- Skip to main content
- Keyboard shortcuts for audio player

How The Pandemic Has Changed The Way We Communicate
NPR's Lulu Garcia-Navarro speaks with Amelia Aldao, a clinical psychologist in New York City, about how the pandemic has impacted the ways we communicate with one another.
LULU GARCIA-NAVARRO, HOST:
Here in the United States, some 1,700 people are still dying every day, and tens of thousands are getting infected. It's been almost a year since the pandemic changed every aspect of our lives and, in particular, the way we communicate. We asked some of you to tell us about how you've talked to the people in your life, what's worked for you over the last year and what hasn't.
JAY DANIELS: Before COVID-19, we would, you know, have our occasional phone calls where I called my parents, like, every Wednesday. And I talked to my sister every once in a while. But the pandemic has changed all that. So we've gone from infrequent communication to now every Friday night, we have a Zoom dinner where the three families can get together, and the grandkids can see each other, and we can talk and have dinner together. We don't ever miss it.
(SOUNDBITE OF MUSIC)
JESSICA LINEHAM: On Thursday, March 20, 2020, my book club was scheduled to meet. Another member suggested we get together on Zoom, something we'd never done before. The rest is history. Since then, we've met up every single Thursday. We don't talk about a book every week, but we do spend a few hours chatting, commiserating and remembering what it's like to see our friends. And while I'm looking forward to getting vaccinated and seeing them in person, I have a feeling we'll keep up our more frequent Zooms, too.
KAREN FREEMAN: I've always really loved writing handwritten letters and receiving them in the mail. So at the beginning of the pandemic, when I was missing my colleagues and friends, I gathered a bunch of postcards and started writing one to someone every day at lunch, someone I was thinking of and missing. And it was a great opportunity to connect with them. I loved receiving notes back and texts and people telling me how much it meant that I was thinking of them.
CLAIRE O'KEEFE: I teach community college, and probably the biggest change that I've witnessed is how the technologies that we rely on for remote learning have this tendency to bring new student voices into the conversation. Traditional face-to-face classes have a way of rewarding one kind of student, the one who's good at speaking extemporaneously and who is comfortable raising their hand. But now I hear from everybody, whether it's via discussion boards or the chat feature. And all of those multiple entry points have this wonderful, magical way of just blowing the class wide open.
CHRIS WELLS: My friends and I always found it hard to get together. And then the pandemic struck last March, and we found ourselves home alone. One thing that we all have in common is that we are Trekkies, meaning we love "Star Trek." And so we got together one night on Zoom and decided to watch an episode of "Star Trek: The Next Generation" together through one of the watch party services. Believe it or not, we've been getting together almost every night since then.
GARCIA-NAVARRO: That was Jay Daniels (ph), Jessica Lineham (ph), Karen Freeman (ph), Claire O'Keefe (ph) and Chris Wells (ph). While technology has been great for some people - and shoutout there to those "Star Trek" fans - there's a lot we do lose through a screen - eye contact, body language, nonverbal cues. We spoke with Amelia Aldao - she's a therapist in New York - about the future of post-pandemic communication. I asked her if we found ways to compensate for what we've lost.
AMELIA ALDAO: To be honest, no. If you actually think about it - right? - we are not necessarily making eye contact. We're looking at the person on the screen, but we're not really looking at the camera. And if we are looking at the camera, we're not actually looking at the person. And that's actually very different, right? It's sort of changing the way in which we are looking into each other. So the eye contact is off.
And I've noticed myself, my clients and also some of my friends as well that then when we go see people in real life, we get a little awkward with the whole eye contact because we're sort of forgetting how to do it outside of the small circle of people that maybe live in our household or that we see regularly. So the eye contact is a big adjustment that we're all going to be facing in the next few months, to be honest.
GARCIA-NAVARRO: So I asked people on Twitter what their experience has been with communicating during COVID, and some people had some really wonderful responses. You know, people are now handwriting each other letters as a reaction against this kind of enforced virtual world that we find ourselves in. They're playing board games virtually. They're talking with family that lives far away more often than they would otherwise. So there is, you know, something positive that we can take away from all this. Do you think we will take away some of this virtual connection when we move forward - there'll be a sort of hybrid?
ALDAO: Yeah, I absolutely think so, and I hope so as well. It is convenient to use all these technologies to communicate, and that's useful. What we're missing by doing things that are efficient - this is usually in general, right? Whenever we optimize for efficiency, we tend to lose depth, and we tend to lose connection. So I think it's going to be finding a balance between using technology so that we can do certain things more efficiently, faster, better and then find time and space to connect with people differently, one-on-one, in the sort of messiness of the real world.
GARCIA-NAVARRO: What do you tell your clients about how they should go back into the world as this pandemic and its effects end?
ALDAO: So the first thing that I tell my clients and my friends and myself and everybody who's willing to listen, to be honest, is that this is not going to be a switch that we turn on and off. Basically, approach this as a quote-unquote "exposure exercise." You know, maybe you grab a coffee with a friend one week. And then maybe two weeks later, you decide to make that into a dinner with a friend or a dinner with a friend and another friend.
So that's what I tell people - be patient. It's going to take a long time. But at the same time, you have to take agency and put yourself out there. And it's going to be awkward. It's going to be difficult. It's going to be anxiety-provoking. But it's really the only path forward. So that's how we're going to get through all of this.
GARCIA-NAVARRO: Dr. Amelia Aldao is a therapist in New York City.
Thank you very much.
ALDAO: Yeah, thank you for having me.
Copyright © 2021 NPR. All rights reserved. Visit our website terms of use and permissions pages at www.npr.org for further information.
NPR transcripts are created on a rush deadline by an NPR contractor. This text may not be in its final form and may be updated or revised in the future. Accuracy and availability may vary. The authoritative record of NPR’s programming is the audio record.
Changes in Digital Communication During the COVID-19 Global Pandemic: Implications for Digital Inequality and Future Research
Affiliation.
- 1 University of Zurich, Switzerland.
- PMID: 34192039
- PMCID: PMC7481656
- DOI: 10.1177/2056305120948255
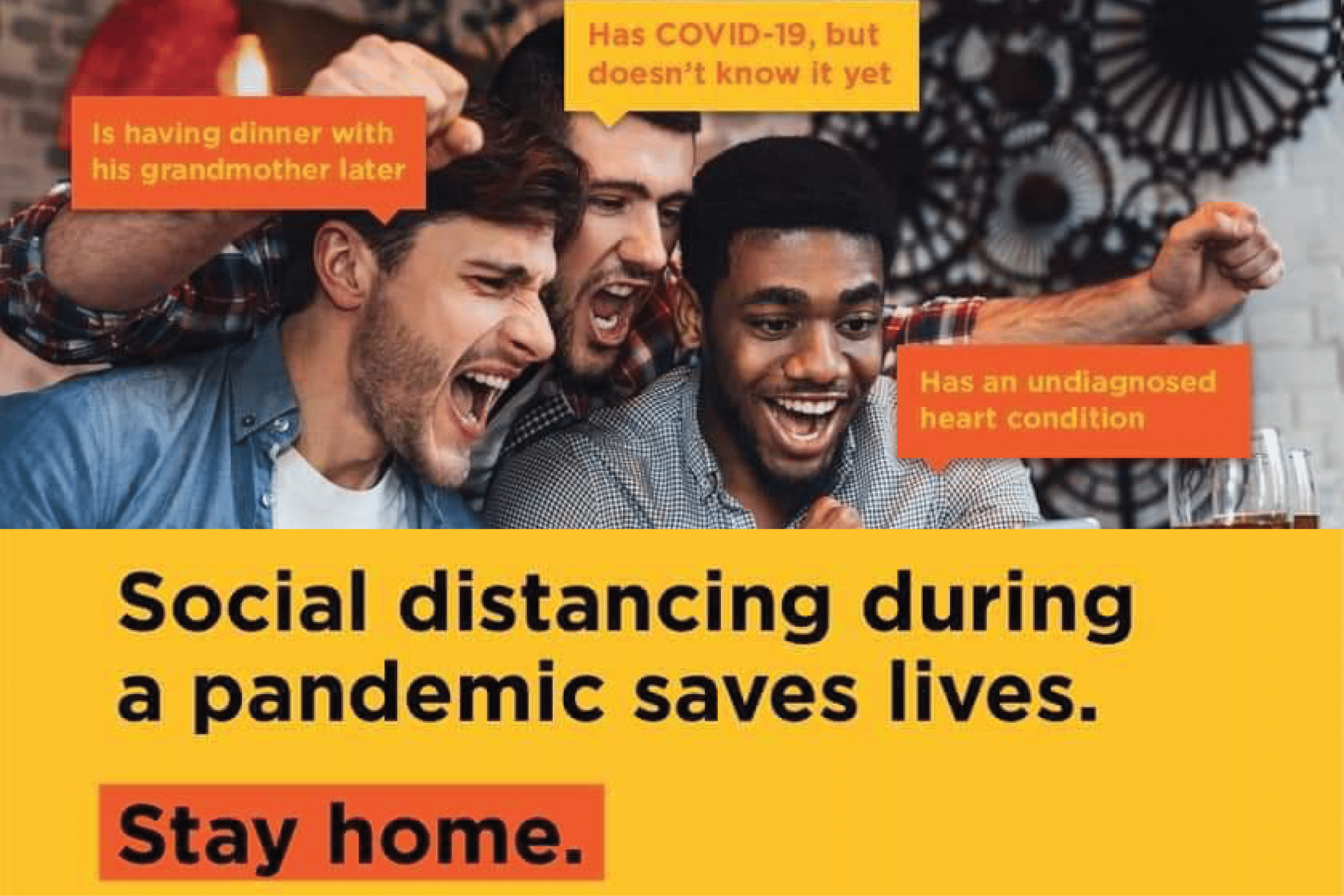
Governments and public health institutions across the globe have set social distancing and stay-at-home guidelines to battle the COVID-19 pandemic. With reduced opportunities to spend time together in person come new challenges to remain socially connected. This essay addresses how the pandemic has changed people's use of digital communication methods, and how inequalities in the use of these methods may arise. We draw on data collected from 1,374 American adults between 4 and 8 April 2020, about two weeks after lockdown measures were introduced in various parts of the United States. We first address whether people changed their digital media use to reach out to friends and family, looking into voice calls, video calls, text messaging, social media, and online games. Then, we show how age, gender, living alone, concerns about Internet access, and Internet skills relate to changes in social contact during the pandemic. We discuss how the use of digital media for social connection during a global public health crisis may be unequally distributed among citizens and may continue to shape inequalities even after the pandemic is over. Such insights are important considering the possible impact of the COVID-19 pandemic on people's social wellbeing. We also discuss how changes in digital media use might outlast the pandemic, and what this means for future communication and media research.
Keywords: COVID-19; digital communication; digital inequality; social connection.
© The Author(s) 2020.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 23 May 2022
The impact of COVID-19 on digital communication patterns
- Evan DeFilippis ORCID: orcid.org/0000-0001-9757-4374 1 ,
- Stephen Michael Impink ORCID: orcid.org/0000-0002-5910-642X 2 ,
- Madison Singell 3 ,
- Jeffrey T. Polzer 1 &
- Raffaella Sadun 1
Humanities and Social Sciences Communications volume 9 , Article number: 180 ( 2022 ) Cite this article
20k Accesses
16 Citations
20 Altmetric
Metrics details
- Business and management
We explore the impact of COVID-19 on employees’ digital communication patterns through an event study of lockdowns in 16 large metropolitan areas in North America, Europe, and the Middle East. Using de-identified, aggregated meeting and email meta-data from 3,143,270 users, we find, compared to pre-pandemic levels, increases in the number of meetings per person (+12.9 percent) and the number of attendees per meeting (+13.5 percent), but decreases in the average length of meetings (−20.1 percent). Collectively, the net effect is that people spent less time in meetings per day (−11.5 percent) in the post-lockdown period. We also find significant and durable increases in length of the average workday (+8.2 percent, or +48.5 min), along with short-term increases in email activity. These findings provide insight into how formal communication patterns have changed for a large sample of knowledge workers in major cities. We discuss these changes in light of the ongoing challenges faced by organizations and workers struggling to adapt and perform in the face of a global pandemic.
Similar content being viewed by others
The effects of remote work on collaboration among information workers
Longqi Yang, David Holtz, … Jaime Teevan

