- Anxiety Disorder
- Bipolar Disorder
- Schizophrenia
- Adjustment Disorder
- Agoraphobia
- Antisocial Personality Disorder
- Borderline Personality Disorder
- Childhood ADHD
- Dissociative Identity Disorder
- Narcissistic Personality Disorder
- Oppositional Defiant Disorder
- Panic Attack
- Postpartum Depression
- Schizoaffective Disorder
- Seasonal Affective Disorder
- Sex Addiction
- Social Anxiety
- Specific Phobias
- Teenage Depression
- Black Mental Health
- Emotional Health
- Sex & Relationships
- Understanding Therapy
- Workplace Mental Health
- My Life with OCD
- Caregivers Chronicles
- Empathy at Work
- Sex, Love & All of the Above
- Parent Central
- Mindful Moment
- Mental Health News
- Live Town Hall: Mental Health in Focus
- Inside Mental Health
- Inside Schizophrenia
- Inside Bipolar
- ADHD Symptoms Quiz
- Anxiety Symptoms Quiz
- Autism Quiz: Family & Friends
- Autism Symptoms Quiz
- Bipolar Disorder Quiz
- Borderline Personality Test
- Childhood ADHD Quiz
- Depression Symptoms Quiz
- Eating Disorder Quiz
- Narcissim Symptoms Test
- OCD Symptoms Quiz
- Psychopathy Test
- PTSD Symptoms Quiz
- Schizophrenia Quiz
- Attachment Style Quiz
- Career Test
- Do I Need Therapy Quiz?
- Domestic Violence Screening Quiz
- Emotional Type Quiz
- Loneliness Quiz
- Parenting Style Quiz
- Personality Test
- Relationship Quiz
- Stress Test
- What's Your Sleep Like?
- Find Support
- Suicide Prevention
- Drugs & Medications
- Find a Therapist

