Special Issue: COVID-19
This essay was published as part of a Special Issue on Misinformation and COVID-19, guest-edited by Dr. Meghan McGinty (Director of Emergency Management, NYC Health + Hospitals) and Nat Gyenes (Director, Meedan Digital Health Lab).

Promoting health literacy during the COVID-19 pandemic: A call to action for healthcare professionals
Article metrics.
CrossRef Citations
Altmetric Score
PDF Downloads
The extraordinary spread of misinformation during the COVID-19 pandemic is impressive. And, to public health professionals like us, it’s worrying: We know that good information and good health go hand in hand. Knowing what we do about the practice of public health and what the science tells us about how people fall for misinformation, we see promising strategies for intervention in our own field. We therefore call on fellow healthcare professionals to take concerted action against misinformation, and we suggest here one lever our field is perfectly situated to address: health literacy. In this commentary, we propose concrete strategies for colleagues at four levels of practice: in healthcare organizations, community-based partnerships, cross-sector collaborations, and as individual healthcare providers.
Bloomberg School of Public Health, Johns Hopkins University, USA

Introduction
Health literacy is crucial for health, and healthcare professionals must acknowledge and prioritize its importance in every interaction with patients and communities (Berkman et al., 2011; Paasche-Orlow & Wolf, 2007). But we can’t stop there. Given its impact on health itself, health literacy merits a privileged position in our entire scope of operations, from program planning to evaluation to patient safety to communications. A strong body of evidence testifies to the benefits of integrating individual healthcare practice with public health strategy, and the current pandemic is the perfect moment for professionals from these two sectors to join forces in a shared battle against misinformation (Linde-Feucht & Couluris, 2012; Committee on Integrating Primary and Public Health, Board on Population Health and Public Health Practice & Institute of Medicine, 2012). In the midst of what the WHO has called a “misinfodemic,” the stakes of health literacy – or illiteracy – are high, and we consider it our duty, as healthcare professionals, to do everything we can to help people access and act on the sort of health-related information that effectively promotes the achievement of good health. A strengthened commitment to health literacy throughout the entire family of healthcare professionals, within and across organizations and down to each individual provider, offers us great promise for addressing this urgent problem. Here we show why and how.
Before officially declaring COVID-19 a pandemic, the World Health Organization described the massive info demic surrounding it, pointing to a global overabundance of information that had already made it difficult for the public to distinguish trustworthy health sources from phony experts and created widespread confusion about real evidence-based safety measures (Zarocostas, 2020). Indeed, a recent Pew survey of American adults found that close to half (48%) of the respondents reported seeing at least some made-up news about COVID-19 (Mitchell & Oliphant, 2020).
Research suggests that several key factors drive individual and collective belief in health-related misinformation (Scheufele & Krause, 2019; Uscinski et al., 2016). One of the most important is low health literacy – and the extraordinarily scope and scale of the current COVID-19 “misinfodemic” represents an acute challenge to healthcare professionals in just this regard (Gyenes & Marrelli, 2019; Mian & Khan, 2020). History has shown us the tragic consequences that the spread of misinformation can carry during health crises. (For example, the South African government’s outright denial of the efficacy of antiretroviral therapies and its mass promotion of herbal remedies to combat HIV/AIDS under President Thabo led to the loss of over 300,000 lives as a result of excess HIV transmission, particularly among pregnant mothers)(Nlooto & Naidoo, 2016; Bateman, 2007). The Affordable Care Act (2010) defines health literacy as “the degree to which an individual has the capacity to obtain, communicate, process, and understand health information and services to make appropriate health decisions.” In short, it is the sort of competence that enables people to recognize the severity of a given situation, acquire a basic grasp of how to protect themselves and others, and understand the scope of their choices. In the context of COVID-19, it is what makes people able to differentiate between proposals to take social distancing measures and ones to drink bleach.
While limited health literacy affects people of all ages, incomes, and education levels, some are more vulnerable than others. According to the Centers for Disease Control and Prevention (CDC), racial and ethnic minorities, non-native speakers of English, those with low socioeconomic status, and medically underserved people (e.g., the uninsured and Medicaid-insured) are disproportionately susceptible. Hispanic adults have the lowest average health literacy scores of all racial and ethnic groups, followed by African Americans and American Indian/Alaska Natives; one study found that 74% of Spanish-speaking patients, for example, demonstrated ”below basic” health literacy (the lowest level possible), while only 7% of English-speaking patients did. And disadvantages such as these matter because there are serious consequences: People with low health literacy are twice as likely as others to report poor health status (Cutilli & Bennett, 2009).
Recent scientific work has affirmed that misinformation (generally) and limited health literacy (specifically) are major obstacles to health, and have helped to explain and respond to the problem (The National Academies of Sciences, Engineering, and Medicine, 2016; The National Academies of Sciences, Engineering, and Medicine, 2017). In 2017, the National Academies of Sciences (NAS) convened a Committee on the Science of Science Communication to highlight the challenges inherent in effectively conveying scientific information to the public. Additional thought leaders in the field have built on the committee’s work by recognizing misinformation as a product of individual information processing as well as of macro-level causes that include the pervasiveness of social networks and the tenure of highly varied information ecologies (Scheufele & Krause, 2019). Previous studies have noted a lack of understanding of science, the inability to recognize misinformation, the holding of beliefs inconsistent with the best available science, and credence in conspiracy theories as a few of the individual factors associated with the acceptance of inaccurate information (Uscinski et al., 2016; Garrett & Weeks, 2017; Southwell & Thorson, 2015). Other research has suggested that emotional states can influence individuals’ ideologies and alter their propensity to assimilate falsehoods from the information environment (Kalichman et al., 2012; Flynn, Nyhan & Reifler, 2017).
Group -level dynamics have also been found to influence individuals’ uptake of misinformation. For example, insular social networks can shape people’s attitudes and beliefs, allowing for the normalization of falsehoods and making it difficult to counter unfounded beliefs with correct information (DiFonzo et al., 2013). There are also major systems -level factors that contribute to the spread of misinformation in the United States, including: (1) declining social capital; (2) growing economic inequalities; (3) increasing political polarization; (4) declining trust in science; (5) politically asymmetric credulity; (6) an evolving media landscape; and (7) a fractioning of the media that rewards political extremism (The National Academies of Sciences, Engineering, and Medicine, 2017).
Understanding how these individual-, group-, and systems-level factors condition health literacy gives us clues about how misinfodemics are born and spread. But they also suggest measures that might be levered to develop intervention strategies and solutions to this slippery problem. We have identified a few such strategies, and we issue to healthcare professionals of all sorts a call to action. In the following recommendations, we propose health literacy promotion approaches that can be taken by four key professional stakeholder groups: healthcare organizations; community-based partnerships; cross-sector collaborations; and individual providers.
Healthcare organizations should strengthen their commitment to health literacy across the scope of operations
Healthcare systems are staffed by a clinical workforce that can leverage its therapeutic relationships with patients to promote and track progress in health literacy. Organizational leadership should avail of these relationships to prioritize the promotion of health literacy in all its outward-facing interactions, integrating health literacy content into planning, evaluation, communication, and patient safety strategies (Brach, 2017). It should identify appropriate “teachable moments” for addressing misinformation – such as care transitions, the prescription of medicines, and vaccination appointments – and plan appropriate health literacy interventions for each one.
Community health centers are sites of great potential for the promotion of health literacy. For over 50 years, health centers funded by the U.S. Health Resources and Services Administration (HRSA) have functioned as the nation’s primary care backbone for the medically underserved, coordinating care for over 29 million people across the U.S. And since part of these health centers’ statutory mission is to provide comprehensive healthcare to the medically underserved regardless of their insurance status or ability to pay, their patients include 1 of every 3 people living in poverty, 1 in 5 rural residents, 1 in 5 uninsured persons, 1 in 6 Medicaid beneficiaries, 1.4 million homeless people, and 385,000 veterans. Its more than 12,000 service delivery locations reach every state and territory, and 45% are in rural areas (National Association of Community Health Centers, 2019). If the healthcare organizations that manage these health centers recognize their potential, they could become key sites for promoting health literacy among the most vulnerable members of society – and for combatting the misinfodemics that thrive in just those contexts of exclusion where health literacy does not.
Healthcare professionals should build and enhance partnerships with the communities they serve
Healthcare organizations and providers already interact with the populations they serve, but strengthening relationships with diverse community organizations, congregations, and non-medical service agencies will strengthen their position in communities and open new opportunities for information exchange. For example, community-targeted forums can be organized in locally important venues such as churches, recreation centers, and community centers and designed to deliver and discuss relevant health information with the public. Similarly, local organizations can be recruited to serve as direct sources of timely, accurate information, leveraging their existing relationships and rapport with individuals and communities. These entities have an insider’s perspective and can offer valuable insights regarding the best ways to disseminate information and help to reach even the hardest-to-reach members of their communities.
Establishing strong partnerships with local organizations is especially important since the oral cultures of many communities make personal interactions crucial for information dissemination. At the same time, there is a strong scientific evidence base supporting participatory program design processes and demonstrating the benefits of involving members of target audiences in the design and testing of communication products (Cyril et al., 2015).
Healthcare professionals should reinforce their cross-sector collaborations with public health systems
In 2010, The Affordable Care Act expanded health insurance coverage for millions of Americans. But it also highlighted the need for healthcare and public health systems to work together to address individual health within the context of the larger community, incentivizing practices such as accountable care organizations and patient-centered medical homes that adopt integrative strategies (42 U.S.C. § 18001). Two years later, recognizing similar benefits, the Institute of Medicine’s (IOM) Committee on Integrating Primary Care and Public Health outlined a set of recommendations for aligning primary care with public health strategy. Its review examined over 400 collaborations between medical and public health actions and identified benefits for both primary care providers (such as the provision of population-based information that effectively enhanced their capacity to address behavioral and other underlying causes of illness) and public health entities (which received support from primary care providers in the execution of population-based strategies such as the collection of individual-level data for surveillance purposes and the dissemination of health education and health promotion messages) (Committee on Integrating Primary and Public Health, Board on Population Health and Public Health Practice & Institute of Medicine, 2012; Lassker, 1997).
Similarly, just last year, the American Academy of Family Physicians (AAFP) issued a position paper insisting on the importance and value of primary care and public health integration and urging its members to pursue and support integrative collaborations and interventions (American Academy of Family Physicians, 2015).
The current crisis is a prime opportunity for healthcare and public health professionals to build on their growing legacy of collaboration to partner once more, joining forces now to combat the misinfodemic that threatens the health and well-being of individuals and populations alike.
Individual healthcare providers should make every effort to understand and respond to their patients’ unique health-related knowledge, belief, and literacy conditions
A 2018 Gallup poll found that four in five Americans (84%) rated the honesty and ethical standards of nurses as “very high” or “high,” making them the most well-regarded professionals among those considered; doctors ranked second at 67% (Brenan, 2018). Another Gallup poll, conducted this March in the midst of the COVID-19 pandemic, produced similar findings, showing hospitals and health agencies to be the most trustworthy of the nine major national institutions and leaders proposed (Newport, 2020). Despite this privileged social regard, however, many front-line providers remain unaware of their patients’ beliefs – because they never ask. The notion of a personal explanatory model of illness refers to a patient’s representation of disease and is based on beliefs, emotions, knowledge, and experiences that are grounded in culture (Kleinman, 1980).
These representations of disease are associated with illness-related beliefs (such as how strongly they believe in self-control over health) and behaviors (such as how long patients stay in treatment) (Lau et al., 1989; Leventhal et al., 1980). While these personal explanatory models can differ radically from scientific models concerning the causation of disease, what people actually do in the face of illness is often a logical extension of their personal beliefs rather than of the scientific standard (Good, 1992). Individual doctors must recognize, then, that understanding a patient’s beliefs is the starting point for engaging in a discussion of how the patient encounters her world and what matters most to her – and that can become an important, personal, and personalized opportunity to correct misinformation, to improve health literacy, and – ultimately – to improve health.
Reiterating our call to action: A multi-level healthcare response to the misinfodemic
Countering the COVID-19 misinfodemic is a critical task for individual and public health. Healthcare professionals in all sectors and at all levels must strengthen their commitment to health literacy. Here we have issued four recommendations describing how healthcare organizations, community-based partnerships, cross-sector collaborations, and individual healthcare providers can play roles in the fight against misinformation by strengthening their efforts to build health literacy among the people and populations they serve.
And play a role they must: This battle is scored in lives and deaths.
- / Healthcare
- / Public Health
Cite this Essay
Damian, A. J., & Gallo, J. J. (2020). Promoting health literacy during the COVID-19 pandemic: A call to action for healthcare professionals. Harvard Kennedy School (HKS) Misinformation Review . https://doi.org/10.37016/mr-2020-027
Bibliography
Affordable Care Act of 2010, 42 U.S.C. § 18001 et seq . (2010). https://www.law.cornell.edu/uscode/text/42/18001
American Academy of Family Physicians. (2015). Integration of primary care and public health (position paper) . https://www.aafp.org/about/policies/all/integration-primary-care.html
Berkman, N. D., Sheridan, S. L., Donahue, K. E., Halpern, D. J., & Crotty, K. (2011). Low health literacy and health outcomes: An updated systematic review. Annals of Internal Medicine, 155 (2), 97-107. https://doi.org/10.7326/0003-4819-155-2-201107190-00005
Brach, C. (2017). The journey to become a health literate organization: A snapshot of health system improvement. Studies in Health Technology and Informatics, 240 , 203-237.
Brenan, M. (2018, December 20). Nurses again outpace other professions for honesty, ethics . Gallup. https://news.gallup.com/poll/245597/nurses-again-outpace-professions-honesty-ethics.aspx
Committee on Integrating Primary and Public Health, Board on Population Health and Public Health Practice & Institute of Medicine. (2012). Primary care and public health: Exploring integration to improve population health. The National Academies Press. https://doi.org/10.17226/13381
Cutilli, C. C., & Bennett, I. M. (2009). Understanding the health literacy of America: Results of the national assessment of adult literacy. Orthopaedic Nursing, 28 (1), 27-32. https://doi.org/10.1097/01.NOR.0000345852.22122.d6
Cyril, S., Smith, B. J., Possamai-Inesedy, A., & Renzaho, A. M. N. (2015). Exploring the role of community engagement in improving the health of disadvantaged populations: A systematic review. Global Health Action, 8 (1), 1-12. https://doi.org/10.3402/gha.v8.29842
DiFonzo, N., Bourgeois, M. J., Suls, J., Homan, C., Stupak, N., Brooks, B. P., Ross, D. S., & Bordia, P. (2013). Rumor clustering, consensus, and polarization: Dynamic social impact and self-organization of heresay. Journal of Experimental Social Psychology, 49 (3), 378-399. https://doi.org/10.1016/j.jesp.2012.12.010
Flynn, D. J., Nyhan, B., & Reifler, J. (2017). The nature and origins of misperceptions: Understanding false and unsupported beliefs about politics. Political Psychology, 38 (S1), 127-150.
Garrett, R. K., & Weeks, B. E. (2017). Epistemic beliefs’ role in promoting misperceptions and conspiracist ideation. PLoS One, 12 (9), e0184733. https://doi.org/10.1371/journal.pone.0184733
Good, B. J. (1992). Culture and psychopathology: Direction for psychiatric anthropology. In T. Schwartz, G. M. White & C. A. Lutz (Eds.), New Directions in Psychological Anthropology (pp. 181-205). Cambridge University Press.
Gyenes, N., & Marrelli, M. (2019). Health equity through health fact-checking: A primer . Meedan Digital Health Lab. https://health.meedan.com/primer.pdf
Kalichman, S. C., Cherry, C., & White, D. (2012). Use of dietary supplements among people living with HIV/AIDS is associated with vulnerability to medical misinformation on the internet. AIDS Research and Therapy, 9 (1), 1. https://doi.org/10.1186/1742-6405-9-1
Kleinman, A. (1980). Patient and healer in the context of culture: An exploration of the borderland between anthropology, medicine, and psychiatry . University of California Press.
Lassker, R. D. (1997). Medicine and public health: The power of collaboration . Health Administration Press.
Lau, R. R., Bernard, T. M., & Hartman, D. T. (1989). Further explorations of common-sense representations of common illness. Health Psychology, 8 (2), 195-219. https://doi.org/10.1037/0278-6133.8.2.195
Leventhal, H., Meyer, D., & Nerenz, D. T. (1980). The common sense representation of illness danger. In S. Rachman (Ed.), Contributions to Medical Psychology (pp. 7-30) . Pergamon Press.
Linde-Feucht, S., & Coulouris, N. (2012). Integrating primary care and public health: A strategic priority. American Journal of Public Health , 102 (3), S310-311. https://doi.org/10.2105/AJPH.2012.300849
Mitchell, A., & Oliphant, J. B. (2020, March 18). Americans immersed in COVID-19 news; most think media are doing fairly well covering it . Pew Research Center. https://www.journalism.org/2020/03/18/americans-immersed-in-covid-19-news-most-think-media-are-doing-fairly-well-covering-it/
National Association of Community Health Centers. (2019). America’s health centers . http://www.nachc.org/wp-content/uploads/2019/09/Americas-Health-Centers-Updated-Sept-2019.pdf
Newport, F. (2020, March 27). Six emerging conclusions: Public opinion and COVID-19 . Gallup. https://news.gallup.com/opinion/polling-matters/304646/five-emerging-conclusions-public-opinion-covid.aspx
Passche-Orlow, M. K., & Wolf, M. S. (2007). The causal pathways linking health literacy to health outcome. American Journal of Health Behavior, 31 (1), 19-26.
Scheufele, D. A., & Krause, N. M. (2019). Science audiences, misinformation, and fake news. PNAS, 116 (16), 7662-7669. https://doi.org/10.1073/pnas.1805871115
Southwell, B. G., & Thorson, E. A. (2015). The prevalence, consequence, and remedy of misinformation in mass media systems. Journal of Communication, 65 (4), 589-595. https://doi.org/10.1111/jcom.12168
The National Academies of Sciences, Engineering, and Medicine. (2016). Science literacy: Concepts, contexts, and consequences. The National Academies Press. https://doi.org/10.17226/23595
The National Academies of Sciences, Engineering, and Medicine. (2017). Communicating science effectively: A research agenda. The National Academies Press. https://doi.org/10.17226/23674
Uscinski, J. E., Klofstad, C., Atkinson, M. D. (2016). What drives conspiratorial beliefs? The role of information cues and predisposition. Political Research Quarterly, 69 (1), 57-71. https://doi.org/10.1177/1065912915621621
Zatocostas, J. (2020). How to fight an infodemic. The Lancet, 395 (10225), 676. https://doi.org/10.1016/S0140-6736(20)30461-X
This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided that the original author and source are properly credited.
Health Literacy and Access to Healthcare Services: Problems, Interventions, and Suggestions for Improvements Essay
Introduction, literature review.
Being aware of health threats and responding to them adequately is one of the fundamental skills that every person needs to possess in order to remain safe and secure. Unfortunately, due to the emergence of new health threats and the lack of accessibility to healthcare, as well as the absence of basic health literacy in an upsettingly large number of the U.S. population, changes have to be made to the current health management programs.
The Healthy People 2020 initiative was a rather noble endeavor that embraced a number of health concerns, including health literacy and accessibility, yet the outcomes have been less than satisfactory so far. Due to the problems in infrastructure, communication, and staffing, the issues of health education and accessibility remain unresolved (Office of Disease Prevention and Health Promotion, 2018). Thus, further efforts must be made in order to support vulnerable groups and increase overall health literacy and accessibility.
Thesis Statement
Despite the efforts made with the help of the Healthy People 2020 initiative to increase the accessibility of healthcare services, essential health support remains inaccessible for a large range of people due to the infrastructure issues, lack of financial support, absence of effective insurance, and low health literacy, which could be addressed with the help of an intervention that involves the use of IT and ICT tools for the dialogue between healthcare experts and communities.
Problem Description
Although the problem at hand cannot be considered as clearly visible as a specific disease or a disorder, it still has a clear and rather disturbing effect on public health. The problem of health accessibility and appropriate levels of health literacy has been quite prominent in the U.S. (Lyles, Fruchterman, Youdelman, & Schillinger, 2017).
Although several attempts have been made in order to prompt responsibility and the development of basic skills of self-care in patients, the recent outbreak of pandemics in the U.S. has shown that American citizens lack preparedness and the ability to apply the necessary skills. Moreover, the general levels of well-being in the U.S. also indicate that a substantial range of the American population does not have the access to decent healthcare (Office of Disease Prevention and Health Promotion, 2018). Thus, the key factors aggravating the situation and the main strategies for handling the problem need to be identified.
The burden of the Disease
Changes in recent years.
Notably, there have been several important changes to the management of health inaccessibility and the promotion of health literacy to vulnerable groups. For instance, the introduction of new frameworks that healthcare workers could use to provide sufficient support to a larger number of people has been incorporated into the framework. For instance, the creation of the Synergy Model for nursing (SM), which was expected to increase the extent of collaboration in the cross-disciplinary environment and, thus, allow for better management of information-related needs in target audiences, can be considered an important change (Coleman, Hudson, & Pederson, 2017).
In addition, nurse administrators have included a plethora of new tools for boosting the efficacy of patient-nurse communication, both in the hospital setting and for outpatients. Specifically, the application of Telehealth and relevant technologies have become an important tool for handling the process of patient education (Wittenberg, Goldsmith, Ferrell, & Ragan, 2017). In addition, devices for remote monitoring of outpatients’ health status have been extraordinarily helpful in preventing issues such as heart attack or kidney failure from having a fatal impact on patients’ lives (Friis, Lasgaard, Osborne, & Maindal, 2016).
However, the specified technologies still remain unattainable for a range of facilities (Friis et al., 2016). In addition, extra tools have to be included so that the process of health education could start. Thus, the levels of accessibility to health-related information and crucial services will rise.
Concepts to Be Considered
When considering the problem of the lack of health literacy and the inaccessibility of health services to certain populations, one would consider that the notions of disease incidence, prevalence, and case-fatality are irrelevant. At first glance, there is indeed little connection to be made between the problem of health literacy and the notions in question since the absence of health awareness itself is neither a condition nor a disease.
However, one should remember that the absence of health literacy leads to the development of a plethora of issues that have a very high incidence rate, bear significant prevalence, and even lead to lethal outcomes in patients. For example, the lack of awareness about health-literacy-related issues has led to the subsequent rise in the incidence of myocardial infractions, the prevalence of the disease, and the number of fatalities (17,900,000 annually worldwide) (World Health Organization, 2020). Therefore, considering the concepts of incidence, prevalence, and morbidity in relation to the health topic at hand is necessary since it will give approximate information about the scale and scope of the problem.
The notion of disease incidence is quite important to the estimation of its scale and the extent of the threat that vulnerable groups may face. Disease incidence represents a “proportion of newly developed cases divided by the number of individuals at risk for the same outcome during a specified time interval” (Inman & Sieper, 2016, p. 14). Therefore, the concept of incidence is typically used to characterize the development of a specific disease within a community, as well as the threat that it represents and the approximate level of contagion that it will imply. However, the phenomenon of incidence can also be used in relation to health awareness. Specifically, changes in the level of incidence will show the extent of health education in the target population and the effects that health literacy and access to health services have on their well-being.
Similarly, the concept of prevalence is traditionally used to characterize the extent of the spread of a particular disease. However, unlike incidence, which requires defining the number of new cases within a specific time period, disease prevalence is “The number of existing cases of disease at a particular point in time” (Woodward, 2013, p. 9). The analysis of prevalence helps to evaluate the extent of the present problem and calculate the number of resources needed to address it. Thus, the phenomenon of prevalence is closely connected to the concept of health accessibility and health literacy as the indicator of the current levels of it and the extent of changes that have to be made to increase it.
