Avoiding preventable illness is the responsibility of individuals and their families, not governments. Do you agree?
Unauthorized use and/or duplication of this material without express and written permission from this site’s author and/or owner is strictly prohibited. Excerpts and links may be used, provided that full and clear credit is given to Writing9 with appropriate and specific direction to the original content.

Fully explain your ideas
To get an excellent score in the IELTS Task 2 writing section, one of the easiest and most effective tips is structuring your writing in the most solid format. A great argument essay structure may be divided to four paragraphs, in which comprises of four sentences (excluding the conclusion paragraph, which comprises of three sentences).
For we to consider an essay structure a great one, it should be looking like this:
- Paragraph 1 - Introduction
- Sentence 1 - Background statement
- Sentence 2 - Detailed background statement
- Sentence 3 - Thesis
- Sentence 4 - Outline sentence
- Paragraph 2 - First supporting paragraph
- Sentence 1 - Topic sentence
- Sentence 2 - Example
- Sentence 3 - Discussion
- Sentence 4 - Conclusion
- Paragraph 3 - Second supporting paragraph
- Paragraph 4 - Conclusion
- Sentence 1 - Summary
- Sentence 2 - Restatement of thesis
- Sentence 3 - Prediction or recommendation
Our recommended essay structure above comprises of fifteen (15) sentences, which will make your essay approximately 250 to 275 words.
Discover more tips in The Ultimate Guide to Get a Target Band Score of 7+ » — a book that's free for 🚀 Premium users.
- Check your IELTS essay »
- Find essays with the same topic
- View collections of IELTS Writing Samples
- Show IELTS Writing Task 2 Topics
The most important aim of science should be to improve people’s lives. To what extent do you agree or disagree with this statement ?
The personal information of many people is held by large internet companies and organisations. do you think the advantages of this outweigh the disadvantages, it is generally believed that some people are born with certain talents, for instance for sport or music, and others are not. however, it is sometimes claimed that any child can be taught to become a good sports person or musician. discuss both these views and give your own opinion., in spite of the advances made in agriculture,many people around the world still go hungry. why is this the case what can be done about this problem, some people feel that paparazzi should not follow celebrities and invade their privacy by taking pictures of them everywhere, while others believe this is just the price of fame. discuss both sides and give your opinion. give reasons for your answer, and include any relevant examples from your own knowledge or experience..
- Open access
- Published: 09 March 2022
Social responsibility perspective in public response to the COVID-19 pandemic: a grounded theory approach
- Lee Lan Low 1 ,
- Seng Fah Tong 2 ,
- Ju Ying Ang 3 ,
- Zalilah Abdullah 1 ,
- Maimunah A Hamid 4 ,
- Mikha Saragi Risman 1 ,
- Yun Teng Wong 1 ,
- Nurul Iman Jamalul-lail 1 ,
- Kalvina Chelladorai 1 ,
- Yui Ping Tan 1 ,
- Yea Lu Tay 1 ,
- Awatef Amer Nordin 1 &
- Amar-Singh HSS 5
BMC Public Health volume 22 , Article number: 469 ( 2022 ) Cite this article
6571 Accesses
4 Citations
18 Altmetric
Metrics details
Combating viral outbreaks extends beyond biomedical and clinical approaches; thus, public health prevention measures are equally important. Public engagement in preventive efforts can be viewed as the social responsibility of individuals in controlling an infectious disease and are subjected to change due to human behaviour. Understanding individuals’ perception of social responsibility is crucial and is not yet explored extensively in the academic literature. We adopted the grounded theory method to develop an explanatory substantive theory to illustrate the process of how individual responded to the outbreak from a social responsibility perspective.
In-depth interviews were conducted among 23 Malaysians either through telephone or face-to-face depending on the participant’s preference. Both purposive and theoretical sampling were used. Participants were invited to share their understanding, perceptions and activities during the COVID-19 pandemic. They were further probed about their perceptions on complying with the public health interventions imposed by the authorities. The interviews were audio-recorded and transcribed verbatim. Data was analysed via open coding, focus coding and theoretical coding, facilitated by memoing, sketching and modelling.
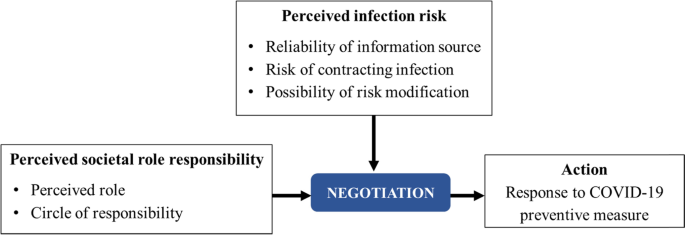
Study findings showed that, social responsibility is perceived within its role, the perceived societal role responsibility. In a particular context, an individual assumed only one of the many expected social roles with their perceived circle of responsibility. Individuals negotiated their actions from this perspective, after considering the perceived risk during the outbreak. The four types of behaviour depicted in the matrix diagram facilitate the understanding of the abstract concept of negotiation in the human decision-making process, and provide the spectrum of different behaviour in relation to public response to the COVID-19 pandemic.
Conclusions
Our study adopted the grounded theory approach to develop a theoretical model that illustrates how individual response to COVID-19 preventive measures is determined by the negotiation between perceived societal role responsibility and perceived infection risk. This substantive theoretical model is abstract, thus has relevance for adoption within similar context of an outbreak.
Peer Review reports
COVID-19 caught the world’s attention when it was declared a pandemic by the World Health Organisation (WHO) [ 1 ]. With its rapid spread within and between countries, COVID-19 was classified as a public health emergency of international concern that required a systematic international response [ 2 ]. COVID-19 is caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), which is a novel coronavirus similar to SARS-associated coronavirus (SARS-CoV) and Middle East Respiratory Syndrome Coronavirus (MERS-Cov) that infect the respiratory tract and cause severe respiratory infections. In December 2019, the disease was first reported in Wuhan City, China, in a wholesale food market and infected different groups of people such as stall owners, market employees and regular visitors [ 3 ]. Previously, Malaysia experienced a Nipah virus outbreak from September 1998 to May 1999 which resulted in 265 human cases affected and substantial economic loss to the pig-farming industry [ 4 , 5 ]. Other viral disease outbreaks such as H1N1 and SARS have also affected Malaysia, but none have caused as deep an impact on society as the current COVID-19 pandemic. Similar to other countries, Malaysia has faced challenges in containing the virus and in urging the general public to comply with preventive measures introduced by the government. The first measure that was implemented was the restriction of entry visas from Wuhan City after three Chinese citizens tested positive for COVID-19 in Malaysia on 25th January 2020 [ 6 ]. Subsequently, with the rapid rise in local cases, a country level lock-down with a Movement Control Order (MCO) was implemented starting on 18th March 2020, raising the alarm of potential threat to national security [ 7 , 8 , 9 ].
An MCO is only effective if there is adherence by the public as the virus spreads via human-to-human transmission. With the increasing burden of cases in the country, mirroring the spread that also occurred internationally, an urgent focus of the government was to prevent the spread and reduce the number of infected cases, thus relieving the strain on health resources. Various preventive measures such as the use of face masks, personal hygiene, restriction of travelling and physical distancing were necessary since vaccines are only just becoming available [ 10 ]. The outbreak occurred in an unprecedented manner, causing a burden that was felt by every level of the society. Members of society were urged to assume relevant responsibilities in controlling the spread of this disease, by complying with the MCO. Nevertheless, the action of each individual in adhering to the MCO may vary depending on each person’s perceptions of the disease. Thus, solely relying on community mitigation measures during a pandemic has limitations as it is difficult to change habitual behaviour such as hygiene and social interaction [ 11 ]. An evaluation of public knowledge and perception of SARS in Hong Kong showed that enhanced personal hygiene and health protective measures relied critically on public psychological responses and widespread perceptions and beliefs of the community at large [ 12 ]. The research group found considerable misinformation and false beliefs among the community in Hong Kong at an advanced stage of the SARS epidemic, despite the wide coverage and substantial mass media and public service announcements. Hence, public perception is very important in improving health risk communication, building public trust and cooperating with the government’s preventive effort to control an outbreak [ 13 ].
Combating viral outbreaks extends beyond biomedical and clinical approaches; thus, public health prevention measures are equally important. Hence, it is essential to understand the Malaysian public response to COVID-19 preventive measures. Malaysians should practise social responsibility by complying with the Standard Operating Procedure (SOP) and guidelines imposed by the government [ 9 , 14 ]. Public engagement in preventive efforts can be viewed as the social responsibility of individuals in controlling an infectious disease [ 15 ] and are subject to change due to human behaviour. While human behaviour is complex, many health behaviour models have been developed to understand health, behaviour and health system phenomena by incorporating various features of individuals, communities and organisations. Other health behaviour models include the health belief model [ 16 ] and the COM-B model [ 17 ]. Although the health belief model was established to study health-related phenomena [ 18 , 19 , 20 ], it has a limitation that it does not directly incorporate societal features such as social norms and community assumptions, which are assumed in underlying demographic factors [ 21 ]. The COM-B model introduced Capability, Opportunity and Motivation into a model by focusing on promoting individual behaviour adherence to public health interventions [ 22 ].
Studying human behaviour extends beyond the individual’s level and it involves examining collective efforts and societal participation. Understanding how people conceptualise social responsibility during an outbreak can provide useful information for improving future preventive and control interventions. Hence, this study aims to explore public conceptualisation of social responsibility and to develop a model explaining the role of social responsibility during the early COVID-19 pandemic in Malaysia.
Study design
In-line with the aim of developing an explanatory substantive theory explaining the role of social responsibility during the early COVID-19 outbreak, the grounded theory methodology was adopted [ 23 ]. An in-depth interview (IDI) was used to capture emic perspectives and provided a detailed account of a person’s view, reactions (personal responsibility) and social processes (social responsibility) among the general public during the early COVID-19 outbreak in Malaysia. The purposive sampling strategy was used with the intention of exploring a range of individuals from various social backgrounds and different experiences encountered in relation to the current pandemic. Subsequently, the theoretical sampling was applied to aid the saturation of the model, which enabled enrichment of data that could illustrate the process of how individuals perceived societal role responsibility within the outbreak environment. This led to the identification of a ‘core category’ for this study and the theoretical saturation.
Recruitment & participants
Participants were purposively recruited from different demographic backgrounds to elicit their diverse experience during the early COVID-19 outbreak. Potential participants were identified from the social networks of the research team as well as referrals by the social network among their friends. All participants selected resided in different locations within Malaysia when the interview was conducted. In total, 23 Malaysian adults with various sociodemographic were interviewed. Figure 1 shows the locations of study participants.
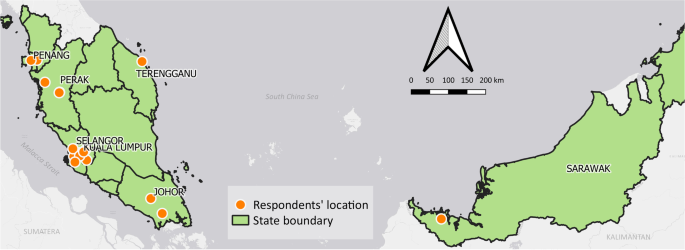
Malaysia map with locations of the selected participants. *Notes: respondents = study participants
Data collection
The interviews were conducted between March to July 2020 by researchers who were trained in qualitative method. The movement restriction order that was implemented during the worsening stages of COVID-19 outbreak in Malaysia [ 8 ] limited physical accessibility to conduct face-to-face interviews. This limitation was surmounted by conducting telephone interview. Hence, only one IDI was conducted face-to-face at the workplace based on the participant’s request, while the other 22 IDIs were through telephone interviews. A semi-structured interview guide was developed to facilitate IDI sessions, containing a list of questions pertaining to the understanding of COVID-19, “perceptions on the outbreak progression and consequences of the outbreak on everyday lives and activities”, “experiences and perceptions upon searching for and receiving COVID-19 information”, further probing to explore their “ways in handling the information received and reasons behind their actions”. Participants were also asked about their “activities and perceptions in complying with the public health interventions imposed by authorities during the outbreak”. The interviews sessions lasted between 25 and 110 min. They were conducted either in English, Malay or Mandarin language depending on the participant’s preference. Participant information sheet which included study objective, the purpose of the interview and the interview process was shared through email or WhatsApp message prior to the interview and informed consent was obtained from all participants. Assurance of confidentiality was given that data would be used only for this study. All IDIs were transcribed verbatim and cross-checked against audio recording by another team member to ensure accuracy of the transcripts. Data collection continued until data saturation. Upon interviewing 23 participants, no new emerging theme was observed from two consecutive IDIs. No repeat interviews were carried out since the information gaps were probed in the subsequent interviews.