The online language of work-personal conflict
Gloria Liou, Juhi Mittal, … Sharath Chandra Guntuku
The effect of co-location on human communication networks
Daniel Carmody, Martina Mazzarello, … Carlo Ratti
Introduction
The COVID-19 global pandemic disrupted the way organizations function, just as it disrupted life more generally. As the number of infections increased, governments across the globe closed their borders and shut down physical work sites to reduce the spread of infection caused by the virus. By April 7, 2020, 95 percent of Americans were required to shelter-in-place within their homes, similar to the citizens of many other countries. Organizations responded by altering their work arrangements to accommodate these new realities, including a rapid shift to working from home for large segments of knowledge workers. Many workers were forced to work remotely to perform their jobs regardless of how conducive their home environment or task requirements were to such arrangements. Given the large-scale economic and social upheaval wrought by COVID-19, this abrupt transition to remote work occurred at a time when organizational coordination, decision-making processes, and productivity were never more consequential.
This paper provides a large-scale analysis of how formal digital communication patterns changed in the early stages of the pandemic. For all the anecdotes and speculation about working from home during the pandemic, there is still little systematic evidence on how day-to-day work activities changed due to these unexpected shocks. This paper explores, in particular, how the pandemic altered patterns of interactions—measured through a comprehensive set of meeting and email activity metrics—as organizations rapidly moved their activity to remote work. The analysis is based on de-identified meta-data from an information technology services provider that licenses digital communications solutions to organizations worldwide. We use digital meta-data on emails and meetings for 3,143,270 users across 21,478 de-identified firms located in 16 large metropolitan areas, aggregated by the provider to the Metropolitan Statistical Area (MSA) and day across all available firms (see Appendix, Figs. B1 and B2 ). The meta-data provides information on both email and meeting frequency, as well as other salient aspects of digital communications, such as meeting size, meeting duration, the number of email recipients, the time an email was sent, and related dimensions (see Appendix, Table A1 ).
The precise geographical and longitudinal information contained in the communication meta-data allows us to study the evolution of meeting and email activity before and throughout the first stage of the pandemic. To identify the time at which workers presumably shifted to remote work, we selected 16 metropolitan statistical areas (MSAs) that experienced government-mandated lockdowns. These lockdowns established a clear breakpoint, after which we could infer that people were working away from their offices. The earliest lockdown in our data occurred on March 8, 2020, in Milan, Italy, and the latest lockdown occurred on March 25, 2020, in Washington, DC (see Table 1 for more information). We report data from a window starting 8 weeks before the lockdown and ending 8 weeks after the lockdown in each MSA to explore how the behavior of workers changed.
Digital communication and remote work
Theorizing about how employees might have responded to the COVID-19 crisis is challenging for many reasons. First, research conducted before the pandemic examined transitions to remote work that were voluntary, less widespread, and performed under less dramatic circumstances (Bloom et al., 2013 ; Choudhury et al., 2019 ). These circumstances are fundamentally different from the situation that organizations found themselves in shortly after the start of the pandemic.
Second, the few examples of forced transitions to remote work which do exist occurred in the aftermath of acute disasters, such as the Christchurch earthquakes in New Zealand or the 2011 Tōhoku tsunami in Japan (e.g. Donnelly and Proctor-Thomson, 2015 ; Dye et al., 2014 ), rather than a persistent crisis more similar to the COVID-19 pandemic. As a result, these transitions typically involved a smaller fraction of the workforce over a shorter duration, making it harder to generalize from them to the circumstances surrounding the COVID-19 pandemic.
Third, there is scarce prior evidence on digital communication across many firms, even in the absence of a crisis. For example, the nascent literature on the “science of meetings” tends to examine the behavior of a single or handful of firms, or use self-report measures derived from survey responses from a subset of firms or workers, instead of digitally-stored communications data at the scale examined in this paper (e.g. Rogelberg et al., 2006 , 2010 ; Allen et al., 2015 ). While there is a growing body of research examining how digital communications have changed since the pandemic (e.g. Cao et al., 2021 ; Yang et al., 2021 ), these studies tend to examine a single company, making it difficult to generalize results across different organizational features, such as size and industry.
Finally, existing research provides little guidance on how various dimensions of organizational communication activities relate to each other, even though they are likely to be interdependent. For example, meeting count—the number of meetings employees attend in a day—is likely to depend on other dimensions of meeting activity, such as meeting duration or size. Organizations may be reluctant to have meetings that are too long, involve many participants, and occur too frequently, as this may inhibit employees from accomplishing their individual work. Similarly, having infrequent, short, and small meetings may also be suboptimal, as it would limit opportunities for organization-wide coordination on broader tasks. The lack of research about how organizations navigate this balancing act makes it difficult to distill clear hypotheses about how the forced shift to remote work during the pandemic affected the different, interrelated dimensions of communication activity examined in this paper.
Because of the lack of existing theory and the novelty of these widespread, forced transitions to remote work, we do not generate a set of hypotheses. Instead, we summarize what we might infer from adjacent research on the individual variables considered in this paper.
Meeting frequency
The communication literature shows that digital communication is generally less information-dense than face-to-face interaction (Sproull and Kiesler, 1986 ; Daft and Lengel, 1986 ). Because virtual work must take place via “lean” informational channels, such as emails and videoconferences, certain social cues that are readily apprehended in-person can be lost when translated into digital mediums (Denstadli et al., 2012 ; Han et al., 2011 ). According to this reasoning, newly virtual teams adjusting to the pandemic should communicate more frequently via email and meet more often to compensate for the lack of rich social and contextual information previously conveyed through face-to-face interaction (Carletta et al., 2000 ; DeSanctis et al., 1993 ). We can arrive at a similar prediction by examining research on virtual teams, which finds that teams working remotely often suffer from a lack of formal accountability as managers cannot directly observe their employees’ performance (Kurland and Bailey, 1999 ). To compensate for this fact, managers on virtual teams may meet more frequently to ensure that employees accomplish organizational tasks (Maurer, 2020 ; White, 2014 ; Wiesenfeld et al., 1999 , 2001 ).
However, emerging research suggests that an unconditional increase in meeting frequency is unlikely, given that virtual meetings tend to be more cognitively demanding, more prone to distraction, and less effective in many ways than their in-person counterparts (Wiederhold, 2020 ). Adding to this problem are the unique challenges associated with technological adoption, including unanticipated service interruptions and the need for skilled meeting organizers who are fluent in the advanced features of meeting platforms and can resolve issues when they arise (Deakin and Wakefield, 2014 ; Seitz, 2016 ). These issues might offset the inclination to hold more meetings if managers acknowledge the diminishing returns to virtual meetings and modulate their frequency as teams transition remotely (Nardi and Whittaker, 2002 ; Wiederhold, 2020 ).
Meeting size
The literature is equally equivocal when it comes to the topic of meeting size. Research on collaboration, for example, observes that organizations often have different norms and conventions governing average meeting size, and that these norms are important predictors of meeting effectiveness, task performance, and inclusiveness in remote collaboration (Allen et al., 2020 ). But the literature is largely silent on whether these pre-existing organizational differences in meeting norms are likely to be preserved as firms transition remotely, or if organizations will be forced to adopt new norms as employees adjust to working from home. Convincing cases can be made for either prediction. For example, we might expect meetings to become larger as organizations shift to remote work since meeting organizers can be more inclusive about who gets invited to virtual meetings, since they do not have to worry about the physical capacity of meeting rooms. Managers may even see advantages to increasing the total number of people invited to meetings, as the problems that organizations face during this time will likely be relevant to a greater fraction of the workforce.
On the other hand, there are also good reasons to predict that meetings would become smaller as organizations get accustomed to remote work. Managers who use meetings primarily as an accountability tool to check-in with remote employees could increase the frequency of one-on-one meetings, which would drive the average size of meetings downward. Meeting organizers are also likely to consider workers’ attentional limitations, which are exacerbated in larger digital meetings where expectations regarding listening behaviors and interaction are less strict (Lyons and Kim, 2010 ). To mitigate these concerns, managers may opt for smaller meetings to minimize the risk of distraction.
Meeting length
Meeting length is another topic about which the literature is inconclusive. While there is a wealth of research discussing the challenges of long or inefficiently staggered meetings (e.g. Rogelberg et al., 2006 ; Stray et al., 2013 ), there is very little empirical research directly testing the dimension of meeting length, and few theoretical pieces that might inform predictions about what to expect as organizations transition remotely. As with other dimensions of meeting activity, plausible cases can be made for expecting either an increase or a decrease in the average length of meetings that employees attend. For example, employees are likely to have a hard time staying engaged in long virtual meetings (Wiederhold, 2020 ), which may force managers to respond by decreasing the length of meetings to reduce strain on employees’ attention. Similarly, as a greater proportion of meetings are used as a “check-in” tool to enforce employee accountability remotely, we might also expect a decrease in average meeting length, since check-in meetings can be completed in a shorter amount of time than other meeting types (Arnfalk and Kogg, 2003 ).
However, we might also expect the average meeting length to increase for a different set of reasons. For example, organizations may simply face more severe and frequent problems in the middle of a pandemic than they usually do. These problems may require longer meetings to adequately share information and ensure tasks are effectively coordinated across employees. Online meetings may also be less efficient than their in-person counterparts, owing to technical problems, communication challenges, and distractions at home. These inefficiencies may require meeting organizers to schedule relatively longer meetings to accommodate challenges inherent to digital media.
Email activity
The trade-offs entailed in these decisions not only affect meeting activity, but communication activity more broadly. After all, much of the information that is exchanged in meetings could be conveyed in written form via email or other text-based tools. For this reason, our paper also focuses on email activity, which continues to be a prominent channel of communication in many organizations. In the context of this paper, email is a particularly important communication stream because it can act as both a complement to and substitute for meeting activity. Many tasks, for example, can be more efficiently accomplished via email, given its asynchronous, text-based format and the potential for one-to-many communication (Larsen et al., 2008 ). Other tasks which may require significant coordination or a large amount of social context and nuance may be better suited for meetings. The degree to which organizations will rely on emails as a complement to or substitute for meeting activity as they transition remotely remains an open question.
To understand how organizations changed their digital communication patterns in response to the pandemic, we analyzed a large sample of aggregated meeting and email meta-data from 3,143,270 users across 21,478 firms in 16 international cities that have been affected by official lockdown orders, reported in Appendix, Figures B1 and B2 . From this meta-data, our data provider, which licenses digital communications services to organizations around the world, built measures of the communication frequency for email (the average count of distinct, internal, and external emails and the average count of recipients) and meetings (the average count of meetings, average meeting duration, and the average count of attendees per meeting). Additionally, we measured broader changes to work patterns, such as the average length of workday (measured from the first communication to the last communication in a given day), the cumulative number of hours people spent in meetings, and the average number of emails sent outside of regular business hours, reported in the Appendix, Table A1 . More details on our measures are reported in the Appendix, Note A6 .
Our data provider cleaned the data in several ways to increase the likelihood that calendar metadata reflected actual organizational activity. First, they dropped meetings with only one attendee or meetings that lasted longer than 8 h since those meetings overwhelmingly corresponded with out-of-office notices or people blocking out personal time on their calendar rather than formal meeting activity. Next, they excluded meetings with greater than 250 attendees to filter out company-wide notices and spam invitations. Lastly, they only provided internal emails based on correspondence between two employees who shared the same corporate domain address (e.g. @company.com).
The data provider matched meeting and email metadata to a list of metropolitan statistical areas (MSAs). For each MSA in our data, we included the central business district of the cities and surrounding suburbs and townships within the MSA with populations greater than 100,000 people. The 16 major cities included in the sample were selected based on the following criteria: (1) each city must average at least 50,000 active users across 500 firms in the time period examined; (2) each city must have implemented a clear, government-mandated order for non-essential employees to work from home; and (3) these orders had to take effect around the same time (between March 8 and 28) to more explicitly control for time-specific factors related to the organizational response to COVID-19. The third criteria resulted in the exclusion of Asian cities from the analysis since their lockdowns took place at least a month before other major international cities. Each variable used in this analysis was computed by our provider and delivered to us pre-aggregated at the MSA-level. At no point did the research team have access to personally identifiable or user-level data.
In a secondary data set, our provider calculated and shared email communication aggregates at the industry (SIC-1) and organization size level (i.e., small <250 users, medium 250–500 users, large 1000–2500 users, and enterprise 2500+ users) for each of the 16 MSAs included in this study. Our email provider was unable to provide the industry-level data for meeting measures. We use this dataset only to show that our results are consistent across industry and size levels in various robustness tests.
For the main set of results, we used average meeting and email activity aggregated at the MSA level in the post-lockdown period relative to the pre-lockdown period. We used the following specification for our first set of results, which uses a single dummy variable to test the overall difference between pre- and post-lockdown periods for each outcome variable.
To analyze the change in email and meeting measures over different weeks, we used the following specification:
where y i , t are logged email and meeting data at the MSA i and day t level, post is an indicator variable for the period after lockdown, Dτ t is a week indicator variable, relative to the lockdown week, γ i are MSA-level fixed effects, d t are day of the week indicator variables (Monday, Tuesday, Wednesday, etc.), and u i,t is an error-term. Note that MSA-level fixed effects were selected since that was the level at which our communication data was aggregated by our data provider. MSA-level fixed effects control for average differences across MSAs for the outcome of interest, enabling us to report within-MSA changes.
The “lockdown week” is the 7-day period that includes the lockdown date at its center. Every prior and subsequent week indicator is defined relative to that week. The base week for our regression is defined as one week before the lockdown week since many organizations began making arrangements days in advance of official lockdowns based on news of impending policy changes. Email and meeting measures do not display evidence of a pre-trend in the weeks leading up to the base week and lockdown week. All standard errors are clustered at the MSA level (see Tables 2a , b for details).
We use an OLS regression-based event study to examine how these measures vary before and after government-mandated lockdowns. Our method is similar to other approaches in the literature used to evaluate event-related changes in an outcome of interest (e.g. Henderson, 1990 ; Kothari and Warner, 2007 ). We group digital communication measures into three categories of interest: meeting, email, and work–life balance.
We find an increase in the total meeting count (+12.9% [CI: +11.4% to +14.4%], +0.8 meetings per person per day) Footnote 1 , a decrease in the average meeting duration (−20.1% [−23.0% to −17.1%], −12.1 min per meeting), and an increase in the average number of attendees (+13.5% [+10.6% to +16.5%], +2.1 attendees per meeting). Our results suggest that organizations in the post-lockdown period had shorter, more frequent meetings with more attendees than in the prior period. Additionally, we find that the net effect of all these changes was to significantly reduce the total number of hours employees spent in meetings during the post-lockdown period (−11.5% [−14.3% to −8.7%], −18.6 min per person per day). We report these models in the Appendix in Table A2 .
After assessing the overall post-lockdown changes in meeting activities, we conducted more granular tests to understand how these changes unfolded week by week. Using a similar regression specification, but with dummy variables corresponding to each week, we computed the weekly change in digital communication patterns following the enacted lockdown relative to the base week. In this weekly specification, we find consistent increases in the size and count of meetings and consistent decreases in the length of meetings each week after the lockdown date. The cumulative effect of these changes is a decrease in the total amount of hours employees spend in meetings each week after the lockdown date, relative to the base week. We report the coefficients, denoting the weekly changes in communication relative to the base week and corresponding standard errors, in Table 2a , and graph these coefficients in Fig. 1 .
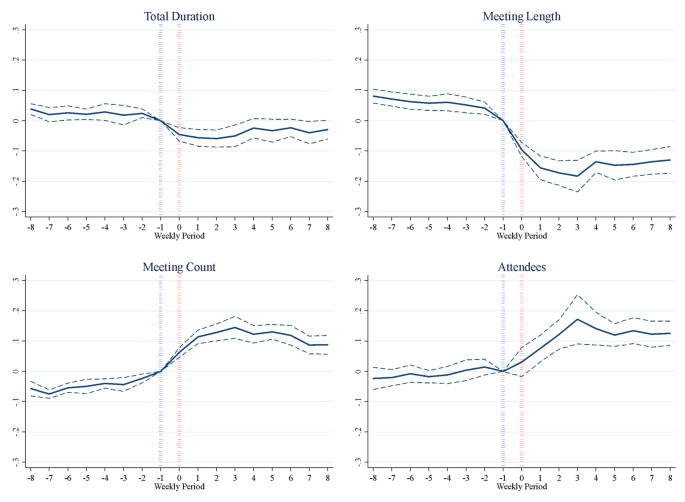
Depiction of the coefficients from Table 2a .
Turning to emails, we find that two types of email communication increased in the post-lockdown period. First, the average number of internal emails sent increased (+5.2% [+3.0% to +7.6%], +1.4 emails per person per day). Additionally, there is a significant increase in the average number of recipients included in emails sent in the post-lockdown period (+2.9% [+0.3% to +5.5%], +0.25 recipients per email sent). However, external emails did not significantly change in the post-lockdown period. We report the coefficients, denoting the weekly changes in communication relative to the base week and corresponding standard errors, in Table 2b , and graph these coefficients in Fig. 2 . To better understand how these results unfold over time, we analyze our main email measures up to nine months after the initial lockdowns. Appendix Table A5 depicts results from our main specification for all email measures, controlling for industry-level fixed effects. We find that, even 9 months after the lockdown, the total number of internal emails sent remains significantly higher than pre-lockdown levels. However, the average number of email recipients appears to return to pre-lockdown levels by the third month. We interpret this as evidence that certain changes to communication activity, such as increases in the total number of emails sent, reflect enduring changes to digital communication that are associated with the semi-permanent adoption of remote work. In contrast, other changes, such as increases in the average number of recipients per email, are less durable and fade in the immediate aftermath of lockdowns.
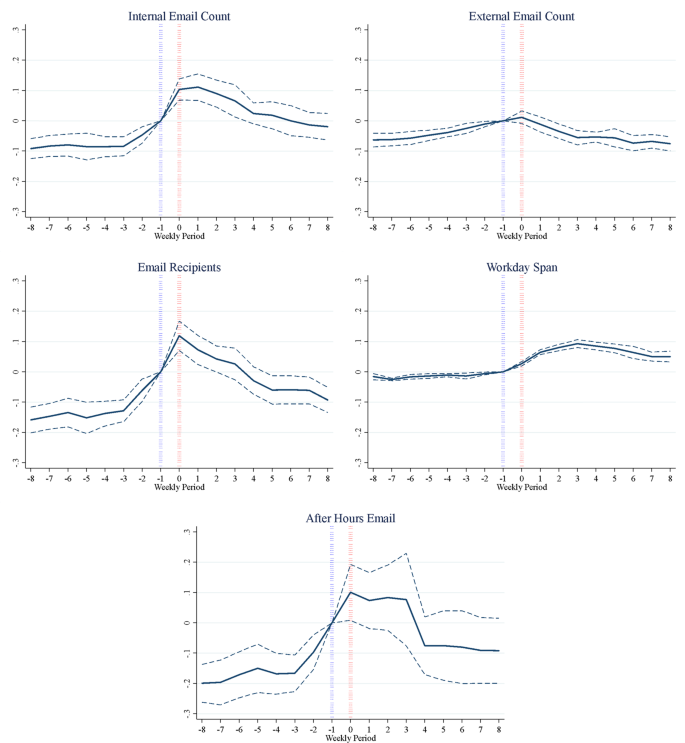
Depiction of the coefficients from Table 2b .
We find that the average workday span, defined as the span of time from the first to the last email sent or meeting attended in a 24-h period, increased by +48.5 min (+8.2% [+7.1% to +9.3%]). Consistent with longer workdays, emails sent after business hours also increased (+8.3% [+4.0% to +12.7%], +0.63 emails per person per day). We report these details in the Appendix in Table A2 . Even in the weekly specification, the employee’s average workday span remains elevated, higher than pre-pandemic levels, for the eight post-lockdown weeks examined in the weekly specification. Furthermore, the total number of emails sent increases steeply the week of the lockdown and then decreases persistently in the weeks after, returning to pre-lockdown levels around week four.
We run numerous analyses with different weighting and aggregation schemes to ensure that our results are consistent across specifications. All results, except for email recipients, are robust to weighting regressions by the total number of users in each MSA, as described in the Appendix in Table A3 . Next, we run additional analyses using weekly instead of daily aggregations, reported in the Appendix in Table A4 . These models are consistent with our main set of findings, regardless of the level of aggregation chosen. Furthermore, in additional analysis (available upon request), we examined whether the changes in communication activity observed in the data were driven by specific sectors of the economy, but found similar responses, both in terms of sign and magnitude, across various industries.
Interestingly, Europe is more negatively impacted by the lockdowns than other cities in our sample when controlling for relevant holidays. However, this could be due to a greater intensity of the lockdown regulations in these areas, disrupting life more in the first two months of the pandemic. It is also possible that pre-existing work–life balance norms in European countries contributed to this result due to a ceiling effect. That is, cities with low baseline levels of communication, perhaps owing to stronger work–life balance norms, have more room to increase their email and meeting activity than cities with higher baseline levels of communication. Lastly, we confirm that the user base remains similar throughout this period and share a graphical depiction of meeting and email users in the Appendix in Figs. B1 and B2 .
Careful inspection of these weekly results reveals that some communication patterns began to change even earlier than one week before the lockdown. To account for this variation, we reran the main analysis, but set the reference category to 8 weeks before the lockdown date to formally test whether meeting and email trends 8 weeks into a lockdown were different from the trends observed 8 weeks before the lockdown. We share these results in the Appendix in Figs. B3 and B4 . With few exceptions, we find that the broad trends in meeting and email activity described above hold regardless of whether the reference week is 8 weeks before the lockdown or one week before the lockdown.
Furthermore, we share additional analysis by MSA and industry. We graph each measure by MSA in the Appendix in Figs. B5 – B14 . Lastly, in Appendix Fig. B15 , we provide an industry analysis showing the heterogeneous effect of industry on email intensity, based on the additional industry-level data provided in the secondary data set. This analysis confirms that our results do not vary much by industry. The only industry differentially affected by the pandemic lockdown is the services industry (excluding financial services). In the services industry, we find that email communication does not recover as quickly as other industries after the lockdown, possibly suggesting a reduction in demand for in-person services.
With the COVID-19 pandemic forcing employees worldwide to work from home, organizations have had to make challenging and urgent decisions about how best to utilize digital communication technology in the absence of a shared physical workspace. Our paper examines two important types of digital communication—meeting and email activity—and shows that on average, employees significantly changed their communication behavior in response to the pandemic. While our results are more descriptive in nature and cannot rule out several competing explanations for the observed findings, the existing literature does help us to identify which explanations are most plausible. Overall, our results suggest that the organizations made communication trade-offs in response to the pandemic, increasing meeting and email activity in terms of frequency and the number of people included, but decreasing the overall time spent doing these activities. While our data cannot speak to whether these changes were due to explicit strategic managerial decisions or a consequence of organizations transitioning to remote work, these patterns are consistent with the idea that virtual forms of communication were leveraged to replace the face-to-face interaction typical in an office setting in a way that might have freed up time for employees to get work accomplished throughout the day.
Though an increase in the quantity of virtual communication is perhaps unsurprising in the middle of a pandemic, the extant literature could not have predicted the specific ways in which this occurred. The literature does, however, help us interpret our findings. For example, despite the potential drawbacks of large meetings or emails with many recipients, these forms of communication practices may help synchronize how information is shared (Allen et al., 2015 ; Cohen et al., 2011 ; Mroz et al., 2018 ). Furthermore, expanding the number of email recipients and meeting attendees increases the likelihood that important information is received by all relevant individuals in an organization (Skovholt and Svennevig, 2006 ).
The hypothesis that organizations were forced to leverage meetings and emails as an imperfect substitute to face-to-face interaction is plausible. Still, one finding that should be explained is why internal emails increased (and remained significantly higher than pre-lockdown levels even 9 months after lockdowns), but external email communication did not. One possibility is that communication turned inward as organizations adapted to remote work. Organizations working remotely for the first time likely have a greater need to use email for internal activities (e.g. synchronizing work activity, enforcing accountability, and communicating information), than for external activities, such as establishing new external partnerships. Another important possibility is that a meaningful amount of external communication in our dataset consisted of mass emails sent out as part of newsletters or promotional campaigns, rather than unique external communication efforts with specific individuals. If these mass emails were automated before the pandemic, and therefore not subject to changes in remote working status, then we would not expect to observe significant increases in external communication.
In addition to observing increases in internal email communication, we also observed important changes to meeting activity. Specifically, we found an increase in the frequency and size of meetings, which can be explained by the fact that virtual work limits opportunities for in-office social engagement and serendipitous information sharing with other employees. Managers may have found it necessary to correct this problem by increasing the frequency of “all-hands” meetings for their teams or departments to overcome feelings of social isolation (Carletta et al., 2000 ; Nilles, 1994 ) and maintain a sense of identification with the organization (Wiesenfeld et al., 1999 ).
The observed decline in meeting length is also consistent with research on virtual teams, which finds that employees find it harder to stay engaged in long, virtual meetings compared to in-person meetings (Wasson, 2004 ; Cummins, 2020 ). Additionally, natural distractions at home which compete for attention, such as demands from family and household responsibilities, may make it even harder to focus during a working day (Cummins, 2020 ; Davis and Green, 2020 ). The collective effect of these demands on attention may have motivated managers to shorten the average length of meetings to avoid overwhelming employees adjusting to working-from-home.
The joint effect of having both an increase in meeting frequency and a decrease in meeting length suggests an interesting possibility that meetings may have become more difficult to coordinate efficiently while organizations adapted to working remotely. A greater quantity of meetings involving a greater number of people implies a substantial requirement for coordination among attendees to schedule these meetings. For at least some of these employees, it would be impossible to schedule meetings consecutively so as to minimize interruption to work activity. From the perspective of employee well-being, the total amount of time spent in meetings is less important than the total number of interruptions (Rogelberg et al., 2006 ). For employees involved in highly interdependent tasks (Barrick et al., 2002 ), an increased quantity of meetings may result in greater distraction and deterioration of well-being over time, even if the net amount of time spent in these meetings is decreasing.
Consistent with this possibility, our findings also point to a spillover of virtual communication beyond normal working hours. Employees worked an average of 48.5 min longer after COVID-19 lockdowns, and were significantly more likely to send emails outside of standard working hours. This points to yet another trade-off organizations should be sensitive to—the decision to expand the scope and frequency of communications, with all its attendant coordination costs, is synonymous with a decision to expand the working day for employees. Even with reduced time spent in meetings, the work demands brought about by the pandemic, coupled with personal demands that are always close at hand, likely made it hard to meet obligations within the bounds of normal working hours.
One explanation for why employees might be working more while working from home comes from research on non-traditional work schedules. This literature has shown that managers have a tendency to view employees who take advantage of flexible working hours as less productive or committed to the organization (Chung, 2020 ; Kaplan et al., 2018 ). Given this perception, employees in virtual teams tend to work longer hours to overcome this “flexibility stigma” and to signal progress on certain assignments by communicating more regularly with managers (Chung, 2020 ; Golden and Eddleston, 2020 ). Another worrying possibility is that workers who would rather not work remotely consider having an office away from their home as essential to keeping their work and personal lives separate. For these workers, working from home may blur the distinction between work and other aspects of their personal life, which may result in them working longer hours without being fully aware of doing so.
Some employees may work a similar amount of time, but spread across an irregular schedule, increasing the span of their workdays. Employees working from home, for example, may decide to take periodic breaks throughout the day to accommodate idiosyncratic demands associated with home life (e.g. childcare, spousal responsibilities, etc.) and compensate for these breaks by working later. Because our measure of the working day is computed by taking the length of time between the first and last meeting or email each day, it does not necessarily capture the total amount or intensity of working time. Despite this caveat, the possibility that employees’ working hours have become less regular is still an important feature of work during the pandemic, as there are well-studied consequences to deviating from formal, organization-wide working schedules (e.g. Piasna, 2018 ; Joshi and Bogen, 2007 ).
In addition to estimating the effects of COVID-related lockdowns on patterns of digital communication, our results also offer a few relevant insights for managers and leaders within organizations. First, our data show that organizations are not merely reactive, but remarkably proactive to external shocks. Organizations of different sizes, in different industries, in different parts of the world, changed their patterns of digital communication at least one full week, on average, before government-imposed lockdowns. That is, our findings show that organizations can (and did) rapidly adjust their communication patterns in anticipation of formal policy requirements or response to local environmental conditions (e.g., the increasing spread of the virus in workplaces.) This degree of responsiveness is surprising when juxtaposed with the literature showing that many organizations can be slow to adapt and change, especially as they become large or are required to respond to rapid political and regulatory change (Woods, 2020 ; Wright et al., 2004 ).
Second, our findings point to the utility of passively collected digital communications data. It is worth noting that this study would not have been possible 20 years ago. Researchers would have had to infer the organizational impact of the crisis via survey data shared from a smaller number of organizations, and such data would have taken months, if not years, to collect. Today, however, because of the widespread use of calendar platforms by organizations that automatically collect communications meta-data, it is now possible to glimpse the impact of any event on organizational communication in real-time (Salganik et al., 2020 ). Because we wanted to ensure our results apply to a large number of organizations, we limited our analysis to broad communication measures shared across organizations worldwide. However, communications data can be collected at a much more granular level than the measures used in this paper. For example, Yang et al. ( 2021 ), in a study that complements our broader approach, examines network data at greater depth for a single firm to show that collaboration networks have become more siloed since the adoption of remote work.
Lastly, our findings have implications for managers by highlighting the importance of considering the trade-offs in organizational communication. Shortly after COVID-related lockdowns were imposed, managers found themselves in charge of newly remote workers and had to decide, in real-time, how best to communicate with employees. Difficult decisions had to be made regarding how many emails to send to employees, how many people to include on meeting invitations, and how frequently to schedule “check-in” meetings to heighten accountability. While our data cannot speak to whether managers consciously made these decisions, our data do show meaningful trade-offs in the dimensions of communication activity. In the context of meetings, organizations varied along different dimensions of meeting activity: the number of meetings, the size of meetings, and the length of meetings. While our paper focuses on the short-term response to the emergency situation created by the pandemic, in the long run, the correct balance of these parameters may vary across organizations. How managers and organizations proactively think about the ideal balance of these parameters (if at all) is an important question for future research.
Limitations
While our data establish that employees changed their email and meeting activity patterns in response to lockdowns, our findings are not without limitations. First, our data only represent a subset of the possible communication occurring within a firm. Non-email communication, such as messaging via consumer or other business communication platforms, and informal meetings not scheduled via calendar invitations, are not reflected in our data. Our analysis does not capture these cross-platform substitutions outside our provider’s data. Therefore, this paper’s findings should be interpreted cautiously as the effect of COVID-19 lockdowns on more formal digital communication patterns, the email and meeting activity facilitated through the company’s communication platform, rather than the net effect of all communication occurring within a firm. As such, other types of communication (e.g. watercooler conversations, instant messenger, phone calls, etc.) were not captured by our email provider’s email and calendar system and were not analyzed in our study. As a result, our analysis may miss important ways in which organizations responded to the pandemic by increasing their use of non-email and meeting channels. For example, organizations might have reacted to the loss of serendipitous in-person conversation by increasing their use of other business communication platforms, like Slack or Microsoft Teams, which are not captured in our data.
A second limitation is that at least three distinct events or phenomena can occur in concert with COVID-related lockdowns: firms transition to remote work, there is a shock to demand due to macroeconomic forces, and behavior is changed for non-work-related reasons. Even controlling for industry and firm size, we cannot disentangle which of these forces is responsible for the effects observed in the paper. As such, the effects documented in the paper should be interpreted as the joint effect of all the forces that co-occur with COVID-19 lockdowns. Related to this, we treat all government-mandated lockdowns as similar in terms of their influence on organizational communication. In reality, firms may have responded to lockdowns in distinct and important ways. For example, Yang et al. ( 2021 ) note that some firms may have adopted a “hybrid work model” in response to the pandemic in which employees spend part of their week working remotely and the other part working in the office. Other organizations are more likely to adopt a “mixed-mode” model in which some employees work remotely full-time, and other employees are full-time office workers. Whether a firm adopted a hybrid working model, a mixed-mode model, or something more extreme has important implications for assessing the impact of remote work on organizational communication.
Third, even though we take great lengths to ensure that calendar data reflects real organizational activity, there is still the possibility that some fraction of our meeting meta-data may not perfectly capture organizational work. For our meeting length variable, a similar problem occurs if a meeting lasts longer or shorter than scheduled on the calendar. The extent to which meeting length, frequency, and size are incorrectly estimated will likely vary substantially across firms, but we have no reason to expect that this bias will vary systematically in a particular direction rendering our estimates unreliable. Measurement error of this sort also does not diminish the practical significance of the results.
Given the unprecedented nature of the changes wrought by COVID-19, it was unclear from the outset how employees would adapt their communication patterns as they transitioned to working from outside their offices. We find that COVID-related lockdowns are associated with: (1) an increase in the total volume of meeting and email activity; (2) a decrease in the average length of meetings; and (3) an increase in the span of the workday. We also found an increase in the average size of meetings and a decrease in the total amount of time spent in meetings after the implementation of COVID-19 lockdowns.
In analyzing digital communication patterns across a large number of firms and regions, we build upon an emerging literature that uses communication meta-data to measure the relationship between patterns of communication and organizational outcomes (Impink et al., 2020 ; Polzer et al., 2018 ; Kleinbaum et al., 2013 ; Srivastava et al., 2018 ). More substantively, we contribute to the literature on virtual work, which has traditionally focused on the impact to organizations when a small subset of employees voluntarily transition to remote work (e.g., Bloom et al., 2013 ; Choudhury et al., 2019 ). Our findings clarify how core communicative functions in an organization change when remote work is implemented under less auspicious conditions—when the transition is mandatory and involves entire organizations.
Data availability
Please contact the corresponding author: Jeffrey Polzer ([email protected]) to be provided with information on how to contact the email provider in our study to apply for access to use the data or to be provided with the code (R and STATA) used to run our analyses.
The details reported in parentheticals are the following: the percentage change of the outcome variable compared to pre-lockdown levels computed from the regression, the 95% confidence interval for this percentage change, and the raw change in the outcome variable in its original units.
Allen TD, Golden TD, Shockley KM (2015) how effective is telecommuting? Assessing the status of our scientific findings. Psychol Sci Public Interest 16(2):40–68. https://doi.org/10.1177/1529100615593273
Article PubMed Google Scholar
Allen JA, Lehmann-Willenbrock N, Rogelberg SG (Eds) (2015) The Cambridge handbook of meeting science. Cambridge University Press, New York, NY
Google Scholar
Allen JA, Tong J, Landowski N (2020) Meeting effectiveness and task performance: meeting size matters. J Manag Dev. https://doi.org/10.1108/JMD-12-2019-0510
Arnfalk P, Kogg B (2003) Service transformation—managing a shift from business travel to virtual meetings. J Clean Prod 11(8):859–872. https://doi.org/10.1016/S0959-6526(02)00158-0
Article Google Scholar
Barrick MR, Stewart GL, Piotrowski M (2002) Personality and job performance: test of the mediating effects of motivation among sales representatives. J Appl Psychol 87(1):43–51. https://doi.org/10.1037/0021-9010.87.1.43
Bloom N, Liang J, Roberts J, Ying ZJ (2013) Does working from home work? Evidence from a Chinese experiment (No. w18871 ) . National Bureau of Economic Research. https://doi.org/10.3386/w18871
Cao H, Lee C-J, Iqbal S, Czerwinski M, Wong PNY, Rintel S, Hecht B, Teevan J, Yang L (2021) Large scale analysis of multitasking behavior during remote meetings. In: Association for Computer Machinery (ACM) (eds), Proceedings of the 2021 CHI conference on human factors in computing systems. Association for Computing Machinery, pp. 1–13.
Carletta J, Anderson AH, McEwan R (2000) The effects of multimedia communication technology on non-collocated teams: a case study. Ergonomics 43(8):1237–1251. https://doi.org/10.1080/00140130050084969
Article CAS PubMed Google Scholar
Choudhury P, Foroughi C, Larson B (2019). Work-from-anywhere: the productivity effects of geographic flexibility. SSRN Electron J. https://doi.org/10.2139/ssrn.3494473
Chung H (2020) Gender, flexibility stigma and the perceived negative consequences of flexible working in the UK. Soc Indic Res 151(2):521–545. https://doi.org/10.1007/s11205-018-2036-7
Cohen MA, Rogelberg SG, Allen JA, Luong A (2011) Meeting design characteristics and attendee perceptions of staff/team meeting quality. Group Dyn: Theory Res Pract 15(1):90–104. https://doi.org/10.1037/a0021549
Cummins E (2020). Why you can’t help screwing around while working from home. Vox. https://www.vox.com/the-highlight/21317485/work-from-home-coronavirus-covid-19-zoom-distraction-animal-crossing
Daft RL, Lengel RH (1986) Organizational information requirements, media richness and structural design. Manag Sci 32(5):554–571. https://doi.org/10.1287/mnsc.32.5.554
Davis M, Green J (2020) Three hours longer, the pandemic workday has obliterated work–life balance. Bloomberg.Com. https://www.bloomberg.com/news/articles/2020-04-23/working-from-home-in-covid-era-means-three-more-hours-on-the-job
Deakin H, Wakefield K (2014) Skype interviewing: reflections of two PhD researchers. Qual Res 14(5):603–616. https://doi.org/10.1177/1468794113488126
Denstadli JM, Julsrud TE, Hjorthol RJ (2012) Videoconferencing as a mode of communication: a comparative study of the use of videoconferencing and face-to-face meetings. J Bus Tech Commun 26(1):65–91. https://doi.org/10.1177/1050651911421125
DeSanctis G, Poole MS, Dickson GW, Jackson BM (1993) Interpretive analysis of team use of group technologies. J Organ Comput 3(1):1–29. https://doi.org/10.1080/10919399309540193
Donnelly N, Proctor-Thomson SB (2015) Disrupted work: home-based teleworking (HbTW) in the aftermath of a natural disaster (SSRN Scholarly Paper ID 2583246). Social Science Research Network. https://doi.org/10.1111/ntwe.12040
Dye KC, Eggers JP, Shapira Z (2014) Trade-offs in a Tempest: stakeholder influence on hurricane evacuation decisions. Organ Sci 25(4):1009–1025. https://doi.org/10.1287/orsc.2013.0890
Golden TD, Eddleston KA (2020) Is there a price telecommuters pay? Examining the relationship between telecommuting and objective career success. J Vocat Behav 116:103348. https://doi.org/10.1016/j.jvb.2019.103348
Han H, Hiltz SR, Fjermestad J, Wang Y (2011) Does medium matter? A comparison of initial meeting modes for virtual teams. IEEE Trans Prof Commun 54(4):376–391. https://doi.org/10.1109/TPC.2011.2175759
Henderson Jr, GV (1990). Problems and solutions in conducting event studies. J. Risk Insur 282–306.
Impink SM, Prat A, Sadun R (2020) Measuring collaboration in modern organizations. AEA Pap Proc 110:181–186. https://doi.org/10.1257/pandp.20201068
Joshi P, Bogen K (2007) Nonstandard schedules and young children’s behavioral outcomes among working low-income families. J Marriage Family 69(1):139–156
Kaplan S, Engelsted L, Lei X, Lockwood K (2018) Unpackaging manager mistrust in allowing telework: comparing and integrating theoretical perspectives. J Bus Psychol 33(3):365–382. https://doi.org/10.1007/s10869-017-9498-5
Kleinbaum AM, Stuart TE, Tushman ML (2013) Discretion within constraint: homophily and structure in a formal organization. Organ Sci 24(5):1316–1336. https://doi.org/10.1287/orsc.1120.0804
Kothari SP, Warner JB (2007). Econometrics of event studies. In Handbook of empirical corporate finance (pp. 3–36). Elsevier.
Kurland NB, Bailey DE (1999) Telework: The advantages and challenges of working here, there, anywhere, and anytime. Organ Dyn 28(2):53–68. https://doi.org/10.1016/S0090-2616(00)80016-9
Larsen J, Urry J, Axhausen K (2008) Coordinating face-to-face meetings in mobile network societies. Inf Commun Soc 11(5):640–658
Lyons K, Kim H, Nevo, S (2010) Paying attention in meetings: Multitasking in virtual worlds. In First Symposium on the Personal Web, Co-located with CASCON (Vol. 2005, p. 7).
Maurer R (2020) Some companies are making virtual internships work during COVID-19. Remote work. Retrieved, 5 October 2020 from https://www.shrm.org/resourcesandtools/hr-topics/talent-acquisition/pages/remote-virtual-internships-covid19-hr.aspx ).
Mroz JE, Allen JA, Verhoeven DC, Shuffler ML (2018) Do we really need another meeting? The science of workplace meetings. Curr Dir Psychol Sci 27(6):484–491. https://doi.org/10.1177/0963721418776307
Nardi BA, Whittaker S (2002) The place of face-to-face communication in distributed work. In: The MIT Press. Distributed work. Boston Review, pp. 83–110.
Nilles JM (1994) Making telecommuniting happen: a guide for telemanagers and telecommuters. https://trid.trb.org/view/405282
Piasna A (2018) Scheduled to work hard: the relationship between non-standard working hours and work intensity among European workers (2005–2015). Hum Resource Manag J 28(1):167–181
Polzer JT, DeFilippis E, Tobio K (2018) Countries, culture, and collaboration. Acad Manag Proc 2018(1):17645. https://doi.org/10.5465/AMBPP.2018.17645abstract
Rogelberg SG, Leach DJ, Warr PB, Burnfield JL (2006) “Not another meeting!” Are meeting time demands related to employee well-being? J Appl Psychol 91(1):83
Rogelberg SG, Allen JA, Shanock L, Scott C, Shuffler M (2010) Employee satisfaction with meetings: a contemporary facet of job satisfaction. Hum Resource Manag (Published in Cooperation with the School of Business Administration, The University of Michigan and in alliance with the Society of Human Resources Management) 49(2):149–172
Salganik MJ, Lundberg I, Kindel AT, Ahearn CE, Al-Ghoneim K, Almaatouq A, ... & McLanahan S (2020) Measuring the predictability of life outcomes with a scientific mass collaboration. Proceedings of the National Academy of Sciences 117(15):8398–8403
Seitz S (2016) Pixilated partnerships, overcoming obstacles in qualitative interviews via Skype: a research note. Qual Res 16(2):229–235. https://doi.org/10.1177/1468794115577011
Sproull L, Kiesler S (1986) Reducing social context cues: electronic mail in organizational communication. Manag Sci 32(11):1492–1512. https://doi.org/10.1287/mnsc.32.11.1492
Srivastava SB, Goldberg A, Manian VG, Potts C (2018) Enculturation trajectories: language, cultural adaptation, and individual outcomes in organizations. Manag Sci 64(3):1348–1364. https://doi.org/10.1287/mnsc.2016.2671
Skovholt K, Svennevig J (2006) Email copies in workplace interaction. J Comput-Mediat Commun 12(1):42–65
Stray VG, Lindsjørn Y, Sjøberg DI (2013). Obstacles to efficient daily meetings in agile development projects: a case study. In: ACM Woods. Benoît J, Hervé L, Corinne B, Claude G (eds) 2013 ACM/IEEE international symposium on empirical software engineering and measurement. IEEE, pp. 95–102
Wasson C (2004) Multitasking during virtual meetings. Hum Resource Plan 27(4):47
White M (2014) The management of virtual teams and virtual meetings. Bus Inf Rev 31:111–117
Wiederhold BK (2020) Connecting through technology during the coronavirus disease 2019 pandemic: avoiding “zoom fatigue”. Cyberpsychol Behav Soc Netw 23(7):437–438. https://doi.org/10.1089/cyber.2020.29188.bkw
Wiesenfeld BM, Raghuram S, Garud R (1999) Communication patterns as determinants of organizational identification in a virtual organization. Organ Sci 10(6):777–790. https://doi.org/10.1287/orsc.10.6.777
Wiesenfeld BM, Raghuram S, Garud R (2001) Organizational identification among virtual workers: the role of need for affiliation and perceived work-based social support. J Manag 27(2):213–229. https://doi.org/10.1177/014920630102700205
Woods DD (2020) The strategic agility gap: how organizations are slow and stale to adapt in turbulent worlds. In: Human and organisational factors. Springer, Cham, pp. 95–104
Wright G, Van Der Heijden K, Bradfield R, Burt G, Cairns G (2004) The psychology of why organizations can be slow to adapt and change. J General Manag 29(4):21–36
Yang L, Holtz D, Jaffe S, Suri S, Sinha S, Weston J, Joyce C, Shah N, Sherman K, Hecht B, Teevan J (2021) The effects of remote work on collaboration among information workers. Nat Hum Behav 1–12. https://doi.org/10.1038/s41562-021-01196-4 .
Download references
Author information
Authors and affiliations.
Harvard University, Cambridge, USA
Evan DeFilippis, Jeffrey T. Polzer & Raffaella Sadun
New York University, New York, USA
Stephen Michael Impink
Stanford University, Stanford, USA
Madison Singell
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Jeffrey T. Polzer .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Informed consent
Additional information.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
DeFilippis, E., Impink, S.M., Singell, M. et al. The impact of COVID-19 on digital communication patterns. Humanit Soc Sci Commun 9 , 180 (2022). https://doi.org/10.1057/s41599-022-01190-9
Download citation
Received : 18 September 2021
Accepted : 28 April 2022
Published : 23 May 2022
DOI : https://doi.org/10.1057/s41599-022-01190-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
“the magic triangle between bed, office, couch”: a qualitative exploration of job demands, resources, coping, and the role of leadership in remote work during the covid-19 pandemic.
- Elisabeth Rohwer
- Volker Harth
- Stefanie Mache
BMC Public Health (2024)
Emotional, coping factors and personality traits that influenced alcohol consumption in Romanian students during the COVID-19 pandemic. A cross-sectional study
- Cornelia Rada
- Cristina Faludi
- Mihaela Lungu
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
The Role of Crisis Communication in the COVID-19 pandemic
By Anushka Singh
Over the past year, the coronavirus outbreak has created uncertainty, stress, emotional disruption, and more in the world. Businesses and organizations are struggling to provide their stakeholders with the appropriate set of resources to overcome the current crisis. During a crisis, effective communication is essential. Business leaders need to communicate with transparency and empathy consistently. Effective communication helps build trust and hope in organizations and their efforts to adapt to the challenges they face. However, seeing how the world has never seen a crisis quite like this one in the past, leaders, and communicators are struggling to design a crisis communication plan that connects with employees, communities, and other stakeholders. Leaders and communicators need to be careful about the course of action they take while creating crisis plans, making sure it is appropriate, informative, and effective.
Some worthwhile tips for creating a strong crisis plan include:
Making sure all communication efforts are consistent, clear, and continual. A crisis, especially one as long as this pandemic, limits people’s ability to cope with excessive amounts of information. Continual communication efforts reduce fear amongst stakeholder groups and guarantee that these groups have understood the organization’s key messages over time and build trust. With so much negativity in the world, leaders and communicators need to make the messaging as positive, reassuring, and hopeful as possible and remind their stakeholder groups of ways the organization has faced and overcome challenges in the past.
Helping stakeholder groups cope with the emotional disruption that comes along with this crisis. Leaders and communicators should put out frequent messages that focus on helping employees, customers, surrounding communities deal with the global pandemic. Leaders and communicators need to go beyond just focusing on how this crisis impacts the organization – but also focus on the stakeholder groups involved. Through crisis messaging, leaders and communicators should try and build a community and focus on its common social identity. For instance, creating virtual campaigns that allow for employees to interact with one another – outside of work – can encourage employee morale. Additionally, the organization should also focus on ensuring that its messaging with various stakeholder groups is one-to-one and varies between each group.
Reminding stakeholder groups of the organization’s goals and missions. Leaders and communicators need to ensure that all messaging ties back to a deeper sense of purpose. Early on in the crisis, organizations need to emphasize their goals during this pandemic. Oftentimes, especially during a long-drawn crisis, stakeholder groups can lose sight of the overarching purpose of the organization before the crisis. It is important for communicators to remind stakeholders of these missions and goals and work towards achieving them during the crisis. For instance, if an organization prides itself on serving its employees, the crisis plan should involve ways in which the organization can support its employees – like providing them with wellness days, sick leave (with pay), and more.
The unexpected and long-lasting nature of the coronavirus outbreak has led to hesitancy and skepticism when it comes to creating a crisis plan. However, leaders and communicators must remember that everyone is in the same boat with respect to implementing a new kind of crisis plan. Organizations must set aside time, effort, and resources to formulate a well-thought-out, strategic plan which acknowledges the lows, emphasizes the highs, and frames a clear plan for the future.
Source: https://www.mckinsey.com/ business-functions/ organization/our-insights/a- leaders-guide-communicating- with-teams-stakeholders-and- communities-during-covid-19
Share this:

5 Lessons for Communicating About Coronavirus
- March 17, 2020
- By Susan Krenn | Johns Hopkins Center for Communication Programs Executive Director
The coronavirus pandemic has put the business of risk communication front and center. Every day, it seems, we are getting mixed messages from our leaders, messages that differ in their tone and content depending on who is talking.
In a situation full of unknowns, as with the early days of the Ebola outbreak in West Africa five years ago, sometimes communication is all we have. Good communication lets people know what they should do, how they can protect themselves and others and helps them balance their fears with concrete information they can use.
Here are some communication lessons to keep in mind as the coronavirus interrupts life as we know it. So much has already changed, with the closure of schools, restaurants and gyms, many workers being asked to stay away from the office, the cancellation of major life celebrations such as weddings and graduations and directives to keep our distance from one another. What is key is that we focus on how to help one another navigate the way forward.
- Build trust: People need information from sources with expertise and they need to hear from trusted public health experts at regular intervals. If incorrect information is shared, experts need to correct the record quickly to ensure that trust is maintained. And when too much time passes between communications, people tend to fill the void with inaccurate information from unreliable sources. Be honest about what you know – and don’t know – in a crisis.
- Have one set of messages: All spokespeople must be on the same page. This is crucial so that people know exactly what to do to reduce the spread of the virus. Otherwise, people make up their own minds about how to behave – which won’t slow the spread of disease.
- Counter myths and misinformation: Ignoring rumors and hoping that they dissipate on their own is a poor course of action, especially in a crisis. Create a system to dispel myths and correct the record by sharing the clear, accurate messages that experts have agreed on.
- Promote action: In an unprecedented crisis, some people just don’t know what to do and why to do it. Being anxious right now is completely normal, but we need to balance that with the ability to act to prevent paralysis. Giving them concrete things to do calms anxiety and promotes a restored sense of control. We’ve already seen some people change social norms, such as avoiding hugs and handshakes upon greeting. Our trusted leaders need to role model this behavior and talk about what else people can do to protect themselves such as vigorous handwashing, avoiding public events and settings and keeping your distance from others, especially older people who are particularly at risk for complications.
- Be empathetic: We are all in this together and we need communication that reflects this. The unknowns are scary, but helping people understand that they need to take action for the greater good can help foster community.
For more information on the coronavirus:
Subscribe to our monthly newsletter
Related posts.