Case-fatality
Another important ratio that allows determining the scale and progression of a disease and the rates of health accessibility and health literacy within a community, the case-fatality formula implies “the number of people who die of a disease divided by the number of people who have the disease” (Celentano, Hopkins, & Szklo, 2018, p. 125). Thus, the case-fatality ratio will help to identify the urgency of a problem and the speed at which a health accessibility program needs to be created.
At the same time, one should give credit to some success in the target area. For instance, a recent article shows that the incidence, prevalence, and case-morbidity associated with CVD has dropped (Mensah et al., 2017). When considering the changes that have occurred in the levels and extent of health accessibility and health literacy over the past decade, a rather depressing trend can be noticed. Although the usage of new media and innovative technology for communication has helped to advance the conversation between a nurse and the American community, the increase in the amount of false information has also risen (Klein, Quisenberry, Shoben, Romer, & Peters, 2019). As a result, a larger number of people have embraced health-related myths despite their absurdity, thus increasing the threat to their health and well-being.
Consequently, although the current trends in prevalence, incidence, and case-fatality across different disorders and diseases in American citizens vary to a great extent, the fact that some of the health issues are still characterized by high rates of at least one of the described characteristics is quite worrisome (Klein et al., 2019). Moreover, addressing some of the most recent health issues, one should mention that the absence of health accessibility and literacy poses a tremendous threat to the lives of millions of people. Specifically, the astounding rise in prevalence, incidence, and case-fatality of COVID-19 across the U.S. and especially in New York indicate that people need to be instructed in detail about crucial health management strategies.
Main Issues
When approaching the previous frameworks for the promotion of health literacy and defining why they did not work, one should mention the absence of detailed and easily understandable clarifications on the mechanisms of the virus contraction, disease development, and its prevention. Therefore, it will be critical to providing explanations about the reasons for particular health management measures to be imposed on citizens, as well as the reasons why the proposed strategies work.
In addition, the issue of health accessibility needs to be addressed in greater detail. While there are currently several reasons for American citizens not to be able to use health-related services, some of the obstacles are more prominent than others. For example, the presence of the language barrier can be deemed as the foundational obstacle in increasing health literacy rates among the representatives of ethnic minorities living in the U.S.
According to the study performed by Martínez-Delgado (2016), the promotion of oral health literacy in the target population has been failing so far due to the challenges in dispersing information among the target audiences. Moreover, even with the increased dissemination of data and better understanding, the threat of misconceptions, and the inability to communicate with the target groups freely implies a drop in the overall health literacy levels. Thus, strategies for handling the language barrier need to be introduced.
The lack of competent nursing experts, who could engage in the active education of vulnerable groups and promote the dynamic development of basic health management skills in Americans is another problem that has to be addressed on the nation-wide level. According to Vermeir et al. (2017), the issue of nurse shortage has risen drastically in its scale and effects over the past decade, causing the efficacy of healthcare to drop. As a result, the quality of communication between nurses and patients has been faltering, leading to massive gaps in people’s health awareness (Vermeir et al., 2017). The outcomes of the shortage of nursing experts can be observed currently as the U.S. is facing the pandemics of COVID-19 (Lee, Ng, & Khong, 2020).
According to the latest data, despite the tremendous efforts put into the management of health needs of vulnerable populations and the improvement of communication, a vast number of American citizens remain oblivious to the importance of taking appropriate precaution measures.
The cost of healthcare services is another factor that prevents many U.S. citizens from getting the health support that they require. Specifically, a staggering number of Americans cannot afford Medicaid as a personal choice, which is why their options for addressing health issues or even receiving preventive health services, are very limited (Bhatt & Bathija, 2018). The specified issue outlines the problems of private insurance and emphasizes the need to provide high-quality care for all individuals, which may require deviating from the income-based approach.
In turn, the Medicare framework requires the approval of the Social Security Disability service, which is why it may be complicated for some people that have reached the age of retirement to receive appropriate financial support. The problem of financing is one of the foundational issues with contemporary U.S. healthcare. While private health insurance as one of the possible suggestions cannot be accepted due to the lack of consistency and certainty in their framework, the current public ones do not provide sustainable finances for supporting retirees.
Recent Strategies
In order to address the problem of health accessibility, several notable efforts have been made. Among the key strategies that have been developed to manage the lack of health accessibility and health literacy, the increase in the number of primary care providers can be seen as an important, even if somewhat mishandled, attempt. An endeavor at raising the number of primary care providers and reinforcing their role in health education among patients has recently been undertaken, yet the problems with staffing have been preventing the proposed strategy from being implemented (Huh, Shin, & Peck, 2020). Indeed, with the services of primary care providers, patients would have easier access not only to key health services such as vaccinations, regular health examinations, and other opportunities, but also relevant literature.
Another important step that has been taken in the direction of increasing healthcare accessibility is the need to address disparities in the management of citizens’ healthcare needs. Unfortunately, even with a plethora of programs launched to address the instances of discrimination or negligence of minority groups’ needs, the specified populations still suffer from significant underrepresentation and the lack of access to basic healthcare services (Lee & Vang, 2010). As a result, the levels of mortality, disease development, incidence, prevalence, and case-fatality are particularly high among the specified demographics (Lee & Vang, 2010).
Therefore, cross-cultural strategies for addressing the health concerns of vulnerable populations have been created recently (Rudd, 2019). As emphasized above, language issue represents a particularly strong obstacle to overcome along with false health-related beliefs, yet economic and financial issues also take the toll on representatives of ethnic and racial minorities in the U.S. (Bhatt & Bathija, 2018). Consequently, the programs such as the National Prevention Strategy have been launched to improve the current situation (Rudd, 2019). To their credit, the programs in question have delivered certain results, yet further improvements are still needed.
Proposed Measures
Although the existing frameworks for managing the problems of patients who have few opportunities for accessing health services are quite impressive, further adjustments will be needed to ensure that these programs are culturally inclusive and accessible to people from all social backgrounds. In order to increase the process of spreading health accessibility, nurses have to use innovative tools and techniques, including modern media and ICT devices. For instance, the use of Telehealth, telemedicine, and health portals as the main resources for patients to derive crucial information and support from deserving a mentioning (Rouleau, Gagnon, & Côté, 2015).
In addition, the tools for evaluating the efficacy and overall coverage of insurance offered to American citizens will be strongly needed. Since the current coverage rates leave much to be desired, it is imperative to monitor them more closely to locate the opportunities for increasing them and removing the factors that prevent people from getting the required insurance.
Therefore, a communication system between American residents, in general, and vulnerable groups, such as people living in poverty, people belonging to multicultural backgrounds, and other disadvantaged members of the U.S. population, has to be introduced. The application of innovative communication tools for receiving feedback and providing crucial guidance to target audiences will be needed. Specifically, the use of social media is highly encouraged as a means of communicating key principles of health management to patients.
In addition, to address the linguistic and cultural barriers, healthcare facilities will have to consider hiring nurses from different cultural backgrounds. Thus, the issues of cultural miscommunication or misunderstanding will be addressed. Moreover, multiple myths about health and healthcare will be removed from the discourse, encouraging patients to follow the provided guidelines. As a result, patients will be able to recognize threats and utilize the available tools to respond to these threats promptly.
The problem of insurance is another concern that has to be managed in order to increase e healthcare accessibility. The use of mobile clinics can be considered a solution for assisting those that live in remote areas (Rudd, 2019). The specified approach has been utilized in several states, yet further support will be needed to manage the transition to a new framework for tending to the needs of patients with low healthcare accessibility options.
Finally, tools for monitoring the application of appropriate measures and especially the use of newly developed communication channels will be needed. In order to improve communication between nurses and their communities, one may consider using the Telehealth option (Bhatt & Bathija, 2018), Although not being a recent introduction into the healthcare context, the Telehealth framework offers quite a number of opportunities for increasing the efficacy of communication between patients and nurses. For instance, the adoption of Telehealth services has been considered as a response to the current coronavirus pandemic (Lee & Wang, 2010).
However, while some hospitals have deployed the specified strategies, the lack of homogeneity in their approaches and the fact that very few other healthcare facilities have followed suit indicate that changes have to be made on a fundamental level. Therefore, health promotion policies must be instated to deploy Telehealth techniques as the means of building awareness, educating patients, monitoring their progress, and controlling their exposure to health threats.
The problem of health accessibility has been building over the past decade to reach a truly grandiose form presently despite the efforts to increase awareness among the target audiences, which means that improved information channels have to be used to address the issue. Namely, the introduction of the strategies based on dismantling the existing stereotypes concerning the management of health issues in individuals.
It is believed that the creation of additional communication channels that will help nurses in managing the process of patient education will help in building awareness concerning emergent health threats. As a result, the overall rates of health accessibility and preparedness toward health concerns will increase. Moreover, the change in question will affect the levels of health literacy and contribute to the management of the low levels of health education among general audiences. Thus, the levels of public health, health literacy, and accessibility of healthcare services will increase.
Bhatt, J., & Bathija, P. (2018). Ensuring access to quality health care in vulnerable communities. Academic Medicine, 93 (9), 1271-1275. Web.
Celentano, D. D., Hopkins, J., & Szklo, M. (2018). Gordis epidemiology (6th ed.). New York, NY: Elsevier Health Sciences.
Coleman, C., Hudson, S., & Pederson, B. (2017). Prioritized health literacy and clear communication practices for health care professionals. HLRP: Health Literacy Research and Practice, 1 (3), 91-99. Web.
Friis, K., Lasgaard, M., Osborne, R. H., & Maindal, H. T. (2016). Gaps in understanding health and engagement with healthcare providers across common long-term conditions: A population survey of health literacy in 29 473 Danish citizens. BMJ Open, 6 (1), 1-12. Web.
Huh, K., Shin, H. S., & Peck, K. R. (2020). Emergent Strategies for the Next Phase of COVID-19. Infection & Chemotherapy, 52 (1), 105-109. Web.
Inman, R., & Sieper, J. (Eds.). (2016). Oxford textbook of axial spondyloarthritis . Oxford University Press.
Klein, E. G., Quisenberry, A. J., Shoben, A. B., Romer, D., & Peters, E. (2019). The influence of health numeracy and health warning label type on smoking myths and quit-related reactions. Nicotine and Tobacco Research, 21 (7), 974-978. Web.
Lee, E. Y., Ng, M. Y., & Khong, P. L. (2020). COVID-19 pneumonia: what has CT taught us?. The Lancet Infectious Diseases, 20 (4), 384-385. Web.
Lee, H. Y., & Vang, S. (2010). Barriers to cancer screening in Hmong Americans: The influence of health care accessibility, culture, and cancer literacy. Journal of Community Health, 35 (3), 302-314. Web.
Lyles, C. R., Fruchterman, J., Youdelman, M., & Schillinger, D. (2017). Legal, practical, and ethical considerations for making online patient portals accessible for all. American Journal of Public Health, 107 (10), 1608-1611.
Martínez-Delgado, C. M. (2016). Some considerations on the Latin American oral health literacy. Journal of Oral Research, 5 (2), 59-60.
Mensah, G. A., Wei, G. S., Sorlie, P. D., Fine, L. J., Rosenberg, Y., Kaufmann, P. G.,… Gordon, D. (2017). Decline in cardiovascular mortality: Possible causes and implications. Circulation Research, 120 (2), 366-380. Web.
Office of Disease Prevention and Health Promotion. (2018). Access to health services . Web.
Rouleau, G., Gagnon, M. P., & Côté, J. (2015). Impacts of information and communication technologies on nursing care: an overview of systematic reviews (protocol). S ystematic Reviews, 4 (1), 75. Web.
Rudd, R. E. (2019). Health literacy considerations for a new cancer prevention initiative. The Gerontologist, 59 (Supplement_1), S7-S16.
Vermeir, P., Degroote, S., Vandijck, D., Mariman, A., Deveugele, M., Peleman, R.,… Vogelaers, D. (2017). Job satisfaction in relation to communication in health care among nurses: A narrative review and practical recommendations. SAGE Open, 7 (2), 1-11. Web.
Wittenberg, E., Goldsmith, J., Ferrell, B., & Ragan, S. L. (2017). Promoting improved family caregiver health literacy: evaluation of caregiver communication resources. Psycho‐Oncology, 26 (7), 935-942. Web.
Woodward, M. (2013). Epidemiology: Study design and data analysis (3rd ed.). New York, NY: CRC Press.
World Health Organization. (2020). Cardiovascular diseases . Web.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, March 25). Health Literacy and Access to Healthcare Services: Problems, Interventions, and Suggestions for Improvements. https://ivypanda.com/essays/health-literacy-and-access-to-healthcare-services-problems-interventions-and-suggestions-for-improvements/
"Health Literacy and Access to Healthcare Services: Problems, Interventions, and Suggestions for Improvements." IvyPanda , 25 Mar. 2024, ivypanda.com/essays/health-literacy-and-access-to-healthcare-services-problems-interventions-and-suggestions-for-improvements/.
IvyPanda . (2024) 'Health Literacy and Access to Healthcare Services: Problems, Interventions, and Suggestions for Improvements'. 25 March.
IvyPanda . 2024. "Health Literacy and Access to Healthcare Services: Problems, Interventions, and Suggestions for Improvements." March 25, 2024. https://ivypanda.com/essays/health-literacy-and-access-to-healthcare-services-problems-interventions-and-suggestions-for-improvements/.
1. IvyPanda . "Health Literacy and Access to Healthcare Services: Problems, Interventions, and Suggestions for Improvements." March 25, 2024. https://ivypanda.com/essays/health-literacy-and-access-to-healthcare-services-problems-interventions-and-suggestions-for-improvements/.
Bibliography
IvyPanda . "Health Literacy and Access to Healthcare Services: Problems, Interventions, and Suggestions for Improvements." March 25, 2024. https://ivypanda.com/essays/health-literacy-and-access-to-healthcare-services-problems-interventions-and-suggestions-for-improvements/.
- The Relation of Health to Geography
- Minimizing Flood Fatalities in Canada
- Mountaineering Fatalities in Denali 1903-2006
- Accessibility and Spatial Accessibility
- Reproductive Oppression as a Source of Disparity in Maternal Fatalities
- Reading Commentary About Literacy Articles: What Does Literacy Mean?
- Article Reflection about Literacy
- Literacy Development in Adults
- Health Literacy: Does It Make a Difference?
- Implementation of the Health Literacy Programs
- Situational Analysis of Obesity in the United Arab Emirates
- The Outcomes of Appliance Digital Therapeutics in Healthcare
- Hyper Granulation Tissue: Capstone Project
- Telehealth: A Mind Map and Telehealth Implementation
- Opioid Disease Prevention: Levels of Disease Prevention
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Health Promot Int

Critical health literacy: reflection and action for health
Thomas abel.
Institute of Social and Preventive Medicine University of Bern, Bern, Switzerland
Richard Benkert
Health literacy research is growing rapidly and broadly; however, conceptual advances in critical health literacy (CHL) seem hampered by a lack of a clear definition. In this paper, we refer to key features of the concept as identified in earlier works, offer a new definition of CHL and briefly discuss its theoretical roots. Reflection and action are suggested as the two constituent components of CHL. Consequences for future research are also discussed.
In public health and health promotion, health literacy is considered an important resource for individual and collective empowerment ( Nutbeam, 2000 ; Kickbusch, 2001 ). Among the different types of health literacies, critical health literacy (CHL) has recently gained increased attention in health research with the number of publications substantially increasing since 2010 ( Benkert and Abel, 2022 ). It was originally drawn from the concept of critical literacy, which focused on individuals’ abilities to analyse and use information as a means of greater autonomy and empowerment ( Nutbeam, 2000 ; Sykes et al., 2013 ). Beyond this, CHL was also introduced to address socio-political dimensions of health literacy ( Sykes et al., 2013 ). These socio-politico dimensions refer to agency as the ability to bring about social and political change and—through an improved capacity to act on the social determinants of health (SDOH)—overcome ‘structural barriers to health’ ( Nutbeam, 2000 , p. 267). Thus, CHL is not limited to achieving individual health benefits; it also entails empowering communities and reducing social health inequalities.
Although Nutbeam’s foundational work introduced the concept of CHL, he did so without providing a concise definition. In principle, this openness could have meant opportunities to develop definitions of CHL that address its distinct features and account for dynamic, evolving contexts. However, without such attempts and a concise definition, later works addressing CHL often fell back onto notions of ‘critical literacy’ losing socio-political dimensions originally considered a key component of CHL ( Sykes et al., 2013 ). Over time, as Sykes and colleagues (2013) pointed out, critical literacy has almost become the de facto definition of CHL. Yet, although the definition of critical literacy alludes to greater individual control over life events, consequent notions of CHL tend to ‘lack... specific reference to social and political action and existence at a population level’ ( Sykes et al., 2013 , p. 8). Therefore, ‘these elements are in danger of becoming lost so distorting the original meaning and emphasis’ ( Sykes et al., 2013 , p. 8). Although there are many descriptions of what CHL entails, to the best of our knowledge to date, there is still no clear definition of this term that accounts for its conceptual origins regarding empowerment and social inequality.
Current CHL approaches address an awareness of social and cultural conditions as prerequisite to acquire competencies required to act for reducing health inequalities ( Chinn, 2011 ); however, these approaches, and health literacy research in general, including research on CHL, often omit theoretical support ( Pinheiro, 2021 ). Referring to CHL’s theoretical underpinnings, Pithara (2020) notes that ‘CHL adopts an emancipatory, empowerment-led understanding, where people are cognizant of social, economic and environmental determinants of health and are able to tackle these through community action’ (p. 2). Intervention frameworks have been designed to promote awareness, understanding and reflection by educating individuals and communities about SDOH; thereby contextualizing CHL and teaching community members how to empower people to ameliorate health inequalities ( Mogford et al., 2011 ). Yet, until today, CHL’s basic role in the social reproduction of health inequalities remains an open issue. With socio-political features of CHL as a core attribute ( Nutbeam, 2000 ; Sykes et al., 2013 ), it seems warranted that social theories would guide CHL research and practice; still, theoretical frames in CHL research are markedly absent. One noticeable exception is the work of Sykes and Wills (2018 , 2019 ). These authors suggest a socio-critical approach, tracing the concept of CHL back to the idea of ‘critical consciousness’ developed by Brazilian educator and philosopher Paulo Freire.
In what follows, we present our definition of CHL and briefly revisit Freire’s Pedagogy of the Oppressed (1970/2005) as it provides theoretical support for CHL’s socio-emancipatory function. We provide examples of how the new definition can illuminate current CHL assessments. We then refer to Pierre Bourdieu’s ‘theory of practice,’ as an example of a theoretically meaningful application of our new definition of CHL within the broader health inequality discourse. Our definition of CHL is meant as a starting point for further discussion, development, and application in future research about CHL and social health inequality.
DEFINING CRITICAL HEALTH LITERACY
Building upon those earlier works referenced above, we focus on reflection and action as two constituent components for our definition of CHL for public health and health promotion. We define CHL as the ability to reflect upon health determining factors and processes and to apply the results of the reflection into individual or collective actions for health in any given context . Developed with a focus on empowerment and health inequalities, our definition is suitable and flexible to serve a wide range of research questions and address more specific forms of CHL that can consider the social contexts in which CHL operates. For both purposes, reflection and action remain the two major constituent components of CHL, which allow addressing individual and collective agency and its structural conditions.
ROOTS OF REFLECTION AND ACTION FROM PAULO FREIRE
Providing useful theoretical grounding for conceptualizing CHL, health literacy scholars have drawn from Freire’s (1970 / 2005 ) critical pedagogy work ( Gould et al., 2010 ; Chinn, 2011 ; Mogford et al., 2011 ; Estacio, 2013 ; Sykes et al., 2013 ; Renwick 2017 ; Sykes and Wills, 2018 ). We argue the social conditions of health find strong anchoring among Freire’s components: reflection and action. Freire explores how oppression is socially installed and how to liberate from it. He challenges traditional approaches in education, which he calls the ‘education as the practice of domination’ in a hierarchically structured society ( Freire, 1970 / 2005 , p. 81). According to the so-called ‘banking concept’ of education, students are treated as recipients of knowledge or ‘depositories’, deprived of the possibility to acquire ‘critical consciousness’ ( Freire, 1970 / 2005 , pp. 72, 73, 83) and thus depleted of the ability to liberate themselves from dominating systems.
For Freire, empowerment in general presupposes that social determinants are questioned. He advocates for a ‘problem-posing education’ pedagogical theory in which education is understood as ‘the practice of freedom’ and where students are treated as people who are educated into being ‘critical thinkers’ in a participatory and dialogical way of learning ( Freire, 1970 / 2005 , p. 81). He explains, ‘In problem-posing education, people develop their power to perceive critically the way they exist in the world with which and in which they find themselves’ ( Freire, 1970 / 2005 , p. 83). In other words, all individuals need to acquire a critical attitude towards the socio-cultural reality that shapes their lives— reflection . Furthermore, individuals must also develop the ability to change their life-world through action . With reference to Prilleltensky (1989 , p. 800), Jemal (2017) notes that ‘the process whereby people achieve an illuminating awareness both of the socio-economic and cultural circumstances that shape their lives and their capacity to transform that reality is parallel with an empowerment process’ (p. 3). A person’s capability to reflect upon their world and the action it takes to change it are considered central instruments for empowerment ( Freire, 1970 / 2005 , p. 79).
Reflection and action have been conceptualized as the two main components of Freire’s critical consciousness. Reflection means ‘examining everyday realities to analyse relationships between personal contexts and the wider social forces of structural oppression (e.g. social, economic and political environments) that restrict access to opportunity and resources, and thus, sustain inequity and perpetuate injustice that limit well-being and human agency’ ( Jemal, 2017 , p. 6). Action refers to ‘the overt engagement in individual or collective action taken to produce socio-political change of the unjust aspects (e.g., institutional policies and practices) of society that cause unhealthy conditions’ ( Jemal, 2017 , p. 6). Others describe critical action as an ‘individual’s objective ability or potency to act given structural constraints’ ( Campbell and MacPhail, 2002 , p. 333). In fact, the ability of individuals or communities to reflect and act with the aim of improving structural conditions for health was already addressed in Nutbeam’s (2000) first delineation of CHL. He puts it like this: CHL ‘reflects the cognitive and skills development outcomes which are oriented towards supporting effective social and political action, as well as individual action’ (p. 265). In a further remark, he states, implying reference to reflection, that CHL encompasses the ‘development of skills which investigate the political feasibility and organizational possibility of various forms of action to address social, economic and environmental determinants of health’ ( Nutbeam, 2000 , p. 265). In this regard, it has been pointed out that CHL is linked to understanding the determinants and policy context of health, as well as of opportunities to challenge these determinants and policies. At the same time, it is linked to motivation and actual action at political and broader social levels ( Sykes et al., 2013 , p. 5).
CONSEQUENCES FOR CRITICAL HEALTH LITERACY ASSESSMENTS
Several studies have provided empirical measures assessing selected aspects of CHL (e.g. Ishikawa et al., 2008 ; Osborne et al., 2013 ; Abel et al., 2015 ). Most of these, however, were focused on assessing individuals’ abilities to critically evaluate information or their critical literacy. From a theoretical perspective, empirical measures of empowerment linked to reflection and action that could address social forces at structural and individual levels in comprehensive, theoretically coherent ways are missing.
While reflection and action have rarely been measured explicitly in CHL research to date, some empirical instruments are available, addressing single elements of empowerment and political components of CHL, such as Chinn and McCarthy’s (2013) All Aspects of Health Literacy Scale (AAHLS); Matsumoto and Nakayama’s (2017) Health Literacy on the Social Determinants of Health Questionnaire (HL-SDHQ); and Shannon and Parker’s (2020) Health Communication Questionnaire. In this respect, our definition of CHL might prove useful to illuminate previous findings. For example, Matsumoto and Nakayama (2017) addressed socio-political dimensions of CHL and the ability to bring about health-relevant changes at the population level (i.e. community empowerment). Their HL-SDHQ tool points to a more advanced assessment of CHL since it includes items about an individual’s ‘ability to cooperate in the creation of a fair society in which everyone can live a healthy life’ (p. 6) or to ‘involve oneself in politics and public administration on various health-related issues’ (p. 7). Applying our new definition of CHL can facilitate a focused interpretation of their findings. For instance, those two items clearly addressing the ‘action’ part of CHL, while also encouraging researchers to pursue theory-guided assessments.
