
Essays About Depression: Top 8 Examples Plus Prompts
Many people deal with mental health issues throughout their lives; if you are writing essays about depression, you can read essay examples to get started.
An occasional feeling of sadness is something that everyone experiences from time to time. Still, a persistent loss of interest, depressed mood, changes in energy levels, and sleeping problems can indicate mental illness. Thankfully, antidepressant medications, therapy, and other types of treatment can be largely helpful for people living with depression.
People suffering from depression or other mood disorders must work closely with a mental health professional to get the support they need to recover. While family members and other loved ones can help move forward after a depressive episode, it’s also important that people who have suffered from major depressive disorder work with a medical professional to get treatment for both the mental and physical problems that can accompany depression.
If you are writing an essay about depression, here are 8 essay examples to help you write an insightful essay. For help with your essays, check out our round-up of the best essay checkers .
- 1. My Best Friend Saved Me When I Attempted Suicide, But I Didn’t Save Her by Drusilla Moorhouse
- 2. How can I complain? by James Blake
- 3. What it’s like living with depression: A personal essay by Nadine Dirks
- 4. I Have Depression, and I’m Proof that You Never Know the Battle Someone is Waging Inside by Jac Gochoco
- 5. Essay: How I Survived Depression by Cameron Stout
- 6. I Can’t Get Out of My Sweat Pants: An Essay on Depression by Marisa McPeck-Stringham
- 7. This is what depression feels like by Courtenay Harris Bond
8. Opening Up About My Struggle with Recurring Depression by Nora Super
1. what is depression, 2. how is depression diagnosed, 3. causes of depression, 4. different types of depression, 5. who is at risk of depression, 6. can social media cause depression, 7. can anyone experience depression, the final word on essays about depression, is depression common, what are the most effective treatments for depression, top 8 examples, 1. my best friend saved me when i attempted suicide, but i didn’t save her by drusilla moorhouse.
“Just three months earlier, I had been a patient in another medical facility: a mental hospital. My best friend, Denise, had killed herself on Christmas, and days after the funeral, I told my mom that I wanted to die. I couldn’t forgive myself for the role I’d played in Denise’s death: Not only did I fail to save her, but I’m fairly certain I gave her the idea.”
Moorhouse makes painstaking personal confessions throughout this essay on depression, taking the reader along on the roller coaster of ups and downs that come with suicide attempts, dealing with the death of a loved one, and the difficulty of making it through major depressive disorder.
2. How can I complain? by James Blake
“I wanted people to know how I felt, but I didn’t have the vocabulary to tell them. I have gone into a bit of detail here not to make anyone feel sorry for me but to show how a privileged, relatively rich-and-famous-enough-for-zero-pity white man could become depressed against all societal expectations and allowances. If I can be writing this, clearly it isn’t only oppression that causes depression; for me it was largely repression.”
Musician James Blake shares his experience with depression and talks about his struggles with trying to grow up while dealing with existential crises just as he began to hit the peak of his fame. Blake talks about how he experienced guilt and shame around the idea that he had it all on the outside—and so many people deal with issues that he felt were larger than his.
3. What it’s like living with depression: A personal essay by Nadine Dirks
“In my early adulthood, I started to feel withdrawn, down, unmotivated, and constantly sad. What initially seemed like an off-day turned into weeks of painful feelings that seemed they would never let up. It was difficult to enjoy life with other people my age. Depression made typical, everyday tasks—like brushing my teeth—seem monumental. It felt like an invisible chain, keeping me in bed.”
Dirks shares her experience with depression and the struggle she faced to find treatment for mental health issues as a Black woman. Dirks discusses how even though she knew something about her mental health wasn’t quite right, she still struggled to get the diagnosis she needed to move forward and receive proper medical and psychological care.
4. I Have Depression, and I’m Proof that You Never Know the Battle Someone is Waging Inside by Jac Gochoco
“A few years later, at the age of 20, my smile had fallen, and I had given up. The thought of waking up the next morning was too much for me to handle. I was no longer anxious or sad; instead, I felt numb, and that’s when things took a turn for the worse. I called my dad, who lived across the country, and for the first time in my life, I told him everything. It was too late, though. I was not calling for help. I was calling to say goodbye.”
Gochoco describes the war that so many people with depression go through—trying to put on a brave face and a positive public persona while battling demons on the inside. The Olympic weightlifting coach and yoga instructor now work to share the importance of mental health with others.
5. Essay: How I Survived Depression by Cameron Stout
“In 1993, I saw a psychiatrist who prescribed an antidepressant. Within two months, the medication slowly gained traction. As the gray sludge of sadness and apathy washed away, I emerged from a spiral of impending tragedy. I helped raise two wonderful children, built a successful securities-litigation practice, and became an accomplished cyclist. I began to take my mental wellness for granted. “
Princeton alum Cameron Stout shared his experience with depression with his fellow Tigers in Princeton’s alumni magazine, proving that even the most brilliant and successful among us can be rendered powerless by a chemical imbalance. Stout shares his experience with treatment and how working with mental health professionals helped him to come out on the other side of depression.
6. I Can’t Get Out of My Sweat Pants: An Essay on Depression by Marisa McPeck-Stringham
“Sometimes, when the depression got really bad in junior high, I would come straight home from school and change into my pajamas. My dad caught on, and he said something to me at dinner time about being in my pajamas several days in a row way before bedtime. I learned it was better not to change into my pajamas until bedtime. People who are depressed like to hide their problematic behaviors because they are so ashamed of the way they feel. I was very ashamed and yet I didn’t have the words or life experience to voice what I was going through.”
McPeck-Stringham discusses her experience with depression and an eating disorder at a young age; both brought on by struggles to adjust to major life changes. The author experienced depression again in her adult life, and thankfully, she was able to fight through the illness using tried-and-true methods until she regained her mental health.
7. This is what depression feels like by Courtenay Harris Bond
“The smallest tasks seem insurmountable: paying a cell phone bill, lining up a household repair. Sometimes just taking a shower or arranging a play date feels like more than I can manage. My children’s squabbles make me want to scratch the walls. I want to claw out of my own skin. I feel like the light at the end of the tunnel is a solitary candle about to blow out at any moment. At the same time, I feel like the pain will never end.”
Bond does an excellent job of helping readers understand just how difficult depression can be, even for people who have never been through the difficulty of mental illness. Bond states that no matter what people believe the cause to be—chemical imbalance, childhood issues, a combination of the two—depression can make it nearly impossible to function.
“Once again, I spiraled downward. I couldn’t get out of bed. I couldn’t work. I had thoughts of harming myself. This time, my husband urged me to start ECT much sooner in the cycle, and once again, it worked. Within a matter of weeks I was back at work, pretending nothing had happened. I kept pushing myself harder to show everyone that I was “normal.” I thought I had a pattern: I would function at a high level for many years, and then my depression would be triggered by a significant event. I thought I’d be healthy for another ten years.”
Super shares her experience with electroconvulsive therapy and how her depression recurred with a major life event despite several years of solid mental health. Thankfully, Super was able to recognize her symptoms and get help sooner rather than later.
7 Writing Prompts on Essays About Depression
When writing essays on depression, it can be challenging to think of essay ideas and questions. Here are six essay topics about depression that you can use in your essay.

Depression can be difficult to define and understand. Discuss the definition of depression, and delve into the signs, symptoms, and possible causes of this mental illness. Depression can result from trauma or personal circumstances, but it can also be a health condition due to genetics. In your essay, look at how depression can be spotted and how it can affect your day-to-day life.
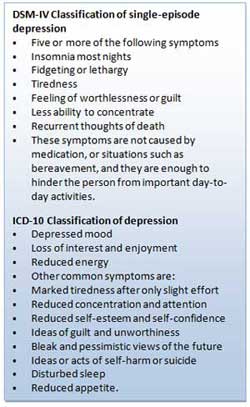
Depression diagnosis can be complicated; this essay topic will be interesting as you can look at the different aspects considered in a diagnosis. While a certain lab test can be conducted, depression can also be diagnosed by a psychiatrist. Research the different ways depression can be diagnosed and discuss the benefits of receiving a diagnosis in this essay.
There are many possible causes of depression; this essay discusses how depression can occur. Possible causes of depression can include trauma, grief, anxiety disorders, and some physical health conditions. Look at each cause and discuss how they can manifest as depression.

There are many different types of depression. This essay topic will investigate each type of depression and its symptoms and causes. Depression symptoms can vary in severity, depending on what is causing it. For example, depression can be linked to medical conditions such as bipolar disorder. This is a different type of depression than depression caused by grief. Discuss the details of the different types of depression and draw comparisons and similarities between them.
Certain genetic traits, socio-economic circumstances, or age can make people more prone to experiencing symptoms of depression. Depression is becoming more and more common amongst young adults and teenagers. Discuss the different groups at risk of experiencing depression and how their circumstances contribute to this risk.
Social media poses many challenges to today’s youth, such as unrealistic beauty standards, cyber-bullying, and only seeing the “highlights” of someone’s life. Can social media cause depression in teens? Delve into the negative impacts of social media when writing this essay. You could compare the positive and negative sides of social media and discuss whether social media causes mental health issues amongst young adults and teenagers.
This essay question poses the question, “can anyone experience depression?” Although those in lower-income households may be prone to experiencing depression, can the rich and famous also experience depression? This essay discusses whether the privileged and wealthy can experience their possible causes. This is a great argumentative essay topic, discuss both sides of this question and draw a conclusion with your final thoughts.
When writing about depression, it is important to study examples of essays to make a compelling essay. You can also use your own research by conducting interviews or pulling information from other sources. As this is a sensitive topic, it is important to approach it with care; you can also write about your own experiences with mental health issues.
Tip: If writing an essay sounds like a lot of work, simplify it. Write a simple 5 paragraph essay instead.
FAQs On Essays About Depression
According to the World Health Organization, about 5% of people under 60 live with depression. The rate is slightly higher—around 6%—for people over 60. Depression can strike at any age, and it’s important that people who are experiencing symptoms of depression receive treatment, no matter their age.
Suppose you’re living with depression or are experiencing some of the symptoms of depression. In that case, it’s important to work closely with your doctor or another healthcare professional to develop a treatment plan that works for you. A combination of antidepressant medication and cognitive behavioral therapy is a good fit for many people, but this isn’t necessarily the case for everyone who suffers from depression. Be sure to check in with your doctor regularly to ensure that you’re making progress toward improving your mental health.
If you’re still stuck, check out our general resource of essay writing topics .

Amanda has an M.S.Ed degree from the University of Pennsylvania in School and Mental Health Counseling and is a National Academy of Sports Medicine Certified Personal Trainer. She has experience writing magazine articles, newspaper articles, SEO-friendly web copy, and blog posts.
View all posts
- Essay Samples
- College Essay
- Writing Tools
- Writing guide
↑ Return to College Essay
Definition Essay – Defining depression
Depression is a mental illness under the psychological sector “Clinical psychology.” It has a few facets to it, and has numerous causes. It is also known as a mental state that most people undergo at some point in their lives. However, there are some people that get chronic depression, or forms of depression that need intervention to help bring them out of it.
A low mood is not depression
Some people think that because they are in a low mood they are depressed. Women seem to use the word depression as often as they use the toilet. Depression is a state of mind whereby there appears no future, past or hope for a person. The person feels nothing but a void and will not envision a happy future or pleasant present without provocation. It is a default position that a person takes on a conscious level that bores its way into the subconscious, which creates a negative feedback loop.
Bi-Polar (Manic Depressive) has a deeper root
People may go through a tough time and become temporarily depressed. In fact, depression is one of the five stages of the Kublar Ross grieving process, and yet a tough time, even a very bad time, does not create bi-polar disorder. This is because the condition has a deeper root that is either nestled in psychology, brought on by biochemistry, brought on by something physical, or all three.
People with Bi-polar depression go through psychological cycles that to the outside observer appear to be polar opposites. A sufferer will undergo periods of extreme sadness and hopelessness where he or she only sees a void in their past, present and future. The sufferer is often unwilling and unable to do anything productive and will feel low and horrible most of the time.
The polar opposite also occurs where the person experiences great degrees of optimism and even excitement and passivity. The person is often highly motivated and pushes him or herself to do things that they wouldn’t do otherwise. For example, if that person has been putting off re-paving the patio, then he or she may start right away by taking up the paving slabs and putting them on the drive to be collected. Many times, people undergoing such positive highs are often stricken with a negative low and their half-completed tasks remain uncompleted.
Causes can be environmental, biological, physical, genetic and psychological
Depression is not a mood, but it has as many causes as a mood. For example, if you were to define yourself as happy, which is a mood, it could be due to your environment, a drug, through a physical sensation, a psychological reason, and may even be because there is a gene that makes people predisposed to happiness. Depression works in a very similar way, except that the state of being depressed is far more serious and can be very difficult to get out of. Conclusion
Depression has a number of causes and is more than just a low or a bad mood. It can be easy to get into, though it is sometimes thrust upon people without their prior knowledge, expectation or understanding. Furthermore, it is sometimes easy to get out of depression, but many ex-sufferers have trouble “staying” un-depressed.
Follow Us on Social Media
Get more free essays

Send via email
Most useful resources for students:.
- Free Essays Download
- Writing Tools List
- Proofreading Services
- Universities Rating
Contributors Bio