CCP Launches Campaign to Promote Vaccination During Africa Cup of Nations Tournament

Integrating COVID-19 Vaccines into Basic Health Care
Elderly Heroes Help Fellow Indonesians Get COVID-19 Vaccines
Subscribe to ccp's monthly newsletter.
Receive the latest news and updates, tools, events and job postings in your inbox every month

Privacy Policy
Communication During a Pandemic
Featured Clinical Reviews
- Screening for Atrial Fibrillation: US Preventive Services Task Force Recommendation Statement JAMA Recommendation Statement January 25, 2022
- Evaluating the Patient With a Pulmonary Nodule: A Review JAMA Review January 18, 2022
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
COVID-19 Communication—The Need for Humanity, Empathy, and Grace
- 1 Department of Family Medicine, University of Michigan Medical School, Ann Arbor
On Sunday, November 8, my 69-year-old mother was taken to the emergency department of her local hospital after fainting. She tested positive for coronavirus disease 2019 (COVID-19) 3 days prior and was feeling quite ill. Following her admission, she gave me one job—to send daily updates about her condition to a group of friends and family members. She felt that I could translate the oft-complicated medical information into digestible bits and contextualize this for the myriad recipients. With her request, I became the family’s sole source of information, a mini chief medical information officer, sending out information to about 22 people. My mother’s instructions were clear: send twice-a-day updates on her condition.
After sending my first update, on Sunday evening, the response I received, though well-intentioned, was poorly executed.
“Did you know that in a study published by JAMA this Monday, physicians in Italy reported that 90% of 1300 critically ill patients with COVID-19 were intubated and put on a ventilator; one-quarter died in the ICU; 58% were still in the ICU, and 16% had been discharged?”
I tried to receive the message as it was intended—a show of concern for my mother. Nevertheless, I found it unsettling. I had read these articles and I knew the statistics—as a cancer survivor with an autoimmune disease my mother’s outlook was grim. I took a deep breath and replied, “Thank you for your continued concern, we know how much you love her.”
Responses to my daily updates grew more disconcerting. Three days after she was hospitalized, my mother was struggling to breathe on 100% oxygen. Suddenly everyone was an armchair intensivist.
“My neighbor’s girlfriend’s friend is a nurse and says a lot of people have oxygen saturations in the 70s for days. She's even had a patient 'sat’ in the 40s and do just fine.”
There were requests for blood levels and the type and dosage of her antibiotics. There was an abundance of medical information—but a scarce amount of empathy. My mom’s condition worsened.
“What about the latest experimental drug—the one the president got?”
My replies grew curt: “She’s being given an appropriate course of medications.”
By this time, I had developed an overwhelming desire to scream at the top of my lungs, “ARE YOU KIDDING ME?” “QUIT WATCHING TV!” “QUIT READING MEDICAL JOURNALS!”
Suddenly my small “communications” task had become a full-time job. The unsolicited medical advice and requests for specifics about my mother’s treatment was taking up precious time. I knew I needed to reserve my energy for the communication with her physicians and other health care professionals.
By Thursday, COVID-19 day 7, my mom was transferred to the intensive care unit (ICU); things were not going well. I jumped into my car and drove the 18 hours to Florida, setting up a “base camp” in a hotel directly across from the hospital. Everything became overwhelming. A simple drive to the store to get water and necessities revealed a COVID-19–optional world, where wearing a mask was more of a light suggestion vs a mandate, adding insult to the very real injury of knowing my mother would likely die as a result of someone’s carelessness. I found myself wanting to scream again, this time—“WEAR A MASK!” But I was numb, void of the energy to feel, a single tear making its way in slow descent from my tired eyes to the ground signaling that everything was not OK.
I spent the next 2 days living in the hotel room, unable to visit or even talk to my mother. Her texts would arrive once a day, “It’s getting bad. I don’t think I can do this anymore.” My updates to others stopped. I couldn’t bring myself to respond to ongoing inquiries.
The ICU staff made themselves available to me 24/7 to interpret test results, describe treatment plans, and help me manage expectations and prepare for every stage of treatment. The communication with them was decidedly different from those of my mother’s extended family and friends, and I found solace in my calls with these frontline workers. First, came empathy. At the beginning of each call, I was comforted:
“Hi Lisa, my name is nurse X, and I have the privilege of taking care of your mother today. I just want to tell you how sorry I am that you and your family are going through this.”
Their words struck a different chord, fine-tuned by the experiences of the last year and cognizant of the human in their care, beyond the articles, beyond the statistics. It seems that the physicians and nurses in the ICU remembered a key tenet of medicine— first treat the person, not the disease —this care and attention to the patient, my mother, was also extended to me as a family member.
Fortunately, I have the privilege of working with amazing pulmonary and critical care physicians. Members of the “home team” at my institution were among the kindest. They patiently answered my questions, did not offer unsolicited advice, and did not cite the latest articles or ask for test results, despite the fact that they were well qualified to speak to my mother’s condition. They listened to me weep and held space for me to be vulnerable. I was no longer viewed as their colleague; they understood that I was a scared daughter who desperately wanted to hold her mother.
Those closest to the pandemic, the physicians and nurses on the frontline of caring for seriously ill patients with this unrelenting disease, have been tasked with tapping into the deepest core of their humanity. On a daily basis, they pronounce death, hold the hands of loved ones whose families are precluded from being at the bedside, and witness disparities in outcomes linked to the color of their patients’ skin, disability status, and historical access to health care. Every day, as they enter the wards, instead of becoming immune to the death and despair, they dig deeper. In the middle of the worst crisis of our time, they are back at the bedside delivering medicine with humanity, humility, and grace.
The kindness these “ICU angels” show their patients and families is critical if we are to get through this cruel pandemic. While medicine is important—humanity must come first. Each conversation must begin with empathy and understanding. Over the span of 7 days, I shared some of the most intimate conversations of my life with strangers—the ICU angels who brushed my mother’s hair, shared her tears, and calmed her fears.
In the early morning hours of November 16, COVID-19 day 10, they held her hand, lifted the phone to her ear, and stood in the background bearing witness to the intensely intimate and desperate last words between a mother and daughter. I remained in a hotel room, 50 yards away, never getting to see my mother.
I share more than my mother’s smile and zest for life. I share her genetics and her vulnerability to this virus. As a result, I live in constant fear of contracting COVID-19. I am thankful, however, that should I need medical care I will be surrounded by health care professionals who practice humanity and empathy first.
As the pandemic enters the new year, people are dying in larger numbers than ever before. They often die alone, frightened and away from loved ones. As we head towards the light promised by the availability of vaccines, we must remain vigilant. We must protect ourselves and our communities by taking the recommended precautions. For all the mothers, fathers, and loved ones—please continue to wear a mask, maintain social distance, and wash your hands. But above all, should you find yourself communicating with family about COVID-19, lead with humanity and empathy, not statistics.
Corresponding Author: Lisa M. Meeks, PhD, University of Michigan, Department of Family Medicine, 1018 Fuller St, Ann Arbor, MI 48104 1213 ( [email protected] ).
Conflict of Interest Disclosures: None reported.
Additional Contributions: I thank my colleagues and friends who provided valuable support and medical knowledge during this time: Elizabeth Viglianti, MD, MPH, MSc; Steven Gay, MD, MS; and Caroline Richardson, MD, University of Michigan Medical School; Christopher Moreland, MD, MPH, Dell School of Medicine, University of Texas at Austin; Rahul Patwari, MD, Rush Medical College; and Gilles Pinault, MD, and Lina Mehta, MD, Case Western Reserve University School of Medicine. I thank especially the physicians and ICU nurses at Viera Hospital in Viera, Florida, and the many frontline workers who care for and hold many hands of patients across the world.
See More About
Meeks LM. COVID-19 Communication—The Need for Humanity, Empathy, and Grace. JAMA. 2021;325(8):725–726. doi:10.1001/jama.2021.0119
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Sounds of Silence: How the Pandemic Has Impacted Our Communication Skills
Face-to-face communication and in-person socialization have suffered over the past year.
Pandemic Impact on Communication Skills
Every year since 1927, the month of May has been designated "Better Hearing & Speech Month" to promote awareness about communication disorders and the wide array of effective available treatment opportunities.

Getty Images
Though the month has long passed, the need this year is greater than ever – all year long.
Changes to Our Way of Life
The pandemic has turned our lives upside-down. In early 2020, we had to transition from brick-and-mortar to virtual systems overnight . We jumped from our business offices to working from home and from in-person medical visits to telehealth. We embraced streaming services, takeout from restaurants and virtual holiday celebrations.
The timing of the pandemic was uncanny. Americans actually had the infrastructure to support it; we had become accustomed to online banking, Amazon deliveries and FaceTime chats with our out-of-town friends and relatives.
What a different scenario from 2014, when I came up with my business plan to create a virtual speech therapy company, called Great Speech Inc. Before the pandemic, our ability to conceive life virtually was not on the public's radar and was indeed groundbreaking. Today, telehealth and telemedicine are not only mainstream, but expected.
What we were not prepared for was the infectious nature and deadly capacity of this virus and how it affected face-to-face communication and in-person socialization. We sheltered in place, worked from home and Zoom-schooled our children. We found new ways to connect, share ideas around virtual conference tables and enjoy after-work activities. Our children were jolted from their daily school routines of sitting face-to-face in classrooms, participating in after-school activities and enjoying sleepovers, parties and play dates. With parks closed and field trips canceled, socialization and language development opportunities were unnaturally limited.
Face Coverings Complicate Connection
Beyond the day-to-day disruption, mandatory mask-wearing complicates our ability to communicate even further. Masks can make it hard to breathe, project our voices and use facial expressions to share our emotions.
As social creatures, we naturally crave connections and facial expressions are an essential part of non-verbal communication. It gives us the cues we need to promote conversation and establish and maintain social relationships.
We have all struggled to communicate with a mask. I personally have experienced the stress of making myself understood, particularly in a store with a lot of background noise. For the hearing-impaired, the combination of wearing a mask has been extraordinarily challenging. Unable to lip read, and without the visual cues of nonverbal communication, this segment of the population has been at an extreme disadvantage.
Communication Struggles Are a Universal Crisis
Most of us will bounce back from these challenges. The concern is for those who culturally, financially or geographically have limited access to health care services even during non-pandemic times.
Promoting better speech and hearing awareness is key in addressing these social determinants of health. Resources that enhance quality of life can have a significant influence on population health outcomes.
According to the Centers for Disease Control and Prevention , there are 34.2 million Americans diagnosed with diabetes. The National Institute on Deafness and Other Communication Disorders approximates 46 million Americans experience some form of communication disorder and 37.5 million Americans report having some form of hearing disorder. And these were the numbers before COVID. Yet, "diabetes is associated with substantial clinical and economic burdens" on patients and on the U.S. health care system, while communication disorders are not.
As a country, we spend billions of dollars treating diabetes which is the seventh leading cause of death in the U.S. Perhaps it's the mortality factor which naturally garners more awareness. Though communication disorders may cost the U.S. up to 186 billion dollars per year and may impact an individual's physical, social, educational and vocational health, the awareness is surprisingly limited.
What's Next
We need to create awareness for those who are not in grave danger yet are medically impaired and give a voice to those who cannot effectively speak for themselves.
I strongly suspect we will see the number rise for post-pandemic communication disorders. I have personally seen a dramatic increase in the inquiries in my virtual speech therapy practice; other therapists are reporting a similar increase. Think of the havoc COVID-19 wreaked on the larynx and vocal cords of those who were intubated, the front-line workers who had to work with masks and overuse their voices. Let us not forget those students who were not diagnosed during this school year with a speech or language delay.
The needs for communication remediation are not just limited to COVID-related issues. With the medical advances and increased survival rates of stroke patients, victims of car accidents and others who have sustained traumatic brain injuries, the State of Texas alone has guesstimated a 32% increase in speech therapy demand by 2028.
Awareness and Advocacy Are Key
While promoting awareness is key in remediating the problem of lack of access and the lack of education about the efficacy of virtual speech therapy , advocacy is also needed. Health care professionals should be encouraged to ask questions about communication issues and patients need to be empowered to express their need for services. The addition of communication concerns to the health care provider-patient conversation may be the powerful advocacy tool needed to propel the awareness to the level needed for action.
We are making strides with insurance companies who have been reluctant in the past to cover telehealth services but rose to the occasion during COVID for two reasons:
- One reason was that traditional delivery of services was impossible.
- The other reason is that consumers did not accept denial as the final act, but used it as an opportunity to continue the conversation and broaden the coverage for services.
Demand is one of the driving forces for change. Awareness and advocacy are equal partners.
By raising awareness, increasing demand and promoting advocacy, we can address communication disorders – both those related and unrelated to the pandemic – and promote the promising opportunities available for remediation by the speech and language therapy community.
How to Describe Medical Symptoms

Tags: Coronavirus , speech problems , hearing problems , therapy
Most Popular

Patient Advice

OTC Medicine & Health Products

health disclaimer »
Disclaimer and a note about your health ».
Sign Up for Our 3-Day Guide to Medicare
Confused about Medicare? We can help you understand the different Medicare coverage options available to help you choose the best Medicare coverage for you or a loved one.
Sign in to manage your newsletters »
Sign up to receive the latest updates from U.S News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
You May Also Like
Medicare advantage hmos vs. ppos.
Paul Wynn March 29, 2024
Symptoms of Magnesium Deficiency
Elaine K. Howley March 29, 2024
How Chemotherapy Works
Payton Sy March 28, 2024
Stomach Bloating Causes and Relief
Tamara Duker Freuman and Gretel Schueller March 27, 2024

Medicare vs. Medicaid
David Levine March 27, 2024

Early Signs of Diabetes
Toby Smithson March 26, 2024

How to Request a Hospital Transfer
Elaine K. Howley March 26, 2024

Breastfeeding Tips
Vanessa Caceres March 22, 2024

Does Medicare Cover Home Health Care?
Paul Wynn March 21, 2024


Coming Soon: Best Senior Living Ratings
Ben Harder , Zach Adams and Joshua H. Sandefur March 18, 2024

- Share full article
Advertisement
Supported by
Student Opinion
How Did the Covid-19 Pandemic Affect You, Your Family and Your Community?
This week is the fourth anniversary of the pandemic. What are your most lasting memories? How did it reshape your life — and the world?

By Jeremy Engle
It has been four years since the World Health Organization declared Covid-19 a global pandemic on March 11, 2020. The New York Times writes of the anniversary:
Four years ago today, society began to shut down. Shortly after noon Eastern on March 11, 2020, the World Health Organization declared Covid — or “the coronavirus,” then the more popular term — to be a global pandemic. Stocks plummeted in the afternoon. In the span of a single hour that night, President Donald Trump delivered an Oval Office address about Covid, Tom Hanks posted on Instagram that he had the virus and the N.B.A. announced it had canceled the rest of its season. It was a Wednesday, and thousands of schools would shut by the end of the week. Workplaces closed, too. People washed their hands frequently and touched elbows instead of shaking hands (although the C.D.C. continued to discourage widespread mask wearing for several more weeks). The worst pandemic in a century had begun.
For some people, the earliest days of the pandemic may feel like a lifetime ago; for others, it may feel like just yesterday. But for all of us Covid has indelibly changed our lives and the world. What do you remember about the earliest days of the pandemic? When did it first hit home for you? How did it affect you, your family and your community? What lessons did you learn about yourself and the world?
In “ Four Years On, Covid Has Reshaped Life for Many Americans ,” Julie Bosman writes that while the threat of severe illness and death has faded for many people, the pandemic’s effects still linger:
Jessie Thompson, a 36-year-old mother of two in Chicago, is reminded of the Covid-19 pandemic every day. Sometimes it happens when she picks up her children from day care and then lets them romp around at a neighborhood park on the way home. Other times, it’s when she gets out the shower at 7 a.m. after a weekday workout. “I always think: In my past life, I’d have to be on the train in 15 minutes,” said Ms. Thompson, a manager at United Airlines. A hybrid work schedule has replaced her daily commute to the company headquarters in downtown Chicago, giving Ms. Thompson more time with her children and a deeper connection to her neighbors. “The pandemic is such a negative memory,” she said. “But I have this bright spot of goodness from it.” For much of the United States, the pandemic is now firmly in the past, four years to the day that the Trump administration declared a national emergency as the virus spread uncontrollably. But for many Americans, the pandemic’s effects are still a prominent part of their daily lives. In interviews, some people said that the changes are subtle but unmistakable: Their world feels a little smaller, with less socializing and fewer crowds. Parents who began to home-school their children never stopped. Many people are continuing to mourn relatives and spouses who died of Covid or of complications from the coronavirus. The World Health Organization dropped its global health emergency designation in May 2023, but millions of people who survived the virus are suffering from long Covid, a mysterious and frequently debilitating condition that causes fatigue, muscle pain and cognitive decline . One common sentiment has emerged. The changes brought on by the pandemic now feel lasting, a shift that may have permanently reshaped American life.
As part of our coverage of the pandemic’s anniversary, The Times asked readers how Covid has changed their attitudes toward life. Here is what they said:
“I’m a much more grateful person. Life is precious, and I see the beauty in all the little miracles that happen all around me. I’m a humbled human being now. I have more empathy and compassion towards everyone.” — Gil Gallegos, 59, Las Vegas, N.M. “The pandemic has completely changed my approach to educating my child. My spouse and I had never seriously considered home-schooling until March 2020. Now, we wouldn’t have it any other way.” — Kim Harper, 47, Clinton, Md. “I had contamination O.C.D. before the pandemic began. The last four years have been a steady string of my worst fears coming true. I never feel safe anymore. I know very well now that my body can betray me at any time.” — Adelia Brown, 23, Madison, Wis. “I don’t take for granted the pleasure of being around people. Going to a show, a road trip, a restaurant, people watching at the opera. I love it.” — Philip Gunnels, 66, Sugar Land, Texas “My remaining years are limited. On the one hand, I feel cheated out of many experiences I was looking forward to; on the other hand, I do not want to live my remaining years with long Covid. It’s hard.” — Sandra Wulach, 77, Edison, N.J.
Students, read one or both of the articles and then tell us:
How did the Covid-19 pandemic affect you, your family and your community? How did it reshape your life and the world? What are your most lasting memories of this difficult period? What do you want to remember most? What do you want to forget?
How did you change during this time? What did you learn about yourself and about life? What do you wish you knew then that you know now?
Ms. Bosman writes that some of the people she interviewed revealed that four years after the global pandemic began, “Their world feels a little smaller, with less socializing and fewer crowds.” However, Gil Gallegos told The Times: “I’m a much more grateful person. Life is precious, and I see the beauty in all the little miracles that happen all around me. I’m a humbled human being now. I have more empathy and compassion towards everyone.” Which of the experiences shared in the two articles reminded you the most of your own during and after the pandemic and why? How did Covid change your overall outlook on life?
“The last normal day of school.” “The nursing home shut its doors.” “The bride wore Lululemon.” These are just a few quotes from “ When the Pandemic Hit Home ,” an article in which The Times asked readers to share their memories of the world shutting down. Read the article and then tell us about a time when the pandemic hit home for you.
In the last four years, scientists have unraveled some of the biggest mysteries about Covid. In another article , The Times explores many remaining questions about the coronavirus: Are superdodgers real? Is Covid seasonal? And what’s behind its strangest symptoms? Read the article and then tell us what questions you still have about the virus and its effects.
How do you think history books will tell the story of the pandemic? If you were to put together a time capsule of artifacts from this era to show people 100 years from now, what would you include and why? What will you tell your grandchildren about what it was like to live during this time?
Students 13 and older in the United States and Britain, and 16 and older elsewhere, are invited to comment. All comments are moderated by the Learning Network staff, but please keep in mind that once your comment is accepted, it will be made public and may appear in print.
Find more Student Opinion questions here. Teachers, check out this guide to learn how you can incorporate these prompts into your classroom.
Jeremy Engle joined The Learning Network as a staff editor in 2018 after spending more than 20 years as a classroom humanities and documentary-making teacher, professional developer and curriculum designer working with students and teachers across the country. More about Jeremy Engle
Business communication during the pandemic grew in three key areas
Learn effective messaging techniques for every audience.
You can save this article by registering for free here . Or sign-in if you have an account.
Reviews and recommendations are unbiased and products are independently selected. Postmedia may earn an affiliate commission from purchases made through links on this page.
Article content
This article was created by StackCommerce. While Postmedia may collect a commission on sales through the links on this page, we are not being paid by the brands mentioned.
It’s pretty fair to say that communication is everything to human beings; we’ve been using it— and evolving our language —for possibly millions of years. As the world continues to change, so must our communication style. This is especially important in professional settings, where we can offend people or miscommunicate our intent and lose out on building something great. In a pandemic-upended world, the levels of communication have seen shifts more quickly than usual, so how can you make sure you’re sharing ideas and exchanging messages effectively?
Business communication during the pandemic grew in three key areas Back to video
Subscribe now to read the latest news in your city and across Canada.
- Exclusive articles from Barbara Shecter, Joe O'Connor, Gabriel Friedman, Victoria Wells and others.
- Daily content from Financial Times, the world's leading global business publication.
- Unlimited online access to read articles from Financial Post, National Post and 15 news sites across Canada with one account.
- National Post ePaper, an electronic replica of the print edition to view on any device, share and comment on.
- Daily puzzles, including the New York Times Crossword.
Create an account or sign in to continue with your reading experience.
- Access articles from across Canada with one account.
- Share your thoughts and join the conversation in the comments.
- Enjoy additional articles per month.
- Get email updates from your favourite authors.
Sign In or Create an Account
Internal communication.
In any organization, how a company communicates internally, i.e., manager to employee, C-level to management, etc., is of the utmost importance. Having open and transparent comms throughout the business builds trust and fosters creativity, which in turn impacts profit margins. An easy way to improve communication is by ensuring staff at all levels possess high emotional intelligence, which is something you can foster. The Emotional Intelligence and Decision-Making Bundle teaches everything from conflict management to understanding personality to self-awareness. This training gives you the tools you need to ensure your team is on the same page about everyday tasks, big-picture goals, and interdepartmental relationships.
Public Speaking and Team Motivation
Between misunderstood tone in emails and Slack chats, awkward pauses and interruptions on Zoom meetings, or just plain poor internet connections dropping people out of calls, getting a message across in 2020 was chaotic at times. And then there’s the general sense of uncertainty about job security that made many workers hesitant or anxious about communicating. Speaking to team members with positive energy and using confident communication methods can motivate people and put them at ease in scary times. The Mastering Presentation and Public Speaking Certification Bundle offers indispensable tools that will help you not only perfect your own public speaking and presentation skills but also coach team members through times of change, share these skills with them to build confidence, and make yourself more approachable.
External Communication
How your organization is understood and seen by the world determines its success. Now, more than ever, people want to know your company’s story. Consumers are more aware, more curious, and more selective about who exactly they’re doing business with. Advance your brand and build awareness with the 2020 Complete Digital Copywriting Master Class Bundle . You’ll learn all the most effective ways to market your brand with transparency and secure a good reputation through various copywriting-driven campaigns.
You already know that staying agile is a key aspect of success in the COVID economy; apply that thinking to your brand’s communication style and strengthen your business’s safety net.
Prices subject to change.