Another example of how the new definition of CHL can illuminate previous findings comes from Chinn and McCarthy’s (2013) AAHLS instrument. This measure contains questions that indirectly provide information about reflection and action. For instance, one question elicits the ‘perceived possibilities’ of the individual’s contribution to community health, alluding to ‘reflection.’ Another question from the AAHLS deals with active participation in health-promoting processes, implying the action part of CHL. Reflection and action and their acquisition and application are dependent on the context in which people strive for better health ( Abel, 2008a ; Nutbeam, 2009 ; Pithara, 2020 ; Pinheiro, 2021 ). Recent studies have used qualitative research methods for deeper understandings of inequality dynamics in the context of health care, including the application of CHL ( de Wit et al., 2017 ; Dubbin et al., 2021 ). Insights obtained via qualitative methods and analyses may also provide evidence for interventions for improving CHL, spurring community empowerment and reducing health inequalities ( Gould et al., 2010 ; Mogford et al., 2011 ).
Since any definition of CHL for health research should facilitate empirical study by providing theoretical guidance without restricting the breadth of immanent research questions, our definition above is kept sufficiently broad to support empirical measures for different health themes and fields (e.g. health-relevant lifestyles and consumer markets, healthcare contexts, workplace, and housing conditions). Moreover, previous empirical approaches to health literacy have been subject to basic criticism for measures that tend to address health issues from class-biased or context-insensitive perspectives ( Abel, 2008a ; Pinheiro, 2021 ), such as those addressing health lifestyle items that are out of reach or less relevant for health in materially deprived living conditions. For example, measures assessing individuals’ knowledge about selecting healthy, yet often more expensive foods or risks overestimating agency, while downplaying the role of structural constraints for action and reflection. Thus, definitions of CHL that aim at supporting empirical study should facilitate a broad range of research questions about inequality, while also avoiding conceptual biases.
CRITICAL HEALTH LITERACY AND THE REPRODUCTION OF INEQUALITY—PIERRE BOURDIEU
Considering our definition of CHL, questions about social inequalities and inequities arise: how does CHL affect health, health behaviours and their social conditions? What are the individual and communal conditions in which CHL can best be acquired? What are the social, economic and cultural resources needed for a successful application of CHL in various contexts, such as healthcare systems, workplaces and leisure time activities? Such questions refer directly to unequal and inequitable chances for an individual’s agency to achieve good health. They also lead to basic questions about structural factors and processes, including broader questions about how CHL ties into the dynamics of reproducing social inequalities at the population level.
Theoretical guidance seems warranted to address these larger questions and anchor the concept of CHL firmly within social health inequality discourse. To assist more comprehensive understandings of links between a person’s structural living conditions and their chances to reflect upon and act on SDOH (i.e. their CHL), we call upon Pierre Bourdieu’s theory of practice ( Bourdieu, 1977a ; Bourdieu and Passeron, 1990 ) and his concepts of habitus and capital ( Abel and Frohlich, 2012 ). Bourdieu’s theory of practice has been successfully applied to study how health inequalities are reproduced ( Williams, 1995 ; Veenstra 2007 ; Schori et al. 2014 ; Jeong and Veenstra, 2017 ), including social patterning of health lifestyles, beliefs and health behaviours ( Cockerham et al., 1997 ; De Clercq et al., 2017 ; Gagné et al., 2018 ; Kandt, 2018 ).
The concepts of habitus and capital bear specific relevance for theoretically grounding CHL. In a Bourdieusian approach, reflection and action are primarily of social origin. They can be explained as an expression of the habitus that ‘serves as a cognitive map or set of perceptions that routinely guides and evaluates a person’s choices and options’ ( Cockerham, 2005 , p. 61). The habitus ties an individual’s reflection to action and operates as a constant, yet dynamic and flexible filter and guide across different contexts. Researchers of health inequality have used this concept to explain the reproduction of inequalities via health-relevant social practices and lifestyles ( Cockerham, 2005 ; Veenstra, 2018 ). Habitus and health lifestyles are closely tied to the availability of economic, social and cultural capital; therefore, they are inextricably linked to an individual’s social position in a ‘field of struggles’ ( Bourdieu and Wacquant, 1992 , p. 101), such as those over resources needed to live healthy lives or achieve good health across different contexts ( Khawaja and Mowafi, 2006 ; Missinne et al., 2014 ; Deshmukh et al., 2015 ; Paccoud et al., 2020 ).
Among the different forms of capital, cultural capital bears special importance for health literacy research ( Abel, 2007 ; Adkins and Corus, 2009 ). Cultural capital allows an individual to succeed in the competition over privilege, power, and status ( Bourdieu and Passeron, 1990 ; Bourdieu, 1977b ). Applied to health, the concept of cultural capital addresses issues of unequal distribution of health and its resources in a theoretically coherent way ( Abel, 2008b ; Shim, 2010 ; Veenstra and Abel, 2019 ). Cultural capital comes in three different types, namely, institutionalized, objectivized and embodied cultural capital. Educational degrees and other formal qualifications, typically issued by accredited institutions of higher education, are the most widely used measures of institutionalized cultural capital . Material forms, objects or goods of cultural value signifying higher or superior social status (e.g. art in the home, possession of highbrow books or clothes) indicate an individual’s objectivized cultural capital . Finally, e mbodied cultural capital refers to various kinds of behaviours, skills and socially relevant, valued knowledge acquired through formal and informal education in schools, families, sport clubs, etc. ( Abel, 2007 , 2008b ; Oude Groeniger et al., 2020 ). It comprises health-relevant tastes, preferences and dispositions that are physically embodied, part of the habitus and practised through lifestyles ( Cockerham, 2005 ). Health literacy broadly defined can be understood as part of this embodied cultural capital, and with it, CHL addresses social conditions and processes operating in the reproduction of health inequalities ( Abel, 2007 ). Explaining CHL as part of an individual’s cultural capital, health-related habitus and lifestyles— with the latter structured along the lines of social class, status or milieu—thus provides a theoretically coherent way of linking CHL to the prevailing social structures of health inequalities.
Moreover, a theoretical approach via cultural capital identifies two interrelated functions of CHL. First, being part of an individual’s cultural capital, CHL can strengthen individual and collective agency, operating as a resource for individuals in their pursuit of better health. Second, since chances to acquire and use CHL are unequally distributed along the lines of established social hierarchies (e.g. via educational systems), it operates as a transmitter of collective inequality in different contexts. For example, contexts where there is group-based competition over health resources and power, community struggle over environmental resources ( King et al., 2021 ), or patients’ struggles over access to quality health services ( Shim, 2010 ; Rasmussen et al., 2021 ).
From its beginning, CHL has been discussed as a concept that illuminates the factors and processes at work when individuals actively deal with health matters by critically considering the social conditions of health. However, in the absence of a clear definition of CHL most research approaches showed a neglect of the concept’s focus on social conditions and socio-political features ( Sykes et al., 2013 ; Chinn, 2011 ; Chinn and McCarthy, 2013 ; Guzys et al., 2015 ; Diviani, 2019 ). The new definition we offer in this paper is geared towards two components of individual and collective agency: reflection and action on health matters. It considers SDOH as structural factors and recognizes contextual conditions for people to acquire and apply CHL.
Along with Freire and other critical researchers, we propose that reflection and action need to be linked conceptually and practically to reach empowerment for health ( Rubinelli et al., 2009 ; Chinn, 2011 ; Mogford et al., 2011 ; Estacio, 2013 ; Sykes et al., 2013 ; Renwick, 2017 ; Sykes and Wills, 2018 ). This is because action without purposeful reflection runs the risk of mere ‘activism’ ( Freire, 1970 / 2005 , p. 88); and reflection without action might result in intellectual discovery only or what Freire identified as empty ‘verbalism’ (p. 87). CHL should capture the interplay of reflection and action, particularly in times when the contextual conditions for health become more and more complex. Many healthcare systems today increasingly turn into diversified markets with vested interest groups competing over profits and patients or consumers, making it progressively difficult for individuals and whole population groups to critically choose and act according to that choice (e.g. selecting healthcare services and insurance plans). CHL can and should address the SDOH but also the basic principles of power, whether economic markets or political systems.
We further suggested that Bourdieu’s theory of practice might be a viable option for anchoring CHL to the broader health inequality discourse. Again, our discussion is meant only as a starting point. Future studies might show how Bourdieu’s work can provide further and more specific contributions to situate CHL firmly in the context of social reproduction. However, other social theories can provide support for applying the new definition of CHL in health inequality research. Linking reflection and action to understand the basic components of agency and how it contributes to social reproduction or how it may lead to social change, opens CHL to insights from capabilities theory ( Sen, 1985 / 1993 ; Robeyns, 2005 ; Abel and Frohlich, 2012 ; Pithara 2020 ) and health lifestyle theory ( Cockerham, 2005 ). These theories both address fundamental issues of structure and agency in health inequalities. Future studies might explore questions about CHL’s role in individuals’ freedom to achieve health or the importance of CHL for the practice of health lifestyles to achieve better health and social status.
Our new definition also seeks to overcome some of the theoretical limitations previous approaches faced. Defined this way, CHL avoids individual reductionism —a point of critique for previous health literacy approaches ( Guzys et al., 2015 ). By stressing reflection and action on social factors that determine health, as well as including the contextual conditions, individuals and communities strive for better health within, these can safeguard against risks of individualizing health literacy approaches. From our new definition, questions for future studies arise, such as how reflection can strengthen contextualizing health actions and strengthen individuals as agents and experts for health in their own life worlds. The focus on refection and action under conditions of social inequality suggests even farther-reaching topics. For instance, CHL theory and measurement might need to consider issues of intersectionality when addressing questions about what form of health inequities are at stake in specific contexts. Drawing on works from Crenshaw (1991) and those writing drawing from intersectionality theory ( Collins, 2015 ) might also help advance the concept of CHL and augment critical discussions of health literacy in general.
The new definition also avoids too much normativity and the risks that come with it. As Huber et al. (2012) note:
the health literacy movement, at least in its current form, operates in a top-down model, where the establishment is primarily prescribing action plans designed to identify individuals with limited or low health literacy and provide interventions that seek to improve one’s ability to comprehend and use health information in appropriate ways. (p. 440)
Our definition of CHL points to a different direction, namely critical reflection by individuals opposing highly normative ‘prescriptions’ and instead, critically thinking about health, its social conditions, and the manifold interests of those involved in its production and distribution. When applied in research about SDOH, our new definition might be helpful to overcome the prevailing divides into ‘structural versus behavioural factors’ and ‘material versus non-material factors’ ( Macintyre, 1997 ). Both divides are implicitly opposed by our definition that links structure and agency and stresses critical reflection and action relevant at all levels.
Although our discussion above has pointed to pending issues in theory development, the new definition of CHL also has implications for empirical research. Empirical studies on CHL can benefit from a theory-based definition in the development of new assessment tools in several ways. First, reflection and action define a clear focus for developing new indicators (quantitative approaches) and for observing systematically (qualitative approaches). For example, the new definition does not include value-laden criteria, for example, for what is a ‘high or low’ CHL. This will allow and ideally encourage future studies to develop measures of CHL that account for contextual variation in the meaning and effectiveness of reflection and action. For current studies on CHL exploring the importance of reflection and action for health (e.g. Haugen et al. 2022 ), the new definition may provide additional theoretical support for their empirical measures. The interplay between reflection and action will present a key challenge for future research then—ideally addressed through mixed-methods approaches. Second, a focus on the social conditions of health allows empirical research on CHL to integrate (i.e. draw from and feedback into) established research fields such as the ‘SDOH’, ‘social class, capital and health’ theory, or ‘health lifestyles’ research. Third, the basic proposition that CHL includes yet goes beyond the individual to account for collective patterns in the acquisition and application of CHL requires that data should be collected on each societal level, ranging from individuals to families to communities and even countries (e.g. EU Health Literacy Survey). Similarly, interventions should lay a focus on the social conditions that facilitate CHL at all relevant levels. Together, these three points indicate how applying our new definition of CHL can assist and complement future empirical studies in developing new measures and producing knowledge relevant for interventions that aim to strengthen individual and collective agency to reduce social health inequalities.
CONCLUSIONS
Defining CHL based on reflection and action as its two constituent components can provide a focus for its application in research on health inequalities. Guidance from social theory can facilitate coherence in its definition and strengthen its application in empirical studies. Our definition and brief discussion may serve as a starting point for advancements needed to utilize and realize the full potential of CHL in future health promotion research and practice.
Acknowledgement
We thank Kristin Marie Bivens for her editorial guidance and support.
Contributor Information
Thomas Abel, Institute of Social and Preventive Medicine University of Bern, Bern, Switzerland.
Richard Benkert, Institute of Social and Preventive Medicine University of Bern, Bern, Switzerland.
- Abel, T. (2007) Cultural capital in health promotion. In McQueen, D. V. and Kickbusch, I. (eds), Health and Modernity: The Role of Theory in Health Promotion . Springer, New York, NY, pp. 43–73. [ Google Scholar ]
- Abel, T. (2008a) Measuring health literacy: moving towards a health-promotion perspective . International Journal of Public Health , 53 , 169–170. doi: 10.1007/s00038-008-0242-9. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Abel, T. (2008b) Cultural capital and social inequality in health . Journal of Epidemiology and Community Health , 62 , e13. doi: 10.1136/jech.2007.066159. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Abel, T. and Frohlich, K. L. (2012) Capitals and capabilities: linking structure and agency to reduce health inequalities . Social Science & Medicine , 74 , 236–244. [ PubMed ] [ Google Scholar ]
- Abel, T., Hofmann, K., Ackermann, S., Bucher, S. and Sakarya, S. (2015) Health literacy among young adults: a short survey tool for public health and health promotion research . Health Promotion International , 30 , 725–735. doi: 10.1093/heapro/dat096. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Adkins, N. and Corus, C. (2009) Health literacy for improved health outcomes: effective capital in the marketplace . Journal of Consumer Affairs , 43 , 199–222. [ Google Scholar ]
- Benkert, R. and Abel, T. (2022) Kritische Gesundheitskompetenz: Eine konstruktiv-kritische Bestandsaufnahme. In Rathmann, K., Dadaczynski K., Okan O. and Messer, M. (eds), Gesundheitskompetenz, Springer Reference Pflege – Therapie – Gesundheit . Springer, Berlin, Heidelberg, pp. 1–10. doi: 10.1007/978-3-662-62800-3_108-1. [ CrossRef ] [ Google Scholar ]
- Bourdieu, P. (1977a) Outline of a Theory of Practice . Cambridge University Press, Cambridge. [ Google Scholar ]
- Bourdieu, P. (1977b) Cultural reproduction and social reproduction. In Karabel, J. and Halsey, A. H. (eds), Power and Ideology in Education . Oxford University Press, New York, NY, pp. 487–511. [ Google Scholar ]
- Bourdieu, P. and Passeron, J. (1990) Reproduction in Education, Society and Culture , 2nd edn. Sage Publications, London. [ Google Scholar ]
- Bourdieu, P. and Wacquant, L. (1992) An Invitation to Reflexive Sociology . Polity Press, Oxford. [ Google Scholar ]
- Campbell, C. and MacPhail, C. (2002) Peer education, gender and the development of critical consciousness: participatory HIV prevention by South African youth . Social Science & Medicine , 55 , 331–345. [ PubMed ] [ Google Scholar ]
- Chinn, D. (2011) Critical health literacy: a review and critical analysis . Social Science & Medicine , 73 , 60–67. doi: 10.1016/j.socscimed.2011.04.004. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chinn, D. and McCarthy, C. (2013) All Aspects of Health Literacy Scale (AAHLS): developing a tool to measure functional, communicative and critical health literacy in primary healthcare settings . Patient Education and Counselling , 90 , 247–253. [ PubMed ] [ Google Scholar ]
- Cockerham, W. C. (2005) Health lifestyle theory and the convergence of agency and structure . Journal of Health and Social Behavior , 46 , 51–67. doi: 10.1177/002214650504600105. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cockerham, W. C., Rütten, A. and Abel, T. (1997). Conceptualizing contemporary health lifestyles: moving beyond Weber . Sociological Quarterly , 38 , 321–342. [ Google Scholar ]
- Collins, P. H. (2015) Intersectionality’s definitional dilemmas . Annual Review of Sociology , 41 , 1–20. doi: 10.1146/annurev-soc-073014-112142. [ CrossRef ] [ Google Scholar ]
- Crenshaw, K. (1991) Mapping the margins: intersectionality, identity politics, and violence against women of color . Stanford Law Review , 43 ( 6 ), 1241–79. doi: 10.2307/1229039. [ CrossRef ] [ Google Scholar ]
- Deshmukh, P. R., Dongre, A. R., Rajendran, K. and Kumar, S. (2015) Role of social, cultural and economic capitals in perceived quality of life among old age people in kerala, India . Indian Journal of Palliative Care , 21 ( 1 ), 39–44. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- De Clercq, B., Abel, T., Moor, I., Elgar, F. J., Lievens, J., Sioen, I.et al. (2017) Social inequality in adolescents’ healthy food intake: the interplay between economic, social and cultural capital . European Journal of Public Health , 27 ( 2 ), 279–286. [ PubMed ] [ Google Scholar ]
- de Wit, L., Fenenga, C., Giammarchi, C., di Furia, L., Hutter, I., de Winter, A.et al. (2017) Community-based initiatives improving critical health literacy: a systematic review and meta-synthesis of qualitative evidence . BMC Public Health , 18 ( 1 ), 40. doi: 10.1186/s12889-017-4570-7. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Diviani, N. (2019) On the centrality of information appraisal in health literacy research. Health Literacy Research and Practice , 3 ( 1 ), e21–e24. doi: 10.3928/24748307-20181214-01. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dubbin, L., Burke, N., Fleming, M., Thompson-Lastad, A., Napoles, T. M., Yen, I.et al. (2021) Social literacy: nurses’ contribution toward the co-production of self-management . Global Qualitative Nursing Research , 8 , 1–13. doi: 10.1177/2333393621993451. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Estacio, E. V. (2013) Health literacy and community empowerment: it is more than just reading, writing and counting . Journal of Health Psychology , 18 , 1056–1068. [ PubMed ] [ Google Scholar ]
- Freire, P. (1970) Pedagogy of the oppressed, translated by Myra Bergman Ramos. Continuum, New York, NY. [ Google Scholar ]
- Freire, P. (2005) Pedagogy of the Oppressed, 30th anniversary edition, translated by Myra Bergman Ramos. Continuum, New York, NY. [ Google Scholar ]
- Gagné, T., Ghenadenik, A. E., Abel, T. and Frohlich, K. L. (2018) Social inequalities in health information seeking among young adults in Montreal . Health Promotion International , 33 , 390–399. [ PubMed ] [ Google Scholar ]
- Gould, L., Mogford, E. and DeVoght, A. (2010) Successes and challenges of teaching the social determinants of health in secondary schools: case examples in Seattle, Washington . Health Promotion Practice , 11 , 26S–33S. [ PubMed ] [ Google Scholar ]
- Guzys, D., Kenny, A., Dickson-Swift, V. and Threlkeld, G. (2015) A critical review of population health literacy assessment . BMC Public Health , 15 , 215. doi: 10.1186/s12889-015-1551-6. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Haugen, A., Riiser, K., Esser-Noethlichs, M. and Hatlevik, O. E. (2022) Developing indicators to measure critical health literacy in the context of Norwegian lower secondary schools . International Journal of Environmental Research and Public Health , 19 , 3116. doi: 10.3390/ijerph19053116. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Huber, J. T., Shapiro, R. M. and Gillaspy, M. L. (2012) Top down versus bottom up: the social construction of the health literacy movement . The Library Quarterly , 82 , 429–451. doi: 10.1086/667438. [ CrossRef ] [ Google Scholar ]
- Ishikawa, H., Takeuchi, T. and Yano, E. (2008) Measuring functional, communicative, and critical health literacy among diabetic patients . Diabetes Care , 31 , 874–879. doi: 10.2337/dc07-1932. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jemal, A. (2017) Critical consciousness: a critique and critical analysis of the literature . Urban Review , 49 , 602–626. doi: 10.1007/s11256-017-0411-3. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jeong, B. G. and Veenstra, G. (2017) The intergenerational production of depression in South Korea: results from a cross-sectional study . International Journal for Equity in Health , 16 , 13. doi: 10.1186/s12939-016-0513-7. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Khawaja, M. and Mowafi, M. (2006) Cultural capital and self-rated health in low income women: evidence from the Urban Health Study, Beirut, Lebanon . Journal of Urban Health: Bulletin of the New York Academy of Medicine , 83 , 444–458. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kandt, J. (2018) Social practice, plural lifestyles and health inequalities in the United Kingdom . Sociology of Health and Illness , 40 , 1294–1311. doi: 10.1111/1467-9566.12780. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kickbusch, I. S. (2001) Health literacy: addressing the health and education divide . Health Promotion International , 16 , 289–297. doi: 10.1093/heapro/16.3.289. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- King, A. C., Odunitan-Wayas, F. A., Chaudhury, M., Rubio, M. A., Baiocchi, M., Kolbe-Alexander, T.et al. (2021) Community-based approaches to reducing health inequities and fostering environmental justice through global youth-engaged citizen science . International Journal of Environmental Research and Public Health , 18 , 892. doi: 10.3390/ijerph18030892. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Macintyre, S. (1997) The Black Report and beyond: what are the issues? Social Science & Medicine , 44 , 723–745. [ PubMed ] [ Google Scholar ]
- Matsumoto, M. and Nakayama, K. (2017) Development of the health literacy on social determinants of health questionnaire in Japanese adults . BMC Public Health , 17 , 30. doi: 10.1186/s12889-016-3971-3. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Missinne, S., Neels, K. and Bracke, P. (2014) Reconsidering inequalities in preventive health care: an application of cultural health capital theory and the life-course perspective to the take-up of mammography screening . Sociology of Health & Illness , 36 , 1259–1275. doi: 10.1111/1467-9566.12169. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mogford, E., Gould, L. and Devoght, A. (2011) Teaching critical health literacy in the US as a means to action on the social determinants of health . Health Promotion International , 26 , 4–13. doi: 10.1093/heapro/daq049. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nutbeam, D. (2000) Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st Century . Health Promotion International , 15 , 259–267. doi: 10.1093/heapro/15.3.259. [ CrossRef ] [ Google Scholar ]
- Nutbeam, D. (2009) Defining and measuring health literacy: what can we learn from literacy studies? International Journal of Public Health , 54 , 303–305. doi: 10.1007/s00038-009-0050-x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Osborne, R. H., Batterham, R. W., Elsworth, G. R., Hawkins, M. and Buchbinder, R. (2013) The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ) . BMC Public Health , 13 , 658. doi: 10.1186/1471-2458-13-658 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Oude Groeniger, J., de Koster, W., van der Waal, J., Mackenbach, J. P., Kamphuis, C. and van Lenthe, F. J. (2020) How does cultural capital keep you thin? Exploring unique aspects of cultural class that link social advantage to lower body mass index . Sociology of Health & Illness , 42 , 1497–1515. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Paccoud, I., Nazroo, J. and Leist, A. (2020) A Bourdieusian approach to class-related inequalities: the role of capitals and capital structure in the utilisation of healthcare services in later life . Sociology of Health & Illness , 42 , 510–525. doi: 10.1111/1467-9566.13028. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pinheiro, P. (2021) Conceptualizations of health literacy: past developments, current trends, and possible ways forward toward social practice . Health Literacy Research and Practice , 5 , e91–e95. doi: 10.3928/24748307-20210316-01. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pithara, C. (2020) Re-thinking health literacy: using a capabilities approach perspective towards realising social justice goals . Global Health Promotion , 27 , 150–158. doi: 10.1177/1757975919878151. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Prilleltensky, I. (1989) Psychology and the status quo . American Psychologist , 44 , 795–802. doi: 10.1037/0003-066x.44.5.795. [ CrossRef ] [ Google Scholar ]
- Rasmussen, A. N., Guise, A. and Overgaard, C. (2021) Understanding social inequalities in cardiac treatment through the lens of cultural health capital: a study of Danish socially disadvantaged ischemic heart patients’ lived experiences of healthcare interactions. Social Theory & Health (in press). doi: 10.1057/s41285-021-00173-1. [ CrossRef ] [ Google Scholar ]
- Renwick, K. (2017) Critical health literacy in 3D . Frontiers in Education , 2 , 40. doi: 10.3389/feduc.2017.00040. [ CrossRef ] [ Google Scholar ]
- Robeyns, I. (2005) The capability approach: a theoretical survey . Journal of Human Development , 6 , 93–117. [ Google Scholar ]
- Rubinelli, S., Schulz, P. J. and Nakamoto, K. (2009) Health literacy beyond knowledge and behaviour: letting the patient be a patient . International Journal of Public Health , 54 , 307–311. [ PubMed ] [ Google Scholar ]
- Schori, D., Hofmann, K. and Abel, T. (2014) Social inequality and smoking in young Swiss men: intergenerational transmission of cultural capital and health orientation . International Journal of Public Health , 59 , 261–270. doi: 10.1007/s00038-013-0537-3. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sen, A. (1985) Commodities and Capabilities . Elsevier Science Publishers, Amsterdam. [ Google Scholar ]
- Sen, A. (1993) Capability and well-being. In Nussbaum, M. and Sen, A. (eds), The Quality of Life . Clarendon Press, Oxford, pp. 30–53. [ Google Scholar ]
- Shannon, H. A. and Parker, A. W. (2020) Evaluation of a health literacy instrument designed for the mining industry . Health Literacy Research and Practice , 4 , e84–e93. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Shim, J. K. (2010) Cultural health capital: a theoretical approach to understanding health care interactions and the dynamics of unequal treatment . Journal of Health and Social Behavior , 51 , 1–15. doi: 10.1177/0022146509361185. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sykes, S. and Wills, J. (2018) Challenges and opportunities in building critical health literacy . Global Health Promotion , 25 , 48–56. doi: 10.1177/1757975918789352. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sykes, S. and Wills, J. (2019) Critical health literacy for the marginalised: empirical findings. In Orkan, O., Ullrich, B., Levin-Zamir, D., Pinheiro, P. and Sørensen, K (eds), International Handbook of Health Literacy: Research, Practice and Policy Across the Lifespan . Policy Press, Bristol, pp. 167–182. [ Google Scholar ]
- Sykes, S., Wills, J., Rowlands, G. and Popple, K. (2013) Understanding critical health literacy: a concept analysis . BMC Public Health , 13 :150. doi: 10.1186/1471-2458-13-150. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Veenstra, G. (2007) Social space, social class and Bourdieu: health inequalities in British Columbia, Canada . Health & Place , 13 , 14–31. doi: 10.1016/j.healthplace.2005.09.011. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Veenstra, G. (2018) Infusing fundamental cause theory with features of Bourdieu’s theory of symbolic power . Scandinavian Journal of Public Health , 46 , 49–52. doi: 10.1177/1403494817748253. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Veenstra, G. and Abel, T. (2019) Capital interplays and social inequalities in health . Scandinavian Journal of Public Health , 47 , 631–634. doi: 10.1177/1403494818824436. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Williams, S. J. (1995) Theorising class, health and lifestyles: can Bourdieu help us? Sociology of Health & Illness , 17 , 577–604. [ Google Scholar ]
- Research article
- Open access
- Published: 29 December 2018
Evidence on the effectiveness of health literacy interventions in the EU: a systematic review
- Boudewijn B. Visscher 1 ,
- Bas Steunenberg 1 ,
- Monique Heijmans 2 ,
- Jolien M. Hofstede 2 ,
- Walter Devillé 2 , 3 ,
- Iris van der Heide 2 &
- Jany Rademakers 2 , 4
BMC Public Health volume 18 , Article number: 1414 ( 2018 ) Cite this article
26k Accesses
157 Citations
45 Altmetric
Metrics details
In the last decade, the attention for health literacy has increased in the European Union. This is due to three main reasons. First, reviews have shown that inadequate health literacy is associated with worse health outcomes, higher health care use and expenditure. Second, in all European countries the population is aging and the number of chronically ill people is rising. Improving health literacy in this group can offer greater opportunities to take an active part in society, be independent and improve quality of life. Third, since most research on health literacy has been conducted outside Europe and relatively little is known about the development of health literacy interventions and its effects on outcome measures in European countries. The aim of this systematic review was to assess the evidence on the effectiveness of health literacy interventions in the European Union published between 1995 and 2018.