How Stress Affects Mental Health

Everyone experiences stress from time to time. When it becomes chronic, it can affect your mental health.
While we all feel stress from time to time, when it’s long lasting or chronic, it may begin to affect our mental health.
When stress interferes with your everyday life and causes you to stop doing the things that you love, consider acting to take care of yourself and your future health.
Though stress can be challenging to deal with, many things are within your control to help minimize and manage stress.
Psychological effects of stress
Stress can cause psychological and emotional distress. When it becomes chronic, it can increase your risk for anxiety and depression .
Experiencing long-term stressful situations, like caregiving , without stress management efforts can lead to emotional overwhelm and burnout .
Chronic stress can have negative effects on your body and mind and create a multitude of unpleasant physical and psychological symptoms. For example, it can cause tension, leading to muscle pain and headaches, or memory issues.
Mental health conditions that may be linked to stress include:
- substance use difficulties
- sleep issues
- chronic pain
The biology of stress and mental health
How do our bodies respond to stress and why does chronic stress often lead to some mental health conditions? Scientists have started to find biological answers.
Within seconds of perceiving a stressor, the brain signals serotonin and adrenaline to be released. Those chemicals are quickly followed by stress hormones, which impact regulate areas of the brain important for memory and regulating emotions.
When facing danger, the body engages the fight, flight, or freeze response . While this works well when running away from a tiger, it’s less effective for chronic stress like an endlessly demanding job. Over time this stress response can wear you down, mentally and physically.
A study reports that chronic stress is linked to changes in certain areas of the brain, such as the prefrontal cortex and limbic system. This has the potential to cause cognitive, emotional, and behavioral changes.
Stress can also be associated with changes in your gut, which can also influence your mood. Chronic stress can also make it harder to get pregnant and dampen sex drive.
All of those physical symptoms can lead to increase stress.
Causes of stress
What causes stress for one person may be different for another. Stress often happens if you feel high pressure or are trying to meet a deadline. It can also arise if there’s a threat to your health or relationships, or if you don’t have enough resources to answer all the demands of your life.
Mental health conditions such as anxiety or depression may make some people feel more easily stressed than others.
Common causes of stress include:
- relationships
- health problems
- job stability
- family responsibilities
- life changes
- poor sleep or diet
- a history of trauma
Signs of stress
The symptoms you experience when stressed can manifest in the way you think and how you feel emotionally. Stress can also show up physically or in your behavior. Because everyone experiences stress differently, symptoms may vary from person to person and range from mild to severe.
Cognitive symptoms of stress include:
- difficulty making decisions
- difficulty concentrating
- memory problems
- cognitive distortions
Emotional symptoms of stress include:
- irritability
- feeling anxious
- nervousness
- feeling sad or depressed
- low self-confidence
Physical symptoms of stress include:
- muscle pain
- digestive issues
- skin rashes and acne
- lack of energy
- low sex drive and reproductive issues
Behavioral symptoms of stress include:
- changes in eating habits
- crying more often than usual
- social withdrawal
- changes in sex drive
- increased use of tobacco, alcohol, or other substances
Tips for managing stress
There are many ways you can take charge of your stress. Here are some ideas to cope better with the stress you’re faced with and improve how your body and brain respond to stressors.
Stay active and exercise regularly
Just 20 minutes outdoors can help lower stress hormone levels, according to a study . If you want to get the most out of your walk and reap all of the benefits, then try walking in nature.
Explore relaxation techniques
Your breath is an effective stress reliever that’s easily accessible.
Deep breathing techniques , such as the 4-7-8 breathing technique, are designed to bring your body to a relaxing state. They’re great to use in times of high stress.
To try this method, sit comfortably and breathe in through your nose for 4 seconds, hold your breath for 7 seconds, then breathe out through your mouth for 8 seconds.
Progressive muscle relaxation can also help. This involves tensing and then relaxing the muscle groups throughout your body to relieve tension.
Slow down and prioritize
Life can be busy and sometimes it’s hard to say no to things, even though you know the added commitment may stress you out. Take time to slow down and prioritize. Think about what needs to get done, what can wait, what you can ask for help on, and what just doesn’t need to be done.
You can also try managing feelings of overwhelm by breaking larger tasks into smaller, easier tasks.
Setting healthy boundaries with others and yourself can also help you manage stress better.
Connect with others
A strong support system of people you trust, feel safe with, and are supported by can get you through tough times. A community is also great for strengthening your mental health and preventing side effects from stress.
Sharing your feelings or concerns can help you let off some steam, which may reduce your feelings of isolation. Also, others that aren’t as close to your situation might be able to think of solutions you haven’t thought of yet.
Talk with a therapist
If you feel stressed more often than you’re not, it may help to talk with your doctor or mental health professional.
If stress is affecting your life or relationships, a good therapist can help you find the appropriate treatment for your specific symptoms.
Consider looking for a therapist that integrates cognitive behavioral therapy (CBT) techniques into their practice. CBT is proven to help with anxiety, trauma, and depression.
Want to learn more about starting therapy? Psych Central’s How to Find Mental Health Support resource can help.
You can read more about healthy ways to cope with stress here.
Let’s recap
Chronic stress can affect your mental health. But you have the power to learn how to cope effectively — even if you can’t change the stressful situation.
Getting better at managing stress involves looking after your mental health and learning effective coping skills. Consider taking a walk, breathing, or tapping into CBT techniques.
Last medically reviewed on October 27, 2022
8 sources collapsed
- Hunter Mr, et al. (2019). Urban nature experiences reduce stress in the context of daily life based on salivary biomarkers. https://www.frontiersin.org/articles/10.3389/fpsyg.2019.00722/full?
- 5 things you should know about stress. (n.d.). https://www.nimh.nih.gov/sites/default/files/documents/health/publications/stress/19-mh-8109-5-things-stress.pdf
- Anxiety disorders. (2015). https://www.nami.org/NAMI/media/NAMI-Media/Images/FactSheets/Anxiety-Disorders-FS.pdf
- Chetty S, et al. (2014). Stress and glucocorticoids promote oligodendrogenesis in the adult hippocampus. https://pubmed.ncbi.nlm.nih.gov/24514565/
- Coping with stress. (2020). https://www.nimh.nih.gov/health/publications/so-stressed-out-fact-sheet
- I’m so stressed out! [Fact sheet]. (n.d.). https://www.nimh.nih.gov/health/publications/so-stressed-out-fact-sheet
- Mariotti A, et al. (2015). The effects of chronic stress on health: New insights into the molecular mechanisms of brain–body communication. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5137920/
- Stress effects on the body. (2018). https://www.apa.org/topics/stress/body#:~:text=When%20the%20body%20is%20stressed,tension%20when%20the%20stress%20passes
Read this next
Chronic stress can have a serious impact on not only our mental health, but also our physical health. But there are ways you can help reduce stress.
Stress hits us all in life, and while a little stress is good, too much can be overwhelming. But there are steps you can take to cope.
Everyone experiences stress, but not always in the same way. Learn about the types and causes of stress and practical ways to manage it better.
Chronic stress can have a significant impact on your physical and mental health. Support and resources are available to help you cope and manage…
GAS is a three-stage response to stress that includes alarm reaction, resistance, and exhaustion. Understanding what triggers stress can help you…
Stress rashes are inflamed parts of your skin that often present as hives, due to increased stress or anxiety. But treatment is available to help you…
The holiday season is a time to be surrounded by friends and family. Delegating responsibility and setting boundaries can help you manage holiday…
Research shows that the body’s fight, flight, or freeze response to stress plays a key role in turning hair gray.
Stress can make your body want to shut down. Try these 5 tips to gain your energy back.
Stress can affect all systems of the body, including the amount of vital oxygen getting to your muscles and organs.
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- Winter 2024 | VOL. 36, NO. 1 CURRENT ISSUE pp.A5-81
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
The Links Between Stress and Depression: Psychoneuroendocrinological, Genetic, and Environmental Interactions
- Gustavo E. Tafet , M.D., Ph.D. ,
- Charles B. Nemeroff , M.D., Ph.D.
Search for more papers by this author
The role of stress in the origin and development of depression may be conceived as the result of multiple converging factors, including the chronic effect of environmental stressors and the long-lasting effects of stressful experiences during childhood, all of which may induce persistent hyperactivity of the hypothalamic-pituitary-adrenal axis. These changes, including increased availability of corticotropin-releasing factor and cortisol, are also associated with hyperactivity of the amygdala, hypoactivity of the hippocampus, and decreased serotonergic neurotransmission, which together result in increased vulnerability to stress. The role of other monoaminergic neurotransmitters, genetic polymorphisms, epigenetic mechanisms, inflammatory processes, and altered cognitive processing has also been considered in the development of a comprehensive model of the interactions between different factors of vulnerability. Further understanding of the underlying mechanisms that link these factors may contribute significantly to the development of more effective treatments and preventive strategies in the interface between stress and mood disorders.
The link between stressful life events and the origin and development of depression has been widely investigated, providing an increasing body of evidence supporting this association. 1 – 3 Environmental factors likely affect individuals in somewhat different manners, therefore triggering an adaptive response to stress, which depends on both psychological and biological aspects in the interaction between stressors and individual resources. Psychological aspects include all of the cognitive processing related to incoming information; the subjective appraisal of different features related to stressors, such as magnitude and chronicity, predictability, and controllability; and potential resources to cope with them. Biological mediators include the activation of different neural structures underlying information processing, including sensory pathways, which convey environmental input to the CNS, and the resulting activation of neural and neuroendocrine cascades of molecular events, mediated by the subsequent activation of the sympathetic division of the autonomic nervous system and the hypothalamic-pituitary-adrenal (HPA) axis. 4 The efficacy of an adaptive response implies that it may be rapidly activated, to allow reacting in a successful and effective manner during stressful situations, and it should be efficiently controlled and concluded afterward. If it continues in a prolonged and excessive manner (e.g., during chronic stressful situations), it may lead to maladaptive changes, which in turn may contribute to the development of pathological conditions such as anxiety and mood disorders, including depression, particularly in individuals with increased genetic vulnerability. In this regard, various polymorphisms have been investigated as candidate genes, which are known to participate in important molecular pathways involved in the origin of depression. The presence of these genetic variations appears to be involved in the development of depression in response to stressful events, including adverse experiences during childhood and environmental stressors during adulthood. 5 – 10 Moreover, various studies have focused on the role of gene–environment interactions, including the search for these polymorphic variants and the role of transcriptional regulation by epigenetic mechanisms. 6 , 11 – 13 In addition, inflammatory processes associated with adaptive responses to stressful situations, with the consequent synthesis and release of proinflammatory cytokines, may lead to further maladaptive changes of neural and neuroendocrine systems, therefore contributing to the development of depressive symptoms, particularly in chronically stressed individuals.
This article aims to review the evidence for the role played by stress, associated with different converging factors, including a genetic diathesis, a history of adverse early life events, hyperactivity of the HPA axis, decreased monoamines, increased proinflammatory cytokines, and epigenetic mechanisms, such as those observed in response to environmental stressful conditions, and their potential interactions in the etiology of depression. An increased understanding of these factors and their potential interactions may lead to more effective strategies for the treatment of this disorder.
Processing of Environmental Stressors in the Brain
Environmental stressors are perceived and transmitted through sensory pathways to different structures in the CNS, such as the thalamus, which convey projections to the amygdala, and to sensory and association cortices, which in turn also project to different areas of the prefrontal cortex (PFC), including the orbitofrontal cortex, the medial PFC, and the anterior cingulate cortex (ACC). 4 , 7 Direct projections from the thalamus to the amygdala contribute to activate arousal and early alarm reactions, with the subsequent activation of the autonomic nervous system and the HPA axis, whereas indirect projections may reach the amygdala from sensory and association cortices as well as from transition cortices. The latter areas, including the entorhinal, perirhinal, and parahippocampal cortices, in turn project to the hippocampus, where sensory input is integrated with contextual cues, to convey more elaborated information to the amygdala. 14
The amygdala plays a critical role in emotional processing, including the assessment of the emotional relevance of environmental stimuli as well as internal stressors. It plays a key role in the regulation of autonomic and neuroendocrine responses, through projections to the lateral hypothalamus, which mediate the activation of the sympathetic branch of the autonomic nervous system; through direct projections to the paraventricular nucleus of the hypothalamus; or indirectly through the bed nucleus of the stria terminalis, which is involved in activation of the HPA axis. 14 In addition, the amygdala shares important connections with the orbitofrontal cortex and the medial PFC, 15 including Brodmann areas 10 and 32, and the subgenual ACC (Brodmann area 25). 16 The orbitofrontal cortex (Brodmann areas 11–14) has been associated with integration of multimodal sensory stimuli and primary appraisal of their positive or negative value, therefore participating in their affective assessment. 17 The medial PFC overlaps with the ACC, particularly in the subgenual ACC, 17 which regulates emotional responses generated by the amygdala. 18 These structures are in turn connected with the dorsolateral PFC (Brodmann areas 9 and 46) and the ventrolateral PFC (Brodmann areas 45 and 47), which participate in cognitive control and voluntary regulation of emotion. The dorsolateral PFC, which has been associated with executive aspects of cognitive processing 19 (most notably with conscious processing and working memory), receives input from the amygdala through the orbitofrontal cortex and ACC. 15 , 17 The dorsolateral PFC reciprocally projects back to limbic structures, mostly through indirect connections to the ventromedial PFC (Brodmann area 32), which projects to the subgenual ACC. 19 It has been proposed that projections from the ventromedial PFC and the subgenual ACC exert a modulatory effect on the amygdala, 19 , 20 which in turn sends excitatory output to the hypothalamus, 17 – 19 therefore regulating the activity of the HPA axis.
Decreased volume of the subgenual ACC has been described, together with hyperactivity of the amygdala, in individuals with mood disorders, 16 , 21 which has been associated with the role of the subgenual ACC in the top-down regulatory pathway between the dorsolateral PFC and the amygdala, allowing conscious down-regulation of negative emotions. These corticolimbic pathways may be dysfunctional in patients with depression, in which the dorsolateral PFC, dorsomedial PFC, orbitofrontal cortex, and ACC appear to be dysfunctional, particularly during cognitive-emotional tasks, with the consequent disruption of their top-down inhibitory effect expressed in the impaired cognitive modulation of emotions. 20 , 21 Recovery of conscious regulation of negative emotions has been associated with clinical recovery. In addition, decreased hippocampal volume has also been observed, along with increased activity of the amygdala and reduced activity of the dorsolateral PFC. 21 More recently, we documented changes in cortical thickness in patients exposed to child abuse and neglect, with the findings specific to the nature of the abuse. 22
Figure 1 illustrates the network of functional connections among different neural structures involved in adaptive responses to stress, including the processing of environmental stimuli through cortical and subcortical structures, and the activation of the HPA axis.
FIGURE 1. Schematic Representation of Neural Structures Involved in the Stress Response a
a Stressors are perceived by sensory receptors, which convey information to the thalamus, primary sensory cortices, association cortices, transition cortices, the hippocampus, and the amygdala. The amygdala also receives direct input from the thalamus. The orbitofrontal cortex and the medial prefrontal cortex are reciprocally connected and, together with the anterior cingulate cortex, convey information from sensory cortices and association cortices to subcortical structures, including direct connections to the hypothalamus and reciprocal connections with the amygdala. The amygdala participates in the activation of the HPA axis through stimulatory projections to the paraventricular nucleus of the hypothalamus, with consequent synthesis and release of CRF, which stimulates the release of ACTH from the pituitary. In turn, this stimulates the release of glucocorticoids from the adrenals, particularly cortisol. Cortisol exerts negative feedback at the level of the hypothalamus and the pituitary, as well as through the hippocampus, which exerts an inhibitory effect on the HPA axis. Activation of the HPA axis is also regulated by norepinephrine, through projections from the locus coeruleus, and serotonin, and through projections from the raphe nuclei. Both aminergic systems participate in regulation of the stress response through connections with the amygdala and the hippocampus, therefore exerting regulatory effects on both limbic structures. The amygdala is also involved in the activation of the autonomic component of the stress response through CRF inputs to the locus coeruleus. Solid lines indicate stimulatory inputs, whereas dotted lines indicate inhibitory inputs. ACC, anterior cingulate cortex; ACTH, adrenocorticotropin; CRF, corticotropin-releasing factor; DLPFC, dorsolateral prefrontal cortex; HPA, hypothalamic-pituitary-adrenal; MPFC, medial prefrontal cortex; OFC, orbitofrontal cortex.
Role of the HPA Axis
Activation of the HPA axis is initiated in limbic structures, including direct projections from the central nucleus of the amygdala, or indirectly through the bed nucleus of the stria terminalis, which projects to the hypothalamic paraventricular nucleus, where corticotropin-releasing factor (CRF) is synthesized in parvocellular neurons and released to reach the anterior pituitary. There, CRF regulates the transcription of the proopiomelanocortin gene (a common precursor for adrenocorticotropin, β-endorphin, and related peptides) and stimulates the release of adrenocorticotropin into the systemic circulation. Adrenocorticotropin acts upon the adrenal cortex to stimulate the biosynthesis and release of glucocorticoids, particularly cortisol. 23
At the molecular level, cortisol binds to mineralocorticoid receptors (type I) and glucocorticoid receptors (GRs; type II), constituting a hormone-receptor complex, which in turn undergoes conformational changes to allow its recognition and binding to a glucocorticoid response element, in the promoter region of many target genes. 24 Cortisol regulates the activity of the HPA axis through multiple negative feedback loops, which require its binding to GRs located in the paraventricular nucleus and the pituitary, where it down-regulates the synthesis and release of CRF and adrenocorticotropin, respectively, and GRs in the hippocampus, which in turn activates GABAergic projections to the paraventricular nucleus that inhibit HPA axis activity. Hence, many of the effects of cortisol may be understood as a result of transcriptional regulation of various genes, including those involved in the negative feedback loops responsible for the regulation of the HPA axis. 24
In response to short-term exposure to environmental stressors, the amygdala stimulates the HPA axis with the consequent synthesis and release of cortisol, 14 which is self-regulated by negative feedback mechanisms mediated by the glucocorticoid. In addition, the HPA system interacts with CRF neurons in the amygdala, activating a positive feedback loop involved in fear and anger reactions; the HPA also activates catecholaminergic neurons, stimulating arousal and improving cognitive functions. Hence, upon exposure to acute or short-term stressors, cortisol is expected to exert widespread metabolic effects, which is mostly necessary to maintain or restore homeostasis. 25 Cortisol is actively involved in the mobilization of energetic resources, including the stimulation of gluconeogenesis with the resulting increased levels of circulating glucose, and the down-regulation of inflammatory processes, therefore contributing to coping with the stressful situation.
Chronic and persistent activation of the HPA system may disrupt physiological mechanisms, including negative feedback loops, resulting in persistent activation of the system. Circadian rhythms normally characterized by wide variations, with morning zeniths and evening nadirs, are markedly altered during chronic stress, with the consequent increase in plasma cortisol levels and blunted circadian rhythm, mostly due to increased levels of cortisol during the evening and mild changes in the morning. 25 Prolonged exposure to increased levels of cortisol may induce detrimental effects on hippocampal neurons, reducing dendritic branching and inhibiting neurogenesis. 26 Moreover, hypersecretion of CRF and cortisol was also associated with decreased hippocampal volume, particularly in individuals exposed to childhood trauma. 27 Because the hippocampus is involved in the regulation of the HPA axis, it is conceivable that patients with major depression and early life trauma who exhibit reduced hippocampal volume 28 , 29 may also exhibit decreased hippocampal function, therefore resulting in further sensitization of stress responses. 5 These observations support previous reports that associated the origin of depressive symptoms with decreased expression of GRs at the hypothalamic and hippocampal levels, 24 with the resulting hypercortisolism. Hence, an increasing body of evidence supports the association between chronic stress and depression at the molecular level, where hyperactivity of the HPA axis, with the consequent increase of cortisol, represents one of the most consistent findings in both syndromal mood and certain anxiety disorders. 23 , 26
Various studies have focused on genes involved in the regulation of the HPA system, including both the mineralocorticoid receptor and GR genes, resulting in the identification of different single-nucleotide polymorphisms (SNPs). Among these, two different SNPs in the GR gene (BclI and Asp363Ser) have been associated with increased vulnerability for depression in the general population, probably through increased glucocorticoid sensitivity. 30 More recently, various studies have focused on the FK506-binding protein FKBP5, a cochaperone of hsp-90 involved in the regulation of GR sensitivity, 31 which is also involved in HPA axis responsivity. This protein is a component of the GR heterocomplex, which, upon binding of cortisol, is replaced by FKBP4, which in turn facilitates the nuclear translocation of the hormone-receptor complex and its transcriptional activity. 32 Altered GR function may lead to impaired feedback regulation, with the resulting HPA hyperactivation commonly observed in chronic stress and depression. Therefore, various SNPs have been identified in the FKBP5 gene, some of them associated with increased FKBP5 protein expression, which in turn may lead to changes in GR, with the resulting effect on HPA axis regulation. 32 Increased FKBP5 protein expression may reduce hormone-binding affinity and may interfere with the translocation of the hormone-receptor complex. It is noteworthy that glucocorticoids may induce increased expression of this cochaperone, constituting an intracellular negative feedback loop to regulate GR activity. 33 One of the SNPs of the FBPP5 gene, defined as the substitution of a cytosine (C) by a thymine (T) and therefore identified as the high-induction allele T, was associated with increased FKBP5 protein expression and altered HPA response. Upon exposure to stressful stimuli, carriers of the T allele exhibited slower recovery of the cortisol response and homozygous carriers of the allele who experienced severe abuse during childhood presented increased vulnerability for the development of depression during adulthood, 34 which may also be associated with having an increased number of depressive episodes. 32
Role of CRF
CRF-containing circuits in the CNS play a critical role in the coordination of the stress response, both as a neuroendocrine factor regulating the HPA axis and through its function as a neurotransmitter, mediating behavioral, immune, and autonomic responses to stress. 35 CRF neurons are localized throughout different cortical areas, participating in neural pathways involved in cognitive responses, and limbic areas such as the central nucleus of the amygdala and the bed nucleus of the stria terminalis, where it participates in the regulation of emotional responses. 23 CRF projections from the amygdala have been shown to reach the hypothalamic paraventricular nucleus (therefore enhancing the activation of the HPA axis in response to stress) and the monoaminergic nuclei in the brainstem, including the locus coeruleus (LC) and the raphe nuclei (RN). 3 Moreover, CRF stimulates norepinephrine release in the LC, 36 with the consequent noradrenergic activation of the autonomic nervous system and the HPA axis, while mainly inhibiting serotonergic neurons in the RN, 37 which in turn may affect other structures through serotonergic projections to the amygdala, hippocampus, and paraventricular nucleus. 3 Therefore, through the regulation of these monoaminergic systems, CRF participates in neurobiological processes underlying mood and anxiety disorders, producing anxiogenic and depressogenic effects. 35 Increased CSF concentrations of CRF have consistently been reported in depressed and suicidal patients. 38 In addition, CRF may also be involved in anxiety and the encoding of emotional memories, 23 , 35 playing a critical role in the stress response not only during adulthood but also in mediation of the long-lasting effects of trauma and other early life stressful experiences. Moreover, increased levels of CRF may also be involved in neuroplastic changes induced by chronic stress, 39 and this effect may also be enhanced by glucocorticoids as a component of the stress response. 40
Various studies have focused on CRF, CRF-binding protein, and CRF type 1 receptor (CRHR1) genes, resulting in several important findings. 41 Indeed, several SNPs in the CRHR1 and haplotypes formed by certain SNPs involved in mediating the effects of early adverse experiences on the risk for adult depression have been identified. 42 Upon binding to CRF, this receptor participates in the activation of the HPA axis and plays a critical role in emotional and cognitive functions mediated by CRF in extrahypothalamic brain regions, including the amygdala and the LC, 35 therefore influencing arousal, attention, conscious perception of emotional experiences, and memory consolidation. Two haplotypes formed by different SNPs in the CRHR1 gene were associated with reduced symptoms of depression in subjects exposed to early stressful experiences. Because CRHR1 may be critically involved in the consolidation of emotionally charged memories, such as those produced by childhood aversive experiences, it was proposed that carriers of two copies of these haplotypes, which also exhibited overrepresentation of the protective alleles of the studied SNPs, 42 may have altered activation of memory consolidation processes. This may lead to decreased emotional influence in the cognitive processing of these memories, therefore protecting the individual from his or her potentially depressogenic and anxiogenic effects. 43
Role of Serotonin
The serotonergic hypothesis of depression posits deficient serotonergic activity in the CNS with increased vulnerability for the development of depression. The main groups of serotonergic neurons in the CNS are located within the boundaries of the RN, where an array of ascending projections arise from the dorsal RN (B6 and B7) and the medial RN (B8). The dorsal RN–forebrain tract projects to the PFC, amygdala, nucleus accumbens, and ventral hippocampus, among other forebrain structures, 44 and it participates in the state of anticipatory anxiety and thus plays an adaptive role during stressful situations. 45 The dorsal RN–forebrain tract has been associated with activation of the limbic structures (e.g., the amygdala) in the presence of environmental stressors associated with unpleasant experiences, and it is also involved in the regulation of potential emotional reactions. Alterations of this system, particularly involving dorsal RN–amygdala projections, may be associated with symptoms of anxiety. 45 The medial RN–forebrain tract projects to the dorsal hippocampus and hypothalamus, among other neural structures, 44 , 45 and it participates in conferring tolerance to unpleasant, unavoidable, and persistent aversive stimuli such as those perceived during chronic stressful situations. The medial RN–forebrain tract is also associated with adaptive control on negative emotional experiences. Therefore, alterations of this system, particularly involving medial RN–hippocampal projections, may be associated with decreased tolerance to aversive stimuli, learned helplessness, and subsequent depression. 45 , 46 Serotonergic neurons in the RN are also interconnected and are physiologically integrated with other monoaminergic systems in the brainstem, including noradrenergic and dopaminergic circuits. 47 It has been shown that both the dorsal RN and the medial RN receive noradrenergic projections, 48 which appear to be excitatory. The LC receives serotonergic projections from the RN reciprocally, 48 which appear to exert an indirect modulatory effect by inhibiting glutamatergic activation of the LC. The dorsal RN also modulates dopaminergic activity through projections to the ventral tegmental area, which appear to be excitatory, 49 and dopaminergic projections to the dorsal RN reciprocally exert an indirect inhibitory effect by increasing the activity of somatodendritic 5-hydroxytryptamine (serotonin [5-HT]) autoreceptors. 44
Figure 2 illustrates the network of functional connections between different neurotransmitter systems in the CNS, as well as their respective connections with different cortical and limbic structures involved in the stress response.
FIGURE 2. Schematic Representation of Neurotransmitter Systems Involved in the Stress Response and Regulation of Emotional and Cognitive Functions a
a The raphe nuclei send serotonergic projections from their medial component to the hippocampus and from their dorsal component to the amygdala and the DLPFC. The locus coeruleus sends noradrenergic projections to the hippocampus and the amygdala. The ventral tegmental area sends dopaminergic projections to the nucleus accumbens and the DLPFC. The nucleus accumbens is reciprocally connected with the amygdala and the OFC, which in turn is reciprocally connected with the medial prefrontal cortex and the ACC. All of these are reciprocally connected with the amygdala and with the DLPFC. Reciprocal connections between the raphe nuclei, the locus coeruleus, and the ventral tegmental area are also represented. ACC, anterior cingulate cortex; D, dorsal; DLPFC, dorsolateral prefrontal cortex; M, medial; OFC, orbitofrontal cortex.
At the molecular level, 5-HT is released into the synaptic cleft, where it binds to both presynaptic and postsynaptic receptors. A growing number of 5-HT receptors have been identified, including 14 different types, classified in seven families with various subtypes each. Each of the serotonin receptor subtypes exhibits a unique regional neuroanatomic distribution, conferring specificity on the effects of activation of this widespread and diffuse serotonergic innervation. Synaptic concentrations of 5-HT are regulated by the serotonin transporter (5-HTT), which is responsible for its reuptake, therefore regulating its availability to bind and activate specific 5-HT receptors. 47 The 5-HTT is believed to be the primary molecular target of selective serotonin reuptake inhibitors antidepressants. Hence, 5-HTT blockade by selective serotonin reuptake inhibitors is translated into higher 5-HT concentrations in the synaptic cleft, allowing increased activation of 5-HT receptors. 46 , 47 The clinical efficacy of antidepressants is not directly associated with this acute mechanism; instead, it is linked to more adaptive changes. Continuous administration of selective serotonin reuptake inhibitors leads to desensitization or down-regulation of somatodendritic 5-HT 1A autoreceptors in the RN after several days (which are known to moderate the release of 5-HT into the synaptic cleft) and up-regulation of postsynaptic 5-HT 1A and desensitization of 5-HT 2A receptors. 50
In addition to serotonergic projections directly involved in cognitive and emotional functions, projections from the RN have been shown to innervate CRF-containing neurons in the paraventricular nucleus. 51 There is evidence that these projections stimulate the HPA axis and the autonomic nervous system; glucocorticoids and catecholamines may reciprocally affect the serotonergic system during stressful situations. 46 Various studies have shown that postsynaptic 5-HT 1A receptors in different limbic structures may be down-regulated or desensitized by glucocorticoids or exposure to chronic stress. 52 , 53 In addition, it has been shown that cortisol may increase 5-HT uptake in vitro, an effect attributed to increased expression of the 5-HTT gene by the glucocorticoid, 54 therefore providing further support for the reciprocal regulation of the HPA and 5-HT systems and their potential interplay in the interface between stress and depression. 46
Various studies have also focused on the structure of the 5-HTT gene, in which a polymorphism was identified in its promoter region. 55 The promoter activity is regulated by sequence elements located in the upstream regulatory region, known as the 5-HTT gene-linked polymorphic region (5-HTTLPR), where a short (S) and a long (L) allele have been identified. 6 Hence, the short promoter variant (5-HTTLPR-S) was associated with decreased transcriptional efficiency compared with the long allele (5-HTTLPR-L), resulting in decreased expression of the 5-HTT gene, 55 which may affect the modulation of serotonergic activity in response to stress. This notion has been supported by multiple clinical and preclinical studies, 56 including evidence observed in functional brain imaging studies, in which carriers of the S allele (homozygous or heterozygous for the short allele) exhibited increased amygdala reactivity to fearful and threatening stressors compared with those homozygous for the L allele, 57 which suggests that variations in the 5-HTT gene may be involved in psychological responses to stress. 6 Although various studies have shown increasing evidence that this polymorphism moderates the relationship between stress and depression, 56 there are still other studies suggesting certain controversy around this hypothesis.
The amygdala participates in the regulation of emotional reactions to stressful events, and its increased reactivity was associated with anxiety and altered mood regulation. 14 Hence, a potential association between 5-HTT gene polymorphism and increased reactivity of the amygdala in response to negative stressors 58 may contribute to a better understanding of the potential effect of the molecular mechanisms underlying this association. Moreover, the amygdala also plays a critical role in the activation of the HPA axis, and hyperactivation of the amygdala may also lead to increased plasma levels of cortisol. Indeed, carriers of the S allele exhibit increased activation of the amygdala and elevated cortisol levels in response to a laboratory stressor. 11 The association between the 5-HTTLPR-S variation and a potentially decreased expression of the 5-HTT gene may appear paradoxical, considering the potential vulnerability attributed to 5-HTTLPR-S carriers. Therefore, it is conceivable that alterations in 5-HTT gene regulation (and consequent effects on synaptic 5-HT levels) may differ, with the former expressed as a result of constitutive conditions and the latter triggered by environmental factors. It has been proposed that 5-HTTLPR-S carriers may exhibit “essentially” increased concentrations of 5-HT, which may result in down-regulation of postsynaptic 5-HT receptors. This may lead to a relative desensitization of the serotonergic system, 58 providing a potential explanation for the vulnerability exhibited by 5-HTTLPR-S carriers. By contrast, up-regulation of the 5-HTT gene, associated with the effect of environmental stressors and the resulting hyperactivation of the HPA axis and hypercortisolism, may lead to increased 5-HT reuptake and decreased concentrations of 5-HT in the synaptic cleft, 54 which has been widely associated with the development of mood disorders.
Role of Dopamine
Dopamine has also been implicated in the neural mechanisms of stress responses, including stress-related regulation of the HPA axis, as well as in the pathophysiology of depression. 59 , 60 The main groups of dopaminergic neurons in the CNS comprise the retro-rubro field (A8), the substantia nigra pars compacta (A9), and the ventral tegmental area (A10), where the mesolimbic and mesocortical pathways arise. The mesolimbic pathway projects mainly to the nucleus accumbens and other limbic structures, including the amygdala, hippocampus, bed nucleus of the stria terminalis, and septum. This pathway is implicated in the processing and reinforcement of rewarding stimuli, motivation, and the subjective experience of pleasure. 59 The mesocortical pathway projects mainly to the PFC, ACC, and entorhinal cortex and is critically involved in cognitive functions such as concentration and working memory. 59
Environmental stressors provoke increased activity in the amygdala, which in turn may increase the concentrations of dopamine in the mesocortical pathway (particularly in the PFC), therefore conferring exaggerated salience to relatively mild negative stimuli 60 and contributing to the resulting negative bias in cognitive processing. Regarding the mesolimbic pathway, it has been shown that stressful events may induce opposite responses, depending on the potential controllability of the stimuli, 61 and the consequent subjective assessment. Therefore, exposure to acute and controllable stressors was associated with increased dopamine release in the ventral striatum, whereas exposure to chronic and uncontrollable stressful stimuli was associated with decreased dopaminergic activity 61 with resulting anhedonia. Moreover, it has been shown that unavoidable or uncontrollable stressors may lead to decreased dopamine release in the nucleus accumbens and impaired response to environmental stimuli, which may result in the expression and exacerbation of depressive symptoms induced by stress. 62 The inability to experience pleasure, associated with loss of interest and motivation in usual activities, constitutes the pathognomonic anhedonia exhibited by patients with depression, 59 , 60 and it has been shown that impaired dopaminergic function is critically involved in altered reward processing underlying anhedonia. 63 , 64 Moreover, the mesolimbic dopaminergic pathway, particularly the nucleus accumbens, participates in the processing of rewarding and hedonic experiences in association with the orbitofrontal cortex, which may be involved in the subjective assessments of hedonic and rewarding value. 65 The orbitofrontal cortex is connected with the ACC and dorsolateral PFC, where this emotional input participates in cognitive processes; by contrast, the nucleus accumbens receives dopaminergic projections from the ventral tegmental area, which may be enhanced by glutamatergic stimulation from the amygdala, to increase motivation. 65 Substantial interaction has also been described between the ventral tegmental area and the RN, 59 which may be critically involved in emotional processing.
Because increased dopamine release in the mesolimbic pathway has been observed not only in response to rewarding stimuli but also in the presence of aversive situations (particularly when these are perceived as controllable and escapable 61 ), it has been suggested that dopamine plays an adaptive role associated with motivation, increased arousal, and behavioral control in response to stress, including both appetitive and aversive conditions. 66
Role of Norepinephrine
Catecholamines (and more specifically norepinephrine) have long been posited to play a major role in the pathophysiology of affective disorders, forming the catecholamine hypothesis of depression. The main group of norepinephrine-containing neurons in the CNS is located within the LC (A6), where various projections arise to widely innervate cortical and subcortical areas, 48 including the amygdala, the hippocampus, and the paraventricular nucleus of the hypothalamus. 36 Projections from the LC to the ventral tegmental area have been described, in which norepinephrine has been shown to potentiate dopamine release. Projections from the LC to the RN have also been described, in which norepinephrine exerts regulatory effects on 5-HT release. 48 There is also evidence of reciprocal regulation between norepinephrine and 5-HT, not only through connections between both aminergic systems but also through limbic structures such as the hippocampus. 67 In addition, reciprocal connections between norepinephrine - and CRF-containing neurons suggest a critical role of the LC in the regulation of neural and neuroendocrine responses to stress. 36
In response to acute stressors, norepinephrine is released throughout different structures in the CNS, resulting in enhanced arousal and hypervigilance, in the context of adaptive responses to stress. Moreover, activation of the LC has been associated with subsequent stimulation of the lateral hypothalamus, which in turn participates in the activation of the sympathetic branch of the autonomic nervous system, therefore complementing the adaptive response to stress. 36 A potential dysfunction of the LC has been observed during chronic stress (particularly upon exposure to unavoidable or uncontrollable stressors), leading to altered norepinephrine release, which was associated with some features of learned helplessness as well as problems in cognitive functions such as attention and memory, which are frequently observed in depression. In addition, dysregulation of the norepinephrine system has also been described in altered states of arousal, 48 which is commonly observed in anxiety disorders as well as in depression.
Neuroplasticity and Neurogenesis: Role of Neurotrophic Factors
Several studies have focused on the potential role of neurotrophic factors in critical neural processes, with particular attention on the neurotrophin family, which is composed of nerve growth factor, brain-derived neurotrophic factor (BDNF), neurotrophin-3, neurotrophin-4/5, and neurotrophin-6. Among these neurotrophins, a growing body of research has focused on the role of BDNF in the regulation of brain development, neuroplasticity, and neurogenesis. 68 Various studies strongly suggest that decreased levels of BDNF may lead to depressive symptoms, whereas up-regulation of BDNF is associated with clinical recovery. 69 In vitro studies have demonstrated that BDNF may decrease 5-HT uptake, suggesting a potential role of the neurotrophin in regulation of 5-HTT. 70 Chronic stress, with the resulting activation of the HPA axis, may damage neurons in certain CNS structures (particularly in the hippocampus, where high levels of GRs have been found) and these changes have been associated with decreased availability of neurotrophic factors such as BDNF. 71 Moreover, it has been shown that increased levels of glucocorticoids, at least partially, may be involved in down-regulation of BDNF. 72 By contrast, it has been demonstrated that various antidepressants increase the expression of BDNF in the hippocampus 69 in a dose-dependent and time-dependent manner, which is consistent with the time dependency of therapeutic effects of antidepressants, therefore suggesting a role for BDNF in their mechanism of action. 73 The potential association between successful pharmacotherapy and the observed up-regulation of BDNF in the hippocampus suggests that BDNF may be involved in the long-lasting effects of antidepressants through neuroplastic changes in certain neural structures such as the hippocampus, amygdala, and PFC. 69 Moreover, it has been shown that BDNF and 5-HT may induce hippocampal neurogenesis. 74
Most neurons in the CNS are generated during early periods of development, although more recent studies have demonstrated that some neural structures, such as the dentate gyrus of the hippocampus, actually continue generating neurons later in life. 75 Therefore, neurogenesis in the adult CNS may be stimulated by special conditions, particularly those related to enhanced hippocampal activity and increased levels of 5-HT, 76 , 77 but it may be inhibited by stressful situations and increased levels of glucocorticoids. 78 Under chronic stress conditions, with increased activation of the HPA axis, inhibition of hippocampal neurogenesis may interfere with the formation of new cognitions, therefore contributing to provoking and sustaining ongoing depressogenic conditions. According to this hypothesis, successful therapeutic interventions may require recovery of the normal rate of hippocampal neurogenesis. This recovery may be associated with a direct effect of antidepressants through increasing levels of 5-HT 75 or indirectly through modulation of the HPA axis and increasing levels of BDNF, which was associated with up-regulation of neuroplasticity and increasing neurogenesis. This hypothesis remains quite controversial because of failure to confirm the increase in neurogenesis after long-term antidepressant treatment. 79
Various studies have focused on BDNF gene regulation and variations potentially involved in mood disorders, resulting in the identification of different SNPs. Among these, an SNP has been identified at nucleotide position 196 in the coding region of the BDNF gene, where a guanine (G) is replaced by an adenine (A), resulting in the substitution of valine (Val) by methionine (Met) at codon 66, which is thus termed Val66Met. This is where the presence of a Met allele has been associated with a functional alteration (i.e., abnormal intracellular trafficking and decreased secretion of BDNF). 73 , 76 Studies on carriers of the Met-BDNF allele revealed relatively smaller hippocampal volumes compared with those individuals who were homozygous for the Val-BDNF allele. 73 This was also associated with reduced hippocampal activation and deficient cognitive performance, 12 , 73 which have also been associated with lower emotional stability and increased vulnerability for the development of depressive symptoms.
Inflammatory Processes: Role of Cytokines
It has been demonstrated that acute and chronic psychosocial stress may activate inflammatory responses. 80 Increased blood concentrations of proinflammatory cytokines, such as interleukin-1, interleukin-6, and tumor necrosis factor-alpha, have been associated with the effect of diverse environmental stimuli, including psychosocial stress, 81 and this immune activation has also been observed in major depression. 82 Moreover, major depression may induce increased inflammatory responses to stress, and this has been observed mostly in patients exposed to adverse early life events, therefore suggesting a link between these and increased inflammatory responses to stress later in life. 80 To understand the role of proinflammatory cytokines in chronic stress and the subsequent development of depression, various studies have focused on their potential mechanisms of action. Environmental stressors activate the sympathetic branch of the autonomic nervous system, with the resulting release of catecholamines, which in turn activates their receptors on immune cells and thus stimulates the release of proinflammatory cytokines. 83 Chronic inflammatory responses in the CNS may result in excessive release of proinflammatory cytokines, which in turn may lead to decreased concentrations of neurotrophins (including BDNF), leading to impaired neuroplasticity 83 and decreased neurogenesis (particularly in the hippocampus 82 ), which have been associated with the origin of cognitive impairment and mood disorders. Proinflammatory cytokines have also been involved in regulation of the HPA axis, stimulating release of CRF with resulting hypercortisolism, 83 which has been associated with reduced sensitivity of GRs and glucocorticoid resistance. 81 , 83 Increased levels of cortisol, such as those observed during chronic stress, may lead to decreased synthesis of 5-HT due to reduced activity of the rate-limiting enzyme tryptophan hydroxylase. Hypercortisolism has been also associated with increased activity of tryptophan dioxygenase (indoleamine-pyrrole 2,3-dioxygenase), which is responsible for the degradation of tryptophan to kynurenine, with the resulting decreased synthesis and release of 5-HT. 83 Proinflammatory cytokines such as interferon have also been involved in the modulation of this pathway, stimulating indoleamine-pyrrole 2,3-dioxygenase and thus leading to reduced synthesis of 5-HT and increased synthesis of kynurenine. 84 Degradation of kynurenine leads to the formation of 3-hydroxykynurenine, which produces free radical species involved in oxidative stress, and kynurenic acid and quinolinic acid, which activate the glutamatergic system. This leads to neurotoxicity and neuronal apoptosis, which are also involved in the pathophysiology of depression. 83 , 84 In addition, certain proinflammatory cytokines, such as interleukin-1 and tumor necrosis factor, have been shown to affect serotonergic neurotransmission by stimulating the 5-HTT and thus reducing intersynaptic concentrations of 5-HT in the CNS. 83 , 85
Understanding the molecular mechanisms underlying neuroinflammatory processes in the CNS, particularly the role played by proinflammatory cytokines in mood disorders, has inspired various studies aimed at improving depressive symptoms by attenuating these processes. Preclinical studies have demonstrated the efficacy of certain anti-inflammatory cytokines to block the depressive-like state induced by proinflammatory cytokines in rodents. 83 Other studies have also approached the consequences of proinflammatory cytokines, antagonizing the activity of the glutamatergic system, activated by the kynurenine pathway. 81
Stress, Appraisal, and Coping: Role of Psychological Vulnerability
Psychological vulnerability depends on various features related to stressful life events (including strength, intensity, and length of the impact) and the availability of personal resources to cope with them. More remarkably, however, it may depend on cognitive appraisal, particularly the balance between stressors and individual resources, and the resulting coping strategies. 86 Chronic exposure to unavoidable and uncontrollable stressors may lead to decreasing cognitive and behavioral coping strategies to handle environmental events, mostly as a result of cognitive appraisals that personal resources are not enough, which has been associated with increasing feelings of helplessness. 86 According to the cognitive model of depression, 87 early life experiences provide the background to develop cognitive schemas, which in turn represent the basis to transform simple data into cognitions that are learned and stored in long-term memory. Adverse early life events, including childhood sexual or physical abuse 88 and peer victimization 89 (also known as bullying), may contribute to the formation of particular cognitive schemas. These schemas may be inactive during long periods and reactivated by new experiences at a later time, particularly those with strong emotional valence. In response to stressful situations in adulthood, activated dysfunctional schemas may induce negative biases during information processing, with consequent dysfunctional effects, including cognitive processing, emotional reactions, and behavioral responses, constituting the essential core of cognitive vulnerability. 87 Therefore, dysfunctional schemas shaped during childhood, with systematic negative biases, may lead to negatively biased appraisals, with consequent limitations in further processing of the resulting cognitions, therefore leading to feelings of helplessness and subsequent depression.
Epigenetics: Role of Gene–Environment Interactions
The term epigenetics refers to heritable characteristics that are not determined by structural changes in the underlying genetic sequence. At the molecular level, epigenetic mechanisms involve biochemical changes of nucleotides, without altering the DNA sequence, and the associated histone proteins, which constitute chromatin. Changes in the structure of chromatin may affect gene expression by allowing transcription factors to gain access to gene regulatory elements. Hence, environmental factors may induce changes in the chromatin state, which in turn may improve exposure of genes to the impact of different transcription factors, therefore increasing or decreasing gene expression while the original DNA sequence remains unaltered. 90 Potential changes include DNA methylation, which has been associated with down-regulation of gene expression; histone acetylation, which may induce up-regulation of gene expression; and histone methylation and phosphorylation, both of which may lead to activation or repression of transcriptional events. 90 Recent research has contributed to identifying epigenetic mechanisms in the context of stressful situations, which may induce long-lasting changes in gene expression in different neural structures. In turn, such changes have been associated with the development of stress-related conditions such as anxiety disorders and depression. Preclinical studies have revealed that chronic stress may regulate histone acetylation in the hippocampus, inducing transient increases and subsequent decreases; transient increases have also been observed in the amygdala. 91
In addition, preclinical studies also revealed that increased levels of CRF, observed during chronic stress conditions, have been associated with decreased DNA methylation at the promoter region of the CRF gene. 92 Moreover, a history of early adverse experiences has been associated with changes in histone markers and DNA methylation of the GR gene, particularly in the hippocampus, and changes in DNA methylation have also been observed in the GR and BDNF genes. 41 Therefore, chronic stress, including early stressful experiences, may induce diverse epigenetic changes in different neural structures, with a subsequent effect on their respective functions. This, in turn, may predispose individuals to increased vulnerability to stress and to the development of diverse clinical conditions such as depression.
Childhood Trauma: Role of Early Adverse Experiences
Early life stress, defined as adverse conditions and traumatic events experienced during childhood, represents a major factor of vulnerability in the origin and development of depression and bipolar disorder. 3 , 5 , 27 The association between a history of adverse and traumatic experiences during childhood and the development of mood disorders later in life has been observed particularly after additional stressful events during adulthood. 5 It has been shown that adverse early life events (including abuse, neglect, or loss) contribute to the formation of dysfunctional cognitive schemas, which may induce negative biases in response to stressful situations at a later time, therefore contributing to generating cognitive vulnerability. 56 This mechanism was also recently described in victims of bullying. 89 Moreover, it has been proposed that certain early life events, such as neglect, may lead to the formation of dysfunctional attitudes; this has also been associated with long-term hyperactivity of the HPA axis. 93 The effect of adverse early life events has been conclusively demonstrated to induce long-lasting changes in neural and neuroendocrine systems involved in adaptive responses to stress, particularly in CRF neurotransmission. 23 This, in turn, may be translated into persistent sensitization and increased responsiveness to stress. 3 , 5 Increased levels of CRF may lead to hyperactivity of the HPA axis and hypercortisolism, which may induce morphologic changes such as reduced hippocampal volume. 72 In this regard, various studies have focused on the role of hippocampal GRs, and increased levels of cortisol (in a sustained and prolonged manner) have been shown to induce down-regulation of GRs in certain areas of the hippocampus. 94 Moreover, additional research has suggested that the availability and efficacy of hippocampal GRs may be permanently affected as a result of early stressful experiences, 88 therefore contributing to glucocorticoid resistance and the consequent hyperreactivity of the HPA axis observed in response to additional stressful situations. In addition, increased concentrations of cortisol and decreased GR availability, induced by stressful situations during childhood, have been associated with decreased hippocampal volume and neural activity in adulthood as well as increased reactivity of the HPA axis, with the consequent functional alterations observed in adulthood. 88 , 95 A history of early life adverse experiences was also associated with hyperreactivity of neural and neuroendocrine responses to stress, which is reflected through increased CRF activity, hypercortisolism, and glucocorticoid resistance. 27 , 96
Klengel et al. 97 reported that a polymorphism in the FKBP5 gene increases the risk for the development of stress-related psychiatric disorders in adults by an allelic-specific, child abuse/neglect–dependent DNA demethylation in functional glucocorticoid response elements of FKBP5. Thus, activation of a sensitized system in the presence of additional stressful situations later in life may result in an exaggerated and maladaptive activation of the stress response, therefore generating increased vulnerability to the development of depressive symptoms upon exposure to additional stressors in adulthood. 42 , 98
Conclusions
The role of stressful life events in the origin and development of depression may be conceptualized as the result of multiple interactions between the effect of environmental stressors and individual factors of vulnerability. Figure 3 illustrates the role of these factors and their potential interactions at the interface between chronic stress and depression. Genetic factors, including SNPs, may be associated with functional and structural alterations in certain neural structures, including increased reactivity of the amygdala and decreased function of the hippocampus. Adverse early life events have been shown to engender biological changes in the developing CNS, as well as psychological changes reflected in the formation of dysfunctional cognitive schemas, 99 with the resulting biased cognitive processing of environmental stimuli, which may be translated into cognitive and emotional vulnerability. 87 These may be further activated in response to stress in adulthood, contributing to increased vulnerability to depression. 27
FIGURE 3. Schematic Representation of Different Factors Involved in the Stress Response and Their Potential Role in Stress and Depression a
a Genetic polymorphisms (represented as genetic vulnerability) participate in the development of the CNS and, together with the influence of early environmental factors (represented by early life stress) and chronic stress, result in a particular CNS phenotype. Early life stress may also induce certain cognitive vulnerability, which in turn may result in emotional vulnerability. Upon the impact of traumatic events or chronic stress, a predisposed CNS responds with increased levels of CRF, hyperactivation of the HPA axis, and increased levels of cortisol, which may lead to molecular changes in different circuits (represented by molecular vulnerability), as well as altered cognitive and emotional responses (represented by emotional vulnerability). This, in turn, may result in increased vulnerability for the development of symptoms of anxiety and depression. CRF, corticotropin-releasing factor; HPA, hypothalamic-pituitary-adrenal.
The impact of abuse and neglect during childhood clearly leads to persistent changes in neural and neuroendocrine systems involved in the regulation of adaptive responses. Functional or structural alterations in the CNS, particularly in the cerebrocortical regions as well as in the amygdala and the hippocampus, along with cognitive biases, may induce biological changes such as increased levels of CRF. Upon exposure to environmental stressors, this mechanism may be translated into hyperactivity of the HPA system, with increased levels of CRF and cortisol, which in turn may lead to transcriptional events. Such molecular changes affecting different aminergic systems, particularly on the regulation of 5-HT together with altered cognitive processing, may result in emotional changes, thereby predisposing to symptoms of anxiety and depression. Therefore, multiple vulnerability factors (including psychological, biological, cognitive, genetic, and epigenetic factors) converge on different aspects of HPA regulation. This complex set of pathways likely links vulnerability to stress with the pathogenesis of depression. In addition, environmental stress has also been associated with inflammatory responses in the CNS with excessive release of proinflammatory cytokines, which may lead to further stimulation of the HPA axis, with resulting hypercortisolism and impaired 5-HT neurotransmission. Proinflammatory cytokines have also been associated with decreased neurotrophins, with resulting decreases in neuroplasticity and neurogenesis. Therefore, a better understanding of the molecular mechanisms underlying these processes may allow novel strategies aimed at improving depressive symptoms by attenuating neuroinflammation.
The observation that some individuals may exhibit stronger vulnerability to environmental stressors but others may be less sensitive, more resistant, or even resilient to similar experiences highlights the importance of further investigation of the nature of different risk factors. Future research should focus on further understanding the neurobiological background underlying these factors and should identify potential windows of intervention, including neural and molecular mechanisms involved in the interface between cognitive processing of environmental stressors and their potential effects in epigenetic processes. This may lead to the development of more successful treatments aimed at not only restoring altered neural and neuroendocrine mechanisms but also preventing the development of anxiety and mood disorders in vulnerable individuals.
This may be achieved either by identifying different vulnerability factors, which in turn may become targets for novel therapeutic interventions, or by increasing and promoting protective resources in individuals exposed to stressful conditions, particularly those exposed to traumatic events or adverse conditions during childhood.
Dr. Nemeroff has in the last 3 years consulted to Takeda, Xhale, Mitsubishi, Clintara, Taisho, Prismic, and Gerson Lehrman, has received grants/research support from NIH and the Agency for Healthcare Research and Quality, has served on the scientific advisory boards for Xhale, AFSP, the Brain and Behavior Research Foundation, Clintara, and the Anxiety and Depression Association of America, and holds stock in Celgene, Seattle Genetics, Abbvie, Titan, OPKO, and Xhale. Dr. Tafet reports no financial relationships with commercial interests.
1 Gold PW : The organization of the stress system and its dysregulation in depressive illness . Mol Psychiatry 2015 ; 20:32–47 Crossref , Medline , Google Scholar