'Crying out for relief': Bank of Canada to cut rates more sharply than Fed, says CIBC
Diane francis: why our friends down under are doing so much better than us, posthaste: cash-strapped canadians are taking on side hustles — but many aren't telling the cra, bank of canada says the country faces a productivity 'emergency', home sellers forced to confront new market realities this spring.
This website uses cookies to personalize your content (including ads), and allows us to analyze our traffic. Read more about cookies here . By continuing to use our site, you agree to our Terms of Service and Privacy Policy .
You've reached the 20 article limit.
You can manage saved articles in your account.
and save up to 100 articles!
Looks like you've reached your saved article limit!
You can manage your saved articles in your account and clicking the X located at the bottom right of the article.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Topic Collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Online First
- ‘You just don’t feel like your work goes recognised’: healthcare worker experiences of tension related to public discourse around the COVID-19 pandemic
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0001-5302-3941 George Thomas Timmins 1 ,
- Julia I Bandini 2 ,
- Sangeeta C Ahluwalia 3 ,
- Armenda Bialas 4 ,
- Lisa S Meredith 3 ,
- Courtney Gidengil 2
- 1 Pardee RAND Graduate School , RAND Corporation , Santa Monica , California , USA
- 2 RAND Corporation , Boston , Massachusetts , USA
- 3 RAND Corporation , Santa Monica , California , USA
- 4 RAND Corporation , Pittsburgh , Pennsylvania , USA
- Correspondence to George Thomas Timmins, RAND Corporation, Santa Monica, California, USA; gtimmins{at}rand.org
Objectives To understand the impact of public discourse and reaction around the COVID-19 pandemic on healthcare worker (HCW) experiences and well-being caring for patients with COVID-19.
Methods We conducted 60 min in-depth interviews with 11 physicians and 12 nurses who were providing care to patients with COVID-19 in acute care settings at two health systems in the Western USA. Interviews were conducted in Spring-Summer 2022 using a semi-structured interview protocol that guided respondents through different stages of the pandemic.
Results Three themes emerged from the data around providing care in the unique social context of the COVID-19 pandemic including: (1) public polarisation and disagreement with science; (2) feelings of hope and optimism during the pandemic and (3) the compounded strain of providing care within this unique social context of the pandemic.
Conclusions To prepare for future pandemics, improved public health communications and social-emotional supports for HCWs are critical to ameliorate the physical and emotional impacts related to the social context of modern US pandemic response.
- mental health
- health system
Data availability statement
No data are available. Not Applicable.
https://doi.org/10.1136/leader-2024-000983
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
Healthcare workers (HCWs) such as physicians and nurses have been among those on the frontlines of the COVID-19 pandemic and of the political discourse surrounding the pandemic. Over time, heroic framing of HCWs shifted to more polarised attitudes towards COVID-19 infection and healthcare broadly. Little is known about how HCWs felt and were impacted by the social and political discourse in the USA during the COVID-19 pandemic in which they provided care throughout this highly public pandemic.
WHAT THIS STUDY ADDS
HCWs received comments and experiences public polarisation and disagreement with science within their occupational and in their personal interactions. Yet, many felt hopeful and optimistic during the pandemic from their own clinical progress in treating COVID-19 and the continued improvement in prevention and treatment. Together the interactions between the polarisation and optimism experienced compounded the tensions of providing care within this unique social context of the pandemic.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
These dynamics have resulted in conditions that are physically and emotionally unsafe for HCWs, resulting in HCW burnout, turnover, and trends of suicide and self-harm. Considering the endemic nature of COVID-19 and continued emergence of other disease pandemics, it is clear that pandemic response is at the forefront of healthcare leadership and workers alike. Social-emotional supports through peer interventions like Stress First Aid and structural health system changes including hazard pay for HCWs are critical to ameliorate the physical and emotional impacts on HCWs related to the social context of modern US pandemic response.
Introduction
The COVID-19 pandemic has been arguably one of the most public and politically charged health crises of our time, with an impact on nearly every aspect of social life. Healthcare workers (HCWs) such as physicians and nurses have been among those on the frontlines of the pandemic and of the political discourse surrounding the pandemic. In March 2020 as COVID-19 spread within the USA and hospitals became overwhelmed and crowded with sick patients, the public response was largely positive in terms of support for those on the frontlines. 1 2 The public praised ‘healthcare heroes’ 3 for their bravery and dedication in providing care during the first surge, particularly given the direct risk of becoming infected by COVID-19 themselves and the indirect risk for their loved ones.
Over time, this heroic framing slowly shifted to more polarised attitudes towards COVID-19 infection and healthcare broadly. As COVID-19 became more contained with improved messaging around protective measures and later, vaccine distribution, the public’s diminished perceptions of risks related to COVID-19 infection led to growing anger, resentment and backlash, often at the expense of HCWs themselves. 4 5 Backlash against frontline HCWs were due in part to continued COVID-19 activity restrictions, masking requirements, COVID-19 treatment protocols and most notably, vaccination against COVID-19. 6
Against this social backdrop, physicians and nurses remained hard at work during the slow and often bumpy recovery from peak pandemic conditions with repeated surges, all of which contributed to increasing stress and burnout. 7 Recent work has noted some of the negative responses of the public toward the pandemic stresses within clinical settings, including increases in violence towards HCWs. 8 Studies have also demonstrated the rise of emotional distress and burnout among HCWs, suggesting that the stresses of increased workload and patient backlash have caused long-term concerns for HCW well-being and the future of the healthcare workforce. 9 10
However, little is known about how HCWs felt and were impacted by the social and political discourse in the USA during the COVID-19 pandemic in which they provided care throughout this highly public pandemic. In this paper, we explore the impact of this widespread and varied public discourse on HCW experiences during the pandemic. Drawing from interviews with 23 physicians and nurses working in emergency and critical care settings during the pandemic, we examine the tension, frustration, and growing physical and emotional burdens faced by HCWs caring for patients with COVID-19 in the unique context of intense social and political divisiveness over healthcare. We used a relativist ontological approach 11 that focuses on the perceptions and personally constructed narratives of participants to consider the role of their perceptions of public discourse and polarisation on their overall well-being in the healthcare work environment. Empirical evidence of this political polarisation and negative public discourse has continued to demonstrate credence to these perceived realities as we will demonstrate.
As part of a larger study to evaluate a well-being intervention for HCWs during the COVID-19 pandemic, 12 we invited physicians and nurses working in emergency department or critical care settings from two large academic medical centres in the western part of the USA to participate in a one-on-one interview about HCW perspectives and experiences during the pandemic. Our primary study contact at each of the two medical centres shared a description of the interview effort via email; interested clinicians were asked to contact project team members for further information and if applicable, to consent to and schedule an interview.
Interviews were conducted in the Spring and Summer of 2022, approximately 2 years after the start of the COVID-19 pandemic. We developed the interview protocol to elicit HCW perspectives and experiences at different stages of the pandemic. Prior to beginning the interview protocol, participants were provided a brief description of the study and asked for verbal consent to participate in the interview and to be audio-recorded. We asked interviewees to describe their experiences over the course of the pandemic, probing on specific stages of the pandemic, which enabled us to examine the cumulative impact of working in acute care settings during the pandemic on interviewees over time. Interviews were conducted by two researchers trained in qualitative research by phone or video platform, for example, Microsoft Teams, based on participant preference and were generally 60 min in length. Participants were given a $50 e-gift card for their participation in the interview.
Interviews were transcribed and de-identified, and transcripts were uploaded to Dedoose, a qualitative software programme. We used a rigorous thematic analysis 13 to analyse the interview data, which included identifying emerging patterns within the data. We developed an initial codebook based on emerging themes from the interviews and tested the codebook on a set of five transcripts. The codebook was designed to look for patterns between interviewees but also, to use the longitudinal narrative of the interviews to look for patterns over time. On finalising the codebook, four researchers with extensive experience in qualitative research coded the remaining transcripts and discussed emerging findings throughout the data collection and analysis process. We coded the data simultaneously as data were collected to enable us to identify when data saturation was reached (eg, when no new themes emerged). 14
12 nurses and 11 physicians (four attendings and seven trainees that is, residents or fellows) participated in the interviews. The sample was chosen in order to keep discipline variation limited and to specifically describe the experiences of nurses and physicians in their frontline experiences. Our findings revealed three themes: (1) public polarisation and disagreement with science; (2) feelings of hope and optimism during the pandemic and (3) the compounded strain of providing care within this unique social context of the pandemic.
Public polarisation and disagreement with science
The stress of trying to provide care throughout the COVID-19 pandemic was compounded by highly polarised public discourse amplified by various media sources that often conveyed and reinforced non-evidence-based information. Some interviewees reflected on the conundrum of providing care to unvaccinated patients, especially those who were not vaccinated and severely ill but demanded certain treatments that were not evidence-based:
And so those were always interesting families and patients to encounter who just went, ‘how do you know for sure I had it?’ And then patients were actually watching the news, and we were getting things like ‘we want plasma’. We had a lot of patients at that point demanding therapies that weren’t necessarily the right therapies. (Attending physician) We had people [patients] trying to sue [hospital] to try to make us give ivermectin. But they wouldn’t get that vaccine and we were just like ‘you’re crazy’ and ‘this sucks’, and we’re just like working so hard to keep your family member alive and the family is all unvaccinated … It was very frustrating because like at the beginning we were like ‘oh the heroes, they’re working with nothing and there’s no way to stop this and you guys are amazing’. And then like it kind of polarized, like unexpectedly, it polarized so much that like it was like a political identity to either get the vaccine or not get the vaccine and we’re just like ‘why would you do that?’ (Nurse)
In addition to causing frustration, this constant media coverage further taxed the ability of HCWs to compartmentalise the difficulties they faced in their professional lives. One trainee physician described feeling that rhetoric around ‘healthcare heroes’ was ‘100% meaningless’, especially when science and medicine were concurrently being questioned, leaving them with feelings of being invisible and unheard by the public:
I did not feel any better walking into a hospital with a banner above the wall that said ‘welcome our health care heroes’. … It’s hard, like you’re telling people who have no grasp of really what’s going on to change their way of life for the sake of someone else. And a lot of people just are not willing to change, because they don’t believe. Because they’re skeptical, because they have conspiracy thoughts. So, it’s just such a difficult task and it’s one that we all struggled with. (Trainee physician)
Sources of hope and optimism in the pandemic
Even as providers were faced with this polarisation of information and attitudes in the clinical domain, interviewees also described feelings of hope and optimism when reflecting on different stages of the pandemic. For example, interviewees spoke of increased availability of testing for COVID-19, which eased the stress around caring for patients in the hospital. Notably, the rollout of a vaccine for COVID-19 provided hope for many frontline HCWs who had fewer worries about contracting the virus with the protection from the vaccine. The vaccine was noted not only for this potential of protecting HCWs themselves from the virus, but for its symbolic role as a potential end to the pandemic and ultimately as a pathway to more safely seeing friends and family.
I feel relieved. I feel like there’s something like there’s a vaccine and there’s medications, you have clinical trials going on still like in our ICU to treat COVID cases and we just kind of know what we’re dealing with now and just knowing what you’re dealing with that’s half the battle. (Nurse)
Many interviewees described growing optimism with increased knowledge around how to treat patients with COVID-19, and with new advances based on COVID-19-related needs, such as new innovations in immunology and treatment of long COVID.
After two years of it [pandemic], I think like now when a COVID patient rolls around, I just see it as another patient. You’re not terrified of it. It’s just … it’s just another, just like any other patient. (Nurse) My experience was definitely one of, ‘oh this is great, this is going, hopefully this will help’. Especially when we’re in the thick of it, it was like kind of like a light at the end of the tunnel almost. It was like, ‘okay we’re moving somewhere, we’re not just like seeing these sick people and not having treatments for them’, it was kind of like okay we got the test now, we have the rapid test so we can accurately see who has it. (Nurse)
Clinical improvements in treating patients with COVID-19 throughout the pandemic were also accompanied by HCWs working together during even the most difficult days of the pandemic. Interviewees expressed feelings of collective comradery and resilience, in addition to a sense of professionalism that produced optimism among HCWs. This optimism was also noted in relation to the reduction in charting and documentation that allowed a focus on bedside care and being present with patients.
I want to say that [early pandemic] experience is truly bittersweet. It was bitter for the obvious reasons …. But it was also sweet. It was sweet because it was nice to see a group of people dedicated to the common good … But it was nice and really refreshing to see people really do care and there are people who are willing to put themselves on the line, like older physicians who, if they got COVID during that time, they would be dead. (Trainee physician) It was just nice to see the staff be present again. I think that was the biggest thing. I think it was nice to see actual nursing again. I think there was room for less charting because they relaxed a little bit on that, and nurses got to be at bedside because the patients really needed it. I think we get stuck on charting and everything else that I think ultimately the patients don’t get the quality that they should …. (Nurse)
Compounding stress of social context on healthcare worker experiences during COVID-19
However, the optimism that the physicians and nurses described, was tempered by frustration and stress at various points in the pandemic. Interviewees commonly described frustration due to repeated interactions with patients or family members with ‘anti-vax’ attitudes. Interviewees tended to define such attitudes as those held by individuals who did not receive the COVID-19 vaccine due to personal beliefs about effectiveness or safety, distrust in medicine, religious exemptions or other non-medical reasonings. 15 Some interviewees reported that they viewed unvaccinated patients or families of patients as ‘selfish’ or less deserving of care, while others described the challenge of situations when unvaccinated patients wanted a second chance at life. Both situations created a sense of inner conflict in caring for these patients:
And it was just awful because then you’re put in a position as a provider to see someone who’s unvaccinated, going to be on their deathbed and they’re begging you like, ‘hey I don’t want to die, I don’t want to go on a ventilator, can you just give me the vaccine now?’ And it’s too late like the damage is done. (Trainee physician) It was more like an inner battle of we’re doing the right thing, and everyone is deserving of all attention and to try to still feel sympathetic towards that patient even if they were or were not vaccinated. (Trainee physician)
In addition, some interviewees’ described feelings of disbelief and isolation challenges when interacting with unvaccinated patients and their families, in the face of such staunch opposition to a vaccine that they saw as the primary means of stopping the spread of the virus and, ultimately, ending the pandemic. Some remarked:
There are such staunch ‘Anti-Vaxxers’ or ‘Anti-COVID’ people. I just still can’t wrap my head. We watched one family where they lost two adult children and the dad, and they were proud of being ‘Anti-Vaxxers’ and they didn’t even really believe they died of COVID and we just all sat there in such disbelief … I thought was just so, just mind boggling from a rational perspective. (Attending physician) It was difficult for me to know that we had a vaccine that we could actually get out of this. And again, people were not doing what could have actually helped us out in terms of slaving away in the hospital. (Attending physician)
These compounding stressors led to further strain in HCWs’ ability to do their jobs. Interviewees described needing additional time and effort to connect with and try to change patient beliefs, negotiate arguments based on patient demands for medically unsound treatments, and try to perform additional vaccination education. This added burden was exacerbated by a perceived lack of support from health system leadership and the public. Many interviewees expressed how hard it was to see the earlier sentiments of ‘healthcare heroes’ fade to anger, resentment and outright dismissal by the public even as the pandemic continued. One attending physician commented:
I think it’s been very hard for us to understand how somebody really could go out and protest against something that’s essentially lifesaving. It’s just really hard to understand and the flip side of that is that despite all the suspicion of the health care system as soon as they got sick, there was no problem with them coming to the hospital and occupying our time and resources despite their earlier bad decisions. So, there wasn’t any distrust of the system then, it was ‘please help me’ and ‘I don’t want to die’. But there wasn’t the ability to just go get a vaccine to start with, so that I think contributed to our frustration, our anxiety. (Attending physician)
The findings from this qualitative study of HCW experiences during the pandemic suggest that feelings of hope related to clinical improvements and camaraderie were important and salient, but that there were also challenges of complex, compounded stress related to the backdrop of the pandemic’s unique social context. The polarised and often negative discourse surrounding the COVID-19 pandemic affected HCWs’ ability to care for patients efficiently and effectively, which led to a sense of frustration and tension in the face of an already strained healthcare system.
This negative discourse and associated resentment by patients and the public has contributed to unsafe working conditions for HCWs. 16 17 Recent research suggests that HCWs are facing greater risk of violent outbursts by patients, which has a profound impact not only on the physical safety of HCWs, but on their emotional and psychological health. 18–20 This is likely to further exacerbate the distress and burnout that has been linked to HCW turnover and even trends of self-harm and suicide. 21 22 In addition, similar to COVID-19’s overall impact highlighting and disproportionately affecting black, Asian and minority ethnic (BAME) patients, future research would benefit from looking further at the experiences of BAME clinicians to better understand and address the potentially intensified distress and burnout for this marginalised population. 23 24
Globalisation and the interconnectedness of society at large mean that continued outbreaks are inevitable. 25 As future pandemics emerge, HCWs’ experiences of strain related to public response to COVID-19 and other pathogens are likely to exacerbate the potential for distress and burnout in future public health crises. Continued burnout and the exit of HCWs from their professions—particularly those now prepared for future public health emergencies—would be disastrous for the nation’s ability to recover from future pandemics. HCW well-being is therefore critical not just for HCWs’ themselves, but for ensuring the safety and sustainability of the US health system.
In our interviews, HCWs noted that some key sources of optimism and joy was an increased interconnectedness and pride in working with fellow staff. 26 Steps to support joy in work, as discussed in the IHI Framework for Improving Joy in Work, will foster this type of optimism within daily work life and can be integrated into workflows to promote greater mental health and well-being among HCWs. 27 Additionally, piloting and tailoring available interventions and policies that allow for camaraderie to flourish among coworkers would support this dynamic, though few evidence-based strategies exist. Some of these strategies include train-the-trainer educational and reflection sessions, such as the Stress First Aid programme 12 piloted during the pandemic. Such strategies should allow for increased empathy between HCWs and sharing of experiences to support building of team bonds. 28 29 It is also recommended to provide additional employment benefits for HCWs, such as hazard pay and paid time off to recharge away from work, would provide additional support and demonstrate appreciation for HCWs’ stressful work environments. 30 These efforts would support HCWs as they grapple with tensions created by public discourse; however, larger systemic changes are also clearly needed to optimise HCW well-being. 30
The HCWs that we interviewed noted that the challenges of caring for patients in a stressful and everchanging environment of COVID-19 were exacerbated by continued frustration associated with public, clinical and personal encounters with antiscience movements as well as overall continued failures on the part of the public health system. Stronger approaches to sharing credible public health communication and building trust for scientific and public health sources of information are desperately needed. 31 32 Public health messaging during the COVID-19 pandemic was often inconsistent, and science-based communication was just one voice in an overwhelming array of information, which was often referred to as the ‘infodemic’. 33–35 Improvement of public understanding of evidence and science in future public health emergencies is essential for the future to build greater trust in health and government institutions and limit polarisation in future discourse. 36–39 While necessary supports such as hazard pay and more sufficient time away from work are critical in the short-term, the loss of compartmentalisation and hope for meaning in work requires stronger evidence-based communication on a national scale for the health of the public and well-being of HCWs to serve those future patients.
Limitations
The participants interviewed are not representative of all HCW types; for example, we did not interview respiratory therapists, medical assistants and other members of the healthcare workforce. We sampled from two urban, academic medical centres in the west whose experience of the pandemic will be different from others who work in different settings or in other parts of the country.
These physicians and nurses described their journey retrospectively over the first 2 years of the pandemic and therefore, may suffer from recall bias regarding their thoughts and emotions from the earlier times of the pandemic. While this bias may exist, it is important to note that these recollections are still an important part of HCWs’ continued narrative and mental model of the pandemic that shape HCWs’ ability to continue working and coping with stress.
Better, targeted support for HCWs and improved communications to the public to prevent misinformation and further stress on HCWs is critical. Antiscience ideologies not only directly affect patients’ health, but also affect HCW stress, burnout and patient interactions, as is demonstrated by the results of our interviews. Efforts to leverage current evidence and develop novel, effective health communication strategies that can be implemented prior to a future public health emergency will be essential for improving overall HCW well-being. The healthcare workforce is already taking on greater risk for infection and higher workloads to care for patients in need. Policymakers and public health authorities must work to meet their efforts with evidence-based, effective public health communications and medical trust building at the community, state and federal levels.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
This study involves human participants and was approved by RAND Human Subjects Protection approved (ID: 2020-N0697). Participants gave informed consent to participate in the study before taking part.
Acknowledgments
The COVER-HCW team including the substudy team includes the PIs (CG and LM) and coinvestigators (particularly SCA and JIB for leading this substudy) at the RAND Corporation, as well as our partners at Vizient, Clinical Directors Network (CDN), and Stanford University School of Medicine, and the study's Working Group. The authors are grateful to our partners at Vizient and CDN for their efforts with recruitment during the pandemic. The study team also deeply appreciates the hard work of all participating sites, site leaders, site champions and healthcare workers, particularly during a period of many other challenges. We particularly appreciate those healthcare workers willing to describe their experiences during this difficult time with us and for their willingness to share those stories and experiences with us.
- ↵ The heroism of health workers in the Coronavirus crisis . The New York Times . Available : https://www.nytimes.com/2020/03/26/opinion/letters/coronavirus-health-care.html [Accessed 26 Jan 2023 ].
- ↵ In praise of quarantine clapping . The New York Times . Available : https://www.nytimes.com/2020/04/09/arts/virus-quarantine-clapping.html [Accessed 26 Jan 2023 ].
- Hegland A ,
- Zichettella B , et al
- Allcott H ,
- Conway J , et al
- ↵ Backlash against health care workers adds to pandemic’s physical and emotional toll . CBS Bay Area . Available : https://www.cbsnews.com/sanfrancisco/news/covid-backlash-against-health-care-workers-adds-to-pandemics-physical-and-emotional-toll/ [Accessed 19 Jun 2023 ].
- Zarabian K ,
- Devine K , et al
- van Stekelenburg BCA ,
- De Cauwer H ,
- Barten DG , et al
- Meredith LS ,
- Bouskill K ,
- Chang J , et al
- McLoughlin C ,
- Stillman M , et al
- Rassokha IM
- Farmer CM , et al
- Saunders B ,
- Kingstone T , et al
- Benoit SL ,
- Silvestri MC ,
- Bruno A , et al
- Blanchard J ,
- Bentley SK , et al
- Jeffree MS ,
- Saupin SS , et al
- Tiesman H ,
- Konda S , et al
- Hu X , et al
- Bruffaerts R ,
- Voorspoels W ,
- Jansen L , et al
- World Health Organization
- Cushman E ,
- Munson C , et al
- Swenson S , et al
- Bader-Larsen KS ,
- Cruthirds DF , et al
- Weston LE ,
- Robinson C , et al
- Bridgman A ,
- Merkley E ,
- Loewen PJ , et al
- van der Linden S ,
- Roozenbeek J ,
- Truelove S ,
- Gerste AK , et al
- Batteux E ,
- Bilovich A ,
- Johnson SGB , et al
- Tangcharoensathien V ,
- Calleja N ,
- Nguyen T , et al
- Stenseth NC ,
- Dharmarajan G ,
- Li R , et al
- Crowley DM ,
- Long EC , et al
- Schulz AJ ,
- Mehdipanah R ,
- Chatters LM , et al
Contributors SCA and JIB led the study design, protocol development and interviewing. GTT, AB, JIB and SCA all supported the analysis. GTT led manuscript drafting with significant editing and support from JIB. CG and LM led the parent study which this grew from and also participated in the editing and review of the manuscript. All read, edited and contributed to the manuscript development at various stages in the writing process. GTT acted as the guarantor for this work.
Funding Research reported in this report was funded through a Patient-Centered Outcomes Research Institute (PCORI) Award (PCORI ID: COVID‐2020C2‐10721). Further information available at: https://www.pcori.org/research-results/2020/does-stress-first-aid-program-improve-well-being-among-healthcare-workers-during-covid-19-pandemic-cover-hcw-project
Disclaimer The statements presented in this article are solely the responsibility of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors or Methodology Committee.
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
- Open access
- Published: 20 September 2023
Older adults’ experiences during the COVID-19 pandemic: a qualitative systematic literature review
- Elfriede Derrer-Merk ORCID: orcid.org/0000-0001-7241-0808 1 ,
- Maria-Fernanda Reyes-Rodriguez ORCID: orcid.org/0000-0002-2645-5092 2 ,
- Laura K. Soulsby ORCID: orcid.org/0000-0001-9071-8654 1 ,
- Louise Roper ORCID: orcid.org/0000-0002-2918-7628 3 &
- Kate M. Bennett ORCID: orcid.org/0000-0003-3164-6894 1
BMC Geriatrics volume 23 , Article number: 580 ( 2023 ) Cite this article
1523 Accesses
5 Citations
2 Altmetric
Metrics details
Relatively little is known about the lived experiences of older adults during the COVID-19 pandemic. We systematically review the international literature to understand the lived experiences of older adult’s experiences during the pandemic.
Design and methodology
This study uses a meta-ethnographical approach to investigate the included studies. The analyses were undertaken with constructivist grounded theory.
Thirty-two studies met the inclusion criteria and only five papers were of low quality. Most, but not all studies, were from the global north. We identified three themes: desired and challenged wellbeing; coping and adaptation; and discrimination and intersectionality.