Find more useful services for students
Free plagiarism check, professional editing, online tutoring, free grammar check.
Depression: A Cognitive Perspective Essay
Depression is one of the mood disorders and is a distorted mood or negative mood caused by complex imbalance in the activity in the brain or external circumstances. Therefore, those factors causing the aforementioned imbalance or negative mood can be considered as causing depression or contributing to it. It is not yet clear according to Barlow & Durand (2005) because depression has been evidenced even in 3-month old babies. However, 60% to 80% of the causes of depression can be attributed to psychological experiences according to Barlow & Durand (2005), who also adds that the cases are unique to individuals. According to the author, the major reasons that could be blamed for psychological disorders are stress and trauma resulting from life events such as loss of a job, having a child, getting divorced, and starting a career, but more importantly, individual reactions and the settings play a very important role in determining the developments. For example, some individuals sees loosing a job as opportunity to working out their hobbies, while others may be depressed because they already have a family to care for after loosing a job.
Depression is a negative emotional state arising from, usually, subconscious thoughts pulled out of the “store of thoughts” to explain circumstances. Perhaps, the implication can be well understood in considering that the cognitive therapy modules are designed to help individuals change the ways one think. This is a systematic process because, for example, negative thoughts may have been repeated overtime and for long, thus becoming automatic thoughts applied by people to respond to most conditions and circumstances or happenings in life. Maladaptive and erroneous processing of information causes depression. The individuals have faulty assumptions and beliefs arising from the biased thinking. Family experiences which are traumatic and historic may cause people to develop negative memories and cognition which cause sadness, depression or anxiety (Sarasola Mental Health Institute, 2008).
Negative core beliefs, low self-esteem and family history have been indicated as causatives of depressions. Family history has been connected to the changing in the structure of the brain and its functioning. Negative core beliefs are implicated in causing depression in that it influence thoughts, which in turn generate negative emotional states.
Cognitive approach to depression focuses on the self-repressive critical self-evaluations, pessimism, and unrealistic expectations and perceptions. These do not only establish depression but also sustain it. Cognitive approach to treating depression helps individuals change these behaviors and feelings, develop more positive assessment and develop positive life goals. Defense mechanisms expresses unconscious id whose impulses’ expression in behavior cause anxiety. When an individual represses conflict issues or has a decay of memory, unconscious thoughts (which are any mental contents and functions that are out of awareness) may emanate, according (Kihlstrom, Barnhardt & Tetaryn, 1992; Buci, 1997; qtd. in Blatt & Auerbach, 2000). Cognitive elements such as desires, personal evaluations, fears, attitudes, and expectations have been linked to human behavior and each affect the other. Therefore, cognitive approach to depression may link with behavioral explanations as well.
Historically, depression has been indicated to occur as a response to a perceived loss or imaginary loss and self-critic of ego according to Freud (1917). Cognitive approach to depression explain the causes of maladaptive cognitions as variety of life experiences such as distressful life events, family experiences, lack of proper social learning and shortage of adaptive learning.
When a person is depressed, he has a tendency of taking responsibility for all that goes wrong while he gives others credit for positive-appearing things. According to psychologists, the result of self-criticism in depressed persons may be a sense of failure, low self-esteem and criticism. Negative self-evaluation in Mary is well evident in her comments that she can’t find anyone who love her and has nothing special to offer. Negative self-evaluation may be as a result of perceived loss and family experiences that make one feel inadequate.
Another cognitive aspect of depression is identification of skill deficits where, in addition to identifying the shortage of skills, the person assumes that he or she cannot learn to act differently or achieve better results. Shortage of skills may be right, and this makes the person under depression assume that other deficits are real too. Therefore, the cause of depression on this line may be a real shortage of skills, accompanied by negative self-evaluation because the individual is more likely to see the negative aspects or the skills he lacks than those that he has. In the case study, Mary cannot see the achievement of being a graduate but recognizes that the award is without honors, he is not beautiful but was only referred to as being pretty. Causes of depression attacking an individual in this way have an influence on individuals’ values and how they feel about themselves. Life experiences and traumatic incidences may also make the individual to identify mostly with the negative aspects in his life than the positive aspects, or feel inadequate.
Unrealistic expectations cause individuals to always focus on the negative aspects of life even when the overall experience was good. In other words, these individuals focus almost always on the negative events, conditions, practices or thoughts. They evaluate incidences on an overall, based on the happening of a few bad incidences or only one incidence. These individuals may always want and expect perfection, and hence the frustration after failure, because life ahead of them may be full of imperfect situations. The individuals fail to consider or appreciate the fact that wrong things, incidences, practices and results can be repaired, corrected, started again or mended and that mostly in most of life incidences on an average scale, only a little things may be amiss. Negative self-talks may be a way of immobilizing someone to solve problems, and may result in depression. Although self-talk is normal, sometimes healthy, a process of thinking and helpful if positive, negative self-talk may impact negatively to our ability to solve problems arising and see ourselves as incapable. Negative automatic thoughts can also influence someone’s perspective of the surrounding, the people he meets with and how they relate to him. Negative automatic thoughts, like positive ones may not offer a chance for an analysis of the encountered situation or incidence, and goes ahead to judge them as presumed. If negative, automatic thoughts may cause individuals to reach a quick analysis of a situation such as people hate them or dislike them, for example when people smile at them talking, a quick negative thought would estimate that they are laughing at them rather than for example, being impressed by them. The impact of quick negative thoughts may be low self-evaluation and low attitude which have been linked to depression.
Because every person needs to cope to the world not only through physical encounter but also assumptions, perceptions and judgment, cognitive distortion manifesting through wrong or false evaluation of situations may cause depression or worsen the state of a person under depression. People may carry false assumptions about how people think about them, may over-generalize simple mistakes, or carry irrational ideas about incidences or situations (Donald, 2003).
According to Blatt and Auerbach (2000), dynamic unconsciousness which have intentionally been excluded from awareness by the individual, may manifest through unusual circumstances like dream formation, experimental primation, therapeutic process and free association. As individuals conflict with their personality issues, they may adopt defense mechanisms that repress dynamic unconsciousness. The dynamic unconscious mental contents so excluded include certain wishes or feelings that contradict with his or her other wishes or feelings. The drive of the id is suppressed by the superego (personality component holding all internalized moral standards and ideals) which is implanted in individuals by their parents. Shortly after birth, ego (personality component responsible for dealing with reality) is developed. Some individual states such as anxiety would develop when the id or the superego challenges the conscious ego. Freud’s conceptualization of development of defense mechanisms that are applied to ward off anxiety may be implicated in the theory of depression, specifically because those individuals who are depressed may show denial objective reality that is apparent to others even through erroneous interpretation of events, conditions, or circumstances. For example, loss of an immediate family member may cause people to develop most of the symptoms of major depressive episode: denial, anxiety an emotional numbness (Barlow & Durand, 2005). When severe grieving proceeds for more than a year, there is low likelihood of recovery without treatment. In addition, repression-which is the blocking of disturbing wishes, thoughts or experiences from conscious awareness-may be present in the depression status. Under such circumstance, depression may occur because the grieving process was ineffective.
- Allen Josiah. (2003). An Overview of Beck’s Cognitive Theory of Depression in Contemporary Literature . Web.
- Barlow, D.H. & Durand, V.M. (2005). Abnormal Psychology: An Integrative Approach. (5th Edition). Australia: Wadsworth
- Blatt Sidney and Auerbach John. (2000). Psychoanalytic Models of the Mind and their Contributions to Personality Research. European Journal of Personality. 14: 429-447
- Bucci W.1997. Psychoanalysis and Cognitive Science: A Multiple Code Theory. Guilford: New York
- Donald Franklin. Cognitive therapy for depression. Web.
- Gonca, S., & Savasir, I. (2001). The relationship between interpersonal schemas and depressive symptomatology. Journal of Counseling Psychology, 48, 359-364
- Freud S.(1957). The Unconscious, Strachey J. (ed.), orig.workpubl.1915, Vol.14. The Standard Edition of the Complete Psychological Works of Sigmund Freud . Hogarth: London; 166204
- Kihlstrom JF., Barnhardt TM., Tetaryn DJ.1992.The psychological unconscious: found, lost, and regained. American Psychologist 47:788791.
- Moilanen, D. L. (1993). Depressive information processing among nonclinic, nonreferred college students. Journal of Counseling Psychology, 40, 340-347
- Sarasola Mental Health Institute. (2008). Cognitive Therapy is Effective in Treating Depression and Anxiety.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, May 13). Depression: A Cognitive Perspective. https://ivypanda.com/essays/depression-and-causes/
"Depression: A Cognitive Perspective." IvyPanda , 13 May 2022, ivypanda.com/essays/depression-and-causes/.
IvyPanda . (2022) 'Depression: A Cognitive Perspective'. 13 May.
IvyPanda . 2022. "Depression: A Cognitive Perspective." May 13, 2022. https://ivypanda.com/essays/depression-and-causes/.
1. IvyPanda . "Depression: A Cognitive Perspective." May 13, 2022. https://ivypanda.com/essays/depression-and-causes/.
Bibliography
IvyPanda . "Depression: A Cognitive Perspective." May 13, 2022. https://ivypanda.com/essays/depression-and-causes/.
- Self-Evaluation of Students' Achievements
- Leadership: Self-Evaluation and Comparison
- Self-Evaluation of Understanding Knowledge Development in Nursing
- Judge and Bono on Relationships of Core Self-Evaluation Traits to Job Satisfaction and Performance
- The Contraceptives Project Self-Evaluation
- Personal Cultural Awareness in Management: Self-Evaluation
- Zara Company and the Automatic ID System
- Distinction between automatic and controlled processing
- Social Psychology: Cognitive Dissonance
- Reducing Cognitive Dissonance by Restoring Positive Self-Evaluations
- Posttraumatic Stress Symptom Disease
- Analyzing Psychological Disorders: Schizophrenia
- Various Limitations Upon Clear Thinking in the Halpern “Thought and Knowledge”
- Depression, Substance Abuse and Suicide in Elderly
- Psychological Disorder Analysis: A Case of Bipolar Disorder
Psychological Theories of Depression
Saul Mcleod, PhD
Editor-in-Chief for Simply Psychology
BSc (Hons) Psychology, MRes, PhD, University of Manchester
Saul Mcleod, PhD., is a qualified psychology teacher with over 18 years of experience in further and higher education. He has been published in peer-reviewed journals, including the Journal of Clinical Psychology.
Learn about our Editorial Process
Olivia Guy-Evans, MSc
Associate Editor for Simply Psychology
BSc (Hons) Psychology, MSc Psychology of Education
Olivia Guy-Evans is a writer and associate editor for Simply Psychology. She has previously worked in healthcare and educational sectors.
On This Page:
Depression is a mood disorder that prevents individuals from leading a normal life at work, socially, or within their family. Seligman (1973) referred to depression as the ‘common cold’ of psychiatry because of its frequency of diagnosis.
Depending on how data are gathered and how diagnoses are made, as many as 27% of some population groups may be suffering from depression at any one time (NIMH, 2001; data for older adults).
Behaviorist Theory
Behaviorism emphasizes the importance of the environment in shaping behavior. The focus is on observable behavior and the conditions through which individuals” learn behavior, namely classical conditioning, operant conditioning, and social learning theory.
Therefore, depression is the result of a person’s interaction with their environment.
For example, classical conditioning proposes depression is learned through associating certain stimuli with negative emotional states. Social learning theory states behavior is learned through observation, imitation, and reinforcement.
Operant Conditioning
Operant conditioning states that depression is caused by the removal of positive reinforcement from the environment (Lewinsohn, 1974). Certain events, such as losing your job, induce depression because they reduce positive reinforcement from others (e.g., being around people who like you).
Depressed people usually become much less socially active. In addition, depression can also be caused by inadvertent reinforcement of depressed behavior by others.
For example, when a loved one is lost, an important source of positive reinforcement has lost as well. This leads to inactivity. The main source of reinforcement is now the sympathy and attention of friends and relatives.
However, this tends to reinforce maladaptive behavior, i.e., weeping, complaining, and talking of suicide. This eventually alienates even close friends leading to even less reinforcement and increasing social isolation and unhappiness. In other words, depression is a vicious cycle in which the person is driven further and further down.
Also, if the person lacks social skills or has a very rigid personality structure, they may find it difficult to make the adjustments needed to look for new and alternative sources of reinforcement (Lewinsohn, 1974). So they get locked into a negative downward spiral.
Critical Evaluation
Behavioral/learning theories make sense in terms of reactive depression, where there is a clearly identifiable cause of depression. However, one of the biggest problems for the theory is that of endogenous depression. This is depression that has no apparent cause (i.e., nothing bad has happened to the person).
An additional problem of the behaviorist approach is that it fails to consider cognitions (thoughts) influence on mood.
Psychodynamic Theory
During the 1960s, psychodynamic theories dominated psychology and psychiatry. Depression was understood in terms of the following:
- inwardly directed anger (Freud, 1917),
- introjection of love object loss,
- severe super-ego demands (Freud, 1917),
- excessive narcissistic , oral, and/or anal personality needs (Chodoff, 1972),
- loss of self-esteem (Bibring, 1953; Fenichel, 1968), and
- deprivation in the mother-child relationship during the first year (Kleine, 1934).
Freud’s psychoanalytic theory is an example of the psychodynamic approach . Freud (1917) proposed that many cases of depression were due to biological factors.
However, Freud also argued that some cases of depression could be linked to loss or rejection by a parent. Depression is like grief in that it often occurs as a reaction to the loss of an important relationship.
However, there is an important difference because depressed people regard themselves as worthless. What happens is that the individual identifies with the lost person so that repressed anger towards the lost person is directed inwards towards the self. The inner-directed anger reduces the individual’s self-esteem and makes him/her vulnerable to experiencing depression in the future.
Freud distinguished between actual losses (e.g., the death of a loved one) and symbolic losses (e.g., the loss of a job). Both kinds of losses can produce depression by causing the individual to re-experience childhood episodes when they experience loss of affection from some significant person (e.g., a parent).
Later, Freud modified his theory stating that the tendency to internalize lost objects is normal and that depression is simply due to an excessively severe super-ego. Thus, the depressive phase occurs when the individual’s super-ego or conscience is dominant. In contrast, the manic phase occurs when the individual’s ego or rational mind asserts itself, and s/he feels control.
In order to avoid loss turning into depression, the individual needs to engage in a period of mourning work, during which s/he recalls memories of the lost one.
This allows the individual to separate himself/herself from the lost person and reduce inner-directed anger. However, individuals very dependent on others for their sense of self-esteem may be unable to do this and so remain extremely depressed.
Psychoanalytic theories of depression have had a profound impact on contemporary theories of depression.
For example, Beck’s (1983) model of depression was influenced by psychoanalytic ideas such as the loss of self-esteem (re: Beck’s negative view of self), object loss (re: the importance of loss events), external narcissistic deprivation (re: hypersensitivity to loss of social resources) and oral personality (re: sociotropic personality).
However, although highly influential, psychoanalytic theories are difficult to test scientifically. For example, its central features cannot be operationally defined with sufficient precision to allow empirical investigation. Mendelson (1990) concluded his review of psychoanalytic theories of depression by stating:
“A striking feature of the impressionistic pictures of depression painted by many writers is that they have the flavor of art rather than of science and may well represent profound personal intuitions as much as they depict they raw clinical data” (p. 31).
Another criticism concerns the psychanalytic emphasis on the unconscious, intrapsychic processes, and early childhood experience as being limiting in that they cause clinicians to overlook additional aspects of depression. For example, conscious negative self-verbalization (Beck, 1967) or ongoing distressing life events (Brown & Harris, 1978).
Cognitive Explanation of Depression
This approach focuses on people’s beliefs rather than their behavior. Depression results from systematic negative bias in thinking processes.