Searches have been performed in Medline, PubMed, EMBASE, CINAHL, Cochrane library, PsychINFO, ERIC, Web of Science and SCOPUS for publications on health literacy intervention studies in European Union countries. Studies were included if the research was conducted in one or more Member States of the European Union, the publication described an intervention study, the intervention was aimed at health literacy, the publication described an outcome measure related to health literacy and the publication was written in English, French or German.
A total of 23 studies were included. Three types of interventions were identified; aimed at improving health literacy, tailored to different health literacy levels and aimed at improving health outcomes in general that differentiated in effects for people with different health literacy levels. Most interventions identified in the review focus on the functional level of health literacy or numeracy. The strength of evidence from the European health literacy intervention studies was low and there was a huge heterogeneity in study design, measurement tools and outcomes measured.
Conclusions
Promising interventions were tailored to the needs of patients, addressing functional, interactive and critical skills and use not difficult animated spoken text. Future research should focus on the development and assessment of such interventions and use stronger designs.
Peer Review reports
Health literacy is a topic of growing importance in European public health research. In general, health literacy is ‘linked to literacy and encompasses people’s knowledge, motivation and competences to access, understand, appraise, and apply health information in order to make judgments and take decisions in everyday life concerning healthcare, disease prevention and health promotion to maintain or improve quality of life during the life course.’ This is the definition of health literacy as it was developed in the European Health Literacy Project (HLS-EU) [ 1 , 2 ]. This definition includes the public health perspective on health literacy and can also be specified to an individual approach.
Apart from this one, there are many different definitions and conceptualisations of health literacy [ 2 ]. Narrow definitions focus on basic literacy (the ability to read and write), while others also include a wider range of cognitive and psychosocial skills in the definition. Furthermore, definitions differ with respect to the actions, information and resources, objectives, context and time aspects which they do or do not include [ 2 ]. Nutbeam et al. [ 3 ] distinguishes in the broad definition of health literacy three dimensions of health literacy: functional, interactive and critical literacy. Functional health literacy is the ability to read health information. Sometimes numeracy (the ability to use mathematics in everyday life) is also included in the concept of functional health literacy. Interactive health literacy refers to ‘more advanced cognitive and literacy skills which, together with social skills, can be used to actively participate in everyday situations, extract information and derive meaning from different forms of communication, and apply this to changing circumstances.’ [ 3 ] Critical health literacy refers to ‘more advanced cognitive skills which, together with social skills, can be applied to critically analyse information and use this to exert greater control over life events and situations’. [ 3 ] Most of existing research on health literacy focusses on functional health literacy.
Especially in the last decade, the attention for health literacy has increased in the European Union (EU). This is due to three main reasons. First, studies mainly from the United States of America (USA) have shown that inadequate health literacy is associated with worse health outcomes, poor preventive care behaviours, higher health care service use and expenditures. In addition these studies showed that health literacy influences the effects social determinants of health have on health status and as such is an important determinant of health inequalities [ 4 , 5 , 6 , 7 , 8 ]. Therefore more attention for health literacy can lead to a substantial return at both the individual and the community level, by improving health and well-being on one hand and reducing unnecessary healthcare visits and costs on the other. Second, in all European countries the population is aging and the number of chronically ill people is rising. Much is expected from this group in terms of self-management. However, adequate health literacy is required to fulfil an active role regarding health and healthcare. Third, most research on health literacy has been conducted outside Europe, in the USA and more recently in Japan, Taiwan and Australia. As a consequence, relatively little is known about the development of health literacy interventions and its effects on outcome measures in European countries. While many of the USA studies on health literacy primarily focus on functional health literacy in the clinical or medical setting, EU studies more often use a broader definition of health literacy, and address issues both inside and outside the clinical setting [ 9 ]. Instead of a risk (inadequacy in the context of healthcare), health literacy is also defined as an asset, a means to exert greater control over health and over personal, social and environmental determinants of health [ 2 , 3 , 9 ]. Furthermore, the health and social welfare systems between USA and Europe differ. The USA health systems have a limited government involvement with an important role for the private sector stakeholders (e.g. health care providers and insurers) and most of the payment is on fee for service basis [ 10 ]. In Europe there is a stronger government involvement than in the USA. In some countries (e.g. the Netherlands) there is a gatekeeping role for the primary care and paying on capitation basis, and in other countries (e.g. the UK) there is a system of National Health Service which offers (predominantly) free health care services [ 10 , 11 ]. These fundamental differences between the USA and Europe areas an important reason why the largely USA based body of evidence cannot simply be assumed to also be true in a European setting. In the USA, Sheridan et al. [ 12 ] and Berkman et al. [ 13 ]. Sheridan et al. [ 12 ] and Berkman et al. [ 13 ] found interventions that improved participants´ comprehension of health information. Moreover, interventions aimed at self-management that took the level of health literacy of patients into account reduced emergency department visits and hospitalizations and self- and disease-management interventions reduced disease severity. Effects of health literacy interventions on other outcomes were mixed or limited. Most studies in the field of health literacy are correlational, there is a lack of convincing studies that show that health literacy can change as a result of an intervention.
To determine the efficacy of health literacy interventions in the EU context, a similar systematic review as the review conducted by Berkman et al. [ 13 ] and Dennis et al. [ 14 ] in the USA was undertaken for EU countries, using similar search strategies for optimal comparability of the results. The aim of this systematic review is to assess the evidence on the effectiveness of health literacy interventions in the EU published from 1995 until 2018. This is the first systematic review on health literacy interventions in the EU context. The results of this review will be compared to the results of the review in the USA context.
This systematic review was conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [ 15 ]. This research is based on and an update of the work done in Work Package 1 of the HEALIT4EU research project, executed under the EU Health Programme (2008–13) in the framework of contract no. 20146201 with the Consumers, Health and Food Executive Agency (Chafea) acting under the mandate of the European Commission. The content of this article represents the views of the contractor (the EPHORT consortium) and is its sole responsibility; it can in no way be taken to reflect the views of the European Commission and/or Chafea or any other body of the European Union. The full HEALIT4EU report is available via https://ec.europa.eu/health/sites/health/files/health_policies/docs/2015_health_literacy_en.pdf .
Search methods for identification of studies
Studies were identified by searching Medline, PubMed, EMBASE, CINAHL, the Cochrane library, PsychINFO, ERIC, Web of Science and SCOPUS. English, French and German language publications on health literacy intervention studies in EU countries. According to our knowledge, no research on health literacy has been done before 1995, therefore studies from January 1995 to Augusts 2018 were included. Recent reviews on health literacy that developed search strategies based on a list of key words and text words for use in the different databases were used to construct our own search strategy. For the search strategy, the reviews of Berkman et al. [ 13 ] and Dennis et al. [ 14 ] were combined into a new search strategy (see Additional file 1 ). Contrary to most other search strategies, this search strategy for health literacy publications explicitly included ‘functional health literacy’, ‘interactive health literacy’ and ‘critical health literacy’ [ 3 ]. As in Berkman et al. [ 13 ] we also used the terms ‘literacy’, ‘literate’, ‘reading skills’, ‘writing skills’ etc.). This led to 2515 publications in PubMed and Embase alone. All these abstracts were screened by two researchers but it turned out that the majority of these publications did not address health literacy (or health related issues) at all. Therefore we limited the search terms for health literacy by leaving out the terms of general literacy, reading and writing skills and dyslexia. The terms used in our search strategies to find ‘interventions studies’ were the same search terms as used by Dennis et al. [ 14 ].
Types of studies
All studies that describe an intervention study with one of the following designs were included: randomized controlled trials, quasi randomized controlled trials, controlled before and after studies or interrupted time series. Studies with no original data, studies with only case report and studies with only ecological data were excluded.
Studies involving people living in one or more member states of the EU were included. The Member States of the EU are Austria, Belgium, Bulgaria, Croatia, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Poland, Portugal, Romania, Slovakia, Slovenia, Spain, Sweden and the United Kingdom.
Types of interventions
Studies with an intervention that focused on health literacy were included. Interventions at population level, as well as interventions on specific populations and individual level were searched for and included. Studies on the basic experimental science of reading ability were excluded as were studies examining normal reading development in children and studies about dyslexia. Contrary to the strategy of Berkman et al. [ 11 ], the search was not limited to publications mentioning the use of a health literacy measurement tool, because the way health literacy in Europe was measured differed from the way described in reviews with predominantly American studies (where validated health literacy instruments are used more often).
Types of outcome measures
Studies that described an outcome measure related to health literacy were included. These outcome measure included among others: knowledge, skills, attitudes, self-efficacy, stages of change, motivation and patient activation, behaviour change, health care access, service use, health status, costs of care.
Data collection and analysis
The study selection consisted of two phases: first the selection on title and/or abstract and second the selection of the remaining articles based on full text. The search results were screened by two researchers each in two independent phases (JH, MH (1995–2014); BV, BS (2015–2018)). Consensus meetings were held with the researchers of both phases to resolve disagreements. A 20% sample of the excluded scientific publications was screened by a third researcher (JR 1995–2018). Studies were included if they met the inclusion criteria.
The abstracts were systematically screened on the basis of our in- and exclusion criteria. In case a publication did not meet a criterion, the publication was excluded and the next publication was screened. Of all the studies, fulfilling the inclusion criteria, full texts were read. For the inclusion of full texts the same in- and exclusion criteria were used. To assess the quality of the studies the “Quality Assessment Tool For Quantitative Studies” developed by the Effective Public Health Practice Project (EPHPP) [ 16 ] was used. The criteria for quality in this tool include selection bias, study design, confounders, blinding, data collection methods, withdrawals, intervention integrity and data analysis. The gl obal rating is calculated using information across all six domains (selection bias, study design, confounders, blinding, data collection methods & withdrawals and drop-outs): strong (no weak ratings), moderate (one weak rating), or weak (two or more weak ratings) .
Our literature search yielded 6206 publications between 1995 and mid-2018. Of these publications 6042 (97%) were excluded based on title and abstract because they did not fulfil one or more of the inclusion criteria: 3950 (65%) were excluded because not describing an intervention, 1037 (17%) did not meet the first criterion (being conducted in one or more of the European Member States), 1024 (17%) of the European interventions were excluded because they were not focusing on health literacy and 26 (1%) of the studies were excluded because there was no health literacy outcome measure (see also Fig. 1 , PRISMA diagram). The remaining 164 publications were retrieved in full text for further assessment, of which 141 failed to meet the inclusion criteria. The main reason for excluding full texts was that they were unrelated to health literacy. Finally, 23 articles were included.
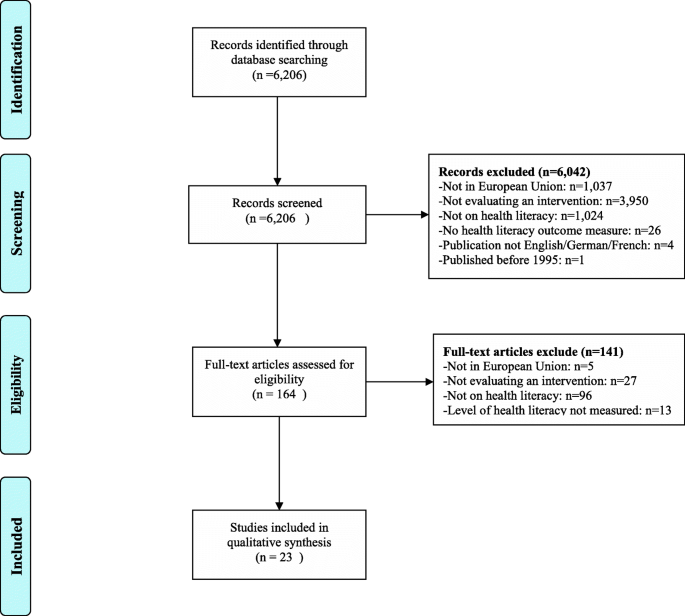
PRISMA diagram
Principal findings
There were not a sufficient number of studies with similar outcome measures or similar interventions to consider quantitative analysis (meta-analysis or statistical pooling) of data; therefore a qualitative analysis was performed. The 23 included intervention studies and their characteristics are summarized in Table 1 . The references, the evidence tables, the intervention type and outcome of each of these studies can be found in Table 2 . All studies were conducted in North-western Europe, no studies from Eastern and Southern European countries were found. All studies except one [ 17 ] were interventions developed for adults.
Health literacy measure
Studies varied considerably in their measurement of health literacy. Commonly used instruments in the USA to assess health literacy such as the Raped Estimate of Adult Literacy in Medicine (REALM) [ 18 , 19 ], the Newest Vital Sign (NVS) [ 20 ], Test Of Functional Health Literacy in Adults (TOFHLA) [ 21 , 22 , 23 ], and the Short Assessment of Health Literacy (SAHL) [ 23 , 24 ] were used in eight studies. All these measures focus on functional health literacy. Four other studies also focused on functional health literacy skills by assessing reading ability [ 25 , 26 ] or the level of mild intellectual disability [ 27 ]. Three studies measured critical health literacy skills by questionnaire [ 28 ] or interview [ 29 ] or assessing skills towards decision-making [ 30 ]. The study by Webb et al. [ 31 ] focussed on functional and interactive health literacy skills by measuring health literacy as the level of verbal and cognitive abilities. Three studies measured health literacy by the level of disease-specific knowledge [ 20 , 32 , 33 ]. One study measured health literacy by the Brief questions to identify inadequate health literacy [ 34 ]. In one study the way health literacy was measured was not specified [ 31 ]. Numeracy was assessed in four studies [ 35 , 36 , 37 , 38 ].
Type of intervention
There was also a huge variation in the type of interventions given: group interventions, individual interventions, web-based interventions, one component interventions (e.g. an information leaflet) and multi-component interventions including chat-groups, lectures, training sessions, a help-desk, computer programs and leaflets among others. Most interventions were web-based interventions ( n = 9). The web-based interventions were conducted during the most recent years, most of them ( n = 7) in 2015, 2016 and 2017. In only one study it was explicitly mentioned that the patients were involved in the development of the intervention on a module designed for the development of a decision aid about MS-immunotherapy [ 38 ].
Study design
Five studies used a Randomised Clinical Trial (RCT) design [ 19 , 23 , 26 , 27 , 34 ] and five studies a Controlled Clinical Trial (CCT) design [ 18 , 21 , 24 , 25 , 33 ]. In two studies two groups were compared pre- and post-test (Cohort analytic design) [ 17 , 28 ], but most studies ( n = 9) used the same group that was pretested and post-tested immediately after the intervention (Cohort study). The study by White et al. [ 31 ] used an interrupted time series design and there was one observational study. The type of design in combination with the frequent missing or nor reported use of covariates makes that for most studies ( n = 15) the quality was rated as weak (EPHPP [ 16 ], Table 2 ). The quality of seven studies was rated as moderate on the base of the EPHPP [ 16 ] assessment tool and one study was judged as strong.

Types of intervention studies
The types of interventions in the 23 studies could be categorized as follows;
Interventions aimed at improving (aspects of) the health literacy level of individuals.
Interventions that were specifically tailored to different health literacy levels.
General interventions that aimed at improving health outcomes, which described the specific effects for patients with different health literacy or numeracy levels.
Interventions aimed at improving (aspects of) health literacy
A group training of 2 × 2,5 days in evidence based-medicine for patients, patient counsellors, consumer representatives and healthcare professionals resulted in a significant increase in health related knowledge and in the level of critical health literacy of the participants [ 29 ]. In the evaluation of the training they stated that they had broadened their knowledge, were more critical in handling health information and considered themselves more confident on making the right decisions on the basis of the information they found. The content of the training was tailored to the needs of the participants. A second group intervention [ 39 ] specifically focused on so-called ‘hard to reach’ groups (e.g. unemployed women of minority groups and female migrants from Islamic backgrounds). This intervention combined different elements: computer courses, lectures, and language training. Topics related to health and well-being were being discussed. Also this intervention led to an increase in knowledge and comprehensive health literacy. Another group intervention targeted patients with mild intellectual disabilities and was tailored to their verbal and cognitive abilities. In the training, patients were taught how and when to access healthcare [ 22 ]. The evaluation showed that the intervention had a significant positive effect on the participants’ ability to recognize disease symptoms, identify illnesses and choose appropriate courses for action.
An intervention that was developed to improve self-care among diabetes patients was evaluated after two years. The patients had received tailored tele-carer education as well as support to change specific lifestyle behaviours [ 30 ]. The evaluation showed that these diabetes patients were better able to use knowledge in their day-to-day self-care and expressed a greater control over their self-care decision-making. A UK community study that evaluated the impact of a self-care skills training initially (after 6 months) found a positive effect on decision making skills regarding use of health services (critical health literacy). However, after 12 months the effect was no longer found [ 31 ]. In three studies in Denmark, the tele-homecare intervention 'Telekit' was evaluated. The Telekit focuses on the management of COPD in general, how to manage COPD during exacerbations and collect date on the current state of the patient’s health. Both studies did not found a significant difference on functional health literacy [ 21 , 22 , 23 ]. The Telekit increases the feeling of insecurity, greater freedom, more control and greater awareness of symptoms [ 22 ].
Five interventions specifically focused on the improvement of numeracy skills, i.e. the ability to understand numerical risk information [ 18 , 21 , 35 , 36 , 37 ]. The evaluations of these interventions had similar conclusions. In general numerical information is presented in ways too difficult for people with low competencies. Another way of presenting (e.g. by using visual aids and/or lowering the level of detail of information) led to improved understanding in participants with low numeracy competencies.
Interventions tailored to different health literacy levels
Three studies [ 17 , 27 , 28 ] performed an evaluation with an intervention and a control group, comparing the outcome variables. In one study among children with diabetes (age 8–12) the impact of a personalized robot on diabetes knowledge and motivation for self-management was compared to a neutral robot. The reactions of the personalized robot were adjusted to the knowledge level of the child. In the evaluation, children in the intervention group (with the personalized robot) scored higher on diabetes knowledge and motivation for self-management. A tailored training programme on peritoneal dialysis for renal patients with low health literacy resulted in lower incidence of peritonitis and stronger feelings of control and ownership over treatment among the participants in the intervention group, as well as less supervision time needed of nurses [ 28 ]. The intervention comprised lowering the amount of written information and using more verbal material, and reducing the use of medical jargon. A computer-tailored intervention for smoking-cessation (booklet and web-based programme) was compared to a general self-help booklet. The tailored approach led to more attempts to quit smoking as well as higher abstinence rates, specifically for participants with lower literacy levels [ 27 ]. An intervention that was tailored to the verbal and cognitive abilities of patients with mild intellectual disabilities was evaluated in a one group pre/post-test design [ 32 ]. The evaluation showed there was an improvement in symptom recognition, better health-related decision making, improved understanding of medical procedures and a better ability in formulating personal health goals.