2 Nemeroff CB : The preeminent role of early untoward experience on vulnerability to major psychiatric disorders: the nature-nurture controversy revisited and soon to be resolved . Mol Psychiatry 1999 ; 4:106–108 Crossref , Medline , Google Scholar
3 Heim C, Nemeroff CB : The role of childhood trauma in the neurobiology of mood and anxiety disorders: preclinical and clinical studies . Biol Psychiatry 2001 ; 49:1023–1039 Crossref , Medline , Google Scholar
4 López JF, Akil H, Watson SJ : Neural circuits mediating stress . Biol Psychiatry 1999 ; 46:1461–1471 Crossref , Medline , Google Scholar
5 Heim C, Newport DJ, Mletzko T, et al. : The link between childhood trauma and depression: insights from HPA axis studies in humans . Psychoneuroendocrinology 2008 ; 33:693–710 Crossref , Medline , Google Scholar
6 Caspi A, Sugden K, Moffitt TE, et al. : Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene . Science 2003 ; 301:386–389 Crossref , Medline , Google Scholar
7 Kaufman J, Plotsky PM, Nemeroff CB, et al. : Effects of early adverse experiences on brain structure and function: clinical implications . Biol Psychiatry 2000 ; 48:778–790 Crossref , Medline , Google Scholar
8 Kaufman J, Yang BZ, Douglas-Palumberi H, et al. : Brain-derived neurotrophic factor-5-HTTLPR gene interactions and environmental modifiers of depression in children . Biol Psychiatry 2006 ; 59:673–680 Crossref , Medline , Google Scholar
9 Bradley RG, Binder EB, Epstein MP, et al. : Influence of child abuse on adult depression: moderation by the corticotropin-releasing hormone receptor gene . Arch Gen Psychiatry 2008 ; 65:190–200 Crossref , Medline , Google Scholar
10 Nemeroff CB, Seligman F : The pervasive and persistent neurobiological and clinical aftermath of child abuse and neglect . J Clin Psychiatry 2013 ; 74:999–1001 Crossref , Medline , Google Scholar
11 Gotlib IH, Joormann J, Minor KL, et al. : HPA axis reactivity: a mechanism underlying the associations among 5-HTTLPR, stress, and depression . Biol Psychiatry 2008 ; 63:847–851 Crossref , Medline , Google Scholar
12 Gatt JM, Nemeroff CB, Dobson-Stone C, et al. : Interactions between BDNF Val66Met polymorphism and early life stress predict brain and arousal pathways to syndromal depression and anxiety . Mol Psychiatry 2009 ; 14:681–695 Crossref , Medline , Google Scholar
13 Binder EB, Owens MJ, Liu W, et al. : Association of polymorphisms in genes regulating the corticotropin-releasing factor system with antidepressant treatment response . Arch Gen Psychiatry 2010 ; 67:369–379 Crossref , Medline , Google Scholar
14 LeDoux JE : Brain mechanisms of emotion and emotional learning . Curr Opin Neurobiol 1992 ; 2:191–197 Crossref , Medline , Google Scholar
15 Ghashghaei HT, Hilgetag CC, Barbas H : Sequence of information processing for emotions based on the anatomic dialogue between prefrontal cortex and amygdala . Neuroimage 2007 ; 34:905–923 Crossref , Medline , Google Scholar
16 Drevets WC, Savitz J, Trimble M : The subgenual anterior cingulate cortex in mood disorders . CNS Spectr 2008 ; 13:663–681 Crossref , Medline , Google Scholar
17 Price JL, Drevets WC : Neural circuits underlying the pathophysiology of mood disorders . Trends Cogn Sci 2012 ; 16:61–71 Crossref , Medline , Google Scholar
18 Etkin A, Egner T, Kalisch R : Emotional processing in anterior cingulate and medial prefrontal cortex . Trends Cogn Sci 2011 ; 15:85–93 Crossref , Medline , Google Scholar
19 Ray RD, Zald DH : Anatomical insights into the interaction of emotion and cognition in the prefrontal cortex . Neurosci Biobehav Rev 2012 ; 36:479–501 Crossref , Medline , Google Scholar
20 Motzkin JC, Philippi CL, Wolf RC, et al. : Ventromedial prefrontal cortex is critical for the regulation of amygdala activity in humans . Biol Psychiatry 2015 ; 77:276–284 Crossref , Medline , Google Scholar
21 Zhong M, Wang X, Xiao J, et al. : Amygdala hyperactivation and prefrontal hypoactivation in subjects with cognitive vulnerability to depression . Biol Psychol 2011 ; 88:233–242 Crossref , Medline , Google Scholar
22 Heim CM, Mayberg HS, Mletzko T, et al. : Decreased cortical representation of genital somatosensory field after childhood sexual abuse . Am J Psychiatry 2013 ; 170:616–623 Crossref , Medline , Google Scholar
23 Arborelius L, Owens MJ, Plotsky PM, et al. : The role of corticotropin-releasing factor in depression and anxiety disorders . J Endocrinol 1999 ; 160:1–12 Crossref , Medline , Google Scholar
24 Holsboer F : The corticosteroid receptor hypothesis of depression . Neuropsychopharmacology 2000 ; 23:477–501 Crossref , Medline , Google Scholar
25 Chrousos GP : Stress and disorders of the stress system . Nat Rev Endocrinol 2009 ; 5:374–381 Crossref , Medline , Google Scholar
26 Baumeister D, Lightman SL, Pariante CM : The interface of stress and the HPA axis in behavioural phenotypes of mental illness . Curr Top Behav Neurosci 2014 ; 18:13–24 Crossref , Medline , Google Scholar
27 Nemeroff CB, Binder E : The preeminent role of childhood abuse and neglect in vulnerability to major psychiatric disorders: toward elucidating the underlying neurobiological mechanisms . J Am Acad Child Adolesc Psychiatry 2014 ; 53:395–397 Crossref , Medline , Google Scholar
28 Bremner JD, Narayan M, Anderson ER, et al. : Hippocampal volume reduction in major depression . Am J Psychiatry 2000 ; 157:115–118 Link , Google Scholar
29 Vythilingam M, Heim C, Newport J, et al. : Childhood trauma associated with smaller hippocampal volume in women with major depression . Am J Psychiatry 2002 ; 159:2072–2080 Crossref , Medline , Google Scholar
30 DeRijk RH, Schaaf M, de Kloet ER : Glucocorticoid receptor variants: clinical implications . J Steroid Biochem Mol Biol 2002 ; 81:103–122 Crossref , Medline , Google Scholar
31 Horstmann S, Lucae S, Menke A, et al. : Polymorphisms in GRIK4, HTR2A, and FKBP5 show interactive effects in predicting remission to antidepressant treatment . Neuropsychopharmacology 2010 ; 35:727–740 Crossref , Medline , Google Scholar
32 Binder EB, Salyakina D, Lichtner P, et al. : Polymorphisms in FKBP5 are associated with increased recurrence of depressive episodes and rapid response to antidepressant treatment . Nat Genet 2004 ; 36:1319–1325 Crossref , Medline , Google Scholar
33 Vermeer H, Hendriks-Stegeman BI, van der Burg B, et al. : Glucocorticoid-induced increase in lymphocytic FKBP51 messenger ribonucleic acid expression: a potential marker for glucocorticoid sensitivity, potency, and bioavailability . J Clin Endocrinol Metab 2003 ; 88:277–284 Crossref , Medline , Google Scholar
34 Appel K, Schwahn C, Mahler J, et al. : Moderation of adult depression by a polymorphism in the FKBP5 gene and childhood physical abuse in the general population . Neuropsychopharmacology 2011 ; 36:1982–1991 Crossref , Medline , Google Scholar
35 Nemeroff CB : Neurobiological consequences of childhood trauma . J Clin Psychiatry 2004 ; 65(Suppl 1):18–28 Medline , Google Scholar
36 Valentino RJ, Foote SL, Page ME : The locus coeruleus as a site for integrating corticotropin-releasing factor and noradrenergic mediation of stress responses . Ann N Y Acad Sci 1993 ; 697:173–188 Crossref , Medline , Google Scholar
37 Kirby LG, Rice KC, Valentino RJ : Effects of corticotropin-releasing factor on neuronal activity in the serotonergic dorsal raphe nucleus . Neuropsychopharmacology 2000 ; 22:148–162 Crossref , Medline , Google Scholar
38 Nemeroff CB, Widerlöv E, Bissette G, et al. : Elevated concentrations of CSF corticotropin-releasing factor-like immunoreactivity in depressed patients . Science 1984 ; 226:1342–1344 Crossref , Medline , Google Scholar
39 Regev L, Baram TZ : Corticotropin releasing factor in neuroplasticity . Front Neuroendocrinol 2014 ; 35:171–179 Crossref , Medline , Google Scholar
40 Timmermans W, Xiong H, Hoogenraad CC, et al. : Stress and excitatory synapses: from health to disease . Neuroscience 2013 ; 248:626–636 Crossref , Medline , Google Scholar
41 McEwen BS, Eiland L, Hunter RG, et al. : Stress and anxiety: structural plasticity and epigenetic regulation as a consequence of stress . Neuropharmacology 2012 ; 62:3–12 Crossref , Medline , Google Scholar
42 Kendler KS, Kuhn JW, Prescott CA : Childhood sexual abuse, stressful life events and risk for major depression in women . Psychol Med 2004 ; 34:1475–1482 Crossref , Medline , Google Scholar
43 Polanczyk G, Caspi A, Williams B, et al. : Protective effect of CRHR1 gene variants on the development of adult depression following childhood maltreatment: replication and extension . Arch Gen Psychiatry 2009 ; 66:978–985 Crossref , Medline , Google Scholar
44 Hensler JG : Serotonergic modulation of the limbic system . Neurosci Biobehav Rev 2006 ; 30:203–214 Crossref , Medline , Google Scholar
45 Deakin JF, Graeff FG : 5-HT and mechanisms of defence . J Psychopharmacol 1991 ; 5:305–315 Crossref , Medline , Google Scholar
46 Tafet GE, Bernardini R : Psychoneuroendocrinological links between chronic stress and depression . Prog Neuropsychopharmacol Biol Psychiatry 2003 ; 27:893–903 Crossref , Medline , Google Scholar
47 Hamon M, Blier P : Monoamine neurocircuitry in depression and strategies for new treatments . Prog Neuropsychopharmacol Biol Psychiatry 2013 ; 45:54–63 Crossref , Medline , Google Scholar
48 Ressler KJ, Nemeroff CB : Role of norepinephrine in the pathophysiology and treatment of mood disorders . Biol Psychiatry 1999 ; 46:1219–1233 Crossref , Medline , Google Scholar
49 Kranz GS, Kasper S, Lanzenberger R : Reward and the serotonergic system . Neuroscience 2010 ; 166:1023–1035 Crossref , Medline , Google Scholar
50 Gray NA, Milak MS, DeLorenzo C, et al. : Antidepressant treatment reduces serotonin-1A autoreceptor binding in major depressive disorder . Biol Psychiatry 2013 ; 74:26–31 Crossref , Medline , Google Scholar
51 Lesch KP, Gutknecht L : Focus on The 5-HT1A receptor: emerging role of a gene regulatory variant in psychopathology and pharmacogenetics . Int J Neuropsychopharmacol 2004 ; 7:381–385 Crossref , Medline , Google Scholar
52 López JF, Chalmers DT, Little KY, et al. : A.E. Bennett Research Award. Regulation of serotonin1A, glucocorticoid, and mineralocorticoid receptor in rat and human hippocampus: implications for the neurobiology of depression . Biol Psychiatry 1998 ; 43:547–573 Crossref , Medline , Google Scholar
53 van Riel E, van Gemert NG, Meijer OC, et al. : Effect of early life stress on serotonin responses in the hippocampus of young adult rats . Synapse 2004 ; 53:11–19 Crossref , Medline , Google Scholar
54 Tafet GE, Toister-Achituv M, Shinitzky M : Enhancement of serotonin uptake by cortisol: a possible link between stress and depression . Cogn Affect Behav Neurosci 2001 ; 1:96–104 Crossref , Medline , Google Scholar
55 Lesch KP, Bengel D, Heils A, et al. : Association of anxiety-related traits with a polymorphism in the serotonin transporter gene regulatory region . Science 1996 ; 274:1527–1531 Crossref , Medline , Google Scholar
56 Karg K, Burmeister M, Shedden K, et al. : The serotonin transporter promoter variant (5-HTTLPR), stress, and depression meta-analysis revisited: evidence of genetic moderation . Arch Gen Psychiatry 2011 ; 68:444–454 Crossref , Medline , Google Scholar
57 Hariri AR, Mattay VS, Tessitore A, et al. : Serotonin transporter genetic variation and the response of the human amygdala . Science 2002 ; 297:400–403 Crossref , Medline , Google Scholar
58 Hariri AR, Drabant EM, Munoz KE, et al. : A susceptibility gene for affective disorders and the response of the human amygdala . Arch Gen Psychiatry 2005 ; 62:146–152 Crossref , Medline , Google Scholar
59 Dunlop BW, Nemeroff CB : The role of dopamine in the pathophysiology of depression . Arch Gen Psychiatry 2007 ; 64:327–337 Crossref , Medline , Google Scholar
60 Nestler EJ, Carlezon WA Jr : The mesolimbic dopamine reward circuit in depression . Biol Psychiatry 2006 ; 59:1151–1159 Crossref , Medline , Google Scholar
61 Suridjan I, Boileau I, Bagby M, et al. : Dopamine response to psychosocial stress in humans and its relationship to individual differences in personality traits . J Psychiatr Res 2012 ; 46:890–897 Crossref , Medline , Google Scholar
62 Cabib S, Puglisi-Allegra S : The mesoaccumbens dopamine in coping with stress . Neurosci Biobehav Rev 2012 ; 36:79–89 Crossref , Medline , Google Scholar
63 Krishnan V, Nestler EJ : Linking molecules to mood: new insight into the biology of depression . Am J Psychiatry 2010 ; 167:1305–1320 Crossref , Medline , Google Scholar
64 Bogdan R, Nikolova YS, Pizzagalli DA : Neurogenetics of depression: a focus on reward processing and stress sensitivity . Neurobiol Dis 2013 ; 52:12–23 Crossref , Medline , Google Scholar
65 Der-Avakian A, Markou A : The neurobiology of anhedonia and other reward-related deficits . Trends Neurosci 2012 ; 35:68–77 Crossref , Medline , Google Scholar
66 Pruessner JC, Champagne F, Meaney MJ, et al. : Dopamine release in response to a psychological stress in humans and its relationship to early life maternal care: a positron emission tomography study using [11C]raclopride . J Neurosci 2004 ; 24:2825–2831 Crossref , Medline , Google Scholar
67 Mongeau R, Blier P, de Montigny C : The serotonergic and noradrenergic systems of the hippocampus: their interactions and the effects of antidepressant treatments . Brain Res Brain Res Rev 1997 ; 23:145–195 Crossref , Medline , Google Scholar
68 Mitchelmore C, Gede L : Brain derived neurotrophic factor: epigenetic regulation in psychiatric disorders . Brain Res 2014 ; 1586:162–172 Crossref , Medline , Google Scholar
69 Duman RS, Monteggia LM : A neurotrophic model for stress-related mood disorders . Biol Psychiatry 2006 ; 59:1116–1127 Crossref , Medline , Google Scholar
70 Mössner R, Daniel S, Albert D, et al. : Serotonin transporter function is modulated by brain-derived neurotrophic factor (BDNF) but not nerve growth factor (NGF) . Neurochem Int 2000 ; 36:197–202 Crossref , Medline , Google Scholar
71 Ota KT, Duman RS : Environmental and pharmacological modulations of cellular plasticity: role in the pathophysiology and treatment of depression . Neurobiol Dis 2013 ; 57:28–37 Crossref , Medline , Google Scholar
72 Suri D, Vaidya VA : Glucocorticoid regulation of brain-derived neurotrophic factor: relevance to hippocampal structural and functional plasticity . Neuroscience 2013 ; 239:196–213 Crossref , Medline , Google Scholar
73 Duman RS : Role of neurotrophic factors in the etiology and treatment of mood disorders . Neuromolecular Med 2004 ; 5:11–25 Crossref , Medline , Google Scholar
74 Mahar I, Bambico FR, Mechawar N, et al. : Stress, serotonin, and hippocampal neurogenesis in relation to depression and antidepressant effects . Neurosci Biobehav Rev 2014 ; 38:173–192 Crossref , Medline , Google Scholar
75 Jacobs BL, van Praag H, Gage FH : Adult brain neurogenesis and psychiatry: a novel theory of depression . Mol Psychiatry 2000 ; 5:262–269 Crossref , Medline , Google Scholar
76 Malberg JE, Eisch AJ, Nestler EJ, et al. : Chronic antidepressant treatment increases neurogenesis in adult rat hippocampus . J Neurosci 2000 ; 20:9104–9110 Crossref , Medline , Google Scholar
77 Alenina N, Klempin F : The role of serotonin in adult hippocampal neurogenesis . Behav Brain Res 2015 ; 277:49–57 Crossref , Medline , Google Scholar
78 Krugers HJ, Lucassen PJ, Karst H, et al. : Chronic stress effects on hippocampal structure and synaptic function: relevance for depression and normalization by anti-glucocorticoid treatment . Front Synaptic Neurosci 2010 ; 2:24 Medline , Google Scholar
79 Hanson ND, Nemeroff CB, Owens MJ : Lithium, but not fluoxetine or the corticotropin-releasing factor receptor 1 receptor antagonist R121919, increases cell proliferation in the adult dentate gyrus . J Pharmacol Exp Ther 2011 ; 337:180–186 Crossref , Medline , Google Scholar
80 Haroon E, Raison CL, Miller AH : Psychoneuroimmunology meets neuropsychopharmacology: translational implications of the impact of inflammation on behavior . Neuropsychopharmacology 2012 ; 37:137–162 Crossref , Medline , Google Scholar
81 Capuron L, Miller AH : Immune system to brain signaling: neuropsychopharmacological implications . Pharmacol Ther 2011 ; 130:226–238 Crossref , Medline , Google Scholar
82 Cattaneo A, Macchi F, Plazzotta G, et al. : Inflammation and neuronal plasticity: a link between childhood trauma and depression pathogenesis . Front Cell Neurosci 2015 ; 9:40 Crossref , Medline , Google Scholar
83 Leonard BE : The concept of depression as a dysfunction of the immune system . Curr Immunol Rev 2010 ; 6:205–212 Crossref , Medline , Google Scholar
84 Loftis JM, Huckans M, Morasco BJ : Neuroimmune mechanisms of cytokine-induced depression: current theories and novel treatment strategies . Neurobiol Dis 2010 ; 37:519–533 Crossref , Medline , Google Scholar
85 Zhu CB, Blakely RD, Hewlett WA : The proinflammatory cytokines interleukin-1beta and tumor necrosis factor-alpha activate serotonin transporters . Neuropsychopharmacology 2006 ; 31:2121–2131 Crossref , Medline , Google Scholar
86 Folkman S, Lazarus RS : The relationship between coping and emotion: implications for theory and research . Soc Sci Med 1988 ; 26:309–317 Crossref , Medline , Google Scholar
87 Beck AT : The evolution of the cognitive model of depression and its neurobiological correlates . Am J Psychiatry 2008 ; 165:969–977 Crossref , Medline , Google Scholar
88 Heim C, Binder EB : Current research trends in early life stress and depression: review of human studies on sensitive periods, gene-environment interactions, and epigenetics . Exp Neurol 2012 ; 233:102–111 Crossref , Medline , Google Scholar
89 Gibb BE, Abramson LY, Alloy LB : Emotional maltreatment from parents, verbal peer victimization, and cognitive vulnerability to depression . Cogn Ther Res 2004 ; 28:1–21 Crossref , Google Scholar
90 Stankiewicz AM, Swiergiel AH, Lisowski P : Epigenetics of stress adaptations in the brain . Brain Res Bull 2013 ; 98:76–92 Crossref , Medline , Google Scholar
91 Peña CJ, Bagot RC, Labonté B, et al. : Epigenetic signaling in psychiatric disorders . J Mol Biol 2014 ; 426:3389–3412 Crossref , Medline , Google Scholar
92 Elliott E, Ezra-Nevo G, Regev L, et al. : Resilience to social stress coincides with functional DNA methylation of the Crf gene in adult mice . Nat Neurosci 2010 ; 13:1351–1353 Crossref , Medline , Google Scholar
93 Peng H, Long Y, Li J, et al. : Hypothalamic-pituitary-adrenal axis functioning and dysfunctional attitude in depressed patients with and without childhood neglect . BMC Psychiatry 2014 ; 14:45 Crossref , Medline , Google Scholar
94 Sapolsky RM, Krey LC, McEwen BS : Stress down-regulates corticosterone receptors in a site-specific manner in the brain . Endocrinology 1984 ; 114:287–292 Crossref , Medline , Google Scholar
95 Korosi A, Naninck EF, Oomen CA, et al. : Early-life stress mediated modulation of adult neurogenesis and behavior . Behav Brain Res 2012 ; 227:400–409 Crossref , Medline , Google Scholar
96 Meaney MJ, Szyf M : Environmental programming of stress responses through DNA methylation: life at the interface between a dynamic environment and a fixed genome . Dialogues Clin Neurosci 2005 ; 7:103–123 Medline , Google Scholar
97 Klengel T, Mehta D, Anacker C, et al. : Allele-specific FKBP5 DNA demethylation mediates gene-childhood trauma interactions . Nat Neurosci 2013 ; 16:33–41 Crossref , Medline , Google Scholar
98 Hammen C, Henry R, Daley SE : Depression and sensitization to stressors among young women as a function of childhood adversity . J Consult Clin Psychol 2000 ; 68:782–787 Crossref , Medline , Google Scholar
99 Gould F, Clarke J, Heim C, et al. : The effects of child abuse and neglect on cognitive functioning in adulthood . J Psychiatr Res 2012 ; 46:500–506 Crossref , Medline , Google Scholar
- How inflammation influences psychiatric disease 19 March 2024 | World Journal of Psychiatry, Vol. 14, No. 3
- The relationship between neuroticism and the acute psychological stress response: Evidence from the autonomic nervous system 18 March 2024 | Current Psychology, Vol. 92
- Fermented mixed grain ameliorates chronic stress-induced depression-like behavior and memory deficit 27 July 2023 | Food Science and Biotechnology, Vol. 33, No. 4
- Virtual Reality Breathing Interventions for Mental Health: A Systematic Review and Meta-Analysis of Randomized Controlled Trials 18 January 2024 | Applied Psychophysiology and Biofeedback, Vol. 49, No. 1
- Unraveling the associations between unhealthy lifestyle behaviors and mental health in the general adult Chinese population: A cross-sectional study Journal of Affective Disorders, Vol. 349
- Stress exposure, perceived stress severity, and their effects on health 1 April 2024 | Sociology: Theory, Methods, Marketing, Vol. 49, No. 1
- The Role of Lysophosphatidic Acid in Neuropsychiatric and Neurodegenerative Disorders 4 March 2024 | Future Pharmacology, Vol. 4, No. 1
- Value of serum brain-derived neurotrophic factor and glial fibrillary acidic protein for detecting depression in patients with Helicobacter pylori infection Neuroscience Letters, Vol. 825
- Evaluation of the anxiolytic activity of ethanolic extract of Ziziphus mauritiana Lam. in Swiss albino mice Pharmacological Research - Modern Chinese Medicine, Vol. 10
- A soy protein enzymatic digest mitigates Nrf2-related oxidative stress and attenuates depression-like behavior in a mouse model of sub-chronic restraint stress Heliyon, Vol. 10, No. 6
- Alleviating Stress in Parkinson’s Disease: Symptomatic Treatment, Disease Modification, or Both? Journal of Parkinson's Disease, Vol. 9
- Life Stressors and Mental Well-Being: Experiences of African American Women Navigating Perinatal Loss and Pregnancy Subsequent to Loss 6 February 2024 | Journal of Black Psychology, Vol. 2
- Behavioural characteristics and sex differences of a treatment-resistant depression model: Chronic mild stress in the Wistar-Kyoto rat Behavioural Brain Research, Vol. 457
- A mouse model of oral contraceptive exposure: Depression, motivation, and the stress response Hormones and Behavior, Vol. 158
- Effects of relaxation interventions during pregnancy on maternal mental health, and pregnancy and newborn outcomes: A systematic review and meta-analysis 25 January 2024 | PLOS ONE, Vol. 19, No. 1
- Histone 3 Trimethylation Patterns are Associated with Resilience or Stress Susceptibility in a Rat Model of Major Depression Disorder 16 January 2024 | Molecular Neurobiology, Vol. 13
- Diet Quality Mediates the Relationship Between Chronic Stress and Inflammation in Patients With Metabolic Syndrome 9 January 2024 | Journal of Cardiovascular Nursing, Vol. 14
- Socioecological Model of a Military Family’s Health and Well-Being: Inside a Slovenian Military Family 24 August 2022 | Armed Forces & Society, Vol. 50, No. 1
- Association between inflammatory bowel disease and subsequent depression or anxiety disorders - A retrospective cohort study of 31,728 outpatients Journal of Psychiatric Research, Vol. 169
- Clotrimazole ameliorates chronic mild stress-induced depressive-like behavior in rats; crosstalk between the HPA, NLRP3 inflammasome, and Wnt/β-catenin pathways International Immunopharmacology, Vol. 127
- Assessing the Effectiveness of STAPP@Work, a Self-Management Mobile App, in Reducing Work Stress and Preventing Burnout: Single-Case Experimental Design Study 29 February 2024 | Journal of Medical Internet Research, Vol. 26
- Depression in Final-Year Medical Students in Ho Chi Minh City, Vietnam: The Role of Career-Choice Motivation 18 March 2024 | Journal of Medical Education and Curricular Development, Vol. 11
- Interplay of G-proteins and Serotonin in the Neuroimmunoinflammatory Model of Chronic Stress and Depression: A Narrative Review Current Pharmaceutical Design, Vol. 30, No. 3
- A neuronal coping mechanism linking stress-induced anxiety to motivation for reward Science Advances, Vol. 9, No. 49
- Effect of breathwork on stress and mental health: A meta-analysis of randomised-controlled trials 9 January 2023 | Scientific Reports, Vol. 13, No. 1
- Chronic social defeat alters brain vascular-associated cell gene expression patterns leading to vascular dysfunction and immune system activation 28 June 2023 | Journal of Neuroinflammation, Vol. 20, No. 1
- Wistar-Kyoto rats and chronically stressed Wistar rats present similar depression- and anxiety-like behaviors but different corticosterone and endocannabinoid system modulation Progress in Neuro-Psychopharmacology and Biological Psychiatry, Vol. 127
- Investigating the potential effects of α-synuclein aggregation on susceptibility to chronic stress in a mouse Parkinson’s disease model 19 September 2023 | Pharmacological Reports, Vol. 75, No. 6
- A comparative analysis of depressive-like behavior: Exploring sex-related differences and insights 29 November 2023 | PLOS ONE, Vol. 18, No. 11
- Effect of consumption of blue maize tortilla on anxiety-like behaviour, learning, memory and hippocampal BDNF expression in a chronic stress model in rats 29 September 2022 | Nutritional Neuroscience, Vol. 26, No. 11
- Lactobacillus reuteri ATG-F4 Alleviates Chronic Stress-induced Anhedonia by Modulating the Prefrontal Serotonergic System Experimental Neurobiology, Vol. 32, No. 5
- The presentation of anxiety and depression among children and youth diagnosed with hidradenitis suppurativa: A review 10 October 2023 | Pediatric Dermatology, Vol. 63
- Psychological, behavioural and biological factors associated with gastrointestinal symptoms in autistic adults and adults with autistic traits 16 February 2023 | Autism, Vol. 27, No. 7
- Effects of Online Pilates and Face-to-Face Pilates Intervention on Body Composition, Muscle Mechanical Properties, Cardiometabolic Parameters, Mental Health, and Physical Fitness in Middle-Aged Women with Obesity 19 October 2023 | Healthcare, Vol. 11, No. 20
- Antidepressant effects of coumarins and their derivatives: A critical analysis of research advances European Journal of Pharmacology, Vol. 956
- Adverse Childhood Experiences, Intimate Partner Violence, and Mental Well-Being Among Mothers of Toddlers in Tirana, Albania: A Cross-Sectional Mediation Analysis 29 September 2023 | Violence Against Women, Vol. 9
- Emphasizing the Crosstalk Between Inflammatory and Neural Signaling in Post-traumatic Stress Disorder (PTSD) 25 April 2023 | Journal of Neuroimmune Pharmacology, Vol. 18, No. 3
- Stress-mediated dysregulation of the Rap1 small GTPase impairs hippocampal structure and function iScience, Vol. 26, No. 9
- Exploring Novel Therapeutic Approaches for Depressive Disorders: The Role of Allopregnanolone Agonists Cureus, Vol. 291
- Nervous-System-Wise Functional Estimation of Directed Brain–Heart Interplay Through Microstate Occurrences IEEE Transactions on Biomedical Engineering, Vol. 70, No. 8
- Stress in the social context: a behavioural and eco-evolutionary perspective 2 August 2023 | Journal of Experimental Biology, Vol. 226, No. 15
- Pathways to Psychopathology Among Autistic Adults 28 June 2023 | Current Psychiatry Reports, Vol. 25, No. 8
- Stress-Activated Protein Kinase JNK Modulates Depression-like Behaviors in Mice 18 January 2023 | Molecular Neurobiology, Vol. 60, No. 5
- Chronic oral ketamine prevents anhedonia and alters neuronal activation in the lateral habenula and nucleus accumbens in rats under chronic unpredictable mild stress Neuropharmacology, Vol. 228
- Dietary tryptophan-rich protein hydrolysate can acutely impact physiological and psychological measures of mood and stress in healthy adults 28 March 2022 | Nutritional Neuroscience, Vol. 26, No. 4
- Mental health as part of the integrative palliative care in all levels of care in urooncology 23 April 2022 | Aging & Mental Health, Vol. 27, No. 4
- Antidepressant and Neuroprotective Effects of 3-Hydroxy Paroxetine, an Analog of Paroxetine in Rats 26 November 2022 | International Journal of Neuropsychopharmacology, Vol. 26, No. 3
- Cortisol Biosensors: From Sensing Principles to Applications 15 March 2023 | World Scientific Annual Review of Functional Materials
- Elevated Hippocampal CRMP5 Mediates Chronic Stress-Induced Cognitive Deficits by Disrupting Synaptic Plasticity, Hindering AMPAR Trafficking, and Triggering Cytokine Release 3 March 2023 | International Journal of Molecular Sciences, Vol. 24, No. 5
- Can a single session of noninvasive brain stimulation applied over the prefrontal cortex prevent stress-induced cortisol release? Progress in Neuro-Psychopharmacology and Biological Psychiatry, Vol. 121
- Psychoneuro-oncology: How chronic stress grows cancer Clinics in Dermatology, Vol. 54
- Peripheral brain-derived neurotrophic factor (BDNF) and salivary cortisol levels in college students with different levels of academic stress. Study protocol 22 February 2023 | PLOS ONE, Vol. 18, No. 2
- The Role of Genetics in the Development and Pharmacotherapy of Depression and Its Impact on Drug Discovery 2 February 2023 | International Journal of Molecular Sciences, Vol. 24, No. 3
- Role of group II metabotropic glutamate receptors in ketamine's antidepressant actions Pharmacology Biochemistry and Behavior, Vol. 223
- Relating parental stress with sleep disorders in parents and children 25 January 2023 | PLOS ONE, Vol. 18, No. 1
- Anxiety, depression, and academic stress among medical students during the COVID-19 pandemic 11 January 2023 | Frontiers in Psychology, Vol. 13
- Associations Between Demographic, Clinical, and Symptom Characteristics and Stress in Oncology Patients Receiving Chemotherapy 4 March 2022 | Cancer Nursing, Vol. 46, No. 1
- Prevalence of Common Alleles of Some Stress Resilience Genes among Adolescents Born in Different Periods Relative to the Socioeconomic Crisis of the 1990s in Russia 21 December 2022 | Current Issues in Molecular Biology, Vol. 45, No. 1
- Introducing a depression-like syndrome for translational neuropsychiatry: a plea for taxonomical validity and improved comparability between humans and mice 14 September 2022 | Molecular Psychiatry, Vol. 28, No. 1
- Targeting the Arginine Vasopressin V1b Receptor System and Stress Response in Depression and Other Neuropsychiatric Disorders 1 April 2023 | Neuropsychiatric Disease and Treatment, Vol. Volume 19
- Efficacy and Anti-Inflammatory Activity of Ashwagandha Sustained-Release Formulation on Depression and Anxiety Induced by Chronic Unpredictable Stress: in vivo and in vitro Studies 1 July 2023 | Journal of Experimental Pharmacology, Vol. Volume 15
- Gender Differences in Older Adults’ Muscle Strength and Depressive Symptoms: A Relationship Mediated Through Perceived Stress 27 September 2023 | Research in Community and Public Health Nursing, Vol. 34
- Increased academic stress is associated with decreased plasma BDNF in Chilean college students 3 November 2023 | PeerJ, Vol. 11
- Interaction effect between childhood abuse and interleukin-1β levels on suicidality in depressed patients 25 April 2022 | European Archives of Psychiatry and Clinical Neuroscience, Vol. 272, No. 8
- Prevalence, associated factors and perinatal outcomes of antepartum depression in Ibadan Nigeria 18 March 2022 | BMC Pregnancy and Childbirth, Vol. 22, No. 1
- Stress, mental disorder and ketamine as a novel, rapid acting treatment European Neuropsychopharmacology, Vol. 65
- Neighbourhood crime and major depression in Sweden: A national cohort study Health & Place, Vol. 78
- Preschool Depression and Hippocampal Volume: The Moderating Role of Family Income Journal of the American Academy of Child & Adolescent Psychiatry, Vol. 61, No. 11
- HPA Axis Responsiveness Associates with Central Serotonin Transporter Availability in Human Obesity and Non-Obesity Controls 25 October 2022 | Brain Sciences, Vol. 12, No. 11
- Restraint Stress and Repeated Corticosterone Administration Differentially Affect Neuronal Excitability, Synaptic Transmission and 5-HT7 Receptor Reactivity in the Dorsal Raphe Nucleus of Young Adult Male Rats 18 November 2022 | International Journal of Molecular Sciences, Vol. 23, No. 22
- Sleep disorders mediate the link between childhood trauma and depression severity in children and adolescents with depression 28 October 2022 | Frontiers in Psychiatry, Vol. 13
- The cumulative effect of chronic stress and depressive symptoms affects heart rate in a working population 13 October 2022 | Frontiers in Psychiatry, Vol. 13
- Depression among people with dyspepsia and H. pylori infection: A community based cross-sectional study in Ethiopia 6 October 2022 | PLOS ONE, Vol. 17, No. 10
- Cross-Sectional Analysis of Mental Health among University Students: Do Sex and Academic Level Matter? 3 October 2022 | International Journal of Environmental Research and Public Health, Vol. 19, No. 19
- Hormonal contraceptives, stress, and the brain: The critical need for animal models Frontiers in Neuroendocrinology, Vol. 67
- Olfactory loss is a predisposing factor for depression, while olfactory enrichment is an effective treatment for depression 28 September 2022 | Frontiers in Neuroscience, Vol. 16
- Understanding the basis of major depressive disorder in oncological patients: Biological links, clinical management, challenges, and lifestyle medicine 16 September 2022 | Frontiers in Oncology, Vol. 12
- The Lived Experiences of Depression in Huntington’s Disease: A Qualitative Study Journal of Huntington's Disease, Vol. 11, No. 3
- Exaggerated amygdala response to threat and association with immune hyperactivity in depression Brain, Behavior, and Immunity, Vol. 104
- Causal Symbolic Information Transfer for the Assessment of functional Brain-Heart Interplay through EEG Microstates Occurrences: a proof-of-concept study
- Mental Health Conditions According to Stress and Sleep Disorders 29 June 2022 | International Journal of Environmental Research and Public Health, Vol. 19, No. 13
- Different Areas of Chronic Stress and Their Associations with Depression 19 July 2022 | International Journal of Environmental Research and Public Health, Vol. 19, No. 14
- Vestibular Disability/Handicap in Fibromyalgia: A Questionnaire Study 11 July 2022 | Journal of Clinical Medicine, Vol. 11, No. 14
- Perceived stress and E-cigarette use during emerging adulthood: A longitudinal examination of initiation, progression, and continuation Preventive Medicine, Vol. 160
- Efficacy of Withania somnifera supplementation on adult’s cognition and mood Journal of Ayurveda and Integrative Medicine, Vol. 13, No. 2
- CCR2 monocytes repair cerebrovascular damage caused by chronic social defeat stress Brain, Behavior, and Immunity, Vol. 101
- The interplay between self-esteem, expectancy, cognitive control, rumination, and the experience of stress: A network analysis 14 February 2022 | Current Psychology, Vol. 79
- The Cortisol Assessment List (CoAL) A tool to systematically document and evaluate cortisol assessment in blood, urine and saliva Comprehensive Psychoneuroendocrinology, Vol. 9
- Introduction to the Study of Stress 17 May 2022
- Neurobiological Approach to Stress 17 May 2022
- Clinical Approach to Stress 17 May 2022
- Medical Comorbidities of Hispanics with Mental Health Problems 2 December 2022
- Specific and cumulative lifetime stressors in the aetiology of major depression: A longitudinal community-based population study 26 January 2022 | Epidemiology and Psychiatric Sciences, Vol. 31
- Associations of state-level and county-level hate crimes with individual-level cardiovascular risk factors in a prospective cohort study of middle-aged Americans: the National Longitudinal Survey of Youths 1979 19 January 2022 | BMJ Open, Vol. 12, No. 1
- The role of pre-pandemic depression for changes in depression, anxiety, and loneliness during the COVID-19 pandemic: Results from a longitudinal probability sample of adults from Germany 3 November 2022 | European Psychiatry, Vol. 65, No. 1
- Interleukin-6 expression and its modulation by diacerein in a rat model of chronic stress induced cardiac dysfunction Heliyon, Vol. 7, No. 12
- Psychometric properties and correlates of Chinese version of Perceived Stress Scale (CPSS-10) in people with common mental disorders with different employment Statuses 4 August 2021 | Hong Kong Journal of Occupational Therapy, Vol. 34, No. 2
- Association between the expression of lncRNA BASP-AS1 and volume of right hippocampal tail moderated by episode duration in major depressive disorder: a CAN-BIND 1 report 8 September 2021 | Translational Psychiatry, Vol. 11, No. 1
- Psychoneuroimmunology in the context of perinatal depression - Tools for improved clinical practice Brain, Behavior, & Immunity - Health, Vol. 17
- MicroRNAs as Critical Biomarkers of Major Depressive Disorder: A Comprehensive Perspective 10 November 2021 | Biomedicines, Vol. 9, No. 11
- Treadmill exercise sex-dependently alters susceptibility to depression-like behaviour, cytokines and BDNF in the hippocampus and prefrontal cortex of rats with sporadic Alzheimer-like disease Physiology & Behavior, Vol. 241
- Childhood trauma and depression in college students: Mediating and moderating effects of psychological resilience Asian Journal of Psychiatry, Vol. 65
- Back to nature: herbal treatment, environmental enrichment, and social play can protect against unpredictable chronic stress in Long-Evans rats (Rattus norvegicus) 1 August 2021 | Psychopharmacology, Vol. 238, No. 10
- Maternal chewing improves prenatal stress-induced cognitive deficit and anxiety-like behavior associated with alterations of the apoptotic response and serotonin pathway in mouse offspring Archives of Oral Biology, Vol. 130
- HPA Axis in the Pathomechanism of Depression and Schizophrenia: New Therapeutic Strategies Based on Its Participation 30 September 2021 | Brain Sciences, Vol. 11, No. 10
- Roles of fibroblast growth factor 21 in the control of depression‐like behaviours after social defeat stress in male rodents 1 September 2021 | Journal of Neuroendocrinology, Vol. 33, No. 10
- Weak and uneven associations of home, neighborhood, and school environments with stress hormone output across multiple timescales 4 May 2020 | Molecular Psychiatry, Vol. 26, No. 9
- Impact of depression and stress on placental DNA methylation in ethnically diverse pregnant women Epigenomics, Vol. 13, No. 18
- Stress and Western diets increase vulnerability to neuropsychiatric disorders: A common mechanism 16 September 2019 | Nutritional Neuroscience, Vol. 24, No. 8
- Associations of job strain and family strain with risk of major depressive episode: A prospective cohort study in U.S. working men and women Journal of Psychosomatic Research, Vol. 147
- Prolonged Maternal Separation Induces the Depression-Like Behavior Susceptibility to Chronic Unpredictable Mild Stress Exposure in Mice BioMed Research International, Vol. 2021
- Endometriosis and related pelvic pain: association with stress, anxiety and depressive symptoms Minerva Obstetrics and Gynecology, Vol. 73, No. 3
- Title: “Labels Matter: Is it stress or is it Trauma?” 10 July 2021 | Translational Psychiatry, Vol. 11, No. 1
- Depression, anxiety, and the COVID-19 pandemic: Severity of symptoms and associated factors among university students after the end of the movement lockdown 27 May 2021 | PLOS ONE, Vol. 16, No. 5
- Traditional Chinese Medicine Body Constitutions and Psychological Determinants of Depression among University Students in Malaysia: A Pilot Study 18 May 2021 | International Journal of Environmental Research and Public Health, Vol. 18, No. 10
- A pioneering FreeSurfer volumetric study of a series of patients with mesial temporal lobe epilepsy and hippocampal sclerosis with comorbid depression Psychiatry Research: Neuroimaging, Vol. 311
- Increased Stress Resistance and Lifespan in Chaenorhabditis elegans Wildtype and Knockout Mutants—Implications for Depression Treatment by Medicinal Herbs 24 March 2021 | Molecules, Vol. 26, No. 7
- Activation of PPG neurons following acute stressors differentially involves hindbrain serotonin in male rats Neuropharmacology, Vol. 187
- Comorbid anxiety-like behavior in a rat model of colitis is mediated by an upregulation of corticolimbic fatty acid amide hydrolase 15 January 2021 | Neuropsychopharmacology, Vol. 46, No. 5
- Prenatal Alcohol Exposure and Hypothalamic-Pituitary-Adrenal Axis Activity of the Offspring in Humans: a Systematic Review 5 January 2021 | Current Addiction Reports, Vol. 8, No. 1
- Depression and anxiety in the Malaysian urban population and their association with demographic characteristics, quality of life, and the emergence of the COVID-19 pandemic 19 February 2021 | Current Psychology, Vol. 16
- Hypothalamic Inflammation as a Potential Pathophysiologic Basis for the Heterogeneity of Clinical, Hormonal, and Metabolic Presentation in PCOS 5 February 2021 | Nutrients, Vol. 13, No. 2
- Potential Interactions Between Environmental and Psychoneurobiological Factors in the Interface Between Stress and Depression: A Road Map to Resilience 24 January 2021
- The 2020 Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders 22 December 2020 | Australian & New Zealand Journal of Psychiatry, Vol. 55, No. 1
- Effects of an African Circle Dance Programme on Internally Displaced Persons with Depressive Symptoms: A Quasi-Experimental Study 19 January 2021 | International Journal of Environmental Research and Public Health, Vol. 18, No. 2
- Yoga and Lifestyle Factors in Heart Disease
- Association between depression, anxiety, stress and perceived quality of life in a Malaysian B40 urban community during the COVID-19 lockdown: A cross-sectional study 29 July 2021 | F1000Research, Vol. 10
- Fluoxetine increases hippocampal neural survival by improving axonal transport in stress-induced model of depression male rats Physiology & Behavior, Vol. 227
- A Systematic Review of the Association Between Psychological Stress and Dementia Risk in Humans Journal of Alzheimer's Disease, Vol. 78, No. 1
- A Gut Feeling: The Importance of the Intestinal Microbiota in Psychiatric Disorders 19 October 2020 | Frontiers in Immunology, Vol. 11
- Efficacy of probiotics on stress in healthy volunteers: A systematic review and meta‐analysis based on randomized controlled trials 14 July 2020 | Brain and Behavior, Vol. 10, No. 9
- The influence of the duration of chronic unpredictable mild stress on the behavioural responses of C57BL/6J mice 18 May 2020 | Behavioural Pharmacology, Vol. 31, No. 6
- Corticosterone Induced the Increase of proBDNF in Primary Hippocampal Neurons Via Endoplasmic Reticulum Stress 6 May 2020 | Neurotoxicity Research, Vol. 38, No. 2
- Monoaminergic balances predict non-depression-like phenotype in Learned Helplessness Paradigm Neuroscience, Vol. 440
- Abnormal functional connectivity as neural biological substrate of trait and state characteristics in major depressive disorder Progress in Neuro-Psychopharmacology and Biological Psychiatry, Vol. 102
- Chronic stress and endothelial dysfunction: mechanisms, experimental challenges, and the way ahead American Journal of Physiology-Heart and Circulatory Physiology, Vol. 319, No. 2
- Heart Rate Variability as an Index of Differential Brain Dynamics at Rest and After Acute Stress Induction 2 July 2020 | Frontiers in Neuroscience, Vol. 14
- Early life stress and glutamate neurotransmission in major depressive disorder European Neuropsychopharmacology, Vol. 35
- Prevalence of and factors associated with depression among hill tribe individuals aged 30 years and over in Thailand Heliyon, Vol. 6, No. 6
- State-of-the-Art: Inflammatory and Metabolic Markers in Mood Disorders 6 June 2020 | Life, Vol. 10, No. 6
- Pharmacological Treatment of Anxiety Disorders: The Role of the HPA Axis 15 May 2020 | Frontiers in Psychiatry, Vol. 11
- Neuroinflammation and depressive disorder: The role of the hypothalamus Journal of Clinical Neuroscience, Vol. 75
- From Work Well-Being to Burnout: A Hypothetical Phase Model 30 April 2020 | Frontiers in Neuroscience, Vol. 14
- Finding intestinal fortitude: Integrating the microbiome into a holistic view of depression mechanisms, treatment, and resilience Neurobiology of Disease, Vol. 135
- Role of glucocorticoid- and monoamine-metabolizing enzymes in stress-related psychopathological processes 19 July 2019 | Stress, Vol. 23, No. 1
- Is Stress a Cause or a Consequence of Endometriosis? 6 January 2020 | Reproductive Sciences, Vol. 27, No. 1
- Hypothalamic–pituitary–adrenal axis and stress
- Immune response to stress induction as a predictor of cognitive-behavioral therapy outcomes in adolescent mood disorders: A pilot study Journal of Psychiatric Research, Vol. 120
- Enduring and Sex-specific Changes in Hippocampal Gene Expression after a Subchronic Immune Challenge Neuroscience, Vol. 428
- Childhood maltreatment and risk for suicide attempts in major depression: a sex-specific approach 7 May 2019 | European Journal of Psychotraumatology, Vol. 10, No. 1
- How Do Couples Cope With Unemployment: Examining Relationships Among Support, Undermining, and Depression 10 March 2019 | The Family Journal, Vol. 27, No. 3
- REM sleep’s unique associations with corticosterone regulation, apoptotic pathways, and behavior in chronic stress in mice 25 January 2019 | Proceedings of the National Academy of Sciences, Vol. 116, No. 7
- Subclinical Lipopolysaccharide from Salmonella Enteritidis Induces Dysregulation of Bioactive Substances from Selected Brain Sections and Glands of Neuroendocrine Axes 2 February 2019 | Toxins, Vol. 11, No. 2
- Advance in Stress for Depressive Disorder 30 November 2019
- Antidepressant and anxiolytic effects of the proprietary Chinese medicine Shexiang Baoxin pill in mice with chronic unpredictable mild stress Journal of Food and Drug Analysis, Vol. 27, No. 1
- Frontiers in Neuroscience, Vol. 13
- A gene–gene interaction between the vascular endothelial growth factor a and brain-derived neurotrophic factor genes is associated with psychological distress in the Taiwanese population Taiwanese Journal of Psychiatry, Vol. 33, No. 3
- An investigation into the stress-relieving and pharmacological actions of an ashwagandha (Withania somnifera) extract 1 September 2019 | Medicine, Vol. 98, No. 37
- Cortisol and alpha-amylase assessment in psychotherapeutic intervention studies: A systematic review Neuroscience & Biobehavioral Reviews, Vol. 95
- Neighborhood disorder, exposure to violence, and perceived discrimination in relation to symptoms in midlife women 19 October 2018 | Women's Midlife Health, Vol. 4, No. 1
- Potassium 2-(1-hydroxypentyl)-benzoate improves depressive-like behaviors in rat model Acta Pharmaceutica Sinica B, Vol. 8, No. 6
- Emotional stress regulation: The role of relative frontal alpha asymmetry in shaping the stress response Biological Psychology, Vol. 138
- Late chronotype is associated with enhanced amygdala reactivity and reduced fronto-limbic functional connectivity to fearful versus happy facial expressions NeuroImage, Vol. 171
- Behavioral and structural adaptations to stress Frontiers in Neuroendocrinology, Vol. 49
- The Neurochemistry of Stress: the Chemistry of the Stress Response and Stress Vulnerability 30 June 2018 | Neurochemical Journal, Vol. 12, No. 2
- Hair cortisol and the relationship with chronic pain and quality of life in endometriosis patients Psychoneuroendocrinology, Vol. 89
- miRNAs As Critical Epigenetic Players in Determining Neurobiological Correlates of Major Depressive Disorder 25 October 2017
- Hepatology International, Vol. 12, No. 4
- Neuropsychopharmacology, Vol. 43, No. 5
- Bibliographie
- Medical Yoga Therapy 10 February 2017 | Children, Vol. 4, No. 2
- Psihijatrija danas, Vol. 49, No. 1
- Hippocampal volume and integrity as predictors of cognitive decline in intact elderly NeuroReport, Vol. 27, No. 11
- Psychosocial stress based on public speech in humans: is there a real life/laboratory setting cross-adaptation? 4 July 2016 | Stress, Vol. 19, No. 4
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- March 01, 2024 | VOL. 181, NO. 3 CURRENT ISSUE pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
The Critical Relationship Between Anxiety and Depression
- Ned H. Kalin , M.D.
Search for more papers by this author
Anxiety and depressive disorders are among the most common psychiatric illnesses; they are highly comorbid with each other, and together they are considered to belong to the broader category of internalizing disorders. Based on statistics from the Substance Abuse and Mental Health Services Administration, the 12-month prevalence of major depressive disorder in 2017 was estimated to be 7.1% for adults and 13.3% for adolescents ( 1 ). Data for anxiety disorders are less current, but in 2001–2003, their 12-month prevalence was estimated to be 19.1% in adults, and 2001–2004 data estimated that the lifetime prevalence in adolescents was 31.9% ( 2 , 3 ). Both anxiety and depressive disorders are more prevalent in women, with an approximate 2:1 ratio in women compared with men during women’s reproductive years ( 1 , 2 ).
Across all psychiatric disorders, comorbidity is the rule ( 4 ), which is definitely the case for anxiety and depressive disorders, as well as their symptoms. With respect to major depression, a worldwide survey reported that 45.7% of individuals with lifetime major depressive disorder had a lifetime history of one or more anxiety disorder ( 5 ). These disorders also commonly coexist during the same time frame, as 41.6% of individuals with 12-month major depression also had one or more anxiety disorder over the same 12-month period. From the perspective of anxiety disorders, the lifetime comorbidity with depression is estimated to range from 20% to 70% for patients with social anxiety disorder ( 6 ), 50% for patients with panic disorder ( 6 ), 48% for patients with posttraumatic stress disorder (PTSD) ( 7 ), and 43% for patients with generalized anxiety disorder ( 8 ). Data from the well-known Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study demonstrate comorbidity at the symptom level, as 53% of the patients with major depression had significant anxiety and were considered to have an anxious depression ( 9 ).
Anxiety and depressive disorders are moderately heritable (approximately 40%), and evidence suggests shared genetic risk across the internalizing disorders ( 10 ). Among internalizing disorders, the highest level of shared genetic risk appears to be between major depressive disorder and generalized anxiety disorder. Neuroticism is a personality trait or temperamental characteristic that is associated with the development of both anxiety and depression, and the genetic risk for developing neuroticism also appears to be shared with that of the internalizing disorders ( 11 ). Common nongenetic risk factors associated with the development of anxiety and depression include earlier life adversity, such as trauma or neglect, as well as parenting style and current stress exposure. At the level of neural circuits, alterations in prefrontal-limbic pathways that mediate emotion regulatory processes are common to anxiety and depressive disorders ( 12 , 13 ). These findings are consistent with meta-analyses that reveal shared structural and functional brain alterations across various psychiatric illnesses, including anxiety and major depression, in circuits involving emotion regulation ( 13 ), executive function ( 14 ), and cognitive control ( 15 ).
Anxiety disorders and major depression occur during development, with anxiety disorders commonly beginning during preadolescence and early adolescence and major depression tending to emerge during adolescence and early to mid-adulthood ( 16 – 18 ). In relation to the evolution of their comorbidity, studies demonstrate that anxiety disorders generally precede the presentation of major depressive disorder ( 17 ). A European community-based study revealed, beginning at age 15, the developmental relation between comorbid anxiety and major depression by specifically focusing on social phobia (based on DSM-IV criteria) and then asking the question regarding concurrent major depressive disorder ( 18 ). The findings revealed a 19% concurrent comorbidity between these disorders, and in 65% of the cases, social phobia preceded major depressive disorder by at least 2 years. In addition, initial presentation with social phobia was associated with a 5.7-fold increased risk of developing major depressive disorder. These associations between anxiety and depression can be traced back even earlier in life. For example, childhood behavioral inhibition in response to novelty or strangers, or an extreme anxious temperament, is associated with a three- to fourfold increase in the likelihood of developing social anxiety disorder, which in turn is associated with an increased risk to develop major depressive disorder and substance abuse ( 19 ).
It is important to emphasize that the presence of comor‐bid anxiety symptoms and disorders matters in relation to treatment. Across psychiatric disorders, the presence of significant anxiety symptoms generally predicts worse outcomes, and this has been well demonstrated for depression. In the STAR*D study, patients with anxious major depressive disorder were more likely to be severely depressed and to have more suicidal ideation ( 9 ). This is consistent with the study by Kessler and colleagues ( 5 ), in which patients with anxious major depressive disorder, compared with patients with nonanxious major depressive disorder, were found to have more severe role impairment and more suicidal ideation. Data from level 1 of the STAR*D study (citalopram treatment) nicely illustrate the impact of comorbid anxiety symptoms on treatment. Compared with patients with nonanxious major depressive disorder, those 53% of patients with an anxious depression were less likely to remit and also had a greater side effect burden ( 20 ). Other data examining patients with major depressive disorder and comorbid anxiety disorders support the greater difficulty and challenge in treating patients with these comorbidities ( 21 ).
This issue of the Journal presents new findings relevant to the issues discussed above in relation to understanding and treating anxiety and depressive disorders. Drs. Conor Liston and Timothy Spellman, from Weill Cornell Medicine, provide an overview for this issue ( 22 ) that is focused on understanding mechanisms at the neural circuit level that underlie the pathophysiology of depression. Their piece nicely integrates human neuroimaging studies with complementary data from animal models that allow for the manipulation of selective circuits to test hypotheses generated from the human data. Also included in this issue is a review of the data addressing the reemergence of the use of psychedelic drugs in psychiatry, particularly for the treatment of depression, anxiety, and PTSD ( 23 ). This timely piece, authored by Dr. Collin Reiff along with a subgroup from the APA Council of Research, provides the current state of evidence supporting the further exploration of these interventions. Dr. Alan Schatzberg, from Stanford University, contributes an editorial in which he comments on where the field is in relation to clinical trials with psychedelics and to some of the difficulties, such as adequate blinding, in reliably studying the efficacy of these drugs ( 24 ).
In an article by McTeague et al. ( 25 ), the authors use meta-analytic strategies to understand the neural alterations that are related to aberrant emotion processing that are shared across psychiatric disorders. Findings support alterations in the salience, reward, and lateral orbital nonreward networks as common across disorders, including anxiety and depressive disorders. These findings add to the growing body of work that supports the concept that there are common underlying factors across all types of psychopathology that include internalizing, externalizing, and thought disorder dimensions ( 26 ). Dr. Deanna Barch, from Washington University in St. Louis, writes an editorial commenting on these findings and, importantly, discusses criteria that should be met when we consider whether the findings are actually transdiagnostic ( 27 ).
Another article, from Gray and colleagues ( 28 ), addresses whether there is a convergence of findings, specifically in major depression, when examining data from different structural and functional neuroimaging modalities. The authors report that, consistent with what we know about regions involved in emotion processing, the subgenual anterior cingulate cortex, hippocampus, and amygdala were among the regions that showed convergence across multimodal imaging modalities.
In relation to treatment and building on our understanding of neural circuit alterations, Siddiqi et al. ( 29 ) present data suggesting that transcranial magnetic stimulation (TMS) targeting can be linked to symptom-specific treatments. Their findings identify different TMS targets in the left dorsolateral prefrontal cortex that modulate different downstream networks. The modulation of these different networks appears to be associated with a reduction in different types of symptoms. In an editorial, Drs. Sean Nestor and Daniel Blumberger, from the University of Toronto ( 30 ), comment on the novel approach used in this study to link the TMS-related engagement of circuits with symptom improvement. They also provide a perspective on how we can view these and other circuit-based findings in relation to conceptualizing personalized treatment approaches.
Kendler et al. ( 31 ), in this issue, contribute an article that demonstrates the important role of the rearing environment in the risk to develop major depression. Using a unique design from a Swedish sample, the analytic strategy involves comparing outcomes from high-risk full sibships and high-risk half sibships where at least one of the siblings was home reared and one was adopted out of the home. The findings support the importance of the quality of the rearing environment as well as the presence of parental depression in mitigating or enhancing the likelihood of developing major depression. In an accompanying editorial ( 32 ), Dr. Myrna Weissman, from Columbia University, reviews the methods and findings of the Kendler et al. article and also emphasizes the critical significance of the early nurturing environment in relation to general health.
This issue concludes with an intriguing article on anxiety disorders, by Gold and colleagues ( 33 ), that demonstrates neural alterations during extinction recall that differ in children relative to adults. With increasing age, and in relation to fear and safety cues, nonanxious adults demonstrated greater connectivity between the amygdala and the ventromedial prefrontal cortex compared with anxious adults, as the cues were being perceived as safer. In contrast, neural differences between anxious and nonanxious youths were more robust when rating the memory of faces that were associated with threat. Specifically, these differences were observed in the activation of the inferior temporal cortex. In their editorial ( 34 ), Dr. Dylan Gee and Sahana Kribakaran, from Yale University, emphasize the importance of developmental work in relation to understanding anxiety disorders, place these findings into the context of other work, and suggest the possibility that these and other data point to neuroscientifically informed age-specific interventions.
Taken together, the papers in this issue of the Journal present new findings that shed light onto alterations in neural function that underlie major depressive disorder and anxiety disorders. It is important to remember that these disorders are highly comorbid and that their symptoms are frequently not separable. The papers in this issue also provide a developmental perspective emphasizing the importance of early rearing in the risk to develop depression and age-related findings important for understanding threat processing in patients with anxiety disorders. From a treatment perspective, the papers introduce data supporting more selective prefrontal cortical TMS targeting in relation to different symptoms, address the potential and drawbacks for considering the future use of psychedelics in our treatments, and present new ideas supporting age-specific interventions for youths and adults with anxiety disorders.
Disclosures of Editors’ financial relationships appear in the April 2020 issue of the Journal .
1 Substance Abuse and Mental Health Services Administration (SAMHSA): Key substance use and mental health indicators in the United States: results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18-5068, NSDUH Series H-53). Rockville, Md, Center for Behavioral Health Statistics and Quality, SAMHSA, 2018. https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHFFR2017/NSDUHFFR2017.htm Google Scholar
2 Kessler RC, Chiu WT, Demler O, et al. : Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication . Arch Gen Psychiatry 2005 ; 62:617–627, correction, 62:709 Crossref , Medline , Google Scholar
3 Merikangas KR, He JP, Burstein M, et al. : Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A) . J Am Acad Child Adolesc Psychiatry 2010 ; 49:980–989 Crossref , Medline , Google Scholar
4 Kessler RC, McGonagle KA, Zhao S, et al. : Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey . Arch Gen Psychiatry 1994 ; 51:8–19 Crossref , Medline , Google Scholar
5 Kessler RC, Sampson NA, Berglund P, et al. : Anxious and non-anxious major depressive disorder in the World Health Organization World Mental Health Surveys . Epidemiol Psychiatr Sci 2015 ; 24:210–226 Crossref , Medline , Google Scholar
6 Dunner DL : Management of anxiety disorders: the added challenge of comorbidity . Depress Anxiety 2001 ; 13:57–71 Crossref , Medline , Google Scholar
7 Kessler RC, Sonnega A, Bromet E, et al. : Posttraumatic stress disorder in the National Comorbidity Survey . Arch Gen Psychiatry 1995 ; 52:1048–1060 Crossref , Medline , Google Scholar
8 Brawman-Mintzer O, Lydiard RB, Emmanuel N, et al. : Psychiatric comorbidity in patients with generalized anxiety disorder . Am J Psychiatry 1993 ; 150:1216–1218 Link , Google Scholar
9 Fava M, Alpert JE, Carmin CN, et al. : Clinical correlates and symptom patterns of anxious depression among patients with major depressive disorder in STAR*D . Psychol Med 2004 ; 34:1299–1308 Crossref , Medline , Google Scholar
10 Hettema JM : What is the genetic relationship between anxiety and depression? Am J Med Genet C Semin Med Genet 2008 ; 148C:140–146 Crossref , Medline , Google Scholar
11 Hettema JM, Neale MC, Myers JM, et al. : A population-based twin study of the relationship between neuroticism and internalizing disorders . Am J Psychiatry 2006 ; 163:857–864 Link , Google Scholar
12 Kovner R, Oler JA, Kalin NH : Cortico-limbic interactions mediate adaptive and maladaptive responses relevant to psychopathology . Am J Psychiatry 2019 ; 176:987–999 Link , Google Scholar
13 Etkin A, Schatzberg AF : Common abnormalities and disorder-specific compensation during implicit regulation of emotional processing in generalized anxiety and major depressive disorders . Am J Psychiatry 2011 ; 168:968–978 Link , Google Scholar
14 Goodkind M, Eickhoff SB, Oathes DJ, et al. : Identification of a common neurobiological substrate for mental illness . JAMA Psychiatry 2015 ; 72:305–315 Crossref , Medline , Google Scholar
15 McTeague LM, Huemer J, Carreon DM, et al. : Identification of common neural circuit disruptions in cognitive control across psychiatric disorders . Am J Psychiatry 2017 ; 174:676–685 Link , Google Scholar
16 Beesdo K, Knappe S, Pine DS : Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V . Psychiatr Clin North Am 2009 ; 32:483–524 Crossref , Medline , Google Scholar
17 Kessler RC, Wang PS : The descriptive epidemiology of commonly occurring mental disorders in the United States . Annu Rev Public Health 2008 ; 29:115–129 Crossref , Medline , Google Scholar
18 Ohayon MM, Schatzberg AF : Social phobia and depression: prevalence and comorbidity . J Psychosom Res 2010 ; 68:235–243 Crossref , Medline , Google Scholar
19 Clauss JA, Blackford JU : Behavioral inhibition and risk for developing social anxiety disorder: a meta-analytic study . J Am Acad Child Adolesc Psychiatry 2012 ; 51:1066–1075 Crossref , Medline , Google Scholar
20 Fava M, Rush AJ, Alpert JE, et al. : Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report . Am J Psychiatry 2008 ; 165:342–351 Link , Google Scholar
21 Dold M, Bartova L, Souery D, et al. : Clinical characteristics and treatment outcomes of patients with major depressive disorder and comorbid anxiety disorders: results from a European multicenter study . J Psychiatr Res 2017 ; 91:1–13 Crossref , Medline , Google Scholar
22 Spellman T, Liston C : Toward circuit mechanisms of pathophysiology in depression . Am J Psychiatry 2020 ; 177:381–390 Link , Google Scholar
23 Reiff CM, Richman EE, Nemeroff CB, et al. : Psychedelics and psychedelic-assisted psychotherapy . Am J Psychiatry 2020 ; 177:391–410 Link , Google Scholar
24 Schatzberg AF : Some comments on psychedelic research (editorial). Am J Psychiatry 2020 ; 177:368–369 Link , Google Scholar
25 McTeague LM, Rosenberg BM, Lopez JW, et al. : Identification of common neural circuit disruptions in emotional processing across psychiatric disorders . Am J Psychiatry 2020 ; 177:411–421 Link , Google Scholar
26 Caspi A, Moffitt TE : All for one and one for all: mental disorders in one dimension . Am J Psychiatry 2018 ; 175:831–844 Link , Google Scholar
27 Barch DM : What does it mean to be transdiagnostic and how would we know? (editorial). Am J Psychiatry 2020 ; 177:370–372 Abstract , Google Scholar
28 Gray JP, Müller VI, Eickhoff SB, et al. : Multimodal abnormalities of brain structure and function in major depressive disorder: a meta-analysis of neuroimaging studies . Am J Psychiatry 2020 ; 177:422–434 Link , Google Scholar
29 Siddiqi SH, Taylor SF, Cooke D, et al. : Distinct symptom-specific treatment targets for circuit-based neuromodulation . Am J Psychiatry 2020 ; 177:435–446 Link , Google Scholar
30 Nestor SM, Blumberger DM : Mapping symptom clusters to circuits: toward personalizing TMS targets to improve treatment outcomes in depression (editorial). Am J Psychiatry 2020 ; 177:373–375 Abstract , Google Scholar
31 Kendler KS, Ohlsson H, Sundquist J, et al. : The rearing environment and risk for major depression: a Swedish national high-risk home-reared and adopted-away co-sibling control study . Am J Psychiatry 2020 ; 177:447–453 Abstract , Google Scholar
32 Weissman MM : Is depression nature or nurture? Yes (editorial). Am J Psychiatry 2020 ; 177:376–377 Abstract , Google Scholar
33 Gold AL, Abend R, Britton JC, et al. : Age differences in the neural correlates of anxiety disorders: an fMRI study of response to learned threat . Am J Psychiatry 2020 ; 177:454–463 Link , Google Scholar
34 Gee DG, Kribakaran S : Developmental differences in neural responding to threat and safety: implications for treating youths with anxiety (editorial). Am J Psychiatry 2020 ; 177:378–380 Abstract , Google Scholar
- Cited by None
- Neuroanatomy
- Neurochemistry
- Neuroendocrinology
- Other Research Areas
- Australia edition
- International edition
- Europe edition