The interviews were audio-taped as permitted by the participants, transcribed and imported into the Nvivo 11 (Qualitative data analysis computer software) to facilitate data analysis. Participants’ identifiers were replaced with researcher-assigned codes to maintain the anonymity of the transcripts prior to analysis. Data analysis began immediately after the first interview. Theoretical saturation was observed and achieved after 23 interviews, whereby no new categories were found to add further understanding of the complex human behaviour and social responsibility in facing the early COVID-19 outbreak. Data analysis involved various stages of coding, memoing, sketching and modelling. Coding began with open coding, followed by identifying categories and grouping. The coding process started with immersion in the data, whereby the texts were read several times before they were coded. Focus coding was carried out subsequently, followed by a theoretical coding. Eventually, the core category was identified, and the study theoretical framework was conceptualised. The core category “negotiation” was identified based on its ability to subsume the main categories in explaining the entire process of an individual’s conceptualisation of social responsibility and how they exercised their social responsibility.
The research team consisted of multi-disciplinary researchers with various experiences, composing those with experience in behavioural sciences (medical anthropologist), public health and clinical research, health systems research and primary care services. Trained in qualitative research and interviewing techniques, all research team members are fluent in English and Malay languages and a few are also fluent in Mandarin.
Ethical considerations
This study was registered with the National Medical Research Register (NMRR-20-574-54389). Ethical approval was granted by the Medical Research and Ethics Committee, Ministry of Health Malaysia (KKM/NIHSEC/ P20-701(7)). Participants’ identity and data confidentiality were assured throughout the data collection. Informed consent to participate and permission for audio recording were obtained from all participants prior to interviews.
The results of this study were obtained from in-depth interviews with 23 individuals from the general public between March to July 2020 in Malaysia. Table 1 summarises the characteristics of the participants. More than half were female (69.6%), Malay ethnic group (52.2%) and 78.3% of them had at least a tertiary education level. They ranged from 29 to 73 years old, work as public civil servants (39.1%), in private sector (39.1%) and 21.8% were retirees.
From the perspective of an individual’s obligation to act for the benefit of society, the participants conceptualised social responsibility from two dimensions: (1) the individual perceived roles in their society, and (2) the individual perceived circle of responsibility. To finally exercise social responsibility would involve individuals considering the perceived risk of infection.
The individual perceived role defines their actions. The extent of the action regarding the level of societal involvement depends on how wide a person casts his or her circle of responsibility in the society. Individuals often hold multiple roles; thus, their respective circles of responsibility vary, as are their actions. The individuals’ perception of infection risk is constructed from their response to information received and their self-efficacy in possible risk modification. Under a pandemic circumstance, the recommended preventive measures such as movement restriction, personal hygiene and the use of protective equipment are negotiated from this perspective of societal role responsibility. The negotiation involves reaching an agreement [ 24 ] and in the context whether one would decide to take the preventive measures deemed necessary. This negotiation is produced by the intersection between societal role responsibility and perceived infection risk.
Figure 2 shows the theoretical model, which illustrates that the individuals’ actions of social responsibility are a result of the intersection between perceived infection risk and societal role responsibility. These two are negotiated. The individuals’ perceived infection risk is constructed from their response to the information received and their self-efficacy in risk modification.
Public response to preventive measures from social responsibility perspective during the COVID-19 outbreak
Perceived societal role responsibility
The societal role is the perception of an individual. This role varies according to the context and current time since it depends on the type of relationship involved. A person can be a member of a workplace, family or society. Each role has a sense of responsibility attached to it, with obligations to be carried out by the individuals as members of the society. The type of relationship determines how far a person casts his or her circle of responsibility. There are two dimensions of societal role responsibility: the perceived role and the circle of responsibility.
Perceived role
The perceived role, which comes with a set of expected behaviours and conduct, influences a person’s decision in determining the best action [ 25 ]. A person can and often has multiple roles, but they only assume one role at a moment in time. For example, a person could be a mother who may also be a healthcare worker and an event host. Depending on her role in each situation, she would assume the role of a mother or a healthcare worker and think of the best interest for her children in some situations, and patients in other situations respectively.
A groom’s mother who was expected to take care of the guests’ safety in a wedding function stated the following:
“I am a mother, who was just about to organise my son’s wedding at that time. It was…not MCO yet, but it’s still in warning status…where we can still organise feast…. we’d like to hold the wedding…but in a safe way, as you would have to invite a lot of guests.” (P09, female, 52 y/o).
If a person became the host for a social event, he or she would be responsible for the comfort and safety of the guests. Despite his or her desire to host the event during the outbreak, the person was driven to consider the safety of others. Therefore, on the basis of the guests’ safety, he or she might cancel the event.
A social event host who was expected to take responsibility for his guests’ safety expressed:
“I wanted to keep it going but I was persuaded by my family to cancel it. I wasn’t really concerned about the epidemic, but it was getting serious and I got scared. What if the virus infected other people?” (P05, male, 29 y/o).
Similarly, a grandmother perceiving her responsibility towards the health of her grandsons stated:
“We always wear the mask, even for small kids, my little grandson. I wear it for him even though he doesn’t want to.” (P23, female, 61 y/o).
Circle of responsibility
The circle of responsibility depends on the size of the person’s definition of his or her social responsibility. There is a continuum of self, which is the smallest circle of responsibility, to as large a definition of society as one can perceive. The large circle of responsibility can stretch to include the global society and produce a more ‘collective effort’. The word ‘circle’ indicates that the circle can expand to a degree at the personal, society, national or global levels. Thus, the definition of this circle is personal, and defining it involves identifying the weight an individual would place on the importance of his or her personal goals such as health, enjoyment, life value, financial matters and societal relationship.
“[I wear] a mask because we [healthcare provider] are contacting patient in hospital, so we have… to protect ourselves” (P13, female, 33 y/o).
With the same act of adhering to public health measures, a large circle of responsibility expands beyond the self with the intention of avoiding spreading the disease to others.
“When I’m back from work or the supermarket, I must clean myself before meeting my family. I’m staying with my mom. When I’m back, I’ll shower before meeting her because as an elder, she’s at-risk group.” (P21, female, 45 y/o).
The “perceived societal role responsibility” cannot, by itself, explain a person’s societal behaviour regarding the pandemic; however, it forms the foundation for negotiation with a person’s perceived infection risk for an action he or she would take for preventive measures. While an intention to act may be present, the decision to act is balanced with the perceived infection risk.
Perceived COVID-19 infection risk
Since the content of pandemic information includes risk of exposure and the protective measures, the perceived infection risk among members of the society is an outcome of an individual’s assessment of how high the risk of contracting the infection and the possibility of reducing the risk through protective measures. Before the government announced COVID-19 mitigation strategies, some individuals developed early risk perception and practised preventive measures after discovering local disease spread. However, other individuals perceived the risk only when the government enforced an MCO, indicating an imminent risk of infection. With increasingly government intervention, which indicated a widespread disease transmission, individuals began to perceive a higher risk of infection and considered reducing the risk through some protective measures.
“When it began to spread here [in Malaysia] at that time…two weeks before the Prime Minister announced [the MCO], I was already scared of…this virus. Then, I started wearing a mask.” (P07, female, 61 y/o).
“I was a person that not really taking serious about this [pandemic], but when the government started to announce the lock-down or the movement restriction, that kind of [action] make me nervous… [that was] the point where I think… I have changed from not care to… give more concerned about it.” (P05, male, 29 y/o).
How an individual comprehends the disease risk depends on a few factors:
Reliability of information source
Insight into COVID-19 serves as the starting point from which an individual understands the risk and determines how to respond. Initially, COVID-19 information was available from multiple sources, allowing a person to create his or her personal perception of the information. The source and type of COVID-19 information varied, each carrying a different weight and reliability as perceived by the individual. At one end of the information spectrum is the verified information from credible sources such as announcements by health authorities and global news. An individual tends to value such information, especially the information received from recognised sources and media.
“I used to buy newspapers every day. So, usually I read papers, and then you see in the TV, the CNN and…other news.” (P02, male, 73 y/o).
In contrast, unverified social media such as Twitter, WhatsApp and Facebook are also sources of information for the public. However, the information from these sources carried less weight and was perceived as being less reliable.
“At that time, they (from Facebook) said that [MAEPS 8,24 ] was for those who came back from overseas (quarantine centre). Then, I WhatsApp my sister…because those who stayed in Malaysia knew better about it (to verify the information).” (P23, female, 61 y/o).
The source and type of COVID-19 information ranged from newspaper reports to individual opinions from respectable professionals. These sources were considered in variable weight and reliability.
“We have a number of people in our group…who are politicians and doctors. There are public health doctors in the group as well. All of us… [thought that] it’s okay to go to Australia… after all, Australia is safer than Malaysia. All the reports [showed that]… all the cases in Australia were in Sydney, Gold Coast, not in Perth. We were prepared to go actually…” (P03, female, 64 y/o).
The perceived risk of contracting the infection from public exposure
Risk through public exposure is perceived as how easy an individual could contract the infection while in public places. An individual perceived risk based on risk characteristics such as the infectious nature of the disease, proximity of infection based on the geographical spread, the similarity of social-cultural factors among infected individuals and one’s own susceptibility due to health status. A high perceived infection risk indicates that the infectious agent was easily spread, as well as positive cases were occurring in close proximity and in similar socio-cultural setting. A person also perceived high risk after assessing a location with high incidence of cases within their surroundings.
“At first, when I looked at the Wuhan [condition]…I wasn’t afraid yet, I thought it only happened in Wuhan and wouldn’t reach Malaysia, it’s just Wuhan.” (P07, female, 61 y/o).
“Once it reached Malaysia, I mean, Wuhan and Malaysia are far from each other. So, when it reached Malaysia, it’s quite bad… I assumed that it could be prolonged and turn into a pandemic.” (P11, female, 29 y/o).
“I did not take this [COVID-19] seriously…and then there was actually…a new virus. They firstly say it comes out from the wild animals where they [people in China] eat wild animal… Malaysian less likely to take these wild animals.” (P04, female, 33 y/o).
Possibility of risk modification through protective measures
An individual’s perceived infection risk could also be altered by their confidence in adopting some protection measures. The possibility of an individual engaging in risk modification is a personal evaluation of the effectiveness of protective measures, which may or may not be according to recommended guides or SOP. Confidence in protective measures is developed when the outcome of practising protective measures was evaluated and perceived as successful compared to the absence of protective measures.
“I have confidence in preventive measures because…before this, my child went to a childcare centre…mingled with other kids, who had fever and everything. So, my child always gets a fever. When he was staying at home, he never had any fever. I believe in… the importance of social distancing to protect us from COVID-19.” (P21, female, 45 y/o).
The negotiation
Public response to the COVID-19 pandemic, which was reflected by their actions during the pandemic, was preceded by their corresponding intentions to act. The intentions were constructed from their perceived societal role responsibility. These intentions to finally complete the act were negotiated after they considered their perception of the risk of infection. As part of the ‘negotiation’, placing a heavy weight on one’s self in the societal role responsibility may tilt the balance towards an act that benefits one’s own agenda over infection risk. For instance, a person could undervalue infection risk over an important social event.
