles. Outbreaks of vaccine-preventable diseases, such as mumps, are infrequent and are also quite newsworthy on the rare occasion that they do occur. And people like Rafe Hollister can survive a run-in with a rusty saw or an animal bite.
The life-saving benefits of vaccination often overshadow the vast economic and personal benefits it has helped provide. Jonas Salk’s cure for polio has spared generations from a life hindered by the devastating physical handicaps of that terrible affliction. Children no longer must miss vast stretches of school to overcome a debilitating battle with pertussis (although there is no doubt that some children lament this decline in excused absences from school). Parents no longer have to spend restless hours worrying as their children suffer the body’s natural response to disease. In economic terms, this translates directly into fewer missed hours of work and less administrative difficulty, leading to a generally more productive society.
For all the benefits of vaccines, of course, it is important not to ignore the costs. The National Vaccine Injury Compensation Program is one way of dealing with the economic costs of vaccination, but this may provide little solace to the parent of a child who has been injured by a vaccine for a disease that is seemingly in decline. Side effects with very low probability will sometimes occur; though from a community-wide view this possibility is acceptable, for the individual who experiences the adverse effect the vaccination may not have been the best medical decision. Many who view natural immunity as a rite of passage for children might not desire a means of bypassing the disease entirely.
Some may accuse public health officials of dreaming for an unreachable day when all diseases are controlled by vaccination. Zeal on the part of public health officials, however, should not overshadow the actual benefits of vaccination generally. Soon may come the day when diphtheria, like smallpox, will be eradicated globally. At that point, it can be removed from the vaccination schedule and future generations will reap the benefits of vaccination while undertaking none of the costs.
This prospect, I think, sheds light on the ultimate solution to vaccination issues that have been discussed in this paper. Highly communicable and especially terrible diseases should continue on the vaccination schedule until they are virtually eliminated. The eventual elimination of these scourges will someday make vaccination unnecessary, and the costs of vaccination will drop to zero. Until that time, officials should seek stricter enforcement of the mandatory vaccination laws and should tighten down on non-medical exemptions. At the same time, information campaigns should be considered in the interest of reminding the public of the continued importance and relevance of vaccine programs. Though risks are unavoidable when dealing with vaccines, parents should constantly be reminded that immunity depends on a high level of cooperation. This will hopefully keep immunization rates high, at least for the most harmful diseases.
Meanwhile, public health officials may be wise to consider an alternate stance toward somewhat less-important vaccines such as Hepatitis B and varicella (chickenpox). [203] With such diseases it may be worthwhile to wait longer before placing the vaccines on the recommended schedule. This will undoubtedly make herd immunity more difficult if not impossible to attain, while simultaneously announcing to parents that undertaking the vaccine in question is a personal medical decision. Most of those who choose to vaccinate (and accept the risk of adverse effects from these newer vaccines) will still acquire immunity. Without a mandatory program in place, however, one would still expect to see regular occurrences of the disease. Given the relatively high likelihood of outbreak under these circumstances, a percentage of those who vaccinate will probably get the disease. They will likely turn to those who did not vaccinate at all and see them as the cause of the outbreak. In time, social pressures may lead to greater vaccination rates, and the time may be ripe for greater acceptance of mandatory vaccination for the disease.
One significant benefit to this approach lies in its natural tendency to point out to parents the importance of receiving the more important vaccines. When some vaccines are mandatory and others are not, the distinction between the two types of vaccines is impossible to neglect. It would hopefully make parents think more carefully before attempting to gain an insincere exemption. This approach would fail to satisfy those who want parents to have the option to choose “one, ten, or no vaccines,” [204] but it would at least allow an element of choice for some vaccines while hopefully maintaining a sufficient level of immunization for the more important vaccines. It is also important to remember that parents with serious reservations about any vaccines will usually have the option of home schooling. Overall, this approach might have the advantage of winning over those who only partially object to the vaccination schedule, thus helping bring about a greater chance of herd immunity for diseases associated with less objectionable vaccines.
Vaccination certainly is unique among medical treatments, both for its incredible potential and its coercive nature. It is unfortunate that questionable evidence has led many concerned parents to question the wisdom of vaccination programs that still serve important goals. Given the importance of public support for the achievement of these goals, however, public health officials must account for sometimes questionable concerns in determining vaccination policy. Greater information dissemination, combined with more sharply drawn (and potentially vaccine-specific) guidelines, can hopefully further the important goals of vaccination policy.
[1] Center for Disease Control, “Smallpox Disease Overview,” at http://www.bt.cdc.gov/agent/smallpox/overview/disease-facts.asp (last visited April 27, 2006).
[2] GlaxoSmithKline is currently developing an ear infection vaccine and plans to seek regulatory approval shortly. Jessica Said, “Vaccine Could End Children’s Ear Infections,” CNN online article, March 3, 2006 (on file with author).
[3] Institute of Medicine. CP Howson, et al. eds. Adverse Effects of Pertussis and Rubella Vaccines. Washington, DC: National Academy Press; 1991, at 1.
[4] James G. Hodge, Jr. and Lawrence O. Gostin, School Vaccination Requirements: Historical, Social, and Legal Perspectives , 90 Ky. L. J. 831, 867 (2001).
[5] See, e.g., Jacobson v. Massachusetts , 197 U.S. 11 (1905).
[6] Hodge and Gostin, supra note 4, at 867.
[7] Id. at 868.
[8] “Rather than having health departments require immunization in emergency conditions, legislatures acted to prevent disease by mandatory immunization as a condition of enrollment or attendance in schools or licensed day care facilities.” Id.
[9] See id. ; see also infra Part I (chart describing the current recommended vaccination schedule).
[10] The Center for Disease Control has gone so far as to suggest that “to have a medical intervention as effective as vaccination in preventing disease not use it would be unconscionable.” Center for Disease Control, National Immunization Program publication, “Six Common Misconceptions About Vaccination and How to Respond to Them,” at http://www.cdc.gov/nip/publications/6mishome.htm (last visited April 27, 2006) (hereinafter “Six Common Misconceptions”).
[11] Center for Disease Control, National Immunization Program publication, “Ten Things You Need to Know about Immunizations,” at http://www.cdc.gov/nip/publications/fs/gen/shouldknow.htm (last visited April 27, 2006).
[12] This is not to imply that parents who vaccinate without carefully considering the pros and cons of vaccination are in the wrong. The health and safety of a child is of paramount importance to most parents, and every parent must make decisions that affect the welfare of the child. Most parents approach such decisions with a sincere desire to promote the child’s best interests, and this desire is no different in the context of vaccination.
[13] “Despite its utility, vaccination has provoked popular resistance from the beginning.” Hodge and Gostin, supra note 4, at 834.
[14] “Some opponents express valid scientific objections about effectiveness or need for mass vaccinations; some fear harmful effects arising from the introduction of foreign particles into the human body; and others worry that vaccination actually transmits, rather than prevents, disease, or weakens the immune system.” Id.
[15] See, e.g. , Jacobson v. Massachusetts , 197 U.S. 11 (1905) (constitutional challenge to government mandated smallpox vaccination); “Six Common Misconceptions,” supra note 10 (“[s]ome see mandatory vaccination as interference by the government into what they believe should be a personal choice”).
[16] “Six Common Misconceptions,” supra note 10.
[17] A more detailed explanation of this subject appears in Part I of this paper.
[21] See, e.g. , “Ten Things You Need to Know about Immunizations,” supra note 11.
[22] Angie A. Welborn, “Mandatory Vaccinations: Precedent and Current Laws,” CRS Report for Congress, at http://www.fas.org/sgp/crs/RS21414.pdf (last updated Jan. 18, 2005).
[23] For a typical scenario of public health response to outbreak, see the facts of Jacobson v. Massachusetts , 197 U.S. 11 (1905).
[24] Hodge and Gostin, supra note 4, at 833-34.
[25] Id. at 867-68.
[26] Id. at 833.
[29] This level of immunity is often referred to as “herd immunity,” the concept that not everyone in a population must be vaccinated in order for the entire population to be protected. Abi Berger, “How Does Herd Immunity Work?” 319 BMJ 1466 (1999). “As long as a sufficient number of children are immunised against each disease for which there is a vaccine, protection against that disease will be conferred on everybody.” Id. Also, the level of vaccination necessary to attain herd immunity increases as the infectivity of the disease increases. Id. Highly infectious diseases, therefore, require higher levels of immunity for herd immunity to occur. Id. The concept of herd immunity will arise throughout this paper, with particular emphasis in Part III.
[30] This is evidenced by the fact that in time of outbreak, the vaccinated population can still be susceptible to the disease, although usually the vaccinated population is far less susceptible to the disease than the unvaccinated population. Vaccines typically produce the desired antibody in an individual around 90% of the time, with actual percentages varying from vaccine to vaccine. Some vaccines, moreover, lose their efficacy and require boosters. These concepts will be further developed throughout this paper.
[31] Hodge and Gostin, supra note 4, at 850-51.
[32] Id. at 851.
[33] Id. at 834.
[34] Id. at 834-35.
[35] See, e.g. , Duffield v. Sch. Dist. , 29 A. 742 (Penn. 1894).
[36] 197 U.S. 11 (1905).
[38] Id. at 26.
[39] Welborn, supra note 22.
[41] 260 U.S. 174 (1922).
[42] Id. at 175.
[43] Id. (“[t]he bill charges that there was then no occasion for requiring vaccination” and that the ordinances “in effect, mak[e] vaccination compulsory”).
[45] Id. at 176.
[48] Id. at 177.
[49] Hodge and Gostin, supra note 4, at 867-68.
[50] Id. at 868.
[51] The schedule of immunizations is published by the Center for Disease Control, and follows the recommendations of the Advisory Committee on Immunizations Practices, the American Academy of Pediatrics’ Committee on Infectious Diseases, and the American Academy of Family Physicians. Id.
[52] Id. at 869.
[54] Based on chart publicized by Center for Disease Control, approved by Advisory Committee on Immunization Practices, American Academy of Pediatrics, American Academy of Family Physicians, available at http://www.cispimmunize.org/IZSchedule_2006.pdf (last visited April 27, 2006).
[55] Indeed, the law in Jacobson was challenged for this reason.
[56] Statement of Barbara Fisher, founder of National Vaccine Information Center, quoted in Neenyah Ostrom, “First Do No Harm,” at http://www.chronicillnet.org/online/Fisher.html (last visited April 27, 2006).
[57] K.N.O.W. Vaccines, Vaccine Awareness of Florida fact sheet, at http://www.know-vaccines.org/vaccine_fact.html (last visited April 27, 2006).
[58] The most direct way in which this occurs surrounds the concept of herd immunity, as discussed elsewhere throughout this paper. If a sufficient number of persons in the community does not vaccinate, herd immunity may be unattainable and others may be put at risk.
[59] See, e.g. , the discussion in Part III involving The Andy Griffith Show.
[60] See Statement of Barbara Fisher, quoted in Ostrom, supra note 56. See also “Autism and Vaccines: Activists Wage a Nasty Campaign to Silence Scientists,” Wall Street Journal, February 16, 2004, at http://www.opinionjournal.com/forms/printThis.html?id=110004700 (last visited April 27, 2006) (citing vaccination critics who had accused the vaccination-defending writers of “having an ‘industry profit promoting agenda’”).
[61] See Statement of Barbara Fisher, quoted in Ostrom, supra note 56.
[64] See the discussion in Part II regarding vaccine safety.
[65] See, e.g. , “Six Common Misconceptions,” supra note 10.
[66] Mission Statement of Vaccination News website, at http://www.vaccinationnews.com (last visited April 27, 2006).
[67] As the discussion in Part II on vaccine safety demonstrates, pre-licensing testing for very rare adverse effects cannot take place if vaccines are ever to reach the market. Phase 4 post-licensing testing does exist, but may take years to discover extremely rare adverse effects.
[68] World Health Organization Immunization Safety page, “Adverse Events Following Immunization,” at http://www.who.int/immunization_safety/aefi/en/ (last visited April 27, 2006).
[69] As the recent mumps outbreak in Iowa demonstrates, not everyone who receives a vaccine develops immunity to the disease. For this reason, the success of vaccination depends on a sufficient level of vaccination in the community. When a significant percentage of the population has not received the vaccine, an outbreak can occur and even threaten some of those who have been vaccinated. See David Pitt, “Iowa Mumps Epidemic Continues to Broaden,” Associated Press, April 13, 2006, at http://www.breitbart.com/news/2006/04/13/D8GVGL600.html (last visited April 27, 2006). See also the above discussion of the history of vaccination.
[70] Mission Statement of Vaccination News website, supra note 66.
[71] See, e.g. , Ross D. Silverman, “No More Kidding Around: Restructuring Non-Medical Childhood Immunization Exemptions to Ensure Public Health Protection,” 12 Annals Health L. 277, 278-79 (2003).
[A]s risks of contracting many deadly and crippling diseases continue to decline to near negligible levels, and rates of childhood immunization continue to reach record levels, the public today places greater attention on the relative weaknesses and dangers of immunizations, and the systems through which they are administered.
[72] Hodge and Gostin, supra note 4, at 874.
[73] Usually this requires physician certification. Id.
[74] Indeed, the CDC itself presupposes the existence of medical exemptors in any broad mandatory vaccination program. See “Six Common Misconceptions,” supra note 10 (noting that the mandatory vaccination program can work to protect even those few who cannot vaccinate because of the possibility of adverse medical reactions).
[76] Hodge and Gostin, supra note 4, at 874.
[77] Jacobson v. Massachusetts , 197 U.S. 11 (1905). See also Employment Division v. Smith , 494 U.S. 872 (1990) (permitting neutral laws of general applicability that incidentally affect religion); Boone v. Boozman , 217 F.Supp.2d 938 (E.D. Ark. 2002) (“constitutionally-protected free exercise of religion does not excuse an individual from compulsory immunization...the right to free exercise of religion and parental rights are subordinated to society’s interest in protecting against the spread of disease”).
[78] W. Va. Code Sec. 16-3-4 (2004).
[79] See, e.g. , Boone v. Boozman , 217 F.Supp.2d 938 (E.D. Ark. 2002). The challenged Arkansas immunization statute exempted “individuals for whom ‘immunization conflicts with the religious tenets and practices of a recognized church or religious denomination of which [they are] an adherent or member.’” The statute was struck down under the Establishment Clause using the test laid out in Lemon v. Kurtzman , 403 U.S. 602 (1971). 217 F.Supp.2d at 950. The Arkansas legislature subsequently amended the exemption generally to allow for religious or philosophical objections without regard to recognized churches. Ark. Code Sec. 6-18-702(d).
[80] See Silverman, supra note 71, at 290-93.
[81] See id.
[82] Hodge and Gostin, supra note 4, at 874.
[83] Cal. Health and Safety Code Sec. 120365 (2003).
[84] Silverman, supra note 71, at 284.
[85] Id. at 285.
[87] See id.
[88] Recall that for those unable to vaccinate for medical reasons, herd immunity provides the only protection from the disease. See “Six Common Misconceptions,” supra note 10.
[89] Silverman, supra note 71, at 285.
[90] Id. The recent mumps outbreak may directly demonstrate this. Officials have pointed out that vaccination only confers immunity on 95% of patients, and of those affected in the recent outbreak, 25% have been vaccinated. See Pitt, supra note 69. The strong implication is that the 75% of those inflicted who were not vaccinated have put the entire community at risk.
[91] Center for Disease Control, National Immunization Program publication, “What Would Happen If We Stopped Vaccinations?” at http://www.cdc.gov/nip/publications/fs/gen/WhatIfStop.htm (last visited April 27, 2006).
[92] Silverman, supra note 71, at 293.
[93] Silverman suggests that eliminating philosophical and religious exemptions would do more harm than good. This approach, he believes, “would exacerbate feelings of animosity and skepticism toward vaccination and the public health system in general.” Id. at 293. On this score he is probably correct, and I agree that wider knowledge, at the very least, is a better initial response to this problem.
[94] Incidentally, it is worth mentioning that of the more longstanding vaccines, the tetanus vaccine stands out as unique. Tetanus is a very harmful disease with about a 20% fatality rate. “What Would Happen If We Stopped Vaccinations?” supra note 91. What makes it unique in the vaccine schedule is that tetanus is not contagious. That is, herd immunity is not attainable and cannot be used to justify mandatory tetanus vaccination. The reason for the general acceptance of the tetanus vaccine seems to stem both from the high risk of the disease and the fact that tetanus can only be prevented by immunization. In addition, the tetanus vaccine for infants has been combined with the vaccines for diphtheria and pertussis. On strictly public health grounds, however, the status of the tetanus shot on the compulsory vaccination schedule comes closest to government fiat of individual health decisions.
[95] Because medical risks may vary from vaccine to vaccine, and thus the justification for such exemptions remains even if the risk is to some but not all vaccines, medical exemptions are somewhat outside the scope of this discussion.
[96] Sean Coletti, Taking Account of Partial Exemptors in Vaccination Law, Policy, and Practice , 36 Conn. L. Rev. 1341, 1344 (2004).
[98] This follows directly from the all-or-nothing nature of the vaccination decision in this world.
[99] Again, this follows directly from the nature of the decision.
[100] See, e.g. , National Vaccine Information Center, at http://www.nvic.org (last visited April 27, 2006) (urging parents to consider eight questions before vaccinating, none of which inform parents of the effect their decision may have on others).
[101] See “Six Common Misconceptions,” supra note 10.
[102] 42 U.S.C. §§ 300aa-1 to 300aa-34.
[103] U.S. Food and Drug Administration, Center for Biologics Evaluation and Research, “Vaccine Product Approval Process,” updated July 27, 2002, at http://www.fda.gov/cber/vaccine/vacappr.htm (last visited April 27, 2006) (hereinafter “Vaccine Product Approval Process”).
[104] See id.
[105] See, e.g. , Isadora Stehlin, “How FDA Works to Ensure Vaccine Safety,” FDA Consumer magazine (December 1995), at http://www.fda.gov/fdac/features/095_vacc.html (last visited April 27, 2006).
[106] “Licensing of a vaccine is only the beginning of FDA’s oversight.” Id.
[109] “Vaccine Product Approval Process,” supra note 103.
[112] Stehlin, supra note 105.
[115] Id. ; “Vaccine Product Approval Process,” supra note 103.
[116] Stehlin, supra note 105.
[118] “Vaccine Product Approval Process,” supra note 103.
[121] Id. ; Stehlin, supra note 105.
[123] Indeed, the National Immunization Program has confidently pointed to the FDA’s role in continued oversight of vaccines:
FDA would recall a lot of vaccine at the first sign of problems. There is no benefit to either the FDA or the manufacturer in allowing unsafe vaccine to remain on the market. The American public would not tolerate vaccines if they did not have to conform to the most rigorous safety standards. The mere fact that a vaccine lot [is] still in distribution says that the FDA considers it safe.
“Six Common Misconceptions,” supra note 10.
[124] “Vaccine Product Approval Process,” supra note 103.
[127] Stehlin, supra note 105.
[128] So states Susan Ellenberg, Ph.D., director of CBER’s division of biostatistics and epidemiology. Id.
[129] “Vaccine Product Approval Process,” supra note 103.
[130] Stehlin, supra note 105.
[136] See, e.g. , “Six Common Misconceptions,” supra note 10 (“[o]nly some of the reported health conditions are side effects related to vaccines. A certain number of VAERS reports of serious illnesses or death do occur by chance alone among persons who have been recently vaccinated”).
[137] “VAERS reports have many limitations since they often lack important information, such as laboratory results, used to establish a true association with the vaccine.” Id.
[138] “In summary, scientists are not able to identify a problem...based on VAERS reports alone without scientific analysis of other factors and data.” Id.
[139] U.S. Food and Drug Administration, Center for Biologics Evaluation and Research, “Thimerosal in Vaccines,” at http://www.fda.gov/Cber/vaccine/thimerosal.htm (last updated Sept. 6, 2005).