Overall, the studies’ findings were varied and reflected different times during the pandemic. Studies reported the impact of mass media messaging and its mostly negative impact on older adults. Many studies highlighted the impact of the COVID-19 pandemic on participants' social connectivity and well-being including missing the proximity of loved ones and in consequence experienced an increase in anxiety, feeling of depression, or loneliness. However, many studies reported how participants adapted to the change of lifestyle including new ways of communication, and social distancing. Some studies focused on discrimination and the experiences of sexual and gender minority and ethnic minority participants. Studies found that the pandemic impacted the participants’ well-being including suicidal risk behaviour, friendship loss, and increased mental health issues.
The COVID-19 pandemic disrupted and impacted older adults’ well-being worldwide. Despite the cultural and socio-economic differences many commonalities were found. Studies described the impact of mass media reporting, social connectivity, impact of confinement on well-being, coping, and on discrimination. The authors suggest that these findings need to be acknowledged for future pandemic strategies. Additionally, policy-making processes need to include older adults to address their needs. PROSPERO record [CRD42022331714], (Derrer-Merk et al., Older adults’ lived experiences during the COVID-19 pandemic: a systematic review, 2022).
Peer Review reports
Introduction
In March 2020 the World Health Organisation declared a pandemic caused by the virus SARS-CoV2 (COVID-19) [ 1 ]. At this time 118,000 cases in 114 countries were identified and 4,291 people had already lost their lives [ 2 ]. By July 2022, there were over 5.7 million active cases and over 6.4 million deaths [ 2 ]. Despite the effort to combat and eliminate the virus globally, new variants of the virus are still a concern. At the start of the pandemic, little was known about who would be most at risk, but emerging data suggested that both people with underlying health conditions and older people had a higher risk of becoming seriously ill [ 3 ]. Thus, countries worldwide imposed health and safety measures aimed at reducing viral transmission and protecting people at higher risk of contracting the virus [ 4 ]. These measures included: national lockdowns with different lengths and frequencies; targeted shopping times for older people; hygiene procedures (wearing masks, washing hands regularly, disinfecting hands); restricting or prohibiting social gatherings; working from home, school closure, and home-schooling.
Research suggests that lockdowns and protective measures impacted on people’s lives, and had a particular impact on older people. They were at higher risk from COVID-19, with greater disease severity and higher mortality compared to younger people [ 5 ]. Older adults were identified as at higher risk as they are more likely to have pre-existing conditions including heart disease, diabetes, and severe respiratory conditions [ 5 ]. Additionally, recent research highlights that COVID-19 and its safety measures led to increased mental health problems, including increased feelings of depression, anxiety, social isolation, and loneliness, potentially cognitive decline [ 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 ]. Other studies reported the consequences of only age-based protective health measures including self-isolation for people older people (e.g. feeling old, losing out the time with family) [ 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 ].
Over the past decade, the World Health Organisation (WHO) has recognised the importance of risk communication within public health emergency preparedness and response, especially in the context of epidemics and pandemics. Risk communication is defined as “the real-time exchange of information, advice and opinions between experts or officials, and people who face a threat (hazard) to their survival, health or economic or social well-being” ([ 31 ], p5). This includes reporting the risk and health protection measurements through media and governmental bodies. Constructing awareness and building trust in society are essential components of risk communication [ 32 ]. In the context of the pandemic, the WHO noted that individual risk perception helped to prompt problem-solving activities (such as wearing face masks, social distancing, and self-isolation). However, the prolonged perception of pandemic-related uncertainty and risk could also lead to heightened feelings of distress and anxiety [ 31 , 33 ], see also [ 34 , 35 , 36 , 37 ].
This new and unprecedented disease provided the ground for researchers worldwide to investigate the COVID-19 pandemic. To date (August 2022), approximately 8072 studies have been recorded on the U.S. National Library of Medicine ClinicalTrials.gov [ 38 ] and 12002 systematic reviews have been registered at PROSPERO, concerning COVID-19. However, to our knowledge, there is little known about qualitative research as a response to the COVID-19 pandemic and how it impacted older adults’ well-being [ 39 ]. In particular, little is known about how older people experienced the pandemic. Thus, our research question considers: How did older adults experience the COVID-19 pandemic worldwide?
We use a qualitative evidence synthesis (QES) recommended by Cochrane Qualitative and Implementation Methods Group to identify peer-reviewed articles [ 40 ]. This provides an overview of existing research, identifies potential research gaps, and develops new cumulative knowledge concerning the COVID-19 pandemic and older adults’ experiences. QES is a valuable method for its potential to contribute to research and policy [ 41 ]. Flemming and Noyes [ 40 ] argue that the evidence synthesis from qualitative research provides a richer interpretation compared to single primary research. They identified an increasing demand for qualitative evidence synthesis from a wide range of “health and social professionals, policymakers, guideline developers and educationalists” (p.1).
Methodology
A systematic literature review requires a specific approach compared to other reviews. Although there is no consensus on how it is conducted, recent systematic literature reviews have agreed the following reporting criteria are addressed [ 42 , 43 ]: (a) a research question; (b) reporting database, and search strategy; (c) inclusion and exclusion criteria; (d) reporting selection methods; (e) critically appraisal tools; (f) data analysis and synthesis. We applied these criteria in our study and began by registering the research protocol with Prospero [ 44 ].
The study is registered at Prospero [ 44 ]. This systematic literature review incorporates qualitative studies concerning older adults’ experiences during the COVID-19 pandemic.
Search strategy
The primary qualitative articles were identified via a systematic search as per the qualitative-specific SPIDER approach [ 45 ]. The SPIDER tool is designed to structure qualitative research questions, focusing less on interventions and more on study design, and ‘samples’ rather than populations, encompassing:
S-Sample. This includes all articles concerning older adults aged 60 + [ 1 ].
P-Phenomena of Interest. How did older adults experience the COVID-19 pandemic?
D-Design. We aim to investigate qualitative studies concerning the experiences of older adults during the COVID-19 pandemic.
E-Evaluation. The evaluation of studies will be evaluated with the amended Critical Appraisal Skills Programme CASP [ 46 ].
R-Research type Qualitative
Information source
The following databases were searched: PsychInfo, Medline, CINAHL, Web of Science, Annual Review, Annual Review of Gerontology, and Geriatrics. A hand search was conducted on Google Scholar and additional searches examined the reference lists of the included papers. The keyword search included the following terms: (older adults or elderly) AND (COVID-19 or SARS or pandemic) AND (experiences); (older adults) AND (experience) AND (covid-19) OR (coronavirus); (older adults) AND (experience) AND (covid-19 OR coronavirus) AND (Qualitative). Additional hand search terms included e.g. senior, senior citizen, or old age.
Inclusion and exclusion criteria
Articles were included when they met the following criteria: primary research using qualitative methods related to the lived experience of older adults aged 60 + (i.e. the experiences of individuals during the COVID-19 pandemic); peer-reviewed journal articles published in English; related to the COVID-19 pandemic; empirical research; published from 2020 till August 2022.
Articles were excluded when: papers discussed health professionals’ experiences; diagnostics; medical studies; interventions; day-care; home care; or carers; experiences with dementia; studies including hospitals; quantitative studies; mixed-method studies; single-case studies; people under the age of 60; grey literature; scoping reviews, and systematic reviews. We excluded clinical/care-related studies as we wanted to explore the everyday experiences of people aged 60 + . Mixed-method studies were excluded as we were interested in what was represented in solely qualitative studies. However, we acknowledge, that mixed-method studies are valuable for future systematic reviews.
Meta-ethnography
The qualitative synthesis was undertaken by using meta-ethnography. The authors have chosen meta-ethnography over other methodologies as it is an inductive and interpretive synthesis analysis and is uniquely “suited to developing new conceptual models and theories” ([ 47 ], p 2), see also [ 48 ]. Therefore, it combines well with constructivist grounded theory methodology. Meta-ethnography also examines and identifies areas of disagreements between studies [ 48 ].
This is of particular interest as the lived experiences of older adults during the COVID-19 pandemic were likely to be diverse. The method enables the researcher to synthesise the findings (e.g. themes, concepts) from primary studies, acknowledging primary data (quotes) by “using a unique translation synthesis method to transcend the findings of individual study accounts and create higher order” constructs ([ 47 ], p. 2). The following seven steps were applied:
Getting started (identify area of interest). We were interested in the lived experiences of older adults worldwide.
Deciding what was relevant to the initial interest (defining the focus, locating relevant studies, decision to include studies, quality appraisal). We decided on the inclusion and exclusion criteria and an appropriate quality appraisal.
Reading the studies. We used the screening process described below (title, abstract, full text)
Determining how the studies were related (extracting first-order constructs- participants’ quotes and second-order construct- primary author interpretation, clustering the themes from the studies into new categories (Table 3 ).
Translating the studies into one another (comparing and contrasting the studies, checking commonalities or differences of each article) to organise and develop higher-order constructs by using constant comparison (Table 3 ). Translating is the process of finding commonalities between studies [ 48 ].
Synthesising the translation (reciprocal and refutational synthesis, a lines of argument synthesis (interpretation of the relationship between the themes- leads to key themes and constructs of higher order; creating new meaning, Tables 2 , 3 ),
Expressing the synthesis (writing up the findings) [ 47 , 48 ].
Screening and Study Selection
A 4-stage screening protocol was followed (Fig. 1 Prisma). First, all selected studies were screened for duplicates, which were deleted. Second, all remaining studies were screened for eligibility, and non-relevant studies were excluded at the preliminary stage. These screening steps were as follows: 1. title screening; 2. abstract screening, by the first and senior authors independently; and 3. full-text screening which was undertaken for almost all papers by the first author. However, 2 papers [ 9 , 23 ] were assessed independently by LS, LR, and LMM to avoid a conflict of interest. The other co-authors also screened independently a portion of the papers each, to ensure that each paper had two independent screens to determine inclusion in the review [ 49 ]. This avoided bias and confirmed the eligibility of the included papers (Fig. 1 ). Endnote reference management was used to store the articles and aid the screening process.
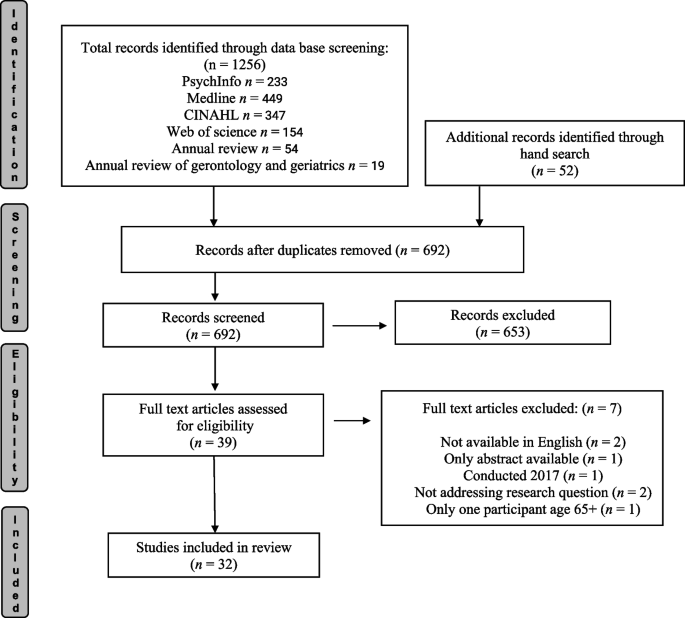
Prisma flow diagram adapted from Page et al. [ 50 ]. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ, 372, n71. https://doi.org/10.1136/bmj.n71 )
Data extraction
After title and abstract screening, 39 papers were selected for reading the full article. 7 papers were excluded after the full-text assessment (1 study was conducted in 2017, but published in 2021; 2 papers were not fully available in English, 2 papers did not address the research question, 1 article was based on a conference abstract only, 1 article had only one participant age 65 +).
The full-text screening included 32 studies. All the included studies, alongside the CASP template, data extraction table, the draft of this article, and translation for synthesising the findings [ 47 , 48 ] were available and accessible on google drive for all co-authors. All authors discussed the findings in regular meetings.
Quality appraisal
A critical appraisal tool assesses a study for its trustworthiness, methodological rigor, and biases and ensures “transparency in the assessment of primary research” ([ 51 ], p. 5); see also [ 48 , 49 , 50 , 51 , 52 , 53 ]. There is currently no gold standard for assessing primary qualitative studies, but different authors agreed that the amended CASPS checklist was appropriate to assess qualitative studies [ 46 , 54 ]. Thus, we use the amended CASP appraisal tool [ 42 ]. The amended CASP appraisal tool aims to improve qualitative evidence synthesis by assessing ontology and epistemology (Table 1 CASP appraisal tool).
A numerical score was assigned to each question to indicate whether the criteria had been met (= 2), partially met (= 1), or not met (= 0) [ 54 ]; see also [ 55 ]. The score 16 – 22 are considered to be moderate and high-quality studies. The studies scored 15 and below were identified as low-quality papers. Although we focus on higher-quality papers, we did not exclude papers to avoid the exclusion of insightful and meaningful data [ 42 , 48 , 52 , 53 , 54 , 55 , 56 , 57 ]. The quality of the paper was considered in developing the evidence synthesis.
We followed the appraisal questions applied for each included study and answered the criteria either ‘Yes’, ‘Cannot tell’, or ‘No’. (Table 1 CASP appraisal criteria). The tenth question asking the value of the article was answered with ‘high’ of importance, ‘middle’, or low of importance. The new eleventh question in the CASP tool concerning ontology and epistemology was answered with yes, no, or partly (Table 1 ).
Data synthesis
The data synthesis followed the seven steps of Meta-Ethnography developed by Noblit & Hare [ 58 ], starting the data synthesis at step 3, described in detail by [ 47 ]. This encompasses: reading the studies; determining how the studies are related; translating the studies into one another; synthesis the translations; and expressing synthesis. This review provides a synthesis of the findings from studies related to the experiences of older adults during the COVID-19 pandemic. The qualitative analyses are based on constructivist grounded theory [ 59 ] to identify the experiences of older adults during the COVID-19 pandemic (non-clinical) populations. The analysis is inductive and iterative, uses constant comparison, and aims to develop a theory. The qualitative synthesis encompasses all text labelled as ‘results’ or ‘findings’ and uses this as raw data. The raw data includes participant’s quotes; thus, the synthesis is grounded in the participant's experience [ 47 , 48 , 60 , 61 ]. The initial coding was undertaken for each eligible article line by line. Please see Table 2 Themes per author and country. Focused coding was applied using constant comparison, which is a widely used approach in grounded theory [ 61 ]. In particular, common and recurring as well as contradicting concepts within the studies were identified, clustered into categories, and overarching higher order constructs were developed [ 47 , 48 , 60 ] (Tables 2 , 3 , 4 ).
We identified twenty-seven out of thirty-two studies as moderate-high quality; they met most of the criteria (scoring 16/22 or above on the CASP; [ 54 ]. Only five papers were identified as low qualitative papers scoring 15 and below [ 71 , 73 , 74 , 86 , 91 ]. Please see the scores provided for each paper in Table 4 . The low-quality papers did not provide sufficient details regarding the researcher’s relationship with the participants, sampling and recruitment, data collection, rigor in the analysis, or epistemological or ontological reasoning. For example, Yildirim [ 91 ] used verbatim notes as data without recording or transcribing them. This article described the analytical process briefly but was missing a discussion of the applied reflexivity of using verbatim notes and its limitations [ 92 ].
This systematic review found that many studies did not mention the relationship between the authors and the participant. The CASP critical appraisal tool asks: Has the relationship between the researcher and participants been adequately considered? (reflecting on own role, potential bias). Many studies reported that the recruitment was drawn from larger studies and that the qualitative study was a sub-study. Others reported that participants contacted the researcher after advertising the study. One study Goins et al., [ 72 ] reported that students recruited family members, but did not discuss how this potential bias impacted the results.
Our review brings new insights into older adults’ experiences during the pandemic worldwide. The studies were conducted on almost all continents. The majority of the articles were written in Europe followed by North America and Canada (4: USA; 3: Canada, UK; 2: Brazil, India, Netherlands, Sweden, Turkey 2; 1: Austria, China, Finland, India/Iran, Mauritius, New Zealand, Serbia, Spain, Switzerland, Uganda, UK/Ireland, UK/Colombia) (see Fig. 2 ). Note, as the review focuses on English language publications, we are unable to comment on qualitative research conducted in other languages see [ 72 ].
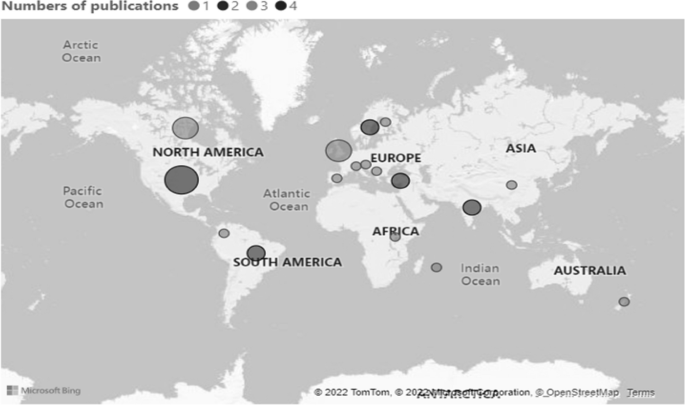
Numbers of publications by country
The characteristics of the included studies and the presence of analytical themes can be found in Table 4 . We used the following characteristics: Author and year of publication, research aims, the country conducted, Participant’s age, number of participants, analytical methodology, CASP score, and themes.
We identified three themes: desired and challenged wellbeing; coping and adaptation; discrimination and intersectionality. We will discuss the themes in turn.
Desired and challenged wellbeing
Most of the studies reported the impact of the COVID-19 pandemic on the well-being of older adults. Factors which influenced wellbeing included: risk communication and risk perception; social connectivity; confinement (at home); and means of coping and adapting. In this context, well-being refers to the evidence reported about participants' physical and mental health, and social connectivity.
Risk perception and risk communication
Politicians and media transmitted messages about the response to the pandemic to the public worldwide. These included mortality and morbidity reports, and details of health and safety regulations like social distancing, shielding- self-isolation, or wearing masks [ 34 , 35 , 36 , 37 ]. As this risk communication is crucial to combat the spread of the virus, it is also important to understand how people perceived the reporting during the pandemic.
Seven studies reported on how the mass media impacted participants' well-being [ 23 , 67 , 68 , 70 , 72 , 81 , 85 ]. Sangrar et al. [ 68 ] investigated how older adults responded to COVID-19 messaging: “My reaction was to try to make sure that I listen to everything and [I] made sure I was aware of all the suggestions and the precautions that were being expressed by various agencies …”. (p. 4). Other studies reported the negative impact on participants' well-being of constant messaging and as a consequence stopped watching the news to maintain emotional well-being [ 3 , 67 , 68 , 70 , 72 , 81 , 85 ]. Derrer-Merk et al. [ 23 ] reported one participant said that “At first, watching the news every day is depressing and getting more and more depressing by the day, so I’ve had to stop watching it for my own peace of mind” (p. 13). In addition, news reporting impacted participants’ risk perception. For example, “Sometimes we are scared to hear the huge coverage of COVID-19 news, in particular the repeated message ‘older is risky’, although the message is useful.” ([ 81 ], p5).
- Social connectivity
Social connectivity and support from family and community were found in fourteen of the studies as important themes [ 9 , 62 , 66 , 67 , 68 , 75 , 76 , 77 , 78 , 79 , 80 , 83 , 84 , 90 ].
The impact of COVID-19 on social networks highlighted the diverse experiences of participants. Some participants reported that the size of social contact was reduced: “We have been quite isolated during this corona time” ?([ 80 ], p. 3). Whilst other participants reported that the network was stable except that the method of contact was different: “These friends and relatives, they visited and called as often as before, but of course, we needed to use the telephone when it was not possible to meet” ([ 77 ], p. 5). Many participants in this study did not want to expand their social network see also [ 9 , 77 , 78 , 79 ]. Hafford-Letchfield et al. [ 76 ] reported that established social networks and relationships were beneficial for the participants: “Covid has affected our relationship (with partner), we spend some really positive close time together and support each other a lot” (p. 7).
On the other hand, other studies reported decreases of, and gaps in, social connectedness: “I couldn’t do a lot of things that I’ve been doing for years. That was playing competitive badminton three times a week, I couldn’t do that. I couldn’t get up early and go volunteer in Seattle” [ 9 , 67 , 75 ]. A loss of social connection with children and grandchildren was often mentioned: “We cannot see our grandchildren up close and personal because, well because they [the parents] don’t want us, they don’t want to risk our being with the kids … it’s been an emotional loss exacerbated by the COVID thing” ([ 68 ] p.10); see also [ 9 , 67 , 78 ]. On the contrary, Chemen & Gopalla [ 66 ] note that those older adults who were living with other family members reported that they were more valued: “Last night my daughter-in-law thanked me for helping with my granddaughter” (p.4).
Despite reports of social disconnectedness, some studies highlighted the importance of support from family members and how support changed during the COVID-19 pandemic [ 9 , 62 , 81 , 83 , 90 ]. Yang et al. [ 90 ] argued that social support was essential during the Lockdown in China: “N6 said: ‘I asked my son-in-law to take me to the hospital” (p. 4810). Mahapatra et al. [ 81 ] found, in an Indian study, that the complex interplay of support on different levels (individual, family, and community) helped participants to adapt to the new situation. For example, this participant reported that: “The local police are very helpful. When I rang them for something and asked them to find out about it, they responded immediately” (p. 5).
Impact of confinement on well being
Most articles highlighted the impact of confinement on older adults’ well-being [ 9 , 62 , 63 , 65 , 67 , 69 , 70 , 72 , 75 , 77 , 78 , 79 , 81 , 82 , 83 , 85 , 89 , 90 ].
Some studies found that participants maintained emotional well-being during the pandemic and it did not change their lifestyle [ 79 , 80 , 82 , 83 , 89 , 92 ]: “Actually, I used this crisis period to clean my house. Bookcases are completely cleaned and I discarded old books. Well, we have actually been very busy with those kind of jobs. So, we were not bored at all” ([ 79 ], p. 5). In McKinlay et al. [ 82 ]’s study, nearly half of the participants found that having a sense of purpose helped to maintain their well-being: “You have to have a purpose you see. I think mental resilience is all about having a sense of purpose” (p. 6).
However, at the same time, the majority of the articles (12 out of 18) highlighted the negative impact of confinement and social distancing. Participants talked of increased depressive feelings and anxiety. For example, one of Akkus et al.’s [ 62 ] participants said: “... I am depressed; people died. Terrible disease does not give up, it always kills, I am afraid of it …” (p. 549). Similarly, one of Falvo et al.’s [ 67 ] participants remarked: “I am locked inside my house and I am afraid to go out” (p. 7).
Many of the studies reported the negative impact of loneliness as a result of confinement on participants’ well-being including [ 69 , 70 , 72 , 78 , 79 , 90 , 93 ]. Falvo et al. [ 67 ] reported that many participants experienced loneliness: “What sense does it make when you are not even able to see a family member? I mean, it is the saddest thing not to have the comfort of having your family next to you, to be really alone” (p. 8).
Not all studies found a negative impact on loneliness. For example, a “loner advantage” was found by Xie et al. ([ 82 ], p. 386). In this study participants found benefits in already being alone “It’s just a part of who I am, and I think that helps—if you can be alone, it really is an asset when you have to be alone” ([ 82 ], p. 386).
Bundy et al. [ 80 ] investigated loneliness from already lonely older adults and found that many participants did not attribute the loneliness to the pandemic: “It’s not been a whole lot, because I was already sitting around the house a whole lot anyway ( …). It’s basically the same, pretty well … I’d pretty well be like this anyway with COVID or without COVID” (p. 873) (see also [ 83 ]).
A study from Serbia investigated how the curfew was perceived 15 months afterward. Some participants were calm: “I realized that … well … it was simply necessary. For that reason, we accepted it as a measure that is for the common good” ([ 70 ], p.634). Others were shocked: “Above all, it was a huge surprise and sort of a shock, a complete shock because I have never, ever seen it in my life and I felt horrible, because I thought that something even worse is coming, that I even could not fathom” ([ 70 ], p. 634).
The lockdowns brought not only mental health issues to the fore but impacted the physical health of participants. Some reported they were fearful of the COVID-19 pandemic: “... For a little while I was afraid to leave, to go outside. I didn’t know if you got it from the air” ([ 75 ]. p. 6). Another study reported: “It’s been important for me to walk heartily so that I get a bit sweaty and that I breathe properly so that I fill my lungs—so that I can be prepared—and be as strong as possible, in case I should catch that coronavirus” ([ 77 ], p. 9); see also [ 70 , 78 , 82 , 85 ].
Coping and adaptation
Many studies mentioned older adults’ processes of coping and adaptation during the pandemic [ 63 , 64 , 68 , 69 , 72 , 75 , 79 , 81 , 85 , 87 , 88 , 89 , 90 ].
A variety of coping processes were reported including: acceptance; behavioural adaptation; emotional regulation; creating new routines; or using new technology. Kremers et al. [ 79 ] reported: “We are very realistic about the situation and we all have to go through it. Better days will come” (p. e71). Behavioural adaptation was reported: “Because I’m asthmatic, I was wearing the disposable masks, I really had trouble breathing. But I was determined to find a mask I could wear” ([ 68 ], p. 14). New routines with protective hygiene helped some participants at the beginning of the pandemic to cope with the health threat: “I am washing my hands all the time, my hands are raw from washing them all the time, I don't think I need to wash them as much as I do but I do it just in case, I don’t have anybody coming in, so there is nobody contaminating me, but I keep washing” ([ 69 ], p. 4391); see also [ 72 ]. Verhage et al. [ 87 ] reported strategies of coping including self-enhancing comparisons, distraction, and temporary acceptance: “There are so many people in worse circumstances …” (p. e294). Other studies reported how participants used a new technology: “I have recently learned to use WhatsApp, where I can make video phone calls.” ([ 88 ], p. 163); see also [ 89 ].
Discrimination -intersectionality (age and race/gender identity)
Seven studies reported ageism, racism, and gender discrimination experienced by older adults during the pandemic [ 23 , 63 , 67 , 70 , 76 , 84 , 88 ].
Prigent et al. [ 84 ], conducted in a New Zealand study, found that ageism was reciprocal. Younger people spoke against older adults: “why don’t you do everyone a favour and drop dead you f******g b**** it’s all because of ones like you that people are losing jobs” (p. 11). On the other hand, older adults spoke against the younger generation: “Shame to see the much younger generations often flout the rules and generally risk the gains made by the team. Sheer arrogance on their part and no sanctions applied” (p.11). Although one study reported benevolent ageism [ 23 ] most studies found hostile ageism [ 23 , 63 , 67 , 70 , 76 , 84 ]. One study from Canada exploring 15 older adult’s Chinese immigrants’ experiences reported racism as people around them thought they would bring the virus into the country. The negative impact on existing friendships was told by a Chinese man aged 69 “I can tell some people are blatantly despising us. I can feel it. When I talked with my Caucasian friends verbally, they would indirectly blame us for the problem. Eventually, many of our friendships ended because of this issue” ([ 88 ], p161). In addition, this study reported ageism when participants in nursing homes felt neglected by the Canadian government.
Two papers reported experiences of sexual and gender minorities (SGM) (e.g. transgender, queer, lesbian or gay) and found additional burdens during the pandemic [ 63 , 76 ]. People experienced marginalisation, stereotypes, and discrimination, as well as financial crisis: “I have faced this throughout life. Now people look at me in a way as if I am responsible for the virus.” ([ 63 ], p. 6). The consequence of marginalisation and ignorance of people with different gender identities was also noted by Hafford- Letchfield et al. [ 76 ]: “People have been moved out of their accommodation into hotels with people they don't know …. a gay man committed suicide, community members know of several that have attempted suicide. They are feeling pretty marginalised and vulnerable and you see what people are writing on the chat pages” (p.4). The intersection of ageism, racism, and heterosexism and its negative impact on people’s well-being during the pandemic reflects additional burden and stressors for older adults.
This systematic literature review is important as it provides new insights into the lived experiences of older adults during the COVID-19 pandemic, worldwide. Our study highlights that the COVID-19 pandemic brought an increase in English-written qualitative articles to the fore. We found that 32 articles met the inclusion criteria but 5 were low quality. A lack of transparency reduces the trustworthiness of the study for the reader and the scientific community. This is particularly relevant as qualitative research is often criticised for its bias or lack of rigor [ 94 ]. However, their findings are additional evidence for our study.