The link between stress and depression … and the 10 simple words that could help
Neurological insights into how the brain processes stress, and how it can develop into depression, have led to new interventions
I t’s a damp, midweek afternoon. Even so, Cardiff’s walk-in stress management course has pulled in more than 50 people. There are teenagers, white-haired older people with walking aids, people from Caucasian, Asian and Middle Eastern backgrounds. There is at least one pair who look like a parent and child – I’m unsure who is there to support whom.
The course instructor makes it clear that she is not going to ask people to speak out about their own stress levels in this first class: “We know speaking in public is stressful in itself.” She tells us a bit about previous attendees: a police officer whose inexplicable and constant worrying prevented him from functioning; a retired 71-year-old unable to shake the incomprehensible but constant fatigue and sadness that blighted his life; a single mother unable to attend her daughter’s school concert, despite the disappointment it would cause.
What is the common theme that links these people – and the varied group sitting there this afternoon and listening?
Stress may once just have been a kind of executive trophy – “I’m so stressed!” – but recent research suggests it is a key element in developing mental health problems such as depression and anxiety.
The constant, stress-induced stimulation of key brain regions seems to be a major contributor to anxiety. And, in turn, vital brain regions becoming unresponsive and inflexible is believed to be a fundamental element of depressive disorders. Why do these regions become unresponsive? Possibly because they’re overworked, exhausted, by the effects of stress. This would explain why anxiety and depression regularly occur together.
So what is stress? In essence, it is the first stage of the fight-or-flight response, the classic reaction to danger, the ingrained reflex that compels you to tackle danger head-on or run screaming from it. A third option, freeze, is also included in the modern-day understanding, which explains that inability to move when you’re truly scared.
This potent fear response isn’t like a switch, a simple yes/no thing. There are neurological and biochemical systems that prepare your brain, and body, for having to deal with a threat. It’s regulated by a complex suite of brain networks and hormonal reactions, and one key element in the stress response is the amygdala, the part of the brain that (among other things) decides whether or not stress is warranted.
The stress response has numerous potent effects on us. It increases our focus on negative things, such as whatever is causing the stress, because when you’re dealing with a problem you can’t afford to waste time pondering irrelevant things. It puts your brain and body into a more alert state, meaning you become more sensitive to hazards and risks, both physically and mentally. It’s useful for keeping you safe, but again leads to you focusing on the negatives, the unpleasant aspects of your current existence, and downplays the potentially distracting positives.