Three studies focused on the way of presenting information to persons with different health literacy levels [ 24 , 25 , 34 ]. One study varied in presenting information on spoken versus written text and illustration versus animation. In almost all conditions, the high health literate persons had a better recall on information compared to the low health literate persons, except for the spoken animations. In the spoken animation condition, the low health literate persons recalled the same amount of information as the high literate persons. The other study varied in presenting information on illustrated versus text-only and in not difficult versus difficult texts. Persons with low and high health literacy recalled the not difficult information better than difficult information. Illustrated text improved the recall and attitudes in low health literate persons and had no effect in high health literate persons. Another study stated audio-visual leads to better knowledge. The study also stated that clear, person-based intervention development is more important than interactivity and audio-visual presentation to improve health literacy outcomes.
General interventions that aimed at improving health outcomes, which described the specific effects for patients with different health literacy or numeracy levels
In general, patients with low health literacy benefit less from general interventions compared to patients with higher levels of literacy, e.g. with respect to understanding medication labels [ 18 , 35 ] and other health messages [ 19 , 20 ]. In a study on the knowledge level of rheumatoid arthritis patients after being exposed to a pictorial ‘mind map’ together with a arthritis campaign booklet, analysis showed that less literate participants gained fewer knowledge from both the booklet alone and the booklet in combination with the mind map, compared to high literate patients [ 19 ]. Similarly, a leaflet was developed to improve gynaecological cancer symptom awareness and to reduce barriers to access medical services [ 20 ]. Though in general after reading the leaflet awareness improved and barriers to access medical services were reduced, these effects were less in patients with lower health literacy. In general, patients with low levels of health literacy were found to experience more barriers to access health care services
Four studies reported on outcomes relevant for the daily management of chronic illness or health in general such as knowledge, empowerment, ability to self-manage, decision-making skills, ability to taken an active role in treatment. Increased levels of health literacy were associated with higher levels of empowerment, better decision-making skills, and a more active role in treatment [ 29 , 30 , 31 , 32 ]. The evidence were graded as weak due to the fact that results mainly came from uncontrolled studies and results were often based on small groups or a limited number of observations. One study focused on a mobile phone app intervention targeting fruit and vegetable consumption. The information provided via the app where either textual or auditory tailored to the person’s characteristics. The app increased the fruit and vegetable intake, but only in persons with high health literacy [ 26 ].
In this systematic review the evidence on the effectiveness of health literacy interventions in the EU published from 1995 until mid-2018 was assessed. There were not a sufficient number of studies with similar outcome measures or similar interventions to consider quantitative analysis (meta-analysis or statistical pooling) of data; therefore a qualitative analysis was performed. The evidence collected gives insight into the gaps in research in the context of the European Union, compared to the evidence presented in the already published reviews outside Europe, and provide recommendations for research. To our knowledge, this is the first systematic review on health literacy interventions in the EU context. The results of this review are compared to the results of reviews in the USA context.
In total, 23 intervention studies were identified. The interventions described in these studies either (a) aimed at improving (aspects of) health literacy, (b) were specifically tailored to different health literacy levels or (c) were general interventions that aimed at improving health outcomes, which described the specific effects for patients with different health literacy or numeracy levels. As was found in other review studies [ 13 , 14 , 40 ] most interventions focus on functional health literacy, fewer (also) target interactive or critical health literacy.
The studies varied with respect to their study design, measurement instruments and outcomes. Health literacy was also operationalized and measured differently, thus impeding comparability of the results. Most studies did not give information whether their study results were stratified across health literacy levels. This was also concluded in the review of D ‘Eath et al. [ 40 ]. As a result of this, it is not possible to measure the impact of interventions on people with varying levels of health literacy. The quality of most studies was weak (15) or moderate (7). Only one was rated as strong. The number of RCT’s or controlled studies was limited.
Because of the low quality of the studies no firm conclusions can be drawn with respect to the effective components of health literacy interventions. It seems that the type of intervention (e.g. group, individual, community based) is not of major importance. However, three factors are likely to be distinctive of promising interventions: (1) they tailor their activities to the needs of the (low health literate) participants, (2) they also address interactive and/or critical skills (instead of knowledge only) and (3) they present the information in an appropriate way, i.e. not difficult and using animated spoken text. Studies that also focus on interactive and/or critical skills led to improvements in outcomes such as motivation, knowledge, empowerment and self-confidence. These findings are congruent with those from the review by Berkman et al. [ 13 ]. Interventions that present the information in an appropriate way results in better recall, positive attitudes and more informed decision making [ 24 , 25 , 34 ].
Despite the small number of studies, findings from the EU are in line with the results from other international reviews [ 6 , 7 , 8 , 13 , 14 , 40 ]. Most interventions in this review focus on functional level of health literacy, these results were also found in the other USA reviews [ 6 , 7 , 13 , 14 , 40 ]. In our review we found that not all studies identified whether the study results were stratified across health literacy levels. These results were also found by the USA review [ 40 ]. Similar to the review of Berkman et al. [ 13 ] we identified that increased levels of health literacy were associated with higher levels of empowerment, better decision making skills, and a more active role in treatment. In our review, the quality of most of the studies were rated as low. In contrast to our included studies, the quality of most of the included studies of the USA reviews [ 6 , 7 , 8 , 13 , 14 , 40 ] were rated as moderate/fair and high/good.
There are definitely considerable gaps in the research evidence concerning which interventions are most effective in improving health literacy or health literacy related outcomes in Europe. In order to be able to draw firm conclusions, there should be more agreement among researchers about the definition of health literacy, and more systematic use of validated measurement tools in interventions as a “golden standard”. In the past years several studies on the development, translation and validation of (both subjective and objective) health literacy measurement instruments have been done. As a consequence, the assessment of health literacy varies depending on the setting and scope of the health literacy definition. The results of future intervention research then become more comparable and generalizable, leading to a more rapid insight in what constitutes effective health literacy interventions in the EU context.
New developed interventions should be tailored to the needs of the patients; address functional, critical and interactive skills and the way of presenting should be not difficult animated spoken text. Web-based interventions might be suitable for patients that have digital skills, but also blended interventions (combining face-to-face with online activities) and other types of interventions might integrate these three factors in their design. Future research should focus on the assessment of such interventions and use stronger designs e.g. in well-reported, large-sampled randomized controlled trials.
Abbreviations
Effective Public Health Practice Project
European Union
European Health Literacy Project
Preferred Reporting Items for Systematic Reviews and Meta Analyses
United States of America
European Commission: Together for health: a strategic approach for the EU 2008-2013. Com (2007) 630 final. 2007.
Sorensen, K., Van den Broucke, S., Fullam, J., Doyle, G., Pelikan, J., Slonska, Z., & Brand H. (HLS-EU) Consortium Health Literacy Project European. (2012). Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health, 12, 80–2458-12-80. doi: https://doi.org/10.1186/1471-2458-12-80 .
Nutbeam D. Health literacy as a public goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. 2000;15(3):259–67. https://doi.org/10.1093/heapro/15.3.259 .
Article Google Scholar
Rasu RS, Bawa WA, Suminski R, Snella K, Warady B. Health literacy impact on national healthcare utilization and expenditure. Int J Health Policy Manag. 2015;4(11):747–55. https://doi.org/10.15171/ijhpm.2015.151 .
Article PubMed PubMed Central Google Scholar
WHO Commission on the Social Determinants of Health. Achieving health equity: from root causes to fair outcomes. Geneva: World Health Organisation; 2007.
Google Scholar
DeWalt DA, Hink A. Health literacy and child health outcomes: a systematic review of the literature. Pediatrics. 2009;124(Suppl 3):S265–74. https://doi.org/10.1542/peds.2009-1162B .
Article PubMed Google Scholar
Mantwill S, Monestel-Umana S, Schulz PJ. The relationship between health literacy and health disparities: a systematic review. PLoS One. 2015;10(12):e0145455. https://doi.org/10.1371/journal.pone.0145455 .
Article CAS PubMed PubMed Central Google Scholar
Sanders LM, Federico S, Klass P, Abrams MA, Dreyer B. Literacy and child health: a systematic review. Archives of Pediatrics & Adolescent Medicine. 2009;163(2):131–40. https://doi.org/10.1001/archpediatrics.2008.539 .
Nutbeam D. The evolving concept of health literacy. Soc Sci Med. 2008;67(12):2072–8. https://doi.org/10.1016/j.socscimed.2008.09.050 .
Rice T, Rosenau P, Unruh LY, Barnes AJ, Saltman RB, van Ginneken E. United States of America: health system review. Health Syst Transit. 2013;15(3):1–431.
PubMed Google Scholar
Loewenson R, Simpson S. Strengthening integrated care through population-focused primary care services: international experiences outside the United States. Annu Rev Public Health. 2017;38:413–29. https://doi.org/10.1146/annurev-publhealth-031816-044518 .
Sheridan SL, Halpern DJ, Viera AJ, Berkman ND, Donahue KE, Crotty K. Interventions for individuals with low health literacy: a systematic review. J Health Commun. 2011;16(Suppl 3):30–54. https://doi.org/10.1080/10810730.2011.604391 .
Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Viera A, Crotty K, et al. Health literacy interventions and outcomes: An updated systematic review. Evid Rep Technol Assess. 2011;(199):1–941.
Dennis, S., Williams, A., Taggart, J., Newall, A., Denney-Wilson, E., Zwar, N., . . . Harris, M. F. (2012). Which providers can bridge the health literacy gap in lifestyle risk factor modification education: A systematic review and narrative synthesis. BMC Fam Pract, 13:44. doi: https://doi.org/10.1186/1471-2296-13-44 .
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int J Surgery. 2010;8(5):336–41. https://doi.org/10.1016/j.ijsu.2010.02.007 .
Effective Public Health Practice Project (EPHPP). (2009). Quality assessment tool for quantitative studies. https://www.nccmt.ca/knowledge-repositories/search/14 . Accessed 23 Mar 2017.
Blanson Henkemans OA, Bierman BP, Janssen J, Neerincx MA, Looije R, van der Bosch H, van der Giessen JA. Using a robot to personalise health education for children with diabetes type 1: a pilot study. Patient Educ Couns. 2013;92(2):174–81. https://doi.org/10.1016/j.pec.2013.04.012 .
Sahm LJ, Wolf MS, Curtis LM, Behan R, Brennan M, Gallwey H, Mc Carthy S. What's in a label? An exploratory study of patient-centered drug instructions. Eur J Clin Pharmacol. 2012;68(5):777–82. https://doi.org/10.1007/s00228-011-1169-2 .
Walker D, Adebajo A, Heslop P, Hill J, Firth J, Bishop P, Helliwell PS. Patient education in rheumatoid arthritis: the effectiveness of the ARC booklet and the mind map. Rheumatology (Oxford). 2007;46(10):1593–6.
Article CAS Google Scholar
Boxell EM, Smith SG, Morris M, Kummer S, Rowlands G, Waller J, et al. Increasing awareness of gynecological cancer symptoms and reducing barriers to medical help seeking: does health literacy play a role? J Health Commun. 2012;17(Suppl 3):265–79. https://doi.org/10.1080/10810730.2012.712617 .
Korsbakke Emtekaer Haesum L, Ehlers L, Hejlesen OK. Interaction between functional health literacy and telehomecare: Short-term effects from a randomized trial. Nurs Health Sci. 2016;18(3):328–33. https://doi.org/10.1111/nhs.12272 .
Lilholt PH, Haesum LK, Ehlers LH, Hejlesen OK. Specific technological communication skills and functional health literacy have no influence on self-reported benefits from enrollment in the TeleCare north trial. Int J Med Inform. 2016;91:60–6. https://doi.org/10.1016/j.ijmedinf.2016.04.010 .
Haesum LKE, Ehlers LH, Hejlesen OK. The long-term effects of using telehomecare technology on functional health literacy: results from a randomized trial. Public Health. 2017;150:43–50 doi:S0033-3506(17)30175-0.
Meppelink CS, Smit EG, Buurman BM, van Weert JC. Should we be afraid of simple messages? The effects of text difficulty and illustrations in people with low or high health literacy. Health Commun. 2015;30(12):1181–9. https://doi.org/10.1080/10410236.2015.1037425 .
Meppelink CS, van Weert JC, Haven CJ, Smit EG. The effectiveness of health animations in audiences with different health literacy levels: an experimental study. J Med Internet Res. 2015;17(1):e11. https://doi.org/10.2196/jmir.3979 .
Elbert SP, Dijkstra A, Oenema A. A mobile phone app intervention targeting fruit and vegetable consumption: the efficacy of textual and auditory tailored health information tested in a randomized controlled trial. J Med Internet Res. 2016;18(6):e147. https://doi.org/10.2196/jmir.5056 .
Gilbert HM, Leurent B, Sutton S, Alexis-Garsee C, Morris RW, Nazareth I. ESCAPE: a randomised controlled trial of computer-tailored smoking cessation advice in primary care. Addiction. 2013;108(4):811–9. https://doi.org/10.1111/add.12005 .
Neville A, Jenkins J, Williams JD, Craig KJ. Peritoneal dialysis training: a multisensory approach. Perit Dial Int. 2005;25(Suppl 3):S149–51.
Berger B, Gerlach A, Groth S, Sladek U, Ebner K, Muhlhauser I, Steckelberg A. Competence training in evidence-based medicine for patients, patient counsellors, consumer representatives and health care professionals in Austria: a feasibility study. Zeitschrift Fur Evidenz, Fortbildung Und Qualitat Im Gesundheitswesen. 2013;107(1):44–52. https://doi.org/10.1016/j.zefq.2012.11.013 .
Long AF, Gambling T. Enhancing health literacy and behavioural change within a tele-care education and support intervention for people with type 2 diabetes. Health Expect. 2012;15(3):267–82. https://doi.org/10.1111/j.1369-7625.2011.00678.x .
White A, South J, Bagnall AM, Forshaw M, Spoor C, Marchant P, Witty K. The self-care for people initiative: the outcome evaluation. Prim Health Care Res Dev. 2012;13(4):382–94. https://doi.org/10.1017/S146342361200014X .
Webb J, Stanton M. Better access to primary healthcare for adults with learning disabilities: evaluation of a group programme to improve knowledge and skills. Br J Learn Disabil. 2009;37:116–22. https://doi.org/10.1111/j.1468-3156.2008.00527.x .
Matic-Strametz M, Strametz R, Bohrt K, Ochsendorf F, Weberschock T. Students in training to become biology teachers - a controlled phase II trial (NCT01567267). [Evaluation eines Lehrkonzepts in EbM fur Lehramtsstudierende der Biologie - eine kontrollierte Phase-II-Studie (NCT01567267)]. Zeitschrift Fur Evidenz, Fortbildung Und Qualitat Im Gesundheitswesen. 2013;107(1):53–61. https://doi.org/10.1016/j.zefq.2012.11.017 .
Muller I, Rowsell A, Stuart B, Hayter V, Little P, Ganahl K, et al. Effects on engagement and health literacy outcomes of web-based materials promoting physical activity in people with diabetes: an international randomized trial. J Med Internet Res. 2017;19(1):e21. https://doi.org/10.2196/jmir.6601 .
Garcia-Retamero R, Galesic M. Who profits from visual aids: overcoming challenges in people's understanding of risks [corrected]. Soc Sci Med. 2010;70(7):1019–25. https://doi.org/10.1016/j.socscimed.2009.11.031 .
Galesic M, Garcia-Retamero R. Communicating consequences of risky behaviors: life expectancy versus risk of disease. Patient Educ Couns. 2011;82(1):30–5. https://doi.org/10.1016/j.pec.2010.02.008 .
Galesic M, Garcia-Retamero R. Using analogies to communicate information about health risks. Appl Cognit Psychol. 2013;27:33–42. https://doi.org/10.1002/acp.2866 .
Kasper J, Kopke S, Muhlhauser I, Heesen C. Evidence-based patient information about treatment of multiple sclerosis--a phase one study on comprehension and emotional responses. Patient Educ Couns. 2006;62(1):56–63. https://doi.org/10.1016/j.pec.2005.06.002 .
Reiter, A. (2012). “Evaluierung “Gesundheit kommt nachhause – Mehr Wissen hilft!”.”.
D’Eath M, Barry MM, Sixsmith J. Rapid evidence reviews of interventions for improving health literacy. Stockholm: ECDC; 2012.
Download references
Acknowledgments
Not applicable.
This work was partly funded by the Consumers, Health and Food Executive Agency (Chafea) acting under the mandate of the European Commission (HEALIT4EU study; contract no. 20146201). The Agency had no role in the design of the study, the collection, analysis, and interpretation of data and in the writing of the original report or of this manuscript. The content of this publication represents the views of the authors and is their sole responsibility. It can in no way be taken to reflect the views of the European Commission and/or Chafea or any other body of the European Union.
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and affiliations.
University of Applied Sciences Utrecht, Heidelberglaan 7, 3584, CS, Utrecht, The Netherlands
Boudewijn B. Visscher & Bas Steunenberg
Nivel (Netherlands institute for health services research), Otterstraat 118, 3513, CR, Utrecht, The Netherlands
Monique Heijmans, Jolien M. Hofstede, Walter Devillé, Iris van der Heide & Jany Rademakers
Julius Global Health, Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, Utrecht, The Netherlands
Walter Devillé
Department of Family Medicine, Maastricht University, CAPHRI, (Care and Public Health Research Institute), Maastricht, The Netherlands
Jany Rademakers
You can also search for this author in PubMed Google Scholar
Contributions
JR and WD designed the original HEALIT4EU study. All authors contributed to the background section of the paper. MH, JH, WD, IH, JR performed the search and selection of articles published between 1995 and 2014. BV, BS, JR did the same for the articles published between 2015 and 2018. MH, JH, WD, IH, JR performed the analyses for the articles published between 1995 and 2014. BV, BS, JR added to these analyses the results of articles published between 2015 and 2018 and compared all results. MH, JH, WD, IH, JR. contributed to the discussion and conclusions of the study of the articles published between 1995 and 2014. BV, BS and JR updated and modified the discussion and conclusions with the results from the articles published between 2015 and 2018. BV is a major contributor in the writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Jany Rademakers .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:.
Final search strategy (DOCX 13 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Visscher, B.B., Steunenberg, B., Heijmans, M. et al. Evidence on the effectiveness of health literacy interventions in the EU: a systematic review. BMC Public Health 18 , 1414 (2018). https://doi.org/10.1186/s12889-018-6331-7
Download citation
Received : 23 July 2018
Accepted : 17 December 2018
Published : 29 December 2018
DOI : https://doi.org/10.1186/s12889-018-6331-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health literacy
- Interventions
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- MEMBER DIRECTORY
- Member Login
- Publications
- Clinician Well-Being
- Culture of Health and Health Equity
- Fellowships and Leadership Programs
- Future of Nursing
- U.S. Health Policy and System Improvement
- Healthy Longevity
- Human Gene Editing
- U.S. Opioid Epidemic
- Staff Directory
- Opportunities
- Action Collaborative on Decarbonizing the U.S. Health Sector
- Climate Communities Network
- Communicating About Climate Change & Health
- Research and Innovation
- Culture of Health
- Fellowships
- Emerging Leaders in Health & Medicine
- Culture & Inclusiveness
- Digital Health
- Evidence Mobilization
- Value Incentives & Systems
- Substance Use & Opioid Crises
- Reproductive Health, Equity, & Society
- Credible Sources of Health Information
- Emerging Science, Technology, & Innovation
- Pandemic & Seasonal Influenza Vaccine Preparedness and Response
- Preventing Firearm-Related Injuries and Deaths
- Vital Directions for Health & Health Care
- NAM Perspectives
- All Publications
- Upcoming Events
- Past Events
- MEMBER HOME

Health Literacy: A Necessary Element for Achieving Health Equity
A core aim for improving health care is to provide equitable care or “care that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status” (IOM, 2001). We believe that an essential ingredient in the effort to increase health equity and reduce health disparities is eliminating health literacy barriers. The challenge of aligning health care system demands and complexities with individual skills and abilities across the spectrum of public health and clinical delivery will be difficult, but critical in the effort to achieve health equity.
In this paper, we intend to demonstrate that the concepts of health literacy, health equity, and health disparities are connected, both in practice and in research. We also explore work that can be done at their intersection through the use of examples and selective review of data. Finally, we intend to convey three important messages:
- Health literacy is intrinsically linked to both an individual’s and a community’s socioeconomic context, and is a powerful mediator of the social determinants of health.
- Health literacy interventions are viable options among other evidence-based strategies to address social adversity and environmental health determinants and should be considered when assessing meaningful actions to address health disparities.
- Health literacy interventions and practices contribute to reducing health disparities, which fosters health equity and social justice.
This paper is divided into two major sections. The first section addresses issues related to research on health equity and health literacy. The second section provides real-world examples of the interplay of these concepts. Each section provides selected examples from the literature and is not a comprehensive literature review.
Research: Different Perspectives but Similar Issues
Health disparities and health literacy researchers commonly recognize the impact on health of social determinants such as poverty, educational status, and geographic location (Sorensen et al, 2012; Logan, In press). More specifically, both health literacy and health disparities researchers are concerned with the significantly different risks of illness associated with an unequal distribution of wealth, opportunities, and privileges in the United States as well as other nations. For example, health literacy and health equity researchers are mindful of the robust relationship between income and education and how both impact inequities in health services and outcomes in most countries (Health at a Glance 2013 OECD Indicators; Devaux, 2015).
Despite these commonalities in orientation and populations served, there seems to be little recognition within the literature that the concepts of health literacy and health equity are related (Volandes and Paasche-Orlow, 2007; Paasche-Orlow and Wolf, 2010). Cooper (IOM, 2011), noted that the researchers and practitioners who advance health literacy and health equity, while not necessarily working at cross purposes, may not be seeking opportunities to collaborate. This could stem from different research interventions sites, disparate funding streams, and diverse approaches to public advocacy.
For example, health literacy research and practice have often emphasized clinical interventions whereas health equity and health disparities research and practice often originate within community-based settings. Some of the federal agencies and foundations that fund health disparities research do not always emphasize health literacy funding and vice versa.
The rate of low health literacy in the United States is significantly linked to race, ethnicity, income, educational attainment, and age (Kutner et al, 2006). In addition, low health literacy is independently related to health outcomes. For example, Baker (2006) found that health literacy predicts desirable clinical and health administrative outcomes (e.g., hospitalization use) after controlling for sociodemographic variables such as education and income levels. Sudore and colleagues (2006) found that health literacy was an independent risk factor for all-cause mortality after adjusting for age, race, gender, income, education, health status, and other sociodemographic variables. Similar findings are evident in an array of diseases and health settings ranging from prevention to chronic disease (Peterson et al/, 2011; Wolf et al, 2006).
Further systematic reviews of health literacy research suggest that health literacy interventions are associated with improvements in clinical outcomes and health care utilization (Sheridan et al., 2011; Berkman et al., 2011; Jacobs et al., 2014; Taggart et al., 2012). For example, DeWalt and colleagues (2012) found that a literacy-sensitive self-care intervention for patients with heart failure improved outcomes for people with low literacy. Similarly, Rothman and colleagues (2004) showed that a diabetes disease management program addressing literacy may be particularly beneficial for patients with low literacy, and that increasing access to such a program could help reduce health disparities. Findings from these studies suggest that health literacy interventions should be considered in campaigns to address health disparities.
Mediational analyses that explore how one variable affects a second variable have begun to elaborate examples of how apparent race differences disappear when controlling for health literacy (Osborn et al, 2007; Osborn et al, 2011). Within the health disparities literature, race is sometimes suggested as a demographic characteristic that undergirds population differences, and thus these findings could be seen as providing evidence that health literacy may be a critical mediator reflective of the social determinants that impact health disparities. Functionally speaking, the authors believe that these findings mean that addressing health literacy is an important way to address health disparities (Wollesen and Peifer, 2006; Smith 2009; Smith and Moore, 2011; Smith 2011; Smith and Moore, 2012; Smith et al., 2012; Carroll et al., 2014).