“…but then again at that time, [it was] not so serious that you would protest against an assignment or project… So, that’s why I took the flight anyway.” (P14, male, 33 y/o).
A person has the autonomy to decide what is best for himself or herself amidst the outbreak and the government’s restriction order. Hence, his or her decision also illustrated how far a person could align himself to societal goals without disregarding personal goals.
“I’m worried because… the reception cannot be carried out. If we postpone [the wedding ceremony], we would never know when coronavirus is going to end. It could take one year, two years…five or six months. So, it would have been postponed due to an endless thing.” (P18, female, 33 y/o).
In a different context, a person’s perceived societal roles vary, as does the perceived infection risk. Figure 3 illustrates these negotiations and the resulting range of actions from a spectrum quadrant of the the two factors of perceived societal roles and perceived infection risk. The spectrums include the following: perceived high infection risk and small circle of societal role responsibility; perceived high infection risk and large circle of societal role responsibility; perceived low infection risk and small societal role responsibility; and perceived low infection risk and large societal role responsibility.
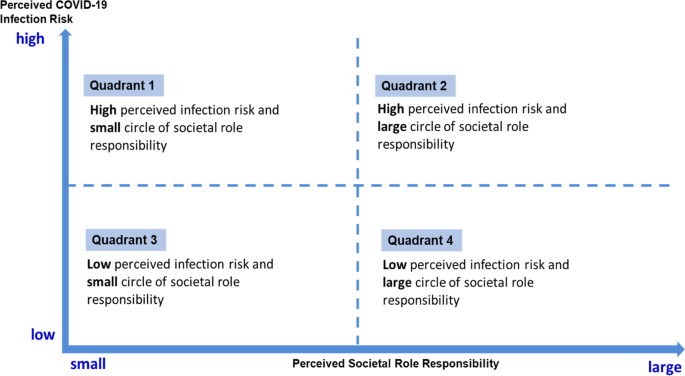
Intersection between perceived societal role responsibility and COVID-19 infection risk
Quadrant 1 Perceived high infection risk and perceived small circle of societal role responsibility
Perceived high risk of infection during a pandemic, places an individual at a “threatened” state of mind, thus invoking one’s “safeguarding” or “protecting” nature. However, from the perspective of a small role and circle of responsibility, the action was negotiated within the context of oneself and his or her safety, resulting in containing the action without intending to influence the behaviour of others.
“We have to get prepared [to wear a mask]… because the awareness of people around us is not very high, so we have to protect ourselves.” (P13, female, 33 y/o, perceived role: self).
Quadrant 2 Perceived high infection risk and perceived large societal role responsibility
Similarly, for a person who perceived a high infection risk with the perspective of a large role and circle of responsibility, the focus of his or her concerns expanded from oneself to others, especially those within the circle of care. The individual’s action was negotiated towards a proactive approach, aiming to mitigate others’ exposure to infection risk or influence others to reduce risky behaviour.
“If I go [abroad] and know that Spain is already very badly affected, I don’t want to be one of the culprits that bring back the virus. I think that [is] very irresponsible… Even though I self-quarantine at home, I don’t think it’s good…” (P06, female, 58 y/o, perceived role: a responsible citizen).
Quadrant 3 Perceived low infection risk and perceived small societal role responsibility
Perceived low risk of infection and small societal role responsibility placed an individual at ease and did not invoke the need to protect oneself or the society from the disease. As such, a perceived low infection risk of infection did not trigger an individual to adhere to preventive measures. The actions were negotiated for the benefit of oneself, guided by personal needs and interests. He or she was less concerned with the consequences of their actions on the society.
“Well, there’s nothing to be afraid of… I had this sea license by [the authority] when [the police] asked me where to go; I would just tell him that I am going to catch cockle. Our hobby is to go out to sea…and no one spreads (virus) to you.” (P17, male, 63 y/o, perceived role: self).
Quadrant 4 Perceived low infection risk and perceived large societal role responsibility
A person who perceived a low infection risk might not discern the necessity to negotiate a change of action or decision that has been made thus far. However, adequate information necessary for carrying out risk modification would be negotiated with the perceived large society role responsibility of a person. Eventually, some protective measures were adopted, and the benefit and safety of others would be taken into consideration.
“…rumours said that MCO might be enforced. People began asking me if the wedding would be continued. Since there’s no announcement yet, if Allah wills, we would continue it but after the announcement, we updated them that we could only do the marriage ceremony specifically for closed family members.” (P18, female, 33 y/o, perceived role: a host).
Action – response to COVID-19 preventive measure
Action is the outcome of the negotiation between perceived societal role responsibility and perceived infection risk. An individual might take preventive measures by complying with the SOP such as wearing a mask, cancelling his or her social event, avoiding crowded places and reducing activities or social events. However, the notion of social responsibility for each action was shaped by the negotiation. As the conceptualisation of social responsibility differs across individuals, a person’s action during a pandemic may also vary contextually.
Another action a person can take is sharing information. In a specific situation, such as the COVID-19 outbreak, delivering information about the outbreak or preventive measures was similar to risk communication. However, there was a sense of control over information sharing. For example, a healthcare worker acted as a gatekeeper for information that he or she received directly from his or her work organisation. Whether or not the worker should share information with family members or friends depended on his or her personal decision.
“Sometimes when I get news from MKN [National Security Council] or CPRC [National Crisis Preparedness and Response Centre] which I feel should be shared with my family members or friends, I will do that.” (P08, female, 56 y/o).
A person’s action can also help prevent the spread of infection for self-protection or for public good. A person who perceived a larger societal role responsibility included the safety of oneself and others in his or her actions to prevent the spread of infection by adhering to specific SOPs.
“The best thing is just to try to avoid gathering, because I got…two risk [groups]… My father-in-law…they are old….and my kids. So, I don’t want to be infected by this thing and bring it to my family.” (P15, male, 35 y/o).
The individual’s action is generally similar for those who perceive high infection risk, but there is a variation in explaining their actions from the perspective of social role responsibility. He or she would generally adhere to guidelines during a pandemic. However, one’s actions vary considerably when he or she perceives low infection risk.
This study developed a substantive theoretical model to illustrate the process of how individuals responded to an early COVID-19 outbreak from the perspective of social responsibility. Individual response to COVID-19 was directly constructed from their perceived societal role responsibilities and further negotiated after considering the risk of infection. “Negotiation” was identified as an important intersection within this process. The different spectrums of social responsibility within an individual and among the society during the pandemic were noted to be the foundation for this negotiation to take place.
A pandemic urgently requires multi-disciplinary teams to work together, including and not limited to public health, clinical scientists, pharmaceutical industry and health policy specialists. The public also plays a significant role in mitigating the situation. Hence, understanding human behaviour is equally important since personal behaviour is a key factor in reducing the transmission of respiratory viruses [ 22 ]. Social scientists have acknowledged the importance of understanding the COVID-19 pandemic response from the social and behavioural lens and have highlighted some insights for outbreak preparedness [ 26 ]. Other public health frameworks such as the Health Belief Model [ 16 , 21 ] and the COM-B Model [ 22 ] may provide behaviour diagnosis and reinforce mitigation behaviours during the outbreak of COVID-19 through careful arrangement of compliance with public health measures. The Health Belief model [ 21 ] focuses on the perceived threat, benefits, barriers and efficacy in mitigating the COVID-19 infection and focuses on the person’s perception of the disease; however, the health belief model does not incorporate society perspective although the pandemic is a condition closely related to the society [ 16 ]. The COM-B model has described a wide range of principles that can encourage individuals to engage in COVID-19 preventive behaviour [ 22 ]. The COM-B model indicates that preventive behaviour can only be practised when an individual has both the capability and the opportunity to show this behaviour; individuals are more motivated to choose personal protective behaviour. It shows that three components (Capability, Opportunity and Motivation) are closely linked to a person’s behaviour. COM-B model states that capability and opportunity are the primary parts of the model; however, during the MCO period, capability and opportunity were present, variation in behaviour remain.
Our model provides the additional contextual perspectives of the effect of infection risk, societal role and responsibilities perceived by individuals in negotiating behaviour for preventing COVID-19 infections. The government and many other authorised agencies may play a crucial role in influencing individual health behaviour but only to some extent. Our model implies that individuals exercise autonomy in determining which action to take when mitigating COVID-19 infection. Motivation to modify behaviour is contextual since it is derived from perceived societal role responsibility and infection risk. Our model provides a contextual relevance of undesirable behaviours. The MCO is seen as an undesirable event, and there was a tension between self and society as highlighted in our model. The important process of “negotiation” results in variation of behaviour, corresponding to perceived infection risk, whether low or otherwise. Importantly, our model presents a novel context – the context of pandemic; furthermore, it shows that undesirable behaviour is easy to engage with during the pandemic. Thus, capability and opportunity as highlighted in the COM-B model can be applicable during this situation. However, motivation varies across individuals, which is where our model offers substantive value.
Social responsibility is a perceived value which is significantly apparent across layers of society. However, application of social responsibility is commonly understood at the corporate level, which is defined as “any ‘responsible’ activity that allows a firm to achieve a sustainable competitive advantage, regardless of motive” [ 27 , 28 ]. The individual perspective is equally important. From the same perspective, collective efforts in facilitating health improvement have gradually emphasised personal control over individual health behaviour through health education in order to create a collective social responsibility [ 29 ]. Such efforts were driven by the assumption that each individual could change societal norms through their habits or modifications of their lifestyles [ 30 ]. In 1986, the WHO promoted health as “a process of enabling people to increase control over, and to improve their health” [ 31 ]. The conventional health education is disease-oriented and has been used extensively in managing communicable and non-communicable diseases. In this study, we found the individual’s perspective was useful in analysing public health interventions during a pandemic situation. We found that an individual’s action is shaped by the tension between individual agenda and social responsibility, before the negotiation with perceived infection risk. This model provides a framework for Malaysian social responsibility during the COVID-19 outbreak and insights into understanding the interplaying elements. The time frame of the interviews was in the early stages of the outbreak in Malaysia, around the same time the MCO commenced; this was considered in the analysis of the findings. Nevertheless, these perceptions depict an early visualisation of individuals’ response to a pandemic and potentially shifts accordingly as the pandemic progresses.
Policy implication, strengths and limitations
In terms of policy implication, our model explains that the action of a person during the early COVID-19 pandemic was the outcome of the “negotiation” between perceived societal role responsibility and perceived risk infection. In order to influence an individual’s response to an outbreak, the information provided to the public needs to articulate the exact role a person should play. Associations and organisations can empower members of the society by emphasising their potential roles during the pandemic and recommend actions. However, the spectrum of social responsibility in a different context indicates that human behaviour is complex, and a person’s action is influenced by the negotiation within a person. Hence, risk communication strategies could incorporate the element of negotiation, with clear SOPs that portray the importance of social responsibility during a pandemic. Authority figures could optimise various platforms to play their specific roles, such as an educator, adviser, or informer to alert society members and protect the public. Our model is useful for developing new norms during a pandemic and future intervention for behaviour change by emphasizing human negotiation behaviour.
By adopting a grounded theory approach, this study provides a substantive theory derived from emerging empirical data that attempts to explain the societal role responsibility during the COVID-19 outbreak. To enhance the theory, the sampling strategy used purposeful and theoretical sampling to ensure a maximum variation of demography and data collection within the context of an outbreak. In addition, the findings from this study can provide insight to various stakeholders, from health managers to policy makers, to strengthen preparedness for future outbreaks by understanding the spectrum of individual behaviours. The results from the ground up yielded valuable information with relevance to an outbreak context. Nevertheless, the context was in Malaysian, in the early stages of the outbreak, when resources and economic factors were not a major issue.