Problematically, because of these things, stress is also very stimulating. It releases several potent chemicals into your bloodstream – cortisol for instance, which amps up your heart rate, muscle tension, glucose uptake, even your immune system responses.
The trigger, the activation of the stress response, comes from our brains, with the hypothalamic-pituitary-adrenal (HPA) axis – a complex association between the hypothalamus and the pituitary and adrenal glands – as the key element. The HPA axis is basically the link between the brain and the body when it comes to stress. When our brain decides that stress is required, signals are sent to the HPA axis, which in turn releases a complex sequence of chemicals that ends up with stress hormones, such as cortisol and glucocorticoids, being released into our bloodstream.
But here’s the problem. In many people, this ability of the HPA axis to recognise when there’s enough stress chemical in the body and so cease production is disrupted in some way. The HPA axis can start the physical stress response but doesn’t seem to know when to stop.
This might sound like a mild annoyance but there’s mounting evidence to suggest that it’s a cause of multiple mental health problems, particularly depression. Those who have chronic depression, and many who have killed themselves, have been shown to have significantly elevated levels of glucocorticoids, cortisol and other stress chemicals in their blood and tissues.
The constant bombardment from stress chemicals potentially underlies many of the physical symptoms of depression. Weight gain, hypertension, a suppressed immune system, heart problems – all can be attributed to the persistent action of stress chemicals in the body. For example, these stress chemicals and hormones seem to have a potent effect on neurons, and therefore the functioning of the brain. Specifically, they seem to stimulate areas such as the hippocampus and prefrontal cortex to enhance our memory, thinking and focus, because when you’re in a stressful situation, you need to have your wits about you, and you need to remember what happens in case it happens again.
Unfortunately, this causes a problem. Neurons can handle a certain amount of increased signalling, some excitation. But too much leads to excitotoxicity, a phenomenon whereby too much activity damages and impairs the neuron. The complex biochemical processes a neuron engages in are quite demanding. Give them time to restock and replenish after being pushed to their limit and they’ll be fine. But keep pushing them and they’ll suffer.
So, stress chemicals stimulate many areas of the brain. But when the HPA axis keeps pumping them out, those brain areas are stimulated too much, exhausting and damaging the neurons, causing them to lose plasticity. And a loss of neuroplasticity is now believed by some scientists to be a key part of depression. Simultaneously, there’s no reason why other parts of the brain, with neurons that have subtly different properties, can’t respond differently to the stress hormones, possibly being enhanced by them.
There is a possibility that it’s the unhampered stress response that causes some or even all of the issues of depression, inducing the physical symptoms, reducing neuroplasticity in certain key areas by overworking them while enhancing other regions to the extent that they become dominant to a disruptive extent.
But what causes stress and how can we deal with it? The “handling stress” course that I attended is based on the works of acclaimed Scottish psychologist and stress-control proponent Dr Jim White . It’s provided by the local NHS trust, and most trusts offer an equivalent. The programme has been running nationally for 30 years, helping tens of thousands of people.
So what stresses us out? Failure to meet expectations. Having to do more than we can handle. A loss of status, or living standards, or security, or something or someone important. But all of our expectations, standards, capacities, understandings and baselines are derived from a mental model of how the world works, a model our brains create and maintain based on our memories, experiences and beliefs.
Stress is largely subjective. It often comes from negative changes or influences in our lives, when they occur with too much intensity. That our lives remain positive overall compared with those of others is irrelevant. That’s why questions such as: “What have you got to be stressed about?” don’t make sense. Thanks to how our brain works, if you don’t like something or don’t want it to happen, it can, and will, stress you out.
Breathing exercises can genuinely help. A new therapy widely in use today that bears a significant resemblance to breathing exercises is biofeedback , or in some cases neurofeedback . The affected person is hooked up to monitors that display the physical outputs of their body, such as heart rate, muscle tension, skin conductance, brainwaves in the case of neurofeedback. These physiological actions typically occur at a subconscious level; we aren’t really “aware” of them. Bio/neurofeedback makes us aware, meaning we can focus on them and try to control them with our conscious minds.
This appears to help because it reduces uncertainty; not knowing what is happening or going to happen can be more stressful than knowing something bad is going to happen. That’s just the way the brain is wired. It reacts much better to knowing than not knowing. And being aware of our breathing or heart rate provides certainty where we didn’t have any before.
Small steps, incremental progress, are something that is emphasised repeatedly on the Cardiff course. This is a way to help break the “stress cycle” , which describes how stress becomes chronic and self-sustaining. Let’s start with a relationship breakdown. This causes stress, with low mood, lack of motivation, etc. This leads to reduced socialisation; your friendships suffer, and you end up more miserable, more stressed. So you drink more to feel better, albeit briefly. But this makes you less healthy, more sluggish, and your work suffers. Now your job’s in trouble, your health declining. This causes more stress. So you drink more. Which means more stress. And on and on.
There is no easy fix. But at the very start of the session, we are given a brief, basic set of instructions that could, if adhered to, tangibly reduce stress. There were just 10 words: “Face your fears. Be more active. Watch what you drink.” While simple-sounding, these things conform to what we know about stress, and even mental health problems, in the scientific sense.
Facing your fears is often easier said than done but it’s a valid approach. When we confront something that scares us, that stresses us, we may not enjoy it but we impose certainty on it. All the things that could have happened and had the power to cause stress have been cancelled out. In many cases, facing your fear has a net reduction of your stress due to how our brains work.
Being more physically active is helpful in so many ways. As well as the health benefits, it also maintains a sense of control. My friend Dan found that dealing with his stress and depression has been a lot easier since getting a dog. She needs to be walked no matter what he’s feeling. Taking her means he’s stayed active and achieved something.
And “watch what you drink”. Not just alcohol, with it’s short-term euphoric effects but long-term depressive and anxiety-inducing ones. Caffeine is something to be wary of, too, as it stimulates the parts of the brain already overworked due to stress, and also disrupts sleep, another thing that can enhance/prolong stress.
Ten words. Three simple instructions. But, given enough time, sometimes that’s all it takes to make significant changes.
Dean Burnett is a neuroscientist . His new audiobook, Psycho-Logical, is available at audible.co.uk
- Neuroscience
- In mind: focus on mental health
- Mental health
Most viewed
- Share full article
Advertisement
Supported by
Personal Health
The Devastating Ways Depression and Anxiety Impact the Body
Mind and body form a two-way street.

By Jane E. Brody
It’s no surprise that when a person gets a diagnosis of heart disease, cancer or some other life-limiting or life-threatening physical ailment, they become anxious or depressed. But the reverse can also be true: Undue anxiety or depression can foster the development of a serious physical disease, and even impede the ability to withstand or recover from one. The potential consequences are particularly timely, as the ongoing stress and disruptions of the pandemic continue to take a toll on mental health .
The human organism does not recognize the medical profession’s artificial separation of mental and physical ills. Rather, mind and body form a two-way street. What happens inside a person’s head can have damaging effects throughout the body, as well as the other way around. An untreated mental illness can significantly increase the risk of becoming physically ill, and physical disorders may result in behaviors that make mental conditions worse.
In studies that tracked how patients with breast cancer fared, for example, Dr. David Spiegel and his colleagues at Stanford University School of Medicine showed decades ago that women whose depression was easing lived longer than those whose depression was getting worse. His research and other studies have clearly shown that “the brain is intimately connected to the body and the body to the brain,” Dr. Spiegel said in an interview. “The body tends to react to mental stress as if it was a physical stress.”
Despite such evidence, he and other experts say, chronic emotional distress is too often overlooked by doctors. Commonly, a physician will prescribe a therapy for physical ailments like heart disease or diabetes, only to wonder why some patients get worse instead of better.
Many people are reluctant to seek treatment for emotional ills. Some people with anxiety or depression may fear being stigmatized, even if they recognize they have a serious psychological problem. Many attempt to self-treat their emotional distress by adopting behaviors like drinking too much or abusing drugs, which only adds insult to their pre-existing injury.
And sometimes, family and friends inadvertently reinforce a person’s denial of mental distress by labeling it as “that’s just the way he is” and do nothing to encourage them to seek professional help.
How common are anxiety and depression?
Anxiety disorders affect nearly 20 percent of American adults . That means millions are beset by an overabundance of the fight-or-flight response that primes the body for action. When you’re stressed, the brain responds by prompting the release of cortisol, nature’s built-in alarm system. It evolved to help animals facing physical threats by increasing respiration, raising the heart rate and redirecting blood flow from abdominal organs to muscles that assist in confronting or escaping danger.
These protective actions stem from the neurotransmitters epinephrine and norepinephrine, which stimulate the sympathetic nervous system and put the body on high alert. But when they are invoked too often and indiscriminately, the chronic overstimulation can result in all manner of physical ills, including digestive symptoms like indigestion, cramps, diarrhea or constipation, and an increased risk of heart attack or stroke.
Depression, while less common than chronic anxiety, can have even more devastating effects on physical health. While it’s normal to feel depressed from time to time, more than 6 percent of adults have such persistent feelings of depression that it disrupts personal relationships, interferes with work and play, and impairs their ability to cope with the challenges of daily life. Persistent depression can also exacerbate a person’s perception of pain and increase their chances of developing chronic pain.
“Depression diminishes a person’s capacity to analyze and respond rationally to stress,” Dr. Spiegel said. “They end up on a vicious cycle with limited capacity to get out of a negative mental state.”
Potentially making matters worse, undue anxiety and depression often coexist, leaving people vulnerable to a panoply of physical ailments and an inability to adopt and stick with needed therapy.
A study of 1,204 elderly Korean men and women initially evaluated for depression and anxiety found that two years later, these emotional disorders increased their risk of physical disorders and disability. Anxiety alone was linked with heart disease, depression alone was linked with asthma, and the two together were linked with eyesight problems, persistent cough, asthma, hypertension, heart disease and gastrointestinal problems.
Treatment can counter emotional tolls
Although persistent anxiety and depression are highly treatable with medications, cognitive behavioral therapy and talk therapy, without treatment these conditions tend to get worse. According to Dr. John Frownfelter, treatment for any condition works better when doctors understand “the pressures patients face that affect their behavior and result in clinical harm.”
Dr. Frownfelter is an internist and chief medical officer of a start-up called Jvion. The organization uses artificial intelligence to identify not just medical factors but psychological, social and behavioral ones as well that can impact the effectiveness of treatment on patients’ health. Its aim is to foster more holistic approaches to treatment that address the whole patient, body and mind combined.
The analyses used by Jvion, a Hindi word meaning life-giving, could alert a doctor when underlying depression might be hindering the effectiveness of prescribed treatments for another condition. For example, patients being treated for diabetes who are feeling hopeless may fail to improve because they take their prescribed medication only sporadically and don’t follow a proper diet, Dr. Frownfelter said.
“We often talk about depression as a complication of chronic illness,” Dr. Frownfelter wrote in Medpage Today in July . “But what we don’t talk about enough is how depression can lead to chronic disease. Patients with depression may not have the motivation to exercise regularly or cook healthy meals. Many also have trouble getting adequate sleep.”
Some changes to medical care during the pandemic have greatly increased patient access to depression and anxiety treatment. The expansion of telehealth has enabled patients to access treatment by psychotherapists who may be as far as a continent away.
Patients may also be able to treat themselves without the direct help of a therapist. For example, Dr. Spiegel and his co-workers created an app called Reveri that teaches people self-hypnosis techniques designed to help reduce stress and anxiety, improve sleep, reduce pain and suppress or quit smoking.
Improving sleep is especially helpful, Dr. Spiegel said, because “it enhances a person’s ability to regulate the stress response system and not get stuck in a mental rut.” Data demonstrating the effectiveness of the Reveri app has been collected but not yet published, he said.
Jane Brody is the Personal Health columnist, a position she has held since 1976. She has written more than a dozen books including the best sellers “Jane Brody’s Nutrition Book” and “Jane Brody’s Good Food Book.” More about Jane E. Brody
Jane Brody’s Personal Health Advice
After joining the new york times in 1965, she was its personal health columnist from 1976 to 2022. revisit some of her most memorable writing:.
Brody’s first column, on jogging , ran on Nov. 10, 1976. Her last, on Feb. 21. In it, she highlighted the evolution of health advice throughout her career.
Personal Health has often offered useful advice and a refreshing perspective. Declutter? This is why you must . Cup of coffee? Yes, please.
As a columnist, she has never been afraid to try out, and write about, new things — from intermittent fasting to knitting groups .
How do you put into words the pain of losing a spouse of 43 years? It is “nothing like losing a parent,” she wrote of her own experience with grieving .
Need advice on aging? She has explored how to do it gracefully , building muscle strength and knee replacements .
Stress, Anxiety and Depression
- First Online: 29 October 2022
Cite this chapter

- Robert W. Baloh 2
622 Accesses
Stress, defined as a feeling of being overwhelmed and unable to cope, can affect anyone but it is how we react to that feeling that determines whether or not it is detrimental to our health. Short bouts of stress are usually well tolerated and may even improve performance but chronic stress produces a wide range of chemical and structural changes in the brain that are usually detrimental. Stress triggers the release of adrenalin and cortisol from the adrenal gland that can trigger a variety of somatic symptoms.
Chronic stress can impair the cardiovascular and immune systems and inhibit neuroplasticity and neurogenesis in the brain. Exercise and improved physical fitness can prevent all of these stress related changes. Long periods of stress can lead to anxiety and depression and often symptoms of anxiety and depression overlap. Exercise is a proven treatment for both anxiety and depression and in many cases it is more effective than currently prescribed medications.
- Pituitary gland
- Adrenal gland
- Antidepressants
- Post traumatic stress disorder
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Levone BR, Cryan JF, O’Leary OF. Role of adult hippocampal neurogenesis in stress resilience. Neurobiol Stress. 2015;1:147e155.
Google Scholar
Watson D, Pennebaker JW. Health complaints, stress, and distress: exploring the central role of negative affectivity. Psych Rev. 1989;96:234–54.
Article CAS Google Scholar
Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol Bull. 2004;130:601–30.
Article PubMed PubMed Central Google Scholar
Liu LY, Coe CL, Swenson CA, et al. School examination enhances airway inflammation to antigen challenge. Am J Respir Crit Care Med. 2002;165:1062–7.
Article PubMed Google Scholar
Mohd RS. Life event, stress and illness. Malaysian J Med Sci. 2008;15:9–18.
Cannon WB. Bodily changes in pain, hunger, fear and rage: an account of recent researches into the function of emotional excitement. New York: Appleton; 1915.
Book Google Scholar
Selye H. Stress and psychiatry. Am J Psychiatr. 1956;113:423–7.
Article CAS PubMed Google Scholar
Notaras M, van den Buuse M. Neurobiology of BDNF in fear memory, sensitivity to stress, and stress-related disorders. Mol Psychiat. 2020;25:2251–74.
Article Google Scholar
Notaras M, van den Buuse M. Brain-derived neurotrophic factor (BDNF): novel insights into regulation and genetic variation. Neuroscientist. 2019;25:434–54.
McEwwn BS, Nasca C, Gray JD. Stress effects on neuronal structure: hippocampus, amygdala and prefrontal cortex. Neuropsychopharmacology. 2016;41:3–23.
Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psych. 2009;65:732–41.
Raison CL, Capuron L, Miller AH. Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends Immunol. 2006;27:24–31.
Koo JW, Duman RS. Evidence for IL-1 receptor blockade as a therapeutic strategy for the treatment of depression. Curr Opin Invest Drugs. 2009;10:664–71.
CAS Google Scholar
Leknes S, Tracey I. A common neurobiology for pain and pleasure. Nat Rev Neurosci. 2008;9:314–20.
Chekroud SR, Gueorguieva R, Zheutlin AB, et al. Association between physical exercise and mental health in 1.2 million individuals in the USA between 2011 and 2015: a cross-sectional study. Lancet Psychiatry. 2018;5:739–46.
Di Liegro CM, Schiera G, Proia P, Di Liegro I. Physical activity and brain health. Genes. 2019;10:720.
Article CAS PubMed Central Google Scholar
Nay K, Smiles WJ, Kaiser J, et al. Molecular mechanisms underlying the beneficial effects of exercise on brain function and neurological disorders. INt J Mol Sci. 2021;22:4052.
Article CAS PubMed PubMed Central Google Scholar
Breus MJ, O’Connor PJ. Exercise-induced anxiolysis: a test of the “time out” hypothesis in high anxious females. Med Sci Sports Exerc. 1998;30(7):1107–12.
Baloh RW. PTSD, The prototypical delayed stress disorder. In: Baloh RW, editor. Medically unexplained symptoms. A brain-centered approach. New York: Springer; 2020. p. 71–5.
Hegberg NJ, Hayes JP, Hayes SM. Exercise intervention in PTSD: a narrative review and rationale for implementation. Front Psych. 2019;10:133.
LeardMann CA, Kelton ML, Smith B, et al. Prospectively assessed posttraumatic stress disorder and associated physical activity. Public Health Rep. 2011;126:371–83.
Fetzner MG, Asmundson GJ. Aerobic exercise reduces symptoms of posttraumatic stress disorder: a randomized controlled study. Cogn Behav Ther. 2015;44:301–13.
Goldstein LA, Mehling WE, Metzer TJ, et al. Veterans group exercise: a randomized pilot trial of an integrative exercise program for veterans with post-traumatic stress. J Affect Disord. 2018;227:345–52.
Bystritsky A. Current diagnosis and treatment of anxiety disorders. Pharm Therapeut. 2013;38:30–8.
Price JS. Evolutionary aspects of anxiety disorders. Dialogues Clin Neurosci. 2003;5:223–36.
Kandola A, Stubbs B. Exercise and anxiety. In: Xiao J, editor. Physical exercise for human health. Singapore: Springer; 2020. p. 345–51.
Chapter Google Scholar
Stonerock GL, Hoffman BM, Smith PJ, Blumenthal JA. Exercise as treatment for anxiety: systematic review and analysis. Ann Behav Med. 2015;49:542–56.
DeMoor MHM, Beem AL, Stubbe JH, et al. Regular exercise, anxiety, depression and personality: a population-based study. Prev Med. 2006;42:273–9.
American Psychiartic Association. Diagnostic and statistical manual of metal disorders. In: DSM-5, vol. 991. 5th ed. Arlington VA: Am Psychiat Assoc; 2013. p. 555–8.
Khan AR, Geiger L, Wiborg O, Czeh B. Stress-induced morphological, sellular and molecular changes in the brain—lessons learned from the chronic mild stress model of depression. Cell. 2020;9:1026.
Morgan WP. A pilot investigation of physical working capacity in depressed and nondepressed psychiatric males. Res Q. 1969;40:859–61.
CAS PubMed Google Scholar
Teychenne M, Ball K, Salmon J. Physical activity and likelihood of depression in adults: a review. Prev Med. 2008;46:397–411.
Schuch FB, Vancampfort D, Firth J. Physical activity and incident depression: a meta-analysis of prospective cohort studies. Am J Psychiat. 2018;175:631–48.
Aberg MAI, Waern M, Nyberg J, et al. Cardiuovascular fitness in males at age 18 and risk of serious depression in adulthood: Swedish prospective population-based study. Br J Psychiatry. 2012;201:352–9.
Blumenthal JA, Smith PJ, Hoffman BM. Is exercise a viable treatment for depression. ACSMs Health Fit J. 2012;16:14–21.
Roeh A, Kirchner SK, Malchow B, et al. Depression in somatic disorders: is there a beneficial effect of exercise? Front Psych. 2019;10:14.
Download references
Author information
Authors and affiliations.
Neurology, University of California, Los Angeles, Los Angeles, CA, USA
Robert W. Baloh
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Robert W. Baloh .
Rights and permissions
Reprints and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Baloh, R.W. (2022). Stress, Anxiety and Depression. In: Exercise and the Brain. Springer, Cham. https://doi.org/10.1007/978-3-031-13924-6_7
Download citation
DOI : https://doi.org/10.1007/978-3-031-13924-6_7
Published : 29 October 2022
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-13923-9
Online ISBN : 978-3-031-13924-6
eBook Packages : Behavioral Science and Psychology Behavioral Science and Psychology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Narrative Essay about Anxiety and Depression
Everyone has a unique story, each with its hallmarks, learning lessons, and experiences. But despite our differences, we can all relate to having a major challenge in our life. Sometimes it's a stressful job, a medical condition, an accident, and sometimes it's losing a loved one. For me, my biggest challenge in life has been my mental health. In the last two years, I have battled anxiety and depression, grappling with a roller coaster of treatment options and the stigma that comes with it. This challenge has forced me to have a coming of age- I have had to learn important lessons, balance giving to others and caring for myself, and finally, I have realized my self-worth.
Anxiety and depression are hard for anyone to deal with, but especially for young adults like me when these problems are seen at large to 'only be faced by adults'. Feeling isolated and lost causes many people to not get the help they need- and often it can be too late before a step is taken to reach out for help. Luckily I was able to reach out for assistance and come to terms with my mental health, which many people of my age cannot do. This experience taught me to be brave, that it is okay to struggle, and that I am not alone.
I used to feel that I did not matter to others, and only cause them pain. I would 'make up for my existence' by trying to please others while neglecting myself. After getting support from those I love, I now know it's not narcissistic to take time for myself or to say 'no, not today.' Conversely, taking me-time and caring for myself allows me to have more energy and love to give to others. Now if I need some time, I don't feel like a terrible person, but instead relaxed and ready to bounce back.
Having feelings of intense sadness and worry for long periods of time can severely damage self-esteem. Personally, this prevented me from seeing any good in myself- I was stuck thinking I was a burden or terrible if I made a small mistake. I lost sight of my self-worth. After some healing, I began to reverse how I say myself and the world, until today where I realize that I can make the world a better place, and making mistakes is a part of being human.
I have had a great battle with my mental health in recent years. I am no stranger to feeling lost, isolated, and unloved. Although I am not quite an adult, I have learned hard lessons though to only be faced by 'grown-ups', learned to care for myself and recognize my true worth. Today I still struggle with negative thoughts and worry, but I have built a strong inner voice that keeps me going: I am not perfect, I am human, I learn from my mistakes, make the world a better place with my life, and most importantly I am worthy of love from myself and others just the way I am.
Related Samples
- The Importance of Stem Cell Research Essay Sample
- QSEN Nursing Essay Example
- Wage Inequality Research Paper
- Blended Learning in the Age of COVID-19
- Personal Essay: The Career of a Dairy Nutritionist
- Pesonal Narrative Essay about Baking
- Essay Sample: Nursing Care and NHS Partnerships and Values
- Personality Changes Throughout Lifespan Essay Example
- Economic impact of the COVID-19 pandemic
- Essay On Racism And Discrimination In Health Care
Didn't find the perfect sample?

You can order a custom paper by our expert writers

What it’s like living with depression: A personal essay

For most people, emotions are non-linear. Feelings of despair and sadness are normal, along with good feelings, like joy and peace of mind. Depression can turn that regular range of emotions into an unusual and long-lasting period of despair, wherein the happy moments are non-existent—or few and far between. Here’s my experience of living with depression.
What depression feels like
In my early adulthood, I started to feel withdrawn, down, unmotivated, and constantly sad. What initially seemed like an off-day turned into weeks of painful feelings that seemed they would never let up. It was difficult to enjoy life with other people my age. Depression made typical, everyday tasks—like brushing my teeth—seem monumental. It felt like an invisible chain, keeping me in bed.
What I didn’t know at the time was, my skin color could make my journey to treatment even more challenging. Living with depression can be harder for Black people, explains Lauren Harris, Psy.D., a licensed clinical psychologist based outside of Chicago, Illinois. “Black adults are more likely than adults of other races to report depressive symptoms… and… less likely to receive treatment,” Harris says. This occurs for a variety of reasons, such as racism, stigma, and stereotypes that Black women in particular are strong and able to withstand pain more than other races.
RELATED: 9 questions to ask a doctor if you’re Black, Indigenous, or a person of color
Symptoms of depression
My depression sapped my energy and dulled my mood, but there are many different types of mood disorders—and the symptoms are different for everyone. According to the National Institute of Mental Health , some common signs include the following, when they linger all day, for at least two weeks:
- Persistent sad, anxious, or “empty” mood
- Feelings of hopelessness, or pessimism
- Irritability
- Feelings of guilt, worthlessness, or helplessness
- Loss of interest or pleasure in activities you normally enjoy
- Decreased energy or fatigue
- Moving or talking more slowly
- Feeling restless or having trouble sitting still
- Difficulty concentrating, remembering, or making decisions
- Difficulty sleeping, early-morning awakening, or oversleeping
- Appetite and/or weight changes (weight loss or weight gain)
- Thoughts of death or suicide, or suicide attempts
- Aches or pains, headaches, cramps, or digestive problems without a clear physical cause and/or that do not ease even with treatment
If you’re experiencing these signs, talk to your healthcare provider about a depression assessment.
Treating my depression
My diagnosis took longer than expected due to the stigma of mental health issues and racism. A series of doctors dismissed my symptoms and even told me to be strong, that surely I had been through worse. My symptoms got worse and more severe, and I realized that I could not continue as if everything were normal. I finally saw a psychiatrist who took my concerns seriously and prescribed an antidepressant called fluoxetine (the generic of Prozac ), alongside therapy with a psychologist. Initially, I was reluctant to start on antidepressants because of the stigma associated with it.
I was pleasantly surprised when—after around three weeks—I started feeling results. My intense feeling of overwhelming sadness and hopelessness slowly started to lift and the fears I had about not feeling like myself dissipated. I had worried I would feel less like myself on fluoxetine, but instead for the first time, in a long time—I felt more like myself and able to function throughout the day. Receiving treatment and building healthy coping mechanisms has allowed me to continue to function, even when a depressive episode hits.
Aside from cognitive behavioral therapy and medication, there are many natural remedies that can help alleviate symptoms of depression, according to Tiffany Bowden, Ph.D., diversity consultant, mental health professional. “Exercise and a healthy diet are particularly supportive,” Bowden says. “Self-care regimen, caring for plants, aromatherapy, yoga, music, engaging with positive friends, hair care, caring for animals, and family time when families are in healthy balance are all great supports.”
Simple and practical steps like these work for me. Learning to be more mindful and staying present in the moment (not freaking out about the future) has lessened many depressive feelings for me. Repetitive tasks, like hair care while listening to my favorite music, help me self-soothe and work through my feelings. Aromatherapy with certain herbal scents, like lavender, helps to calm me—and doubles as a natural remedy for my anxiety and insomnia . It is also helpful on the go. I carry dried lavender or lavender essential oil with me and inhale it or dab some on my wrist for an instant calming effect.
Living with depression
A part of managing my depression is accepting it, as with any other illness. It is a lifelong healing journey that requires changes to my treatment plan, patience, and most importantly loving kindness to myself.
Learning to understand my feelings, stressors, and triggers has helped me to manage my symptoms. That self-awareness makes it possible to avoid the situations, environments, or people that start my spiral into a low mood—and makes it easier to manage dips when they happen.
Overcoming and understanding depression can be daunting for anyone, but with a combination of therapy, medication, and homeopathic treatment, I’m able to live a normal life.
For anyone out there living with depression, know this: It is not the end, and you’re not alone. More than 17 million adults in the United States have had at least one major depressive episode, and 25 million adults have been taking antidepressants for at least two years. With effective treatment tailored to your symptoms, depression can be managed like any other health condition.
For more information on seeking help or treatment or depression support, visit the National Alliance on Mental Health or call the Substance Abuse and Mental Health Services Administration helpline at 1-800-662-HELP. You can also find a peer support group here . If you or a loved one is experiencing suicidal thoughts or self-harm, call the National Suicide Prevention Lifeline at 1-800-273-8255 or visit the nearest emergency room.
Top Reads in Community

Best 2023 SingleCare reviews

The best SingleCare reviews

Our favorite January reviews

Our best SingleCare reviews of 2022

Not Just Sadness: Decomposing Depression
What stops us from completing the work of sorrow and getting rid of depression.
Posted March 27, 2024 | Reviewed by Davia Sills
- What Is Depression?
- Find a therapist to overcome depression
- Sadness often accompanies depression, but they are not the same thing.
- Depression has also been linked to repressed anger and fear.
- Addressing the many possible components of depression can help people recover from it.
I often hear my clients say, "I don't want to discuss this subject—I don't want to be sad and get depressed."
Depression is indeed accompanied by sadness, so connecting depression with sadness is common. But so is confusing these two conditions.
Sadness vs. Depression
Sadness is a normal reaction to adverse situations. It develops when expected gratification is unavailable because of a separation from or loss of something important. We process sadness by means of sorrow and letting go.
Depression is a more complex condition. In addition to unremitting sadness, depression is defined by low mood, apathy, lack of joy ( anhedonia ), and inability to concentrate and stay focused. Corpus Hippocraticum , the classic work published between 500 and 400 BC and attributed to Hippocrates, among other authors, includes one of the first attempts to describe depression as a medical condition. It places fear above sadness as a psychotic symptom of depression, thus postulating that fear can be a more significant factor in depression than sadness (9).
Researchers such as John Bowlby , the creator of attachment theory, have concluded that sadness often appears as a reaction to some forms of loss "of a loved person or else of familiar and loved places, or of social roles" (Bowlby, 1980). Depression is also closely related to loss and to fear that this loss will recur. Bowlby described depression as a "real or feared loss of the parent figure, either temporary or permanent," and believed vulnerability to depression derived from these early insecure attachments and experiences of early loss or abandonment.
We process sadness by means of sorrow and grieving to accept and let go of the things we cannot change. Grief tends to come in waves. In contrast, depression is unyielding. In this way, depression can be seen as the antithesis of grief. Nancy McWilliams says, "People who grieve normally tend not to get depressed, even though they can be overwhelmingly sad during the period that follows bereavement or loss" (7).
The major role of anger in depression has been long known to psychoanalytic researchers and clinicians. In his classic work, Mourning and Melancholia , Sigmund Freud , the founding father of psychoanalysis , a precursor to all modern therapies, viewed depression "as hate turned upon the self after the loss of an important love object" (1). His close associate Karl Abraham noted a propensity towards hatred in patients with depression based on temperament or early experience. The authors speculated two things: 1) the experience of premature loss creates vulnerability to depression, and 2) depression results from anger turned inward in response to loss.
The melancholic state that Freud was exploring exhibited lost connections to something important to the extent that the depressed individuals became so identified with this lost object that they kept it firmly within themselves. They were unable to establish a meaningful connection or part from it and grieve its loss. Sadness became inseparable from their condition.
In sadness, one knows what they have lost, but in depression, the loss is often indiscernible and can't be addressed consciously. It is often interpreted by the individual as a sign of their own inadequacy, unlovability, or damage. They feel rejected, abandoned, and angry toward themselves in the form of shame , self-criticism, and guilt that their "badness" might have driven this thing away from their life. Thus, they feel inherently corrupt.
There Is a Lot of Further Research Connecting Depression With Anger.
Friedman, A. S. (1970) found that individuals diagnosed with depression scaled higher on the Resentment subscale of the Buss-Durkee Inventory than non-depressed people. Resentment is defined here as "repressing the experience of the hostile affect from consciousness" (4). Subjects reported significantly less verbal open hostility but significantly more resentment. Becker & Lesiak (1977) found that in clinic outpatients, the severity of depression correlated with covert hostility, including guilt, resentment, irritability, and suspicion, but not with overt hostility.
In earlier research by Friedman et al. (10), people were asked if it is ever right to be angry. Hospitalized depressed patients answered "yes" significantly less often than non-depressed control subjects. This suggests difficulty with acceptance and expression of anger or aggression at the time of depression. Riley et al. (1989) concluded in their study that "the results […] generally support the hypothesis that depression is related to an inhibition in anger expression. The depressed group reported higher levels of anger suppression than either the normal or PTSD groups" (11).