Emotional, behavioral (and possibly physical) symptoms result from cognitive abnormality. This means that depressed patients think differently from clinically normal people. The cognitive approach also assumes changes in thinking precede (i.e., come before) the onset of a depressed mood.
Beck’s (1967) Theory
One major cognitive theorist is Aaron Beck. He studied people suffering from depression and found that they appraised events in a negative way.
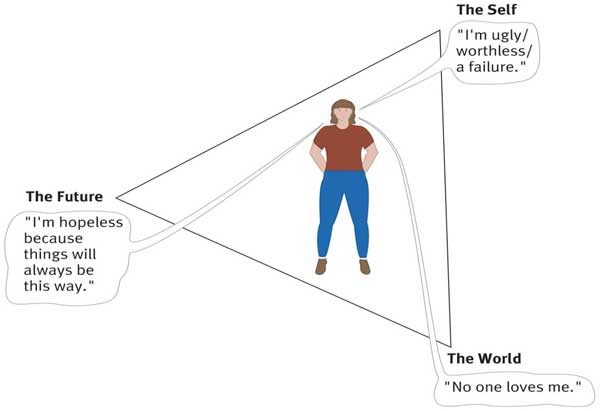
Beck (1967) identified three mechanisms that he thought were responsible for depression:
The cognitive triad (of negative automatic thinking) Negative self schemas Errors in Logic (i.e. faulty information processing)
The cognitive triad is three forms of negative (i.e., helpless and critical) thinking that are typical of individuals with depression: namely, negative thoughts about the self, the world, and the future. These thoughts tended to be automatic in depressed people as they occurred spontaneously.
For example, depressed individuals tend to view themselves as helpless, worthless, and inadequate. They interpret events in the world in an unrealistically negative and defeatist way, and they see the world as posing obstacles that can’t be handled.
Finally, they see the future as totally hopeless because their worthlessness will prevent their situation from improving.
As these three components interact, they interfere with normal cognitive processing, leading to impairments in perception, memory, and problem-solving, with the person becoming obsessed with negative thoughts.
Beck believed that depression-prone individuals develop a negative self-schema . They possess a set of beliefs and expectations about themselves that are essentially negative and pessimistic. Beck claimed that negative schemas might be acquired in childhood as a result of a traumatic event. Experiences that might contribute to negative schemas include:
- Death of a parent or sibling.
- Parental rejection, criticism, overprotection, neglect, or abuse.
- Bullying at school or exclusion from a peer group.
However, a negative self-schema predisposes the individual to depression, and therefore someone who has acquired a cognitive triad will not necessarily develop depression.
Some kind of stressful life event is required to activate this negative schema later in life. Once the negative schema is activated, a number of illogical thoughts or cognitive biases seem to dominate thinking .
People with negative self-schemas become prone to making logical errors in their thinking, and they tend to focus selectively on certain aspects of a situation while ignoring equally relevant information.
Beck (1967) identified a number of systematic negative biases in information processing known as logical errors or faulty thinking. These illogical thought patterns are self-defeating and can cause great anxiety or depression for the individual. For example:
- Arbitrary Inference: Drawing a negative conclusion in the absence of supporting data.
- Selective Abstraction: Focusing on the worst aspects of any situation.
- Magnification and Minimisation: If they have a problem, they make it appear bigger than it is. If they have a solution they make it smaller.
- Personalization: Negative events are interpreted as their fault.
- Dichotomous Thinking: Everything is seen as black and white. There is no in between.
Such thoughts exacerbate and are exacerbated by the cognitive triad. Beck believed these thoughts or this way of thinking become automatic.
When a person’s stream of automatic thoughts is very negative, you would expect a person to become depressed. Quite often these negative thoughts will persist even in the face of contrary evidence.
Alloy et al. (1999) followed the thinking styles of young Americans in their early 20s for six years. Their thinking style was tested, and they were placed in either the ‘positive thinking group’ or ‘negative thinking group’.
After six years, the researchers found that only 1% of the positive group developed depression compared to 17% of the ‘negative’ group. These results indicate there may be a link between cognitive style and the development of depression.
However, such a study may suffer from demand characteristics. The results are also correlational. It is important to remember that the precise role of cognitive processes is yet to be determined. The maladaptive cognitions seen in depressed people may be a consequence rather than a cause of depression.
Learned Helplessness
Martin Seligman (1974) proposed a cognitive explanation of depression called learned helplessness .
According to Seligman’s learned helplessness theory, depression occurs when a person learns that their attempts to escape negative situations make no difference.
Consequently, they become passive and will endure aversive stimuli or environments even when escape is possible.
Seligman based his theory on research using dogs.
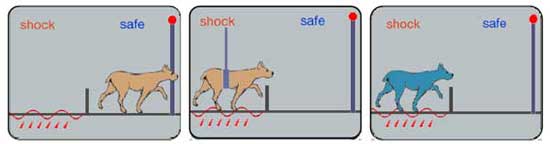
A dog put into a partitioned cage learns to escape when the floor is electrified. If the dog is restrained whilst being shocked, it eventually stops trying to escape.
Dogs subjected to inescapable electric shocks later failed to escape from shocks even when it was possible to do so. Moreover, they exhibited some of the symptoms of depression found in humans (lethargy, sluggishness, passive in the face of stress, and appetite loss).
This led Seligman (1974) to explain depression in humans in terms of learned helplessness , whereby the individual gives up trying to influence their environment because they have learned that they are helpless as a consequence of having no control over what happens to them.
Although Seligman’s account may explain depression to a certain extent, it fails to take into account cognitions (thoughts). Abramson, Seligman, and Teasdale (1978) consequently introduced a cognitive version of the theory by reformulating learned helplessness in terms of attributional processes (i.e., how people explain the cause of an event).
The depression attributional style is based on three dimensions, namely locus (whether the cause is internal – to do with a person themselves, or external – to do with some aspect of the situation), stability (whether the cause is stable and permanent or unstable and transient) and global or specific (whether the cause relates to the “whole” person or just some particular feature characteristic).
In this new version of the theory, the mere presence of a negative event was not considered sufficient to produce a helpless or depressive state. Instead, Abramson et al. argued that people who attribute failure to internal, stable, and global causes are more likely to become depressed than those who attribute failure to external, unstable, and specific causes.
This is because the former attributional style leads people to the conclusion that they are unable to change things for the better.
Gotlib and Colby (1987) found that people who were formerly depressed are actually no different from people who have never been depressed in terms of their tendencies to view negative events with an attitude of helpless resignation.
This suggests that helplessness could be a symptom rather than a cause of depression. Moreover, it may be that negative thinking generally is also an effect rather than a cause of depression.
Humanist Approach
Humanists believe that there are needs that are unique to the human species. According to Maslow (1962), the most important of these is the need for self-actualization (achieving our potential). The self-actualizing human being has a meaningful life. Anything that blocks our striving to fulfill this need can be a cause of depression. What could cause this?
- Parents impose conditions of worth on their children. I.e., rather than accepting the child for who s/he is and giving unconditional love , parents make love conditional on good behavior. E.g., a child may be blamed for not doing well at school, develop a negative self-image and feel depressed because of a failure to live up to parentally imposed standards.
- Some children may seek to avoid this by denying their true selves and projecting an image of the kind of person they want to be. This façade or false self is an effort to please others. However, the splitting off of the real self from the person you are pretending to cause hatred of the self. The person then comes to despise themselves for living a lie.
- As adults, self-actualization can be undermined by unhappy relationships and unfulfilling jobs. An empty shell marriage means the person is unable to give and receive love from their partner. An alienating job means the person is denied the opportunity to be creative at work.
Abramson, L. Y., Seligman, M. E., & Teasdale, J. D. (1978). Learned helplessness in humans: critique and reformulation . Journal of abnormal psychology, 87(1) , 49.
Alloy, L. B., Abramson, L. Y., Whitehouse, W. G., Hogan, M. E., Tashman, N. A., Steinberg, D. L., … & Donovan, P. (1999). Depressogenic cognitive styles : Predictive validity, information processing and personality characteristics, and developmental origins. behavior research and therapy, 37(6) , 503-531.
Beck, A. T. (1967). Depression: Causes and treatment . Philadelphia: University of Pennsylvania Press.
Beck, A. T., Epstein, N., & Harrison, R. (1983). Cognitions, attitudes and personality dimensions in depression. British Journal of Cognitive Psychotherapy .
Bibring, E. (1953). The mechanism of depression .
Brown, G. W., & Harris, T. (1978). Social origins of depression: a reply. Psychological Medicine, 8(04) , 577-588.
Chodoff, P. (1972). The depressive personality: A critical review. Archives of General Psychiatry, 27(5) , 666-673.
Fenichel, O. (1968). Depression and mania. The Meaning of Despair . New York: Science House.
Freud, S. (1917). Mourning and melancholia. Standard edition, 14(19) , 17.
Gotlib, I. H., & Colby, C. A. (1987). Treatment of depression: An interpersonal systems approach. Pergamon Press.
Klein, M. (1934). Psychogenesis of manic-depressive states: contributions to psychoanalysis . London: Hogarth.
Lewinsohn, P. M. (1974). A behavioral approach to depression .
Maslow, A. H. (1962). Towards a psychology of being . Princeton: D. Van Nostrand Company.
National Institute of Mental Health. (2001). Depression research at the National Institute of Mental Health http://www.nimh.nih.gov/health/publications/depression/complete-index.shtml.
Seligman, M. E. (1973). Fall into helplessness. Psychology today, 7(1) , 43-48.
Seligman, M. E. (1974). Depression and learned helplessness . John Wiley & Sons.
Further Information
- List of Support Groups
- Campaign against Living Miserably
- Men do cry: one man’s experience of depression
- NHS Self Help Guides
- Patient Care & Health Information
- Diseases & Conditions
- Depression (major depressive disorder)
- What is depression? A Mayo Clinic expert explains.
Learn more about depression from Craig Sawchuk, Ph.D., L.P., clinical psychologist at Mayo Clinic.
Hi, I'm Dr. Craig Sawchuk, a clinical psychologist at Mayo Clinic. And I'm here to talk with you about depression. Whether you're looking for answers for yourself, a friend, or loved one, understanding the basics of depression can help you take the next step.
Depression is a mood disorder that causes feelings of sadness that won't go away. Unfortunately, there's a lot of stigma around depression. Depression isn't a weakness or a character flaw. It's not about being in a bad mood, and people who experience depression can't just snap out of it. Depression is a common, serious, and treatable condition. If you're experiencing depression, you're not alone. It honestly affects people of all ages and races and biological sexes, income levels and educational backgrounds. Approximately one in six people will experience a major depressive episode at some point in their lifetime, while up to 16 million adults each year suffer from clinical depression. There are many types of symptoms that make up depression. Emotionally, you may feel sad or down or irritable or even apathetic. Physically, the body really slows down. You feel tired. Your sleep is often disrupted. It's really hard to get yourself motivated. Your thinking also changes. It can just be hard to concentrate. Your thoughts tend to be much more negative. You can be really hard on yourself, feel hopeless and helpless about things. And even in some cases, have thoughts of not wanting to live. Behaviorally, you just want to pull back and withdraw from others, activities, and day-to-day responsibilities. These symptoms all work together to keep you trapped in a cycle of depression. Symptoms of depression are different for everyone. Some symptoms may be a sign of another disorder or medical condition. That's why it's important to get an accurate diagnosis.
While there's no single cause of depression, most experts believe there's a combination of biological, social, and psychological factors that contribute to depression risk. Biologically, we think about genetics or a family history of depression, health conditions such as diabetes, heart disease or thyroid disorders, and even hormonal changes that happen over the lifespan, such as pregnancy and menopause. Changes in brain chemistry, especially disruptions in neurotransmitters like serotonin, that play an important role in regulating many bodily functions, including mood, sleep, and appetite, are thought to play a particularly important role in depression. Socially stressful and traumatic life events, limited access to resources such as food, housing, and health care, and a lack of social support all contribute to depression risk. Psychologically, we think of how negative thoughts and problematic coping behaviors, such as avoidance and substance use, increase our vulnerability to depression.
The good news is that treatment helps. Effective treatments for depression exist and you do have options to see what works best for you. Lifestyle changes that improve sleep habits, exercise, and address underlying health conditions can be an important first step. Medications such as antidepressants can be helpful in alleviating depressive symptoms. Therapy, especially cognitive behavioral therapy, teaches skills to better manage negative thoughts and improve coping behaviors to help break you out of cycles of depression. Whatever the cause, remember that depression is not your fault and it can be treated.
To help diagnose depression, your health care provider may use a physical exam, lab tests, or a mental health evaluation. These results will help identify various treatment options that best fit your situation.
Help is available. You don't have to deal with depression by yourself. Take the next step and reach out. If you're hesitant to talk to a health care provider, talk to a friend or loved one about how to get help. Living with depression isn't easy and you're not alone in your struggles. Always remember that effective treatments and supports are available to help you start feeling better. Want to learn more about depression? Visit mayoclinic.org. Do take care.
Depression is a mood disorder that causes a persistent feeling of sadness and loss of interest. Also called major depressive disorder or clinical depression, it affects how you feel, think and behave and can lead to a variety of emotional and physical problems. You may have trouble doing normal day-to-day activities, and sometimes you may feel as if life isn't worth living.
More than just a bout of the blues, depression isn't a weakness and you can't simply "snap out" of it. Depression may require long-term treatment. But don't get discouraged. Most people with depression feel better with medication, psychotherapy or both.
Depression care at Mayo Clinic
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Although depression may occur only once during your life, people typically have multiple episodes. During these episodes, symptoms occur most of the day, nearly every day and may include:
- Feelings of sadness, tearfulness, emptiness or hopelessness
- Angry outbursts, irritability or frustration, even over small matters
- Loss of interest or pleasure in most or all normal activities, such as sex, hobbies or sports
- Sleep disturbances, including insomnia or sleeping too much
- Tiredness and lack of energy, so even small tasks take extra effort
- Reduced appetite and weight loss or increased cravings for food and weight gain
- Anxiety, agitation or restlessness
- Slowed thinking, speaking or body movements
- Feelings of worthlessness or guilt, fixating on past failures or self-blame
- Trouble thinking, concentrating, making decisions and remembering things
- Frequent or recurrent thoughts of death, suicidal thoughts, suicide attempts or suicide
- Unexplained physical problems, such as back pain or headaches
For many people with depression, symptoms usually are severe enough to cause noticeable problems in day-to-day activities, such as work, school, social activities or relationships with others. Some people may feel generally miserable or unhappy without really knowing why.
Depression symptoms in children and teens
Common signs and symptoms of depression in children and teenagers are similar to those of adults, but there can be some differences.
- In younger children, symptoms of depression may include sadness, irritability, clinginess, worry, aches and pains, refusing to go to school, or being underweight.
- In teens, symptoms may include sadness, irritability, feeling negative and worthless, anger, poor performance or poor attendance at school, feeling misunderstood and extremely sensitive, using recreational drugs or alcohol, eating or sleeping too much, self-harm, loss of interest in normal activities, and avoidance of social interaction.
Depression symptoms in older adults
Depression is not a normal part of growing older, and it should never be taken lightly. Unfortunately, depression often goes undiagnosed and untreated in older adults, and they may feel reluctant to seek help. Symptoms of depression may be different or less obvious in older adults, such as:
- Memory difficulties or personality changes
- Physical aches or pain
- Fatigue, loss of appetite, sleep problems or loss of interest in sex — not caused by a medical condition or medication
- Often wanting to stay at home, rather than going out to socialize or doing new things
- Suicidal thinking or feelings, especially in older men
When to see a doctor
If you feel depressed, make an appointment to see your doctor or mental health professional as soon as you can. If you're reluctant to seek treatment, talk to a friend or loved one, any health care professional, a faith leader, or someone else you trust.
When to get emergency help
If you think you may hurt yourself or attempt suicide, call 911 in the U.S. or your local emergency number immediately.
Also consider these options if you're having suicidal thoughts:
- Call your doctor or mental health professional.
- Contact a suicide hotline.
- In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline, available 24 hours a day, seven days a week. Or use the Lifeline Chat . Services are free and confidential.
- U.S. veterans or service members who are in crisis can call 988 and then press “1” for the Veterans Crisis Line . Or text 838255. Or chat online .
- The Suicide & Crisis Lifeline in the U.S. has a Spanish language phone line at 1-888-628-9454 (toll-free).
- Reach out to a close friend or loved one.
- Contact a minister, spiritual leader or someone else in your faith community.
If you have a loved one who is in danger of suicide or has made a suicide attempt, make sure someone stays with that person. Call 911 or your local emergency number immediately. Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
More Information
Depression (major depressive disorder) care at Mayo Clinic
- Male depression: Understanding the issues
- Nervous breakdown: What does it mean?
- Pain and depression: Is there a link?
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.

Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
It's not known exactly what causes depression. As with many mental disorders, a variety of factors may be involved, such as:
- Biological differences. People with depression appear to have physical changes in their brains. The significance of these changes is still uncertain, but may eventually help pinpoint causes.
- Brain chemistry. Neurotransmitters are naturally occurring brain chemicals that likely play a role in depression. Recent research indicates that changes in the function and effect of these neurotransmitters and how they interact with neurocircuits involved in maintaining mood stability may play a significant role in depression and its treatment.
- Hormones. Changes in the body's balance of hormones may be involved in causing or triggering depression. Hormone changes can result with pregnancy and during the weeks or months after delivery (postpartum) and from thyroid problems, menopause or a number of other conditions.
- Inherited traits. Depression is more common in people whose blood relatives also have this condition. Researchers are trying to find genes that may be involved in causing depression.
- Marijuana and depression
- Vitamin B-12 and depression
Risk factors
Depression often begins in the teens, 20s or 30s, but it can happen at any age. More women than men are diagnosed with depression, but this may be due in part because women are more likely to seek treatment.
Factors that seem to increase the risk of developing or triggering depression include:
- Certain personality traits, such as low self-esteem and being too dependent, self-critical or pessimistic
- Traumatic or stressful events, such as physical or sexual abuse, the death or loss of a loved one, a difficult relationship, or financial problems
- Blood relatives with a history of depression, bipolar disorder, alcoholism or suicide
- Being lesbian, gay, bisexual or transgender, or having variations in the development of genital organs that aren't clearly male or female (intersex) in an unsupportive situation
- History of other mental health disorders, such as anxiety disorder, eating disorders or post-traumatic stress disorder
- Abuse of alcohol or recreational drugs
- Serious or chronic illness, including cancer, stroke, chronic pain or heart disease
- Certain medications, such as some high blood pressure medications or sleeping pills (talk to your doctor before stopping any medication)
Complications
Depression is a serious disorder that can take a terrible toll on you and your family. Depression often gets worse if it isn't treated, resulting in emotional, behavioral and health problems that affect every area of your life.
Examples of complications associated with depression include:
- Excess weight or obesity, which can lead to heart disease and diabetes
- Pain or physical illness
- Alcohol or drug misuse
- Anxiety, panic disorder or social phobia
- Family conflicts, relationship difficulties, and work or school problems
- Social isolation
- Suicidal feelings, suicide attempts or suicide
- Self-mutilation, such as cutting
- Premature death from medical conditions
- Depression and anxiety: Can I have both?
There's no sure way to prevent depression. However, these strategies may help.
- Take steps to control stress, to increase your resilience and boost your self-esteem.
- Reach out to family and friends, especially in times of crisis, to help you weather rough spells.
- Get treatment at the earliest sign of a problem to help prevent depression from worsening.
- Consider getting long-term maintenance treatment to help prevent a relapse of symptoms.
- Brown AY. Allscripts EPSi. Mayo Clinic, Rochester, Minn. Nov. 17, 2016.
- Research report: Psychiatry and psychology, 2016-2017. Mayo Clinic. http://www.mayo.edu/research/departments-divisions/department-psychiatry-psychology/overview?_ga=1.199925222.939187614.1464371889. Accessed Jan. 23, 2017.
- Depressive disorders. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. Arlington, Va.: American Psychiatric Association; 2013. http://www.psychiatryonline.org. Accessed Jan. 23, 2017.
- Depression. National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/depression/index.shtml. Accessed Jan. 23, 2017.
- Depression. National Alliance on Mental Illness. http://www.nami.org/Learn-More/Mental-Health-Conditions/Depression/Overview. Accessed Jan. 23, 2017.
- Depression: What you need to know. National Institute of Mental Health. https://www.nimh.nih.gov/health/publications/depression-what-you-need-to-know/index.shtml. Accessed Jan. 23, 2017.
- What is depression? American Psychiatric Association. https://www.psychiatry.org/patients-families/depression/what-is-depression. Accessed Jan. 23, 2017.
- Depression. NIH Senior Health. https://nihseniorhealth.gov/depression/aboutdepression/01.html. Accessed Jan. 23, 2017.
- Children’s mental health: Anxiety and depression. Centers for Disease Control and Prevention. https://www.cdc.gov/childrensmentalhealth/depression.html#depression. Accessed. Jan. 23, 2017.
- Depression and complementary health approaches: What the science says. National Center for Complementary and Integrative Health. https://nccih.nih.gov/health/providers/digest/depression-science. Accessed Jan. 23, 2017.
- Depression. Natural Medicines. https://naturalmedicines.therapeuticresearch.com/databases/medical-conditions/d/depression.aspx. Accessed Jan. 23, 2017.
- Natural medicines in the clinical management of depression. Natural Medicines. http://naturaldatabase.therapeuticresearch.com/ce/CECourse.aspx?cs=naturalstandard&s=ND&pm=5&pc=15-111. Accessed Jan. 23, 2017.
- The road to resilience. American Psychological Association. http://www.apa.org/helpcenter/road-resilience.aspx. Accessed Jan. 23, 2017.
- Simon G, et al. Unipolar depression in adults: Choosing initial treatment. http://www.uptodate.com/home. Accessed Jan. 23, 2017.
- Stewart D, et al. Risks of antidepressants during pregnancy: Selective serotonin reuptake inhibitors (SSRIs). http://www.uptodate.com/home. Accessed Jan. 23, 2017.
- Kimmel MC, et al. Safety of infant exposure to antidepressants and benzodiazepines through breastfeeding. http://www.uptodate.com/home. Accessed Jan. 23, 2017.
- Bipolar and related disorders. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. Arlington, Va.: American Psychiatric Association; 2013. http://www.psychiatryonline.org. Accessed Jan. 23, 2017.
- Hirsch M, et al. Monoamine oxidase inhibitors (MAOIs) for treating depressed adults. http://www.uptodate.com/home. Accessed Jan. 24, 2017.
- Hall-Flavin DK (expert opinion). Mayo Clinic, Rochester, Minn. Jan. 31, 2017.
- Krieger CA (expert opinion). Mayo Clinic, Rochester, Minn. Feb. 2, 2017.
- Antidepressant withdrawal: Is there such a thing?
- Antidepressants and alcohol: What's the concern?
- Antidepressants and weight gain: What causes it?
- Antidepressants: Can they stop working?
- Antidepressants: Selecting one that's right for you
- Antidepressants: Side effects
- Antidepressants: Which cause the fewest sexual side effects?
- Atypical antidepressants
- Clinical depression: What does that mean?
- Depression in women: Understanding the gender gap
- Depression, anxiety and exercise
- Depression: Supporting a family member or friend
- MAOIs and diet: Is it necessary to restrict tyramine?
- Monoamine oxidase inhibitors (MAOIs)
- Natural remedies for depression: Are they effective?
- Selective serotonin reuptake inhibitors (SSRIs)
- Serotonin and norepinephrine reuptake inhibitors (SNRIs)
- Treatment-resistant depression
- Tricyclic antidepressants and tetracyclic antidepressants
Associated Procedures
- Complete blood count (CBC)
- Electroconvulsive therapy (ECT)
- Psychotherapy
- Transcranial magnetic stimulation
- Vagus nerve stimulation
News from Mayo Clinic
- Mayo Clinic Q and A: How to support a loved one with depression Oct. 23, 2022, 11:00 a.m. CDT
- Mayo study lays foundation to predict antidepressant response in people with suicide attempts Oct. 03, 2022, 03:30 p.m. CDT
- Science Saturday: Researchers validate threshold for determining effectiveness of antidepressant treatment Aug. 27, 2022, 11:00 a.m. CDT
- Mayo Clinic expert explains differences between adult and teen depression May 24, 2022, 12:19 p.m. CDT
Mayo Clinic in Rochester, Minnesota, has been recognized as one of the top Psychiatry hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Let’s celebrate our doctors!
Join us in celebrating and honoring Mayo Clinic physicians on March 30th for National Doctor’s Day.
Home — Essay Samples — Nursing & Health — Depression — Depression: Definition, Risks, Symptoms and Treatment
Depression: Definition, Risks, Symptoms and Treatment
- Categories: Depression
About this sample