The role of social responsibility has not been explored extensively in the academic literature, though it has been mentioned by country leaders and in risk communication materials. Our study adopted the grounded theory approach to develop a theoretical model that illustrates how individual response to early stage of COVID-19 preventive measure is the outcome of the negotiation between perceived societal role responsibility and perceived infection risk. The matrix diagram with the four types of behaviour facilitates the understanding of the abstract concept of negotiation in individual’s decision-making process. It also provides the spectrum of different types of behaviour in relation to public response to the COVID-19 pandemic. Although the model was conceptualised during the early stage of COVID-19 outbreak in Malaysia, we believe the model has relevance for adoption within the similar context of a disease outbreak.

Availability of data and materials
The dataset that support the findings of this article belongs to this study (The role of social responsibility during COVID-19 outbreak, NMRR-20-574-54389). At present, the data are not publicly available but can be obtained from the corresponding author and Head of Centre for Biostatistics & Data Repository, National Institutes of Health, Ministry of Health Malaysia on reasonable request and with the permission from the Director General of Health, Malaysia.
Abbreviations
Capability, Opportunity and Motivation Behaviour
in-depth interview
Movement Control Order
Middle East Respiratory Syndrome Coronavirus
Severe Acute Respiratory Syndrome Coronavirus 2
Standard Operating Procedure
World Health Organisation
World Health Organization [WHO]: Coronavirus disease. (COVID-19): situation report, 51. In. Geneva: World Health Organization; 2019. p. 2020.
Google Scholar
World Health Organization: Addendum to Fact Sheet 15 on National Implementation Measures for the InternationalHealth Regulations 2005 (IHR): COVID-19 as a Public Health Emergency of International Concern (PHEIC) under the IHR. In.: The Verification Research Training and Information Centre [VERTIC],; 2020.
World Health Organization [WHO]: Coronavirus disease 2019 (COVID-19): situation report, 94. In. Geneva: World Health Organization; 2020.
John Oxford, Paul Kellam, Collier L: Human Virology Fifth Edition, 5th edn. New York, United States of America: Oxford University Press; 2016.
Looi LM, Chua KB: Lessons from the Nipah virus outbreak in Malaysia. Malaysian Journal of Pathology 2007, 29(2):63–67.
Expatriate Application For People Republic Of China (PRC) Passport Issued in Wuhan City, Hubei Province of China https://esd.imi.gov.my/portal/latest-news/announcement/announcement-for-coronavirus-outbreak/
Tang KHD. Movement control as an effective measure against Covid-19 spread in Malaysia: an overview. J Public Health. 2022;30:583–586.
Shakirah MS, Ang ZY, Jailani AS, Cheah KY, Kong YL, Selvarajah S, Balqis-Ali NZ, Fun WH, Sararaks S. The COVID-19 Chronicles of Malaysia. Setia Alam, Selangor: National Institutes of Health; 2020.
Institute for Health Systems Research: Universal Health Coverage and COVID-19 Preparedness & Response (Malaysia). In.; 2020.
Khosravi M: Perceived Risk of COVID-19 Pandemic: The Role of Public Worry and Trust. Electronic Journal of General Medicine 2020, 17(4):em203.
Article CAS Google Scholar
Cowling B, Ng D, Ip D, Liao Q, Lam W, Wu J, Lau J, Griffiths S, Fielding R: Community Psychological and Behavioral Responses through the First Wave of the 2009 Influenza A(H1N1) Pandemic in Hong Kong. The Journal of infectious diseases 2010, 202:867–876.
Article Google Scholar
Leung GM, Lam TH, Ho LM, Ho SY, Chan BHY, Wong IOL, Hedley AJ: The impact of community psychological responses on outbreak control for severe acute respiratory syndrome in Hong Kong. Journal of Epidemiology & Community Health 2003, 57(11):857–863.
Cori L, Bianchi F, Cadum E, Anthonj C. Risk Perception and COVID-19. International journal of environmental research and public health. 2020;17(9):3114.
Health DG calls for Malaysians to practise social responsibility https://focusmalaysia.my/mainstream/health-dg-calls-for-malaysians-to-practise-social-responsibility/
Baker JA: Real risk of resurgence in COVID-19 cases, clusters if too many activities resume too quickly: Gan Kim Yong. In.; 4 June 2020.
Rosenstock IM, Strecher VJ, Becker MH: Social Learning Theory and the Health Belief Model. Health Education & Behavior 1988, 15(2):175–183.
CAS Google Scholar
West R, Michie S. A brief introduction to the COM-B model of behaviour and the PRIME theory of motivation. 2020. Available at: https://www.qeios.com/read/WW04E6.2/pdf . Accessed 2 Mar 2022
Skinner BF: The Behavior of Organisms: An Experimental Analysis. New York: Appleton- Century- Crofts, Inc.; 1938.
Turner AP, Kivlahan DR, Sloan AP, Haselkorn JK: Predicting ongoing adherence to disease modifying therapies in multiple sclerosis: utility of the health beliefs model. Multiple sclerosis 2007, 13(9):1146–1152.
Ghaffari M, Tavassoli E, Esmaillzadeh A, Hassanzadeh A: Effect of Health Belief Model based intervention on promoting nutritional behaviors about osteoporosis prevention among students of female middle schools in Isfahan, Iran. Journal of education and health promotion 2012, 1:14.
Carico RR Jr, Sheppard J, Thomas CB. Community pharmacists and communication in the time of COVID-19: applying the health belief model. Res Social Adm Pharm. 2021;17(1):1984-7.
West R, Michie S, Rubin GJ, Amlot R: Applying principles of behaviour change to reduce SARS-CoV-2 transmission. Nature human behaviour 2020, 4(5):451–459.
Creswell JW, Poth CN. Qualitative Inquiry and Research Design Choosing among Five Approaches. 4th ed. Thousand Oaks: SAGE Publications, Inc.; 2018.
Cambridge Dictionary https://dictionary.cambridge.org/dictionary/english/negotiation]
Kundu SC, Kumar S, Lata K. Effects of perceived role clarity on innovative work behavior: a multiple mediation model. RAUSP Manag J. 2020;55(4):457-72.
Bavel JJV, Baicker K, Boggio PS, Capraro V, Cichocka A, Cikara M, Crockett MJ, Crum AJ, Douglas KM, Druckman JN et al : Using social and behavioural science to support COVID-19 pandemic response. Nature human behaviour 2020, 4(5):460–471.
McWilliams A, Siegel DS: Creating and Capturing Private and Social Value: Strategic Corporate Social Responsibility, Resource Based Theory and Sustainable Competitive Advantage. Journal of Management 2011, 37(5):1480–1495.
Kritas D, Tzagkarakis S, Atsipoulianaki Z, Sidiropoulos S: The Contribution of CSR during the COVID-19 Period in Greece: A Step Forward. HAPSc Policy Briefs Series, 2020, 1(1):238–243.
Takala T, Paul P: Individual, Collective and Social Responsibility of the Firm. Business Ethics: A European Review 2002, 9:109–118.
Minkler M. Personal Responsibility for Health? A Review of the Arguments and the Evidence at Century’s End. Health Education & Behavior. 1999;26(1):121–40.
World Health Organization. The Ottawa Charter for Health Promotion. In: International Conference on Health Promotion. 1st ed. Canada: Ottawa; 1986.
Download references
Acknowledgements
The authors would like to thank the Director General of Health Malaysia for the permission to publish this paper. The authors are also immensely grateful to all participants who participated in this study. We would like to thank Mr Jabrullah AB Hamid, the GIS analyst for generating image for the purpose of this publication.
This study was made possible with funding from the National Institutes of Health, Ministry of Health Malaysia research grant [(110)KKM/NIHSEC/800-3/2/2 Jld.10]. Publication of this article was sponsored by the Ministry of Health Malaysia. The funder is a stakeholder of the study but did not participate in the study process.
Author information
Authors and affiliations.
Institute for Health Systems Research, National Institutes of Health Malaysia, Ministry of Health Malaysia, B2, Jalan Setia Murni U13/52 Seksyen U13, Bandar Setia Alam, Selangor, 40170, Shah Alam, Malaysia
Lee Lan Low, Zalilah Abdullah, Mikha Saragi Risman, Yun Teng Wong, Nurul Iman Jamalul-lail, Kalvina Chelladorai, Yui Ping Tan, Yea Lu Tay & Awatef Amer Nordin
Department of Family Medicine, Faculty of Medicine, Universiti Kebangsaan Malaysia, Jalan Yaacob Latif, Bandar Tun Razak, 56000, Cheras, Kuala Lumpur, Malaysia
Seng Fah Tong
Clinical Research Centre, Hospital Raja Permaisuri Bainun, Ministry of Health Malaysia, Level 4, Ambulatory Care Centre (ACC), Jalan Raja Ashman Shah, 30450, Ipoh, Perak, Malaysia
Ju Ying Ang
Department of Community Medicine, School of Medicine, International Medical University Malaysia, No. 126, Jalan Jalil Perkasa 19, Bukit Jalil, 57000, Kuala Lumpur, Malaysia
Maimunah A Hamid
Galen Centre for Health and Social Policy, Suite C-13A-12, Block C, The Scott Garden SOHO, Jalan Klang Lama, 58100, Kuala Lumpur, Malaysia
Amar-Singh HSS
You can also search for this author in PubMed Google Scholar
Contributions
LLL (Principal Investigator for this project), TSF, ZA, NIJ, KC, TYL, ASH were involved in conception and design of this study. LLL, AJY, ZA, NIJ, KC, TYP, AAN were involved in data collection, LLL, TSF, AJY, ZA, MAH, MSR, WYT, NIJ, KC, TYP, TYL, AAN contributed to the data analysis. LLL, TSF, AJY, ZA, MAH, MSR, WYT, ASH involved in drafting and writing the manuscript. All authors read and approved the final version of manuscript for publication and agreed to be responsible for all aspect of the manuscript that in ensuring that questions related to accuracy or integrity of any part of the manuscript are appropriately investigated and resolved.
Corresponding author
Correspondence to Lee Lan Low .
Ethics declarations
Ethics approval and consent to participate.
This study was registered in the National Medical Research Register, Ministry of Health Malaysia (NMRR-20-574-54389). Ethical approval was granted by the Medical Research and Ethics Committee, Ministry of Health Malaysia (KKM/NIHSEC/ P20-701(7)). Informed consent was obtained from the participants in this study and permission for audio recording were obtained from participants prior to interviews. In addition, confidentiality of participants involved was assured throughout the data collection and all methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Low, L.L., Tong, S.F., Ang, J.Y. et al. Social responsibility perspective in public response to the COVID-19 pandemic: a grounded theory approach. BMC Public Health 22 , 469 (2022). https://doi.org/10.1186/s12889-022-12819-4
Download citation
Received : 09 August 2021
Accepted : 21 February 2022
Published : 09 March 2022
DOI : https://doi.org/10.1186/s12889-022-12819-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Social responsibility
- Societal role
- Infection risk
- Theoretical model
- Qualitative
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Advancing Health Equity, Eliminating Health Disparities, and Improving Population Health
EDITORIAL — Volume 18 — August 12, 2021
Leonard Jack Jr, PhD, MSc 1 ( View author affiliations )
Suggested citation for this article: Jack L Jr. Advancing Health Equity, Eliminating Health Disparities, and Improving Population Health. Prev Chronic Dis 2021;18:210264. DOI: http://dx.doi.org/10.5888/pcd18.210264 external icon .