As the research discussed suggests, health literacy is associated both with key social determinants of health and with health outcomes. As a result, the authors believe there is a benefit to explicitly connecting the concepts of health literacy and health equity and exploring the work that can be done at their intersection.
Practice: Examples of Integration
There are many examples of health literacy interventions that address health disparities and achieve, in one or more domains, reduction of disparities, thereby increasing health equity. The following discussion highlights a few of these that have been conducted outside of traditional health care settings. Ongoing efforts to reduce health literacy barriers in health care settings are crucial; however, we draw these examples from projects conducted in community settings to highlight some of the important health literacy work that can be done to address social determinants of disease in a diversity of settings.
According to Anderson and Whitaker (2010), children who are economically and socially disadvantaged are more likely to be obese. In fact, about one-third (According to the CDC, in 2011-2012, 8.4 percent of children aged 2 to 5 were obese. http://www.cdc.gov/healthyyouth/obesity/facts.htm (accessed June 19, 2015).) of the children in Head Start programs are overweight or obese (Aiken et al., 2010). In order to address obesity prevention, the University of California at Los Angeles/Johnson and Johnson Health Care Institute developed “Eat Healthy, Stay Active!,” a low health literacy training program for Head Start staff, parents, and children. The program’s goal was to increase knowledge and awareness about obesity risks and prevention of chronic disease. Low-literacy materials included information about food groups, portion size, shopping on a budget, and the importance of including physical activity. At the end of six months, there was a significant reduction in the rate of obesity in adult and child participants. The Eat Healthy, Stay Active! health literacy intervention demonstrates the contributions such programs can make to reducing health disparities, thereby promoting health equity.
Another example is an initiative developed by Herman and colleagues (2010) to address patient use of hospital emergency departments by 7,200 families from Head Start and Early Head Start agencies. While previous studies suggested characteristics such as socioeconomic status and the social environment were associated with use of the emergency department for routine care (Halfon et al., 1996), the introduction of a self-help health book, written at a third-grade reading level and used in a one-month training program, was shown to reduce unnecessary emergency department and primary care provider visits by 58 percent and 41 percent, respectively. Training interventions were delivered in English, Spanish, Hmong, and Somali.
In another effort, a Kit for New Parents (a multimedia health and parenting resource intended to help parents improve prenatal and early childhood health), which used health literacy principles and user engagement in its production, was found to significantly improve parental knowledge and child care development practices compared to a peer, control group among medically underserved audiences (Neuhauser et al., 2007).
Another example is the Canyon Ranch Institute Life Enhancement Program (LEP) (Pleasant et al., in press) which was launched with a South Bronx based-federally-qualified health center (FQHC) as a local partner. The South Bronx is among the lowest per capita income congressional districts in the United States and, according to diverse indicators, is also less healthy than the combined average of the boroughs of New York City. (See The New York City Community Health Survey of 2013, Age-adjusted data available at https://a816-healthpsi.nyc.gov/SASStoredProcess/guest?_PROGRAM=%2FEpiQuery%2FCHS%2Fchsindex&year=2013 (accessed June 19, 2015).)
Following the intervention researchers found that depression (measured with the PHQ-9) was cut by 50.1 percent and that stress levels dropped 30.2 percent. The number of self-reported unhealthy days dropped by 46.4 percent, self-reported level of strenuous exercise increased 89.4 percent, and moderate exercise increased 135.4 percent.
The examples described here strongly suggest that targeted, culturally appropriate interventions, delivered in a community setting with health literacy tools and reviews, have a positive impact on participant knowledge, attitudes, and behaviors. In addition, the use of an underlying health literacy perspective that examines the challenges in peoples’ lives and promotes empowerment for health ensured that the tools and interventions were comprehensively assessed, community-based, and culturally appropriate. Moreover, all the health literacy-specific interventions showed success in reducing health disparities in the target populations and achieved, in their own domains, greater health equity.
The trajectories of health literacy and health equity practice and research have intermingled yet autonomous paths. Health literacy barriers have clear associations with both short- and long-term deleterious effects on health. Health equity as a domain to understand and frame the elusive goal of optimizing health for all reminds us that health is linked to larger social issues of inequality and social justice.
Research and the development of operational principles to overcome health literacy barriers hold promise for a tangible set of activities and intentional strategies that can mitigate inequalities in treatment and outcomes. Health literacy interventions offer health care systems, providers, and those working in the community new approaches to use in addressing disparities that extend beyond the conventional view of screening, treatment, and care delivery. Moreover, a growing body of evidence suggests that these practices improve outcomes. We believe that advancing health literacy is a necessary and promising, component of how health equity can be realized.
To date, the majority of health literacy interventions have focused on ameliorating poor practices within the clinical setting rather than addressing social determinants of health at the community level. However, the examples presented here show that interventions using principles of health literacy, applied in community-based settings, can result in improved outcomes at the population level. Interventions in nonclinical settings should increase as health literacy becomes more integral to community-based interventions to promote health equity—such as the efforts described here.
Confronting issues of health literacy in the United States is a critical feature of addressing disparities. Health literacy’s application to community-based and population-level interventions remains to be defined in the larger issue of fostering health equity. We encourage research funding to develop the empirical basis for the concept that health literacy can be an asset to promote health equity. We also encourage policy development to advance the implementation and evaluation of health literacy interventions to foster health equity.
- Aiken, N., L. Tarullo, L. Hulsey, C. Ross, J. West, and Y. Xue. 2010. A year in Head Start: Children, families and programs. Washington, DC: U.S. Department of Health and Human Services, Administration for Children and Families.
- Anderson, S., and R. Whitaker. 2010. Household routines and obesity in US preschool-aged children. Pediatrics 125:420–428. https://doi.org/10.1542/peds.2009-0417
- Baker, D. W. 2006. The associations between health literacy and health outcomes: Self-reported health, hospitalization, and mortality. In Proceedings of the surgeon general’s workshop on improving health literacy. Rockville, MD: Office of the Surgeon General. Available at: http://www.ncbi.nlm.nih.gov/books/NBK44260/#proc-healthlit.panel1.s14 (accessed June 19, 2015).
- Berkman, N.D., S. L. Sheridan, K. E. Donahue, D. J. Halpern, A. Viera, K. Crotty, A. Holland, M. Brasure, K. N. Lohr, E. Harden, E. Tant, I. Wallace, and M. Viswanathan. 2011. Health literacy interventions and outcomes: An updated systematic review. Evidence Report/Technology Assessment No. 199. Prepared by RTI International–University of North Carolina Evidence-based Practice Center under contract No. 290-2007-10056-I. AHRQ Publication Number 11-E006. Rockville, MD: Agency for Healthcare Research and Quality. Available at: https://pubmed.ncbi.nlm.nih.gov/23126607/ (accessed July 17, 2020).
- Carroll, L. N., S. A. Smith, and N. R. Thomson. 2014. Parents as Teachers Health Literacy Demonstration project: Integrating an empowerment model of health literacy promotion into home-based parent education. Health Promotion Practice . https://doi.org/10.1177/1524839914538968
- Devaux, M. 2015. Income-related inequalities and inequities in health care services utilization in 18 selected OECD countries. European Journal of Health Economics 16(1):21–33. https://doi.org/10.1007/s10198-013-0546-4
- DeWalt, D. A., D. Schillinger, B. Ruo, K. Bibbins-Domingo, D. W. Baker, G. M. Holmes, M. Weinberger, A. Macabasco-O’Connell, K. Broucksou, V. Hawk, K. L. Grady, B. Erman, C. A. Sueta, P. P. Chang, C. W. Cene, J. R. Wu, C. D. Jones, and M. Pignone. 2012. Multisite randomized trial of a single-session versus multisession literacy-sensitive self-care intervention for patients with heart failure. Circulation 125(23):2854–2862. https://doi.org/10.1161/CIRCULATIONAHA.111.081745
- Halfon, N., P. W. Newacheck, D. L. Wood, and R. F. St. Peter. 1996. Routine Emergency Department use for sick care by children in the United States. Pediatrics 98(1),28–34. Available at: https://pubmed.ncbi.nlm.nih.gov/8668408/ (accessed July 17, 2020).
- OECD Library. 2013. Health at a Glance. http://dx.doi.org/10.1787/health_glance-2013-en
- Herman, A., and P. Jackson. 2010. Empowering low-income parents with skills to reduce excess pediatric emergency room and clinic visits through a tailored low literacy training intervention. Journal of Health Communication 15(8):895–910. http://dx.doi.org/10.1080/10810730.2010.522228.
- Institute of Medicine. 2001. Crossing the Quality Chasm: A New Health System for the 21st Century . Washington, DC: The National Academies Press. https://doi.org/10.17226/10027
- Institute of Medicine. 2011. Innovations in Health Literacy Research: Workshop Summary . Washington, DC: The National Academies Press. https://doi.org/10.17226/13016
- Jacobs, R. J., J. Q. Lou, R. L. Ownby, and J. Caballero. 2014. A systematic review of eHealth interventions to improve health literacy. Journal of Health Informatics. https://doi.org/10.1177/1460458214534092
- Kutner, M., E. Greenberg, Y. Jin, and C. Paulsen. 2006. The health literacy of America’s adults: Results from the 2003 National Assessment of Adult Literacy. NCES 2006–483. U.S. Department of Education. Washington, DC: National Center for Education Statistics. Available at: https://nces.ed.gov/pubs2006/2006483.pdf (accessed July 17, 2020).
- Logan, R. A. In press. Health literacy. In Crucial conversations: Meeting health information needs outside of healthcare, edited by C. Arnott-Smith and A. Keselman. New York: Chandos.
- Neuhauser, L., W. L. Constantine, N. A. Constantine, K. Sokal-Gutierrez, S. K. Obarski, L. Clayton, M. Desai, G. Sumner, and S. L. Syme. 2007. Promoting prenatal and early childhood health: Evaluation of statewide materials–based intervention for parents. American Journal of Public Health 97(10):1813–1819. https://doi.org/10.2105/AJPH.2006.089532
- Osborn, C. Y., K. Cavanaugh, K. A. Wallston, S. Kripalani, T. A. Elasy, R. L. Rothman, and R. O. White. 2011. Health literacy explains racial disparities in diabetes medication adherence. Journal of Health Communication 16(Suppl 3):268–278. https://doi.org/10.1080/10810730.2011.604388
- Osborn, C. Y., M. K. Paasche-Orlow, T. C. Davis, and M. S. Wolf. Health literacy: An overlooked factor in understanding HIV health disparities. American Journal of Preventive Medicine 33(5):374–378. https://doi.org/10.1016/j.amepre.2007.07.022
- Paasche-Orlow, M. K., and M. S. Wolf. 2010. Promoting health literacy research to reduce disparities. Journal of Health Communication 15(Suppl 2):34–41. https://doi.org/10.1080/10810730.2010.499994
- Peterson, P. N., S. M. Shetterly, C. L. Clarke, D. B. Bekelman, P. S. Chan, L. A. Allen, D. D. Matlock, D. J. Magid, and F. A. Masoudi. 2011. Health literacy and outcomes among patients with heart failure. Journal of the American Medical Association 305(16):1695–1701. https://doi.org/10.1001/jama.2011.512
- Pleasant, A., J. Cabe, K. Patel, J. Consenza, and R. Carmona. 2015. Health literacy research and practice: A needed paradigm shift. Health Communication 30(12):1176-1180. https://doi.org/10.1080/10410236.2015.1037426
- Rothman, R. L., D. A. DeWalt, R. Malone, B. Bryant, A. Shintani, B. Crigler, M. Weinberger, and M. Pignone. 2004. Influence of patient literacy on the effectiveness of a primary care-based diabetes disease management program. JAMA 292(14):1711–1716. https://doi.org/10.1001/jama.292.14.1711
- Sheridan S. L., D. J. Halpern, A. J. Viera, N. D. Berkman, K. E. Donahue, and K. Crotty. 2011. Interventions for individuals with low health literacy: A systematic review. Journal of Health Communication 16(Suppl 3):30–54. https://doi.org/10.1080/10810730.2011.604391
- Smith, P. C., J. H. Brice, and J. Lee. 2012. The relationship between functional health literacy and adherence to emergency department discharge instructions among Spanish-speaking patients. Journal of the National Medical Association 104(11–12):521–527. https://doi.org/10.1016/s0027-9684(15)30218-2
- Smith, S. A. 2009. Promoting health literacy: Concept, measurement and intervention. PhD diss., Union Institute and University. Ann Arbor, MI: Dissertation Abstracts International.
- Smith, S. A. 2011. Health literacy and social service delivery. In New directions in behavioral health: Service delivery strategies for vulnerable populations, edited by S. A. Estrine, H. G. Arthur, R. T. Hettenbach, and M. G. Messina. New York: Springer.
- Smith, S. A., and E. J. Moore. 2011. Health literacy and depression in the context of home visitation. Journal of Maternal and Child Health. Available at: http://www.springer.com/home?SGWID=0-0-1003-0- 0&aqId=2111233&download=1&checkval=ffd392d488b3752bf1d2e6a3e258b189 (accessed June 7, 2014).
- Smith, S. A., and E. J. Moore. 2012. Health literacy and depression in the context of home visitation. Journal of Maternal Child Health 16(7):1500–1508. https://doi.org/10.1007/s10995-011-0920-8
- Sorensen, K., S. V. Broucke, J. Fullam, G. Doyle, J. Pelikan, A. Slonska, H. Brand, and HLS-EU Consortium Health Literacy Project European. 2012. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 12(80). https://doi.org/10:1186/1471-2458/12/80
- Sudore, R. L., K. Yaffe, S. Satterfield, T. B. Harris, K. M. Mehta, E. M. Simonsick, A. B. Newman, C. Rosano, R. Rooks, S. M. Rubin, H. N. Ayonayon, and D. Schillinger. 2006. Limited literacy and mortality in the elderly: The heat, aging, and body composition study. Journal of General Internal Medicine 21(8): 806–812. https://doi.org/10.1111/j.1525-1497.2006.00539.x
- Taggart, J., A. Williams, S. Dennis, A. Newall, T. Shortus, N. Zwar, E. Denney-Wilson, and M. F. Harris. 2012. A systematic review of interventions in primary care to improve health literacy for chronic disease behavioral risk factors. Database of Abstracts of Reviews for Effects (DARE): Quality-assessed reviews. Available at: http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0052469/ (accessed July 22, 2015).
- Volandes, A. E., and M. K. Paasche-Orlow. 2007. Health literacy, health inequality and a just healthcare system. American Journal of Bioethics 7(11):5–10. https://doi.org/10.1080/15265160701638520
- Wolf, M. S., S. J. Knight, E. A. Lyons, R. Durazo-Arvizu, S. A. Pickard, A. Arseven, A. Arozullah, K. Colella, P. Ray, and C. L. Bennett. 2006. Literacy, race, and PSA level among low-income men newly diagnosed with prostate cancer. Urology 68(1):89–93. https://doi.org/10.1016/j.urology.2006.01.064
- Wollesen, L., and K. Peifer. 2006. Life Skills Progression: An outcome and intervention planning instrument for use with families at risk. Baltimore, MD: Brookes.
https://doi.org/10.31478/201507a
Suggested Citation
Logan, R. A., W. F. Wong, M. Villaire, G. Daus, T. A. Parnell, E. Willis, and M. K. Paasche-Orlow. 2015. Health Literacy: A Necessary Element for Achieving Health Equity. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201507a
Author Information
Robert A. Logan, PhD is a communications research scientist at the National Library of Medicine. Winston F. Wong, MD, MS, is Medical Director of Community Benefit at Kaiser Permanente and a member of the Roundtable on Health Literacy. Michael Villaire MSLM, is Chief Executive Officer for the Institute for Healthcare Advancement and a member of the Roundtable on Health Literacy. Gem Daus, MA is a Public Health Analyst in the Office of Health Equity at the Health Resources and Services Administration and is a member of the Roundtable on Health Literacy. Terri Ann Parnell, DNP, RN is Principal and Founder of Health Literacy Partners and is a member of the Roundtable on Health Literacy. Earnestine Willis, MD, MPH is the Kellner Professor in Pediatrics at the Medical College of Wisconsin and a member of the Roundtable on Health Literacy. Michael K. Paasche-Orlow, MD, PPH, MA is Associate Professor of Medicine at Boston University School of Medicine and a member of the Roundtable on Health Literacy.
The views expressed in this Perspective are those of the author(s) and not necessarily of the author(s) organizations or of the National Academy of Medicine (NAM). The Perspective is intended to help inform and stimulate discussion. It has not been subjected to the review procedures of, nor is it a report of, the NAM or the National Academies of Sciences, Engineering, and Medicine. Copyright by the National Academy of Sciences. All rights reserved.
Join Our Community
Sign up for nam email updates.
Health Literacy for Public Health Professionals Resources
On this page, you will find the list of resources for the Centers for Disease Control and Prevention’s online course, Health Literacy for Public Health Professionals .
- Bibliographies
- Cultural Competency
- Curricula and Educational Resources
- Funding Opportunities
- Guides and Manuals
- Health Communication Resources
- Health Information for Audiences with Limited Health Literacy
- Health Literacy Initiatives and Programs
- Health Literacy Listservs
- Planning and Assessment Tools
- Training Programs
- User-Centered Design
An Overview of Medical and Public Health Literature Addressing Literacy Issues: An Annotated Bibliography
The National Center for the Study of Adult Learning and Literacy created this report presenting results from a computer-assisted search of the medical and public health literature addressing literacy issues in health care and in health promotion and education published between 1990 and the end of 1999. This bibliography includes 241 citations which are arranged into a variety of categories.
Health, Communication and Literacy: An Annotated Bibliography
The Centre for Literacy compiled an annotated listing of articles on literacy and health published from 1990 through 1998. Articles are arranged alphabetically by keywords.
Understanding Health Literacy and Its Barriers
The National Library of Medicine’s bibliography provides a comprehensive list of health literacy citations from varying disciplines and publications from January 1998 through November 2003, plus selected earlier and later citations. The bibliography is divided into specific topic areas.
Current Bibliographies in Medicine/Health Literacy
The National Library of Medicine’s bibliography was compiled to help define and describe the evidence base for advancing health literacy programs by examining theories, strategies, and tactics in the published literature. It covers articles from January 1990 through October 1999, plus selected earlier and later citations.
Doak CC, Doak LG, Root JH. Teaching Patients with Low Literacy Skills. 2nd ed. Philadelphia, PA: J. B. Lippincott, 1996.
Osborne H. Overcoming Communication Barriers in Patient Education. Gaithersburg, MD: Aspen Publishers, Inc, 2001.
Thompson TL, Dorsey AM, Miller KL, Parrott R, editors. Handbook of Health Communication . Mahwah, NJ: Lawrence Erlbaum Associates, 2003.
Schwartzberg JG, VanGeest JB, Wang CC, editors. Understanding Health Literacy: Implications for Medicine and Public Health . Chicago, IL: AMA Press, 2005.
Zarcadoolas C, Pleasant AF, Greer DS. Advancing Health Literacy A Framework for Understanding And Action. San Francisco, CA: Jossey-Bass, 2006.
CDC’s Health Equity Guiding Principles for Inclusive Communication emphasize the importance of addressing all people inclusively and respectfully. These principles are intended to help public health professionals adapt their communication products and strategies to the specific cultural, linguistic, environmental, and historical situation of each population or audience of focus.
U.S. Department of Health and Human Services (HHS) Office of Minority Health. Cultural and Linguistic Competency .
HHS Health Resources and Services Administration. Cultural Competence Resources for Health Care Providers.
HHS Agency for Healthcare Research and Quality. Setting the Agenda for Research on Cultural Competence in Health Care.
A Physician’s Practical Guide to Culturally Competent Care
The U.S. Department of Health and Human Services, Office of Minority Health developed this guide that includes cultural competency curriculum modules designed to equip family physicians with awareness, knowledge, and skills in cultural competency to better treat the increasingly diverse U.S. population.
California Health Literacy Initiative Health Literacy Resource Center :
The Health Literacy Resource Center is a central resource for health literacy information and training. It is a one- stop shop for Web-based health literacy resources. The information is provided for literacy practitioners, health care professionals, adult literacy and ESL students, and anyone who seeks a clear understanding of health information.
El Paso Adult Education Health Literacy Curriculum
The El Paso Community College Health Occupations Literacy Project provides health literacy and cultural competency training for medical and health care professionals and trains youth and schools on health education topics using community health workers.
Harvard School of Public Health, Health Literacy Curricular Resources
The Harvard School of Medicine, Health Literacy Studies, offers a collection of materials, including a series of plainlanguage glossaries, plain language materials for Seniors, and how-to-guides focusing on participatory processes anddiversity.
Health Literacy Public Health Forums: Partners for Action
The National Center for the Study of Adult Learning and Literacy developed this guide to assist public health professionals and members of departments of health to conduct a forum on health literacy and thereby raise awareness about health literacy and links to health outcomes.
World Education, Health and Literacy Curricular Resources
World Education provides educational resources and projects summaries on how to integrate health topics into basic skills instruction, trains health care providers how to develop easy-to-read materials and forms, and provides online courses for entry-level health care employees and adult education students to prepare for college programs leading to nursing and other allied health professions. World Education charges a few for some programs and resources.
Federally Funded Research
CDC links to many health literacy funding opportunities, research findings, and training initiatives on its Federally Funded Research web page .
Accessible Health Information Technology (IT) for Populations with Limited Literacy: A Guide for Developers and Purchasers of Health IT
This guide and checklist, developed by the U.S. Department of Health and Human Services, National Resource Center for Health IT, are intended for developers and purchasers of health information technology (HIT) that is designed to be accessed and used by consumers. This guide can be used to evaluate HIT products and to direct and validate a developer’s work.
Clear & Simple: Developing Effective Print Materials for Low-Literate Readers.
This guide, developed by the U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute, outlines a process for developing publications for people with limited-literacy skills. The guide features both proven principles and a discussion of real-life issues that individuals developing low-literacy materials face, such as the constraints of time, budget, organizational pressures, and the government publications process.
Health Literacy Study Circles
These guides, designed by Dr. Rima Rudd fromHarvardUniversityandtheNationalCenterfortheStudyofAdultLearning and Literacy, are intended to help literacy instructors integrate health literacy skills into their curriculum.
Quick Guide to Health Literacy
The U.S. Department of Health & Human Services, Office of Disease Prevention and Health Promotion’s Quick Guide to Health Literacy is for government employees, grantees, contractors, and community partners working in healthcare and public health fields. The guide provides information on key health literacy concepts; techniques for improving health literacy through communication, navigation, knowledge-building, and advocacy; examples of health literacy best practices; and suggestions for addressing health literacy in your organization.
Rhode Island Health Literacy Project Health Literacy Toolkit: Better Communication for Better Care
This toolkit offers resources to help physicians/providers and their staff address communication challenge that may result from patients’ literacy levels or language/cultural barriers.
Simply Put: A guide for creating easy-to-understand materials
The guidance in Simply Put helps you transform complicated scientific and technical information into communication materials your audiences can relate to and understand. The guide provides practical ways to organize information and use language and visuals. This guide will be useful for creating fact sheets, FAQ’s, brochures, booklets, pamphlets, and other materials, including web content.
Toolkit for Making Written Material Clear and Effective .
The Toolkit for Making Written Material Clear and Effective is a health literacy resource from the Centers for Medicare and Medicaid Services. This 11-part toolkit provides a detailed and comprehensive set of tools to help you make written material in printed formats easier for people to read, understand, and use.
Beyond the Brochure: Alternative Approaches to Effective Health Communication
This brochure, developed by AMC Cancer Research Center, provides guidelines for the use of print and audio- visual materials when communicating health messages to the community.