[141] See, e.g. , Gardiner Harris and Anahad O’Connor, “On Autism’s Cause, It’s Parents vs. Research,” New York Times, June 25, 2005, at http://www.nytimes.com/2005/06/25/science/25autism.html (last visited April 27, 2006) (reporting the ongoing tension between parents of autistic children and the medical community over the use of thimerosal in vaccines).
[142] See, e.g. , Center for Disease Control, National Immunization Program publication, “Mercury and Vaccines (Thimerosal),” at http://www.cdc.gov/nip/vacsafe/concerns/thimerosal/default.htm (last visited April 27, 2006) (studies have failed to find any association between exposure to thimerosal in vaccines and autism); “On Autism’s Cause, It’s Parents vs. Research,” supra (noting that the amount of ethyl mercury in each childhood vaccine was once about the same as the amount of methyl mercury, a more toxic compound, found in an average tuna sandwich).
[143] “Thimerosal in Vaccines,” supra note 139.
[146] Stehlin, supra note 105.
[149] “On Autism’s Cause, It’s Parents vs. Research,” supra note 141.
[150] “Thimerosal in Vaccines,” supra note 139; see also “On Autism’s Cause, It’s Parents vs. Research,” supra note 141 (“[b]y 2001, no vaccine routinely administered to children in the United States had more than half a microgram of mercury – about what is found in an infant’s daily supply of breast milk”).
[151] “Autism and Vaccines: Activists Wage a Nasty Campaign to Silence Scientists,” Wall Street Journal editorial, February 16, 2004, at http://www.opinionjournal.com/forms/printThis.html?id=110004700 (last visited April 27, 2006).
[152] “On Autism’s Cause, It’s Parents vs. Research,” supra note 141.
[153] Indeed, one recent study has suggested that neurological disorders have decreased with the removal of thimerosal from most vaccines. See David A. Geier and Mark R. Geier, “Early Downward Trends in Neurodevelopmental Disorders Following Removal of Thimerosal-Containing Vaccines,” 11 J. Am. Physicians and Surgeons 8 (2006). This study should be taken with a grain of salt, however, as the Geiers are widely known thimerosal critics. Years before this study, Dr. Mark Geier called thimerosal use in vaccines the world’s “greatest catastrophe that’s ever happened, regardless of cause.” “On Autism’s Cause, It’s Parents vs. Research,” supra note 141. A witness in many vaccine cases, a judge once ruled that he was “a professional witness in areas for which he has no training, expertise and experience.” Id. Scientists have criticized his prior studies and even called his methods “voodoo science.” Id.
[155] See id.
[156] See “The Politics of Autism: Lawsuits and Emotion vs. Science and Childhood Vaccines,” Wall Street Journal editorial, Dec. 29, 2003, at http://www.opinionjournal.com/forms/printThis.html?id=110004487 (last visited April 27, 2006) (characterizing the position of thimerosal critics as “scientifically untenable”).
[157] See generally “On Autism’s Cause, It’s Parents vs. Research,” supra note 141.
[161] “The Politics of Autism,” supra note 156.
[162] Id. ; “Study: Autism Rise from Labeling, Not Epidemic,” April 3, 2006, at http://www.cnn.com/2006/EDUCATION/04/03/health.autism.reut/index.html (last visited April 27, 2006) (noting rise in diagnosed cases of autism since 1994 is correlated with fall in diagnosed cases of mental retardation and learning disabilities).
[163] The Politics of Autism,” supra note 156.
[164] See, e.g. , “Six Common Misconceptions,” supra note 10 (noting that many anti-vaccine publications claim vaccines are unsafe on the basis of sheer numbers of reports to VAERS without noting that many of them may not represent actual vaccine side-effects).
[165] National Vaccine Information Center, “The Vaccine Injury Compensation Program,” at http://www.909shot.com/Issues/Comp_Summary.htm (last visited April 27, 2006).
[166] Center for Disease Control, National Vaccine Program Office, Vaccine Fact Sheets, “National Vaccine Injury Compensation Program,” at http://www.hhs.gov/nvpo/factsheets/fs_tableIV_doc1.htm (last visited April 27, 2006).
[167] See National Vaccine Injury Compensation Program, at http://www.hrsa.gov/vaccinecompensation/ (last visited April 27, 2006).
[169] The Andy Griffith Show: The County Nurse (CBS television broadcast, March 19, 1962).
[177] Id. That is, there will be a high probability of death.
[179] See the discussion above in Part I of this paper.
[180] For example, she begs Rafe to consider his family and what his decision could mean to them. She literally appears to be on the verge of tears as he refuses.
[181] In utilizing the theoretical framework of economic analysis, it is useful to keep in mind a few foundational concepts. First, a policy or program (in this case mandatory vaccination) is desirable if the overall benefit to society as a whole outweighs the cost of the program, where benefits and costs include both monetary and non-monetary factors. Second, individuals making rational choices regarding vaccination will vaccinate when the benefits of vaccination outweigh the risks or costs of non-vaccination to the individual. This decision-making process can be skewed by externalities, such as an unforeseeable decrease in the effectiveness of a vaccine due to a reduction in vaccination by others unknown to the individual at the time of the decision.
[182] 197 U.S. 11 (1905).
[183] Id. at 12.
[185] Id. at 13, 22.
[186] Id. at 36.
[187] Id. at 12.
[188] As the CDC itself explains, “[e]ven one serious adverse effect in a million doses of vaccine cannot be justified if there is no benefit from the vaccination.” “Six Common Misconceptions,” supra note 10.
[189] In Japan in the 1970s, for instance, pertussis vaccination coverage fell from 80% to 20%, leading to an outbreak in 1979 resulting in 13,000 cases and 41 deaths. “What Would Happen If We Stopped Vaccinations?” supra note 91.
[190] Judge Richard Posner has suggested that this difference between sexually transmitted diseases and air- and water-borne diseases may imply a lesser imperative to eliminate sexually transmitted diseases:
[T]he externality created by sexually transmitted diseases is smaller than in the case of other contagious diseases. Sexually transmitted disease is spread primarily by voluntary contact, implying (to the economist) that a person is compensated...for assuming the risk of contracting the disease. Hence the number of cases of sexually transmitted diseases may be closer to the optimum than in the usual air-borne or water-borne or insect-borne epidemics.
Posner, Economic Analysis of Law 162. (6th Ed. 2003).
[191] Additionally, if vaccination rates are high, these individuals may assume that those in society who have already made the choice to vaccinate have performed a similar cost-benefit analysis. These individuals choose to vaccinate based simply on vaccination rates in the community. See John C. Hershey et al., The Roles of Altruism, Free Riding, and Bandwagoning in Vaccination Decisions , 59 Organizational Behavior and Human Processes 177, 178 (1994).
[192] See, e.g. , id. (behavioral survey studying various factors individuals use to make vaccination decisions).
[194] See id. at 178 (“[i]f a patient believes vaccination is in his own best interests, then he has two reasons to vaccinate. One is selfish, in that he will improve his own well being. The other is altruistic, in that he can improve the health prospects of those around him who might otherwise become infected if he is not vaccinated himself”).
[195] The concept of herd immunity is discussed in Part I. Note that “[i]n economic terms, herd immunity is a positive externality of vaccination. Altruistic individuals who recognize and value this externality may undergo vaccination partly to help others in addition to themselves.” Id. See also Berger, supra note 29 (“‘[h]erd immunity’...is the concept that not everybody in a population has to be immunised to protect everyone in that population. As long as a sufficient number of children are immunised against each disease for which there is a vaccine, protection against that disease will be conferred on everybody”).
[196] The CDC has pointed to this as one of the two most important reasons to vaccinate:
There is a small number of people who cannot be vaccinated (because of severe allergies to vaccine components, for example), and a small percentage of people don’t respond to vaccines. These people are susceptible to disease, and their only hope of protection is that people around them are immune and cannot pass disease along to them. A successful vaccination program, like a successful society, depends on the cooperation of every individual to ensure the good of all.
[197] In economic terms, “[w]idening vaccine use decreases each individual’s benefit from being vaccinated, but leaves unchanged each individual’s risk from the vaccination itself.” Hershey, supra note 191, at 178.
[198] “Six Common Misconceptions, supra note 10.
[199] Hershey, supra note 191, at 178.
[200] Suppose, for sake of example, that a vaccination program, if implemented, would save ten lives out of a thousand that would otherwise have perished without the program. Unfortunately, the vaccine will randomly cause death to five persons out of a thousand. From an ex ante perspective, the vaccination program should be implemented as it will save five lives overall. Concerns or complaints from those five persons who die (or their estates) represent ex post objections, and, though unfortunate, should not affect evaluations of the soundness of the program.
[201] This mathematical explanation is a slight variation of that found at CDC, “Six Common Misconceptions,” supra note __.
[202] Note that no vaccine is 100% effective, and vaccination efficacy rates for most childhood vaccinations range from 85 to 95%. Id. As stated in an earlier section, herd immunity is relied upon to protect those who do not develop full immunity from the vaccine.
[203] Given that these particular vaccines are already on the schedule, I think it would be unwise to remove them now. My analysis applies to comparable vaccines that may arise in the future – vaccines for those communicable diseases that do not pose relatively significant health risks. The definition of such diseases, of course, would be a matter of debate. Vaccines for noncommunicable diseases like ear infections would also fall within this rubric.
[204] Statement of Barbara Fisher, quoted in Ostrom, supra note 56.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 17 July 2023
Psychological profiles of anti-vaccination argument endorsement
- Dawn L. Holford ORCID: orcid.org/0000-0002-6392-3991 1 ,
- Angelo Fasce 2 ,
- Thomas H. Costello 3 &
- Stephan Lewandowsky ORCID: orcid.org/0000-0003-1655-2013 1
Scientific Reports volume 13 , Article number: 11219 ( 2023 ) Cite this article
5827 Accesses
10 Citations
31 Altmetric
Metrics details
- Health care
- Human behaviour
The proliferation of anti-vaccination arguments online can threaten immunisation programmes, including those targeting COVID-19. To effectively refute misinformed views about vaccination, communicators need to go beyond providing correct information and debunking of misconceptions, and must consider the underlying motivations of people who hold contrarian views. Drawing on a taxonomy of anti-vaccination arguments that identified 11 “attitude roots”—i.e., psychological attributes—that motivate an individual’s vaccine-hesitant attitude, we assessed whether these attitude roots were identifiable in argument endorsements and responses to psychological construct measures corresponding to the presumed attitude roots. In two UK samples (total n = 1250), we found that participants exhibited monological belief patterns in their highly correlated endorsements of anti-vaccination arguments drawn from different attitude roots, and that psychological constructs representing the attitude roots significantly predicted argument endorsement strength and vaccine hesitancy. We identified four different latent anti-vaccination profiles amongst our participants’ responses. We conclude that endorsement of anti-vaccination arguments meaningfully dovetails with attitude roots clustering around anti-scientific beliefs and partisan ideologies, but that the balance between those attitudes differs considerably between people. Communicators must be aware of those individual differences.
Similar content being viewed by others

The vaccination rift effect provides evidence that source vaccination status determines the rejection of calls to get vaccinated
J. Lukas Thürmer & Sean M. McCrea

Trust and COVID-19 vaccine hesitancy
Vincenzo Carrieri, Sophie Guthmuller & Ansgar Wübker
A taxonomy of anti-vaccination arguments from a systematic literature review and text modelling
Angelo Fasce, Philipp Schmid, … Stephan Lewandowsky
Introduction
Vaccinations are one of the most successful medical inventions for controlling and preventing deaths from infectious diseases 1 . Curiously, however, opposition to vaccines remains prevalent and therefore poses a substantial threat to global health 2 . In particular, the proliferation of anti-vaccination arguments on the Internet has curtailed the benefits of many immunisation programmes 3 , 4 —with COVID-19 vaccinations offering an especially salient recent example 5 . These arguments influence individuals’ decisions to have vaccinations. Indeed, mere exposure to online vaccine misinformation may lower vaccination intentions 6 and belief in misinformation is cross-culturally associated with lower readiness to be vaccinated against COVID-19 7 . The perpetuation of misconceptions and logical fallacies by vaccine opponents have also influenced the intentions of parents to vaccinate their children 8 , 9 .
Vaccine-hesitant individuals express arguments that can range expansively from exaggerated safety concerns, to the use of fallacious logic, to reliance on misinformation, to conspiratorial beliefs, to give some examples 10 . This can make it difficult for vaccine communicators—such as fact-checkers, healthcare professionals, and scientists—to counter the many different arguments that spread rapidly on the Internet 11 . Compounding the problem, facts and evidence to debunk flawed contrarian argumentation may not be sufficient. Opposition to vaccines that stems from social and cultural factors, rather than a failure to understand the science of vaccination, will not necessarily be satisfactorily countered with scientific evidence 12 . Certain anti-vaccination arguments also target cognitive systems that are used in intuitive judgements and motivated reasoning, which can make it harder to combat those arguments with statistics, facts, and logic 13 . Further, people may be motivated to reject scientific evidence if it is in conflict with their personal interests, worldviews, or beliefs 14 , 15 . In those cases, people may engage in motivated reasoning such that they interpret scientific findings in a manner that is compliant with their existing beliefs 16 . For example 17 , found that people evaluated information compatible with their existing attitudes about flu vaccination to be more convincing than attitude-inconsistent information.
Effective rebuttal of anti-vaccination arguments therefore requires an approach that goes beyond addressing flaws in the arguments, by also considering the underlying psychological attributes, known as “attitude roots” 18 , 19 , that drive opposition to vaccines. This means looking beyond the content of arguments to assess what motivates someone to endorse an anti-vaccination argument. Such motivations could be based on very different psychological constructs, including “fears, ideologies, worldviews, and identity needs” 18 . For instance, individuals high in conspiratorial ideation (a psychological tendency) may tend to argue that one should reject vaccinations because they are part of a secret plot to control the population by implantation of microchips embedded in the vaccines, whereas individuals who are politically libertarian (a worldview) may argue that one should reject vaccinations because they are a political tool that removes people’s freedoms (e.g., through mandates). Ultimately, the attitude roots identifiable in the expression of an argument should serve as a veneer for stable individual differences (e.g., personality, values, worldviews, or emotions) that are also related to vaccine hesitancy.
Understanding the attitude root of an individual’s resistance to vaccines may thus allow vaccine communicators to align their message with the individual’s motivation for holding their position, and avoid triggering their motivation to reject the pro-vaccination message 18 , 20 . However, identifying an attitude root is no easy task. As the terminology suggests, attitude roots lie beneath a surface expression and are not always obvious to the interlocutor. Individuals may themselves lack insight into their own motivations for endorsing a particular anti-vaccination argument 18 . Further complicating matters, even the manifestations of attitude roots can overlap. As seen in the example above, a secret plot to control the population will also remove people’s freedoms. Therefore, to better understand how to address the attitude roots of vaccine opposition, there is a need for research to investigate the manifestations of anti-vaccination sentiment (i.e., arguments) and link those manifestations to underlying psychological factors. Earlier work showed that across 24 different countries, three psychological factors (conspiratorial beliefs, disgust about blood and injections, and reactance) were associated with negative attitudes about the safety and effectiveness of children’s vaccinations, suggesting that these could be potential attitude roots to investigate as motivations to reject vaccination science 20 . More recent work 21 sought to classify a wider range of anti-vaccination arguments and map them to potential attitude roots. In this work, the authors identified 2414 anti-vaccination arguments through a PRISMA-compliant systematic review of 152 scientific publications, and classified them into a hierarchical taxonomy with 11 overarching attitude roots. This classification, initially done by qualitative thematic analysis, was validated using machine learning to classify arguments based on their linguistic expression. Trained researchers classified the attitude roots in two different datasets—the arguments obtained from the systematic literature review, and an additional dataset of 582 anti-vaccination arguments obtained from a database of fact-checked COVID-19 vaccine claims circulating on the Internet. A Natural Language Processing model trained on a subset of the data was able to predict the attitude root classifications with a high level of accuracy.
This taxonomy 21 integrated decades of prior research on the typologies of anti-vaccination arguments (e.g., 10 , 22 ). It conceptualised anti-vaccination arguments, which form the base level of the taxonomy, as an expressed proposition that opposes vaccination—i.e., the given reason for not having a vaccine. The 11 attitude roots that form its top level (see Table 1 ) reflect psychological characteristics that have been found in past research to be related to vaccine hesitancy (e.g., conspiracist beliefs 23 , 24 ).
Fasce et al.’s 21 taxonomy provided the most comprehensive framework to date of a wide range of arguments and their links to the underlying attitude roots of anti-vaccination belief—i.e., their psychological motivators. We used the taxonomy as a springboard for the present investigation of the psychological factors that motivate people’s anti-vaccination attitudes. We investigated these attitude roots in two ways. First, we sought to assess whether it would be possible to observe clusters of argument endorsement that reflect correlated levels of endorsements for anti-vaccination arguments within the same attitude root. Of course, the boundary between attitude roots may be blurred, with overlaps between those that share similarities (such as religious and moral concerns 21 ). An individual could also hold more than one attitude root, thus strengthening their motivation to endorse anti-vaccination arguments 19 . Indeed, there is evidence from research into conspiracist beliefs that individuals may form monological belief systems, where belief in one conspiracy theory supports belief in others 25 , 26 .
Our second goal was to determine if argument endorsements were associated with specific psychological characteristics that were identified as individual difference measures for the attitude roots. Here, we expected that if attitude roots were discernible among argument endorsements, those clusters of argument endorsements would relate to a specific psychological determinant of vaccine hesitancy. That is, a set of different arguments that invoke conspiracies should be preferentially endorsed by people who tend to view the world through a conspiratorial lens, whereas arguments that emerge from a libertarian lens should be preferentially endorsed by free-market advocates, and so on. However, as many of these psychological constructs may themselves be intercorrelated 15 , 24 , 27 , 28 , this could hinder the ability to discern specific associations of one psychological construct with its expected argument endorsements. Nonetheless, each psychological construct should at minimum be associated with argument endorsement strength.
Factor structure of argument endorsements
We first analysed the internal structure of participants’ endorsement of the anti-vaccination arguments (66 in Sample 1, 33 in Sample 2). We started exploring both datasets through Exploratory Factor Analysis (EFA) with maximum likelihood estimation and promax rotation. In the first sample, parallel analysis suggested to retain 3 factors. However, the 3-factor solution displayed numerous cross-loadings and the factors were not interpretable from a theoretical point of view, which suggested that the 1-factor solution, which displayed acceptable item loadings in all cases ( \(> 0.34\) ), would be preferable. In the second sample, a parallel analysis suggested a 2-factor solution, with religious concerns grouped into a separate factor. As in Sample 1, a 1-factor EFA solution was viable, with all loadings \(> 0.36\) .
We then used pre-registered Confirmatory Factor Analyses (CFA) to evaluate 3 models compatible with the taxonomy of anti-vaccination arguments 21 : a 1-factor model, an 11-factor model in which all the attitude roots were represented as different latent variables, and a 7-factor model in which 4 pairs of thematically related attitude roots were collapsed into combined factors: (1) conspiracist ideation and distrust, (2) religious and moral concerns, (3) fear and phobias and distorted risk perception, and (4) perceived self-interest and reactance. Parameters were estimated by maximum likelihood method, which allows the calculation of the commonly used criteria for acceptable goodness-of-fit: Comparative Fit Index (CFI) and Tucker-Lewis Index (TLI) close to 0.90 or above, Root Mean Square Error of Approximation (RMSEA) close to 0.08 or below, and Standardised Root Mean Square Residual (SRMR) close to 0.05 or below 29 . The 7-factor and 11-factor models were not acceptable due to poor fit indices in both samples and because they implied mathematically impossible variance-covariance matrices. We theorise that this is attributable to extremely high correlations among items that were designed to measure distinct roots. We also explored statistical approaches that are more tolerant under conditions of substantial intercorrelation between latent variables, such as confirmatory bi-factor models or exploratory structural equation modeling, and those were also found to be unsatisfactory. The 1-factor model was unproblematic in both samples. The results are displayed in Table 2 . Sample 1 uses all 66 items, whereas Sample 2 uses the substantially narrowed item pool described above. Our results confirm the notion that people who are opposing vaccinations will tend to endorse any and all anti-vaccination arguments within the taxonomy.