In another study by Kellner, R., Hernandez, J., & Pathak, D. (1992), 100 participants diagnosed with depression were given an extensive questionnaire about their condition. In all four groups, depression predicted inhibited anger for both sexes.
Improvement in all domains of inwardly directed hostility has been reported with the alleviation of depression (Blackburn et al. 1979; Mayo 1978; Friedman 1970).
Goldman & Haaga (1995) connected both anger and fear in depression. In comparison to non-depressed subjects, depressed subjects express more anger toward close family members than to others. This finding seems plausible considering the high rates of marital conflicts in couples that include a depressed partner (Schmaling and Jacobson, 1990). The fear of expressing anger to other people was highly correlated with anger suppression because of the fear of the consequences of such expression.
Brody et al. (1999) demonstrated that, in comparison to the never-depressed control group, recovered depressed patients reported suppressing their anger and being afraid of expressing it because they viewed it as damaging toward other people. The authors hypothesized that anger inhibition may play a causal role in the recurrence of depression.
These findings link both anger and the fear of expressing it, causing depressed individuals to suppress their anger out of fear. Thus, the role of inhibited anger in depressive conditions seems to be crucial.
There might also be confusion when we describe sadness as opposed to anger. Castel, P.-H. (2016) indicates confusion between these notions:
The very fact of saying "You make me sad" to somebody often expresses not so much sadness as anger and resentment. From a more psychological standpoint, sadness is often consciously experienced as an inward rage barred from public display; anger, similarly, when not fully acted out, commonly reverts to grief and feelings of helplessness. The opposition of inward vs. outward feelings will often reflect socially coded constraints on the legitimacy of the public exhibition of affective states. Agitated and violent children may actually be sad, while passive or submissive women are internally consummated with rage. (2).
Researchers such as Arieti, Bemporad, and Bowlby view depression as a sadness that cannot be "metabolized," so the work of sorrow cannot be completed. Inhibited anger, fear of expressing it, and lack of knowledge or positive previous experience on how to express anger constructively might play a crucial role in hindering the process of sorrow to eventually be rid of sadness and the symptoms of depression.
When dealing with depression both on a personal and therapeutic level, we need to take into account the possible presence of suppressed anger and equip ourselves and our clients with tools to deal with and express it constructively. Nancy McWilliams (2011) suggests that depressed individuals be in long-term or open-ended therapy instead of a pre-set number of sessions. If they have sufficient time to recognize their anger in a therapeutic environment, they will be able to address it. McWilliams states:
Treatments that are arbitrarily limited to a certain number of sessions may provide welcome comfort during a painful episode of clinical depression, but the time-limited experience may be ultimately assimilated unconsciously by the depressive person as another relationship that was traumatically cut short—further evidence that the patient is a failure in maintaining attachments (7).
Recognizing inhibited anger in a depressive state, learning to express it constructively in a therapeutic environment, and addressing the fear of losing important relationships due to anger can be salubrious strategies in helping one alleviate the symptoms of depression.
1. Freud S. (1917). Mourning and Melancholia. The Standard Edition of the Complete Psychological Works of Sigmund Freud, Volume XIV (1914-1916).
2. Castel, P.-H. (2016). Loss, Bereavement, Mourning, and Melancholia: A Conceptual Sketch, in Defence of Some Psychoanalytic Views. In Sadness or Depression? (pp. 109-119).
3. Painuly, N., Sharan, P., & Mattoo, S. K. (2004). Relationship of anger and anger attacks with depression. European Archives of Psychiatry and Clinical Neuroscience, 255(4), 215–222.
4. Friedman, A. S. (1970). Hostility Factors and Clinical Improvement in Depressed Patients. Archives of General Psychiatry, 23(6), 524.
5. GOLDMAN, L., & HAAGA, D. A. F. (1995). Depression and the Experience and Expression of Anger in Marital and Other Relationships. The Journal of Nervous and Mental Disease, 183 (8), 505-509.
6. Busch FN (2009). Anger and depression. Advances in Psychiatric Treatment, 15(4):271-278.
7. McWilliams, Nancy. (2011). Psychoanalytic diagnosis: Understanding personality structure in the clinical process (2nd ed.). ISBN 978-1-60918-494-0.
8. Kellner, R., Hernandez, J., & Pathak, D. (1992). Self-Rated Inhibited Anger, Somatization and Depression. Psychotherapy and Psychosomatics, 57(3), 102–107.
9. Azzone, Paolo. Depression as a Psychoanalytic Problem. University Press of America, 2012.
10. Friedman AS, Granick S: A note on anger and aggression in old age. J Geront 18:283-285, 1963.
11. RILEY, W. T., TREIBER, F. A., & WOODS, M. G. (1989). Anger and Hostility in Depression. The Journal of Nervous and Mental Disease, 177(11), 668–674.
12. Allan, S., & Gilbert, P. (2002). Anger and anger expression in relation to perceptions of social rank, entrapment and depressive symptoms. Personality and Individual Differences, 32(3), 551–565.

Boris Herzberg has been working with individuals, couples and groups for more than a decade as a counselor, consultant and coach.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
Study Tracks Shifts in Student Mental Health During College
Dartmouth study followed 200 students all four years, including through the pandemic.

Phone App Uses AI to Detect Depression From Facial Cues
A four-year study by Dartmouth researchers captures the most in-depth data yet on how college students’ self-esteem and mental health fluctuates during their four years in academia, identifying key populations and stressors that the researchers say administrators could target to improve student well-being.
The study also provides among the first real-time accounts of how the coronavirus pandemic affected students’ behavior and mental health. The stress and uncertainty of COVID-19 resulted in long-lasting behavioral changes that persisted as a “new normal” even as the pandemic diminished, including students feeling more stressed, less socially engaged, and sleeping more.
The researchers tracked more than 200 Dartmouth undergraduates in the classes of 2021 and 2022 for all four years of college. Students volunteered to let a specially developed app called StudentLife tap into the sensors that are built into smartphones. The app cataloged their daily physical and social activity, how long they slept, their location and travel, the time they spent on their phone, and how often they listened to music or watched videos. Students also filled out weekly behavioral surveys, and selected students gave post-study interviews.
The study—which is the longest mobile-sensing study ever conducted—is published in the Proceedings of the ACM on Interactive, Mobile, Wearable and Ubiquitous Technologies .
The researchers will present it at the Association of Computing Machinery’s UbiComp/ISWC 2024 conference in Melbourne, Australia, in October.
These sorts of tools will have a tremendous impact on projecting forward and developing much more data-driven ways to intervene and respond exactly when students need it most.
The team made their anonymized data set publicly available —including self-reports, surveys, and phone-sensing and brain-imaging data—to help advance research into the mental health of students during their college years.
Andrew Campbell , the paper’s senior author and Dartmouth’s Albert Bradley 1915 Third Century Professor of Computer Science, says that the study’s extensive data reinforces the importance of college and university administrators across the country being more attuned to how and when students’ mental well-being changes during the school year.
“For the first time, we’ve produced granular data about the ebb and flow of student mental health. It’s incredibly dynamic—there’s nothing that’s steady state through the term, let alone through the year,” he says. “These sorts of tools will have a tremendous impact on projecting forward and developing much more data-driven ways to intervene and respond exactly when students need it most.”
First-year and female students are especially at risk for high anxiety and low self-esteem, the study finds. Among first-year students, self-esteem dropped to its lowest point in the first weeks of their transition from high school to college but rose steadily every semester until it was about 10% higher by graduation.
“We can see that students came out of high school with a certain level of self-esteem that dropped off to the lowest point of the four years. Some said they started to experience ‘imposter syndrome’ from being around other high-performing students,” Campbell says. “As the years progress, though, we can draw a straight line from low to high as their self-esteem improves. I think we would see a similar trend class over class. To me, that’s a very positive thing.”
Female students—who made up 60% of study participants—experienced on average 5% greater stress levels and 10% lower self-esteem than male students. More significantly, the data show that female students tended to be less active, with male students walking 37% more often.
Sophomores were 40% more socially active compared to their first year, the researchers report. But these students also reported feeling 13% more stressed during their second year than during their first year as their workload increased, they felt pressure to socialize, or as first-year social groups dispersed.
One student in a sorority recalled that having pre-arranged activities “kind of adds stress as I feel like I should be having fun because everyone tells me that it is fun.” Another student noted that after the first year, “students have more access to the whole campus and that is when you start feeling excluded from things.”
In a novel finding, the researchers identify an “anticipatory stress spike” of 17% experienced in the last two weeks of summer break. While still lower than mid-academic year stress, the spike was consistent across different summers.
In post-study interviews, some students pointed to returning to campus early for team sports as a source of stress. Others specified reconnecting with family and high school friends during their first summer home, saying they felt “a sense of leaving behind the comfort and familiarity of these long-standing friendships” as the break ended, the researchers report.
“This is a foundational study,” says Subigya Nepal , first author of the study and a PhD candidate in Campbell’s research group. “It has more real-time granular data than anything we or anyone else has provided before. We don’t know yet how it will translate to campuses nationwide, but it can be a template for getting the conversation going.”
The depth and accuracy of the study data suggest that mobile-sensing software could eventually give universities the ability to create proactive mental-health policies specific to certain student populations and times of year, Campbell says.
For example, a paper Campbell’s research group published in 2022 based on StudentLife data showed that first-generation students experienced lower self-esteem and higher levels of depression than other students throughout their four years of college.
“We will be able to look at campus in much more nuanced ways than waiting for the results of an annual mental health study and then developing policy,” Campbell says. “We know that Dartmouth is a small and very tight-knit campus community. But if we applied these same methods to a college with similar attributes, I believe we would find very similar trends.”
Weathering the pandemic
When students returned home at the start of the coronavirus pandemic, the researchers found that self-esteem actually increased during the pandemic by 5% overall and by another 6% afterward when life returned closer to what it was before. One student suggested in their interview that getting older came with more confidence. Others indicated that being home led to them spending more time with friends talking on the phone, on social media, or streaming movies together.
The data show that phone usage—measured by the duration a phone was unlocked—indeed increased by nearly 33 minutes, or 19%, during the pandemic, while time spent in physical activity dropped by 52 minutes, or 27%. By 2022, phone usage fell from its pandemic peak to just above pre-pandemic levels, while engagement in physical activity had recovered to exceed the pre-pandemic period by three minutes.
Despite reporting higher self-esteem, students’ feelings of stress increased by more than 10% during the pandemic. By the end of the study in June 2022, stress had fallen by less than 2% of its pandemic peak, indicating that the experience had a lasting impact on student well-being, the researchers report.
In early 2021, as students returned to campus, their reunion with friends and community was tempered by an overwhelming concern about the still-rampant coronavirus. “There was the first outbreak in winter 2021 and that was terrifying,” one student recalls. Another student adds: “You could be put into isolation for a long time even if you did not have COVID. Everyone was afraid to contact-trace anyone else in case they got mad at each other.”
Female students were especially concerned about the coronavirus, on average 13% more than male students. “Even though the girls might have been hanging out with each other more, they are more aware of the impact,” one female student reported. “I actually had COVID and exposed some friends of mine. All the girls that I told tested as they were worried. They were continually checking up to make sure that they did not have it and take it home to their family.”
Students still learning remotely had social levels 16% higher than students on campus, who engaged in activity an average of 10% less often than when they were learning from home. However, on-campus students used their phones 47% more often. When interviewed after the study, these students reported spending extended periods of time video-calling or streaming movies with friends and family.
Social activity and engagement had not yet returned to pre-pandemic levels by the end of the study in June 2022, recovering by a little less than 3% after a nearly 10% drop during the pandemic. Similarly, the pandemic correlates with students sticking closer to home, with their distance traveled nearly cut in half during the pandemic and holding at that level since then.
Campbell and several of his fellow researchers are now developing a smartphone app known as MoodCapture that uses artificial intelligence paired with facial-image processing software to reliably detect the onset of depression before the user even knows something is wrong.
Morgan Kelly can be reached at [email protected] .
- Mental Health and Wellness
- Innovation and Impact
- Arts and Sciences
- Class of 2021
- Class of 2022
- Department of Computer Science
- Guarini School of Graduate and Advanced Studies
- Mental Health
A Q&A With Film Critic and Theorist Vinzenz Hediger


After a Year of Turmoil, Harvard’s Applications Drop

Popular Services
- Patient & Visitor Guide
Committed to improving health and wellness in our Ohio communities.
Health equity, healthy community, classes and events, the world is changing. medicine is changing. we're leading the way., featured initiatives, helpful resources.
- Refer a Patient
Treating anxiety, depression significantly impacts heart disease outcomes
March 20, 2024
- For people who received both medication and talk therapy for anxiety or depression; the risk of hospitalization dropped 68 – 75%; the risk of being seen in the emergency department fell 67 – 74%, and the risk of death from any cause was reduced by about 67%.
- Talk therapy alone cut the risk of hospital readmission nearly in half (46 – 49%) and led to a similar reduction in emergency room visits (48 – 53%).
- Medication treatment alone reduced hospital readmission by up to 58% and reduced ER visits by up to 49%.
Study details and background
- 1,563 adults ages 22 – 64 were enrolled over a three-year period. All participants had a first hospital admission for blocked arteries or heart failure and had two or more health insurance claims for an anxiety disorder or depression.
- 68% were women, and 81% were noted as white. All were enrolled in Ohio’s Medicaid program during the six months prior to the hospital admission. Health data was from two sources: Ohio Medicaid claims and Ohio death certificate files from July 1, 2009, to June 30, 2012.
- Participants were followed through the end of 2014 or until death or the end of Medicaid enrollment.
- About 23% of participants received both antidepressant medications and psychotherapy; nearly 15% received psychotherapy alone; 29% took antidepressants alone; and 33% received no mental health treatment.
- About 92% of participants in the study were diagnosed with anxiety and 55.5% with depression prior to hospitalization.
Subscribe. Get just the right amount of health and wellness in your inbox.
- Skip to main content
- Keyboard shortcuts for audio player
Your Health
- Treatments & Tests
- Health Inc.
- Public Health
From anxiety to cancer, the evidence against ultra-processed food piles up

Allison Aubrey

Ultra-processed foods contain substances you wouldn't find in your own kitchen, like high-fructose corn syrup, artificial flavor and color enhancers, anti-caking agents and emulsifiers. Dan Kitwood/Getty Images hide caption
Ultra-processed foods contain substances you wouldn't find in your own kitchen, like high-fructose corn syrup, artificial flavor and color enhancers, anti-caking agents and emulsifiers.
At a time when Americans consume more than half of their daily calories from ultra-processed foods, there is increasing evidence that eating too many of these foods can make us sick.
A study published in the British Medical Journal finds people who consume high amounts of these foods have an increased risk of anxiety, depression, obesity, metabolic syndrome, certain cancers including colorectal cancer and premature death.
The data come from more than 9 million people who participated in dozens of studies, which researchers analyzed as part of umbrella review.
"Taking the body of literature as a whole, there was consistent evidence that regularly eating higher – compared to lower – amounts of ultra-processed foods was linked to these adverse health outcomes," says study author Melissa Lane , of Deakin University in Australia.

Shots - Health News
The u.s. diet is deadly. here are 7 ideas to get americans eating healthier.
Ultra-processed foods are abundant in our food supply. Among the most common are highly refined breads, fast food, sugary drinks, cereals, cookies, and other packaged snacks. They are often high in salt, sugar, fat and calories and low in fiber and micro-nutrients such as vitamins.
The Dietary Guidelines for Americans recommend filling half our plates with fruits and vegetables, and eating plenty of whole grains, and not too much of the refined grains found in ultra-processed foods.
One telltale sign that a food is ultra-processed is if its ingredient label includes substances you would not find in your own kitchen such as high-fructose corn syrup, hydrogenated oils, hydrolysed protein, or additives such as artificial colors, flavor enhancers, emulsifiers, anti-caking agents and thickeners.
Ultra-processed foods are everywhere. Here's how to avoid them

- LISTEN & FOLLOW
- Apple Podcasts
- Google Podcasts
- Amazon Music
Your support helps make our show possible and unlocks access to our sponsor-free feed.
The evidence piles up
The observational studies included in this new review do not prove that consumption of ultra-processed foods can cause anxiety, cancer or other health conditions. These studies point to associations, not causation. But at a time when diet is a leading cause of chronic disease , it adds to a growing body of evidence that ultra-processed foods contribute to the development of these conditions.
For instance, a study published last year found people in the habit of consuming high levels of ultra-processed foods were about three times more likely to develop colorectal cancer, compared to those who consumed the least. The exact mechanisms by which these foods may increase the risk is not clear, though the overlap with metabolic disease is striking.
"One mechanism of how ultra-processed food can be associated with colorectal cancer is through leading to increased weight," says Jeff Meyerhardt , an oncologist at Dana Farber Cancer Institute. Weight increases the risk of diabetes and metabolic syndrome factors, "that are closely tied to colorectal cancer," he says.

What we know about the health risks of ultra-processed foods

An ultra-processed diet made this doctor sick. Now he's studying why
When it comes to mood and mental health conditions, there is evidence to show that adults who maintain a healthy diet have fewer depressive symptoms . For instance, a French study found adherence to a Mediterranean diet in mid-life is linked to a lower risk of depression, particularly in men. There's also evidence that healthy diets may help tamp down anxiety .
"We're seeing a roughly 20 to 50% increased risk of depressive symptoms in people who have diets that are high in these ultra- processed foods," says Wolfgang Marx , a Senior Research Fellow at the Food & Mood Centre at Deakin University in Australia, and a senior author of the new research.
There could be a 'threshold effect' Marx says, meaning people who consume small amounts, under a certain threshold, are not at increased risk. Though it is not clear exactly how much is OK, because it may vary from person to person and depend on other lifestyle habits. However, the research shows people who consume the most are more likely to be affected by mood and mental health struggles.
Should consumers be warned about ultra-processed food?
A panel of advisors is currently evaluating all the latest diet and nutrition studies as part of a process to update the federal government's Dietary Guidelines . It is possible advisors could recommend limits on ultra-processed foods, though it would likely be difficult to get people to follow them.
On the regulatory side, the Food and Drug Administration is moving ahead to finalize a new definition of the term "healthy" – which is expected soon.
The FDA says a "healthy" claim on food labels could help consumers identify healthier choices at a quick glance and may prompt food companies to reformulate their products. The revised definition aims to make Americans more aware of healthy fats found in foods such as avocados and salmon, and of the relative harms of foods that contain lots of salt, added sugars and saturated fats.
The FDA is also moving towards front-of-package labeling that will flag foods that contain high amounts of sodium, sugar and saturated fat. These types of labels "will make it easier for consumers to make healthier choices and better understand the nutritional value of the foods and beverages they buy," says Nancy Brown, CEO of the American Heart Association.
And while the FDA is not currently tackling ultra-processed foods head on with labeling, Jim Jones, the FDA's first Deputy Commissioner for Human Foods says by focusing on these three ingredients – sodium, sugar and saturated fat – the agency aims to make people aware of the risks.
"The science around added sugars, saturated fat, and sodium intake is quite clear," says Jones. "We will also likely make progress on reducing consumption of ultra-processed food because there is a high correlation between those three ingredients and ultra-processed food," he says.
Jones says all regulatory decisions are based on scientific evidence, and there's still a lot that's unclear about the link between ultra-processed foods and disease.
Is it caused by more than the overlap with obesity and metabolic diseases? Given how palatable, convenient and inexpensive many of these foods are, is it easier to over-consume them? Or are there other mechanisms at play, such as ingredients or additives that can harm our gut health?
"Our feeling is that we need more science before we're ready to make recommendations or think of a voluntary or a regulatory program," he says.
And there is agreement from researchers and physicians that more research is needed to fully understand the connections between ultra-processed food consumption and disease risks.

This diet swap can cut your carbon footprint and boost longevity
This story was edited by Jane Greenhalgh & Carmel Wroth
- Diet-related disease
- ultra-processed foods
Anxiety and Depression Among College Students Essay
Education is expected to have appositive importance on the student’s life by enhancing their capability to think and improving their competency. However, it often acts as a source of stress that affects students’ mental health adversely. This causation of academic stress often emanates from the need to have high grades, the requirement to change attitude for success, and even pressures put by various school assignments. These pressures introduced by education can make the student undergo a series of anxiety, depression, and stress trying to conform to the forces. The causes of academic stress are well-researched but there is still no explanation why the rate of strain increases despite some measures being implemented to curb student stress. This research explores this niche by using 100 participants who study at my college.
Introduction
Nowadays there are many reasons that cause stress among growing number of students who might not know they are going through the condition most of the time. Hence, undiscovered discouragement or uneasiness can cause understudies to feel that they are continually passing up unique open doors. It prompts substance misuse; self-destruction is the second most typical reason for death among undergrads. The main hypothesis of this article is that college and university students have higher depression rates.
Problem Statement
This proposal undercovers how the problem of anxiety and depression is progressing if not addressed. With such countless youngsters experiencing undiscovered tension, it may be challenging for them to appreciate school. Understudies’ emotional well-being is risked when pressure and trouble go unnoticed, which can prompt social and educational issues (Nelson & Liebel, 2018). Educators might battle to perceive uneasiness since these circumstances manifest themselves contrastingly in different people.
Anxiety and depression are complicated disorders with numerous elements that impact people differently. Teachers and staff must be well trained to deal with these unforeseen events. Understudies coming to college come from various financial foundations, which can prompt an assortment of psychological wellness chances (Li et al., 2021). Additionally, current works will be evaluated to differentiate the risk factors associated with stress among university undergraduates worldwide.
There are various reasons which might cause the onset of anxiety and depression. It can be absence of rest, terrible dietary patterns, and lack of activity add to the gloom in undergrads (Ghrouz et al., 2019). Scholarly pressure, which incorporates monetary worries, strain to track down a decent profession after graduation, and bombed connections, is sufficient to drive a few understudies to exit school or more awful.
Numerous parts of school life add to despondency risk factors. For example, understudies today are owing debtors while having fewer work prospects than prior. Discouraged kids are bound to foster the problems like substance misuse (Lattie et al., 2019). For adaptation to close-to-home trouble, discouraged understudies are more inclined than their non-discouraged companions to knock back the firewater, drink pot, and participate in unsafe sexual practices.
Hypothesis on the Topic
The central hypothesis for this study is that college students have a higher rate of anxiety and depression. The study will integrate various methodologies to prove the hypothesis of nullifying it. High rates of anxiety and depression can lead to substance misuse, behavioral challenges, and suicide (Lipson et al., 2018). Anxiety is one of the most critical indicators of academic success, it shows how students’ attitudes change, reflecting on their overall performance.
Methods Section
Participants.
The study will use college students who are joining and those already in college. The research period is planned to last six months; college students are between the ages of 18 and 21 and life is changing rapidly at this age (Spillebout et al., 2019). This demography will come from the college where I study. The participants will be chosen randomly, the total number will be 100, both female and male, and from all races.
Apparatus/ Materials/ Instruments
Some of the materials to be used in the study will include pencils, papers, and tests. Paper and pencil are typical supplies that students are familiar with, so using them will not cause additional stress. It will be used during the interview with the students and throughout the study will be in effect (Huang et al., 2018). These have been applied in various studies before, and, hence, they will be instrumental in this study.
The study will follow a step-wise procedure to get the required results. First, the students’ pre-depression testing results would be researched and recorded. Second, the students would undergo standardized testing in the same groups. Scholarly accomplishment is impacted by past intellectual performance and standardized testing (Chang et al., 2020). Third, the students’ levels of depression and anxiety would be monitored along with their test results.
The study will use a descriptive, cross-sectional design with categorical and continuous data. The sample demographic characteristics were described using descriptive statistics. Pearson’s proportion of skewness values and common mistake of skewness was utilized to test the ordinariness of the persistent factors. The distinctions in mean scores between sociodemographic variables and stress will be examined using Tests (Lipson et al., 2018). The independent variable will be essential because it will provide the basis of measurement.
The 100 participants had different anxiety levels, as seen from the Test taken and the various evaluations. Forty-five of the participants had high levels, 23 had medium levels, while the remaining 32 had low levels (Lipson et al., 2018). The correlation and ANOVA, which had a degree of era margin of 0.05, were allowed (Lipson et al., 2018). This finding aligns intending to have clear and comprehensive outcomes.
Significance of the Study
If the results would be not significant, it means that students are not subjected to more pressure on average. If the study results in significant outcomes, this would mean that there is much that needs to be done to reduce student’s anxiety. The idea that scholarly accomplishment is indispensable to progress is built up in higher instructive conditions (Nelson & Liebel, 2018). Many colleges devote money to tutoring, extra instruction, and other support services to help students succeed.
APA Ethical Guidelines
The study will have to follow the APA ethical guidelines because it involves experimenting with humans. Some of the policies include having consent from the participant, debriefing the participant on the study’s nature, and getting IRB permission (Nelson & Liebel, 2018). Ethical guidelines should comply with proficient, institutional, and government rules. They habitually administer understudies whom they likewise instruct to give some examples of obligations.
Limitations
The study also had some limitations, making it hard to get the desired outcomes. It was not easy to detect the population-level connections, but not causality. This case hardened the aspect of confounding and getting the relevant random assignment needed for the study had to access (Nelson & Liebel, 2018). For the right individuals for the investigation to be identified, the sampling was not easy.
This study would be essential as it will create a platform for future studies. The result that was gotten shows that many college students are undergoing the problem of anxiety and depression without knowing that it is happening. Educators will have awareness on what aspects of academics they need to modify to ensure their students are not experiencing mental health challenges. Hence, it makes it possible for future researchers to conduct studies to provide possible solutions.
Chang, J., Yuan, Y., & Wang, D. (2020). Mental health status and its influencing factors among college students during the epidemic of COVID-19. Journal of Southern Medical University , 40(2), 171-176.
Ghrouz, A. K., Noohu, M. M., Manzar, D., Warren Spence, D., BaHammam, A. S., & Pandi-Perumal, S. R. (2019). Physical activity and sleep quality in relation to mental health among college students. Sleep and Breathing Journal , 23(2), 627-634.
Huang, J., Nigatu, Y. T., Smail-Crevier, R., Zhang, X., & Wang, J. (2018). Interventions for common mental health problems among university and college students: A systematic review and meta-analysis of randomized controlled trials. Journal of Psychiatric Research , 107, 1-10.
Lattie, E. G., Adkins, E. C., Winquist, N., Stiles-Shields, C., Wafford, Q. E., & Graham, A. K. (2019). Digital mental health interventions for depression, anxiety, and enhancement of psychological well-being among college students: A systematic review. Journal of Medical Internet Research , 21(7), e12869.
Li, Y., Zhao, J., Ma, Z., McReynolds, L. S., Lin, D., Chen, Z.,… & Liu, X. (2021). Mental health among college students during the COVID-19 pandemic in China: A 2-wave longitudinal survey. Journal of Affective Disorders , 281, 597-604.
Lipson, S. K., Kern, A., Eisenberg, D., & Breland-Noble, A. M. (2018). Mental health disparities among college students of color. Journal of Adolescent Health , 63(3), 348-356.
Nelson, J. M., & Liebel, S. W. (2018). Anxiety and depression among college students with attention-deficit/hyperactivity disorder (ADHD): Cross-informant, sex, and subtype differences. Journal of American College Health , 66(2), 123-132.
Spillebout, A., Dechelotte, P., Ladner, J., & Tavolacci, M. P. (2019). Mental health among university students with eating disorders and irritable bowel syndrome in France. Journal of Affective Disorders , 67(5), 295-301.
The following table shows the significant issues that affect the mental health state of most college students. Based on Huang et al.’s research, the biggest concern for most students included stress about their loved ones. Additionally, the authors found that worrying about one’s academics and schooling was the second depressing experience among most college students.
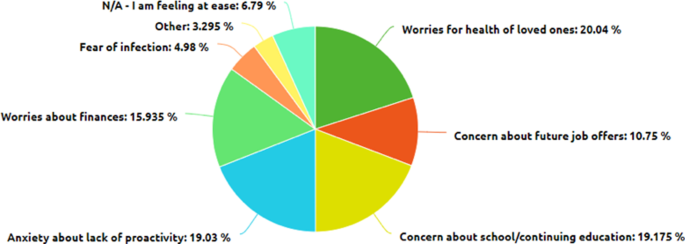
The following figure shows how on top of the current stressors for students, COVID-19 affects their mental health. Li et al.’s research demonstrates that COVID-19 placed more financial burden than before, especially on students with part-time jobs who often face anxiety and stress due to lack of tuition fees (Li et al., 2021). Generally, the research shows that the financial consequences of coronavirus affect the mental state of most college students.
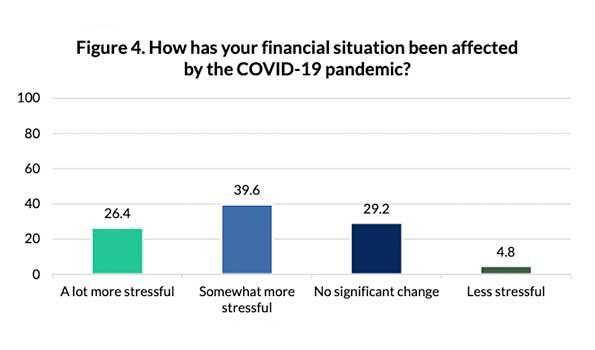
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2023, April 10). Anxiety and Depression Among College Students. https://ivypanda.com/essays/anxiety-and-depression-among-college-students/
"Anxiety and Depression Among College Students." IvyPanda , 10 Apr. 2023, ivypanda.com/essays/anxiety-and-depression-among-college-students/.
IvyPanda . (2023) 'Anxiety and Depression Among College Students'. 10 April.
IvyPanda . 2023. "Anxiety and Depression Among College Students." April 10, 2023. https://ivypanda.com/essays/anxiety-and-depression-among-college-students/.
1. IvyPanda . "Anxiety and Depression Among College Students." April 10, 2023. https://ivypanda.com/essays/anxiety-and-depression-among-college-students/.
Bibliography
IvyPanda . "Anxiety and Depression Among College Students." April 10, 2023. https://ivypanda.com/essays/anxiety-and-depression-among-college-students/.
- Incorporating Technology in Science Curriculum
- The Targeting Market of the Sustainable Coffee Shop
- Academic Writing: Flipped Classroom Method
- Racism: Healthcare Crisis and the Nurses Role
- The African American Women Leadership in Higher Education
- Undiscovered Killers: The Ineffectiveness of Zero-Tolerance Policies
- Fear associated with sexuality issues in society
- Mean-Variance Skewness Portfolio Performance Gauging
- Medication and Preventive Systems
- How Cognitive Behavioral Therapy Benefits Children
- Defense Mechanisms and Brain Structure
- Coping with Stress and Physical Health Problems
- Quality of Life With Schizophrenia
- Schizophrenia: The Etiology Analysis
- Schizophrenia as a Chronic Mental Disorder
‘Boys are disappearing’ from mental health care as signs of depression go undetected