Making Health Communication Programs Work (the “Pink Book”)
This guide, from the U.S. Department of Health and Human Services, National Cancer Institute, offers planning steps for helping make any communication program work, regardless of size, topic, intended audience, or budget. The Pink Book describes a practical approach for planning and implementing health communication efforts.
PhotoNovels: Harvard School of Public Health
PhotoNovels are like comic books with photographs and captions. Two handbooks, prepared by the Harvard School of Public Health, Health Literacy Studies, provide practical examples.
Plainlanguage.gov
This site, developed by The Plain Language Action and Information Network (PLAIN), is designed to improve communication from the federal government to the public. This website contains excellent tools and examples of plain language.
Healthy Roads Media
This site, started by the National Library of Medicine, contains free health education materials in a number of languages and a variety of formats.
MedlinePlus
This site, a service of the U.S. National Library of Medicine and the National Institutes of Health, provides directories, a medical encyclopedia and a medical dictionary, easy-to-understand tutorials on common conditions, tests, and treatments, health information in Spanish, extensive information on prescription and nonprescription drugs, health information from the media, and links to thousands of clinical trials.
MyHealthfinder
MyHealthfinder include links to over 6,000 government and nonprofit health information resources on hundreds of health topics. Information is in English and Spanish.
California Health Literacy Initiative
The goal of the California Health Literacy Initiative is to inform and partner with individuals and organizations to craft collective, lasting solutions which will positively impact the health and well-being of individuals with low- literacy skills, their families, and their communities.
Minnesota Health Literacy Partnership
The Minnesota Health Literacy Partnership, a program of the Minnesota Literacy Council, was formed to help coordinate health literacy efforts across the state. The Partnership’s goals are to train health care providers about health literacy, empower patients to ask for clear communication, and share health literacy resources.
North Carolina Institute of Medicine’s Task Force on Health Literacy
The task force was a collaborative effort between the North Carolina (NC) Institute of Medicine, the NC Department of Health and Human Services (NC DHHS), and the Area Health Education Centers (AHEC) program. The goal of the task force was to study literacy problems and develop workable solutions to ensure that healthcare needs of people with low health literacy skills were met.
Pfizer Clear Health Communication Initiative
The initiative provides a wealth of information, resources, and opportunities on clear health communication for researchers, physicians and other providers, public health professionals, the media, and those interested in public policy.
CDC Health Literacy Updates
Subscribe to CDC’s weekly health literacy updates for health communicators, public health professionals, clinicians, community leaders, and anyone who communicates with the public about public health or personal health. The updates provide information and tools on health literacy research, practice, and evaluation.
Institute for Healthcare Advancement’s (IHA) Health Literacy Discussion List
The IHA hosts a listserv for the health literacy community. The listserv provides a forum to share ideas, get advice, ask questions, and make announcements. Subscribe to the listserv emails.
Public Health Image Library (CDC)
This is a public collection of photos, illustrations, and media files. Most of the collection is medical and scientific photos, but there are some photos of people and food.
Visuals Online (National Cancer Institute)
The NCI Visuals Online database contains images of food and people that can be used free of charge
Council of State Governments (CSG) Guide to Health Literacy
Using data from its National Survey on Health Literacy Initiatives, CSG published the State Official’s Guide to Health Literacy , an overview of how health literacy affects states and what states can and are doing to address this issue.
Making Health Literacy Real: The Beginnings of My Organization’s Plan for Action
This resource, developed by the Centers for Disease Control and Prevention, provides the steps to help you and your organization develop a plan to change organizational and professional practices to improve health literacy. Includes a downloadable template.
Harvard Health Literacy Studies
This site is designed for professionals in health and education who are interested in health literacy. The site contains a variety of research, materials, literature, and curricula on health literacy.
HLE2: The Health Literacy Environment of Hospitals and Health Centers
This resource enables you to identify and rate literacy and related factors within your organization. Findings will support efforts to improve health literacy by initiating action, identifying and action on priority areas, and measuring change over time. The resource is the product of a partnership between Dr. Rima Rudd, of the Harvard School of Public Health, and the Health Literacy Task Force of the University of Texas Medical Center.
Is Our Pharmacy Meeting Patients’ Needs? Pharmacy Health Literacy Assessment Tool User’s Guide
This tool, from the U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality, helps pharmacies assess how well they are set up to serve patients with limited health literacy.
Readability Formulas
- Fog Readability Formula
- Flesch-Kinkaid Readability Formula
- SMOG Readability Formula
World Education Health and Literacy Compendium
World Education and its partners produce a variety of publications. Most can be downloaded from this site for free. This site includes a compendium of guides, handbooks, books, and other resources on the issues of literacy, health, and related issues.
A Vision for a Health Literate Canada: Report of the Expert Panel on Health Literacy
This report, prepared by Canada’s Public Health Leader’s Expert Panel on Health Literacy, consolidates the research on health literacy and points to changes in communication strategies, practices, procedures and policies that will ultimately improve health literacy and the well-being of all Canadians.
Communicating Health: Priorities and Strategies for Progress
This action plan, developed by the U.S. Department of Health and Human Services Office of Disease Prevention and Health Promotion, is intended to achieve the health communication objective 11.2 in Healthy People 2010―improvedhealthliteracy.
Health Literacy: A Prescription to End Confusion
This 2004 report, from the Institutes of Medicine (now the National Academies of Sciences, Engineering, and Medicine [NASEM]) examines the body of knowledge that applies to the field of health literacy and recommends actions to promote a health-literate society. NASEM also has more current health literacy reports .
Health Literacy Interventions and Outcomes
To synthesize the increasing volume of literature on health literacy, the HHS Agency for Healthcare Research and Quality (AHRQ) commissioned the RTI International–University of North Carolina Evidence-Based Practice Center (RTI–UNC EPC) to provide a systematic literature review examining the effects of health literacy on health outcomes and interventions to improve those outcomes.
Healthy People
Healthy People, established by the U.S. Department of Health and Human Services (HHS), Office of Disease Prevention and Health Promotion, is a comprehensive set of disease prevention and health promotion objectives developed to improve the health of the nation. The Health Communication and Health Information Technology objectives address health literacy.
National Assessment of Educational Progress (NAEP): The Nation’s Report Card
NAEP is the only assessment that measures what U.S. students know and can do in various subjects across the nation, states, and in some urban districts. Subjects include reading, writing, math, and science. Also known as The Nation’s Report Card, NAEP has provided important information about how students are performing academically since 1969. You can also find additional information about NAEP .
Proceedings of the Surgeon General’s Workshop on Improving Health Literacy
This report discussed outcomes from the 2006 Surgeon General’s Workshop on Improving Health Literacy held by Acting Surgeon General Kenneth Moritsugu.
Program for the International Assessment of Adult Competencies (PIAAC)
This cyclical, large-scale study was developed under the auspices of the Organization for Economic Cooperation and Development (OECD). It collects data in 24 countries on adults’ proficiency in three domains: literacy, numeracy, and problem-solving in technology-rich environments.
The Health Literacy of America’s Adults: Results from the 2003 National Assessment of Adult Literacy (NAAL)
These downloadable documents report the NAAL health literacy results. The results are based on assessment tasks specifically designed to measure the health literacy of adults living in the United States. Health literacy was reported using four performance levels: Below Basic, Basic, Intermediate and Proficient.
Toward Health Equity and Patient-Centeredness: Integrating Health Literacy, Disparities Reduction, and Quality Improvement. Workshop Summary
The Forum on the Science of Health Care Quality Improvement and Implementation, the Roundtable on Health Disparities, and the Roundtable on Health Literacy jointly convened the workshop “Toward Health Equity and Patient- Centeredness: Integrating Health Literacy, Disparities Reduction, and Quality Improvement” on May 12, 2008, to address issues surrounding quality and disparities, and the ability of individuals to make appropriate decisions based on basic health knowledge and services. During this workshop, speakers and participants explored how equity in care delivered and a focus on patients could be improved.
Equipped for the Future
Equipped for the Future was a national, standards-based, educational improvement initiative for adult basic education and English-language learning. The mission of this initiative was to provide the tools, professional development, and technical assistance to implement standards-based adult education in ways that meet the needs of adult learners.
National Health Education Standards
The National Health Education Standards (NHES) were developed by the American Cancer Society to establish, promote, and support health-enhancing behaviors for students in all grade levels, from pre-k through grade 12. The standards provide a framework for teachers, administrators, and policy makers to design or select curricula, allocate instructional resources, and assess student achievement and progress.
National Standards for Culturally and Linguistically Appropriate Services in Health Care
The U.S. Department of Health and Human Services, Office of Minority Health developed comprehensive standards on culturally and linguistically appropriate services (CLAS) in health care. CLAS standards are intended to advance health equity, improve quality, and help eliminate health care disparities by establishing a blueprint for health and health care organizations to respond to cultural and linguistic issues presented by diverse populations.
Centers for Disease Control and Prevention (CDC) Health Literacy Trainings
CDC offers several free, online, self-paced health literacy trainings in addition to the training you are taking now.
Non-CDC Training
Many non-CDC organizations offer training on health literacy, plain language, cultural and communication, consumer and patient skill building, and shared decision making.
Tools to Bring Human-centered Design into Your Project
Many subject-matter experts use the term “human-centered design” and “user-centered design” interchangeably. The human-centered design tools on this page help federal offices and other organizations carry out the phases of user-centered (or human-centered) design.
User-Centered Design Basics
Find the basics on the phases of the product design and development life-cycle and on how to gain an understanding of who will be using the product.
To receive email updates about this page, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
California Literacy, Inc., makes no claim as to the accuracy of the information provided in the California Health Literacy Initiative Resource Center.
California Family Health Council, Inc. (CFHC) http://www.epahealth.org Offices EPA Division of CFHC 492 Division Street Campbell, CA 95008 Phone: (800) 428-5438 ext. 3213 Fax: (408) 374-7385 Contact: Veronica Estrella Murillo, Director of Health Education Resources Email: [email protected] 3600 Wilshire Boulevard, Suite 600 Los Angeles, CA 90010 Phone: (213) 386-5614 Fax: (213) 386-4410 ThE EPA Division of California Family Health Council is devoted to helping health care providers give their communities the best health care possible. It has two Resource Centers of health education materials, available at no charge to health care providers nationwide. EPA also provides customized training in health literacy and consultation to assist agencies in developing plain language materials for their clients. In addition, it publishes easy-to-read patient education materials in multiple languages.
California Health Literacy Initiative: California Literacy, Inc.
http://cahealthliteracy.org
Offices 1475 Powell Street, Suite 106 Emeryville, CA 94608-2026 Phone: (510) 655-3264 Fax: (510) 655-3268 Contact: Beccah Rothschild, M.P.A., Health Literacy Manager Email: [email protected]
133 N. Altadena Drive, Suite 410 Pasadena, CA 91107 Phone: (626) 395-9989 ext. 19 Fax: (626) 395-9987 Contact: Faith Ruperto, Health Literacy Coordinator Email: [email protected]
The goal of the California Health Literacy Initiative is to inform and partner with individuals and organizations to positively impact the health and well-being of individuals with low-literacy skills, their families, and their communities. This plan for California will serve as a groundbreaking, national model for health literacy. Currently, no statewide efforts of such complexity are being undertaken.
Institute for Healthcare Advancement http://www.iha4health.org/index.cfm/MenuItemID/174.htm
501 S. Idaho St., Suite 300 La Habra, CA 90631 Phone: (800) 434-4633 or (562) 690-4001 ext. 201 Fax: (562) 690-8988 Contact: Gloria Mayer, RN, Ed.D., FAAN, CEO/President Email: [email protected]
The Institute for Healthcare Advancement has mounted efforts to combat low health literacy with the What to Do For Health book series and the Annual Health Literacy Conference: Organizational Solutions to Low Health Literacy. The four books in the What To Do For Health series were written with one goal in mind: to provide basic, necessary health care information in an easy-to-read, easy-to-use format. The annual conference brings together health literacy leaders from organizations that have developed programs and solutions to low health literacy.
Latino Health Access: Health Promoter Training and Program http://www.latinohealthaccess.org/
1717 N. Broadway Santa Ana, CA 92706-2605 Phone: (714) 542-7792 General email: [email protected]
The mission of Latino Health Access is to assist in improving the quality of life and health of uninsured, underserved people through quality preventive services and educational programs. Promotores are highly trained community health workers. They are recruited, hired and trained from the communities in which they live. They are educators and role models who are highly skilled at leading their peers toward wellness. Latino Health Access has been on the cutting edge of the Promotores movement for the past ten years. Their programs and trainings, based on the teachings of Brazilian educator Paulo Friere, incorporate the principles of adult education and are highly interactive.
National Libraries of Medicine: Southwest Regional Consumer Health Information Services http://nnlm.gov/psr/about/fs/fs_cons_hlth.html
University of California, Los Angeles, Louise M. Darling Biomedical Library Academic Library: Regional Medical Library Phone: (800) 338-7657 Contact: Heidi Theissen-Sandstrom, R.N., Interim Associate Director Email: [email protected]
The goal of the services provided is to improve the general public's awareness of and ability to access valuable health information. Their services aim to fulfill the potential of health information providers to meet the health information and health literacy needs of the public in the Pacific Southwest Region (AZ, CA, HI, NV and the U.S.-Affiliated Pacific Basin). They do this through promotion of reputable health information resources/services, training, development of the regional information infrastructure, and expansion of partnerships and collaborations.
PlaneTree Health Library http://www.planetreesanjose.org
PlainTree Health Library 15891 Los Gatos-Almaden Road Los Gatos, CA 95032 Phone: (408) 358-5667 Contact: Candace Ford, M.L.S., Executive Director General email: [email protected] PlaneTree is a comprehensive consumer health and medical library, free and open to the public. The library's most fundamental service is providing access to information for informed decisions about health and healthy choices in life. Their extensive collection of current, useful health information is provided in a variety of formats. Resources range from easy-to-understand materials to technical, professional literature. Computer services feature Internet access, including health sites not publicly available, and help with online searching. PlaneTree covers both conventional and complementary (alternative) therapies. Some books, articles, and videos are available in Spanish and in Vietnamese.
Venice Family Clinic: Health Empowerment Initiative http://www.venicefamilyclinic.org/
604 Rose Avenue Venice, CA 90291 Phone: (310) 664-7839 Fax: 310-396-8279 Contact: Jeannette Hilgert, M.S.G., M.S.W., Program Administrator Email: [email protected]
Health care and medicine each have their own language filled with specialized and "common" terms, which are rarely heard in everyday conversation. Clinic visits often include unfamiliar surroundings, specialized technical procedures, and new information about health topics that may be intimidating and difficult for many patients to understand. The Venice Family Clinic received a grant from the California Endowment to address these barriers. The Health Empowerment Initiative (HEI) strives to enhance patients’ understanding of health, disease, and the health care system and to increase patients’ self-efficacy and health management techniques.
Vision Literacy http://www.visionliteracy.org/
Offices North County Office 40 N. Milpitas Boulevard Milpitas, CA 95035 Phone: (408) 262-1349 Main Line Fax: (408) 262-5806 Contact: Pat Lawson-North, Executive Director Direct Line: (408) 262-1349 ext. 3671 Email: [email protected]
West County Office 585 Franklin Street Mountain View, CA 94041 Phone: (650) 526-7016 Main Line Fax: (650) 962-0438 Contact: Ellen Loebl Direct Line: (408) 293-2326 ext. 3070 Email: [email protected]
Vision Literacy is dedicated to enriching the community by helping adults improve their literacy skills. They provide innovative literacy services. They also empower adults to reach their goals and potential by promoting mutual commitments between learners and community partners, and providing an accessible process for investing time, funding, and other resources. Vision Literacy is a nationally recognized leader of community partnerships designed to empower adults through literacy.
Vision Literacy in Partnership with PlaneTree Health Library: Community Learning Centers (CLCs) http://www.visionliteracy.org/about/clc.html Branches: South County Office (serving Morgan Hill, San Martin and Gilroy) Community Learning Center (CLC) 42 Martin St. Gilroy, CA 95020 Phone: (408) 848-5366 Fax: (408) 848-2950 Contact: Judy Walko Community Learning Center (CLC), North County Santa Clara Valley Medical Center, Administration Building 751 S. Bascom Ave. San Jose, CA 95128 Phone: (408) 293-2326 ext. 3070 Fax: (408) 885-3222 Contact: Ellen Loebl Email: [email protected] The Community Learning Center (CLC), North County is an innovative partnership between Vision Literacy, PlaneTree Health Library, and Santa Clara Valley Medical Center. The center was established to provide people who have limited reading skills with access to free health information and adult literacy services, and to provide the general public with a resource on a wide array of health issues. The CLC features a health library with video, audio and print materials, including items for adult new readers. The Community Learning Center (CLC), South County recently opened its doors to the public. Located at Vision Literacy's South County office, the expanded partnership between Vision Literacy and PlaneTree Health Library, is the first program of its kind in Gilroy. Featuring the same resources and services as its North County predecessor, the collaborative effort is funded in part by the U.S. Institute of Museum and Library Services under the provisions of the Library Services and Technology Act, administered in California by the State Librarian.

Chapter 5: African American English and the communities it influences
5.4.3 The way rap and hip-hop have influenced today’s African American youth (research essay)
Amiri Austin
English 102, November 2020
Today I believe young people not just limited to African American’s find themselves being in a situation in which they have turned to their favorite rapper for motivation, a voice to listen to, or even just background music. Since I started this topic, I’ve been intrigued to find out just how big of an impact Rap and Hip-Hop have had on African American youth in areas of high income along with impoverished areas. Music has helped many of these kids get through tough situations and help escape their reality of gang violence and perhaps not the best circumstances. Rap and Hip-Hop music have also helped influence this generations views on certain topics and helped create opportunities young men and women of color otherwise wouldn’t have had the chance to experience.
Now you may be wondering how exactly music can help African American communities. To start I will introduce you to a study used and created by counselors to better help them understand their clients of color. In the article titled “Using Rap Music to Better Understand African American Experiences.”, the authors start off by describing Hip-Hop as more than just a culture you can adopt by buying certain clothes or going to see a few concerts. Hip-Hop is described as more of a dream or an emotional outlet or a way to build relationships and to help young people network their way to a career or profession to get out of the projects or another tough living situation. The authors went about this study by using a content analysis design and chose a genre known as conscious rap, featuring multiple artists and 10 different songs. The songs included were NWA-F**K The Police, 2Pac-rapped, Killer Mike- Don’t Die, Rage Against the Machine-Killing the Name, MainSource- Just a Friendly Game of Baseball, Dead Prez-Cop Shot, Gil Scott Heron- No Knock, Ice-T – Cop Killer, KRS-One-Sound of Da Police, and UGK-Protect and Serve.(7) Each of the researchers listened to the songs in 30 second intervals and then wrote down their thoughts/decoded versions. Time was taken to relisten and truly feel what the artist was trying to describe to its listeners. The authors found that these songs were more than just lyrics for people to memorize and recite at concerts, they were words used to help these artists get out of their struggle and help their family members out, they were words used to inspire other youth and let them know that even in the worst situations you can achieve the biggest of dreams. This advancement of understanding the lyrics and usage of certain verbiage in songs helped counselors become more culturally competent and helped them institute encouraging activities and helped bring out locked up stories from clients of color. It also helped them understand their social identity and made them feel more wanted even in a world of privilege and oppression. This study is important to the climate of today’s world because I think a lot of people have a misunderstanding of Rap and Hip-Hop music and how it can be used to help. Counseling especially is now more important than ever with the increased awareness of mental illness in the United States and around the world. Suicide rates are at the highest they’ve been in a long time especially in teens and youth and a lot of these kids talk about artists like Juice Wrld or Lil Peep who helped them get through rough times in their life where they thought the only way out was suicide. My next topic will be moving from a health perspective in counseling to ways in which rap and hip-hop have helped African American youth from an education perspective.
From my education experience I never really was forced to have music as a class until 5th grade when I had a required recorder class and we learned how to read basic sheets of music and perform songs in front of our peers. In a scholarly article titled “Connecting Black Youth to Critical Media Literacy Through Hip-Hop Making in the Music Classroom” a program called Foundations of Music encouraged participants to increase their effort and maximize their abilities in the classroom through making music of the hip-hop genre. The Foundation of Music program introduces students to both the process of writing lyrics of a rap song and the technology used to produce rap songs in a classroom. Each day the authors would record observations like the concept’s kids learned every day, reactions from student-to-student and student-to-teacher, along with informal conversations between the students. It was discovered that having the same group of kids come in every day and work on a new hobby built a sense of belonging among them that replicated what it felt like to be a part of a team. A common goal of bettering themselves every day and a sense of having an actual end goal of creating a song or producing a song helped them create a work ethic they weren’t otherwise used to or aware of. Many kids were also able to express their emotions and real-life experiences and let their stories be heard in their communities without being harassed by their normal teachers for talking during a lesson or being off topic. One of my research questions I’d like to answer with this topic would be just “How effective are these literacy practices involving rap music” and “How do African-Americans benefit as a whole from literacy teaching practices involving rap or hip-hop music.” In the article titled “Toward a Critical Pedagogy of popular Culture: Literacy Development Among Urban Youth”, the author talks about how educators have wanted to use new strategies and approaches to teach literacy to urban youth. It can be argued that hip-hop music is the representative voice of urban youth because it was created by and for urban youth, in addition to acting as voices in their urban communities’ rappers consider themselves educators and see at least a portion of their goal as raising consciousness of their communities. The author and his colleague in this article first designed a unit in their curriculum that incorporated hip-hop music and culture into a traditional senior English poetry unit. The major portion of the unit was a group presentation of a poem and a rap song from a historical period that was discussed in the class. The groups were asked to prepare a justifiable interpretation of their poem and song with relation to their specific historical and literary periods and analyze the links between the two. The students generated quality interpretations and made interesting connections between the poems and the rap songs. Their critical investigations of popular texts brought about oral and written critiques like those in college preparatory English classrooms. The students moved beyond critical reading of literary texts to become cultural producers themselves, creating and presenting poems that provided crucial commentary and encouraged action for social justice. Another area used by this study was teaching with popular film. The notion of films as visual texts worthy of academic study has been growing within the postsecondary academy for some time. The critical studies field has grown in prominence, and there are now academics who use critical theory to study film at nearly every major university in the U.S. During the units, the students watched the films in class while reading the accompanying texts at home. By combining popular film with canonical texts, the students were able to hone their critical and analytical skills and use them in interpretations. They were also able to understand the connection between literature, popular culture, and their everyday lives. Further they were able to translate their analyses into quality oral debates and expository pieces. While working with urban youth in Los Angeles, the author coordinated a group of research seminars that brought high school students to the local university to study access to corporate media and the corporate media’s portrayal of urban youth. The students read literature relating to critical media literacy and the sociology of education, designed a study, conducted interviews, analyzed countless hours of news coverage, and performed a content analysis of major U.S. daily newspapers. The author noticed that through the teens research process they were increasingly able to meaningfully draw upon personal experiences during the reading of texts concerning critical media literacy or during interviews they conducted with members of the mainstream media. Motivated and empowered by the prospect of addressing a real problem in their community, the students learned the tools of research, read difficult texts, and produced their own text of high academic merit.