Associations of anti-vaccination argument endorsement
Following our pre-registered hypotheses, we next examined the relationship between argument endorsements and the assays of the attitude roots. As shown in Table 3 , 11 out of 13 of the measured psychological constructs in Sample 2 were significantly correlated in the expected direction with argument endorsements drawn from the target attitude root. The constructs were also associated with total endorsements of all the arguments, is in line with the unidimensional structured revealed by the factor analyses. These correlations remained significant, with similar effect sizes, when controlling for age, gender, education, and political orientation (see Supplementary Information, Table S4 ). We interpret these results as partial support for our hypotheses. Although we found 11 of the 13 hypothesised correlations, these associations are not exclusive to the target attitude, but rather extend to the rest of attitude roots, which, again, suggests a monological belief system among those who endorse anti-vaccinations arguments.
Two exceptions, Trait Fear and Prosocial Behavioural Intentions, did not correlate significantly with argument endorsements from the target attitude root—and Prosocial Behavioural Intentions did not correlate at all with overall argument endorsements. However, these constructs were also not significantly associated with their related dimensions of the 5C scale—confidence ( r = − 0.02) and collective responsibility ( r = − 0.03), respectively. By contrast, all other psychological constructs were significantly correlated to the 5C measures, indicating that these were predictive of the vaccine hesitancy determinants. We are inclined to attribute this lack of association for the two exceptions to the scales used to measure Trait Fear and Prosocial Behavioural Intentions, which may be too general and, consequently, do not reflect the specific psychological processes related to healthcare or vaccination.
In addition, average argument endorsement correlated positively with the 5C subscales Constraints, Complacency, Calculation, Collective, as well as negatively with the Confidence subscale 30 , as shown at the bottom of Table 3 . Greater endorsement of the arguments therefore indicated greater vaccine hesitancy. We also found in exploratory hierarchical linear regressions (available in Supplementary Information, Table S5 ) that argument endorsements had incremental validity in predicting the psychological constructs, over and above the 5C items.
We also observed that the psychological constructs were significantly correlated with each other, albeit to a lesser extent than the argument endorsements (correlation coefficients among the psychological constructs can be found in Supplementary Information, Table S6 ). This prompted us to further examine how the psychological constructs might overlap among individuals through an exploratory analysis of psychological profiles at the participant level.
We next used Latent Profile Analysis (LPA) to identify different profiles of participants in Sample 2 ( n = 590) based on their responses to the psychological constructs. LPA is a variant of latent class analysis that allows the use of continuous variables. LPA is a person-centered analytic tool that offers a classification of each participant in the most probable profile based on a set of observable variables, rather than classifying the variables 31 . A range of indices determine the most appropriate number of latent profiles: Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), sample-size adjusted BIC (SABIC), and a measure of entropy. Lower values for AIC, BIC, and SABIC indicate greater fit. For entropy, values above 0.80 denote reliable separation of profiles.
We included in the LPA the 11 psychological constructs that were associated with argument endorsements at p < 0.001 (see Table 3 ). To distinguish between pro-vaccination and anti-vaccination profiles, we included the average of participants’ endorsements for all arguments to classify their overall vaccination attitude. We additionally included Political Orientation as it was positively associated with argument endorsement ( r = 0.16, \(\textit{p} < 0.001\) ). Table 4 shows the fit indices of models with 1–10 profiles. We selected the 8-profile model, which exhibited the lowest BIC and a high entropy. We used the scores of each profile in endorsement of anti-vaccination arguments to define their respective attitude toward vaccinations (i.e., if they were below or above the mean). Four profiles were characterised as pro-vaccination and four as anti-vaccination (see Fig. 1 ).
Two of the identified profiles (“unspecified” pro- and anti-vaccination) did not show any distinctive association and exhibited moderate levels of pro- and anti-vaccination attitudes. The remaining six profiles had distinctive and consistent patterns. Among the anti-vaccination profiles, we found an “alternative epistemology” profile characterised by a combination of anti-scientific beliefs and epistemology, with this group being particularly prone to endorsing anti-vaccination arguments. A second “social conservatism” profile was characterised by high religiosity, moral rigidity, and traditionalism. The last, “free-market ideology”, anti-vaccination profile was predominantly characterised by its strong endorsement of this ideology. In contrast, among the pro-vaccination profiles we found a “critical thinking and leftism” profile characterised by its opposition to anti-scientific beliefs, alternative epistemology, and conservatism, and this profile appeared especially resistant to anti-vaccine arguments. The second “conservatism” profile was characterised by moderate conservative ideology and lower General Reactance and Alternative Epistemology than their anti-vaccination counterparts—which suggests an ideological profile less susceptible to politically motivated reasoning. The final pro-vaccination profile was characterised by its religiosity—which is in line with the context-dependent relationship between religiosity and vaccine hesitancy 32 .
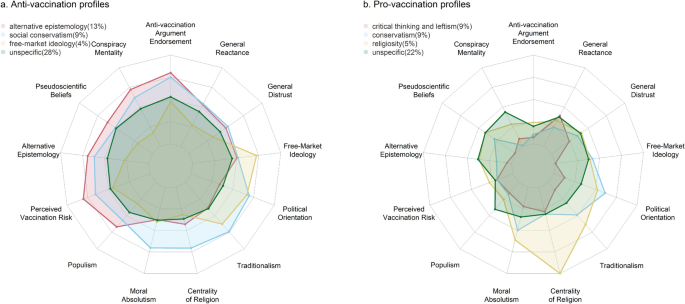
Anti- and pro-vaccination profiles identified in a latent profile analysis using 13 psychological constructs associated with endorsement of anti-vaccination arguments.
We investigated the psychological factors, or “attitude roots”, motivating contrarian views regarding vaccines and the endorsement of these arguments. We selected attitude roots based on a taxonomy of anti-vaccination arguments 21 , and operationalised them in two ways. First, we selected a group of prototypical anti-vaccination arguments to represent themes from each attitude root in the original taxonomy. Second, we selected psychological construct measures that were conceptually aligned with the attitude roots. The analyses of these two different attitude root representations give rise to a complex overall picture of how people may sustain anti-vaccination attitudes. Individuals who scored higher on the psychological antecedents of vaccine hesitancy and the psychological construct representations of the attitude roots endorsed all arguments against vaccines more strongly. These individuals further clustered into four identifiable “profiles” based on the psychological constructs.
In two UK samples totalling 1250 responses, we found that endorsements of arguments selected to represented distinct attitude roots were so correlated that it constrained our ability to fit the proposed 11-factor structure model. We were thus unable to confirm any preferential endorsement patterns among arguments representing different attitude roots. This finding may seem at odds with previous work that was able to classify documented arguments that people had put forth against vaccination, where a computational model trained on scholarly analysis of the arguments could successfully predict the attitude roots of new arguments from a different domain 21 . However, it is important to distinguish endorsement of arguments that one may encounter from the expression of arguments that one may produce. When presented with an arguments against vaccines, an individual who is strongly negative about vaccination may strongly endorse any argument simply because it is consistent with their attitude. This tendency to endorse arguments that support one’s existing perspective has been documented in a family of cognitive biases, such as “belief bias” and “myside bias”, where people evaluate evidence and accept conclusions in a manner that is biased towards their prior opinions and attitudes 33 . Reasoning research in particular has shown that attitude-consistent conclusions are believed more than attitude-inconsistent ones, especially when these conclusions relate to ideological and political issues (e.g., 34 , 35 , 36 ). For example, participants’ prior attitudes towards abortion impeded their ability to discern flawed reasoning when the conclusions supported their abortion position 36 . People also tend to endorse otherwise identical information more if it supports one’s political beliefs rather than challenges them 37 . In extreme circumstances, endorsing one argument can even act as support for the endorsement of others towards the same conclusion, forming a monological belief system that is commonly seen within conspiracist ideation 26 . Indeed, beliefs in distinct conspiracy theories correlate highly with one another, even when those theories are contradictory or fictitious 25 , 38 , 39 , 40 . The motivations for one’s anti-vaccination attitude may thus be captured by one (or several) arguments that one might personally express, but endorsing other attitude-consistent arguments can serve to support, and perhaps strengthen, one’s overall position.
The motivations for endorsing anti-vaccination arguments may instead need to be captured by other measures. We included psychological construct measures in Sample 2 to assess the associations of these assays of the attitude root to argument endorsements. With the exception of trait fear and prosociality (which also did not predict the relevant 5C vaccine hesitancy determinant), each psychological construct was not only associated with argument endorsements from the target attitude root, but also argument endorsements from other attitude roots. In other words, there was an overall tendency for those with high levels of those psychological factors to give stronger endorsements of anti-vaccination arguments in general. The effect sizes of the significant correlations varied from r = 0.14–0.68, so some of these correlations were only weak ones. However, these correlational effect sizes, and their directions, generally match with those found in previous research regarding the relationship of the psychological constructs to other vaccine hesitancy measures 19 , 20 , 23 , 41 , 42 , 43 , 44 , 45 . It is important to clarify that our study related the psychological assays for the attitude root to both argument endorsement strength and vaccine hesitancy determinants (measured by the 5C scale 30 ), as vaccine hesitancy has historically been ambiguously defined, with researchers conceptualising the term in varying ways, from cognition and affect to decisions and behaviour 46 . Our findings thus link this comprehensive set of psychological constructs to their role in motivating cognition about vaccines, which themselves predict previously-validated behavioural determinants of vaccine hesitancy. Where a psychological construct predicted vaccine hesitancy in the literature, it also predicted argument endorsement to a similar extent. In both cases, some of these correlations were weak, which may reflect a difficulty in selecting the right measures to capture the latent psychological variables. More likely, it indicates that people can possess various overlapping motivations, each of which contribute in part to their attitudes and endorsements.
It was difficult to determine unique contributions of attitude roots to anti-vaccination argument endorsement strength. We had expected some level of clustering, where certain attitude roots should be more strongly associated than others, which was captured by the 7-root model that collapsed these attitude roots. For example, conspiracist ideation, which is characterised by a high level of distrust in the “official” narrative 47 ), should be strongly associated with distrust, even if it is distinct in that not all distrust in vaccination involves a belief in a conspiracy theory. We observed not just these expected clusters, but also a more complex pattern of inter-correlations among all the psychological constructs. To some extent, this is supported by past research—for example, conspiracist mentality is correlated with right-wing social conservatism 27 , free-market ideology 15 , distrust of official information sources 24 , and paranormal and pseudoscientific beliefs 28 . However, our study is the first to systematically investigate this many potential attitude roots and assess their overlap.
Making the case for potential overlap among attitude roots 18 , proposed that multiple roots could sustain an individuals’ attitudes and “in combination they could be more powerful than if one were to operate individually.” Our latent profile analysis provided some evidence for this proposal, as we were able to identify four distinct clusters of participants in Sample 2 who tended to endorse anti-vaccination arguments. These profiles were primarily characterised by various elements of anti-science beliefs and ideological partisanship. We consider below how the psychological clusters we found could be targeted for vaccine communication interventions, which future research may wish to build on.
One profile that displayed average scores across all constructs and less strong argument endorsements suggested that this might be an “on-the-fence” group who could be more amenable to informational interventions such as prebunking and debunking 48 . Because no one psychological construct distinguishes this group, it may be worth considering broader spectrum interventions that do not target specific misinformation content but warn against strategies marking out misinformation 49 . Techniques such as Motivational Interviewing may also be useful, as it encourages healthcare professionals engaging with patients who are uncertain about a certain behaviour (including vaccination) to explore their motivations for it and guide patients towards acceptance 50 .
Conversely, the psychological profile with the strongest total endorsement of anti-vaccination arguments and perception of vaccination risks encompassed individuals who may seek to justify their hesitancy through a combination of anti-scientific doctrines (i.e., conspiracy and pseudoscientific theories) and an alternative epistemology that undermines normative epistemological principles such as the primacy of scientific evidence. These attitude roots may also reinforce one another inasmuch as a relativistic epistemology facilitates the adoption and promotion of anti-scientific conceptions 51 . This group would be highly likely to resist correction that are based on a shared acceptance of facts and evidence. Communication with this group would gain most from first establishing a common ground for further discussion before attempting to correct any misconceptions. Consider, for instance, an individual who holds strong beliefs about the effectiveness of alternative medicinal products. Rather than arguing that there is insufficient evidence for alternative medicine and overwhelming evidence for vaccination, it may be more productive to acknowledge that one can reap benefits from different types of therapies—but these are in addition to rather than instead of vaccination.
The final profiles were characterised by high levels of social conservatism, with the smaller of these profiles distinguished by an additional stronger belief in free-market ideology—reflecting a divergence in conservative ideology on social and economic issues 52 , 53 . A vaccine communication strategy for these groups could focus on how vaccination is not at odds with their belief systems. For example, information and corrections will likely be trusted more and seen as compatible with beliefs if they come from authoritative sources within one’s religion, tradition, or community group 54 . Identifying benefits that align with existing worldviews may also be important, for example, positioning vaccination as an individual choice to gain its protective benefits for oneself (as opposed to benefiting society) would be in line with a neoliberal ideology that prizes individualism and deregulation 55 .
Our research also has a few limitations that future research may also wish to address. As a correlational study, although it is reasonable to posit that psychological factors drive anti-vaccination belief, our study design does not allow us to draw such a causal conclusions from the observed significant associations. We also focused on soliciting endorsements of arguments from different roots rather than having participants express reasons for rejecting vaccinations. While this method was necessary to allow us to determine the factor structure of the endorsements and their correlations with the psychological constructs, it could be good for future research to investigate if the psychological constructs are related to the types of arguments people might choose to express against vaccination.
We are also cautious about the generalisability of the psychological profiles in our UK sample, and recommend that future research address whether these profiles are present in other countries and cultures. The associations between some of the psychological constructs and vaccine hesitancy may differ, for example, reactance was previously found to predict anti-vaccination attitudes in the UK ( r = 0.33) but not in Japan ( r = 0.09) 20 . Specifically, associations around worldview and politics will likely be sensitive to different cultural contexts, as the relationship between social and economic conservatism is characteristic of developed countries 56 , 57 .
In sum, our work contributes data covering a comprehensive set of psychological factors associated with vaccine hesitancy, and, specifically, its cognitive manifestation as endorsements of anti-vaccination arguments. We found that these endorsements exhibit a monological response pattern, with high inter-correlations, but the psychological factors that predicted argument endorsement strength clustered into distinct psychological profiles. These indicate that two key motivators of anti-vaccination belief relate to anti-scientific conceptions and political polarisation, which may require different communication strategies to tackle.
Before data collection, the study was approved by the University of Bristol School of Psychological Science Research Ethics Committee (references: 10309 and 10708) and the study methods and planned analyses were pre-registered. The pre-registration, study materials, data, and analysis scripts to derive our reported results are shared on the Open Science Framework: https://osf.io/27f5u/ . All study methods were performed in accordance with the relevant guidelines and regulations approved by the Research Ethics Committee. Informed consent was obtained from all participants prior to their participation in the study.
Participants
We recruited 1250 participants (Sample 1: n = 660; Sample 2: n = 590) from the UK via Prolific, who were paid at a rate of \(\pounds\) 9/h. We determined sample sizes based on a recommended ratio for performing factor analyses of at least 10 participants per measured anti-vaccination argument 58 . For Sample 1, we pre-selected participants who had stated they either felt negatively or neutral towards the COVID-19 vaccine in a Prolific screening question. This was to ensure we would have enough participants who would endorse the anti-vaccination arguments to enable a factor analysis. For Sample 2, we did not apply this pre-selection filter because we aimed to assess a wider range of attitudes and psychological characteristics that would enable the correlational analyses and allow us to build profiles of individuals with pro- and anti-vaccination views. This also meant that Sample 2 should be less prone to monological thinking than Sample 1. In both cases, we obtained a balanced distribution of gender and political leanings.
At the end of each data gathering process, participants provided demographic information. Participants in Sample 1 were 50% male, 49% female (1% did not identify with either gender), with ages ranging between 18-84 years ( M = 38.36, SD = 12.13). Participants in Sample 2 were 49% male, 51% female, with ages ranging between 18–85 years ( M = 43.10, SD = 14.12). In both samples, 48% had at least a Bachelor’s degree, and there was a normal distribution across political leanings on an 11-point scale representing the left-right political spectrum 27 , 59 (Sample 1: M = 5.74, SD = 2.33, skewness = 0.06, kurtosis = − 0.37; Sample 2: M = 5.83, SD = 2.40, skewness < 0.01, kurtosis = − 0.62).
Anti-vaccination arguments
We assessed participants’ endorsements of anti-vaccination arguments using a methodology similar to that used in research investigating conspiracist beliefs (e.g., 60 . Participants endorsed arguments by indicating how much they agreed with each argument on a 7-point Likert scale (1: strongly disagree, 7: strongly agree). All arguments and their mean endorsement ratings in our two samples are available in Supplementary Information (Table S2 ).
In the first sample, participants rated their endorsement of 66 prototype anti-vaccination arguments that were spread evenly across the 11 attitude roots. All but four of the arguments were prototypical arguments identified in Fasce et al.’s 21 taxonomy. The remaining four were created for the purposes of this study to ensure no root had disproportionately fewer arguments for analysis than the others. The levels of skewness and kurtosis of most of the arguments assessed in Sample 1 were within the usual thresholds for a normal distribution (+ 2/− 2). Only three arguments (the second and fourth of religious concerns, and the second of reactance) exhibited a kurtosis slightly above the threshold (2.71, 2.12, and 2.47, respectively). These 66 arguments showed high internal consistency ( \(\alpha\) of the six arguments within each attitude root ranged from 0.67 to 0.91; total \(\alpha\) = 0.98).
We used a 11 exploratory bi-factor latent variable models (i.e., with the Schmid-Leiman transformation 61 ) of each set of argument endorsements in Sample 1 to identify arguments most diagnostic for their attitude root to use in Sample 2. Specifically, we selected the three arguments for each attitude root that were most saturated with the general factor. Explained Common Variance of the general factors ranged from .43 (moral concerns) to .86 (epistemic relativism), with a median of .74, suggesting that most target roots were relatively unidimensional. The three items with general factor loadings > .60 for each target root were retained for Sample 2, resulting in 33 anti-vaccination arguments (the list of selected arguments and their respective mean endorsements can be found in the Supplementary Information, Table S2 ). This shortened the overall questionnaire while maintaining a minimum of three items per attitude root required for a confirmatory factor analysis on these data. Participants in Sample 2 rated their endorsement of these 33 arguments. The parameters of skewness and kurtosis of almost all the 33 anti-vaccination arguments included in the second sample were within the thresholds of normality, except for the second and fourth arguments of religious concerns, which showed higher levels of kurtosis (3.55 and 2.17, respectively). The total \(\alpha\) of the 33 anti-vaccination arguments was 0.98, with the internal consistency of the attitude roots ranging from 0.75 to 0.91. We found very similar patterns of argument endorsement between the two samples, indicating that the three items per root chosen for the second sample remained representative of that root.
Psychological constructs
In Sample 2, we also collected data on participants’ responses to 13 previously validated measures of psychological constructs that were selected as independent assays of the 11 attitude roots. Participants also responded to the short version 5C scale 30 , which composes five items for each of its dimensions, to be used independently: Confidence, Constraints, Complacency, Calculation, and Collective (responsibility). This gave us a general measure of the psychological antecedents of vaccination behaviour and, consequently, vaccine hesitancy, which provided further validation that the argument endorsements were associated with vaccine hesitancy (see Table 3 ). We summarise the psychological construct measures here, with relevant statistics in the Supplementary Information (Table S3 ).
Conspiracy Mentality . Conspiracy Mentality Questionnaire 62 , five items measuring generic conspiracy beliefs.
General distrust . (Dis)trust Scale 63 ’s, eight items measuring general trust towards other people (reverse coded for distrust).
Pseudoscientific beliefs . Short-form Pseudoscientific Belief Scale 28 , eight items measuring general unwarranted beliefs falsely presented as scientific.