Words: 585 |
Published: Jan 29, 2019
See expert comments
Words: 585 | Page: 1 | 3 min read
- Serotonin-norepinephrine reuptake inhibitors (SNRIs),
- Atypical antidepressants,
- Tricyclic antidepressants,
- Monoamine oxidase inhibitors (MAOIs), or other medications.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 1087 words
1 pages / 605 words
1 pages / 618 words
2 pages / 834 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Depression
Pessimism and depression are two psychological phenomena that often go hand in hand, creating a complex and challenging experience for those who grapple with them. While pessimism is a general outlook characterized by a negative [...]
Nurse burnout has become a pressing issue in the healthcare industry, with detrimental effects on both nurses and patient care. Understanding the causes and effects of burnout, as well as implementing strategies for prevention, [...]
Depression is a prevalent mental health condition that affects millions of people worldwide. According to the World Health Organization (WHO), depression is the leading cause of disability globally, and it is a major contributor [...]
Depression is a common mental health disorder that affects millions of people worldwide. It can have a significant impact on an individual's quality of life and overall well-being. Understanding the causes, symptoms, and [...]
In the world of psychology, the case study of Ileana Chivescu stands out as a compelling and complex examination of the human mind. This tale of a young woman's struggle with anxiety, depression, and self-doubt offers a poignant [...]
Obesity and Depression today are one of the biggest issues that our societies are facing. These two problems are looked differently upon by the masses however they both share common links and connections between in which both [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Essay On Depression: Causes, Symptoms And Effects
Our life is full of emotional ups and downs, but when the time of down lasts too long or influences our ability to function, in this case, probably, you suffer from common serious illness, which is called depression. Clinical depression affects your mood, thinking process, your body and behaviour. According to the researches, in the United States about 19 million people, i.e. one in ten adults, annually suffer from depression, and about 2/3 of them do not get necessary help. An appropriate treatment can alleviate symptoms of depression in more than 80% of such cases. However, since depression is usually not recognized, it continues to cause unnecessary suffering.
Depression is a disease that dominates you and weakens your body, it influences men as well as women, but women experience depression about two times more often than men.
Since this issue is very urgent nowadays, we decided to write this cause and effect essay on depression to attract the public attention one more time to this problem. I hope it will be informative and instructive for you. If you are interested in reading essays on similar or any other topic, you should visit our website . There you will find not only various essays, but also you can get help in essay writing . All you need is to contact our team, and everything else we will do for you.
Depression is a strong psychological disorder, from which usually suffers not only a patients, but also his / hers family, relatives, friends etc.
General information
More often depression develops on the basis of stress or prolonged traumatic situation. Frequently depressive disorders hide under the guise of a bad mood or temper features. In order to prevent severe consequences it is important to figure out how and why depression begins.
Symptoms and causes of depression
As a rule, depression develops slowly and insensibly for a person and for his close ones. At the initial stage most of people are not aware about their illness, because they think that many symptoms are just the features of their personality. Experiencing inner discomfort, which can be difficult to express in words, people do not ask for professional help, as a rule. They usually go to doctor at the moment, when the disease is already firmly holds the patient causing unbearable suffering.
Risk factors for depression:
- being female;
- the presence of depression in family anamnesis;
- early depression in anamnesis;
- early loss of parents;
- the experience of violence in anamnesis;
- personal features;
- stressors (parting, guilt);
- alcohol / drug addiction;
- neurological diseases (Parkinson's disease, apoplexy).
Signs of depression
Depression influences negatively all the aspects of human life. Inadequate psychological defense mechanisms, in their turn, affect destructively not only psychological, but also biological processes.
The first signs of depression are apathy, not depending on the circumstances, indifference to everything what is going on, weakening of motor activity; these are the main clinical symptoms of depression . If their combination is observed for more than two weeks, urgent professional help is required.
Psychological symptoms:
- depressed mood, unhappiness;
- loss of interest, reduced motivation, loss of energy;
- self-doubt, guilt, inner emptiness;
- decrease in speed of thinking, inability to make decisions;
- anxiety, fear and pessimism about the future;
- daily fluctuations;
- possible delirium;
- suicidal thoughts.
Somatic symptoms:
- vital disorders;
- disturbed sleep (early waking, oversleeping);
- eating disorders;
- constipation;
- feeling of tightness of the skull, dizziness, feeling of compression;
- vegetative symptoms.
Causes of depression
It is accepted to think in modern psychiatry that the development of depression, as well as most of other mental disorders, requires the combined effect of three factors: psychological, biological and social.
Psychological factor (“Personality structure”)
There are three types of personality especially prone to depression:
1) “Statothymic personality” that is characterized by exaggerated conscientiousness, diligence, accuracy;
2) Melancholic personality type with its desire for order, constancy, pedantry, exessive demands on itself;
3) Hyperthymic type of personality that is characterized by self-doubt, frequent worries, with obviously low self-esteem.
People, whose organism biologically tends to depression development, due to education and other social environmental factors form such personality features, which in adverse social situations, especially while chronic stress, cause failure of psychological adaptation mechanisms, skills to deal with stress or lack of coping strategies.
Such people are characterized by:
- lack of confidence in their own abilities;
- excessive secrecy and isolation;
- excessive self-critical attitude towards yourself;
- waiting for the support of the close ones;
- developed pessimism;
- inability to resist stress situations;
- emotional expressiveness.
Biological factor:
- the presence of unfavorable heredity;
- somatic and neurological head injury that violated brain activity;
- changes in the hormonal system;
- chronobiological factors: seasonal depressive disorders, daily fluctuations, shortening of REM sleep;
- side effects of some medications.
- Heredity and family tendency to depression play significant role in predisposition to this disease. It is noticed that relatives of those who suffer from depression usually have different psychosomatic disorders.
Social factor:
- the presence of frequent stress situations, chronic stress;
- adverse family relationships;
- adverse childhood experience, the absence of tenderness from parents, ill-treatment and sexual harassment, interpersonal loss, severe methods of education, negative childhood memories;
- urbanization;
- significant changes in the life;
- population migration;
- increased lifetime.
People in a state of chronic stress suffer from depression more often. If some acute stress situation happens during the period of chronic stress, the probability of depression symptoms development increases.
If you decide to fight the depression, remember that you are not alone! Every fifth person in the world at least once in the life experienced depression. If you notice the signs of depression that disturb you for more than two weeks, you should go to the specialist.
Do not delay visit, in this case time does not heal. The professionalism of the doctors and a complex program of treatment will help to get rid of any kind of depression.
Where to go for help
If you do not where to go for help, ask your family physician, obstetrician, gynecologist or the clinic. In an emergency situation, the emergency doctor can provide temporary help for patients with emotional problems and give them an advice where and how they can ask for the further help.
Here is the list of people and organizations that can diagnose and suggest a course of treatment, or can give a direction to the examination and treatment.
- Family doctors.
- Such specialists as psychiatrists, psychologists, social workers and consultants on mental health.
- Health maintenance organizations.
- Local centers for the treatment of mental illness.
- The Department of Psychiatry in hospitals and outpatient clinics.
- Programs at universities and medical schools.
- Family assistance services and social services departments.
- Private clinics and institutions.
- Care centers in the workplace.
- Local health and (or) mental health communities.
It is very important in depressive episode treatment to understand that this is depression of a certain person, do not make attempts to excessive generalization of symptoms and factors of disease development. It requires personal approach to each patient.
So, as you can see, depression is a serious disease that requires professional treatment. If you manage to recognize the signs of depression at its early stage and ask for professional help, you can successfully overcome this problem. I hope this essay about depression was useful for you, and you got what you were looking for.
Calculate Your Price
- Free Samples
- Popular topics
Recent posts
- Best Dissertation Writer: Stop Being Helpless
- Essay On Empathy: How Not to Lose Yourself
- Competent and Experienced Online Assignment Writing Service
- Papers Editing Services Help to Find Your Calling
- It Is Time to Order Best Dissertation Writing Services
Tired of endless home tasks on quarantine? No more worries!
Use your limited chance to get a special 22% OFF!
Apply the code "stayhome" while placing your order and enjoy the outstanding results!
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Dialogues Clin Neurosci
- v.10(3); 2008 Sep
Language: English | Spanish | French
Basic concepts of depression
Conceptos básicos sobre la depresión, concepts de base de la dépression, eugene s. paykel.
University of Cambridge, Department of Psychiatry, Cambridge, UK
This paper reviews concepts of depression, including history and classification. The original broad concept of melancholia included all forms of quiet insanity. The term depression began to appear in the nineteenth century as did the modern concept of affective disorders, with the core disturbance now viewed as one of mood. The 1930s saw the introduction of defined criteria into official diagnostic schemes. The modern separation into unipolar and bipolar disorder was introduced following empirical research by Angst and Perris in the 1960s. The partially overlapping distinctions between psychotic and neurotic depression, and between endogenous and reactive depression, started to generate debate in the 1920s, with considerable multivariate research in the 1960s. The symptom element in endogenous depression currently survives in melancholia or somatic syndrome. Life stress is common in various depressive pictures. Dysthymia, a valuable diagnosis, represents a form of what was regarded earlier as neurotic depression. Other subtypes are also discussed.
Este articulo revisa conceptos sobre la depresión, los que incluyen historia y clasificación. El amplio concepto original de melancolía incorporaba todas las formas leves de locura. El término depresión comenzó a aparecer en el siglo XIX, y al igual que el concepto moderno de trastornos afectivos, consideró como esencial la alteración del ánimo. En la década de 1980 se produjo la introducción de criterios definidos en esquemas diagnósticos oficiales. La moderna separación entre el trastorno unipolar y bipolar surgió a partir de la investigación empírica de Angst y Perris en la década de 1960. Las distinciones que se traslapan parcialmente entre depresión psicótica y neurótica, y entre depresión endógena y reactiva comenzaron a generar debate en la década de 1920 con una importante investigación de multiples variables en la década de 1960. El síntoma central de la depresión endógena perdura actualmente en la melancolía o el síndrome somático. El estrés de la vida es común a varios cuadros depresivos. La distimia, un diagnóstico útil, representa una forma de lo que antes se consideró la depresión neurótica. También se discuten otros subtipos de depresión.
Cet article fait le point sur les concepts de la dépression, incluant son histoire et sa classification. À l'origine, la notion large de mélancolie englobait toutes les formes de folie calme. Le terme de dépression est apparu au XIX e siècle, comme le concept moderne de troubles affectifs, les troubles de l'humeur étant aujourd'hui au coeur de la dépression. Des critères précis ont fait leur apparition dans les années 80 avec des arbres diagnostiques officiels. La séparation moderne entre maladie uni- et bipolaire a suivi la recherche empirique d'Angst et Perris dans les années 60. C'est dans les années 20 que les distinctions, bien que comprenant des similarités, entre dépression psychotique et névrotique, et entre dépression endogène et réactive ont commencé à faire débat, générant une recherche considérable dans les années 60. La mélancolie ou le syndrome somatique persistent aujourd'hui comme symptômes dans la dépression endogène. Les événements de vie stressants sont fréquemment retrouvés dans des tableaux dépressifs variés. La dysthymie, entité diagnostique valable, est une forme de ce que l'on appelait autrefois dépression névrotique. L'article analyse également d'autres types de dépression.
Historical background
Prior to the late 19th century, although detailed systems of classification abounded, the main problem for psychiatric nosology was the establishment of the broad major disorders. Melancholia was recognized as early as the time of Hippocrates, and continued through Galenic medicine and medieval times. The earlier connotation of the term was very wide, and included all forms of quiet insanity. It was linked with the humoral theory of causation, specifically, as the term indicates, with black bile.
Most psychiatric terms have changed meaning over their history, and they are always partly dependent on language. Melancholia later became more clearly associated with the more modern idea of melancholy or despair, for instance, in the classic work of the English Renaissance author, Richard Burton, The Anatomy of Melancholy, 1 first published in 1621. The alternation of melancholia and mania in what is now termed bipolar disorder or manic-depressive disorder, although in some respects suggested in the writings of Arateus of Cappadocia, and those of later authors, was not clearly described until 1854, independently by the French psychiatrists, Falret and Baillarger.The term depression also began to appear in the 19th century, to indicate a state of sadness. Detailed accounts of these aspects and later history can be found in Jackson' and Berrios. 3
When Kraepelin, in the late nineteenth century, built on the work of his predecessors and simplified it to delineate the foundations of the modem classification of psychiatric disorders, one of his major categories was that of manicdepressive insanity. Kraepelin's classic textbook went through successive editions, which included some changes in his views. Initially he distinguished a further category, involutional melancholia, but in later editions' he returned it to the manic-depressive category. The latter not only included cases of alternating mania and melancholia, but all cases of mania, and seemed to include all depressions. Kraepelin regarded psychiatric disorders as disease entities based on a medical, neurological model, with specific, organic etiology and pathology. He believed that manicdepressive insanity was largely independent of psychological stress. While such stress might precede the onset of some attacks, it could not be the true cause, but merely something akin to a trigger mechanism. He did, however, regard some pathological depressions as psychogenic in origin. While he did not completely clarify his views on their position in his classification, or how they were to be distinguished from manic-depressive illness with incidental stress, he appeared to regard them as a separate, but relatively small and unimportant, group.
At the same time as Kraepelin and others were establishing a generally accepted classification of the major psychiatric disorders in terms of disease entities based on a medical model and organic etiology, another growing school of European psychiatrists were developing a very different approach. These were the psychoanalysts. Freud and Abraham, in a perceptive group of studies, developed a theory of the origin of depression in relation to actual or symbolic losses of a love object. Here was a theory regarding the origin of most, if not all, depressions as psychogenic.
The case material of Kraepelin, and others like him, consisted of severely ill patients in institutions. The first depressed patients studied psychoanalytically were also severely ill. Subsequently, increasing attention began to be paid to milder forms of disorders, at first particularly by the psychoanalysts. Psychological theories of causation became more widely accepted for these disorders. A challenge now arose as to how to reconcile these theories with older ones of organic causation. Adolf .Meyer, a Swiss psychiatrist who became the highly influential head of the Henry Phipps Psychiatric Clinic at Johns Hopkins University, moved away from the idea of clearcut disease entities, and viewed all psychiatric disorders as reaction types, or psychobiological reactions of the organism to stress. 5 Both psychological and organic factors had to be taken into account. Others preferred to retain a view which kept separate the two types of psychiatric disorders. On one hand were the psychoses, severe illnesses requiring admission to an asylum, and presumed to have organic causes. On the other hand were the neuroses, milder and not requiring admission to an institution, regarded as more related to psychological stress, and amenable to psychological treatment. Hie stage was now set for two competing theories as to the classification of depression, which were to figure strongly in debates about subtypes in later years, and will be reviewed in due course.
The modern concept of depression
The modern concept of depression, as viewed by most psychiatrists and enshrined in the two official classifications, The ICD-10 Classification of Menial and Behavioral Disorders. Clinical descriptions and diagnostic guidelines (ICD 10) 6 and Diagnostic and Statistical Manual of Mental Disorders. 4th ed. (DSM-IV), 7 is essentially one of a clinical syndrome, defined by presence of a number of clinical features, but not requiring a specific etiology, and acknowledging the possibility of both psychological and biological causative factors in a somewhat Meyerian way. DSM-IV does exclude states where the symptoms are “better accounted for by bereavement,” an imprecise criterion, which is expanded by specifications of not persisting for longer than 2 months, or characterized by marked functional impairment, morbid preoccupation with worthless ness, suicidal ideation, psychotic symptoms, or psychomotor retardation. The value of this exclusion has been debated. 8 Evidence from symptom studies indicates considerable similarities to nonbereavement depression. Further studies arc still needed, particularly some which focus on the 2-month period which is crucial in the DSM-IV définition, and include investigations which ask if the picture of bereavement depressions in this period is different from other depressions, and whether they subside or continue outside this time.
This definition of depression is essentially syndromal and medical, resembling that of a syndrome in other fields of medicine. This implies a cluster of symptoms and signs which tend to occur together, which are assumed to reflect a common pathophysiology, that may not yet be understood, but may have diverse etiologies in different cases. Examples from internal medicine include the malabsorption syndrome, and congestive cardiac failure.
This is an aspect of the medical theory of diseases. In the medical concept each disease is regarded as having a specific, well defined etiology, pathology, clinical picture, and often a specific treatment. The advantages of being able to assign individuals to the correct disease have been great. Essentially, as pointed out many years ago by a philosopher, C. G. Hempcl, 9 they involve generalization of information. Once a patient is correctly diagnosed, much additional information is available regarding such aspects as underlying mechanisms, causation, prediction of outcome, and best treatment.
A syndrome at the level indicated above does not correspond fully to a disease, since multiple causes, and therefore separate diseases, may underlie it. In psychiatry, matters are more complex and often not clearcut. Different syndromes may overlap and co-occur. Defining pure diseases by etiology has generally not succeeded, since causes often appear to be multiple, even in the single case, and not all etiological factors arc known. Nevertheless, many of the above advantages do apply to syndromal diagnoses, including assignment of appropriate treatment and prediction of outcome. It is possible that, as genes involved in psychiatric disorders become elucidated, endophenotypes reflected in underlying disturbances, and genetically defined disorders, may come to correspond more closely to true diseases.
The classical method of identifying a disorder, for most of the history of psychiatry, was for the influential psychiatrist to discern and describe disorders based on his or her clinical experience, with little attempt at precise definition or method-based research. The main method of forming diagnoses in modern psychiatric nosology has been by committee agreement, based sometimes on quite limited empirical, research. Diagnostic criteria are then defined by listing certain symptoms, to define the number necessary for the diagnosis, with duration of time, other requirements, and exclusions. In DSM-IV, eight symptoms are listed as qualifying for major depression, with a requirement that at least five be present, including at least one of two core symptoms, together with duration of 2 weeks or more, presence of clinically significant distress or impairment of function, with absence respectively of mixed episode, direct effects of a drug of abuse, a medication or other substance, or of a general medical condition, or of bereavement, and for depressive disorder, of bipolar disorder or certain other psychotic diagnoses. For dysthymia, fewer symptoms are required, but for a longer period of 2 years, and from a shorter list of eligible symptoms.
For ICD-10 depressive episode, the definitions in the clinical criteria are not tightly specified, but they are well specified in the separate Research Criteria, where they tend to be more restrictive than in the clinical criteria. The Research Criteria are less used, and the existence of two different sets of criteria in the classification causes some obvious problems. Eligible symptoms for depressive episode are the same as in DSM-IV, with the addition of one further symptom, loss of confidence or selfesteem, with the number of symptoms required to be present depending on the severity of the episode, and a third symptom, fatigue, placed as eligible with the two other core symptoms, rather than in the additional list. There is an identical minimum length, of 2 weeks, and somewhat similar excluding criteria, but without specifying bereavement. The list of eligible symptoms for dysthymia is longer, with three required.
The core symptoms
The core symptoms of depression, of which at least one is required in DSM-IV, are depressed mood, and loss of interest or pleasure. The further eligible symptom in ICD-10 is decreased energy or fatigability, but, since two core symptoms must be present, in effect depressed mood or loss of interest/pleasure are required in this schema also. The reason for the addition of decreased energy to the core is not clear.
These core symptoms reflect the view that depressive disorder is essentially a disorder of mood or affect. Although textbooks have suggested variously that the word “affect” should refer to short-term states or states which are observable, and “mood” for sustained ones or internal ones, there has been much confusion regarding these two terms. 10 In practice they have long been used as more or less synonymous. The term “depression” came into use in the 19th century, originally as “mental depression,” to describe lowering of spirits, and came to replace melancholia as a diagnosis. The English-language word really uses an analogy, and its earlier, and also still valid, meaning relates to being pressed down, or an area of something which is pressed down. It can now also refer to other quite different phenomena of lowering, one economic and one barometric, as used in meteorology.
The modern word for loss of interest and pleasure, anhe donia, came into official English-speaking psychiatry with DSM-III. 3 The absence of pleasure, and occurrence of feelings of emptiness and flatness rather than overt sadness, have often been described as occurring in some depressions, particularly the more severe ones.
The assignment of mood lowering to ccntrality in the disorder is to some extent a Western concept, and a more recent one. Other aspects of the disorder such as behavioral change were seen as more important earlier. In other cultures, physical and other disturbances may be seen as more important, and may be reflected in the terms used to describe what appears to be the same disorder.
A more neurobiological view would regard all these phenomena as peripheral and subjective, and would regard the key disturbance as a neurobiological one, not yet adequately elucidated, which drives the other phenomena.
Additional symptoms
The additional symptoms which contribute towards a diagnosis of depression in the two official schemes are: appetite or weight loss or gain; insomnia or hypersomnia; agitation or retardation; loss of energy or fatigue (DSM-IV); loss of confidence or self-esteem (ICD-10); worthlessness or guilt; reduced concentration or indecisiveness; thoughts of suicide or suicide attempt. The wording and definitions are not always identical in the two schemes. Some of these symptoms are not specific, as they can be caused by other physical or mental disorders. .For some, such as pathological guilt, this is not the case, and the placing in the subsidiary list does seem to reflect more the view that the mood disturbance is central.
The diagnostic concept as reflected in the use of criteria which in essence count the number of symptoms present has not usually been formulated explicitly. What there appears to be is an assumption that as the disease becomes more severe it also becomes more pervasive, sucking in more of the accompanying symptoms and disturbances. There are not many empirical studies which have looked directly at the validity of this assumption. Studies using latent trait analyses have tended to produce a dimension corresponding to a list of core symptoms. 11 , 12 Clinically, as depression becomes more severe, it does also tend to involve the presence of more symptoms.
There have been some studies which have examined the frequency of symptoms present in diagnosed depressions. A classic study was that of Aaron Beck. 13 In an early phase of the work that led ultimately to the genesis of cognitive therapy, and more immediately to his wellknown Beck Depression Inventory, he and his colleagues tabulated the frequency of symptoms in a large sample of psychiatric patients. Dividing depressive symptoms into emotional, cognitive, motivational, physical and vegetative, and delusions, they showed that all increased with severity of depression present, and all except delusions were common with severe depression.
Classification
Depressive disorders have long been recognized as heterogeneous. Their subclassification has generated as much research, and as much heat, as any controversy in psychiatry.