Our aim was to explore, in a systematic literature review, the lived experiences of older adults during the COVID-19 pandemic worldwide. The evidence highlights the themes of desired and challenged wellbeing, coping and adaptation, and discrimination and intersectionality, on wellbeing.
Perceived risk communication was experienced by many participants as overwhelming and anxiety-provoking. This finding supports Anwar et al.’s [ 37 ] study from the beginning of the pandemic which found, in addition to circulating information, that mass media influenced the public's behaviour and in consequence the spread of disease. The impact can be positive but has also been revealed to be negative as well. They suggest evaluating the role of the mass media in relation to what and how it has been conveyed and perceived. The disrupted social connectivity found in our review supports earlier studies that reported the negative impact of people’s well-being [ 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 ] at the beginning of the pandemic. This finding is important for future health crisis management, as the protective health measures such as confinement or self-isolation had a negative impact on many of the participants’ emotional wellbeing including increased anxiety, feelings of depression, and loneliness during the lockdowns. As a result of our review, future protective health measures should support people’s desire to maintain proximity with their loved ones and friends. However, we want to stress that our findings are mixed.
The ability of older adults to adapt and cope with the health crisis is important: many of the reported studies noted the diverse strategies used by older people to adapt to new circumstances. These included learning new technologies or changing daily routines. Politicians and the media and politicians should recognise both older adults' risk of disease and its consequences, but also their adaptability in the face of fast-changing health measures. This analysis supports studies conducted over the past decades on lifespan development, which found that people learn and adapt livelong to changing circumstances [ 95 , 96 , 97 ].
We found that discrimination against age, race, and gender identity was reported in some studies, in particular exploring participants’ experiences with immigration backgrounds and sexual and gender minorities. These studies highlighted the intersection of age and gender or race and were additional stressors for older adults and support the findings from Ramirez et al. [ 98 ] This review suggests that more research should be conducted to investigate the experiences of minority groups to develop relevant policies for future health crises.
Our review was undertaken two years after the pandemic started. At the cut-off point of our search strategy, no longitudinal studies had been found. However, in December 2022 a longitudinal study conducted in the USA explored older adult’s advice given to others [ 99 ]. They found that fostering and maintaining well-being, having a positive life perspective, and being connected to others were coping strategies during the pandemic [ 100 ]. This study supports the results of the higher order constructs of coping and adaptation in this study. Thus, more longitudinal studies are needed to enhance our understanding of the long-term consequences of the COVID-19 pandemic. The impact of the COVID-19 restrictions on older adults’ lives is evident. We suggest that future strategies and policies, which aim to protect older adults, should not only focus on the physical health threat but also acknowledge older adults' needs including psychological support, social connectedness, and instrumental support. The policies regarding older adult’s protections changed quickly but little is known about older adults’ involvement in decision making [ 100 ]. We suggest including older adults as consultants in policymaking decisions to ensure that their own self-determinism and independence are taken into consideration.
There are some limitations to this study. It did not include the lived experiences of older adults in care facilities or hospitals. The studies were undertaken during the COVID-19 pandemic and therefore data collection was not generally undertaken face-to-face. Thus, many studies included participants who had access to a phone, internet, or email, others could not be contacted. Additionally, we did not include published papers after August 2022. Even after capturing the most commonly used terms and performing additional hand searches, the search terms used might not be comprehensive. The authors found the quality of the papers to be variable, and their credibility was in question. We acknowledge that more qualitative studies might have been published in other languages than English and were not considered in this analysis.
To conclude, this systematic literature review found many similarities in the experiences of older adults during the Covid-19 pandemic despite cultural and socio-economic differences. However, we stress to acknowledge the heterogeneity of the experiences. This study highlights that the interplay of mass media reports of the COVID-19 pandemic and the policies to protect older adults had a direct impact on older adults’ well-being. The intersection of ‘isms’ (ageism, racism, and heterosexism) brought an additional burden for some older adults [ 98 ]. These results and knowledge about the drawbacks of health-protecting measures need to be included in future policies to maintain older adults’ well-being during a health crisis.
Availability of data and materials
The systematic literature review is based on already published articles. And all data analysed during this study are included in this manuscript. No additional data was used.
World Health Organisation (WHO): WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020. 2020. Retrieved from https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
WorldOMeter: Coronavirus toll update: Cases & deaths by country. 2022. Worldometers. https://www.worldometers.info/coronavirus/ .
World Health Organisation (WHO): Coronavirus disease. 2022. https://www.who.int/health-topics/coronavirus#tab=tab . Aaccessed 5 Oct 2022.
Ayouni I, Maatoug J, Dhouib W, Zammit N, Fredj SB, Ghammam R, Ghannem H. Effective public health measures to mitigate the spread of COVID-19: a systematic review. BMC Public Health. 2021;21(1):1015.
PubMed PubMed Central CAS Google Scholar
Cerasoli B. The frail future of geriatrics. Lancet Healthy Longev. 2020;1(1):e11.
PubMed PubMed Central Google Scholar
Allen K-A, Arslan G, Craig H, Arefi S, Yaghoobzadeh A, Sharif Nia H. The psychometric evaluation of the sense of belonging instrument (SOBI) with Iranian older adults. BMC Geriatr. 2021;21(1):211.
Bailey L, Ward M, DiCosimo A, Baunta S, Cunningham C, Romero-Ortuno R, Kenny RA, Purcell R, Lannon R, McCarroll K, et al. Physical and mental health of older people while cocooning during the COVID-19 pandemic. QJM. 2021;114(9):648–53.
Dahlberg L. Loneliness during the COVID-19 pandemic. Aging Ment Health. 2021;25(7):1161–4.
PubMed Google Scholar
Derrer-Merk E, Ferson S, Mannis A, Bentall R, Bennett KM. Older people's family relationships in disequilibrium during the COVID-19 pandemic. What really matters? Ageing Soc. 2022:1–18.
Derrer-Merk E, Ferson S, Mannis A, Bentall RP, Bennett KM. Belongingness challenged: Exploring the impact on older adults during the COVID-19 pandemic. PLoS ONE. 2022;17(10):e0276561.
Heidinger T, Richter L. The effect of COVID-19 on loneliness in the elderly. An empirical comparison of pre-and peri-pandemic loneliness in community-dwelling elderly. Front Psychol. 2020;11:(585308).
Richter L, Heidinger T. Hitting close to home: the effect of COVID-19 illness in the social environment on psychological burden in older adults. Front Psychol. 2021;12:(737787).
Krendl AC, Perry BL. The impact of sheltering in place during the COVID-19 pandemic on older adults’ social and mental well-being. J Gerontol B Psychol Sci Soc Sci. 2021;76(2):e53–8.
Litwin, H., & Levinsky, M. Social networks and mental health change in older adults after the Covid-19 outbreak. Aging Ment Health. 2021:1–6. https://doi.org/10.1080/13607863.2021.1902468 .
De Pue S, Gillebert C, Dierckx E, Vanderhasselt MA, De Raedt R, Van den Bussche E. The impact of the COVID-19 pandemic on wellbeing and cognitive functioning of older adults. Sci Rep. 2021;11(1):4636.
Shahid Z, Kalayanamitra R, McClafferty B, Kepko D, Ramgobin D, Patel R, Aggarwal CS, Vunnam R, Sahu N, Bhatt D, et al. COVID-19 and older adults: what we know. J Am Geriatr Soc. 2020;68(5):926–9.
Smith M, Steinman L, Casey E. Combatting social isolation among older adults in a time of physical distancing: the COVID-19 social connectivity paradox. Front Public Health. 2020;8:403.
Cohn-Schwartz E, Finlay JM, Kobayashi LC. Perceptions of societal ageism and declines in subjective memory during the COVID-19 pandemic: longitudinal evidence from US adults aged ≥55 years. J Soc Issues. 2022;78(4):924–38.
Tsoukalis-Chaikalis N, Demsia S, Stamatopoulou A, Chaniotis D, Tel Nu. Systematic Mapping Study of Covid-19 Psychological Impact. 2021;15(3):820.
van Gerwen M, Alsen M, Little C, Barlow J, Genden E, Naymagon L, Tremblay D. Risk factors and outcomes of COVID-19 in New York City; a retrospective cohort study. J Med Virol. 2021;93(2):907–15.
Victor CR, Rippon I, Barreto M, Hammond C, Qualter P. Older adults’ experiences of loneliness over the lifecourse: an exploratory study using the BBC loneliness experiment. Arch Gerontol Geriatr. 2022;102:104740.
Vrach IT, Tomar R. Mental health impacts of social isolation in older people during COVID pandemic. Prog Neurol Psychiatry. 2020;24(4):25–9.
Google Scholar
Derrer-Merk E, Reyes-Rodriguez M-F, Salazar A-M, Guevara M, Rodríguez G, Fonseca A-M, Camacho N, Ferson S, Mannis A, Bentall RP, et al. Is protecting older adults from COVID-19 Ageism? A comparative cross-cultural constructive grounded theory from the United Kingdom and Colombia. J Soc Issues. 2022;78(4):900–23.
Lytle A, Levy SR. Reducing ageism toward older adults and highlighting older adults as contributors during the COVID-19 pandemic. J Soc Issues. 2022;78(4):1066–84.
McDarby M, Ju CH, Picchiello MC, Carpenter BD. Older adults’ perceptions and experiences of ageism during the COVID-19 pandemic. J Soc Issues. 2022;78(4):939–64.
Drury L, Abrams D, Swift HJ. Intergenerational contact during and beyond COVID-19. J Soc Issues. 2022;78(4):860–82.
Kanık B, Uluğ ÖM, Solak N, Chayinska M. “Let the strongest survive”: Ageism and social Darwinism as barriers to supporting policies to benefit older individuals. J Soc Issues. 2022;00:1–25.
Spaccatini F, Giovannelli I, Pacilli MG. “You are stealing our present”: Younger people's ageism towards older people predicts attitude towards age-based COVID-19 restriction measures. J Soc Issues. 2022;78(4):769–89.
Sutter A, Vaswani M, Denice P, Choi KH, Bouchard H, Esses VM. Ageism toward older adults during the COVID-19 pandemic: Intergenerational conflict and support. J Soc Issues. 2022;78(4):815–41.
Swift H, Chasteen A. Ageism in the time of COVID-19. Group Process Intergroup Relat. 2021;24:246–52.
World Health Organisation (WHO): Risk Communication in times of an epidemic or pandemic. Asset paper series Epidemics and Pandemics: 2017. https://www.who.int/emergencies/risk-communicationsWHORCaCERaoSAo .
Bailey A, Harris MA, Bogle D, Jama A, Muir SA, Miller S, Walters CA, Govia I. Coping with COVID-19: health risk communication and vulnerable groups. Disaster Med Public Health Prep. 2021;17:e22.
Li X, Lyu H. Epidemic risk perception PS, and mental health during COVID-19 pandemic: a moderated mediating model. Front Psychol. 2021;11:563741. https://doi.org/10.3389/fpsyg.2020.563741 .
Article PubMed PubMed Central Google Scholar
Sandman P M & American Industrial Hygiene Association: Responding to community outrage: strategies for effective risk communication. American Industrial Hygiene Association. 2003.
Sandman, P M. Introduction and orientation index. https://www.psandman.com/index-intro.htm . Retrieved 13 October 2022.
Anderson M, Pitchforth E, Asaria M, Brayne C, Casadei B, Charlesworth A, Coulter A, Franklin BD, Donaldson C, Drummond M, et al. LSE-Lancet Commission on the future of the NHS: re-laying the foundations for an equitable and efficient health and care service after COVID-19. Lancet. 2021;397(10288):1915–78.
PubMed CAS Google Scholar
Anwar A, Malik M, Raees V, Anwar A. Role of mass media and public health communications in the COVID-19 pandemic. Cureus. 2020;12(9):e10453.
U.S. National Library of Medicine: COVID-19 - Search Details - ClinicalTrials.gov: Clinicaltrials.gov 2022. Retrieved October 13, 2022, from https://clinicaltrials.gov/ct2/results/details?cond=COVID-19 .
Tremblay S, Castiglione S, Audet L-A, Desmarais M, Horace M, Peláez S. Conducting qualitative research to respond to COVID-19 challenges: reflections for the present and beyond. Int J Qual Methods. 2021;20:16094069211009680.
Flemming K, Noyes J. Qualitative evidence synthesis: where are we at? Int J Qual Methods. 2021;20:1609406921993276.
Booth A. Searching for qualitative research for inclusion in systematic reviews: a structured methodological review. Syst Rev. 2016;5(1):74.
Krnic Martinic M, Pieper D, Glatt A, Puljak L. Definition of a systematic review used in overviews of systematic reviews, meta-epidemiological studies and textbooks. BMC Med Res Methodol. 2019;19(1):203.
Phillips V, Barker E. Systematic reviews: structure, form and content. J Perioper Pract. 2021;31(9):349–53.
Derrer-Merk E, Soulsby L, Reyes Rodriguez M, Ferson S, Mannis A, Bennett KM. Older adults' lived experiences during the COVID-19 pandemic: a systematic review. 2022. PROSPERO 2022 CRD42022331714. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022331714 .
Cooke A, Smith D, Booth A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qual Health Res. 2012;22:1435–43.
Long HA, French DP, Brooks JM. Optimising the value of the critical appraisal skills programme (CASP) tool for quality appraisal in qualitative evidence synthesis. Res Methods Med Health Sci. 2020;1(1):31–42.
Sattar R, Lawton R, Panagioti M, Johnson J. Meta-ethnography in healthcare research: a guide to using a meta-ethnographic approach for literature synthesis. BMC Health Serv Res. 2021;21(1):50.
Soundy A, Heneghan NR. Meta-ethnography. Int Rev Sport Exerc Psychol. 2022;15(1):266–86.
Fallon V, Groves R, Halford JCG, Bennett KM, Harrold JA. Postpartum anxiety and infant-feeding outcomes: a systematic review. J Hum Lact. 2016;32(4):740–58.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLoS Med. 2021;18(3):e1003583.
Tod D, Booth A, Smith B. Critical appraisal. Int Rev Sport Exerc Psychol. 2022;15(1):52–72.
Morse J. Why the Qualitative Health Research (QHR) review process does not use checklists. Qual Health Res. 2021;31(5):819–21.
Munthe-Kaas HM, Glenton C, Booth A, Noyes J, Lewin S. Systematic mapping of existing tools to appraise methodological strengths and limitations of qualitative research: first stage in the development of the CAMELOT tool. BMC Med Res Methodol. 2019;19(1):113.
Njau B, Covin C, Lisasi E, Damian D, Mushi D, Boulle A, Mathews C. A systematic review of qualitative evidence on factors enabling and deterring uptake of HIV self-testing in Africa. BMC Public Health. 2019;19(1):1289.
Butler A, Hall H, Copnell B. A guide to writing a qualitative systematic review protocol to enhance evidence-based practice in nursing and health care. Worldviews Evid Based Nurs. 2016;13(3):241–9.
Soilemezi D, Linceviciute S. Synthesizing qualitative research: reflections and lessons learnt by two new reviewers. Int J Qual Methods. 2018;17(1):1609406918768014.
Booth A. Harnessing energies, resolving tensions: acknowledging a dual heritage for qualitative evidence synthesis. Qual Health Res. 2019;29(1):18–31.
Carroll C, Booth A. Quality assessment of qualitative evidence for systematic review and synthesis: Is it meaningful, and if so, how should it be performed? Res Synth Methods. 2015;6(2):149–54.
Charmaz K. Constructing Grounded Theory. 2nd ed. London: Sage; 2014.
Toye F, Seers K, Allcock N, Briggs M, Carr E, Barker K. Meta-ethnography 25 years on: challenges and insights for synthesising a large number of qualitative studies. BMC Med Res Methodol. 2014;14(1):80.
Noblit GW, Hare RD. Meta-ethnography: synthesizing qualitative studies. California: Sage Publications Ltd; 1988.
Akkus Y, Parlak A, Karacan Y, Karatay G. Perceptions and experiences of older people regarding the COVID-19 pandemic process: a phenomenological study. Turk Geriatri Dergisi. 2021;24:546–56.
Banerjee D, Rao TSS. “The Graying Minority”: lived experiences and psychosocial challenges of older transgender adults during the COVID-19 pandemic in India, A qualitative exploration. Front Psychiatry. 2021;11:604472.
Brooke J, Jackson D. Older people and COVID-19: Isolation, risk and ageism. J Clin Nurs. 2020;29(13-14):2044–6.
Bundy H, Lee HM, Sturkey KN, Caprio AJ. The lived experience of already-lonely older adults during COVID-19. Gerontologist. 2021;61(6):870–7.
Chemen S, Gopalla YN. Lived experiences of older adults living in the community during the COVID-19 lockdown - The case of mauritius. J Aging Stud. 2021;57:100932.
Falvo I, Zufferey MC, Albanese E, Fadda M. Lived experiences of older adults during the first COVID-19 lockdown: a qualitative study. PLoS ONE. 2021;16(6):e0252101.
Fiocco AJ, Gryspeerdt C, Franco G. Stress and adjustment during the COVID-19 pandemic: a qualitative study on the lived experience of Canadian older adults. Int J Environ Res Public Health. 2021;18(24):12922.
Fristedt S, Carlsson G, Kylén M, Jonsson O, Granbom M. Changes in daily life and wellbeing in adults, 70 years and older, in the beginning of the COVID-19 pandemic. Scand J Occup Ther. 2022;29(6):511–21.
Gazibara T, Maksimovic N, Dotlic J, Jeremic Stojkovic V, Cvjetkovic S, Milic M. Experiences and aftermath of the COVID-19 lockdown among community-dwelling older people in Serbia: a qualitative study. J Eval Clin Pract. 2022;28(4):631–40.
Giebel C, Ivan B, Ddumba I. COVID-19 public health restrictions and older adults’ well-being in Uganda: psychological impacts and coping mechanisms. Clin Gerontol. 2022;45(1):97–105.
Goins RT, Anderson E, Minick H, Daniels H. Older adults in the United States and COVID-19: a qualitative study of perceptions, finances, coping, and emotions. Front Public Health. 2021;9:660536.
Gomes MACFC, Fontenele NAO, Galindo Neto NM, Barros LM, Frota NM. Elderly people’s experience facing social isolation in the COVID-19 pandemic. Rev Rene. 2021;22:e69236. https://doi.org/10.15253/2175-6783.20212269236 .
Article Google Scholar
Gonçalves AR, Barcelos JLM, Duarte AP, Lucchetti G, Gonçalves DR. Silva e Dutra FCM, Gonçalves JRL: Perceptions, feelings, and the routine of older adults during the isolation period caused by the COVID-19 pandemic: a qualitative study in four countries. Aging Ment Health. 2022;26(5):911–8.
Greenwood-Hickman MA, Dahlquist J, Cooper J, Holden E, McClure JB, Mettert KD, Perry SR, Rosenberg DE. “They’re Going to Zoom It”: a qualitative investigation of impacts and coping strategies during the COVID-19 pandemic among older adults. Front Public Health. 2021;9:679976.
Hafford-Letchfield T, Toze M, Westwood S. Unheard voices: a qualitative study of LGBT+ older people experiences during the first wave of the COVID-19 pandemic in the UK. Health Soc Care Community. 2022;30(4):e1233–43.
Huntley R, Bratt AS. An interpretative phenomenological analysis of the lived experiences of older adults during the covid-19 pandemic in sweden. Nordic Psychol. 2022;75(1)3–19.
Jiménez-Etxebarria E, Bernaras Iturrioz E, Jaureguizar J. Impact of the COVID-19 pandemic as perceived by older people in Northern Spain. Psychol Res Behav Manag. 2021;14:1789–803.
Kremers EM, Janssen JHM, Nieuwboer MS, Olde Rikkert MGM, Peeters GMEE. The psychosocial adaptability of independently living older adults to COVID-19 related social isolation in the Netherlands: a qualitative study. Health Soc Care Community. 2022;30(1):e67–74.
Kulmala J, Tiilikainen E, Lisko I, Ngandu T, Kivipelto M, Solomon A. Personal social networks of community-dwelling oldest old during the Covid-19 pandemic—A qualitative study. Front Public Health. 2021;9:1–10.
Mahapatra P, Sahoo KC, Desaraju S, Pati S. Coping with COVID-19 pandemic: reflections of older couples living alone in urban Odisha India. Prim Health Care Res Dev. 2021;22:e64.
McKinlay AR, Fancourt D, Burton A. A qualitative study about the mental health and wellbeing of older adults in the UK during the COVID-19 pandemic. BMC Geriatr. 2021;21(1):1–10.
Pfabigan J, Wosko P, Pichler B, Reitinger E, Pleschberger S. Under reconstruction: the impact of COVID-19 policies on the lives and support networks of older people living alone. Int J Care Caring. 2022;6(1-2):211–28.
Prigent C, Morgan T, Wiles J, Morgan K, Williams L, Gott M. Intergenerational tension or cohesion during the covid-19 pandemic?: A letter-writing study with older new zealanders. J Intergenerational Relationsh. 2022;20(4):386–405.
Sangrar R, Porter MM, Chesser S. Exploring the interpretation of COVID-19 messaging on older adults. Experiences of vulnerability. Can J Aging Rev Can Vieil. 2021;40(4):533–42.
Sattari S, Billore S. Bring it on Covid-19: being an older person in developing countries during a pandemic. Working Older People. 2020;24(4):281–91.
Verhage M, Thielman L, Kock L, Lindenberg J. Coping of older adults in times of COVID-19: considerations of temporality among dutch older adults. J Gerontol B. 2021;76(7):e290–9.
Wang Q, Liu JKK, Walsh CA. Identities: experiences and impacts of the COVID-19 pandemic from the perspectives of older Chinese immigrants in Canada. China J Soc Work. 2021;14(2):153–71.
Xie B, Shiroma K, De Main AS, Davis NW, Fingerman K, Danesh V. Living through the COVID-19 pandemic: community-dwelling older adults’ experiences. J Aging Soc Policy. 2021;33(4–5):380–97.
Yang Q, Wang Y, Tian C, Chen Y, Mao J. The Experiences of Community-dwelling older adults during the COVID-19 lockdown in Wuhan: a qualitative study. J Adv Nurs (John Wiley & Sons, Inc). 2021;77(12):4805–14.
Yıldırım H. Psychosocial status of older adults aged 65 years and over during lockdown in Turkey and their perspectives on the outbreak. Health Soc Care Community. 2022;30(3):899–907.
Hill Z, Tawiah-Agyemang C, Kirkwood B, Kendall C. Are verbatim transcripts necessary in applied qualitative research: experiences from two community-based intervention trials in Ghana. Emerg Themes Epidemiol. 2022;19(1):5.
Giles D. Performed across Europe and written up in English: the double challenge for qualitative psychologists. Qual Res Psychol. 2019;16(3):503–7.
Anderson C. Presenting and evaluating qualitative research. Am J Pharm Educ. 2010;74(8):141.
Nikitin J, Freund A. The Adaptation Process of Aging. The Cambridge Handbook of Successful Aging. Chapter: 17. Cambridge University Press. 2019. p. 281–98.
Deimling GT, Kahana B, Bowman KF, Schaefer ML. Cancer survivorship and psychological distress in later life. Psychooncology. 2002;11(6):479–94.
Baltes PB, Staudinger UM, Lindenberger U. Lifespan psychology: theory and application to intellectual functioning. Annu Rev Psychol. 1999;50:471–507.
Ramirez L, Monahan C, Palacios-Espinosa X, Levy SR. Intersections of ageism toward older adults and other isms during the COVID-19 pandemic. J Soc Issues. 2022;78(4):965–90.
Van Vleet B, Fuller HR, Hofmann B, Huseth-Zosel A. Untapped insight: a longitudinal qualitative analysis of older adults’ advice during the COVID-19 pandemic. Innov Aging. 2022;6(7):igac071.
Gietel-Basten S, Matus K, Mori R. COVID-19 as a trigger for innovation in policy action for older persons? Evid Asia Policy Soc. 2022;41(1):168–86.
Download references
Acknowledgements
Not applicable
Not applicable.
Author information
Authors and affiliations.
University of Liverpool, Eleanor Rathbone Building, Bedford Street South, Liverpool, L697ZA, UK
Elfriede Derrer-Merk, Laura K. Soulsby & Kate M. Bennett
Universidad de los Andes, Carrera 1 No. 18A-12, Bogotá, Colombia
Maria-Fernanda Reyes-Rodriguez
Principal Health Psychologist, Resilience Hub, Lancashire & South Cumbria Foundation Hospital, Chorley, UK
Louise Roper
You can also search for this author in PubMed Google Scholar
Contributions
Elfriede Derrer-Merk contributed to the design, analysis, and writing the draft. Maria-Fernanda Rodriguez-Reyes contributed to the analysis, revised the draft, and approved the submission. Laura K. Soulsby contributed to the analysis, revised the draft, and approved the submission. Louise Roper contributed to the analysis, revised the draft, and approved the submission. Kate M. Bennett contributed to the design, analysis, writing the draft, and approved the submission.
Corresponding author
Correspondence to Elfriede Derrer-Merk .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Derrer-Merk, E., Reyes-Rodriguez, MF., Soulsby, L.K. et al. Older adults’ experiences during the COVID-19 pandemic: a qualitative systematic literature review. BMC Geriatr 23 , 580 (2023). https://doi.org/10.1186/s12877-023-04282-6
Download citation
Received : 16 November 2022
Accepted : 05 September 2023
Published : 20 September 2023
DOI : https://doi.org/10.1186/s12877-023-04282-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Older adults
- Risk communication
- Discrimination
BMC Geriatrics
ISSN: 1471-2318
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Challenges for healthcare communication during the COVID-19 pandemic
More than one year has passed since the first outbreak of the COVID-19 pandemic. During 2020, the pandemic has become a major health concern in most countries worldwide. By early January, the number of deaths due to the pandemic approached two million. While a number of vaccine programs were being rolled out in January, several countries reported the highest number of new cases so far during the pandemic.
In course of this last year a large number of studies have been conducted on different aspects of the pandemic within a broad range of health related disciplines. Patient Education and Counseling – PEC – has received more than 100 manuscripts on COVID-19, covering topics such as reactions and behaviors among patients, families and the public at large and ideas and interventions on how to improve health communication related to COVID-19. In a number of editorials last year, we have discussed topics such as how to handle uncertainty and promote behavior change in information to the public [ 1 ], clinical communication between health care providers, patients and families during the pandemic [ 2 ], and on how to provide equitable care to patients with limited dominant language proficiency [ 3 ].
When the present issue of PEC is being published, early February 2021, many countries are in the middle of ambitious vaccination programs. It is tempting to believe that when large groups of vulnerable individuals have been vaccinated, we may soon return to normal, and loosen up on infection control behavior regimes. Most probably, that will not be the case. Even if vaccination of the most vulnerable groups will help to grossly reduce the number of deaths, an increase of patients in younger age groups is probable if infection control behavior patterns decline. Such a development may represent a major challenge to healthcare capacity. It will therefore be important to recalibrate our information strategies to help the public understand that infection control behavior will be just as important for a large part of 2021 as it has been up to now. Therefore, we will continue to publish papers in PEC on health communication tasks and strategies to promote infection control behavior and other topics relevant to COVID-19.
In the present issue of PEC, we publish three articles on challenges for healthcare communication during the COVID-19. One of these papers is a Position Paper written by Sarah J. White and colleagues on behalf of the research committee (rEACH) of the International Association for Communication in Healthcare (EACH) [ 4 ]. The authors discuss the experiences so far in the pandemic and suggest ways forward for healthcare communication during COVID-19 pandemic, both in terms of how to provide information on the pandemic to the public and on issues related to clinical communication with individual patients and families.
1. How well do people understand health information?
One major aspect of informing the public is to find a terminology that is well understood by all. There are, however, large differences between us regarding how well we understand information, and health literacy has become a major concern in course of the last twenty years [ 5 ]. In the Position Paper in this issue, White et al. point to the importance of health literacy for the understanding of risk, which is a crucial element in information about the pandemic [ 4 ]. They suggest that policy makers should connect with communication experts and citizen groups to enhance health literacy of key influencers and others in order to promote better understanding of relevant information [ 4 ]. As alluded to above, such information should include an emphasis on why infection control is still important in the current stage of the pandemic when broad vaccination programs are being rolled out.
In another article in the present issue of PEC, Matterne et al. review a large number of studies on health literacy and related phenomena in the context of corona virus outbreaks, including previous outbreaks as well as COVID-19 [ 6 ]. The authors found that only few studies explicitly referred to the concept of health literacy in their studies of health information seeking and other behaviors in a pandemic context. They conclude that future research should be guided from health literacy research in order to learn more about the associations between health literacy, risk perception and infection control behavior.
2. What do people want to know and what do they fear?
Effective information to the public on COVID-19 should be calibrated to the specific information needs of the public. In a paper included in the present issue Leão et al. report data from a content analysis of 293 questions submitted to online, radio, newspaper and TV channel forums during the first months of the pandemic in Portugal [ 7 ]. First of all, they found a high degree of uncertainty and doubt, regarding both medical questions, daily life practicalities related to lockdown and other measures, and questions related to infection control. It is interesting to see how certain uncertainties and doubts were reduced during the early weeks of the pandemic, while the frequencies of others increased.
Second, many individuals reported a considerable amount of concerns and fear, related to the disease itself and to its implications and consequences. Again, there were variations over time in the nature of people’s concerns [ 7 ]. More knowledge on people’s reactions to the pandemic in different phases may be useful background information for those who are involved in communication on the pandemic to the public.
3. How is clinical communication affected by COVID-19?
COVID-19 has also changed clinical communication practices. A major change in the working day of many clinicians is a transition from face-to-face communication to remote encounters. In the next couple of issues of PEC we will publish papers on barriers and facilitators to communication in a COVID-19 context and on different aspects of video consultations and use of virtual assistants.