Teenage boys are drowning in just as much of the depression and anxiety that’s been well documented in girls . Experts warn that many young men struggling with their mental health are left undetected and without the help they need.
“We are right to be concerned about girls,” said Kathleen Ethier, director of the Division of Adolescent and School Health at the Centers for Disease Control and Prevention. “But I don’t ever want us to lose sight of the fact that boys aren’t doing well, either.”
Depression in boys may go unnoticed, Ethier and other experts said, because boys usually don’t show it through signs of melancholy typically found in girls.
“We have this very classic understanding of depression as being sad, being tearful, crying more, not eating as much and losing weight,” said Dr. Lauren Teverbaugh, pediatrician and child psychiatrist at Tulane University in New Orleans. “That’s just not how it looks for a lot of young boys.”
‘Boys are disappearing’
A recent study published in the journal Pediatrics found that while antidepressant prescriptions have risen dramatically for teenage girls and women in their 20s, the rate of such prescriptions for young men “declined abruptly during March 2020 and did not recover.”
Dr. Kao-Ping Chua, a pediatrician at the Susan B. Meister Child Health Evaluation and Research Center at the University of Michigan, led the study. He said that his finding that boys weren’t accessing antidepressant medications once the pandemic hit has been “perplexing.”
“In males, it’s theoretically possible that this reflects improved mental health, but I’m struggling with that explanation,” Chua said. “Given that everybody’s mental health got worse, I would have expected that boys’ antidepressant dispensing would have at least remained stable, not decrease.”
The more likely explanation in Chua’s experience as a pediatrician, he said, was that boys stopped engaging with the health care system overall during the pandemic, leading to an underdetection and, consequently, an undertreatment of mental health problems in young men.
“There was something happening to make male adolescents not come in for mental health,” Chua said. “They didn’t go to their doctors. They skipped physicals.”
“Boys are disappearing,” he said.
What does depression look like in boys?
Boys struggling with their mental health tend to show it with a shorter fuse: They’re easily irritated, frustrated or aggressive.
“A lot of times, parents who have boys with depression say that they’re walking on eggshells around them because they don’t know what would set them off,” said Dr. Mai Uchida, a pediatric psychiatrist and director of the Child Depression Program at Massachusetts General Hospital.
Parents, pediatricians and even psychiatrists may not pick up on mental health problems in boys, Uchida said, because “they don’t fit the stereotypical image of depression.”
Women have long been much more likely to be diagnosed with depression than men. But a 2013 study found that when “irritability” is considered a main symptom, the rate of depression actually equalized between the sexes: 30.6% of men and 33.3% of women.
In addition to irritability, depression symptoms in boys can include impulsivity, risk-taking behavior and being more argumentative than usual.
Dr. Willough Jenkins, a psychiatrist and the medical director of emergency and consultation liaison psychiatry at Rady Children’s Hospital in San Diego, blamed, in part, a societal normalization of teenage angst and irritability.
“There’s a myth that teenagers are supposed to be irritable, that they’re supposed to be cranky,” she said. “I think too many parents have heard that and think it’s normal behavior, when it’s really indicating that there could be a struggle.”
Evidence of mental health distress among teens — especially young girls — has been mounting for years. Covid-19 lockdowns worsened the situation.
In 2023, a sobering report from the CDC revealed that girls experienced unprecedented levels of sadness and hopelessness early in the pandemic.
The research might indicate that boys don’t require the same level of mental health care as girls. That’s not true, experts insist.
“Both boys and girls are struggling,” Jenkins said. “None of our young people are doing well in terms of their mental health.”
‘Anger caused by sadness’
Eighteen-year-old Noah Power, who lives in Yukon, Canada, said his struggles with anxiety and depression began when he was about 12 years old.

His mental health symptoms first took the form of headaches and crushing pressure in his chest. Over time, those symptoms developed into a “rush of anger that I couldn’t explain,” he said. “It was like anger caused by sadness.”
Power said that expressing himself through anger and irritability felt like a natural, healthy outlet.
“It can be a bit much, but for us, we feel like we’re doing something good for our own brain,” he said.
In addition to long-term psychotherapy and medication, Power has relied on physical outlets for his anxiety and depression. Running, he said, is key.
“Being able to run and run and run and get all of my energy out has been the most helpful thing for me,” Power said. “You sweat out all of your energy.”
Lockdowns led to fewer referrals
Teachers, coaches and other caregivers outside of the home are on the front lines of monitoring teen mental health, Tulane’s Teverbaugh said.
“Not only do they see that child, but they see other children their same age also experiencing some of the same environmental factors,” she said. “They’re a really good measure for being able to pick up on something that is beyond the norm.” Teverbaugh and other experts said that many referrals for boys seeking mental health treatment stem from behavioral issues in school.
When schools went remote and sports and other activities were canceled in 2020, those referrals decreased.
“We’re often not seeing [boys] in the office, because it’s just not being picked up as much in the community,” she said.
Advice for parents
Mass General’s Uchida — a mother of three young boys — encourages parents to permit sons to express their sadness and frustrations.
“We have to really allow them to feel that and hold their hand and appreciate that they are expressing that kind of emotion,” she said. “They’re going through a lot. We often forget to empathize with them.”
Power said that having a parent or caregiver calmly listen, even during verbal outbursts, is helpful. “What we really, really appreciate is the listening and being able to just vent,” he said. “Just getting it all out is a huge relief.”
And if teenage boys can’t find the words to express themselves, allow them other outlets.
“They may not use emotional language like, ‘I feel sad,’” Teverbaugh said. “But when they’re playing their video games together, or they’re on the basketball court just goofing around, that’s engagement. That’s social interaction. That’s them being able to feel connected.”
Power also credits online gaming as a coping skill. “It’s an easy way to talk to your friends and have a good time,” he said. “Face-to-face social pressure can be a lot, especially when you’re going through something and you don’t want to break down in front of the person.”
Erika Edwards is a health and medical news writer and reporter for NBC News and "TODAY."
How to Manage Anxiety and Depression When You Have Kidney Cancer

W hen Katie Coleman was diagnosed at age 29 with a softball-sized tumor on her right kidney and a host of smaller growths in her liver, she was stunned. That astonishment quickly gave way to feelings of hopelessness. “I felt like my entire world was being pulled out from under me,” Coleman, now 32, says. “I went into a very dark spiral.”
Though her surgeon removed all the tumors, it wasn’t clear what her long- or even short- term prognosis was. What she found on the internet just freaked her out more. “One night I spiraled so deep I didn’t know whether life was worth living anymore.”
Coleman knew she needed help dealing with her depression and anxiety, but she didn’t form a strong connection with any of the therapists she met with . “I never found one who really understood what it was like to be 29 and looking fate in the face,” the software engineer from Austin says.
At her darkest point, Coleman started browsing Instagram posts, “looking for anyone who had what I had,” she remembers. “I needed to see someone else who was still alive.”
She eventually found a match, a man in the U.K. She wrote to him: “I’m sorry to be a random stranger on the internet. I was hoping you would share your story.”
The next morning, she discovered a stream of voice memos from someone with a British accent. “First, you need to get the idea of dying out of your mind,” the voice said.
“He told me how full of a life he felt he was living,” Coleman says. “It was the first time I connected with another patient and the amount of hope it brought me is indescribable.”
Coleman started putting together her own internet-based support group. “Folks pulled me out of some very dark places,” she says. “I always had someone to go to to talk things over.”
The value of short-term goals
The National Cancer Institute estimates that there were nearly 82,000 new kidney cancer diagnoses in 2023. Anywhere from 10% to 50% develop symptoms of anxiety and/or depression after diagnosis, experts say.
Because of that, many cancer centers have added psychiatrists, psychologists, and counselors to their treatment teams. “Anxiety and depression are common complications in oncology,” says Dr. Jon Levenson, an associate professor of psychiatry at the Columbia University Vagelos College of Physicians and Surgeons. “One major stressor is the uncertainty about the course their cancer will take. Patients may have surgery to remove the cancer and be physically asymptomatic for many months, or even longer, but still know there’s a high likelihood of recurrence.”
More From TIME
The stress from all that uncertainty can ramp up to full blown depression and/or anxiety, Levenson says.
For Coleman, the uncertainty was initially paralyzing. “At 29, I was very ambitious,” she says. “I was used to setting long-term goals. Now I didn’t know what next week would look like.”
But Coleman found a way to cope. She started to concentrate on short-term goals—small ones that she could accomplish in the three months between scans. Early on she set a goal of designing a health records app that could help others with cancer keep track of their care. She accomplished that in one of the three-month periods between scans. As time went on and her scans remained clear, Coleman decided to take a chance and started writing a memoir.
Read More: 7 Myths About Kidney Cancer, Debunked
Talking helps—but don’t share everything with everyone
Support groups of any kind can make a person with cancer feel less alone, says Shannon La Cava, director of the Simms-Mann/UCLA Health Center for Integrative Oncology. Sometimes patients say they don’t want to attend a support group, but “I say try two or three sessions,” she adds. “A lot of times after dipping a toe in people say ‘Oh wow, finding people like me gave me a lot of support.’”
That doesn’t mean patients need to share everything with everyone.
Patients often struggle with questions of “who to tell, when to tell, and what to tell,” says Dr. Asher Aladjem, medical director of psychological services at the NYU Langone Perlmutter Cancer Center. “If it makes a patient more anxious to have everybody involved in their experience, I advise them to be very selective about who to tell. I tell patients, ‘Pick a small group of people to tell and choose how much detail you want to give.’”
Aladjem says he tries to help patients draw boundaries and stick with them. In some cases, that may mean telling people you’d rather talk about something enjoyable, like movies.
It’s important, Aladjem says, for patients “to maintain control over what their experience is. There’s already a sense of loss of control with the illness. I think empowerment is very important.”
On the other end of the spectrum, some patients don’t want to talk to anyone.
When Travis Ferguson was diagnosed with kidney cancer at age 40, he kept everything to himself. While he felt empowered enough to leave the medical center in Indiana where he was diagnosed to seek care at a center that specialized in cancer, Fox Chase Cancer Center in Philadelphia, he didn’t know what to do with his fears, anxiety, and depression.
“When I first found out, I went into a real depressive state because I have two grandparents who died from cancer,” he remembers. “It felt like a death sentence. I thought talking about it would make it even more real.”
Although Ferguson had a therapist he’d been seeing to figure out how to deal with some other big life changes, including a recent breakup with his girlfriend, he initially didn’t bring up cancer during their sessions. “I finally brought it up with her because I realized I needed help,” he says. “I had been sliding deeper and deeper into the abyss.”
The therapist increased the dosages of the anxiety and depression medications he was already taking. Then she pushed him to start talking to his family. “They helped tremendously,” says Ferguson, now 41.
Read More: The Latest Breakthroughs That Could Improve Kidney Cancer Treatment
Who am I now?
As Jay Wells knows, the diagnosis can steal a patient’s sense of self. He’d been a park ranger for 30 years and saw himself as a rescuer of others until he was diagnosed with advanced kidney cancer at 68.
“I went from feeling strong and invincible to weak and fragile overnight,” says Wells, now 72. “I had been in a profession that was counted on to go in and rescue people in a bind, after a climbing accident or falling into a river. Now the roles were reversed. Everything was out of my control. It was a hard adjustment.”
Wells started worrying about dying and how his death would impact his wife. “She couldn’t take care of the house and 11 acres alone,” he says. “And who was going to take care of my dog?”
Depression and anxiety set in. At first, Wells resisted going to see a therapist. Then, “I started showing signs of depression,” he remembers. “I’d start thinking about stuff, and sometimes I’d break out crying in front of my wife, and even good friends. They could see I was in emotional pain.”
Eventually, Wells took the advice of those who loved him. He found a therapist who specialized in treating patients with cancer. “She suggested a bunch of things that helped, like meditation and breathing exercises to calm my anxiety. She had me do exercises where I would write about my fears of dying, what I was leaving undone, who I would leave behind, and how I would want to be remembered.”
The writing and conversations with the therapist made a big difference. “It was a way of getting at the anxiety and fears that were lurking just below the surface,” says Wells, who now lives in Ashland, Oregon. “Though it seemed like every time emotions were evoked that choked me up, I felt so much better afterwards.”
A kidney cancer diagnosis often comes as a shock because there haven’t been any obvious symptoms, says Dr. George Schade, a surgeon, associate professor at the University of Washington, and physician with the Fred Hutchinson Cancer Center in Seattle. So it shouldn’t be a surprise that many are shaken by it, he says, adding that some 70% to 80% of patients experience symptoms of anxiety and/or depression.
Those who need help with their emotional distress are generally referred to in-house team members, Schade says. But many patients don’t live close enough for weekly or biweekly appointments. “Patients might be five minutes away or from Alaska or Montana,” Schade says. “So telemedicine has been a huge game changer for us.”
Not every cancer center has mental health professionals on their teams, which means patients need to seek help in their local community, says Dr. Rafael Tamargo, an assistant professor in the department of psychiatry and behavioral sciences at Vanderbilt University Medical Center.
Unfortunately, there is a nationwide shortage of people in these professions now.
While patients look for someone, Tamargo recommends a few self-help methods—such as breathing techniques —to calm anxiety and soothe depression. For example, he suggests an exercise where one breathes slowly through the nose for four seconds, then holds their breath for four, then exhales through the mouth for four, and then waits another four before repeating.
Another way to calm down, he says, is to lie on your back with your eyes closed on a flat surface with your legs and arms extended. Then starting with your toes and working up to your head, focus on relaxing the muscles in each area until they go limp.
Another technique: Imagining a calm scene, such as a babbling brook, and hearing the sound of it and the scent of the surrounding grass, can also bring relaxation.
These kinds of techniques occasionally come in handy for Wells, the senior in Oregon. Even though he’s O.K. much of the time, there’s still some lingering anxiety lurking below the surface. “Before I go to see one of my doctors, or the dentist, or even an eye doctor, I can feel the anxiety building in me,” he says. “Sometimes I use the techniques I learned. I do a breathing exercise and think, ‘Wait a minute, Jay, this is nothing. Just calm down.’”
More Must-Reads From TIME
- Jane Fonda Champions Climate Action for Every Generation
- Biden’s Campaign Is In Trouble. Will the Turnaround Plan Work?
- Why We're Spending So Much Money Now
- The Financial Influencers Women Actually Want to Listen To
- Breaker Sunny Choi Is Heading to Paris
- Why TV Can’t Stop Making Silly Shows About Lady Journalists
- The Case for Wearing Shoes in the House
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]
You May Also Like
People with depression see no immediate change from common GP assessment, study shows
But phq-9 questionnaire used to monitor primary care patients did reveal benefits across six months.
A commonly used questionnaire adopted by GPs to monitor the treatment of depression does not provide any immediate benefits to patients, a new study has found.
Primary care researchers testing the PHQ-9 assessment, which measures the severity of depression, found it did nothing to improve people's symptoms after 12 weeks.
Doctors use the forms to assess depression and recommend appropriate treatments.
The study by the University of Southampton did, however, reveal that patients reported a better quality of life at six months if they completed the PHQ-9 consistently.
Findings from the four-year investigation, conducted with the University of Liverpool and University College London, are published in the British Journal of General Practice.
Professor of Primary Care Tony Kendrick, from Southampton, said current evidence that PHQ-9s improve the management of depression for patients in primary care is inconsistent.
He added: "Our study shows that people who tracked their PHQ-9 scores reported significantly improved overall wellbeing across a longer period of about six months.
"It also showed that a benefit for depression at six months could not be ruled out.
"Despite this, asking GPs to use these tools more regularly in primary care remains a challenge -- particularly as patients struggle to book appointments at their surgeries."
Monitoring with patient-reported outcome measures, or PROMS, is recommended by NICE and they are used regularly by psychologists in NHS Talking Therapies as well doctors in Europe and the USA.
The Southampton study enrolled more than 500 adults with depression treated in GP practices -- half the patients received the PHQ-9 questionnaire twice.
After 12 weeks, there was no significant difference in depression scores between the groups.
But, after 26 weeks, those who received the questionnaire reported a better quality of life and improved on some measures of anxiety and depression.
Those with GP-recorded follow up PHQ-9 scores were also more likely to be prescribed antidepressants and to see a mental health professional.
Prof Kendrick added: "More research into PROMs is needed but clearly patients who were monitored using PHQ-9s showed some improvements at six months.
"Self-assessment tools like the PHQ-9 are still well valued by many GPs and patients for monitoring depression treatment.
"We would like to see future studies test PROMs which are automatically administered and integrated into patients' records, and which create more specific recommendations for treatment, possibly using artificial intelligence."
- Mental Health Research
- Patient Education and Counseling
- Today's Healthcare
- Wounds and Healing
- Mental Health
- Postpartum depression
- Environmental impact assessment
- Clinical depression
- Antidepressant
- Bipolar disorder
- Deep brain stimulation
- Hyperthyroidism
Story Source:
Materials provided by University of Southampton . Note: Content may be edited for style and length.
Journal Reference :
- Tony Kendrick, Christopher Dowrick, Glyn Lewis, Michael Moore, Geraldine Leydon, Adam W A Geraghty, Gareth Griffiths, Shihua Zhu, Guiqing Yao, Carl May, Mark Gabbay, Rachel Dewar-Haggart, Samantha Williams, Lien Bui, Natalie Thompson, Lauren Bridewell, Emilia Trapasso, Tasneem Patel, Molly McCarthy, Naila Khan, Helen Page, Emma Corcoran, Jane Sungmin Hahn, Molly Bird, Mekeda X Logan, Brian Chi Fung Ching, Riya Tiwari, Anna Hunt, Beth Stuart. Depression follow-up monitoring with the PHQ-9: open cluster-randomised controlled trial . British Journal of General Practice , 2024; BJGP.2023.0539 DOI: 10.3399/BJGP.2023.0539
Cite This Page :
Explore More
- Illuminating Oxygen's Journey in the Brain
- DNA Study IDs Descendants of George Washington
- Heart Disease Risk: More Than One Drink a Day
- Unlocking Supernova Stardust Secrets
- Why Do Some Memories Become Longterm?
- Cell Division Quality Control 'Stopwatch'
- What Controls Sun's Differential Rotation?
- Robot, Can You Say 'Cheese'?
- Researchers Turn Back the Clock On Cancer Cells
- Making Long-Term Memories: Nerve-Cell Damage
Trending Topics
Strange & offbeat.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Psychiatry
Family and Academic Stress and Their Impact on Students' Depression Level and Academic Performance
1 School of Mechatronics Engineering, Daqing Normal University, Daqing, China
2 School of Marxism, Heilongjiang University, Harbin, China
Jacob Cherian
3 College of Business, Abu Dhabi University, Abu Dhabi, United Arab Emirates
Noor Un Nisa Khan
4 Faculty of Business Administration, Iqra University Karachi Pakistan, Karachi, Pakistan
Kalpina Kumari
5 Faculty of Department of Business Administration, Greenwich University Karachi, Karachi, Pakistan
Muhammad Safdar Sial
6 Department of Management Sciences, COMSATS University Islamabad (CUI), Islamabad, Pakistan
Ubaldo Comite
7 Department of Business Sciences, University Giustino Fortunato, Benevento, Italy
Beata Gavurova
8 Faculty of Mining, Ecology, Process Control and Geotechnologies, Technical University of Kosice, Kosice, Slovakia
József Popp
9 Hungarian National Bank–Research Center, John von Neumann University, Kecskemét, Hungary
10 College of Business and Economics, University of Johannesburg, Johannesburg, South Africa
Associated Data
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Current research examines the impact of academic and familial stress on students' depression levels and the subsequent impact on their academic performance based on Lazarus' cognitive appraisal theory of stress. The non-probability convenience sampling technique has been used to collect data from undergraduate and postgraduate students using a modified questionnaire with a five-point Likert scale. This study used the SEM method to examine the link between stress, depression, and academic performance. It was confirmed that academic and family stress leads to depression among students, negatively affecting their academic performance and learning outcomes. This research provides valuable information to parents, educators, and other stakeholders concerned about their childrens' education and performance.
Introduction
Higher education institutions (HEIs) are believed to be one of the strongest pillars in the growth of any nation ( 1 ). Being the principal stakeholder, the performance of HEIs mainly relies on the success of its students ( 2 ). To successfully compete in the prevailing dynamic industrial environment, students are not only supposed to develop their knowledge but are also expected to have imperative skills and abilities ( 3 ). In the current highly competitive academic environment, students' performance is largely affected by several factors, such as social media, academic quality, family and social bonding, etc. ( 4 ). Aafreen et al. ( 2 ) stated that students continuously experience pressure from different sources during academic life, which ultimately causes stress among students.
Stress is a common factor that largely diminishes individual morale ( 5 ). It develops when a person cannot handle their inner and outer feelings. When the stress becomes chronic or exceeds a certain level, it affects an individual's mental health and may lead to different psychological disorders, such as depression ( 6 ). Depression is a worldwide illness marked by feelings of sadness and the inability to feel happy or satisfied ( 7 ). Nowadays, it is a common disorder, increasing day by day. According to the World Health Organization ( 8 , 9 ), depression was ranked third among the global burden of disease and predicted to take over first place by 2030.
Depression leads to decreased energy, difficulty thinking, concentrating, and making career decisions ( 6 ). Students are a pillar of the future in building an educated society. For them, academic achievement is a big goal of life and can severely be affected if the students fall prey to depression ( 10 , 11 ). There can be several reasons for this: family issues, exposure to a new lifestyle in colleges and universities, poor academic grades, favoritism by teachers, etc. Never-ending stress or academic pressure of studies can also be a chief reason leading to depression in students ( 12 ). There is a high occurrence of depression in emerging countries, and low mental health literacy has been theorized as one of the key causes of escalating rates of mental illness ( 13 ).
Several researchers, such as ( 6 , 14 , 15 ) have studied stress and depression elements from a performance perspective and reported that stress and depression negatively affect the academic performance of students. However, Aafreen et al. ( 2 ) reported contradictory results and stated that stress sharpens the individual's mind and reflexes and enables workers to perform better in taxing situations. Ardalan ( 16 ) conducted a study in the United States (US). They reported that depression is a common issue among students in the US, and 20 percent of them may have a depressive disorder spanning 12 months or more. It affects students' mental and physical health and limits their social relationships and professional career.
However, the current literature provides mixed results on the relationship between stress and performance. Therefore, the current research investigates stress among students from family and academic perspectives using Lazaru's theory which describes stress as a relation between an individual and his environment and examines how it impacts students' depression level, leading to their academic performance. Most of the available studies on stress and depression are from industrial perspectives, and limited attention is paid to stress from family and institutional perspectives and examines its impact on students' depression level, leading to their academic performance, particularly in Pakistan, the place of the study. Besides, the present study follows a multivariate statistical technique, followed by structural equation modeling (SEM) to examine the relationship between stated variables which is also a study's uniqueness.
This paper is divided into five main sections. The current section provided introduction, theoretical perspective, and background of the study. In the second section, a theoretical framework, a detailed literature review and research hypotheses of the underlying relationships are being proposed. In the third and fourth section, methodology and analysis have been discussed. Finally, in the last section, the conclusion, limitations, implications, and recommendations for future research have been proposed.
Theory and Literature
The idea of cognitive appraisal theory was presented in 1966 by psychologist Richard Lazarus in Psychological Stress and Coping Process. According to this theory, appraisal and coping are two concepts that are central to any psychological stress theory. Both are interrelated. According to the theory, stress is the disparity between stipulations placed on the individuals and their coping resources ( 17 ). Since its first introduction as a comprehensive theory ( 18 ), a few modifications have been experienced in theory later. The recent adaptation states that stress is not defined as a specific incitement or psychological, behavioral, or subjective response. Rather, stress is seen as a relation between an individual and his environment ( 19 ). Individuals appraise the environment as significant for their well-being and try to cope with the exceeding demands and challenges.
Cognitive appraisal is a model based on the idea that stress and other emotional processes depend on a person's expectancies regarding the significance and outcome of an event, encounter, or function. This explains why there are differences in intensity, duration, and quality of emotions elicited in people in response to the environment, which objectively, are equal for all ( 18 ). These appraisals may be influenced by various factors, including a person's goals, values, motivations, etc., and are divided into primary and secondary appraisals, specific patterns of which lead to different kinds of stress ( 20 ). On the other hand, coping is defined as the efforts made by a person to minimize, tolerate, or master the internal and external demands placed on them, a concept intimately related to cognitive appraisal and, therefore, to the stress-relevant person-environment transactions.
Individuals experience different mental and physiological changes when encountering pressure, such as stress ( 21 , 22 ). The feelings of stress can be either due to factors in the external environment or subjective emotions of individuals, which can even lead to psychological disorders such as anxiety and depression. Excess stress can cause health problems. A particularly negative impact has been seen in students due to the high level of stress they endure, affecting their learning outcomes. Various methods are used to tackle stress. One of the methods is trying to pinpoint the causes of stress, which leads us to different terms such as family stress and academic stress. The two factors, stress and depression, have greatly impacted the students' academic performances. This research follows the Lazarus theory based on stress to examine the variables. See the conceptual framework of the study in Figure 1 .