The two official schemes are parallel, but not identical, and neither is entirely satisfactory. 14 DSM-IV is simpler. Its major categories are depressive disorders and bipolar disorders. Both have subcategories. Within depressive disorders (unipolar depression), the main concern of this paper, the major subcategories are major depressive disorder (itself divided into single episode and recurrent disorder), dysthymic disorder, and the catch-all required to make any official scheme comprehensive for all users, depressive disorder not otherwise specified. The most recent episode can be additionally specified by a set of severity/psychotic/remission specifiers; as chronic; with catatonic features; with melancholic features; with atypical features; with postpartum onset. There is also a further major category for other mood disorders, which include mood disorders due to general medical conditions and substance-induced mood disorder.
In ICD-10 the major categories are manic episode; bipolar affective disorder; depressive episode; recurrent depressive disorder; persistent mood (affective) disorders (dysthymia, cyclothymia); other mood (affective) disorders; unspecified mood (affective) disorder. The two major axes are really bipolar-unipolar, and course (single episode, recurrent, persistent). Within any depressive episode, single or recurrent, there are subcategories by severity (mild, moderate, severe without psychotic symptoms, with psychotic symptoms, in remission for recurrent disorders) and an additional specifier is available for somatic syndrome (melancholia).
DSM-III and ICD-10 represented quite major advances on their predecessors, DSM-II (rooted much more in psychoanalytic and Meyerian concepts of reaction types) and ICD-9, by their use of structured criteria and their use of modern concepts. Structured criteria were used particularly in DSM-III and successors. ICD-10 is ambiguous in this respect, with its two sets of criteria, the Research Criteria which are well defined, the clinical criteria which are not. Both classifications do also have disadvantages. 14 They are complex, in their fine categories. They are not identical, and, national susceptibilities aside, would be much better fused to a single classification, employing the advantages of each, without the disadvantages, sometimes different, that each has. The strong separation into single episode and recurrent is not justified by empirical research, and it is not useful as a major division: all disorders which become recurrent are single episode on the first occasion. The DSM definitions are better. The specification in DSM-III of depressions related to medical disorder and to substance use is not helpful, since there is little to show they differ from the rest of depressions in any major ways.
Bipolar and unipolar disorder
Much of the discussion about the nosology of affective disorder concerns various subtypes. Depression was for many years a fertile ground for classifiers. 15 , 16 Although much of the heat and pressure have subsided, the issues still complicate diagnostic schemes.
The best-accepted and best-substantiated distinction is the bipolar-unipolar one. This was not always so. As described above, Kraepelin viewed all affective disorders as manic-depressive. As late as ICD -9, published in 1978, the ICD did not clearly make the separation, although hidden within the subcategories of manic-depressive disorder (296) for readers of very small print, was a distinction between 296.1, manic-depressive, depressed, which was meant to be unipolar, and 296.3, manic-depressive, circular, depressed, which was meant to be bipolar. Most users of the classification did not realize this, so the distinction was in practice ver}' erratically recorded. The unipolar-bipolar distinction was incorporated into DSMIII when it was issued in 1980, and later into the ICD when ICD-10 was issued.
It was pathfinding work in the 1960s by Angst 17 and Penis 18 that established the value of the distinction. They had been influenced by descriptions by Karl Leonhard, a 20th-century German psychiatrist with a very 19th-century approach to nosology based on his mental hospital clinical experience, of monopolar and bipolar cycloid psychoses. 19
The bipolar-unipolar distinction is clcarcut by definition, depending on the occurrence of a manic episode. Usually it is also so in practice, although late first manic episodes lead to embarrassing changes of diagnosis, and it is hard to be sure of the nature of minor mood elevations, in some cases which are regarded as bipolar II disorder or cyclothymic disorder, or in some subjects with milder mood changes in community epidemiology studies. The status of single-episode mania is debated, but is accepted by most as indicating true bipolar disorder. Some would regard recurrent depression as related to bipolar disorder, but there is not good evidence that this is the case. TTttcrc are good validating features for the distinction. 20 , 21 Bipolar disorder is more familial, and there is much more evidence of bipolar disorder in first-degree relatives of bipolars than in relatives of unipolars, although about half the cases of affective disorder in the relatives of bipolars are nevertheless unipolar. There is also better evidence from twin studies that the familial elevation is genetic. Molecular genetic evidence of different genes could confirm the distinction, but this evidence is not yet clearcut. There is a different sex ratio in bipolar disorder, equal or nearly so, possibly a more equal social class distribution, and some association with milder cyclothymic disorder, although the full status of more recent work on cyclothymia still requires confirmation by validating studies. Treatment response differs, with a better response to maintenance lithium and possibly to anticonvulsants, although in unipolars the evidence is not yet adequate. More manic episodes occur on antidepressants. Bipolar disorder has an earlier onset than severe unipolar disorder, and tends to be more recurrent. Onsets in women are not uncommonly postpartum, particularly in the case of mania.
The present review mainly concerns unipolar depression. There have been a number of recent reports comparing bipolar and unipolar depressions. 22 - 24 In addition to the history features indicated above, bipolar depressions have variously been reported to show more of the following symptom features compared with unipolar: more retardation, hypersomnia, anxiety, mood lability, psychotic features (especially when the age is under 35); less evidence of sad mood, and various somatic complaints. However, often the pictures are indistinguishable.
Psychotic depression and melancholia/somatic syndrome
The greatest controversy of a previous era concerned a dualistic theory of depression, with a dichotomy between what was variously termed psychotic or endogenous depression on the one hand, and neurotic or reactive depression on the other. Starting in the later 1920s, and throughout the 1930s, fierce debates took place, particularly in British psychiatry, between those advancing a dualistic view and those taking a unitary stance, viewing all depressions as part of a single disorder, without any clear separation into subtypes. 15 The debate subsided with the greater preoccupations of World War II, and reappeared in the form of empirical studies using multivariate statistics in the 1960s. 16
Terminology was confused. The term “psychotic” refers to a severe disorder with delusions and hallucinations, “neurotic” to a milder disorder without these, and often with the connotation of a vulnerable personality. “Endogenous” and “reactive” refer in this context to absence or presence of life stress. The reason for the partial fusion is that, in the fully evolved concept, there were viewed as three aspects: (i) absence of life stress; (ii) presence of a clinical picture characterized by greater severity, sometimes delusions or hallucinations, diurnal variation with morning worsening, delayed insomnia with early-morning wakening, greater somatic disturbances such as loss of appetite and weight, psychomotor retardation or agitation; this was the so-called endogenous clinical picture, or what in the 1970s was termed endogenomorphic depression 25 ; (iii) a personality, associated with reactive or neurotic depression, which was stress-vulnerable or maladaptive.
Over time, the concept of psychotic depression has become separated from that of endogenous depression. Psychotic depression has retained a secure place in the official schemes, as a variant of severe depression. It is clearly definable, by presence of delusions (particularly if mood-congruent) or hallucinations and there is validating evidence, for instance in the better response of such depressions to electroconvulsive therapy (ECT) or antipsychotic drugs, than to antidepressants alone.
Endogenous depression and its opposite arc more problematic, both regarding classificatory status and terminology. There is evidence in support. The factor-analytic and cluster- analytic studies of the 1960s and 1970s in most cases found a dimension or group. 26 On detailed examination, this sometimes looks more like the psychotic element and sometimes the melancholic. However, neurotic depression did not emerge as clearly as a single group in these studies, and is heterogeneous. 26 Dexamethasone nonsuppression occurs predominantly in the endogenous group, and to some extent, so do other neuroendocrine abnormalities, such as blunting of growth hormone response to clonidinc and prolactin response to tryptophan. Regarding treatment, the best ECT response is associated with the presence of psychomotor retardation and depressive delusions, characteristic of psychotic depression. 27 The endogenous picture may be useful as a characteristic of depressions that respond better to antidepressants than placebo, but this is not clear. However, boundaries are weak, with mixed cases common, and distributions on factors do not show consistent and convincing bimodality which would indicate separation of disorders. The relationship to severity, the loose and confusing definitions, and the overlap between psychotic depression and melancholia bedevil the area.
Terminology has remained unsatisfactory. The term neurotic has dropped out of use, particularly in American psychiatry, where it was abandoned because of its diversity of meaning, 28 partly because of previous associations with psychoanalysis, and partly to avoid the emphasis placed earlier in the US on personality and charactero logical aspects. Dysthymia, a chronic disorder that would earlier have been regarded as one form of neurotic depression, is now viewed as a mood disorder. In a somewhat parallel way, the term cyclothymic personality has been replaced by cyclothymic disorder, a form of bipolar mood disorder. The term endogenous was abandoned in official schemes because it is really a symptom syndrome that we refer to these days. The term melancholia, used in DSM-III and its successors, is only nonloaded once its original meaning of black bile is forgotten. It seems preferable to the term somatic depression used in ICD-10, because it is easier to use in English, where it easily forms the adjective melancholic. The concept of somatic depression can also refer to something quite different, associated with somatic disease, or with somatization. Whether this classification will survive forthcoming revisions of the official schemes in the next few years remains to be seen, but it still figures extensively in research and the literature. A spirited case has recently been made for its retention. 29
The place of life stress in this distinction has changed considerably. In older views of endogenous and non endogenous depression, life stress had a central role. However, the distinction is now made on the basis of symptom pattern rather than causal factors. Studies 30 have shown that there is little relationship between measures of preceding life events and the presence of melancholic symptoms. Most depressions are preceded by some life stress, often not sufficient to fully account for the episode so that other factors are also involved. In three of our own studies, in two of which the symptom data and the life event data were collected by different interviewers, we found little relationship between symptom type and previous life events. 30 Other studies of patients with and without the symptom pattern have found little difference between the groups regarding the occurrence of stressful life events prior to onset. However, there may be some differences once depressions have become severe and recurrent. In a sample of depressed females, when a melancholic/psychotic score based on the presence and severity of biological and psychotic symptoms was used, then severe life events were significantly less frequent in the melancholic/psychotic group. 31 This significant difference emerged only when episodes other than the first were included. In another study, 32 in which the sample comprised highly recurrent dépressives, fewer life events were found in endogenous than nonendogenous Research Diagnostic Criteria subtypes, which depend on symptom features.
Severity and minor depression
The severity issue deserves further consideration. It is elevated to an important consideration in ICD-10. As an episode qualifier it is useful, since severity does carry implications for treatment, and severe depressions also tend to have worse outcome than do mild. It is not well recognized that, in practice, ICD-10 mild depressive episode is by no means minor, at least in the Research Criteria. The definitions for individual symptoms and the absence of some symptoms from the list means that subjects who fit these criteria usually have sufficient depression also to qualify as DSM-IV major depressives.
This raises another issue, the lower boundary to distinguish pathological depression from normal mood change. Although defined by the number of symptoms present, it is not in fact well-defined, since the thresholds for individual symptoms are not clear or easy to be sure about: when does lowering of mood, even if present every day, cross the threshold in severity to count as being present? The issue is not crucial in the clinic, but it has become important as psychiatric research has extended to the community, and to community epidemiology. Comparatively high rates of depression arc found in community prevalence studies. 33 It is not clear whether all these depressions share fully the qualities of depression presenting for medical or psychiatric treatment. Similar issues arise in the use of “symptomatic volunteers” for research.
There have been a number of studies examining boundaries of DSM major depression. 11 , 12 , 34 - 36 These do support the validity of summing the number of symptoms, although it is doubtful whether there is any true threshold rather than a somewhat arbitrary cutoff on a continuum, and one which as defined may be a little too high. In terms of treatment response, there is good evidence of a threshold, a little below major depression, at which superiority of tricyclic antidepressants to placebo first appears. 37 The threshold for response to serotonin reuptake inhibitors may be a little lower. 38
Dysthymia and subsyndromal depression
Dysthymia was introduced into official classifications in DSM-III, using a term which had been originated by the 19th-century French psychiatrist, Janet. The concept had previously been introduced for research in the predecessor of DSM-III, The Research Diagnostic Criteria, as Intermittent Depression. 39 Partly the use of the term was to avoid use of the term neurotic depression. It reflected the wider modern trend to view such chronic phenomena as primarily disorders of mood rather than of personality.
In the last 20 years dysthymia has proved a useful concept, delineating a form of mood disorder which can produce many problems and have an adverse impact on the life of the sufferer, and it has generated much research. 40 There is a high rate of comorbidity, particularly of anxiety disorders and substance abuse. The majority of dysthymics ultimately also develop an episode of major depression, and such episodes, so-called double depression, have a worse prognosis than pure major depression, both in respect of remission and of recurrence. There appears therefore to be continuity between dysthymia and major depression. The DSM-IV definition rules out an episode of major depression in the first 2 years, but the ICD-10 definition does not. In practice the differentiation of dysthymia from milder chronic major depression or from the residual symptoms with partial remission which frequently occur after major depression, 41 is difficult and may be artificial. There is evidence that dysthymia responds to antidepressants, 42 but controlled trials do not always distinguish uncomplicated dysthymia from superimposed major depression.
A further, milder chronic disorder which has been delineated, recurrent brief depression, 43 has not received general acceptance. Described as comprising frequent episodes of depressive symptoms sufficiently severe for major depression, but only lasting a few days, it does not appear to be very common in patients presenting for treatment, and has not been found to respond to antidepressants in the few studies which have been undertaken. There is also another DSM-IV diagnosis, minor depression, which is included in an appendix of the manual as a provisional category for research. Minor depression was included in the Research Diagnostic Criteria (RDC),but not in DSM-III. Both RDC and the possible criteria in DSM-IV refer to episodes of depression milder than major depression, rather than persistent dysthymia. Minor depressive episodes, excluding dysthymia, have been found to be more prevalent than major depression in an epidemiological study. 44
In recent years, there has been a growing literature regarding so-called subthreshold or subsyndromal depressions, which are common in the community and can cause considerable disability. 45 It is not always clear whether this is episodic or chronic, or residual after major depression and what its overlap is with dysthymia or other milder syndromes.
There may be a case for inclusion of one or more diagnoses equivalent to minor or subsyndromal depression in the official schemes in the future. This would be useful in primary care, and in postpartum depression, where much of the literature refers to mild depressions which are important because of their potential impact on the baby. On the other hand, minor depression as defined in the RDC occurred less commonly than might have been expected, perhaps because by the time the criteria were reached, most depressions also fitted another RDC subcategory which was not included in DSM-IV, probable (but not definite) major depression. More research in this area would be timely
Single depressive episode versus recurrent depression
The strong ICD-10 distinction between single depressive episode and recurrent depression is not useful. Its appearance in ICD-10 was rather unexpected, as it has not been used much in the past in affective disorder. Unfortunate]}', in the light of what we have learned in the last 15 years about the risk of recurrence of depression, the distinction is not helpful. If high proportions of people with their first depressive episodes have further episodes and are redefined later as recurrent, the distinction becomes of little value. There is not much to distinguish first depressive episodes from recurrences in other respects, except where the depression has become quite recurrent, when the role of life stress becomes less, response to treatment poorer, and risk of recurrence higher.
A step change has indeed occurred in conceptualization of depression in the last 30 years. In the 1960s and earlier 1970s, the disorder was seen as an episodic one, with complete remission and often without recurrence. Since then follow-up studies of hospitalized dépressives have shown that at least 60% will be readmitted over 16 years, and rates for recurrence of episodes any severity, not necessarily needing hospital admission, may be up to 90%. 46 We do not yet know if this is true for milder depressions outside hospital, and probably there are many single episodes at community level, linked to stress, which do not recur, but severe depression is undoubtedly a recurrent disorder. Moreover, since remission may be incomplete and partial, and mild and subsyndromal disorder are common in the community and may ultimately be followed by major episodes, it is now common to view depression as often a chronic disorder encompassing, and varying through, a spectrum or continuum.
Other subtypes
There are also some other subtypes. ICD-10 does not have them, nor do previous DSM versions. This is understandable in view of the need not to clutter official classifications with the evanescent. The problem is that clinicians do commonly recognize and use some of them, but have nowhere to record them. DSM-IV does include some which are not coded and seem to be viewed somewhat tentatively.
There are four subtypes among the specifiers in DSM-IV, in addition to those already considered and others related to course. The first is postpartum depression. This is potentially important; although the issue goes wider than mood disorder. 14 At present, researchers and others interested in postpartum disorders have a major problem: there is no official way of recording the disorder. Frequencies of treated disorder are unobtainable. Retrospective identification of subjects for follow-up and other studies is not possible from coded diagnostic records. ICD-10 has a category of mental disorders associated with the pucrperium (F53),but it can only be used if the criteria for disorders coded elsewhere are not met. There is also a qualifier, in the research criteria only, to indicate disorder associated with the puerperium, but as it is not in the clinical guidelines, few people know about it. DSM-IV does have a noncoded specifier for postpartum onset which can be applied to major depression, mania, mixed episode, or brief psychotic disorder, but it is limited to these disorders and the onset requirement, which is within 4 weeks of deliver}', is too short. Case register and other studies indicate a peak of onsets which goes on longer, up to 3 months. 47 What is needed is a specifier which can apply to any disorder, is coded, and applies to the onset in the first 3 postpartum months. Inclusion of this should be a high priority for the future. The second specifier is for seasonal depression. There is now a vast literature on seasonal affective disorder and its treatment. 48 It is time that it was included in official classifications.
A third specifier in DSM-IV is for atypical depression, defined in terms of increased sleep, increased appetite, and other symptoms. Here, the case for inclusion is less clearcut, and there are arguments in either direction. The concept originally came from William Sargent and colleagues at St Thomas' Hospital, London. The meaning of the term has fluctuated. The originators probably had in mind nonendogenous depression and later, depression with anxiety or anxiety disorder alone, rather than the more recent meaning of the term, which focuses on vegetative symptoms reversed from their usual directions in endogenous depression. 49 The concept has always been associated with response to monoamine oxidase inhibitors (MAOIs), but the evidence that atypical depression in its current meaning is associated with good MAOI response is mainly limited to one very influential US research group. Other evidence would point to anxious or phobic patients, but in general, selectivity appears to be weak, and there is evidence that MAOIs, in a high enough dose, are effective in quite a range of depressives. 50 In practice, it appears that clinicians, at least in Europe, do not use the term as much today as they did in the 1960s and 1970s, and its importance may be diminishing. So, too, is research in relation to it.
The fourth DSM-IV specifier is for the presence of catatonic features. This is idiosyncratic, and does not correspond to much in the earlier literature. Its meaning is not very clear, but much of the description seems to be that of psychomotor retardation. Retarded depression does have a considerable lineage, but has not proved a very useful classification and is not very stable between episodes. This subtype could be dropped without loss.
DSM-IV has some other provisional classifications in its appendix. Recurrent brief depression appeared and generated much excitement, but has not proven very useful and now receives less attention, so the case has not been made for its continuing inclusion. Mixed anxiety -depression is common, but can easily be handled by modern ideas of comorbidity and two diagnoses. Premenstrual dysphoric disorder is not purely depressive, and is beyond the scope of this review.
Transcultural aspects
The modern concept of depression, with emphasis on psychological feelings, is particularly Western, and to some extent a 20th-century development. Earlier Western concepts were less psychological. Some other cultures and languages place emphasis on other aspects. 51 It was thought at one time that mood disorders were less common in other cultures, for instance African, than in Western. In general this does not now appear to be the case, but to have been an artefact of previous Western psychiatrists failing to recognize the disorder in other cultural and linguistic groups. Mood disorders do appear to be universal, once they are sought by local psychiatrists who understand the culture, language, and metaphors used to express mood. Rates may differ to a lesser extent, but this is not clear, since it faces formidable problems in establishing equivalence of translated interview instruments and questionnaires.
Presentations may differ. In Zimbabwe, the language lacks a term directly equivalent to depression, and presentations are typically with somatic symptoms. 52 In Chinese subjects, presentations may also be more somatic, but there is evidence that with Western acculturation, this changes. 53 In Hong Kong, 54 lower rates of depression and higher rates of anxiety have been reported than in similar epidemiological studies from the US and other Western countries, suggesting some redirection of symptoms.
It is also possible that other syndromes limited to one or more cultures may be equivalents of depression. Equivalence to depression is difficult to prove in nonde pressed subjects. It would, however, be inappropriate to imply that these are any less valid than disorders seen in Western cultures. There may also be additional nonWestern subtypes which justify inclusion in international diagnostic schemes.
The concepts involved in depression are complex. They have evolved over the years, and often, as is common in psychiatry, the meanings have changed subtly in the process. The core elements, and workable definitions for the disorder and its boundaries, are now well established. Some aspects of classification remain problematic, but the separation of bipolar and unipolar disorder was a major advance. Depressions are the most common disorders in psychiatry, both for psychiatrists and for general practitioners, so that understanding of their elements is important.
The Biology of Depression
Reviewed by Psychology Today Staff
Depression makes deep inroads on biology to bring about the many symptoms of depression, from sleep disruption and an inability to experience pleasure to lack of motivation and feelings of guilt. Many factors influence how a person reacts to stressful events, whether an individual gets depressed, and how the disorder manifests. These include genetic inheritance, life experience, temperament, personality traits, social supports, and beliefs.
Still, exactly how biological changes give rise to depressive symptoms is not well understood. Because of its complexity—and because the disorder contributes so much to human suffering—the biology of depression is a major subject of ongoing research.
On This Page
- What is the role of genetics in depression?
- Can genes for depression be modified?
- What happens in the brain with depression?
- How does lack of sleep alter brain function?
- How does the brain regulate mood?
- What role does serotonin play in depression?
- Does dopamine play a role in depression?
- How does nerve cell communication go awry in depression?
- How does stress affect the brain
- How does childhood stress affect adult brain function?
- What areas of the brain play a role in depression?
- What does brain imaging look at in depression?
- How does depresson itself change the brain?
- Can talk therapy change the way the brain functions?
- Why is nerve cell growth, or neuroplasticity, important?
- What are ways of stimulating neuroplasticity?