Non-Peer Reviewed
Author Information
In June 2017, Preventing Chronic Disease (PCD) invited a panel of 7 nationally recognized experts in scientific publishing to respond to key questions about the journal’s mission, quality of scientific content, scope of operations, intended audience, and future direction (1). PCD and the panel of experts recognized that chronic disease is a major contributor to poor health outcomes, an increase in health care costs, and a reduction in quality of life. Reducing the burden of chronic disease is a challenge requiring diverse collaborations and dissemination and adoption of effective interventions in multiple settings. The expert panel strongly encouraged the journal to focus more on complementing its rich body of published work on epidemiological studies with content that is attentive to evaluating population-based interventions and policies.
Since its inception in 2004, PCD’s mission has been to promote dialogue among researchers, practitioners, and policy makers worldwide on the integration and application of research findings and practical experience to address health disparities, advance health equity, and improve population health. To better advance that mission, PCD used the panel’s recommendations to refine the journal’s focus, addressing 4 main areas of public health research, evaluation, and practice:
Behavioral, psychological, genetic, environmental, biological, and social factors that influence health
Development, implementation, and evaluation of population-based interventions to prevent chronic diseases and control their effect on quality of life, illness, and death
Interventions that reduce the disproportionate incidence of chronic diseases among at-risk populations
Development, implementation, and evaluation of public health law and health policy–driven interventions
Refining the focus on these 4 areas has allowed PCD to receive a wide range of content from authors around the world. In addition to manuscripts received through the journal’s regular submission process, PCD has issued calls for papers on topics that bring to the forefront timely public health issues and targeted public health responses to improve population health.
Advancing health equity and eliminating health disparities have been and continue to be critical factors to PCD in addressing these topic areas. Healthy People 2020 defines health equity as the attainment of the highest level of health for all people (2). According to Healthy People 2020, “Achieving health equity requires valuing everyone equally with focused and ongoing societal efforts to address avoidable inequalities, historical and contemporary injustices, and the elimination of health and health care disparities” (2). Healthy People 2020 defines health disparities as “a particular type of health difference that is closely linked with social, economic, and/or environmental disadvantage” (2).
As part of its mission to address these important issues, PCD is excited to release this collection, “Advancing Health Equity, Eliminating Health Disparities, and Improving Population Health.” Of the 17 articles in the collection, 10 were submitted in response to PCD’s call for papers for the collection and 7 were previously published in the journal. All articles underwent the journal’s rigorous peer-review process. In addition, this collection features a position statement on the journal’s commitment to advancing diversity, equity, and inclusion in its scientific leadership, peer review process, research focus, training, and continuing education (3).
Over the past decade, there has been a range of community-based, technically innovative, and clinically driven prevention strategies in public health to prevent and reduce the burden of chronic conditions among diverse populations worldwide. Articles in this collection describe innovative and successful work to address factors contributing to advancing health equity, eliminating health disparities, and improving population health. They provide the latest information on ways to better understand contextual factors responsible for influencing health outcomes (both negatively and positively) and effective approaches to improve population health among diverse populations in various settings. The 18 articles address these core themes from multiple perspectives:
PCD’s Commitment to Advancing Diversity, Equity, and Inclusion in Its Scientific Leadership, Peer Review Process, Research Focus, Training, and Continuing Education (3)
Engaging With Communities — Lessons (Re)Learned From COVID-19 (4)
Global Perspectives on Improving Chronic Disease Prevention and Management in Diverse Settings (5)
Reaching the Hispanic Community About COVID-19 Through Existing Chronic Disease Prevention Programs (6)
Community Engagement of African Americans in the Era of COVID-19: Considerations, Challenges, Implications, and Recommendations for Public Health (7)
Addressing Racial and Ethnic Disparities in COVID-19 Among School-Aged Children: Are We Doing Enough? (8)
A Framework for Mobilizing Health Care to Respond to the Community Within the COVID-19 Pandemic (9)
Addressing Emotional Wellness During the COVID-19 Pandemic: The Role of Promotores in Delivering Integrated Mental Health Care and Social Services (10)
COVID-19 and Chronic Disease: The Impact Now and in the Future (11)
Screening and Referral Care Delivery Services and Unmet Health-Related Social Needs: A Systematic Review (12)
Community and Research Perspectives on Cancer Disparities in Wisconsin (13)
Urban–Rural Disparities in Access to Low-Dose Computed Tomography Lung Cancer Screening in Missouri and Illinois (14)
Quantification of Potential Inequities in Breast Cancer Incidence in New Mexico Through Bayesian Disease Mapping (15)
HbA 1c Performance in African Descent Populations in the United States With Normal Glucose Tolerance, Prediabetes, or Diabetes: A Scoping Review (16)
Reducing Tobacco Use in Oregon Through Multisector Collaboration: Aligning Medicaid and Public Health Programs (17)
“We’re, Like, the Most Unhealthy People in the Country”: Using an Equity Lens to Reduce Barriers to Healthy Food Access in Rural Appalachia (18)
Oral Health Behaviors in Very Young Children in Low-Income Urban Areas in Chicago, Illinois, 2018–2019 (19)
A Randomized Trial to Improve Adherence to Follow-up Eye Examinations Among People With Glaucoma (20)
Positioning a scientific journal to address matters related to diversity, equity, and inclusion requires careful and intentional thinking and action. Going back to PCD’s inaugural issue in 2004, featuring an essay on social determinants of health by Dr Leonard Symes, professor emeritus of epidemiology at the University of California, Berkeley, the journal has created a space to highlight the importance of these topics in chronic disease prevention and health promotion. Since that first issue, PCD has continued to demonstrate a dedication to these issues at all levels: through its leadership and staff, the content it publishes, its expanding pool of talented volunteers (PCD’s external review panel, editorial board, associate editors, statistics review committee), the rigorous peer-review process, a comprehensive and inclusive variety of article types, calls for papers related to these issues, and more. In its 18 years of publication, PCD has consistently worked to assure the public of its commitment to achieving diversity, equity, and inclusion.
Peer-reviewed journals around the world are also focusing attention on these issues. In keeping with this movement, as PCD’s editor in chief I have authored the first article featured in this collection, which is a position statement on the steps already taken by the journal, steps planned for the next 5 years, and key measurable outcomes (3). PCD hopes to serve as a model in identifying and implementing best practices for diversity, equity, and inclusion to build an even stronger trust with the public.
And trust is needed: mistrust of the health care system has emerged as a primary barrier among members of communities of color to seeking care in health care systems (21). Mistrust stems from historical events, including the Tuskegee syphilis study, and is reinforced by health system issues and discriminatory events that continue to this day (21). This collection includes an article by Michener and colleagues, which posits that COVID-19 has underscored long-standing societal differences in drivers of health (4). The authors offer insights into this historical reality and suggest using a health equity lens to engage communities at risk of poor health outcomes, improve bidirectional communication, establish data sharing, and improve involvement in program implementation, dissemination, and evaluation. Authors share concrete ways these can be achieved by presenting successful examples around the US.
The global impact of COVID-19 among people at risk or living with a chronic condition in multicultural communities necessitates that health communication messages are created and delivered from a health equity perspective (22). Airhihenbuwa and coauthors, in their commentary, discuss the importance of culture in unpacking messages that may be the same globally (eg, physical/social distancing) yet different across cultures and communities (individualist vs collectivist) (5). Authors discuss how use of the PEN-3 framework can facilitate a community-engaged communication response to COVID-19.
Populations with low socioeconomic status and certain racial and ethnic groups (eg, Native American, Hispanic, and African American people) have historically been disproportionately affected by chronic disease, COVID-19 diagnosis, hospitalization, and mortality (23). Calo and associates discuss how COVID-19 has disproportionately affected Hispanic communities throughout the US (6). This commentary describes how Better Together REACH, a community–academic coalition promoting chronic disease prevention, and Project ECHO (a telementoring program based at Penn State University), were adopted to support a coordinated COVID-19 response in the Hispanic community in Pennsylvania. Authors provide insights into how the existing infrastructure of chronic disease programs can be used to leverage resources and provide trusted and continuous services to reach Hispanic populations during the pandemic.
African Americans, like the Hispanic population, are more likely to contract COVID-19, be hospitalized, and die of the disease (24). Akintobi et al describe how psychosocial, sociocultural, and environmental vulnerabilities, compounded by preexisting health conditions, exacerbate the burden of COVID-19 among African Americans (7). Authors share important information based on their years of experience on ways to create and implement approaches to intentionally engage African Americans at higher risk of COVID-19. Insights and recommendations can advance community leadership and be used to prepare public health practitioners, researchers, and evaluators for future pandemics — both assisting in advancing health equity and addressing historical aspects of health disparities among African Americans.
The disproportionate impact of COVID-19 and associated disparities among Hispanic, non-Hispanic Black, and non-Hispanic American Indian/Alaska Native children and teenagers has been widely reported (25). Children from some racial and ethnic minority groups have a higher prevalence of obesity, asthma, type 2 diabetes, and hypertension; were diagnosed more frequently with COVID-19; and had more severe outcomes compared with their non-Hispanic White counterparts (26). In addition, a higher proportion of children from some racial and ethnic minority groups, compared with White children, live in families with incomes less than 200% of the federal poverty level or in households lacking secure employment (8). White et al argue that the COVID-19 pandemic reemphasizes the importance of implementing policy, systems, and environmental changes in school systems to support emergency preparedness and recovery, as well as resilience, through collaborations among local health departments, local school systems, and other public and private organizations (8). Topics addressed in this article include disparities in underlying medical conditions and social determinants of health, inequities in social determinants of health, and community-based approaches to reducing COVID-19 disparities. The article concludes by discussing ways to implement strategies to advance health equity through partnership.
It has long been recognized that disparities in health care access and patient outcomes are associated with factors related to race, sex, gender, sexual orientation, primary language, and socioeconomic status (27). Epps and coauthors recognize that African Americans and other underrepresented racial and ethnic groups are often not included in health decision making and policy development (9). As a result, these public health experts describe steps undertaken to improve participation, joint decision making, and capacity building between an integrated academic health system and a community coalition to address complex health challenges with the aim of increasing the capacity of health systems to reduce the burden of COVID-19. This article describes a call to action by the chair of a health care board of trustees to its board members consisting of clinicians, researchers, educators, and health advocates to identify ways to mitigate disparities and determine how the health care system could play a role in advancing and implementing effective strategies to reduce the disproportionate burden of COVID-19 among communities of color. Authors provide insight into the organizational planning process to generate a community outreach and health disparities collaborative with goals for governance, messaging and education, community partnerships, data, and research and evaluation.
COVID-19 has exacted a tremendous toll on the physical, emotional, and psychological well-being of many Americans, thus requiring a population health response (28). The disproportionate impact of the COVID-19 pandemic on Hispanic communities has resulted in a greater burden of depression, anxiety, and stress along with the need for increased assistance with housing, access to food, and supplemental income (29). Moon and colleagues offer original research that reports findings on demographic characteristics and factors associated with service volume, types of services, and referrals in the pre-COVID-19 and COVID-19 periods (10). They report that referrals shifted from primarily mental health services and disease management during the prepandemic period to affordable housing support, food assistance, and supplemental income during the COVID-19 period. This study presents findings on how a community-based organization with a long-standing presence in the Hispanic community effectively expanded its emotional wellness program, using promotores to provide integrated mental health care and social services to clients disproportionately affected by COVID-19.
Hacker et al discuss the problem of COVID-19 and chronic disease in their essay (11). They describe 3 categories of challenges facing public health professionals and identify solutions needed to improve health outcomes and lessen health inequities among people at risk or living with a chronic disease. Authors also discuss the evolving response by the Centers for Disease Control and Prevention’s National Center for Chronic Disease Prevention and Health Promotion to implement a multipronged approach to enhance access to data at the local level, focus on addressing social determinants of health through a health equity lens, and expand partnerships and communication about the impact of COVID-19 on chronic disease.