Free market ideology . Free-market Endorsement Scale 15 , five items measuring economic conservatism through the promotion of laissez-faire capitalism and private enterprise.
Traditionalism . Four items from the conventionalism factor of the Aggression-Submission-Conventionalism Scale 64 that express traditionalism (as opposed to respect for social norms).
Populism . Three items with the highest factor loading on the Populist Attitudes Scale 65 , defined as a political attitude with three core features: sovereignty of “the people”, opposition to the elite, and the Manichean division between “good” people and “evil” elites.
Centrality of religion . Centrality of Religion Scale 66 , five items measuring salience of religious meanings in personality.
Moral absolutism . Moral Absolutism Scale 67 , six items measuring desire for certainty in the moral domain. An additional measure of moral exporting was discarded due to poor internal consistency.
Trait fear . Six items with factor loadings> 0.70 from the Trait Fear Scale 68 , measuring self-reported variations in fear and fearlessness.
Perceived vaccination risk . Following 30 , we asked participants to rate the risk of four diseases (Covid-19, influenza, measles, and HPV) and the risk of their respective vaccines. To calculate the likelihood and magnitude of perceived risk of vaccination in comparison to that of vaccine-preventable diseases, we subtracted the risk of vaccines scores from the risk of disease scores.
Prosocial behavioral intentions . Prosocial Behavioral Intentions Scale 69 , four items measuring participants’ general prosociality in common situations.
Alternative epistemology . Epistemic Beliefs Scale 51 , 12 items with 3 sub-factors measuring epistemic beliefs. The first factor measures reliance on intuition for factual beliefs, the second reflects conviction that facts are politically constructed, and the third measures importance of consistency between empirical evidence and beliefs. The third factor was reversed to denote rejection of evidence and, subsequently, calculate a total score in alternative epistemology.
General reactance . A condensed version of the Hong Psychological Reactance Scale 70 used in 20 , with five items measuring motivation to reject consensus views as part of a nonconformist identity.
To assess the convergent and discriminant validity of the argument endorsements in relation to their associated psychological constructs, we pre-registered the following predictions based on previous findings on anti-vaccination arguments and vaccine hesitancy:
Endorsement of conspiracist ideation arguments would be positively correlated with Conspiracy Mentality (correlation coefficients ranging from 0.14 to 0.52 15 , 20 , 23 , 24 , 71 ).
Endorsement of distrust arguments would be positively correlated with General Distrust (correlation coefficients ranging from 0.20 to 0.58 19 , 24 , 72 ).
Endorsement of unwarranted belief arguments would be positively correlated with Pseudoscientific Beliefs (correlation coefficients ranging from 0.24 to 0.50 24 , 41 ).
Endorsement of worldview and politics arguments would be positively correlated with Free Market Ideology (correlation coefficients ranging from 0.22 to 0.24 41 , 42 ), Traditionalism (correlation coefficients ranging from 0.14 to 0.38 20 ), and Populism (correlation coefficients ranging from 0.72 to 0.79 43 ).
Endorsement of religious concern arguments would be positively correlated with Centrality of Religion ( r = 0.18 42 ).
Endorsement of moral concern arguments would be positively correlated with Moral Absolutism (no correlation coefficient previously reported 44 , 73 ).
Endorsement of fear and phobia arguments would be positively correlated with Trait Fear (correlation coefficients ranging from 0.09 to 0.50 20 , 74 , 75 ).
Endorsement of distorted risk perception arguments would be positively correlated with Perceived Vaccination Risk (correlation coefficients ranging from 0.11 to 0.86 30 ).
Endorsement of perceived self-interest arguments would be negatively correlated with Prosocial Behavioral Intentions (no correlation coefficient previously reported 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 ).
Endorsement of epistemic relativism arguments would be positively correlated with Alternative Epistemology (correlation coefficients ranging from 0.17 to 0.20 45 , 84 , 85 ).
Endorsement of reactance arguments would be positively correlated with General Reactance (correlation coefficients ranging from 0.14 to 0.47 20 , 24 ).
Data availibility
All datasets used in this article are publicly available at https://osf.io/27f5u/ .
Code availibility
All source code used in this article is publicly available at https://osf.io/27f5u/ .
Greenwood, B. The contribution of vaccination to global health: Past, present and future. Philos. Trans. R. Soc. B Biol. Sci. https://doi.org/10.1098/RSTB.2013.0433 (2014).
Article Google Scholar
World Health Organization. Ten threats to global health in 2019 (2019).
Wilson, R. J. I., Vergélys, C., Ward, J., Peretti-Watel, P. & Verger, P. Vaccine hesitancy among general practitioners in southern France and their reluctant trust in the health authorities. Int. J. Qual. Stud. Health Well-being 15 , 1757336. https://doi.org/10.1080/17482631.2020.1757336 (2020).
Article PubMed PubMed Central Google Scholar
Garett, R. & Young, S. D. Online misinformation and vaccine hesitancy. Transl. Behav. Med. 11 , 2194–2199. https://doi.org/10.1093/TBM/IBAB128 (2021).
Pierri, F. et al. Online misinformation is linked to early COVID-19 vaccination hesitancy and refusal. Sci. Rep. 12 , 1–7. https://doi.org/10.1038/s41598-022-10070-w (2022).
Article CAS Google Scholar
Loomba, S., de Figueiredo, A., Piatek, S. J., de Graaf, K. & Larson, H. J. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat. Hum. Behav. 5 , 337–348. https://doi.org/10.1038/s41562-021-01056-1 (2021).
Article PubMed Google Scholar
Roozenbeek, J. et al. Susceptibility to misinformation about COVID-19 around the world. R. Soc. Open Sci. 7 , 20119. https://doi.org/10.1098/RSOS.201199 (2020).
Bradshaw, A. S. et al. Propagandizing anti-vaccination: Analysis of vaccines revealed documentary series. Vaccine 38 , 2058–2069. https://doi.org/10.1016/J.VACCINE.2019.12.027 (2020).
Bradshaw, A. S., Shelton, S. S., Wollney, E., Treise, D. & Auguste, K. Pro-vaxxers get out: Anti-vaccination advocates influence undecided first-time, pregnant, and new mothers on facebook. Health Commun. 36 , 693–702. https://doi.org/10.1080/10410236.2020.1712037 (2021).
Hughes, B. et al. Development of a codebook of online anti-vaccination rhetoric to manage COVID-19 vaccine misinformation. Int. J. Environ. Res. Public Health 18 , 7556. https://doi.org/10.3390/ijerph18147556 (2021).
Article CAS PubMed PubMed Central Google Scholar
Johnson, N. F. et al. The online competition between pro- and anti-vaccination views. Nature 582 , 230–233. https://doi.org/10.1038/s41586-020-2281-1 (2020).
Article CAS PubMed ADS Google Scholar
Lander, D. & Ragusa, A. T. ‘A rational solution to a different problem’; understanding the verisimilitude of anti-vaccination communication. Commun. Res. Pract. 7 , 89–105. https://doi.org/10.1080/22041451.2020.1816022 (2020).
Okuhara, T., Ishikawa, H., Okada, H., Ueno, H. & Kiuchi, T. Dual-process theories to counter the anti-vaccination movement. Prev. Med. Rep. 20 , 101205. https://doi.org/10.1016/J.PMEDR.2020.101205 (2020).
Lewandowsky, S. & Oberauer, K. Motivated rejection of science. Curr. Dir. Psychol. Sci. 25 , 217–222. https://doi.org/10.1177/0963721416654436 (2016).
Lewandowsky, S., Gignac, G. E. & Oberauer, K. The role of conspiracist ideation and worldviews in predicting rejection of science. PLoS ONE 8 , e75637 (2013).
Article CAS PubMed PubMed Central ADS Google Scholar
Kunda, Z. The case for motivated reasoning. Psychol. Bull. 108 , 480–498. https://doi.org/10.1037/0033-2909.108.3.480 (1990).
Article CAS PubMed Google Scholar
Giese, H., Neth, H., MoussaÏd, M., Betsch, C. & Gaissmaier, W. The echo in flu-vaccination echo chambers: Selective attention trumps social influence. Vaccine 38 , 2070–2076. https://doi.org/10.1016/j.vaccine.2019.11.038 (2020).
Hornsey, M. J. & Fielding, K. S. Attitude roots and Jiu Jitsu persuasion: Understanding and overcoming the motivated rejection of science. Am. Psychol. 72 , 459–473. https://doi.org/10.1037/a0040437 (2017).
Hornsey, M. J. Why facts are not enough: Understanding and managing the motivated rejection of science. Curr. Dir. Psychol. Sci. 29 , 583–591. https://doi.org/10.1177/0963721420969364 (2020).
Hornsey, M. J., Harris, E. A. & Fielding, K. S. Relationships among conspiratorial beliefs, conservatism and climate scepticism across nations. Nat. Clim. Change 8 , 614–620. https://doi.org/10.1038/s41558-018-0157-2 (2018).
Article ADS Google Scholar
Fasce, A. et al. A taxonomy of anti-vaccination arguments: Systematic literature review and text modeling. Nature Human Behaviour . https://doi.org/10.1038/s41562-023-01644-3 (2023).
Kata, A. Anti-vaccine activists, web 2.0, and the postmodern paradigm—An overview of tactics and tropes used online by the anti-vaccination movement. Vaccine 30 , 3778–3789. https://doi.org/10.1016/j.vaccine.2011.11.112 (2012).
Goldberg, Z. J. & Richey, S. Anti-vaccination beliefs and unrelated conspiracy theories. World Affairs 183 , 105–124. https://doi.org/10.1177/0043820020920554 (2020).
Soveri, A., Karlsson, L. C., Antfolk, J., Lindfelt, M. & Lewandowsky, S. Unwillingness to engage in behaviors that protect against COVID-19: The role of conspiracy beliefs, trust, and endorsement of complementary and alternative medicine. BMC Public Health 21 , 1–12. https://doi.org/10.1186/S12889-021-10643-W/FIGURES/2 (2021).
Swami, V. et al. Conspiracist ideation in Britain and Austria: Evidence of a monological belief system and associations between individual psychological differences and real-world and fictitious conspiracy theories. Br. J. Psychol. (London, England : 1953) 102 , 443–463. https://doi.org/10.1111/J.2044-8295.2010.02004.X (2011).
Goertzel, T. Belief in conspiracy theories. Polit. Psychol. 15 , 731–742. https://doi.org/10.2307/3791630 (1994).
Imhoff, R. et al. Conspiracy mentality and political orientation across 26 countries. Nat. Hum. Behav. 6 , 392–403. https://doi.org/10.1038/s41562-021-01258-7 (2022).
Fasce, A., Avendaño, D. & Adrián-Ventura, J. Revised and short versions of the pseudoscientific belief scale. Appl. Cogn. Psychol. 35 , 828–832. https://doi.org/10.1002/acp.3811 (2021).
Schumacker, R. E. & Lomax, R. G. A Beginner’s Guide to Structural Equation Modeling 5th edn. (Routledge, 2022).
MATH Google Scholar
Betsch, C. et al. Beyond confidence: Development of a measure assessing the 5c psychological antecedents of vaccination. PLoS ONE 13 , e0208601 (2018).
Berlin, K. S., Williams, N. A. & Parra, G. R. An introduction to latent variable mixture modeling (part 1): Overview and cross-sectional latent class and latent profile analyses. J. Pediatr. Psychol. 39 , 174–187. https://doi.org/10.1093/JPEPSY/JST084 (2014).
Eriksson, K. & Vartanova, I. Vaccine confidence is higher in more religious countries. Hum. Vaccines Immunother. 18 , 1–3. https://doi.org/10.1080/21645515.2021.1883389 (2022).
Stanovich, K. E., West, R. F. & Toplak, M. E. Myside bias, rational thinking, and intelligence. Curr. Dir. Psychol. Sci. 22 , 259–264. https://doi.org/10.1177/0963721413480174 (2013).
Aspernäs, J., Erlandsson, A. & Nilsson, A. Motivated formal reasoning: Ideological belief bias in syllogistic reasoning across diverse political issues. Think. Reason. https://doi.org/10.1080/13546783.2022.2038268 (2022).
Calvillo, D. P., Swan, A. B. & Rutchick, A. M. Ideological belief bias with political syllogisms. Think. Reason. 26 , 291–310. https://doi.org/10.1080/13546783.2019.1688188 (2019).
Čavojová, V., Šrol, J. & Adamus, M. My point is valid, yours is not: Myside bias in reasoning about abortion. J. Cogn. Psychol. 30 , 656–669. https://doi.org/10.1080/20445911.2018.1518961 (2018).
Ditto, P. H. et al. At least bias is bipartisan: A meta-analytic comparison of partisan bias in liberals and conservatives. Perspect. Psychol. Sci. 14 , 273–291. https://doi.org/10.1177/1745691617746796/ASSET/IMAGES/LARGE/10.1177_1745691617746796-FIG1.JPEG (2019).
Miller, J. M. Do COVID-19 conspiracy theory beliefs form a monological belief system? Canadian Journal of Political Science. Revue Canadienne De Science Politique 53 , 1. https://doi.org/10.1017/S0008423920000517 (2020).
Imhoff, R. & Lamberty, P. A bioweapon or a hoax? The link between distinct conspiracy beliefs about the coronavirus disease (COVID-19) outbreak and pandemic behavior. Soc. Psychol. Pers. Sci. 11 , 1110–1118. https://doi.org/10.1177/1948550620934692 (2020).
Wood, M. J., Douglas, K. M. & Sutton, R. M. Dead and alive: Beliefs in contradictory conspiracy theories. Soc. Psychol. Pers. Sci. 3 , 767–773. https://doi.org/10.1177/1948550611434786 (2012).
Lewandowsky, S., Woike, J. K. & Oberauer, K. Genesis or evolution of gender differences? Worldview-based dilemmas in the processing of scientific information. J. Cogn. https://doi.org/10.5334/JOC.99/METRICS/ (2020).
Lewandowsky, S. & Oberauer, K. Worldview-motivated rejection of science and the norms of science. Cognition 215 , 104820. https://doi.org/10.1016/J.COGNITION.2021.104820 (2021).
Kennedy, J. Populist politics and vaccine hesitancy in western Europe: An analysis of national-level data. Eur. J. Public Health 29 , 512–516. https://doi.org/10.1093/EURPUB/CKZ004 (2019).
Amin, A. B. et al. Association of moral values with vaccine hesitancy. Nat. Hum. Behav. 1 , 873–880. https://doi.org/10.1038/s41562-017-0256-5 (2017).
Schindler, J., Schindler, S. & Pfattheicher, S. The role of intuition in vaccination attitudes. J. Health Psychol. 26 , 2950–2957. https://doi.org/10.1177/1359105320925160 (2021).
Bussink-Voorend, D., Hautvast, J. L. A., Vandeberg, L., Visser, O. & Hulscher, M. E. J. L. A systematic literature review to clarify the concept of vaccine hesitancy. Nat. Hum. Behav. https://doi.org/10.1038/s41562-022-01431-6 (2022).
Pierre, J. M. Mistrust and misinformation: A two-component, socio-epistemic model of belief in conspiracy theories. J. Soc. Polit. Psychol. 8 , 617–641. https://doi.org/10.5964/JSPP.V8I2.1362 (2020).
Lewandowsky, S. & van der Linden, S. Countering misinformation and fake news through inoculation and prebunking. Eur. Rev. Soc. Psychol. https://doi.org/10.1080/10463283.2021.1876983 (2021).
Roozenbeek, J., van der Linden, S., Goldberg, B., Rathje, S. & Lewandowsky, S. Psychological inoculation improves resilience against misinformation on social media. Sci. Adv. 8 , eabo6254. https://doi.org/10.1126/sciadv.abo6254 (2022).
Gagneur, A. Motivational interviewing: A powerful tool to address vaccine hesitancy. Can. Commun. Dis. Rep. https://doi.org/10.14745/ccdr.v46i04a06 (2020).
Garrett, R. K. & Weeks, B. E. Epistemic beliefs’ role in promoting misperceptions and conspiracist ideation. PLoS ONE 12 , e0184733 (2017).
Costello, T. H. & Lilienfeld, S. O. Social and economic political ideology consistently operate as mutual suppressors: Implications for personality, social, and political psychology. Soc. Psychol. Pers. Sci. 12 , 1425–1436 (2021).
Feldman, S. & Johnston, C. Understanding the determinants of political ideology: Implications of structural complexity. Polit. Psychol. 35 , 337–358 (2014).
Viskupič, F. & Wiltse, D. L. The messenger matters: Religious leaders and overcoming COVID-19 vaccine hesitancy. Polit. Sci. Polit. 55 , 504–509. https://doi.org/10.1017/S104909652200004X (2022).
Sanders, C. & Burnett, K. The neoliberal roots of modern vaccine hesitancy. J. Health Soc. Sci. 4 , 149–156, https://doi.org/10.19204/2019/thnl4 (2019).
Malka, A., Soto, C. J., Inzlicht, M. & Lelkes, Y. Do needs for security and certainty predict cultural and economic conservatism? A cross-national analysis. J. Pers. Soc. Psychol. 106 , 1031 (2014).
Beattie, P., Bettache, K. & Chong, K. C. Y. Who is the neoliberal? Exploring neoliberal beliefs across east and west. J. Soc. Issues 75 , 20–48 (2019).
Nunnally, J. C. Psychometric Theory (McGraw-Hill, 1967).
Google Scholar
British Election Study. British election study 2014-2023 combined waves 1-21 internet panel codebook (2021).
Brotherton, R., French, C. & Pickering, A. Measuring belief in conspiracy theories: The generic conspiracist beliefs scale. Front. Psychol. 4 , 279. https://doi.org/10.3389/fpsyg.2013.00279 (2013).
Mansolf, M. & Reise, S. P. Exploratory bifactor analysis: The Schmid-Leiman orthogonalization and Jennrich-Bentler analytic rotations. Multivariate Behav. Res. 51 , 698–717. https://doi.org/10.1080/00273171.2016.1215898 (2016).
Bruder, M., Haffke, P., Neave, N., Nouripanah, N. & Imhoff, R. Measuring individual differences in generic beliefs in conspiracy theories across cultures: Conspiracy mentality questionnaire. Front. Psychol. 4 , 225 (2013).
Yamagishi, T. The provision of a sanctioning system in the United States and Japan. Soc. Psychol. Q. 51 , 265–271. https://doi.org/10.2307/2786924 (1988).
Dunwoody, P. T. & Funke, F. The aggression-submission-conventionalism scale: Testing a new three factor measure of authoritarianism. J. Soc. Polit. Psychol. 4 , 571–600. https://doi.org/10.5964/jspp.v4i2.168 (2016).
Akkerman, A., Mudde, C. & Zaslove, A. How populist are the people? measuring populist attitudes in voters. Compar. Polit. Stud. 47 , 1324–1353. https://doi.org/10.1177/0010414013512600 (2013).
Huber, S. & Huber, O. W. The centrality of religiosity scale (CRS). Religions 3 , 710–724. https://doi.org/10.3390/rel3030710 (2012).
Peterson, B., Smith, J. A., Tannenbaum, D. & Shaw, M. P. On the “exporting’’ of morality: Its relation to political conservatism and epistemic motivation. Soc. Justice Res. 22 , 206–230. https://doi.org/10.1007/S11211-009-0101-8/FIGURES/1 (2009).
Kramer, M. D. et al. Quantifying dispositional fear as threat sensitivity: Development and initial validation of a model-based scale measure. Assessment 27 , 533–546. https://doi.org/10.1177/1073191119837613 (2020).
Baumsteiger, R. & Siegel, J. T. Measuring prosociality: The development of a prosocial behavioral intentions scale. J. Pers. Assess. 101 , 305–314. https://doi.org/10.1080/00223891.2017.1411918 (2019).
Hong, S.-M. & Faedda, S. Refinement of the Hong psychological reactance scale. Educ. Psychol. Meas. 56 , 173–182. https://doi.org/10.1177/0013164496056001014 (1996).