The next topic I will move on to is the “healing power of hip-hop” as stated in an article written by authors Alexander Crooke and Raphael Travis Jr on theconversation.com. Hip-hop and rap culture alike have been criticized as a criminal threat and numerous studies have been undertaken on the harmful influence of hip-hop on kids. While there’s no denying that the lyrical content of hip-hop can be confrontational and many rappers do glorify violence and drugs if you look past certain artists and certain situations you find the “hidden gem” that everyone loves and enjoys. Hip-hop at its core is built on the values of social justice, peace, respect, self-worth, community, and having fun. That is why it is so increasingly popular to youth all around the world and why many kids alike idolize these artists and truly believe they are a therapeutic tool. At its simplest you can make a beat with your mouth or by using a pencil on a school desk or just recite lyrics about anything and with cost-friendly music creating software, young kids are able to take their talents to new levels and pathways to entrepreneurship. Aside from assisting African American youth in urban areas in career options, hip-hop music can also just be a way to cope with problems in their life. I know at least for me that in my first semester in college 10 hours away from home I have definitely used music as an outlet in many situations. In fact for the first week or two my roommates and I would come back from lacrosse practice, sit on the couch and listen to music or “vibe” as we call it. Each day we played different music depending on our mood and just talked about our problems or just listened to the music and relaxed. It was the only time we really interacted to be honest but after two or three days it was what I looked forward to the most in my day, just listening to music and screaming lyrics with my friends. In his U.S. based research Dr. Travis found that those who listen to hip-hop have strong benefits to individual mental health, in areas of coping, emotions, identity and personal growth, can help promote resilience in communities. Marginalized urban communities around the world share the feeling of resisting exclusion or discrimination and fighting for equity and justice and the rappers that come from these areas have a certain sound that echoes this feeling. Hip hop is not a cure or antidote and it isn’t perfect, but its promise is undeniable. It is a culture with complicated social and historical roots. Its complicated history enables us to critically reflect on our society, and forces us to face issues of race, privilege, class, and cultural appropriation.
I’d like to discuss a very controversial topic in today’s society for many reasons but the main one is that this topic often intertwines with African American youth today and I believe Rap and Hip-Hop music play a very big part in this. That topic would be Police brutality and the way in which Rap lyrics are used as a political force against it. In the scholarly article titled “Rap Music as a Positive Influence on Black Youth and American Politics” the author Natalie Wilson discusses lyrics from an artist named Ice-T in his song titled “Squeeze the Trigger”. He raps “Cops hate kids, kids hate cops. Cops kill kids with warnin’ shots. What is Crime and what is not? What is justice? I think I forgot.” The lyrics in this song are quite blunt but I do believe he is stating true information and addresses the grey area of our justice system. African-American youth are constantly the victims of homicide by cops in most cases they are unarmed and in most cases cops are let off with no charges. I believe a lot negativity in rap songs comes from the artist just speaking on the climate they were raised in whether it be around gang violence and drugs or living in harsh situations where their parents couldn’t provide them with certain necessities. Many young black men are in a situation in which they get a sudden sense of discomfort around police wondering of they’ll be the next hashtag or next face on a t-shirt that people are purchasing in order to support my family. I do understand that in some situations the teens or people are in the wrong and the media takes some stories are out of context but like Ice-T said cops kill kids with warning shots and certain precautions are not taken. I also understand that it can be out of self-defense but in cases in which the civilian is unarmed how are they supposed to protect themselves or even attack without a weapon. There is no question that black youth are unproportionally racially profiled and stooped and questioned simply because of their skin color. I will now discus an artist named Kendrick Lamar who is a positive role model to black youth across the U.S. as he persevered as a good kid and escaped the dangerous streets of Compton. In one of his songs titled “good kid” he shares his experience of gang violence while never being affiliated with one himself. He depicts memories of being jumped by gang members despite his disaffiliation, he is self-described as a good kid who stays out of trouble and attends bible studies regularly. When recognized by the wrong person he is a victim of conflict simply because he associates with friends who are gang members, he then recognizes he is a good kid trapped in a mad city, alluding to the title of this song being good kid and the title of the album m.A.A.d. city. I believe many young African American kids struggle with this situation and often turn to music as a way to escape their city and live a better life away from conflict.
In the next article I will be introducing titled “Hip-Hop & the Global Imprint of a Black Cultural Form” helps me take a slightly odd view on my thesis but nonetheless it states that hip-hop is one of the most popular genres’ in America and that it is really becoming the lingua franca for popular and political youth culture around the world. As hip-hop has skyrocketed in global popularity, its defiant and self-defining voices have been both multiplied and amplified as they challenge conventional concepts of identity and nationhood. Global hip-hop has emerged as a culture that encourages and integrates innovative practices of artistic expression, knowledge production, social identification, and political mobilization. The hip-hop nation is an international, transnational, multiracial, multiethnic, multilingual community made up of individuals with diverse class, gender, and sexual identities. While hip-hop heads come from all age groups, hip-hop culture is primarily youth driven. The global influence of hip-hop directly relates to its popularity as a major music source among youth in the United States. According to the national Gallup poll of adolescents between the ages of thirteen and seventeen in 1992, hip-hop music had become the preferred music of youth (26 percent). Along with hip-hop’s cultural norm of inclusion, global hip-hop remains symbolically associated with African Americans. It has incorporated many aspects of African American language ideology. Hip-hop presents African American English (AAE) as a symbolic and politicized dialect where speakers are aware of complex and contradictory processes of stigmatization, valorization, and social control. The hip-hop speech community is not necessarily linguistically and physically located but rather bound by this shared language ideology as part of politics, culture, social conditions, and norms, values, and attitude.
It would be unfair if after discussing all the positive effects and influence rap and hip-hop has on African American youth I didn’t discuss the negative effects. I will be doing so with the help of an article titled “How Hip-Hop holds Blacks Back” and it is by John H. McWhorter who’s podcast we listened to earlier this year in class. He believed that encouraging rap culture reinforced stereotypes that long hindered people of color, and by teaching young African Americans that a thuggish appearance or dialect is the “authentic” response to a presumptively racist society impedes future black success. Of course, not all hip-hop is belligerent or profane, entire CDs of gang-banging, police-baiting, and woman-bashing would get old fast to most listeners, but it’s the nastiest rap that sells the best, and the nastiest cuts that make a career. The top ten best-selling hip-hop recordings all celebrate the ghetto as “where it’s at”. Keeping the thug front and center has become the quickest and most likely way to become a star. So much so that many artists nowadays try to cultivate a gangsta image, even if they aren’t actually from an area they claim to be or if they never struggle like they say they do. Many fans, rappers, producers, and intellectuals defend hip-hop’s violence, both real and imagined as a revolutionary cry of frustration from disempowered youth. While I do agree with McWhorter on some of his stances about hip-hop, not all rappers or hip-hop artists preach violence and negative energy. I do believe there was a time period where there was a lot of civil unrest and racial tension where artists did just seem like their music was just angry rants about rival gangs or police or certain events but I believe that rap and hip-hop, like all things evolve and grow and we have a new generation of artists who are trying to turn the views of rap and hip-hop around. There will always be some artists that just rap to rap and say what they want to say but if you’re really looking for someone speaking real lyrics you can find it. That’s another great part of music that I enjoy, you can really find anything you want for your mood and it doesn’t always have to be someone speaking deeply about their story, you can just listen to someone mumbling over a cool beat if you want.
To conclude my paper, I will discuss my final thoughts on how rap and hip-hop influence African American youth. As I’ve stated many times above, music can be used in many ways to help people get through their days whether it’s playing music in the car or listening to a playlist while working out. So, music isn’t just tailored to those who are in tough times or those who need it to get out of a certain situation. I just believe that rap and hip-hop have had an extremely significant impact on African-American youth because to some of those kids it’s all they have, and even for me some days this semester when I missed home or just didn’t feel like doing anything, turning on some music was always my go-to. For some African American youth music is what drives them to do well in school, as you saw in the studies above adding music to a curriculum helped students stay engaged longer and helped them learn multiple advanced techniques just by creating what they thought was a silly rap. The study of rap and hip-hop songs helped counselors better understand their clients of color just by hearing what the artists had to say, it helped them come to a better understanding of possibly what some of their clients were going through and they were able to better connect with clients and truly fulfill their task of helping people feel better. Many artists are telling their stories of their youth through their songs and you really get a look into the good, bad, and the ugly. I believe that rap and hip-hop both get a bad reputation for being all about drugs, violence, or disrespecting women but maybe it’s just what these artists saw growing up and at that moment they weren’t able to tell right from wrong. I bring this up to say that we must come together as a society and understand the cries out for help and instead of just letting songs go by without any action we must get out and help these people and save them from their struggles and help break this everlasting cycle of poverty and recession in black communities. Especially with the political climate of the United States right now, there’s riots in the streets over a black man being killed by the police and there were protests in all 50 states at one point. It’s more important than ever to understand what is going on with African American youth and I believe that rap and hip-hop music are a good gateway to an inside look on their lives, of course their stories don’t represent all of the youth but there is a fairly good representation of different cities that rappers are from and each of their stories relate in some way or another. This topic has been a rollercoaster of emotions for me, from being confused at the start of what I really wanted to write about but I did enjoy truly understanding stories and seeing interpretations of a hobby so simple as listening to music because I do it just about every day.
Works Cited
Brooks, Michael. “Using Rap Music to Better Understand African American Experiences.” Taylor & Francis , 26 Feb. 2020, www.tandfonline.com/doi/abs/10.1080/15401383.2020.1732251.
Evans, Jabari. “Connecting Black Youth to Critical Media Literacy through Hip Hop Making in the Music Classroom.” Latest TOC RSS , Intellect, 1 July 2020, www.ingentaconnect.com/content/intellect/jpme/pre-prints/content-intellect_jpme_00020.
Morrell, Ernest. “Toward a Critical Pedagogy of Popular Culture: Literacy Development among Urban Youth.” Journal of Adolescent & Adult Literacy , vol. 46, no. 1, 2002, pp. 72–77. JSTOR , www.jstor.org/stable/40017507. Accessed 4 Nov. 2020.
Powell, Catherine Tabb. “Rap Music: An Education with a Beat from the Street.” The Journal of Negro Education , vol. 60, no. 3, 1991, pp. 245–259. JSTOR , www.jstor.org/stable/2295480. Accessed 4 Nov. 2020 .
Wilson, Natalie, “Rap Music as a Positive Influence on Black Youth and American Politics” (2018). Pop Culture Intersections . 21. https://scholarcommons.scu.edu/engl_176/21
McWhorter, John H., et al. “How Hip-Hop Holds Blacks Back.” City Journal , City Journal, 18 June 2019, www.city-journal.org/html/how-hip-hop-holds-blacks-back-12442.html.
Crooke Postdoctoral Research Fellow in Music Therapy, Alexander, and Raphael Travis Jr. Associate Professor of Social Work. “The Healing Power of Hip Hop.” The Conversation , 18 May 2019, theconversation.com/the-healing-power-of-hip-hop-81556.
“Positive Impacts.” Impacts of Rap Music on Youths , impactofrapmusiconyouths.weebly.com/positive-impacts.html.
Morgan, Marcyliena, and Dionne Bennett. “Hip-Hop & the Global Imprint of a Black Cultural Form.” Daedalus , vol. 140, no. 2, 2011, pp. 176–196. JSTOR , www.jstor.org/stable/23047460. Accessed 5 Nov. 2020 .
D’Amico, Francesca. “Welcome to the Terrordome: Race, Power and the Rise of American Rap Music, 1979-1995.” YorkSpace Home , 11 May 2020, yorkspace.library.yorku.ca/xmlui/handle/10315/37409.
Understanding Literacy in Our Lives by Amiri Austin is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License , except where otherwise noted.
Share This Book
Act on Student Ideas to Improve Mental Health, Youth Advocate Urges

- Share article
As schools confront a youth mental health crisis, they must engage students in finding solutions, said Rick Yang, 17, a senior at Scarsdale High School in New York.
The Jed Foundation (JED), an organization that promotes mental health and suicide prevention for teens and young adults, honored Yang as one of two recipients of its 2024 Student Voice of Mental Health Award in recognition of his state and local advocacy work.
Yang, who is Chinese American, was inspired to action when he saw the barriers a fellow Asian American friend faced in seeking mental health treatment during the COVID-19 pandemic. He attributes some of those barriers to the “model minority myth,” a term that refers to cultural stereotypes of Asian American students as high-achieving and academically gifted—a perception that may cause some adults and peers to overlook their needs.
He later advocated for wellness centers in his school district , and he co-founded “Frontiers of Fulfillment,” a group that provides online coaching for student leaders to advocate for policies like excused school absences for mental health.
This interview has been edited for length and clarity.
How did your experience during the COVID-19 pandemic influence your advocacy?
I was pretty isolated during [the beginning of] the pandemic. As an incoming freshman, I would say that my transition from middle school to high school wasn’t the greatest. I started high school half remote and half in-person, and it was pretty surreal to live in a world where I kind of stuck in my room most of the time.

I was pretty depressed, locked in my room, playing every video game you could possibly imagine. And sometimes I was even unable to eat dinner with my family. And I think it was certainly that experience, coupled with what I went through with my friend, that showed me that student mental health was a real concern that needed to be addressed.
My friend and I would FaceTime every night. She was depressed and wanted to seek help, but her parents wouldn’t let her at first. They eventually did, and she was actually diagnosed with bipolar disorder. Now she’s doing great; she’s thriving now.
My hypothesis is that—coming from a relatively high-achieving community with a lot of Asian Americans—the model minority myth prevented [her family] from seeking help. She’s a good student, and they didn’t want her to be perceived as weak.
How does your cultural identity as a Chinese American inform your work?
Oftentimes, culture and mental health are interconnected. When we approach mental health challenges in a certain community, I think it’s important to understand how the people in that community have grown up.
I try to highlight the diversity among Asian Americans because we are obviously not all the same. But a lot of us have encountered the model minority myth, even through subtle microaggressions in the hallways. I try to promote education among adults, including teachers, to break down some of the barriers that might keep students from seeking care.
How can schools more effectively address student mental health?
Mental health supports need to be comprehensive in order to effectively reach students. That means all students should be considered, supported, and protected. What works for one student may not help another. There is no one-size-fits-all approach.
What I admire about the Jed Foundation is [its] comprehensive approach to mental health promotion and suicide prevention. It recognizes that there are multiple areas of well-being—like learning about life skills, or having a counseling center—that can make a difference in someone’s life.
Ultimately, I think schools need to listen to the students themselves.
How did you advocate for student mental health in your school district?
The main initiative I started is called SchoolSight. In 2021, I realized the stress students faced at Scarsdale High School needed to be addressed. I attended a conference with Congressman Jamal Bowman where I essentially crafted a proposal to implement universal school-based wellness centers in Westchester County, which eventually blossomed into a countywide initiative.
The response was overwhelmingly enthusiastic. I began creating blueprints for introducing these [centers] in schools—universal wellness spaces for all students—starting with a pilot in my high school. So far, I’ve secured over $125,000 in grant funding to develop these spaces. They include things like de-stress zones with beanbags and yoga balls, board games, and places to study privately. Eventually, I’d like to see this scaled up to other districts.
What do you want educators to know about student mental health?
If we genuinely want to make a difference, we must not only allow but actively encourage young people to speak up. We must create environments where young people feel safe to express their thoughts, struggles, and ideas and treat them as equal partners. It fosters a sense of ownership and empowerment among the youth when they see their ideas and feedback being taken seriously.
I think school administrators, policymakers, community leaders must not only try to create platforms for youth to express their views, but they need to actually use that input in decision-making. Co-creation and agency are essential for young people to feel supported.
Sign Up for The Savvy Principal
Edweek top school jobs.

Sign Up & Sign In

- Share full article
Advertisement
California Congressional Primary Has a Rare Tie for a Runoff Spot
Never before has California’s primary system resulted in a three-way runoff for a congressional seat.
By Jill Cowan
Reporting from Los Angeles
- April 4, 2024
California’s primary system — in which the top two vote-getters, regardless of party, advance to the general election — has seeded plenty of unusual showdowns since it was established a little more than a decade ago.
But never before has the system resulted in a three-way runoff for a congressional seat.
That’s the situation facing three candidates in California’s 16th Congressional District, in the heart of the Silicon Valley, who could vie for the seat during a November runoff. The final count shows two primary candidates in an exact tie for second place.
After nearly a month of counting, both Evan Low, a state lawmaker, and Joe Simitian, a Santa Clara County supervisor, received 30,249 votes, or 16.6 percent each.
They trailed Sam Liccardo, the former mayor of San Jose, who received 38,489 votes, or 21.1 percent.
The three men — all Democrats — were among 11 candidates vying to replace Rep. Anna Eshoo, who opted not to run again after more than three decades in the House.
In California, vote counting takes several weeks because the state relies on mail balloting and gives latitude to voters who wait until Election Day to send their ballots. All county election officials are required to certify their March election results by Thursday.
But the tie for second place is not a certainty: Any campaign or any voter in the district can request a recount, as long as the request is filed within five days of the 31st day after the election — and as long as they pay for it. A full recount by hand would likely cost more than $300,000 . That means a recount can be requested as late as next Wednesday.
All three campaigns face a tough decision, said Paul Mitchell, a Democratic political consultant and political data expert. If Mr. Low or Mr. Simitian seek a recount, it could backfire; each could end up paying to knock himself out of the race.
And the campaigns likely don’t have data showing clearly that a two-person or a three-person race in November would be easier to win, Mr. Mitchell said.
Still, he noted that “it only takes one rich, eccentric person” to set the recount wheels in motion. “And they’re on every corner in this district.”
Both Mr. Low’s and Mr. Simitian’s campaigns declined to comment until the results were certified later Thursday. Mr. Liccardo’s campaign also declined to comment on whether he would request a recount.
“We welcome the opportunity to continue to talk to voters about the issues facing our communities, including the high cost of living, utility rates and housing and Sam’s long record of fighting on behalf of residents,” Mr. Liccardo’s campaign said in a statement.
Because of an editing error, an earlier version of the headline incorrectly described the tie in the congressional race. It is a two-way tie for second place, not a three-way tie.
How we handle corrections
Jill Cowan is a Times reporter based in Los Angeles, covering the forces shaping life in Southern California and throughout the state. More about Jill Cowan

COMMENTS
Health literacy is defined as "The degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisi ... This essay had considered a range of issues to do with health literacy including an estimation of the extent of the problem and strategies to ...
Introduction. Health literacy, as a term first proposed in the 1970s, 1 generally concerns whether an individual is competent with the complex demands of promoting and maintaining health in the modern society. 2 Over the past two decades, increasing attention has been attached to the concept due to its significant benefits to individual and public health and the sustainability of healthcare ...
Moreover, many patients have lost their lives because of misunderstanding discharge instructions (Boodman, 2011, p. 1). In essence, health literacy is very important to all stakeholders in health care settings. This is mainly because it ensures that patients follow the right instructions for their own safety. Moreover, it ensures that the right ...
This essay was published as part of a Special Issue on Misinformation and COVID-19, guest-edited by Dr. Meghan McGinty (Director of Emergency Management, NYC Health + Hospitals) and Nat Gyenes (Director, Meedan Digital Health Lab). ... Health literacy is crucial for health, and healthcare professionals must acknowledge and prioritize its ...
A. Physical health disparities: Discuss the health gaps in life expectancy, morbidity, and mortality rates between different socioeconomic groups. B. Mental health disparities: Examine the higher prevalence of mental health issues among disadvantaged populations, including depression, anxiety, and substance abuse.
Essay on Health Literacy. Decent Essays. 776 Words. 4 Pages. Open Document. Health Literacy. Health illiteracy has become referred to as the silent epidemic. According to the U.S. Department of Health and Human Services website, the National Assessment of Adult Literacy showed only 12 percent of adults have proficient health literacy.
This essay, "Health Literacy and Access to Healthcare Services: Problems, Interventions, and Suggestions for Improvements" is published exclusively on IvyPanda's free essay examples database. You can use it for research and reference purposes to write your own paper. However, ...
health literacy cost the US economy up to $238 billion every year, or 17 percent of all personal health-care expenditure (Vernon, 2007). Health literacy is an intermediate social determinant of health in a model where individual-level characteristics interact with context-dependent determinants and
BACKGROUND. In public health and health promotion, health literacy is considered an important resource for individual and collective empowerment (Nutbeam, 2000; Kickbusch, 2001).Among the different types of health literacies, critical health literacy (CHL) has recently gained increased attention in health research with the number of publications substantially increasing since 2010 (Benkert and ...
T. his National Action Plan to Improve Health Literacy is based on the principles that (1) everyone has the right to health information that helps them make informed decisions and (2) health services are delivered in ways that are understandable and beneficial to health, longevity, and quality of life.
A systematic review of available generic health literacy definitions and models for children and young people aged 18 or younger was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for ensuring high quality and transparent reporting of reviews [].Within this research, health literacy is regarded as a multidimensional ...
Health Literacy Essay. 888 Words4 Pages. - Introduction. Health literacy is about how a person is able to have access to health information that is accurate, understandable and actionable. It is dependent on the communication skills between individuals and a professional. Health literacy is important internationally where basic skills is needed ...
Health literacy is a topic of growing importance in European public health research. In general, health literacy is 'linked to literacy and encompasses people's knowledge, motivation and competences to access, understand, appraise, and apply health information in order to make judgments and take decisions in everyday life concerning healthcare, disease prevention and health promotion to ...
Health Literacy: A Necessary Element for Achieving Health Equity. A core aim for improving health care is to provide equitable care or "care that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status" (IOM, 2001). We believe that an essential ingredient in the ...
CDC Health Literacy. This site provides information and tools to improve health literacy and public health. These resources are for all organizations that interact and communicate with people about health, including public health departments, healthcare providers and facilities, health plans, government agencies, non-profit/community and advocacy organizations, childcare and schools, the media ...
Health literacy, the degree to which an individual can access, process, and comprehend basic health information and services in order to inform and participate in health decisions, 1 has a pivotal, decisive role in healthcare delivery and outcomes. Limited health literacy is an invisible barrier to healthcare delivery that has profound costs for individual and public health.
Health literacy is defined as "The degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisi ... This essay had considered a range of issues to do with health literacy including an estimation of the extent of the problem and strategies to ...
Organizational health literacy is the degree to which organizations equitably enable individuals to find, understand, and use information and services to inform health-related decisions and actions for themselves and others. These definitions are a change from the health literacy definition used in Healthy People 2010 and Healthy People 2020 ...
School of Public Health and Information Sciences, University of Louisville, Kentucky A report on colon cancer narratives for low-literacy adult learners focused on
An Overview of Medical and Public Health Literature Addressing Literacy Issues: An Annotated Bibliography. The National Center for the Study of Adult Learning and Literacy created this report presenting results from a computer-assisted search of the medical and public health literature addressing literacy issues in health care and in health promotion and education published between 1990 and ...
Health Literacy is the ability to read, understand and act upon health information. $73 billion is the estimated annual cost of low literacy skills in the form of longer hospital stays, emergency room visits, increased doctor visits, and increased medication ( National Academy on an Aging Society). Health Literacy represents the cognitive and ...
Pasadena, CA 91107. Phone: (626) 395-9989 ext. 19. Fax: (626) 395-9987. Contact: Faith Ruperto, Health Literacy Coordinator. Email: [email protected]. The goal of the California Health Literacy Initiative is to inform and partner with individuals and organizations to positively impact the health and well-being of individuals with low ...
3.5.3 Nursing literacy (research essay) 3.6.1 The effects of musical illiteracy (argument from experience) 3.6.2 Marching band literacy (synthesis) ... In his U.S. based research Dr. Travis found that those who listen to hip-hop have strong benefits to individual mental health, in areas of coping, emotions, identity and personal growth, can ...
As schools confront a youth mental health crisis, they must engage students in finding solutions, said Rick Yang, 17, a senior at Scarsdale High School in New York. The Jed Foundation, an ...
April 5, 2024, 9:00 a.m. ET. Once the Oakland A's leave the East Bay, it will mark the end of its existence in Oakland after 57 seasons. Jungho Kim for The New York Times. Sports fans in ...
Former President Donald J. Trump, who has portrayed jailed Jan. 6 rioters as martyrs in his effort to subvert the 2020 election, decried the guilty verdict in the jury trial of Rebecca Lavrenz, a ...
Never before has California's primary system resulted in a three-way runoff for a congressional seat. Sam Liccardo, the former mayor of San Jose, Calif., received the most votes in the primary ...