Unmet health-related social support needs among people being served by health care systems can contribute to high patient morbidity and poor population health (30,31). However, little is known about the overall impact of screening and referral programs that address unmet health-related social needs on outcomes related to experience of care, population health, and cost. Ruiz Escobar et al conducted a systematic review of peer-reviewed articles in PubMed published over the past 10 years (as of March 2020) to determine the impact of screening and referral care delivery services on unmet health-related social needs (12). Thirty-five articles met the systematic review’s inclusion criteria. After conducting their review, the authors concluded that although evidence exists of a positive influence of screening and referral program outcomes related to experience of care and population health, no definitive conclusions could be made on the overall impact on changes in patient connection to resources, patient satisfaction, and patient-reported outcomes because of the potential high risk of bias across studies. Their findings can inform the use of screening and referral programs in health care organizations, including ways to strengthen future studies to examine their effectiveness.
Qualitative research is an important methodological tool that provides critical insights in identifying subjective meaning in the context of health (32). Qualitative research is a necessary exploratory approach that can be used to better understand and improve health equity research and practice. Olson and her team of researchers conducted 10 listening sessions and 28 interviews with people from diverse backgrounds to identify themes in causes, solutions, and opportunities to collaborate across sectors to address cancer disparities (13). Researchers validated the use of qualitative approaches to engage diverse participants representing many different sectors. Qualitative findings identified medical mistrust, the need for equitable multilevel partnerships, influences of environmental threats on cancer burden, and location of cancer disparities as key concerns among people participating in the listening sessions and interviews. The researchers describe how these findings will be used to form multisector teams to address local social, cultural, and biological influences of cancer disparities and achieve health equity in Wisconsin.
Geographic location continues to be an important contributor in shaping access to timely and necessary screening and treatment options (33). Rohatgi et al conducted original research examining relationships among rurality, sociodemographic characteristics, and access to low-dose computed tomography (LDCT) screening for lung cancer and screening access and lung cancer mortality (14). This study revealed that more than 97% of metropolitan residents had access to LCDT screening, compared with just over 40% of nonmetropolitan residents. Researchers learned that residents of southeastern Missouri, a rural and impoverished area, had low screening access, high smoking prevalence, and high lung cancer mortality. Researchers concluded that targeted strategies to implement rural LDCT screening could reduce geographic disparities in access, and future research could help identify factors that increase access to screening to eliminate rural-related disparities in lung cancer mortality.
Breast cancer is the most frequently diagnosed cancer and a leading cause of cancer mortality among American Indian/Alaska Native (AI/AN) women (34). Despite having a lower incidence of breast cancer than White women, AI/AN women are more likely to be diagnosed at younger ages and later stages (35). Breast cancer incidence among non-AI/AN women has largely been quantified in large geographic regions in the US, and substantial regional variation in breast cancer inequities in non-Hispanic AI/AN populations has been reported. Zahrieh and colleagues conducted research to obtain a deeper understanding at a granular level to identify potential inequities in breast cancer incidence by applying county-level Bayesian disease mapping (a model-based approach that offers a means to improve county-level incidence estimates) to population surveillance data from 2005 through 2014 in New Mexico (30). They found a significant overall disparity effect across New Mexico, evidenced by the age-adjusted rate of breast cancer among non-Hispanic AI/AN women being appropriately 0.38 times the corresponding age-adjusted rate among non-Hispanic White women. Researchers also suggest that findings can be used to facilitate targeted statewide and county-level cancer control interventions to mitigate breast cancer disparities among AI/AN women in New Mexico.
Historically, type 2 diabetes has disproportionately affected racial and ethnic minority groups (31). To ensure accurate detection of type 2 diabetes, we must understand the ability of hemoglobin A 1c (HbA 1c ) to correctly classify type 2 diabetes status and evaluate intra-ethnic variation. Toward this end, Khosla et al conducted a scoping review to determine HbA 1c performance in African descent populations in the US with normal glucose tolerance, prediabetes, and diabetes (16). Results included 7 studies that analyzed HbA 1c performance among African Americans, 1 study that analyzed HbA 1c performance in Afro-Caribbean people, and 4 studies that analyzed HbA 1c performance among Africans. Researchers found that current HbA 1c cutoffs for prediabetes and type 2 diabetes may overestimate glycemic status in African Americans and underestimate glycemic status in Afro-Caribbean and African people. Researchers indicated that alternating testing, such as the oral glucose tolerance test, fasting plasma glucose, and other glycated blood proteins in place of or in combination with HbA 1c may better assess glycemic status in populations of African descent.
Tobacco use remains the leading cause of preventable morbidity and mortality in the US (33). Livingston and colleagues evaluated changes in tobacco cessation benefits, patient access, and cigarette smoking prevalence before and after 16 coordinated care organizations began providing comprehensive cessation benefits for reducing tobacco use prevalence among Medicaid members in Oregon (17). This implementation evaluation identified changes in tobacco cessation benefits, patient–provider discussions of smoking cessation, and cigarette smoking prevalence before and after the introduction of statewide incentives for reducing cigarette smoking. Evaluators reported that statewide effort accelerated progress toward tobacco use reduction among members of coordinated care organizations.
Obesity among adults living in Appalachia continues to be a major problem, and policy, systems, and environmental interventions may help to address long-standing underlying factors that have historically contributed to this persistent public health concern (35). Cardarelli and associates reported findings from a qualitative study that used a grounded theory approach to identify barriers and facilitators for healthy food access in a rural county in Kentucky (18). The goal was to design interventions responsive to social, cultural, and historical contexts from an equity perspective. Focus group participants were asked, for example, if it was easy to get fruits and vegetable at locations where they purchase food, if many people in their community purchase food at farmers markets, and what factors in their community make it easier or harder to eat healthy. The authors concluded that efforts to address food access through policy, systems, and environmental interventions must be sensitive to characteristics of the rural setting, acknowledge social inequities in the region, and proactively engage community members throughout all stages of intervention planning, implementation, and evaluation.
Oral health disparities among children have been linked to socioeconomic inequalities, access to care, health systems barriers, and lack of access to foods that promote optimal oral health outcomes (39). Martin et al conducted original research that explored the frequency of tooth brushing among children with a mean age 21.5 months (19). Their results indicated that the frequency of brushing among children, as reported by guardians, was higher when the correct amount of toothpaste was used, brushing occurred for a longer duration, and other family members helped children with brushing. Their findings strongly suggest that parental and family support for brushing are critically important in promoting and sustaining tooth-brushing behaviors.
According to the Lancet Global Health Commission on Global Eye Health, women, rural populations, and racial/ethnic minority groups are more likely to have vision impairment, a pervasive inequality that needs to be addressed (40). This PCD collection on advancing health equity and reducing health disparities concludes with a research study by Leiby et al investigating the effectiveness of an enhanced intervention among people with glaucoma: using patient navigators and social workers to improve patient adherence to follow-up eye care in community settings (20). The study compared the intervention group with a group of patients in usual care. Participants in usual care were provided with a local ophthalmologist’s contact information and a copy of their eye examination results; they were not provided access to patient navigators or social workers. Study participants, who were randomly assigned to either the enhanced or usual care intervention, were a diverse group of participants aged over 40 with a family history of glaucoma or currently diagnosed with diabetes. Only participants who had not seen an ophthalmologist in the previous 12 months were permitted to enroll in the study. Study participants consisted largely of African Americans, followed by White, Asian American, and Hispanic residents of Philadelphia, Pennsylvania. The study found that the use of patient navigators and social workers doubled the rate of adherence to annual recommended eye care follow-up, compared with participants assigned to the study’s usual care intervention. The study highlights that formalized use of social support in partnership with local ophthalmologists can be an effective approach to increasing access to local ophthalmological services.
At the center of this collection of articles is a shared commitment to the goal of eliminating health disparities, particularly those that continue to persist despite aggressive efforts to ameliorate them. The collection describes a range of diverse and timely examples of efforts to eliminate health disparities and advance health equity among racial and ethnic groups in the US. Articles appearing here represent various types of PCD articles that encompass multiple perspectives, from original research and systematic reviews to implementation evaluation to expert commentaries to tools that can be used in public health practice. As a discipline, we have important work to do, not only to better understand how social determinants of health and other contextual factors impact health but also to design, implement, and evaluate effective multilevel systems approaches that create optimal conditions to promote health for all. PCD will continue to move forward in its commitment to these goals, and we encourage authors to visit the journal’s Author’s Corner website (https://www.cdc.gov/pcd/for_authors/index.htm) to learn more about article types that best fit their research addressing population-based approaches to eliminating health disparities and advancing health equity.
Corresponding Author: Leonard Jack, Jr, PhD, MSc, Editor in Chief, Preventing Chronic Disease: Public Health Research, Practice, and Policy, Office of Medicine and Science, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, 4770 Buford Hwy, NE, Mailstop S107–8, Atlanta, GA 30341. Email: [email protected] .
Author Affiliations: 1 Office of Medicine and Science, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta, Georgia.
- Jack L Jr. Using PCD’s first-ever external review to enhance the journal’s worldwide usefulness to researchers, practitioners, and policy makers. Prev Chronic Dis 2018;15:E41. CrossRef external icon PubMed external icon
- US Department of Health and Human Services. Section IV: Advisory Committee findings and recommendation. In: The Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020. Phase I report: recommendations for the framework and format of Healthy People 2020. http://www.healthypeople.gov/sites/default/files/phaseI_0.pdf. Accessed July 8, 2021.
- Jack L Jr. PCD’s commitment to advancing diversity, equity, and inclusion in its scientific leadership, peer review process, research focus, training, and continuing education. Prev Chronic Dis 2021;18:210269.
- Michener L, Aguilar-Gaxiola S, Alberti PM, Castaneda MJ, Castrucci BC, Harrison LM, et al. Engaging with communities — lessons (re)learned from COVID-19. Prev Chronic Dis 2020;17:E65. CrossRef external icon PubMed external icon
- Airhihenbuwa CO, Tseng TS, Sutton VD, Price L. Global perspectives on improving chronic disease prevention and management in diverse settings. Prev Chronic Dis 2021;18:E33. CrossRef external icon PubMed external icon
- Calo WA, Murray A, Francis E, Bermudez M, Kraschnewski J. Reaching the Hispanic community about COVID-19 through existing chronic disease prevention programs. Prev Chronic Dis 2020;17:E49. CrossRef external icon PubMed external icon
- Akintobi HT, Jacobs T, Sabbs D, Holden K, Braithwaite R, Johnson LN, et al. Community engagement of African Americans in the era of COVID-19: considerations, challenges, implications, and recommendations for public health. Prev Chronic Dis 2020;17:E83. CrossRef external icon PubMed external icon
- White A, Liburd LC, Coronado F. Addressing racial and ethnic disparities in COVID-19 among school-aged children: are we doing enough? Prev Chronic Dis 2021;18:E55. CrossRef external icon PubMed external icon
- Epps F, Wiley Z, Teunis LJ, Johnson TM 2d, Patzer RE, Ofotokun I, et al. A framework for mobilizing health care to respond to the community within the COVID-19 pandemic. Prev Chronic Dis 2021;18:E30. CrossRef external icon PubMed external icon
- Moon KJ, Montiel GI, Cantero PJ, Nawaz S. Addressing emotional wellness during the COVID-19 pandemic: the role of promotores in delivering integrated mental health care and social services. Prev Chronic Dis 2021;18:E53. CrossRef external icon PubMed external icon
- Hacker KA, Briss PA, Richardson L, Wright J, Petersen R. COVID-19 and chronic disease: the impact now and in the future. Prev Chronic Dis 2021;18:210086. CrossRef external icon PubMed external icon
- Ruiz Escobar R, Pathak H, Blanchard C. Screening and referral care delivery services and unmet health-related social needs: a systematic review. Prev Chronic Dis 2021;18:2000569.