Shapiro, G. K., Holding, A., Perez, S., Amsel, R. & Rosberger, Z. Validation of the vaccine conspiracy beliefs scale. Papillomavirus Res. 2 , 167–172. https://doi.org/10.1016/J.PVR.2016.09.001 (2016).
Jolley, D. & Douglas, K. M. The effects of anti-vaccine conspiracy theories on vaccination intentions. PLoS ONE 9 , e89177. https://doi.org/10.1371/JOURNAL.PONE.0089177 (2014).
Article PubMed PubMed Central ADS Google Scholar
Rossen, I., Hurlstone, M. J., Dunlop, P. D. & Lawrence, C. Accepters, fence sitters, or rejecters: Moral profiles of vaccination attitudes. Soc. Sci. Med. 224 , 23–27. https://doi.org/10.1016/J.SOCSCIMED.2019.01.038 (2019).
Karlsson, L. C. et al. Fearing the disease or the vaccine: The case of COVID-19. Pers. Individ. Differ. 172 , 110590. https://doi.org/10.1016/j.paid.2020.110590 (2021).
Freeman, D. et al. Injection fears and COVID-19 vaccine hesitancy. Psychol. Med. https://doi.org/10.1017/S0033291721002609 (2021).
Betsch, C., Böhm, R. & Korn, L. Inviting free-riders or appealing to prosocial behavior? Game-theoretical reflections on communicating herd immunity in vaccine advocacy. Health Psychol. 32 , 978 (2013).
Hershey, J. C., Asch, D. A., Thumasathit, T., Meszaros, J. & Waters, V. V. The roles of altruism, free riding, and bandwagoning in vaccination decisions. Organ. Behav. Hum. Decis. Processes 59 , 177–187. https://doi.org/10.1006/OBHD.1994.1055 (1994).
Ibuka, Y., Li, M., Vietri, J., Chapman, G. B. & Galvani, A. P. Free-riding behavior in vaccination decisions: An experimental study. PLoS ONE 9 , e87164. https://doi.org/10.1371/JOURNAL.PONE.0087164 (2014).
Gidengil, C., Chen, C., Parker, A. M., Nowak, S. & Matthews, L. Beliefs around childhood vaccines in the united states: A systematic review. Vaccine 37 , 6793. https://doi.org/10.1016/J.VACCINE.2019.08.068 (2019).
Meszaros, J. R. et al. Cognitive processes and the decisions of some parents to forego pertussis vaccination for their children. J. Clin. Epidemiol. 49 , 697–703. https://doi.org/10.1016/0895-4356(96)00007-8 (1996).
Attwell, K., Smith, D. T. & Ward, P. R. ‘If your child’s vaccinated, why do you care about mine?’ Rhetoric, responsibility, power and vaccine rejection. J. Sociol. 57 , 268–285. https://doi.org/10.1177/1440783319893468 (2019).
Benin, A. L., Wisler-Scher, D. J., Colson, E., Shapiro, E. D. & Holmboe, E. S. Qualitative analysis of mothers’ decision-making about vaccines for infants: The importance of trust. Pediatrics 117 , 1532–1541. https://doi.org/10.1542/PEDS.2005-1728 (2006).
Hatokova, M., Masaryk, R. & Tunyiova, M. How slovak mothers view child vaccination: Focus group analysis. Ceskoslovenska Psychologie 62 , 101–118 (2018).
Kate, J. T., Koster, W. D. & der Waal, J. V. “Following your gut’’ or “questioning the scientific evidence’’: Understanding vaccine skepticism among more-educated Dutch parents. J. Health Soc. Behav. 62 , 85–99. https://doi.org/10.1177/0022146520986118 (2021).
Tomljenovic, H., Bubic, A. & Erceg, N. It just doesn’t feel right—the relevance of emotions and intuition for parental vaccine conspiracy beliefs and vaccination uptake. Psychol. Health 35 , 538–554. https://doi.org/10.1080/08870446.2019.1673894 (2020).
Download references
Acknowledgements
This project has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No 964728 (JITSUVAX).
Author information
Authors and affiliations.
School of Psychological Science, University of Bristol, Bristol, BS8 1TU, UK
Dawn L. Holford & Stephan Lewandowsky
University of Coimbra, 3004-531, Coimbra, Portugal
- Angelo Fasce
Massachusetts Institute of Technology, Cambridge, MA, 02139, USA
Thomas H. Costello
You can also search for this author in PubMed Google Scholar
Contributions
D.L.H.: conceptualisation, data curation, formal analysis, investigation, methodology, project administration, resources, validation, visualisation, writing—original draft, and writing—review and editing. A.F.: conceptualisation, formal analysis, investigation, methodology, resources, writing—original draft, and writing—review and editing. S.L.: conceptualisation, funding acquisition, investigation, methodology, supervision, and writing—review and editing. T.H.C.: formal analysis, methodology, resources, software, and writing—review and editing.
Corresponding author
Correspondence to Dawn L. Holford .
Ethics declarations
Competing interests..
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Holford, D.L., Fasce, A., Costello, T.H. et al. Psychological profiles of anti-vaccination argument endorsement. Sci Rep 13 , 11219 (2023). https://doi.org/10.1038/s41598-023-30883-7
Download citation
Received : 11 October 2022
Accepted : 02 March 2023
Published : 17 July 2023
DOI : https://doi.org/10.1038/s41598-023-30883-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
- Philipp Schmid
- Stephan Lewandowsky
Nature Human Behaviour (2023)
Boosting human capacities: attitudes toward Human Enhancement and vaccination in the context of perceived naturalness and invasiveness
- Niklas Alexander Döbler
- Claus-Christian Carbon
Discover Psychology (2023)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- How the case against...
How the case against the MMR vaccine was fixed
- Related content
- Peer review
- Brian Deer , journalist
- 1 London, UK
- briandeer.com
In the first part of a special BMJ series, Brian Deer exposes the bogus data behind claims that launched a worldwide scare over the measles, mumps, and rubella vaccine, and reveals how the appearance of a link with autism was manufactured at a London medical school
When I broke the news to the father of child 11, at first he did not believe me. “Wakefield told us my son was the 13th child they saw,” he said, gazing for the first time at the now infamous research paper which linked a purported new syndrome with the measles, mumps, and rubella (MMR) vaccine. 1 “There’s only 12 in this.”
That paper was published in the Lancet on 28 February 1998. It was retracted on 2 February 2010. 2 Authored by Andrew Wakefield, John Walker-Smith, and 11 others from the Royal Free medical school, London, it reported on 12 developmentally challenged children, 3 and triggered a decade long public health scare.
“Onset of behavioural symptoms was associated by the parents with measles, mumps, and rubella vaccination in eight of the 12 children,” began the paper’s “findings.” Adopting these claims as fact, 4 its “results” section added: “In these eight children the average interval from exposure to first behavioural symptoms was 6.3 days (range 1-14).”
Mr 11, an American engineer, looked again at the paper: a five page case series of 11 boys and one girl, aged between 3 and 9 years. Nine children, it said, had diagnoses of “regressive” autism, and all but one were reported with “non-specific colitis.” The “new syndrome” brought these together, linking brain and bowel diseases. His son was the penultimate case.
Running his finger across the paper’s tables, over coffee in London, Mr 11 seemed reassured by his anonymised son’s age and other details. But then he pointed at table 2—headed “neuropsychiatric diagnosis”—and for a second time objected.
“That’s not true.”
Child 11 was among the eight whose parents apparently blamed MMR. The interval between his vaccination and the first “behavioural symptom” was reported as 1 week. This symptom was said to have appeared at age 15 months. But his father, whom I had tracked down, said this was wrong.
“From the information you provided me on our son, who I was shocked to hear had been included in their published study,” he wrote to me, after we met again in California, “the data clearly appeared to be distorted.”
He backed his concerns with medical records, including a Royal Free discharge summary. 5 Although the family lived 5000 miles from the hospital, in February 1997 the boy (then aged 5) had been flown to London and admitted for Wakefield’s project, the undisclosed goal of which was to help sue the vaccine’s manufacturers. 6
Wakefield’s “syndrome”
Unknown to Mr 11, Wakefield was working on a lawsuit, 7 for which he sought a bowel-brain “syndrome” as its centrepiece. Claiming an undisclosed £150 (€180, $230) an hour through a Norfolk solicitor named Richard Barr, he had been confidentially 8 put on the payroll two years before the paper was published, eventually grossing him £435 643, plus expenses. 9
Curiously, however, Wakefield had already identified such a syndrome before the project which would reputedly discover it. “Children with enteritis/disintegrative disorder [an expression he used for bowel inflammation and regressive autism 10 ] form part of a new syndrome,” he and Barr explained in a confidential grant application to the UK government’s Legal Aid Board 11 before any of the children were investigated. 12 “Nonetheless the evidence is undeniably in favour of a specific vaccine induced pathology.”
The two men also aimed to show a sudden-onset “temporal association”—strong evidence in product liability. “Dr Wakefield feels that if we can show a clear time link between the vaccination and onset of symptoms,” Barr told the legal board, “we should be able to dispose of the suggestion that it’s simply a chance encounter.” 13
But child 11’s case must have proved a disappointment. Records show his behavioural symptoms started too soon . “His developmental milestones were normal until 13 months of age,” notes the discharge summary. “In the period 13-18 months he developed slow speech patterns and repetitive hand movements. Over this period his parents remarked on his slow gradual deterioration.”
That put the first symptom two months earlier than reported in the Lancet, and a month before the boy received the MMR vaccination. And this was not the only anomaly to catch the father’s eye. What the paper reported as a “behavioural symptom” was noted in the records as a chest infection.
“Please let me know if Andrew W has his doctor’s license revoked,” wrote Mr 11, who is convinced that many vaccines and environmental pollutants may be responsible for childhood brain disorders. “His misrepresentation of my son in his research paper is inexcusable. His motives for this I may never know.”
The father need not have worried. My investigation of the MMR issue exposed the frauds behind Wakefield’s research. Triggering the longest ever UK General Medical Council fitness to practise hearing, and forcing the Lancet to retract the paper, last May it led to Wakefield and Walker-Smith being struck off the medical register. 14 15 16
Wakefield, now 54, who called no witnesses, was branded “dishonest,” “unethical,” and “callous.” 14 15 16 Walker-Smith, now 74, the senior clinician in the project, was found to have presided over “high risk” 17 research without clinical indication or ethical approval. The developmentally challenged children of often vulnerable parents were discovered to have been treated like the doctors’ guinea pigs. 18
Lawsuit test case
But Mr 11 was not the first parent with a child in the study whom I interviewed during my inquiries. That was Mrs 2: the first of the parents to approach Wakefield. She was sent to him by an anti-vaccine campaign called JABS. 19 Her son had regressive autism, 20 longstanding problems with diarrhoea, 21 and was the prime example of the purported bowel and brain syndrome—still unsubstantiated 14 years later. 22 This boy would appear in countless media reports, and was one of the four “best” cases in Barr’s lawsuit.
I travelled to the family home, 80 miles northeast of London, to hear about child 2 from his mother. That was in September 2003, when the lawsuit fell apart after counsel representing 1500 families said that, on the evidence, Barr’s autism claims would fail. 23 By that time, Mrs 2 had seen her son’s medical records and expert reports written for her case at trial.
Her concerns about MMR had been noted by her general practitioner when her son was 6 years old. 24 But she told me the boy’s troubles began after his vaccination, which he received at 15 months. 25 “He’d scream all night, and he started head banging, which he’d never done before,” she explained.
“When did that begin, do you think?” I asked.
“That began after a couple of months, a few months afterward, but it was still, it was concerning me enough, I remember going back . . .”
“Sorry. I don’t want to be, like, massively pernickety, but was it a few months, or a couple of months?”
“It was more like a few months because he’d had this, kind of, you know, slide down. He wasn’t right. He wasn’t right. Before he started.”
“Not quicker than two months, but not longer than how many months? What are we talking about here?”
“From memory, about six months, I think.”
The next day, she complained to my editors. She said my methods “seemed more akin to the gutter press.” But I was perplexed by her story, since there was no case in the Lancet that matched her careful account.
According to the paper, child 2 had his “first behavioural symptom” two weeks, not six months , after MMR. This was derived from a Royal Free history (citing “headbanging” and “screaming” as the start 26 ) taken by Mark Berelowitz, a child psychiatrist and a coauthor of the paper. 27 He saw Mrs 2 during the boy’s admission, at age 8, after she had discussed her son’s story with Wakefield. 28
As I later discovered, each family in the project was involved in such discussions before they saw the hospital’s clinicians. 29 Wakefield phoned them at home, and must have at least suggestively questioned them, potentially impacting on later history taking. But I knew little of such things then, and shared my confusion with Walker-Smith, whom I met shortly after Mrs 2.
“There is no case in the paper that is consistent with the case history [Mrs 2] has given me,” I told him. “There just isn’t one.”
“Well that could be true,” the former professor of paediatric gastroenterology replied, disarmingly. He knew the case well, having admitted the boy for the project and written reports for Barr, who paid him £23 000. 30
“Well, so either what she is telling me is not accurate, or the paper’s not accurate.”
“Well I can’t really comment,” he said. “You really touch on an area which I don’t think should be debated like this. And I think these parents are wrong to discuss such details, where you could be put in a position of having a lot of medical details and then try to match it with this, because it is a confidential matter.”
It was not merely medically confidential, it was also legally protected: a double screen against public scrutiny. But responding to my first MMR reports, in the Sunday Times in February 2004, 31 the GMC decided to investigate the cases and requisitioned the children’s records. 32
The regulator’s main focus was whether the research was ethical. Mine was whether it was true. So as a five member disciplinary panel 33 trawled through the records, with five Queen’s counsel 34 and three defendant doctors, 35 I compared them with what was published in the journal. 36
Multiple discrepancies
The paper gave the impression that the authors had been scrupulous in documenting the patients’ cases. “Children underwent gastroenterological, neurological, and developmental assessment and review of developmental records,” it explained, specifying that Diagnostic and Statistical Manual of Mental Disorders IV 37 criteria were used for neuropsychiatric diagnoses. “Developmental histories included a review of prospective developmental records from parents, health visitors, and general practitioners.”
But, when the details were dissected before the GMC panel, multiple discrepancies emerged. A syndrome necessarily requires at least some consistency, but, as the records were laid out, Wakefield’s crumbled.
First to crack was “regressive autism,” the bedrock of his allegations. 38 39 “Bear in mind that we are dealing with regressive autism in these children, not of classical autism where the child is not right from the beginning,” he later explained, for example, to a United States congressional committee. 40
But only one—child 2—clearly had regressive autism. 41 Three of nine so described clearly did not. None of these three even had autism diagnoses, either at admission or on discharge from the Royal Free.
The paper did not reveal that two of this trio were brothers, living 60 miles south of the hospital. Both had histories of fits and bowel problems 42 recorded before their MMR vaccinations. 43 44 The elder, child 6, aged 4 years at admission, had Asperger’s syndrome, 45 which is distinct from autism under DSM-IV, is not regressive, 46 and was confirmed on discharge. 47 His brother, child 7, was admitted at nearly 3 years of age without a diagnosis, 48 and a post-discharge letter from senior paediatric registrar and Lancet coauthor David Casson 49 summarised: “He is not thought to have features of autism.” 50
The third in the trio, child 12, was enrolled on the advice of the brothers’ mother—reported in media to be a JABS activist, and who had herself “only relatively recently” 51 blamed the vaccine. Child 12 was aged 6 at admission and had previously been assessed for possible Asperger’s syndrome at Guy’s Hospital, London, by a renowned developmental paediatrician. 52 53 She diagnosed “an impairment in respect of language”—an opinion left undisturbed by Berelowitz. 54 55
Mrs 12 was a GMC witness at its mammoth hearing, which between July 2007 and May 2010 ran for 217 days. She explained that the brothers’ mother had made her suspicious of MMR and had given her Barr’s and Wakefield’s names. 56 Mrs 12 then approached them and filed a statement for legal aid before her son was referred. 57
“It was like a jigsaw puzzle—it suddenly seemed to fit into place,” she told the panel, describing how she concluded, four years after the boy was vaccinated, that MMR was to blame for his problems. “I had this perfectly normal child who, as I could see, for no apparent reason started to not be normal.”
The 12 children were admitted between July 1996 and February 1997, and others had connections not revealed in the paper, almost as striking as the trio’s. The parents of child 9 and child 10 were contacts of Mrs 2, who ran a group that campaigned against MMR. 58 And child 4 and child 8 were admitted—without outpatient appointments 59 —for ileocolonoscopy and other invasive procedures, from one Tyneside general practice, 280 miles from the Royal Free, after advice from anti-MMR campaigners. 60
Pre-existing problems
Both child 4 and child 8 were among the eight whose parents were reported to have blamed the vaccine. But although the paper specified that all 12 children were “previously normal,” 61 both had developmental delays, and also facial dysmorphisms, noted before MMR vaccination.
In the case of child 4, who received the vaccine at age 4 years, Wakefield played down problems, suggesting that early issues had resolved. “Child four was kept under review for the first year of life because of wide bridging of the nose,” he reported in the paper. “He was discharged from follow-up as developmentally normal at age 1 year.”
But medical records, presented by the GMC, give a different picture for this child. Reports from his pre-MMR years were peppered with “concerns over his head and appearance,” 62 “recurrent” diarrhoea, 63 “developmental delay,” 64 “general delay,” and restricted vocabulary. 65 And although before his referral to Wakefield his mother had inquired about vaccine damage compensation, 66 his files include a report of a “very small deletion within the fragile X gene,” 67 and a note of the mother’s view that her concerns about his development had begun when he was 18 months old. 68
“In general, his mother thinks he developed normally initially and subsequently his problems worsened, and he lost some of his milestones, but he subsequently improved on a restrictive exclusion diet,” wrote his general practitioner, William Tapsfield, referring the boy, then aged 9, after a phone conversation with Wakefield. “The professionals who have known [child 4] since birth don’t entirely agree with this, however, and there is a suggestion that some of his problems may have started before vaccination.” 69
Similarly with child 8, who was also described in the Lancet as having overcome problems recorded before vaccination. “The only girl . . . was noted to be a slow developer compared with her older sister,” the paper said. “She was subsequently found to have coarctation of the aorta. After surgical repair of the aorta at the age of 14 months, she progressed rapidly, and learnt to talk. Speech was lost later.”
But Wakefield was not a paediatrician. He was a former trainee gastrointestinal surgeon with a non-clinical medical school contract. 70 And his interpretation differed from that of local consultants (including a developmental paediatrician and a geneticist) who had actually looked after the girl. Her doctors put the coarctation side by side with the delay and dysmorphism, 71 and noted of her vocabulary that, before MMR at 18 months, she vocalised only 72 “two or three words.” 73
“[Child 8’s] mother has been to see me and said you need a referral letter from me in order to accept [child 8] into your investigation programme,” the general practitioner, Diana Jelley, wrote to Wakefield at referral, when the girl was aged 3 and a half years. “I would simply re-iterate . . . that both the hospital and members of the primary care team involved with [child 8] had significant concerns about her development some months before she had her MMR.” 74
The girl’s general practice notes also provide insight into the background to the 12 children’s referrals. After person(s) unknown told Mrs 8 that her daughter may have inflammatory bowel disease, Jelley wrote: “Mum taking her to Dr Wakefield, Royal Free Hospital for CT scans/gut biopsies ?Crohn’s—will need ref letter—Dr W to phone me. Funded through legal aid.” 75
The child was “pale”
The remaining five children served Wakefield’s claims no better. There was still no convincing MMR syndrome. Child 1, aged 3 years when he was referred to London, lived 100 miles from the Royal Free, and had an older brother who was diagnosed as autistic. 76 Child 1’s recorded story began when he was aged 9 months, with a “new patient” note by general practitioner Andrea Barrow. 77 One of the mother’s concerns was that he could not hear properly—which might sound like a hallmark presentation of classical autism, the emergence of which is often insidious. Indeed, a Royal Free history, by neurologist and coauthor Peter Harvey, noted “normal milestones” until “18 months or so.” 78
Child 1 was vaccinated at 12 months of age, however. 79 Thus neither 9 nor 18 months helped Wakefield’s case. But in the Lancet , the “first behavioural symptom” was reported “1 week” after the injection, holding the evidence for the lawsuit on track.