The inheritance of risk for depression is considered, at best, polygenetic—that is, a number of unknown genes each contributes a tiny risk under certain environmental conditions. None of them makes depression inevitable. The baseline risk of depression in the population is 10 percent; having a first-degree relative (parent or sibling) with depression doubles or triples an individual’s risk, to 20 to 30 percent over the course of a lifetime.
There are many non-genetic factors that contribute to risk of onset of major depression, and there are some inherited factors as well. To make matters a bit more complex, some non-genetic factors, including certain kinds of adverse childhood experience—such as repeated child abuse or neglect—can have a lasting impact on the function of genes (such as those that activate the stress system) to increase the risk of depression later on.
Variation of one gene associated with the serotonin system ( the serotonin transporter gene ) has been most linked to depression susceptibility—it is thought to moderate the impact of stressful life events—but the evidence has been disappointing. Life experience and lifestyle factors are believed to play more significant roles in depression risk.
Scientists know that the expression and function of many genes can be altered without doing the near-impossible—making any changes to the gene structure itself. Such changes are known as epigenetic modifications. Some life experiences can create vulnerability to depression through epigenetic changes. For example, in rat pups, lack of maternal care can permanently reset the sensitivity of receptors to stress hormones. If their mothers fail to lick and groom them, they grow up to display an exaggerated response to stress hormones and develop depression-like behavior in response to stress.
But there are also ways to strategically induce epigenetic changes to reverse symptoms of depression. For example, the nutritional supplement SAM-e , a synthetic version of a compound found in the body, contains a substance that chemically augments the activation and deactivation of genes. Some studies show it is effective against symptoms of depression.
Overexcitability of the stress response system, shifts in activity of various neurochemicals in the brain, diminished efficiency of nerve circuitry and nerve generation, disturbances in energy use nerve cells, the intrusion of inflammatory substances in the brain, upsets in the brain’s 24-hour (circadian) clock—all play a role in depression onset or progression and influence the kind and severity of symptoms.
Two major areas of the brain—the hippocampus (seat of memory) and the cortex (the thinking part of the brain)— undergo shrinkage . Both the size of nerve cells and the number of their connections with other neurons are reduced. At the same time, depressive behavior is linked to overactivation of the hypothalamus, which coordinates the stress response, and overactivity of the amygdala, which signals threat and generates negative emotions.
Reduced activity in the prefrontal cortex, which interprets and regulates emotional signals coming from the amygdala, accounts for the difficulties in decision-making and the cognitive fog that depressed people experience.
The human brain may be unique in its ability to generate new nerve connections, called neuroplasticity ; this is what underlies all adaptation and learning. In depression, neuroplasticity is impaired, especially in the hippocampus. In addition, reward centers of the brain shrink and fail to activate in response to stimulation. There are changes in sensitivity to the hormones that regulate feeding behavior, resulting in changes in appetite.
Disruption of the sleep-wake cycle is one of the hallmarks of depression and is a major source the mood disturbance in major depression. Lack of sleep upsets the body’s circadian clock that orchestrates the natural daily rhythm of most biological functions, including patterns of secretion, release, and activity of many neurochemicals in the brain.
Sleep deprivation is thought to impede the transmission of neural signals. One result is that sleep deprivation makes people emotionally reactive , increasing activity in the amygdala and decreasing it in the emotion regulation center of the prefrontal cortex. Sleep deprivation impairs the brain’s ability to control negative thoughts.
Mistimed light input resulting from sleep disturbance also disrupts the dopamine-sensitive nucleus accumbens. Studies show that people with mood disorders benefit from maintaining a strict sleep/wake routine, rising in the morning and going to sleep at night at the same time every day.
Emotions are fleeting responses to stimuli; mood is a more sustained state of emotion. Like emotions, mood probably originates with activity of the amygdala, where emotions are coded. But it also involves the prefrontal cortex, which, through bundles of two-way circuitry with the amygdala, helps regulate emotional response and influences the general state of reactivity of the amygdala.
Under normal conditions, moods are relatively stable. But the persistence of negative mood in major depression suggests something is amiss in the nerve pathways between the amygdala and cortex.
Another important influence on mood is the circadian rhythm that governs the timing of much physiological activity, most prominently the sleep-wake cycle . Disturbances in biological rhythms are known to disrupt mood, and studies of depressed patients find that they exhibit abnormal patterns of many body functions, from temperature regulation to hormone secretion.
The neurotransmitter serotonin is one of many signaling chemicals in the brain associated with depressive symptoms. Under normal conditions, serotonin inhibits pain, influences the processing of various emotions, and mediates many mental capacities important in social life .
But like the other neurotransmitters involved in depression, its production and activity are affected by the hormones the body secretes in response to threat or stress, such as cortisol. One result is a functional lack of serotonin, which, among other things, disrupts the circuitry that regulates moral emotions. Growing evidence suggest that is why those who are depressed are haunted by excessive self-blame and a sense of guilt.
The neurotransmitter dopamine, which mediates motivation and desire, is one of several brain signaling chemicals that are implicated in depression . It is associated with two of the most prominent features of depression—anhedonia, or the inability to experience pleasure, and appetite alterations.
Many neurons that use dopamine to relay signals are sensitive to the effects of stress, which can alter their excitability and activity. Studies have also shown that reward-generating areas of the brain—such as the nucleus accumbens, where dopamine signals originate—may be underactive in depression.
Where once researchers and clinicians focused on the role of neurotransmitters such as serotonin in depression, they now know that neurotransmitters are only one part of a much larger story of how nerve cells function in circuits to relay messages from one part of the brain to another. In fact, many experts see depression as a nerve circuit disorder, marked by a power failure in the brain’s wiring, affecting communication between one area of the brain and another.
The nerve cell connections between the amygdala and the prefrontal cortex (PFC) are sometimes called the “depression circuit;” depression results when emotion-laden signals from the amygdala overpower the ability of the PFC to regulate the signals. The prolonged or excessive release of stress hormones can lead to a failure of activation of key nodes in neural networks or impair the strength of signals between them, especially when processing emotion-related or reward stimuli.
It’s important that depression is now seen as a nerve circuit disorder, because that influences the search for effective treatments.
Stress can be beneficial to the brain, depending on how intense and long-lasting the stressor is. In brief bursts, stress fosters alertness, learning, and adaptation. Severe or prolonged stress, however, can disrupt many aspects of brain function and lead to depression .
Such stress dysregulates the normal stress response through the overproduction of cortisol. Cortisol is especially toxic to cells in the brain’s hippocampus, and one consequence of uncontrolled stress is shrinkage of the hippocampus, manifest in the impaired memory and learning that are characteristic of depression.
Cortisol also turns off the generation of new nerve cells in some areas of the brain, affecting the circuitry of the brain. In addition, prolonged cortisol exposure affects production of the insulating myelin sheath surrounding nerve cells, diminishing the overall efficiency or nerve signaling.
Severe or sustained early life adversity shifts the course of brain development and can lastingly impair emotion regulation and cognitive development. Excessive or prolonged activation of the stress response in childhood, studies show, can sensitize the stress response system so that it overresponds to minimal levels of threat, making people feel easily overwhelmed by life’s normal difficulties.
Severe or prolonged childhood adversity can affect the function of genes important for the wiring of the brain, so that emotional control is difficult—overproducing neural connections in regions such as the amygdala that signal threat and other negative emotions while underendowing neural connectivity in brain areas responsible for behavioral control, reasoning, and planning.
Nevertheless, adult brains retain the capacity for neuroplasticity. Although it takes effort, and often the guidance of psychotherapy, people can learn to overcome many of the ill effects of early adversity.
Many areas of the brain contribute to the symptoms of depression, such as the hippocampus, which is the seat of memory and learning, and the superchiasmatic nucleus, which is the “body clock” that paces all physiologic activity, notably the sleep-wake cycle. But brain imaging studies suggest that there is a primary “depression circuit,” consisting of the amygdala, which flags emotion-related stimuli; the prefrontal cortex, which analyzes and interprets experience, modulates emotional reactivity, and controls attention; and the two-way network of nerve fibers that connect them.
In this model of depression, the amygdala becomes hyperactive, sending out a constant flood of emotions, and the PFC becomes hypoactive, unable to regulate the stream of emotional input. Through feedback loops, the failure of the PFC further dysregulates the amygdala and leaves unchecked its inherent bias toward negative emotions.
Some types of brain imaging, such as CT scans and magnetic resonance imaging (MRI), take static pictures of the brain to determine whether any specific structures are larger or smaller than normal in depressed patients. Positron emission tomography (PET) scans and functional magnetic resonance imaging (fMRI) look at the brain in action, to see whether and where there are problems in the way the brain processes specific types of information .
In fMRI studies, normal controls and depressed patents are typically given some task to perform in the scanner. For example, subjects may be asked to look at a series of pictures, some of them with emotionally disturbing content, to see how the brain handles negative stimuli. The brain scanners measure blood flow or metabolic activity, based on the concentration of agents earlier injected into the bloodstream. Comparison of hot spots and dead spots of activity between controls and depressed patients highlight areas of the brain that malfunction in response to challenging stimuli.
The longer an episode of depression lasts, the greater the likelihood of a recurrence of depression. That is because depression changes the brain in ways that are only now yielding to understanding. If left untreated, depression can become a progressive disease leading to neurodegeneration.
The sustained stress that triggers depression releases a cascade of hormones linked to shrinkage of the hippocampus, a part of the brain essential for learning and storing and retrieving memories. Prominent changes to other brain areas, including the amygdala, create a sustained tendency to generate negatively coded emotions.
Untreated depression also changes the activity of substances that help regulate the mitochondria, the energy factories of all cells, especially critical to function of the brain because it is such a metabolically active organ. Depression also causes changes in the network of brain areas involved in processing physical pain , and the degree of hyperactivity in such areas as seen on brain scans correlates with the severity of depression that patients experience.
Recent studies show that like other neurodegenerative conditions, longstanding depression increases levels of inflammatory substances in the brain that further impair its function , affecting many brain regions and circuits of connectivity.
The most studied form of psychotherapy—cognitive behavioral therapy (CBT)—has been shown to produces long-lasting changes in emotion, cognition, behavior, and somatic symptoms of patients with depression and other mental health conditions. Using functional magnetic resonance imaging (fMRI), researchers find that CBT alters patterns of connections between brain regions, notably in circuits related to the processing of emotions.
Images show decreased reactivity of the brain’s amygdala, which processes emotion, and increased activity in the prefrontal cortex, the thinking and executive control center of the brain, indicating more control over emotional reactions and memories, and greater flexibility in finding solutions to problems . The changes in cognition power help reduce negative emotionality by increasing people’s ability to calmly manage experiences and thoughts that stir emotions.
Throughout life, the growth of new nerve cell connections, or neuroplasticity, is the major way brains adapt to new or challenging circumstances. It’s called learning, and it’s the brain’s major means of problem-solving. Depression is characterized by a loss of plasticity—negative neuroplasticity; patients feel imprisoned in their own repetitive negative thoughts.
It’s long been known that prolonged or excessive outpouring of stress hormones curbs the growth of nerve cells, particularly in the hippocampus, seat of memory and learning.Such changes are reflected in a smaller size hippocampus and impaired memory in depressed patients.
Changes also occur in the prefrontal cortex, undermining regulation of emotional experience, limiting the ability to set goals, and much more. All effective treatments of depression restore the capacity for mental and behavioral change and are known to stimulate the growth of new nerve cells —they enable the brain to rewire itself.
All known therapies for depression stimulate the growth of new nerve cell connections. But the growth of new nerve cell connections is not dependent on antidepressant drugs. Researchers find that there are many ways to bring about neuroplasticity.
One of the most effective ways is aerobic exercise. And it doesn’t have to be intense to have an effect. In fact, all physical activity is linked to the generation of neurotrophic factors, chemicals that stimulate the growth and recovery of brain cells.
Research also pinpoints diet, and especially i ntermittent fasting as a way to generate BDNF , or brain-derived neurotrophic factor, one of the best studied agents of nerve cell growth. Intermittent fasting is known to be neuroprotective, shielding brain cells from the degeneration that often accompanies aging.