- Olson J, Cawthra T, Beyer K, Frazer D, Ignace L, Maurana C, et al. Community and research perspectives on cancer disparities in Wisconsin. Prev Chronic Dis 2020;17:E122. CrossRef external icon PubMed external icon
- Rohatgi KW, Marx CM, Lewis-Thames MW, Liu J, Colditz GA, James AS. Urban–rural disparities in access to low-dose computed tomography lung cancer screening in Missouri and Illinois. Prev Chronic Dis 2020;17:E140. CrossRef external icon PubMed external icon
- Zahrieh D, Golafshar MA, Patel SH, DeWees TA. Quantification of potential inequities in breast cancer incidence in New Mexico through Bayesian disease mapping. Prev Chronic Dis 2021;18:E23. CrossRef external icon PubMed external icon
- Khosla L, Bhat S, Fullington LA, Horlyck-Romanovsky MF. HbA1c performance in African descent populations in the United States with normal glucose tolerance, prediabetes, or diabetes: a scoping review. Prev Chronic Dis 2021;18:E22. CrossRef external icon PubMed external icon
- Livingston CJ, Bartelmann SE, Goff NM, Aird KG. Reducing tobacco use in Oregon through multisector collaboration: aligning Medicaid and public health programs. Prev Chronic Dis 2020;17:E155. CrossRef external icon PubMed external icon
- Cardarelli K, DeWitt E, Gillespie R, Norman-Burgdolf H, Jones N, Mullins JT. “We’re, like, the most unhealthy people in the country”: using an equity lens to reduce barriers to healthy food access in rural Appalachia. Prev Chronic Dis 2020;17:E165. CrossRef external icon PubMed external icon
- Martin M, Pugach O, Avenetti D, Lee H, Salazar S, Rosales G, et al. Oral health behaviors in very young children in low-income urban areas in Chicago, Illinois, 2018–2019. Prev Chronic Dis 2020;17:E152. CrossRef external icon PubMed external icon
- Leiby BE, Hegarty SE, Zhan T, Myers JS, Katz LJ, Haller JA, et al. A randomized trial to improve adherence to follow-up eye examinations among people with glaucoma. Prev Chronic Dis 2021;18:E52. CrossRef external icon PubMed external icon
- Webb Hooper M, Mitchell C, Marshall VJ, Cheatham C, Austin K, Sanders K, et al. Understanding multilevel factors related to urban community trust in healthcare and research. Int J Environ Res Public Health 2019;16(18):3280. CrossRef external icon PubMed external icon
- Finset A, Bosworth H, Butow P, Gulbrandsen P, Hulsman RL, Pieterse AH, et al. Effective health communication — a key factor in fighting the COVID-19 pandemic. Patient Educ Couns 2020;103(5):873–6. CrossRef external icon PubMed external icon
- Alcendor DJ. Racial disparities-associated COVID-19 mortality among minority populations in the US. J Clin Med 2020;9(8):2442. CrossRef external icon PubMed external icon
- Vahidy FS, Nicolas JC, Meeks JR, Khan O, Pan A, Jones SL, et al. Racial and ethnic disparities in SARS-CoV-2 pandemic: analysis of a COVID-19 observational registry for a diverse US metropolitan population. BMJ Open 2020;10(8):e039849. CrossRef external icon PubMed external icon
- Bassett MT, Chen JT, Krieger N. The unequal toll of COVID-19 mortality by age in the United States: quantifying racial/ethnic disparities. Working paper. Cambridge (MA): Harvard T.H. Chang School of Public Health; 2020.https://www.hsph.harvard.edu/social-and-behavioral-sciences/2020/06/23/the-unequal-toll-of-covid-19-mortality-by-age-in-the-united-states-quantifying-racial-ethnic-disparities/. Accessed July 13, 2021.
- Kim L, Whitaker M, O’Halloran A, Kambhampati A, Chai SJ, Reingold A, et al. ; COVID-NET Surveillance Team. Hospitalization rates and characteristics of children aged <18 years hospitalized with laboratory-confirmed COVID-19 — COVID-NET, 14 states, March 1–July 25, 2020. MMWR Morb Mortal Wkly Rep 2020;69(32):1081–8. CrossRef external icon PubMed external icon
- Okoro CA, Zhao G, Fox JB, Eke PI, Greenlund KJ, Town M. Surveillance for health care access and health services use, adults aged 18–64 years — Behavioral Risk Factor Surveillance System, United States, 2014. MMWR Surveill Summ 2017;66(7):1–42. CrossRef external icon PubMed external icon
- Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun 2020;89:531–42. CrossRef external icon PubMed external icon
- Waitzkin H, Getrich C, Heying S, Rodríguez L, Parmar A, Willging C, et al. Promotoras as mental health practitioners in primary care: a multi-method study of an intervention to address contextual sources of depression. J Community Health 2011;36(2):316–31. CrossRef external icon PubMed external icon
- Tough H, Siegrist J, Fekete C. Social relationships, mental health and wellbeing in physical disability: a systematic review. BMC Public Health 2017;17(1):1414. Erratum in BMC Public Health 2017;17(1)580. CrossRef external icon PubMed external icon
- Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med 2010;7(7):e1000316. CrossRef external icon PubMed external icon
- Mykhalovskiy E, Eakin J, Beagan B, Beausoleil N, Gibson BE, Macdonald ME, et al. Beyond bare bones: critical, theoretically engaged qualitative research in public health. Can J Public Health 2018;109(5-6):613–21. CrossRef external icon PubMed external icon
- Tsui J, Hirsch JA, Bayer FJ, Quinn JW, Cahill J, Siscovick D, et al. Patterns in geographic access to health care facilities across neighborhoods in the United States based on data from the National Establishment Time-Series between 2000 and 2014. JAMA Netw Open 2020;3(5):e205105. CrossRef external icon PubMed external icon
- White MC, Espey DK, Swan J, Wiggins CL, Eheman C, Kaur JS. Disparities in cancer mortality and incidence among American Indians and Alaska Natives in the United States. Am J Public Health 2014;104(Suppl 3):S377–87. CrossRef external icon PubMed external icon
- Melkonian SC, Jim MA, Haverkamp D, Wiggins CL, McCollum J, White MC, et al. Disparities in cancer incidence and trends among American Indians and Alaska Natives in the United States, 2010–2015. Cancer Epidemiol Biomarkers Prev 2019;28(10):1604–11. CrossRef external icon PubMed external icon
- Lin J, Thompson TJ, Cheng YJ, Zhuo X, Zhang P, Gregg E, et al. Projection of the future diabetes burden in the United States through 2060. Popul Health Metr 2018;16(1):9. CrossRef external icon PubMed external icon
- Creamer MR, Wang TW, Babb S, Cullen KA, Day H, Willis G, et al. Tobacco product use and cessation indicators among adults — United States, 2018. MMWR Morb Mortal Wkly Rep 2019;68(45):1013–9. CrossRef external icon PubMed external icon
- Smith LH, Laurent D, Baumker E, Petosa RL. Rates of obesity and obesogenic behaviors of rural Appalachian adolescents: how do they compare to other adolescents or recommendations? J Phys Act Health 2018;15(11):874–81. CrossRef external icon PubMed external icon
- Shen A, Bernabé E, Sabbah W. Systematic review of intervention studies aiming at reducing inequality in dental caries among children. Int J Environ Res Public Health 2021;18(3):1300. CrossRef external icon PubMed external icon
- Burton MJ, Ramke J, Marques AP, Bourne RRA, Congdon N, Jones I, et al. The Lancet Global Health Commission on Global Eye Health: vision beyond 2020. Lancet Glob Health 2021;9(4):e489–551. CrossRef external icon PubMed external icon
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors’ affiliated institutions.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Am J Lifestyle Med
- v.13(6); Nov-Dec 2019
Why Are Preventable Illnesses Still Killing So Many People?
‘Although many individuals attribute their chronic illness to genetics or a family history of said disease, research shows that the overwhelming majority of the most common chronic illnesses are associated with lifestyle and not genetics.’
It is not like we do not know that cardiovascular disease (CVD) is the most common cause of death and disability in Westernized countries; and it is not like we do not know that the majority of CVD is preventable. Why then are these preventable illnesses still killing so many people?
Similar to the situation with cigarettes, we have known for many years that the standard American diet and the standard American lifestyle increase the risk of CVD. When individuals change their eating habits and get some exercise, the risk and incidence of CVD, most chronic illnesses, and many of the common cancers declines rapidly.
The standard American diet diet and the standard American lifestyle are filled with several risk factors for CVD including high blood pressure, high blood lipids and glucose (sugar), cigarette smoking, sedentary lifestyle, excess stress, not enough quality sleep, mental and behavioral illness, obesity, and more. Although many individuals attribute their chronic illness to genetics or a family history of said disease, research shows that the overwhelming majority of the most common chronic illnesses are associated with lifestyle and not genetics.
Also, the science of epigenetics (how one’s behavior and what he/she is exposed to influences gene function) shows that a healthy lifestyle can essentially turn off bad genes and turn on good genes. For example, the work of Dr Dean Ornish showed that 400 genes that influence prostate cancer are affected by an intensive lifestyle intervention program.
When we start to look at the risk factors for chronic illness and specifically CVD, we see that recently the American Heart Association revised its guidelines for hypertension (high blood pressure) based on these new guidelines, and almost half of Americans are now classified as hypertensive and, therefore, have at least this as a risk factor for CVD, strokes, renal disease, dementia, and more ( Figure 1 ). In past years physicians would be happy when their patients had a blood pressure of <140/90 mm Hg. Now we know that a much lower blood pressure is necessary to avoid complications that include heart attacks, strokes, peripheral vascular disease, dementia, erectile dysfunction, and more.

Risks for CVD.
When we look at cholesterol and other blood lipids as a risk factor for CVD, why is it that so many people with normal lipids still go on to have complications of CVD? The answer is that lipids alone are not the best test for the evaluation of endothelial dysfunction, which some people have called the other ED!
In addition to the general lipid profile, there are other blood tests that specifically evaluate the function of the endothelium including oxidized LDL (low-density lipoprotein), which reflects damage to the LDL particles. These oxidized LDL particles, especially when they are small in size, get into the endothelial cells lining the blood vessels resulting in endothelial dysfunction and the start of plaque formation. F2 Isoprostane is a blood test that measures oxidation within the endothelial cells. Oxidation is analogous to rusting metal. When the cells rust from within, they cannot function normally. Reactive oxygen species (ROS) form as a result of this oxidation and damage the cells, the DNA, and the mitochondria, which function to produce energy for the cells ( Figures 2 and and3 3 ).

Progression of Endothelial Inflammation.

Vessel wall Inflammation.
The LP-Plac2 blood test (aka the PLAC test) measures inflammation within the arterial wall ( Figure 4 ). This is an early sign of endothelial inflammation and can be detected long before abnormalities are seen in a calcium score test, ultrasound, or catherization. The calcium score test is essentially a CT (computed tomography) scan of the arteries in the heart and represents the body’s attempt to wall off the plaque formation (keeping it localized and less likely to spread). An ultrasound of the heart reveals the pumping ability of the heart; it does not directly tell what is happening inside the arteries. The cardiac catherization is the gold standard to evaluate the stenosis/occlusion of arteries in the heart. Since it is an invasive procedure, there is more risk associated with doing this test.

Advanced Tests for Endothelial Inflammation.
Davidson MH, Corson MA, Alberts MJ, et al. Consensus panel recommendation for incorporating lipoprotein-associated phospholipase A 2 testing into the cardiovascular risk assessment guidelines. Am J Cardiol . 2008;101(suppl):51F-57F
This is an important distinction since many people have these tests completed to represent late-stage disease, meaning the endothelial damage has been occurring for some time—usually years. If we as health care professionals are to practice preventive medicine, we need to start looking for disease early when we can have a significant positive impact on treating and reversing the disease. The LP-Plac2 test measures the amount of plaque within the arterial wall due to the accumulation of oxidized LDL. The more plaque formation the more arterial dysfunction, stenosis, and impaired blood flow.