Step 1 to achieve this: two and a half years after the child was vaccinated, Walker-Smith took an outpatient history. Although the mother apparently had no worries following her son’s vaccination, 80 the professor elicited that the boy was “pale” 7-10 days after the shot. He also elicited that the child “possibly” had a fever, and “may” have been delirious, as well as pale. 81
“It’s difficult to associate a clear historical link with the MMR and the answer to autism,” Walker-Smith wrote to the general practitioner, 82 with a similar letter to Wakefield, “although [Mrs 1] does believe that [child 1] had an illness 7-10 days after MMR when he was pale, ?fever, ?delirious, but wasn’t actually seen by a doctor.”
Step 2: for the Lancet , Wakefield dropped the question marks, turning Walker-Smith’s queries into assertions. And, although Royal Free admission 83 and discharge 84 records refer to “classical” autism, step 3, the former surgeon reported “delirium” as the first “behavioural symptom” of regressive autism, with, step 4, a “time to onset” of 7 days.
So here—behind the paper—is how Wakefield evidenced his “syndrome” for the lawsuit, and built his platform to launch the vaccine scare.
“It is significant that this syndrome only appeared with the introduction of the polyvalent MMR vaccine in 1988 rather than with the monovalent measles vaccine introduced in 1968,” he claimed in one of a string of patents he filed for businesses to be spun from the research. 85 “This indicates that MMR is responsible for this condition rather than just the measles virus.”
Three of the four remaining children were seen in outpatients on the same day—in November 1996. None of their families were reported in the paper as blaming the vaccine. Child 5, from Berkshire, aged 7 at admission, had received MMR at 16 months. 86 The paper reported concerns at 18 months, but the medical records noted fits 87 and parental worries 88 at 11 months. Child 9, aged 6, from Jersey, also had MMR at 16 months. 89 His mother dated problems from 18-20 months. 90 Child 10, aged 4, from south Wales, contracted a viral infection, which was suspected by parents and doctors to have caused his disorder, four months after his vaccination. 91
“Behavioural changes included repetitive behaviour, disinterest in play or head banging,” said a question and answer statement issued by the medical school, concerning the Lancet 12, on the day of the paper’s publication.
Another discrepancy to emerge during the GMC hearing concerned the number of families who blamed MMR. The paper said that eight (1, 2, 3, 4, 6, 7, 8, and 11) linked developmental issues with the vaccine. But the total in the records was actually 11. The parents of child 5, 92 9, 93 and 12 94 were also noted at the hospital as blaming the vaccine, but their stated beliefs were omitted from the journal.
Case selection
The frequency of these beliefs should not have surprised Wakefield, retained as he was to support a lawsuit. In the month that Barr engaged him—two years before the paper was published—the lawyer touted the doctor in a confidential newsletter to his MMR clients and contacts. “He has deeply depressing views about the effect of vaccines on the nation’s children,” Barr said. 95 “He is also anxious to arrange for tests to be carried out on any children . . . who are showing symptoms of possible Crohn’s disease. The following are signs to look for. If your child has suffered from all or any of these symptoms could you please contact us, and it may be appropriate to put you in touch with Dr Wakefield.”
The listed symptoms included pain, weight loss, fever, and mouth ulcers. Clients and contacts were quickly referred. 96 Thus, an association between autism, digestive issues, and worries about MMR—the evidence that launched the vaccine scare—was bound to be found by the Royal Free’s clinicians because this was how the children were selected. 97
Moreover, through the omission from the paper of some parents’ beliefs that the vaccine was to blame, the time link for the lawsuit sharpened. With concerns logged from 11 of 12 families, the maximum time given to the onset of alleged symptoms was a (forensically unhelpful) four months. But, in a version of the paper circulated at the Royal Free six months before publication, reported concerns fell to nine of 12 families but with a still unhelpful maximum of 56 days. 98 Finally, Wakefield settled on 8 of 12 families, with a maximum interval to alleged symptoms of 14 days.
Between the latter two versions, revisions also slashed the mean time to alleged symptoms—from 14 to 6.3 days. “In these children the mean interval from exposure to the MMR vaccine to the development of the first behavioural symptom was six days, indicating a strong temporal association,” he emphasised in a patent for, among other things, his own prophylactic measles vaccine, 99 eight months before the Lancet paper.
This leaves child 3. He was 6½ and lived on Merseyside: 200 miles from the hospital. He received MMR at 14 months, 100 with the first concerns recorded in the general practitioner’s notes 15 months after that. 101 His mother—who 4 years later contacted Wakefield on the advice of JABS 102 —told me that her son had become aggressive towards a brother, and records say that his vocabulary had not developed. 103
“We both felt that the MMR needle had made [child 3] go the way he is today,” the parents wrote to a local paediatric neurologist, Lewis Rosenbloom, 18 months before their son’s referral to London. 104 They told him they wanted “justice” from the vaccine’s manufacturer, and that they had been turned down for legal aid. 105 “Although it is said that the MMR has never been proven to make children to be autistic, we believe that the injection has made [child 3] to be mentally delayed, which in turn may have triggered off the autism.”
I visited this family twice. Their affected son was now a teenager and a challenge both to himself and to others. His mother said his diagnosis was originally “severe learning difficulties with autistic tendencies” but that she had fought to get it changed to autism. 106
As for a connection with MMR, there was only suspicion. I do not think his family was sure, one way or the other. 107 When I asked why they took him to the Royal Free, his father replied: “We were just vulnerable, we were looking for answers.”
What was unquestionably true was that child 3 had serious bowel trouble: intractable, lifelong, constipation. 108 This was the most consistent feature among the 12 children’s symptoms and signs 109 but, being the opposite of an expected finding in inflammatory bowel disease, 110 111 it was nowhere mentioned in the paper. This young man’s was so severe that he was dosed at his special school, his mother said, with up to five packets of laxative a day.
“You always knew when his stomach was hard,” she told me, in terms echoed over the years by many parents involved with Wakefield . “He would start headbutting, kicking, breaking anything in the house. Then he would go to the toilet and release it.”
For the Royal Free team, however, when reporting on these patients, such motility issues 112 were sidelined in the hunt for Wakefield’s syndrome. In almost all the children, they noted commonly swollen glands in the terminal ileum, and what was reported as “non-specific colitis.” 113 114 In fact, as I revealed in the BMJ last April, 115 the hospital’s pathology service found the children’s colons to be largely normal, but a medical school “review” changed the results.
In this evolution of the gut pathology noted in the records to what was published in the paper, child 3’s case is a prime example. After ileocolonoscopy (which, GMC prosecution and defence experts agreed, was not clinically indicated 116 ), the hospital’s pathologists found all colonic samples to be “within normal histological limits”. 117 But three months after the boy was discharged, Walker-Smith recalled the records and changed the diagnosis to “indeterminate ileocolitis”. 118
“I think, sadly, this was the first child who was referred, and the long term help we were able to give in terms of dealing with constipation was not there,” he told the GMC panel. “However, we had excluded Crohn’s disease and we had done our best to try and help this child, but in the end we did not.”
So that is the Lancet 12: the foundation of the vaccine scare. No case was free of misreporting or alteration. Taken together, NHS records cannot be reconciled with what was published, to such devastating effect, in the journal (table ⇓ ).
Comparison of three features of the 12 children in the Lancet paper with features apparent in the NHS records, including those from the Royal Free hospital
- View inline
Wakefield, however, denies wrongdoing, in any respect whatsoever. 119 He says he never claimed that the children had regressive autism, nor that he said they were previously normal. He never misreported or changed any findings in the study, and never patented a measles vaccine. None of the children were Barr’s clients before referral to the hospital, and he never received huge payments from the lawyer. There were no conflicts of interest. He is the victim of a conspiracy. 120 121 He never linked autism with MMR.
“Mr Deer’s implications of fraud against me are claims that a trained physician and researcher of good standing had suddenly decided he was going to fake data for his own enrichment,” he said in a now abandoned complaint against me to the UK Press Complaints Commission. “The other authors generated and ‘prepared’ all the data that was reported in the Lancet . I merely put their completed data in tables and narrative form for the purpose of submission for publication.”
But, despite signing up to claim credit for a paper in the Lancet , his co-authors Walker-Smith and Murch did not even know which case was which. Walker-Smith said he had “trusted” Wakefield. 122 “When I signed that paper, I signed with good intent,” he told the GMC panel. Denying any wrongdoing, he argued that the published report was not even about MMR, but merely described a new “clinico-pathological entity”. He said that the admissions to the Royal Free were “entirely related to gastroenterological illness” and how the children were sourced was “irrelevant” and “immaterial.” His lawyers said that he was appealing against the panel’s decision and on these grounds they had advised him not to respond to my questions.
The journal, meanwhile, took 12 years to retract the paper, by which time its mischief had been exported. As parents’ confidence slowly returned in Britain, the scare took off around the world, unleashing fear, guilt, and infectious diseases—and fuelling suspicion of vaccines in general. In addition to measles outbreaks, other infections are resurgent, with Mr 11’s home state of California last summer seeing 10 babies dead from whooping cough, in the worst outbreak since 1958. 123
Wakefield, nevertheless, now apparently self-employed and professionally ruined, remains championed by a sad rump of disciples. “Dr Wakefield is a hero,” is how one mother caught their mood in a recent Dateline NBC TV investigation, featuring the story of the doctor and me. 124 “I don’t know where we would be without him.”
How the link was fixed
The Lancet paper was a case series of 12 child patients; it reported a proposed “new syndrome” of enterocolitis and regressive autism and associated this with MMR as an “apparent precipitating event.” But in fact:
Three of nine children reported with regressive autism did not have autism diagnosed at all. Only one child clearly had regressive autism
Despite the paper claiming that all 12 children were “previously normal,” five had documented pre-existing developmental concerns
Some children were reported to have experienced first behavioural symptoms within days of MMR, but the records documented these as starting some months after vaccination
In nine cases, unremarkable colonic histopathology results—noting no or minimal fluctuations in inflammatory cell populations—were changed after a medical school “research review” to “non-specific colitis”
The parents of eight children were reported as blaming MMR, but 11 families made this allegation at the hospital. The exclusion of three allegations—all giving times to onset of problems in months—helped to create the appearance of a 14 day temporal link
Patients were recruited through anti-MMR campaigners, and the study was commissioned and funded for planned litigation
Cite this as: BMJ 2011;342:c5347
Funding: Brian Deer’s investigation was funded by the Sunday Times of London and the Channel 4 television network. Reports by Deer in the BMJ were commissioned and paid for by the journal. No other funding was received, apart from legal costs paid to Deer by the Medical Protection Society on behalf of Andrew Wakefield.
Competing interests: The author has completed the unified competing interest form at www.icmje.org/coi_disclosure.pdf (available on request from him) and declares no support from any organisation for the submitted work; no financial relationships with any organisation that might have an interest in the submitted work in the previous three years; BD’s investigation led to the GMC proceedings referred to in this report, including the charges. He made many submissions of information but was not a party or witness in the case, nor involved in its conduct.
Provenance and peer review: Commissioned; externally peer reviewed.
- ↵ Wakefield AJ, Murch SH, Anthony A, Linnell, Casson DM, Malik M, et al. Ileal lymphoid nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet 1998 ; 351 : 637 -41 [retracted]. OpenUrl CrossRef PubMed Web of Science
- ↵ Editors of the Lancet. Retraction: ileal lymphoid nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet 2010 ; 375 : 445 . OpenUrl CrossRef PubMed Web of Science
- ↵ One child, child 5, was admitted without any developmental diagnosis, but was in treatment for epilepsy.
- ↵ Although the paper makes clear that the research did not prove an association between MMR and the purported syndrome, it describes its table 2 as summarising “the apparent precipitating events; onset of behavioural features; and age of onset of both behaviour and bowel symptoms.”
- ↵ David Casson. Discharge summary. 21 May 1997.
- ↵ Although Wakefield and the Lancet would later claim that the Legal Aid Board commissioned a quite separate “viral” study, the work specified in the documents submitted to the Legal Aid Board, seeking funding, on 6 June 1996, included clinical examination, ilecolonoscopy, histology, immunohistochemistry and molecular analysis for measles virus, neuropsychiatric studies, MRI brain scan, lumbar puncture, EEG and evoked potentials, B12 studies, modified Schilling test, and various blood and urine tests. The document includes costings, such as £1750 for colonoscopy with four night’s stay, £1000 for MRI scans, and £1400 for medical reports. Molecular, immunohistochemical, and electron microscopic analysis of tissues was priced at £500 per child. Named investigators for the legal project who would also be authors of the Lancet paper were Andrew Wakefield, John Walker-Smith, Simon Murch, David Casson, Amar Dhillon, John Linnell, Mark Berelowitz, and Peter Harvey. The document states: “The objective is to seek evidence which will be acceptable in a court of law of the causative connection between either the mumps, measles and rubella vaccine or the measles/rubella vaccine and certain conditions which have been reported with considerable frequency by families of children who are seeking compensation. It is hoped that using the testing protocol attached it will be possible to establish the causal link between the administration of the vaccines and the conditions outlined in this proposed protocol and costing proposal.” The board commissioned the project under an “authority to do contract work,” naming Wakefield, issued on 22 August 1996. The technical specification is materially identical to a protocol submitted for approval by the Royal Free’s ethics committee, and the work to be performed is materially identical to the study submitted by Wakefield to the Lancet , with data sliced into two paired papers, which were peer reviewed together. One was published on 28 February 1998 , and the other was rejected by the journal.
- ↵ MMR and MR Vaccine Litigation Sayers and others v Smithkline Beecham plc and others - [2007] All ER (D) 30 (Jun).
- ↵ Although some of his professional colleagues have admitted awareness of a relationship between Wakefield and the lawyer, his co-authors have denied any knowledge that he was contractually employed and funded by Barr. For example, in an email dated 27 February 2004, Walker-Smith wrote: “No financial details of Andy’s work was ever discussed with me by anyone and I was totally unaware of the grant of £55,000 that had been paid to him in an NHS Trust Fund, until Deer told me to my astonishment in December 2003.” Also in February 2004, John O’Leary, a Wakefield research collaborator and business partner, issued a statement to Deer, through lawyers: “We were not made aware, nor were we aware, of any liaison between Dr Wakefield and Mr Richard Barr of Alexander Harris Solicitors that apparently existed since 1996. In addition, we had never been informed that the LSC [the Legal Services Commission, successor to the Legal Aid Board] had funded Dr Wakefield.”
- ↵ Deer B. MMR doctor given legal aid thousands. Sunday Times 2006 December 31. www.timesonline.co.uk/tol/news/uk/article1265373.ece/ .
- ↵ Wakefield A. Introduction to the rationale, aims and potential therapeutic implications of the investigation of children with Disintegrative disorder (regressive autism; Heller’s disease and intestinal symptomatology.” (Document issued by Wakefield and mailed to doctors and parents who approached the Royal Free , dated 3 February 1997.)
- ↵ Barr R, Wakefield A. Proposed protocol and costing proposals for testing a selected number of MR and MMR vaccinated children (and attached specification). Submitted to the Legal Aid Board 6 June 1996. [GMC fitness to practise panel hearing in the case of Wakefield, Walker-Smith and Murch. Day 11.]
- ↵ Child 1 attended an outpatient appointment on 19 June 1996, and was admitted on 21 July 1996.
- ↵ Barr R. Letter to the Legal Aid Board. 22 November 1996. Day 11.
- ↵ General Medical Council. Dr Andrew Wakefield: determinations on serious professional misconduct and sanctions. 24 May 2010. Wakefield: www.gmc-uk.org/Wakefield_SPM_and_SANCTION.pdf_32595267.pdf .
- ↵ General Medical Council. Professor John Walker-Smith: determinations on serious professional misconduct and sanctions, 24 May 2010. www.gmc-uk.org/Professor_Walker_Smith_SPM.pdf_32595970.pdf .
- ↵ General Medical Council. Fitness to practise panel. Findings of fact. 28 January 2010. www.gmc-uk.org/static/documents/content/Wakefield__Smith_Murch.pdf .
- ↵ British Paediatric Association. Guidelines for the ethical conduct of medical research involving children. Bull Med Ethics 1992 ; 80 : 13 -20. OpenUrl PubMed
- ↵ Panel findings of fact. Ten children (1, 2, 3, 5, 6, 7, 8, 9, 10, 12) were found to have been subjected to invasive investigations for research purposes without ethical approval. In seven cases (1,2,3,5,8,9,12) this was found to be contrary to the child’s clinical interests..Eight children (1, 2, 3, 4, 5, 8, 9, 12) were caused to undergo colonoscopies which were not clinically indicated. Seven children (1, 2, 3, 5, 8, 9, 12) were caused to undergo barium meals and follow throughs which were not clinically indicated. Three children (3, 9, 12) were caused to undergo lumbar punctures which were not clinically indicated.
- ↵ Interviewed by Brian Deer, both Mrs 2 and the organiser of JABS confirmed this.
- ↵ (a) Neil Thomas. Evidence to the panel. Day 107. (b) Michael Rutter. Evidence to the panel. Day 35.
- ↵ (a) Richard Cartmel. Evidence to the panel. Day 14. (b) Royal Free history taken: 2 September 1996. Day 40.
- ↵ Buie T, Campbell DB, Fuchs GJ, Furata GT, Levy J, VandeWater J, et al. Evaluation, diagnosis, and treatment of gastrointestinal disorders in individuals with ASDs: a consensus report. Pediatrics 2010;125(suppl 1): s1-18.
- ↵ Lord Justice May. Judgment in the court of appeal, London. R on the application of “H” v the Legal Services Commission. 28 February 2006 .
- ↵ Richard Cartmel. GP record. 2 November 1994. Day 14. “Nil obvious re MMR story.”
- ↵ Child 2 was born on 29 July 1988 (mother’s interview with Deer; register of births), and vaccinated with MMR on 8 November 1989 (GP records. Day 14)
- ↵ (a) David Casson. Discharge summary. 16 September 1996. Day 24. “Mum notes a normal developmental progress. Mum does recount that at 13 months of age he had his MMR immunisation and two weeks following this had started with head banging behaviour and screaming throughout the night. Subsequently seemed generally sickly but nevertheless the main changes appeared to have stemmed from the age of 20 months when he started losing words and became hyperactive and stopped recognising people and responding normally.” The summary, like the Lancet paper, gives a wrong age (13 months) for child 2’s vaccination, taken from the mother by Mark Berelowitz. (b) Peter Harvey. Neurology report. 9 September 1996 . Day 107. “Head banging after MMR inoculation followed by progressive intellectual damage.”
- ↵ Berelowitz told the panel that the “core part” of the job to which he was appointed in 1993 was to head the paediatric liaison service, which helped children and families deal with psychological complications of severe physical illness. Day 12.
- ↵ Panel findings of fact. Page 13.
- ↵ Andrew Wakefield. Evidence to the panel. Day 59. “Firstly, as with all other potential referrals, the parents had made contact with me and had described their child’s problems as they perceived them...” In some cases, he sent them documents setting out his theories and plans. Day 59. Although an academic researcher with no clinical duties, Wakefield was anxious to talk with parents before referral. For example, he wrote to family of child 4. Day 51. “Thank you very much for your letter regarding your son. I would be very grateful if you could phone me or my secretary with your telephone number so that we can discuss this directly.” He wrote to the parents of child 12. Day 42. “It will be necessary for me to discuss the nature of the referral with your GP and I would be grateful if you could let me have his/her name, telephone number. Also could you please let me have your telephone number so that I can speak to you directly on the subject.”
- ↵ Deer B. Revealed: Undisclosed payments to Andrew Wakefield at the heart of vaccine alarm. http://briandeer.com/wakefield/legal-aid.htm
- ↵ Deer B. Revealed: MMR research scandal. Sunday Times 2004 ; Feb 22. www.timesonline.co.uk/tol/life_and_style/health/article1027636.ece .