IMAGES
VIDEO
COMMENTS
The coronavirus pandemic has changed the way we communicate. Advised to wear facial coverings and keep our distance from each other, we've had to find substitutes for the greetings, gestures and other nonverbal cues we used to take for granted. When we communicate, "nonverbal is everything but the actual language itself," said Tricia ...
During a pandemic, communication is not only conveying messages to people but has a much wider approach. Current scenario. The most important factor in preventing the spread of the COVID-19 is to empower the people with the right information. Today in the era of COVID-19 pandemic there is an overabundance of information leading to 'infodemic'.
Given the shift to instant communication, and in a post-pandemic world where we're actively discouraged from being face-to-face with someone, being able to read the conversation, the flow and the ...
This essay addresses how the pandemic has changed people's use of digital communication methods, and how inequalities in the use of these methods may arise. ... There are also people who reduced their digital communication during the pandemic. While a small minority (5%) used text messages less often, more people reduced their communication ...
Tim Levine, Ph.D., chair and distinguished professor in the College of Arts and Sciences Department of Communication Studies at the University of Alabama at Birmingham, explains how the novel coronavirus pandemic has affected the way we communicate and its critical impact on our daily communication skills. "The most obvious changes are that ...
It's been almost a year since the pandemic changed every aspect of our lives and, in particular, the way we communicate. We asked some of you to tell us about how you've talked to the people in ...
On May 20, 2021, the National Academies of Sciences, Engineering, and Medicine held a virtual convening of public health and communications practitioners to examine the challenges, opportunities, and lessons they saw while executing effective communications and community engagement in response to the COVID-19 pandemic.
This essay addresses how the pandemic has changed people's use of digital communication methods, and how inequalities in the use of these methods may arise. We draw on data collected from 1,374 American adults between 4 and 8 April 2020, about two weeks after lockdown measures were introduced in various parts of the United States.
Turning to emails, we find that two types of email communication increased in the post-lockdown period. First, the average number of internal emails sent increased (+5.2% [+3.0% to +7.6%], +1.4 ...
Leaders and communicators need to ensure that all messaging ties back to a deeper sense of purpose. Early on in the crisis, organizations need to emphasize their goals during this pandemic. Oftentimes, especially during a long-drawn crisis, stakeholder groups can lose sight of the overarching purpose of the organization before the crisis.
The coronavirus pandemic has put the business of risk communication front and center. Every day, it seems, we are getting mixed messages from our leaders, messages that differ in their tone and content depending on who is talking. In a situation full of unknowns, as with the early days of the Ebola outbreak in West Africa five years ago ...
This article offers best practices for company communication during a pandemic, such as the current COVID-19 global emergency. The author emphasizes the need to make company communications responsible and thoughtful, not only in these challenging times, but always. Discussed are best practices for communication through many mediums, such as ...
Suddenly my small "communications" task had become a full-time job. The unsolicited medical advice and requests for specifics about my mother's treatment was taking up precious time. I knew I needed to reserve my energy for the communication with her physicians and other health care professionals.
The COVID-19 pandemic has set the tone for a "new normal" of health and well-being. This feature series aims to empower readers to take control of their mental and emotional health.
With the onset of the COVID-19 pandemic, social media has rapidly become a crucial communication tool for information generation, dissemination, and consumption. In this scoping review, we selected and examined peer-reviewed empirical studies relating to COVID-19 and social media during the first outbreak from November, 2019, to November, 2020. From an analysis of 81 studies, we identified ...
By Avivit Ben-Aharon, MS Ed, MA, CCC-SLP. |. July 23, 2021, at 8:00 a.m. Pandemic Impact on Communication Skills. More. Every year since 1927, the month of May has been designated "Better Hearing ...
3. The communication strategies during the COVID-19 pandemic. It is of great importance to ensure that the measures recommended by health authorities are complied with by the community to prevent the spread of the COVID-19 pandemic. How this information is communicated to the community is also crucial to provide compliance with the precautions.
As communicators, Covid-19 has impacted our duties as well. Typically, we are trained to prepare for a crisis: to have contingency plans and spokespeople ready to go. But most of us have never ...
It has been four years since the World Health Organization declared Covid-19 a global pandemic on March 11, 2020. The New York Times writes of the anniversary:. Four years ago today, society began ...
In any organization, how a company communicates internally, i.e., manager to employee, C-level to management, etc., is of the utmost importance. Having open and transparent comms throughout the business builds trust and fosters creativity, which in turn impacts profit margins. An easy way to improve communication is by ensuring staff at all ...
Muffled sound through 15 months (and counting) of masked communication may also impact on how we pronounce our words. At Michigan State University Sociolinguistics Lab, a team of researchers have been collecting recorded speech from Michigan residents since the beginning of April 2020 to track changes to language during the pandemic.
Conclusions To prepare for future pandemics, improved public health communications and social-emotional supports for HCWs are critical to ameliorate the physical and emotional impacts related to the social context of modern US pandemic response. No data are available. ... feelings of hope and optimism during the pandemic and (3) the compounded ...
The current labor market is characterized by drastic changes linked to the use of information and communication technologies (ICT) and post-COVID-19 transformations, which have decreased job security and job stability. As a result, the feeling of losing one's job has become even more common among European workers. In this study, we aimed to investigate whether and how job insecurity would be ...
That's why we feel that effective communication and health literacy are inter-connected and directly proportional to each other. On the 11th of March 2020, the World Health Organization (WHO) declared the ongoing outbreak of unusual pneumonia caused by SARS-CoV-2 in Wuhan province of China as the global COVID-19 pandemic. The virus was novel ...
Relatively little is known about the lived experiences of older adults during the COVID-19 pandemic. We systematically review the international literature to understand the lived experiences of older adult's experiences during the pandemic. This study uses a meta-ethnographical approach to investigate the included studies. The analyses were undertaken with constructivist grounded theory.
These widespread public health measures have been accompanied by a massive flow of COVID-19 information, misinformation, and disinformation. We are concurrently inundated with a global epidemic of misinformation, or an infodemic, primarily being spread through social media platforms; its effects on public health cannot be underestimated. 7 Thus, the pandemic provides an opportunity to develop ...
Through this paper, we examine the impact of telemedicine among patients and healthcare professionals during the second wave of COVID-19 pandemic in India. Using the electronic and communication technologies, telemedicine is used to transfer the information from one place to another place. The foremost utility peculiar to telemedicine is to render assistance in medical aid by referring to ...
In the present issue of PEC, we publish three articles on challenges for healthcare communication during the COVID-19. One of these papers is a Position Paper written by Sarah J. White and colleagues on behalf of the research committee (rEACH) of the International Association for Communication in Healthcare (EACH) [ 4 ].