The myeloperoxidase (MPO) test measures inflammation outside the arterial wall ( Figure 5 ). Inflammation inside and outside the arteries stimulates an immune reaction that brings white blood cells and other mediators of inflammation to the area in an attempt to combat the damage. MPO is also a specific marker of plaque vulnerability, meaning its potential to rupture. When plaque ruptures, it allows the release of cholesterol and other harmful substances, which then travel downstream to the smallest artery causing blockage of blood flow resulting in a heart attack (if the blood vessel is within the heart) or a stroke (if the blood vessel is within the brain).

The “PLac” test.
Brennan ML, Penn MS, Van Lente F, et al. Prognostic value of myeloperoxidase in patients with chest pain. N Engl J Med . 2003;349:1959-1604
Plaque vulnerability is an important piece of information for the physician and the patient since it will dictate the aggressiveness of the treatment. This latter point cannot be overemphasized since the complications of vascular disease are often minimized when the degree of stenosis is not significant. As mentioned above, the cardiac catherization is the gold standard used to measure the percentage of occlusion in an artery, and when the percentage is not high, the action plans may be less than helpful particularly if the patient does not understand how important it is to change their lifestyle. Any percentage of stenosis/occlusion of an artery is not good since it tells the physician and the patient that the individual has caused damage to the largest and one of the most important organs in the body, the endothelium. If the person does not improve the quality of food they eat, do not start an exercise program, do not address the stress in life, and do not improve the quality of their sleep, then the endothelium damage will continue until the occlusion gets to the degree where a heart attack or stroke occurs. Thus, the point is to emphasize to the patient the importance of working to reverse any degree of stenosis.
Another simple test to do is a microalbumin test to measure the amount of albumin protein in the urine. When the arteries in the kidneys are damaged (another example of endothelial dysfunction), they spill more albumin protein into the urine than when the arteries are healthy.
Ridker PM, Danielson E, Fonseca FA, et al. Reduction in C-reactive protein and LDL cholesterol and cardiovascular event rates after initiation of rosuvastatin: a prospective study of the JUPITER trial. Lancet . 2009;373:1175-1182
Hs-CRP, or high sensitivity C-reactive protein, is a simple blood test that is a general measure of inflammation within the body and is a good marker of successful treatment ( Figure 6 ). As the CRP number decreases, it tells the health care provider and the patient that inflammation is decreasing and the individual and the endothelium are getting healthier.

CRP versus LDL.
The above-mentioned advanced tests beyond the traditional lipid panel gives more detailed and specific information about what is happening within and around the arteries. These tests add to the list of risk factors that should be itemized for the patient and the health care provider. Even when an individual does not have a specific diagnosis, if they have many risk factors, this becomes a problem list that should be worked on to help the individual become and stay healthier.
Diabetes and prediabetes represent conditions of elevated glucose and abnormal insulin function. When glucose in the circulation is elevated above the normal level, the glucose molecules attach to proteins in the body creating a distortion of the proteins and, therefore, dysfunction of the proteins. This is one mechanism thought to be related to the cause of dementia, which is now being called type 3 diabetes . These changes (protein dysfunction) also occur in the prediabetic state. This is one reason health care providers should be as diligent with prediabetic patients as they are with their diabetic patients. Over time, the same complications occur in both groups. Therefore, it is incumbent upon the health care provider to impress upon the patient the seriousness of this disease. With aggressive lifestyle change, both diabetes and prediabetes can be effectively managed, and we know from many clinical studies that intensive lifestyle change programs bring about the same or better clinical results than many of the first-line medications for diabetes and other chronic illnesses.
Diabetes, CVD, obesity, metabolic syndrome, and a host of other chronic illnesses are to a large extent lifestyle-related illnesses. They are not in most cases genetic/inherited and certainly are not related to advancing age. As such, the public needs (as do many health care providers) to be aware that these illnesses are largely preventable!
Knowler WC, Barrett-Connor E, Fowler SE, et al; Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med . 2002;346:393-403
With this background, then why are so many people still dying of preventable illnesses? Is this related to social determinants of health (ie, food insecurity, financial problems, excess stress, inadequate social support, addictions, transportation issues, and unemployment), or is it just that life is too stressful and many folks are unable to make health a priority?
The solution to this problem is not impeded by the cause. By this I mean we can largely avoid these preventable chronic illnesses regardless of the cause (lifestyle or social determinants of health). Since life and lifestyle contributed to the problem in the first place, we know that life and lifestyle changes can help solve these problems. Starting with the standard American lifestyle, the health care provider and the patient can work on a plan to improve nutrition, increase exercise time, deal with excess stress, develop a healthy sleeping plan, support mental and behavioral health, and help the individual understand their purpose in life ( Figure 7 ).

Exercise and All-Cause Mortality.
What is the evidence that lifestyle treats and prevents chronic illnesses such as hypertension, diabetes, heart disease, obesity, as well as many common cancers?
One of the best researchers in this area is Dr Dean Ornish, who has shown that intensive lifestyle intervention positively influences hundreds of genes related to prostate cancer. His program incorporates healthy eating with active living, meditation, and yoga and has significant impact on the development of CVD such that many insurance programs now pay for this prevention program.
Dr Caldwell Esselstyn has also contributed a tremendous amount of clinical information to the world of CVD. He has shown by using cardiac catherization studies that CVD can indeed be effectively treated and even reversed! His program is a strict plant-based program with no animal products and no oil. This intensive program has proven that CVD can be reversed and is now used by hundreds, if not thousands, of individuals.
Another program that treats, reverses, and prevents chronic disease is the Complete Health Improvement Program (CHIP). This is a 9-week in-classroom program facilitated by an instructor who teaches the participants how to shop, cook, and enjoy plant-based meals. The participants have homework assignments including restocking their pantry and kitchen. The participants are asked to eliminate all junk food and to keep only healthy food in the home so this becomes the easy choice. The program also emphasizes increased physical activity and stress reduction.
Realize the number of choices we make daily and understand how many of these choices affect our health in the short term and long term. When we choose to stop at a fast food restaurant, when we choose to smoke a cigarette, when we choose to stay up late and not get enough sleep, all these choices negatively affect health in the present and in the future if such behaviors continue. Conversely, when we choose to stop for a salad and a veggie burger, when we stop smoking, and make quality sleep a habit, we positively influence present and future health.
As a practicing internist for 25 years and as a specialist in preventive health care, I have seen firsthand the power of what is known as lifestyle medicine as well as able to compare this to traditional health care methods. The latter type of health care is delivered via prescription medications and surgical procedures. As I have critically evaluated and compared preventive health care and traditional medical care, I have been amazed at how effective preventive health care is. Rather than take a heartburn medication, individuals do better after they stop eating the offending foods. Rather than take high cholesterol medications, individuals (without previous evidence of CVD) do better after they start on a healthy low-fat diet and exercise. For those with diabetes, I have witnessed the amazing results from the CHIP program and have seen many individuals decrease and even stop many of their medication as their diabetes markers come into the normal range.
When I relay this information in public presentations as well as to medical professionals, I often see that people are surprised by these findings, and I wonder how this can occur. This information has been accumulating for decades; unfortunately, it has not been disseminated as well as the propaganda people hear from the meat and dairy industry. The clinical evidence is clear—animal protein increases the risk and incidence of most of the chronic illnesses and many cancers. Dairy makes the bones weaker not stronger as the television commercials tell the public. All a person needs to do is to start reading some of the clinical reports that are on the website www.nutritionfacts.org as well as listen to the video blogs from Dr Michael Greger, who is one of the most knowledgeable physicians in the area of plant-based research. This information is supported by the work of many others including Dr Joel Fuhrman, Dr Joel Kahn, Dr T. Colin Campbell, Dr Garth Davis, Dr Scott Stoll, and dozens of others who have devoted their professional careers to helping health care providers and the public understand the role of nutrition in good health.
Once we understand this and know what is stated above is grounded in evidence-based, scientifically validated research, and not opinion or philosophy, what we do next is most important. As health care providers, we are all responsible for understanding the current clinical evidence. With this information we should be educating our patients on the benefits of healthy living, plant-based eating, and intensive lifestyle interventions. I believe we, as health care providers, are also responsible for being role models for healthy living. We cannot just tell our patients what to do—we have to believe this enough to live our lives in the same fashion. In this way we talk the talk and walk the walk. When we do this, the results are tremendous!
We transform our clinical work from a sick care system to a true health care system. In the United States, we have a sick care system. We essentially wait for people to become sick and then we try to cure them rather than focusing on keeping healthy people healthy in the first place. Included in my public presentations, I often show the YouTube video, Make Health Last , which shows how most people in America spend the last 10 years of their lives—in sickness and not in wellness. Most people get old and die after a long bout with a chronic illness or cancer. Most Americans do not live the last years of their lives in wellness. In contrast, many live in the Blue Zones of the world where there are more centenarians than any other place on the planet. The reason for this is the people who live in the Blue Zones (Sardinia, Ikaria, Okinawa, Loma Linda, and Costa Rica) eat healthy food daily, they are regularly active, they sleep well, manage their stress, and live with purpose. They have great social support and do not worry about who is going to take care of them as they age because family and friends are all around for support. When you watch this video, most people say, “I want to live like that!”
Certainly, that is how we should structure our lives. Again, it is all about choices. We can choose to be healthy or we can choose to live a life that leads us down the road to sickness, chronic disease, disability, and early death. Lifestyle either creates a problem or creates a solution! Each day the choice is ours—so how are you going to live?
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Not applicable, because this article does not contain any studies with human or animal subjects.
Informed Consent: Not applicable, because this article does not contain any studies with human or animal subjects.
Trial Registration: Not applicable, because this article does not contain any clinical trials.

IMAGES
VIDEO
COMMENTS
Responsibility for health should be a collaborative effort among individuals and the societies in which they live. Individuals should care for their own health and help to pay for their own healthcare, and societies should promote health and help to finance the costs of healthcare. Though access to care tends to dominate discussions of social ...
In recent years the debate of who held the responsibility to avoid preventable illnesses between individuals and the government has gained a lot of traction. The government, in particular, is always getting the heat when it comes to this debate | Band: 6.5
Some people believed that health is their responsibility while on the other hand, many people believe that taking care of themselves and their family's health by avoiding preventable illness is not their responsibility, but the government's responsibilities to control using regulation and it is wrong. | Band: 4.5
A great argument essay structure may be divided to four paragraphs, in which comprises of four sentences (excluding the conclusion paragraph, which comprises of three sentences). For we to consider an essay structure a great one, it should be looking like this:
Personal Responsibility for Health: The Individual’s Role in Health. The distribution of responses for the two survey items on personal responsibility are reported in Table 3. The survey results showed that the principle of personal responsibility for health was well accepted by most of the respondents, with 98 per cent stating that ...
Background Combating viral outbreaks extends beyond biomedical and clinical approaches; thus, public health prevention measures are equally important. Public engagement in preventive efforts can be viewed as the social responsibility of individuals in controlling an infectious disease and are subjected to change due to human behaviour. Understanding individuals’ perception of social ...
‘There is no such thing as getting sick justly or unjustly’ – a qualitative study of clinicians’ beliefs on the relevance of personal responsibility as a basis for health prioritisation ...
Preventing Chronic Disease (PCD) is a peer-reviewed electronic journal established by the National Center for Chronic Disease Prevention and Health Promotion. PCD provides an open exchange of information and knowledge among researchers, practitioners, policy makers, and others who strive to improve the health of the public through chronic disease prevention.
The solution to this problem is not impeded by the cause. By this I mean we can largely avoid these preventable chronic illnesses regardless of the cause (lifestyle or social determinants of health). Since life and lifestyle contributed to the problem in the first place, we know that life and lifestyle changes can help solve these problems.
Government needs to decide on the main objectives of mitigation--is it minimising morbidity and associated mortality, avoiding an epidemic peak that overwhelms health-care services, keeping the ...