- ↵ The GMC panel examined records for all of the Lancet children except child 11. It also examined the records of an additional patient, child JS, a Barr client who was denied by his paediatrician enrolment into the study, despite repeated requests from Wakefield and Walker-Smith. This boy was later admitted as a private patient and became a lead claimant, alongside child 2, in the lawsuit.
- ↵ Sylvia Dean, lay member; Wendy Golding, lay member; Surendra Kumar, GP (chair); Parimala Moodley, psychiatrist; Stephen Webster, geriatrician.
- ↵ Kieran Coonan QC for Wakefield. Stephen Miller QC for Walker-Smith. Adrian Hopkins QC for Simon Murch. Sally Smith QC appeared for the GMC. The independent legal assessor, advising the panel, was Nigel Seed QC.
- ↵ The third defendant was Simon Murch, at the time of these events consultant paediatric gastroenterologist at the Royal Free, and now professor of medicine at Warwick University. On 28 January 2010, Day 197, he was found to have misled the Royal Free’s ethics committee, acted contrary to the clinical interests of children, and failed in his duties as a responsible consultant. On 24 May 2010, Day 217, the panel noted that Murch’s involvement with the project was “subsidiary to and more limited” than Wakefield’s and Walker-Smith’s, that he had shown insight into his conduct, and had “demonstrated errors of judgment but had acted in good faith”. He was acquitted of serious professional misconduct.
- ↵ Deer B. MMR doctor fixed data on autism. Sunday Times 2009 Feb 8. www.timesonline.co.uk/tol/life_and_style/health/article5683671.ece .
- ↵ American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders . 4th ed. 1994 .
- ↵ Andrew Wakefield. Evidence to the panel. (a) Day 49. “Q: What did you understand that phrase to mean, ‘pilot study’? A: This refers specifically and exclusively to the Legal Aid Board pilot study. That is, the investigation of five children with Crohn’s disease and five children with regressive autism and gastrointestinal symptoms.” (b) Day 52. “Q: The second aspect concerns the second box down, which is noted ‘Diagnosis’ and you see what you have written there: ‘Regressive autism + ? inflammatory bowel disease’. Again, what did you intend to convey by using that expression on this document? A: Based upon my understanding at the time, that was the likely diagnosis in this child.”
- ↵ Mr Justice Bell. Judgment in the high court, London. Paul Sayers & Ors v SmithKline Beecham & Ors. 19 December 2001 . “The mechanisms all take their point of departure from the demonstrated persistence of measles virus in the body of children with regressive autism.”
- ↵ Andrew Wakefield. Evidence to the House of Representatives committee on government reform. 25-6 April 2001.
- ↵ Michael Rutter. Evidence to the panel. Day 37. Day 39.
- ↵ Dr N. GP records. Day 6.
- ↵ Dr N. GP note. 18 March 1993. Day 6. The record says child 6 received MMR on 15 June 1993.
- ↵ John Trounce. Report. June 1995. Day 6. Child 7 received MMR on 24 November 1995.
- ↵ John Walker-Smith. Letter to Andrew Wakefield. 4 October 1996. Day 41.
- ↵ Filipek PA. Autistic Spectrum Disorders. In Swaiman KF, Ashwal S. Pediatric neurology: principles and practice. 3rd ed. Mosby, 1999 .
- ↵ Panel findings of fact. Page 25.
- ↵ Panel findings of fact. Page 93.
- ↵ Repeated, multiple comparisons between Casson’s documentation shows an exceptional degree of concordance with clinical records generated by consultants.
- ↵ David Casson. Letter to Sian Bennett. May 1997. Day 102.
- ↵ John Walker-Smith. Outpatient history, taken from the mother. 2 October 1996. Day 41. “He had behaviour changes within a week, although the mother has only relatively recently associated the change of behaviour with MMR.”
- ↵ Andrew Wakefield. Letter to Mrs 12. 19 July 1996. Day 28. “Thank you for your letter regarding your son. We have recently taken a profound interest in this subject, particularly in view of the link between bowel problems and Asperger’s Syndrome. I would greatly appreciate if you would mind calling me at the Royal Free before 3rd August and in addition I would like you to seek a referral from your GP to Professor John Walker-Smith, Professor of Paediatric Gastroenterology at the Royal Free Hospital, for investigation.”
- ↵ Gillian Baird, at the Newcomen Centre, Guy’s hospital. September 1996. Day 36.
- ↵ Panel findings of fact. Page 34.
- ↵ Michael Rutter, an expert witness for the GMC, said that there was “no evidence that I could identify” in the child’s records indicating any significant regressive element in his disorder. Day 36.
- ↵ Mrs 12. Evidence to the panel. Day 28.
- ↵ Richard Barr. Letter to Mrs 12. 14 August 1996. Day 28.
- ↵ Mrs 2 ran Allergy-induced Autism, a since-disbanded national group.
- ↵ Panel findings of fact. Page 22 (child 4); page 37 (child 8).
- ↵ An academic pharmacist in Sunderland, England, and JABS.
- ↵ “We identified associated gastrointestinal disease and developmental regression in a group of previously normal children, which was generally associated in time with possible environmental triggers.” This claim was retracted by 10 of the 13 authors in March 2004. (Murch SH, Anthony A, Casson DH, Malik M, Berelowitz M, Dhillon AP, et al. Retraction of an interpretation. Lancet 2004 ; 363 : 750 .) OpenUrl CrossRef PubMed Web of Science
- ↵ Dr Steel. Letter to Dr Sendall. 19 May 1988. Day 6 and Day 36.
- ↵ William Tapsell. GP records. Day 6.
- ↵ Dr Jackson. Letter to health visitor. 1988. Day 6.
- ↵ ENT surgeon. Day 36. “At the age of two years and one month he apparently has a few single words only. He does not seem able to communicate his needs to his mother... Obviously I am more concerned about his increasingly apparent general delay. Mum was asking about this and although initially denying any problem, is obviously concealing quite deep seated worries about him being ‘backward’.”
- ↵ Government vaccine damage payments unit. Request for information. 18 September 1995. Day 36.
- ↵ Consultant geneticist letter. Day 6. “We are not sure whether this deletion is significant at all and certainly there is a very high possibility that it has nothing to do with [child 4’s] autism.”
- ↵ Consultant to consultant letter. Day 6.
- ↵ William Tapsfield. Referral letter to Wakefield. 1 July 1996. Day 41.
- ↵ Panel findings of fact. Page 4.
- ↵ Wheldon Houlsby. Letter to Neela Shabde. 17 February 1995. Day 29. “I was asked to see [Child 8] last year when there was concern about her development generally. When I saw her in clinic at the age of 10½ months I discovered that she had a coarctation, and referred her to the paediatric cardiologists. This was repaired surgically, and she is now well from this point of view. However concern about her development persists.”
- ↵ For reference, according to Medline Plus, from the US National Library of Medicine and the National Institutes of Health, the typical 18 month old “Can say 10 or more words when asked”. According to the Early Identification of Developmental Delay and Disability project, funded by the state of California, at age 15 months, a child typically “uses 4-6 words”, and at 16-18 months “uses 7-20 words”.
- ↵ Michael Rutter. Evidence to the panel. Day 37. “It is the kind of account that one often gets with an autism spectrum disorder. The fact that the child had only two to three words would make one uncertain as to whether this is a true bill or not, in that that is a very small amount of language to lose, but this is the kind of thing that one often sees so that the picture that comes out of all of these records is of a developmental problem that began early, involves language, involves some autistic-like features, quite a lot of hyperactivity, so that there does not seem much doubt that there was some sort of pervasive developmental disorder that could be regarded as falling on the autism spectrum at an earlier point.”
- ↵ Diana Jelley. Referral letter to Wakefield. 3 October 1996. Day 29.
- ↵ Diana Jelley. Note of a telephone call from Mrs 8. 30 September 1996. Day 29.
- ↵ Andrea Barrow. Referral letter to Walker-Smith. 17 May 1996. Day 5.
- ↵ Andrea Barrow. GP record. 4 November 1993. Day 5.
- ↵ Hospital record. 23 October 1996. Day 36.
- ↵ Child 1 was born on 14 January 1993 and received MMR on 19 January 1994.
- ↵ Anthea Barrow. Referral letter. 17 May 1996. “Mr & Mrs 1’s most recent concern is that the MMR vaccination given to their son may be responsible for the autism.” Day 5.
- ↵ John Walker-Smith. Letter to Wakefield. 21 June 1996. Day 36.
- ↵ John Walker-Smith. Letter Andrea Barrow. 21 June 1996. Day 77. Day 102.
- ↵ David Casson. Child 1 admission clerking note. 21 July 1996. Day 24.
- ↵ David Casson. Child 1 discharge summary. 9 August 1996. Day 24.
- ↵ Patent Office. Pharmaceutical composition for regressive behavioural disease. UK patent GB 2 325 856 A. Priority date 6 June 1997. Publication date 9 December 1998.
- ↵ Child 5 was born on 10 December 1988 and received MMR on 10 April 1990.
- ↵ Geoffrey Shillam. GP records. 24 November 1989. Day 11.
- ↵ Dr Williams. Letter to Dr Wilkinson. January 1992. Day 11. Day 36. “At one year he had convulsions which led to a further hospital admission but these appear to have been due to a high fever. From then on his parents noticed a difference in his development and feel that these febrile epileptic seizures continue to the present day... At 10 months of age he was saying mummy and daddy but then became very miserable and appeared to lose ground in his development after he had been in hospital.”
- ↵ Child 9 was born on 11 June 1990 and received MMR in October 1991.
- ↵ Mohsin Malik. Discharge summary. 14 January 1997. Reported in the first statement of Clifford Spratt. Day 23.
- ↵ Trevor Hopkins. GP records. Day 5.
- ↵ (a) Peter Harvey. Neurology record. 5 December 1996. Day 64. “No doubt about relationship with MMR at onset. No doubt of normal earlier development... Parents have no doubt about the relationship with MMR.” (b) David Casson. Discharge summary. 6 December 1996. Day 24. “His parents feel that the onset of his neurodevelopmental symptoms stems from the period two months after having had the MMR vaccination which he received on the 10 April 1990. A few months subsequent to this he started losing his skills.”
- ↵ Mohsin Malik. Discharge letter. 14 January 1997. Reported in the first statement of Clifford Spratt. Day 23. Spratt said: “The letter also informed me that [child 9]’s mother linked his mental regression at age 18-20 months to MMR which he was given at 16 months of age.”
- ↵ Andrew Wakefield. Royal Free form, ordering tests. Day 61. Day 36. “Autistic spectrum disorder and bowel disorder after MMR”. Note also: (a) Legal aid certificate to sue the vaccine’s manufacturer issued 9 October 1996, prior to a first outpatient clinic dated 18 October. (b) Mary Stuart. GP record. 25 July 1996. “Call from Dr Wakefield. Needs colonoscopy B12 absorption tests. History of measles vaccination reaction.” Day 7. Day 64. (c) Mrs 12. Evidence to the panel. Day 28.
- ↵ Dawbarns. Newsletter. February 1996. Day 37. Day 58.
- ↵ The first referral letter for any child in the Lancet series—child 3—was dated 19 February 1996 .
- ↵ Andrew Wakefield. Evidence to the panel. Day 66. “Q: What I am suggesting to you and what I now want to ask you is where you make it clear that the children had come to the Royal Free in the first place, at least in the majority of cases, in the letters that we have looked at, because their parents, or in some cases their doctor through their parents, thought that MMR might have caused the damage? A: That is implicit to anyone reading this paper. When we talk in the discussion about a possibility of a referral, selection bias, in a self-referred group, the group is self-referred because of the symptoms manifest by the children, including the history of a possible exposure to a vaccine or an infection that has led to the problem, and then seeking help from a specific unit. That is explicitly what self-referral means. Inherent in that is, to the reader, those elements of the history of the patient that have caused them to come to that unit. To anyone reading this, we would have considered that to be self-evident. Self-referral on the basis of one or more of the symptoms of gastrointestinal problems, developmental regression and an association with environmental exposure... Q: I asked you why you did not make it clear, as we have seen from the letters that we looked at yesterday, that, at least in the vast majority of cases, these children came in the first place because their parents thought that MMR had caused that condition. You immediately to go a line where you talk about self-referral, but that particular reference does not include the very point that I am asking about, and you say is implicit, namely the association with MMR. How does any reader, whether a scientist, doctor or otherwise, read that into what you say there? A: The patients, children, are self-referred based on their symptoms and their history. That contains the three key elements of an environmental exposure, gastrointestinal problems and developmental regression. That self-referral encapsulates those three elements. That is, I would have thought, evident to any reader.”
- ↵ Deer B. It’s all change as MMR paper reveals key differences from published Lancet study. http://briandeer.com/mmr/lancet-versions.htm
- ↵ Patent Office. Filing receipt. 6 June 1997, published at Deer B. Revealed: the first Wakefield MMR patent describes “safer measles vaccine”. http://briandeer.com/wakefield/vaccine-patent.htm
- ↵ Child 3 was born on 1 January 1990 and received MMR on 1 March 1991.
- ↵ Ajjegowda Shantha. Evidence to the panel. Day 5. “Q: I think the first record of any parental concern in relation to development was when child 3 was 2½ in June 1992... A: Yes.”
- ↵ John Walker-Smith. Letter to Ajjegowda Shantha. 4 April 1996. Day 5.
- ↵ Lewis Rosenbloom. Letter to Dr Oppenheim. “The mother’s main concerns are [child 3’s] lack of speech.” GP records. Day 5.
- ↵ Mr and Mrs 3. Letter to Lewis Rosenbloom. August 1994. Day 36.
- ↵ The family reapplied through Barr, and were granted legal aid.
- ↵ Child 3’s development was plainly delayed from at least a very early point. A consultant letter, written in December 1992, when the boy was almost 3 years old, summarised the history. “He walked at 13 months of age and used 2-3 words of speech until he was 18 months when this left him. He now has lots of unintelligible babble and appears to understand at one word level.” Day 36.
- ↵ Although, in addition to making a legal claim, they also made a claim to the government’s vaccine damage payments unit, prior to referral. Day 36.
- ↵ (a) Ajjegowda Shantha. GP records and evidence to the panel. Day 5. (b) John Walker-Smith. Evidence to the panel. Day 91.
- ↵ Murch S, Thomson M, Walker-Smith J. Author’s reply [letter]. Lancet 1998 ; 351 : 908 . OpenUrl
- ↵ Squires RH and Colletti RB, Indications for pediatric gastrointestinal endoscopy: A medical position statement of the North American Society for Pediatric Gastroenterology and Nutrition. Journal of Pediatric Gastroenterology and Nutrition 1996 ; 23: 107-110.
- ↵ Ian Booth. Evidence to the panel. Day 41. “Looking for inflammatory bowel disease would be a most unusual way of approaching a patient with severe, long-standing constipation.”
- ↵ Afzal N, Murch S, Thirrupathy K, Berger L, Fagbemi A, Heuschkel R. Constipation with acquired megarectum in children with autism. Pediatrics 2003 ; 112 : 939 -42 OpenUrl Abstract / FREE Full Text
- ↵ Deer B. Wakefield MMR-autism sign was recognized for years: as benign finding in children. http://briandeer.com/wakefield/ileal-hyperplasia.htm
- ↵ Turunen S, Karttonen TJ, Kokkonen J. Lymphoid nodular hyperplasia and cow’s milk hypersensitivity in children with chronic constipation. Journal of Pediatrics 2004 ; 145 : 606 -11. OpenUrl CrossRef PubMed Web of Science
- ↵ Deer B. Wakefield’s “autistic enterocolitis” under the microscope. BMJ 2010 ; 340 : 838 -41. OpenUrl
- ↵ Panel findings of fact. Page 70.
- ↵ Histology report for child 3. Printed 13 September 1996.
- ↵ Walker-Smith J. Letter to Ajjegowda Shantha, with revised discharge summary. 31 December 1996. Day 5.
- ↵ Wakefield A. Complaint to the Press Complaints Commission. March 2009 (suspended by the PCC on 10 February 2010 on grounds of non-pursuit by the complainant). http://briandeer.com/solved/wakefield-complaint.pdf
- ↵ Deer B. Vaccine victim: Andrew Wakefield invents a bizarre conspiracy [video]. http://briandeer.com/solved/tall-story.htm
- ↵ Profile: Andrew Wakefield , the man at the centre of the MMR scare. Times 2010 May 24. http://www.timesonline.co.uk/tol/news/uk/article7135099.ece
- ↵ Walker-Smith J. Evidence to the panel. Day 97. “We all rely on trust. I trusted Dr Wakefield.”
- ↵ California Department of Public Health. Pertussis report. 15 December 2010. www.cdph.ca.gov/programs/immunize/Documents/PertussisReport2010-12-15.pdf .
- ↵ NBC News. A dose of controversy. Dateline NBC, with Matt Lauer. 30 August 2009, repeated and updated 30 May 2010.
- Share full article
Advertisement
Supported by
The Morning Newsletter
Vaccine Persuasion
Many vaccine skeptics have changed their minds.

By David Leonhardt
When the Kaiser Family Foundation conducted a poll at the start of the year and asked American adults whether they planned to get vaccinated, 23 percent said no.
But a significant portion of that group — about one quarter of it — has since decided to receive a shot. The Kaiser pollsters recently followed up and asked these converts what led them to change their minds . The answers are important, because they offer insight into how the millions of still unvaccinated Americans might be persuaded to get shots, too.
First, a little background: A few weeks ago, it seemed plausible that Covid-19 might be in permanent retreat, at least in communities with high vaccination rates. But the Delta variant has changed the situation. The number of cases is rising in all 50 states .
Although vaccinated people remain almost guaranteed to avoid serious symptoms, Delta has put the unvaccinated at greater risk of contracting the virus — and, by extension, of hospitalization and death. The Covid death rate in recent days has been significantly higher in states with low vaccination rates than in those with higher rates:
(For more detailed state-level charts, see this piece by my colleagues Lauren Leatherby and Amy Schoenfeld Walker. The same pattern is evident at the county level, as the health policy expert Charles Gaba has been explaining on Twitter.)
Nationwide, more than 99 percent of recent deaths have occurred among unvaccinated people, and more than 97 percent of recent hospitalizations have occurred among the unvaccinated, according to the C.D.C. “Look,” President Biden said on Friday, “the only pandemic we have is among the unvaccinated.”
The three themes
What helps move people from vaccine skeptical to vaccinated? The Kaiser polls point to three main themes.
(The themes apply to both the 23 percent of people who said they would not get a shot, as well as to the 28 percent who described their attitude in January as “wait and see.” About half of the “wait and see” group has since gotten a shot.)
1. Seeing that millions of other Americans have been safely vaccinated.
Consider these quotes from Kaiser’s interviews :
“It was clearly safe. No one was dying.” — a 32-year-old white Republican man in South Carolina “I went to visit my family members in another state and everyone there had been vaccinated with no problems.” — a 63-year-old Black independent man in Texas “Almost all of my friends were vaccinated with no side effects.” — a 64-year-old Black Democratic woman in Tennessee
This suggests that emphasizing the safety of the vaccines — rather than just the danger of Covid, as many experts (and this newsletter) typically do — may help persuade more people to get a shot.
A poll of vaccine skeptics by Echelon Insights, a Republican firm, points to a similar conclusion. One of the most persuasive messages, the skeptics said, was hearing that people have been getting the vaccine for months and it is “working very well without any major issues.”
2. Hearing pro-vaccine messages from doctors, friends and relatives.
For many people who got vaccinated, messages from politicians, national experts and the mass media were persuasive. But many other Americans — especially those without a college degree — don’t trust mainstream institutions. For them, hearing directly from people they know can have a bigger impact.
“Hearing from experts,” as Mollyann Brodie, who oversees the Kaiser polls, told me, “isn’t the same as watching those around you or in your house actually go through the vaccination process.”