A Personal Perspective: I wasn’t broken or stupid because I couldn’t see what was going on. The flight-or-freeze response was my nervous system’s innate wisdom to keep me from harm.

Psychedelics are making headlines around the world. How can the public know when medications are harmful, helpful, or somewhere in between?

How intense is your reaction to a colleague dismissing you or a romantic interest breaking up with you? Many people have some degree of rejection sensitivity.

Anxiety and depression share many common features and often occur together. Recognizing the anxiety-depression cycle can lead to more effective treatment outcomes.

Some cognitive therapists may show some of the same cognitive distortions they’re trying to address in their clients. Does a "do-as-I-say-not-as-I-do" approach work?

Discover the impact of gray divorce on adult children through two sisters' journey from shock and overwhelm to healing and supporting others.

Humor is an underappreciated element in psychotherapy—one that can reduce anxiety, increase perspective, and strengthen the psychotherapeutic relationship.

Wherever you go, you take your trauma with you—including the workplace. Leaders have the opportunity to reduce the impact.

Sleep is essential to mental health and well-being. The relationship between the amount and quality of sleep a person gets and their mental-emotional health is reciprocal.

New studies show the risk of cannabis use disorder is the same for medicinal and recreational cannabis users. How would the brain know the difference?
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
Customer Reviews
Finished Papers
- Member Login
Gombos Zoran

IMAGES
VIDEO
COMMENTS
Essay grade: Good. 2 pages / 978 words. Depression is a disease that afflicts the human psyche in such a way that the afflicted tends to act and react abnormally toward others and themselves. Therefore it comes to no surprise to discover that adolescent depression is strongly linked to teen suicide.
Here are six essay topics about depression that you can use in your essay. 1. What Is Depression? In your essay, discuss the definition of depression, and delve into the signs, symptoms, and possible causes of this mental illness. Depression can be difficult to define and understand. Discuss the definition of depression, and delve into the ...
Depression is a disorder characterized by prolonged periods of sadness and loss of interest in life. The symptoms include irritability, insomnia, anxiety, and trouble concentrating. This disorder can produce physical problems, self-esteem issues, and general stress in a person's life. Difficult life events and trauma are typical causes of ...
Depression is a common and debilitating mental health condition whose underlying aetiology and pathophysiology is still relatively poorly understood. ... In this short essay, we will first turn to the past and briefly review what neuroscientific investigations have taught us so far about depression. ... et al. (2006) Elevated monoamine oxidase ...
Depression is one of the leading causes of disability, and, if left unmanaged, it can increase the risk for suicide. ... and commentaries, were identified. After applying the inclusion and exclusion criteria, 470 papers were included in this review (Supplementary Table S1). We focused on aspects related to biological, psychological, and social ...
Depression can cause a range of psychological and physical symptoms, including: persistent depressed mood. loss of interest or pleasure in hobbies and activities. changes in appetite and body ...
The Present Definition of a Depressive Disorder. Depression can be defined as a disorder that affects a person's mental health, resulting in a dampened emotional state for an extended time. It is an exhausting mental condition that affects people's daily lives by influencing them towards adopting negative patterns of behavior (Lu, Li, Li ...
Depression is more than just sadness; it is the most common mental disorder. People with depression may also experience physical, cognitive, and social changes, including altered eating or sleeping habits, lack of energy or motivation, difficulty concentrating or making decisions, and withdrawal from social activities.
Definition Essay - Defining depression Depression is a mental illness under the psychological sector "Clinical psychology." It has a few facets to it, and has numerous causes. It is also known as a mental state that most people undergo at some point in their lives. However, there are some people that get chronic depression, or forms of ...
Therefore, cognitive approach to depression may link with behavioral explanations as well. Historically, depression has been indicated to occur as a response to a perceived loss or imaginary loss and self-critic of ego according to Freud (1917). Cognitive approach to depression explain the causes of maladaptive cognitions as variety of life ...
Psychodynamic Theory. Cognitive Explanation of Depression. Learned Helplessness. Humanist Approach. Depression is a mood disorder that prevents individuals from leading a normal life at work, socially, or within their family. Seligman (1973) referred to depression as the 'common cold' of psychiatry because of its frequency of diagnosis.
Depression, in psychology, is a mood or emotional state marked by feelings of low self-worth or guilt and a reduced ability to enjoy life. Depression differs from simple grief or mourning and can be classified into different types. Learn more about the causes, symptoms, types, and treatments for depression.
Depression is a mood disorder that causes feelings of sadness that won't go away. Unfortunately, there's a lot of stigma around depression. Depression isn't a weakness or a character flaw. It's not about being in a bad mood, and people who experience depression can't just snap out of it. Depression is a common, serious, and treatable condition.
The essay on Depression is informative but could be improved in several ways. One major issue is the lack of engaging language, which makes the essay feel dry and academic. The essay could benefit from the use of more examples or personal anecdotes to illustrate the points made, which would help to make the topic more relatable and interesting ...
Depression is a disease that dominates you and weakens your body, it influences men as well as women, but women experience depression about two times more often than men. Since this issue is very urgent nowadays, we decided to write this cause and effect essay on depression to attract the public attention one more time to this problem.
The DSM-IV definition rules out an episode of major depression in the first 2 years, but the ICD-10 definition does not. In practice the differentiation of dysthymia from milder chronic major depression or from the residual symptoms with partial remission which frequently occur after major depression, 41 is difficult and may be artificial.
The baseline risk of depression in the population is 10 percent; having a first-degree relative (parent or sibling) with depression doubles or triples an individual's risk, to 20 to 30 percent ...
Abstract. Major depression is a mood disorder characterized by a sense of inadequacy, despondency, decreased activity, pessimism, anhedonia and sadness where these symptoms severely disrupt and ...
Definition Essay On Depression. Depression is the feeling of severe despondency and dejection and a long and severe recession in an economy or market. Depression can be misleading by lots of people have felt depression at times over challenging situations that can set back ones career and or the ending of an important relationships.
Topic: Depression, Mental Illness, Suicide. Pages: 1 (658 words) Views: 669. Grade: 4.8. Download. You've lost connections with friends and family, you can't bring yourself to go outside, it feels like the world is against you. This is the life of having depression, a horrible cycle of low moods, sadness and an overall feeling of dejectedness.
Definition Essay Depression Depression is a common and significant mood disorder. It is defined by the Mayoclinic.org as a mood disorder that causes a persistent feeling of sadness and loss of interest. Depression is a real illness causing symptoms such as feelings of guilt, worthlessness, irritability, weight change, feelings of emptiness and ...
Avail our cheap essay writer service in just 4 simple steps. To get a writer for me, you just must scroll through these 4 stages: Order preparation While our expert is working on your order, you will be able to communicate with them and have full control over the process. 652. Finished Papers. 12 Customer reviews.