Conceptual framework.
Academic Stress
Academic issues are thought to be the most prevalent source of stress for college students ( 23 ). For example, according to Yang et al. ( 24 ), students claimed that academic-related pressures such as ongoing study, writing papers, preparing for tests, and boring professors were the most important daily problems. Exams and test preparation, grade level competitiveness, and gaining a big quantity of knowledge in a short period of time all contribute to academic pressure. Perceived stress refers to a condition of physical or psychological arousal in reaction to stressors ( 25 , 26 ). When college students face excessive or negative stress, they suffer physical and psychological consequences. Excessive stress can cause health difficulties such as fatigue, loss of appetite, headaches, and gastrointestinal issues. Academic stress has been linked to a variety of negative effects, including ill health, anxiety, depression, and poor academic performance. Travis et al. ( 27 ), in particular, discovered strong links between academic stress and psychological and physical health.
Family Stress
Parental participation and learning effect how parents treat their children, as well as how they handle their children's habits and cognitive processes ( 28 ). This, in turn, shapes their children's performance and behaviors toward them. As a result, the parent-child relationship is dependent on the parents' attitudes, understanding, and perspectives. When parents have positive views, the relationship between them and their children will be considerably better than when they have negative attitudes. Parents respond to unpleasant emotions in a variety of ways, which can be classified as supportive or non-supportive ( 29 ). Parents' supportive reactions encourage children to explore their emotions by encouraging them to express them or by assisting them in understanding and coping with an emotion-eliciting scenario. Non-supportive behaviors, such as downplaying the kid's emotional experience, disciplining the child, or getting concerned by the child's display, transmit the child the message that expressing unpleasant emotions is inappropriate and unacceptable. Supportive parental reactions to unpleasant emotions in children have been linked to dimensions of emotional and social competence, such as emotion comprehension and friendship quality. Non-supportive or repressive parental reactions, on the other hand, have been connected to a child's stored negative affect and disordered behaviors during emotion-evoking events, probably due to an inability or unwillingness to communicate unpleasant sentiments ( 30 , 31 ).
Academic Stress and Students' Depression Levels
Generally, it is believed that mental health improves as we enter into adulthood, and depression disorder starts to decline between the age of 18 and 25. On the other hand, excessive depression rates are the highest pervasiveness during this evolution ( 15 ), and many university students in the particular screen above clinical cut-off scores for huge depression ( 14 , 32 ). Afreen et al. ( 2 ) stated that 30% of high school students experience depression from different perspectives. This means a major chunk of fresh high school graduates are more likely to confront depression or are more vulnerable to encountering depression while enrolling in the university. As the students promote to a higher level of education, there are many factors while calculating the stress like, for example, the syllabus is tough to comprehend, assignments are quite challenging with unrealistic deadlines, and accommodation problems for the students who are shifted from other cities, etc. ( 33 ). Experiences related to university can also contribute while studying depression. The important thing to consider is depression symptoms vary from time to time throughout the academic years ( 34 ); subjective and objective experiences are directly connected to the depression disorder ( 6 ), stress inherent in the university situation likely donates to the difference in university students' depressing experiences.
Stress negatively impacts students' mental peace, and 42.3% of students of Canadian university respondents testified devastating levels of anxiety and stress ( 35 , 36 ). Moreover, there were (58.1%) students who stated academic projects are too tough to handle for them. In Germany, Bulgaria, and Poland, a huge sample of respondents consider assignments a burden on their lives that cannot stand compared to relationships or any other concern in life ( 14 ).
In several countries, university students were studied concerning stress, and results show that depression disorder and apparent anxiety are correlated to educational needs and demands ( 37 ). In their cross-sectional study conducted on a sample of 900 Canadian students, Lörz et al. ( 38 ) concluded that strain confronted due to academic workload relatively has high bleak symptoms even after controlling 13 different risk affecting factors for depression (e.g., demographic features, abusive past, intellectual way, and personality, currently experienced stressful trials in life, societal support). Few have exhibited that students who are tired of educational workload or the students who name them traumatic tend to have more depressing disorders ( 15 ).
These relations can be described by examining the stress and coping behaviors that highlight the role of positive judgments in the stress times ( 39 ), containing the Pancer and colleagues' university modification framework ( 40 , 41 ). The evaluation concept includes examining the circumstances against the available resources, for instance, the effectiveness of coping behavior and societal support. As per these frameworks, if demand is considered unapproachable and resources are lacking, confronted stress and interrelated adverse effects will be high, conceivably giving birth to difficulties in an adjustment like mental instability. Stress triggering situations and the resources in the educational area led to excessive workload, abilities, and study and enhanced time managing skills.
Sketching the overall evaluation frameworks, Pancer et al. ( 40 ) established their framework to exhibit the constructive and damaging adjustment results for the university students dealing with the academic challenges. They stated that while students enroll in the university, they evaluate all the stress-related factors that students confront. They consider them manageable as long as they have sufficient resources. On the other hand, if the available resources do not match the stress factors, it will surely result in a negative relationship, which will lead students to experience depression for sure. Based on the given arguments, the researcher formulates the following hypothesis:
- H1: Increased academic stress results in increased depression levels in students.
Family Stress and Students' Depression Levels
According to Topuzoglu et al. ( 42 ), 3% to 16.9% of individuals are affected by depression worldwide. There are fewer chances for general people to confront depression than university students ( 43 , 44 ). In Mirza et al.'s ( 45 ) study, 1/3 of students encounter stress and depression (a subjective mean occurrence of 30.6%) of all participant students, which suggests students have a 9% higher rate of experiencing depression than general people. Depression can destroy life; it greatly impacts living a balanced life. It can impact students' personal and social relationships, educational efficiency, quality of life, affecting their social and family relationships, academic productivity, and bodily operations ( 46 , 47 ). This declines their abilities, and they get demotivated to learn new things, resulting in unsatisfactory performances, and it can even result in university dropouts ( 48 ). Depression is a continuous substantial risk aspect for committing suicide for university students ( 49 ); thus, it is obliged to discover the factors that can give rise to students' depression.
Seventy-five percentage of students in China of an intermediate school are lucky enough to enroll in higher education. The more students pursue higher education, the more they upsurge for depression (in 2002, the depression rate was 5 to 10%, 2011 it rises 24 to 38%) ( 5 ). Generally, University students' age range is late teens to early twenties, i.e., 18–23 years. Abbas ( 50 ) named the era of university students as “post-adolescence. Risk factors for teenage depression have several and complicated problems of individual characteristics and family and educational life ( 51 ). Amongst the huge depression factors, relationship building with family demands a major chunk of attention and time since factors like parenting and family building play an important role in children's development ( 52 , 53 ). Halonen et al. ( 54 ) concluded that factors like family binding play a major role in development, preservation, and driving adolescent depression. Generally speaking, depressed teenagers tend to have a weaker family relationship with their parents than non-depressed teenagers.
There are two types of family risk factors, soft and hard. Hard factors are encountered in families with a weak family building structure, parents are little to no educated at all, and of course, the family status (economically). Several studies have proved that students of hard risk factors are more likely to encounter depression. Firstly, students from broken families have low confidence in every aspect of life, and they are weak at handling emotional breakdowns compared to students from complete and happy families ( 55 – 57 ). Secondly, the university students born in educated families, especially mothers (at least a college degree or higher degree), are less likely to confront depression than the university students born in families with little to no educated families. Secondly, children born with educated mothers or mothers who at least have a college degree tend to be less depressive than the children of less-educated mothers ( 58 ). However, Parker et al. and Mahmood et al. ( 59 , 60 ) stated a strong relationship between depression and mothers with low literacy levels.
On the other hand, Chang et al. ( 46 ) couldn't prove the authentication of this relationship in university students. Thirdly, university students who belong to lower class families tend to have more unstable mental states and are more likely to witness depression than middle or upper-class families ( 61 ). Jadoon et al. and Abbas et al. ( 62 , 63 ) said that there is no link between depression and economic status. Their irrelevance can be because medical students often come from educated and wealthy families and know their jobs are guaranteed as soon as they graduate. Therefore, the relationship between the hard family environment and depression can be known by targeting a huge audience, and there are several factors to consider while gauging this relationship.
The soft family environment is divided into clear factors (parenting style example, family guidelines, rules, the parent with academic knowledge, etc.) and implied factors (family norm, parent-child relationship, communication within the family, etc.). The soft factor is the key factor within the family that cannot be neglected while studying the teenagers' mental state or depression. Families make microsystems within the families, and families are the reason to build and maintain dysfunctional behavior by multiple functional procedures ( 64 ). Amongst the soft family environmental factors, consistency and struggles can be helpful while forecasting the mental health of teenagers. The youth of broken families, family conflict, weak family relationships, and marital issues, especially unhappy married life, are major factors for youth depression ( 65 ). Ruchkin et al. ( 66 ) stated that African Americans usually have weak family bonding, and their teenagers suffer from depression even when controlling for source bias. Whereas, few researchers have stated, family unity is the most serious factor while foreseeing teenagers' depression. Eaton noted that extreme broken family expressions might hurt emotionality and emotional regulation ( 67 , 68 ).
Social circle is also considered while studying depression in teenagers ( 69 – 71 ). The traditional Pakistani culture emphasizes collectivism and peace and focuses on blood relations and sensitive sentiments. Adolescents with this type of culture opt to get inspired by family, but students who live in hostels or share the room with other students lose this family inspiration. This transformation can be a big risk to encounter depression ( 72 ). Furthermore, in Pakistan securing employment is a big concern for university students. If they want a good job in the future, they have to score good grades and maintain GPA from the beginning. They have to face different challenges all at once, like aggressive educational competition, relationships with peers and family, and of course the biggest employment stress all alone. The only source for coping with these pressures is the family that can be helpful for fundings. If the students do not get ample support the chances are of extreme depression. The following hypothesis is suggested:
- H2: Increased family stress level results in increased depression levels in students.
Students' Depression Levels and Students' Academic Performance
University students denote many people experiencing a crucial conversion from teenagers to adulthood: a time that is generally considered the most traumatic time in one's ( 73 ). This then gets accumulated with other challenges like changes in social circle and exams tension, which possibly puts students' mental health at stake. It has been concluded that one-third of students experience moderate to severe depression in their entire student life ( 74 ). This is the rate that can be increased compared to the general people ( 75 , 76 ). Students with limited social-class resources tend to be more helpless. Additionally, depressed students in attainable-focused environments (for instance, higher academic institutes) are likely to score lower grades with a sense of failure and more insufficient self-assurance because they consider themselves failures, find the world unfair, and have future uncertainties. Furthermore, students with low self-esteem are rigid to take on challenging assignments and projects, hence they are damaging their educational career ( 77 ).
Depression can be defined as a blend of physical, mental, bodily processes, and benightedness which can make themselves obvious by symptoms like, for example, poor sleep schedule, lack of concentration, ill thoughts, and state of remorse ( 78 , 79 ). But, even after such a huge number of depressions in students and the poor academic system, research has not explored the effect of depression on educational performance. A study has shown that the relationship between emotional stability and academic performance in university students and financial status directly results in poor exam performance. As the study further concluded, it was verified depression is an independent factor ( 80 ). Likewise, students suffering from depression score poor grades, but this relationship vanished if their depression got treated. Apart from confidence breaking, depression is a big failure for their academic life. Students with depression symptoms bunk more classes, assessments, and assignments. They drop courses if they find them challenging than non-depressed peers, and they are more likely to drop out of university completely ( 81 ). Students suffering from depression can become ruthless, ultimately affecting their educational performance and making them moody ( 82 ).
However, it has been stated that the association between anxiety and educational performance is even worse and ambiguous. At the same time, some comprehensive research has noted that the greater the anxiousness, the greater the student's performance. On the other hand, few types of research have shown results where there is no apparent relationship between anxiety and poorer academic grades ( 83 ). Ironically, few studies have proposed that a higher anxiety level may improve academic performance ( 84 , 85 ). Current research by Khan et al. ( 86 ) on the undergraduate medical students stated that even though the high occurrence of huge depression between the students, the students GPA is unharmed. Therefore, based on given differences in various research findings, this research is supposed to find a more specific and clear answer to the shared relationship between students' depression levels and academic performance. Based on the given arguments, the researcher formulates the following hypothesis:
- H3: Students' depression level has a significant negative effect on their academic performance.
Methodology
Target population and sampling procedure.
The target audience of this study contains all male and female students studying in the public, private, or semi-government higher education institutions located in Rawalpindi/Islamabad. The researchers collected data from undergraduate and postgraduate students from the management sciences, engineering, and computer science departments. The sampling technique which has been used is the non-probability sampling technique. A questionnaire was given to the students, and they were requested to fill it and give their opinion independently. The questionnaire is based on five points Likert scale.
However, stress and depression are the most common issue among the students, which affects their learning outcomes adversely. A non-probability sampling technique gathered the data from February 2020 to May 2020. The total questionnaires distributed among students were 220, and 186 responses were useful. Of which 119 respondents were females, 66 males, and 1 preferred not to disclose. See Table 1 for detailed demographic information of respondents.
Respondent's demographic profile.
Measurement Scales
We have divided this instrument into two portions. In the first section, there is demographic information of respondents. The second section includes 14 items based on family stress, academic stress, students' depression levels, and students' academic performance. Academic and family stress were measured by 3 item scale for each construct, and students' depression level and academic performance were measured by 4 item scale for each separate construct. The five-point Likert scale is used to measure the items, in which one signifies strongly disagree (S.D), second signifies disagree (D.A), third signifies neither agree nor disagree (N), fourth signifies agree (A.G), and the fifth signifies strongly agree (S.A). The questionnaire has been taken from Gold Berg ( 87 ), which is modified and used in the given questionnaire.
Data Analysis and Results
The researchers used the SEM technique to determine the correlation between stress, depression, and academic performance. According to Prajogo and Cooper ( 88 ), it can remove biased effects triggered by the measurement faults and shape a hierarchy of latent constructs. SPSS v.23 and AMOS v.23 have been used to analyze the collected data. Kaiser-Meyer-Olkin test is used to test the competence of the sample. The value obtained is 0.868, which fulfills the Kaiser et al. ( 89 ), a minimum requirement of 0.6. The multicollinearity factor was analyzed through the variance inflation factor (VIF). It shows the value of 3.648 and meets the requirement of Hair et al. ( 90 ), which is < 4. It also indicates the absence of multicollinearity. According to Schwarz et al. ( 91 ), common method bias (CMB) is quite complex in quantitative studies. Harman's test of a single factor has been used to analyze CMB. The result obtained for the single factor is 38.63%. As stated by Podsakoff et al. ( 92 ), if any of the factors gives value < 50% of the total variance, it is adequate and does not influence the CMB. Therefore, we can say that there is no issue with CMB. Considering the above results are adequate among the measurement and structural model, we ensure that the data is valued enough to analyze the relation.
Assessment of the Measurement and Structural Model
The association between the manifest factors and their elements is examined by measuring model and verified by the Confirmatory Factor Analysis (CFA). CFA guarantees legitimacy and the unidimensional of the measurement model ( 93 ). Peterson ( 94 ) stated that the least required, i.e., 0.8 for the measurement model, fully complies with its Cronbach's alpha value, i.e., 0.802. Therefore, it can confidently be deduced that this measurement model holds satisfactory reliability. As for the psychological legitimacy can be analyzed through factor loading, where the ideal loading is above 0.6 for already established items ( 95 ). Also, according to the recommendation of Molina et al. ( 96 ), the minimum value of the average variance extracted (AVE) for all results is supposed to be >0.5. Table 2 gives detail of the variables and their quantity of things, factor loading, merged consistency, and AVE values.
Instrument reliability and validity.
A discriminant validity test was performed to ensure the empirical difference of all constructs. For this, it was proposed by Fornell and Larcker ( 97 ) that the variance of the results is supposed to be greater than other constructs. The second indicator of discriminant validity is that the square root values of AVE have a greater correlation between the two indicators. Hair et al. ( 90 ) suggested that the correlation between the pair of predictor variables should not be higher than 0.9. Table 3 shows that discriminant validity recommended by Hair et al. ( 90 ) and Fornell and Larcker ( 97 ) was proved clearly that both conditions are fulfilled and indicates that the constructs have adequate discriminant validity.
Discriminant validity analysis.
Acd. Strs, Academic Stress; Fam. Strs, Family Stress; Std. Dep. Lev, Student's Depression Level; Std. Acd. Perf, Student's Academic Performance .
Kaynak ( 98 ) described seven indicators that ensure that the measurement model fits correctly. These indicators include standardized root mean squared residual (SRMR), root means a square error of approximation (RMSEA), comparative fit index (CFI), normative fit index (NFI), adjusted goodness of fit index (AGFI), the goodness of fit index (GFI) and chi-square to a degree of freedom (x 2 /DF). Tucker-Lewis's index (TLI) is also included to ensure the measurement and structural model's fitness. In the measurement model, the obtained result shows that the value of x 2 /DF is 1.898, which should be lower than 2 suggested by Byrne ( 99 ), and this value also meets the requirement of Bagozzi and Yi ( 100 ), i.e., <3. The RMSEA has the value 0.049, which fully meets the requirement of 0.08, as stated by Browne and Cudeck ( 101 ). Furthermore, the SRMR acquired value is 0.0596, which assemble with the required need of < 0.1 by Hu and Bentler ( 102 ). Moreover, according to Bentler and Bonett ( 103 ), McDonald and Marsh ( 104 ), and Bagozzi and Yi ( 100 ), the ideal value is 0.9, and the values obtained from NFI, GFI, AGFI, CFI, and TLI are above the ideal value.
Afterward, the structural model was analyzed and achieved the findings, which give the value of x 2 /DF 1.986. According to Browne and Cudeck ( 101 ), the RMSEA value should not be greater than 0.08, and the obtained value of RMSEA is 0.052, which meets the requirement perfectly. The minimum requirement of Hu and Bentler ( 102 ) should be <0.1, for the structural model fully complies with the SRMR value 0.0616. According to a recommendation of McDonald and Marsh ( 104 ) and Bagozzi and Yi ( 100 ), the ideal value must be up to 0.9, and Table 4 also shows that the values of NFI, GFI, AGFI, CFI, and TLI, which are above than the ideal value and meets the requirement. The above results show that both the measurement and structural models are ideally satisfied with the requirements and the collected data fits correctly.
Analysis of measurement and structural model.
Testing of Hypotheses
The SEM technique is used to examine the hypotheses. Each structural parameter goes along with the hypothesis. The academic stress (Acd. Strs) with the value β = 0.293 while the p -value is 0.003. These outcomes show a significant positive relationship between academic stress (Acd. Strs) and students' depression levels (Std. Dep. Lev). With the β = 0.358 and p = 0.001 values, the data analysis discloses that the family stress (Fam. Strs) has a significant positive effect on the students' depression level (Std. Dep. Lev). However, the student's depression level (Std. Dep. Lev) also has a significant negative effect on their academic performance (Std. Acd. Perf) with the values of β = −0.319 and p = 0.001. Therefore, the results supported the following hypotheses H 1 , H 2 , and H 3 . The sub-hypotheses analysis shows that the results are statistically significant and accepted. In Table 5 , the details of the sub-hypotheses and the principals are explained precisely. Please see Table 6 to review items with their mean and standard deviation values. Moreover, Figure 2 represents the structural model.
Examining the hypotheses.
Description of items, mean, and standard deviation.

Structural model.
Discussion and Conclusion
These findings add to our knowledge of how teenage depression is predicted by academic and familial stress, leading to poor academic performance, and they have practical implications for preventative and intervention programs to safeguard adolescents' mental health in the school context. The outcomes imply that extended academic stress positively impacts students' depression levels with a β of 0.293 and a p -value sof 0.003. However, according to Wang et al. ( 5 ), a higher level of academic stress is linked to a larger level of school burnout, which leads to a higher degree of depression. Satinsky et al. ( 105 ) also claimed that university officials and mental health specialists have expressed worry about depression and anxiety among Ph.D. students, and that his research indicated that depression and anxiety are quite common among Ph.D. students. Deb et al. ( 106 ) found the same results and concluded that depression, anxiety, behavioral difficulties, irritability, and other issues are common among students who are under a lot of academic stress. Similarly, Kokou-Kpolou et al. ( 107 ) revealed that depressive symptoms are common among university students in France. They also demonstrate that socioeconomic and demographic characteristics have a role.
However, Wang et al. ( 5 ) asserted that a higher level of academic stress is associated with a higher level of school burnout, which in return, leads to a higher level of depression. Furthermore, Satinsky et al. ( 105 ) also reported that university administrators and mental health clinicians have raised concerns about depression and anxiety and concluded in his research that depression and anxiety are highly prevalent among Ph.D. students. Deb et al. ( 106 ) also reported the same results and concluded that Depression, anxiety, behavioral problems, irritability, etc. are few of the many problems reported in students with high academic stress. Similary, Kokou-Kpolou et al. ( 107 ) confirmed that university students in France have a high prevalence of depressive symptoms. They also confirm that socio-demographic factors and perceived stress play a predictive role in depressive symptoms among university students. As a result, academic stress has spread across all countries, civilizations, and ethnic groups. Academic stress continues to be a serious problem impacting a student's mental health and well-being, according to the findings of this study.
With the β= 0.358 and p = 0.001 values, the data analysis discloses that the family stress (Fam. Strs) has a significant positive effect on the students' depression level (Std. Dep. Lev). Aleksic ( 108 ) observed similar findings and concluded that many and complicated concerns of personal traits, as well as both home and school contexts, are risk factors for teenage depression. Similarly, Wang et al. ( 109 ) indicated that, among the possible risk factors for depression, family relationships need special consideration since elements like parenting styles and family dynamics influence how children grow. Family variables influence the onset, maintenance, and course of juvenile depression, according to another study ( 110 ). Depressed adolescents are more likely than normal teenagers to have bad family and parent–child connections.
Conversely, students' depression level has a significantly negative impact on their academic performance with β and p -values of −0.319 and 0.001. According ( 111 ), anxiety and melancholy have a negative influence on a student's academic performance. Adolescents and young adults suffer from depression, which is a common and dangerous mental illness. It's linked to an increase in family issues, school failure, especially among teenagers, suicide, drug addiction, and absenteeism. While the transition to adulthood is a high-risk period for depression in general ( 5 ), young people starting college may face extra social and intellectual challenges that increase their risk of melancholy, anxiety, and stress ( 112 ). Students' high rates of depression, anxiety, and stress have serious consequences. Not only may psychological morbidity have a negative impact on a student's academic performance and quality of life, but it may also disturb family and institutional life ( 107 ). Therefore, long-term untreated depression, anxiety, or stress can have a negative influence on people's ability to operate and produce, posing a public health risk ( 113 ).
Theoretical Implications
The current study makes various contributions to the existing literature on servant leadership. Firstly, it enriches the limited literature on the role of family and academic stress and their impact on students' depression levels. Although, a few studies have investigated stress and depression and its impact on Students' academic performance ( 14 , 114 ), however, their background i.e., family and institutions are largely ignored.
Secondly, it explains how the depression level impacts students' academic learning, specifically in the Asian developing countries region. Though a substantial body of empirical research has been produced in the last decade on the relationship between students' depression levels and its impact on their academic achievements, however, the studies conducted in the Pakistani context are scarce ( 111 , 115 ). Thus, this study adds further evidence to prior studies conducted in different cultural contexts and validates the assumption that family and academic stress are key sources depression and anxiety among students which can lead toward their low academic grades and their overall performance.
This argument is in line with our proposed theory in the current research i.e., cognitive appraisal theory which was presented in 1966 by psychologist Richard Lazarus. Lazarus's theory is called the appraisal theory of stress, or the transactional theory of stress because the way a person appraises the situation affects how they feel about it and consequently it's going to affect his overall quality of life. In line with the theory, it suggests that events are not good or bad, but the way we think about them is positive or negative, and therefore has an impact on our stress levels.
Practical Implications
According to the findings of this study, high levels of depressive symptoms among college students should be brought to the attention of relevant departments. To prevent college student depression, relevant departments should improve the study and life environment for students, try to reduce the generation of negative life events, provide adequate social support for students, and improve their cognitive and coping capacities to improve their mental qualities.
Stress and depression, on the other hand, may be managed with good therapy, teacher direction, and family support. The outcomes of this study provide an opportunity for academic institutions to address students' psychological well-being and requirements. Emotional well-being support services for students at Pakistan's higher education institutions are lacking in many of these institutions, which place a low priority on the psychological requirements of these students. As a result, initiatives that consistently monitor and enhance kids' mental health are critical. Furthermore, stress-reduction treatments such as biofeedback, yoga, life-skills training, mindfulness meditation, and psychotherapy have been demonstrated to be useful among students. Professionals in the sector would be able to adapt interventions for pupils by understanding the sources from many spheres.
Counseling clinics should be established at colleges to teach students about stress and sadness. Counselors should instill in pupils the importance of positive conduct and decision-making. The administration of the school should work to create a good and safe atmosphere. Furthermore, teachers should assume responsibility for assisting and guiding sad pupils, since this will aid in their learning and performance. Support from family members might also help you get through difficult times.
Furthermore, these findings support the importance of the home environment as a source of depression risk factors among university students, implying that family-based treatments and improvements are critical in reducing depression among university students.
Limitations and Future Research Implications
The current study has a few limitations. The researcher gathered data from the higher education level of university students studying in Islamabad and Rawalpindi institutions. In the future, researchers are required to widen their region and gather information from other cities of Pakistan, for instance, Lahore, Karachi, etc. Another weakness of the study is that it is cross-sectional in nature. We need to do longitudinal research in the future to authoritatively assert the cause-and-effect link between academic and familial stress and their effects on students' academic performance since cross-sectional studies cannot establish significant cause and effect relationships. Finally, the study's relatively small sample size is a significant weakness. Due to time and budget constraints, it appears that the capacity to perform in-depth research of all firms in Pakistan's pharmaceutical business has been limited. Even though the findings are substantial and meaningful, the small sample size is predicted to limit generalizability and statistical power. This problem can be properly solved by increasing the size of the sample by the researchers, in future researches.
Data Availability Statement
Ethics statement.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
All authors contributed to conceptualization, formal analysis, investigation, methodology, writing and editing of the original draft, and read and agreed to the published version of the manuscript.
This work was funded by the 2020 Heilongjiang Province Philosophy and Social Science Research Planning Project on Civic and Political Science in Universities (Grant No. 20SZB01). This work is supported by the Scientific Grant Agency of the Ministry of Education, Science, Research, and Sport of the Slovak Republic and the Slovak Academy Sciences as part of the research project VEGA 1/0797/20: Quantification of Environmental Burden Impacts of the Slovak Regions on Health, Social and Economic System of the Slovak Republic.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
Authors would like to thank all persons who directly or indirectly participated in the completion of this manuscript.

IMAGES
VIDEO
COMMENTS
Depression and anxiety occur at a similar time. Anxiety is caused due to an overwhelming fear of an expected occurrence of an event that is unclear to a person. More than 25 million people globally are affected by anxiety disorders. People feel anxious in moments such as when making important decisions, before facing an interview panel, and ...
Research reveals that a wayward stress system attack on the brain can lead to depression. The legacy of our evolutionary and biological stress responses is a significant burden for humans today ...
Depression is a disorder characterized by prolonged periods of sadness and loss of interest in life. The symptoms include irritability, insomnia, anxiety, and trouble concentrating. This disorder can produce physical problems, self-esteem issues, and general stress in a person's life. Difficult life events and trauma are typical causes of ...
Psychological effects of stress. Stress can cause psychological and emotional distress. When it becomes chronic, it can increase your risk for anxiety and depression. Experiencing long-term ...
The link between stressful life events and the origin and development of depression has been widely investigated, providing an increasing body of evidence supporting this association. 1-3 Environmental factors likely affect individuals in somewhat different manners, therefore triggering an adaptive response to stress, which depends on both psychological and biological aspects in the ...
Abstract. Major depressive disorder is a serious mental disorder that profoundly affects an individual's quality of life. Although the aetiologies underlying this disorder remain unclear, an increasing attention has been focused on the influence imposed by psychological stress over depression. Despite limited animal models of psychological ...
The effect of stress on depression, its role in triggering the subsequent phases of the disease, and the factors that mediate the stress-depression relationship are increasingly common topics of research in psychiatry and psychology . Currently, depression is understood as a multifactorial disorder. Interacting genetic, biological and ...
In addition, initial presentation with social phobia was associated with a 5.7-fold increased risk of developing major depressive disorder. These associations between anxiety and depression can be traced back even earlier in life. For example, childhood behavioral inhibition in response to novelty or strangers, or an extreme anxious temperament ...
Even in rodent studies, stress has a negative impact: chronic and unpredictable stress (and other forms of tension or stress) have been linked to unusual behaviour and depression symptoms . The depression process and related brain changes, however, have also been linked to the hyperactivity or dysregulation of the HPA axis [ 127 , 130 , 131 ...
Stress may once just have been a kind of executive trophy - "I'm so stressed!" - but recent research suggests it is a key element in developing mental health problems such as depression ...
Anxiety disorders affect nearly 20 percent of American adults. That means millions are beset by an overabundance of the fight-or-flight response that primes the body for action. When you're ...
Maladaptive response to stress results in various physical, psychological, and behavioral negative effects. Negative effects of stress on physical health include increased heart rates, sweating, high blood pressure, and long-term development of the cardiac condition. Psychological effects include the development of anxiety, depression, and ...
In this essay, we have briefly reviewed a selected range of key discoveries that neuroscientific research has made on the topic of depressive disorders in the last decades. ... (2012) Balance of brain oxytocin and vasopressin: Implications for anxiety, depression, and social behaviors. Trends in Neurosciences 35(11): 649-659. Crossref. Google ...
Exercise and improved physical fitness can prevent all of these stress related changes. Long periods of stress can lead to anxiety and depression and often symptoms of anxiety and depression overlap. Exercise is a proven treatment for both anxiety and depression and in many cases it is more effective than currently prescribed medications. Keywords
Essay grade: Good. 2 pages / 821 words. This may be one of the largest silent epidemics the world has ever had. Students and teenagers everywhere are depressed. Up to one in five children show signs of depression or some other mental disorder every year. The worst part is, nearly 80% of the...
Several factors contribute to the development and exacerbation of anxiety and depression in college students. Academic pressure, financial stress, social isolation, and the challenges of transitioning to a new environment are all common stressors that can trigger or worsen these mental health disorders. Additionally, college students may face ...
Narrative Essay about Anxiety and Depression. Everyone has a unique story, each with its hallmarks, learning lessons, and experiences. But despite our differences, we can all relate to having a major challenge in our life. Sometimes it's a stressful job, a medical condition, an accident, and sometimes it's losing a loved one.
Living with depression. A part of managing my depression is accepting it, as with any other illness. It is a lifelong healing journey that requires changes to my treatment plan, patience, and most importantly loving kindness to myself. Learning to understand my feelings, stressors, and triggers has helped me to manage my symptoms.
Depression is a mood-affective disorder that causes a persistent feeling of sadness, loneliness, and starting loss of interest in things. A major depressive disorder or clinical depression is that which affects feeling, thinking, and behavior and can lead to a variety of emotional and physical problems. Depression causes feelings of sadness and ...
Anxiety and Depression. Anxiety and depression are both very common and serious disorders. They affect a wide variety of people in a variety of ways. These disorders have the power to affect a diagnosed individuals daily life (Chen 5). It overwhelms the individual with feelings of sadness and worryness also leading to demoralized attidudes.
Depression is a more complex condition. In addition to unremitting sadness, depression is defined by low mood, apathy, lack of joy (), and inability to concentrate and stay focused.Corpus ...
The team made their anonymized data set publicly available—including self-reports, surveys, and phone-sensing and brain-imaging data—to help advance research into the mental health of students during their college years.. Andrew Campbell, the paper's senior author and Dartmouth's Albert Bradley 1915 Third Century Professor of Computer Science, says that the study's extensive data ...
Financial stress has been proposed as an economic determinant of depression. However, there is little systematic analysis of different dimensions of financial stress and their association with depression. This paper reports a systematic review of 40 observational studies quantifying the relationship between various measures of financial stress ...
For people who received both medication and talk therapy for anxiety or depression; the risk of hospitalization dropped 68 - 75%; the risk of being seen in the emergency department fell 67 - 74%, and the risk of death from any cause was reduced by about 67%.
A study published in the British Medical Journal finds people who consume high amounts of these foods have an increased risk of anxiety, depression, obesity, metabolic syndrome, certain cancers ...
Anxiety and depression are complicated disorders with numerous elements that impact people differently. Teachers and staff must be well trained to deal with these unforeseen events. Understudies coming to college come from various financial foundations, which can prompt an assortment of psychological wellness chances (Li et al., 2021).
Eighteen-year-old Noah Power, who lives in Yukon, Canada, said his struggles with anxiety and depression began when he was about 12 years old. Noah Power, 18, who lives in the Yukon province of ...
The value of short-term goals. The National Cancer Institute estimates that there were nearly 82,000 new kidney cancer diagnoses in 2023. Anywhere from 10% to 50% develop symptoms of anxiety and ...
Aug. 7, 2023 — Chronic pain is often accompanied by depression and anxiety. Experts discuss the relationship between pain, the most common symptom for which individuals visit a physician, and ...
Therefore, long-term untreated depression, anxiety, or stress can have a negative influence on people's ability to operate and produce, posing a public health risk . Theoretical Implications The current study makes various contributions to the existing literature on servant leadership.