Here are more Kaiser interviews:
“My daughter is a doctor and she got vaccinated, which was reassuring that it was OK to get vaccinated.” — a 64-year-old Asian Democratic woman in Texas “Friends and family talked me into it, as did my place of employment.” — a 28-year-old white independent man in Virginia “My husband bugged me to get it and I gave in.” — a 42-year-old white Republican woman in Indiana “I was told by my doctor that she strongly recommend I get the vaccine because I have diabetes.” — a 47-year-old white Republican woman in Florida
These comments suggest that continued grass-roots campaigns may have a bigger effect at this stage than public-service ad campaigns. The one exception to that may be prominent figures from groups that still have higher vaccine skepticism, like Republican politicians and Black community leaders.
3. Learning that not being vaccinated will prevent people from doing some things.
There is now a roiling debate over vaccine mandates , with some hospitals, colleges, cruise-ship companies and others implementing them — and some state legislators trying to ban mandates. The Kaiser poll suggests that these requirements can influence a meaningful number of skeptics to get shots, sometimes just for logistical reasons.
“Hearing that the travel quarantine restrictions would be lifted for those people that are vaccinated was a major reason for my change of thought.” — a 43-year-old Black Democratic man in Virginia “To see events or visit some restaurants, it was easier to be vaccinated.” — a 39-year-old white independent man in New Jersey “Bahamas trip required a COVID shot.” — a 43-year-old Hispanic independent man in Pennsylvania
More on the virus:
Indonesia is the pandemic’s new epicenter , with the highest count of new infections.
After Los Angeles County reinstated indoor mask requirements, the sheriff said the rules were “not backed by science” and refused to enforce them.
The American tennis star Coco Gauff tested positive and will not participate in the Tokyo Olympics.
THE LATEST NEWS
Remote voting in Congress has become a personal and political convenience for House members of both parties.
The Times’s Mark Leibovich profiled Ron Klain , Biden’s chief of staff, whom some Republicans call “Prime Minister Klain.”
Flooding in Western Europe killed at least 183 people, with hundreds still missing . “The German language has no words, I think, for the devastation,” Chancellor Angela Merkel said.
Burned-out landscapes and dwindling water supplies are threatening Napa Valley, the heart of America’s wine industry .
Here’s the latest on the extreme heat and wildfires in the West.
Other Big Stories
A Japanese court sentenced two Americans to prison for helping the former Nissan leader Carlos Ghosn escape from Japan in a box.
Although the Me Too movement heightened awareness of the prevalence of sexual assault, the struggle to prosecute cases has endured.
Mat George, co-host of the podcast “She Rates Dogs,” died after a hit-and-run in Los Angeles. He was 26 .
The green economy is shaping up to be filled with grueling work schedules, few unions, middling wages and limited benefits, The Times’s Noam Scheiber reports .
Several governments use a cyberespionage tool to target rights activists, dissidents and journalists, leaked data suggests.
Tadej Pogacar, a 22-year-old cycling phenom from Slovenia, won his second straight Tour de France .
Bret Stephens and Gail Collins discuss big government .
MORNING READS
Into the woods: Smartphones are steering novice hikers onto trails they can’t handle .
Driven: Maureen Dowd meets Dara Khosrowshahi, Uber’s “weirdly normal” C.E.O.
The Games: Has the world had enough of the Olympics ?
A Times classic: Try this science-based 7-minute workout .
Quiz time: The average score on our most recent news quiz is 8.1 out of 11. See if you can do better .
Lives Lived: Gloria Richardson famously brushed aside a National Guardsman’s bayonet as she led a campaign for civil rights in Cambridge, Md. She died at 99 .
ARTS AND IDEAS
What matters in a name sign.
Shortly after the 2020 presidential election, five women teamed up to assign Vice President-elect Kamala Harris a name sign — the equivalent of a person’s name in American Sign Language.
The women — Ebony Gooden, Kavita Pipalia, Smita Kothari, Candace Jones and Arlene Ngalle-Paryani — are members of the “capital D Deaf community,” a term some deaf people use to indicate they embrace deafness as a cultural identity and communicate primarily through ASL.
Through social media, people submitted suggestions and put the entries to a vote. The result: A name sign that draws inspiration, among other things, from the sign for “lotus flower” — the translation of “Kamala” in Sanskrit — and the number three, highlighting Harris’s trifecta as the first Black, Indian and female vice president.
“Name signs given to political leaders are usually created by white men, but for this one we wanted to not only represent women, but diversity — Black women, Indian women,” Kothari said. Read more about it, and see videos of the signs . — Sanam Yar, a Morning writer
PLAY, WATCH, EAT
What to cook.
Debate ham and pineapple pizza all you want. There’s no denying the goodness of caramelized pineapple with sausages .
What to Watch
Based on books by R.L. Stine, the “Fear Street” trilogy on Netflix offers gore and nostalgia.
“ Skipped History ,” a comedy web series, explores overlooked people and events that shaped America.
Now Time to Play
The pangram from Friday’s Spelling Bee was lengthened . Here is today’s puzzle — or you can play online .
Here’s today’s Mini Crossword , and a clue: Hot tub nozzles (four letters).
If you’re in the mood to play more, find all our games here .
Thanks for spending part of your morning with The Times. See you tomorrow. — David
P.S. Ashley Wu , who has worked for Apple and New York magazine, has joined The Times as a graphics editor for newsletters. You’ll see her work in The Morning soon.
Here’s today’s print front page .
“ The Daily ” is about booster shots. On the Book Review podcast , S.A. Cosby talks about his new novel.
Lalena Fisher, Claire Moses, Ian Prasad Philbrick, Tom Wright-Piersanti and Sanam Yar contributed to The Morning. You can reach the team at [email protected] .
Sign up here to get this newsletter in your inbox .
David Leonhardt writes The Morning, The Times's main daily newsletter. Previously at The Times, he was the Washington bureau chief, the founding editor of The Upshot, an Op-Ed columnist, and the head of The 2020 Project, on the future of the Times newsroom. He won the 2011 Pulitzer Prize for commentary. More about David Leonhardt
February 17, 2021
COVID Vaccines Are Safe and Effective—What the Research Says
As more coronavirus vaccines are rolled out, researchers are learning about the extent and nature of side effects
By Ariana Remmel & Nature magazine

A healthcare worker administers a dose of the Pfizer-BioNTech Covid-19 vaccine at the Sun City Anthem Community Center vaccination site in Henderson, Nevada, U.S., on Thursday, Feb. 11, 2021.
Roger Kisby Getty Images
As people around the world receive COVID-19 vaccines, reports of temporary side effects such as headaches and fevers are rolling in. Much of this was expected—clinical-trial data for the vaccines authorized so far suggested as much. But now that millions of people are vaccinated, compared with the thousands enrolled in early studies, reports of some rare, allergic reactions are surfacing, and questions are arising about whether any deaths are linked to the shots.
There is no question that the current vaccines are effective and safe. The risk of severe reaction to a COVID-19 jab, say researchers, is outweighed by the protection it offers against the deadly coronavirus. Nature looks at what scientists are learning about the frequency and nature of side effects as huge numbers of people report their reactions to physicians and through safety-monitoring systems, such as smartphone apps.
How many people experience common side effects from COVID-19 vaccines?
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
For the two available messenger RNA (mRNA) vaccines—one made by Moderna at Cambridge, Massachusetts, and the other developed through a collaboration between Pfizer in New York City and BioNTech in Mainz, Germany—a significant portion of people experience non-serious reactions, such as injection-site pain, headache and fatigue. These vaccines deliver bits of RNA that code for coronavirus proteins, which the body mounts a response against.
According to data from the US Vaccine Adverse Event Reporting System (VAERS), about 372 out of every million administered doses of the mRNA vaccines lead to a non-serious reaction report. This number is lower than would be expected from clinical-trial data, which indicated that at least 80% of people would experience injection-site pain. Researchers running trials monitor patients closely and record every reaction. VAERS, meanwhile, relies on health-care workers and vaccinated individuals to self-report side effects.
So far, reactions to the mRNA vaccines are similar. These vaccines are administered in a two-dose regimen: the first shot triggers an immune reaction, and the second is a ‘booster’ that strengthens the body’s ability to fight the coronavirus. For the Pfizer–BioNTech vaccine, which has been in use longer than the Moderna vaccine and therefore has generated more data, side effects increase with the second dose.
In the United Kingdom, three million doses of another vaccine, developed by the University of Oxford and pharmaceutical firm AstraZeneca, have been doled out. This vaccine, which also requires a two-dose regimen, contains a inactivated cold-causing adenovirus with genetic instructions for making coronavirus proteins to trigger immunity. According to UK safety-monitoring system the Yellow Card Scheme, about 4,000 doses out of every million administered lead to adverse reactions. Again, clinical-trial data suggest that a higher frequency is more accurate: around 50% of participants had injection-site pain, headache or fatigue, according to data reported to the European Medicines Agency (EMA).
Few people have received a second dose of the Oxford–AstraZeneca vaccine because the United Kingdom used its supplies to administer a first dose to as many people as possible, but clinical-trial data presented to the EMA suggest that side effects of the second shot are milder than those caused by the first.
Safety data for shots rolling out in other parts of the world, such as the COVID-19 vaccines in China, are harder to come by. Preliminary data from clinical trials of the adenovirus-based Sputnik V vaccine in Russia suggest its most common side effects include flu-like symptoms and injection-site reactions.
How does that compare with side effects from an annual flu shot?
At least for the mRNA vaccines, physicians are seeing more side effects than for flu shots, says Helen Chu, an infectious-disease specialist at the University of Washington School of Medicine in Seattle, who directs the Seattle Flu Study. In clinical trials for the Pfizer–BioNTech vaccine, for instance, 75% of participants reported a ‘systemic reaction’, such as headache, fever or chills. In a clinical trial for the common influenza vaccine Flubok Quadravalent, around 34% of participants aged 18–49 had a systemic reaction. Side effects were even less frequent in study participants who were at least 50 years old.
Chu says the mRNA COVID-19 vaccines generate a particularly strong immune response that increases the risk of side effects, although this also means that the vaccines are working. She notes that her second dose of the Pfizer–BioNTech vaccine made her ill. “I got the vaccine, and 6 hours later, I had chills, a high fever, muscle aches and I went to bed for 24 hours,” she says. “Then by 36 hours later, it was totally over and I was back to normal.” But Chu would rather be temporarily ill from a vaccine than deal with COVID-19, “a potentially mortal disease that could kill me”, she says.
Have investigations linked any deaths to a COVID-19 vaccine?
Although some have questioned whether the vaccines have led to deaths, none have been directly attributed to a COVID-19 jab. After 33 elderly care-home residents in Norway died within 6 days of receiving the Pfizer–BioNTech vaccine, investigations by both the Norwegian Medicines Agency and the World Health Organization concluded that these deaths were in line with normal death rates in this age group and that the vaccine is still safe for older people. India's Ministry of Health and Family Welfare reported 27 deaths in the country, but none of these have been linked directly to a COVID-19 vaccine either.
It is “extremely difficult” to definitively link a death to the vaccine itself, says Hilda Bastian, a writer and scientist who specializes in validating evidence-based health claims. That is partially because the deaths reported so far have occurred days or weeks after an injection, making it hard to rule out other circumstances. Another reason is that, right now, clinicians are prioritizing vaccines largely for a population of older people with underlying health conditions. Most of those who have died after vaccination have been in this group, according to reports from the United Kingdom and the United States .
What do researchers know about the rare, but severe, allergic reactions to the vaccines?
The Moderna vaccine elicits about three anaphylactic reactions per million doses administered, and the Pfizer–BioNTech vaccine triggers five reactions per million doses, according to VAERS data . This is a higher rate than most other vaccines—including annual flu shots, which trigger anaphylaxis for only one out of every million doses administered. For the Oxford–AstraZeneca vaccine, 30 cases of anaphylaxis have been confirmed overall so far, out of a little more than 3 million administered doses. Vaccine specialists expect that these rates might change as more shots are administered.
Although some people have required hospitalization, all have fully recovered. Public-health officials advise people with a history of allergies to any of the vaccines’ ingredients not to get a COVID-19 jab.
Unlike COVID-19, anaphylaxis is treatable with drugs such as epinephrine if caught quickly, says Paul Offit, a vaccine and infectious-disease specialist at the Children’s Hospital of Philadelphia in Pennsylvania, who participated in the US Food and Drug Administration advisory-committee meetings that led the agency to authorize both mRNA vaccines. “I wish that SARS-CoV-2 could be immediately treated with a shot of epinephrine!” he says.
Most of the people who experienced anaphylaxis had reacted to other substances before: about 80% of people who reacted to the Pfizer–BioNTech vaccine, and 86% to the Moderna vaccine, had a history of allergies, according to the US Centers for Disease Control and Prevention.
The specific cause of the anaphylactic reactions remains unknown, but the US National Institute of Allergy and Infectious Diseases told Nature in an e-mail that the agency has designed a clinical trial to determine the underlying mechanism, but did not specify when the trial would begin.
What could be causing the allergic reactions?
Some researchers have had their eye on polyethylene glycol (PEG) as the anaphylaxis-causing agent in the mRNA vaccines. The Moderna and Pfizer–BioNTech vaccines use hollow lipid nanoparticles to store and then deliver their mRNA payload to cells. PEG is linked to the lipids in these particles and, under normal circumstances, helps them to sneak by the immune system. Although PEG-linked molecules are found in a variety of products, such as laxatives and gout medicines, they have been known to cause allergic reactions.
Follow-up studies in people who experienced anaphylaxis could help to determine whether PEG is the culprit, says Samuel Lai, a pharmaco-engineer at the University of North Carolina at Chapel Hill. If blood samples from these people contain anti-PEG antibodies, it could be an indicator, says Lai, but it is as yet unclear how long these proteins remain in the bloodstream after anaphylaxis.
Vaccines that don’t use PEG—such as the not-yet-authorized shot from Johnson & Johnson, which also uses an adenovirus to trigger immunity to the coronavirus—might be a way to vaccinate people with a sensitivity to the polymer, he adds.
Because mRNA vaccines have shown such promise, Ulrich Schubert, a polymer scientist at the University of Jena in Germany, thinks now is the time to invest in developing vaccine-compatible polymers that don’t cause allergic reactions. At the German Research Foundation-funded collaborative research center PolyTarget, where Schubert works, these studies are already in progress. “If we want to be ready for the next pandemic—which will come—we have to start now,” he says.
This article is reproduced with permission and was first published on February 16 2021.

IMAGES
VIDEO
COMMENTS
Argument against Vaccine Mandates. Utilitarianism appeals to us during times of crisis. It offers an enticing solution: do the greatest good, to the greatest number of people. However, the pursuit of utilitarian ideals often challenges the rights of the individual. In the COVID-19 pandemic, the utilitarian argument has been applied to vaccine ...
An additional aspect of vaccines many parents are troubled with is the increase in suggested vaccines for young children. "Today, the CDC recommends that children receive vaccines for 10 diseases — plus the flu vaccine — by age 6, which can mean up to 37 separate shots. That compares to five vaccines for the same age group in 1995 ...
Background By mid 2023, European countries reached 75% of vaccine coverage for COVID-19 and although vaccination rates are quite high, many people are still hesitant. A plethora of studies have investigated factors associated with COVID-19 vaccine hesitancy, however, insufficient attention has been paid to the reasons why people get vaccinated against COVID-19. Our work aims to investigate the ...
Key Summary Points. The pro- vs anti-vaccine discussion has gained traction in the light of the recent COVID-19 pandemic. In our discussion we review the anti-vaccine movement in its current state, including associated demographics, argumentative patterns, and putative developments. We provide a discussion on the appeal of anti-vaccine ...
The vaccine debate—including the argument as to whether vaccines are safe, effective, or could cause conditions like autism —has received a lot of attention from the media in recent years. With so much conflicting information being publicized, it can be a challenge to discern what is true and what is not.
Several vaccines against COVID-19 have now been developed and are already being rolled out around the world. The decision whether or not to get vaccinated has so far been left to the individual citizens. However, there are good reasons, both in theory as well as in practice, to believe that the willingness to get vaccinated might not be sufficiently high to achieve herd immunity.
Discussion. Although vaccines demonstrate effectiveness against this disease, vaccine hesitancy reveals concerns towards short-term and long-term side effects or adverse reactions such as post-inoculation death. Mandatory vaccination is used to provide herd immunity, but is refutable due to infringement of human rights and autonomy.
The proliferation of anti-vaccination arguments is a threat to the success of many immunization programmes. Effective rebuttal of contrarian arguments requires an approach that goes beyond ...
of vaccines despite availability" (Macdonald, 2015, p. 34). After a thorough literature review, evidence reveals that there is a gap between perceived vaccine importance and perceived vaccine safety in developed nations as many survey respondents believe in the efficacy and importance of vaccines but lack confidence in the safety of vaccines.
Vaccination is widely considered one of the greatest medical achievements of modern civilization. Childhood diseases that were commonplace less than a generation ago are now increasingly rare because of vaccines. In order to be effective at eliminating communicable diseases, vaccines must be administered to sufficient levels of persons in the community.
Psychological profiles of anti-vaccination argument endorsement. We next used Latent Profile Analysis (LPA) to identify different profiles of participants in Sample 2 ( n = 590) based on their ...
When the United States was fighting smallpox long ago, it took mandates to get enough people vaccinated. To eradicate polio, the same was true. Nearly all major infectious diseases in the country ...
When I broke the news to the father of child 11, at first he did not believe me. "Wakefield told us my son was the 13th child they saw," he said, gazing for the first time at the now infamous research paper which linked a purported new syndrome with the measles, mumps, and rubella (MMR) vaccine.1 "There's only 12 in this." That paper was published in the Lancet on 28 February 1998.
Introduction. The COVID-19 pandemic continues, but its potential end is in sight. The first COVID-19 vaccines have been distributed.1 2 Multiple vaccine allocation plans rooted in fair, just and equitable global vaccine allocation aim to maximise the benefits of vaccination programmes.3-6 One common factor in COVID-19 vaccine allocation plans to date is the prioritisation of healthcare ...
Caroline Gutman for The New York Times. 2. Hearing pro-vaccine messages from doctors, friends and relatives. For many people who got vaccinated, messages from politicians, national experts and the ...
There is no question that the current vaccines are effective and safe. The risk of severe reaction to a COVID-19 jab, say researchers, is outweighed by the protection it offers against the deadly ...
A. Vaccines save lives and they can save money too. It's cheaper to prevent a disease than to treat it. The routine childhood immunization in one child saves $13.6 billion in direct cost. Every dollar spent on childhood vaccinations has saved $18.40 (Colorado Children's Immunization Coalition, 2019).
For the Community Interest + Embarrassment message we estimated a 15 percentage point increase (95 % CI: 0.088, 0.209; p < .01, two tailed test,) in a binary intention to advise others to vaccinate outcome, a proportional increase of 27 % compared to the control group baseline of 53 % (0.15/0.53).
Thesis Statement: Research shows that the benefits of vaccination outweigh the risks because vaccines can prevent serious illness and disease in individuals, vaccinations can also prevent widespread outbreaks of diseases in populations and the side effect of vaccinations, though occasionally serious, are vary rare. Don't use plagiarized sources.
250 Words Essay on Vaccination. Vaccination is a cornerstone of public health, crucial in controlling and eradicating infectious diseases. It works by stimulating the body's immune system to recognize and combat pathogens, such as bacteria or viruses, without causing the actual disease. This protective process shields the vaccinated individual ...
Brief History of Vaccine Development. Human use of preparations to prevent specific infections have been described since 1500 AD, beginning in China (Needham, 2000) where smallpox was prevented by variolation, which is the introduction of material from scabs into the skin.In 1796 in the United Kingdom, Edward Jenner observed the immunity to smallpox of milkmaids having previously had natural ...
Topic: To what extent do you support or oppose the governments' mandatory vaccination policies against the Covid-19 pandemic? For more than a year, people from many countries have been living through the peak of the global COVID-19 pandemic around the world, which has caused serious and terrible consequences, because of this, there is now a chase for the development of the necessary vaccines.
The achievements of vaccine research and development bring a hope to our societies that we may cope with the COVID‐19 pandemic. There are two aspects that should be maintained in balance: the immediate necessity for speed of vaccine research and the inherent need for protection of research subjects, which is the foremost concern of research ethics.